胃腸科POMR範本
advertisement
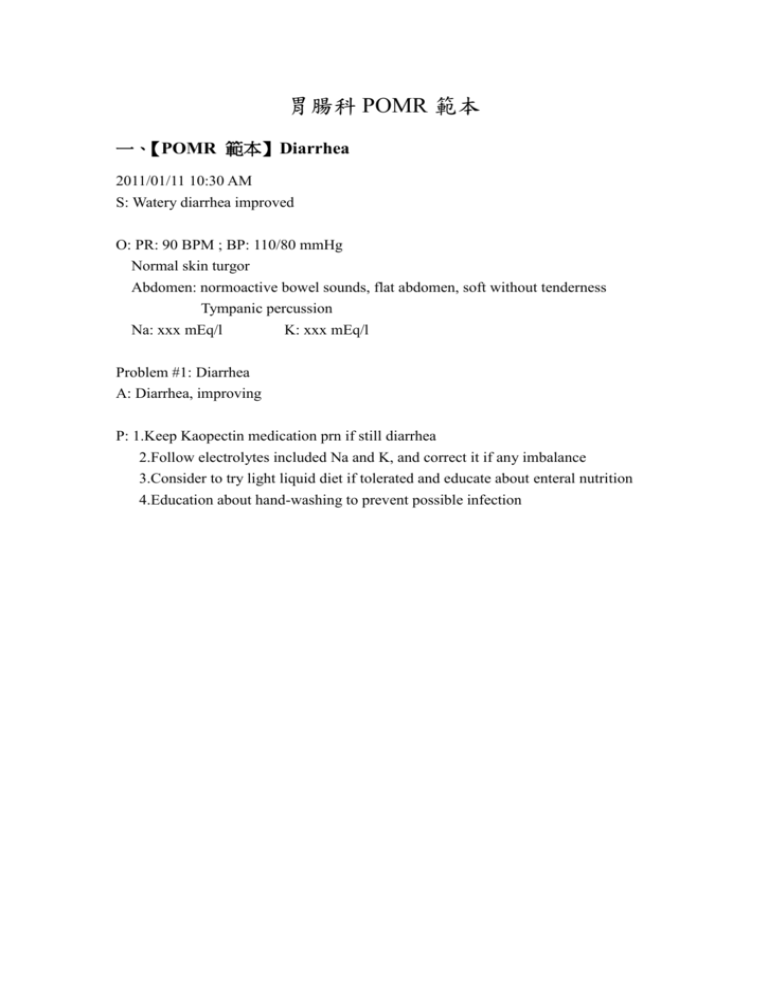
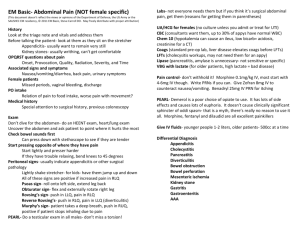
胃腸科 POMR 範本 一、【POMR 範本】Diarrhea 2011/01/11 10:30 AM S: Watery diarrhea improved O: PR: 90 BPM ; BP: 110/80 mmHg Normal skin turgor Abdomen: normoactive bowel sounds, flat abdomen, soft without tenderness Tympanic percussion Na: xxx mEq/l K: xxx mEq/l Problem #1: Diarrhea A: Diarrhea, improving P: 1.Keep Kaopectin medication prn if still diarrhea 2.Follow electrolytes included Na and K, and correct it if any imbalance 3.Consider to try light liquid diet if tolerated and educate about enteral nutrition 4.Education about hand-washing to prevent possible infection 二、【POMR 範本】Dysphagia 2011/01/11 10:30 AM S: Difficulty in swallowing persisted O: T: ; PR: ; RR: ; BP: Clear conscious and no specific neurologic change No oral ulcer or palpable neck mass, but the patient has still difficulty in swallowing even liquid and easy choking Chest: symmetric expansion, bilateral clear breath sounds Abdomen: normoactive bowel sounds, flat abdomen, soft without tenderness Tympanic percussion Na: xxx mEq/l K: xxx mEq/l Problem #1: Dysphagia A: Suspected esophageal cancer, stationary P: 1.Arrange computed tomography from neck to chest and UGI endoscopy for examination and biopsy 2.Begin parenteral nutritional support if enteral route is not available 3.follow electrolytes included Na and K, and correct if any imbalance 4.Adequate pain control 5.Explain and discuss with the patient and family members about possible need of gastrostomy or jejunostomy for the enteral nutrition; and consult general surgeon for the evaluation and explain risks and benefits 三、【POMR 範本】Ileus 2011/01/11 10:30 AM S: Abdominal fullness mild improved O: PR: 90 BPM ; BP: 110/80 mmHg EKG: Normal sinus rhythm Flatus(+); Stool passage(+) Abdomen: normoactive bowel sounds, mild distended abdomen, soft without tenderness; Tympanic percussion, no shifting dullness No murphy sign Na: xxx mEq/l K: xxx mEq/l KUB: Diffuse ileus of abdomen Ca: xxx mEq/l Problem #1: Ileus A: Ileus, improving P: 1.Arrange abdominal sonography and/or computed tomography 2.Follow electrolytes and correct if any imbalance 3.Keep NG decompression and use of prokinetic agents 4.Education about high fiber diet and adequate exercise 5.Consult GS surgeon, if prolonged ileus with peritoneal sign(+) 四、【POMR 範本】Acute cholecystitis 2011/01/11 10:30 AM S: RUQ abdominal pain improved, less nausea. Fever subsided Started liquid diet this morning. O: Consciousness: clear Vital signs: BT 36.6 C; RR: 15 breaths/min PR: 84 beats/min; BP: 108/64 mm Hg Breath sounds: clear and equal bilaterally Heart: RHB, no murmur Abdomen: non-distended, normoactive bowel sounds: trivial RUQ tenderness; no Murphy’s sign, guarding or rebound pain. Lab data: K+ 3.01(12/19) 3.05(12/21) Problem #1: Acute cholecystitis A: day 4, improved, food intake started today. P: 1.Allow ambulation and advance to soft diet today if tolerated 2.Shift to oral antibiotics tomorrow if no further abdominal pain or fever 3.Keep recording I/O and maintaining adequate iv hydration until full diet 4.Pain relief prn 5.Educate patient to avoid high-fat diet intake Problem #2: Hypokalemia A: potassium level still inadequate P: Add 20 meq KCL to every 500 ml of IV fluid Recheck K+ tomorrow 五、【POMR 範本】Acute pancreatitis 2011/01/11 10:30 AM ( day ? after admission) S: central/epigastric pain improved, less nausea. Started liquid diet this morning. O: Consciousness: clear Vital signs: BT 36.6 C; RR: 15 breaths/min PR: 84 beats/min; BP: 108/64 mm Hg Breath sounds: clear and equal bilaterally Heart: RHB, no murmur Abdomen: non-distended, normoactive bowel sounds: Mild epigastric tenderness, no guarding or rebound pain. Problem #1: Acute pancreatitis A: day 4, improved, food intake started today. P: 1.Allow ambulation and advance to soft diet today if tolerated 2.Abdominal CT prn if abdominal pain worsened or fever occurred 3.Keep recording I/O and maintaining adequate iv hydration until full diet 4.Pain relief prn 5.Educate patient to avoid high-fat diet intake 六、【POMR 範本】Jaundice 2011/01/11 10:30 AM ( day ? after admission) S: RUQ abdominal pain improved, less nausea. Fever subsided, no chills today Started liquid diet this morning. O: Consciousness: clear Vital signs: BT 36.6 C; PR: 84 beats/min; Sclera: anicteric RR: 15 breaths/min BP: 108/64 mm Hg Breath sounds: clear and equal bilaterally Heart: RHB, no murmur Abdomen: non-distended, normoactive bowel sounds: trivial RUQ tenderness; no Murphy’s sign, guarding or rebound pain. PTCD: 30 ml (wound clean, no redness or discharge) Lab data: K+ 3.01(12/19) 3.05(12/21) Bilirubin total 3.5(12/19) 1.1(12/21) Problem #1: Acute cholangitis A: day 4, improved, anicteric sclera, food intake started today. P: 1.Allow ambulation and advance to soft diet today if tolerated 2.Arrange ERCP tomorrow for CBD stone removal. 3.Shift to oral antibiotics tomorrow if no further abdominal pain or fever 4.Keep recording PTCD&I/O and maintaining adequate iv hydration until full diet 5.Pain relief prn #2. Hypokalemia A: potassium level still inadequate P: Add 20 meq KCL to every 500 ml of IV fluid Recheck K+ tomorrow 七、【POMR 範本】Cirrhosis 2011/01/11 10:30 AM ( day ? after admission) S: abdominal fullness for ? days O: Consciousness: clear/ alert/ irritable/ drowsy/ coma , E?V?M? Vital signs: BT ? C; RR: ? breaths/min PR: ? beats/min; BP: ?/? mm Hg Breath sounds: clear/ rales(pleural effusion?) bilateral or unilateral? Heart: RHB, no murmur Abdomen: distended, hyperactive bowel sounds, whole abdominal tenderness Shifting dullness. No palpable mass, no guarding or rebound pain. Abdominal sonography: PES: AFP: Albumin: PT: Ammonia: Bil. T: Problem #1: #1. Cirrhosis child ? (score: ) A: P: massive ascites with jaundice under lasix + aldacton use, disease wosening 1. Keep diuretic use + Alubumin or FFP supply 2. correct coagulopathy 3. If advanced stage, discuss hospice care to patient and family 4. consider EVL for prevent variceal bleeding 5. consult dietician for nutrition support 6. Inderal use for portal hypertension. 7. keep I/O balance 8. ascites tapping if diuretic is insufficient. 八、【POMR 範本】Colon cancer 2011/01/11 10:30 AM ( day ? after admission) S: consipation for ? days O: Consciousness: clear, E?V?M? Vital signs: BT ? C; RR: ? breaths/min PR: ? beats/min; BP: ?