PhysDxII-test1notes
advertisement

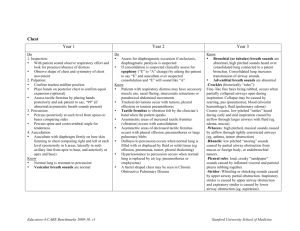
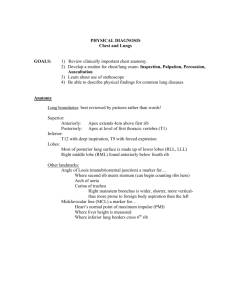
Thursday, September 11, 1997: Respiratory symptoms Stridor – Noisy breathing Voice changes Swelling of ankles- dependent edema (heart failure, renal ds, liver ds, obstruction of venous flow) anasarcageneralized fluid Other factors in the pt information or ROS that indicate the need for a respiratory exam: Related HX. Risk factors Employment, Nutritional status, Home environment, Traveling, Tobacco use, Hobbies, Exposure to Resp. infections. Risk Factors Associated With Respiratory Disability: Table located in Folder in the Library: COUGH: OPPQRST Describe Assoc. Sx. Smoking is the most common cause of chronic coughing – marked A.M. Note: Pack-years of smoking. Descriptors of cough: Possible Cause: Dry, hacking Viral inf. Tumor, allergies, stress, Chronic Productive Bronchiectasis, TB, abscess, chronic bronchitis, bact. pneum Wheezing Bronchiospasm-asthma, allergy Barking Croup Stridor Tracheal obstruction Morning Smoking Nocturnal Post nasal drip, CHF Assoc. with eating Esophageal NMS ds Chronic bronchitis: person has chronic productive cough for at least three months during a year for two consecutive years. Exam findings may be normal. Wednesday, September 17, 1997: 20 minutes late: Sputum Appearance Possible Cause Mucoid Tumor, asthma, TB, emphysema Mucopurulent " " & pneumonia Purulent-Rusty Bacterial pneumonia Purulent – yellow/green Chronic Bronchitis, bronchiectasis, TB, pneumonia Foul odor Lung abscess, bronchiectasis Blood tinged bacterial pneumonia, CHF Pink, frothy Pulmonary edema CLASSIC FOR PULMONARY EDEMA Profuse, colorless carcinoma, advanced and large tumor in the apical area. Bloody Pulmonary emboli, TB, tumor, abscess, bronchiectasis, CA, Cardiac problems, bleeding disorder HEMOPTYSIS: Do you smoke? Did this occur suddenly? Recurrent? How long? Blood tinged or actual clots Associated symptoms – Vomiting, coughing, nausea, SOB, hoarseness Recent surgery? Oral contraceptives, blood thinners Coughed up blood (hemoptysis) vs. vomited blood (Hematemesis) Features: Hemoptysis Hematemesis Preceded by: coughing N/V Past history: ? Hx./CR ds ? Hx./GI ds Appearance: frothy airless Color: br. Red br. Red or dark Contains: nothing/pus ? Food TABLE 2-5: Cough and Hemoptysis CHEST PAIN Cardinal symptom of cardiac disease Pulmonary disease associated with diseases of chest wall or parietal pleura OPPQRST Chest wall – NMS diseases & quality of pain varies with problem Parietal pleura - term: Pleuritis or pleurisy caused by irritation or inflammation (pneumonia, TB, empyema, tumor pneumothorax) pain described as sharp, stabbing, localized to one side felt more on inspiration and patient may splint to avoid pain. TABLE 2-3: Chest pain. Other systems besides cardiovascular can lead to chest pain. Parietal pleura is one of the most common. Dyspnea: Shortness of breath, a subjective difficulty or distress in breathing, usually associated with disease of the heart or lungs; occurs normally during intense physical exertion or at high altitude. Can also be positional Next part will be on TEST! Paroxysmal Nocturnal Dyspnea (PND) - Sudden Onset of SOB occurring at night while a pt. Sleeps. Pt. Sits up and improves. Orthopenia – SOB while lying flat, pt requires more pillows mc assoc. with: CHF, mitral valve ds Trepopnea – pt more comfortable breathing lying on side associated with CHF Platypnea – rare symptom where patient breaths easier in a recumbent position, associated with brainstem or spinal lesions. Important to qualify the dyspnea – exercise tolerance (DOE Dyspnea on Exertion) Grade 1 – excessive activity or exercise (relative to that person) Not necessarily abnormal. If a person runs a marathon look at the recovery time Grade 2 – moderate activity Grade 3 – mild activity Grade 4 – minimal activity Grade 5 – dyspnea at rest WHEEZING (N) Breath sounds: quiet, easy, barely audible near the open mouth, no definite pitch (a.k.a. – white noise) Onset? Occurrence? Smoking history Precipitating factors-allergies? Palliative/Provocative Causes: Bronchiospasm – asthma, severe CHF Aspirated foreign bodies or secretions – mucosal edema Extrinsic compression of bronchus – tumor CYANOSIS Location? Onset? Palliative/Provocative.? Associated symptoms: SOB, cough, bleeding Differentiate central vs. peripheral Central peripheral Decreased O2 in lungs inc. extraction of O2 Chronic lung disease exposure to cold