Chapter 18 - Las Positas College
advertisement

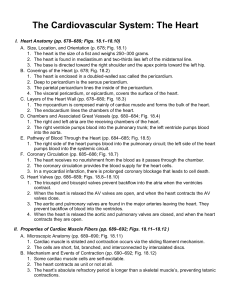
Chapter 18 The Heart I. Location and Orientation Within the Thorax (pp. 529–531, Figs. 18.1–18.2) A. The heart is a double pump; the right side pumps blood to the lungs for oxygenation, i.e., the pulmonary circuit; the left side pumps blood throughout the body to nourish tissues, i.e., the systemic circuit. (p. 529, Fig. 18.1) B. The four chambers are the right and left atria (receiving chambers) and the right and left ventricles (pumping chambers). (p. 529, Fig. 18.1) C. The cone-shaped heart lies obliquely in the mediastinum; the size of a fist, approximately 250–350 grams, its apex points toward the left hip and the broad posterior base is directed toward the left shoulder. (pp. 529–531, Fig. 18.2) II. Structure of the Heart (pp. 531–536, Figs. 18.3–18.5) A. The heart is enclosed by the pericardium; the pericardium consists of a superficial layer (the fibrous pericardium and parietal layer of serous pericardium), and a deeper visceral layer of the serous pericardium that covers the heart surface. (p. 531, Fig. 18.3) B. The wall of the heart has three layers: a superficial epicardium (same as the visceral layer of serous pericardium), a middle myocardium (the cardiac muscle), and a deep endocardium (heart lining). (p. 531, Figs. 18.3–18.4) C. The heart has four chambers. (pp. 532–533, Fig. 18.5) 1. Right and left atria are located superiorly and separated by an interatrial septum. 2. Right and left ventricles are located inferiorly and separated by an interventricular septum. III. Pathway of Blood Through the Heart (pp. 536–537, Figs. 18.6–18.7) A. The pathway of blood through the heart begins with a drop of oxygen-poor systemic blood arriving at the right atrium and terminates with an oxygen-rich drop of blood leaving the left ventricle. (pp. 529 and 536–537, Fig. 18.6) B. A sequence of atrial contractions and ventricular contractions (called a heartbeat) propels blood through the heart. (p. 537) C. The muscular walls of the right and left ventricles reflect differential pressures in the pulmonary and systemic circuits. (p. 537, Fig. 18.7) IV. Heart Valves (pp. 537–540, Figs. 18.8–18.11) A. The four heart valves are the two atrioventricular valves and the two semilunar valves. (p. 537, Fig. 18.8) 1. The right AV valve is the tricuspid and the left AV valve is called the bicuspid or mitral. 2. The two semilunar valves are the pulmonary semilunar valve and the aortic semilunar valve. B. The fibrous skeleton of the heart surrounds the heart valves and functions in several ways, one of which is to anchor the valve cusps. (p. 537) C. A valve consists of two or three flaps of endocardium called cusps; the AV valves lie at the junctions between the atria and ventricles; the semilunar valves lie at the junctions between the ventricles and great arteries. (p. 537, Fig. 18.8) D. Heart valves open to allow blood to flow and close to prevent backflow in response to differences in blood pressure on each side of the valves. (pp. 537 and 540, Figs. 18.9–18.10) E. Heart sounds (the familiar “lub-dup”) are produced by the closing of the valves. (p. 540, Fig. 18.11) V. Cardiac Muscle Tissue (pp. 540–542, Figs. 18.12–18.13) A. Cardiac muscle tissue forms the myocardium of the heart wall. B. Cardiac muscle cells are short, branching cells with one or two centrally-located nuclei. (p. 541, Fig. 18.12b) C. Intercalated discs are complex cell junctions joining cardiac muscle cells. (pp. 541–542, Figs. 18.12a–c and 18.13) D. Cardiac muscle cells are triggered to contract by ionic calcium. (p. 542) VI. Conducting System and Innervation (pp. 542–544, Figs. 18.14–18.15) A. Heart muscle generates and conducts electrical impulses; the intrinsic production of impulses can be altered by extrinsic neural controls. (pp. 542–543) B. The conducting system of the heart is a series of specialized cardiac muscle cells that carries impulses throughout the heart; among the several components are the SA node and AV node. (p. 543, Fig. 18.14) C. Innervation to the heart is served by visceral sensory fibers, parasympathetic fibers, and sympathetic fibers; parasympathetic fibers slow the heart rate and sympathetic fibers increase the heart rate. (p. 544, Fig. 18.15) VII. Blood Supply to the Heart (pp. 544–545, Fig. 18.16) A. Coronary arteries supply oxygenated blood to the heart muscle; cardiac veins drain the deoxygenated blood from the heart. VIII. Disorders of the Heart (pp. 545–548) A. Coronary artery disease is caused by atherosclerotic blockage of the coronary arteries. (p. 545) B. Heart failure is a progressive weakening of the heart as it fails to keep pace with the demands of pumping blood and thus cannot meet the body’s need for oxygenated blood. (pp. 545–546) C. Disorders of the conduction system include atrial and ventricular fibrillation. (p. 548) IX. The Heart Throughout Life (pp. 548–551, Figs. 18.17–18.19) A. The embryonic heart starts pumping around day 22 and four chambers are apparent; four final chambers are defined during month two. (pp. 548–549, Figs. 