Unit IX: Identification of a Gram
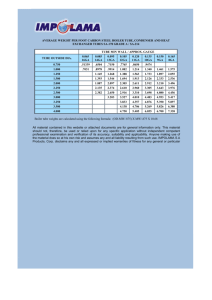
advertisement

MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 1 Unit IX: Identification of a Gram-Negative Intestinal Pathogen: Activities: 20.1 Isolation & Phenetic ID of Enteric Pathogens (Ex 26) 22.1 Molecular ID of Enteric Pathogens (Ex 27) 25.1 Enterotube II Multiple Test System (Ex 28) p 1 p 6 p 12 Introduction: The enteric pathogens of prime medical concern are the salmonella and shigella. They cause enteric fevers, food poisoning, and bacillary dysentery. Salmonella typhi, which causes typhoid fever, is by far the most significant pathogen of the salmonella group. In addition to the typhoid organism, there are 10 other distinct salmonella species and over 2,200 serotypes. The shigella, which are the prime causes of human dysentery, comprise four species and many serotypes. Serotypes within genera are organisms of similar biochemical characteristics that can most easily be differentiated by serological typing, testing of the unknown bacterium for reactivity to different antibodies specific to each serotype. Routine testing for the presence of these pathogens is a function of public health laboratories at various governmental levels. The isolation of these pathogenic enterics from feces is complicated by the fact that the colon contains a diverse population of bacteria. Species of such genera as Escherichia, Proteus, Enterobacter, Pseudomonas, and Clostridium exist in large numbers; hence it is necessary to use media that are differential and selective to favor the growth of the pathogens. In this laboratory unit, we will isolate putative intestinal pathogens and other enteric bacteria on differential and selective media, and proceed to confirm the isolate to be a pathogenic species using two different identification (ID) procedures. Identification of bacteria has traditionally relied on phenetic characters, such as morphological features and metabolic or physiological potential. The later characters can be assessed rapidly using miniaturized multiple-test kit systems, such as the Enterotube II designed for identifying species of the Enterobacteriaceae. Molecular techniques provide alternate approaches to the identification of unknown bacteria. Here we will PCR amplify the 16SrRNA gene from our putative isolates and compare its 16SrDNA restriction fragment length polymorphism (RFLP) pattern to a set of known patterns for identification. 20.1 Isolation & Phenetic ID of Enteric Pathogens: (Ex 26) Identification of unknown enteric bacteria to genus will follow a standard separation outline procedure used to demonstrate the presence of salmonella or shigella in a patient's blood, urine, or feces (Figure 26.1). Note that lactose fermentation separates the salmonella and shigella from most of the other Enterobacteriaceae. Final differentiation of these two enteric pathogens from Proteus relies on motility, hydrogen sulfide production, and urea hydrolysis. Differentiation of the positive lactose fermenters on the left side of the separation outline is used for the identification of enteric coliform bacteria, some genera of which can include pathogen strains, like Escherichia coli O157. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen Figure 26.1. Separation outline for genus level identification of the Enterobacteriaceae. In this experiment you will be given a mixed culture containing a coliform and Proteus, and salmonella or shigella. The pathogens will be of the less dangerous types, but their presence will, naturally, demand utmost caution in handling. Your problem will be to isolate the pathogen from the mixed culture and make genus identification. There are five steps that are used to prove the presence of these pathogens in a stool sample: (1) enrichment, (2) isolation, (3) fermentation tests, (4) final physiological tests (Figure 26.2), and (5) serotyping. We will not perform the latter. Enrichment from stool: There are two enrichment media that are most frequently used to inhibit the non-pathogens and favor the growth of pathogenic enterics. They are selenite F and gramnegative (GN) broths. While most salmonella grow unrestricted in these two media, some of the shigella are inhibited to some extent in selenite F broth; thus, for shigella isolation, GN broth is preferred. In many cases, stool samples are plated directly on isolation media. In actual practice, 1 to 5 grams of feces are placed in 10 ml of enrichment broth. In addition, plates of various kinds of selective media are inoculated directly. The broths are usually incubated for 4 to 6 hours. Because we are not using stool samples in this exercise, the enrichment procedure is omitted. Instead, you will streak the agar isolation media directly from the unknown broth culture and broth cultures of other unknowns