Lips, mucosa, nail beds tips of fingers, toes, nose Inc. w/warming disappears w/warming Dec. O2 intake: foreign body, emphysema, and asthma Dec. O2 absorption: pulmonary fibrosis, emphysema, and metastatic carcinoma INFANT EVALUATION AT BIRTH – APGAR SCORING SYSTEM 012 1.Heart rate absent Slow > 100 BPM 2.Respiratory effort absent Slow/Irregular Good crying 3.Muscle tone Limp some flexion active motion 4.Response to catheter No response Grimace Cough or sneeze In nostrils (tested after Orophaynx is clear) 5.Color Blue/Pale Body Pink Completely Pink __ Extremities Blue Anterior: MCL – Mid clavicular line AAL – Anterior Axillary Line Lateral side: PAL – Posterior axillary line MAL – Mid Axillary Line AAL – Anterior Axillary Line KNOW WHERE LUNGS GO BY DIMENSION AND IMPORTANT LAND MARKS ON EXPIRATION AND INSPIRATION. This is good for her test and for boards. Frequently asked to demonstrate the right middle lobe in testing situations The right middle lobe CANNOT be evaluated posteriorly. It can only be assessed in the mid-axillary line in the anterior. COMPONENTS OF THE EXAM Inspection Palpation Percussion Auscultation Inspection: Note shape of the chest and the movement Normal adult chest is wider than deep and lateral diameter is larger than it’s AP diameter In children the two dimensions approximate due to increased thoracic kyphosis COPD and emphysema lead to a barrel shaped chest. An increase in the AP diameter. Abnormal motion of the chest or paradoxal movement. Happens at area of multiple rib fracture. Flail chest is another term for this. Funnel chest associated with Marphans. Depression of lower portion of sternum. Murmurs. Associated with rickets but not too often. Important thing to note is compression of mediastinal structures. Note patient’s posture Thursday, September 18, 1997: Missed first hour of notes: Talked about lung problems and asthma, deviation of the trachea ect.. Sound transmission can be increased or inhibited with certain conditions. Causes of INC/DEC tactile fremitus referenced form side-to-side: WE WILL NEED TO KNOW THIS INCREASED DECREASED (Unilateral) Pneumonia (Consolidation) Pneumothorax (pleural sp. Air) Atelectasis Pleural effusion (fluid separates) Bronchial obstruction (fibrosis) Inflitrative tumor DECREASED (Bilaterally) COPD Chest wall thickening (Fat, mm) Percussion Notes: & their characteristics Will only asses superficial changes, no deep seeded changes unless they are consistent all the way through. She will not test on the chart for percussion. She will test on certain notes where the sound can be produced and what diseases associated KNOW THIS INFORMATION FOR HER EXAMS AND OTHER EXAMS: Percussion Notes Example Pathology Flatness Thigh Large Pleural Effusion Dullness Liver Lobar Pneumonia (consolidation) Resonance Normal lung Bronchitis Hyperresonance None normally Emphysema, active asthma attack, small pnumthorax Tympani Gastric air bubble of Large Pneumothorax Puffed-out cheek Evaluate lung fields with across and down pattern – ICS Resonance: over all areas of lung filed Abn: chronic bronchitis Dullness: N à 3-4 ICS (L) heart, Abn: consolidation Missed the rest of this overhead. Diaphragmatic excursion: Done bilaterally. Check diaphragm with full inspiration and expiration. Start at inferior angle of scapula and work your way down. Percuss down and you should hear resonant percussion note. When it changes to a dull percussion note you make a mark. Anterior aspects do it from the nipple line down. Right will go from resonant to dull. On left side it will go from resonant to tympani. It is usually done posteriorly but can be done posteriorly also. Diaphragmatic excursion: Level between the dullness of on full expiration and full inspiration --- N: 4-6 cm Decrease excursion: emphysema, obesity, collapses Absent excursion: inflammation of diaphragm or visceral below, phrenic nerve palsy, peritonitis AUSCULTATION: 4 Normal breath sounds heard: (H.O.) Tracheal Bronchial Vesicular Bronchovesicular Inc. Intensity of breath sounds: by consolidation, which promotes sound transmission better than air-filled alveoli. Consolidation Ateclestias Pneumonia Characteristics of breath sounds chart will be in the library and we have one in our book. Dec. intensity of breath sounds: by impedance of airflow through bronchi and alveoli or when the transmission of sound is poor: Bronchial obstruction Pneumothroax Pleural effusion Emphysema COPD Obesity In an upright position, breath sounds