Introduction to Psychology
advertisement

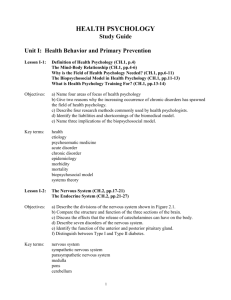
HEALTH PSYCHOLOGY Study Guide Unit I: Health Behavior and Primary Prevention Lesson I-1: What is Health Psychology? Objectives: a) Name four areas of focus of health psychology b) Give two reasons why the increasing occurrence of chronic disorders has spawned the field of health psychology. c) Describe four research methods commonly used by health psychologists. d) Identify the liabilities and shortcomings of the biomedical model. e) Name three implications of the biopsychosocial model. Key terms: health etiology psychosomatic medicine acute disorder chronic disorder epidemiology morbidity mortality biopsychosocial model systems theory Lesson I-2: The Nervous System and Endocrine System Objectives: a) Describe the divisions of the nervous system shown in Figure 2.1. b) Compare the structure and function of the three sections of the brain. c) Discuss the effects that the release of catecholamines can have on the body. d) Describe seven disorders of the nervous system. e) Identify the function of the anterior and posterior pituitary gland. f) Distinguish between Type I and Type II diabetes. Key terms: nervous system sympathetic nervous system parasympathetic nervous system medulla pons cerebellum thalamus hypothalamus cerebral cortex neurotransmitter catecholamine 1 endocrine system pituitary gland adrenal glands Lesson I-3: The Cardiovascular System and Respiratory System Objectives: a) Discuss the role of the blood as a transport system. b) Explain how the arteries and veins differ in their function. c) Distinguish between the systole and diastole phases of the cardiac cycle. d) Identify the factors that affect heart rate. e) Describe the common disorders of the cardiovascular system, including those related to blood cell production and clotting. f) Identify the factors that influence blood pressure. g) List the components of blood. h) Name thee major functions of the respiratory system. i) Describe the common disorders the respiratory system. Key terms: cardiovascular system atherosclerosis angina pectoris myocardial infarction (MI) blood pressure platelets respiratory system Lesson I-4: The Digestive System, Renal System, and Reproductive System Objectives: a) Discuss the role of the stomach, pancreas, liver, small intestine, and large intestine in digestion. b) Describe the common disorders of the digestive system. c) Identify the contents and function of urine. d) Name two functions of the kidneys. e) Describe the common disorders of the renal system. f) Discuss the role of estrogen, progesterone and testosterone in sexual development. g) Describe the common disorders of the reproductive system. Key terms: renal system kidney dialysis Lesson I-5: The Immune System Objectives: a) Compare the four ways in which microbes are transmitted to people. b) List three factors that determine whether or not invading microbes will produce an infection. c) Identify the four phases of an infection and the three types of infections. d) Distinguish between specific and nonspecific immune mechanisms. 2 e) Describe the four main ways that nonspecific immunity is mediated. f) Distinguish between humoral and cell-mediated immunity. g) Discuss the role of the spleen, tonsils and thymus gland in immunity. h) Describe common disorders related to the immune system. Key terms: immunity specific immune mechanism nonspecific immune mechanism phagocytosis humoral immunity cell-mediated immunity lymphatic system autoimmunity Lesson I-6: Health Promotion and Health Behavior Objectives: a) Explain how disease patterns in the U.S. have changed in the last 90 years. b) List four beneficial effects associated with the modification of health behaviors. c) Name seven good health habits that can lower mortality rates. d) Describe two general strategies of primary prevention. e) List the most common teachable moments in the life cycle. f) Discuss the difficulties in working with at-risk populations. g) Identify the focus of health promotion efforts with the elderly. Key terms: health promotion health behavior health habit primary prevention health locus of control socialization teachable moment window of vulnerability PRACTICE TEST I-A Lesson I-7: Changing Health Habits Objectives: a) Identify the problems that can occur when an educational appeal focuses on negative information regarding health risks. b) Discuss the two factors that determine whether or not a person will practice a specific health behavior, according to the health belief model. c) Describe the relationship between self-efficacy and health behavior. d) Name the three components of behavioral intention. Key terms: fear appeal health belief model 3 self-efficacy theory of planned behavior Lesson I-8: Cognitive-Behavioral Approaches Objectives: a) List two steps in self-observation. b) Give an example of how classical and operant conditioning can be used to change health behavior. c) Identify the conditions under which modeling is most effective in reducing fear. d) Explain how stimulus-control interventions can be used to treat obesity. e) Summarize the findings of Mahoney (1974). f) Identify two conclusions concerning the use of self-punishment. g) Give examples of contingency contracting and cognitive restructuring. h) List three goals of social skills programs. i) Identify the relapse rates for addictive disorders. j) Explain why relapse occurs. k) List the positive and negative consequences of relapse. l) Describe three interventions used to reduce the rate of relapse. Key terms: cognitive-behavior therapy self-observation self-monitoring classical conditioning operant conditioning modeling discriminative stimulus stimulus-control intervention self-reinforcement contingency contracting covert self-control cognitive restructuring self-talk behavioral assignment social skills (or assertiveness) training relaxation training abstinence violation effect relapse prevention lifestyle rebalancing Lesson I-9: Models and Venues for Health-Behavior Change Objectives: a) Discuss the five stages in the trans-theoretical model of behavior change. b) Give examples of how social engineering has been used for behavior change. c) Explain why health practitioners consider family, school, and work to be desirable venues for behavior change. d) Discuss the effectiveness of work-site interventions. 