Y4 BBN - Central Manchester University Hospitals
advertisement

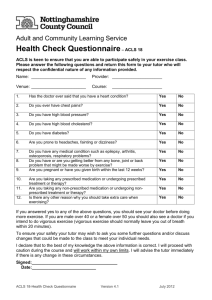
1 University of Manchester Breaking Bad News Course Communication teaching - Year 4 medical students Tutor notes 2011 - 12 Course written by Drs Heather Anderson & Simon Cocksedge Revised June 2011 Simon Cocksedge Index Section Points for all weeks Session 1 Session 2 Session 3 Roles for session 1 Roles for session 2 Roles for session 3 Student handouts Page & notes 2-5 5 6 7 8 - 15 16-23 24 - 31 32 - 35 SPIKES is on page 32 Changed for 2011-2012 in response to student feedback – there is now longer for the group work with SPs in weeks 2 and 3 [roles have 35mins not 30mins] 2 Breaking Bad News: year 4 Communication Aims of the course This course runs over three half day sessions and is the major communication teaching for Year 4 medical students. The aims are: Week 1- life changing events To review basic communication skills To introduce topic of BBN and SPIKES – focus: life changing events/conditions Week 2 – life threatening events To practise with more challenging situations – focus: life threatening conditions, patient not expecting such news Week 3 – handling strong emotions; relatives To learn how to deal with strong emotions e.g. anger, To learn how to cope with relatives in ‘bad news’ situations Clinical topics in the course Some students ask to know the clinical topics covered each week – we send these to them in advance and ask them to prepare to discuss these topics: Week 1 Hypertension Multiple sclerosis Rheumatoid arthritis Diabetes Ankle fracture Week 2 Myocardial infarction Breast carcinoma Oesophageal carcinoma Uterine carcinoma Bowel carcinoma Week 3 Rectal carcinoma Chronic obstructive airways disease Breast carcinoma Pancreatic carcinoma Myocardial infarction 3 Guidance on running the small group sessions for all weeks Before the first SP arrives Distribute sticky labels to be used as name badges - ask each student to write the name that they would like to be known by during the session! Make sure that the chairs are in a circle and that you are sitting in the circle so that you give the sense of being collaborative. Explain what will happen in the session. That is you will be visited by 3 simulated patients; there will be three interviews and time to give feedback to the interviewer. Explain that as this is a safe environment the SPs won’t be emotionally damaged by the content of the session. Preparing for the role play with the SP Either ask for a volunteer to conduct the first interview or allocate people for all three interviews to save time later in the session. Give the student conducting the interview the doctor’s role notes - while he/she familiarises themselves with the role, you read the role out to the group. Check if there are any questions or points of clarification – the students may need to share their knowledge of the illness/condition described in the role. Feedback from previous tutors has been that when students are unclear about the required medical knowledge that they are unable to practice and develop their communication skills. You may need to spend 1-2 minutes discussing the condition to ensure the student feels equipped to explain it to a patient. To ensure students don’t passively watch, consider allocating tasks for giving feedback. For example, you could ask pairs of students to focus on aspects of SPIKES or on different question styles, use of empathy etc. Ensure observers make precise notes to enable specific & focused feedback. Always speak to the SP briefly before he/she comes into the room. You may possibly suggest what you would like the focus of their feedback to be or how you want them to play the role [particularly in week 3]. Some students will wish to increase the emotional intensity demonstrated by the SP. Consider negotiating this with your group. Pause button/rewind facility Tell the students that they may use an imaginary ‘pause button’ at any time, and this is positive as it shows they are really thinking about what they are doing and the effect of their intervention with a patient. It means they can temporarily come out of the interview to talk with the group about what to ask next or which areas they may want to pursue. It is important that you facilitate group discussion, wherever possible, rather than you making the suggestions Reinforce that using the pause button [as often as necessary] is a positive thing to do, showing that students want to think about the issues/questions. The student can also rewind the interview and try a different question or approach. The SP will be ready for this possibility. 4 The interview Check that the interviewer is clear about how he/she is going to start. If the student is not sure, have a brief group discussion to pool ideas. Possible questions for you to ask the student at the beginning are: ‘How are you going to start?’; ‘What help do you need before starting?’; ‘How are you going to explain…?’ The interview should last no more than 6-8 minutes. You can bring it to a close or pause it if necessary. Keeping to the overall time schedule is crucial. Please ensure that the students use SPIKES – particularly that they check the patient’s concerns and perceptions about what may be wrong with them. You could ask other students to have a go at a section of an interview or even ask students to try something different. Rules of feedback We generally use Pendleton’s Feedback Rules. Observers briefly clarify points of fact Interviewer reflects on what went well Group members state what went well, giving specific examples Simulated Patient in role contributes feedback Interviewer state what might be done differently Group members, then SP in role, state what might be done differently SP taken out of role formally, and asked to comment out of role. Interviewer notes the learning points There are other possibilities in terms of how feedback is managed including asking the interviewer what they would like feedback on. The group feedback is captured by another member of the group who records this on the Student Feedback form. Please encourage role playing students to write a reflection & develop an action plan from this to keep this in their portfolio. Finishing the session Go around the group and ask everyone for one learning point that they will take away from the session. Emotional Health Warning Occasionally, a student may become upset during the session. This is generally as a result of the themes of the session resonating with their own lives. If a student wants/needs to leave the room, then please let them go but perhaps ask one of their friends to go and act as support. Also, try to see the student yourself at the end of the session. You could offer support from either yourself or another member of the tutor team. It would be helpful if you could let the Lead Tutor or one of the site administrators know the name of the person concerned. You could also suggest that the student contacts the University Counselling Service: Tel: 275 2864; www.staffnet.manchester.ac.uk/theguide/ or the pastoral support team at your site. Click on ‘student support and services office’ for details of counselling service. 