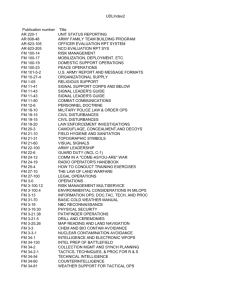
Commander's Guide to Combat Health Support
advertisement

Commander's Guide to Combat Health Support US Army PAM-40-19 Commander's Guide to Combat Health Support Army Pamphlet 40-19 24 March 1995 Unclassified PIN: 073466-000 P.1 Commander's Guide to Combat Health Support US Army PAM-40-19 Change Summary This new pamphlet contains information on the combat health support system. It is intended to be a guide for commanders of nonmedical units. Title Page PICTURE 1 History. This UPDATE printing publishes a new informational pamphlet. Summary. This new informational pamphlet is published for commanders of nonmedical units. The information presented in this publication describes the combat health support system and how it interfaces with and provides support to the organization in wartime and peacetime. Applicability. This pamphlet is published for use by commanders of nonmedical units in the Active Army, the Army National Guard, and the U.S. Army Reserve. This publication is not applicable during mobilization. Proponent and exception authority. The proponent of this regulation is The Surgeon General. The proponent has the authority to approve exceptions to this regulation that are consistent with controlling law and regulation. Proponents may delegate the approval authority, in writing, to a division chief under their supervision within the proponent agency who holds the grade of colonel or the civilian equivalent. Supplementation. Supplementation of this pamphlet is prohibited without prior approval from Headquarters, Department of the Army (DASG-HCD), 5109 Leesburg Pike, Falls Church, VA 22041-3258. Interim changes. Interim changes to this pamphlet are not official unless they are authenticated by the dministrative Assistant to the Secretary of the Army. Users will destroy interim changes on their expiration dates unless sooner superseded or rescinded. Suggested improvements. The proponent agency of this pamphlet is the U.S. Army Medical Department Center and P.2 Commander's Guide to Combat Health Support US Army PAM-40-19 School. Users are invited to send comments and suggested improvements on DA Form 2028 (Recommended Changes to Publications and Blank Forms) directly to the Commander, U.S. Army Medical Department Center and School, ATTN: MCCS-FCD-L, Fort Sam Houston, TX 78234-6100. Distribution. Distribution of this publication is made in accordance with DA Form 12-09-E, block number 5377, intended for command levels C, D, and E for Active Army, Army National Guard, and U.S. Army Reserve. P.3 Commander's Guide to Combat Health Support US Army PAM-40-19 Table of Contents COVER CHANGES TITLE-PAGE CONTENTS FIGURES 1.0 1.1 1.2 Book Cover Change Summary Title Page Table of Contents Figures Introduction Purpose References 1.3 1.4 1.5 Explanation of abbreviations and terms History of the Army Medical Department Mission 1.6 1.7 2.0 2.1 2.2 2.3 2.4 Personnel Quality assurance Combat Health Support Within a Theater of Operations Combat health support system Modular medical support system Echelons of combat health support Theater hospital system 2.5 2.6 2.7 2.8 2.9 2.10 3.0 3.1 3.2 Hospital support requirements Dental support in a theater of operations Veterinary support in a theater of operations Area medical laboratory Theater evacuation policy Intratheater evacuation policy Combat Health Support Logistics Combat Health Logistics System Division Combat Health Logistics System 3.3 3.4 3.5 3.6 3.7 4.0 4.1 4.2 Corps Combat Health Logistics System Echelons Above Corps Combat Health Logistics System Medical equipment maintenance support Optical Combat Health Logistics System Blood management Medical Intelligence What is medical intelligence? Health service intelligence resources P.4 Commander's Guide to Combat Health Support US Army PAM-40-19 4.3 Combat health support planning in historical examples 4.4 5.0 5.1 5.2 6.0 6.1 6.2 6.3 6.4 6.5 Criticality of medical intelligence Law of Land Warfare Provisions Affecting Medical Operations Law of land warfare Medical implications of Geneva Conventions Personnel Personnel Reliability Program Physical profiling Physical Performance Evaluation System Medical Evaluation Board Physical Evaluation Board 6.6 7.0 7.1 Professional Filler System Training Expert Field Medical Badge 7.2 7.3 7.4 7.5 7.6 7.7 Initial unit training and sustainment training Combat lifesaver Field sanitation team training Medical proficiency training The Joint Medical Readiness Training Center and the Combat Casualty Care Course U.S. Army physician assistant 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Soldier Health Maintenance/Current Health Problems Soldier health maintenance elements Sleep Stress Alcohol/drug abuse Suicide prevention Immunizations/prophylaxes The Oral Health Fitness Program Sexually transmitted diseases 8.9 8.10 8.11 8.12 8.13 8.14 9.0 9.1 Acquired immunodeficiency syndrome Occupational safety and health Field sanitation team Army Aviation Medicine Program (flight surgeon) Veterinary services Nutrition The Military Family TRICARE P.5 Commander's Guide to Combat Health Support US Army PAM-40-19 9.2 Civilian Health and Medical Program of the Uniformed Services 9.3 9.4 9.5 9.6 9.7 A.0 GLOSSARY USAPPC-INDEX Primary Health Care for the Uniformed Services Uniformed Services Dependents Dental Insurance Plan Family Advocacy Program Exceptional Family Member Program Veterinary treatment facilities Appendix A. References Glossary Index Figures 2-1. Echelons of combat health support 2-2. Component hospital system 2.10 2.10 P.6 Commander's Guide to Combat Health Support US Army PAM-40-19 1.0 Introduction 1.0 Introduction Subtopics 1.1 Purpose 1.2 References 1.3 Explanation of abbreviations and terms 1.4 History of the Army Medical Department 1.5 Mission 1.6 Personnel 1.7 Quality assurance 1.1 Purpose The purpose of this pamphlet is to provide commanders of nonmedical units with information on the combat health support (CHS) system. It is not intended to be all-inclusive but to provide a summary for the target audience. The information presented in this pamphlet is based on doctrine, policy, and procedures published in Army Medical Department (AMEDD) manuals. 1.2 References Required and related publications and referenced forms are listed in appendix A. 1.3 Explanation of abbreviations and terms Abbreviations and special terms used in this pamphlet are explained in the glossary. 1.4 History of the Army Medical Department a. Today's medics trace their history back to the siege of Boston in 1775 under the leadership of George Washington. At Washington's request, the Continental Congress established the "hospital," which was the forerunner to the AMEDD. The AMEDD was not permanently established under that name until 1818. The physicians of the AMEDD did not receive the status of commissioned officers until 1847, but they had gained a reputation for efficient service and high professional standards well before then. As early as 1827, the Inspector General of the U.S. Army noted that the service "is truly fortunate in having such a medical corps . . . how could it be that the government was able to employ such professional worth at so paltry a price?" b. The AMEDD lacked a supporting staff of specially trained enlisted men to aid the surgeons in preserving the health of the troops. Although in 1838 Congress had authorized the enlistment of P.7 Commander's Guide to Combat Health Support US Army PAM-40-19 men for exclusive duty as hospital stewards, it reversed this policy in 1842. To meet the needs of the AMEDD, Surgeon General Thomas Lawson had established a training school for hospital stewards in 1840. In 1844 Lieutenant General Winfield Scott, Commanding General of the Army, ordered that all soldiers detailed temporarily from their units for service as hospital stewards should remain officially attached to the hospitals throughout their service. Lieutenant General Scott's order forced the training school for hospital stewards to close for lack of eligible students. In 1887 a hospital corps was established to provide a standing body of educated, permanently assigned, enlisted personnel for service with the AMEDD. c. During the late nineteenth and early twentieth centuries, the AMEDD also provided officers who made major contributions to the other branches of the Service. While stationed at Fort Davis, Texas, during the 1850's, Surgeon Albert J. Myer became interested in the problems of field communications using flags and torches. He presented his study on the subject to War Department, and in 1863 became the first chief of the newly created Signal Corps. the Organizational skill and a passion for systematic procedures won Surgeon Fred C. Ainsworth appointment first as acting Secretary of War and later as Adjutant General of the Army in 1907. During the same period Surgeon Leonard Wood, a Medal of Honor recipient for earlier service in the Indian Wars, shattered all precedent by becoming Chief of Staff of the Army. d. The drive for professional excellence through education continued in the AMEDD. On 28 April 1920, Surgeon General Merritte W. Ireland addressed a letter to the Adjutant General requesting permanent authority to use the U.S. Military Reservation at Carlisle Barracks, Pennsylvania, as a field school. In June 1920, the Medical Field Service School (MFSS) was officially established at that post. e. The school at Carlisle Barracks consisted of five departments: military art, enlisted training, hygiene, administration, and equipment and transportation. The school started with a basic course for medical, dental, and veterinary officers of the Regular Army. It soon added courses for Reserve and National Guard officers and noncommissioned officers (NCOs). It also added summer training for officers of the Reserve and the Reserve Officers Training Corps. f. Some notable activities other than training were carried on at Carlisle. One was the equipment laboratory, which experimented with new equipment used in the treatment and evacuation of casualties. The first-aid dressing carried today by every soldier, once called the Carlisle dressing, was developed in that laboratory. Tentage for field hospitals (FHs), electrical equipment, improved litters, field dental dispensaries, new P.8 Commander's Guide to Combat Health Support US Army PAM-40-19 ambulances, field x-ray equipment, and many other items of medical equipment used by the Army were developed there. g. The helicopter's potential for rapid evacuation of casualties from battlefields to hospitals, where prompt and definitive surgical care is available, was demonstrated first at Carlisle Barracks in 1935. h. In 1940, as the nation mobilized for World War II, the AMEDD expanded and the school geared its activities to new requirements. Facilities and space at Carlisle Barracks were lacking to support expansion, large-scale field exercises, and demonstrations. The end of World War II saw selection of a larger site for the school--Fort Sam Houston, Texas. In 1946, the school moved from Carlisle Barracks to the new site where it became an organizational element of Brooke Army Medical Center (BAMC). i. In training medical department personnel for their mission, the school enlarged its facilities and expanded and adapted courses of instruction to support changing requirements for field medical service. The U.S. Army Health Services Command (HSC) was established on 1 April 1973; this command consolidated many elements (including 36 post hospitals and 7 medical centers) of the continental United States (CONUS) AMEDD under a single major Army command. Concurrently, BAMC was reorganized as two commands under HSC: a medical center (designated BAMC), and several education/training elements (including the discontinued MFSS) consolidated under an Academy of Health Sciences (AHS), U.S. Army. Major new AHS facilities were completed; and, nearly 20 years later, on 1 July 1991, the AHS was redesignated as the AMEDD Center and School (AMEDDC&S). As a reaction to increasing medical centralization as well as post-Cold War developments, realignments accelerated; and, on 1 October 1994, HSC was redesignated and expanded as the U.S. Army Medical Command (MEDCOM)--a worldwide major command led by The Surgeon General. j. The basic objectives of the first school were to train medical personnel to recover wounded from the battlefield and to treat them rapidly and effectively. These two elements of military medicine are studied as exhaustively today as they were in that first class at Carlisle Barracks. 1.5 Mission a. The mission of the AMEDD mirrors the medical mission of the Department of Defense (DOD): P.9 Commander's Guide to Combat Health Support (1) To provide US Army PAM-40-19 and maintain readiness to provide medical services and support to the armed forces during military operations. (2) To provide services and support to members of the armed forces, their dependents, and others entitled to DOD medical care. b. The AMEDD has responsibility for all medical services provided within the Department of the Army (DA). These services include-(1) Patient evacuation and medical regulation. (2) Hospitalization. (3) Combat health logistics/blood management. (4) Dental services. (5) Veterinary services. (6) Preventive medicine (PVNTMED) services. (7) Combat stress control (CSC) services. (8) Area medical support. (9) Command, control, communications, computers, and intelligence. (10) Medical laboratory services. (11) Garrison outpatient services. (12) Coordination of complementary health services among other Federal and civilian agencies. 1.6 Personnel The AMEDDC&S trains both officer and enlisted personnel in a variety of medical functional areas and medical military occupational specialties (MOSs). Some of these medically trained officer and enlisted personnel may be assigned to a medical platoon organic to your battalion. a. Officer personnel. Officers normally assigned to a medical platoon include Medical Corps (MC) officers (physicians), Medical Service Corps (MS) officers, and Army Medical Specialist Corps (SP) physician assistants (PAs). (1) The MC officer has three major areas of responsibility. The first responsibility is to serve as platoon leader of the medical element of the battalion (medical platoon leader). The second responsibility is to serve as the medical advisor and special staff officer to the battalion commander. The third responsibility is to treat patients. Other responsibilities and functions of the battalion medical platoon leader include-P.10 Commander's Guide to Combat Health Support US Army PAM-40-19 (a) Planning and directing unit-level CHS of the battalion. (b) Assisting the Operations and Training Officer (S3) in planning and supervising individual and collective training of the medical platoon/section and in training nonmedical personnel within the battalion. (c) Advising the battalion commander and staff on the current health of the command. (d) Supervising the administration, discipline, equipment maintenance, supply functions, organizational training, and employment of the assigned medical element. (e) Treating casualties. Note. In the absence of the physician or when there is none assigned, the physician's duties and responsibilities, except the treatment of patients, will be assumed by the senior commissioned officer. The treatment of patients will remain with the patient treatment protocol. (2) The MS officer (field medical assistant) serves as the medical operations officer and is responsible for the operational readiness of the medical platoon. The responsibilities and functions include but are not limited to-(a) Coordinating CHS operations with the battalion S3. (b) Coordinating nonmedical supplies with the headquarters and headquarters company supply personnel. (c) Coordinating patient medical company. evacuation and medical resupply with the supporting (3) The PA, while not a physician, is a skilled clinician who, by formal training and experience, is qualified to perform medical tasks formerly undertaken only by a physician. This individual functions in the battalion medical platoon under the direction and technical supervision of the medical platoon leader. The PA, in conjunction with the platoon leader, is responsible for-(a) Conducting and/or supervising training of all battalion personnel in first aid, field sanitation, personal hygiene, medical evaluation procedures, and medical aspects of injury prevention. (b) Arranging for the conduct of the battalion CSC program, with technical assistance from the psychiatrist and other officers and NCOs of the division mental health section or its equivalent. This program includes training battalion troop leaders in methods of controlling stress and preventing stress casualties, especially battle fatigue (BF) and misconduct stress behaviors. P.11 Commander's Guide to Combat Health Support US Army PAM-40-19 (c) Establishing and operating the battalion aid station (BAS). (d) Treating, within the individual's medical capability, those patients reporting for sick call or those evacuated from the maneuver companies. (e) Providing emergency medical care to the wounded and injured to include-1. 2. 3. 4. 5. 6. Establishing and maintaining a patient's airway. Controlling bleeding. Preventing and treating shock. Dressing wounds. Immobilizing fractures. Relieving pain and undue suffering. b. Enlisted personnel. Enlisted personnel who assist in the operation of the medical platoon include but are not limited to the medical specialist (MOS 91B10/20) and the medical NCO (MOS 91B30). (1) A medical specialist, trained and certified per civilian standards, is referred to as an Emergency Medical Technician (EMT). This specialist assists the medical NCO in accomplishing assigned duties and also performs triage and emergency medical treatment for battlefield casualties. Specific duties of the medical specialist include-(a) Assisting with outpatient care and treatment. (b) Assisting with care and treatment under the supervision of a physician, PA, or medical NCO. (c) Erecting and breaking down field medical shelter systems, to include chemical protective shelters. (d) Initiating patient records (DD Form 1380 (U.S. Field Medical Card)). (e) Logging patients seen or treated in the medical treatment facility (MTF). (f) Operating and maintaining assigned vehicle, tactical radio, and power generation equipment. (2) A medical NCO is qualified as a medical specialist and completes either the C-8-C40 (91B) and/or the AMEDD NCO basic (NCO Education System) course. Just like the medical specialist, the medical NCO, with additional civilian training and certification, may be classified as an EMT or a paramedic. This NCO assists the physician and the PA in the accomplishment of their clinical duties. This NCO performs triage and emergency medical treatment procedures in the care and management of the trauma (including chemically contaminated) patient, assists in the care and management of the BF P.12 Commander's Guide to Combat Health Support patient, performs routine patient US Army PAM-40-19 care, and performs nuclear, biological, and chemical (NBC) detection procedures. This NCO is also trained to-(a) Supervise and train medical specialists. (b) Supervise field and clinical medical facilities. (c) Assist with technical and administrative management of MTFs under the supervision of a physician or PA. (d) Administer emergency and routine outpatient medical treatment to battle and nonbattle casualties. (e) Assist with outpatient care and treatment. (f) Assist in the establishment and operation of a unit-level field MTF. (g) Maintain the patient accountability/casualty reporting system. (h) Maintain medical equipment sets. (i) Conduct training in first aid and emergency medical procedures for assigned personnel and combat lifesavers. (j) Conduct sanitation inspections of troop living areas, field food service preparation areas, waste disposal areas, and potable water distribution points and equipment. 1.7 Quality assurance a. The AMEDD has established a formal Quality Assurance Program to-(1) Provide quality care and treatment to all beneficiaries in their need for health services, subject to the availability of space and facilities and the capabilities of the health care staff. (2) Make improvements resulting in higher quality health care. (3) Promote the professional development and enhance the capabilities of the military and civilian members of the AMEDD. The scope of the program is broad, encompassing health care services provided in all table of distribution and allowances and table of organization and equipment (TOE) treatment facilities. b. The objectives of the Quality Assurance Program are to-(1) Assure that health care personnel deliver quality patient care. (2) Reduce risk-creating incidents and adverse effects to patients. (3) Improve provider-patient communication and patient satisfaction. (4) Enhance coordination and communication among health care providers and clinical and ancillary services. (5) Improve the health care provider screening, selection, and accession process. (6) Objectively evaluate performance through performance-based criteria and other quality P.13 Commander's Guide to Combat Health Support US Army PAM-40-19 assurance information. (7) Educate health care personnel on quality assurance requirements. (8) Enhance the skills and knowledge of practitioners. (9) Consolidate quality assurance efforts into one comprehensive program. (10) Reduce medical malpractice and claims to the maximum extent possible. c. The Quality Assurance Program involves an ongoing process to monitor and evaluate objectively and systematically the access to and quality and appropriateness of patient care, pursue opportunities to improve patient care and clinical performance, and resolve identified problems in care and performance. Quality is the degree of adherence to generally recognized standards of good practice and achievement of anticipated outcomes for a particular service, procedure, diagnosis, or clinical problem. Appropriateness is the extent to which a particular procedure, treatment, test, or service is efficacious and clearly indicated for the patient. The components of the Quality Assurance Program are: patient care evaluation, credentials review and privileging, utilization management to include access to patient care, and risk management. P.14 Commander's Guide to Combat Health Support US Army PAM-40-19 2.0 Combat Health Support Within a Theater of Operations Subtopics 2.1 Combat health support system 2.2 Modular medical support system 2.3 Echelons of combat health support 2.4 Theater hospital system 2.5 Hospital support requirements 2.6 Dental support in a theater of operations 2.7 Veterinary support in a theater of operations 2.8 Area medical laboratory 2.9 Theater evacuation policy 2.10 Intratheater evacuation policy 2.1 Combat health support system a. CHS plays a vital role as a force multiplier. Sustaining the health of the fighting forces is a critical factor in the success or failure of the combat mission. The number and type of CHS organizations will be based on the-(1) Mission, enemy, terrain, troops, and time available. (2) Size of force being supported. (3) Projected patient work loads. (4) Availability of evacuation assets. (5) Evacuation policy. b. The CHS mission--to conserve the fighting strength-- dictates that patients be collected, triaged, treated, evacuated, and/or returned to duty as far forward as possible. c. The multifunctional CHS system is a single, integrated system that extends from the forward line of own troops (FLOT) back through the communications zone (COMMZ) and ends in CONUS. This system is dependent upon effective medical regulating and the evacuation of sick, injured, and wounded soldiers in the shortest possible time. Patients who are expected to return to duty (RTD) within the theater evacuation policy are evacuated to a corps and/or a COMMZ hospital. Those patients classified as nonreturn to duty within the theater evacuation policy are treated and stabilized for evacuation out of theater. 2.2 Modular medical support system P.15 Commander's Guide to Combat Health Support a. CHS in the division is US Army PAM-40-19 provided by a modular support system that standardizes all medical subelements. The CHS modular design enables the medical resources manager to rapidly tailor, augment, reinforce, or reconstitute the CHS units as needed. This system is designed to acquire, receive, and triage patients, and to provide emergency medical treatment and advanced trauma management (ATM). CHS originates in the forward areas of the division, separate brigade, and armored cavalry regiment (ACR) with the combat medic supporting each platoon or company/troop team. From this point, the patient is evacuated to the battalion/squadron medical platoon treatment squad (battalion/squadron aid station) and then to the medical company/troop treatment platoon (clearing station). b. The modular medical support system is built around six modules organic to division and nondivisional CHS units. These modules are oriented to casualty collection, treatment, and RTD or evacuation. (1) Combat medic module. The combat medic module consists of one combat medical specialist and the prescribed load of medical supplies and equipment. Combat medics are organic to the medical platoons or sections of combat support (CS) and combat service support (CSS) battalions and squadrons. (2) Ambulance squad module. An ambulance squad module is comprised of four medical specialists and two ambulances. This squad provides patient evacuation throughout the division, corps, and COMMZ and provides en route care. Ambulance squads are organic to the medical platoons or sections in maneuver battalions and squadrons, some CS battalions, and medical companies of divisional and nondivisional support battalions/squadrons. These squads are also organic to medical companies of area support medical battalions (ASMBs) in the corps and COMMZ. Medical company ambulance squads are employed in the brigade support area (BSA), division support area (DSA), corps support area (CSA), and in all areas of the COMMZ. The medical platoon's ambulance squads may be collocated with the companies of the maneuver battalions. (3) Treatment squad module. This squad consists of a primary care physician, a PA, and six medical specialists. The squad is trained and equipped to provide ATM to the battlefield casualty. ATM is physician- or PA-directed emergency medical care designed to resuscitate and stabilize the patient for evacuation to the next echelon of medical care, or to treat and RTD. ATM provides maximum benefit if received within 60 minutes of injury. To maintain contact with the combat maneuver elements, each squad has two emergency treatment vehicles. Each squad can split into two treatment teams. These squads are organic to medical platoons or sections in maneuver battalions/squadrons and designated CS units, as well as being the basic building block of the medical companies. (4) Area support squad. This squad is comprised of one dentist trained in ATM, a dental P.16 Commander's Guide to Combat Health Support US Army PAM-40-19 specialist, an x-ray specialist, and a medical laboratory specialist. The squad is organic to the medical companies within the BSA, DSA, CSA, and COMMZ. (5) Patient-holding squad. This squad consists of two practical nurses and two medical specialists. It is capable of holding and providing minimal care for up to 40 RTD patients for a maximum of 72 hours. This squad is organic to the medical companies within the BSA, DSA, CSA, and COMMZ. Note. When a treatment squad, an area support squad, and a patient-holding squad are collocated, they form an area support section. This section provides CHS on an area basis to all forces within a geographical area of responsibility (clearing station). The area support section normally operates in the BSA, DSA, CSA, and COMMZ. The area support and patient-holding squads are incapable of independent operations. (6) Surgical squad/detachment.This module is comprised of two surgeons, two nurse anesthetists, two operating room specialists, one medical/surgical nurse, and two practical nurses. It is organized to provide early resuscitative surgery for seriously wounded or injured patients, to save life, and to preserve physical function. Early surgery is performed whenever a likely delay in the evacuation of a patient threatens life or the quality of recovery. Postsurgical patients awaiting evacuation are held by the patient-holding squad. This squad collocates with the surgical modules. The surgical squad provides the required nursing care. Surgical squads are organic to the medical battalions of the airborne and air assault divisions. All other surgical modules are called detachments. These detachments are not organic to divisions. They normally are employed in the DSA but may be employed in the BSA during brigade task force operations. (7) Forward surgical team. A forward surgical team (FST) will replace the two surgical squads in each of the following: the Airborne Division; the Air Assault Division; and the 2d ACR. The FSTs will also replace the medical detachment (surgical) and the 30-bed mobile Army surgical hospital (MASH). This team will be a corps augmentation for divisional and nondivisional medical companies. It will provide emergency/urgent initial surgery and nursing care after surgery for the critically wounded/injured patient until sufficiently stable for evacuation to a theater hospital. The FSTs not organic to divisions and the 2nd ACR will be assigned to a medical brigade or group and normally attached to a corps hospital when not operationally employed and further attached for support to a divisional or nondivisional medical company. 