4 e) Give examples of community-based interventions. Key terms: trans-theoretical model of behavior change social engineering Lesson I-10: Exercise Objectives: a) Identify the health benefits of aerobic exercise. b) Discuss the prevalence of physical inactivity among Americans. c) Explain why exercise has positive effects on mood. d) List the characteristics of the individual, of the setting, and of the exercise program that predict participation. Key terms: aerobic exercise Lesson I-11: Accident Prevention, Cancer-Related Health Behaviors, and Maintaining a Healthy Diet Objectives: a) Identify the conditions under which parents are most likely to undertake injury prevention activities to protect their children. b) Explain why the rate of accidents in the home and workplace has declined. c) Describe the safety measures that have reduced the number of severe injuries and fatalities related to motorcycle and automobile accidents. d) List the factors that affect the regular practice of BSE. e) Explain why the use of mammography declines with age. f) Identify the factors that influence effective sunscreen use. g) Discuss the relationship between dietary habits and health. h) Explain why people have a hard time modifying their diet. i) Cite the dangers associated with a low-cholesterol diet. j) Summarize the findings on community interventions designed to modify diet. Key terms: breast self-examination (BSE) Lesson I-12: Weight Control (Part 1) Objectives: a) Explain how leptin and insulin control eating behavior. b) Describe the role of ghrelin in weight gain. c) Indicate the effects that ventromedial hypothalamus damage produces in rats. d) Identify the health risks associated with obesity. e) Explain why the prevalence of childhood obesity is increasing. f) Compare “apples” and “pears.” g) Discuss the effects of genetics, family history, SES and culture on obesity. h) Describe the effects of stress on eating behavior. Key terms: obesity yo-yo dieting 5 set point theory of weight PRACTICE TEST I-B Lesson I-13: Weight Control (Part 2) Objectives: a) List the three factors that are reliably related to staying slim. b) Describe the negative effects of dieting on psychological functioning. c) Identify the populations for whom gastric surgeries are recommended. d) Discuss the elements of a multimodal approach to modifying eating behavior. e) Identify the work-site intervention that is most effective. f) Describe the social engineering strategies recommended by the World Health Organization. Lesson I-14: Eating Disorders and Sleep Objectives: a) Identify possible factors in the development of anorexia nervosa and bulimia. b) Discuss the course of treatment for anorexia nervosa and bulimia. c) Briefly describe the stages of sleep. d) List the effects of sleep deprivation on health. e) Describe the symptoms of sleep apnea. Key terms: anorexia nervosa bulimia Lesson I-15: Health-Compromising Behavior: Alcoholism and Problem Drinking (Part 1) Objectives: a) List the characteristics shared by most health-compromising behaviors. b) Name some common disorders linked to alcohol consumption. c) Distinguish between alcoholism and alcohol abuse. d) Identify the factors that may contribute to alcoholism. Key terms: physical dependence tolerance craving addiction withdrawal alcoholism problem drinking Lesson I-16: Health-Compromising Behavior: Alcoholism and Problem Drinking (Part 2) Objectives: a) Identify the types of alcoholics who are most likely to do well in treatment. b) Describe the goals of treatment programs such as AA. c) Name the types of behavior modification techniques used in alcohol treatment. d) List the factors that determine the effectiveness of alcohol treatment programs. 6 e) Give examples of how social engineering can be used to deal with alcoholism. f) Identify two advantages of promoting moderate drinking versus abstinence. g) Discuss the political impact of Mothers Against Drunk Driving (MADD). h) List the beneficial effects of moderate drinking. Key terms: detoxification Lesson I-17: Smoking (Part 1) Objectives: a) List the health risks associated with smoking. b) Identify the synergistic effects of smoking. c) Cite evidence that smoking has a genetic component. d) Name the environmental factors and personality traits that are most conducive to adolescent smoking behavior. e) Explain how nicotine interacts with neurotransmitters to enhance memory, mood, and, and the performance of basic tasks. f) Cite evidence that nicotine addiction alone is not enough to account for smoking behavior. Lesson I-18: Smoking (Part 2) Objectives: a) Identify the main advantages of nicotine patches over nicotine gum. b) Describe the focus of relapse prevention programs. c) Compare the factors that predict short-term and long-term maintenance. d) List the characteristics of smokers who are most likely to relapse. e) Name the conditions that reduce the likelihood of relapse. f) Explain why it is so hard for smokers to modify their behavior. g) Identify the traits of smokers who quit on their own. h) List the three components of a social influence intervention program. i) Describe the characteristics of effective anti-smoking materials. j) Discuss the effectiveness of social influence programs. k) Describe the life-skills-training approach to smoking prevention. l) Identify four social engineering techniques that can be used to modify smoking behavior. Key terms: self-help aids social influence intervention behavioral inoculation PRACTICE TEST I-C Unit II: Stress, Coping and Treatment Lesson II-1: Theoretical Contributions to the Study of Stress Objectives: a) Summarize the theories of Walter Cannon and Han Selye. 