5 BBN Session 1 Aim: To review basic Communication skills To introduce topic of BBN and SPIKES – focus life changing events/conditions Materials for this session: SPIKES handout, pre-evaluation sheet if used WHEN WHAT WHO NB Get students to sit at the front 0.0 Lead Introduction and complete initial evaluation sheet, if used in Tutor lecture theatre 15min 65min 80min to small group 90min 180min Aims of course Introduce tutors and simulated patients Outline programme for the session Mention possibility of student life problems (to raise the issue that this course deals with difficult issues, which may touch on current problems in students’ personal lives). Students may wish to discuss these with tutors during/after this course or with others e.g. student counselling service – see pg 4; exceptionally, individual students may need to limit their role-playing in the groups. Brainstorm of communication skills learnt so far Write up on board: E.g. open/closed questions, room arrangement, body language, eye contact, summarising, reflecting, pausing Talk on breaking bad news: to include giving out/discussing the student handout (SPIKES) and mentioning the rules of feedback Role play by tutors with debriefing Tutor & SP run a brief role play (7 mins max) - NB this is a diagnosis of hypertension. They stay on the stage while another tutor facilitates student debrief using the rules of feedback– on stage participants model the Pendleton feedback rules and students need to be told to make notes and be specific with their feedback Identify tutors/groups/ venues – emphasise that punctuality is crucial. Coffee break 15 mins Group forming Discussion of format/name badges/order of role-playing SPs visit groups for 90 mins (3 roles x 30 mins each). N.B. check role no. and order allocated to your group on the detailed schedule Student role plays with SP for six mins, and then is debriefed by the group using the rules of feedback. Capture group feedback on Student Feedback form, encourage role-playing students to develop an action plan/reflection for their portfolios. Must run to time. Students depart when finished. Tutor/SP debriefing- venue site specific Lead tutor Lead tutor TUTORS TUTORS tutors 6 BBN Session 2 Aim: To practise with more challenging situations – focus: life threatening conditions, patient not expecting such news WHEN WHAT WHO 0.00 Introduction Lead tutor lecture Aims of session theatre Outline programme for the session Talk recap of SPIKES, & skills learnt so far, talk Lead tutor 5min on reactions, importance of hope (student LT handout on hope), more challenging BBN and role of palliative care team 40min 55min in small groups in rooms 165min 180min Role play by tutors with debriefing Front of house role play- wife Mrs. Liz Clarke, arrives at hospital, husband, Jim, has died Tutor & SP run a brief role play (7 mins max) and stay on the stage while a third tutor facilitates the students to give feedback structured on SPIKES(See back of Tutor notes) Identify groups/tutors/venues and break for coffee – 15min break Into groups – 5mins re-forming group then 3 role-plays of 35 mins each. Capture group feedback on Student Feedback form, encourage role-playing students to develop an action plan/reflection for their portfolio. There is a student handout for this session on ‘The importance of hope’ see page 34. Please refer to this for at least one of the scenarios. Students should also have the SPIKES handout from the last session to refer to. NB check role no. and order allocated to your group on the detailed schedule Debriefing in small groups Discussion on things learnt so far – each group member to identify one thing. Please use this time to encourage students to reflect on what this learning means for them individually. Invite students to share examples of their own experience of bad news [seen as a student or in their own lives], relating it to this course. Help them to think about the doctor as a person as well as a professional. How do doctors manage difficult professional situations which may overlap in their personal lives? Eg a doctor whose father has terminal lung cancer telling someone they have ca bronchus. Reflect on what coping/support doctors may need. Students depart - Tutor/SP debriefing TUTORS TUTORS 7 BBN Session 3 Aim: To learn how to deal with strong emotions e.g. anger, To learn how to cope with relatives in bad news situations Materials for this session: relatives & anger handouts, evaluation sheets WHEN WHAT WHO 0.00 lecture theatre 5 min Lecture theatre Introduction Aims of session Outline programme for the session Brief recap of SPIKES, & skills learnt so far, talk on anger and strong emotions Lead tutor 40min 55min small groups in rooms Lead tutor Role play by tutors with debriefing. Patrick/Patricia son/daughter of Maud Thompson (patient) Tutor & SP run a brief role play, a third tutor facilitates the interaction – pauses role play and asks for advice from students ‘What could you say/do now?’ Debrief comments at end Student handouts: Anger and relatives Identify groups/tutors/venues and break for coffee – 15mins Into groups - 5 mins reforming group then 3 TUTORS roles with SPs @ 35 min. each Capture group feedback on Student Feedback form & encourage each student who role-plays to develop an action plan/reflection for their portfolio. NB check role no. and order allocated to your group on the detailed schedule It is important to practise concluding an interview at least once during the three sessions with your group. It is vital to do this today perhaps do it by re-running the scenario. 