2.3 Echelons of combat health support There are four echelons of CHS in a theater of operations (TO) that have a direct impact on patients as they are treated and evacuated from the FLOT to the CONUS base. (See fig 2-1.) P.17 Commander's Guide to Combat Health Support US Army PAM-40-19 a. Echelon I. This echelon is also known as unit level. Care is provided by designated individuals or elements organic to combat and CS units and elements of the ASMB. Major emphasis is placed on those measures necessary to stabilize the patient (maintain airway, stop bleeding, prevent shock) and allow for evacuation to the next echelon of care. (1) Combat medic. This is the first individual in the CHS chain who makes medically-substantiated decisions based on medical MOS-specific training. The combat medic is supported by first-aid providers in the form of self-aid and buddy aid and the combat lifesaver. (a) Self-aid and buddy aid. The individual soldier is trained to be proficient in a variety of specific first-aid procedures with particular emphasis on lifesaving tasks. This training enables the soldier, or a buddy, to apply immediate first aid to alleviate a life-threatening situation. (b) Combat lifesaver. Enhanced first-aid training is provided to selected individuals who are called combat lifesavers. These individuals are nonmedical unit members selected by their commander for additional training to become proficient in a variety of first-aid procedures. A minimum of one individual per squad, crew, team, or equivalent-sized element is trained. All combat units and some CS and CSS units have combat lifesavers. The primary duty of these individuals does not change. The additional duties of combat lifesavers are performed when the tactical situation permits. These individuals provide enhanced first aid for injuries prior to treatment by the combat medic. The training is normally provided by medical personnel assigned or attached to the unit. The training program is managed by a senior medical person designated by the commander. (2) Treatment squad (BAS).Personnel are trained and equipped to provide ATM to the battlefield casualty. Like elements provide this echelon of care in the division, corps, and COMMZ. Echelon I care for units not having an organic capability is provided on an area basis by the organization responsible in the sector. b. Echelon II. This echelon may also be known as division level. Care at this echelon is rendered at the clearing station (division, corps, or COMMZ). Here the casualty is examined and his or her wounds and general status are evaluated to determine the treatment and evacuation precedence, as a single casualty among other casualties. Emergency medical treatment (including beginning resuscitation) is continued and, if necessary, additional emergency measures are instituted; however, they do not go beyond the measures dictated by the immediate necessities. The division clearing station has limited blood replacement P.18 Commander's Guide to Combat Health Support US Army PAM-40-19 capability, limited x-ray and laboratory services, patient-holding capability, and emergency dental care. An FST will augment the divisional/nondivisional medical companies to provide emergency/urgent initial surgery. (See para 2-2b(7).) Division-level CHS also includes PVNTMED activities and CSC. Those patients who can RTD within 1 to 3 days are held for treatment. These functions are performed typically by company-sized medical units organic to brigades, divisions, and ASMBs. c. Echelon III. The first hospital facilities are located at this echelon. Within the combat zone (CZ), the MASH and the combat support hospital (CSH) are staffed and equipped to provide resuscitation, initial wound surgery, and postoperative treatment. Although the MASH is an Echelon III facility, it is designed to be employed within the division area. At the CSH, patients are stabilized for continued evacuation or returned to duty. Those patients who are expected to RTD within the theater evacuation policy are regulated to a facility that has the capability for reconditioning and rehabilitation. d. Echelon IV. At this echelon, the patient may be treated at the general hospital (GH) or the FH. The GHs are staffed and equipped for general and specialized medical and surgical care. Those patients not expected to RTD within the theater evacuation policy are stabilized and evacuated to CONUS. At the FH, reconditioning and rehabilitation services are provided for those patients who will be RTD within the theater evacuation policy. e. Echelon V. This echelon of care is provided by the CONUS base. Hospitalization is provided by DOD hospitals (military hospitals of the triservices) and Department of Veterans Affairs (DVA) hospitals. Under the National Disaster Medical System, patients overflowing DOD and DVA hospitals will be cared for in designated civilian hospitals. 2.4 Theater hospital system a. Medical Force 2000 is the modernization effort to restructure the hospitalization system in support of a TO. This system consists of four hospitals, a medical company (holding), and six medical/surgical teams. The hospitals normally located in the corps are the MASH and the CSH. The hospitals normally located in the COMMZ are the GH and the FH. In addition to these hospitals, the medical company (holding) provides a 1200-cot convalescent capability. For a detailed discussion on the Medical Force 2000 Hospital System, refer to FM 8-10. (1) MASH. This hospital is a 30-bed facility with the primary mission of providing lifesaving surgical intervention to stabilize patients for further evacuation to either the P.19 Commander's Guide to Combat Health Support US Army PAM-40-19 CSH or COMMZ hospitals. Patients are held approximately 24 to 36 hours until considered stable enough to tolerate a bed-to-bed transfer without incurring further risk to their condition. The MASH is normally employed near a divisional rear boundary to support a two divisional force. However, an element of the MASH, the hospital unit surgical-forward (HUSF) may be employed within a particular division. The HUSF may be employed within the DSA or BSA and collocated with a support battalion medical company. The MASH is 100 percent mobile with organic vehicles. (2) CSH. This organization is a 296-bed facility with the mission of stabilizing patients for further evacuation and RTD of those who fall within the corps evacuation policy. It is capable of handling all types of patients and will be employed in the corps area. The CSH is 35 percent mobile with organic vehicles. (3) FH. This organization is a 504-bed facility with the mission of providing hospitalization for patients and for reconditioning and rehabilitating those patients who can RTD within the theater evacuation policy. The majority of patients within this facility will be in the convalescent care category. The FH is normally located in the COMMZ, but could be used in the corps rear when geographical and tactical operational constraints dictate. Its mobility with organic vehicles is 20 percent. (4) GH. This organization is a 476-bed facility with the mission of providing stabilization and hospitalization for patients who require either further evacuation out of the TO, or who can RTD within the theater evacuation policy. The GH is normally located in the COMMZ. Its mobility is 10 percent with organic vehicles. (5) Medical company (holding).This unit provides for reconditioning and rehabilitation of convalescent care patients who are expected to RTD. It consist of 1200 cots and is minimally staffed and equipped. This facility has the capability to task organize by separating the company into five holding platoons, each capable of operating 240 cots. These elements can be attached to augment hospitals and mobile aeromedical staging facilities. Additionally, the medical company (holding) can be used in the combat stress reconditioning programs. (6) Medical/surgical teams. These teams provide specialized medical and surgical augmentation to CZ and COMMZ hospitals. These teams provide the following services: (a) Renal hemodialysis. (b) Infectious disease treatment. P.20 Commander's Guide to Combat Health Support US Army PAM-40-19 (c) Pathology services. (d) Head and neck surgery. (e) Neurosurgery. (f) Eye surgery. b. All of the hospitals, except the MASH, are configured using various combinations of a four-module concept. The four modules include-(1) Hospital unit, base (HUB). (2) Hospital unit, surgical (HUS). (3) Hospital unit, medical (HUM). (4) Hospital unit, holding (HUH). c. The CSH, FH, and GH consist of a base component and one or more mission-adaptive components. The base can operate independently and is clinically similar in each hospital. The other three mission-adaptive modules (HUS, HUM, and HUH) are dependent upon the base. (See fig 2-2.) The hospital's capability can be further enhanced by the attachment of medical or surgical teams. 2.5 Hospital support requirements a. In deployment and sustainment of operations, the theater hospitals are dependent upon appropriate elements of the corps and COMMZ for-(1) Personnel and administrative services. (2) Finance. (3) Mortuary affairs. (4) Legal services. (5) Transportation services. (6) Laundry and bath services for other than patient-related support. (7) Security (to include enemy prisoners of war (EPW) security during processing and evacuation). (8) Transportation and reequipping (to include the balance of their individual Class II clothing and equipment and weapon and ammunition) for discharged patients. The hospital will provide the minimal basic uniform items and, if required, mission-oriented protective posture gear, to RTD soldiers to protect them during transit to replacement companies. b. During deployment and sustainment of operations, engineer support is required for site preparation, waste disposal, and minor construction. 2.6 Dental support in a theater of operations P.21 Commander's Guide to Combat Health Support US Army PAM-40-19 Dental service support is an integral part of the theater CHS system and shares in the overall responsibility of conserving the fighting force. As part of the mission, the responsibility of the field dental care system is to prevent and treat dental disease and injury. Dental support in the TO is organized into a modular and flexible system which can respond to rapidly changing conditions across the continuum of dental operations. Dental assets in the TO are found at Echelons II, III, and IV. Most dental assets in the theater are organized into dental units whose primary mission is to provide dental service. However, a significant number of dental resources are organic to medical companies and hospitals. During periods of increased combat activity, dental soldiers augment the medical capability of medical units by performing alternate wartime roles such as triage and ATM. a. Categories of dental care.Dental treatment is classified into four categories: emergency, sustaining, maintaining, and comprehensive. These categories are not absolute in their limits; however, they are the general basis for the definition of capability at the various echelons of CHS. Each category is successively greater in service provided and corresponding resources required to provide that service. Sustaining care is capable of less definitive treatment than maintaining care, but requires less equipment and is more suited to use further forward on the battlefield where weight and mobility are greater concerns. Conversely, maintaining care provides a much wider spectrum of services, but is far more resource-dependent and less suited for use in a rapidly moving scenario. Of the four categories of care, only the first three, emergency, sustaining, and maintaining are available in the TO. Comprehensive care is normally provided in fixed facilities in CONUS. b. Types of dental support. There are three types of dental support in the TO: unit, hospital, and area (the largest category). They are defined primarily by the relationship the dental assets with the supported patient population. of (1) Unit. Unit dental support is provided by dental personnel organic to Echelon II medical units. Dental modules are part of the area support squads in the medical companies of divisions, separate brigades, and ACRs and the medical element of the special forces group. Dental modules are also found in the area support squads of the area support medical companies located throughout the CZ and COMMZ. The dental module consists of a dental officer, a dental assistant, and compact high technology dental equipment. Their primary objective is to return the soldier to duty as rapidly as possible consistent with the tactical situation. (2) Hospital. CSH, FH, and GH. Hospital dental support is provided by dental personnel organic to the The MASH has no capability for dental support. The primary P.22 Commander's Guide to Combat Health Support US Army PAM-40-19 mission of hospital dental sections is to minimize loss of life and disability resulting from severe oral and maxillofacial injury, whether battle or nonbattle. When casualty care work load permits, dental resources provide dental treatment to hospital patients and staff. In addition, treatment is provided to patients referred by other dental and medical facilities when oral and maxillofacial care is beyond the capability of the referring facility. The maxillofacial surgery capability in these hospitals can be augmented by attaching a medical team, head and neck surgery. (3) Area. Area dental support is provided by dental personnel and equipment organized into dental service units capable of providing all categories of dental care up to and including maintaining care. These units are the medical company (dental service), medical detachment (dental service), and medical team (prosthodontics). They are usually organized under the command of a medical battalion (dental service) which is assigned to a corps or COMMZ medical brigade. Dental units may also be attached to a medical group. As the name suggests, area dental support is provided within a designated geographic area of responsibility. Within this area of responsibility, area dental support units may be tasked to provide direct support to unit or hospital dental support elements. They may also be tasked to reconstitute unit dental support modules from like modules within their own unit. Area dental support represents a major share of the dental capability within the TO. 2.7 Veterinary support in a theater of operations As an integral part of the theater CHS system, the primary responsibility of field veterinary service detachments is to ensure the wholesomeness and food safety of all Class A and operational rations consumed and to provide veterinary health care to all military working dogs, military mascots, and indigenous animals in the TO. Veterinary support in the TO is organized into a mobile, modular, and flexible system capable of split base operations. Veterinary support is capable of responding to rapidly changing mission requirements in the TO. Veterinary units are found at Echelons II, III, and IV. Veterinary support is provided on an area basis. There are no organic veterinary units in the division. Veterinary units will be assigned to a medical group or medical brigade in the TO. These units may be attached in direct support of division Class 1 supply points to ensure the food safety of all subsistence or to military police military working dog units to provide on-site veterinary health care. a. Categories of veterinary food safety support. This support is divided into four categories: surveillance inspections of subsistence at Class 1 P.23 Commander's Guide to Combat Health Support US Army PAM-40-19 supply points, in-country commercial sanitary inspections for procurement of Class A rations, receipt inspections of all subsistence entering the TO, and food microbiology laboratory support. These categories are not absolute; however, they are the general basis for determining the veterinary support required in the TO. Veterinary detachments do possess a significant nuclear and chemical agent surveillance monitoring capability. This ensures timely information to the Class 1 officer on the disposition and suitability for human consumption of possible NBC contaminated subsistence. b. Categories of veterinary health care support. This support is divided into three categories that will be available in the TO. Level 1 will be limited to sick call and emergency first aid for Government animals. This support is located in the division rear area. Level II will involve complete health care (to include emergency surgery under gas anesthesia) for Government animals. The emphasis will be on health care for military working dogs. This support will be located near a major air base to facilitate air evacuation. Additionally, veterinary units have the capability to investigate zoonotic disease outbreaks (e.g., rabies), or unexplained deaths in the indigenous animal population. 2.8 Area medical laboratory a. The area medical laboratory (AML) provides the theater commander the analytical and scientific capabilities to assess chemical, biological warfare and endemic disease agents. This unit is a high-technology, hospital-independent laboratory with a degree of complexity and sophistication exceeding that present in hospital-based medical laboratories. b. Unlike conventional medical laboratories, the AML performs investigative protocols and analytical procedures to evaluate environmental health issues with the potential to affect military operations in the TO. The focus is on a broader scope related to the health of theater armed forces as a whole as opposed to direct support of individual patient care. c. The AML may task-organize its resources to provide laboratory support for military contingency operations, civic action programs, humanitarian P.24 Commander's Guide to Combat Health Support support missions, or to US Army PAM-40-19 deploy an investigative team forward into the corps area once the base laboratory is established in the theater. 2.9 Theater evacuation policy a. This policy is established by the Secretary of Defense, with the advice of the Joint Chiefs of Staff, and upon the recommendation of the theater commander. The policy establishes, in number of days, the maximum period of noneffectiveness (hospitalization and convalescence) that patients may be held within the theater for treatment. This policy does not mean that a patient will be held in the theater for the entire period of noneffectiveness. A patient who is not expected to be ready for RTD within the number of days established in the theater evacuation policy is evacuated to CONUS or some other safe haven. This is done providing that the treating physicians determine that such evacuation will not aggravate the patient's disabilities or medical condition. For example, a theater evacuation policy of 60 days does not mean that a patient is held in the theater for 59 days and then evacuated. Instead, it means that a patient will be evacuated as soon as possible after a determination is made that the patient cannot be returned to duty within 60 days following admission. b. When unforeseen increases in the number of patients occur (due perhaps to an epidemic or heavy combat casualties), a temporary reduction in the policy may be necessary to adjust the volume of patients in the theater hospital system. A reduction in the evacuation policy increases the number of patients requiring evacuation out of theater, increases the requirement for evacuation assets, and increases the requirement replacement/filler personnel. This action is necessary to relieve the congestion caused by the increased number of patients. c. The time period established in the theater evacuation policy starts on the date the patient is admitted to the first hospital (CZ or COMMZ). The total time a patient is hospitalized in the theater, including transit time between MTFs, for a single uninterrupted episode of illness or injury should not exceed the number of days stated in the theater evacuation policy. Although the medical company (holding) is not a hospital, the time a patient spends in one is included in the calculation of the duration of the hospital stay. Though guided by the evacuation policy, the actual selection of a patient for evacuation will be based on clinical judgment P.25 for Commander's Guide to Combat Health Support as to US Army PAM-40-19 the patient's ability to tolerate and survive the movement to the next level of hospitalization. 2.10 Intratheater evacuation policy a. Subordinate commands may establish intratheater patient evacuation policies within the limits of the theater patient evacuation policy and subject to approval by the theater commander. For example, a short evacuation policy may be established for corps hospitals to maintain their mobility and their capability to accommodate surges of patients. The intratheater evacuation policy, usually stated in days at the corps level, represents the maximum period of allowable hospitalization in corps hospitals. Any patient who can be expected to RTD within the stated policy is retained by a CSH for definitive care and subsequent RTD. Any patient who cannot be expected to RTD within the stated policy is evacuated to the COMMZ as soon as the patient's condition transportation resources permit. Intratheater patient evacuation policies must be flexible and changed as dictated by the tactical situation. (These policies may be adjusted in the early days of a contingency operation as the availability of treatment facilities and evacuation means permit.) Intratheater evacuation policies may differ among hospitals depending on their location, facilities, staff, and the numbers and types of patients received. b. When patients are received at a constant rate, the evacuation policy at a specific echelon may be adjusted to retain and subsequently RTD those patients who do not require specialized treatment in COMMZ GHs. However, when increased patient loads are anticipated, the intratheater evacuation policy must be adjusted downward to make additional beds available for current and anticipated needs. As a result, a larger proportion of patients admitted to hospitals in the CZ are evacuated to the COMMZ. PICTURE 2 Figure 2-1. Echelons of combat health support PICTURE 3 Figure 2-2. Component hospital system P.26 and Commander's Guide to Combat Health Support US Army PAM-40-19 3.0 Combat Health Support Logistics Subtopics 3.1 Combat Health Logistics System 3.2 Division Combat Health Logistics System 3.3 Corps Combat Health Logistics System 3.4 Echelons Above Corps Combat Health Logistics System 3.5 Medical equipment maintenance support 3.6 Optical Combat Health Logistics System 3.7 Blood management 3.1 Combat Health Logistics System a. The Combat Health Logistics System (CHLS) encompasses the activities of medical supply (Class VIII), medical equipment maintenance, optical fabrication, contracting services, single integrated medical logistical manager (SIMLM) for joint operations, and blood management for Army, joint, or combined operations. The CHLS is modular in design to provide the flexibility, mobility, and capability to support war and operations other than war. The system is anticipatory and projects its support based on operational objectives. b. The organizational structure for CHLS in a TO consists of four types of units: medical logistics (MEDLOG) battalion (forward), MEDLOG battalion (rear), theater medical materiel management center (TMMMC), and MEDLOG support detachment. (1) The MEDLOG battalion (forward) provides Class VIII supplies, single-vision optical lens fabrication, medical equipment maintenance support, and blood processing, storage, and distribution to divisional and nondivisional units operating in the corps area. This organization will function, if required, as the SIMLM for the task force/theater. (2) The MEDLOG battalion (rear) provides Class VIII logistical support to echelons above corps (EAC) and the MEDLOG battalion (forward). This organization has the capability for single-vision and multivision optical lens fabrication. This organization will function, if required, as the SIMLM for a joint task force/theater. P.27 Commander's Guide to Combat Health Support US Army PAM-40-19 (3) The TMMMC has primary responsibility for providing centralized theater-level inventory management of Class VIII logistical support to the theater. It may also serve as executive agent (SIMLM) for Class VIII supply and materiel for other services in the theater. (4) The MEDLOG support detachment provides Class VIII supply, single-vision optical lens fabrication, and medical equipment maintenance augmentation capability to MEDLOG battalions where work load or special operations require an increment of less than a battalion-sized unit. c. Medical logistics support is normally a Service responsibility. However, in joint operations, a SIMLM may be designated to provide central logistical support to all participating Services in the combatant CINCs area of responsibility. As the dominant user, the U.S. Army has been formally tasked by DOD to perform the peacetime SIMLM mission in the European and Korean theaters. Under wartime or crisis conditions, the U.S. Army, in all probability, will be the dominant Class VIII user and must plan for the SIMLM mission. d. The Theater Army Medical Management Information System provides state-of-the-art automation systems to facilitate supply management. Electronic data communications to include satellite links will be established between MEDLOG battalions, their MEDLOG forward support platoons (FSPs), theater MEDLOG organizations, and MTFs. Other enhancements to MEDLOG organizations include: global positioning systems, advanced cargo handling systems, and the application of standard bar code reading systems (in-transit visibility). 