7 b) List three criticisms of the general adaptation syndrome. c) Describe Taylor’s tend-and-befriend theory. d) Distinguish among harm, threat and challenge. e) Summarize the findings of Speisman et al (1964). f) Discuss the role of the SAM system and the HPA axis in stress response. g) Describe the long-term effects of stress on the body. h) Indicate how cardiovascular reactivity is related to stress. i) Identify the indicators used to assess allostatic load. Key terms: stress stressor fight-or-flight response general adaptation syndrome primary appraisal secondary appraisal reactivity allostatic load Lesson II-2: What Makes Events Stressful? Objectives: a) Describe the methods that are commonly used as indicators of stress. b) List the methodological problems associated with stress indicators. c) Identify the population for which positive life events are more stressful than negative ones. d) Name five characteristics of events that are likely to be appraised as stressful. Key terms: chronic strain post-traumatic stress disorder Lesson II-3: How Stress Has Been Studied Objectives: a) Identify three discoveries about stress reactions that have come out of the acute stress paradigm. b) Summarize the findings of studies that induce disease. c) Describe the relationship between SLE scores and illness. d) Name five problems associated with the use of SLE scales e) Discuss the findings of research using the “hassle scale.” Key terms: acute stress paradigm stressful life events (SLE) daily hassles Lesson II-4: Sources of Chronic Stress Objectives: a) Summarize the findings on the effects of early stressful life experiences. b) Discuss the relationship between work overload and stress. 8 c) Explain why air traffic controllers have higher rates of illness than second-class airmen. d) Describe the demand-control-support model. e) Summarize the findings on the health effects of unemployment. f) List seven ways to reduce occupational stress. g) Discuss the positive and negative effects of multiple roles. Key terms: role conflict Lesson II-5: Stress and Illness Objectives: a) Describe the effects of stress on health behaviors. b) Discuss the effects of negative affectivity on stress and illness. c) List the three elements of a pessimistic explanatory style. d) Compare the effects of optimism and pessimism on health. Key terms: stress moderator coping negative affectivity pessimistic explanatory style Lesson II-6: Coping with Stress Objectives: a) Describe the relationship between perceived control and health. b) Compare the following coping styles: avoidant vs. confrontative, problem-solving vs. emotion-focused. c) Discuss the effects of disclosure on stress and illness. Key terms: coping style avoidant coping style confrontative coping style PRACTICE TEST II-A Lesson II-7: Coping, External Resources and Social Support Objectives: a) Discuss the effects of external resources on health. b) Name two characteristics of psychological resilience. c) Describe three forms of social support. d) Identify two potential costs of social support. e) Summarize the beneficial effects of social support on stress and health. f) Distinguish between the direct effects hypothesis and the buffering hypothesis. g) Identify the kinds of support that are most and least effective. h) Compare the health benefits of marriage for men and for women. i) Discuss the relationship between marital conflict and health. j) Describe the health effects associated with giving social support to others. 9 Key terms: social support direct effects hypothesis buffering hypothesis matching hypothesis Lesson II-8: Coping Outcomes and the Management of Stress Objectives: a) List three criteria of successful coping. b) Identify the illnesses that stress management programs have been effective in treating. c) Describe three phases of a stress management program. d) Identify the common forms and the health benefits of relaxation training. Key terms: coping outcome stress management stress inoculation time management stress carrier Lesson II-9: Recognizing Symptoms and Using Health Services Objectives: a) Indicate who is most likely to recognize and report physical symptoms of stress. b) Describe the effect of prior experience, expectations, and seriousness on the interpretation of symptoms. c) List the kinds of information included in an illness schema. d) Distinguish among three models of illness based on duration. e) Name some of the more commonly used “unconventional” therapies. f) Discuss age, gender and social class on the use of health services. g) Explain why women use medical services more than men. h) Describe the effectiveness of the health belief model in predicting the use of health services. Key terms: illness representation (or schema) lay referral network Lesson II-10: Misusing Health Services Objectives: a) Identify five reasons why people use health services for emotional disturbances. b) Distinguish among the four types of delays in the use of health services. c) Indicate who is most likely to delay seeking treatment. d) Describe the kinds of symptoms that lead to delay behavior. Key terms: worried