Volume 13 (Number 3) - The Ethiopian Journal of Health Development
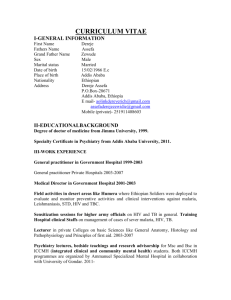
advertisement

Original article Diarrhoea-associated parasitic infectious agents in AIDS patients within selected Addis Ababa Hospitals Bitew Fisseha1, Beyene Petros2, Tilahun Woldemichael 1, Hussien Mohammed 1 Abstract: The aim of the study was to determine the prevalence of gastrointestinal parasites in Acquired Immunodeficiency Syndrome (AIDS) patients with chronic diarrhea. This prevalence was compared with two control groups: Human Immunodeficiency Virus (HIV) seronegative diarrheal patients and HIV seropositive individuals without diarrhoea. Stool specimens from clinically diagnosed hospitalized AIDS patients in some hospitals in Addis Ababa were screened for parasite infection. Of 147 AIDS patients with chronic diarrhoea, 74 (50.3%) were infected with one kind or more of parasites. Out of 56 non-AIDS (seronegative) diarrhoeal patients, 41.1% (23/56) and out of the 43 non-diarrhoeal (seropositive) patients, 41.9% (18/43) were infected by a variety of intestinal protozoa and helminths. The parasites detected in AIDS patients were Cryptosporidium spp, Isospora spp, Blastocystis spp, Ascaris lumbricoides, Giardia lamblia, Strongyloides stercoralis, Taenia spp, Trichuris trichiura, Entamoeba histolytica, and Hook worm spp. Among the intestinal parasites, Cryptosporidium spp was exclusively associated with AIDS patients. The high proportion of the study subjects who had diarrhoea in the absence of identifiable parasitic infections suggests that other infectious agents (eg. Bacteria and Virus) or mechanisms other than infectious agents, are responsible for the diarrhoea. [Ethiop. J. Health Dev. 1999;13(3):169-173] Introduction Diarrhoea is the clinical manifestation of HIV-1 infection in both developing and developed countries. In tropical countries chronic diarrhoea associated with weight loss (“slim disease”) is often the presenting illness of HIV-1 infected individuals (1). This diarrhoea-wasting syndrome in association with a positive HIV-1 serology test is an AIDS-defining illness in the World Health Organization’s classification (2,3). The acquired immunodeficiency syndrome (AIDS) caused by human immunodeficiency virus (HIV) infection predisposes to several parasitic diseases such as Pneumocystis carnii pneumonia and Toxoplasma encephalitis. Among intestinal parasites, the intracellular coccidia, Isospora belli, and Cryptosporidium parvum are clearly opportunistic (4). The microsporidian Enterocytozoon bieneusi may also be a significant enteric pathogen (5). Investigations for intestinal parasitic infections in AIDS patients in Africa has focused on patients with diarrhoea. Isospora and Crypotosporidium have been found consistently in such patients at prevalence rates varying from 8% to 32% and 12% to 19%, respectively, among patients with chronic diarrhoea (1,6,7,14). In nearly all studies, opportunistic infections were more common than the more commonly encountered parasitic protozoa and helminths which are probably more prevalent in the general community (17). Most of the clinical manifestations of HIV-1 infections result either from the reactivation of preexisting latent pathogens or exposure to locally predominant pathogens. Consequently, clinical presentations of AIDS and the pathogens responsible in different geographical areas reflect the differing prevalence of endogenous infections. On the other hand, some reports ______________________________________ 1 Ethiopian Health and Nutrition Research Institute, P.O. Box 1242, Addis Ababa, Ethiopia; 2Dept. of Biology, Addis Ababa University, Addis Ababa, Ethiopia indicate that there is no convincing evidence on the etiological agents isolated from African AIDS 170 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── patients with diarrhoea that their prevalence or incidence is increasing due to the HIV epidemic (15). Patterns in developing countries, where hygiene is poor and intercurrent infection rates are high, differ in several important ways from patients in the industrialized countries. The commonest presentation of AIDS in Africa is ‘slim disease’ or enteropathic AIDS, which is characterized by severe loss of weight and chronic watery diarrhoea and prolonged fever (9,16,17). The role of HIV in diarrhoea, malabsorption, and other gastrointestinal disorders has been elucidated (8). However, the presence of the virus in bowel mucosa of individuals with symptoms and no known pathogen suggests that HIV could give rise to this disorder. In particular, HIV infection of neuroendocrine cells (eg. Enterocromiffin cells) could result in disorders of intestinal motility and function (8,9,16). Intestinal nematodes, amoebae, and other protozoa have not been shown to be opportunistic in AIDS patients. There is no convincing evidence to show that, for parasitic diarrhoeal infections, their prevalence or incidence is increasing due to the HIV epidemic (13,15). For reasons which are unclear, parasites such as S. stercoralis and E. histolytica, where cell-mediated immune response is thought to be significant, do not appear to be opportunist infections (13). Although strongloidiasis and AIDS often coexist in regions of endemicity such as Central Africa, only few cases of disseminated disease in people infected with HIV have been reported (10-13). The aim of this study was to determine the prevalence of gastrointestinal parasitic agents in AIDS patients with chronic diarrhoea. Methods The study was conducted between January 1995 and May 1996. The sample size for the study was computed by considering a 95% level of confidence, 80% power and an expected ratio of 1:3 (Not ill/ill). Two hundred forty six stool samples were examined in this study, 147 from AIDS patients with chronic diarrhoea, 56 from HIV seronegative diarrhoeal patients (control group I) and 43 from HIV seropositives without diarrhoea (control group II). During the study period, patients (cases, control groups I and II) visiting the study sites were included until the required sample size was reached. A questionnaire relating to the history and clinical status was completed for each subject included in the study by the AIDS coordinator physicians and trained counselors in hospitals where this study was conducted. Statistical analysis was performed using EPI-INFO software to test differences between the cases and the two control groups. In the hospital laboratories, 10 ml of venous blood was taken from each patient using a vacuum system. Serological testing for HIV-1 antibodies was done with the Vironostika Uniform II (Organon Teknika, Holland). Reactive sera were retested using Wellcozyme ELISA (Murex, UK) (18,19) in the National Referral Laboratory for AIDS (NRLA) which is located at the Ethiopian Health and Nutrition Research Institute (EHNRI). Stool specimens were collected fresh and processed in the clinical parasitology laboratory of the EHNRI within four hours of collection. Parasite detection was made by examination of stool specimens by the following methods: fresh hospital specimens were first examined as wet mounts using normal saline followed by Formal-ether concentration (1). Air-dried thin smears were stained by modified Ziehl-Neelsen technique (20) for Cryptosporidium and Isospora oocysts. The smears were fixed in methanol for three minutes, stained with carbol fuschin for 60 minutes, decolorized in 2% H2SO4 for one minute, washed in running tap water, counter-stained with 5% malachite green for five minutes, washed in running tap water, and air dried. The thin-walled oocysts stain an intense red and are easily recognized against the green background under high power or oil immersion for detailed visualization. Results The age profile of the study and control subjects is similar to the HIV/AIDS profile in the general population reported by the Ministry of Health (21) and the normal population pattern reported by the Central Statistical Authority (22), where both young and older individuals are represented in the Diarrhoea associated parasitic infections and AIDS 171 ──────────────────────────────────────────────────────────── sample (Table 1). Table 1: Age and gender distribution of the study population (cases) and the control groups (controls I and II), in selected Addis Ababa hospitals, 1995/96. Age (year) Sex Cases Control I Control II No. (%) No. (%) No. (%) 15-24 M 7(4.8) 5(8.9) 5(11.6) F 9(6.1) 5(8.9) 3(7.0) 25-34 M 62(42.2) 20(35.7) 16(37.2) F 26(17.9) 12(21.4) 8(18.6) 35-44 M 21(14.3) 7(12.5) 4(9.3) F 7(4.8) 3(5.4) 2(4.7) >45 M 12(8.2) 3(5.4) 4(9.3) F 2(1.4) 1(1.8) 1(2.3) Total 47(100) 56(100) 43(100) Oocysts of Cryptosporidium species were isolated from 38/147 (25.9%) AIDS patients with chronic diarrhoea. In addition, among the opportunistic parasites frequently associated with AIDS, 2/147(1.4%) Isospora belli and 1/147 (0.7%) Blastocystis species were found in 74/147 (50.3%) of the AIDS patients with chronic diarrhoea (Table 2). The only parasite clearly more prevalent in AIDS patients was Cryptosporidium (P<0.001), although Isospora and Blastocystis were also found only in AIDS patients. Parasites were identified in 74 out of 147 (50.3%) AIDS patients with chronic diarrhoea, and in 18 out of 43 (41.9%) who did not suffer from diarrhoea. Chronic diarrhoea occurred in all 38 patients with cyptosporidiasis which was the only infection clearly associated with this symptom. The parasites detected in stools of all AIDS hospital patients with diarrhoeal consisted of A. Lumbricoides (11.8%), E. histolytica (8.2%), G. lamblia (4.1%), S. stercoralis (3.4%), Taenia spp (3.4%) and T. trichiura (7.5%). These common parasites often occurred as multiple infections (Table 3). Table 2: Parasite species identified in AIDS patients with chronic diarrhoea (cases), HIV negative diarrhoeal patients (control I) and HIV seropositive individuals without diarrhoea (control II). Parasite species Cryptosporidium spp A. lumbricoides S. stercoralis G. lamblia Isospora belli T. trichiura E. histolytica Taenia spp Blastocystis spp S. mansoni Hook worm spp Total infected ** : P<0.001 Cases(N = 147) n (%) 38(25.9)** 17(11.8) 5(3.4) 6(4.1) 2(1.4) 11(7.5) 12(8.2) 4(3.4) 1(0.7) 0 0 74(50.3) Control I (N = 56) n (%) 0 12(21.4) 1(1.8) 2(3.6) 0 7(12.5) 3(5.4) 2(3.6) 0 1(1.8) 2(1.8) 23(41.1) Control II(N = 43) n (%) 0 7(16.3) 0 2(4.6) 1(2.4) 6(14.0) 3(7.0) 3(7.0) 1(2.4) 1(2.4) 2(4.6) 18(41.9) 172 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Table 3: Prevalence of single and multiple parasitic infections in AIDS patients with diarrhoea and the control groups in selected hospitals in Addis Ababa, 1995/96. Subjects Parasites detected in the study subjects One No. (%) Two No. (%) Three No. Four No. (%) (%) AIDS patients 54(73.0) 15(20.3) 4(5.4) 1(1.4) (n = 74) Control group I 16(69.6) 7(30.4) 0 0 (n = 23) Control group II (n 10(55.6) 8(44.4) 0 0 = 18) Discussion These findings suggest that patients with AIDS do not have more intestinal parasite infections than the control groups. Only Crytosporidium, a recognized opportunistic pathogen was more prevalent in the AIDS group in which it was strongly associated with chronic diarrhoea. Associations between AIDS, other parasite infections, and chronic diarrhoea were not evident. Of course, there are other important causes of diarrhoea, such as viral, bacterial and microsporidian infections, for which this study was not designed. Diagnosed cases of I. belli were considerably fewer in this study than reported in Zaire (7%), Uganda (13%), and Zambia (16%), which could possibly be either due to more sensitive detection methods or a reflection of low prevalence in this study population (23). In addition Blastocystis species, which has been reported as a causative agent of diarrhoea in a number of cases in patients with AIDS, was detected in one case of AIDS with diarrhoea and in an HIV seropositive individual, but none in HIV seronegative patients with Diarrhoea(24). The finding suggests that Blastocystis species may be associated with HIV infection and AIDS. Therefore, it will be necessary to conduct further studies to determine the importance of this parasite in relation to HIV/AIDS in Ethiopia. Our findings tend to support the view that the more ‘common’ parasites (Ascaris, Strongyloides, G.lamblia, T. trichiura, Taenia and E.histolytica) are not opportunistic in AIDS patients (13). Identification of these common parasites in up to 12-21% of AIDS patients and the controls is a reflection of poor environmental hygiene. The high proportion of AIDS patients who had diarrhoea in the absence of identified parasite infections strongly indicates the existence of other diarrheaogenic agents or mechanisms. The detection of these will require more comprehensive and better controlled studies. In conclusion, diarrhoeal illnesses remain a major clinical problem for patients infected with HIV-1, particularly those with AIDS. Opportunistic enteric pathogens, for which there is no effective treatment, the emergence of new opportunistic infections, and the enlarging pattern of drug resistance continues to be a challenging task. However, better understanding of HIV-1-induced mucosal immunosuppression, sound clinical management, careful diagnostic evaluation, development of newer antimicrobial agents, and judicious patient management should help meeting this challenge and can be necessary in attempting to improve the quality of life. References 1. Colebunders R, et al. Persistent diarrhoea in Zairian AIDS patients: an endoscopic and histologic study. Gut. 1990;29:687-1691. 2. WHO. Provisional WHO clinical case definition for AIDS. Weekly Epidemiological Record. 1986;10(72):303-306. 3. Widely-Wirski R, et. al. Evaluation of the WHO clinical case definition for AIDS in Uganda. J Amer Med Ass. 1988;260:286-3289. 4. Fleming AF. Opportunistic infections in AIDS in developed and developing countries. Trans Roy Trop Med Hyg. 1990;84:supl 1,1-5. 5. Canning EV and Hollister WS. Enterocytozoon beineusi (Microspora): prevalence and pathogenicity in AIDS patients. Trans Roy Soc Trop Med Hyg. 1990;84:181-186. 6. Henry MC, et al. Parasitological observations of chronic diarrhoea in suspected adult AIDS patients in Kinshasa (Zaire). Trans Roy Soc Trop Med Hyg. 1986;80:309-310. 7. Colon CP, et al. HIV-related enteropathy in Zambia: a clinical, microbiological, and histological study. Amer J Trop Med Hyg. 1990;42:83-88. 8. Pape JW et al. The acquired immunodeficiency syndrome in Haiti. Annals of Internal Medicine. 1985;103:674-678. 9. Serwada D, et al. Slim disease: a new disease in Uganda and its association with HLTV-III infection. Lancet. 1985;ii:849-852. 10. Petithory JC and Derouin F. AIDS and strongyloidiasis in Africa. Lancet. 1987;1:921. 11. Gompels MN, et al. Disseminated strongyloidiasis in AIDS: uncommon but important. AIDS. 1991;5:329-332. 12. Torres JR, et al. Efficacy of ivermectin in the treatment of strongyloidiasis complicating AIDS. Clinical Infectious Diseases. 1993;17:900-902. 13. Lucas SB. Missing infection in AIDS. Trans Roy Soc Trop Med Hyg. 1990;84:suppl 1, 34-38. 14. Hunter L, et al. Intestinal parasites in Zambian patients with AIDS. Trans Roy Soc Trop Med Hyg. 1992;86:543-545. 15. Khumalo-Ngwenya A, et al. Gut parasites in HIV-seropositive Zambian adults with diarrhoea. East African Med J. 1994;6:379-382. 16. Mhiri C, et al. The slim disease in African patients with AIDS. Trans Roy Soc Trop Med Hyg. 1992;86:303-306. 17. Smith PD. Infectious diarrhoea in patients with AIDS. Gastroenterology clinics of North America. 1993;22(3):535-548. 18. World Health Organization and United Nations Joint Program on HIV/AIDS: Revised recommendations for the selection and use of HIV antibody tests. WHO Wkly Epidemiol. 1997;72:81-87. 19. Nkengasong J et al. HIV screening and confirmation: A simple and less expensive testing algorithm. Ann Soc Belg Med Trop. 1992;72:129-139. 20. Baxy D and Blundel N. Sensitive, rapid, simple method for detecting Cryptosporidium in faeces. Lancet. 1982;2:149. 21. Ministry of Health (MOH). AIDS in Ethiopia. Prepared by Epidemiology and AIDS Department, Addis Ababa, 1996;2-5. 22. Central Statistical Authority. Population estimates by, area, density and administrative regions. Ethiopia Statistical Abstract. 1988;20-34. 23. Dallabetta GA and Miotti PG. Chronic diarrhoea in AIDS patients in the tropics. Tropical Doctor. 1992;22:3-9. 24. Garavelli PL, et al. Blastocystosis: a new disease in AIDS? International Journal of STD and AIDS. 1990;1:134-135. Original article Evaluation of five commercial assays for detecting HIV 1 & 2 antibodies, Addis Ababa Belete Tegbaru, Hailu Meles, Bitew Fisseha, Yared Mekonnen, Hagos Haile Abstract: The major operational characteristics of five commercially available assays for the detection of antibodies to Human Immunodeficiency Virus (HIV1 & 2) were evaluated. Four Enzyme Linked Immuno-sorbent assays (ELISAs) and one simple immuno-dot assay with visual reading, were assessed using a panel of 265 sera (18.8% hospital suspected patients, 18.8% commercial sex-workers (CSW), 31.5% blood donor sample (BDS), and 30.9% of them were scholarship winners (SSW)). Sensitivity, specificity, positive predictive value, test efficiency, delta (δ) values (for the four ELISAs) were determined. All the assays had higher sensitivities (98.7-100%), specificities (97.2-99.1%), and test efficiencies (98.1-99.6%). Higher positive and negative delta (δ+,δ -) values, +1.17 and –0.99, were observed for ICE*HIV 1-0-2 and Vironostika Uniform II PLUS O, respectively. HIV-SPOT HIV 1 & 2 showed highest value of ease of performance and suitability for small blood bank collection centers. Results of this study showed that the test efficiency, sensitivity, and specificity of the test kits were excellent as compared to the reference test. Further studies on cost-effectiveness and evaluation of newly arrived test kits before use at different levels are recommended. [Ethiop. J. Health Dev. 1999;13(2):175-180] Introduction The first Enzyme Linked Immuno Sorbent Assay (ELISA) for antibodies to Human Immunodeficiency Virus (HIV) were manufactured by coating purified HIV lysate on to the surface of micro-titration plates or beads (First Generation Assays). Later on, ELISAs have been developed which use antigens of either HIV recombinant polypeptide or synthetic peptide (Second or Third generation Immuno assays) (1-3). The use of the third generation immunoassay for the detection of HIV has reduced the interval between infection and antibody detection. These assays detect antibody to HIV earlier than the first and second generation assays including Western Blot (WB) from serum and urine (4-6). Incomplete cross-reactivity between HIV-1 and HIV-2 needs to have a combination of assays with acceptable sensitivity and specificity for both viruses. Even with HIV antibody screening, assays that have excellent sensitivity and specificity, false-positive results can not be ruled out, especially when used in a population with low prevalence of HIV antibodies (1,7,8). However, ELISAs require 1.5 to 3.5 hours to perform and need sophisticated and expensive equipment. This makes the assays technologically inappropriate for use in small laboratories in developing countries. On the other hand, simple immuno dot assays for HIV have been developed that do not require much equipment and that yield results after a few minutes (1,2,3,9). In countries like ours, where resource is scarce, the need for less expensive, more reliable and simpler assays for the detection of HIV antibody is very important. In the light of this, the present study attempts to investigate and evaluate an assay which gives the most reliable result with a good test performance, relatively lower price, and less complexity. Accordingly, five commercial HIV-antibody assays were evaluated at the Ethiopian Health and Nutrition research Institute (EHNRI), National Referral Laboratory for AIDS (NRLA). _______________________________________ Ethiopian Health and Nutrition Research Institute, P.O. Box 1242, Addis Ababa, Ethiopia. Evaluation of five commercial assays for detecting antibodies to HIV 175 ──────────────────────────────────────────────────────────── Methods In the evaluation of the assays for the detection of antibodies for HIV, a panel of 265 human sera was tested, 18.8% were hospital suspected patients, 18.8% commercial sex- workers (CSW), 31.5% blood donor samples (BDS), and 30.9% were Scholarship winners (SSW). A series type of test was conducted and the results obtained using a combination of assays were compared with those obtained using HIV-1 Western Blot (Genelabs Diagnostics), which is used as a reference (gold standard) test (1,3,10-12). Of these samples 57.7% were Western Blot (WB) (HIVBLOT 2.2, Genelabs, Diagnostics, Singapore) reactives, 1.5% were WB indeterminate, and 40.8% were non-reactive samples. The interpretation of the result for WB was according to the criteria given by the American Red Cross Society (3). The prevalence of HIV among SSW, BDS,CSW was reported as 5.3% (13), 6.6% (14), and 47-59% (15), respectively. Originally, these samples were sent to NRLA for confirmation and diagnosis of HIV infection. Five test kits, viz., HIV-SPOT HIV 1 & 2, Vironostika Uniform II PLUS 0 HIV 1 & 2, ICE* HIV 10-2, Innotest HIV 1 & 2 and RecombigenR EIA HIV 1 & 2 combination assays, which were available in NRLA were evaluated. Three of the ELISAs (Vironostika Uniform II PLUS 0, Innotest HIV 1 & 2 and ICE* HIV 1-0-2,) were third generation, while RecombigenR HIV 1 & 2 EIA was a second generation test kit (2). All the test kits were combination assay types for the detection of HIV 1 & 2. Their characteristics are summarized in Table1. The tests were performed according to the manufacturers’ instructions. In short, weak reactivity for HIV SPOT HIV 1 & 2 was evaluated visually according to the criteria given in the manufacturer’s manual, while for the other test kits, optical density (OD) reading just above the cut-off value was used. Except for HIV-SPOT HIV 1 & 2 test kit, all others require the following equipment and reagents in the laboratory: automatic washer, spectrophotometer reader, water bath, refrigerators for storage of test kits, incubation boxes, stop solutions (sulfuric acid), pipettes (multi channel and single channel), micro titration plates, dilution tubes, racks, distilled water, agitator, aspiration devices, incubators, troughs, graduated cylinders, pipette tips, distiller and thermal paper for spectrophotometer readers. Sensitivity (SEN), specificity (SPEC), positive predictive values (PPV), Test Efficiency (TE), Delta Values (δ+ and δ -, except for HIV SPOT HIV 1 & 2), false-positive ratio (FPR), the ease of performance and suitability for use in small blood bank collection centers for a particular HIV antibody assay were determined using the formula as described in Kerchoven, IV, et al. (1), Constantine, NT et al. (3), and Rose, NR, et al. (16). The statistical analyses were performed using the computer program STATA (Stata corporation, Texas, USA). Table 1: Characteristics of five commercial HIV antibody test kits evaluated in the study, Ethiopian Health and Nutrition Research Institute, National Referral Laboratory for AIDS, 1998. Paramete HIV-Spot HIV1 & 2 Vironostika Uniform II plus 0 Innotest HIV 1 & 2 ICE* HIV 1-0-2 RecombigenR EIA Manufacturer Test Type Antigen Type Coating on Genelabs Diagn DOT SP/RP Membrane Flat wells 1.50 10min Organon Teknika IE SP Innogenetics IE SP Flat wells Murex IE SP U-shaped wells Cambridge IE SP Flat wells 0.50 2 hours 0.50 2 hours 0.50 2 ½ hours 0.50 Cost USD/test** Time for Test **- Price is according to the World Health Organisation (WHO), 1998 SP- Synthetic peptide, RP-Recombinat protein, IE-Indirect ELISA Table 2: Sensitivity (SEN%), specificity (SPEC %), positive predictive value (PPV %), test efficiencty (TE %), and Delta values (δ+δ-) of the test kits, Ethiopian Health and Nutrition Research Institute, National Referral Laboratory for AIDS, 1998. 