Junior Core Syllabus - Clinical Departments
advertisement
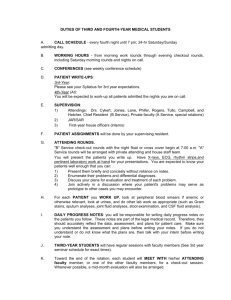
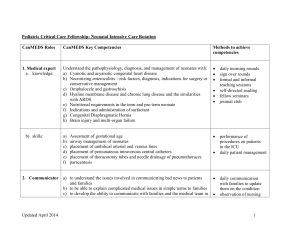
INTERNAL MEDICINE SYLLABUS THIRD YEAR JUNIOR CORE CLERKSHIP Deborah DeWaay, M.D., Clerkship Director Mary Ann Snell, Student Education Coordinator Medical University of South Carolina Charleston, South Carolina 2015 – 2016 Junior Core Checklist Activity Requirements Attestation & Call Review syllabi and objectives Sign Attestation Call Will receive a call schedule Activity Admit a patient 1 History card □ week 2 1 PE card □ week 3 1 SOAP note card □ week 4-5 1 H&P card □ week 4-5 Midpt Feedback 2 cards □ □ (1 must be an attending) Late Shifts 3 shifts over 6 weeks □ □ □ Over-night Shifts 4 shifts over 6 weeks □ □ □ □ EBM project Create clinical question with your team PICO search Pick best evidence Email librarian with your question, your search and your article choice Meet with librarian Discuss article w/team Turn in article with librarian and attending signature Faith Assessment Read articles Attend workshop Interview w/ FICA Present to team IPE Activity Complete activity in E-value Due? after orientation but w/in 48 hours Will do at noon on 1st day Turn in @ end of Clerkship □ □ □ Before Ice Cream social Cards due @ end of Clerkship Cards due @ end of Clerkship Meet with librarian before the end of week 5. Paper due the last Wednesday of Clerkship □ □ @ end of Clerkship hand in card □ □ □ □ (not mandatory) Diagnosis & Procedure list Simulation Online Cases Attend 11 Morning Reports Evaluations Fill out E-value form by the □ See all required dx with direct/team based care 5th Friday of the rotation Check with attending at midpoint for help Complete all procedures on list 5th Friday of Clerkship □ Attend lecture (if a conflict with call watch tegrity) Simulation Session (mandatory attendance) General Internal Medicine □ Rheumatology □ Noon before professor rounds Infectious Disease □ Endocrinology □ Cardiology □ Nephrology □ Gastroenterology □ Heme/Onc □ Pulmonary □ Pain Manage. □ 11 over 6 weeks. STUDENTS MUST SWIPE IN □ □ □ □ □ □ □ □ □ □ □ Need to get course grade At end of rotation □ 1 OVERVIEW You (the student) will spend six weeks assigned to the inpatient teams at the Department of Medicine at the Veterans Affairs Medical Center or the General Medicine service at the Medical University Hospital (Main hospital or Ashley River Tower). The student will participate with the team in the evaluation and therapy of the patients on these inpatient clinical services. Each team is composed of an attending physician, a medicine resident (PGY 2 or 3), two interns (PGY 1), and possibly an extern (senior medical student). You will work with this team every day. You will evaluate patients admitted to the service. Attendings and residents should give you an orientation session at the beginning of their service, clearly outlining what they expect from you. Please be sure that you and your attending and resident sit down to discuss these expectations. GOALS During the Medicine Clerkship, students will acquire patient care skills, professional behaviors, medical knowledge, interpersonal and communication skills, practice-based lifelong learning and system-based practice skills that are necessary to evaluate and deliver safe, quality and evidence-based care for adult patients under the consistent supervision of residents and attending physicians. OBJECTIVES Internal Medicine Clerkship Objectives At the end of this rotation, the student should be able to do the following: 1. Medical Knowledge (MK) a. Apply knowledge of the pathophysiology, epidemiology, and natural history of diseases to common patient conditions listed in the Core Required and Recommended Medical Conditions. (MK3, MK4) b. Describe the scientific principles underlying diagnostic methods, including laboratory and radiologic testing, and treatment approaches (pharmacologic and non-pharmacologic) that may be applied to major diseases and conditions. (MK5) c. Explain how preventive measures, health behaviors and social determinants affect disease, injury and health in individual patients and across populations. (MK7) 2. Patient Care (PC) a. Demonstrate proper techniques for interviewing a patient to obtain a medical history and performing a physical examination in the inpatient setting. (PC1) b. Demonstrate analysis, synthesis, and integration of pertinent patient data. (PC2) c. Formulate a comprehensive, ordered differential diagnosis for common inpatient medical conditions. (PC2) d. Demonstrate an ability to build a positive, healing relationship with a patient inclusive of culture, ethnicity, spirituality, gender, age, health beliefs, practices, and decisions. (PC4) 3. Interpersonal and Communication Skills (CS) a. Present patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. (CS1) 2 b. Document patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. (CS1) c. Demonstrate effective and professional interpersonal and communication skills in interactions with patients and families, including an awareness of psychosocial factors related to patients’ problems. (CS2) 4. Professionalism (PR) a. Demonstrate honesty, integrity, respect, and compassion in all interactions with patients, peers, faculty, staff, and other health care professionals in all settings. (PR1) b. Demonstrate ethical, patient-centered decision making and respect for the confidentiality of patient information in all settings (i.e., clinical, academic, electronic, or web-based). (PR2) c. Demonstrate sensitivity and responsiveness to the personhood of the patient inclusive of culture, ethnicity, spirituality, gender, age, disabilities, and other aspects of personal and health beliefs, practices, and decisions. (PR3) d. Demonstrate accountability for academic, patient care and professional responsibilities, and a commitment to continuous professional development. (PR4) e. Acknowledge personal limitations and mistakes openly and honestly, and critically evaluate mistakes to promote professional development. (PR5) 5. Practice-based Learning and Improvement (PL) a. Use evidence-based medicine to determine patient care decisions. (PL3, MK8) b. Identify errors in patient care and knowledge deficits, and change future practices based on past mistakes. (PL4) c. Use information technology successfully to access and manage patient information. (PL4) 6. Systems-based Learning (SL) a. Identify issues related to the cost-effectiveness of diagnostic evaluations and patient care. (SL1) b. Demonstrate appreciation for and collaboration with other members of the health care team including nursing, social workers, care managers, pharmacy, etc. (SL3, PC8) 3 Entrustable Professional Activity: With significant supervision, admit a patient to the General Medicine Service You will receive cards to have your residents and attendings fill out documenting your progress accomplishing the milestones listed below. Please ask Mary Ann Snell if you require more cards. Sometimes one evaluator cannot give feedback in all areas, so you will need to have another session or evaluator watch you. Also, you may not accomplish all of the milestones as quickly as other students. If that is the case, you should get additional cards in order to be monitored accomplishing all of the milestones. YOU NEED TO TELL YOUR PRECEPTOR BEFORE YOUR HISTORY/PRESENTATION/EXAMINATION THAT YOU WOULD LIKE TO BE EVALUATED (HAVE YOUR CARD FILLED OUT). Milestones Historical Data Gathering: 1. Acquire accurate and relevant history from the patient 2. Seek and obtain data from secondary sources (e.g. family, records, pharmacy) 3. Document and report clinical information truthfully Performing a Physical Exam: 1. Perform an accurate physical examination and identify pertinent abnormalities using common maneuvers 2. Accurately track important changes in the physical examination over time in the inpatient settings Clinical Reasoning: 1. Synthesize all available data, including interview, physical examination, and preliminary laboratory data, to define each patient’s central clinical problem 2. Formulate a comprehensive, ordered differential diagnoses, followed by an evidence based diagnostic and therapeutic plan for common inpatient conditions 3. Modify differential diagnosis and care plan based upon clinical course and data as appropriate 4. Students will acquire and demonstrate knowledge of the basic and clinical science of medical problems of adult patients listed in the core curriculum medical conditions (See Medical Knowledge Objectives Section ) Diagnostic Tests: 1. Understand indications for, report and interpret common diagnostic testing, including CBC, BMP, LFTs, UA, CXR, arterial blood gas, blood cultures, and EKG Technology 1. Use information technology successfully to access and manage patient information Patient Management 4 COM Competency Assessment Methods PC1 PC1 Direct Observation Team Rounds Review of Student Note Simulation PR1 PC1 PC1 PC2 PC2, PL3 Direct Observation Team Rounds Review of Student Note Simulation Direct Observation Team Rounds Review of Student Note Simulation EBM activity PC2, PC3, MK6 MK3, MK4 MK 5, PC7 Direct Observation Team Rounds Review of Student Note Simulation PC3, PL4 Team Rounds Review of Student Note 1. Present patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. 2. Document patient data gathered from patient interviews, physical examinations, and laboratory sources, including progress notes on patients, in standardized format. 3. Begin to learn to recognize situations with a need for urgent or emergent medical care including life threatening conditions 4. Recognize when to seek additional guidance 5. Customize care in the context of the patient’s preferences and overall health 6. Take a spiritual assessment of a patient and apply the findings to the patients care 7. Demonstrate an ability to build a positive, healing relationship with a patient 8. Communicate effectively with non-physician members of the health care team (PharmDs, Case Managers, Nurses) to better patient care and assist patients in dealing with system complexities CS1 CS1 PC3 Direct Observation Team Rounds Review of Student Note Simulation Faith Assessment Activity Interprofessional Activity Night Shift Activity PR5 PC4 PC4 CS2 PC8, CS3, SL2, SL3 Key: MK = Medical Knowledge; PC = Patient Care; PL = Practiced Based and Lifelong Learning; PR = Professionalism; SL = System-based Learning; CS = Interpersonal Communication 5 Core Medical Conditions You will be required to maintain a Patient Diagnoses Log and Procedure Log in E-value in order to document your clinical activities while on the medicine rotation. You will be given a card to help you with this. This report indicates the diagnosis and level of responsibility. Data from these reports are used by the department to judge the adequacy of clinical exposure each student experiences. It is important