File
advertisement

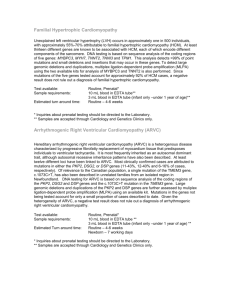
HYPERTROPHIC OBSTRUCTIVE CARDIOMYOPATHY Cahill Expressway, oil on canvas, Jeffrey Smart, 1962, National Gallery Victoria Australia Collins St, 5p.m. oil on canvas, John Brack 1955, National Gallery Victoria, Australia. They paved paradise And put up a parking lot With a pink hotel, a boutique And a swinging hot spot Don’t it always seem to go That you don’t know what you’ve got ‘Til it’s gone They paved paradise And put up a parking lot They took all the trees And put them in a tree museum Then they charged the people A dollar and a half just to see ‘em Don’t it always seem to go, That you don’t know what you’ve got ‘Til it’s gone They paved paradise And put up a parking lot Hey farmer, farmer Put away that DDT now Give me spots on my apples But leave me the birds and the bees Please! That you don’t know what you’ve got ‘Til its gone They paved paradise And put up a parking lot Late last night I heard the screen door slam And a big yellow taxi Come and took away my old man Don’t it always seem to go That you don’t know what you’ve got ‘Til it’s gone They paved paradise And put up a parking lot I said Don’t it always seem to go That you don’t know what you’ve got ‘Til it’s gone They paved paradise And put up a parking lot They paved paradise And put up a parking lot They paved paradise And put up a parking lot Don’t it always seem to go Big Yellow Taxi, Joni Mitchell, 1970. “I wrote “Big Yellow Taxi” on my first trip to Hawaii. I took a taxi to the hotel and when I woke up the next morning, I threw back the curtains and saw these beautiful green mountains in the distance. Then, I looked down and there was a parking lot as far as the eye could see, and it broke my heart... this blight on paradise. That’s when I sat down and wrote the song”. Joni Mitchell Jeffrey Smart’s “Cahill Expressway” and John Brack’s “Collins St, 5p.m”, brilliantly depict the sterility of modern day big city living. The figures are totally divorced from the natural environment, in the case of Brack, they are even divorced from each other, unseeing, without interaction, automatons that are seemingly oblivious to all around them, apart from their own immediate mundane “9-5” concerns. In Smart’s work the lone figure stares back at us, from a lifeless world, not even one tree is seen. These images show us the soulless environment that humanity has created for itself. A lone tree is seen in Brack’s work, in Smart’s there is no natural environment at all, it has been completely replaced by concrete and steel, there is not even a single bird in the sky. In the 1950s there was no awareness at all of the danger that humans had put our environment into. In Smart’s work we do see that in some way, our cities, great as they were, did not seem “quite right”…something was missing, but it wasn’t sure just exactly what this was. In the 1960s only the barest glimmer of insight began to emerge. Brack’s work shows us how this soullessness has even extended to the way in which people interacted with each other…they did not! It was not until the 1970s that humanity seemed to have developed the faintest awareness of the destruction of the planet that “civilization” was causing. Then a seemingly inconsequential little “ditty” by Joni Mitchell in 1970 suddenly sky rocketed the popular awareness, a ditty that has now become a cultural icon of the modern conservation movement. What makes a work of art “great” is not always the scale, or the technical brilliance of it, but rather the ability to change the way in which people see things. In this sense Mitchell’s song can in fact be considered “great”. It took a young 27 year old Canadian female singer to look out of her hotel room in Hawaii one morning, to articulate to the world, what Smart and Brack had hinted at decades before…“Don’t it always seem to go, That you don’t know what you’ve got till its gone!” In the medical field Joni Mitchell’s words, ring truer than even she imagined that morning in Hawaii in 1970. Young people have a sense of invulnerability, immortality even. Mitchell’s phrase, “you don’t know what you’ve got till it’s gone” rings truest when it comes to life itself, especially to a young life not yet lived! The number one cause of sudden cardiac death in young people, especially in the case of seemingly invulnerable young athletes, is hypertrophic cardiomyopathy. It is for this reason that any young patient has who has an unexplained syncopal episode must have an ECG to look for any tell tales signs of hypertrophic cardiomyopathy or indeed any other cardiac abnormality. HYPERTROPHIC OBSTRUCTIVE CARDIOMYOPATHY Introduction Hypertrophic Obstructive Cardiomyopathy (HOCM) is a genetically inherited condition characterized by abnormal hypertrophy of the left ventricular or right ventricular outflow tract or both. HOCM has also been called IHSS (idiopathic hypertrophic sub-aortic stenosis) in the past, but this term is now obsolete, (as hypertrophy can occur in any region of the left ventricle The major pathology involves a dynamic obstruction of the ventricular outflow tract late in systole. Management consists of medical and surgical strategies to relieve this dynamic outflow tract obstruction, as well as controlling secondary complications