outline27762
advertisement
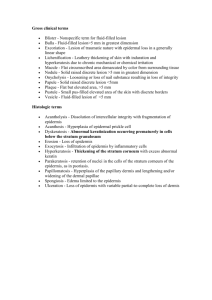
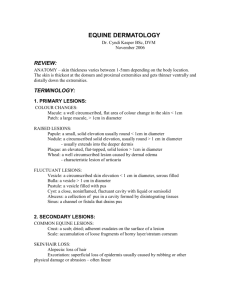
Skorin/Page 1 of 4 EXTREME DERMATOLOGY Leonid Skorin, Jr., OD, DO, FAAO, FAOCO Albert Lea Medical Center - Mayo Health System skorin.leonid@mayo.edu I. Skin A. Anatomy 1. Epidermis a. outer keratinizing, stratified squamous epithelium b. self-regenerating c. contains appendages 2. Dermis a. fibroelastic tissue b. 2 main functions-support and nourishment c. appendages arise from this layer 3. Subcutaneous a. adipose tissue B. Eyelid Skin 1. Thinnest skin in body 2. <1 mm thickness 3. Lacks subcutaneous tissue 4. Rests directly on orbicularis muscle C. Epidermal Appendages 1. Apocrine gland a. Gland of Moll b. sweat gland c. oily secretion d. duct opens into hair follicle 2. Glands of Zeis a. pilosebaceous units b. oily secretion c. lubricates cilia 3. Meibomian gland a. modified sebaceous gland D. Glossary – Macroscopic Morphology 1. Macule – non-palpable small area of color change 2. Papule – small palpable lesion < 1.5 mm in diameter 3. Nodule – a papule which has enlarged in height, width and length 4. Plaque – a papule which has enlarged in length and width only 5. Pustule – vesicle laden with neutrophils (white blood cells) 6. Scale – any increase in thickness of stratum corneum secondary to either excess formation or delay in exfoliation 7. Erosion – focal loss of epidermis resulting in shallow excavation 8. Ulcer – focal loss of epidermis and dermis resulting in deep excavation Skorin/Page 2 of 4 E. Glossary – Histopathological Features 1. Acantholysis – breakdown of cell-cell attachments 2. Acanthosis – increase in size and number of cells in prickle cell layer 3. Bullae – fluid filled cavity either within or below the epidermis 4. Crusting – dried plasma proteins either replacing lost epidermis or arising from intact epidermis 5. Dyskeratosis – abnormal keratinisation associated with pre- and malignant tumors that arise within the epidermis or in association with acantholytic disorders 6. Orthokeratosis – increased thickness of stratum corneum (hyperkeratosis) without retention of keratinocyte nuclei 7. Parakeratosis – hyperkeratosis characterized by incomplete keratinisation with retention of keratinocyte nuclei 8. Vesicle – collection of fluid smaller than bullae F. Examination 1. Become an osteopathic optometrist a. birds-eye-view b. press c. squeeze d. stretch e. manipulate f. clues to extent of invasion into underlying structures g. slit lamp – high magnification h. Wood’s light – pigmented lesions i. photography – documentation, follow-up j. press +10 Diopter lens on surface of nodular lesion for 30 sec. if involution hemangioma not melanoma k. transillumination – solid lesion shows shadow 2. Lymph Node Evaluation a. Preauricular – lateral lid b. Submandibular – medial lid 3. ABCDE Criteria a. Asymmetry b. Border Irregularity 1. blurred, ragged, spills into surrounding skin c. Color Variegation 1. 3 or more colors or shades of a single color d. Diameter 1. larger than 6 mm (size of a pencil eraser) e. Evolving 1. change in size, shape, symptoms (itching), surface (bleeding), color II. General A. Eyelid and Facial Lesions 1. Often NOT a patient’s chief complaint 2. Often diagnosed by OD’s with a comprehensive approach to patient Skorin/Page 3 of 4 B. C. D. E. III. 3. Easier to treat when small 4. Denial regarding malignancy common among patients with skin cancers History 1. Previous skin cancer 2. sunburn/blistering in adolescence 3. Previous radiation therapy (acne) 4. Celtic or Scandinavian Ancestry: patients with red hair, fair skin, blue eyes Is It Cancer? Worrisome Signs! 1. Growth or change in lesion 2. Induration: firmness to lesion 3. Malignant lesions not painful 4. Abnormal vessels: telangectasias 5. Irregular or “pearly” borders 6. Lid margin and gray line disruption 7. Eyelash loss - madarosis Biopsy 1. EXCISIONAL – remove entire lesion and 1 – 3 mm of normal border 2. SHAVE – superficial sample of tissue 3. PUNCH – obtain deeper tissue sample The 6 Essential D’s For Pathology Forms 1. Demographics a. patient’s name b. age c. sex d. race/ethnicity 2. Description a. biopsy site b. color c. symptoms d. other areas of involvement i. previous therapy ii. previous biopsy at lesion site 3. Diseases and Drugs (pertinent patient illnesses and medications) 4. Duration of condition 5. Diameter of lesion or eruption 6. Differential diagnosis (in order of likelihood) a. can be broad categories, such as malignancy, dermatitis or infection Skin Lesions A. Benign Lesions 1. Sebaceous cysts – retention cysts of sebum 2. Milia – intracutaneous sebaceous cysts 3. Cyst of Zeis 4. Cyst of Moll – apocrine hidrocystoma 5. Xanthelasma – lipid-laden macrophages 6. Nevus – difficult to distinguish from BCC or MM Skorin/Page 4 of 4 7. Molluscum contagiosum – pox virus 8. Verrucae (Papilloma) – skin tag a. vulgaris – pedunculated b. plana – flat (sessile) c. cutaneous horn – keratinized verruca vulgaris 9. Seborrheic keratosis B. Premalignant Lesions 1. Keratoacanthoma – umbilicated nodule with a keratin filled center a. spontaneous involution b. slight risk of SCC 2. Actinic keratosis – solar keratosis a. elderly, fair skin, sunlight exposure b. evolve into SCC C. Malignant Lesions 1. Basal Cell Carcinoma a. 90% of malignant eyelid lesions b. consequence of UV exposure c. lower eyelid, medial canthus d. 0.2% - 1.0% metastize 2. Nodular BBC – 75% a. firm, raised, pearly nodules; telangectasia b. rodent ulcer 3. Diffuse Morpheaform BCC – 15% (Sclerosing) a. more invasive than nodular BCC b. margins difficult to estimate c. lesions are firm, ulceration common d. lesions may mimic surgical scar 4. Squamous Cell Carcinoma a. potentially lethal; 10% of malignant eyelid tumors b. extends to underlying dermis c. lower eyelid, medial canthus 5. SCCA Metastatic Spread a. from AK 2%, de novo much higher b. direct extension c. perineural invasion – trigeminal, facial extraocular motor nerves d. lymphatic or hematological spread 6. Sebaceous Gland Carcinoma a. rare, <1% of all eyelid tumors b. meibomian, Zeis, caruncle c. upper eyelid d. great masquerader (recurrent chalazion) e. chronic unilateral blepharoconjunctivitis f. madarosis 7. Malignant Melanoma a. rare (< 1%) but incidence increasing b. increase depth of lesion, increased risk of metastasis c. ABCDE criteria