are heard earlier in the upper part of lung. Tracheal breath sounds are very loud because there is not very much overlying tissue. Adventitious sounds (added) H.O. Superimposed on Normal (N) sounds Crackles (rales) Wheezes & rhonchi Pleural friction rub Stridor Transmitted Voice Sounds – Vocal Resonance: Used to further evaluate abnormal Exam finding Normal voice sounds are muffled & unclear Wednesday, September 24, 1997: 20 minutes late to class Auscultation Tracheal: harsh and loud because there is nothing covering trachea. Bronchial Vesicular Bronchovesicular Increase intensity of breath sounds: by consolidation, which promotes sound transmission better than air-filled alveoli. Decrease intensity: of breath sounds by impedance of airflow through bronchi and alveoli or when the transmission of sound is poor. Bronchial obstruction Pneumothorax Pleural effusion Obesity COPD Look for scenarios on test: Shortness of breath, barrel shaped chest with diminished chest motion. Tactile fremitus diminished with no sore spots. Change in angulatoin becoming more horizontal toward ribs. Percussion is hyperresonant and breath sounds diminished throughout the whole field. DIAGNOSIS IS EMPHYSEMA Adventitious Sounds (Added) H.O. Superimposed on N Sounds Crackles (rales): fluid is inside lung tissue surrounding alveoli. Alveoli don’t open up as well and when they open, they snap or pop open. Sounds like rice crispies. Wheezes & rhonchi Pleural friction rub Stridor: harsh inspiratory wheeze due to obstruction in either the larynx or trachea TABLE 8-4 IN TEXT: Transmitted voice sounds – Vocal Resonance: Used to further evaluate abnormal exam findings Normal voice sounds are muffled and unclear Abnormal Conditions: (do not need to do all of them but in a testing situation you should assess. These are transmitted vocal resonance test) Bronchophony: greater clarity or increased loudness Egophony: specific type of Bronchophony. When pt. Says e, it will sound like a Whispered Pectoriloqy: whisper sounds will have increased appreciation. Assess when you have Bronchovesicular sounds where they should not be. If you have bronchial sounds where you should have vesicular sounds do one of these tests. Increased Vocal Resonance: consolidation, collapse. Decreased Vocal Resonance: (blockage of respiratory tree) emphysema. TABLE 8-5 IN TEXT "You will absolutely learn it or learn to hate it" Second hour watch video: Respiratory sound video from the library. Wednesday, September 24, 1997: Extra hour for case studies: She likes to test on the location of the middle lobe of the right lung. Pattern to look at on a chest x-ray Look at soft tissue of the neck and supraclavicular Examine bony thorax and look for bony symmetry Diaphragm should be relatively smooth AP Chest Radiograph: Patient in for routine physical. Had chronic productive cough for years. It was clear with little black specks occasionally (tobacco). Suffers from nocturnal as well as morning cough. Clavicle appears to be missing on the right. There are no scars. Clavicle was still there but it was diminished enough that it did not show up on x-ray. There is bony destruction in this patient. Neoplasia leads to bony destruction. Metastasis from the lungs to the clavicle. Diaphragm is elevated on the left as to the right. This is because of the liver. There is a problem with the diaphragm There is respiratory lag, reduced diaphragmatic excursion, labored breathing Can usually see lung vessels, if you cannot see them it could be pneumothorax . In this patient do tests to rule out neoplasia. Do bone scan, blood tests, biopsy ect… NEW CASE: Lateral x-ray: look at pre-cardiac space, cardiac space and post-cardiac space. 39 year old female and sent her x-rays as a new patient. (Chest x-rays) Mid thoracic pain with a 39 year old female with no exam findings because she is not there yet. Only one breast shadow on patient. Vascularity on side of no breast increases the film density. This patient has had a mastectomy. Make sure you do a very thorough examination. Breast carcinoma can metastasize into the spine and this was an example of a national board question 77 year old man Presents with chest pain and shortness of breath following an automobile accident The whole right side was sore. Wearing seatbelt as a passenger Not cyanotic in any way. Do history, OPPQRST Past history is working on the docks on the riverfront lifting heavy boxes, is a smoker, and has had a bout with tuberculosis. Auto