well somaticizer secondary gain 10 delay behavior Lesson II-11: The Patient in the Hospital Setting Objectives: a) Compare the treatment goals of physicians and nurses. b) Discuss the risk of nosocomial infection among hospitalized patients. c) Identify two cost-containment strategies that affect hospital care. d) Describe the role of psychologists in hospital care. Key terms: nosocomial infection diagnostic-related group (DRG) preferred provider organization (PPO) Lesson II-12: The Hospitalized Child Objectives: a) Summarize the findings of Janis (1958) and of Egbert et al (1964). b) Compare the anxiety response of children in different age ranges. c) Describe the preparation interventions that are most effective for children. Key terms: control-enhancing intervention psychological control PRACTICE TEST II-B Lesson II-13: Patient-Provider Communication Objectives: a) Distinguish among four types of advanced-practice nurses. b) Name the criteria by which patients judge the quality of the care they receive. c) Identify at least three sources of patient dissatisfaction with HMOs. d) List three components of holistic health care. e) Discuss the findings of Beckman & Frankel (1984). f) Offer three possible reasons why health care providers may use jargon. g) Describe four types of negative stereotypes that providers may have of patients, including the effects of each stereotype on the quality of treatment. h) Identify three ways that patients may contribute to faulty communication with providers. Key terms: nurse-practitioner physicians’ assistant health maintenance organization (HMO) managed care holistic health Lesson II-14: Results of Poor Patient-Provider Communication Objectives: a) Discuss the prevalence of non-adherence among patients in different situations. 11 b) Name four ways to enhance adherence by promoting good learning. c) Identify the types of treatment regimens that are most likely to produce adherence. d) List three impediments to adherence cited by non-adherent patients. e) Name three things that patients seek when a medical mistake occurs. Key terms: adherence non-adherence creative non-adherence Lesson II-15: Improving Communication and Using Placebos Objectives: a) Identify the one reliable predictor of physician sensitivity. b) Describe the characteristics and benefits of “patient-centered communication.” c) Discuss the qualities that a good communication course should have. d) Name two institutional interventions that can foster adherence. e) Identify ways of presenting the treatment regimen that improve adherence. f) Give an example of the role of placebo effects in active treatment. g) Describe the qualities of the provider, the patient and the setting that are most conducive to placebo effects. h) Discuss the prevalence of medication use among hospitalized and nonhospitalized patients. Key terms: placebo placebo effect double-blind experiment Lesson II-16: The Significance and Elusive Nature of Pain Objectives: a) Compare the patient’s and provider’s view of pain. b) Discuss the prevalence of chronic pain in the U.S. c) Identify factors that influence the experience of pain. d) Name two dimensions of pain that are measured by pain questionnaires. e) Distinguish among the three kinds of pain perception. f) Describe the pathway followed by nociceptors. g) Distinguish among the two major never fibers involved in nociception. h) Identify the two neurotransmitters that are implicated in pain transmission. i) List the three families of endogenous opioid peptides. j) Cite evidence that endogenous opioid peptides are involved in stress-induced analgesia (SIA). Key terms: pain behavior nociception endogenous opioid peptide 12 Lesson II-17: Clinical Issues in Pain Management Objectives: a) Distinguish among three types of chronic pain. b) List three ways that acute and chronic pain differ. c) Describe the impact of chronic pain on the sufferer’s life. d) Discuss the relationship between chronic pain and MMPI scores. Key terms: acute pain chronic pain pain-prone personality Lesson II-18: Pain Control Techniques and the Management of Chronic Pain Objectives: a) Cite evidence that the risk of addiction to painkillers is not particularly great. b) Explain why surgical control of pain is not a practical form of treatment. c) Describe the process of biofeedback training. d) Discuss the effectiveness of biofeedback and relaxation in controlling pain. e) Identify the kinds of pain that hypnosis has been effective in controlling. f) Cite evidence that distraction works as a method for controlling pain. g) Describe two very different types of imagery used to control pain. h) Identify the kinds of cognitive-behavioral techniques that are especially successful in controlling pain. i) Name the components of chronic pain management programs. Key terms: pain control counterirritation biofeedback hypnosis acupuncture guided imagery pain management PRACTICE TEST II-C Unit III: Management of Chronic and Terminal Illness Lesson III-1: Quality of Life and Personal Issues in Chronic Illness Objectives: a) List the components of quality of life for individuals with chronic illness. b) Indicate how and when denial can be an adaptive response to chronic illness. c) Identify the conditions that are most conducive to anxiety in the chronically ill. d) Describe the problems associated with anxiety and depression in the chronically ill. e) Explain why it is hard to assess depression in the chronically ill. f) Compare the coping strategies used by the chronically ill and by individuals encountering other kinds of stressful events. 