3.2 Division Combat Health Logistics System a. The MEDLOG battalion (forward) is responsible for Class VIII supply support to divisional and nondivisional medical units. The MEDLOG battalion coordinates with the corps movement control center or movement control team for movement of bulk medical materiel to supported customers. It also coordinates with the medical evacuation battalion for air movement of emergency resupply of blood products and other items of critical need to support customers. Ambulance backhaul is used to supplement divisional or corps transportation assets on an as required basis. P.28 Commander's Guide to Combat Health Support US Army PAM-40-19 b. Requests for Class VIII resupply in the division are supplied via push packages using unit distribution (UD). This UD is from the MEDLOG battalion (forward) through the division/brigade/regimental medical supply office, forward support battalions (FSBs), forward support medical company (FSMC), and down to the BASs. c. An FSP of the MEDLOG battalion (forward) establishes a MEDLOG base to receive and distribute Class VIII push packages and blood to medical elements deployed in the divisional area of operations. The MEDLOG FSP has the capability of handling emergency line item requests from supported customers. The MEDLOG FSP will push Class VIII preconfigured packages to the division medical supply office (DMSO). d. In the division, brigade, and regimental support areas, Class VIII resupply is performed by the division/brigade/regimental medical supply offices. These elements coordinate with the division medical operations center (DMOC), division support command (DISCOM), for transportation of Class VIII to the forward areas. As a secondary means of transportation, ground ambulances are utilized to backhaul Class VIII supplies. e. Each FSMC operates a secondary Class VIII supply point in the BSA for the emergency resupply of maneuver battalions and other medical elements on an area basis. Emergency requests are forwarded to the FSMC by any available means. If the request cannot be filled from stock on hand, it is passed to the supporting DMSO. 3.3 Corps Combat Health Logistics System a. The MEDLOG battalion (forward) is the Class VIII manager in the corps area. This unit provides Class VIII support to corps and division units using forward positioned elements. The MEDLOG battalion (forward) provides medical supply support to division medical units through the DMSO and to the DMSO by UD of preconfigured resupply (push) packages. b. Medical supply support to the ASMB and hospitals in the corps area is accomplished primarily by line item requisition and UD from the MEDLOG battalion (forward). In the ASMBs area of responsibility, medical resupply support to other medical elements and nonmedical units is accomplished on P.29 Commander's Guide to Combat Health Support US Army PAM-40-19 an area support basis. c. The authorized stockage list (ASL) for the MEDLOG battalion (forward) is established based on the programmed force structure and equipment densities consistent with theater policy. A Medical Standby Equipment Program (MEDSTEP) is maintained at the MEDLOG battalion (forward) to support medical equipment maintenance repair programs. d. The corps MEDLOG battalion (forward) is supported by line item requisition from the theater MEDLOG battalion (rear), local procurement, and contracting and throughput from the wholesale medical supply system. e. In a single corps theater, the MEDLOG battalion (forward) must be prepared to perform the Class VIII management functions of the TMMMC; the MEDLOG battalion may also assume the role of SIMLM for the joint theater. 3.4 Echelons Above Corps Combat Health Logistics System a. The MEDLOG battalion (rear) provides Class VIII supplies and blood support to EAC and MEDLOG battalions (forward). The MEDLOG battalion (rear) will use forward positioned elements (MEDLOG area support platoon) to accomplish its mission. The MEDLOG battalion (rear) uses line item requisition to supply the MEDLOG battalion (forward) and other major customers. The MEDLOG battalion (rear) maintains preconfigured push packages in support of the MEDLOG battalion (forward). Medical supply support for other EAC medical/nonmedical units is provided on an area basis by the ASMB. b. The ASL for the MEDLOG battalion (rear) is established based on programmed force structure and equipment densities. The ASL at the MEDLOG battalion (rear) will be consistent with TO policy. A MEDSTEP is maintained at the MEDLOG battalion (rear) to support medical equipment maintenance programs for corps and EAC units. c. The MEDLOG battalion (rear), in support of joint and/or combined operations, performs the SIMLM in conjunction with the TMMMC. d. The TMMMC is the Class VIII supply, medical maintenance, blood, and contracting manager for the theater. It provides the link between the P.30 Commander's Guide to Combat Health Support US Army PAM-40-19 wholesale system and the theater for Class VIII supplies. Using automated systems, the TMMMC manages Class VIII materiel, contracting services, and end items. The TMMMC maintains in-transit visibility, redirects shipments, and directs theaterwide cross-leveling of Class VIII assets in joint and/or combined operations. e. The MEDLOG support detachment is modular in design and capable of augmenting the CHLS structure at any echelon in the theater. The MEDLOG support detachment provides organizational and operational flexibility through its modular design to meet peak logistical work loads. The detachment augments the MEDLOG battalions (forward and rear) as an additional FSP or an area support platoon. Additionally, individual sections of the detachment are used to tailor specific functional missions such as reconstitution or temporary increases in medical equipment maintenance or optical fabrication requirements. 3.5 Medical equipment maintenance support a. Medical equipment maintenance capability in the division consists of operator- and unit-level maintenance at the FSMC and the main support medical company (MSMC). The FSMC has a medical equipment repairman who performs unit-level medical equipment maintenance on the FSMCs medical equipment and unit-level equipment maintenance to units without organic maintenance support on an area basis. The MSMC has two medical equipment repairmen assigned to the DMSO. The DMSO provides unit-level equipment maintenance to the MSMC and direct support medical equipment maintenance to the FSMC; it provides unit-level/direct support medical equipment maintenance to units without organic maintenance support on an area basis. These repairmen are responsible for scheduled services, equipment repair, documentation, maintenance of the medical prescribed load list and ASL, and equipment publications, and for coordination for evacuation of unserviceable capabilities. equipment or equipment whose repair exceed their b. At corps level, the MEDLOG battalion (forward) provides direct support maintenance to the DMSO and to corps-level medical units through their FSPs. It provides unit-level/direct support maintenance to units without organic maintenance support on an area basis. The DMSO coordinates with the MEDLOG FSP for the evacuation/repair of medical equipment which exceed P.31 Commander's Guide to Combat Health Support US Army PAM-40-19 their capabilities. The MEDLOG battalion (forward) receives direct support and general support from the MEDLOG battalion (rear). c. In the COMMZ, the MEDLOG battalion (rear) provides general support maintenance on medical equipment for the MEDLOG battalion (forward). It provides direct and unit-level maintenance, on an area basis, for medical units in the COMMZ. The MEDLOG battalion (rear) coordinates with the TMMMC for the evacuation of medical equipment which exceed their capabilities to CONUS (U.S. Army Medical Materiel Agency). 3.6 Optical Combat Health Logistics System a. Division. (1) The optometry section of the MSMC is responsible for providing single-vision fabrication and limited eyewear repair to Echelons I and II units in the supported division. If appropriate materials are not available at the MSMC or the prescription exceeds the MSMC fabrication capability, it is passed to the MEDLOG battalion (forward) for fabrication with return of the prescription to the originator. (2) The FSMC will request replacement of corrective eyewear from the MSMC via the best communications available with delivery back to the request originator. Prescriptions which cannot be filled from on-hand stock or which exceed the MSMC capability are passed to the MEDLOG battalion (forward). (3) Separate brigades and ACRs have optometric support with limited eyewear repair capabilities but no optical fabrication capabilities. All requests for prescription eyewear are forwarded via data link to the MEDLOG battalion (forward) for fabrication and return to the originator. b. Corps. (1) The optometry section of the ASMB is responsible for providing single-vision fabrication and repair of corrective eyewear for units on an area basis. Medical treatment elements supported by the ASMB will request replacement corrective eyewear via electronic data links to the ASMBs optometry section. Prescriptions which exceed its capabilities are passed P.32 Commander's Guide to Combat Health Support to the MEDLOG US Army PAM-40-19 battalion (forward) for fabrication with delivery back to the ASMB. (2) The MEDLOG battalion (forward) provides single-vision optical lens fabrication to divisional and nondivisional units operating in the corps area. All prescriptions requested from the MEDLOG battalion (forward) optical section that cannot be filled are passed to the MEDLOG battalion (rear) with delivery of the request to the originating medical activity. Medical logistics support detachment optical fabrication modules provide additional temporary capabilities when required. c. EAC. The MEDLOG battalion (rear) provides single-vision and multivision support to EAC and general support (backup) to the corps. The MEDLOG battalion (rear) modular design allows its optical section to relocate as necessary to support the TO. 3.7 Blood management a. Blood support is a combination of four systems (medical, technical, operational, and logistical) and should be considered separately from clinical laboratory support. The management and distribution of resuscitative fluids in the TO, including blood and blood products, are functions of combat health logistics. The management of blood and blood products incorporates storage and distribution plans that encompass rigid time-sensitive specifications. In the mature theater, blood management is based on resupply of needs from the CONUS donor base. In a developing theater, during the buildup period, blood requirements may include the use of pre-positioned frozen blood stockpiles. These stocks are designed to meet initial blood requirements until the logistical system can deliver liquid blood to the TO. When supply channels open, frozen blood utilization normally will no longer be required. b. Blood and blood products enter the theater through the U.S. Air Force (USAF) Blood Transshipment Centers (BTCs) for further distribution to the Army blood bank platoons located in the MEDLOG battalions (forward or rear). Army MTFs are supplied required blood products from the blood bank platoons. MASHs operating in divisional areas and Echelon II medical treatment elements are supplied by the FSP of the MEDLOG battalion (forward). Liquid blood, limited to Group O red blood cells, is issued as P.33 Commander's Guide to Combat Health Support US Army PAM-40-19 required down to divisional medical companies. c. Blood follows: and blood product support to the TO is provided by echelon as (1) Echelon I. No blood product support is provided at this echelon. (2) Echelon II. Blood storage and transportation refrigerators are used by the FSP to provide Group O red blood cells to divisional units. The FSP is supplied by the blood bank platoon assigned to the corps MEDLOG battalion (forward). (3) Echelon III. (a) Each MASH is limited to Group O red blood cells only. Each CSH stores red blood cells of various groups and types; additionally, limited quantities of other blood products are available. Each Echelon III hospital has an emergency blood collection capability but does not have the capability to perform serological testing of the donor units (i.e., hepatitis, human immunodeficiency virus (HIV), and syphilis testing). All Echelon III hospitals are routinely supplied with blood and blood products by a blood bank platoon assigned to the MEDLOG battalion. (b) The blood bank platoon is resupplied from a supporting USAF BTC. The blood bank platoon leader serves as the Corps Blood Program Officer. He or she manages blood and blood products through a system of specific blood report formats. (4) Echelon IV. Each FH and GH stores liquid blood products of various groups and types. Blood distribution and reporting is similar to that for Echelon III hospitals. The blood bank platoon assigned to the MEDLOG battalion (rear) is resupplied from a supporting USAF BTC. The platoon leader may also serve as the theater Army blood manager until the TMMMC is operational. (5) Echelon V. The Army blood support system is an integral part of the Armed Services Blood Program. Upon mobilization, donor centers and CONUS MTFs increase their blood drawing capabilities as directed by the Army P.34 Commander's Guide to Combat Health Support Blood Program US Army PAM-40-19 Officer. Additional donor centers are opened as required. All of these facilities draw, process, and prepare blood and blood products for shipment to the Armed Services Whole Blood Processing Laboratory who sends the blood to the TO. d. Blood collection in the theater is governed by theater policy, but normally is done to provide platelets for emergency situations. Testing of blood drawn in the theater is not currently available. P.35 Commander's Guide to Combat Health Support US Army PAM-40-19 4.0 Medical Intelligence Subtopics 4.1 What is medical intelligence? 4.2 Health service intelligence resources 4.3 Combat health support planning in historical examples 4.4 Criticality of medical intelligence 4.1 What is medical intelligence? Medical intelligence is that product resulting from the collection, evaluation, analysis, and interpretation of foreign medical, biotechnological, and environmental information. It includes intelligence on-a. Endemic and epidemic diseases, public health capabilities, and the quality and availability of health services. standards and b. Medical supplies, medical services, health service facilities, and the number of trained CHS personnel. c. Environmental conditions. d. Foreign animal transmissible to humans. and plant diseases, especially those diseases e. Health problems relating to the use of local food supplies. f. Medical effects of and prophylaxis for chemical and biological and radiation. agents g. The impact of newly developed foreign weapons systems as they relate to casualty production. 4.2 Health service intelligence resources a. In the normal course of duty, medical personnel at all echelons may gain information of medical intelligence value. Medical personnel are responsible for reporting information gained through casual observation of P.36 Commander's Guide to Combat Health Support activities in US Army PAM-40-19 plain view during the discharge of their duties. This does not violate the law of war obligation of the U.S. nor constitute grounds for denial of protected status to medical personnel. For additional information on medical intelligence, see FM 8-10-8. b. Requests for medical intelligence and requirements for military intelligence of medical interest should be accomplished through the command's supporting intelligence staff element, or the military intelligence analytical elements. (Some of these elements are the echelon above corps intelligence center (EACIC) and the tactical operations center support element.) c. There is no medical intelligence or health service intelligence analytical and production capability within the theater. There is a military intelligence officer that performs medical intelligence functions located in detachment O of military intelligence units at EAC. However, the primary focus of this officer is the exploitation of weapons, equipment, and other material found, captured, or acquired within the theater. Medical intelligence officers and NCOs at medical command, medical brigade, and medical group level will be required to fill the void in the absence of additional health service intelligence analytical resources. A special health service intelligence analytical cell may be established within the theater at medical command, medical brigade, and/or EACIC. Other possible health service intelligence resources include: (1) DMOC. (2) ASMB. (3) Medical battalion (evacuation). (4) MEDLOG battalion (forward). (5) MEDLOG battalion (rear). (6) AML. (7) PVNTMED elements. P.37 Commander's Guide to Combat Health Support US Army PAM-40-19 4.3 Combat health support planning in historical examples Studying the medical threat of past battles or military experiences provides us with information concerning the type and quality of water supply, endemic/epidemic diseases, effects of heat and cold, flora and fauna, operational and combat stressors, chemical agents, and terrain. Some historical examples of military experiences attributed to proper or improper planning are-a. French wars. Some of the greatest fiascoes in military history resulted from a breakdown in sanitation and disease control. Even though history holds Napoleon as a military genius, he often failed to preventive measures to protect the health of his troops. take (1) For example, in 1803 when Napoleon sent a force of 22,000 men to suppress a rebellion in the French Colony of Haiti, 20,000 men died from yellow fever. As a result, Haiti achieved independence with little French opposition and from Napoleon's lack of good judgment in sending a force into an area where yellow fever was epidemic. There was no vaccine against yellow fever or any other prophylactic measure to control the disease. (2) Another example of Napoleon's lack of good judgment occurred in 1813 when he invaded Russia with a force of 480,000 men. Although he succeeded in taking Moscow, the guerrillas, a lack of provisions, disease (particularly typhus), and cold injuries decimated his troops and forced his retreat. As a result, only 10,000 men returned to France. Of the 470,000 men lost in battle, only 60,000 men were killed in action; the remainder either abandoned Napoleon's army or died of disease and cold injuries. b. World War I. (1) As an example of the benefits accrued from heeding the lessons of past military experiences, consider the disease of tetanus. During World War I, the soil in France was particularly rich in bacteria that caused tetanus which was a constant danger to those wounded in action. The British occupational troops, for example, had a tetanus rate of 52 per 1,000 wounded. Of these casualties, 90 percent died. Although the tetanus P.38 Commander's Guide to Combat Health Support US Army PAM-40-19 antitoxin had been developed before the war, British medical authorities did not immunize their troops because of the uncomfortable side effects--chills, fever, and injection pain caused by the antitoxin. The U.S. Army recognized this medical threat and immunized its troops with the tetanus antitoxin prior to deploying to France. Consequently, the U.S. Army had negligible tetanus rates, saving many soldiers' lives. (2) Chemical agents were used extensively throughout the war. Countless chemical agents were experimented with; however, the chemical agents that were most effective and thus most often used were phosgene and mustard. Numerous medical personnel suffered from cross contamination with mustard during patient treatment. This put tremendous burden on health care capabilities. It is unfair to judge the errors committed in the past based on the knowledge subsequently gained from the experience. This experience, however, taught the AMEDD that CHS personnel must protect themselves first from the effects of these chemical agents. Since warfare has become increasingly sophisticated, this caution also applies to self-protection from the effects of NBC weapons. (3) Prior to deploying the American Expeditionary Force to Europe, the Surgeon General sent a medical team to collect lessons learned from our new British and French allies. The psychiatrist on that team reported the major problems the allies had were with"psychiatric casualties" (called "shell shock" or "war neurosis" at that time). The U.S. Army adopted the same techniques and organization which the allies had found effective in preventing overevacuation, maximizing RTD, and minimizing chronic disability. A psychiatrist was allocated to each division. Special medical units behind the division had the sole function of providing brief treatment for evacuated cases. A special base hospital provided longer treatment for required cases. c. World War II. (1) Combat psychiatry. The system for preventing and treating stress casualties which had worked in World War I was forgotten. It had to be rediscovered and recreated in World War II after an epidemic of stress casualties had been overevacuated from the North African and Pacific Theaters. Those incidents proved again that stress casualties who are P.39 Commander's Guide to Combat Health Support overevacuated seldom RTD and are US Army PAM-40-19 very likely to develop permanent disability. Cases that are treated immediately, close to their units, with positive expectation of rapid recovery have good RTD rates. (2) Togatabu Island. The 134th Artillery and the 404th Engineer Battalions were part of a task force preparing to attack Guadalcanal in 1942. Fifty-five percent of the engineers and 65 percent of the artillerymen contracted a disease called filariasis which is transmitted by mosquitoes. Both units were medically evacuated without seeing any enemy action. The use of an insect repellent would have prevented this. (3) Merrill's Marauders.Merrill's Marauders, officially known as the 5307th Composite Unit (Provisional), served in Burma during World War II from January through June 1944. It was an all-volunteer force of 3,000 men who pioneered long-range penetration tactics in jungle and mountain terrain behind enemy lines. Despite an extensive training program and the soldiers' combat experience, most fell prey to a variety of diseases including malaria, dysentery, exhaustion, and respiratory infections. Soldiers with high fever were evacuated and medical officers were ordered to treat most soldiers in the field. One entire platoon cut the seats from their pants because severe diarrhea had to be relieved on the move. After an initial successful attack on Myitkyina Airfield on 17 May, the majority of Merrill's Marauders were forced to be evacuated to a base for treatment and rest. d. The French Campaign in Indochina, the British experience in Malaya, and World War II experiences in relation to the U.S. experience in Vietnam. In Vietnam, official and professional attitudes toward skin diseases were much the same as they were in previous wars--essentially benign neglect until experience revealed that these apparently trivial conditions could cause an enormous substantial drain on medical resources. amount of disability and create a (1) During the French Campaign in Indochina (1945 to 1954), skin diseases created an enormous drain on manpower and caused a great deal of suffering. Fungal infections were most frequent and were followed in precedence by staphylococcal infections. Streptococcal infections were rarer. There were no effective means of preventing any of these infections. P.40 Commander's Guide to Combat Health Support US Army PAM-40-19 (2) In the late 1940's and well into the 1950's, British forces were actively engaged in counterinsurgency operations in the Malayan jungles. They suffered a great deal from skin diseases. This experience afforded a chance to observe militarily important skin diseases under circumstances similar to those that would prevail in Vietnam. However, as we note from the U.S. experience in Vietnam, the U.S. Army missed the lessons of history. (3) In Vietnam, the U.S. suffered an enormous drain on manpower and a great deal of suffering because of skin diseases just as did the French in 1945 to 1954 and the British in the Malayan jungles in the 1940's and 1950's. The U.S. Army could have diminished suffering and temporary disability resulting from skin diseases among infantrymen if they had learned the lessons of history from French and British experiences. Likewise, many of the same problems faced by the U.S. Army and its allies in World War II reappeared in Vietnam. The most important of these were that-(a) The medical statistical cutaneous disease problem. system failed to reveal the size of the (b) Well-trained and highly motivated physicians often were unable to properly diagnose and treat the most common skin disorders. (c) Educational programs and materials concerning militarily important skin diseases were grossly inadequate. (d) Research and development programs were not appropriately focused and supported until after skin disease became a serious problem. (e) A system for provision of consultant coverage was not devised at the start of the war as it had been for other classes of disease, but was instituted only after the situation had reached epidemic proportions. e. Vietnam. The U.S. Army leaders thought they had solved the problem of stress casualties with the policy of setting a fixed (365 day) combat tour with permissive rest and recreation leave. Those measures, coupled with P.41 Commander's Guide to Combat Health Support other operational US Army PAM-40-19 procedures, made traditional "combat exhaustion " rare in relation to wound casualties. What we did not realize was that our individual rotation plans and other leadership policies seriously undermined unit cohesion. Furthermore, the guerrilla/terrorist tactics of the enemy deliberately sought to create ambiguity, frustration, boredom, and tension. Their intention was to provoke misconduct combat stress behaviors which would turn the local and U.S. population and world opinion against the U.S. And indeed, frustration and rage over the inability to distinguish friend from foe among the Vietnamese led to the commission of criminal atrocities. The breakdown in unit cohesion resulted in incidents of threatening and even killing unpopular unit members and leaders. By late 1972, 60 percent of all medical evacuations from Vietnam were " neuropsychiatric cases," mostly related to substance abuse. The failure to correctly identify and counteract the special stressors of the conflict contributed to the ultimate failure of U.S. policy objectives in Vietnam, even though our combat forces were not defeated in the field. f. Operation "Urgent Fury" in Grenada. As recently as 1983, in their rush to plan and conduct this contingency operation, military planners overlooked the significance of the medical threat in the area of operations. As a result, U.S. forces suffered from preventable injuries, incapacitation, and degradation of performance. Because the medical threat was not examined or analyzed prior to the operation, proper preventive measures were not taken. Had this obvious oversight not been made-(1) The lightweight jungle fatigue uniforms would have been issued to U.S. forces. (The troops deployed wearing the battle dress uniform which proved to be much too heavy and hot. The lightweight jungle fatigue uniforms were subsequently sent from Fort Bragg, North Carolina, but not before U.S. forces suffered numerous heat casualties.) (2) Provisions for sufficient amounts of insect repellent, aerosol insecticide, and bed nets would have been made. (The troops quickly used the small quantities of insect repellent with which they deployed in an effort to combat the swarms of mosquitoes and other jungle insects that feasted on their bodies.) (3) The U.S. forces would have been cautioned to protect themselves P.42 Commander's Guide to Combat Health Support US Army PAM-40-19 against a species of extremely aggressive fire ants. (Some troops were not careful around this dangerous insect which claimed many victims.) (4) The U.S. forces would have been warned to stay away from indigenous poisonous vegetation such as the manchineel tree. (Some soldiers developed large blisters on their bodies after sweeps through the jungle and underbrush. Early reports of this alarmed the task force leadership. They thought that a chemical agent that burns and blisters the skin and damages the respiratory tract had been employed by enemy forces. Just as the leadership was prepared to order mission-oriented protective posture level 4, the local inhabitants and a PVNTMED officer with tropical plant background confirmed the problem--the manchineel tree. Inhabitants in the Caribbean avoid this tree and its fruit because the caustic sap can greatly irritate one's skin and eyes.) (5) Water discipline would have been emphasized throughout deployment. The incorrect assumption that potable water would be readily available led to-- the (a) Inadequate resources to supply water. (b) Insufficient command emphasis sufficient amounts of safe water. on ensuring that troops 4.4 Criticality of medical intelligence Medical intelligence is critical to strategic and tactical planning and operations to conserve the fighting strength and return injured soldiers to duty. See FM 8-10-8 for a complete discussion to include the requesting and reporting channels of medical intelligence. It is a highly technical area which must retain its integrity so that the end product technically accurate and contains all required information. a. At the strategic level, medical intelligence contributes significantly to the formulation of national and international policy predicated in part on foreign military and civilian capabilities of the medical/biological