accident 2 days ago and things are getting more irritation for him. He is leaning into the side when he sits Breathing is increased and shallow. See paradoxical motion of the chest We expect to see fractures and in the X-Ray and we see multiple fractures 66 year old Man complaining of shortness of breath that has been progressive over the years. Medical doctor told him he has arthritis in his back Was a salesman who did lots of driving Smoker of at least 45 years (2-3 packs/day) Currently smokes ½ pack a day Has labored breathing but does not purse lips. Uses accessory muscles of respiration Not cyanotic and you do not note clubbing Everything moving symmetrically No respiratory lag but there is not much motion in chest even when he takes deep breath He is a large man but not obese Increased thoracic kyphosis Palpation findings note no areas of tenderness on chest wall Tender areas in T4-T6 in thoracics and there is no motion Trachea is midline Vocal and tactile fremitus Percussion is hyperresonant all over (diffusely) Diminished breath sounds on auscultation DDX is emphysema (bolus emphysema) Air trapping in upper lungs. Major pockets of air in upper lungs. 60 year old with left lung and chest pain Pleuritic chest pain is a friction rub Diaphragm is blunted because of fluid There is a gigantic mass under the sternum Mediastinal mass is a bronchiogenic carcinoma. Lateral sulcus is blunted DDX is a tumor with pleural effusion. Thursday, September 25, 1997: 20 minutes late to class Factors Associated With Breast Cancer Age (80% of cases occur after age 40) Early menarche (before age 12) Late menopause ( after age 50) Nulliparity (condition of having borne no children) Late age at birth of first child (after age 30) Personal history of premalignant mastpathy Personal history of ovarian, endometral, or colon cancer Family history of breast cancer Diet high in animal fats Obesity (may be a diagnostic factor) Mass Questions: When did your first notice Change with menses Tender Any skin changes Recent injury Nipple discharge or retraction Pain Questions OPPQRST Describe the pain Unilateral or bilateral (infection is unilateral) Associated symptoms Recent injury Nipple discharge Questions: Color of discharge Onset Unilateral or bilateral Related to menses Associated symptoms On medication or orat contraceptives m/c – bloody, serous, milky Serous – thin & watery, may appear as yellow stain Intraductal papilloma Carcinoma B/L: oral contraceptives Bloody discharge Intraductal papilloma Malignant Intraductal papillary carcinoma Milky: milk Late pregnancy: lactation Persistent lactation – galactorrhea Pituitary tumor Fibrocystic changes do not mean carcinoma 100% Many women get carcinoma without first having fibrocystic changes. Diet: benefic of soy in the diet. Soy is a precursor to estrogen. Look at this instead of hormone replacement Ginseng is also a precursor to estrogen. Exam Procedures (missed most of this overhead) Inspection Examination of the axilla (done in seated position as well as supine) Palpation Inspection: Sitting and supine Number, size shape, symmetry Slight asymmetry in size is normal Nipples: To bring out dimpling or retraction have pt perform various maneuvers 1.raise arms over the heads – stretching skin 2.press hands against hips – contrast pecs Palpation: Supine: place a pillow under patients shoulder on side of exam Proceed systematically: quadrant, linear, circular, zigzag Note consistency of tissue – N varies widely physiologic nodularity may inc. become painful during or before menses. Best time to perform exam is 1-2 weeks or 7-10 days after menses. Tenderness, mass, temperature of skin. Note lesions in clock method with cm from the nipple. Nodules Size Shape (round, regular, or irregular) Consistency (soft, firm or hard) Delimitation (margins) Tenderness Mobility – motility – fixed Palpate each nipple Compress or strip Squeeze nipple and note any discharge Thickening or blood discharge à cancer Evaluate Axillary Nodes Note: number, site, size, tenderness Mobility Rash – deodorant, dermatitis Infection – sweat glands infection Unusual pigmentation – may mean cancer Flow sheet of lymph nodes of the breast. Axillary nodes à apical (central) ex. Nodes à infraclavicular nodes à thoracic duct & supraclavicular à Missed the rest of the flow sheet. Video of breast exam: Friday, September 26, 1997: Case Studies (extra lecture) CASE 1 Late 20’s Female Chronic cold that lead to productive cough with