such as arrhythmias and heart failure. It is an important condition to recognize, as it is one of the causes of sudden cardiac death in the young. It is the most common cause of sudden death among young athletes. Epidemiology The overall prevalence of HOCM is low and has been estimated to occur in about 0.05-0.2% of the population The average age at diagnosis is about 30-40 years. Pathology Genetics Hypertrophic Obstructive cardiomyopathy is usually inherited as an autosomal dominant trait with variable penetrance. The defect appears to involve genes that encode for certain protein components of the cardiac sarcomere. Mechanical consequences of HOCM Hypertrophic Obstructive Cardiomyopathy (HOCM) is a genetically inherited condition characterized by abnormal hypertrophy of the left ventricular (or right ventricular outflow tract or both). The region of hypertrophy is usually the inter-ventricular septum. The ventricular hypertrophy occurs in the absence of ventricular dilation. The major pathology involves obstruction of the ventricular outflow tract late in systole, when the hypertrophied region contracts. Dynamic systolic outflow tract obstruction occurs as a result of two factors: ● Obstruction by the hypertrophied segment of the septal wall of the ventricle. ● Systolic displacement of the mitral valve leaflets into the left ventricular outflow tract. This abnormal movement of the mitral valve, also results in a degree of mitral valve regurgitation. Some patients have labile obstruction that is absent at rest but provoked with changes in preload, afterload, and contractility. Thus, symptoms may become manifest only when certain drugs (e.g., vasodilator or diuretic agents) are given or when hypovolemia occurs. In other patients, the obstruction is present at rest, with its magnitude dependent on loading conditions. Transverse section of heart through a pathologic specimen of a case of hypertrophic obstructive cardiomyopathy. Complications of HOCM 1. 2. Sudden cardiac death: ● Lethal arrhythmias, (VT/ VF) ● Severe acute outflow tract obstruction. Other arrhythmias: ● AF, Atrial flutter, ectopy 3. Syncope 4. Endocarditis. 5. Heart failure, (uncommon): ● This can be from mitral regurgitation, or diastolic heart failure, systolic failure occurs late Clinical Features Symptoms 1. Sudden death: ● 2. Syncope: ● 3. Unfortunately sudden cardiac death in a young person may be the first indication that the patient had the condition. Unexplained syncope in a young person, particularly an athlete. Angina ● Often on exertion. This may occur in the absence of detectable coronary atherosclerosis and is related to impaired diastolic relaxation and markedly increased myocardial oxygen consumption caused by ventricular hypertrophy that results in subendocardial ischemia. 4. Palpitations ● 5. Often on exertion Dyspnea ● Often on exertion Signs The classically described clinical signs suggestive of HOCM include: 1. Pulse ● This may be sharp rising and “bifid”, (or sometimes described merely as “jerky”. This feature is a result of rapid ejection by the hypertrophied ventricle early in systole which is followed by obstruction of the outflow tract in late systole. The nature of this pulse, to an experienced cardiologist, is quite different from the pulse of aortic stenosis, (it is said). 2. Blood pressure: ● 3. JVP: Blood pressure is not usually significantly altered. ● There may be a prominent “a” wave, (to an experienced observer). This is due to forceful atrial contraction of the atrium against a noncompliant right ventricle. 4. Apex Beat: ● The apex beat may be felt as a double or triple impulse. This is said to be due to a pre-systolic expansion of the ventricle caused by atrial contraction. 5. Heart sounds: ● 6. An S4 may be present Murmur: There may be a late systolic murmur, which can be altered by certain “dynamic manoeuvres”. It is typically heard best at the lower left sternal edge and apex. Mitral regurgitation may also produce a pan-systolic murmur, at the apex. The murmur is made louder by manoeuvres that decrease the preload: ● Valsalva ● Standing ● Isotonic exercise. (Note that reducing the preload will make the much more common murmur of aortic stenosis, softer). The murmur is made softer by manoeuvres that increase the preload or increase the afterload: ● Leg raising, or squatting, (increasing the preload). ● Handgrip, (isometric exercise, that increases the afterload) (Note that increasing the preload will make the much more common murmur of aortic stenosis louder, whilst increasing the afterload will make the murmur of aortic stenosis softer). Risk Factors for Sudden Death in Patients with Hypertrophic Cardiomyopathy 1 The overall mortality among patients with hypertrophic cardiomyopathy is less than 1 percent per year. However, a subgroup of patients is at high risk for sudden death, primarily as a result of ventricular arrhythmias. Risk factors can be stratified into major and minor. These include: Major risk factors: ● Cardiac arrest (ventricular fibrillation) ● Spontaneous sustained ventricular tachycardia ● Family history of sudden death Minor risk factors: ● Unexplained syncope ● Left ventricular wall thickness >30 mm ● Abnormal blood pressure on exercise ● Nonsustained ventricular tachycardia ● Left