/? mm Hg Breath sounds: clear and equal bilaterally Heart: RHB, no murmur Abdomen: distended, hyperactive bowel sounds, whole abdominal tenderness No palpable mass, no guarding or rebound pain. KUB: Abdominal sonography: Abdominal CT: Colonoscopy CEA: Albumin: Problem #1: Colon cancer, still staging A: constipation and ileus, suspect tumor obstruction, disease wosening P: 1.Consult GS for relief of obstruction, consider colonostomy 2.Consult oncologist for CCRT or chemotherapy 3.If advanced stage, discuss hospice care to patient and family 4.NPO if complete obstruction and adequate nutrition support. 5.Explain the staging result with the patient and family 九、【POMR 範本】Hepatoma 2011/01/11 10:30 AM ( day ? after admission) S: poor appetite O: Consciousness: clear, E?V?M? Vital signs: BT ? C; RR: ? breaths/min PR: ? beats/min; BP: ?/? mm Hg Breath sounds: clear and equal bilaterally Heart: RHB, no murmur Abdomen: non-distended, normoactive bowel sounds: No palpable mass, no guarding or rebound pain. Abdominal sonography: Abdominal CT: AFP: PT: Albumin: Bil. T.: Problem #1: Hepatoma A: no abominal pain, no jaundice, BCLC ?, Child score ? still poor appetite P: 1.Consult GS if resection is indicated, or RFA/PEI if BCLC (A) 2.If not resection, consider TACE if BCLC (B) 3.If advanced stage, discuss hospice care to patient and family 4.Consult dietician for nutrition support. 5.Sympatic treatments for his multiple discomforts 十、【POMR 範本】Variceal bleeding or UGI bleeding 2011/01/11 10:30 AM S: Bloody vomitus / hematemesis for (duration) O: Conciousness – clear / drowsy / loss Vital signs – T/P/R – ? SpO2 – ? Conjunctiva – pale/pink Skin – cool/warm/dry/moist Chest – rales/wheezing Abdomen – soft/rigidity/flat/distended Normo/hypo/hyperactive bowel sounds. Tymphanic/dull/hyperesonance Tenderness/No tenderness/Rebound tenderness Bloody vomitus amount – ( ) ml Problem #1: Upper gastrointestinal bleeding Assessment – Variceal (EV or GV) bleeding or active peptic ulcer bleeding Plan - Fluid resuscitation with normal saline and blood products transfusion - Check hemoglobin, platelet and coagulation profile - Arrange upper GI endoscopy with intervention - NG tube insertion for adequate drainage - Airway protection if massive bleeding or consciousness loss - Transfer to ICU if massive bleeding. 十一、【POMR 範本】LGI bleeding 2011/01/11 10:30 AM S: Bloody stool passage / melena / brick stool passage for (duration) O: Conciousness – clear/drowsy/loss Vital signs – T/P/R – ? SpO2 – ? Conjunctiva – pale/pink Skin – cool/warm/dry/moist Abdomen – soft/rigidity/flat/distended Normo/hypo/hyperactive bowel sounds. Tymphanic/dull/hyperesonance Tenderness/No tenderness/Rebound tenderness DRE – blood-stained glove / external hemorrhoids noted Bloody stool passage amount – ( ) ml Problem #1: Low gastrointestinal bleeding Assessment – Low gastrointestinal bleeding, suspected colon tumor / rectal tumor / hemorrhoidal bleeding Plan - Fluid resuscitation with normal saline and blood products transfusion - Check hemoglobin, platelet level and coagulation profile Colon preparation and arrange colonoscopy Consult general surgeon for evaluation. Arrange TAE if massive bleeding despite endoscopic therapy.