13 g) Discuss the advantages and disadvantages of self-blame. Key terms: denial depression self-concept self-esteem body image Lesson III-2: Rehabilitation and Chronic Illness (Part 1) Objectives: a) List the goals of physical rehabilitation for the chronically ill. b) Describe the unpleasant side effects of chemotherapy and radiation therapy. Key terms: physical rehabilitation Lesson III-3: Rehabilitation and Chronic Illness (Part 2) Objectives: a) Cite evidence that the chronically ill face job discrimination. b) Describe the financial impact of chronic illness. c) Identify the characteristics of a typical caregiver. d) Distinguish between two categories of caregiving. e) Discuss the risks associated with caregiving. f) Compare the impact of chronic illness on men and on women. g) Describe the positive outcomes of chronic illness. h) Identify the specific challenges associated with chronic illness in children. i) List the factors that can improve a chronically ill child’s ability to cope. Lesson III-4: Psychological Interventions and Chronic Illness Objectives: a) Name four ways that medical patients differ from patients with psychological complaints in terms of the kind of psychotherapy they receive. b) Identify the benefits of using relaxation training with the chronically ill. c) Describe what happens in a support group. d) Give three reasons why support groups may encourage adherence. Key terms: patient education mindfulness-based stress reduction (MBSR) support group Lesson III-5: Death Across the Lifespan Objectives: a) Find the average life expectancy of people in the United States. b) Explain why the infant mortality rate in the U.S. is relatively high. c) Name the main causes of death in infancy and childhood. d) Identify the conditions under which SIDS is most likely to occur. e) Describe three developmental stages in children’s understanding of death. 14 f) Name the main causes of death among the elderly. g) List two psychosocial factors that predict health among the elderly. Key terms: infant mortality rate sudden infant death syndrome (SIDS) premature death Lesson III-6: Psychological Issues in Advancing Illness Objectives: a) Explain why patients with end-stage renal disease decide to discontinue kidney dialysis. b) Discuss the significance of the 1990 U.S. Patient Self-determination Act and the 1997 Oregon Death with Dignity Act. c) Explain why a breakdown in communication may occur between terminally ill patients and their families. Key terms: euthanasia living will PRACTICE TEST III-A Lesson III-7: Stages in Adjustment to Dying Objectives: a) Describe each of Kubler-Ross’ five stages of dying. b) Identify the strengths and weaknesses of Kubler-Ross’ theory. c) Discuss the specific psychotherapeutic needs of dying patients. Key terms: terminal care palliative care curative care clinical thanatology Lesson III-8: Hospice Care and Grieving Objectives: a) Describe the main characteristics of hospice care. b) Identify the psychological advantages of home care. c) Discuss the challenges facing adult survivors. d) Identify the types of grief responses that are most and least adaptive. e) Indicate when it is best to begin helping a child cope with the death of a parent or sibling. Key terms: hospice grief 15 Lesson III-9: Coronary Heart Disease (Part 1) Objectives: a) Indicate how inflammatory processes are related to cardiovascular disease. b) Identify common risk factors for CHD. c) Explain how metabolic syndrome is diagnosed. d) Describe the relationship between cardiovascular reactivity and CHD. e) List the job factors that are related to an increased risk for CHD. f) Cite evidence that social instability is tied to higher rates of CHD. g) Explain why women are protected at young ages from CHD, relative to men. h) Discuss the effectiveness of estrogen replacement therapy following menopause in reducing the risk of CHD in women. i) Compare the medical care received by men and women with CHD. j) Name three components of the Type A behavior pattern. k) Describe the relationship between the Type A behavior pattern and CHD. l) Discuss the relationship between hostility and CHD. m) Identify the child-rearing practices that seem to foster hostility. n) Compare the effects of expressing vs. harboring hostility. o) Describe the role of catecholamines in CHD. Key terms: coronary heart disease (CHD) Type A behavior pattern Lesson III-10: Coronary Heart Disease (Part 2) Objectives: a) Explain how depression predicts heart disease. b) Cite experimental evidence that exercise can reduce the risk of CHD. c) Describe the effects of relaxation training on stress response. d) Identify the factors that predict a delayed response to a heart attack. e) List the goals of cardiac rehabilitation. f) Discuss the effects of psychological factors in recovery from MI. g) Describe the effects of beta-blockers, aspirin and statins. h) Name the populations most at risk for stress after a diagnosis of CHD. i) Identify the components of stress management. j) Cite evidence that stress management programs can help CHD patients. k) Describe the beneficial effects of cholesterol reduction on CHD. Key terms: vigilant coping vital exhaustion cardiac rehabilitation cardiac invalidism cardiopulmonary resuscitation (CPR) Lesson III-11: Hypertension Objectives: a) Identify two health risks associated with hypertension. 