165min 180min Debriefing in groups TUTORS Discussion on things learnt so far – each group member to identify one thing. Continue discussion from previous week - doctor as person & professional, and support for doctors. If possible, pick up the issue about how you manage anger & confront racism from the talk and chat this through with the group Get students to fill in evaluation sheets, collect and return to your site administrator. Students depart Tutor/SP debriefing in start room 8 SP Role Patient’s Name Paul/Paula Course BBN Winters Setting Neurology clinic Session Role Age Sex Other Information 1 1 30-55 M/F Non spectacle wearer preferable You are a publican. Past For several months you have felt a bit weak and run down. This all happened after a viral infection, which made you feel unwell and dizzy with poor vision. Your optician said you did not need glasses. (If you wear spectacles your prescription is OK.) This all quickly settled. Since then you have felt a bit weak. You keep having accidents and drop things. Your partner has started to call you clumsy. About 6 weeks ago you were less well again and people in your pub thought you'd had too much to drink because your walking was poor. Nobody believed you had only had one drink that day! You were concerned and thought it could be stress but at the back of your mind is the possibility of a brain tumour. Your GP arranged for you to see a specialist at the hospital. You were admitted for 6 days and had lots of tests including blood tests, x-rays and a brain scan. You were discharged 2 weeks ago. You have come back to the neurology clinic for the results, but the specialist, who you saw last time is on holiday. Role player task What is your name? Work out your family names e.g. wife or any children. What is the pub called? You are worried about yourself because you slipped on the ladder to the cellar and realise that you could have had a serious accident. Your partner does not know this. What could you be stressed about? If you had these symptoms how would you feel?. 9 Doctor Role Patient’s Name Paul/Paula Winters Setting Neurology clinic Course Session/Role BBN 1/1 You are a ST1. Situation. This patient, who you have not met before, comes to the clinic alone. (Your consultant is on holiday.) His/her partner is running the pub that they have together. For several months he/she has been unwell. This illness started after a viral infection and was associated with dizziness and blurred vision. He/she has felt tired since, has become clumsy - dropping glasses, and his/her legs are weak. People have thought he/she was drunk when he/she was not. One of the GPs arranged for him/her to be admitted to hospital for tests. He/she was discharged two weeks ago. He/she has come back for the results. You read through the notes and see that the MRI scan shows that he/she has demyelination indicating multiple sclerosis. You need to explain the diagnosis, but he/she will then see the nurse specialist to explain the next steps. Role player task What are you going to say? How are you going to start? 10 SP Role Patient’s Name Olive/Clive Dewar Setting GP surgery Course Session Role Age Sex Other Information BBN 1 2 30+ M/F You have run a bakery & confectionery shop with your marital partner for 15 years. It is very successful and now, financially, you do not have to struggle at all. You have four employed staff, but you do most of the baking, still getting up at 5am to start work in the kitchens. Past: You made the fancy cakes and chocolates while your partner was ill with flu. So you had to manage your job and also make the fancy breads that week. Following this, (4 weeks ago), you have had stiffness of the hands. After the first week they both became red, puffy and swollen. You could not bake any more. The joints were swollen and too stiff to move without pain. You attended your GP surgery 3 weeks ago. He/she gave you ibuprofen 400mg every 8 hours and this has helped. The redness and swelling has gone, but your hands remain somewhat stiff, especially in the morning. The GP did blood tests and sent the samples away for analysis and arranged for X-rays of your hands. Now you go to the surgery for the results and to get more tablets. Another problem is indigestion. The doctor said that the tablets may cause indigestion as a side effect. Role player task. Build up a social and work picture. How long do you think you'll be off work? You are supervising at the moment as you cannot do any manual work. You think you may have developed an allergy to the yeast and flour. You must not forget to get more pills and tell him/her about the indigestion. 11 Doctor Role Patient’s Name Olive/Clive Dewar Setting GP surgery Course Session/Role BBN 1/2 You are a GP. Situation This patient came to your colleague three weeks ago with a one week history of stiffness of the hands. Then over the weekend they had become red, puffy and swollen. S/he could not bake in the cake/confectionery shop that s/he runs with his/her marital partner. The joints were swollen and too stiff to move without pain. Your colleague suspected rheumatoid arthritis and did blood tests for this and arranged for X-rays of the hands. He/she also prescribed ibuprofen 400mg every 8 hours. Role player task. You have not met this patient before (your colleague is off sick). The tests confirm rheumatoid arthritis. How are you going to tell him/her? The diagnosis will have possible implications regarding his/her job. You plan to refer to a specialist if s/he is not back to normal. 12 SP Role Patient’s Name Arthur Morris Setting patient in bed on orthopaedic ward Session BBN 1 Role Age Sex 3 25-50 M Course You are a mature student – make up a course you are on. You work part-time (as a store man in a warehouse) to keep some income coming in while studying. Yesterday, whilst doing your temporary job, you were putting some products on a high shelf. The ladder you were using slipped and you fell directly onto your feet about 14 feet below. You were in agony and were rushed to hospital. At casualty Xrays showed a compound fracture of the ankle and calcaneum. You have been put into a plaster of paris splint and have had pethidine. You are feeling a bit better now. You are due to go to Cyprus in two weeks time- make up a reason - could be for a sports tournament, student exchange, visit relative. You are a keen sports enthusiast and play in a competitive team. Sport is a big part of your social life. Role player task Build up a social picture - names parents, siblings, partner, hobbies. What sport(s) and what position do you play? Think about how you would feel having a fractured ankle - how will it affect you now and later? What about your trip to Cyprus? What do you need to know? 13 Doctor Role Patient’s Name Arthur Morris Setting patient in bed on orthopaedic ward Course Session/Role BBN 1/3 You are one of the orthopaedic F2 doctors. Situation Your colleague (who is not here today) saw Arthur Morris yesterday evening. He is a mature student who has had a fall doing a temporary job (to help pay his way as a student). He has a compound fracture of the ankle and calcaneum. This is a fracture in which broken bone fragments lacerate soft tissue and protrude through an open wound in the skin. This is a bad fracture and may well heal poorly. At the X-ray meeting this morning, the prognosis was felt to be poor, and your consultant recommended surgery. This will involve plating. Long term, the foot will be stiff and sports etc. will be difficult. He will probably walk with a limp and competitive sport is likely to be out. He will need intensive physio for several months after the dressings are removed. Role player task You have not met this patient before. You need to explain the position. How do you start? 