you would like to work with. Isolation of coliform and non-coliform enterics: There are several excellent selective differential media that have been developed for the isolation of coliform and non-coliform enteric pathogens. Various inhibiting agents such as brilliant green, bismuth sulfite, sodium desoxycholate, 2 MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 3 and sodium citrate are included in them. For Salmonella typhi, bismuth sulfite agar, or SalmonellaShigella (SS) agar, appears to be the best media. Colonies of S. typhi on these media appear black due to the reduction of sulfite to sulfide. Other widely used media are ENDO agar, MacConkey agar, Hektoen Enteric (HE) agar, and Xylose Lysine Desoxycholate (XLD) agar. These media may contain bile salts and/or sodium desoxycholate to inhibit gram-positive bacteria. Some like SS agar contain citrate to inhibit coliforms and other non-enterics. All of them contain lactose and a dye so that if an organism is a lactose fermenter (putative coliform), its colony will take on a color characteristic of the dye present. Recall, the dark colonies with green-metallic sheen grown on ENDO agar are likely to be coliform enteric bacteria. Once colonies are isolated, we will proceed with fermentation tests. Fermentation tests: Recall, the fermentation characteristic that separates the SS pathogens from the coliforms is their ability to ferment lactose. Once we have isolated colonies on differential media that look like coliforms and those that look like salmonella or shigella, the next step is to determine whether these isolates can ferment lactose. All media for this purpose contain at least two sugars, glucose and lactose. Some contain a third sugar, sucrose. They also contain phenol red to indicate when fermentation occurs; the indicator turns yellow under acid conditions created by sugar fermentation. Russell’s Double Sugar (RDS) agar is one such media. Final Morphological and Physiological Tests: Motility/H2S/indole production and urease activity will be accessed for each isolate using SIM medium and urea broth, respectively. Also, citrate and tryptophan utilization will be determined to differentiate between different lactose-fermenting (coliform) bacteria (Figure 26.1). Any salmonella will be a non-lactose-fermenter that exhibits motility, produces hydrogen sulfide, yet cannot produce urease. Any Shigella will be a non-lactose fermenter with urease activity, but is non-motile and cannot produce hydrogen sulfide (Figure 26.1). You will also be making a gram-stained slide to perform a purity check on your isolates. We will also inoculate Entrotube II multitest kits during the third week of this unit (see Exercise 28 below). Exercise 26 Isolation & Penetic ID: Materials: unknown broth cultures (one a mixture of a coliform, proteus, and a salmonella or shigella) Petri plates of different selective media: ENDO and SS agars Slants of Russell Double Sugar (RDS) agar 1 tube of SIM medium for each SS pathogen 1 tube of urea broth for each SS pathogen or coliform. Gram Stain Kits 1 stab tube of Simmon Citrate agar for each coliform Kovacs' reagent and chloroform for Indole testing (i.e. tryptophan utilization) 5-ml pipettes MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen Figure 26.2. Protocol for SS pathogen isolation. We will add steps to this for coliform isolation. 4 MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 5 Procedure: 1. Fore each unknown, label plates of each media type with your name and unknown number or code. 2. With a loop, streak each plate with your unknown in a manner that will produce good isolation. Incubate the plates at 37° C for 24 to 48 hours. << Ex 26 – Day 2 >> For each unknown and media, inoculate three slants using three different colonies on the selective media that look like either salmonella or shigella, or like a coliform. The reason for using three slants is that you may have difficulty distinguishing Proteus from the SS pathogens. By inoculating three tubes from different colonies, you will be increasing your chances of success. 3. For each unknown, label the three slants with your name and the number of your unknown. 4. Look for isolated colonies that look like salmonella or shigella organisms, and those that look like coliforms. With a straight wire, inoculate the three agar slants from separate SS-appearing colonies. Use the streak-stab technique. When streaking the surface of the slant before stabbing, move the wire over the entire surface for good coverage. 5. Repeat step #3 for any putative coliform isolates. 