best practice statement - The Scottish Renal Registry
advertisement

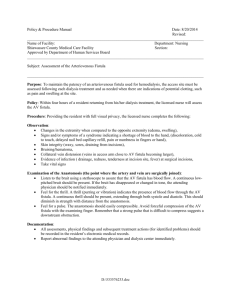
SCOTTISH RENAL NURSING STRATEGY GROUP BEST PRACTICE STATEMENT FOR THE FORMATION AND CARE OF AV FISTULA AND GRAFT DRAFT Table of Contents Introduction 3 KEY PRINCIPLES OF BEST PRACTICE STATEMENTS 4 KEY STAGES IN THE DEVELOPMENT OF THE STATEMENT 5 HOW CAN THE STATEMENT BE USED? WHO WAS INVOLVED IN DEVELOPING THE STATEMENT? 6 GLOSSARY OF TERMS 7 INTRODUCTION TO STATEMENT 8 BEST PRACTICE STATEMENT: THE FORMATION AND CARE OF 12 AV FISTULA AND GRAFT Section 1: PRE DIALYSIS PREPARATION & CARE Section 2: PRE OPERATIVE PREPARATION & CARE Section 3: INTRAOPERATIVE STAGE Section 4: POST OPERATIVE CARE Section 5 ACCESS SURVEILLANCE Appendix 1: TOURNIQUET INFORMATION 32 Appendix 2: RECOMMENDED NEEDLE SIZES 33 Appendix 3: EMERGENCY PROCEDURES 34 Appendix 4: PRE- OP CARE GOOD PRACTICE EXAMPLE 35 Appendix 5: POST OP CARE GOOD PRACTICE EXAMPLE 36 Appendix 6: SOURCES OF EVIDENCE 37 Scotiish renal nursing strategy group 2004-12-15 2 DRAFT Introduction NHS Quality Improvement Scotland (NHS QIS) was established in 2003 by the Scottish Parliament and was an amalgamation of various organisations to take the lead in improving the quality of care and treatment delivered by NHS Scotland. NHS QIS does this by setting standards and monitoring performance, and by providing NHS Scotland with advice, guidance and support on effective clinical practice and service improvements. Background to Best Practice Statements While many examples of clinical guidelines exist, there is a lack of reliable statements focusing specifically on nursing and midwifery practice. The development of best practice statements reflects the current emphasis on delivering care that is patient-centred, cost-effective and fair, and will attempt to reduce existing variations in practice. The common practice that should follow their implementation will allow comparable standards of care for patients wherever they access services. Scotiish renal nursing strategy group 2004-12-15 3 DRAFT Key Principles of Best Practice Statements A best practice statement describes best and achievable practice in a specific area of care. The term ‘best practice’ reflects the commitment of NHS QIS to sharing local excellence on a national level. Best practice statements are underpinned by a number of shared principles below: Best practice statements are intended to guide practice and promote a consistent and cohesive approach to care. Best practice statements are primarily intended for use by registered nurses, midwives and the staff who support them, but they may also contribute to multidisciplinary working and be of guidance to other members of the healthcare team. Statements are derived from the best available evidence at the time they are produced, recognising that levels and types of evidence vary. Information is gathered from a broad range of sources in order to identify existing or previous initiatives at local and national level, incorporate work of a qualitative and quantitative nature and establish consensus. Statements are targeted at practitioners, using language that is accessible and meaningful. Consultation with relevant organisations and individuals is undertaken. Statements will be nationally reviewed and updated every 3 years. Responsibility for implementation of statements will rest at local level. Key sources of evidence and available resources are provided. Use of Evidence in Best Practice Statements The need to embrace evidence in its broadest sense has been acknowledged by NHS QIS in the development of best practice statements. Best practice statements represent a unique synthesis of research evidence, evidence complemented by audit, patient surveys and evidence derived from expert opinion, professional consensus and patient/public experience. The process for developing these statements adopts a rigorous, transparent and consistent ‘bottom-up’ approach to articulating best practice that involves professionals and patients, and is based on all types of available evidence. The following stages describe the process of identifying and reviewing evidence for inclusion in statements: 1 Define question 2 Review evidence from a range of sources including published literature, grey literature and other relevant sources, eg patient groups, manufacturers, professional groups 3 