176 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Parameter SEN SPEC PPV TE δ+ δ- HIV-SPOT HIV1 & 2 98.69(95.36-99.84) 8.15(93.47-99.77) 98.69(95.36-99.84) 98.47(96.12-99.58) NC NC VIRONOSTIKA UNIFORM II PLUS 0 100(97.62-100) 99.07(94.95-99.97) 99.35(96.43-99-98) 99.62(97.88-99.99) 0.438 -0.990 I NOTEST HIV 1 & 2 ICE* HIV 1-0-2 RECOMBIGENR EIA 98.69(95.36-99.84) 97.22(92.09-99.42) 98.05(94.41-99.59) 98.08(95.58-99.37) 0.538 -0.190 100(97.62-100) 97.22(92.09-99.42) 98.07(94.48-99.68) 98.85(96.68-99.76) 1.176 -0.080 98.69(95.36-9.84) 8.15(93.47-99.77) 8.69(95.36-99.84) 8.47(96.12-99.58) 0.997 -0.620 **-95% confidence interval NC-Not calculated Results All the assays evaluated in the study had good sensitivities, specificities, positive predictive values and test efficiencies with ranges of 98.7-100%, 97.2-99.1%, 98.1-99.4% and 98.1-99.6%, respectively. The positive and negative delta values (δ+ and δ -) ranged from 0.438 to 1.176 and –0.99 to –0.08, respectively (Table 2). The rate of false-positivity (FPR) were found to be 0.93%, 1.85% and 1.85%, 2.78% and 2.78% for Vironostika Uniform II PLUS 0, RecombigenR HIV 1 & 2, HIV SPOT HIV 1 & 2, Innotest HIV 1 & 2 and ICE* HIV 1-0-2 test kit, respectively, while the false negativity rates were 0 and 1.3%. Unlike the other four ELISAs, HIV-SPOT (rapid test) was found to be very easy and very suitable in its ease of prformance and suitability for use in small blood bank collection centers (Table 3). Four indeterminate samples (1.5% out of the total), which were determined by Western Blot, were included in the evaluation of these test kits. At least two of the test kits were weakly reactive towards one of the indeterminate samples. However, none of these samples was reactive towards Vironostika Uniform II PLUS 0 HIV1 & 2 test kit (Table 4). Table 3 : Total sera tested (Positives and Negatives) and calculated true positives, true negatives, ease of performance and suitability for use in small blood bank collection centers (SSBBCC) of the evaluated test kits, Ethiopian Health and Nutrition Research Institute, National Referral Laboratory for AIDS, 1998. HIV-SPOT Vironostika Innotest Plus 0 ICE* HIV Rerecombigen R HIV1 & 2 Uniform II HIV1 & 2 1-0-2 EIA Total Negatives Samples 108 108 108 108 108 Total Positives Samples 153 153 153 153 153 True Negatives 106 107 105 105 106 True Positives 151 153 151 153 151 Ease of Performance VE LE LE LE LE SSBBCC VS LS LS LS LS VE-Very easy, LE-Less easy, VS-Very suitable, LS-Less suitable Discussion As already showen by different researchers (1,3,9) and from our laboratory experience, the conventional method of ELISA exhibited a number of shortcomings. The assay requires instrumentation and preparation of reagents; it is not rapid and, as a result, is neither easy to perform nor suitable (ease of performance and suitability test) in places where the time gap between blood donation and transfusion is very short. Moreover, in resource-poor settings Table 4: Test results of the indeterminate samples by the evaluated test kits, Ethiopian Health and Nutrition Research Institute, National Referral laboratory for AIDS, 1998. Sample Code Weakly Reactive by Result of WB Bands observed L-161 RecombigenR HIV ½ EIA Indeterminate P24(weak) L-187 HIV-SPOT, Innotest, ICE*HIV 1-0-2 Indeterminate P24,P66(both weak) L-261 Innotest, ICE* HIV 1-0-2 Indeterminate gp41(weak) Evaluation of five commercial assays for detecting antibodies to HIV 177 ──────────────────────────────────────────────────────────── L-263 Positive control Negative control HIV-SPOT, RecombigenR HIV Indeterminate Reactive Non-reactive gp41(weak) All bands observed No bands observed where frequent electric power interruptions and shortage of distilled water exist, there will be a negative effect on the performance of the test. However, ELISAs are preferable to screen large number of samples as compared to rapid and confirmatory assays (3,17). In contrast, though immuno-dot blot assays are more expensive than ELISAs, they are recommended in rural areas (in field), blood banks, and emergency rooms where there are shortages of water supply and electricity, as these tests are easier to perform, yield result after few minutes and easy to interpret in such conditions (10,12,18-22). The sensitivities, specificities, and positive predictive values of the test kits were high, ranges of 98.7-100%, 97.2-99.1%, and 98.1-99.4%, respectively. The highest positive delta value was observed for ICE* HIV 1-0-2 test kit, while the highest negative delta value was observed for Vironostika Uniform II PLUS 0 HIV 1 & 2 test kit. The test performance of these kits (test efficiency), which is dependent on both specificity and sensitivity, was higher for all the kits and was found to be highly satisfactory, being in the range of 98.1-99.6%. The delta (δ) values provide statistical estimates of the test sensitivity and specificity and permit differentiation between ELISAs of similar sensitivity and specificity and help to see the comparison of the efficacy of ELISAs to separate the negative and positive antibody serum populations from the cutoff value. It also reflects the ability of an ELISA test to produce consistently high sample/ cut-off ratios; sample optical density (OD) ratio lie far above or below the cut-off OD for HIV-antibody positive and negative sera, respectively. The higher the positive and negative delta values, the greater the probability that the test will correctly identify antibody-positive and antibody-negative sera (1,2). The higherst δ+ value observed for ICE * HIV 1-0-2 (δ+ =+1.77) shows that this test kit has the ability to characterize the positive samples that lie far above the cut-off value. This is further demonstrated by the fact that the kit has the highest false-positivity ratio. On the other hand, the higherst negative delta value was obtained for Vironostika Uniform II PLUS 0 test kit (δ-=-0.99), which showed the assay has a greater margin for variation in test results without the occurrence of more false positive results (FPR = 0.93%), and this increases the confidence in the specificity estimates. The sensitivity of Vironostika Uniform II PLUS 0 and ICE * HIV 1-0-2 was high (100% in each case) compared to the others. This concurred with the absence of false-negative results in both cases which make these types of ELISAs feasible for screening of large samples as elaborated by different researchers (2,6,17). Eventhough all tested kits had high sensitivities and specificities, Vironostika Uniform II PLUS 0 characterized negative samples in a better way than the other test kits and had a clear margin for separation of the sample OD ratio that lies below the cut-off value. Eventhough the observed test efficiencies were high (98.1-99.6%), Virononstika Uniform II PLUS 0 showed a high test performance (TE, 99.6%) as compared to the other kits which showed better sensitivity and specificity. In general, all the test kits evaluated in the study had good sensitivity, specificity, positive predictive value and test efficiency as compared to the reference test, Western Blot. The ease of performance and suitability for use in small blood bank collection centers was higher for HIV-SPOT (rapid test) which indicates that this test kit is very simple to use in resource limited areas and in emergency conditions as also recommended by Constantine, NT,1993 and Myrmel, H, 1990. In addition, the study will give comparative data to enable the users to arrive at a decision of their own, depending on their needs and conditions, to choose the appropriate sensitive and specific test kits for screening and combinations of ELISAs for confirmation of HIV-infection. Recommendations Since the development, introduction, and use of the newly arriving HIV antibody detection assays is a dynamic process, the evaluation of these assays before use at different levels and condition is essential. The sensitivity, specificity, predictive values, false- positive ratio, ease of performance, suitability for use in small blood bank collection centers, test efficiency and delta values need to be evaluated using different combinations of assays and ELISA systems to confirm antibodies to HIV infetion. Further study on the cost-effectiveness of these and related HIV antibody detection assays is recommended in order to adopt the most cost-effective option. Acknowledgements We greatly acknowledge the Department of Epidemiology and AIDS, AIDS/STD Team, MOH, and the Ethio-Netherlands AIDS Research Project (ENARP) in EHNRI for providing us with the ELISA and Western Blot test kits, respectively. The valuable comments and suggestions on the article by Dr. Arnaud Fontanet and Ato Tesfaye Mengesha are highly appreciated. Finally, EHNRI is aknowledged for providing us with all the required laboratory facilities. References 1. Kerchoven IV, Vercauteren F, Piot P, and Groen,GVD. Comparative evaluation of 36 commercial assays for detecting antibodies to HIV. Bull WHO 1991;69(6):753-60. 2. Constantine NT, Collahan JD, Watts DM. Retroviral Testing, Essentials for Quality Control and Laboratory Diagnosis.2nd edn. Boca Raton: CRC Press Inc, 1992:35. 3. Constantine NT. Serologic tests for the retroviruses:approaching a decade of evolution. AIDS. 1993;7:1-13. 4. Zaaijer HL, Oehlers PVE, Kraaijeveld T, Altena E, Lelie PN. Early detetion of antibodies to HIV1 by third generation assays. Lancet 1992; 340:770-2. 5. Stetler HC, Granade TC, Nunez CA, Meza R, Terrell S, Amador L, George JR. Field evaluation of rapid HIV serologic tests for screening and confirming HIV-1 infection in Honduras. AIDS 1997; 11:369-75. 6. Desai S, Bates H, Michalski FJ. Detection of antibody to HIV-1 in urine. Lancet 1991;337:183-4. 7. Messele T, Zewdie D. Comparison of two generations of Wellcozyme kits. Ethiop J Health Dev 1990;4(2):207. 8. Constantine NT, Fox E, Abatte EA, Woody JN. Diagnostic usefulness of five screening assays for HIV in an East African city where the prevalence of infection is low AIDS 1989; 5:313-17. 9. World Health Oganization and United Nations Joint Program on HIV/AIDS, Revised Recommendations for the selection and use of HIV antibody tests. WHO Wkly Epidemiol 1997; 72:12, March 21, 81-8. 10. Groen GVD, Kerchoven IV, Vercauteren G, Piot P. Simplified and less expensive confirmatory HIV testing Bull WHO 1991; 69(6):747-52. 11. Broder S, Merizan TC, Bolgnesi D. Text Book of AIDS Medicine. Williams & Wilkins, 1994:149. 12. Myrmel H, Holm-Hanson C, Haukenes G. Evaluation of two rapid tests for the detection of HIV-1 & HIV-2 antibodies. AIDS 1990;4(11): 1164-5. 13. Sahlu T, Eshete H. The progression of HIV/AIDS in Ethiopia. Ethiop J Health Dev 1996;10:17990. 14. Fontanet AL, Messele T, Dejene A, Enquselassie F, Abebe A, Cutts FT, De Wolf F, Rinke De Wit TF, Sahlu T, Bindels P, Yeneneh H, Coutinho RA, Nokes DJ. Age-and sex-specific HIV-1 prevalence in the urban community setting of Addis Ababa, Ethiopia. AIDS 1998;12:315-22. 15. Abebe A, Kuiken CL, Goudsmit J, Valk M, Messele T, Sahlu T, Yeneneh H, fontanet A, De Wolf F, Rinke De Wit TF. HIV Type 1 subtype C in Addis Ababa, Ethiopia. AIDS Res Hum Retroviruses. 1997;13(12):1071-75. 16. Rose NR, Friedman H, Fahey JL. Manual of Clinical Laboratory of Immunology, 3 rd edition, American Society for Microbiology, Washington DC, U.S.A. 1986:966. 17. United Nations Joint Program on HIV/AIDS: Blood Safety and HIV, UNAIDS Technical Update (UNAIDS Best Practce Collection: Technical Update) Geneva; October 1997;3. 18. Wilkson D, Wilkson N, Lombard C, Martin D, Smith A, Floyd K, Ballard R. On- site HIV testing in resource-poor settings: is one rapid test enough? AIDS 1997; 11:377-81. 19. Parry JV, McAlpine L, Avillez MF. Sensitivity of six commercial enzyme immunoassay kits that detect both anti-HIV-1 and HIV-2. AIDS 1990; 4:355-60. 20. Spielberg F, Kebeya CM, Ryder RW, Kifuani NK, Harris J, Bender TR, Heyward WL, Quinn TC. Field testing and comparative evaluation of rapid, visually read screening assays for antibody to human immuno-deficiency virus. Lancet 1989;1:580-4. 21. Kebeya CM, Bertozi S, Spielberg F, Ryder RW, Heyward WL, Quinn TC. Cost analysis of dual rapid assay system for screening and confirming of HIV seropositivity. In: Abstracts from IV International conference on AIDS and associated cancers in Africa, Marseille, France, 18-20 October, 1989. P.400, Abstract No.401. 22. Constantine NT, Collahan JD, Watts DM. Time for HIV-1 & HIV-2 combinations tests? J Virol Methods 1989;26:219-22. Original article Fine-needle aspiration of palpable breast lesions with histopathologic correlation Wondwossen Ergete Abstract: Fine-needle aspiration biopsy of the breast has been used as a diagnostic step in the investigation of palpable breast lumps in the Department of Pathology, Tikur Anbessa Hospital, for more than 10 years. The purpose of this study is to evaluate the accuracy of fine-needle aspiration with histopathologic confirmation. A retrospective study was performed using records of fine-needle aspiration and biopsy results and request forms over four and half years. All women and men who had had fine-needle aspiration breast biopsy with histopathologic confirmation of the diagnosis were included. Fine-needle aspirations were interpreted as malignant, suspicious, or benign. Histopathologic diagnosis included incisional, excisional, and mastectomy specimen. A total of 244 patients fulfilled the criteria. Only eight (3.3%) of the specimens were inadequate for study. There were 52 total malignant fine-needle aspiration diagnoses, with only two false-positive specimens. One was flbroadenoma and the other benign phylloides. There were 20 suspicious readings; 14 of these were malignant and six were false-suspicious specimens. Fibroadenoma, fibrocystic change, and papilloma were two each for the the six false suspicious specimens. Of the 164 lesions interpreted as benign, there were 10 false negative specimens. The test had 86% sensitivity, 95% specificity, 89% positive predictive value, and 94% negative predicitive value. Fine-needle aspiration is a sensitive and highly specific test that can be useful as an adjunct in the diagnosis of breast cancer. “Malignant” and “benign” interpretations are highly predictive but must be used only in the context of other diagnostic modalities. “Suspicious” “atypical” or “papillary” lesions require further investigation. [Ethiop. J. Health Dev. 1999;13(3):181-186] Introduction Various diagnostic methods have been developed to evaluate palpable and non- palpable breast lesions with the goal of identifying a sensitive, specific, efficient, and economical approach to diagnose breast cancer. Physical examination, mammography, ultrasonography, core needle biopsy, open excisional biopsy, thermography, and Fine- Needle Aspiration (FNA) are all used to a greater or lesser extent in the diagnostic workup of a palpable breast mass (1). Various combinations of these approaches have been studied and have been found to increase sensitivity and specificity over that of any one test alone (2). FNA has been used as the first diagnostic step in the investigation of palpable breast lumps in the Department of Pathology of the Tikur Anbessa Hospital for more than ten years. FNA of palpable breast masses has become increasingly popular as a diagnostic technique as it provides a sensitive, expedient, and economical method of obtaining cytologic material for examination. Its distinct advantages include accurate diagnosis, low cost, excellent patient acceptance, and minimal or no morbidity. In recent times in the best center, it has largely replaced excisional biopsy. ______________________________________ Department of Pathology, Faculty of Medicine, Addis Ababa University, P.O.Box 9086, Addis Ababa FNA alone, however, is subject to inaccuracies and does not definitively diagnose all breast cancers with the reliability of an open biopsy. It is most commonly used in combination with physical examination and mammography in the so called “triple test” diagnostic triad, which is a highly accurate method of evaluating breast masses. The purpose of this study was to evaluate the experience with FNA biopsy in a series of patients and compare the findings on FNA cytology with that of histopathology. Fine needle aspiration 181 ─────────────────────────────────────────────────────────── ─ Methods A retrospective review of the biopsy requisition forms and reports at the Department of Pathology, Faculty of Medicine, Addis Ababa University (FMAAU) was performed from 1994 to Mid-1998. The records of all female and male patients who had undergone (FNA) and histopathologic diagnoses of palpable breast lesions at the Department of Pathology, FMAAU, were included. Histopathologic confirmation consisted of either incisional biopsy, excisional biopsy or Mastectomy specimen. FNA was performed by either a pathology resident or a pathologist as follows: a 20-23 gauge needle was attached to a 10 ml syringe, which was mounted on an aspiration cameco gun. One or two separate passes were made into the lesion with the needle. During each pass the needle was moved throughout the lesion multiple times while aspirating. Smears from the aspirates were air dried and stained by the May-Grünwald Giemsa. The FNA specimens were examined and assigned to one of the three different diagnoses: malignant, suspicious (including atypical and papillary neoplasms) or benign. The malignant diagnoses were assigned when 1) there are abundant cellularity, loosely cohesive and individual cells; 2) the cells show variable size, nuclear molding, and loss of polarity; or 3) individual tumour cells demonstrate malignant cytologic features, such as increased nucleocytoplasmic ratios, hyperchromatic and coarsely granular chromatin and small to prominent nucleoli. The benign diagnoses were assigned to the specimens lacking the above mentioned picture, and in the presence of abundant bipolar naked nuclei. A “suspicious” diagnosis is when 1) the cytologic features for malignancy are not completely fulfilled, 2) the presence of cell groupings in the form of three dimensional papillary groups along with scattered, high columnar cells, and a bloody diathesis with haemosiderin laden “macrophages” or foam cell are seen. A diagnosis of “atypical ductal hyperplasia” is rendered when 1) the aspirate is highly cellular with crowded groups consisting of cells with both benign and atypical features (greater variation in cell size and shape and loss of polarity); 2) hyperchromatic nuclei with readily visible nucleoli are seen and 3) occasional single atypical cells are present. A diagnosis of “atypical Fibroadenoma” is rendered when there are loose cohesions of the cell groupings with some anisonucleasis and prominent nucleoli of the cells. Sensitivity and specificity, both of which require either a positive or a negative diagnosis, were calculated for the entire group with the assumption that the “suspicious” group was positive for malignancy. The atypical and papillary neoplasm groups were included in the “suspicious” category. This was done to ensure that the most conservative approach was taken to achieve the greatest sensitivity. The positive and negative predictive values were calculated for the malignant and benign diagnoses alone (excluding the suspicious category) and for the entire set of the specimens (including the suspicious category). Results A total of 244 cases that fulfilled the study criteria were identified. Only eight FNA specimens (3.3%) were deemed inadequate for the study (Figure). All histopathologic specimens were adequate to make final pathologic diagnoses. A diagnosis of “malignant” was made for 52(21.3%) of the 244 FNA specimens. Only two (3.8%) were false-positive results when read as malignant; 182 Ethiop.J.Health Dev. ─────────────────────────────────────────────────────────── ─ Figure 1: Summary of results of FNA for entire series. in these two the histopathologic diagnosis were fibroadenoma and benign phylloides. The positive predictive value of an FNA reading of “malignant” was 96%. A diagnosis of “suspicious” was made for 20(8.2%) of the 244 specimens. Of these 14(70%) were malignant and 6(30%) were benign or “false suspicious”, fibroadenoma, fibrocystic change and papilloma accounted for two cases each of the benign cases (false suspicious). A total of 164(67.2%) of the 244 FNA specimens were read as benign and, of these, 154(94%) were true negative benign lesions. Fibroadenoma accounted for 81(52.6%), fibrocystic change 40(25.9%), adenosis 10(6.5%) gynaecomastia 5 (3.2%), adenoma 4(2.6), benign phylloides 4(2.6%), fat necrosis 3(1.9%), chronic non-specific inflammation 3(1.9%), tuberculosis 2(1.3%) and, granuloma 2(1.3%) of the true benign lesions. Ten lesions diagnosed as benign were found to be malignant on histopathologic examination. Most of the cases were high grade invasive ductal carcinoma. This represents a false negative rate of 4.2% for the entire series and 6.0% of the ‘benign’ readings were, infact, malignant. The negative predictive value of a benign reading in this series is 94% when considered alone. For the entire series, the falsepositive rate was 3.4% and the false negative rate was 4.2% (Table 1). The sensitivity of FNA for the entire series was 86% assuming, for calculation purposes as described previously, that the “suspicious” lesions are considered to be positive. The specificity was 95%. The overall positive and Fine needle aspiration 183 ─────────────────────────────────────────────────────────── ─ Table 1: Summary of fine-needle aspiration of 244 palpable breast lesions with histopathologic correlation, Department of Pathology, FMAAU, Addis Ababa, 1999. No. of Samples (% of Total) % Inadequate Sample 3.3 Comparison of True Positives 27.1 Comparison of True Negatives 65.3 Comparison of False Positives 3.4 Comparison of False Negatives 4.2 Sensitivity 86 Specificity 95 Positive Predictive Value 89 Negative Predictive Value 94 Accuracy 92 negative predictive values were 89% and 94%, respectively. The accuracy of FNA in this series is 92%. Discussion The value of any diagnostic test lies in its ability to detect the presence of disease when it is present (sensitivity) and reliably verify the absence of the disease when it is not present (specificity). To contribute to the diagnostic workup of a palpable breast mass, FNA biopsy sensitivity and specificity should approach that of an open excisional biopsy. FNA biopsy of the breast is reported to have an average sensitivity of 87% (range 72% to 99%), specificity of 98% to 100%, negative predictive value of 87% to 99% (4,5). The results from this series of patients confirm that FNA biopsy of palpable breast lesions is an accurate and sensitive method of diagnosing breast carcinoma. The results presented here were comparable to the above series. Breast aspiration results compare favourably with tru-cut or other tissue core biopsy procedures of the breast (6). The accuracy rate of FNA biopsy increases when the pathologist performs the FNA biopsy and uses immediate assessment to guide specimen adequacy (7). There were few unsatisfactory specimens in this series. In most series the inadequate specimen rate is up to 10% to 15% (3). This low rate in this series is, in part, because of the aspirator who performed a great number of the aspirations would perform an initial immediate quick staining to assess specimen adequacy and reaspirate if the specimens were unsatisfactory on the first attempt. The pathologist added the category “suspicious” or “atypical” to include the borderline specimens that could not definitely be diagnosed as being malignant or benign. These were specimens that had some characteristics of malignancy but did not fulfil the criteria of being malignant as previously mentioned. The other category included in the “suspicious” category was a papillary neoplasm because differentiating a benign papilloma from a well differentiated papillary carcinoma can be difficult on FNA sample. Surgical excision is advised when a papillary lesion is encountered. At times this group of neoplasia can be confused with fibroadenoma or fibrocystic change as it was seen in six patients in this series. In general, the suspicious category contained some of both malignant and benign lesions according to final histopathology. So, this category, therefore, contained some of the false positive (benign) lesions. Instead of false-positive they are actually false suspicious. The large number of false positive or false-suspicious readings adversely affect the overall specificity and accuracy of the series. To accurately examine the ability of FNA to diagnose breast carcinoma, the results were generated into different fashions to account for the suspicious category. First, to calculate the overall sensitivity, specificity, positive and negative predictive values and accuracy of FNA, it was chosen to combine the suspicious and malignant categories. This approach decreases the chance of missing a positive result 184 Ethiop.J.Health Dev. ─────────────────────────────────────────────────────────── ─ thereby increasing the sensitivity of the test. As noted previously the sensitivity was close to the reported average. Also, by performing the calculations in this manner,the specificity of the test decreases, as there will necessarily be more false-positive specimens-those that are included in the suspicious category but are benign. In fact the overall specificity in this series is slightly low because of the number of false-positive specimens in the suspicious category. The vast majority of falsepositive specimens classified as suspicious were benign fibrocystic change and fibroadenoma. In the second method by which the predictive values were generated, the calculations were performed using only those specimens that were definitely diagnosed malignant or benign. This was done to determine how reliably the definitive diagnoses were themselves, exclusive of the confounding variable included in the suspicious category. This is to determine how predictive the test was when the pathologist was confident in assigning a definitive diagnosis. When considered by themselves, the malignant and benign diseases posses high positive and negative predictive values, respectively. This indicates that, when a definitive diagnosis is made from FNA, it is a highly accurate and predictive tool. Interpretative errors are most often responsible for false-positive diagnosis. False-positive rates in the literature are reported in the range of 0 to 41%(4,8,9). In this series, there was a low rate of false- positive results in the group read definitely as malignant. The false-positive specimens were all based on what were adequate specimens. One case was histologically diagnosed as fibroadenoma and the other as benign phyilodies. The potential for a false- positive diagnosis of malignancy exists in aspirates from the above and several histologic epithelial proliferations known to be responsible for false-positive diagnoses owing to the hypercellularity and significant epithelial proliferation with various degrees of atypia (10,11). The majority of false-positive specimens in this series were actually false-suspicious. When the pathologist was confident in diagnosis, it was rarely incorrect. The falsenegative rate varies from 1% to 31% with a 10% average rate reported in the literature. A falsenegative FNA is most often due to sampling problems; interpretation errors are rare (12,13). However, tumour-size paucicellularity, special histologic types such as tumours showing extensive fibrosis (therefore, decreased numbers of malignant cells), those with cells having relatively bland cytologic features like lobular carcinoma, colloid carcinoma, papillary carcinoma, monomorphic pattern of ductal carcinoma that can occur in older individuals, can also contribute to an increase in the falsenegative rates. Awareness of these potential pitfalls can be helpful in avoiding a false-negative report in many of these cases. In this study many false- negative cases belong to high grade invasive carcinoma on histopathologic report. These may indicate that the sampling error could be part of the reason. Diagnostic errors with subsequent inappropriate clinical decisions can be best avoided if clinicians use the so called triple (triplet) diagnostic procedure of clinical examination, mammography, and FNA cytology which increases the accuracy for the diagnosis of breast cancer (14). If FNA were used alone as the sole determinant of further therapy its low false-negative rate would still be too high to be acceptable. However, FNA is never used as the sole diagnostic modality determining intervention for palpable breast lesions. The triple test has been shown to be highly sensitive and specific in the diagnosis of breast cancer (14). Of the three tests, FNA has the highest sensitivity and specificity and may prompt further action in cases in which physical examination and mammography are not suspicious. Even with a negative triple tests, there is a certain small subset who will have a carcinoma. In summary, fine-needle aspiration is a sensitive and highly specific method of evaluating palpable breast lumps for malignancy. It can be useful in confirming a diagnosis that is suspected by other diagnostic modalities. When a definitive diagnosis is assigned to a specimen, it is highly predictive of that mass being positive or negative for cancer. When suspicious lesions are included in the analysis, the specificity and sensitivity of the test declines, as there are a considerable number of false-positive Fine needle aspiration 185 ─────────────────────────────────────────────────────────── ─ and false-negative lesions in the suspicious category. Because of the inherent inaccuracies within the test, it is difficult to recommend definitive treatments based on FNA unless the other diagnostic modalities concur with the FNA diagnosis. Even when FNA is combined with other tests there is a small occurrence of false-negative diagnoses. Suspicious, atypical or papillary lesions should be investigated further with open biopsy. Acknowledgement I am very grateful to W/t Abenet Mekonnen for her time in typing the manuscript. References 1. Negri S, Bonetti R, Chpitanio A, Bonzanini M. Preoperative diagnostic accuracy of Fine-Needle aspiration in the management of breast lesions: Comparision of specificity and sensitivity with clinical examination, mammography, echography, and theromo-graphy in 249 patients. Diagn cytopathol 1994;11:4-8. 