16 b) Distinguish between systolic and diastolic pressure. c) Indicate how hypertension is defined, in terms of systolic pressure. d) Name the common risk factors for hypertension. e) Identify common methods of treatment for hypertension. f) Discuss the effectiveness of cognitive-behavioral interventions. g) Describe two problems in the treatment of hypertension. Key terms: hypertension metabolic syndrome Johan Henryism Lesson III-12: Stroke Objectives: a) Identify the two causes of stroke. b) Explain how aspirin reduces the risk of stroke. c) List the risk factors for stroke. d) Discuss three common consequences of stroke. e) Name four types of interventions used with stroke patients. f) Explain how neurorehabilitation works. PRACTICE TEST III-B Lesson III-13: Diabetes Objectives: a) Describe the role of insulin in the body. b) Explain what happens when the body fails to produce enough insulin or develops a tolerance to it. c) Distinguish between the two types of diabetes. d) List the health problems associated with diabetes. e) Describe the effects of stress hormones on insulin. f) Identify the ways that Type I and Type II diabetes are managed. g) Explain why adherence to self-management programs is so low for Type I diabetics. h) Compare the treatment goals of parents and physicians of children with Type I diabetes. i) Cite evidence that lifestyle intervention programs can prevent diabetes. j) Identify cognitive-behavioral interventions used with diabetics. Key terms: diabetes Lesson III-14: Psychoneuroimmunology Objectives: a) Distinguish between natural and specific immunity. b) Identify three types of cells involved in natural immunity, including the function of each. c) Distinguish between the two types of specific immunity. 17 d) Describe the two general approaches to assessing immunocompetence. e) Compare the immune effects of short-term stressors, brief naturalistic stressors, and chronically stressful events. f) Explain how stress-related changes in the HPA axis affect immune response. g) Discuss the documented effects of space travel and Hurricane Andrew on immune response. h) Indicate what happens when healthy participants are asked to write about traumatic experiences in their lives. i) Summarize the findings of studies involving people living near Three Mile Island. j) Identify the health effects experienced by children and adults under stress. k) Describe the effects of depression on cellular immunity. l) Cite evidence that marital disruption, marital conflict, and caregiving have an adverse effect on immunity. m) List three ways that feelings of self-efficacy and control affect immunity. n) Discuss the effects of relaxation training on melanoma patients. Key terms: psychoneuroimmunology mmunocompetence immunocompromise Lesson III-15: AIDS (Part 1) Objectives: a) Discuss the prevalence of AIDS worldwide. b) Describe the effects of HIV on the immune system. c) Explain how HIV is transmitted. d) List the symptoms of AIDS. e) Discuss the effectiveness of HAAVT in the treatment of AIDS. f) Identify the populations most at risk for contracting AIDS. g) Describe the common responses to testing HIV+. h) Discuss the health consequences of disclosure. Key terms: acquired immune deficiency syndrome (AIDS) human immunodeficiency virus (HIV) Lesson III-16: AIDS (Part 2) Objectives: a) Discuss the effect of self-efficacy on risk-related behavior. b) Identify the kinds of interventions that are effective at reducing risk-related behavior. c) List three ways to reduce risky injection practices among IV drug users. d) Explain why peer-based interventions are not effective with adolescents. e) Identify the benefits of the Internet for individuals who are HIV+. f) Describe the psychosocial factors that influence the rate of immune decline from AIDS. 18 Lesson III-17: Cancer Objectives: a) Describe the cellular mechanism underlying cancer. b) Identify common risk factors for cancer. c) Discuss the link between stress and cancer. d) List the common side effects of chemotherapy. e) Describe the effects of social support on cancer patients. f) Explain how cancer can impair sexual relationships. g) List five patterns of coping with cancer and indicate their relative effectiveness. h) Identify a benefit of cancer reported by some patients. i) Name four issues addressed by pharmacological interventions. j) Indicate which drugs address each of these issues. k) List the benefits of mindfulness-based stress reduction interventions. l) Cite evidence that distraction can be successful in treating children undergoing chemotherapy. m) Identify the common issues arising in individual therapy and family therapy with cancer patients. n) Describe the type of cancer patient who is most likely to benefit from social support groups. o) Cite an unanticipated health benefit of support groups for cancer patients. Lesson III-18: Arthritis Objectives: a) Distinguish among the three major forms of arthritis b) Identify the common treatments for RA, osteoarthritis, and gout. Key terms: arthritis rheumatoid arthritis (RA) osteoarthritis gout PRACTICE TEST III-C 19 Practice Test I-A 1. A. B. C. D. Etiology refers to causes of illness. a special kind of disease state. healthy behavior. stress effects. 2. A. B. C. D. Random assignment is an important characteristic of experiments. correlational research. longitudinal research. all of the above. 3. A. B. C. D. Damage to the cerebellum is associated with impaired muscular coordination. respiration. speech. visual acuity. 4. _______________ is chest pain which occurs because the muscle tissue of the heart must continue its activity without a sufficient supply of oxygen or adequate removal of carbon dioxide and other waste products. A. Angina pectoris B. Myocardial infarction C. Phlebitis D. Arteriosclerosis 5. A. B. C. D. The female hormone, estrogen, is secreted by the anterior pituitary. is associated with lactation. is produced during the second half of the menstrual cycle. leads to the development of secondary sex characteristics in the female. 6. A. B. C. D. According to the text, changing health behaviors may be beneficial because it may reduce the number of deaths due to diseases related to lifestyle. may increase individual longevity and life expectancy. may delay the onset of chronic disease and enhance quality of life. all of the above. 