14 SP Role Patient’s Name Lesley/Leslie Hall Setting GP surgery Course BBN Session Role Age Sex Other Information 1 4 20 - 40 M/F You are a mature student. You live at home with your parents. Past You have had some symptoms of cystitis for about three weeks in all. You initially phoned the GP and a course of antibiotics was prescribed after your telephone call. You were asked to report back one week later if you were no better. You were feeling a bit better but still had some urinary symptoms. The fishy smell in your urine had gone, but you still had to pass urine frequently, including at night. You attended your GP’s practice nurse who did a stick test of your urine and took blood for tests. Now You go back (two days later) for the results, from the GP. You have been drinking lots to try and flush the kidneys out. It has been hard to concentrate because you feel tired and intermittently feverish. Role player task. Build up a social picture - names of parents, siblings, partner, hobbies. Think how you would feel about tiredness and your studies. How has the urinary frequency affected you? You really think that you are run down with exams coming up and it is just a bad attack of cystitis. A thought you dismissed was a sexually transmitted disease but you haven't had sex recently and don't really believe this is a problem. 15 Doctor Role Patient’s Name Lesley / Leslie Hall Course BBN Setting GP surgery Session/Role 1/4 You are a GP registrar Situation Leslie / Lesley is a mature student who has been registered with the practice all his/her life and lives locally with his/her parents. You have not met him/her before. He/she had symptoms of cystitis three weeks ago. After a telephone consultation, you initially prescribed a course of antibiotics, and asked the patient to report back one week later if they were no better. He/she presented with persisting frequency to the practice nurse 2 days ago. Dipstick urine showed increased glucose, so MSU, FBC, B/S and U&E were performed and he/she was asked to see you today for the results. . The blood sugar is 36mmol/l; U&E, FBC & MSU normal. He/she appears to have diabetes mellitus and you need to refer him/her urgently to the hospital to the Diabetes Centre. Role player task How will you explain the diagnosis of diabetes? How will you start the conversation? 16 SP Role Patient’s Name Sarah Page Setting One stop Breast Clinic Course Session Role Age Sex Other Information BBN 2 1 30 -75 F You are attending the one stop breast clinic. The doctor has taken brief details and examined you. You have had a mammogram and breast biopsy, all this morning. Past You were having a bath three weeks ago when you noticed that you had a lump in your breast. It is not painful and is about an inch in size. It feels hard. You are aware that this could be something serious e.g. a tumour. You attended the GP surgery and he/she arranged an appointment at the one stop hospital clinic where you are now. You have been told the results will be given to you today. You didn’t know that’s what happened nowadays – all so fast. Now: Role player task. Build up a picture of your family, job, children’s names etc. You are quite tuned into health problems. You know most breast lumps are not cancers and part of you wants to know if this one is. You suspect it may be because the "Readers Digest" article about cancer and all the TV programmes say that painless lumps often are cancers. You are also aware that treatment is usually surgery and these days it may not be necessary to have the whole breast removed. On reflection, you are not sure you want the results today (you came alone) and this is all happening too fast. If asked, please say you would prefer your husband with you but you decide [after some discussion with the doctor/student] that you will hear the news today. 17 Doctor Role Patient’s Name Sarah Page Setting One stop Breast Clinic Course BBN Session/Role 2/1 You are the one of the breast clinic registrars. Situation Sarah Page found a painless breast lump three weeks ago. Her GP has referred her to the hospital. She was seen and examined by your colleague (who has had to leave) earlier this morning. Following that, she has had a mammogram, ultrasound and breast fine needle aspiration (FNA) and core biopsy. The results of her tests are now ready. The lump is hard and about 2cms big. Clinically cancer is suspected, and this has been confirmed by the mammogram and FNA. The FNA report reads MICROSCOPIC DESCRIPTION: Malignant cells present. -C5 malignant. She will see the consultant shortly to discuss the next step. It is likely to be lumpectomy and axillary surgery followed by radiotherapy. Other treatment (e.g. chemotherapy, hormone therapy) will be decided at the MDT post surgery. You need to inform her of the diagnosis and have an initial discussion. Role player task Do you want anyone else there? Decide on the names of colleagues who will be involved in her care (radiologist, surgeon) How will you start the conversation? (fine needle aspiration gives a diagnosis in 1-2hours) 18 SP Role Patients Name Setting Ian/Jan Walker Hospital outpatient clinic Course Session Role Age Sex Other Information BBN 2 2 35 -49 M/F You are a 42-year-old social worker living with Rose/Ron. Past You have a six week history of indigestion and more recently, some loss of appetite, heartburn and soreness on swallowing. You have begun to lose a few pounds in weight. You went to your GP a week after it started as you had never had indigestion before. The GP prescribed ranitidine (stomach tablet twice a day). A week later you were worse so returned to your GP and he arranged a specialist appointment for investigations. The appointment came through very fast. The specialist arranged a gastroscopy and tests for a special germ associated with stomach ulcers, which you had done last week. Your mother had a hiatus hernia. At worst you think it is a stomach ulcer and that you will need tablets. You would be apprehensive about surgery but you understand that surgery is an old-fashioned treatment for stomach ulcers. Now You had your tests last week and have come back for your results. Role player task Build up a social picture. You have no children. What are your hobbies? You last worked yesterday. Your partner is a ward clerk at the local hospital. You are looking forward to your holiday in the USA in three weeks. You have never been ill in your life How would you feel with these symptoms? How do you feel coming for the results? What would you be worried about? 