OkhMatDit, National Specialized Pediatric Hospital Ukrainian
advertisement

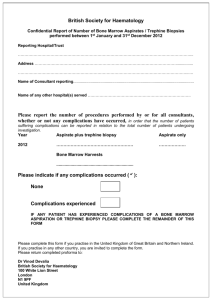
OkhMatDit, National Specialized Pediatric Hospital Ukrainian Ministry of Public Health Center for Pediatric Oncohematology and Bone Marrow Transplantation ul. Chornovola 28/1, Sholudenko 10, Kiev, 01135 Ukraine Phone/fax +38(044)2364215, phone +38(044)2360214 Consultation as of August 18, 2010-09-02 Patient: Karina V. Koryaka, b. 1998 Place of residence: Dnepropetrovsk, Ukraine Diagnosis: myelodysplastic syndrome (according to results of needle biopsy and trephine biopsy of bone marrow) Recommendations 1. Repeated bone marrow aspiration procedure with analysis at laboratory of Center for Pediatric Oncohematology for differential diagnosis between “adult” and “childhood” types of MDS. 2. If “adult”-type MDS is confirmed, the child should undergo allogeneic BMT from an HLA-matching unrelated donor outside Ukraine (a potential matching donor among family members is lacking) as the only method of radical treatment. 3. Iа “childhood”-type (hypocellular) MDS is confirmed, a course of immunosuppressive therapy is recommended. 4. Blood components transfusions should be made through leukocyte removal filters. Head of Center for Pediatric Oncohematology and BMT (Ukrainian Ministry of Public Health) S.B. Donskaya ----------------------------Consultation as of August 31, 2010 Patient: Karina V. Koryaka, b. 1998 Place of residence: Dnepropetrovsk, Ukraine Diagnosis: myelodysplastic syndrome, hypocellular variant Recommended: 1. To begin immunosuppressive therapy with Cyclosporin A 5 mg/kg/day per os daily. 2. To perform further immunosuppressive therapy (ATG + Cyclosporin A + Methylprednisolone) at Center for Pediatric Oncohematology. Head of Center for Pediatric Oncohematology and BMT (Ukrainian Ministry of Public Health) S.B. Donskaya ============================ OkhMatDit, Ukrainian Specialized Pediatric Hospital Case summary No. 545 Patient Karina Vladimirovna Koryaka, born Jan 28, 1998 Home address: ul. Suvorova 15a-127, Dnepropetrovsk, Ukraine Date of admission to hospital: Jul 27, 2010 Date of discharge: Aug 6, 2010 Blood group O(I), Rh(+) No contacts with contagious patients Diagnosis: myelodysplastic syndrome (?), viral hepatitis B Anamnesis morbi: Patient was admitted to Pediatric Department with paleness and hemorrhagic skin rash. In May 2010, there was an episode of gastrointestinal dysfunction and brief episodes of low-grade fever. No CBC control performed. At the end of June, during summer rest at the sea, there were paleness and fatigability. CBC test on Jul 7, 2010; according to its results, the child was taken to Department of Hematology. Admission for trephine biopsy. CBC with diff. WBC, x109/L RBC, x1012/L Hb, g/L PLT, 109/L Jul 27 3.1 2.2 72 2 Jul 28 1.6 2.16 71 8 Jul 30 2.3 2.19 72 3 Aug 5 2.8/1.8 1.9/1.98 63/60 2/80 Aug 6 3.0 1.93 63 72 Date ESR, mm/h 49 eos, % 0 bands, % segs, % lym, % mon, % 1 11 81 7 0 1 23 1 /after PLT transfusion Urinalysis Date Density pH protein, g/L glucose, g/L WBC in HPF RBC in HPF Salts Epithel. Jul 28 1015 7.0 abs abs isol abs abs abs alk abs abs isol isol phosph abs Aug 5 ANA test 1.0 (negative up to 1.5) In view of elevated transaminase levels (found for the first time), the girl underwent a blood test for hepatitis markers. Blood chemistry Jul 28: total protein 75 g/L, glucose 6.1 mmol/L, alpha-amylase 52, seroglycoids 0.15, CRP neg., ASO neg., ALT 170, AST 74, creatinine 36 mol/L, urea 4.0 mmol/L, K 4.5 mmol/L, Na 141 mmol/L, total Ca 1.14 mmol/L. Jul 30: glucose 6.0 mmol/L, total bilirubin 15.6 mol/L, direct bilirubin 3.4 mol/L, ALT 165, AST 74. GGT 16, LDH 226 Cl 107, thymol turbidity test 2.4 units, RhF neg. Protein fractions: albumin=63%, globulins=37%, 1=3%, 2=10%, =4%, =20%, albumin/globulins=1.7. LE test negative. CIC=145 OD units Blood coagulation test as of Jul 28: INR 1.26 (N 0.9-1.3), PT 19.9 (N 15-20), TT 17.7 (N 13-18), APTT 30.7, fibrinogen 2.24 g/L, ethanol gelation test neg. HBsAg, anti-HCV not detected. Anti-HBcore(IgM+IgG) E = 0.198: antibodies to viral hepatitis B core antigen detected. Abdominal ultrasound as of Aug 3: Liver not enlarged, anteroposterior size 115 mm, parenchyma homogeneous, echogenicity diffusely increased, vascular markings decreased. Gallbladder anechoic, with a kink in the region of body. Pancreas not thickened, contour well-delineated, smooth. Spleen enlarged (118x36x68 mm), of moderate echogenicity. Kidneys in normal location, of equal sizes (98x36 mm), without sonographically detectable structural alterations. No abnormal fluid accumulation detected in abdominal cavity at the moment of examination. Thyroid gland ultrasound as of Aug 3: thyroid in normal position, enlarged. Right lobe 5.78 ccm, left lobe 6.51 ccm. Isthmus thickened up to 5.8 mm. Sonographic structure diffusely inhomogeneous owing to multiple hypoechoic regions. Ophthalmologist’s consultation as of Jul 28: Anterior segments and optic media normal. Fundus without