20 Practice Test I-B 1. A. B. C. D. _______________ is the belief that one is able to control one’s practice of a particular behavior. Health locus-of-control Self-esteem Self-control Self-efficacy 2. A. B. C. D. The use of Antabuse in the treatment of alcoholism is an example of shaping. modeling. operant conditioning. classical conditioning. 3. _______________ involves modifying the environment to affect one’s ability to practice a particular behavior. A. Social engineering B. Reconstruction C. Adaptive environmental change D. Passive retraining 4. A. B. C. D. Which of the following people is LEAST likely to exercise regularly? Joe, a 10-year-old boy Jill, a 15-year-old girl Jack, a 35-year-old man Juana, a 45-year-old woman 5. A. B. C. D. Parents are most likely to undertake injury prevention activities if they believe that the recommended steps really will avoid injuries. if they feel knowledgeable and competent to teach safety skills to their children. if they have a realistic sense of how much time will actually be involved. all of the above. 6. A. B. C. D. A person with a BMI (body mass index) above _______________ is obese. 10 20 30 40 21 Practice Test I-C 1. Girls with bulimia differ from girls with anorexia in that A. by definition, girls with anorexia are underweight, whereas girls with bulimia are often of normal weight or overweight B. bulimia is more commonly observed between the ages of 30 to 45. C. anorexia is associated with diminished perceptions of control; bulimia is not. D. anorexia may be associated with certain physiological factors; bulimia is associated with certain psychological factors. 2. A. B. C. D. Sleep apnea is an air pipe blockage that disrupts sleep and can compromise health. causes some people to sleep very soundly. is easy to diagnose. has no effective treatment. 3. Since he stopped smoking last week, John complains about fighting the urge for a cigarette, especially when he is around other smokers. This is an example of A. addiction. B. tolerance. C. craving. D. withdrawal. 4. A. B. C. D. Alcoholics Anonymous is a broad-spectrum treatment program. is a self-help group. has demonstrated lower dropout and relapse rates than inpatient programs. all of the above. 5. A. B. C. D. The best predictor of long-term abstinence among smokers is social support. environmental support. self-efficacy. remaining vigilant about not smoking. 6. Those who quit smoking on their own A. appear to be more successful in maintaining abstinence than participants in smoking cessation programs. B. have high levels of self-control that is related to low relapse rates. C. are more likely to have a socially supportive network that smokes. D. have strong beliefs in the health benefits of stopping smoking. 22 Practice Test II-A 1. A. B. C. D. The correct sequence of phases of the general adaptation syndrome is alarm, resistance, exhaustion. exhaustion, resistance, alarm. resistance, alarm, exhaustion. resistance, exhaustion, alarm. 2. A. B. C. D. The process of secondary appraisal involves the evaluation of one’s current emotional state. perception of the event. coping ability and resources. all of the above. 3. A. B. C. D. The relationship between scores on the Schedule of Recent Life Events (SRE) and illness is negligible. modest. robust. unpredictable. 4. Workers who suffer from work overload _______________ compared with workers who do not experience overload. A. feel more stressed B. practice poorer health habits C. sustain more health risks D. all of the above 5. A. B. C. D. Individuals high in negative affectivity may be described as having a “disease-prone” personality. are more likely to seek out medical care for minor complaints. repress their stress-related symptoms but complain more about their general health. are characterized as being depressed, anxious, and psychotic. 6. The belief that one can determine one’s own internal states and behavior, influence one’s environment, and/or bring about desired outcomes is A. optimism. B. perceived control. C. self-efficacy. D. hardiness. 23 Practice Test II-B 1. Information from others that one is loved and cared for, esteemed and valued, and part of a network of communication and mutual obligation is called A. coping. B. internal resources. C. social support. D. external resources. 2. A. B. C. D. Individuals that cause you special stress are stress carriers. not important to you. easily ignored. none of the above. 3. The _______________ model of illness is represented by alternating periods of either no or many symptoms. A. acute B. chronic C. cyclic D. terminal 4. A. B. C. D. Somaticizers exhibit strong beliefs in self-care. tend to express distress and conflict through physical symptoms. repress their symptoms during times of stress. all of the above. 5. A. B. C. D. The hospital nursing staff has as its primary orientation the goal of cure. care. core. all of the above. 6. A. B. C. D. The most common adverse response by children to hospitalization is anxiety. lack of information about medical procedures. high levels of personal control. all of the above. 24 Practice Test II-C 1. A. B. C. Most patients are good judges of the technical quality of the medical care they receive. consider medical treatment to be of high technical quality if the provider is nice. feel that the technical quality of medical care is somewhat more important than the manner in which it is provided. D. all of the above. 