to remember that not only a patient’s admitting diagnosis will count, but a patient’s co-morbidities should also count. Please keep track of diagnoses that your patient had vs. those you saw with your team vs. those that you were exposed to via other avenues (Professor Rounds/Online curriculum). The following conditions are REQUIRED. The student must see the patient in direct care (the student has responsibility for the patient) or team based care (the patient is on the student’s team). Each student must see at least one patient with each disorder during the rotation in the inpatient setting. If a student is unable to see a patient with the diagnosis, the Clerkship Director will use the following resources to ensure the student has exposure to these important topics. Professor Rounds: ABG Acid-Base Disorder Acute Kidney Disease Professor Rounds: Nephrology Anemia Professor Rounds: Heme-Onc Chest Pain Professor Rounds: Cardiology, Unstable Patient #1 Chronic Kidney Disease Professor Rounds: Nephrology Congestive Heart Failure Professor Rounds: Cardiology Diabetes I or II Professor Rounds: Endocrinology DVT/PE Professor Rounds: General Internal Medicine, Unstable Patient #1 and 2 Dyspnea Professor Rounds: Unstable Patient #1 and #2 Fever Professor Rounds: General Internal Medicine (GIM) GERD Case posted under “Didactics on website Hyperlipidemia Professor Rounds: Cardiology, Unstable Patient #1 and GIM Hypertension Professor Rounds: Cardiology, Unstable Patient #1 & 2 and GIM Pneumonia (CAP/HAP) Professor Rounds: GIM Substance Abuse Simple case 9, 26 UTI Simple case 35 The following procedures are REQUIRED. Please report and interpret the following tests during rounds to your attending and residents: Basic Metabolic Panel (BMP) Liver Function Tests (LFTs) Complete Blood Count (CBC) Urinalysis (UA) Chest X-ray (CXR) Electrocardiogram (EKG) 6 Blood Cultures STUDENT RESPONSIBILITIES 1. All Internal Medicine courses adhere to the “Medical Student Supervision and Teaching Policy” approved by the MUSC COM UCC on June 15, 2012. 2. Students are allowed to see and perform non-invasive exams on patients that have been assigned to them by their attendings or residents unsupervised. For invasive exams (breast, genital, rectal), a resident or attending physician must be present. 3. Students are allowed to participate in ANY procedure that is common to internal medicine with approval and supervision by the certified healthcare provider (this includes but is not limited to: the nurse, respiratory therapist, resident or attending physician) performing that procedure. This includes but is not limited to IV or central line placement, ABGs, lumbar punctures, arthrocentesis, thoracentesis, or paracentesis. 4. New Patients: a. History and Physical: Performance of a complete history and physical examination on a new patient being admitted to the hospital. In addition, you should collect all relevant imaging and laboratory data that is available at the time. b. Documentation: You should write up your history and physical. This record should reflect your findings and your opinions. Do not plagiarize the written assessment of someone else. This record should include: the chief complaint, the history of the present illness, review of systems; family history; social history, medications, physical examination, assessment and plan regarding further evaluation of the patient in order to establish the appropriate diagnosis. Include treatment plans and issues related to short and long term prognosis whenever possible. In general, this assessment and plan should reflect that you have both read and learned about the possible diseases under consideration in your particular patient. Please see the EPIC instructions on how to write your note and send it to the attending or resident for feedback. c. Presentation of the new patient to the attending: this presentation will occur after the patient has been admitted. The presentation should consist of a logical, orderly, concise presentation of the patient’s history and physical examination findings. Be prepared to go to the bedside to demonstrate the relevant findings and discuss further history with the patient. You should have available at the time of the presentation any relevant imaging, graphic or laboratory data related to the patient. Each student will present at least two new patients per week to the attending physician. 5. Current Patients: You should be carrying at least 2-3 patients at a time. By week 3, you should carry 3 patients regularly unless the team patient load is not sufficient to do so. There is no “cap” as to the number of patients a student can carry. a. YOU SHOULD ATTEND THE INTERN – INTERN CHECKOUT EVERY MORNING. INTERN/INTERN HANDOFF: Please attend morning checkout daily while on day shifts – including weekends. Please ask the Chief residents and your team for details of where checkout will occur. b. Pre-Rounds: i. Every morning you will see the patients assigned to you. You will interview them to see how they are doing. In addition, you should speak to ancillary staff to find out if there were any significant events over night that the patient did not tell you about. ii. Collect all other data that has been obtained in the past 24 hours, this includes but is not limited to: vitals, physical exam, new labs (don’t forget to check for labs that were ordered several days ago but may have just come back), new radiology and other procedures. (This