Evaluate evidence using recognized methods of evidence appraisal 4 Integrate evidence with patient-related factors, eg issues of access, equity and ethics 5 Develop recommendations 6 Evaluate process and impact of recommendations. Scotiish renal nursing strategy group 2004-12-15 4 DRAFT KEY STAGES IN THE DEVELOPMENT OF THE STATEMENT The development of this best practice statement has been based on current research to enhance practice. Review Evidence Research major reports, national, local guidelines and standards, existing care guidance, expert nursing opinion and evidence from patients. Draft Best Practice Statement Identify nursing contribution, apply renal nursing values, and identify level and type of evidence. Circulate for consultation Involve al l users, include practice development forums, pool expertise from the renal community, and refine statement. External consultation on the revised draft after evaluation Disseminate and Update 3-yearly Paper copies, on-line in PDF format, face-to-face seminars, training for all staff. Pilot audit at 6 months, audit at 1 year Review available evidence in 3 years time Scotiish renal nursing strategy group 2004-12-15 5 DRAFT Who was involved in developing the statement? Working Group members Anne Allan Clinical Ward Manager, Renal Unit Raigmore Hospital, Inverness Anne Petherick Education Coordinator, Renal Unit, Edinburgh Royal Infirmary Barbara Killoran Education Facilitator, Renal Unit, NHS Greater Glasgow Carol Latta Ward Manager , RDU Gartnavel General Hospital, NHS Greater Glasgow Glasgow Caroline Arnott Ward Manager, Renal Unit, Queen Margaret Hospital, Dunfermline Geraldine Ovens Renal Education Facilitator, Renal Unit, NHS Ayrshire & Arran Ippy Brown Clinical Nurse Manager, Renal Unit, NHS Greater Glasgow Julie English Clinical Educator, Renal Unit, Raigmore Hospital, Inverness Laurie Kirkland Pre-dialysis Nurse, NHS Ayrshire & Arran Margaret Boyd Clinical Facilitator, Renal Unit, Monklands General Hospital Morag McGhee Clinical Nurse Manager, Renal Unit, Monklands General Hospital Noreen McMahon Ward Manager, Crosshouse Hospital, Kilmarnock Rhona Lochiel Vascular Access Nurse, Edinburgh Royal Infirmary Temby Chigaru Clinical Educator, Queen Margaret Hospital, Dunfermline Scotiish renal nursing strategy group 2004-12-15 6 DRAFT Wider reference group Sister Aileen Heminglsey Dr W Smith, Dr M Hand, Dr I Shilliday Dr H Oun, Scotiish renal nursing strategy group 2004-12-15 HD sister Consultant Consultant Consultant Associate specialist 7 DRAFT Glossary of terms TERM DEFINITION Adequacy refers to how well dialysis replaces the function of the kidneys Anastomosis an artificial connection between two tubular organs eg two blood vessels Arterio-venous fistula a surgical connection between an artery and a vein, usually in a limb, to create arterial and venous access for haemodialysis. It can be a direct anastomosis between the artery and vein Asepsis the complete absence of bacteria, fungi, viruses or other microorganisms that could cause disease Autogenous originating in the body of the patient Bruit a sharp or harsh systolic sound heard on auscilation that is due to turbulent blood flow in a peripheral artery. Bruits can be heard over arteriovenous fistulae Cannula a hollow tube designed for insertion into a body cavity or blood vessel Cannulation insertion of a cannula Co morbidity the presence of one or more disorder or disease in addition to the primary disease Scotiish renal nursing strategy group 2004-12-15 8 DRAFT DOQI Dialysis the national kidney foundation Outcomes Quality Initiative. established in 1995 in the USA Duplex imaging a diagnostic technique used to study the flow in blood vessels. End stage renal failure (ESRF) the most advanced stage of kidney failure, which is reached when the glomerular filtrate rate falls to5mls/min (Normal GFR =120ml/min) Extravasation the leakage and spread of blood or fluid from vessels into the surrounding tissues e.g. following injury Glomerular Filtration Rate (GFR) the rate at which substances are filtered from the blood of the glomerulus into the bowman’s capsule of the nephron. It is calculated by measuring the clearance of specific substances and is an index of renal function. Haematoma an accumulation of blood within the tissues that clots to form a solid swelling. Haemodialysis a technique of removing waste materials or poisons