scientific community. b. At the tactical level, the objectives of medical intelligence P.43 are to drank is Commander's Guide to Combat Health Support provide technical US Army PAM-40-19 intelligence evaluation and analyses of the following factors in the theater: (1) Conditions concerning people or animals. (2) Epidemiological information, flora, fauna, and sanitary conditions. (3) The enemy's field medical delivery system. (4) New weapons systems planning factors. (5) Medical aspects from NBC weapons. or employment methods that could alter CHS of the employment, weapon fills, and contamination (6) The enemy's state of health. P.44 Commander's Guide to Combat Health Support US Army PAM-40-19 5.0 Law of Land Warfare Provisions Affecting Medical Operations Subtopics 5.1 Law of land warfare 5.2 Medical implications of Geneva Conventions 5.1 Law of land warfare a. Sources of the law of land warfare. (1) The law of land warfare is drawn from two sources: (a) The first is treaty law. Treaties are formally enacted under procedures set out in the U.S. Constitution. They are laws of the highest order and statutes and regulations must comply with them. They govern all U.S. soldiers and civilians. (b) The second source of the law of war is customary international law. Once a practice is internationally accepted, either by widespread treaty enactment or other agreement, it becomes customary international law. Once this occurs, it regulates even countries which do not agree with the concept concerned. (2) In the area of CHS, the principal treaties are the Geneva Convention for the Amelioration of the Condition of the Wounded and Sick in Armed Forces in the Field, 12 August 1949, and the Hague Resolutions. These are found in DA Pam 27-1. FM 27-10 is a handbook reference which will provide answers to commanders' questions concerning the law of war. b. Geneva Convention for the Amelioration of the Condition of the Wounded and Sick in Armed Forces in the Field (GWS). The GWS provides for protection of armed forces members and other persons who are wounded and sick on the battlefield. It directs members of the conflict to take all possible measures to search for and collect the wounded and sick; to protect them against pillage and ill treatment; to ensure their adequate care; and to search for the dead and prevent their being despoiled. It further provides for the protections afforded AMEDD personnel. P.45 Commander's Guide to Combat Health Support US Army PAM-40-19 5.2 Medical implications of Geneva Conventions a. Provisions for collection of wounded and sick.Provisions must be made for the collection and treatment of wounded and sick personnel, whether friend or foe, military or civilian, regardless of legal status. Only urgent medical reasons will determine priority in the order of treatment to be administered. This means that wounded enemy soldiers may be treated before wounded Americans or allies. For enemy personnel wounded as a result of military operations, dual responsibilities must be carried out--custodial and medical. The custodial activity of guarding the wounded prisoner of war (PW) should be carried out by assets other than AMEDD personnel. Medical personnel should devote their time to the special medical tasks for which they are trained. The echelon commander will designate nonmedical units to act as guards when EPW are in medical channels. b. Accountability and custody of enemy prisoners of war (Geneva Convention Relative to the Treatment of Prisoners of War, 12 August 1949) (GPW). EPW evacuated through medical channels must be identified and their accountability established prior to evacuation per appropriate tactical standing operating procedure (TSOP). Sick, injured, and wounded prisoners may be evacuated through normal medical channels, but they are segregated from U.S. and allied personnel. They may also be evacuated through dedicated or task-organized evacuation assets, particularly in rear areas where they are likely to be moved in a group. c. Responsibility and handling of PWs. The U.S. Army is responsible for the care and treatment of EPW from the moment of capture. Below brigade level, these prisoners are handled by combat troops who bring them to the designated EPW collecting points. EPW patients are evacuated from the CZ as soon as possible. Only those sick or wounded prisoners who would run a greater health risk by being immediately evacuated may be temporarily kept in the CZ. When intelligence sources indicate that large numbers of EPW may result from an operation, medical units may require reinforcement to support the additional EPW patient work load. In this case, the care of the EPW wounded becomes a joint matter between the ground combat commander and the medical commander. Procedures for estimating the medical work load involved in the treatment and care of EPW are described in FM 8-55. For a more detailed discussion on the administration, handling, treatment, and P.46 Commander's Guide to Combat Health Support US Army PAM-40-19 identification of EPW, see AR 190-8, FM 8-10, and FM 19-40. d. Identification and protection of medical personnel. (1) Personnel exclusively engaged in the performance of medical duties in connection with the sick or wounded in medical units or establishments shall wear, affixed to the left arm, a water-resistant brassard/arm band bearing the distinctive emblem (the red cross on a white background) prescribed by the Geneva Convention. The wearing of brassards/arm bands will be at the discretion of the tactical commander in far forward areas. (2) Medical personnel are to carry a special identity card, DD Form 1934 (Geneva Conventions Identity Card for Medical and Religious Personnel Who Serve in or Accompany the Armed Forces), issued to all persons qualifying as protected medical personnel. (See AR 640-3.) It is carried in addition to their regular identification card. (3) Enemy military medical personnel who are captured are considered retained personnel and not PWs. They will receive the benefits and protection of the Geneva Conventions and may be required to treat PWs. Medical personnel or medical units that are captured would do likewise, continuing to provide medical support behind enemy lines. In such a situation, this would probably be a primary source of treatment for U.S. PWs, although enemy wounded could also be treated. (4) Enemy civilian medical personnel who are physicians, surgeons, dentists, nurses, or medical orderlies may be asked, but not forced to use their medical knowledge in the interest of PWs. These medical personnel are protected persons under the Geneva Conventions, as are persons regularly and solely engaged in the operation and administration of civilian hospitals. (5) Personnel protected as medical personnel under the GWS must be exclusively engaged in medical duties or administration of medical units. This covers all members of a medical unit to include cooks, mechanics, drivers, or administration personnel. However, this protection is given only if the soldier is exclusively engaged in medical duties. Performance of any nonmedical duty removes the protection and the DD Form 1934 must be P.47 Commander's Guide to Combat Health Support US Army PAM-40-19 withdrawn. For example, if an ambulance driver is tasked with driving an unmarked vehicle forward with ammunition prior to evacuating casualties rearward, the driver would not be exclusively engaged in medical duties and could not be considered or credentialed as "medical personnel." e. Self-defense. (1) Medical personnel may carry arms for defense of themselves and their patients. This does not mean that they may resist capture or fire on an advancing enemy. It means that, if the enemy is attacking and ignoring the distinctive emblem displayed by the medic or the medical unit, the medic may provide self-protection. Of course, it is preferable attempt to avoid capture by withdrawal. and proper (2) The arms that medics may use are only defensive arms. regulation, these are defined as service rifles (M-16 series) and pistols. Other U.S. Services restrict arms to pistols alone. to By Army (3) An overall defense plan does not require medical units to take offensive action against enemy troops at any time. If a medical force is part of a defensive area containing nonmedical units, the medical unit's personnel (that is, all personnel assigned or attached to that unit) will not routinely be responsible for manning part of the overall perimeter. If located in isolation, the medical unit may provide its own security if other support is not available. A medical unit should not be defended from capture even if military police or other soldiers are manning the defensive perimeters. (4) If medical personnel fire on enemy troops (other than as described in (1) above) or otherwise abuse their protected status, they may lose their special status under the law of war. It is also possible that such a violation could result in a war crimes trial by a capturing force. For instance, if an enemy force was advancing on a marked medical facility but was not firing on it and medical personnel then took advantage of the situation and fired on the enemy, this would be an offense. Under the law of war, this action would constitute an act of perfidy or treason. It would be akin to firing on soldiers exposed under a flag of truce. P.48 Commander's Guide to Combat Health Support US Army PAM-40-19 f. Marking of medical units/facilities and ambulances. (1) Medical units and facilities. (a) The distinctive flag (red cross on a white background) of the conventions shall be hoisted only over such field medical units and facilities (except veterinary) as are entitled to be respected under the convention, and only with the consent of the tactical commander of a brigade-size or larger unit. The marking of facilities and the use of camouflage are incompatible and should not be attempted concurrently. Use of the red cross is authorized. The camouflage of medical units is regulated by Army regulations and also, in the European theater, by North Atlantic Treaty Organization Standardization Agreement (NATO STANAG) 2931. It is not envisioned that fixed, large medical facilities would be camouflaged. The commander must be aware of who has the authority to order camouflage and for what period it may last. The camouflaging of medical facilities, to include ground ambulances and air ambulances while on the ground, is more difficult to reconcile with operational necessities. The problem has been present in past wars, but is now more critical because of the ability of intelligence assets to see deep into the rear area of operations. If the failure to camouflage endangers or compromises the tactical operations, the camouflage of medical facilities may be ordered by a NATO commander of at least brigade level or equivalent. Such an order is to be temporary and local in nature and is countermanded as soon as circumstances permit. (b) The camouflage of a medical unit does not deprive it of protection. However, the enemy is not required to respect a camouflaged facility until he recognizes it as such, so the protection is illusory to a point, especially where indirect fire weapons are involved. The use of defensive arms by medical personnel at a camouflaged site attacked by ground maneuver forces poses a dilemma. The medics should attempt to make the attackers aware of their status rather than fighting back. However, that may be difficult to do on the modern battlefield. (c) If medical facilities are used to commit acts harmful to the enemy, the protection of those facilities may be withdrawn if the acts are not stopped after warning. This might be the case where a facility is used as P.49 Commander's Guide to Combat Health Support an observation post, US Army PAM-40-19 or if combat information was reported or relayed through the facility. (2) Ambulances. (a) Air and ground ambulances will be marked with the distinctive red cross emblem. While there is no legal reason why the ambulances could not have the red cross removed and then be used for nonmedical roles, two points must be remembered. First, as stated above, the aviators and drivers may not do nonmedical tasks without losing their medical status under the Geneva Conventions. Second, some of our ambulances have a distinctive silhouette used by no other vehicle. In many cases, the red crosses may not be visible in low light, over long distance, or through certain sighting devices while the vehicle is nonetheless recognizable as an ambulance. As such, the policy that benefits the mission to the greatest degree is to use ambulances exclusively for medical tasks. (b) It is the Surgeon General's policy that crew-served weapons not be mounted on ground ambulances or air ambulances, even if mounting brackets are present. (c) Vehicles other than ambulances may be used in dual roles, moving wounded to the rear under removable red crosses. However, the red crosses must be removed before nonmedical tasks are attempted, and care must be taken that the protection provided by the red cross is not abused. g. Civilians--wounded and sick (Geneva Convention Relative to the Protection of Civilian Persons in Time of War, 12 August 1949) (GC).Civilians who are wounded or become sick as a result of military operations will be collected and provided initial medical treatment in accordance with theater policies and transferred to appropriate civil authorities as soon as possible. All those wounded and sick as a result of an armed conflict will be collected and cared for. All medical treatment should be documented and appropriate witness signatures obtained. Department of Labor (DOL) Form CA 1 (Federal Employee's Notice of Traumatic Injury and Claim for Continuation of Pay/Compensation) and DOL Form CA 2 (Notice of Occupational Disease and Claim for Compensation) should be provided to any civilian injured or ill as a result of military P.50 Commander's Guide to Combat Health Support operations. The echelon commander US Army PAM-40-19 and medical unit commanders jointly exercise responsibilities for the custody and treatment of the sick, injured, or wounded enemy personnel and detained civilian personnel. h. Captured medical supplies and equipment. Because medical supplies and equipment captured from the enemy are considered neutral and protected, they are not to be intentionally destroyed. If these items are considered unfit for use, or if they are not needed for U.S. and allied forces, noncombatants, or EPW patients, they may be abandoned for enemy use. Since captured medical personnel are familiar with their own medical supplies and equipment, the captured items are especially valuable in the treatment of EPW. Use of these captured items for EPW and the indigenous population helps to conserve other medical supplies and equipment. When the capture of U.S. medical supplies and equipment by enemy forces is imminent, these items are not to be purposely destroyed. Every attempt must be made to evacuate them. Those items which cannot be evacuated are abandoned; however, such abandonment is a command decision. i. Compliance with the Geneva Conventions. (1) As the U.S. is a signatory to the Geneva Conventions, all medical personnel should thoroughly understand the provisions that apply to CHS activities. Violation of these Conventions can result in the loss of the protection afforded by them. Medical personnel should inform the tactical commander of the consequences of violating the provisions of these Conventions. (2) Outright violations of the Geneva Conventions result when-(a) Medical personnel are used to man any offensive-type weapons or weapons systems. (b) Medical personnel are ordered to engage enemy forces other than in self-defense or in the defense of patients and MTFs. (c) Crew-served weapons are mounted on a medical vehicle. (d) Mines or booby traps are placed in and P.51 around medical units and Commander's Guide to Combat Health Support US Army PAM-40-19 facilities. (e) Hand grenades, light antitank weapons, grenade launchers, or any weapons other than rifles and pistols are issued to a medical unit or its personnel. (f) The site of a medical unit is used as an observation post, a fuel dump, or an ammunition storage site. (3) Possible consequences of violations described in (2) above are-(a) Loss of protected status for the medical unit and personnel. (b) Medical facilities attacked and destroyed by the enemy. (c) Medical personnel being considered PWs rather than when captured. retained persons (d) CHS capabilities are decremented. (4) Other examples of violations of the Geneva Conventions include-(a) Making medical treatment decisions for the wounded and sick on any basis other than medical priority, urgency, or severity of wounds. (b) Allowing the interrogation of medically contraindicated. enemy wounded or sick even though (c) Allowing anyone to kill, wounded or sick enemy soldier. torture, mistreat, or in any way harm a (d) Marking nonmedical unit facilities and vehicles with the distinctive emblem or making any other unlawful use of this emblem. (e) Using medical vehicles marked with the distinctive Geneva Emblem for transporting nonmedical troops, equipment, and supplies. (f) Using a medical vehicle as a tactical operations center. P.52 Commander's Guide to Combat Health Support US Army PAM-40-19 (5) Possible consequences of violations described in (4) above are-(a) Criminal prosecution for war crimes. (b) Reprisals taken against our wounded in the hands of the enemy. (c) Medical facilities attacked and destroyed by the enemy. (d) Medical personnel being considered PWs rather than when captured. P.53 retained persons Commander's Guide to Combat Health Support US Army PAM-40-19 6.0 Personnel Subtopics 6.1 Personnel Reliability Program 6.2 Physical profiling 6.3 Physical Performance Evaluation System 6.4 Medical Evaluation Board 6.5 Physical Evaluation Board 6.6 Professional Filler System 6.1 Personnel Reliability Program a. On a tactical battlefield, the possibility of nuclear and chemical weapons employment can be planned for and defended against knowledgeable, well-trained personnel. In peacetime, however, worldwide terrorism presents the possibility of unplanned weapons use or threat of such use by groups determined to disrupt governments and blackmail nations. Minimizing this possibility, as well as protecting these devices from accident, becomes the primary objective of the nuclear and chemical surety programs. Support of these programs by the AMEDD falls principally in the area of personnel reliability. b. The Personnel Reliability Program (PRP) identifies nuclear and chemical duty positions and provides a means to assess the reliability of individuals being considered for (and during) their assignments to these positions. A nuclear surety program (see AR 50-5) includes those controls, procedures, and actions which contribute to the safety, security, and reliability of nuclear weapons without degrading operational performance. The program must also contribute to the assurance that there will be no nuclear weapons accidents, incidents, unauthorized detonations, or degradation's of weapon performance at the target. A chemical surety program (see AR 50-6) includes those controls, procedures, and actions which contribute to the safety, security, and reliability of chemical agents and their associated weapon systems throughout their life cycle without degrading operational performance. c. A nuclear/chemical surety officer is designated by the commander of a medical department activity, a medical center, and all dental activities. P.54 by Commander's Guide to Combat Health Support US Army PAM-40-19 The nuclear/chemical surety officer manages the PRP. This officer acts as the liaison and/or point of contact for PRP units and serves as a member of the Nuclear Surety Board. d. Requirements of the PRP include identifying nuclear/chemical duty positions by checking the nuclear/chemical duty position roster which is updated annually or upon changes and furnished to the supporting personnel office, medical activity or contract physician, dental facility, and alcohol and drug control officer. A preassignment screening of an individual's medical and dental records is performed by the losing unit prior to that individual's departure. These positions are under continual evaluation and when the following disqualification's are observed, they are immediately reported to the individual's commander: (1) Alcohol abuse or dependence. (2) Drug abuse or dependence. (Personnel who have used a hallucinogenic drug with a potential for "flashback " --lysergic acid diethylamide (LSD), phencyclidine (PCP), or other substances with similar properties--will neither be selected nor retained in the PRP under any circumstances.) (3) Negligence or delinquency in duty performance. (4) Nonjudicial punishment. (5) Conviction(s) by a military or civil court of a serious offense. (6) A pattern of behavior or actions that is reasonably indicative of a contemptuous attitude toward the law or other duly constituted authority. (7) Any significant physical or mental condition, as substantiated by competent medical authority, or any characteristic or aberrant behavior that, in the judgment of the certifying official, is prejudicial to reliable performance of the duties of a particular chemical PRP position. (8) Poor attitude or lack of motivation. (9) Inability to wear protective clothing and equipment required by the P.55 Commander's Guide to Combat Health Support US Army PAM-40-19 assigned position (only in a chemical duty position). e. Individuals are medically evaluated to determine physical and mental condition and qualifications under the standards of the PRP. The evaluation will be based on medical history and health records (if current and comprehensive) for this purpose. Dental records need not be evaluated as part of the initial screening process. Medical records are personally screened by a U.S. military medical officer, a U.S. civilian physician under DOD contract or employed by the U.S. Government, or other qualified medical personnel. If insufficient or questionable information is found, the individual's medical record is referred to a military medical officer or civilian physician for evaluation. The certifying official or the reviewing authority will be advised of potentially disqualifying information. If disqualifying information is found, Part II of DA Form 3180-R (Personnel Screening and Evaluation) (see AR 50-5 and AR 50-6) is prepared and signed by the screening facility officer in charge or an officially designated representative. When information is attached that may preclude assignment of the individual, the attachment must be signed by the evaluating physician or military PA. The DA Form 3180-R and its attachments will be returned in a sealed envelope marked " EXCLUSIVE FOR" the certifying official. The medical officer or civilian physician will not decide the suitability of a candidate. The certifying official will make the decision. The final decision will be based on a thorough review of pertinent information provided and consultation with appropriate medical personnel. An individual may be temporarily disqualified (temporary prescription for controlled drug) or permanently disqualified (alcohol or drug abuse or dependence). f. After the personnel and medical records have been screened, the certifying official will review the DA Form 3180-R and any attached information furnished by personnel or medical officers. The certifying official will ensure that a valid personnel security investigation has been completed or initiated and determine if the candidate is acceptable for the PRP. A determination of unsuitability may be made at any time during the screening process. (1) The certifying official will complete DA Form 3180-R, Part III, for an individual found acceptable. P.56 Commander's Guide to Combat Health Support US Army PAM-40-19 (2) The certifying official will brief the individual on the importance of nuclear weapons duties in general, rather than the details of a specific assignment, if the individual is scheduled for school training or for a nuclear duty assignment in another unit. (3) The certifying official will brief an individual unit nuclear/chemical duties. being assigned to (4) An individual will be permanently disqualified if the certifying official makes a determination of unsuitability. The certifying official will complete Part V of DA Form 3180-R after final action by the reviewing authority. g. Upon receipt of a completed copy of DA Form 3180-R showing an individual is qualified for the PRP, the individual's health record, outpatient record, and dental record will be identified in accordance with AR 40-66. If records are maintained in an Army MTF, the DA Form 4515 (Personnel Reliability Program Record Identifier) will be inserted in the Military Personnel Records Jacket. The following records, when present and maintained apart from the health record, must also be identified: (1) Inpatient treatment records. (2) Clinical Psychology Individual Case Files. (3) Social Work Individual Case Files. (4) Alcohol and Drug Abuse Rehabilitation Files. h. Continuing evaluation of personnel is absolutely essential to the PRP. Personnel in nuclear/chemical duty positions and those who function in support of the program must observe and report immediately to the certifying official any incident or condition that might result in restriction from PRP duties or disqualification in the program. This includes prompt notification of any prescribed medication that may tend to detract from the ability of an individual to perform assigned nuclear/chemical duties. Oral or telephonic notification will be confirmed P.57 Commander's Guide to Combat Health Support US Army PAM-40-19 in writing. i. Nuclear and chemical surety programs must rely heavily on AMEDD support in the area of personnel screening for the PRP. It is essential, therefore, that AMEDD personnel receive proper training for duty execution and maximum program support. 6.2 Physical profiling a. The physical profile system is a standardized medical rating system. It is based upon the function of body systems and their relation to military duties. Since the analysis of the individual's medical, physical, and mental status plays an important role in assignment and welfare, not only must the functional grading be executed with great care, but also the descriptions of medical, physical, and mental deviations from normal must be clear and accurate. This information will assist you and your personnel officer in the determination of individual assignments or reclassification actions. b. In developing the system, the functions are categorized under six factors. (1) Physical capacity or stamina (P). (2) Upper extremities (U). (3) Lower extremities (L). (4) Hearing and ears (H). (5) Eyes (E). (6) Psychiatric (S). c. Four numerical designations are assigned for individual's functional capacity in each of the six factors. evaluating the (1) An individual having a numerical designation of "1 " under all factors is considered to possess a high level of medical fitness. P.58 Commander's Guide to Combat Health Support US Army PAM-40-19 (2) A physical profile "2" under any or all factors indicates that an individual possesses a medical condition or physical defect which may require some action. (3) A profile containing one or more numerical designators of"3" signifies that the individual has one or more medical conditions or physical defects which may require significant limitations. The soldier should receive assignments commensurate with his or her physical capability for military duty. (4) A profile serial containing one or more numerical designators of "4" indicates that the individual has one or more medical conditions or physical defects of such severity that performance of military duty must be drastically limited. The numerical designator "4" does not necessarily mean that the soldier is unfit because of physical disability as defined in AR 635-40. When a numerical designator "4 " is used, there are significant assignment limitations which must be fully described if such an individual is returned to duty. d. An individual who is issued a permanent physical profile with a numerical factor of "3" in one or more of the physical profile serial factors will be mandatorily referred for evaluation to an MOS Medical Retention Board (MMRB) through the Physical Performance Evaluation System (PPES). However, if the soldier does not meet the retention standards of AR 40-501, chapter 3, the soldier will be referred directly to a Medical Evaluation Board (MEBD) and will not be reviewed by an MMRB. 6.3 Physical Performance Evaluation System The PPES establishes operating procedures that will upgrade the physical quality of the force and ensure that each individual is physically qualified to perform in his or her primary MOS or specialty code in a worldwide field environment. The system provides for an MMRB to serve as an administrative screening board to determine if an individual with a numerical designator of "3" under the physical profile can perform satisfactorily in his or her primary MOS. Based on the recommendations of the MMRB, an individual may be-- P.59 Commander's Guide to Combat Health Support US Army PAM-40-19 a. Retained in his or her primary MOS or specialty code. b. Reclassified by Headquarters, Department of the Army (HQDA). c. Placed on probationary status for 6 months so a commander can evaluate the soldier's ability to perform in his or her primary MOS. d. Referred to the Army's physical disability system, beginning with MEBD. the 6.4 Medical Evaluation Board The MEBDs purpose is to determine the physical and mental fitness of military patients. The MEBD will refer soldiers to the Physical Evaluation Board (PEB). The PEB determines if a soldier is fit or unfit for duty. If a soldier is determined to be unfit, the PEB will make recommendations for disability discharge or retirement. Cases that require evaluation by the MEBD involve-a. Patients who are referred to the PEB for medical disability. b. Patients whose fitness or unfitness for duty is controversial. c. Patients who have a progressive disease or condition in which a claim may be made against the Government. d. Reservists is questionable. whose fitness for duty upon completion of hospitalization e. Patients whose mental competency is questionable. 