data will go in the “Objective” portion of your note.) iii. Write a daily progress note in the medical record of all of your patients. You are encouraged to discuss your assessment and plan with your resident prior to attending rounds. c. Attending Rounds: each morning the Attending will round with the entire team. Students should present the significant data relating to their patients that they obtained during pre-rounds. Student participation in clinical rounds on weekends is required. d. After Rounds: You will help your residents with the care of the patient: write orders, prescriptions, order radiology… e. Afternoon rounds: you are strongly encouraged to see each of your patients on your own in the afternoon to follow up on the issues that you identified in the morning. If they were vomiting, have they stopped? If they were in pain and you increased their opioids, are they still in pain? Report any findings to your residents so that they can help you address any issues that you have discovered. f. Read about each one of your patients daily. 6. Direct Observation: Mary Ann Snell will email you with the name of an attending and the week that you will have an appointment for direct observation from your attending. IT IS YOUR RESPONSIBILITY TO MAKE SURE THIS APPOINTMENT IS SCHEDULED. Please approach your attending at the beginning of the week to arrange the time. During this exercise you will see a new patient that is being admitted to your team OR one that has been admitted to another team. You will do a focused history of present illness and a focused physical exam. Please ask your attending what they want you to focus on prior to meeting the patient. 7. Weekends: a. At least one student must be present to round with the team each weekend day and minor holiday. 8. Evening shifts/Overnight call: a. The purpose of night shifts is the opportunity to evaluate new patients admitted and to participate actively in the evaluation and management of inpatients who are acutely ill. Thus, the student should work closely with the intern on call, accompanying him or her to the bedside, working up and evaluating emergency admissions. b. You are expected to take your night shifts in the hospital. Lack of availability is considered abandonment of your patient, a violation of professional ethics, and is considered grounds for failure of the course. Your responsibility is to be in house even if your resident tells you to go home. c. An evening shift is until 8 pm on General Medicine. You will do 3 evening shifts in 6 weeks. You may do 1 volunteer shift at a clinic for the underserved in the Charleston area in exchange for 1 of these shifts. d. Overnight call is from 7 am until 12 pm the next day. You will be excused from Professor Rounds when you are post-call, however, your online curriculum must be complete on time (noon the day of professor rounds). We highly recommend you completing the online curriculum the day before your shift. You will do 4 overnight shifts. i. DO NOT COME IN PRIOR TO 7AM. Otherwise you may break work hours. You are still required to complete your pre-rounding prior to morning report and teaching rounds. e. There is a call room located at 124 CSB for your availability. The code to the outside door is 124. The code to the inside female door is 952. f. ART Call Room - The room number is ART 2414. Email your badge number to Dean Braddy to receive access. g. You will meet with Mary Ann at noon on the first day to choose your call schedule. 9. Notes: a. You are expected to write a note on every new patient you admit and a SOAP note on every one of your patients every day. Ask your attending how they want you to send them your notes for review (paper or EPIC routing or VA chart). You should have 2-4 notes/H&Ps reviewed per week. Discharge summaries: you are not allowed to do the actual discharge summary. However, you should practice writing these. They can be done in EPIC (main hospital) using the medical student note tab and the .IMDISCHARGESUMMARY dot phrase. EPIC INSTRUCTIONS Instructions for EPIC can be found on the Internal Medicine Student Website at the following link: http://clinicaldepartments.musc.edu/medicine/education/medstudents/EPIC ACTIVITIES TIME Before Morning Report or Morning Rounds Monday Attend Intern Check out Pre-Rounds 8:00 – 9:00 am 8:30 – 9:30 am 8:30 – 9:30 am 9:30 – 11:30 am Time dependent on faculty member 12:00 – 1:00 pm 3:00 – 4:00 pm 4:00 – 5:00 pm Tuesday Attend Intern Check out Pre-Rounds Wednesday Attend Intern Check out Pre-Rounds Thursday Attend Intern Check out Pre-Rounds Friday Attend Intern Check out Pre-Rounds Attending Rounds (MUH) Attending Rounds (VAH) Morning Report (MUH – 300 CSB) Morning Report (4th fl Med Conf Room VAH) Attending Rounds (MUH) Attending Rounds (VAH) Noon Conf. 300 CSB Noon Conf. 300 CSB Professor Rounds – refer to schedule for specific times and rooms Professor Rounds – refer to schedule for specific times and rooms Grand Rounds IOP Auditorium 1st Floor Morning Report (MUH – 300 CSB) Morning Report (4th fl Med Conf Room VAH) Attending Rounds (MUH) Attending Rounds (VAH) Noon Conf. 300 CSB Discussion of Int. Med., 3 -4 p.m., Rm. 300 CSB Professor Rounds – refer to schedule for specific times and rooms Attending Rounds (MUH) Attending Rounds (VAH) Noon Conf. 300 CSB Morning Report (MUH – 1119 ART) Morning Report (4th fl Med Conf Room VAH) Attending Rounds (MUH) Attending Rounds (VAH) Noon Conf. 300 CSB Professor