2. Vetto J, Pommier R, Schmidt W, Eppich H, Alexander P. Diagnosis of palpable breast lesions in younger women by the modified triple test is accurate and cost-effective. Arch surg 1996;31:967-74. 3. Stephen ON, Melanie C, Paolo G, Lawrence K, Kristh M, Gerard A. Fine-needle aspiration of 697 palpable lesions with histopathologic correlation. Surgery 1997; 122:824-8. 4. Silverman JF. Diagnostic accuracy, Cost-effectiveness, and triage role of fine-needle aspiration biopsy in the diagnosis of palpable breast lesions. Breast 1995;1:3-8. 5. Silverman JF, Finley JL, O’Brien K, et al. Diagnostic accuracy and role of immediate interpretation of fine needle aspiration biopsy specimens from various sites, Acta cytol 1980;33:791-6. 6. Shabot M, Goldberg IM, Schick P, et al. Aspiration cytology is superior to Tru-cut needle biopsy in establishing the diagnosis of clinically suspicious breast masses. Ann surg 1982;196:122-6. 7. Cohen Mb, Rodgers RPC, Hales MS, etal. Influence of training and experience in fine needle aspiration biopsy of breast. Receiver operating characteristics curve analysis. Arch Pathol Lab Med 1987;111:518-20. 8. Bell DA, Hajdu SI, Ubran JA, Gaston JP. Role of aspiration cytology in the diagnosis and management of mammary lesions in office practice. CANCER 1983;51:1182-9. 9. Feldman Ps, Covell JL. BREAST and Lung. In fine Needle Aspiration cytology and its clinical application. Chicago, American Society of Clinical Pathologists press, 1985; 27-43. 10. Bibbo, M. In Comprehensive cyto-pathology 2nd edition. W.B. Saunders company, Philadelphia, 1997;731-65. 11. Kline TS. Handbook of Fine Needle aspiration Biopsy cytology St. Louis, CV Mosby. 1988. 12. Wanebo HJ, Feldman PS, Wilnelm MC, et al. Fine needle aspiration cytology in lieu of open biopsy in management of primary breast cancer. Ann surg 1984;199:576-9. 13. Scopa CD, Koukouras D, Androulakis J, Bonikos D.sources of diagnostic discrepancies in fine needle aspiration of the breast. Diagn-cytopathol 1991;7:546–8. 14. Kaufman Z, Shiptiz B, Shapiro M, Rona R, Lews, Dinbor A. Triple approach in the diagnosis of dominant breast masses: Combined Physical examination, Mammography, and Fine-needle aspiration. J. Surg oncol 1994;56:254-7. Original article The involvement of the general health service staff in the management of leprosy in the Southern Region, Ethiopia Mengistu Asnake1, Melesse W/Dawit 2, Mohammed Ahmed 3, Timotiwos Genebo 4, Bereket Mekbib5 Abstract: A qualitative study to examine the involvement of the General Health Service (GHS) staff in the management of leprosy patients was done between January and March 1997 in the Southern Nations Nationalities and Peoples Region (SNNPR). The aim of the present study was to get qualitative information on the status of the leprosy control program, the possibility of managing leprosy in the GHS, their willingness and future vision. The study used an in-depth interview with key informants and Focus Group Discussion (FGD) with leprosy field workers and GHS staff as an instrument. The result showed that information related to the program is lacking at the woreda and zonal health department levels. The involvement of GHS staff in the leprosy control program was limited to suspecting and referring leprosy cases. The increased availability of the service to patients and better relationships among vertical program and GHS staffs were raised as major advantages of involving the GHS in leprosy work. Decreased attention given to prevention of disability, the occurrence of stigma and the threat to leprosy technical staff of losing incentives, were some of the disadvantages raised, if the program is integrated into the GHS. In general, there was a positive attitude from all participants of the discussion towards integrating leprosy into the GHS. Therefore, all stakeholders should give due attention to promoting the involvement of the GHS staff by gradually integrating the program into the GHS system. [Ethiop. J. Health Dev. 1999;13(3):187-193] Introduction The social picture of leprosy has changed over the last decades, it being regarded more and more as any other public health problem that can be managed in any general health service. All countries have officially adopted the outpatient clinic as the base for treating leprosy, while old stigmatising leprosaria are being phased out. This optimistic approach deserves strong support from health personnel and others at all levels in order to guarantee patients’ adequate treatment as well as self-respect (1). After considerable progress has been made in the control of leprosy through the implementation of multiple drug therapy (MDT) during the last decade, the prevalence of the disease decreased dramatically. As a result of the very encouraging results from MDT within the last decade, the World Health Assembly (WHA) in 1991 resolved to eliminate leprosy (prevalence below 1 per 10,000 people) as a public health problem by the year 2000(2). Since the implementation of MDT, the integration of leprosy control into the GHS has gained much wider acceptance. Integration means that leprosy control activities become the responsibility of the general health service i.e., a multipurpose, permanent, and decentralized health service, that is as ______________________________________ 1 PPHC Coordinatior, BASICS US AID, Awassa, Ethiopia; 2SNNPR tuberculosis, Leprosy, and Blindness Control Program Coordinator, Awassa, Ethiopia; 3Butajira Health Center, Butajira, Ethiopia; 4Ethiopian Health and Nutrition Research Institute, Addis Ababa, Ethiopia; 5Tuberculosis control Program coordinator, Shashemene General Hospital, Shashemene, Ethiopia. close to the community as possible (3). To a great extent this is based on the best utilization of resources,because with the decreasing number of registered cases, vertical programs have become less effective. However, integration of leprosy services with the general medical services should be to the advantage of the patients (4). The involvement of the general health service in leprosy 187 ──────────────────────────────────────────────────────────── Integration may involve the disappearance of specialized health care structures, but not the elimination of the program and/or the specialized staff at the most centralized levels of the health system. Integration involves administrative and operational changes at the level of multifunction health services, since there is no point in integration unless the multifunction health services have been given the means to deal adequately with the problem, taking account of the level of qualification and workload of their staff. Integration will necessitate in varying degrees supplementary training, appropriate instruction manuals, closer supervision, etc. This implies that the managers of the multifunction health services must have sufficient administrative authority and operational control (5). In some countries where leprosy is endemic control programs are still vertical from national to operational level, with specialized staff and clinics, which are separated from other health services. This type of service has its own limitations leading to restricted achievement in leprosy control. The most frequently reported limitations are insufficient coverage, lack of comprehensive and continuous health care, inefficient use of resources, stigma, and dependency on donor’s (3). In order to overcome these limitations, the general health services, which usually provide better coverage of the population than vertical programs must be involved. At present, with the policy of decentralization in Ethiopia, leprosy and its control have become the responsibilities of the regional health bureau (6). In spite of the policy, the control program is still in its vertical implementation. There are several factors, which need investigation before handing over the program to the GHS in order to avoid the disadvantages on patient management. Based on these facts the aim of the present study was to get qualitative information on the involvement of GHS staff in leprosy control and to identify obstacles and future vision related to the management of leprosy patients in Southern Nations Nationalities and peoples Region (SNNPR), Ethiopia. Methods The involvement of the GHS staff in the management of leprosy control in SNNPR was assessed using a qualitative study during Jan– March 1997. The region has a population of 11.3 million within nine Zones and five Special woredas. A total of 28 leprosy field workers are running a vertical leprosy control program in the Region. At present in the SNNPR the integration of Leprosy Control Program into the GHS is in its initial stage. A total of 23 key informants (two from Ministry of Health, two Regional health Bureau, five Zonal Health Department, 12 Woreda Health office, and two Donors (ALERT and GLRA)) selected by purposeful sampling, participated in an in-depth interview. All the leprosy field workers and 18 health workers (six Doctors, six Nurses and six health assistants) participated in a total of seven Focus Group Discussions (FGD). Each FGD included 6-7 participants and took 1-2 hours duration. The in-depth interview was done with in 1-hour duration. Two persons, one as facilitator/ interviewer and the other as recorder using questionnaire guides, held the FGD and in-depth interviews. In the guide, variables such as description of leprosy control programs, level of involvement, attitude of GHS staff, willingness for involvement, and the future vision were included. Qualitative data from FGD and in-depth interviews were analyzed using a matrix for the different items. Results As shown in Table 1, all levels of key informants described the vertical program implementation. At the zonal and woreda Table 1: key informant interview (summary), March 1997. NO. 1 GUIDE General description of leprosy control Program MOH/RHB* Vertical program direction Limited integrated program (Tigray) ZHD/WHO** No information on the . burden of the disease .Vertical implementation .No direct relationship with ZHD/WHO DONORS ...Working as vertical Implementers .Combination with TBC in some areas. Association with charity REMARK 188 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── 2 Involvement of leprosy patients in management .Involved in all 3 Future vision in relation to the involvement of GHS To integrate with other sease in the GHS 4 Ways to reach future vision Policy for integration Training of health workers Support from donors in the direction of policy guidelines components with specialized structure *ministry of Health/Reginal Health Bureau Participation in diagnosis (suspect) of patients and referral .Occasional involvement in health education.No involvement in other activities because of specialized program .Integrate with other diseases such as TB .All health institutions should render the service Fear. of resource shortage if integrated .Involvement in all activities as implementers (ALERT) .Support the implementation of activities (GLRA) .Training of health workers .Budget the program .Support from donors .Clear policy on GHS involvement .Training of health workers .Incentive for health workers (top up, salaries, allowances) .Restructuring from vertical to integrated program .Combination with TBC .Integration with the GHS .Continue with the vertical approach in successful program areas “Fear of job insecurity for leprosy field workers if integrated” **Zonal Health Department/World Health Organization levels, information on the burden of the disease was not known by health officials. In relation to the involvement of the GHS staff in leprosy management at zonal and woreda levels the study showed that health workers are involved in suspecting and referring cases to leprosy clinics and occasional health education programs. As shown in Table 2, a similar result was found during the FGD among the GHS staff. The availability of the service in all health institutions and the decrease in disability were the major advantages raised by the GHS staff in relation to managing leprosy in the GHS (Table 2). Among the disadvantages, a decreased emphasis on specialized services such as prevention of disability and the occurrence of isolation of patients were the major ones (Table 2). In the same discussion, all health workers felt that leprosy as a health problem is their professional responsibility and expressed their willingness to be involved in its management. The FGD, with leprosy field workers (Table 3) revealed a better relationship with the GHS in areas where leprosy is combined with a tuberculosis program. The leprosy field workers felt that most GHS staff are not willing to participate in leprosy management because of fear of the disease. Early treatment in the nearby facilities as an advantage to the patient, and more assistance to the leprosy work for the field staff, were the major points raised by involving the GHS staff. In the same discussion, little attention given to leprosy patients, and fear of losing status for the leprosy field worker, were raised as issues The involvement of the general health service in leprosy 189 ──────────────────────────────────────────────────────────── Table 2: FGD with general health service staff, March 1997 No FGD GUIDE DOCTORS NURSES HEALTH ASSISTANTS 1 Experience related to leprosy .Referring suspects and patients to leprosy clinics .Appointment of patients for treatment day .Referral of patients and .Referral of suspects and patients 2 Is it possible to manage leprosy in the GHS Advantages .Availability of the service in all health institutions .Decreases disability suspects to leprosy clinics .Never worked in leprosy Advantages .Availability of treatment in all institutions .Availability of treatment at any time Decreases disability Disadvantage No time for POD* activities Follow up may not be done by the same person Isolation of patients Disadvantages .Physiotherapy and other activities may not be performed .Care may not be given .Helping in treatment of patients Advantage Decreases labeling of patients .Changes the attitude of the community and health workers .Availability of treatment in all institutions .Early diagnosis without complication .Decreases disease transmission Advantage Decreases labeling of patients .Changes the attitude of the Disadvantage .Increases psychological problem of the patients .Isolation can occur .Care may not be given as the vertical program as needed .Isolation of patients .Irregular follow up 3 4 Willingness to be Involved in leprosy management What should be done in the future .Is a professional responsibility .A professional responsibility Convince health staff to participate in managing leprosy patients Integrate the program slowly Continue with vertical program .Continue as vertical program .If integrated it will lose ownership .Training of GHS staff .Is a professional responsibility .Increases the knowledge of health workers Training of health workers .Use more sites by integrating the service .Give more public education .Patients should not be neglected for the sake of integration on referral of patients *POD = prevention of disability related to involving the GHS staff. The leprosy field workers, in increasing their relationship to the GHS staff, considered the involvement, in work other than leprosy, advantageous. Except the nurses in the GHS who stressed the loss of ownership, integrating the vertical program into the GHS was perceived as a future vision in all levels of the key informant interview and FGD. The fear of resource shortage was raised by zonal and woreda levels. In order to reach the future vision all felt the need for a clear policy, training of health workers, and adequate budget allocation for the program in the GHS. Discussion 190 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── From this study it is evident that the leprosy control program in most places is still a vertical program. Even though the policy of the MOH stresses that any health activity including Leprosy control, should be the responsibility of the Regional Health Bureau and institutions under them, in practice it is not yet fully exercised (6). The lack of information related to disease burdens at Zonal and Woreda offices is mainly due to the recording and reporting system using a vertical structure. This is one of the disadvantages in a vertical program where a single purpose structure, parallel to the GHS, will have its own information system (7). Table 3: FGD With Leprosy field workers, March 1997 NO FGD GUIDE RESPONSES 1 Relationship .Little relationship because of single disease activity with .Referring suspected cases the GHS .Using rooms in the GHS .Better relations in areas with combined TB/Lep program QUOTATIONS “Leprosy field worker is not considered as health worker rather as leprosy patient” “Leprosy is not an emergency disease, therefore priority is not given” 2 Attitude of GHS to participate in leprosy .Does not want to treat patients not paying (free) such as leprosy .Lack of communication with leprosy field workers because of fear of disease transmission .Some feel that leprosy field workers are getting special incentives and doing less job “Most of the time we do not tell our profession to friends because of fear of stigma” 3 Advantage and Disadvantage of Involving the GHS Advantage To the patient .Can be treated in their locality .Increases contact tracing .Can be treated before developing disability .Patients can save money .No stigma (isolation) Disadvantage .Low attitude of GHS leads to no treatment .Little attention for thorough physical examination .Stigma (isolation) .More disability because of difficulty In managing reactions No time for POD activities .Lack of experience in managing other diseases .Fear of decrease in status .Decrease in financial resource .Increase overall work load 4 Willingness to be involved in other works 5 Prospects for better eprosy anagement For leprosy field workers .Can get promotion opportunities like GHS staff .More assistance to the work .Increases relationship with GHS staff .Decrease workload on leprosy .Can help more patients with other diseases .Get more knowledge on different diseases .Decrease status .Practical integration with GHS .Training of health workers .Convince health officials on integration .Continue with vertical programs especially for POD .Form strong TB/LEP units in health institutions like MCH, EPI .In areas with patient load open special program The availability of services in all health facilities and decrease in disability, raised as major advantages of involving the GHS, are related to the early detection and treatment of cases. Stigma or isolation of patients was mentioned as a frequent disadvantage during the FGD. This is mainly associated with lack of exposure to the program, or fear of management by inexperienced staff. The problem of stigma can be decreased by increasing exposure of staff, which can be mainly done by integrating the program into the GHS. In addition, involving the community and public education can solve the problem (8). The better relationship between the GHS and leprosy field workers in areas where the program is combined with tuberculosis control is mainly related to frequent communications at facility level and the use of the leprosy infrastructure for case holding of tuberculosis patients. This is especially useful in supporting the basic health service with an insufficient referral system. In addition to this, both The involvement of the general health service in leprosy 191 ──────────────────────────────────────────────────────────── diseases have similarity in epidemiology, organization, and management of control programs (9,10,11). Integration is felt as a threat to leprosy technical staff. This can only be solved through continuous discussion with the involved personnel by clearly starting their role during integration (12). The fear of incompetence of GHS personnel is mainly related to the lack of training and exposure to the program. This can be solved by giving refresher courses for GHS staff, introduction of leprosy in the curriculum of basic health training, and continuous training of GHS staff (13,14). Most participants of the discussion perceived the need for integration of the program into the GHS. In order to achieve the perceived need some prerequisites, such as political commitment to PHC, adequate training, adequate supply of drugs and equipment, regular supervision, and a well functioning basic health care system in which to integrate should be fulfilled. Unfulfilled prerequisites may end up in program failure (15). One of the principal advantages of in-depth interviews and FGD is the ability to elicit a large amount of information in an efficient manner. In terms of the human and physical resources required, the cost of these methods is considerably less than that of a survey or analytic research design. Limiting factors are the qualitative nature of the information and concerns about the generalizability of the finding (16). In general, the overall result showed a positive attitude from most participants of the discussion toward integrating leprosy into the GHS. Therefore, there is a need to create a forum for discussion among all stakeholders in leprosy control activities on methods of integration. Based on the results of the discussion, a clear policy on the process of integration is required. Acknowledgement The authors would like to thank NSL for financial support, KIT for tecnical assistance through Dr. Prisca Zwanikken, Mr. Leon Bijlmekers and Dr. Peter Lever and ALERT for its institutional support. Finally our gratitude is extended to Ministry of Health officials at different levels, participants of the discussion and the SNNPR Health Bureau for their continuous support through out the study time. References 1. WHO, A Guide to Eliminating Leprosy as a Public Health Problem. Document for Action Program for the Elimination of Leprosy, WHO, 1995;95:1. 2. WHO, Weekly Epidemiological Record. WHO, 1993. 3. Peter Feenstra. Leprosy Control Through General Health Services and/or Combined Programs. Leprosy review. 1993;64:89-96. 4. Becx-Bleumik M. New Developments in ALERT Leprosy Control Program and the Issue of Integration. Ethiopian Journal of Health Development. 1994;1:49-55. 5. Bart Criel, Vincent De Brouwere, Sylvie Dugas. Integration of Vertical Programs in Multifunction Health Services. Studies in Health Services Organization and Policy 1997;3. 6. MOH, Health Policy of the Transitional Government of Ethiopia. MOH, Sept. 1993. 7. WHO, Integration of Health Care Delivery, Report of a WHO Study Group. WHO Technical Report Series, 1996;861. 8. Anita NH. Leprosy and Primary Health Care: The Mandwa Project, India. Leprosy Review 1982;53:205-209. 9. Becx-Bleuming M. Priorities for the Future and Prospects for Leprosy Control. International Journal of Leprosy. 1993;61:82-101. 10. Fine PEM, Leprosy and Tuberculosis, an Epidemiological Comparison. Tubercle. 1984;65:137153. 11. Ad de Rijk Combining Tuberculosis and Leprosy Services in one Program. Ethiopian Journal of Health Development. 1984;1(2):37-43. 192 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── 12. Bainson KA, Integrating Leprosy Control into Primary Health Care: The Experience of Ghana. Leprosy Review. 1994;65:376-384. 13. Wandroff DK and Wandroff J A, Leprosy Control in Zimbabwe: from a Vertical to a Horizontal Program. Leprosy Review 1990;61:183-187. 14. Myint T and Htoon MT, Leprosy in Myanmar: Epidemiological and Operational Changes, 198592. Leprosy review. 1996;67:18-27. 15. Roos BR, Van Brakel WH and Chaurasia AK. Integration of Leprosy Control into Basic Health Services, an Example from Nepal. International Journal of Leprosy. 1995;63:422-429. 