from the blood using the principle of dialysis. Haemodialysis is performed on patients whose kidneys have ceased to function. Heparin an anticoagulant, which acts by inhibiting the action of the enzyme thrombin in the final stage of blood coagulation Scotiish renal nursing strategy group 2004-12-15 9 DRAFT Infiltration the abnormal entry of a substance into tissue. e.g. blood Intima the inner layer of a wall of an artery or vein. NHS Quality Improvement Scotland (NHS QIS) a statutory body established as a special health board in January 2003. Its role is to focus on improving the quality of patient care and the health of patients. Now incorporates Clinical Standards Board for Scotland which a statutory body, established as a special health board in April 1999.Its role, in line with the Scottish executive’s commitment to quality, openness and public accountability, is to promote public confidence that the services provided by the NHS are safe and that they meet nationally agreed standards , and to demonstrate that , within the resources available , the NHS is delivering the highest possible standards of care Patency the condition of being open e.g. blood flow present Protocol correct procedure (should be evidence based) Thrombosed affected by thrombosis Thrombosis a condition in which the blood changes from a liquid to a solid state and produces a blood clot Scotiish renal nursing strategy group 2004-12-15 10 DRAFT Tourniquet an instrument for the compression of a blood vessel by application around an extremity to control the circulation and prevent the flow of blood to or from the area Venepuncture the puncture of a vein for any therapeutic purpose. Scotiish renal nursing strategy group 2004-12-15 11 DRAFT INTRODUCTION TO THE STATEMENT Over the last few years, there has been an increase in the prevalence of renal replacement therapy for patients who reach end stage renal failure. The Scottish Renal Registry report of 2000 – 2001 indicates that the incidence of new patients starting renal replacement therapy has increased from 1479 (1991) to 2673(2001) with projections of an increase in this number by 2005. The annual take in rate is currently 600 per year. The median age range for patients commencing RRT has gone from 58.2years 1992 to 66.4 years 2001 (source SRR 2003 report) Co-morbidity has risen considerably requiring increased nursing intervention. There are ten adult renal units in Scotland with nine satellite or annexe units. In addition there is one paediatric renal unit. The Scottish Renal Nursing Strategy Group have committed to looking at ways in which the services can be developed. The largest growth area is in Haemodialysis The philosophy of this group is to identify nursing priorities for renal services within Scotland to provide clear direction for nurses working within the specialty. The strategy will be developed in collaboration with representatives from all Scottish Renal units' and in consultation with relevant national groups. The purpose of this Best Practice Statement is to guide all haemodialysis nursing and technical staff in the best way to manage and preserve vascular access. Poor vascular access for haemodialysis may contribute to increased risk of infection, unnecessary repeated admissions to hospital and potentially increased mortality. The National Service Framework for Renal Services suggests that: STANDARD TWO All children, young people and adults approaching established renal failure are to receive timely preparation for renal replacement therapy, so the complications and progression of their disease are minimised, and their choice of clinically appropriate treatment options maximised. STANDARD THREE All children, young people and adults with established renal failure are to have timely and appropriate surgery for vascular or peritoneal access, which is monitored and maintained to achieve maximum longevity. Scottish Renal Association and QIS Standards require that: 70% of established patients should have functioning AVF or Graft 60% of new starts should have functioning AVF If known to renal service for more than 3 months. An AV fistula/ graft is a prerequisite for carrying out haemodialysis. The ideal blood vessel should: o Be easily accessible for cannulation by patient and staff o Be suitable for cannulation 1month-4 months after creation (DOQI guideline 9, 2000) (for PTFE graft 3- 