2. You are a consultant who has been hired by an HMO to try to improve patient satisfaction and retention. Based on the research discussed in the text, your most effective recommendation would be to A. increase the number of specialists. B. allow patients more personal choice in their primary provider. C. decrease the annual premium paid. D. ensure that a patient sees a different doctor during each visit. 3. A. B. C. D. When patients do not adopt the recommended medical treatment, the result is malingering. reactance. doctor shopping. nonadherence. 4. Pain has important medical consequences because A. patients’ delay behavior is related to the experience of debilitating pain. B. practitioners are trained to devote a significant amount of time to diagnosing the source of pain, which often impairs the quality of medical interactions. C. it is the symptom most likely to lead an individual to seek treatment. D. after death, pain is the most feared aspect of illness or medical treatment. 5. A. B. C. D. Acute pain is not associated with anxiety and depression. may precede the development of a chronic pain syndrome. seldom responds to the administration of painkillers or other medication. increases with the passage of time. 6. A. B. C. D. Pharmacological control of pain is dangerous in that it usually leads to addiction to prescription drugs. is of no concern to researchers and practitioners. has a low probability of leading to addiction to prescription drugs. is the treatment of last resort. 25 Practice Test III-A 1. A. B. C. D. Denial is useful in helping patients control their emotional reaction to illness. monitor their physical condition. seek treatment. become active in their treatment regimen. 2. A. B. C. D. Chemotherapy may be accompanied by changes in taste and the development of taste aversions. burning of the skin. dietary restrictions. weight gain. 3. More than _______________ of cancer patients report at least some beneficial changes in their life as a result of the cancer. A. 20% B. 45% C. 75% D. 90% 4. Compared to therapy with other clients, psychotherapy provided to medical patients is more likely to A. be continuous and long term in nature. B. involve collaboration with the patient’s family and physician. C. be expensive and time consuming. D. challenge the client’s defenses and promote a realistic assessment of his or her situation. 5. A. B. C. D. The infant mortality rate in the United States is higher than that in most Western European countries. is twice as high for black infants as for white infants. may be associated with inequities in access to health care. all of the above. 6. A. B. C. D. A living will outlines a patient’s wishes to undergo euthanasia. a patient’s request that extraordinary life-sustaining procedures not be used. the conditions under which a patient requests to remain alive. the disposition of one’s belongings after death. 26 Practice Test III-B 1. A. B. C. D. The correct order of Kübler-Ross’s stages of adjustment to dying is depression, anger, bargaining, denial, acceptance. denial, anger, bargaining, acceptance, depression. denial, bargaining, anger, depression, acceptance. denial, anger, bargaining, depression, acceptance. 2. A. B. C. D. The goals of hospice care include palliative care. psychological comfort. improved social support. all of the above. 3. The combination of obesity centered around the waist, high levels of triglycerides, low levels of HDL cholesterol, and difficulty metabolizing blood sugar are symptomatic of A. inflammation due to c reactive protein. B. metabolic syndrome. C. angina pectoris. D. cardiac arrest. 4. A. B. C. D. Cardiac rehabilitation programs involve aerobic exercise. smoking cessation. reduced alcohol consumption. all of the above. 5. A. B. C. D. Diastolic pressure is related to resistance of the blood vessels to blood flow. the amount of force developed during contraction of the heart. the volume of blood leaving the heart. the arteries’ elasticity. 6. A. B. C. D. The risk factors for stroke are independent of those for heart disease. decrease with age. are not subject to modification by lifestyle changes. include cigarette smoking. 27 Practice Test III-C 1. Type II (noninsulin-dependent) diabetes A. develops relatively late in life (after age 40), but is becoming more common in children and adolescents. B. accounts for 90% of all diabetics. C. occurs when insulin is disregulated. D. all of the above. 2. A. B. C. D. Helper T (TH) cells respond to specific antigens. enhance the function of TC cells, B cells, and macrophages by producing lymphokines. produce lymphokines that suppress immune activity. produce immunoglobulins, which are the basis of antigen-specific reactions. 3. A. B. C. D. The most common mode of transmission of AIDS worldwide is via heterosexual sexual activity. homosexual sexual activity. blood transfusions. intravenous drug use. 4. Studies have found that _______________ beliefs about the self and the future are associated with the onset of AIDS in individuals with HIV. A. positive B. negative C. neutral D. none of the above 5. A. B. C. D. For cancer patients, social support improves immunologic responses. improves psychological adjustment can be problematic. all of the above. 6. A. B. C. D. Gout is more prevalent in females than in males. results from the buildup of uric acid in the body. can be managed by maintaining proper weight and taking aspirin. none of the above. 28 Answer Key Practice Test I-A 1. a 2. a 3. a 4. a 5. d 6. d 3. 4. 5. 6. d c b c Practice Test III-A 1. a 2. a 3. d 4. b 5. d 6. b Practice Test I-B 1. d 2. d 3. a 4. d 5. d 6. c Practice Test III-B 1. d 2. d 3. b 4. d 5. a 6. d Practice Test I-C 1. a 2. a 3. c 4. b 5. d 6. d Practice Test III-C 1. d 2. b 3. a 4. a 5. d 6. b Practice Test II-A 1. a 2. c 3. b 4. d 5. a 6. b Practice Test II-B 1. c 2. a 3. c 4. b 5. b 6. a Practice Test II-C 1. b 2. b 29 30