Rounds – refer to schedule for specific times and rooms Professor Rounds – refer to schedule for specific times and rooms MORNING REPORT: Conference with presentations of new and interesting patients, led by the chief residents at each hospital. Students must attend 11 morning reports during their 6 week rotation. Students must swipe in. Students on the Ashley River Tower (ART) team should attending morning report at the main hospital (Mon/Fri) and ART (Wed) with the other students on Gen Med at the Main hospital. GRAND ROUNDS: Weekly presentation in IOP Auditorium. All inpatient students are required to attend. Students are not to swipe in. NOON CONFERENCE: This conference will cover the basic topics of Internal Medicine. Ask your resident what the topic is. You are encouraged to attend but these are not mandatory. In 300 CSB unless otherwise notified. Students are not to swipe in. STUDENTS ARE NOT EXPECTED TO ATTEND CONFERENCES AFTER COMPLETING AN OVERNIGHT SHIFT. OTHER ACTIVITIES PROFESSOR ROUNDS 1. Objectives: see individual case discussions that will be handed out at each session 2. You must log on to Moodle and do your online cases (read the cases, answer the questions and read/study the discussion sections) prior to noon the day of the matching professor rounds to get credit. a. You are required to do these cases in their entirety by noon the day of the session in order to receive credit. The course coordinator will audit these cases for each session. All cases and quizzes must be complete by the last day of the course, even if you did not get credit for them the day of the class. b. Professor rounds will be tegritied and available for viewing if you miss the session because you are pre/post call 3. Arterial Blood Gas workshop: THERE IS NO READING/HOMEWORK PRIOR TO WORKSHOP a. Ideally, after the session the students should be able to interpret an answer the following questions: i. Is the ABG interpretable? ii. What is the primary disorder? iii. If it is a respiratory disorder, is it acute or chronic? iv. If there is an anion gap acidosis, is there another metabolic disturbance also? v. Is there a secondary or tertiary disorder? 4. See Professor Rounds handout for details. EVIDENCE BASED MEDICINE: this activity should be done one time during your rotation. 1. Objectives: a. Be able to formulate a clinical question and put in PICO format. b. Perform a literature search using a medicine database. c. Pick the article with the best level of evidence that answers the clinical question. d. Use the article to formulate a comprehensive and evidence based diagnostic or therapeutic plan for one of your patients. 2. On Attending Rounds you and the other students on your team will create a clinical question with your attending involving one of your patients. Remember, the attending will not prompt you to do this, so you will have to take the initiative to raise the question. With the residents and attending, you should refine the question. The question does not need to be complicated. The question can be to challenge a commonly accepted treatment in internal medicine or answer a question to which no one knows the answer. 3. As a group, you and the other students on your team should do a literature search (using a PICO format) to find an article that answers your question. Please choose an article that is the best level of evidence. 4. Make an appointment with Candace Moorer before the end of the 5th week of the rotation (she may direct you to meet with one of her colleagues): moorerc@musc.edu; 792-5167. Prior to your meeting, email her your clinical question, your article of choice, and your search results (that was done in a PICO format). At your appointment, she will review how to do a search and compare her search results with yours. She will also assess how well you were able to pick the best level of evidence. She will report all of the groups that completed this exercise to Mrs. Snell. 5. Bring the article to rounds, after meeting with the librarian, to discuss how it impacts the choice of care for your patient. Have your attending sign the top of your article, indicating that it was discussed with the group. 6. The article with librarian and attending signature must be turned in when completed or at the end of the rotation. 7. You will be graded out of 5 points. Points are assigned based on your clinical question, having a meeting with the librarian, putting your question in a PICO format, doing the literature search and picking the best level of evidence. 8. It must be completed by Wednesday at 5pm the last week of the rotation. SIMULATION 1. You will be required to attend two lectures on an “Unstable Patient.” If you are on nights, you will be required to watch the lectures on Tegrity. 2. The 5th Friday afternoon of the rotation you will come to the simulation center to practice the concepts taught in the lecture. Some rotations may have a change in the schedule so be sure to check your professor rounds schedule. INTERPROFESSIONAL ACTIVITY: the following activities will be available to you to meet your interprofessional requirements for the third year. Experiences should be logged into E-value. 