6weeks after placement, DOQI guideline 9, 2000). o Have adequate barrier to infection to maintain skin integrity Scotiish renal nursing strategy group 2004-12-15 12 DRAFT Premature cannulation of a fistula may result in a higher incidence of infiltration with associated compression of the vessel by haematoma and permanent loss of the fistula (DOQI guideline 9,2000) The AV fistula/ graft should be: o Patent o Palpable with bruit present o Clean and free from signs of infection The success of vessel access is best assessed by it’s capability to supply and return blood to the general circulation at acceptable flow rates, its duration of effective function, the degree of patient discomfort and limitation and the rate and severity of complications. Why create a fistula first The arterio-venous fistula remains the gold standard access to haemodialysis, showing better survival and lower complication rates than grafts and catheters (Brunori et al 2005). The presence of a catheter and/or its complications may affect the longevity of a native fistula through its earlier utilisation or less favourable maturation. (Rayern et al 2003). DOQI guideline 3 states that in order to determine which type of access is most suitable to the individual patient, an evaluation of the patients venous, arterial and cardiopulmonary systems must be performed. Previous placement of central venous catheter is associated with central venous stenosis. Central venous catheters should be discouraged as permanent vascular access. In the absence of factors associated with contraindications for the formation of A-V fistula, this would be the first preference for vascular access. (DOQI 2000) Scotiish renal nursing strategy group 2004-12-15 13 DRAFT Scotiish renal nursing strategy group 2004-12-15 14 Section One: Pre- Dialysis Stage Key point: Frequent monitoring of fistula parameters is required STATEMENT REASON FOR STATEMENT Referral for vascular To enable planned intervention ensuring best access at the pre-dialysis permanent access with fewer complications stage should be made This will also allow for any remedial intervention when the GFR falls to if required HOW IS IT BEING ACHIEVED By implementation of local patient pathway and audit approximately 14ml/min (Renal Association standard 10, 2002) The site of fistula should be To reduce inconvenience to the patient and By maintaining and supporting, open identified and all other co- facilitate easier care of fistula site. communication between patient, nursing staff morbidities should be To facilitate easier access of the fistula during and surgeon. considered cannulation Staff are able to identify best possible fistula To identify optimum site for a fistula sites Patients requiring vascular If vessels are accessed frequently for Once it is identified that the patient requires access for haemodialysis venepuncture the vessel becomes fragile and access surgery, all Healthcare workers should should have their veins may not be sustainable as adequate vascular be advised that vessels on “fistula” arm are not DRAFT preserved and not utilized access for haemodialysis. used for venepuncture/ cannulation or for blood for any intervention before pressure access is created. During inpatient stay a local means of identification is applied to indicate that this arm should not be used for venepuncture/ cannulation or blood pressure measurement Key challenge: Reasons for failure should be documented and action plan should be out in place Scotiish renal nursing strategy group 2004-12-15 16 DRAFT Section 2 pre-operative and peri-operative stage Key point: Minimum of urea & electrolyte levels must be checked before theatre Key point: Fistula mapping may be implemented at time of surgery STATEMENT REASON FOR STATEMENT HOW IS IT BEING ACHIEVED The patient should be To empower the patient to make Designated person provides information, advice and educated regarding access informed decisions about the forth support for patients and carer where appropriate before formation using a selection coming procedure and encourage access formation. of evidenced based participation in recommended A record is kept of information distributed to patients in material tailored to suit the treatment (CSBS, standard 12, 2002) the pre dialysis period Peri-operative care should To ensure patient suitability and safety Implementation of local protocol