6.5 Physical Evaluation Board a. The purpose of the PEB is to investigate all disability cases referred to the board and to provide a full and fair hearing for the individual. After examining line of duty findings, the PEB determines eligibility benefits. A line of duty "no " determination may result in discharge of the individual without disability benefits. The board will recommend appropriate disposition of the individual or determine percentage of disability, if appropriate. P.60 Commander's Guide to Combat Health Support US Army PAM-40-19 b. Based on the findings of the PEB, an individual is returned to duty if physically fit with or without a profile. The MEBD only makes a recommendation on fitness; the PEB is the decision-making authority. An individual found unfit by the PEB can be placed on the Temporary Disability Retired List or on the Permanent Disability Retired List. The individual receives a lump sum of money for a less than 30 percent disability if not retirement eligible. Note. Administrative, not medical, channels are the most expedient means of removing an individual from your unit and the Army. It can take as long as a year or more to remove an individual through medical channels. Check with your patient administrator if you have any questions. 6.6 Professional Filler System a. In April 1980, The Surgeon General approved the concept of establishing a predesignated AMEDD Professional Filler System (PROFIS) to augment personnel staffing of units in Europe and Korea and CONUS units deploying during the deployment to deployment plus 40 days time frame. The primary feature of the predesignation system is the distribution of requirements, which remains relatively constant. The designation of unit commanders, chief nurses, and other key personnel is accomplished by the Office of The Surgeon General. The designation of MEDCOM units to provide filler personnel is accomplished by the MEDCOM. In conjunction with AR 220-1, commanders who provide designated filler personnel for the PROFIS will send feeder information to the gaining unit commander, including-(1) Preparation of replacements for overseas movement. (2) Area of concentration (AOC) qualification of designees. b. Although it is not mentioned in AR 220-1, some units request that sex gender also be included. These rules also apply for those MEDCOM units which are providing personnel for the Korean Augmentation Package. Specific guidance concerning these requirements has been published by the MEDCOM. c. Although the filler system involves all six AMEDD corps, the P.61 major Commander's Guide to Combat Health Support impact on MEDCOM officer assets US Army PAM-40-19 will be on medical and nurse corps staffing. It is obvious that a personnel drawdown of the magnitude necessary to support a European scenario would have a severe impact on the command's ability to receive and treat casualties returning from the TO. Therefore, significant backfill from Reserve Component units and individuals, as well as preassigned retirees, is of the utmost necessity. P.62 Commander's Guide to Combat Health Support US Army PAM-40-19 7.0 Training Subtopics 7.1 Expert Field Medical Badge 7.2 Initial unit training and sustainment training 7.3 Combat lifesaver 7.4 Field sanitation team training 7.5 Medical proficiency training 7.6 The Joint Medical Readiness Training Center and the Combat Casualty Care Course 7.7 U.S. Army physician assistant 7.1 Expert Field Medical Badge a. The Expert Field Medical Badge (EFMB) is intended to recognize medical personnel who attain high degrees of professional skill and proficiency as field medics. It rewards medical personnel who can expertly perform common soldier tasks and apply the principles of basic medical care in a field environment. This badge also promotes esprit de corps and provides an incentive for greater effort as well as quality training for AMEDD personnel. b. The badge may be awarded to individuals who meet the following eligibility requirements and pass all test components. Individuals classified as conscientious objectors are exempt from weapon requirements. (1) Officers must be assigned to one of the six AMEDD corps. This includes Army officers in training at the Uniformed Services University of the Health Sciences (USUHS). It also includes Army officers enrolled in the Health Professions Scholarship Program. (2) Warrant officers must have an AMEDD primary MOS. Warrant officer pilots are also eligible if they have a "D " special qualifications identifier (aeromedical evacuation pilot) and are assigned to an air ambulance unit. (3) Enlisted personnel must also have an AMEDD primary MOS. This includes all MOSs in the 91 career management field and the 18D Special Operations Medical NCO from the 18 career management field. (See AR 611-201 for a P.63 Commander's Guide to Combat Health Support US Army PAM-40-19 complete list of the 91 career management field.) c. As prerequisites, candidates must-(1) Volunteer for the EFMB test. (2) Be recommended by their unit commander. (3) Qualify with their assigned weapon or their M16-series rifle. (4) Have a passing Army physical readiness test score in accordance with AR 350-15. (5) Meet height and weight standards under provisions of AR 600-9. d. Those authorized to administer the EFMB test and award the badge are-(1) Commanders of Active Army, U.S. Army Reserve, and Army National Guard TOE medical units in the rank of lieutenant colonel or above. (2) Commanders in DISCOMs without medical battalions. (3) Regiment and separate brigade commanders who have the resources and facilities to conduct all test phases prescribed by TC 8-100. (4) Surgeons at corps level and above, lieutenant colonel and above. e. In order to be awarded the badge, candidates must successfully complete the required number of tasks in each of the following 11 critical performance areas: (1) Comprehensive written test.Each candidate must correctly answer 75 of 100 performance-oriented multiple choice questions. (2) Army physical readiness test.Each candidate must achieve a composite score of 180 points or higher with a minimum of 60 points in each of the following three events: push-ups, sit-ups, and a 2-mile run. Alternate events are not authorized. P.64 Commander's Guide to Combat Health Support US Army PAM-40-19 (3) Land navigation. Each candidate must successfully complete a day and a night land navigation course. (4) Weapons qualification. Each candidate must qualify with his assigned weapon or the M16-series rifle within the previous year. or her (5) Communications. Each candidate must successfully demonstrate comprehensive knowledge of field radios and radio techniques. (6) Survival. Using the M16-series rifle, each candidate must demonstrate knowledge of survival skills in an NBC environment and a combat situation. (7) Forced road march. Each candidate must complete a 12-mile road march within 3 consecutive hours. (8) Emergency medical treatment.Each candidate must demonstrate skills in the treatment of various wounds under simulated combat conditions in a battlefield scenario. (9) Evacuation of sick and wounded. Utilizing a variety of vehicles and manual carries, each candidate must demonstrate evacuation techniques under simulated combat conditions in a battlefield scenario. (10) Litter obstacle course.Candidates will be formed into four-person litter teams. Each team, while being tested under simulated combat conditions in a battlefield scenario, must correctly negotiate three out of four obstacles on a litter obstacle course. (11) Cardiopulmonary resuscitation. Using the one-soldier method, each candidate must demonstrate proficiency in cardiopulmonary resuscitation. 7.2 Initial unit training and sustainment training a. The 91B10 Initial Unit Training Package contains instructional materials to train 91B10 critical and mission-essential tasks. All medical specialists (MOS 91B10) are required to complete this new training. Request training materials from the Commander, U.S. Army Medical Department Center and School, ATTN: MCCS-HSN, Fort Sam Houston, TX P.65 Commander's Guide to Combat Health Support US Army PAM-40-19 78234-6100. b. Maintenance of soldiers' skills within their MOS is mission essential. Many soldiers, particularly medical soldiers, perform duties outside their MOS. To maintain MOS proficiency, sustainment training materials are available. The unit furnishes time, equipment, and instructors to provide unit training programs. Exportable sustainment packages for Self-Aid/Buddy Aid, 91B10, 91B30, and Area Support Cross Training, 91C, are available from the Commander, U.S. Army Medical Department Center and School, ATTN: MCCS-HSN, Fort Sam Houston, TX 78234-6100. c. Correspondence courses are available from Commander, U.S. Army Medical Department Center and School, ATTN: MCCS-HSN, Fort Sam Houston, TX 78234-6100. Correspondence courses are generally programmed for individual, self-paced study, but they may be used in the group study mode. (See DA Pam 351-20 for a complete listing of correspondence courses.) 7.3 Combat lifesaver a. The concept for the combat lifesaver was developed as part of the CHS portion of AirLand Battle doctrine. The combat lifesaver is a nonmedical soldier trained to provide enhanced first aid as a secondary mission. The primary mission of this soldier does not change. All combat units employ the combat lifesaver concept. Normally, one member of each squad, crew, team, or equivalent-sized element is a combat lifesaver. CS and CSS units may also train personnel to serve as combat lifesavers in their units. The combat lifesaver provides an intermediate level of first aid between the self-aid/buddy aid skills taught during basic training and the combat medic. b. The combat lifesaver course (listed in DA Pam 351-20) is offered only in the group study mode and is conducted at the unit level. The training program is managed by a senior medical person designated by the unit commander. The course involves prestudy of self-aid/buddy aid tasks and 3 days of classroom instruction/testing. Days 2 and 3 consist of additional training in selected medical tasks such as initiating intravenous infusions and providing initial care to soldiers with BF. Students must pass written and performance examinations in order to become combat P.66 Commander's Guide to Combat Health Support US Army PAM-40-19 lifesavers. Qualified combat lifesavers require annual recertification. Unit commanders wishing to enroll students in the combat lifesaver course must apply to the Army Institute of Professional Development, U.S. Army Training Support Center, ATTN: ATIC-IPS, Newport News, VA 23628-0001. 7.4 Field sanitation team training a. The standard Field Sanitation Team Training Module was developed by the PVNTMED Division, AMEDDC&S, after numerous requests from the field and with extensive support from field units. The module consists of 13 lessons which provide the field sanitation team with the information to contribute to maximizing the fighting strength of their unit. b. This course is designed for 40 hours of hands-on and classroom instruction. AR 40-5 requires that at least two people be on a unit field sanitation team and that one of those individuals be an NCO. If organic medical personnel (91B) are available, these personnel should be appointed as the field sanitation team. Successful completion of the 40-hour field sanitation team certification training course will earn soldiers (private through sergeant) two promotion points. This course appears in DA Pam 351-20 and is usually offered by local PVNTMED assets, such as those organic to divisions and separate brigades, by separate TOE PVNTMED detachments, or by host installation medical department services. activity PVNTMED 7.5 Medical proficiency training a. The purpose of medical proficiency training is to help soldiers possessing a medical MOS and assigned to a TOE unit to train and sustain the proficiency of those tasks which are not routinely performed in a TOE environment. However, current medical proficiency training programs are decentralized and vary widely among the installations conducting the training program. To eliminate this problem, HSC (now the MEDCOM) and the U.S. Army Forces Command signed a Memorandum of Understanding (MOU) authorizing the development and implementation of the Army Medical Department Systematic Modular Approach to Realistic Training, a standardized tool for use in the medical proficiency training program. This standardized training tool is a means to provide hands-on, documented training by using MOS-specific modules/tasks which contain individual, nonfield (clinical) tasks. These modules/tasks assist the MTF trainers in P.67 Commander's Guide to Combat Health Support US Army PAM-40-19 providing standardized sustainment training to TOE soldiers during their 90-day rotation at the MTF. Tasks are listed according to training days; similar or related tasks are placed together as they would be performed or trained. Tasks to be trained are a combination of soldier's training publication tasks, Army Training and Evaluation Program tasks, and other tasks referred to as " clinical" --that is, medical tasks performed in an MTF. b. The TOE commander provides soldiers to be trained. The commander also provides the MTF with mission-essential tasks. This item is just one of many details which must be agreed upon in advance by the TOE and MTF commanders as they develop, sign, and implement a local MOU. The establishment of training requirements and responsibilities and negotiated terms of the agreement are essential for providing the best possible training to the soldier. 7.6 The Joint Medical Readiness Training Center and the Combat Casualty Care Course The Joint Medical Readiness Training Center (JMRTC) is a triservice organization providing (under the auspices of the AMEDDC&S) medical readiness training for officers and selected enlisted personnel from all Active and Reserve Components. The Combat Casualty Care Course (C( 4) ) is the primary course presented by the JMRTC. a. The C( 4) is controlled by the Joint Medical Readiness Education Council (JMREC), which is chaired by the Deputy Assistant Secretary of Defense for Medical Readiness. The membership in the JMREC consists of a flag rank representative from The Surgeon General's office of the Departments of the Army, Navy, and Air Force; flag rank or colonel representatives from the Services' Reserve Component medical departments; and a member appointed by the President, USUHS. The AMEDDC&S, the U.S. Marine Corps, and the U.S. Public Health Service also participate as observers. b. The purpose of C( 4) is to prepare medical department officers to function on an integrated battlefield at the forward points of the casualty care system. The practical goal is to develop skills to the level where casualties can be successfully assessed and treated to RTD in the P.68 Commander's Guide to Combat Health Support US Army PAM-40-19 shortest possible time, or be evacuated to the rear as conditions of the individual and the environment dictate. Practical exercises are also used to introduce and develop skills required of medical staff officers. c. Some of the specific areas of emphasis are as follows: (1) Advanced trauma life support (ATLS). This is the standard ATLS course (from the American College of Surgeons) teaching initial assessment and management of the trauma victim through large group lectures and small group, practical, hands-on training. (2) Field exercises stressing participative training in NBC warfare defense and the identification of medical limitations in NBC environment. (3) Participation in day and night tactical maneuvers giving the student the opportunity to practice the applications of medical concepts and skills in a field environment. (4) Medical officer responsibilities to the commander regarding the assessment of the medical threat to combat forces, combat stress, and the prevention of diseases and nonbattle injuries. d. The C( 4) is conducted in residence as a 9-day consecutive course. It is also presented as a nonresident course in phases, so that personnel from the Reserve Components can complete the course during either weekend drills or annual training. (1) The resident course is conducted at Camp Bullis, Texas, and the AMEDDC&S, Fort Sam Houston, Texas. The students are divided into 12-person squads and live in tents and hutments under field conditions. All equipment required is issued at Camp Bullis. courses annually with 144 officers per class. There are presently 17 (2) With one exception, the nonresident course content is the same as that of the resident course. In the nonresident course, a variety of academic medical education courses may be substituted for ATLS. Examples are advanced burn life support, medical management of chemical casualties, combat anesthesia, and deployment medicine. The course is broken into three phases which can be taken in any order. The course can be P.69 Commander's Guide to Combat Health Support US Army PAM-40-19 completed on weekends over a 1- to 3-year period or during one period of annual training. e. The JMRTC also conducts the Combat Casualty Management Course. This is an 8-day course for senior medical department officers and is offered twice yearly in residence. Some of the major areas emphasized are an in-depth review of war wound management; how medical regulating and the evacuation policy affect critical resources; medical logistics; medical intelligence; and refugee medical problems. 7.7 U.S. Army physician assistant a. The U.S. Army PA course is conducted by the AMEDDC&S, Fort Sam Houston, Texas. The PA course trains Active Component and National Guard personnel who meet the criteria delineated in DA Cir 601-94-3. Applicants are selected by a DA selection board. b. The PA course is a 2-year, multiphased baccalaureate program through affiliation with the University of Texas Health Sciences Center, San Antonio, accredited by the Committee for Allied Health Education Agencies. Phase I is a didactic phase taught at the AMEDDC&S; Phase II is a 1-year clinical practicum taught at various AMEDD activities. A baccalaureate degree is granted by the University of Texas upon completion of the course. Certification by the National Commission for Certification of Physician Assistants is required to be commissioned into the Army SP (AOC 65D). Following completion of the PA course, graduates are required to attend the AMEDD officer basic course. c. The purpose of the PA course is to prepare candidates to-(1) Serve as primary care providers (under the direct supervision of a physician) for combat and CS battalions, troop medical clinics, outpatient clinics, emergency rooms, and other primary care facilities. (2) Provide ATM and care for nonbattle injuries for soldiers during peacetime and times of hostility. (3) Function as special staff officers to commanders of combat and CS battalions and frequently as medical platoon leaders of those battalions. P.70 Commander's Guide to Combat Health Support US Army PAM-40-19 d. The PA is an appointed primary medical care expert who manages the following battalion medical activities: (1) Training. (2) Sick call. (3) Medical support. (4) Tactics. (5) Logistics. (6) Special staff support. (7) Emergencies. (8) Deployment. (9) Medical planning. (10) PVNTMED. (11) Occupational health. (12) Wellness. P.71 Commander's Guide to Combat Health Support US Army PAM-40-19 8.0 Soldier Health Maintenance/Current Health Problems Subtopics 8.1 Soldier health maintenance elements 8.2 Sleep 8.3 Stress 8.4 Alcohol/drug abuse 8.5 Suicide prevention 8.6 Immunizations/prophylaxes 8.7 The Oral Health Fitness Program 8.8 Sexually transmitted diseases 8.9 Acquired immunodeficiency syndrome 8.10 Occupational safety and health 8.11 Field sanitation team 8.12 Army Aviation Medicine Program (flight surgeon) 8.13 Veterinary services 8.14 Nutrition 8.1 Soldier health maintenance elements Physically and mentally fit soldiers are a vital element of your unit's operation. If the soldiers are physically and mentally fit, they are less likely to be a combat loss from disease or injury. To ensure the fitness of your personnel, you should employ the unit's field sanitation team and your supporting surgeon, flight surgeon, PA, CSC personnel, and dental, PVNTMED, and veterinary services in monitoring-a. Sleep. b. Stress. c. Alcohol/drug abuse. d. Suicide prevention. e. Immunizations/prophylaxes. f. The Oral Health Fitness Program. P.72 Commander's Guide to Combat Health Support US Army PAM-40-19 g. Sexually transmitted diseases (STDs). h. Acquired immunodeficiency syndrome (AIDS). i. Occupational safety and health. j. Food wholesomeness. k. Nutrition. 8.2 Sleep a. Sleep is not a luxury, but a necessity for adequate mission performance. While you and your unit can go for 2 or 3 days without sleep to accomplish urgent mission objectives and counter enemy threats, considerable risk is involved. Care must be taken to protect critical task performance with "counterdegradation " or "counterfatigue" measures. With increasing sleep loss, physical strength remains unimpaired, but coordination, alertness, mental ability, and motivation deteriorate. Tasks take longer to perform. The likelihood of serious errors increases as-(1) Signals are missed. (2) Communications become garbled. (3) Judgment falters. (4) Important task steps are neglected. b. Sleep-deprived individuals fall asleep when they should not. Their attention wanders and they are prone to accidental injury and death. If kept awake, they begin to have visual hallucinations and see, very vividly, things which are not there--often what they wish or fear to see. They may also suffer temporary delusions. This is not a sign of mental illness but of insufficient sleep. However, it can endanger you, other unit personnel, and the mission. c. Not every individual needs to be evacuated P.73 for psychiatric care Commander's Guide to Combat Health Support US Army PAM-40-19 because of visual hallucinations or mirages. What the individual needs is a good 6 to 8 hours of sleep, although even 4 hours will be surprisingly restorative. It is your job to see that neither you nor your unit comes to this state. To maintain continuous operations beyond a few days, you must provide guidance and a command climate for a sleep plan which gives all individuals (especially those with critical thinking, decision making, and vigilance tasks) sufficient sleep. The NCOs must assure execution of the plan's details. "Sleep discipline" does not mean prohibiting sleep any more than water discipline means restricting water. Rather, it means assuring that everyone sleeps at times and in places which are safe for the individual, the unit, and the mission. The following are guidelines for your unit's sleep plan. They must, of course, be flexible to adapt to fit your resources and mission. The plan must assure short-term mission accomplishment and unit survival while enabling the unit and its members to function over a longer term. d. Do not allow sleep in unsafe places. The TSOP must specify the designated sleeping areas. When appropriate, the TSOP will outline requirements for perimeter guards and ground guides, day as well as night, for all vehicles to assure personnel safety and security. Depending on the type of threat, this may range from simple dispersion and concealment through sentries, foxholes, and slit trenches, to well dug-in bunkers with three or more layers of sandbags. Have the right TSOP for your situation. Do not relax it just because everyone is tired. e. Provide dry and comfortable sleeping areas as practical. Four hours of sleep stretched out in a sleeping bag or hammock is worth 8 hours wedged in a cramped vehicle or wet hole in the ground. f. Set shifts which give everyone 6 to 10 hours of sleep in 24 hours, when feasible. Ideally, this sleep should be uninterrupted. However, even two or three blocks of 2, 3, or 4 hours which add up to 6 to 8 hours are sufficient for continuous operations which may extend for months. g. Try to give individuals a minimum of 4 hours of uninterrupted sleep per 24 hours when 6 hours of sleep a day is impossible. If possible, give 6 hours of uninterrupted sleep to individuals who are responsible for key tasks and who are more or most susceptible to the effects of sleep loss. P.74 Commander's Guide to Combat Health Support US Army PAM-40-19 h. Allow individuals to get as much sleep as possible before going into sustained operations. Individuals cannot really"stockpile " sleep, but it pays to be well rested before starting a period of sleep deprivation. Even taking an afternoon nap before the night operation can significantly improve performance and delay the onset of deterioration. i. In sustained operations, when shifts are impossible, allow individuals to nap whenever they can do so safely. Never waste a chance for an individual to catch safe sleep. The longer the nap the better, but even 15- to 30-minute catnaps help over the longer term. However, in the short-term, be aware that most sleep-deprived individuals awaken slowly from naps. It may take them several minutes to "warm up their brains" before their alertness and mental ability are as good as they were before they went to sleep. This is especially true if the nap comes at a time when they are accustomed to going into a long sleep period such as from 2400 to 0600 hours. There are big differences in an individual's ability to awaken quickly. Know your unit and yourself and take this into account when allowing naps. j. Allow individuals to catch up on sleep after going without it. Six to 10 hours is best, but even 4 hours is surprisingly restorative, even after 96 hours of no sleep. k. Learn, practice, and teach rapid relaxation techniques such as-(1) Breathing meditation. (2) Progressive muscle relaxation. (3) Imagination of a relaxing situation. l. Skill at these techniques will be useful for taking quick restorative naps in noisy, uncomfortable, and anxiety-filled situations. The techniques also help to get back to sleep after the frightening dreams which are a normal and common reaction to combat experiences. However, individuals should not put themselves into a too relaxed state at those times when vigilance and urgent action are required. P.75 Commander's Guide to Combat Health Support US Army PAM-40-19 m. Conduct cross training in advance so that individuals with critical skills and duties can be relieved in order to sleep. Junior leaders must be trained and kept fully informed so that they can keep watch while the senior leader sleeps. After all, they may have to take over suddenly if the senior leader becomes a casualty, which is inevitable if the leader tries to go too long without sleep. n. Allow