1. Objectives: a. Communicate effectively with non-physician members of the health care team (PharmDs, Case Managers, Nurses) to better patient care and assist patients in dealing with system complexities. b. Practice seeking and obtaining data from secondary sources. c. Recognize when to seek additional guidance in order to benefit patient care 2. MUSC: a. PharmD: there will be a PharmD resident or faculty who rounds regularly with your team. Ask them to meet with you after rounds. Review your patients’ medication lists for the following (including but not limited to): drug interactions, dosage errors, and antibiotic choices. b. Case Manager: meet with the case manager of your team to review the discharge needs of all of your patients. c. Medicine IP: an interprofessional team reviews all of the patients on a team. Time is variable. Ask your resident for the time. 3. VA: a. Case Manager: meet with your case manager who rounds with your team to review the discharge needs of all of your patients. b. Medicine ITP: an interprofessional team reviews all of the patients on a team. Time is variable. Ask your resident for the time. CULTURAL COMPETENCY ACTIVITY 1. Objectives a. Learn how to take a spiritual assessment of a patient and apply the findings to the patients care. b. Demonstrate an ability to build a positive, healing relationship with a patient. c. Recognize when to seek additional guidance in order to benefit patient care – for example calling a chaplain. d. Customize care in the context of the patient’s preferences and overall health 2. Instructions: a. Please read the two articles for this activity prior to the workshop. They can be found at http://clinicaldepartments.musc.edu/medicine/education/medstudents, under “Didactics.” b. You will attend the workshop “Faith and Healing in the Hospital: How to Empower Patient Spirituality Without Preaching.” Here you will learn the importance of a spiritual history and how to take one. Must attend post-call if scheduled at noon or earlier. Do not have to attend if pre-call. c. You will use the FICA interview to take a spiritual assessment of the patient of your choice. i. F = Is faith in God important to you? ii. I = What impact does your faith have on your life? iii. C = How important is your faith community to you? iv. A = How can I can assist you? v. Reference: Puchalski CM. Taking a Spiritual History: FICA. Spirituality and Medicine Connection 1999:3:1. d. In your H&P or SOAP note, please document the following: i. Under the objective section: record the patient’s answers/results to the assessment. ii. Under your plan: state the problem and record how you are going to address the problem. iii. Present your findings as a part of your presentation. iv. Ask your attending to sign off on your card that you did the activity appropriately. If your attending believes the activity was not performed adequately, you will be asked to repeat the activity. e. Grading: this activity must be completed by Wednesday at 5pm of the last week of your rotation. If this activity is not completed, 5 points will be deducted from your educational grade. GRADING POLICY FEEDBACK 1) The following cards will be filled out in order to let you know if you are meeting the milestones set out in order to accomplish the EPA prior to finishing the rotation. a. History card: you will be given 1 card to have an attending fill out in order to give you feedback on your history taking skills. b. Physical exam card: you will be given 1 card to have an attending or upper level resident fill out in order to give you feedback on your physical exam skills. i. They must watch you perform a pertinent physical exam c. SOAP note card: you will be given 1 card to have an attending fill out in order to give you feedback on SOAP notes. 2) d. H&P card: you will be given 1 card to have an attending or a resident fill out in order to give you feedback on your complete admission. e. If you are not meeting your milestones, please discuss the issue(s) with your resident and attending physician. Midpoint cards: you will be given 2 of these cards to be completed by 1 attending and a resident or 2 attending physicians. These cards should be completed prior and brought to the ice cream social. EVALUATIONS 1) This course follows the MUSC COM Clinical Course Grading and Assessment policy as follows: “3rd Year Clerkship & Selectives Failure (Approved on May 1st, 2015) Each clerkship, selective, and required course, sets criteria for failure, pass, and honors for the course prior to the start of each academic year. These criteria will be made available to students at the beginning of each clerkship/course in written form. All clinical faculty and rotations will assess the clinical performance of students using the standardized COM Clinical Performance Evaluation (CPE). A student will FAIL the clerkship or selective if any one of the following conditions is met: A Clinical Performance Evaluation grade of 2.5 or lower (41 out of 64 pts), or at the discretion of the course director if the following occurs, one (1) or more ratings of “rarely, if ever”, or four (4) or more ratings of “inconsistently”. A written exam grade at a minimum of at least two (2) standard deviations below the national norm for that exam. A failing grade on any secondary component (of the grade). Additionally, a student is eligible for failure at the discretion of the Clerkship Director for unprofessional behavior. What if a student fails some component of the grade? If a student fails the clinical component of the grade (CPE), the student must repeat the course. The Medical Student Performance Evaluation (MSPE) and the academic transcript will reflect the failure and repeating of the course. If a student