19 Doctor Role Patients Name Setting Ian/Jan Walker Out-patient clinic Course Session/role BBN 2/2 You are the medical F2 doctor Situation Ian/Jan is a social worker with a six week history of dyspepsia and anorexia. He/she has lost a few pounds in weight but continues to work. He/she has some soreness on swallowing. He/she had a gastroscopy last week and tested negative for H Pylori. There was evidence of oesophageal reflux and an area of redness and ulceration in the lower oesophagus was biopsied. The biopsy report says he/she has adenocarcinoma of the oesophagus. Role player task This person is very young ( late 30s early 40s) to have oesophageal cancer and you are shocked when you see this report on their notes. You need to explain the diagnosis to him/her. You may wish to discuss the immediate plans: He/she needs a pre-operative staging CT scan. This can be done tomorrow. Your plan is to offer an assessment laparoscopy in the next few days. He will need follow-on specialist advice (?chemotherapy etc.) How are you going to explain this unexpected news? NB carcinoma of oesophagus is serious [very poor 5 year survival rate] 20 SP Role Patient’s Name Janice Hand Setting Hysteroscopy Clinic Course BBN Session 2 Role Age Sex Other Information 3 50+ F You You have had no periods for some years and were surprised to have a bleed. Your menopause has caused no problems and you think you’ve been quite lucky with this compared to other women. You have an energetic and satisfying sexual relationship You had some unexpected vaginal bleeding and attended your GP, Dr Johnson, about it last week. She did a smear test and vaginal examination. She referred you to the hospital to see a gynaecologist. Now You have come to the gynaecology clinic. You are anxious as your appointment came through so quickly. When you saw your GP you did not discuss what the cause of the bleeding might be. You have had a pelvic and internal scan and a hysteroscopy (a small telescope passed through the cervix or neck of the womb to look at the lining of the womb) and they took a sample to test/biopsy. You have got dressed and will now discuss the findings with the doctor. Role player task. Build up a social picture - partner’s name, jobs, family & hobbies. Your elderly relative told you she had some bleeding after the menopause and she was given some hormone cream. You hope that this will be the treatment for you as you do not like hospitals. 21 Doctor Role Patient’s Name Janice Hand Setting Hysteroscopy Clinic Course Session/Role BBN 2/3 You are a FY 2 in O&G. Situation Janice was referred by her GP, one week ago, with a history of postmenopausal bleeding The scan shows a normal sized uterus with thickened endometrium measuring 21mm. Your consultant has just performed a hysteroscopy which has shown a suspicious looking polyp at the fundus. Biopsies were taken. Unfortunately, the consultant has been called urgently to theatre and you have been asked to explain the findings to Janice. Until you have the histology results you cannot give a diagnosis.. Role player task You have not met this patient before. You need to explain the position. How are you going to tell her? How do you start? Note: If the histology confirms malignancy she will need an MRI scan to decide further management (surgery or radiotherapy). 22 SP Role Patients Name Setting Mr Alfred/Miss Ethel Brown Bed on ward Course Session Role Age Sex Other Information BBN 2 4 65+ M or F You are an elderly person, who was admitted to hospital with tiredness, weight loss, constipation and poor appetite. Past You have been on this ward now for two weeks. The staff are all wonderful, and they are very kind to you. You have been unwell for 2 months and your tests have shown a bowel cancer and you already know this. You are no better, in fact you feel worse, have no appetite and you have lost more weight. Now You are down today and feel worse. The doctors did not speak to you on the ward round as you were half-asleep, but you saw them slip by. You know that you have cancer and you are starting to realise that you will die because of this. You are not scared of dying but don't want to be incontinent or lose control of your mind / bowels (like your mother did. You nursed her at home). As you have not made a will, by law your house and belongings will go to your brother who you haven’t seen for years, but you want it to go to your nieces who have been so good to you. The young house officer has been looking after you. He/she comes to see you and have a chat. You have had a good and friendly relationship. He/she sits down and greets you. Make sure to ask for advice on this. Role player task – for the students to realise that some patients do want to talk about dying, and want a sympathetic and straightforward approach Build up a social picture - names brother and nieces. What were your mother's problems when she was dying at home and you were looking after her? You are usually a chatty, friendly person, but today you are grumpy and down. You feel the doctors have avoided you when you wanted to talk about what is really going on re your illness and prognosis. You desperately want to talk about how you feel and if you are going to die. You will ask the student about this almost as soon as he/she has sat down. You are not embarrassed to talk about death, you see it as the final phase of life and would like to have some dignity. What are you going to say? 23 Doctor Role – please check gender of role player with your tutor Patients Name Setting Mr Alfred or Miss Ethel Brown Bed on ward Course Session/role BBN 2/4 You are a surgical F1 doctor Situation. Mr or Miss Brown was admitted two weeks ago for investigation. This has shown bowel cancer [stage IV – metastatic] which is terminal. Mr or Miss Brown has anorexia, lethargy and weight loss and is deteriorating quite quickly and is not fit for surgery. At the MDT meeting 3 days ago, it was decided no further treatment should be offered and your consultant told the patient this news 2 days ago on the ward round. Mr/Miss Brown is dying but has not spoken to you about this or about having cancer. The Discharge Planning Team is liaising with social services and the GP/district nurses to arrange support at home - this will include assistance with personal care [toileting and bathing] and pain control. Mr/Miss Brown has no children and lives alone. You have met the two young nieces who are very supportive and visit regularly. You like Mr/Miss Brown, s/he is chatty and easy to talk to. S/he appears to like the nurses and appreciates the attention given in hospital. The ward round has just finished. It did not stop at Mr/Miss Brown’s bed as s/he appeared to be asleep and there has been no change anyway. S/he is now sitting up and you pop over to have a chat. Role player task You are feeling quite cheerful. You are comfortable in Mr/Miss Brown’s company. You go and sit down and ask how s/he is today. You notice s/he is a bit down. 24 SP Role Patient’s Name Timothy Taylor Chris Taylor, son Role or daughter of above Setting The hospital ward office Course Session BBN 3 Role 1 Age Sex Other Information Up to 50 M/F Past Your father Timothy Taylor has been attending the gastro-enterology clinic for three years with troublesome indigestion and more recently weight loss. A