6. Incubate the slants at 37° C for 18 to 24 hours. Longer incubation time may cause alkaline reversion. Even refrigeration beyond this time may cause reversion. Alkaline reversion is a condition in which the medium turns yellow during the first part of the incubation period and then changes to red later due to increased alkalinity by ammonia produced as proteins degrade. << Ex 26 – Day 3 > 7. Examine the slants from the previous period to separate possible coliforms and possible SS pathogens for further testing (Figure 26.2). Select those tubes that have a yellow butt with a red slant as possible SS pathogens. These tubes contain organisms that ferment only glucose (non-lactosefermenters). Slants that are completely yellow are able to ferment lactose as well as glucose, and considered coliforms. Tubes that are completely red are either non-fermenters or examples of alkaline reversion. Ignore the later tubes. 8. With a loop, inoculate one tube of urea broth from each coliform and each possible SS pathogen. 9. With a straight wire, stab one tube of SIM medium from each coliform and each possible SS pathogen. Stab in the center to two-thirds of depth of medium. 10. With a straight wire, stab the Simmon’s Citrate agar for each coliform using the technique in #9. 11. Incubate all of these tubes at 37° C for 18 to 24 hours. 12. Make gram-stained slides from the same slants and confirm the presence of gram-negative rods. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 6 << Ex 26 – Day 4 >> 13. Examine the tubes of SIM medium, checking for motility and H2S production. If you see cloudiness spreading from the point of inoculation, the organism is motile. A black precipitate will be evidence of H2S production. 15. Test for indole production by pipetting 2 mI of chloroform into each SIM tube and then adding 2 mI of Kovacs' reagent. A pink to deep red color will form in the chloroform layer if indole is produced. Salmonella are negative. Some Shigella may be positive. Citrobacter and Escherichia are positive. 16. Examine the urea broth tubes. If the medium has changed from yellow to red color, the organism is urease-positive. 17. Examine the Simmon Citrate tubes. If they have turned from green to blue they are positive for citrate utilization. 18. Summarize all of your results in a table; and use the identification outline (Figure 26.1) to determine the genera of your unknowns – record. 19. Address all questions and discussion points presented at the end of Exercise # 28. 22.1 Molecular ID of Enteric Pathogens: (Ex 27) Another approach to identify bacteria is based on the Restriction Fragment Length Polymorphism (RFLP) of 16SrRNA genes (16SrDNA); its results in a type of DNA-fingerprint. The secondary structure of the 16SrRNA (Figure 27.1) is highly conserved and functions well as a molecular chronometer. For this approach, DNA is extracted from a bacterial culture and the 16SrRNA gene is amplified via the Polymerase Chain Reaction (PCR) of partial or entire PCR amplification of the 16srRNA gene is possible, with more information gained by having more of the molecule. Restriction endonucleases are then used to cleave the gene into fragments of different sizes. Tetrameric restriction endonucleases are preferred, because 4 nucleotide target sequences permit a greater number of “cuts” and are more sensitive to variation among highly conserved rRNA gene sequences than restriction enzymes with a greater number of target nucleotides. Typically 2 to 3 enzymes are used in separate digests of the same sample to obtain adequate information for identification at the species level. Patterns are compared with known patterns, based on the computerized database or determined empirically. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 7 Figure 27.1. Secondary structure of the 1542 base pair 16S rRNA of Escherichia coli. For our project, we will identify an unknown bacterium from a pure culture using the 16S rDNARFLP strategy outlined above. We will begin by extracting the bacterial genomic DNA to use as template for PCR amplification of the 16S rRNA gene. As PCR primers, we will use an oligonucleotide sequence equal that beginning at position 68 on the sense strand (forward primer; 68F; 5’-TNANACATGCAAGTCGAKCG-3’) and the complement sequence of the sense strand ending at position 1406R (reverse primer; 1404R; 5’-ACGGGCGGTGTGTRC-3’) (Figure 27.2). Therefore, our PCR product will be 1338 base pairs, or about 200 base pairs short of the complete 16S rRNA gene. We will select two tetrameric restriction enzymes for digesting the PCR product after its precipitation, and separate the fragments on a 3% agarose gel. To identify your unknown, RFLPs will be compared with a selection of results from known species provided by your instructor. 68 5’ 1406 sense strand 3’ 16SrRNA 3’ 5’ Figure 27.2 Orientation of primers from position 68 forward (68F) and from position 1406 in reverse (1406R) relative to the sense strand DNA. Dark arrows represent primers next to their complement (target); arrow point is the 3’ end of primer where DNA elongation will proceed. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 8 Exercise 27 The exercise is divided into four separate protocols: 1) extraction of genomic DNA from a bacterial culture; 2) PCR amplification of the 16SrRNA gene; 3) Restriction enzyme digest of amplicons; and 4) agarose gel electrophoresis. Extraction of Genomic DNA from Bacteria: Materials: TSB cultures of bacterial unknown(s) Lysozyme Buffer (50mg/ml Lysozyme in 10 mM Tris, 1 mM EDTA, at pH 8.0) GITC Buffer (5M guanidinium isothiocyanate, 100 mM EDTA, 0.5% sarkocyl detergent) 7.5 N NH4Ac (ammonium acetate) Chloroform:Pentanol (24:1 ratio) Isopropanol 70% EtOH Eppendorf tubes Sterile DI-water Micropipetters and appropriate sterile tips. Procedure: (We will need to share the microcentrifuge at each step!) 1) Place 1.5 ml of bacterial culture in a well labelled eppendorf tube. Spin down the bacteria in the microcentrifuge for 1 min at 13,000 rpm. [Always orient your eppendorf tube in the microcentifuge with the hinge-side outwards; this will be the side where your pellet forms.] Pour off the supernatant into the red waste/autoclave bag. Use the 10-100 microliter pipetter to remove the remainder of the supernatant. 2) Add 100 microliters of Lysozyme Buffer (to the bacterial pellet and use the broader tip of the toothpick to mix the suspension by twirling the toothpick between your thumb and forefinger. Place the suspension in the heating block at 37 C for 30 min. 3) Add 50 microliters of GITC Buffer to the eppendorf tube and vortex the suspension. Place the eppendorf tube on ice for 10 min. 4) Add 250 microliters of ice-cold 7.5 N NH4Ac (ammonium acetate) to the eppendorf tube and mix. Return the tube to ice for 10 min. 5) Add 500 microliters of Chloroform:Pentanol (24:1 ratio) to the eppendorf and vortex the tube. 6) Spin the eppendorf tube for 5 min at 13,000 rpm. If the supernatant is still visibly turbid, then spin for another 5 min interval. 7) Carefully remove the upper phase from the eppendorf tube and place this in a new, labelled eppendorf tube. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 9 8) Add 540 microliters of ice-cold Isopropanol to the upper phase and mix. Spin the eppendorf tube for 10 min at 10,000 rpm. 9) Carefully pour off the supernatant into the waste bag. Add 1 ml of 70% ice-cold EtOH (ethanol) to the eppendorf tube and mix. Spin the tube for 10 min at 13,000 rpm. 10) Carefully pour off the supernatant, and use a 10- 100 microliter pipetter to remove the remaining residual 70% EtOH at the bottom of the tube. Be careful to pipet from the side opposite the DNA pellet (i.e., opposite the tube hinge), which may or may not be visible. Place the tube upside down on Kim-Wipe, and leave this on your bench for 20 min. 11) Resuspend the Genomic DNA by slowly washing the side of the eppendorf tube with 50 microliters of TE Buffer (10 mM Tris, 1 mM EDTA at pH 8.0). Have faith that your DNA is there, because you probably won’t see it. This DNA suspension is will be used as template for amplification of the 16SrRNA gene via PCR (polymerase chain reaction). PCR Amplification of the 16SrRNA Gene: << Ex 27 - Day 2 >> Materials: PCR tubes Genomic DNA Reaction Master Mix (see below) Procedure: IMPORTANT NOTE: Because you are amplifying bacterial DNA, there is a need for extremely sterile technique (both lab space and handling). Wear gloves, use only sterile pipetter, keep eppendorf lids closed as much as possible, and NEVER use a pipetter tip more than once for any solution transfer! 1) Label a sterile PCR tube for each genomic DNA sample in your group. 2) Add 48 micrliters of PCR Master Mix to the tube; this represents the following: 39 microliters of sterile deionized H2O 5 microliters of 10X PCR Buffer 1 microliters of 10 mM dNTP (mix of 4 nucleotides) 1 microliters of “68F forward primer” (~100 ng) 1 microliters of “1406R reverse primer” (~100 ng) 0.5 microliters of Tth Polymerase 3) Add 2 microliters of template (genomic) DNA. With a new pipette tip on your 10-100 microliter pipetter, slowly pipett the 50 microliters of PCR reaction “cocktail” up and down to thoroughly mix reagents. 4) Place it in the “PCR machine” (technically caller a thermocycler). 5) The temperature program used (pre-set for you) is as follows: MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen a) 94 C for 1 min (denatures double stranded DNA template); b) 60 C for 1 min (cooling permits the selective annealing of primers with target sequences of the template DNA); c) 72 C 4 min (activates the Tth Polymerase to polymerize, proceeding from the 3’ end of the annealed primers, a DNA strand complimentary to the template strand.) 