fails the written examination, the student will receive a grade of “Incomplete” (IN) and will have the opportunity to remediate that exam. The student will not be eligible to receive honors for the written exam or for the course as a whole regardless of the score obtained on the remediated exam. A note will be made in the Medical Student Performance Evaluation (MSPE) of the need to remediate the exam. If the written examination is failed a second time, the student must repeat the course. The MSPE and the academic transcript will reflect the failure and repeating of the course. If a student fails a secondary component of the grade (i.e., OSCE) the student will receive a grade if “Incomplete” (IN) and will have the opportunity to remediate that portion of the grade. The student will not receive honors for the course as a whole regardless of their performance on the remediated component. If the secondary component is failed a second time, the student must repeat the course. A note will be made in the MSPE of the need to remediate that component. Policy: 3rd Year Clerkship Honors (Approved on November 18, 2011) The criteria for the designation of Honors will be determined by each clerkship and approved by the appropriate academic committees. Each clerkship will publish Honors criteria prior to the start of the academic year and will make this information available to students at the beginning of the clerkship in written form. 2) Criteria for HONORS: a) NBME subject exam score: 79 or higher b) Clinical Performance Evaluations: must obtain an average of 13 “Almost Always” with the rest of the criteria being evaluated as “Consistently”. i) Average of 61 out of 64 points on the CPE form (GPA of 3.81) c) Other: must obtain 21 out of 25 Educational Activities points. d) CAVEAT: If a student receives an average of 62 out of 64 points or higher on their clinical grade, obtains 23 out of 25 Educational Activities points and a 75-78 on their shelf, they will receive HONORS for the overall course (despite not honoring the shelf exam). e) An honors grade may be reviewed and potentially withheld if the student obtains any “Rarely, if ever” on any evaluation, has more than 4 “Inconsistently” marks on any evaluation, or has any professionalism issues raised by on their evaluations as indicated by a “Yes” being checked on questions 19-23. 3) Criteria for FAILING: A student will FAIL the clerkship or selective if any one of the following conditions is met: a) NBME subject exam score: 49 or less – i) Please see below regarding the passing with remediation range b) A Clinical Performance Evaluation: i) <9 frequently marks ii) Average grade of 40 out of 64 points or less (GPA 2.5 or lower), iii) or at the discretion of the course director if the following occurs: (1) One (1) or more ratings of “rarely, if ever” (2) Four (4) or more ratings of “inconsistently”. c) Other: 16 (or less) out of 25 Educational Activities points. d) A passing grade may be reviewed and potentially withheld if the student obtains any professionalism issues raised by on their evaluations as indicated by a “Yes” being checked on questions 19-23. 4) The National Board of Medical Examiners (NBME) mini-board examination. a) This clerkship uses the NBME Subject Exam in Internal Medicine as the written exam. The NBME shares the national performance data with schools to assist with setting pass/fail cut points. A student may fall into one of four categories based on individual exam performance: (1) Honors (2) Pass (3) Passing but required to retake the exam prior to the start of 4th year. Score on retake will not affect the initial grade, however MSPE comments may reflect knowledge base, but the need to retake the exam will not be noted in the MSPE. Honors ineligible on retake. (4) Failing with remediation required to pass. Retaking the exam should occur prior to the start of 4th year and noted in the MSPE. Failing second attempt, will result in failure of the clerkship Score Category Scores Honors Eligible Greater than or equal to 79 Pass Range 58-78 Passing with Required Retake Range 50-57 Failing with Remediation Less than or equal to 49 b) The Clinical Science Medicine content tested in the NBME includes: General Principles 1%–5% Organ Systems Immunologic Disorders 5%–10% Diseases of the Blood and Blood-forming Organs 5%–10% Diseases of the Nervous System and Special Senses 5%–10% Cardiovascular Disorders 15%–20% Diseases of the Respiratory System 15%–20% Nutritional and Digestive Disorders 10%–15% Gynecologic Disorders 1%–5% Renal, Urinary, and Male Reproductive System 10%–15% Disorders of the Skin and Subcutaneous Tissues 5%–10% Diseases of the Musculoskeletal System and Connective Tissue 5%–10% Endocrine and Metabolic Disorders 5%–10% Physician Tasks Promoting Health and Health Maintenance 10%–15% Understanding Mechanisms of Disease 20%–25% Establishing a Diagnosis 40%–45% Applying Principles of Management 20%–25% 5) Clinical Performance Evaluation Form: The Evaluation Committee’s grade is determined from evaluations made by the attending and resident physicians who have worked with the student during the rotation. Feedback to the student occurs principally through a mid-point evaluation form, completed by the student and attending at the mid-point of each rotation. Students should also meet formally with the attending at the end of the rotation to discuss performance. If a student fails their Clinical performance section, they must retake the course in its entirety. 