individuals who need sleep to rest in their units or in the unit's CSS trains. However, if individuals are so"keyed up" or "spaced out" that they could do harm to themselves or others (such as around weapons, dangerous equipment, or possible enemy action), allow them to use the supporting medical unit's cots. 8.3 Stress Fear and physical signs or symptoms of stress are normal reactions before, during, and after combat or other dangerous and/or life-threatening situations. Stress symptoms are also normal, although usually less obvious, in peacetime field training and garrison. Military life involves many "stressors " such as long working hours, periods of separation from family, changing job responsibilities and coworkers, and moves to faraway duty stations. Even when such events are positive, they involve uncertainty and possible cost. Other life events such as marriage, birth of children, spouse's job, and children's progress through school also create stressors, even when positive. They can interact with the military life stressors to cause distressing problems. When negative stressors such as illness or disability in the family, financial problems, or interpersonal discord are added, the normal stress process is overworked. Too much stress impairs mission performance. It can even lead to physical illness such as heart disease or ulcers and can be associated with alcohol and other drug abuse, overeating, depression, problems. or other psychological a. Stress management. Stress management is one aspect of the Army's Wellness and Fitness Program. The objective of Army stress management is not to eliminate stress but to help soldiers and their families use stress adaptively and improve their coping abilities. The peacetime mission of the Army is to prepare for combat, and combat is the most stressful of all P.76 Commander's Guide to Combat Health Support US Army PAM-40-19 human activities. b. Combat stress casualties. In heavy conventional battle, one soldier usually becomes a temporary"BF casualty" for every two to five soldiers wounded in action. More soldiers may suffer wounds, injuries, or preventable diseases because stress has impaired their ability to perform their duties and protect themselves and their buddies. BF and misconduct combat stress behaviors are not unique to combat soldiers. They also occur in CSS unit and headquarters personnel, even in those who are not directly under fire. The division mental health section (or equivalent supporting mental health team) can assist you in the prevention, treatment, and RTD or disposition of BF casualties and other harmful combat stress behaviors. Other soldiers may show misconduct stress behaviors which require disciplinary action, such as-(1) Commitment of criminal acts such as atrocities. (2) Self-inflicted wounds. (3) Desertion. c. Combat stress defense. You can promote the defenses against stress in combat through unit cohesion and tough, realistic training. Ideally, these defenses need to be developed before mobilization; but when necessary, they may be developed during deployment and even in combat. Other important stress management techniques which are part of basic good leadership include-(1) Assuring physical fitness and taking care needs. of the troops' physical (2) Keeping soldiers informed while focusing their perspective on how the unit will overcome difficulties to succeed with the mission. (3) Reassuring soldiers that home front positively. (a) Unit cohesion problems means two things. Cohesion P.77 will is be resolved the personal, Commander's Guide to Combat Health Support US Army PAM-40-19 face-to-face loyalty shared by people who work with and depend on one another. It becomes strongest when these individuals have shared and overcome difficulty, hardship, or danger. Ideally, cohesion matures over months or years, but it can develop over hours and days under intense pressure. Unit refers to a sense of shared identity in the unit and its mission. It defines not only who we are, but also what we do and how and why we do it. Cohesion alone is very strong but flexible--easy to bend but hard to break or pull apart. Unit identity is firm but brittle. Putting the two together creates a result that is much stronger than either alone. To promote unit cohesion, keep the same team members (soldiers, NCOs, and officers) working together as long as possible. Do not move them from one team to another unless absolutely necessary. Assign work details to intact teams. Encourage friendly competition in mission-oriented tasks and in sports events to emphasize the teams, not the individuals. Use awards, ceremonies, and unit-sponsored social activities to promote unit cohesion and to allow individual acquaintances. Include soldiers' families in these activities and encourage a social support network. The family support group will help these families rely on one another if the unit deploys. Intervene, when necessary, to assure that the official social support agencies work smoothly to assist your unit and their families. Using the Army Community Service, the Army Emergency Relief, the Alcohol and Drug Abuse Prevention and Control Program, and the Exceptional Family Member Program (EFMP) can be beneficial. The unit or local chaplains and the mental health personnel of the division mental health section or community mental health activity can assist with individual or marital counseling and/or referral. There must be no stigma or negative career implications attached to those who responsibly use these resources to improve the quality of their lives and their stress tolerance. (b) Unit cohesion alone is not enough. Tough, realistic training is essential. This training contributes to unit cohesion by encouraging joint working efforts for overcoming difficulty and hardship and for accomplishing the unit's mission. Suffering hardship and discomfort and successfully accomplishing the unit's mission are necessary. Tough, realistic training builds the individuals' confidence in themselves, their comrades, and their equipment. It also builds confidence in the leader's competence, candor, courage, commitment to the mission, and concern (caring) for the soldier. Training prepares the soldiers to face and P.78 Commander's Guide to Combat Health Support overcome the rigors, discomforts, US Army PAM-40-19 fears, and horrors of the combat mission. This is especially important for CSS units. Another important aspect of tough training is a routine, progressive program of physical exercise. Physical exercise develops endurance, strength, agility, and calluses in all parts of the body subjected to the demands of the mission. Master physical fitness coordinators in your unit or at the installation or garrison can advise on the most appropriate activities. Implementation of the program promotes unit cohesion and mutual confidence. d. BF. Even with all these preventive measures, soldiers will show symptoms of BF in combat or during highly stressful missions. Your unit's NCOs, medics, and combat lifesavers (if your unit has them), and officers can provide temporarily overstressed soldiers the calm reassurance and the positive expectation that they can continue their duties and are needed by their buddies. Encourage these soldiers to talk about what has happened that bothers them and to express their feelings without fear of being judged or disputed. A good listener helps them to put things back in a perspective which enables them to refocus on the unit and its mission. 8.4 Alcohol/drug abuse a. Alcohol and drug abuse remains a serious problem in the military Services. It affects combat readiness, job performance, and the health of military personnel and their families. It also costs millions of dollars in lost time and productivity and short and long term medical costs; more specifically, it affects the individual. The reasons for alcohol and drug abuse are as varied as the individuals who use them. Individuals abuse these substances to change the way they feel. They may want to feel better and happier or escape from stress, pain, or frustration. Some may want to forget, others may want to be accepted or be sociable. Other individuals abuse alcohol and/or drugs to escape boredom or to satisfy their curiosity. Peer pressure can also be a very strong motivating factor in their abuse. Individuals often feel better about themselves when they use alcohol and/or drugs, but these effects do not last. Alcohol and/or drugs never solve problems--they merely postpone and complicate them. Individuals who abuse alcohol and/or drugs to solve one problem run the risk of continued usage, which creates new problems and makes old problems worse. P.79 Commander's Guide to Combat Health Support b. You are US Army PAM-40-19 responsible for ensuring that the heavy use or abuse of alcohol and/or the abuse of other drugs is not condoned in the unit. You should not promote any official or unofficial function which glamorizes the use of alcohol through drinking contests, games, or initiations or the awarding of alcoholic beverages as prizes for contests. Nonalcoholic beverages should be readily available at military functions to provide alternatives for those who prefer not to drink alcohol. You also should promote and encourage off-duty sports, educational, cultural, religious, or spiritual pursuits as alternatives to use of alcohol and/or drugs. c. Potential alcohol and/or drug abuses in your unit are brought to your attention either by self-disclosure or by evidence provided by biochemical testing, law enforcement apprehension, command investigation, medical identification, inadequate performance attributable to intoxication or withdrawal, witness reports, or other sources. Any soldier who self-refers or who you believe may have an alcohol or drug problem must be referred immediately to the Alcohol and Drug Abuse Prevention and Control Program for assessment and treatment planning, regardless of your administrative intentions. The soldier's problem will be assessed and treatment conducted until it is no longer necessary or until the soldier is deemed unfit for duty and is subsequently separated. 8.5 Suicide prevention a. Suicide is the third leading cause of death of active duty soldiers in peacetime. Many cases of suicide may go unreported, as they can masquerade as accidents. In combat, the suicide rate tends to decrease. Aggressive drives can be channeled toward the enemy. However, some deaths due to inappropriate behavior in combat may, in reality, be suicides. Suicide among family members, including elderly parents, spouses, teenagers, and even children, is also a serious problem which impacts on the entire Army. b. Suicide turns a temporary depression (or a brief loss of self-control due to frustration, anger, or substance abuse) into a fatal illness. Even unsuccessful suicidal attempts can lead to permanent disability. The effectiveness of the entire unit suffers when one soldier or family member attempts suicide. While there is no certain way to predict and prevent all suicides, the risk can and must be kept to a minimum. Soldiers and their families may lessen the risk of suicide by using the emotional P.80 Commander's Guide to Combat Health Support support and cohesion US Army PAM-40-19 of friends and leaders. This must be directed by a caring chain of command and supported by medical personnel, chaplains, and the helping agencies. and mental health c. You are responsible for assuring that your subordinate officers and NCOs know and are alert to the warning signs of depression self-destructive thinking. They should know the kinds of stressors and situations that are often found behind cases of successful or attempted suicide. These include-(1) Loss or breakup of a love relationship. (2) Sexual problems. (3) Trouble with authority. (4) Failure. (5) Other blows to self-esteem. (6) Unwanted retirement. (7) The prospect of a chronic, painful, or disabling disease. d. Alcohol and/or drug abuse greatly increases the danger of suicide. Key emotional factors are-(1) Loneliness. (2) Lack of self-worth. (3) Strong guilt feelings. (4) The sense better. of hopelessness--the belief that things can never get (5) Anger turned inward--the urge to hurt others or to guilty by hurting oneself. P.81 make them feel and Commander's Guide to Combat Health Support US Army PAM-40-19 e. Suicide gestures or other unspoken "cries for help" should not be discounted or ignored. Most of those who have succeeded at suicide have made previous attempts or shown other signs that they have crossed that important line between thinking about it and starting to take action. Ignoring the gesture simply confirms their belief that they are alone and no one cares, while discounting its seriousness is, in effect, daring them to prove their desperation by trying something more dangerous. Anyone who makes a gesture should be evaluated by medical/psychiatric personnel. Those who are judged to be seriously suicidal must be escorted to care--they should not be left alone. f. The DA has directed commanders to educate all junior leaders and supervisors in suicide prevention. A videotape and supporting pamphlet are available at most training and audiovisual support centers. These training aids are not intended to stand by themselves, but rather to be lead-ins to an active discussion led by qualified experts such as the mental health personnel of the division mental health section or post medical activity. g. Note that suicide prevention training should be focused at the junior leaders. Caution is necessary when publicizing the topic among the junior troops since this can unintentionally"glamorize " suicide, especially in the minds of unhappy young people. Suicide is sometimes "epidemic" ; one suicide at a post or in the community may be followed by others. If a suicide or suicide attempt occurs in or near your unit, it is important for the leaders to redouble their vigilance and to actively help the troops work through their reactions. Mental health personnel and chaplains can be helpful. 8.6 Immunizations/prophylaxes a. Immunizations/prophylaxes are major components of the overall Army effort to counter the infectious disease threat. As battalion commander, you are responsible for assuring that all individuals assigned to your unit receive required immunizations/prophylaxes and that appropriate records of such immunizations/prophylaxes are maintained. You are also responsible for assuring that individuals transferred from your unit receive the immunizations/prophylaxes required in the area to which they are ordered. b. The specifics of the Army Immunization/Prophylaxis P.82 Program are established in Commander's Guide to Combat Health Support US Army PAM-40-19 AR 40-562/NAVMEDCOMINST 6230.3/AFR 161-13/CG COMDTINST M6230.4. This regulation discusses requirements for specific immunizations/prophylaxes related to-(1) Mission. (2) Geographic location. (3) Categories of persons such as-(a) Active duty. (b) Basic trainees. (c) Reserve Components. (d) Military dependents. (e) Personnel granted-1. Waivers. 2. Exemptions. c. All requirements are subject to change and amendment based upon current situations and needs. Questions regarding current specific requirements or recent changes should be directed to the local PVNTMED service at your MTF. 8.7 The Oral Health Fitness Program a. Dental maladies account for a significant amount of lost duty time. The rate of dental emergencies varies with the-(1) Amount of predeployment preparation of troops. (2) Length of deployment. (3) Intensity of conflict. (4) Amount of in-theater dental care. b. The rate of dental emergencies from Vietnam and large field training exercises ranges from 142 to 234 dental emergencies per 1,000 troops per year. c. Commanders, the dental care system, and the soldier share the responsibility for dental fitness. The primary focus of this program is to ensure that soldiers do not become "noncombat dental casualties." Within this program, the dental care system has responsibility for-(1) Fitness classification. (2) A yearly 100 percent audit of records to ensure accuracy of classification. (3) Dental treatment of soldiers to achieve a satisfactory dental fitness level. The responsibility for personnel accountability rests with installation personnel support activities and unit commanders. P.83 Commander's Guide to Combat Health Support d. The Oral Health program to Fitness Program US Army PAM-40-19 provides a structured preventive dentistry maximize dental readiness. The four dental fitness classes are-- (1) Dental Fitness Class 1--Includes soldiers who require no dental treatment. (On examination, no further dental appointments are given or recommended; for example, if there are missing teeth and no replacement is recommended, the patient is in Class 1.) (2) Dental Fitness Class 2--Includes soldiers whose existing dental condition is unlikely to result in a dental emergency within 12 months. (3) Dental Fitness Class 3--Includes soldiers who require dental treatment to correct a dental condition that could cause a dental emergency within 12 months. (4) Dental Fitness Class 4--Includes soldiers who require a dental examination. This includes soldiers who require annual or other required dental examinations and soldiers whose dental classifications are unknown. e. A commander should strive to maintain all of his or her troops in Dental Fitness Class 1 or 2. f. Full procedures and responsibilities of the Oral Health Fitness Program are described in AR 40-35. 8.8 Sexually transmitted diseases a. STDs comprise another disease category which can have a negative impact on soldiers and their effectiveness. The increase in sexual promiscuity in our society, coupled with young soldiers out of their home environment, make STDs a common military problem. Chlamydia and other forms of nongonococcal urethritis are the most common STDs followed by the familiar diseases, gonorrhea and syphilis, and a variety of others. b. STDs are generally contracted through sexual contact. Many STDs can be treated and cured with proper medical care but the risk of complications and the existence of incurable STDs such as herpes, hepatitis B, and AIDS make prevention the obvious preference. c. Punishing soldiers who acquire an STD is not only forbidden by regulation is counterproductive to the overall prevention and control effort. but d. When a soldier in your unit suspects he or she may have a problem they should-(1) Report for sick call immediately. (The longer they have the disease, the more serious it may become.) P.84 Commander's Guide to Combat Health Support US Army PAM-40-19 (2) Tell their sexual partner(s) to seek treatment. (3) Abstain from all sexual activity until the problem is resolved. (4) Follow medical instructions exactly and completely. (5) Cooperate with the STD interviewer. e. Assistance in diagnosing and treating STD can be obtained from-(1) Military MTFs. (2) Civilian health care facilities. (3) Municipal public health departments. f. Information about STDs may be obtained from the above sources and from the national hot line (1-800-227-8922). g. An effective program for controlling STDs depends on the cooperation you have from soldiers assigned to your unit. Place particular emphasis on-(1) Commanders. Commanders are responsible for initiating and maintaining an effective STD control program in their units. (2) Education of soldiers. (3) Safe sex practices. (4) Tracing of contacts. h. PVNTMED activities serve as a resource in helping you design an STD control program and may be able to provide personnel to help in the education effort. 8.9 Acquired immunodeficiency syndrome a. HIV has been identified as the etiologic agent of AIDS. The HIV infection covers a spectrum of illness from an absence of physical signs and symptoms to the most severe presentation of immunodeficiency, AIDS. The HIV antibody positive individual is considered to be infectious to other people for the rest of his/her life. b. AIDS is the condition resulting from the natural progression of infection by the virus. The body's immune system is destroyed, causing otherwise controllable infections to invade the body and cause additional diseases. These opportunistic diseases may eventually cause death. AIDS is commonly identified because of the presence of an opportunistic disease, a positive Western Blot laboratory test, and a decrease in T-lymphocytes with a profound compromise of the immune system. P.85 Commander's Guide to Combat Health Support US Army PAM-40-19 c. The last few years have seen a change in the perceived spectrum of HIV disease from that of a uniform, rapidly fatal process to more of a chronic disease, with a poor outcome, but with increasing life span and quality of life. d. Due to because-- the Army's unique mission, soldiers who have HIV must be identified (1) Soldiers who have the HIV antibody may have a deficient immune system and easily become ill from different diseases and are not deployable worldwide. (2) Soldiers are required to donate blood for direct transfusion on the battlefield and transmission of the AIDS virus could occur. Soldiers are screened for antibodies to HIV at least every 2 years. All new recruits are screened before entry into the military. Those who are screened positive are not allowed to enter the military. e. Any soldier assigned to your unit with a positive HIV test has the potential for a serious health problem. The HIV/AIDS is an infectious disease which not only has potentially catastrophic medical implications, but also has a potential for devastating psychological consequences. An individual with HIV/AIDS infection typically requires many forms of assistance in addition to routine medical care. The military community has a multidisciplinary support system to help the HIV/AIDS soldier. Some of these services includes pastoral counseling, mental health, PVNTMED (to include PVNTMED officers and community health nurses), and social services. The objective in using community resources is to assist the soldier in maintaining psychological and social well-being. f. Although there is no cure for AIDS, it can be prevented. The HIV/AIDS virus is contracted through contaminated blood or needles or through sexual contact with an individual who harbors the HIV infection. The following recommendations will help prevent the spread of AIDS: (1) Abstain from sex. (2) Do not use illegal injectable drugs. (3) Minimize the number of sexual contacts. (4) Practice safer sex. Safer sex practices means using barrier precautions such as condoms while having sex. This will help prevent the exchange of blood, vaginal secretions, or semen, the"bodily fluids" in which HIV is easily transmitted. (5) Do not donate blood if you are a potential carrier of the virus. (6) Avoid sexual contact with high risk groups--prostitutes, homosexuals, bisexuals, P.86 Commander's Guide to Combat Health Support US Army PAM-40-19 individuals with many sexual contacts, and drug abusers. g. Information, resources, and publications (in English and Spanish) about HIV/AIDS may be obtained from the National AIDS Clearing House via hot line 1-800-458-5231. 8.10 Occupational safety and health a. Congress passed the Occupational Safety and Health Act in 1970. Subsequent to the passage of the act, executive orders directed DOD to apply guidelines of the Occupational Safety and Health Act to military personnel while in garrison-type workplaces and operations--workplaces and operations comparable to those of business and industry in the private sector. Soldiers who use the correct protective procedures and equipment while in garrison-type workplace settings can continue their success related illness and injury during field training and operations. in preventing occupationally b. As a battalion commander, how does this impact upon your unit? At a recent brigade commander's staff meeting, the annual occupational safety and health injury and illness statistics were published for the division. The results indicated that over 89,000 training man-hours were lost during the past year because of occupational eye injuries alone. The cost, based on average salary per hour at the rank of corporal, was well over $200,000. c. About half of the actual man-hours lost and the associated cost could have been prevented by simply providing and requiring the use of safety eyewear. Can you afford similar losses of manpower and funds in your unit? d. A recent hearing loss survey performed by PAs of a large mechanized infantry division revealed that 30 percent of the senior tankers had suffered sufficient hearing loss and impairment to warrant reclassification to another MOS. Hearing loss is a totally preventable occupational injury/illness. What would be the impact on readiness if 30 percent of your unit suffered from hearing losses and hearing impairments and were reclassified? e. Prevention of occupational injuries and illnesses is a command program. (AR 40-5 and AR 385-10 identify some of the commander's responsibilities in these areas.) The soldier must be protected while performing his/her duties. Without protection, the effects of hazardous workplace exposures can and will prove detrimental to the combat readiness of the individual soldier and the unit. Command emphasis is imperative for the program to succeed. Command emphasis also extends to the appointment and support of unit safety officers. Instead of overwhelming junior officers with another additional duty, consider appointing more senior personnel (officers or NCOs), providing adequate training P.87 Commander's Guide to Combat Health Support for these senior personnel, US Army PAM-40-19 and delegating them the authority to make the program effective. f. Occupational injuries and illnesses can deprive you and your unit of valuable training hours and training assets. There are assets within your unit that are available to you to prevent these injuries and illnesses. The PVNTMED service of the installation MTF has occupational health assets to assist you in managing an effective program. Organic or supporting AMEDD personnel trained in occupational healthcare or industrial hygiene can identify, evaluate, and recommend corrective action for potential occupational health hazards. At the installation/division level, the safety manager can assist in the recognition and evaluation of workplace exposures. Incorporation of occupational safety and health principles into your operations produces a true "combat multiplier," reducing loss of training hours and assets by preventing occupational injuries and illnesses. 8.11 Field sanitation team Make your field sanitation team an asset you can use. It can assist you in carrying out all field sanitation tasks for protecting the health of your unit. This invaluable team is responsible for those PVNTMED measures that affect your unit as a whole or are beyond the resources of the individual soldier. This is a most important responsibility because your unit's effectiveness is greatly dependent upon its members' health. Military units are unable to carry out their missions when unit personnel are weakened by disease. The success or failure of an army, the outcome of a war, and the fate of a nation may, therefore, rest upon how well diseases and nonbattle injuries are prevented through effective PVNTMED measures in the units. The field sanitation team plays a major role in reducing diseases and nonbattle injuries. When you encounter problems beyond the capabilities of the field sanitation team, request assistance from supporting PVNTMED elements. The duties of the field sanitation team may be categorized as both basic sanitation and insect and rodent control. a. Basic sanitation. The duties of the field sanitation team include-(1) Supervising the disinfection of unit water supplies inspecting/maintaining unit water containers and the unit water trailer. and (2) Advising the unit food service personnel in the prevention and elimination of deficiencies in food service sanitation. The team instructs unit personnel, as necessary, in methods of washing individual eating utensils. P.88 Commander's Guide to Combat Health Support US Army PAM-40-19 (3) Supervising the construction of garbage and soakage assisting in inspections for proper disposal of garbage. pits and (4) Supervising the construction of field latrines and urinals assisting in the inspection for proper sanitation. and Note. A unit detail is responsible for the actual construction of field waste disposal facilities. (5) Assisting in the guidance and inspection of personnel and facilities to ensure a high level of personal hygiene. (6) Providing guidance as needed in the use of protective measures to prevent heat and cold injuries. (7) Reporting any sanitation inadequacies to you. b. Insect and rodent control.The duties of include-- the field sanitation team (1) Ensuring the practice of proper waste disposal which is essential for insect and rodent control. (2) Explaining to unit personnel the ways in which insects and rodents may affect their health and instructing them in the use of individual protective measures against insects and rodents. (3) Instructing how to properly wear the uniform to avoid insect-borne diseases. (4) Procuring and distributing components of the DOD insect repellent system (specifically, topical diethyltouluamide (DEET) formulations and permanone formulations for impregnating clothing and tentage). (5) Supervising the proper use of the DOD insect repellent system, battle dress uniform, and bed nets to prevent bites by disease vectors. P.89 Commander's Guide to Combat Health Support US Army PAM-40-19 (6) Supervising the application of authorized "General Use" pesticides for insect pests and disease vectors. (7) Inspecting to ensure the elimination of food and shelter (harborage) for insects and rodents. (8) Performing limited insect and rodent management. (9) Supervising the use of traps and authorized rodenticides as required in the control of rodents. (10) Reporting any other inadequacies. 