10 d) Return to step “a”. Repeat the cycle 30 times, after which the temperature is maintain at 4 C Next time we meet, we will digest the amplified PCR product with a selection of tetrameric restriction endonucleases and separate the digested fragments by size via agarose gel electrophoresis. Restriction Enzyme Digestion of PCR Amplicon: << Ex 27 - Day 3 >> This period we will continue with the molecular identification of our unknown bacterium by use of molecular techniques, specifically the restriction fragment length polymorphism (RFLP) pattern of the PCR amplified 16S rRNA, our amplicon. First, digest your amplicon with tetrameric restriction endonucleases (i.e., restriction enzymes with 4bp recognition sites). Materials: PCR tubes Sterile DI-water PCR reaction for amplicons DNA Selected restriction enzymes and their respective buffers 10x Glycerol Loading Buffer Procedure: 1. Label a 2 new 0.5 microliter eppendorf tube, one for each of 2 restriction enzymes used (details will be provided). Add in order the following to each tube: 12 microliters of sterile dH2O. 2 microliters of 10X restriction enzyme buffer. 4 microliters of precipitated PCR product. 2 microliters of the appropriate restriction enzyme. 2. Mix the contents of the tubes by slowly pipetting up and down and place the tubes into the 37C heating bloack (or thermocycler) for 30 min. Periodically give the tubes a mix and return them to the heating block. 3. After the reactions have been incubated, remove them from the heating block and add 2 microliters of 10x Glycerol-Loading Buffer (GLB) to each tube. 4. An undigested sample of PCR product will need to be prepared for running on the agarose gel along side of the digests. To a new eppendorf tube add the following: MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 11 2 microliters PCR product. 7 microliters sterile dH2O. 1 microliters of 10x GLB. Agarose Gel Electrophoresis to Determine RFLP pattern: << << Ex 27 - Day 3 >>> Materials: 3% agarose gel with Ethidium Bromide (EtBr) staining solution incorporated 0.5x TAE electrophoresis buffer Horizontal electrophoresis apparatus and power supply UV light Transluminator and photo-documentation equipment Marker DNA. Procedure: 1. You will share a 3% agarose gel and horizontal gel apparatus with other groups. Therefore, all samples and standard marker DNA need to be loaded within a reasonable time frame to avoid diffusive loss from the wells. 2. Draw your entire sample into the tip of a pipetter, but do not create an air space between the tip point and the sample within the tip. If you have an air bubble there, it will dislodge your sample out of the well as you attempt to load. 3. Keep your pipetter tilted at an angle so you can view what is going on during loading sample into the gel well. Lower the pipette tip to just inside the side of the next empty well. 4. Slowly expel the tip contents. It will sink to the bottom of the well due to the density of the sucrose-loading buffer. Make sure not to introduce any air bubbles as the last bit of sample leaves the pipette tip. I usually sacrifice the last microliter of sample to avoid bubbles and sample loss. Certainly, never push the pipettes plunger to its second stop when loading gels. 5. When all samples have been loaded, close the cover and insert the electrodes, matching black-withblack and red-with-red. Turn on the voltage. We will run at 50 Volts for 1 hour in 0.5X Tris Acetate EDTA (TAE) Buffer. We have already added Ethidium Bromide (1 ug/ml) to the gel during its casting. 6. After electrophoresis , remove the gel and photo-document while trans-illuminating with UV light. Each student will receive a picture of their gel. It will look similar to that in Figure 27.3. 7. Compare your results to the known database provided by the instructor. 12 3b p 12 Cf oI Rs aI Hp aII 12 3b p Ha eII I MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 492 369 246 123 Figure 27.3. Restriction fragment length polymorphism for a 1338 bp PCR for the E. coli 16SrRNA. Lanes 2, 3, 4, and 5 are restriction enzymes digests using HaeIII, HpaII, CfoI, and RsaI, respectively. Lanes 1 and 6 are molecular size markers. 25.1 Enterotube II Multiple Test System: (Ex 28) The Enterotube II miniaturized multitest system is supplied by Becton-Dickinson of Cockeysville, Maryland, for rapid identification of Enterobacteriaceae. It incorporates twelve different conventional media and fifteen biochemical tests into a single ready-to-use tube that can be simultaneously inoculated in a moment's time with a minimum of equipment. If you have an unknown gram-negative rod or coccobacillus that appears to be one of the Enterobacteriaceae, you may wish to try this system on it. Before applying this test, however, make certain that your unknown is oxidasenegative, since very few of the Enterobacteriaceae are oxidase-positive. Each of the 12 compartments of an Enterotube II contains a different agar-based medium. Compartments that require aerobic