be implemented as per during peri-operative period Staff involved in the peri-operative period are familiar with individual needs of the patient local protocol Scotiish renal nursing strategy group 2004-12-15 local protocol 17 DRAFT Section 3 Post operative care STATEMENT REASON FOR STATEMENT HOW IS IT BEING ACHIEVED Post operative care- Early detection of Observations are performed in accordance with local protocol and following surgery, all complications To maintain AV the needs of the individual patient patients will require fistula/graft patency Patency of fistula should be documented The patient is given To ensure that staff and patient Local development of post op guidelines. available advice following are aware of the appropriate Clear and concise information and advice should be given AV fistula / vein graft after care following access regarding continuing care and maintenance of fistula patency surgery. formation monitoring of their fistula/ graft Key challenge: comprehensive training and education of staff is required Key challenge: Renal Unit Staff should ensure that relevant information regarding care of vascular access accompanies all patients to non-renal areas Scotiish renal nursing strategy group 2004-12-15 18 DRAFT Section 4- Surveillance of AV Fistula STATEMENT REASON FOR STATEMENT HOW IT IS BEING ACHIEVED Pre surgery assessment To assess potency, vessel size Attend designated vascular clinic and suitability for creation of Duplex scan vascular access Pre admission assessment Date for surgery Post surgery assessment To assess success of surgery Pre Dialysis patients: Telephone follow-up, 2-3 days post surgery Established Dialysis patients: Review within 48hrs of surgery All patients: Follow-up vascular access clinic Repeat Duplex scan Cannulation difficulties newly established fistula Re-assess access Refer to vascular access nurse Discuss with dialysis nurse difficulties experienced during cannulation Duplex scan Re-refer to surgeon Scotiish renal nursing strategy group 2004-12-15 19 DRAFT Continued Routine surveillance To highlight potential problems Pre Dialysis patients: Routinely assess at low clearance clinic, only referred back to vascular access nurse if complication occurs Established Dialysis patients: 6 mthly Blood Temperature monitoring/re circulation/transonic Routine monitoring of arterial and venous pressure Highlight any complication to vascular access nurse To source problem with Refer to vascular access nurse established vascular access Duplex scan Discuss with surgeon or interventional radiographer Thrombosed vascular access Rescue vascular access Emergency admission protocol Refer to vascular access nurse Refer to surgeon or interventional radiographer Key challenge: Renal Unit Staff should ensure that relevant information regarding care of vascular access accompanies all patients to non-renal areas Scotiish renal nursing strategy group 2004-12-15 20 DRAFT Section 6 First Cannulation STATEMENT REASON FOR STATEMENT HOW IS IT BEING ACHIEVED New fistula should be examined by nephrologists/vascular surgeon/ interventional radiologist or designated senior renal nurse prior to first cannulation. To establish readiness for cannulation. Local policy in place and mechanism for assignment of staff to initial cannulation. It is essential that vascular access should be Free from redness Free from signs of infection Bruit is present First and subsequent cannulations while fistula is developing are performed by designated staff members Strict aseptic technique should be used to clean the fistula site prior to cannulation, sterile gloves should be worn during the procedure Scotiish renal nursing strategy group 2004-12-15 Local policy in place for examination of new fistula. To ensure continuity and cannulation by staff with suitable level of knowledge and demonstrating best practice cannulation technique To prevent bleeding into surrounding tissue. To prevent contamination and minimise transfer of skin flora during cannulation process. Aqueous chlorhexidine 0.25- 2% is recommended for cleaning the fistula site. All patients should be encouraged to wash their hands and fistula arm Local heparin policy in place. Local policy in place, staff education. 