16. Corlien M. Varkevisser, Indra Pathmanathan, Ann Brownlee, Designing and Conducting health System Research Projects. Health System Research Training Series, 1991;Vol.2:Part-1, IDRC. Original article Retrospective study of childhood experiences of persons with disabilities and high achievement profiles in Ethiopia Tirussew Teferra Abstract: An attempt was made to examine early psychosocial home and school conditions of persons with disabilities and high achievement and resilient personality qualities. The subjects were persons with hearing, visual, and motor impairments. Structured and semi-structured questionnaire and focusgroup discussions were employed for collecting field data. Over 82% of the participants reported that they had a conducive psychosocial home environment in their early childhood development which was manifested in the form of mutual understanding, affection, acceptance, and provision of back-up support. A t-test result also revealed no statistically significant differences (α = 0.05) across the different disability groups. Furthermore, high correlation coefficient (r = 0.89) but no statistically significant differences (α = 0.05) were found between early psychosocial experience of the participants and their current home interaction. It is suggested that the quality of early familial psychosocial support for children with disabilities play a vital role for their subsequent achievement and success in life. [Ethiop. J. Health Dev. 1999;13(3):195-204] Introduction A number of people still take the general hereditary view of achievement potential, which in its extreme form, considers that the ultimate level of an individual's functioning is determined solely by his/her genetic endowment (1). They often assume that a baby with disability (special need) will lead a damaged life. They place the label "handicapped" on such a baby and think that the child's physical condition will, in and of itself, limit and define the person’s being. In the current understanding, disability constitutes a necessary but not a sufficient condition for a handicap (2). The greater the environmental resources, the less the individual’s disability are likely to result in a handicap (3). If society has the right understanding and attitude towards persons with disability and if persons with disabilities (special needs) are provided with the necessary care, upbringing, as well as medical and educational services, they will be able to lead a quality of life like any fellow citizens in the country. Indeed, the basis for the enhancement of the potential of persons with disabilities is opening equal opportunities through creating a conducive social environment. That is, in contrast to the onedimensional traditional model, which focuses on the singular (mainly on the deficit), considering the individual's behavior as a product of the dynamic transactions between the individual (personal factors) and interlocking environmental factors (social factors) at different stages of development seems to be valid (4,5). Therefore, it should be noted that all human beings need to be considered as open systems, liable to be meaningfully modified by environmental intervention (6). The brain’s ability to adapt with experience confirms that early stimulation sets the stage for how children will continue to learn and interact with others throughout life (7). Studies indicate that the capacity to be modified as a result of learning is a characteristic of human beings throughout the entire _______________________________________ Department of Psychology, Addis Ababa University, Addis Ababa, Ethiopia life span (8,9). Children are most susceptible to environmental effects in the early developmental years. They learn several generalized expectations that have the potential of affecting most of their lives. Evidences suggest that there is a clear connection between a child’s ability to settle in a school and the 194 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── school results, and the quality of time he/she has spent together with his/her parents (10). The holistic development of children requires environments in which children feel secure, are stimulated, and have opportunities to explore, to question, to experiment, to play and to symbolize. If young children’s psychosocial needs are neglected, the consequence may be an increasing number of children, youths, and adults who cannot effectively participate in the socio-economic development of society or who feel no need for it (11). Vulnerabilities established during infant and toddler years, in particular, may become evident during later developmental periods (12). The tendency to overlook the role of environmental factors and explaining the behavior of a child with disability as disposition drafting “within individual deficits” is fallacious. Such a paradigm not only distorts our understanding of the problem but also misguides the focus of attention and type of treatment or intervention to be employed for children with special needs (13). The main intention of this study was to explore the nature of early childhood home and school experiences of persons with hearing, visual, and motor impairments of relatively high achievement profile in the country. The investigation was envisaged to help assess the existence of a link between the type of early psychosocial experience and the present living conditions of the participants. The degree of differences or similarities of early childhood experiences among the three groups were examined. Further more, an attempt was made to identify the problems encountered and coping strategies employed to overcome the challenges faced by the participants at different social settings. The data generated through this study is presumed to be a useful learning experience for children with different types of disabilities; and parents, caregivers, teachers, as well as others dealing with such children. Methods The study was carried out in March 1998 in Addis Ababa. The scope of the study was delimited to three groups of persons with disabilities, namely, persons with hearing, visual and motor impairments. Purposeful sampling technique was used to select the participants of the study. Ninety participants were selected with the help of the Ethiopian National Association of the Deaf (ENAD), the Ethiopian National Association of the Blind (ENAB), and the Ethiopian National Association of the Physically Handicapped (ENAPH). The selection criteria set were that the participants should be relatively good achievers, independently leading their livelihoods without any economic constrains. A questionnaire consisting of structured and semi-structured items, and focus-group discussion schedules were developed and employed for collecting data. By using the retrospective approach, attempt was made to explore and map-out the quality of early psychosocial conditions focusing on: Mutual Understanding; Love, Acceptance and Tolerance; and Sharing of Responsibility. These are essential variables, which are considered to be the foundations for promoting feelings of confidence, trust in one's potential, and surrounding as well as for subsequent effective functioning (4,9,8,10,16). A Likert type of four-measure scales were constructed as follows: Strongly Agree = 4, Agree = 3, Disagree = 2, and Strongly Disagree = 1. These options were given to the participants to indicate their degree of agreement or disagreement against the three psychosocial components. The scale has a reliability coefficient of 0.807 as determined by Cronbach alpha with a standard error of measurement of 2.886. Among the ninety copies of questionnaires distributed, 85.5% or 77, that is, 27 by the visually impaired persons, 25 by the hearing impaired and the remaining 25 by persons with motor impairment, were properly completed and returned. The focus-group discussions were held with the executive members of the respective three national associations. The sizes of the focus-group discussions ranged from five to seven. A combination of quantitative and qualitative data were generated and analyzed using the necessary software whenever the need arose. Results Background data of the participants: The age groups of the participants are 18-29 (38.9%), 30-39 (25.9%), 40-50 (22%), and over 50 (1.2%). Their sex-mix indicates that 83.1% are males while 16.8% Retrospective study of childhood experience 195 ──────────────────────────────────────────────────────────── are females. As it is very true for the general population, gender disparity is clearly observed among the respondents who were identified as high achievers and leading successful lives. As to their religions, they were found to be believers and the vast majority (76.6%) pursuing the Ethiopian Orthodox faith. Most of the respondents (60.8%) have successfully completed tertiary education (see Table 1). Even those with lower educational background were found to run their own business, earn a reasonable income, have their own families and lead independent and successful lives. According to the participants of the study, the time of onset of the impairments and the possible causes of their respective disabilities were reported as follows (Figures 1-4). Table 1: Educational level of the respondents Type of Disability Item Hearing Visual No % No 1. Grade (8-12) 13 52 2 2. Certificate 2 8 1 3. Diploma 8 32 4 4. B.A/L.L.B 2 8 17 5. MA 1 6. MD 7. Church School 2 8. No Response Total 25 100 27 Figure 1: Specific time of onset of disability % 7.4 3.7 14.8 63.0 3.7 7.4 100 Motor No 7 2 4 9 2 1 25 % 28 8 16 36 8 4 100 Total No 22 5 16 28 1 2 2 1 77 % 28.6 6.5 20.8 36.3 1.3 2.6 2.6 1.3 100 196 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Figure 2: Causes of motor impairment As reported by the participants of the study, the causes were predominately attributed to infectious childhood diseases and accidents. It was interesting to note from the focus-group discussions that, reported among other factors, accidents, and the use of corporal punishment at home and school (hitting the head, slapping, pinching, spanking, whipping, long time kneeling, etc.) for disciplinary purpose were identified as antecedent for different types of impairments. For instance, the ear is one of the parts of the body exposed for physical punishment in our culture. That is, pinching the lobe, or slapping on the ear, is usually considered as a normal type of punishment at home as well as at school (14). Studies have established that, depending on the degree of pinching or slapping, this can cause a rupture in the eardrum and create hearing difficulty (15). Figure 3: Causes of hearing impairment Early childhood psychosocial experience at home Eighty two per cent of the respondents confirmed that their relationships with their parents understanding type, while 18% disclosed the existence of unsatisfactory understanding with their parents. It is important to note that among those who positively evaluated the quality of interaction with their parents, 42.8% have expressed a very strong feeling about the understanding of their parents. The responses regarding whether the nature of parent-child interaction was loving, accepting and tolerating type were also equally positive like that of the antecedent item. The last component was whether the respondents were given a share of responsibilities in performing household chores or not. Accordingly, 72 % confirmed that they were Retrospective study of childhood experience 197 ──────────────────────────────────────────────────────────── given responsibilities to carry out at home whereas the remaining 28% were not given. A t-test result based on the weighted responses of the Likert type scales has also shown that there is no statistically significant difference (Table 2) among the three groups on the nature of psychosocial home environment during their childhood period. Figure 4: Causes of visual impairment Furthermore, an attempt was made to find out the relationship between early psychosocial home environment and the state of the participants’ current emotional climate. The sum total scores of the responses against the Likert type of scales on the state of early childhood family experience and the current Table 2: T-test result on early childhood experience among the participants Variables Cases Mean SD 2-Tail sig. t- Hearing impairment Visual impairment 13 13 18.4615 18.3077 20.871 16.874 0984 value .02 Hearing Impairment Motor 13 13 18.4615 17.5385 20.871 17.961 .905 .12 Visula Impariment Motor (=0.05) 13 13 18.3077 5.7692 16.874 17.961 .911 .11 familial interaction were compared and the following result was obtained (Table 3). As the correlation coefficient (r=0.89) indicates there is a high correlation between the quality of interaction one has received during his/her childhood period and what one practices at home as an adult. A t-test was also run on the same item and no statistically significant difference was found between the two scenarios (Table 4). An attempt was also made to assess the state of the marital status of the parents of the participants. The finding depicts the following profile: living together (48.5%), widowed (33%), divorced (10.6%) and separated (3.8%). A look at the size of the family indicates that it ranges from 1-5 to 12-14 and almost half of the subjects’ family was found to have 6-8 family members under their responsibility. Early school experiences of the participants The participants were asked to indicate whether they had access to early childhood education or special education services. About 40% had access to early childhood education, while 57.1 % did not. Among the former, 31.1% went to church schools, and only 9% 198 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── attended the so-called “modern” preschools. That is, most of them did not have access to early childhood education. Early childhood educational experience is particularly essential for children with disabilities for cognitive, sensory, communicative stimulation as well as social competencies, which are the corner stones for subsequent learning (13). This obviously needs due consideration on the part of the government as well as the general public at large. On the other hand, 40.2% of the participants had the opportunity to attend special primary schools, while about 57% of the participants pursued their education in regular school settings with nondisabled students. Further breakdowns of the data by type of disability displays that the visuallyimpaired (77.7%) and the hearing-impaired (40%) were the most beneficiaries of special school programs. Relatively speaking, most of the special needs of children with motor impairments can be easily accommodated within the regular school setting, though they still require special equipment, appliances and physical adaptations to overcome the physical barriers which may limit their mobility and Table 3: Correlation index of childhood interaction and the current home interaction Range of agreement Childood interaction Current home interaction Strongly agree 143 104 Agree 62 90 Disagree 10 17 Strongly disagree 2 21 No response 17 2 r=0.89 Table 4: T-test result on early childhood interaction and current home interaction variables Cases Mean SD 2-tail sig. early childhood interaction 13 54.3077 53.153 .712 Current home interaction 13 64.0769 77901 t-value .37 access to various instructional materials. Regarding age of enrollment almost half of the participants registered between five to eight. The remaining, except the 10% who did not respond to this item for joined school at the ages of nine and above. That is, a good number of the participants joined primary school at the right age placing them at an advantage. Generally, evidences indicate that going to school early is actually unusual for children with disabilities in the country. Furthermore, the participants noted down a list of problems encountered and coping strategies they utilized to overcome the challenges during their initial years of integrated school settings. The major and common problems faced across the three disability groups include: being undermined and ridiculed by teachers and non-disabled students, lack of special educational provision or support, and in-accessibility of school facilities. It was further noted that distorted understanding, socio-cultural misconceptions, and misrepresentations such as being perceived as cursed, dependent, unable to learn, and special creatures were wide-spread in the school community. The results of the focus-group discussions also revealed that such unfavorable phenomena negatively impacted a lot on the range and degree of their interpersonal relationships, like being unable to mix-up with non-disabled persons in social gatherings, to play games and develop heterosexual relationships. Moreover, it was reported that the aggregate effect of these conditions has been recorded as the major cause for psychological maladjustment, low academic performance as well as high dropout rate among most children with disabilities. According to most of the participants of the study they were able to withstand all these adverse situations and to succeed in their education because of their personnel strengths and social protective factors. They reported that coping mechanisms such as accepting one’s disability, being tolerant, exerting effort to learn and develop one’s potential, showing one’s own potential through creativity and innovation, trying to be accepted by others, creating close relationships with students, and efficient time management had assisted them to overcome the challenges they faced. Moreover, 36.3% and Retrospective study of childhood experience 199 ──────────────────────────────────────────────────────────── 24.6% of the participants indicated that family members and peers respectively, were the persons consulted in time of crisis (personal, social, educational etc.) during their school years. Discussion The nature of emotional climate, particularly the quality of parent-child interaction in which children were brought up are the foundations for cognitive, social, and communicative growth and development of children (16,10). Throughout the life course, the nature of the person's primary relationships with family and friends represents one of the crucial "proximal processes" considered as the engine of development (17). The aspects of the psychosocial component, which encompasses the emotional, as well as the interactional pattern with parents included in this study were mutual understanding, acceptance, affection, and tolerance, and the caring and supportiveness of the family and the degree of sharing of responsibility in the family affairs. For all except sharing of responsibility, over 82% of the respondents were positive about the components of psychosocial conditions of the home environment. Regarding sharing of responsibility, only 72% indicated that they were doing certain household chores. A t-test result revealed no statistically significant differences (α = 0.05) on the psychosocial dimensions across the three disability groups. This study has also revealed that almost half of the participants (43.6%) were from single-headed families whereas the remaining 48.5% was from nuclear families. Several studies have confirmed that children brought up in twoheaded families tend to have strong emotional bondage and affection, which are essential for children‘s mental health and effective functioning. If this is interrupted by divorce, death, desertion or separation, the child's psychological wellbeing will be adversely affected (5, 18). When parents split up, children suffer from pain, confusion, hate, bitter disappointment, and a sense of failure and self-doubt. No matter how unhappy a marriage has been, its break up usually emerges as a shock to children (5,19). Besides, the economic consequences as well as the increase in the load of childcare and management responsibility on the single-headed family should not be under-estimated. However, in this study children brought up from the two different family settings tend to have shown similar achievement profiles and success in life. In this case, one may argue that there could be other additional factors such as the personal resilient qualities of the children, the profile of the single-headed family , the time and cause for the loss, might have positive effect on their overall performance. This could be an area of interest for further investigation. A look at the size of the family of the parents of the participants indicates that it ranges from 1-5 to 12-14 and almost half of the subjects’ family was found to have 6-8 family members under their responsibility. Against all the adverse consequences of having a large family, one can also argue that in a family where there is a child with disability, members of the family can be an asset rather than a liability. For example, such a child with disability can have multiple stimulation or a wider possibility of interaction, care and playing. In a country like Ethiopia, where shared responsibility among the extended family (including grandmothers, grandfathers, aunts and others) is still more or less practiced, one should be able to capitalize this resource through organizing sensitization and training programs to empower family members so that they can provide appropriate assistance within the context of the home environment. Another attempt was made to examine the degree of relationship between early childhood psychosocial experience of the participants and the quality of their current home psychosocial interaction. The findings revealed high correlation coefficient (r = 0.89) and no statistically significant differences (α = 0.05) between the two variables (see Tables 3&4). The result obtained goes along with other studies which show that the type of treatment or experience one had during childhood period more or less influences his/her current adult-child pattern of interaction, though there are possibilities of being affected by contemporary situations (20). That is, whatever is invested during childhood period pays a lot for the achievement and success of the person in the later years of life. The inability to develop a set of protective resources early in life not only produces early dysfunction, but 200 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── also provides the basis for enhanced life-time exposure to stress, vulnerability and dysfunction (5,11). Achievement and self-esteem seem to be highly interrelated and one influences the other. Nonetheless, the foundation for achievement seems to be positive self-esteem, which has to be cultivated early in life. Low self-esteem is often cited as the ultimate source of poor academic achievement and self-destructive behavior (5). This, in one way or another affects the personal growth of the person as well as his/her role and status in the society at large. The type of self-esteem the child withholds is, by and large, dependent on his/her surrounding (21). Particularly, the type of early childhood upbringing, early school experiences, and peer relations play vital roles in molding the child's self-esteem (13,16). Indeed, the opinions of significant adults (parents, teachers etc.) have an impact on a child’s level of self- esteem. For example, parents or teachers who view a child as competent or attractive communicate their opinion to the child, who eventually internalizes these opinions and begins to view himself/herself accordingly. On the other hand, adults who view a child as unattractive or incompetent also communicate these opinions to the child, who eventually internalizes them and forms unfavorable opinion of himself/herself as well as his surrounding. A child who develops positive self-esteem will become confident about his/her abilities and is likely to become an adult who respects others and will work well and help others with a strong sense of social interest (22,23). Those who consider themselves as effective are usually willing to attempt some solution to whatever problem they face, and they will not give up easily in their efforts to overcome some obstacles. The precondition for adequate functioning is developing self-efficacy (18,23). That is, like having a sense of “I can do it by myself,” “I have the potential to learn and develop” and “I can contribute to my family or community.” It can, therefore, be argued that positive upbringing through which the participants of this study have passed might have assisted them for the development of selfefficacy and subsequent successful functioning. As to the early school environment, the participants, particularly those who were placed in an integrated setting, had faced unfavorable cognitive-affective and instructional conditions indicating the need for an intervention for better adjustment and achievement. However, the participants revealed that they had overcome the problems through employing coping strategies such as accepting one’s disability and being tolerant, personal effort to learn and develop one’s potential, showing one’s own potential through creativity and innovation, trying to be accepted by others, trying to create close relationship with students, and efficient time management. They further declared that, in times of crisis, they consulted the family (36.3%) and peers (24.6%) to help them resolve their personal problems. In this respect, it is worth noting that recent studies have established the effectiveness of peer mediation therapy, particularly in an integrating setting where both children with disabilities and their nondisabled partners are pursuing their education (22,23). Peer-mediated interventions may also facilitate the mainstreaming of children with disabilities. School counselors or teachers can use this student–tostudent learning structures to provide appropriate academic instructions and practice through initiating peer tutoring or co-operative learning. These structures can provide students with opportunities to develop and to practice social and problem solving-skills (25,26). Moreover, fostering peer relationships can provide feelings of support, belonging, acceptance, and caring. Finally, on the basis of the findings of this study, the following observations are made: The early childhood psychosocial experience of the home environment of the three groups involved in the study was found to be conducive. This might have, to a certain degree, influenced the achievement of the participants. A high correlation, and no statistically significant difference, were found on the quality of early psychosocial experiences of the participants and the nature of their current home interaction. Almost half of the participants came from single-headed families indicating that their personal resilient qualities, and the quality of family interaction might have also contributed to overcome the adverse conditions that accompany single-headed family. This calls for further investigation. The unfavorable school experiences encountered by the participants of the study (such as low Retrospective study of childhood experience 201 ──────────────────────────────────────────────────────────── expectation, mockery, exclusion, lack of back-up support) were overcome through using coping mechanisms which involve personal factors (elements of individual strengthens) and social factors (consultation of parents and peers). The causes of disability as reported by the participants of the study seem, to a greater extent, to be preventable if proper family, community, and school-based health education as well as the necessary basic childcare services are put in place. 202 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Acknowledgments This paper is a part of the study entitled “Persons with Disabilities of High Achievement Profile and Resilience in Ethiopia” is part of the project, which was financed by Rädda Barnen (Save the Children Ethiopia). References 1. KirK SA, Gallagher JJ & Anastasion NJ. Educating Exceptional Children.7 rev. ed. Boston: Houghton Mifflin Company, 1993. 2. UNESCO. Helping Handicapped Pupils in Ordinary Schools: Strategies for Teacher Training. Paris: UNESCO Headquarter, 1985. 3. Tirussew T. Psychosocial and Educational Profile of Students with Disabilities in Addis Ababa University. Ethiop J Health Dev. 1994;8(1):44-61. 4. Bronfenbrenner U. Ecology of family as a context for human development perspectives. Developmental Psychology1986;22(6):723-742. 5. Haggerty RJ, SherrodLR, Gramezy N & Rutter. Stress, Risk, and Resilience in Children and Adolescents. UK: Cambridge University Press, 1996. 6. Feuerstein R & Rynders RJ, Helping Retarded People to Excel. London: Polonium, Press, 1988. 7. Newberger JJ Young Children . National Association for Education of Young Children 4 -9, 1997:52(4) NW, Washington DC. 8. Feuerstein R. The Dynamic Assessment of Retarded Performers. New York : University Park Press, 1979. 9. Feuerstein R. Klein P.S. & Tannenbaum A.J. Mediated Learning. Experience : Theoretical Psycosocial Learnign Implications. London: Freund Publishing House LTD, 1991. 10. Rye H. When You and I are Together. A Guide for Parents. Oslo: ICDP, PDC, 1997. 11. Hundeide K. Helping Disadvantage Children : Psycho-social Intervention and Aid to Disadvantaged children in Third World Countries. London: Jessica Kingsley. 1991. 12. Guralnick M. The Next Decade of Research on the Effectiveness of Early Intervention , journal of Exceptional children, 1991. 13. Bernard van Leer Foundation. Building on People's Strengths: Early Childhood in Africa. The Hague: Emmerik & Emmerik, 1994. 14. Fransua Dansa. Hard of Hearing and Clssroom Interaction: Their Effects on Social and Academic Performance (MA, Thesis). Finland : Joensuu University, 1998. 15. Tate M. Principles of Hearing and Audiology .Conson Glasgow, 1994. 16. Klein P, Hundeideide K, Tirussew T, Lakew W, Pramling I, Fuglesang A. et al. Early Intervention Cross-cultural Experiences with Mediational Approach. New York Garland Publishing , INC,1996. 17. Gore S. & Eckenrode. Contex and process in research on risk and reilience.In R. J. Haggerty, L.R. Sherrod , N. Gramezy & M.Rutter (Eds.).Stress, Risk and Resilience in Children and Adolcesents (pp.19-63). UK: Cambridge University Press, 1996. 18. Dlugokinski EL & Allen SF. Empowering Children to Cope with Difficulty and Build Muscles for Mental Health. USA: Taylor & Francis, 1996. 19. Papilla DE. A Child’s World, Infancy through Adolescence . New York: Mcgraw-Hill Publishing Company, 1990. 