conditions have openings for access to air. Those compartments that require anaerobic conditions have layers of paraffin wax over the media. Extending through all compartments of the entire tube is an inoculating wire. To inoculate the media, one simply picks up some organisms on the end of the wire and pulls the wire through each of the chambers in a single, rotating action (Figure 28.1) After incubation, the indole and Voges-Proskauer tests must be performed, and the reactions in all compartments are noted (Figure 30.2). Positive reactions are given numerical values which are totaled to arrive at a five-digit code (Figure 30.1). Identification of the unknown is achieved by consulting a booklet, the Enterotube II Interpretation Guide, which lists these numerical codes for the Enterobacteriaceae. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen Figure 28.1. Enterotube II inoculation and analysis protocol. 13 MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 14 Exercise 28 Enterotube II: Materials: Culture plates of 2 unknowns. Enterotube II for each of two unknowns. Kovacs' reagent for indole test. V-P reagents: 10% KOH with 0.3% creatine solution 5% alpha-naphthol in absolute ethyl alcohol disposable Pasteur pipettes test-tube rack Procedure: (Figure 28.1) 1. Write your initials or unknown number on the white paper label on the side of the tube above V-P. 2. Unscrew both caps from the Enterotube II. 3. Without heat-sterilizing the exposed inoculating wire, insert it into a well-isolated colony. 4. Inoculate each chamber by first twisting the wire and then withdrawing it through all 12 compartments. Rotate the wire as you pull it through. Again, without sterilizing, reinsert the wire, and with a turning motion, force it back through all 12 compartments. 6. Withdraw the wire again until the tip is in the H2S/indole compartment. At this point, break the wire by bending and discard the handle end of the wire. A notch in the wire makes this relatively easy. Leaving the wire in the last three chambers excludes oxygen from the three paraffin covered chambers ( GLU-GAS, LYS, ORN). The fermentation of glucose and the decarboxylation of lysine and ornithine occur anaerobically. The small portion of wire protruding into the H2S/indole compartment will not interfere with these two tests. 7. Replace the caps at both ends. 8. To expose some small holes in the sides of eight of the compartments, strip off the blue plastic strip. If no blue plastic strip is present, the punch holes using the sterile wire. These holes provide aerobic conditions for the following compartments: ADON, LAC, ARAB, SORB, V-P, DUL-PA, UREA, and CIT. 9. Incubate at 30° to 37° C for 18 to 24 hours with the Enterotube II lying on its flat surface. When incubating several tubes together, allow space between them to allow for air circulation. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 15 << Ex 28 - Day 2 >> 10. Record results as positive or negative (Figure 28.2) for all reactions, except the V-P and Indole. 11. Add Kovac’s reagent for indole production, record result. 12. Add reagents for V-P reaction, record results. 13. Interpret the results as indicated by the instructor. This may involve computation of code numbers and comparison to a known database, or by more conventional mean, by comparing each test result to tabular data for various Enterobacteriaceae. 14. Address all questions and discussion points presented at the end of Exercise #28. Figure 28.2. Description of Enterotube II reaction compartment tests, and appearance of negative and positive results for each test. MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen Figure 28.2 (Continued). 16 MICRB 202: Introductory Microbiology Lab Unit IX: Identification of a Gram-Negative Intestinal Pathogen 17 Results Assignment and Discussion: 1) Create a standard curve of log marker band size versus migration distance, and provide the equation for this curve and the r2 value for the linear regression. Use this equation to determine the size of each band in your digested sample. 2) Use the undigested sample to confirm the presence of target PCR product (~1340 bp) and any non-specific PCR product(s). Also, use the information from the undigested sample to determine any undigested or extra non-specific DNA bands in your 2 digested samples. Report any aberrant results and discuss possible sources. 3) Use your RFLP data and the RFLP data for known bacterial species (provided by the instructor) to propose the identity of your unknown. 4) How does this approach compare with phenetic approaches used in Exercises 26 & 28. Which would you use, under what circumstances, and why? 5) How might the phenetic and molecular (phyletic) approaches compliment each other in learning about a newly isolated bacterium for which there is no known species?