ventricular outflow obstruction ● Microvascular obstruction, (as demonstrated by nuclear medicine scans or MRI) ● High-risk genetic defect Investigations Blood tests These may be required to rule out alternative diagnoses or secondary complications in patients who present to the ED. Investigations undertaken in other words will depend on the nature of the presenting complaint. Consider: 1. FBE 2. U&Es/ glucose 3. Mg/ Ca, (if arrhythmias present) 4. Troponin I CXR As the ventricular hypertrophy in HOCM occurs in the absence of ventricular dilation, the cardiac silhouette will usually be normal. A CXR is done predominantly to rule out other differential diagnoses or to help document the presence of secondary heart failure. ECG The ECG may be normal Otherwise findings may include: ● Changes of LV hypertrophy. ● ST-T wave abnormalities ● Left axis deviation, (though right axis deviation may also be seen). ● Conduction abnormalities (P-R prolongation, bundle-branch block) ● Arrhythmias, usually AF or more seriously VT/ VF. ● Prominent (typically deep, but narrow) Q waves in the inferior or lateral limb leads, (I, AVL, V5-6). This is a relatively specific sign of HOCM ● P-wave abnormalities, including signs of left atrial enlargement. ● Tall R waves in V1 ECG of a 30 year old patient who presented with near syncope and palpitations. He had HOCM. Note the prominent q waves in the lateral leads, (I, AVL, V4-6). Echocardiography Although much is made of the large array of supposed clinical signs of HOCM in traditional medical student textbooks, the method of definitive diagnosis in the 21st century is of course echocardiography. Left shows a two dimensional echocardiogram from a Patient with Severe Symptomatic HOCM. 1 Panel A shows a still frame obtained during diastole. There is a marked increase in the thickness of the ventricular septum (VS). Panel B shows a still frame obtained during systole. Systolic anterior motion of the mitral-valve apparatus causes obstruction of the left ventricular (LV) outflow tract (arrow). Ao denotes aorta, LA left atrium, and PW posterior wall. In patients with no obstruction or only slight obstruction (gradient, ≤30 mm Hg), provocative manoeuvres (such as the Valsalva manoeuvre or exercise) should be performed to identify latent obstruction. Management Treatment of patients with HOCM, aims to control symptoms and to prevent sudden death. 1. Medical therapy: Prevention of dynamic outflow obstruction is undertaken with: ● Beta blockers, (generally first line) ● Calcium channel blockers. These agents also slow the heart rate and so will allow for greater diastolic filling time. 2. ICD implantation: ● 3. Patients who are considered to be at high risk of sudden cardiac death, are considered for implantation of an automatic defibrillator device. Surgical therapy: ● If the resting gradient is greater than 30 mm Hg (or the provocable gradient is greater than 50 mm Hg) and if the patient continues to have symptoms of dyspnea or angina that limit daily activity, despite medical therapy, then septal myectomy may be considered. ● Long-term follow-up (over periods of more than 30 years) has shown that patients who have undergone septal myectomy have long-lasting improvements in symptoms and exercise capacity and no recurrence of outflow tract obstruction. See appendix 1 below. 4. 5. Dual chamber cardiac pacing: ● This may be considered in some patients to improve cardiac output by altering the electrical dynamics of ventricular depolarization. ● It has limited effectives however and is currently limited to patients who have coexisting illnesses that are contraindications to other therapies or those who require pacing for bradycardia. Chemical septal infarction: ● This has also been used in some patients with better effectiveness than dual chamber pacemakers. ● It involves the selective catheterization of a segmental septal artery supplying the hypertrophied segment of the septum. This segment is then infarcted by the injection of ethanol. The resulting decrease in septal thickness reduces or even eliminates the intraventricular obstruction. ● The technique is much less invasive, than open heart surgery, but requires great skill to perform. See appendix 2 below. 6. Screening of first degree relatives: ● All first-degree family members should undergo periodic screening with echocardiography. ● In the future, genetic screening of first degree relatives may also be considered. This is not currently done routinely Appendix 1 Septal myectomy Diagram showing the technique of septal myectomy. The procedure not only removes the mechanical septal obstruction it also corrects the abnormal anterior systolic motion of the mitral valve and so abolishes the associated mitral regurgitation as well as the contribution of the abnormal mitral valve movement to dynamic obstruction. 1 Appendix 2 Segmental septal artery infarction Illustration showing the technique of balloon occlusion of a septal coronary artery and alcohol-induced segmental septal infarction, (NEJM October 24, 2002). Joni Mitchell, c. 1970 References 1. Nishimura R.A Hypertrophic Obstructive Cardiomyopathy. NEJM, 350 (13) March 25, 2004, p. 1320-1327. 2. Talley N.J, O’Conner S. Clinical Examination, 3rd ed 1996, p. 79-80. Dr J. Hayes 18 September 2009