gastroscopy 6 months ago showed a small ulcer, which was treated. The symptoms improved, but over the last two months he has been losing weight and has had more indigestion pain, backache and nausea. Now Your father had a clinic appointment this week and they decided to admit him the next day for more tests (two days ago). He has just told you that he has incurable cancer of the pancreas, which has spread to the liver. You are devastated. You stay a while then leave Dad saying you are going home. Your father looks awful, pale and uncomfortable. You can’t believe how ill he looks. How can this be? He’s been attending the hospital clinic frequently. You can’t understand what is happening or why. You are confused and upset. You are angry with the situation and think the cancer was missed by the gastroscopy 6 months ago. Cancer cannot come and make someone so ill in just 2 months. You ask to see the doctor. Role player task What is your job, marital status? What are your main concerns? You are angry that your father told you the diagnosis and you were unprepared for this. Shouldn’t the staff have told you first? Should he have been told at all? What is happening? You are frightened that at this rate he will die soon and you feel quite shocked and shaky inside. NB Please be prepared to adjust the level of anger depending on advice from the group tutor immediately before you join the group. Students feedback that they want to practise talking with really angry/challenging patients/relatives. 25 Doctor Role Patient’s Name Timothy Taylor Interviewee Chris Taylor, son or daughter of above Setting Hospital ward office Course BBN Session/Role 3/1 You are the medical F1 doctor Situation Mr. Timothy Taylor has been attending the gastro-enterology clinic for three years with troublesome indigestion. A gastroscopy 6 months ago showed a small gastric ulcer, which was treated with omeprazole. The symptoms improved, but for two months he has lost weight and had more indigestion, backache and nausea. He was admitted from clinic two days ago. A scan shows incurable pancreatic cancer with liver metastases and repeat endoscopy shows a tumour infiltrating the duodenum from the pancreas. The gastric ulcer has healed. The patient asked for and has been told the diagnosis. It was his wish to tell his son/daughter. Mr Taylor has deteriorated in the last 24 hours and may die within a few days. You have been asked to see the son/daughter of this patient. The nurse involved explains that the relative is quite distressed. Role player task Who will be there? How will you start? 26 SP Role Session BBN 3 Role 2 Age Sex Other Information Up to 55 M/F Course Your name Patient Setting Susan/Simon Broadhurst Mrs Broadhurst [your mother Ward 7 Dr’s office Situation Your mother (age 77) was rushed into the hospital casualty department tonight with a tightness in her chest and severe breathlessness. She saw her doctor about two months ago with chest pain, which was put down to possible gallstones and she is waiting to see the specialist. You visit the hospital and mum is now on ward 7, sleeping but she looks very pale. You ask the nurses what has happened. The nurse is not looking after your mother but says that she will ask the doctor, who is attending your mother, to come and talk to you. You are invited into the doctor's office. Role player task Build up a picture of your family, job etc. Your mother looks awful. You are naturally worried and upset You want to know what the problem is, why the GP did not diagnose it before, and why she is not on the CCU (Coronary Care Unit) if this is a heart problem – you thought people with heart problems went to CCU. You are firm, moderately angry, and challenging to the doctor about these things; you want to know the answers – you don’t mind that she isn’t on CCU but you want to check that she is having the best care [please note that people who are stable often don’t go to CCU if they have a mild heart problem so not being on CCU can be seen as a good thing!]. You are also anxious, talking a lot and ‘in the doctor’s face’. NB: Please be prepared to adjust the level of anger depending on advice from the group tutor immediately before you join the group [perhaps from 1 = mildly irritable to 10 = violently angry!]. Students feedback that they want to practise talking with really angry/challenging patients/relatives. 27 Doctor Role Interviewee’s name Susan/Simon Broadhurst Patient Mrs Broadhurst [mother of Susan/Simon] Ward 7 Dr’s office, you are the Doctor on call Setting Course Session/role BBN 3/2 You are the medical F1 doctor Situation Mrs Broadhurst (age 77yrs) was admitted through casualty tonight with chest pain which had been put down initially to gall stones. You saw her there and her tests have shown that she has angina. She is stable at present on therapy and sleeping after diamorphine for pain. Her BP is normal [124/72], pulse regular 74/min. She is being monitored on ward 7. Her son/daughter has asked to see someone and is in the doctors’ office. Nurse tells you that Mrs Broadhurst is a widow, and that she has given permission for information to be given her son/daughter who is named as her next of kin. Role player task How are you going to start the conversation? Note: It maybe appropriate for patient to be on ward 7 if he/she is stable and would only need transfer to CCU if she developed further problems or a myocardial infarction 28 SP Role Your Name Setting Patient Louise Brooks GP surgery Steve Brooks, your deceased husband Course Session Role BBN 3 3 Age Sex Up to 60 F You are Louise Brooks, wife of Steve, who died on ITU 3 days ago. Past Steve had had severe chronic bronchitis (or obstructive airways disease) for some years for which he was under the care of Professor Woodcock at Wythenshawe. His condition had worsened in the last four months and despite many warnings, he continued to smoke. He was able, with considerable understanding from colleagues and the headmaster, to continue his job as the live-in caretaker for a school in Bredbury near Stockport, until his final illness which started about three weeks before his death. You have no children and no family live nearby. Steve got steadily worse at home, despite two visits from his GP and treatment with steroids/nebuliser which normally helped. He was very poorly when eventually admission was arranged. There was a three hour wait for a bed and the ambulance then took another hour to arrive. When Steve did get to Stepping Hill Hospital, Stockport, one of the doctors who was rushing around treating him commented that he could not understand why Steve had not been admitted sooner. Steve was sent up to a ward but within 12 hours deteriorated further and another specialist said he needed to go onto the Intensive therapy Unit (ITU). Unfortunately, there were no beds on ITU at Stepping Hill, so he ended up going to ITU