18.17–18.18) B. Congenital heart defects mostly are traced to month two of development. (pp. 549–550, Fig. 18.19) C. Age-related changes that affect the heart are the hardening and thickening of the cusps of the heart valves and fibrosis of cardiac muscle. (pp. 550–551) Chapter 18: The Heart To the Student Place your hand over your heart. As you feel the beat of this muscular organ, think about what it does to sustain life for you. It is the force behind pumping blood to the lungs to pick up oxygen and the pumping of blood to deliver oxygen and nutrients to your entire body. In 1 year, the heart pumps an estimated 1 million gallons of blood and beats approximately 40 million times. A daily estimate is 2,700 gallons of blood pumped and 100,000 beats! Add the fact that blood is pumped through an estimated 60,000 miles of vessels in your body, and the heart becomes even more phenomenal. The heart has fascinated and intrigued man for centuries and still today is linked with human emotions. The resemblance to the popular valentine is unmistakable. Your goal in this chapter is to learn the gross anatomy and functions of the heart and its structures, how blood moves through the heart, and circulation patterns. Don’t forget the availability of the The Anatomy Place CD-ROM, The Anatomy Place web site, and A.D.A.M. Interactive Anatomy as additional multimedia resources for study of the heart. Step 1: Explain the orientation and location of the heart in the human body. - Describe the physical characteristics, orientation, and location of the heart in the mediastinum. - Distinguish between the apex and base. - Name the structure that the heart contacts inferiorly. - Define mediastinum. Step 2: Explain systemic, pulmonary, and coronary circuits. - Define artery and vein. - Describe the heart as being organized into two pumps. - Define and summarize the pathway of systemic circulation. - Define and summarize the pathway of pulmonary circulation. - Define and summarize the pathway of coronary circulation. Step 3: Describe the gross anatomy of the heart. - Define pericardium and distinguish between visceral pericardium, parietal pericardium, and pericardial sac. - Name the layers of the heart wall, from external to internal, including tissue components of each layer. - Describe the surface anatomy of the heart. - Name the four chambers of the heart, and list structural features of each. - Draw the heart in an anterior view and cut open, and label as many parts as you can. - Distinguish between the following: • Atrium and auricle • Atrium and ventricle • Pectinate muscle and trabeculae carneae • Trabeculae carneae and papillary muscle • Bicuspid valve and tricuspid valve Step 4: Describe blood flow through the heart, and include valves and heart sounds. - Trace a drop of blood from the right atrium back to the right atrium. - Review pulmonary and systemic pathways. - Define and describe heartbeat. - Name the four valves; describe locations, structures, and functions. - Explain the cause of the first and second heart sounds, “lub,” and “dup,” indicating the location on the anterior chest wall for best observations using a stethoscope. - Describe the fibrous skeleton structural support of the AV valves, including functions. Step 5: Describe cardiac muscle tissue. - Discuss the structure of cardiac muscle tissue. - Describe the function of cardiac muscle tissue, including the role of intercalated discs. - Describe the role of calcium ions in cardiac muscle cell contraction. - Compare cardiac muscle tissue to skeletal muscle tissue. Step 6: Describe the conduction system and explain innervation to the heart. - Discuss the initiation of the heartbeat. (Is innervation needed?) - Distinguish heartbeat from heart rate. - Draw a frontally sectioned heart, and label parts of the conduction system. - List the sequence of events in conduction of an electrical impulse from the SA node to Purkinje fibers, including contraction of chambers. - Name the kind of tissue that composes the conduction system. (Hint: It is not nervous.) - Describe the effects on the heart of innervation by parasympathetic and sympathetic fibers. Step 7: Describe blood supply to and from the heart muscle. - Name the vessels that supply the heart with oxygenated blood. - Name the vessels that drain the heart muscle of deoxygenated blood. - Indicate where venous blood of the heart muscle joins systemic venous blood. - Trace the pathway of a drop of blood from the myocardium back to the myocardium. Step 8: Examine common disorders of the heart. - Describe conditions, causes, and symptoms of disorders of the heart: coronary artery disease, heart failure, and disorders of the conduction system. Step 9: Examine embryonic development of the heart, and effects of old age on the heart. - Summarize the stages in heart development evident in week 4 of gestation, naming the four embryonic chambers. - Draw an adult heart and its great vessels, indicating regions derived from each embryonic heart chamber. - Give examples of congenital heart defects. - List several age-related changes that affect the heart.