6) Educational Activity Points. The educational activity grade will be broken down as follows: a) EBM = 5 possible points - see activities section for details. b) Professor Rounds = 10 possible points (½ pt. for completing the on-line material and questions before noon the day of the discussion and ½ pt. for attending the session except for those post call.) c) Evening/Night shift activities = 10 possible points. Attendance to night and evening shifts is mandatory in order to pass this course. Please complete all activities outlined on your card in order to receive 1 point per shift toward your educational grade. d) Cultural competency activity: if not completed, 5 points will be deducted from your educational activity grade. 7) Students may ask the Clerkship Director to have the Internal Medicine Education Committee review the grade. If the grade is upheld, the student may appeal their grade to the Clinical Sciences Planning and Evaluation Committee. If the matter is not resolved to the satisfaction of the student and the student continues to feel that a wrong has occurred, the student may petition in writing Dr. Donna Kern and Dr. Debra Hazen-Martin for a final appeal. STUDENT CONDUCT Students should exhibit professional and ethical behavior at all times. Among other things, this includes appropriate dress, demeanor, attendance, promptness, and appropriate interactions with health care providers. Code of Conduct MUSC and the College of Medicine are invested in maintaining an academic and clinical environment in which students, faculty, fellows, residents, nurses and staff can work together freely without threat of mistreatment or bias with regard to their race, color, religion, sex, sexual orientation, national or ethnic origin, age, disability or any other factor irrelevant to participation in the activities of the College. Students are responsible for reading and understanding the Code of Conduct Policy. https://www.musc.edu/medcenter/policy/stds_of_conduct.pdf Attendance: 1. You will get 6 weekend days off, and be excused at noon the Wednesday before the written exam. 2. The Thursday and Friday of Thanksgiving weekend are the only holidays observed on this rotation. Minor holidays (Labor Day, Fourth of July, Memorial Day – for example) are not observed. However, these minor holidays will be treated like a weekend day. 3. We adhere to the MUSC College of Medicine 3rd Year Student Absence Policy. See link on Welcome page for details. No make-up necessary for up to 2 days: death, illness (MD note), wedding (immediate family). Any other excused absences must be made up in a timely manner. 4. You have a daily commitment to be at work with your team. You must receive prior approval from Dr. DeWaay, your course director, in order to be absent from the rotation. For absences that are requested in advanced, an absence form must be filled out and emailed to Mary Ann Snell. For emergency situations (illness, death in family, etc.), an email needs to be sent to Dr. DeWaay (dewaay@musc.edu) and the coordinator (snellma@musc.edu). Once that approval has been received it will then be your responsibility to let your team know you will be gone. It is not enough to just notify your team. You are expected to adhere to the specific schedule given to you. Days off cannot deviate from this schedule unless prior approval is obtained. 5. Attendance at all scheduled student activities of the Department of Medicine is required, including, but not limited to, work rounds, attending rounds, teaching rounds, Professor Rounds, medical grand rounds, and morning report. Other conferences are optional and may be attended by the student as desired and these would include such things as residents and primary care noon conferences. Please see Activities section for details. Dress Code: You are expected to dress professionally. Patients will recognize you as a concerned member of the medical team, and will expect (and deserve) appropriate attire on your part. Attendings and residents reserve the right to comment on the appropriateness of dress. Name tags must be worn at all times. Policies and Procedures: This clerkship follows all COM and MUSC policies and procedures regarding students. Please contact the Clerkship Director if any are violated so that the situation can be rectified. Links to pertinent policies can be found on our website. If you cannot find a particular policy please contact Mary Ann Snell. COURSE EVALUATION In order to continue to improve the Internal Medicine Core Rotation, you will be required to critique both the Course, Professor Rounds using the E-value system. You will also be required to critique the attendings, residents, and fellows with whom you worked. These comments are totally anonymous, held in the strictest confidence, and are never seen by the attendings, residents, or fellows. These evaluations need to be completed by the Monday following completion of the rotation. PROBLEMS If you have any questions or problems during your rotation, please call the student coordinator at 7927282 (807 E CSB). If you have any problems on the service during the rotation, please contact the student coordinator, or Clerkship director. If you would like to meet with the Clerkship director during or after the rotation, you may schedule an appointment by contacting your student coordinator. Course Director: Deborah DeWaay, M.D., dewaay@musc.edu Pager #14523