21 DRAFT when they arrive at the dialysis unit Use 2 x 17-gauge needles OR if dialysis catheter in place 1 x 17gauge needle for arterial line and catheter as venous return line. Keep needles a minimum of 1.5-2 cm away from anastamosis. A tourniquet should be applied to the upper arm so that it is tight enough to dilate the vessel though does not occlude or impede venous outflow. The patient may be encouraged to grip their fistula arm instead of using a tourniquet. Gently pull the skin in the opposite direction to the needle insertion and cannulate the fistula using a 25 degree angle with the bevel of the needle UP. Tape needle at the angle of insertion DO NOT flatten against the skin; stabilise the butterfly with tape and secure Never force the needle against resistance to completely flatten the angle before securing the wings Nursing staff must be made aware of the importance of securing needles. Needles for vascular access should Scotiish renal nursing strategy group 2004-12-15 Small gauge needles to minimise risk of infiltration, minimum distance from anastomosis to prevent damage to anastamosis. Compresses peripheral nerve endings between epidermis and dermis with less skin surface area contacting cutting edge of needle Use of KDOQI guidelines Local Policy in place Staff education Audit Taken from KDOQI Stabilises access and dilates fistula. Bevel UP to ensure cutting edge of needle against the skin, and facilitates smoother incision of skin. Less steep angles increase risk of dragging cutting edge of needle along surface of vessel. Steeper angles increase risk of perforating underside Local Policy of vessel. Staff education See table for BFR and Pressing the needle shaft flat against Needle gauges. the skin moves the needle tip from the desired position within the vessel lumen. Local policy To prevent swelling and damage to Staff education the fistula should infiltration occur. To avoid trauma to the intima of the 22 DRAFT be secured with appropriate dressing Cannulation sites should be monitored throughout the dialysis session Dialysis lines should be secured to the patient’s arm or clothing NOT the pillow or arm rest Use blood flow rate of 200 ml/min MAX and reduce to 180ml/min if not tolerated, increase blood flow rates ONLY if infiltration or other problems are not noted. Needles should be removed at the same angle as insertion, firm but gentle pressure should be applied AFTER the needle has been completely removed from the vessel. Pressure should be applied for at least 10 mins without being released Clamps should NOT be used. Scotiish renal nursing strategy group 2004-12-15 vessel. Needles should be secured to ensure that there is no clinical risk to patient. Movement of needles may result in trauma to fistula and /or haemorrhage Local policy Staff /Patient education To avoid accidental dislodgement. Audit of fistula care/ examination. To prevent displacement of needles and thus prevent infiltration. Blood flow rate should be matched with the correct needle gauge. Local policy Staff /patient education To allow time for clot formation to occlude the puncture site and to prevent bruising from seepage under the skin between the skin surface and the vessel wall. Clamps can damage the fistula as there is no control on the amount of pressure being used, thus the clamp could occlude the fistula. Local policy Local policy will dictate needle size and blood flow rate. 23 DRAFT Map the fistula and cannulation sites used, report any problems to designated vascular access nurse/nephrologists/surgeon/radiologi st. To inform next cannulation. If first week is successful continue to week 2 changing to 16 gauge needles, rotating cannulation sites and increasing blood flow rate. Week 3 : as week 2 or if tolerated well increase to 14/15 gauge needles and required BFR To reach optimum delivered blood flow and dialysis adequacy. Infiltration guidelines If the fistula infiltrates let it rest for 1 week then go back to smaller gauge needles. Notify nephrologist. If it infiltrates a second time rest for 2 weeks and then reduce needle size. Notify nephrologist. If infiltration occurs a third time notify nephrologists/radiologist/surgeon or designated vascular access nurse/coordinator. To prevent further damage to fistula, and allow healing. Fistula needle should be removed immediately before pressure is applied To prevent trauma to the intima of the Staff/ patient education vessel caused by the cutting edge of and training the needle and to minimise pain Scotiish renal nursing strategy group 2004-12-15 Local policy Accurate documentation at all stages. Staff/ patient education and training Consecutive infiltration could signify a problem with the fistula that requires radiological or surgical intervention. 