20. Bowlby JA Secure Base. Clinical Applications of Attachment Theory.UK: J.W. Arrowsmith Ltd., Bristol, 1992. 21. Apter T. The Confident Child. Emotional Coaching for Crucial Decade : Ages Five to Fifteen.New York: W.W. Norton & Company, Inc., 1997. 22. Marion M. Guidance of Young Children. Columbus: Merrill Publishing Company,1987. 23. Bandura A. Self-efficacy mechanism in human agency, American Psychology, 1982;37:122-147. Do parents and young people communicate on sexual matters? 203 ──────────────────────────────────────────────────────────── 24. Stone J & Campbell. Student to Student: Curriculum and Development of Peer Relationships. In G.L.Porter, & D. Richler (Eds.), Changing the Canadian Schools . Perspectives on Disability and Education. Canada, York University: The Roeher Institute, 1991:239-256. 25. Maher Chareles A. Zins Joseph E.. Psychosocial Interventions in the Schools. Pergamon General Psychology Series. Oslo: UNIPUB , Akademika, 1987. 26. Kelly B, & Otter den J. Beyond Behavior: A Case of Social Intervention Strategies for a Student with Challenging Behaviors. In G.L.Porter, & D. Richler (Eds.), Changing the Canadian Schools. Perspectives on Disability and Education. Canada, York University: The Roeher Institute, 1991:257280. 204 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Original article Do parents and young people communicate on sexual matters? The situation of Family Life Education (FLE) in a rural town in Ethiopia Negussie Taffa1, Rahel Haimanot 2, Selamu Desalegn 2, Alemayehu Tesfaye 2, Kedir Mohammed2 Abstract: As a result of a cultural taboo, adolescents in many developing countries rarely discuss sexual matters explicitly with their parents. Most information for their patchy knowledge often comes from peers of the same sex, who may themselves be uninformed or incorrectly informed. This report is a summary of two surveys carried out on two occasions (November 1996 and October 1997, respectively) on 343 high school students and 246 families who had children 10-24 years of age in a rural town 160 Km south of Addis Ababa. The purpose was to assess the awareness and attitude of both study groups on major Family Life Education (FLE) components and know the level of parentadolescent communication on matters related to young people’s sexuality. Findings suggest that young people’s knowledge on aspects of their sexuality is incomplete and not enough to minimise risk-taking. Yet, more than half of them believed that is unacceptable to discuss growth changes and sexual issues with parents during adolescence. Different grade and age levels did not influence the consensus except for a female sex, which significantly favoured this negative attitude. For some who approved discussion (sexual matters and contraception), peers were preferred most. Furthermore, 31.5% of the students were sexually active, and 65.7% of the sexually active ones reported use of some contraception (including calendar method) in the past. Likewise, parents had a partial knowledge regarding adolescent sexual maturation and behaviour or complication of teenage pregnancy. Nonetheless, 93% did not approve premarital sex and ironically, not more than 20% of them reported discussion of growth changes during adolescence, sexuality, and contraception in the past. However, parental education and lower family size positively influenced this attitude and practice. Implications of the study were discussed and recommendations made on future needs to initiate a comprehensive FLE in the school system and increase the responsibility of parents in adolescent sexuality. [Ethiop. J. Health Dev. 1999;13(3):205-210] Background Family Life Education is the type of education an individual receives to prepare him/her for adult life. It includes education about the family, human growth and development, adolescent problems (health and disease), sexuality, family planning, and responsible parenthood, etc (1). World Health _______________________________________ 1 Department of Community Health, Faculty of Medicine, P.O. Box 9086 Addis Ababa University, Addis Ababa, Ethiopia; 2Senior Medical Students, Faculty of Medicine, Addis Ababa University, Addis Ababa, Ethiopia Organisation (WHO) defined adolescence (10-19 years) as progression from appearance of secondary Do parents and young people communicate on sexual matters? 205 ──────────────────────────────────────────────────────────── sexual characteristics to sexual and reproductive maturity, development of adult mental process and identity, and transition from total socioeconomic dependence to relative independence (2). Adolescents comprise about a quarter or more of developing countries' populations and this figure appears to be on the increase for the next three decades to comeInformation as a valuable means to delay an early initiation of sex in adolescents should have started early at home by the family and primary school teachers. However, the fact that families in rural communities are either not knowledgable about the subject matter or due to their nature of extendedness, they are not able to give due consideration to the importance of educating young boys and girls on sexuality, parenthood, and other matters. Moreover, such matters are often viewed as a sign of eroded societal values and norms and thus are not welcomed by traditional societies (3,4,5). Policy-makers and the school community, on the other hand, seem to have understood the difficulties only late. This situation, when coupled with the cultural taboos in poor countries that influence decision-making on sensitive issues, such as adolescent sexuality, makes inclusion of Family Life Education (FLE) into school curricula a tough challenge. It is with such a dilemma that we face horrifying figures on the growing rates of illness and death from clandestine abortions, STI’s, and HIV/AIDS, and their remaining social and economic consequences today. The following report is a summary of two surveys carried out on two different occasions in Zway, a rural town located 160 km south-east of Addis Ababa. It was done on high school students and families who have children in the age range of 10-24 years. The purpose was to assess their awareness status and attitude on adolescent sexuality, teen-age pregnancy and its complication, HIV/AIDS and STI, etc (essential components of FLE). These surveys have also attempted to assess the attitude and behaviour regarding parent-youth communication on reproductive health matters at home environment and level of young peoples’ sexuality. Methods Two cross-sectional surveys were carried out in November 1996 and October 1997, on high school students and parents (mostly family heads) who had children aged 10-24 years in Zway, a rural town 160km south of Addis Ababa. A statistically representative sample size was calculated with a 95% significant level and a power of 80% in each case. Multi-stage stratified sampling method was used to obtain study subjects from a list of student rosters in the school (students) and kebele (smallest administrative unit) residents registers in the town (parents). Both students and parents were provided with self-administered a structured questionnaire that was filled anonymously. In both cases, an informed consent was initially obtained. Cultural sanctions on the sensitive nature of the issue were taken care of for parents by gender aggregation of the interviewee and interviewers. Data were collected by senior medical students. Analysis was made using EPI-INFO version 6 statistical software. Results General: Three hundred and forty-three students and 246 adult subjects were studied. Table 1 shows some of the sociodemographic characteristics of the parents. Students were from 9 th to 12 th grades, constituting 38.8% (9th), 28.6% (10th), 21.9% (11th), and 10.8% 206 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Table 1: Sociodemographic characteristics of the parents, Zway, 1996-97. Variables Frequency N= 246 Percent - Relation to the youth under consideration Biological (father/mother) 234 95.1 Foster families 12 4.9 - Education Illiterate Primary education Secondary & above - Occupation 59 106 81 23.9 43.1 32.9 Housewives Employed(private/gov’t*) Small scale merchants Others - Current marital status 123 46 41 36 50 18.7 16.7 14.6 184 62 74.8 14.6 Married Widowed/divorced/ separated Age range was 30-69 Yrs.; (69.5% in the age range of 30 to 49 years) * government Table 2: Knowledge and attitude of the students pertaining to important variables on reproductive health, by sex, Zway, 1996-1997. Variables Males Females OR(95% CI) (N= 218) (N= 125) - It’s normal & acceptable to have 178 (81.6%) 69 (55.2%) 3.6(2.15 sexual feeling during adolescence - Duration of normal menstrual flow 122 (55.9%) 108 (86.4%) 5.0(2.72 correctly known - Correctly knew the unsafe period 25 (11.3%) 18 (14.2%) 1.19(0.59 in the menstrual cycle (12th). Their age range was 14-25 years (mean age = 17 years). The two groups were homogeneous in terms of their ethnic and religious backgrounds (most were Oromo and Orthodox Christian). Students: Fifty four percent of the students felt that it’s culturally shameful to discuss about physical and psychological changes during adolescence (explained to them using examples), though males were relatively free to discuss compared to the female students (OR= 0.58; 95% CI = 0.36,0.93; P<0.02). There was no significant difference among students of different grades (Chi-square for trend = 0.36; P>0.05). Being a female student negatively influenced the tendency to admit that increased sexual feeling during adolescence is normal and acceptable (Table 3). Seventy five percent of the students preferred to discuss about body changes that occur during adolescence with peers of the same sex, none of them wanted it to be with their parents. Regarding the knowledge on other aspects of human reproduction, 74.9% correctly knew the age at menarche and 67.1% knew the average duration of menstrual flow, with dominance of female students (Table, 3). Senior class students were not better knowledgeable compared to the junior ones (Chi-square for trend = 0.2; P >0.05). Of the total, only 13.2% knew the unsafe period during the normal menstrual cycle, and even females were not better off in this aspect (Table 3). Grades did not have any effect in discriminating knowledge on safe period of menstrual cycle either (Chi-square for trend = 2.8; P>0.05). Hundred and eight of the 343 students (31.5%) reported to have had sexual contact before the date of the survey and males were significantly higher in number (OR= 8.3; 95% CI = 4.1,17.3; P<0.000). Seventy one percent of the total knew some form of contraception, most frequently being condoms, Oral Contraceptive Pills (OCPs), Calendar method, and Intra-uterine devices (IUDs) in that order. Among the sexually active, 65.7% reported to have used some form of contraception in the past. Do parents and young people communicate on sexual matters? 207 ──────────────────────────────────────────────────────────── Condom and Calendar methods were the most frequently used ones, 69.7% and 24.3% respectively. Female students resisted the idea of use of contraception at their age more than their male counterparts (OR = 3.56; 95% CI = 2.19,5.82; P < 0.000). Two hundred and twenty nine (66.7%) of the respondents said that they never want to discuss issues of contraception with their parents. Fifty four percent of those who approved it preferred peers of the same sex to discuss with. The appropriate age at first pregnancy (18 years) was known by 223 (65%) of the surveyed students, but 64.5% of them (including those who did not know the ideal age) did not give correct answer(s) regarding complications of abortion to the mother. Ninety five (27.7%) respondents were able to correctly name three commonly known Sexually Transmitted Infections (STIs) (Syphilis, Gonorrhoea, and Chancroid) and 70% and 78.8% of them, respectively, knew the correct routes of transmission and the right action to take whenever infected. The primary source of information for such knowledge was Table 3: Comparison of responses given by the parents and the students regarding selected adolescent reproductive health matters, Zway, 1996-97. Variables - Disapproved pre-marital sex - Age at menarche correctly known - Safe period in menstrual cycle correctly known Parents N=246 228 (92.70%) 148 (60%) Students N=343 247 (72.0%) 257 (74.9%) OR(95% CI) 4.92(2.81 0.51(0.35 65 45 2.33(1.49 (26.4%) (13.2%) said to be schools in 54.8%, while parents served as a source of information for only 9.3% of the students. Parents: Nearly 94% of the 246 subjects admitted that there are some physical and psychological changes that take place during puberty. However, only 148 (60%) of them reported the correct age range for puberty in females, and only 105 (42.7%) knew the corresponding age for males. It is only 65 (26.4%) respondents who correctly told the safe period in the menstrual cycle. Ninety three percent of the parents had a negative attitude towards premarital sex, though later on, 151 (61.4%) approved use of contraception in cases of unprecedented sexual acts in adolescents, and educational levels very much influenced this attitude (OR = 3.73; 95% CI = 1.99, 7.02; P<0.000). Only 66 (26.8%) of the parents said that teenage pregnancy is associated with difficulties in childbirth. Two hundred and six (83.7%) mentioned two commonest types of STIs (gonorrhoea, and Syphilis), and only 70 (28.5%) believed that STIs predispose a person to HIV/AIDS. On the assessment of their practice regarding communication on sexual matters with their children, 51 (20.7%) admitted to have discussed about teenage pregnancy and its complications, 31 (12.6%) on contraceptive use, and 26 (10.6%) on physical and psychological changes at puberty, some time in the past. Educational level above primary school very much influenced having positive attitude regarding discussion between parents and the youth on adolescent reproductive health matters (OR = 3.82; 95% CI = 1.7,8.9; P<0.0005). Free discussion on adolescent sexuality and contraception between parents and the youth was relatively seen more among families with fewer size (< 5 people) than larger sized families (OR = 2.28; 95% CI = 0.98,5.36; P= 0.057). Comparison of the youth and parents on selected knowledge and attitude variables (Table 3) revealed that there are significant differences of practical importance as far as managing reproductive health problems of the adolescents is concerned. Discussions This study has shed light on the issue of adolescent sexuality and problems faced to obtain the necessary information that would have shielded them from the brunt of unprotected sex and its socioeconomic consequences in the rural Ethiopian context. Similar to what has been described by other 208 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── investigators (4,5,7-10), the knowledge of young people about different aspects of their sexuality is incomplete and not enough to avoid risk-taking. Further more, the fact that students of different grades did not differ significantly in their knowledge on selected aspects of reproductive health, indirectly indicates that no such education is being provided even at the school setting. Females were more affected (believed in the shamefulness of discussion on sex, thought that sexual feeling during adolescence is unacceptable, and disapproved contraceptive use during this period) possibly because of the cultural sanction imparted on them by the society. This finding appears to be consistent for other developing countries as well (8,9). However, in some communities where this is not the case, some researchers indicate that female adolescents who practised contraception had a positive image of their parents, with whom they communicated frequently about intimate subjects such as menstruation and avoidance of untimely pregnancies (6,7). Thus, young people disapprove discussing growth changes and sexuality may be just because they belong to the traditional system that considers it as a taboo. Parents were not only the non-preferred source of information, but also were not better knowledgeable on certain issues such as safe period in the menstrual cycle, the fact that STIs underlie, or predispose to, HIV/AIDS, and problems of teen-age pregnancy. To complicate the issue more, they did not approve of premarital sex and had a negative attitude towards discussion with their kids on sexual/reproductive health. But families with limited number of children (<5) and better education were comparably more liberal. Similarly, a study in Zimbabwe which involved parents and adolescents blamed lack of communication on issues pertaining to sexuality. In fact, adolescents reported obtaining sexual information, not from adult family members, but primarily from media, schools, and peers. In the same study, it was shown that, although some mothers and adolescent girls reported communicating about menstruation, most parental communication consisted of vague warnings not to "play" with boys or girls, without explaining what this euphemism means (8). Other studies coming from East Africa (Kenya, Uganda, Tanzania), Nigeria, and India also confirm the same problem (2,9,11,12). Finally, comparison of parents and students on selected variables showed some difference which was not consistent. Conclusion and Recommendations From the study it could be concluded that adolescents have an incomplete understanding of comprehensive reproductive health and discussion on sexual matters still continues to be a cultural taboo by both the youth and their parents. The youth prefer peers of the same sex to be the primary source of information on matters of reproductive health. In spite of these problems, significant numbers of the youth are currently sexually active, and few were knowledgeable of the means for safe sex. In addition to the absence of a helpful information from parents, adolescents in school set-up in Ethiopia do not seem to receive comprehensive FLE/reproductive health education from the school system or the health workers at this moment. In spite of their negative attitudes towards its discussion, adults themselves (at least in rural areas) do not have adequate knowledge on adolescent reproductive health problems. However, educational levels of the parents and lower family sizes were positively associated with free discussion on sexual matters between parents and their adolescent children. Based on the study, it's recommended that a comprehensive FLE be initiated for students in Ethiopia (at home, in the school, churches/mosques, health facilities, etc.) with a sense of responsibility assumed by all partners in this endeavour (the family, the school system, health workers, and young people themselves). Parallel to this, there is quite an enormous job waiting for health workers to educate the parents themselves for a better awareness on the issue and change of attitude and practice towards adolescent sexuality. Acknowledgements This study was made possible with relentless advisory support from the staff of the Department of Community Health, Faculty of Medicine. We would like to thank the school administration and Do parents and young people communicate on sexual matters? 209 ──────────────────────────────────────────────────────────── communities who facilitated the study to take place and most of all, the families and students who took part in the study. References 1. ICDR, MOE. Population and Family Life Education for Ethiopians. 1994. 2. Population Reports. Meeting the Needs of Young Adults. Series J Oct. 1995;41:3-10. 3. Thomas MM, Arjun A, Timothy BF, Vera HB. U.S. Department of Commerce and Statistics Administration, Bureau of The Census. Trends in Adolescent Fertility and Contraceptive use in Developing world. 1996. 4. Fisseha E, David Z, Derege K. The Attitude of Students, Parents, and Teachers towards the Promotion and Provision of Condoms for Adolescents in Addis Ababa. Ethiop J Health Dev, 1997;11(1):7-16. 5. Lisa B. Adolescent Reproductive Health in Ethiopia: An Investigation of Needs, Current Policies and Programmes. 1995 (Unpublished document). 6. Pick-deweibs S, C Afkin L, N-Gribble, Andrew P. Sex, Contraception and Pregnancy among Adolescent in Mexico City. Studies in Family Planning. March/April, 1991;22(2): 7. Nicholes D, Z Woods E, S Gates D, Sherman J. Sexual Behaviour, Contraceptive Practice and Reproductive Health among Liberian Adolescents. Studies in Family Planning. May/June, 1987;18(3): 8. David W, John M, Mandy A, Noleen M, Tendai C, Ellen W, Geeta RG. Intergenerational Communication within the Family: Implications for Developing STD/HIV Prevention Strategies for Adolescents in Zimbabwe. International Center for Research on Women (ICRW). Dec.1994:1-5. 9. Shireen J. Jejeebhoy. Adolescent Sexual and Reproductive Behaviour: A review of the evidence from India Soc Sci Med. 1998;46(10):1275-1290. 10. CERPO (Center for Applied Research on Population and Development). Youth in Danger: Results of Regional Survey in Five West African Countries, 1997. 11. AMREF. Community Perceptions Regarding Critical Adolescent Sexual and Reproductive Health: Needs and Solutions. Promotion and Education; Quarterly/December 1997;(IV/4):16-19. 12. Briggs LA. Parents’ viewpoint on Reproductive Health and Contraceptive Practice among Sexually active Adolescents in the Post Harcourt local Government area of Rivers State, Nigeria. J. Advanced Nursing Feb. 1998; 27(2):261-6. 13. WHO/UNICEF. A Picture of Health: a Review and Annotated Bibliography of the Health of Young People in Developing Countries. WHO/FHE/ADH/95.14), Geneva, 1995. Original article Assessment of the antibacterial activity of Some traditional medicinal plants on some food-borne pathogens Mintesnot Ashebir1, Mogessie Ashenafi2 Abstract: Crude preparations of four types of traditional medicinal plants used in Ethiopia, collected from local markets, were assessed for their antimicrobial activity against some food-borne pathogens. The growth or inhibition of Bacillus cereus, Staphylococcus aureus, Shigella boydii, Shigella flexineri, Salmonella typhimurium, and Escherichia coli was determined in growth media separately containing Artemisia afra (5%), Vernonia amygdalina (7%), Lepidium sativum ((2%) and Carum copticum (10%). None of the test organisms was affected by Lepidium sativum in 24 hours. B. cereus and Staph. aureus had markedly lower final counts in media containing crude preparations of Vernonia amygdalina, Carum copticum, and Artemisia afra when compared to control. Retarding effect was noted on Sh. Flexineri and Sh. Boydii in the initial stages by Vernonia amygdalina and Artemisia afra. Counts of S. typhimurium in all crude preparations were lower by about one log unit than the control until eight hours. None of the crude preparations had any effect on E. coli. The antimicrobial effect of some of the crude preparations may be considerably enhanced in traditional treatment if they are taken at four hour intervals. [Ethiop. J. Health Dev. 1999;13(3):211-216] Introduction The majority of the food-borne diseases, although self limiting, can also be life-threatening needing antibiotic therapy. But most of the aetiologic agents in many countries have already developed resistance to common antibiotics. This type of resistance is also reported in Ethiopia (1-5). In most developing countries where people are living in poor hygienic conditions, the chance of contracting food borne diseases is undoubtedly high. Due to absence of sufficient modern health care system, particularly in the rural areas, people prefer to visit traditional healers. According to Akerele Zimbabwe, for (6), 80% of the world population depends on traditional medicine. Thus they depend on traditional medicine to treat themselves. For example, 80% of the population depends on traditional medicine (7). In Ethiopia, too, a similar proportion of the population also rely on herbal medicine (8). Some traditional healers use medicinal plants. Some of these plants, although they are not investigated scientifically, can cure certain infections (9). It can also be assumed that the major part of traditional therapy involves the use of plant extracts or their active principles (6). With proper investigation these may serve as a source of modern drug. Drugs such as quinine, digitalis etc. were synthesized from medicinal plants (10). They served also as a source of intermediate compounds for synthesizing analog drugs with more desirable properties (9). In developing countries their use has helped to substitute imports of drugs, thus boosting economic self-reliance. Further more local products tend to be more readily accepted than those obtained from abroad (6). _______________________________________ 1 Department of Biology, Faculty of Science Addis Ababa University, Addis Ababa, Ethiopia; 2Institute of Pathobiology, Addis Ababa University, Addis Ababa, Ethiopia. Among African countries, Ethiopia is often quoted as one of the six countries of the world where about 60% of the plants are said to be indigenous with healing potential (11). There are about 213 families of flowering plants in Ethiopia and of these 92 families, with one family of gymnosperm and one family of fern are known to contain species with medicinal properties (12). But despite all these virtues, only few studies have been conducted regarding indigenous medicine (11). Most of such studies concentrated on extracts of the plants and not on the crude preparations, although traditional treatment usually considers crude preparations. The purpose of this study is Antibacterial activity of traditional herbs 211 ──────────────────────────────────────────────────────────── therefore to evaluate the antimicrobial potential of the crude preparations of some of the medicinal plants, Viz. Artemisia afra, “Ariti”; Vernonia amygdalina, “Girawa”; Lepidium sativum, “Feto”; and Carum copticum, “Nech Azmud” against Staphylococcus aureus, Bacillus cereus, Shigella flexineri, Shigella boydii, Salmonella typhimurium and Escherichia coli, respectively. These plants are recorded in the literature as anti-diarrheal (12, 13). Methods Sample collection and processing: Four types of Ethiopian traditional medicinal plants were either collected from home-gardens or purchased from local markets. The seeds of Carum copticum, Lepidium sativum, and leaves of Artemisia afra and Vernonia amygdalina were purchased from local markets or collected from gardens. Samples were thoroughly cleaned with sterile distilled water. The cleaned plant parts were then sun-dried, powdered and sieved with a mesh. Known mass of the prepared powder of each medicinal plant was thoroughly mixed with distilled water to give the maximum concentration that could allow pipetting for microbiological processing. The concentration of the various plant materials thus prepared was as follows:- Carum Copticum 20%; Vernonia amygdalina 10%, Artemisia afra, and Lepidium sativum, 5%(weight/volume). The preparations were separately sterilized at 121C for 15 min. Screening for antimicrobial activity: For antimicrobial testing the following bacterial strains were kindly supplied by Dr. Aberra Geyid of the Ethiopian Health and Nutrition Research Institute (EHNRI): Staphylococcus aureus (ATCC 29213), Escherichia coli (ATCC 25922), Salmonella Typhimurium (ATCC 14028). Bacillus cereus, Shigella Flexineri, and Shigella boydii were from the culture collection of EHNRI. A loopful of the test strains was separately inoculated into sterile Mueller Hinton broth. After incubation for 24h at 37C, the cultures were compared with McFarland turbidity standard as described by Thrupp (14), to adjust to a population of 10 6 cfu/ml. For screening purposes, powder from the various medicinal plants was separately mixed with Mueller Hinton agar at various concentrations (20%, 10%, 5% and 2.5%), sterilized at 121C for 15 minutes and poured on sterile petri dishes. Preparations were also similarly processed as follows: boiling for 10 min., heating at 80C for 10 min., pasteurization at 62C for 30 min. and lyophilization. A loopful of the standardized culture of each organism was separately streaked on the solidified plates and incubated at 37C for 24h. Inoculation on plates without medicinal plant preparations served as control. Inhibition was assessed in terms of reduction of bacterial colonies in comparison to control. Determination of bactericidal activity: Minimum concentrations of crude preparations which showed inhibition in the screening tests were further considered for the determination of bactericidal activity on the test organisms according to Thrupp (14) with slight modification. Thus the following conce-ntrations of the crude preparations were made by mixing with 9ml Muller Hinton broth: Artemisia afra (5%, pH 6.6), Vernonia amygdalina (7%, pH 6.2), Lepidium sativum (2%, pH 6.7), and Carum copticum (10%, pH 6.3). After sterilization at 121C, the broth were separately inoculated with 1 ml of the standardized culture of the test strains to get a final inoculum level of about 105 cfu/ml. A Muller Hinton broth tube without plant material served as a control. Appropriate dilutions of freshly inoculated broth was surface plated on Plate Count agar to determine the initial inoculum level. Samples were then drawn at four hour intervals and appropriate dilutions were similarly plated for counting after incubation at 37C for 24h. This study was undertaken in Addis Ababa between October and April, 1998. 