8.12 Army Aviation Medicine Program (flight surgeon) a. The role of the Army Aviation Medicine Program is to support the Army aviation mission. The Army Aviation Medicine Program accomplishes this role by providing medical support, both clinical and nonclinical, to the aviation population to ensure individual health, flying safety, and successful mission completion. The Army flight surgeon is the program manager. b. The Army flight surgeon is a physician who is specially trained in aviation medicine. This special training ensures that medical problems and their treatment do not compromise the health and safety of personnel in the aviation environment. Underlying the need for this special training is the fact that diseases and medications which are routine on the ground may become very significant in the air, often requiring a temporary or permanent restriction from flying. The focus of aviation medicine is to apply the concepts of PVNTMED and occupational medicine (OCCMED) so that disease is detected and managed at the earliest possible stage, the aeromedical hazards of flying are minimized, and a healthy combat ready aviation force is maintained. This ensures retaining the aircrew member on flying status for the duration of a military career. As a result, the flight surgeon is trained to be uniquely qualified in aeromedical decision making and problem solving. This qualification underlies the flight surgeon's role as a combat multiplier for Army aviation. c. The clinical responsibilities of the flight surgeon can be subdivided P.90 Commander's Guide to Combat Health Support US Army PAM-40-19 into two areas of responsibility. (1) Primary care responsibilities include-(a) Providing clinical care for aviation unit personnel. (b) Providing clinical care for dependents of possible. aviation personnel, when (c) Providing a 24-hour on-call service for aeromedical emergencies and consultation for aeromedical evacuation missions. (d) Coordinating specialty evaluations to determine fitness aircrew with disqualifying medical conditions. to fly for (2) PVNTMED responsibilities include-(a) Performing periodic flying duty medical examinations and other periodic health assessments as prescribed in AR 40-501, to include aeromedical summaries and in-flight evaluations. (b) Disease surveillance in coordination with PVNTMED activity. (c) Health promotion through health risk appraisals, health education (lectures) on life-style modification, and conducting the unit health promotion programs. d. The nonclinical responsibilities of the flight surgeon encompass those aviation medicine duties which occur outside of the clinic, but in direct support of the Army aviation mission. These nonclinical duties include-(1) Unit staff officer functions.As a unit surgeon-(a) Keeps the command. aviation unit staff officer, the flight commander informed of the health of the (b) Provides advice on medical matters to commanders. P.91 Commander's Guide to Combat Health Support US Army PAM-40-19 (c) Participates in medical staff planning activities associated tactical aviation operations. with (d) Ensures that aviation unit personnel are familiar with physiological limitations of flying by conducting an aeromedical training program for the unit. the (e) Advises the commander on crew endurance limitations. (f) Serves as a member of flight evaluation boards which are convened to assess whether an officer should continue an aviation career. (2) Safety program responsibilities. Involvement in the aviation safety program means the flight surgeon-(a) Makes recommendations to improve human factors crashworthiness, and survival features of aircraft. compatibility, (b) Serves as a member of aircraft accident investigations. (c) Ensures that the medical portion of the preaccident plan is adequate and participates in accident plan exercises. (d) Takes part in aviation safety meetings to educate aviation crew members on such topics as the aeromedical aspects of flight, personal health care, and PVNTMED and OCCMED issues as they relate to the flight safety environment. (3) Aviation life support duties.Aviation life support duties require the flight surgeon to-(a) Monitor the fitting, use, and serviceability of aviation life support equipment. (b) Provide advice and training on the training for aircrew personnel. medical P.92 aspects of survival Commander's Guide to Combat Health Support US Army PAM-40-19 (4) OCCMED responsibilities.OCCMED responsibilities require the flight surgeon to-(a) Provide environmental surveillance which evaluates toxic hazards (aerial/ground), and involves monitoring the mess, latrine, alert and maintenance facilities, the flight line, and all aircraft. (b) Provide training and surveillance for a multitude of environment risks--that is, noise and vibration, stress and fatigue, heat and cold injuries, hypoxia, barotrauma, and the psychological aspects of flying. (c) Conduct frequent flight line inspections, to include inspections of air traffic control and crash rescue facilities. (d) Advise and program. assist on the unit hearing and eyesight conservation (5) Flight requirements as an aircrew requirements as an aircrew member includes-(a) Taking part in and observing flight member.Fulfilling flight operations to monitor the interactions of crew members, aircraft, and environment in all Army aircraft as allowed by regulation during all aviation duty hours, to include nap-of-the-earth missions, night vision goggle operations, aeromedical evacuations, and field exercises. (b) Meeting annual flying requirements, in accordance with AR 600-105. e. Two additional clinical missions (location-dependent) which the Army Aviation Medicine Program has responsibility for are-(1) Supporting a local aeromedical (air ambulance) evacuation unit. Support for an aeromedical evacuation unit entails-(a) Acting as the primary advisor to the local MTF commander on matters pertaining to aeromedical evacuation. (b) Participating in the care of patients during aeromedical evacuation. P.93 Commander's Guide to Combat Health Support (c) Assisting in the review of personnel. all US Army PAM-40-19 care delivered by air ambulance (d) Participating in the development and training of local flight medical aidmen. (2) Supporting a includes-- local diving mission. (a) Clinical support providing primary care Support for a diving mission and PVNTMED coverage for diving personnel. See paragraph c above. (b) Screening for decompression sickness (that is, the bends) and referring to the nearest recompression chamber. 8.13 Veterinary services a. Veterinary services can assist you in maintaining the health of your unit, both in garrison and in the field. The Army Veterinary Service is the DOD executive agent for veterinary support to all of the U.S. armed services and, when requested, to other selected Federal agencies. Doctrinally, veterinary units provide their triservice support mission on an area basis. b. Veterinary services inspect all food procured by the military, including operational rations (meals, ready-to-eat, T-rations, and so forth), to ensure wholesomeness and safety. Procured subsistence is also inspected to ensure contractual compliance and to protect the financial interests of the U.S. Government. Veterinary services initially approve the sanitation (facilities and procedures) of commercial establishments, maintain an approved list, and conduct periodic sanitary inspections and compliance procedures for sources of military subsistence to include ice and bottled water. Military funds may be used to purchase subsistence from approved sources only. This includes the expenditure of unit fund monies for food. Veterinary personnel perform sanitary inspections of approved sources to ensure food for the military is produced and stored under sanitary conditions. Military food establishments, such as commissaries, Army and Air Force Exchange Service retail outlets, troop issue P.94 Commander's Guide to Combat Health Support US Army PAM-40-19 subsistence activities, and nonappropriated fund subsistence warehouses are also inspected by veterinary personnel to ensure the proper receipt, storage, and issue of food for military personnel. c. Complete veterinary medical care is provided to all Government-owned animals. Of particular importance to most military commanders is the care given to military working dogs. Army veterinarians also provide as much care as possible to other Government-owned animals such as working and ceremonial horses, nonappropriated recreational horses, and unit mascots. Unit mascots are provided care only if the animals are appointed on unit orders. Commanders should check local regulations to determine the exact requirements for unit mascots. Veterinary personnel inspect all Government animal facilities and make recommendations concerning the feeding, housing, training, utilization, and evaluation of the animals. Veterinary services operate the veterinary treatment facilities located on military installations. Pets are authorized limited veterinary care on a time available basis. Fees charged for privately-owned animal care are under the fiscal management of nonappropriated fund instrumentalities. (See AR 40-905/SECNAVINST 6401.1A/AFI 48-131.) d. The Army Veterinary Service plays an essential role in the prevention of zoonotic diseases in the military environment worldwide. Several diseases transmitted from animals to man (for example, rabies, plague, equine encephalitis, and numerous parasitic diseases) are of significant military importance. Vaccination and other measures are provided for Government-owned animals, and a nominal charge is made for animals belonging to soldiers and their families to control zoonotic diseases in animals. Veterinary personnel make recommendations to commanders on establishing policies concerning the control of animals and the prevention and control of zoonotic diseases (diseases transmissible from animals to humans). e. In a TO, veterinary personnel can be found throughout the COMMZ and CZ where food is received, stored, and/or issued. Local sources of fresh food are also inspected. Veterinary personnel do not normally go into divisional areas. Exceptions include Troop Issue Support Activities, ration break points, and animal care in the divisional areas. Veterinary personnel inspect NBC-contaminated rations to determine which rations can P.95 Commander's Guide to Combat Health Support US Army PAM-40-19 be salvaged and to recommend decontamination procedures. Veterinary units are located throughout a TO to provide care to Government-owned animals and to assist in civic action projects. f. In all areas of operation involving operations other than war, veterinary personnel are extremely valuable health care assets. The agricultural base of other countries provides vast opportunity for the utilization of veterinary service personnel in supporting the interests of the U.S. Government in nation assistance and low intensity conflict. Veterinarians as well as veterinary animal technicians are utilized from the care and treatment of animals to development of alternate forms of agriculture and development of American "goodwill." As the utilization of DOD personnel evolves in the disaster assistance arena, Army veterinary personnel will be key in the functional areas of animal medicine and food safety and quality assurance. g. A paramount role of the Army Veterinary Service is the provision of specialty trained veterinarians in the areas of pathology, laboratory animal medicine, microbiology, physiology, pharmacology, toxicology, and surgery for Army, Navy, and Air Force biomedical research and development laboratories. Also, one-fourth of the Army Veterinary Service's animal care specialists support the DOD biomedical research laboratories. These specialty personnel conduct and support research to develop drugs and vaccines, biological and chemical defense measures, and protective measures for weapon systems hazards. h. Currently, a major component of the Army Veterinary Service CHS is from the Reserve Component. AS DOD restructures, the total number of veterinary Reserve units will decrease, and the Active Component is restructuring to provide a larger share of the support for the war-fighting commanders. Individual Mobilization Augmentees are important components of numerous veterinary units which provide professional backfill during Active Component mobilization, and supplement and conduct special projects which benefit unit commanders, and consequently installations during and as a result of periodic active duty for training. 8.14 Nutrition a. Importance of nutrition.Nutrition may be thought of as an enhancement P.96 Commander's Guide to Combat Health Support US Army PAM-40-19 to military operations. Properly planned and executed, good feeding practices in the field and in garrison maintain and enhance physical performance and morale and significantly contribute to mission accomplishment. Military personnel who establish a strong nutritional status will better endure the harsh environments encountered in today's battlefield. b. Garrison environment. (1) The nutritional goal in garrison is to optimize nutritional status so the soldier will be in the best shape possible to meet the physical and mental demands of training. Keeping a soldier"fit to win" providing sound nutrition information and healthy food alternatives. involves (2) The following Dietary Guidelines for Americans, published by the U.S. Department of Health and Human Services, provide guidance on what to eat to stay healthy. The dietitian at the installation hospital can provide detailed descriptions and information on implementing these guidelines. (a) Eat a variety of foods. (b) Maintain a healthy weight. (c) Choose a diet low in fat, saturated fat, and cholesterol. (d) Choose a diet with plenty of vegetables, fruits, and grain products. (e) Use sugars only in moderation. (f) Use salt and sodium only in moderation. (g) If you drink alcoholic beverages, do so in moderation. c. Nutrition advice for field feeding. Food plays a major role in sustaining performance and morale in the field. Commanders must assure their soldiers are provided an adequate quantity of high quality food with ample time to eat. Commanders and food service officers should work together to tailor food supplies and food management to the tactical P.97 Commander's Guide to Combat Health Support US Army PAM-40-19 situation and unit mission. (1) Inadequate ration consumption. Weight loss, both voluntary and involuntary, is quite common in the field. Soldiers often eat 20 to 40 percent less in the field due to the change from their normal routine, becoming bored with field rations after a few days, not having enough time to eat, etc. If this low food intake is not prevented, body weight loss can quickly reach a level where physical and mental performance is impaired. Weight losses of as little as 2 percent of pre-field body weight may negatively influence performance. Even if soldiers are overweight, the lower food intake may have a negative impact on performance. (a) Soldiers must be taught that adequate consumption of food and water are tactical weapons and how eating and drinking can affect their health and performance. (b) Unit leaders should watch to see what their personnel are eating or failing to eat. (c) Do not permit troops to use field deployments as a convenient way of dieting. (d) Control the use of food brought from home, "junk food," and other non-issue food. Do not allow these foods to be used as substitutes for more nutritious meals or rations. (e) Encourage soldiers to eat at least part of all the ration items served. Various components of operational rations are fortified to provide all the nutrients essential for health and fitness. (f) Establish regularly scheduled meal times if possible. Soldiers tend to eat more when they are in social groups for meals. (2) Dehydration. Soldiers who do not consume enough fluids to replace those lost from sweating and urination become dehydrated and constipated. Even mild dehydration affects performance, reduces the desire to eat, and cause lethargy. Moderate dehydration leads to diminished work capacity, and more severe dehydration may result in severe disability or even death. P.98 Commander's Guide to Combat Health Support US Army PAM-40-19 (a) Leaders should establish a program of regularly scheduled, enforced drinking in order to prevent dehydration. In general, most soldiers need to drink at least four canteens of water per day and considerably more when working in the heat. (b) Provide plenty of fluids at meal times, preferably flavored and served at appropriate temperatures for the environment. (c) Eating too much salt (sodium) may lead to dehydration. Excess salt intake increases the body's water requirement since a person must drink more water to excrete the extra salt. (d) Monitoring the color of one's urine helps determine who may be getting dehydrated. Dark yellow urine indicates inadequate fluid intake; fluid consumption should be increased until urine turns pale yellow. P.99 Commander's Guide to Combat Health Support US Army PAM-40-19 9.0 The Military Family Subtopics 9.1 TRICARE 9.2 Civilian Health and Medical Program of the Uniformed Services 9.3 Primary Health Care for the Uniformed Services 9.4 Uniformed Services Dependents Dental Insurance Plan 9.5 Family Advocacy Program 9.6 Exceptional Family Member Program 9.7 Veterinary treatment facilities 9.1 TRICARE a. Managed care is being implemented in DOD under its overriding managed care program called TRICARE. The coordinating, networking, contracting, and business improvement activities of the Army and the other Services optimize the use of all our health care resources. The objectives are improved access to health care, maintenance of the high quality care we provide, control over the costs of health care for the Government and our beneficiaries, and enhanced readiness. These objectives are particularly important during the time of defense downsizing and declining resources. We must ensure that we meet the medical mission for our forces despite the reduction of our medical force, the closing of facilities, and the dispersion of units into remote locations. b. TRICARE introduces changes into the traditional Army health care system and is the foundation upon which access, quality, cost, and readiness objectives will be met. TRICARE is the clinically directed business approach to health care. Its essential elements include division of the continental United States and Hawaii into 12 DOD Coordinated Health Care Regions and supplementing military MTF capacity with regional managed care contracts. A business plan approach contribute to efficient management of the Army and DOD medical resources and incorporate appropriate use of technology. Some of the changes visible to commanders, soldiers, and their families will include assignment of soldiers to primary care managers (PCMs), administration of Health Risk Appraisals with directed follow-up, use of telephone health care advisors and increased use of automation to process telephone calls, patient clinical records and reports and other soldier information. c. Implementation of TRICARE is an incremental process with health care delivery centered upon the local MTF supported by the contractor's network of civilian providers. Most health care is expected to be provided in the MTF. When the necessary care cannot be provided in the MTF, the providers in the local civilian and regional Federal facilities may provide the necessary care. Upon completion of full implementation of TRICARE, three options for access to health P.100 Commander's Guide to Combat Health Support US Army PAM-40-19 care will be available: (1) Health Maintenance Organization (HMO) TRICARE Prime. (a) Enrollment into the HMO-like option is conducted through the MTF. All active duty personnel are first priority and automatically enrolled in this option for care when it becomes available. (b) Soldiers and families will be administered a Health Risk Appraisal and assigned to a PCM. PCMs are either clinics (e.g., Troop Medical Clinic or Primary Health Care for the Uniformed Services (PRIMUS) clinic (para 9-3)) or individual providers who take care of the patient's first and routine needs for health care. The PCM is the designated source of care the soldier will go to first when health care is needed. Primary care providers may include physicians in Family Practice, Internal Medicine, General Medicine and Pediatrics, PAs, and nurse practitioners. The PCM will be responsible for coordinating the beneficiaries total care. PCMs operate as members of a complementary medical team which includes nurses, PAs, physical therapists, dietitians, etc. The value of assignment to a PCM is the systematic coordination and follow-up of routine care and referrals to specialists. Referrals to specialists will be facilitated by Health Care Finders who are the knowledgeable link to specialists in the TRICARE network which complements the MTF. Health promotion and disease prevention through the development of healthy and safe lifestyles receive greater emphasis, instruction, and follow-up through primary care management. The results of these activities contribute to the medical readiness of our soldiers and their families. Family members may enroll in the HMO option as primary care panels expand. (c) Beneficiary costs for enrollment in the HMO option are significantly less than standard CHAMPUS. Care received in the MTF will continue to be provided at no cost to the patient. Any costs which are incurred by beneficiaries, such as for specialist care in the network, are expected to be nominal as a benefit to enrollment in the HMO. Beneficiaries will always have the freedom of choice for care, including their referral care. However, if the choice is in conflict with the PCM recommendations or the appeals process, the beneficiary may be refused a nonavailability statement and subject to full costs for that care. (2) Preferred Provider Organization (PPO) (TRICARE EXTRA).This option allows the beneficiary more freedom of choice for the site of health care. Nonenrollees in the HMO, will continue to have access to health care in the MTF. If care is not available in the MTF, beneficiaries may use providers in the"network." These are Civilian Health and Medical Program of the Uniformed Services (CHAMPUS) (para 9-2) and MEDICARE providers who have agreed to participate within the local network. Costs to the beneficiaries who P.101 Commander's Guide to Combat Health Support US Army PAM-40-19 use the PPO are lower than standard CHAMPUS and the provider typically completes the CHAMPUS paperwork. (3) Standard TRICARE. The Standard CHAMPUS option with the deductibles and copayments directed by law is always available for eligible beneficiaries. d. In some instances, care outside the MTF must be provided by non-network providers and beneficiaries thus may not receive the discounts or administrative services described above. Health Care Finders and Health Benefits Advisors at the MTF will still be available to assist with the coordination of appointments and claims filing. e. The AMEDD recommends that unit commanders and their soldiers become acquainted with the local TRICARE Service Centers. Current information on implementation status of TRICARE and costs for care to soldiers and their families is available through this office. Soldier and Army health is a team effort of individuals, units, the AMEDD, and many other activities. Understanding how to get one's health care needs taken care of before the need arises should be a part of every soldier's personal and family readiness objectives and responsibilities. 9.2 Civilian Health and Medical Program of the Uniformed Services a. CHAMPUS is a health care entitlement program under chapter 55, title 10, United States Code, and is administered by DOD under DOD 6010.8-R. The program serves all seven uniformed Services: (1) Army. (2) Navy. (3) Marine Corps. (4) Air Force. (5) Coast Guard. (6) Public Health Service. (7) National Oceanic and Atmospheric Administration. b. The following groups are eligible for benefits: (1) Dependents of active duty personnel. (2) Retirees and their dependents. (3) Surviving spouses and children of soldiers who died while on active duty if they were under 65 years of age. Spouses who remarry are not eligible. (4) Reservists and Guardsmen between 60 and 65 years of age who are qualified to receive retired pay. (5) Surviving spouses and children of retirees. Again, spouses who remarry are ineligible. P.102 Commander's Guide to Combat Health Support US Army PAM-40-19 (6) Divorced spouses of military personnel who served at least 20 years on active duty and whose marriages covered at least 20 years of active duty and who are not enrolled in an employer-sponsored health insurance program. (7) Divorced spouses of military personnel who served at least 20 years on active duty and whose marriages covered at least 15 of those years. Individuals divorced after 1 April 1985 are limited to 2 years of DOD Health Insurance Program benefits. c. This program supplements the military's hospitals and clinics and provides medical care for retirees and their families who do not live close to a military installation. The program was never intended to duplicate medical care available at these military installations. d. Because of recent changes in legislation, CHAMPUS-(1) Protects military families from catastrophic medical expenses. (2) Provides help for psychotherapy patients. (3) Requires certification for the necessity of abortions. e. Under the catastrophic protection provision, the cost of deductibles and cost-shares in any fiscal year (FY) for family members of active duty soldiers is capped at $1,000. For retirees and their families and other CHAMPUS beneficiaries, the cap is $7,500 per FY. Charges above the "allowable " and charges for treatment not covered by CHAMPUS are not capped. The cap is not automatic; families must processor. request it from their CHAMPUS claims f. On each Army installation at the installation medical activity, a CHAMPUS advisor is available to answer questions about-(1) Eligibility. (2) Benefits. (3) Administrative procedures that must be followed before benefits can be obtained. 