LBP Went to family physician and was put on antibiotics for the common cold (10 days) They feel like they are doing better but after a few days the cough starts turning color. (yellow productive cough) Now they have a sharp pain upon coughing but now hurts to cough and bring arm back Temp 100.8oF, pulse is about 80 bpm, Respirations 22/min, Blood pressure 126/78 Cervical is positive compression and Spurlings Distraction does not bring relief. George’s maneuver negative Dermatomes and myotomes normal Normal active range of motion Motion palpation with L SI, mid thoracic and rib subluxation Respiratory is relatively normal upon inspection No tender spots posteriorly except rib subluxation spot Tracheal is midline Mid lateral aspect around ant. Axillary line is increase in vocal tactile fremitus percussion in this same are (rib 5 & 6) there is a dull note Auscultation hear Bronchovesicular sounds, on left vesicular, on R 4&5 hear bronchial breast sounds till about 6th intercostal space All vesicular sounds on posterior aspect. Could do Egophony, whisper pectoriloquay, Bronchophony Bronchophony is positive There is consolidation of fluid with increased density in the area. DDX is pneumonia. Probably viral because it is associated with low grade fever. Order sputum culture, swab out throat. CASE 2 2 year old with asthma, problems with breathing. Atelectasis is occurring with this because of bronchial obstruction because of mucous plugs. Closes off portion of bronchial tree and have airless lung. This usually happens with children who have chronic asthma. This will not happen with one asthma attack. This has pulled the mediastinal structures over to the side of airless lung. Atelectasis behaves more like pneumonia than emphysema. If it occurs in the lower lobe further away from bronchus you have diminished tactile fremitus, WILL NOT ASK THIS ON THE TEST BECAUSE IT IS A TRICKY SCENARIO. CASE 3 40 year old male Presents with back pain on the left side, lumbar region History of alcoholism and acute pancreatitis, at least three times. Not considered chronic pancreatitis because after inflammation pancreatic enzymes are still normal. Last episode over a year ago. Still has tenderness over the area. Complains of back pain and cannot take a deep breath without pain. His thoracic spine is very messed up. There are very many trigger points Respiratory exam includes diminishment in motion appreciated on anterior and posterior aspect. Trachea is midline Tactile fremitus is diminished on posterior aspect on left as well as lateral an anterior. Percussion: note a dull or flat percussion note along involved area Diaphragmatic excursion decreased on left side Auscultation shows diminished breath sounds except for above involved area. Consider: Neoplasm Pseudo-abscess due to acute pancreatitis. (may develop in liver and pancreas) Respiratory system consider: X-ray shows more dense on left lower lobe PULMONARY OR PLEURAL EFFUSION IS THE DDX. (How did it get there?) Pleurisy could have developed with the inflammation of the pancreas Blood test should be done to look at pancreatic enzymes CBC should be done to look at possibility of infection. CASE 4. Healthy young man who was outside playing soccer and suddenly has sharp pain on left side and began having difficulty breathing Trachea being pulled to left side Cyanosis of the lips Labored breathing. DDX: Spontaneous pneumothorax. Would be asymmetrical Person sweating with labored breathing. Tactile fremitus would be decreased Percussion note would be hyperresonant or tympanic (if large) Decreased breath sounds on the side of involvement. Can see no vascularity on the side involved in the x-ray Case 5 Patient presents with a complaint of problems around the cervical, thoracic are. Chronic productive cough Low grade fever Night sweats. DDX IS TB Apical area is the most common area for this to develop Chronic fatigue Weight loss Chronic sputum production Chronic coughing Night sweats (classic) Case 6 5 years post radiation therapy for Squamous cell carcinoma for epiglottis. Now having significant respiratory problems On x-ray there is a significant tumor. This is a hylar mass Person will probably develop pleural effusion if they have not already. The thing about carcinoma in early stages it that there may be normal exam findings. Must consider history Shortness of breath in general is grounds for doing a chest x-ray. If there is a productive cough, sputum test may be ok END EXAM I NOTES!