212 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Results Lepidium sativum did not exhibit an inhibitory property against B. cereus (Fig 1). Growth in Lepidium sativum was almost identical with that in the control. Vernonia amygdalina was relatively more inhibitory to Staph. aureus than the other plants (Fig 2). Bacteriostatic property of Carum copticum, Artemisia afra and Vernonia amygdalina was observed after 4h, although growth in Carum copticum increased after 16h. Figure 1: Effect of crude preparations of four medicinal plants on growth pattern of B. cereus. Antibacterial activity of traditional herbs 213 ──────────────────────────────────────────────────────────── Figure 2: Effect of crude preparations of four medicinal plants on growth pattern of Staph. aureus. Both Sh. Flexineri and Sh. Boydii showed similar increasing trends in all crude preparations. Vernonia Amygdalina and Artemisia afra showed a marked initial retarding effect against Sh. Flexineri (Fig 3). Final counts in all cases were, however, higher Figure 3: Effect of crude preparations of four medicinal plants on growth pattern of Sh. Flexineri. 214 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Figure 4: Effect of crude preparations of four medicinal plants on growth pattern of Sh. Boydii. than 109 cfu/ml. Artemisia Afra reduced the initial counts of Sh. Boydii by about 2 log units within four hours. The other crude preparations also had a bacteriostatic effect until 4h. Final counts in Vernonia Amygdalina were all lower by about 2 log units than the control (Fig 4). Figure 5: Effect of crude preparations of four medicinal plants on growth pattern of S.typhimurium. Antibacterial activity of traditional herbs 215 ──────────────────────────────────────────────────────────── Figure 6: Effect of crude preparations of four medicinal plants on growth pattern of E. coli. Counts of S.Typhimurium in all crude preparations were lower by about 1 log unit than the control until about 8h. All resulted in a longer lag phase until 4h followed by a sharp increase in count thereafter. No marked difference was noted between counts in the control and those in the crude preparations after 12h (Fig 5). None of the crude preparations had any bactericidal or bacteriostatic effect on E. coli. Counts in the crude preparations were very similar with those in the control all through the incubation time (Fig 6). Discussion In the preliminary investigation with the agar well plate assay, absence of any clear zone by sterilized crude preparations could be due to either absence or low concentrations of diffusible water soluble active constituents or excessive heating that affect thermo-labile biological active substances. However, the inactiveness of most preparations treated at reduced heating upto 40C indicated that heating might not be a factor. In a similar study, Belachew (15) reported that aqueous extracts of Lepidium sativum were found effective against Staph. aureus and Proteus vulgaris. The absence of inhibition in our study may thus be due to low concentration of active constituents. The fact that some crude preparations in our study showed stronger retardation effect on the Gram-positive test strains than on the Gram-negative ones supported our argument that heat treatment did not have effect on the activity of the crude preparations. In another study, Gram-negative test organisms were less susceptible to extracts than Gram-positive strains (15). Absence of activity in some crude preparations might also be due to a number of factors, such as time of collection of plant material and climate, which might, in turn, affect the amount of active constituents in the plant material. Except for E. coli, the various crude preparations showed varying degrees of retarding effect on all test strains. A shortcoming of our study was to limit crude preparation concentrations to levels that allowed a broth mixture that can be pipetted for bacteriological analysis. If higher concentrations of crude preparations could be studied, a stronger inhibition might have been noted. It is, thus, quite likely that the inhibitory effect of the crude preparations could be considerably enhanced in traditional treatment, if they are taken at four-hour intervals. The Gram-positive species considered in this study are of food intoxication types. Thus, treating diarrhoea caused by food intoxication with the various crude preparations may not be effective at all. Once these pathogens elucidate a sufficient amount of toxin in the food in which they multiply, it is the 216 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── toxin, and not the pathogens, that cause the disease after ingestion. However, the retarding effect shown in some of the Gram-negative test strains would qualify the crude preparations as candidates for further research. It may also be important to consider the crude preparations themselves in the study of their medicinal value. In many cases extracts of active constituents, which are effective in in-vitro experiments, do not show the same effectiveness when applied in-vivo. This may be due to the fact that various components in the crude preparations may show a synergistic effect on pathogens. According to Farnsworth et al., (16), heterogenous phytoconstituents of crude preparations may possess a synergistic effect. Acknowledgements Authors kindly acknowledge the financial assistance by SAREC. References 1. Ashenafi M and Gedebou M. Salmonella and Shigella in adult diarrhea – prevalence and antibiograms.. Trans Royal Soc Trop Med Hyg. 1985;79:719-721. 2. Gebreyohannes A and Drassar, SB. The pattern of drug resistance in Shigella dysenteriae and Shigella flexineri isolates in Ethiopia (1974-1985). Ethiop J Health Dev. 1985;3:45-52. 3. Lindtjorn, B, Degife S and Niemi, M.Sensitivity pattern of bacterial isolates from patients at Sidamo hospital. Ethiop Med J 1989;27:27-31. 4. Mache A, Mengistu M and Cowley S. Shigella serotype identified from adult diarrheal out-patients in Addis Ababa, Ethiopia: Antibiotic resistance and plasmid profile analysis. East Afr Med J 1997;74:179-182. 5. Assefa A and Yohannes G. Antibiotic sensitivity of Staphylococcus aureus and Escherichia coli strains isolated in Gonder, Ethiopia. Trop Doc 1997;27(2):121. 6. Akerele O. Nature’s medical botany do not throw it away. World Health Forum 1993; 14:390-395. 7. Nyazena ZN and Kire FC. The interaction between traditional medicine remedies used for gastrointestinal diseases as conventional drugs. East Afr Med J 1986;63(4):258-262. 8. Abebe D. The development of drug research. EHNRI News Letter 1996;1:5-6. 9. Andrews J. A bibliography on herbs, herbal medicine, “natural” foods, and unconventional medical treatment. 1982; Libraries unlimited, Inc., USA. 10. Tadesse M. Some medicinal plants of central Shewa and South Western Ethiopia. SINET: Ethiop J Sci 1986;9:143-168. 11. Kaba M. Utilization of plant medicine for the treatment of health problems. The case of Oromo District, Illubabor Zone, Western Ethiopia. Ethiop J Health Dev 1996;10:161-162. 12. Edwards S and Asfaw Z. Plants used in African traditional medicine as practiced in Ethiopia and Uganda. Botany 2000: East and Central Africa Monograph Series Number 5 1992; Published by NAPRECA, Addis Ababa University, Addis Ababa. 13. Kloos H, Tekle A, W. Yohannes L, Yosef A, Lemma A. Preliminary study of traditional medicinal plants in nineteen markets in Ethiopia: use patterns and public health aspects. Ethiop Med J 1978;16:33-34. 14. Thrupp D. Susceptibility testing of antibiotics in liquid media. In Antibiotics in laboratory medicine. Lorian, V. (ed). Williams and Wilkins, USA. 1980:73-93. 15. Desta B. Ethiopian traditional herbal drugs. Part II. Antimicrobial activity of 63 medicinal plants. J Ethnopharmacol 1993;39: 129-139. 16. Farnsworths NR, Henry LK, Svogoda GH, Blomster RN, Yates MJ and Euler KL. Biological and phytochemical evaluation of plants. I. Biological test procedures and results from two hundred accessions. Lloydia. 1966;25:101-122. Original article Perception of fertility regulation in a remote community, South Ethiopia Yemane Berhane1, Eyasu Mekonnen1, Legesse Zerihun1, Getachew Asefa2 Abstract: This exploratory study was conducted to describe the traditional methods of contraception and community perception of fertility regulation in a remote rural community of Ethiopia. In-depth interviews were conducted with "key informants" selected from the rural communities of Bensa district, South Ethiopia. Selection of key informants was purposive with the aim of obtaining knowledgeable and articulate individuals. Four categories of individuals were interviewed: elderly men, elderly women, women in reproductive age, and community health workers. The findings are described in three categories: contraception methods, sexual norms and premarital sex, and desired family size. The results showed that, in Bensa Community, postpartum sexual abstinence and prolonged breast-feeding are the main means of fertility regulation. Cultural values regarding sex(postpartum and premarital abstinences) are being disregarded now adays. On the other hand, the effects of unregulated fertility on population growth and societal resources are well perceived by the community. The community expressed willingness to accept modern family planning methods to regulate fertility. Further studies, however, are recommended for a better understanding of the issues using a mixture of quantitative and qualitative research methods. [Ethiop. J. Health Dev. 1999;13(3):217-221] Introduction The population crisis is getting more attention from day to day all over the developing world. According to the official statement, the population of Ethiopia is projected to grow at the rate of 3.1% by the end of the century. This figure was only 0.3% at the beginning of the century(1). The Ethiopian Government, cognizant of the problem, has formulated a population policy(1). A recent study in a southern Ethiopian region has documented a reported total fertility rate(TFR) of 5.46 and lower fertility rates in urban compared to rural communities(2). In spite of the attempts made to create awareness on family planning metheds and promote the use of them, the problem of high rate of fertility still remains unresolved. Every tradition has got its own outlook on population growth. In some parts of Ethiopia, the wealth of the family is measured by the number of children it produces. As a result, families tends to have large numbers of children. The total fertility rate for each woman in Ethiopia was estimated to be 6.6 on the average between the years 1990 and 1995 (3). The widespread failure of family planning campaigns in many developing countries may be attributed to the traditional attitudes held by the communities and the need for large numbers of children. Thus, the understanding of a community’s perception on fertility regulation is crucial for expanding the use of family planning methods, particularly in remote parts of the country. Traditional methods were reported to constitute a considerable proportion of all contraceptive methods in both rural and urban areas(4-7). These methods include pre-marital and post-partum sexual abstinences, withdrawal, and the use of herbs. However, very little is understood about the nature and effectiveness of traditional contraceptive methods in Ethiopia. Further more, the attitude of the people _______________________________________ 1 Faculty of Medicine, Addis Ababa University; 2Ethiopian Health and Nutrition Research Institute, Addis Ababa. living in the remote rural areas of Ethiopia on fertility regulation is also poorly understood. The objective of this study is, therefore, to describe the traditional contraception methods as well as community perception on fertility regulation, sexual and family size norms. 218 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Methods The study utilized an exploratory qualitative research method to collect relevant information. It was conducted in Sedea-Warea peasant village located in Bensa District, Sidama Zone, Southern Nations and Nationalities Peoples Regional (SNNPR). It is one of the 49 Peasant Associations in the District. According to the 1994 census, the population of the village is estimated to be 5701 with female-tomale ratio of 1:1.04. The average household size was 4.8 individuals(8). The study area is one of the remote sites with poor infrastructure and low health service coverage in the Region. The village is located some 10 kilometers from the district town of Bensa. Modern communication means are lacking and the public transport system is underdeveloped. Four categories of individuals: (elderly men, elderly women, women in reproductive age, and community health workers) were identified as "key informants". These individuals were selected purposely for the sake of obtaining people who are believed to be knowledgeable about the subject matter as well as capable of expressing themselves well. Two individuals from each category were interviewed. The study was carried out in January 1998. In-depth interviews were conducted with the "key informants" using a discussion guide in a quiet and private place near their residence. The interviews were intended to generate information on the type of contraception commonly practiced and on the perception of the community on fertility regulation. Each interview took approximately 45 minutes. The researchers served as interviewers and recorders in rotation. With the consent of the interviewees, all the interviews were tape-recorded. The interviews were conducted in the local language with the help of translators from the Zonal Health Department. Analysis of the study was made based on the tape-recorded materials and field notes taken by the researchers. The findings are described in three categories: contraception methods, sexual norms, and desired family size. Results Contraception methods: In Bensa tradition, postpartum sexual abstinence and prolonged breastfeeding are the main methods for fertility regulation. Couples are not allowed to sleep together before the preceding child starts walking or for at least 4-6 months postpartum. This would allow the mother to recover from the burden of the previous pregnancy and give her sufficient time to take care of her new child. The tradition also allows men to have more than one wife. Thus, during the period of postpartum sexual abstinence with the breast-feeding wife the male spends more time with his other wife/wives. This is believed to have contributed to the relatively few number of children born per women. In this community, no traditional medicine is claimed to be used to regulate fertility. Traditions with regard to marriage are changing with the expansion of Christianism these days. The religion discourages polygamy which is most welcomed by women who are not happy about traditional marriages involving polygamy. However, this has its own disadvantages, one of which is a reduced postpartum sexual abstinence period leading to short pregnancy intervals which, in turn, are believed to have resulted in the increased number of children per women. Recently, education on family planning methods has been started in these communities in relation with outreach immunization services. As a result, a few women in the village have started taking modern contraceptives despite the myths and prejudices about it. However, these women are already noticed complaining about the side-effects and ineffectiveness of the methods. The key informants, particularly the community health workers, emphasized the importance of continuing public education on a regular basis to achieve success in introducing modern family planning methods in the area. Sexual norms: The tradition strictly forbids premarital sexual affairs. Girls identified having premarital sex or giving birth before marriage face the risk of being outcasts from the community. They do not get any assistance from the family and the community at large. Perception of fertility regulation in South Ethiopia 219 ──────────────────────────────────────────────────────────── Changes in the pattern of sexual practice are occurring among the youth. Irresponsible sexual affairs are increasing and virginity seems to have lost its value for them. The breakdown of the traditional sexual norms is believed to result in unwanted pregnancy with its complications. Family size desire: Large numbers of children are no more desired by the community as the resources are getting scarce for large families. This idea was shared by all categories of key informants. The elder men described it by saying "We don't want many children any more, the land is getting too small and the coffee plant is not as productive as it used to be. Since the land can no longer support our children, they have no job here and are forced to migrate to towns". Though all categories of respondents expressed that there is a desire to limit the number of children in the community, knowledge about the means to regulate fertility is observed to be lacking. Both female and male informants attributed that to low health service coverage that is not readily accessible to them. On the other hand, male and female respondents blame one another for being the reason for large family size. Female informants reported that, because of the male dominance in the culture, women would be forced to bear large numbers of children. This is reported to be a major obstacle in the fertility regulation decisions by women. Polygamy is also believed to be one of the major causes for the increased population size as reported by all categories of informants. It is not a pleasant experience for women, while men seem to enjoy it because of the comfort they get from their competing wives. Further more, there is no open discussion between the couples to decide on the number of children. Discussion This study was exploratory in nature and a statistically representative sample was not the aim. Hence, the findings may not be generalizable for the community at large. However, as the selected key informants are considered to be knowledgeable about the tradition and to represent different age groups and genders, it is believed that the study gives a fairly realistic impression on the issues studied. Because of the sensitivity of the issue, the youth category was excluded from interviews for fear of cultural taboos. However, the reproductive age informants and particularly the community health workers were relatively young and are believed to have reflected the thoughts of the youth. Nonetheless it is desirable to conduct a large scale study with a mixture of quantitative and qualitative methods in order to fully understand the issues. Both postpartum sexual abstinence and prolonged breast-feeding are known to be effective natural methods of fertility regulation and widely practiced among a considerable proportion of married couples(1). These methods are to be encouraged in rural communities since they are affordable and acceptable by the majority. Furthermore, this helps promote the health of both the mother and the child. However, postpartum sexual abstinence has to be adhered to by both partners. Failure to be committed to it by husbands has been shown to expose the couple to sexually transmitted diseases, including HIV infection(9). As the old tradition of having more than one wife is discouraged by the expanding Christianity in the area, husbands may find it difficult to abstain for a long period which could result in an increased fertility rate per woman and/or to an extra-marital sexual relationship. Public education to promote a faithful relationship and on the use of alternative contraceptive methods needs to be expanded in order to prevent the potentially dangerous behaviour of extra-maital sexual affair. 220 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── The breakdown of traditional sexual norms deserves due attention and action. Besides its contribution to the increasing fertility rate, it will cause unwanted pregnancy and expose the young, productive generation to sexually transmitted diseases, including HIV/AIDS. Though the community members claimed to have realized the disadvantages of unregulated fertility, the couples have not yet taken appropriate action. It seems that there is a projection of the blame to each other. Such spousal disagreement on the desired number of children has been reported elsewhere(10,11). This is an area for appropriate interventions by the local health workers. The involvement of the couples in the decision to adopt family planning methods was shown to be effective in an urban study(12). This study also hinted that there is a desire to use modern contraceptive methods among the population in remote rural areas. Hence, providers of family planning services have to be very active in expanding their services in those areas. Effective client education is invaluable to help women overcome the prejudices against modern contraceptive methods and make a well informed choice of the methods(13). In conclusion, this study indicates that the effect of unregulated fertility is well understood and that there is a positive attitude to fertility regulation, in general, using either traditional or modern methods. The complexity of the issues tried to be addressed in this study warrant further studies using a mixture of qualitative and quantitative methods. Acknowledgments This study was supported by the Ethiopian Science and Technology Commission(ESTC), the Ethiopian Health and Nutrition Research Institute(EHNRI) and the Research and Publication Office(RPO) of the Addis Ababa University. Authors gratefully acknowledge the assistance received from Sidama Zone and Bensa District Health Departments. References 1. The Transitional Government of Ethiopia. Office of the Prime Minister. National Population Policy of Ethiopia. Addis Ababa. 1993. 2. Demographic Training and Research Centre(DTRC), Institute of Development Research(IDR), Addis Ababa University(AAU) and Population Studies and Training Center(PSTC), Brown University(Brown). 1998. Southern Nations and Nationalities People’s Region Community and Family Health Survey 1997. Addis Ababa, Ethiopia:AAU. 1998:77-88. 3. Zelalem Fekadu. Social-psychological factors associated with contraceptive attitudes of married women in the Kechene Community of Addis Ababa, Ethiopia. Ethiop J Health Dev. 1995;10(??):153160. 4. Ministry of Health, Surveillance/Statistics Team, Planning and Project Department. Summary of Annual Health Statistics Report of Ethiopia of 1987 Eth.C. December 1996:31. 5. Central Statistical Authority. The 1990 National Family and Fertility Survey Report. Addis Ababa, 1993. 6. Ministry of Health. Guidelines for Family Planning Services in Ethiopia. Addis Ababa, 1996. 7. Berhane Y and Zakus D. Community awareness and practice of family planning in an urban community in Addis Ababa, Ethiopia. Ethiop J Health Dev. 1995;9(3):133-139. 8. Federal Democratic Republic of Ethiopia. Office of Population and Housing Census Commission. Central Statistical Authority. The 1994 Population and Housing Census of Ethiopia Results for Southern Nations, Nationalities and People’s Region. June 1996;Vol.I(Part I):300-301. 9. Gangakhedkar RR, Bentley ME, Divekar AD, et al . Spread of HIV infection in married monogamous women in India. JAMA. 1997;278(23):2090-2092. 10. Bankole A. and Singh S. Couple’s fertility and contraceptive decision-making in developing countries hearing the man’s voice. International Family Planning Perspective, 1998;24(1):15-24. Staphylococci susceptibility of CHG and antibiotics 221 ──────────────────────────────────────────────────────────── 11. Dodoo FN-A, Luo Y and Panayotova E. Do male reproductive preferences really point to a need to refocus fertility policy? Population Research and Policy Review. 1997;16(5):447-455. 12. Terefe A. and Larson C.. Modern contraception use in Ethiopia: Does involving husbands make a difference? American Journal of Public Health. 1993;83(11):1567-1570. 13. Young Mi Kim, Adrienne Kols and Steohen Mucheke. Informed Choice and Decision-making in family planning counseling in Kenya. International Family Planning Perspectives, 1998;30(1):4-11. 