abnormalities. Consultation by Head of Hematology Center S.B. Donskaya: see attachment. During preparation for trephine biopsy, the child received platelet transfusion for replacement purpose. For prophylactic purposes, received amoxicillin+clavulanic acid and fluconazole. On Aug 5, 2010, trephine biopsy was performed by hematologist at an operating room. Before the manipulation, the patient got 2 doses of apheresis platelets and 140 mL packed RBC. Manipulation was conducted without complications; three hours later the child was transferred to Pediatric Department. Aug 6: stable condition, normal body temperature. According to the parents’ request, the child was discharged from hospital to get specialized in-patient treatment at place of residence. Recommended: specialized treatment; consultation by infectious disease specialist. Physician Oxana Grishchenko Trephine biopsy as of Aug 5, 2010 Patient: Kristina Koryaka, 13 years old, female Biopsy: primary Clinical diagnosis: myelodysplastic syndrome (?) Pathologist’s report No. 19546-47 dated Aug 6, 2010 Number of fragments: 1 Number of specimens: 1 Macro- and microscopic description Trephine biopsy specimen. Bone marrow architecture disrupted, cellularity preserved, fatty/cellular bone marrow ratio 1:1,1:2. Moderate signs of dyserythropoiesis. Reduced number of cells of granulocytic lineage. Increased number of cells of histiocytic (monocytic) lineage. Total number of megakaryocytes significantly reduced; represented by mononuclear and hypolobular forms. Increased amount of eosinophilic leukocytes and plasma cells. Small regions of fine fibrosis. Morphological picture may correspond to myelodysplastic syndrome. Cytogenetic testing recommended. ==================================== Diagnostic Center of Medical Academy pl. Oktyabrskaya 4, Dnepropetrovsk, Ukraine, phone (0562)36-19-50 Patient: Karina Koryaka, aged 12, gender female Material: blood plasma Date of sampling: Aug 16, 2010 Physician: T.V. Mavrutenkova PCR assay Hepatitis B virus DNA, hepatitis G virus RNA, hepatitis D virus RNA, hepatitis C virus RNA: none detected. Report handed to patient on Aug 20, 2010 ============================================= Ukrainian Ministry of Public Health OkhMatDet clinic, Center for Pediatric Oncohematology and BMT Reference laboratory for diagnosis of oncohematologic diseases Patient’s name: Karina Koryaka, DOB Jan 28, 1998 Specimen No. 2010-1302 (bone marrow), 2010-1303 (peripheral blood) Diagnosis: myelodysplastic syndrome? Aplastic anemia? WBC differential as of Jul 8, 2010 Bands 1.0%, segs 6.0%, lym 90.0%, mon 3.0%. Bone marrow analysis as of Jul 7, 2010 Blasts 0.4%; promyelocytes 0.4%, neutrophilic myelocytes 17.4%, neutr. metamyelocytes 14.6%, bands 12.4%, segs 3.4%, eosinophils 3.2%, lymphocytes 11.6%, monocytes 8.0%, erythroblasts 0.8%, basophilic normoblasts 4.0%, polychromatophilic normoblasts 13.2%, orthochromic normoblasts 10.0%, megakaryocytes 74 in specimen. Specimen hypercellular. Reticulum (-). Description: Specimens are hypercellular owing to hyperplasia of all hematopoietic lineages with moderate shift of leukoerythroid ratio toward erythron. Myeloid lineage with marked change of maturation index toward immature forms owing to increased content of neutrophilic myelocytes and low content of segmented neutrophils; representatives of neutrophilic lineage with hypergranulation. Two-lineage dyshematopoiesis: dyserythropoiesis (evidence for megaloblastic elements, fragmentation of nuclei) and dysmegakaryocytopoiesis (some represented by hypolobulated microforms). Megakaryocytes detected in the specimen are without signs of functioning. In view of CBC findings (pancytopenia) and bone marrow analysis (hyperplasia of medullary hematopoiesis with signs of multi-lineage dyshematopoiesis), we recommend histological and cytogenetic analysis of bone marrow for exclusion of myelodysplastic syndrome. Physicians: Sharamok A.I., Smolenskaya T.V., Ponomarenko T.P. Head of Laboratory: Kreminskaya E.S. ========================== WBC differential as of Aug 25, 2010 Bands 1.0%, segs 1.0%, lym 95.0%, mon 3.0%. Bone marrow assay as of Aug 25, 2010 Blasts 1.2%; promyelocytes 3.0%, neutrophilic myelocytes 6.6%, neutr. metamyelocytes 1.4%, bands 0.4%, segs 0.4%, mast cells 0.2%, lymphocytes 66.4%, monocytes 4.2%, plasma cells 3.2%, erythroblasts 1.2%, basophilic normoblasts 4.0%, polychromatophilic normoblasts 1.8%, orthochromic normoblasts 7.0%, megakaryocytes 2 in specimen. Cellularity: normal. Reticulum (+). Description: Marked hypoplasia of all hematopoietic lineages. Moderate dysmyelopoiesis (asynchrony of maturation) and dyserythropoiesis (disruption of cell division, irregularity of cell contours); change in the maturation index of erythroid and myeloid lineages toward immature forms. Increased content of plasma cells and macrophages with signs of hemophagocytosis. Physicians: Sharamok A.I., Smolenskaya T.V., Ponomarenko T.P. Head of Laboratory: Kreminskaya E.S. August 26, 2010 ====================================