24 DRAFT Key point: Closely monitor heparin according to local policy. Scotiish renal nursing strategy group 2004-12-15 25 DRAFT Scotiish renal nursing strategy group 2004-12-15 26 DRAFT Section 7- Emergency Care STATEMENT REASON FOR HOW IS IT BEING ACHIEVED STATEMENT All patients should be Patient must be aware of Patient should be provided with information regarding their access informed about simple what action to take in event site through easily understood verbal and written communication emergency procedures and of haemorrhage A record is kept of information given to patients how to best care for their Patient plays an important dialysis access role in the development and preservation of the fistula and in early detection of complications Scotiish renal nursing strategy group 2004-12-15 27 DRAFT Appendix 1 Tourniquet information o A tourniquet should be used even when the vessel size does not appear to necessitate it. This will prevent unnecessary trauma o A tourniquet is not required when cannulating an av graft Patient education o Encourage the patient to exercise their fistula arm for vessel development approximately 10-14 days post operatively. There should be no swelling around anastomosis before exercises begin. o A rubber ball or rolled up sock may be used or a hand grip. The ball should be squeezed while the other hand is squeezing the upper arm to impede not occlude venous outflow. o If a tourniquet is used then a pulse should be palpable above the applied tourniquet to avoid complete obstruction of flow o Each exercise should be completed four times daily for 5-10 mins each time Scotiish renal nursing strategy group 2004-12-15 29 DRAFT Appendix 2 Recommended needle size and blood flow rates Size 17g- new fistula Aim for size 15g for established fistula Aim for 14g if adequacy requires improvement For single needle dialysis Scotiish renal nursing strategy group 2004-12-15 30 DRAFT Appendix 3 Patient Education –Emergency Procedures Emergency advice for patients following fistula formation Guideline 10 of the DOQI guidelines state that patient education following fistula formation should include: Patients should be taught how to compress bleeding access Patients should be taught how to recognise signs and symptoms of infection Patients should be taught how to palpate for bruit/thrill/pulse daily and after episodes of hypotension, dizziness or light-headedness Patients should be taught to listen for bruit with ear opposite access site if cannot palpate for any reason Patients should be given contact name and number following formation of their fistula Scotiish renal nursing strategy group 2004-12-15 31 DRAFT References Beathard G A (1992) Physical Examination of AV Grafts Sem Dialysis 5 74 Beathard G A (2002) Improving Dialysis Vascular Access Dialysis and Transplantation 31: 4 pp 210217. Brouwer D, Peterson P (2002) The arteriovenous graft: How to use it effectively in the dialysis unit Nephrology News and Issues Nov 2002: pp 41-49. Fistula First National Vascular Access Improvement Initiative (2003) A practitioners resource guide to Physical Examination of Dialysis Vascular Access. Available at: http://www.esrdnetwork.org/fistula_first_qip.htm#pe Konner K, Nonnast-Daniel & Ritz E (2003) The Arteriovenous Fistula Journal of the American Society of Nephrology 14: 1669-1680. Merrill D, Brouwer D, Briones P (2005) Haemodialysis Access: A guide for caregivers and patients. Dialysis and Transplantation. 34:4; 200-206. National Kidney Foundation K/DOQI Clinical Practice Guidelines for vascular Access 2000 (2001) American Journal Kidney Diseases 37:S137-S181 (supplement 1). Vanholder R (2001) Vascular Access: care and monitoring of function Nephrology Dialysis Transplantation 16: 1542-1545. Brunori G, 2005 Fistula maturation, doesn’t time matter at all? NDT. April, 20(4) pp 684-687 Rayner, H 2003 Creation, cannulation and survival of atrerio-venous fistulae:Data from the Dialysis Outcomes and Practice Study. Kidney International. Jan, 63(1) pp 325-330. Vanholder R, 2001 Vascular Access: Care monitoring and function. NDT 16 p1542-1545 Scotiish renal nursing strategy group 2004-12-15 32