9.3 Primary Health Care for the Uniformed Services a. The PRIMUS Program supplements the primary health care services available at select DOD MTFs through contractor-owned and operated satellite clinics. The Navy calls these clinics"Navy Care" (NAVCARE). PRIMUS clinics also serve a key role as PCMs, thereby complementing the DODs managed care programs. The primary objective of these Congressionally-directed clinics is to increase patient access to quality primary health care while containing costs. PRIMUS clinics fulfill this objective by-(1) Providing accessible and convenient primary health care. P.103 Commander's Guide to Combat Health Support US Army PAM-40-19 (2) Reducing patient overcrowding in the MTFs primary care clinics, and, more importantly, the MTFs emergency room. (3) Improving patient satisfaction through improved access and continuity of care. (4) Reducing costs by bringing previous CHAMPUS users into the PRIMUS clinic. b. As PCMs, PRIMUS clinics provide the beneficiary a vital link to the local MTF. Beneficiaries who enroll in the HMO option are assigned a PCM. PCM assignment is normally determined by location to the beneficiary and when PCM capability exists. If a PRIMUS clinic is locally available, it may serve as the beneficiary's PCM. In this role, the clinic staff ensure continuity of care for the enrolled beneficiary. More importantly, the PRIMUS clinic is responsible for all of the beneficiary's health care needs. This responsibility can be fulfilled either by directly providing the required health care services, or if the clinic, through coordination with the local MTF. not available in c. Competitive bidding has demonstrated that these clinics can provide primary care visits at a considerably lower cost than a standard CHAMPUS outpatient visit. Such arrangements allow the Government to maximize the utilization of scarce resources in providing needed health care services. More importantly, the soldier and other eligible beneficiaries do not incur any cost-share by using these health care clinics as they are considered part of the direct care system. d. Not every MTF needs a PRIMUS clinic. Some MTFs already have ample primary care staff to meet their beneficiaries demands for health care services. The decision to pursue a PRIMUS clinic rests with the local MTF commander. If the MTF commander determines a valid need for a PRIMUS clinic, that commander must demonstrate the cost effectiveness of his/her decision. The commander's cost effectiveness study must be approved by the Medical Command before a PRIMUS clinic can be contracted. Funding for the operation of the clinic remains the sole responsibility of the local MTF. 9.4 Uniformed Services Dependents Dental Insurance Plan The Uniformed Services Dependents Dental Insurance Plan is a DOD dental program designed for families of active duty soldiers. This plan pays for basic dental services provided by participating civilian dental care providers. This is a cost-sharing insurance program in which the Government pays for part of the premium and the active duty soldier pays the remainder of the premium through a monthly payroll deduction. Contact your health benefits advisor or the dental plan insurer for information concerning the benefits of this insurance program. P.104 Commander's Guide to Combat Health Support US Army PAM-40-19 9.5 Family Advocacy Program a. The Family Advocacy Program is a program developed by the Army to— (1) Prevent spouse and child abuse. (2) Protect victims of abuse. (3) Treat families affected by abuse. (4) Assure that there are personnel who are professionally trained to intervene in abuse cases. Since many incidents of abuse constitute violations of the law, the program recognizes the commander's authority to take disciplinary or administrative action when necessary. b. The purpose of this program is to promote public awareness within the military community and to coordinate professional intervention at all levels within the civilian and military communities, including— (1) Law enforcement. (2) Social services. (3) Health services. (4) Legal services. c. The program is designed to-(1) Break the cycle of abuse. (2) Identify abuse as early as possible. (3) Provide treatment for affected family members. d. The Family Advocacy Program is a commander's program located within the Army Community Service. As a battalion commander, you should— (1) Attend spouse and child abuse command education programs designed for commanders. (2) Schedule time for soldiers to attend troop awareness briefings. (3) Be familiar with rehabilitative, administrative, and disciplinary procedures relating to spouse and child abuse. (4) Report suspected spouse and child abuse to the designated point of contact and provide all pertinent information to those investigating the report. (5) Consider all recommendations made by the family advocacy case management team. (6) Notify the chairperson of the family advocacy case management team when orders are issued reassigning soldiers or when moving family members who are involved in treatment for spouse or child abuse. (7) Encourage civilian family members to participate in treatment programs. P.105 Commander's Guide to Combat Health Support US Army PAM-40-19 e. To prevent spouse and child abuse, military and civilian agencies can provide services which-(1) Improve family functioning. (2) Ease types of stress that can aggravate or trigger patterns of abusive behavior. (3) Create a community that is supportive of families. f. These services are available to-(1) Young and inexperienced families. (2) Families with closely spaced children. (3) Single-parent families. (4) Lower income families. (5) Families with parents who are soon to deploy. g. Prevention programs provided by military and civilian agencies can also-(1) Create community and command awareness of abuse. (2) Provide information of existing services. (3) Provide specific educational programs: (a) Community Education Program. (b) Commander Education Program. (c) Troop Education Program. (d) Education for Professionals Program. (e) Safety education for children's programs. 9.6 Exceptional Family Member Program a. The EFMP is an Army personnel readiness support program in which the AMEDD is responsible for assessing, documenting, and coding the medical, physical, emotional, developmental, and special educational needs of family members for consideration in the personnel assignment process. Enrollment in the EFMP is mandatory. In locations outside CONUS, the EFMP is also responsible for providing support to students in the Department of Defense Dependents Schools who require special education evaluations and medically related services, i.e., occupational and physical therapy, psychological and social work services. b. An exceptional family member (EFM) is a patient with a serious or chronic medical problem, physical disability, or mental health disorder. Any child with a development disability or special education requirement should be enrolled. For the program to be fully effective in meeting the needs of a soldier's family, it is imperative that identification of potential EFMs be accomplished early. In doing so, the best care for the patient with a serious or chronic medical problem or a need for special education can be planned or programmed as the soldier continues his or her career. c. For a successful program, installation and activity commanders are responsible for ensuring P.106 Commander's Guide to Combat Health Support US Army PAM-40-19 that soldiers with EFMs are informed that— (1) They are responsible for the care and welfare of their dependents. (2) Their participation in the program does not adversely affect their selection for promotions, schooling, or assignments. (3) Enrollment in the EFMP is continuous. Changes in condition status and/or care requirements are the basis for updating enrollment data. Procedures for disenrollment are outlined in AR 608-75. (4) Assignment managers at HQDA will consider the documented special education and medical needs of family members in permanent change of station moves. d. Soldiers with EFMs should become familiar with AR 608-75 and its provisions. 9.7 Veterinary treatment facilities Veterinary treatment facilities are located on most military installations and are operated by Army Veterinary Service personnel. These facilities are used to provide veterinary care to Government-owned animals and to privately-owned animals of eligible DOD beneficiaries. In CONUS, privately-owned animal care is limited to measures that control diseases that are transmissible from animal to animal, and from animal to man, and emergency services to save the life or limb of animals. In CONUS, DOD regulations require additional definitive privately-owned animal care be referred to civilian veterinarians. In most locations outside CONUS, complete veterinary care for privately-owned animals is provided as time, space, and facility capabilities permit. Fees charged for privately-owned animal services are under the fiscal management of nonappropriated fund instrumentalities. P.107 Commander's Guide to Combat Health Support US Army PAM-40-19 A.0 Appendix A. References Section I Required Publications AR 40-5 Preventive Medicine. (Cited in paras 7-4 b and 8-10e.) AR 40-35 Preventive Dentistry. (Cited in para 8-7 e.) AR 40-66 Medical Record Administration. (Cited in para 6-1 g.) AR 40-501 Standards of Medical Fitness. (Cited in paras 6-2 d and 8-12c(2)(a).) AR 40-562/NAVMEDCOMINST 6230.3/AFR 161-13/CG COMDTINST M6230.4 Immunizations and Chemoprophylaxis. (Cited in para 8-6 b and table 8-1.) AR 40-905/SECNAVINST 6401.1A/AFI 48-131 Veterinary Health Services. (Cited in para 8-13 c.) AR 50-5 Nuclear and Chemical Weapons and Materiel--Nuclear Surety. (Cited in paras 6-1 b and 6-1e.) AR 50-6 Nuclear and Chemical Weapons and Materiel--Chemical Surety. (Cited in paras 6-1 b and 6-1e.) AR 190-8 Enemy Prisoners of War--Administration, Employment and Compensation. (Cited in para 5-2 c.) AR 220-1 Unit Status Reporting. (Cited in para 6-6 a.) AR 350-15 The Army Physical Fitness Program. (Cited in para 7-1 c(4).) AR 600-9 The Army Weight Control Program. (Cited in para 7-1 c(5).) AR 608-75 Exceptional Family Member Program. (Cited in paras 9-6 c(3) and 9-6d.) AR 600-105 Aviation Service of Rated Army Officers. (Cited in para 8-12 d(5)(b).) AR 611-201 Enlisted Career Management Fields and Military Occupational Specialties. (Cited in para 7-1 b(3).) AR 640-3 Identification Cards, Tags, and Badges. (Cited in para 5-2 d(2).) DA Cir 601-94-3 Military Physician Assistant Procurement Program, Fiscal Years 1995-1997. (Cited in para 7-7 a.) DA Pam 351-20 Army Correspondence Course Program Catalog. (Cited in paras 7-2 c, 7-3b, and 7-4b.) FM 8-10 Health Service Support in a Theater of Operations. (Cited in paras 2-4 a and 5-2c.) FM 8-10-8 Medical Intelligence in a Theater of Operations. (Cited in paras 4-2 a and 4-4.) FM 8-55 Planning for Health Service Support. (Cited in para 5-2 c.) FM 19-40 Enemy Prisoners of War, Civilian Internees and Detained Persons. (Cited in para P.108 Commander's Guide to Combat Health Support US Army PAM-40-19 5-2 c.) FM 27-10 TC 8-100 The Law of Land Warfare. (Cited in para 5-1 a(2).) Expert Field Medical Badge Test. (Cited in para 7-1 d(3).) Section II Referenced Publications AR 10-5 Department of the Army AR 40-3 Medical, Dental, and Veterinary Care AR 40-25/NAVMEDCOMINST 10110.1/AFR 160-95 Education Nutrition Allowances, Standards, and AR 40-60 Policies and Procedures for the Acquisition of Medical Materiel AR 40-216 Neuropsychiatry and Mental Health AR 40-657/NAVSUPINST 4355.4/MCO P10110.31 Veterinary/Medical Food Inspection and Laboratory Service AR 381-26 Army Foreign Materiel Exploitation Program AR 385-10 The Army Safety Program AR 385-95 Army Aviation Accident Prevention AR 600-85 Alcohol and Drug Abuse Prevention and Control Program AR 600-110 Identification, Surveillance, and Administration of Personnel Infected with Human Immunodeficiency Virus (HIV) AR 601-142 Army Medical Department Professional Officer Filler System AR 608-18 The Army Family Advocacy Program AR 611-101 Officer Classification and Management System AR 635-40 Physical Evaluation for Retention, Retirement, or Separation AR 672-5-1 Military Awards DA Pam 25-51 The Army Privacy Program--System Notices and Exemption Rules DA Pam 27-1 Treaties Governing Land Warfare DA Pam 40-12 Who Needs It--Venereal Diseases DOD 6010.8-R Civilian Health and Medical Program of the Uniformed Services (CHAMPUS) FM 8-10-5 Brigade and Division Surgeon's Handbook for Tactics, Techniques, and Procedures FM 27-1 Legal Guide for Commanders FM 27-2 Your Conduct in Combat Under the Law of War FM 27-14 Legal Guide for Soldiers GTA 21-3-4 Battle Fatigue, Normal Common Signs, What to do for Self and Buddy GTA 21-3-5 Battle Fatigue, " More Serious" Signs: Leader Actions P.109 Commander's Guide to Combat Health Support GTA 21-3-6 US Army PAM-40-19 Battle Fatigue, Company Leader Actions and Prevention STANAG 2931 Camouflage of the Geneva Emblem on Medical Facilities on Land TB 38-750-2 Maintenance Management Procedures for Medical Equipment Section III Prescribed Forms This section contains no entries. Section IV Referenced Forms DA Form 3180-R Personnel Screening and Evaluation DA Form 4515 Personnel Reliability Program Record Identifier DD Form 1380 US Field Medical Card DD Form 1934 Geneva Conventions Identity Card for Medical and Religious Personnel Who Serve In or Accompany the Armed Forces DOL Form CA 1 Federal Employee's Notice of Traumatic Injury and Claim for Continuation of Pay/Compensation DOL Form CA 2 Notice of Occupational Disease and Claim for Compensation P.110 Commander's Guide to Combat Health Support US Army PAM-40-19 GLOSSARY Section I Abbreviations ACR armored cavalry regiment AHS Academy of Health Sciences, U.S. Army AIDS acquired immunodeficiency syndrome AMEDD U.S. Army Medical Department AMEDDC&S U.S. Army Medical Department Center and School AML area medical laboratory AOC area of concentration AR Army regulation ASL authorized stockage list ASMB area support medical battalion ATLS advanced trauma life support ATM advanced trauma management BAMC Brooke Army Medical Center BAS battalion aid station BF battle fatigue BSA BTC brigade support area Blood Transshipment Center C(4) Combat Casualty Care Course CHAMPUS Civilian Health and Medical Program of the Uniformed Services CHS combat health support CHLS Combat Health Logistics System COMMZ communications zone CONUS continental United States CS combat support CSA corps support area CSC combat stress control CSH combat support hospital CSS combat service support CZ combat zone DA Department of the Army P.111 Commander's Guide to Combat Health Support DA Cir US Army PAM-40-19 Department of the Army circular DA Pam Department of the Army pamphlet DD Form Department of Defense form DISCOM division support command DMOC division medical operations center DMSO division medical supply office DOD Department of Defense DOL Department of Labor DSA division support area DVA Department of Veterans Affairs EAC echelons above corps EACIC echelon above corps intelligence center EFM exceptional family member EFMB Expert Field Medical Badge EFMP Exceptional Family Member Program EMT emergency medical technician EPW enemy prisoner(s) of war FH field hospital FLOT forward line of own troops FM field manual FSB forward support battalion FSMC forward support medical company FSP forward support platoon FST forward surgical team FY fiscal year GC Geneva Convention Relative to the Protection of Civilian Persons in Time of War, 12 August 1949 GH general hospital GPW Geneva Convention Relative to the Treatment of Prisoners of War, 12 August 1949 GTA graphic training aid GWS Geneva Convention for the Amelioration of the Wounded and Sick in Armed Forces in the Field, 12 August 1949 HIV human immunodeficiency virus HMO Health Maintenance Organization P.112 Commander's Guide to Combat Health Support HQDA US Army PAM-40-19 Headquarters, Department of the Army HSC U.S. Army Health Services Command HUB hospital unit, base HUH hospital unit, holding HUM hospital unit, medical HUS hospital unit, surgical HUSF hospital unit surgical-forward JMREC JMRTC Joint Medical Readiness Education Council Joint Medical Readiness Training Center MASH mobile Army surgical hospital MC Medical Corps MEBD Medical Evaluation Board MEDCOM U.S. Army Medical Command MEDLOG medical logistics (battalion) MFSS Medical Field Service School MMRB MOS Medical Retention Board MOS military occupational specialty MOU memorandum of understanding MS Medical Service Corps MSB main support battalion MSMC main support medical company MTF medical treatment facility NATO North Atlantic Treaty Organization NBC nuclear, biological, and chemical NCO noncommissioned officer OCCMED occupational medicine PA physician assistant PCM primary care manager PEB Physical Evaluation Board PPES Physical Performance Evaluation System PPO Preferred Provider Organization PRIMUS Primary Health Care for the Uniformed Services PROFIS Professional Filler System P.113 Commander's Guide to Combat Health Support PRP US Army PAM-40-19 Personnel Reliability Program PVNTMED preventive medicine PW prisoner(s) of war RTD return to duty S3 Operations and Training Officer SIMLM single integrated medical logistical manager SP Army Medical Specialist Corps SPD supply point distribution STANAG standardization agreement STD TB sexually transmitted disease technical bulletin TC training circular TMMMC theater medical materiel management center TO theater of operations TOE table(s) of organization and equipment TSA tactical support area TSOP tactical standing operating procedure UD unit distribution USAF U.S. Air Force USUHS Uniformed Services University of the Health Sciences Section II Terms Beneficiary Members and certain former members of the uniformed Services and their dependents entitled to care as described in section 1072 (b), 1076 (a) or (b), chapter 55, title 10, United States Code. Credentials review The review of the documents which constitute evidence of training, licensure, experience, and expertise of a practitioner. Echelon of combat health support/care A North Atlantic Treaty Organization term that can be used interchangeably with the term P.114 Commander's Guide to Combat Health Support US Army PAM-40-19 "level" of combat health support/care. Information The raw material from which intelligence is produced. It becomes available usually in bits and pieces and may take many forms such as facts, statistics, observations, reports, trends, opinions, rumors, documents, photographs, diagrams, maps, and other items. Information may be true or false, positive or negative, organized or unorganized, related or unrelated. Intelligence The product obtained when raw information is collected, collated, and analyzed with other information already on hand to determine its significance in terms of a given mission. Intelligence is sequential, timely, and event-oriented. In a tactical situation, you need intelligence upon which to base your decisions or plans and to concentrate combat power at critical places and times. The degree of success achieved by your unit in accomplishing its mission will be directly affected by the intelligence it develops and uses. a. Strategic Intelligence. Strategic intelligence is that intelligence which is required for the formation of policy and military plans at national and international levels. Directed on national objectives, it assists in determining feasible national policies and in furnishing a basis for planning. Factors which influence the military capabilities, vulnerabilities, and probable courses of action of nations are considered components of strategic intelligence. b. Tactical Intelligence. Tactical intelligence is that knowledge of the enemy, weather, and terrain which you need to plan and conduct combat operations. It may be obtained from within the command or from higher, lower, or adjacent headquarters. c. Technical Intelligence. Technical intelligence is that intelligence concerning foreign technological developments and performance and operational capabilities of foreign materiel which currently has or eventually may have a practical military application. Before and during the AirLand Battle, technical intelligence may contribute significantly to fulfilling the mission of tactical units. There are communications-electronics intelligence; weapons and munitions intelligence; logistics and NBC intelligence; medical intelligence; and mobility intelligence. d. Medical Intelligence. Medical intelligence is a product resulting from the collection, evaluation, analysis, and interpretation of information concerning the medical aspects of foreign countries that has immediate or potential impact on policies, plans, and operations. The key word is "foreign " because this information is only developed on foreign P.115 Commander's Guide to Combat Health Support countries. US Army PAM-40-19 It includes-- (1) Intelligence on foreign epidemiology, public health standards and capabilities, and the number of trained military and civilian combat health support personnel. (2) Intelligence on medical supplies, health service facilities, and medical services. (3) Intelligence on-(a) Foreign animal diseases (especially those diseases transmissible to humans). (b) Health problems relating to the use of local food supplies. (c) Medical effects of prophylaxis against chemical and biological agents. (4) Intelligence concerning the impact of newly developed foreign weapons systems as related to casualties. (5) Intelligence concerning an enemy force or an area of operations that in some way may affect the health of the command or combat health support operations. Medical Force 2000 The development and marked improvement in the ability of the AMEDD to support the AirLand Battle which focuses on a complete medical force package. This force package can more efficiently and effectively support the combat force through enhanced medical care and patients early return to duty while reducing the"confusion " and the support requirements in the corps. Patient care evaluation A process, performed either concurrently or retrospectively, which assesses in depth the quality and/or nature of the utilization of an aspect of health or dental care services. This often is accomplished by observation or medical record audit. Corrective action is taken where indicated and a subsequent analysis (follow-up) is made of the effect of the corrective action. Privileging The processing through credentials committee channels of those individuals given the authority and responsibility for making independent decisions to diagnose, initiate, alter, or terminate a regimen of medical or dental care. Provider (health care provider) Military (Active or Reserve Component) and civilian personnel (civil service and providers working under contractual or similar arrangements) granted privileges to diagnose, initiate, alter, or P.116 Commander's Guide to Combat Health Support US Army PAM-40-19 terminate health care treatment regimens within the scope of his or her license, certification, or registration. This category includes physicians, dentists, nurse practitioners, nurse anesthetists, nurse midwives, podiatrists, optometrists, clinical psychologists, occupational therapists, audiologists, speech pathologists, physician assistants or any others providing direct patient care. Risk management Clinical and administrative activities that hospitals undertake to identify, evaluate, and reduce the risk of injury and financial loss to patients, personnel, visitors, and the institution itself. Standards are applied to evaluate a hospital's performance in conducting risk management activities designed to identify, evaluate, and reduce the risk of patient injury associated with care and services. Utilization management The planning, organization, directing, and controlling of medical or dental services in a cost-effective manner while maintaining acceptable standards. Section III Special abbreviations and terms This section contains no entries. P.117 Commander's Guide to Combat Health Support US Army PAM-40-19 USAPPC-INDEX This index is organized alphabetically by topic and by subtopic within topic. are identified by paragraph number. Acquired immunodeficiency syndrome, 8-9 Advanced trauma life support, 7-6 Advanced trauma management, 2-2 Alcohol and drug abuse, 8-4 Ambulance squad, 2-2 Area support squad, 2-2 Army Medical Department History, 1-4 Mission, 1-5 Services, 1-5 Army medical laboratory, 2-8 Aviation medicine program Army flight surgeon, 8-12 Clinical responsibilities, 8-12 Nonclinical responsibilities, 8-12 Role of Army aviation medicine, 8-12 Basic sanitation, 8-11 Battle fatigue, 8-3 Blood management, 3-1, 3-3, 3-4, and 3-7 Buddy aid, 2-3 Civilian Health and Medical Program of the Uniformed Services, 9-1 Combat Casualty Care Course, 7-6 Combat Health Logistics System Blood management, 3-1 Corps Combat Health Logistics System Medical equipment maintenance, 3-3 Medical logistics battalion (forward), 3-3 Medical logistics battalion (rear), 3-3 Medical supply and blood support, 3-3 Definition, 3-1 P.118 Topics and subtopics Commander's Guide to Combat Health Support US Army PAM-40-19 Division Combat Health Logistics System DMSO, 3-2 and 3-3 Medical equipment maintenance, 3-2 Medical logistics battalion (forward), 3-2. See also Echelons III and IV Medical Standby Equipment Program, 3-2 Echelons I and II, 3-1 Echelons III and IV, 3-1 Echelons above corps Medical logistics battalion (forward), 3-4 Medical logistics battalion (rear), 3-4 Medical logistics support detachment, 3-4 Joint/combined operations, 3-4 Theater medical materiel management center, 3-4 Medical equipment maintenance, 3-1 Optical fabrication, 3-1 Optical combat health logistics system Echelons I and II, 3-5 Echelons III and IV, 3-5 Organizational structure Medical logistics battalion (forward), 3-1 Medical logistics battalion (rear), 3-1 Medical logistics support detachments, 3-1 Theater medical materiel management center, 3-1 U.S. Air Force Blood Transshipment Center, 3-1 and 3-7 Combat health support mission, 2-1 Combat health support system, 2-1 Combat lifesaver, 2-3 Combat medic, 2-2 and 2-3 Combat support hospital, 2-3 and 2-4. See also Echelons of combat health support Dental support in a theater of operations Categories of dental care, 2-6 Dental support in a theater of operations, 2-6 Types of dental support, 2-6 Echelons of combat health support P.119 Commander's Guide to Combat Health Support US Army PAM-40-19 Echelon I, 2-3 and 3-1 Echelon II, 2-3 and 3-1 Echelon III, 2-3 and 3-1 Echelon IV, 2-3 and 3-1 Echelon V, 2-3 Emergency medical treatment, 2-2 and 2-3 Exceptional Family Members Program, 9-5 Expert Field Medical Badge, 7-1 Family Advocacy Program, 9-4 Field hospital, 2-4. See also Echelons of combat health support Field sanitation team, 8-11 Field sanitation team training, 7-4 General hospital, 2-4. See also Echelons of combat health support Health Maintenance Organization, 9-1 Hospital modules, 2-4 Hospital support requirements, 2-5 Immunizations/prophylaxes, 8-6 Initial unit training and sustainment training, 7-2 Insect and rodent control, 8-11 Intratheater evacuation policy, 2-10 Joint Medical Readiness Training Center, 7-6 Law of land warfare Accountability and custody of enemy prisoners of war, 5-2 Captured medical supplies and equipment, 5-2 Civilians--wounded and sick, 5-2 Geneva Convention, 5-1, 5-2 Identification and protection of medical personnel, 5-2 Marking of ambulances, 5-2 Marking of medical units/facilities, 5-2 Provisions for collection of wounded and sick, 5-2 Responsibility and handling of prisoners of war, 5-2 Self-defense, 5-2 P.120 Commander's Guide to Combat Health Support US Army PAM-40-19 Sources of the law of land warfare, 5-1 Medical company, holding, 2-4 Medical Evaluation Board, 6-4 Medical Force 2000, 2-4 Medical intelligence Definition, 4-1 Historical data, 4-3 Resources, 4-2 Strategic level, 4-4 Tactical level, 4-4 Medical proficiency training, 7-5 Medical/surgical teams, 2-4 Mobile army surgical hospital,2-4 and 2-6. See also Echelons of combat health support Modular medical support, 2-2 Nutrition, 8-14 Occupational safety and health, 8-10 Oral Health Fitness Program, 8-7 Patient holding squad, 2-2 Personnel Enlisted personnel, 1-6 MC officer, 1-6 Medical NCO, 1-6 Medical specialist, 1-6 MS officer, 1-6 Officer personnel, 1-6 PA, 1-6 Personnel Reliability Program, 6-1 Physical Evaluation Board, 6-5 Physical Performance Evaluation System, 6-3 Physical profiling, 6-2 Preferred Provider Organization, 9-1 Preventive medicine, 2-3 Primary care managers, 9-1 Primary Health Care for the Uniformed Services, 9-2 and 9-3 P.121 Commander's Guide to Combat Health Support US Army PAM-40-19 Professional Filler System, 6-6 Quality assurance, 1-7 Self-aid, 2-3 Sexually transmitted diseases, 8-8 Sleep, 8-2 Soldier health maintenance elements, 8-1 Stress Battle fatigue, 8-3 Combat stress casualties, 8-3 Combat stress defense, 8-3 Stress management, 8-3 Suicide prevention, 8-5 Surgical squad/detachment, 2-2 Theater evacuation policy, 2-9 Theater hospital support system, 2-4 Treatment squad, 2-2 and 2-3 Treatment squad (battalion aid station) 2-3 TRICARE, 9-1 and 9-2 Uniformed Services Dependents Dental Insurance Plan, 9-3 Veterinary services, 8-13 Veterinary support in a theater of operations, 2-7 Veterinary treatment facilities, 9-6 P.122