in Bolton, 25 miles from Stockport and 35 miles from home, where he died 12 days later. Getting to Bolton was a nightmare for you. Now Your usual GP, who visited Steve twice pre-admission and arranged admission on the second visit, is on holiday for the next 3 weeks. You have arranged to see another doctor, who you haven’t met before, to express your anger about: The delay in arranging the admission – why was he kept at home so long? – The hospital doctor obviously felt he should have gone in sooner. About the wait for a bed and then an ambulance About the lack of ITU beds at SHH You want the wording on the death certificate explained – it says: Cause of death 1a bronchopneumonia 1b obstructive airways disease and emphysema Role play issues: problems of travel to Bolton; nowhere to live now Steve is not caretaker. Please be quietly angry initially and prepared to be sad [about the loss of Steve] if the opportunity arises. NB Please be prepared to adjust the level of anger or grief depending on advice from the group tutor immediately before you join the group [perhaps from 1 = mildly irritable to 10 = violently angry or extremely upset]. Students feedback that they want to practice handling strong emotions. 29 Doctor Role Patient’s Name Steve Brooks (deceased) Mrs. Louise Brooks Interviewee Setting Your GP surgery Course Session/Role BBN 3/3 You are a GP near Stockport. Mrs Louise Brooks, who normally sees one of your partners [now on holiday for 3 weeks], has booked to see you 3 days after the death of her husband Steve. Situation Steve had severe chronic bronchitis (or obstructive airways disease) for years and was under the care of Professor Woodcock at Wythenshawe. His condition had worsened in the last four months but he continued to smoke despite many warnings. Your partner saw him 3 weeks ago with another exacerbation of OAD, but Steve did not respond to treatment which usually helped (antibiotics, steroids, nebuliser). Five days later, on a second home visit, he was admitted to Stepping Hill Hospital, Stockport [your DGH]. He died on ITU in Bolton 12 days later. This is your second day back at work after your holiday. You have had a brief fax from Bolton Hospital saying that Steve died 3 days ago but no cause of death was given. NB He was presumably transferred to Bolton due to lack of ITU beds at Stepping Hill. How are you going to start this conversation? 30 SP Role Your Name Setting Patient George/ Georgina Martin Hospital outpatient Clinic Your mother Mrs. Edith Martin Course BBN Session 3 Role 4 Age Sex Other Information Up to 60 M/F Setting - hospital outpatient clinic - you ask to speak to the doctor whilst mother is having blood taken Your mother Edith lives alone. She is fairly well - her arthritis has slowed her down a bit, but she still cooks and shops for herself. She is very independent and looks after herself. She does not drive so you have brought her to the hospital today for an out patient appointment. You are very fond of your mother and wanted to bring her to the clinic. You run your own business i.e. you are self-employed. She found a breast lump (you haven't seen it) and her GP suggested that she saw the breast specialist. She had tests done one week ago - a mammogram and a biopsy. You have come for the results. You ask to see the clinic doctor in the hospital before he/she sees your mother. You are worried that she may have breast cancer and think that she wouldn't cope and would give up. You do not want the doctor to tell her it is cancer. Role player task What is your name? Why won't mum cope if it is cancer? List two or three reasons for this belief. What are you going to say to the doctor? You have asked to see the doctor whilst your mother is having some blood tests. The clinic doctor is not the one you saw before. Although you don’t want mum told, you must be prepared to compromise with the doctor/student after you have tried to manipulate the doctor/student to get your way. 31 Doctor Role Patient’s Name Mrs. Edith Martin Interviewees George/ Georgina name Martin, son or daughter of above Setting Hospital outpatient Clinic Course BBN Session/Role 3/4 You are the F2 doctor in the breast clinic. Setting - hospital OP clinic – son/ daughter has asked to speak with you Mrs Edith Martin is an elderly lady who lives alone and is attending clinic for the results of tests following her first appointment last week. The referral letter from her GP stated that he suspected breast cancer. She had tests done last week, results now in: a mammogram which shows an 8cm breast mass and a breast biopsy confirming cancer. The consultant, who is on holiday today, has written in the notes ‘Too big for surgery in first instance. To start tamoxifen and reassess in 4 weeks’ She is an independent lady with full mental capacity who manages well and looks after herself despite having arthritis. Today, she is having some blood tests. Her son/daughter has asked to speak to a doctor and the nurses have asked you to see her son/daughter. The consultant, who is on holiday today, has written in the notes ‘Too big for surgery in first instance. To start tamoxifen and reassess in 4 weeks’ (THE DIAGNOSIS HAS BEEN SHARED WITH THE PATIENT OR RELATIVE) She is an independent lady who manages well despite having arthritis. Role player task You have no idea why s/he wants to see you. You were not in this clinic last week. How are you going to start the conversation? 32 SPIKES - a protocol for breaking bad news Breaking Bad News - handout week 1 S Setting and listening skills setting: physical space; privacy; same level, no physical barriers, bleep off, avoid interruptions, clarity on time available, listening: body language; eye contact; open questions; pauses; silences; nods; smiles, reflecting, clarifying, use of touch may help if touch a non-threatening area ( arm, forearm) and you and the patient feel comfortable P Patient’s perception of the condition and its seriousness: - ask patient what he/she knows/suspects already, listen to their response to gauge comprehension, is there a mismatch between medical information and their perception? I Invitation check if the patient wants to know details of diagnosis and/or treatment. ‘Are you the sort of person who..?’ K Knowledge give the facts in small chunks using suitable language i.e. the step approach, start at the point the patient is up to, check understanding at each chunk, respond to the patient’s reactions E Explore emotions & empathise give an empathic response by identifying the emotion, identify the cause and respond in a way that shows you have made a connection between the two e.g. ‘I can see this is unexpected news that has shocked you.’ This skill helps the patient to begin to come to terms with the news. S Strategy and summary suggest a strategy based on the medical facts and the patient’s expectations; assess the patient’s response; agree a plan summarise the main points; check if this agreed and if there are any omissions; agree a clear contract for the next contact RECOMMENDED READING Baile W, Buckman R et al. SPIKES - a six step protocol for delivering bad news. Oncologist 2000; 5[4]: 302-311. Available online via theoncologist.alphamedpress.org Buckman R. Breaking bad news: why is it so difficult? BMJ 1984; 288: 1597-1599. Buckman R. How to Break Bad News. Papermac, Basingstoke, 1992. Buckman R. I don’t know what to say - how to help and support someone who is dying. London, Pan Books, 1996. Lugton J. Communicating with dying people and their relatives. Radcliffe Medical Press , Oxford, 2002. Maguire P, Faulkner A. Handling bad news & difficult questions. BMJ 1988; 297: 907-909. 33 Breaking Bad News: The Importance of Hope. Week 2 handout The care of the patient needs to be multi-layered addressing their physical, psychological, emotional and social needs. With terminal illness it is important to work with the patient’s needs on all these levels and vital to create a climate of hope. Kreiger (1982) described four phases of a terminal illness and the hopes the patient may have during each: 1. In the first phase the patient hopes that there has been some kind of misdiagnosis or that the illness will turn out to be curable. 2. As time passes patients move to the second phase where hope for successful treatment predominates. 3. People may move to a third phase of hope when they are told that nothing more can be done to cure them. Hope is then focussed on prolongation of life. 4. Finally hope for a peaceful death is the main concern. Hope becomes centred on the relief of physical symptoms, the maintenance of dignity and the wish to be loved and forgiven. Hope for some kind of afterlife may form part of this final 5. phase. Lugton states that the attitudes and actions of health professionals can create a climate of hope for patients. Herth found that having one’s individuality respected helps to facilitate hope. Listening to patients and their relatives is the vital communication skill for a doctor in gauging the right amount of information for this individual, at this time. Inappropriate information or too much information can remove a person’s hope. The skill is to listen and discover the anxieties so that they can be alleviated and addressed truthfully, without leading to despair. Buckman (Buckman and Kason 1992) suggests the phrase: ‘We’ll plan for the worst but hope for the best’. Here information is neither totally negative nor falsely reassuring. Short – term goal setting and planning with patients to use their time to achieve what they want helps to foster hope. Psychological and psychiatric morbidity have been linked to situations in which patients’ concerns remained undisclosed and unresolved Parle et al. To be able to address the concerns of patients requires self- awareness from the doctor of their own attitudes to death and bereavement. Often health professionals ‘block’ patients’ anxieties by changing the subject, not hearing or responding to cues and focussing on the physical aspects of care. There are training courses available for health professionals to develop their skills in communicating with patients with a terminal illness e.g. run by Christies Hospital. References Buckman R 1992 How to Break Bad News, Papermac, Basingstoke Herth K Fostering hope in terminally ill people, Journal of Advanced Nursing 15 (11):1250 1259 (1990) Kreiger D 1982 The Renaissance Nurse Harper and Row, New York Lugton J 2002 Communicating with dying people and their relatives Radcliffe Medical Press, Oxford Parle M, Jones B & Maguire P 1996 Maladaptive coping and affective disorder among cancer patients Psychological Medicine 26 (4) 735 -44 34 ANGER Breaking Bad News - handout week 3 is a normal part of loss and grieving is around a lot in health care people may be angry – with us/with others/with the system/with their illness Your communication skills will affect the outcome Signs Speech Facial expression Manner Body language becoming louder, quicker or more quiet changing, flushed, reduced eye contact impatience, non-compliance closing in, sudden expansive movements You need to break the cycle of aggression stop think do nothing that may escalate a threat of violence try to understand the reasons behind the anger be prepared to discuss this with them If you are confronted by an angry patient, try to: - be at their eye level - be polite and firm - acknowledge their feelings - be willing to talk and listen – open questions - create a calm atmosphere - verbally break the cycle of anger and aggression Do not - behave in a threatening way - take personal offence at anything that may be said - interrupt an outburst or contradict the patient - caution their choice of words - become combative or threatening - make promises that cannot be kept Do - remember it is the patient/relative who is angry, not you - take any threat of violence seriously - have a colleague nearby - have an ‘escape route’ yourself & leave them an ‘escape route’ - keep on your guard until the incident is over - be ‘street wise’ e.g. don’t work alone, jewellery etc - use the security guards if necessary but under your supervision 35 Talking with relatives -Breaking Bad News - handout week 3 Assess: information about family and friends patient’s views on the quality of the relationship social support Consider family beliefs and influence: previous personal experience of illness previous experience of illnesses in family and friends beliefs of patient or their family ‘sick role’ within the family When listening to relatives: hear their thoughts/feelings/expectations acknowledge their support give them time and privacy arrange a method of contact give information to the patient first find out which relatives can be told what information always write any important discussions with relatives in the notes do not examine patients/perform procedures in front of relatives – except children Secrets: may be different levels -individual/internal/shared fear creates secrets and prevents discussion check your role discuss with your team consider ethical/legal /confidentiality a general discussion with the patient may sort it out try using hypothetical questions/possibilities with out breaking confidentiality Collusion – a conspiracy (spoken or unspoken) to maintain a mutual pretence ‘The task of the health professional is to act as an arbitrator’ Maguire & Faulkner 1988 You might: ask one of the colluding parties for permission to check the other’s level of awareness tell the relative that the patient is your first responsibility – if they want information, it will be given this risks being confrontational check your patient’s level of knowledge or suspicion – be prepared to confirm these suspicions – get your patient’s permission to inform the relative of this.