222 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Original article In vitro susceptibility of staphylococci to chlorhexidine and antibiotics Yohannes Mengistu, Worku Ergie and Bahrie Bellete Abstract: The study was performed to monitor the susceptibility of clinical isolates of staphylococci to chlorhexidine and antibacterial drugs in vitro. Forty-eight strains of staphylococci were isolated from Tikur Anbessa Hospital patients. All isolates were susceptible to <0.01% chlorhexidine out of which 90% were inhibited at <0.001%. Tetracycline, penicillin, and chloramphenicol were the least effective drugs with 69%, 56%, and 37% of the isolates resistant, respectively. Resistance to any of the other antibiotics tested was less than 30%. Fifty six percent of the isolates were resistant to two or more drugs. The study showed that there was no association between the antibiotic and disinfectant susceptibility. Both susceptible and resistant strains to the antibiotics tested were equally susceptible to low concentrations of chlorhexidine (P>0.05). The study also demonstrated that chlorhexidine is still an effective antiseptic/disinfectant to suppress or prevent staphylococcal infections. The high frequency of drug resistant strains could be an indication of the extensive use of antibacterial drugs in this hospital. Continued surveillance and antibiotic policy are needed in order to minimize the emergence and spread of resistant pathogenic bacteria. [Ethiop. J. Health Dev. 1999;13(3):223-227] Introduction Bacterial infections can be controlled by local administration of disinfectants such as chlorhexidine. Because it is mild and relatively nontoxic to human tissues, chlorhexidine has gained a wide range of application both as an antiseptic and as a disinfectant in medical practice (1). Although it is widely used, staphylococci resistant to chlorhexidine with positive cross resistance to other antiseptics and antibiotics have been documented (2-4). It is possible that a significant proportion of laboratory or hospital acquired infections may be partly due to the use of ineffective or low concentrations of disinfectants. Staphylococci, especially Staphylococcus aureus, are major causes of community and hospital acquired infections. The use of antimicrobial agents has significantly reduced staphylococcal infections. However pathogenic taphylococci have become increasingly resistant to the commonly used antimicrobial agents worldwide. In Ethiopia, previous studies have shown the importance of Staphylococcus aureus in diseases and the emergence of multiple drug resistant strains (5-7). The purpose of this study was to monitor the susceptibility of staphylococci to chlorhexidine and commonly used antibiotics and determine if there is any positive resistance link between the disinfectant and antibiotics. Methods Specimens: A variety of clinical specimens submitted to the Bacteriology Laboratory from adult inpatients of Tikur Anbessa Hospital were processed between January 1996 and March 1997. Out of ______________________________________ Department of Microbiology and Parasitology, Faculty of Medicine, Addis Ababa University, P.O. Box 9086, Addis Ababa, Ethiopia a total of 503 specimens processed, 48 specimens (30 pus, 16 blood, one urine and one throat swab) Staphylococci susceptibility of CHG and antibiotics 223 ──────────────────────────────────────────────────────────── which were positive for staphylococci were tested. Isolation and Identification of bacteria: Appropriate culture media were used for isolation of microrganisms (Oxoid, Basingstoke, Hampshire, UK). Specimens were inoculated onto blood agar and incubated at 37oC for 18-24 h. The bacterial isolates were identified by cultural and biochemical methods following standard procedures (8). S. aureus was differentiated from other staphylococci by coagulase test. Chlorhexidine susceptibility testing: The susceptibility of bacterial isolates to chlorhexidine was determined by agar dilution method following standard procedures (2, 9). Chlorhexidine gluconate supplied as a 20%w/v stock solution was serially diluted with sterile distilled water. Chlorhexidine at a final concentration of 1, 0.1, 0.01, 0.001, and 0.0001%(w/v) was used for each test organism. One ml of diluted disinfectant was mixed to nine ml of molten Meuller-Hinton agar, transferred into 50 mm diameter petri dish. The agar was solidified at room temperature and briefly dried at 37 0C before inoculation with the test organism. Bacterial colonies were removed from an overnight incubated agar plate suspended in sterile saline solution to the proper density. The concentration was estimated by measuring the optical density. The density of the suspension was adjusted to approximately 107 to 10 8 CFU/ml by comparing to a McFarland 0.5 BaSO4 standard. One ml of the bacterial suspension was spread onto the agar plate. As a control, bacterial suspension was also plated on agar plate without disinfectant. All agar plates were incubated at 37oC for 18-24 h. The minimum dilution of chlorhexidine that inhibited growth was considered as the minimum inhibitory concentration (MIC). Antibiotic Susceptibility testing: The susceptibility of staphylococci to different antibiotics was determined by standard agar disk diffusion method (10). Bacterial suspension adjusted to McFarland 0.5 standard (as above) was spread onto Meuller-Hinton agar plate. Bacterial isolates were tested using the following antibiotic disks (Oxoid): Penicillin (10 ug), carbenicillin (100 ug), cephalothin (30 ug), chloramphenicol (30 ug), gentamicin (10 ug), kanamycin (30 ug), tetracycline (30 ug), methicillin (5 ug), eryhtromycin (15 ug) and trimethoprim-sulphamethoxazole (25 ug). For quality control, reference strain (Staphylococcus aureus ATTC #29213) was used.. Statistical analysis: Student t-test was used to compare the mean minimum inhibitory concentration of chlorhexidine required for antibiotic sensitive strains with that of antibiotic resistant strains. Results A total of 48 strains of staphylococci were isolated from 30 pus, 16 blood, one urine and one throat swab specimens. Thirty-one strains were Staphylococcus aureus and 17 strains were coagulase negative staphylococci (CNS). As Table 1 shows, all staphylococci were susceptible to < 0.01% chlorhexidine. About 22% (7/31) of S. aureus and 35% (6/17) of CNS were inhibited by the lowest concentration of the disinfectant used, i.e., 0.0001%. Table 1: Staphylococci strains inhibited with specific MIC of Chlorhexidine. Bacteria spp (no) % inhibition to MIC* chlorhexidine 0.0001 0.001 S. aureus (31) 22.6 90.3 CNS** (17) 35.3 94.1 * MIC: Minimum inhibitory concentration ** CNS: Coagulase negative staphylococci 0.01 100 100 0.1 - 1 - As shown in Table 2, penicillin, tetracycline and chloramphenicol were the least effective antibiotics out of which 37% to 76% of isolates were resistant. Only 12.5% (6/48) of the isolates were susceptible to all antibiotics tested. Over 87% (42/48) of the isolates were resistant to one or more drugs. Over 60% (29/48) were resistant to two or more drugs. Since we were not able to test all isolates of staphylococci for methicillin and erythromycim, the results were interpreted separately. About 19% (6/32) of the isolates tested to methicillin were found resistant. All methicillin resistant strains were 224 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── simultaneously resistant to four or more drugs. Table 2: Staphylococcal isolates resistant to selected antibiotics. Bacteria Number (%) of strains resistant to (no) Pen* Car Ceph Chl Gen Kan S. aureus (31) CNS** (17) Total (48) 7 (22.6) 1 (5.9) 8 (16.7) 20 (64.5) 7 (41.1) 27 (56.2) 7 (22.6) 4 (23.5) 11 (22.9) * Pen - penicillin G Chl - Chloramphenicol Tet - Tetracycline ** Coagulase negative staphylococci 2 (6.4) 0 (0) 2 (4.2) 11 (35.5) 7 (41.1) 18 (37.5) 11 (35.3) 0 (0) 11 (22.9) Car - Carbenicillin Gen - Gentamycin Tsm - Trimethoprim-sulphamethoxazole Tet 19 (61.2) 13 (76.5) 33 (68.7) Tsm 9 (29) 5 (29.4) 14 (29.2) Ceph - Cephalothin Kan - Kanamycin Out of 22 strains tested to erythromycin, 4(18%) were resistant. Comparative analysis was made in order to see whether there was any positive cross resistance link between the antibiotic and disinfectant resistant strains. However, no difference in MIC of chlorhexidine was observed between bacteria which were single or multi-drug resistant to the antibiotics tested (p>0.05). There were six strains sensitive to all antibiotics and their mean MIC of chlorhexidine was similar to that of the antibiotic resistant strains (p>0.05, Table 3). Table 3: The mean MIC of chlorhexidine for antibiotic sensitive and resistant staphylococci. Sensitive to all drugs Resistant to 1 drug Resistant to 2 drugs Resistant to 3 drugs Resistant to 4 drugs Resistant to 5 or more No(%) 6(12.5) 18(37.5) 7(14.6) 7(14.6) 5(10.4) 5(10.4) %(Xgeom)* MIC Chlorhexidine 0.00032 0.00088 0.00072 0.00027 0.0016 0.00063 *:Xgeo Geometric mean of minimum inhibitory concentration (MIC) Discussion Chlorhexidine gluconate (CHG) is widely used for the management of wound infection, periodontal infection and skin disinfection before surgery (11, 12), and for disinfection of heat and moisture sensitive surgical instruments (13). The concentration of chlorhexidine has been found to be variable depending on the nature of application and the manufacturer's recommendation. The use of an appropriate concentration of disinfectant may inhibit most of the nosocomial strains and thus will prevent infection. Chlorhexidine is a bactericidal antiseptic that disrupts cell membrane functions. The mechanism of resistance of bacteria to chlorhexidine has not been well established. Some studies have shown the positive links between resistance to antibiotics and disinfectants (3, 14). In S. aureus strains, a single plasmid has been found to be responsible for both disinfectants and antibiotics (2). The susceptibility of bacterial isolates to chlorhexidine has not been studied previously in Tikur Anbessa Hospital or elsewhere in the country. Comparison was, therefore, not possible. In this study, staphylococci both susceptible and resistant to the antibiotics tested were equally sensitive to <0.01%w/v chlorhexidine which was lower than the MIC used in vivo (0.02- 0.05%). Such observation confirms that there was no positive cross resistance between chlorhexidine and antibiotics. Our results were in agreement with Al-Masaudi et al (15), Cookson et al (16) and Yasuda et al (17). However others have reported an increase in resistance to chlorhexidine or other disinfectants in drug resistant strains including methicillin resistant S. aureus (MRSA, 18). Staphylococci susceptibility of CHG and antibiotics 225 ──────────────────────────────────────────────────────────── Since chlorhexidine was equally effective for both sensitive and multiple antibiotic resistant staphylococci, hospital acquired infection can still be minimized by application of this antiseptic. However, our preliminary study showed that significant number of gram-negative isolates were not inhibited by the recommended concentration of chlorhexidine (unpublished observation). Thus, there may be a need to use either higher concentration of chlorhexidine or in combination with other disinfectants. Antimicrobial resistance is increasing and pathogenic staphylococci have multiple drug resistance to commonly used antimicrobial agents. If one considers the susceptibility of staphylococci (eventhough the number of isolates was small), the resistance rates show an increasing trend compared to previous studies in this hospital (5, 6) or elsewhere in the country (7, 19-21). The low sensitivity rates of the isolates to penicillin and tetracycline (32-44%) may be an indication of the widespread use of these antibiotics. Staphylococcus aureus is the most frequent cause of nosocomial infections caused by gram positive bacteria. Although the strains were highly susceptible to cephalothin, the detection of high rates of resistance to gentamicin is cause for concern. This could be serious because gentamicin is one of the few drugs used for the treatment of serious bacterial infections in this hospital. The cause of high resistance rates to easily available and commonly used antimicorobial agents in this study can not be determined from the available information. Since the strains were isolated from in-patients, selective pressure and spread of drug resistance plasmids might be the most important factors. In conclusion, chlorhexidine is still an effective antiseptic to suppress or prevent staphylococcal infections in the hospital. However, there may be a need to monitor the efficacy of the commonly used disinfectants to other bacteria in order to reduce the risk of infection by resistant microorganisms. The increasing rates of drug resistance among bacteria could be a serious threat to the successful antimicrobial therapy. While appreciating the limitation of this study due to the small number of strains tested, there is compelling evidence for the existence of mutiple antimicrobial resistant strains in this hospital. A continuous surveillance of antimicrobial susceptibility patterns and antibiotic policies are needed in order to minimise the emergence and spread of resistant pathogenic bacteria. Acknowledgements This work was supported by Ethiopian Science and Technology Commission (ESTC) We are grateful to the staff of the Diagnostic Bacteriology Laboratory, Tikur Anbessa Hospital, Faculty of Medicine, Addis Ababa University for their technical assistance. References 1. Russel AD, Hugo WB, Ayliffe GAJ. Principles and practice of disinfection preservation and sterilization. London: Blackwell Scientific Publications, 1982. 2. Yamamoto T, Tamura Y, Yokota T. Antiseptic and antibiotic resistance plasmid in Staphylococcus aureus that possess ability to confer chlorhexidine and acrinol resistance. Antimicrob Agents. Chemother 1988;32:932-935. 3. Maris P. Resistance of 700 gram-negative bacterial strains to antiseptics and antibiotics. Ann Rech Vet 1991;22:11-23. 4. Sasatsu M, Shimizu K, Noguchi N, Komo M. Evaluation of antiseptics by the modified phenol coefficient method: sensitivity of methicillin-resistant Staphylococcus aureus. Biol Pharm Bull 1994;17:36-138. 5. Gedebou M. Staphylococcus aureus strains from a teaching hospital: clinical sources and antibiograms. East Afr Med J 1982; 59:810-815. 6. Tewodros W, Gedebou M. Nasal carrier rates and antibiotic resistance of Staphylococcus aureus 226 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── isolates from hospital and non-hospital populations, Addis Ababa. Trans Roy Soc Trop Med Hyg 1984;78:314-316. 7. Gedebou M, Tassew A, Azene G. Blood culture isolates from Addis Ababa Hospital: frequency and antibiotic sensitivities. East Afr Med J 1984;61:190-196. 8. Lennette H, Balows A, Hausler J, Truant P. Manual of Clinical Microbiology. 4th ed. America Society for Microbiology, 1988. 9. Brown AT, Sims RE, Raybould TP, Lillich TT, Henslee PJ, Ferretti GA. Oral Gram-negative bacilli in bone marrow transplant patients given chlorhexidine rinses. J. Dent Res. 1989;68:1199-1204. 10. Bauer AW, Kirby WMM, Sherris JC, Turk M. Antibiotic susceptibility testings by standardized single disc method. Amer J Clin Pathol 1966;45:493-496. 11. Newsom SW, Rowland C. Studies on preoperative skin flora. J Hosp Infect 1988;(suppl B): 21-26. 12. Agarwal S, Piesco NP, Peterson DE, Charon J, Suzuki JB, Godowski KC, Southard GL. Effects of sanguinarium, chlorhexidine and tetracycline on neutrophil viability and functions in vitro. J Periodontal Res 1997;32: 335-44. 13. Southwood LL, Baxter GM. Instrument sterilzation, skin prepartion and wound management. Vet Clin North Am Equine pract 1996;12:173-194. 14. Kunisada T, Yamada k, Oda S, Hara O. Investigation of the efficacy of povidone-iodine against antiseptic resistant species. Dermatol 1997;195 (Suppl 2):14-18. 15. Al-Masaudi SB, Day MJ, Russel AD. Sensitivity of methicillin resistant Staphylococcus aureus strains to some antibiotics, antiseptics and disinfectants. J Appl Microbiol 1988;65:329-337. 16. Cookson BD, Bolton MC, Platt JH. Chlorhexidine resistance in methicillin-resistant Staphylococcus aureus or just an elevated MIC? An in vitro and in vivo assessment. Antimmicrob Agent Chemother 1991;35: 1997-2. 17. Yasuda T, Yoshimura S, Katsuno Y, Takada H, Ito M, Yahazaki F, et al. Comparison of bactericidal activities of various disinfectants against methicillin-sensitive Staphylococcus aureus and methicillin-resistant Staphylococcus aureus. Postgrad Med J 1993;69 (suppl 3):S66-69. 18. Irizarry L, Merlin T, Rupp J, Griffith J. Reduced susceptibility of methicillin resistant Staphylococcus aureus to cetylpyridinium chloride and chlorhexidine. Chemotherapy 1998;42:248252. 19. Lindtjorn B, Degife S, Mauri N. Sensitivity patterns of bacteria isolated from Sidamo regional hospital. Ethiop Med J 1989;27:27-31. 20. Assefa A, Yohannes G. Antibiotic sensitiviy pattern of prevalent bacterial pathogens in Gondar, Ethiopia. East Afr Med J 1996;73:67-71. 21. Wolday D, Erge W. Increased incidence of resistance to antimicrobials by urinary pathogens isolated at Tikur Anbessa Hospital. Ethiop Med J 1997;35:127-135. Original article Child-feeding practices as predictors of nutritional status of children in a slum area in Addis Ababa, Ethiopia Gugsa Abate1, Wambui Kogi-Makau2, Nelson M. Muroki 2 Abstract: In a across-sectional study carried out in four purposefully selected slum kebeles of Addis Ababa, the nutritional status of 758 children aged 6 - 36 months was measured and subsequently classified into malnourished and well nourished groups. Child-feeding practices of randomly selected mothers of the two groups of children were compared with the view of identifying practices that contribute to child-nutrition insecurity in the study area. The result indicated that the majority of the mothers (i.e. 99.5% in the malnourished and 98.4% in well nourished groups) had initiated breast-feeding, and no significant difference was found either in the median or mean duration of breast-feeding between the two groups of mothers. After adjustment has been made (through logistic regression) for covariates, the study established that exclusive breast-feeding beyond four months, feeding low quality diet with a frequency of less than four times and giving porridge with feeding bottle as well as low household income are the risk factors contributing to young children’s nutritioninsecurity in the slum section of Addis Ababa. Hence, demonstrative and sustained education focusing on appropriate child-feeding is recommended together with initiation of income generating projects with a view of empowerment of those families whose monthly income is low. [Ethiop. J. Health Dev. 1999;13(3):229-2 Introduction About 79% of the population of Addis Ababa lives in low-grade, congested slum areas (1). Studies which address nutritional problems have found that malnutrition continues to be a serious health problem in the slums (2-5). One study in Nairobi slum (6), where 86.2% of the pre-schoolers were reported to have been stunted, provides a good basis for understanding that slum children are most vulnerable to malnutrition. Hofvander and Eksmyer (7), who found about 3% prevalence of severe PEM, reported that PEM is the main nutritional problem for young children in the slum of Addis Ababa. It is a well established fact that malnutrition manifests itself as a function of many and complex factors (8-10). It is directly linked to poor dietary intake and diseases, which in turn result from an interaction of various underlying factors which include crisis in household food security, inappropriate child care and feeding practices, unhealthy place of residence, and insufficient basic health services (8-11). An unfavourable health environment caused by inadequate water and sanitation can increase the probability of infectious diseases and indirectly form certain types of malnutrition (8-11). Further, poor socio-economic variables, cultural beliefs, and lack of parental education, especially that of mothers, are all cited to affect a person's nutritional status (8-13). Thus, nutrition planning and advice to a community needs to be grounded on good information and knowledge of which individual variables of the aforementioned factors are contributing to a high risk of malnutrition in that community. ______________________________________ 1 Ethiopian Health and Nutrition Research Institute, P.O. Box 5654, Addis Ababa, Ethiopia; 2Unit of Applied Human Nutrition Programme, P.O. Box 41607, Nairobi, Kenya Despite many nutritional studies in the urban and rural areas of Ethiopia (7,13-15), very little is known about which attributes of child feeding practices are associated with the nutritional status of infants and young children in the Ethiopian slum settings. This study, therefore, was intended to demonstrate those child-feeding practices that contribute to the prevalence of child-nutrition insecurity among infants and young children in a slum area of Addis Ababa. The findings of this study are expected to enrich the knowledge of all interested parties in the area of applied child-nutrition and provide information to policy-makers to take intervention actions to reduce the risk of malnutrition in the slum areas. 228 Ethiop.J.Health Dev. ─────────────────────────────────────────────────────────── ─ Methods In 1978, the World Bank identified seven kebeles (smallest administrative units) as typical slums and the most congested parts of Addis Ababa (16). An integrated urban development project with a nutrition- intervention component operates in three of the seven kebeles, identified as such by the woreda (district) authorities. This study was carried out from March to May, 1997 in four purposefully selected slum kebeles which were out of the intervention programme. Despite it’s drawbacks of overor under-selection of population elements (17), a convenience sampling procedure was applied to exclude the three intervention kebeles from the study. Because, it is highly probable that the socioeconomic situation and child-feeding behaviours of families in these kebeles have been influenced by the existing intervention programme and that this may bias the study results. All the four kebeles are located in woreda 3, and are named Kebele 31, kebele 34, kebele 44, and kebele 45. The populations of these kebeles are estimated to be 7529, 4879, 9011 and 3293 for kebele 31,34,44, and 45, respectively (18). The population composition of the study kebeles is heterogeneous consisting of various ethnic groups with different languages and cultural backgrounds. This was a cross-sectional study, comparative in nature, and with descriptive and analytical components. The sampling frame was a list of all households in the study areas with children aged of 6-36 months. Six hundred and thirty two households with children of 6-36 months of age (270 from kebele 31, 103 from kebele 34, 184 from kebele 44, and 75 from kebele 45) were identified in all the four kebeles through a house-to-house preliminary survey by which all children in the above age bracket were registered from each household. Age and sex as well as weight and height measurements of 758 children were recorded to determine the nutritional status of the target children. The anthropometric data were collected based on the methods described by the United Nations (19). Two weight measurements were obtained using a Salter weighing scale and the average calculated and recorded to the nearest 0.1 kg. The children were weighed with minimal clothing and without shoes. For measuring height, two types of wooden scales were used-one for recording recumbent length of children under two years of age and the other for taking standing height of the older children. In any case two measurements were recorded and the average calculated and written to the nearest 0.1 cm. The anthropometric data were analyzed in terms of weight-for-age, height-for-age, weight for height and by use of the Anthro package, Z-scores were generated and the numbers of malnourished and wellnourished children were determined among the total children in the four kebeles. The weight-for-age (WFA) index was used to classify the children into the categories of malnourished and well-nourished. This process facilitated polarization of households into two groups: the well-nourished households and the malnourished households. After the households were classified as malnourished and well-nourished, samples were drawn from among the household list of each group using a random sampling method. A total of 384 households (192 for each group) were selected. The statistical formula recommended for comparative studies (17) was used to calculate the desired equal sample size for each group of households. Data on breastfeeding, weaning practices and types of weaning foods as well as household income were collected from sampled households of both groups through inter-viewing of mothers or persons feeding the index child, using a preplanned structured questionnaire as the data collection tool. For those households which had more than one child, interview was made in relation to the youngest child. The diets of children, especially porridge prepared from basic or multi-mixes, was identified as enriched and that made solely from cereal sources was labelled as non-enriched. The data were collected with the assistance of two field workers who had completed grade twelve level of education. The two had also participated in other surveys and as such, were familiar with interviewing and anthropometric measuring techniques. However, further training in anthropometry and interviewing techniques was done. Pre-testing of the questionnaire was undertaken and Child feeding practices as predictors of nutritional status of children 229 ─────────────────────────────────────────────────────────── ─ modifications made prior to its application. Data validity and reliability were achieved through the close supervision of enumerators by the principal investigator. Immunization card was used to ascertain the age of the child. However, mothers in the survey areas were easily able to recall the ages of their children below two years of age. When reliable documentary evidence was not available interviewers used a local event calendar to determine the month and year of a child’s birth. At the end of each day, the completed questionnaires were checked to ascertain that all questions had been answered correctly and consistently. A two kilogram iron bar was used to regularly check scale accuracy and make sure measurements are correct. The data were analyzed using a computer in which SPSS/PC+ software was installed. Comparison of the various parameters of child- feeding practices in the two groups of households (malnourished and well-nourished) was done by administering chi-square and t-test at p value less than 0.05 level of significance. Ranking of risk factors of malnutrition was made by carrying out step-wise multivariate analysis involved the use of multiple logistic regression. Result Age and sex composition of children in the study area: Out of the 758 children, 51.2% were males and 48.8% were females. There were more females in the age group 6-12 months, while the number of males was greater than that of females among the age categories of 13-24 and 25-36 months) Table 1: Distribution of malnourished children by study area, Addis Ababa, 1997 Study area Below-2 SD of NCHS** N Underweight Stunted Kebele 31 294 138(46.9)b* 166(56.5)b Kebele 34 121 33((27.3)a 50(41.3)a Kebele 44 220 59(26.8)a 98(44.5)a Kebele 45 123 33(26.8)a 53(43.1)a Total 758 263(34.7) 67(48.4) Wasted 9(3.1)+ 4(3.3) 0(4.6) 3(2.4) 26(3.4) +Figures in parenthesis are percentages *any two figures followed by different letters in any one column are significant at P<0.01 **NCHS-National Centre for Health Statistics Nutritional status of children in the study area: For the four kebeles covered in the study, as shown in Table 1, slightly over a third (34.7%) of the children were underweight (low weight-for-age), nearly half (48.4%) were stunted (low height-for-age), and a small number (3.4%) were wasted (low weightfor-height). A significantly higher prevalence of underweight and stunting was observed in kebele 31 than was observed in the other three kebeles (P<0.01). The breastfeeding situation: Both the malnourished and well-nourished groups of households had invariably initiated breastfeeding as a great majority of the mothers (99.5%) in malnourished households and 98.4% in well-nourished households had at some time breastfed their children. About the same proportion of mothers, (about two thirds i.e. 66.7% and 65.1% in the malnourished households and well-nourished households, respectively) had practiced exclusive breastfeeding for the first three months of life (Table 2). However, a significantly higher proportion of mothers in the malnourished households (23.9%) had practiced exclusive breastfeeding up to 4-6 Table 2: Distribution of mothers by duration of exclusive breastfeeding, Addis Ababa, 1997 Age of exclusive Bf* practised (months) malnourished households (No=192) well-nourished households(N=192) X2 <4 4-6 7-9 128 (66.7)+ 46(23.9) 21(11.0) 125(65.1) 14(7.3) 8(4.2) 0.05 18.9 5.4 P-value NS <0.001 <0.05 230 Ethiop.J.Health Dev. ─────────────────────────────────────────────────────────── ─ +Figures in parentheses are percentages NS= not significant at p<0.05 B f= breastfeeding months than had mothers in the well nourished households (7.3%) (p<0.001). Further, the proportion of mothers in the malnourished households (11.0%) continued exclusive breastfeeding beyond six months was significantly higher than in well-nourished households (4.2%) (p<0.05). A significantly higher proportion of households in the malnourished group (84.8%), which exclusively breastfed for more than four months, earned 250 Birr than those households in the well nourished group which was 50.0% (p<0.05). There was no significant difference in mean duration of breastfeeding between the two types of households (i.e. 18.2±10.1 and 16.8±10.4 months in malnourished and well nourished households, respectively) (t=0.95, p=0.34). However, a relatively higher median duration of breastfeeding was observed among the households of the malnourished group (22.5) months) than that among the well nourished households (15 months). The result indicated that the two groups of mothers were not the same in the duration of exclusive breastfeeding as the malnourished group continued for a longer period. However, the two were not different in the length of general breastfeeding. Types of supplementary foods, feeding frequency and method of feeding: The mean age at which supplementation was started in malnourished households (4.9±2.9 months) was significantly higher than in the well nourished households which was 4.2±2.4 months (p<0.05). There was a significantly a higher proportion of mothers in malnourished households (44.3%) who fed non-enriched porridge than there were in the well nourished group of households (19.8%) (p<0.0001) (Table 3). Cow-milk was fed by most mothers as first food (i.e. 48.4 and 47.9% in malnourished and well nourished groups of households, respectively) and close to 20% fed bread with tea and “injera fetifit”. Mashed potatoes were fed by more mothers in well nourished households (16%) than in malnourished households where about 10% did, although no significant difference was observed. Child feeding practices as predictors of nutritional status of children 231 ─────────────────────────────────────────────────────────── ─ Table 3: Distribution of children by first foods given at the time of weaning, Addis Ababa, 1997 Type of weaning foods malnourished households well-nourished X2 P-value N=192 households N=192 cow-milk porridge 93(48.4)+ 92(47.9) 0.0 NS (not enriched) porridge 85(44.3) 38(19.8) 25.3 <0.0001 (enriched) 78(40.6) 121(63.0) 18.4 <0.0001 injera fetifit 43(22.4) 35(18.2) 0.8 NS bread+tea 41(21.4) 36(18.8) 0.3 NS mashed potato 19(9.9) 31(16.1) 2.8 NS canned milk 15(7.8) 25(13.0) 2.3 NS others 11(5.7) 11(5.7) 0.1 NS +Figures in parenthesis are percentages NS-not significant at p<0.05 Others:- Boiled flax water, fenugreek water, rice, orange juice and banana. percentages do not add up to 100 because some children consumed more than one type of food As shown in Figure 1, a significantly higher proportion of households in the malnourished group (53.6%) had fed children 1 - 3 times than had households in the well-nourished group (26.5% ; p<0.001). However, the proportion of households with a daily feeding frequency of more than or equal to four times was significantly higher in the well-nourished group (73.5%) than in the malnourished group which was 46.4% (p<0.0001). The mean feeding frequency among children in the well nourished households (four times) was significantly (p<0.01) higher than in the malnourished households where this was 3.4 times. Figure 1: Distribution of households by feeding frequency of Children The number of households which used the bottle to feed milk was practically the same (i.e. 70% in well-nourished and 73% in malnourished groups of households) (Table 4). However, there were significantly higher numbers of mothers in malnourished households (28.8%) who used the bottle to feed their children porridge than there were in well nourished households (8.2%; p<0.0001). In general the two groups of households were not the same in the types of supplementary foods, feeding frequency and method of feeding as the malnourished Table 4: Distribution of households by methods used to feed milk and porridge to children, Addis Ababa, 1997 Feeding Method malnourished well-nourished X2 p-value households households Milk n=108 n=117 Spoon 29(26.9)+ 35(29.9) Bottle 79(73.1) 82(70.1) 0.13 NS Porridge n=163 n=159 Spoon 116(71.2) 46(91.8) Bottle 47(28.8) 13(8.2) 21.3 <0.0001 232 Ethiop.J.Health Dev. ─────────────────────────────────────────────────────────── ─ +Figures in parentheses are percentages NS-not significant at p<0.05 households provide low quality diet with a lesser frequency using feeding bottle. Multivariate analysis of logistic regression was performed to examine the effect of each variable while controlling for the confounding effects of others and adjusted risk odds ratios were estimated. Exclusive breastfeeding beyond four months, feeding frequency, provision of non-enriched porridge, partaking of porridge with bottle, and household income were the variables selected for multivariate analysis due to their apparent statistical significance in the bivariate analysis. The variable enriched porridge is excluded as it can be best expressed by non-enriched porridge. All the variables remained significant as illustrated in Table 5. The risk ratios showed that children who exclusively breastfed for more than four months are about three and a half times more likely to be exposed to malnutrition than those who do not (p<0.01). Table 5: Logistic regression coefficient and the adjusted relative odds of malnutrition by household income and feeding practices Characteristics Exclusive BF 4 months $ >4 months Feeding frequency 4 times$ <4 times Households income (Eth. Birr) >250$ 250 Feeding non-enriched Porridge Yes$ No Giving porridge with feeding bottle Yes$ No Constant term Coefficients Adjusted Relative Odds 95% confidence Limit 1.231* 1.00 3.42 (1.54-7.63) 0.810* 1.00 2.25 (1.28-3.96) 1.059** 1.00 2.88 (1.63-5.12) -2.029 1.00 0.13 (0.07-0.24) -1.735*** -2.172*** 1.00 0.18 (0.08-0.38) $ Reference category in the dummy variable regression * Significance at p<0.01 ** Significance at p<0.001 *** Significance at p<0.0001 Similarly, the risk of malnutrition is also approximately two times more likely to occur in children who do not get four or more meals per day than those who did (p<0.01). The likelihood of occurrence of malnutrition among children of households which earn a monthly income of 250 Birr is about three times greater than among those whose households had an income of more than 250 Birr (p<0.001). The risk of childhood malnutrition in households having the practice of feeding children with non-enriched porridge is about eight times greater than the risk among households which had no such practice (p<0.0001). Finally, children receiving porridge with feeding bottle have five and a half times the risk of malnutrition compared to those who were not taking porridge with the use of bottle (p<0,0001). Discussion Prevalence of malnutrition: The prevalence of stunting and underweight in the study area was found to be relatively high as compared with the findings made by Wolde-Michael and Demeke in 1985 (15). However, even the kebele with highest rates of underweight and stunting (Kebele 31 with Child feeding practices as predictors of nutritional status of children 233 ─────────────────────────────────────────────────────────── ─ prevalence of 46.9% and 56.5%, respectively) had much lower prevalence than those found in a slum area of Nairobi in 1996 where these were 58.4% and 86.2%, respectively. Prevalence of wasting (3.4%) was, however, higher than the one found in the Nairobi slum (1.9%) by Waihenya et al. (11). Child Feeding practices and nutritional status: As in other developing countries, the initiation rate of breastfeeding was found very high regardless of the type of household. Similar studies conducted in Ethiopia and Libiya (14,20,21,22) also observed a comparatively high initiation rate of breastfeeding. In the present study, this indicates that the value attached to breast-feeding by both types of mothers is the same. For this study, therefore, initiation of breast-feeding was not picked as a risk factor for malnutrition. Different authors have different views on the issue of appropriate duration of exclusive breastfeeding and timing of introduction of complementary foods. In this connection, Waterlow et al. (23,24) suggested that breast milk alone is insufficient to meet the nutritional needs of infants after the age of three months. In contrast, others, for example, Juez et al. (4) and Brown et al. (25) reported that introducing complementary foods before six months has no nutritional benefit to children. The observation of prolonged exclusive breastfeeding (beyond four months of age) in a significantly high proportion of mothers in the malnourished type of households supports Waterlow’s contention (23,24) and indicates that exclusive breastfeeding beyond four months of life is a risk factor for developing malnutrition. Hence, this finding suggests that there is a need for a further investigation on the appropriate duration of exclusive breastfeeding and review the current recommendation (26), which supports supplementation to be at six months of age. This study has also shown that the practice of prolonged exclusive breastfeeding (between four and six months and even beyond this age) is a common occurrence among the low income households. This would suggest that delayed introduction of complementary foods which was observed in the malnourished households is a function of household-food insecurity. Thus, an intervention programme that would be initiated in the urban slums should focus on those families whose monthly income falls below 250 Birr. The relatively higher median duration of breastfeeding observed in malnourished households whose income is low is also another confirmation that mothers in these households have little choice other than depend mainly on breast-milk or may be they are not knowledgeable. The observation that, there was a higher proportion of malnourished children receiving non-enriched porridge (only cereal preparations) than well-nourished children is in agreement with the finding of Getaneh et al. (13) who demonstrated that malnutrition is highest in children whose diet is cerealbased. The practice of giving only cereal preparations may be due to lack of mothers’ knowledge about the importance of enriching weaning foods as better child-care practice or their economic constraints may limit their ability to improve the quality of the diet. Although cow-milk was given by most mothers in the two groups of households, the amount of milk fed to both types of children may have been very low to account for differences in nutrient intake. The significantly higher protein intake by children in the well nourished households may have been increased by consumption of enriched porridge and probably by the intake of other foods as shown by the greater frequency of feeding in these households. Most of the traditional weaning foods given to children are known to be bulky and to have low nutrient density. A young child has a limited capacity to manage large amounts of food at a time and, hence, requires frequent feeding to get enough nutrients. Recommendation to date is that feeding frequency be, at least, four times per day (27). The finding that a significantly higher proportion of well-nourished children received four or more meals/day as compared to malnourished children underscores the importance of frequent feeding and confirms that four times is the critical minimum frequency to avoid the risk of malnutrition. The practice of infrequent feeding of foods which are, in fact, too bulky, as reported widely in many 234 Ethiop.J.Health Dev. ─────────────────────────────────────────────────────────── ─ developing countries (28), does not only result in low energy and protein intake but also low intake of micro-nutrient. This could be aggravated by failure to give vegetables and fruits as reported by both types of households and the poor bio-availability of nutrients as most of the weaning foods used by both types of households are composed exclusively of plant sources. The significantly high use of bottles for feeding porridge in the malnourished households could have resulted in more contamination of the porridge due to poor cleaning of the bottles or prolonged holding of porridge in the bottles. This may have resulted in higher diarrhoeal occurrence in these households than in well-nourished households. Contamination of weaning preparations that are fed through feeding bottles result in marasmus and other types of malnutrition, namely, kwashiorkor and marasmic kwashiorkor as a consequence of infections (29). In conclusion, the findings of this study led to the realization that prolongation of exclusive breastfeeding beyond four months of age, feeding supplementary diet with a frequency of less than four times within a day, partaking of porridge using feeding-bottles, and the practice of feeding weaning diets made exclusively from cereal sources are the principal risk factors which brought about nutritional deprivation among children in the slum section of Addis Ababa. Therefore, it is recommended that mothers should be advised not to continue exclusive breastfeeding beyond four months and, instead, supplementation should begin at this age. Since the preparation of weaning diets from a single food group leads to the formulation of low quality diet, demonstrative and sustained nutrition education on preparation of nutritious diets from home- available foods is strongly recommended. The processing of legume-based low-cost weaning foods by women groups can play an important role in making available such an appropriate child food. There is also need to advise the slum communities to avoid the practice of giving porridge with bottle and nutritionists, health workers and other cadres of nutrition should also continue the advocacy of four times a day as the critical minimum feeding frequency. The study has also led to the conclusion that families whose income is less than 250 Birr are the high-risk group of prolonged exclusive breastfeeding and, inevitably, to child-nutrition insecurity. Hence, an intervention programme that would be initiated in the urban slums with a view of enhancing household income should be planned in favour of these groups. Acknowledgments The authors gratefully acknowledge the United Nations University (UNU) for financing this research; the interviewers, Ato Seid Endris and Woizero Brehane Gabissa, for their excellent field work, and the mothers who participated in this study. The authors also express their sincere appreciation and thanks to those who provided assistance whilst analyzing the data at the Unit of Applied Nutrition Programme at the University of Nairobi. References 1. Harpham T, Lusty T and Vaughan P. In the shadow of the city: community health and the urban poor. Oxford University Press, Oxford. 1988;24-31. 2. Khanjanasthiti P and Wray JD. Early protein calorie malnutrition in slum areas of Bankok Municipality, 1970-971. In: Harpham T, Lusty T and Vaughan P. (Eds). In the shadow of the city: Community health and the urban poor. Oxford University Press, Oxford. 1974;50:67. 3. Jha SS. Urban Health in Underdeveloped Countries With Special Reference to Women and Children. In: Harpham T, Lusty T and Vughan P. (Eds). In Shadow of the City: Community Health and the Urban Poor. Oxford University Press, Oxford. 1985;44. 4. Juex G, Diaz S, Casado ME. Growth patterns of selected urban Chilean infants during exclusive breastfeeding. Am J Clin Nutr. 1983;38:462-468. Child feeding practices as predictors of nutritional status of children 235 ─────────────────────────────────────────────────────────── ─ 5. Basta SS. Nutrition and health in low income urban areas of the third world. In : Harpham T, Lusty T and Vughan P. (Eds). In the shadow of the city: Community health and the urban poor. Oxford University Press, Oxford. 1977;46-7. 6. Waihenya EW, Kogi-Makau W and Muita JW. Maternal Nutritional Knowledge and the Nutritional Status of Pre-school Children in a Nairobi Slum. East Afr Med J. 1996; 73(7): 422. 7. Hofvander Y, Eksmyr R. Anthropometry of children in typical rural district and an urban slum in Ethiopia: A cross-sectional survey of 1093 children. Courrier. 1970; xxi(1):1-4. 8. UNICEF. Strategies of Improving Nutrition of Children and Women in Developing Countries. New York. 1990;1-12. 9. Engle PL. Care and child nutrition. Theme paper for the International Conference on Nutrition (ICN): Paper prepared for nutrition section, UNICEF, New York. 1992;5-8,13-47. 10. Latham MC. Human Nutrition in the Developing World. FAO, Rome. 997:15-36. 11. Gopaldas T, Patel P and Bakshi M. Selected socio-economic, environmental, maternal and child factors associated with the nutritional status of infants and toddlers. Food and Nutr Bull. 1988;10(4):29-34. 12. Mazur R and Sanders D. Socioeconomic factors associated with child health and nutrition in periurban Zimbabwe. Ecology of Food and Nutrition. 1988;22:19-32. 13. Getaneh T, Assefa A and Tadesse Z. Protein-Energy Malnutrition in Urban Children: Prevalence and Determinants. Ethiop Med J. 1998;36:153-166. 14. CSA. Report on the National Rural Nutrition Survey, Core Module. Statistical Bull. 1992;69-81. 15. Wolde Michael G and Demeke T. A report on the nutritional status of children in Addis Ababa, Joint Ethiopian Nutrition Institute and Municipality of Addis Ababa Undertaking. 1985;15 (unpublished). 16. Jembere T. A case study of the health component in kebele 41, “Kefitegna”3. In: Harpham T, Lusty T and Vaughan P. (Eds). In the shadow of the city: Community health and the urban poor. Oxford University Press, Oxford. 1985;153-162. 17. Fisher AA, laing JE and Townsend JW. Hand book for family planning operations research and design. Operations Research, population Council, USA. 1991;40-46. 18. CSA. The transitional Government of Ethiopia. The 1994 Population and Housing Census of Ethiopia. Results for Addis Ababa, Ethiopia. 1994;1:18-19. 19. UN. How to weigh and measure children-Assessing the nutritional status of young children in household surveys. United Nations Department of Technical Co-Operation for Development and Statistical office, New York. 1986; 8-11,29-41,60-66. 20. Tessema T and Hailu A. Childhood Feeding Practices in North Ethiopia. East Afr Med J. 1996;74(2):94. 21. Ketsela T and Kebede D. Pattern of feeding of infants in Addis Ababa, Ethiopia. Ethiop J of Hlth Dev. 1996;10(1):57-65. 22. Bredan SA and Shiwah MS. Infant feeding practices among urban Libyan women. Food Nutr Bull. 1988;10(1):39-42. 23. Waterlow JC and Thomson AM. Observations on the adequacy of breastfeeding. Lancet. 1979;2:238-242. 24. Waterlow JC, Ashworth AA, Griffiths M. faltering in infant growth in less developed countries. Lancet. 1980;2:1176-1177. 25. Brown KH, Creed-Kanashiro H and Dewey KG. Optimal complementary feeding practices to prevent childhood malnutrition in developing countries. Food and Nutr Bull. 1995; 16(4):320-336. 26. UNICEF. The State of the World’s Children. New York. 1998;27,98. 27. Brown KH, Sanchez-grinan M, Perez F, Peerson JM, Ganoza L, Stern JS. Effects of dietary energy density and feeding frequency on total daily energy intakes by recovering malnourished children. Am J Clin Nutr. 1995;62(4):13-8. 28. Mitzner K, Scrimshaw N and Morgan R. Improving the Nutritional Status of Children During the Weaning Period. A Manual for Policy makers, Program Planners, and Fieldworkers. International Food and Nutrition Program, Cambridge, USA. 1984;34,56,79, 151,181. 29. Pellet P1. Commentary: marasmus in a newly rich urbanized society. Ecology of Food and Nutrition. 1977; 6:53-56. Original article Chemical, physical, and microbiological characterstics of various sources of water in and around Addis Ababa Yesehak Worku1, Sinknesh Ejigu2, Worku Erge3, Leykun Jemaneh3 Abstract: Every month, from November 1996 to October 1997, water samples from 18 different sites were collected. The samples belong to the following categories: reservoirs that supply Addis Abeba's tap water (Lakes Gefersa and Legadadi) city taps, city swimming pools, Ambo Mineral Water, rain water, Akaki and Bulbula Rivers and Lake Aba Samuel. Four different physical variables (PH, Temperature, Total Dissolved Solids, and Conductivity) and concentration of 19 different cations, anions, and CO2 were determined. The results revealed no health risk except the high concentration of Cr3+, Cd2+, Fe3+, Pb2+, Mn4+ and Nitrate in Akaki and Bulbula Rivers samples. The water from these rivers is not consumed by city residents although they are used by rural communities to the east and southeast of Addis Abeba. Similarly, the two swimming pools included in this study had high TDS,HCO3- and fluoride content as well as slightly increased Cd2+, Pb2+ and Cu2+ levels. On the other hand, parasitological and bacteriological analyses revealed all sources were clean except Akaki, Bulbula and Aba Samuel. Infact these results suggest drinking waters of Addis Abeba are safe, while recreational waters of the city are acceptable for the purpose they serve. However, in view of polluted rivers flowing out of Addis Abeba and Lake Aba Samuel, methods of minimizing the health risks they pose are suggested. [Ethiop. J. Health Dev. 1999;13(3):239-246] Introduction Next to Oxygen, water is the most important substance for human existence(1). It is an essential nutrient, which also sustains agriculture, allows aquatic life, supports industry, produces hydroelectricity, permits aquatic transport, insures personal hygiene, maintains clean environment, and is used for sport as well as for recreation (2,3). Certainly, man gets the benefits listed above from the entire water resources of the world which is estimated to be 1.4 x 109 km3 (4). However for the, most part, human existence depends on fresh water supply which is less than 1% of the water available on Planet earth (5). The fresh water of the world is obtained from the annual precipitation of about 10 5 km3 (6) out of which Ethiopia's yearly share is estimated to be 110km3 (2). However, 75% of this water vanishes through the borders with neighboring countries (7) leaving behind 27.5km3. On the other hand, since this water is not evenly distributed, arid and semiarid regions of the country are threatened by desertification(7). Hence, the need for methods of water impounding and conservation as practised by some regional governments of Ethiopia. This task becomes even more pressing as industrialization and development advances. In addition to the process of desertification, pollution is also reducing the volume of safe fishing, irrigation, and drinking, water. For instance a USA report revealed that consumption of sea food products had led to increased morbidity and mortality(8). Likewise cancer mortality due to exposure _______________________________________ 1 Department of Biochemistry, Faculty of Medicine, Addis Ababa University, Addis Ababa, Ethiopia; 2Ministry of Mines, Addis Ababa, Ethiopia; 3Department of Microbiology, Faculty of Medicine, AAU. of ground water to hazardous chemicals is increasing (9). Radioactive wastes discharged in the1950s 238 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── in some Russian rivers are still contaminating the food chain (10). Furthermore, a review by Pruss (11) indicated that swimming in waters containing upto 30 CFU/100mL of E.coli and faecal streptococci caused gastroenteritis. Notice that there is a minimum level of cleanliness accepted for accidental swallowing and skin exposure let alone for consumption and other sensitive uses of water. Ethiopia is no exception to excreta and organic pollutions mentioned above. It is proving hard to give up open air defecation inspite of the acute sense of embarrassment by those who practise it and its' condemnation by communities (12). Teka (13) had shown that in Ethiopia, water and excreta based diseases are on the rise. Household and other rubbish are thrown away with little, if any, regard to one's actions. It is common knowledge that several factories dump their dangerous waste into ditches and rivers. It is not possible to claim that this carelessness is restricted to organic waste either. While some effort is made to store or bury radioactive waste by some institutions, careless dumping can never be ruled out. In general apathy of offenders, behavioural tolerance of the community, lack of knowledge about consequences of pollution, and cultural insensitivity of the vast majority of the population to environmental degradation is an alarming phenomenon that demands urgent action. It is clear from the above that we should make a ceaseless effort to avoid chemical, microbial, etc. pollution of the environment in general and water resources in particular. In view of the above it is necessary to seek the basic physical, chemical, and microbial profile of Ethiopia's water resources in general. However, this paper focuses on the limited objective of compiling an annual chemical, bacteriological, and parasitilogical composition of some water resources in and around Addis Abeba. It is also a more extended version of an earlier investigation by Worku and Ejigu, 1994 (14) which was based on a single month's sample collection and never included microbial and parasitic analysis. Finaly, it tries to draw attention to water resources that are polluted by the city. Methods Sample collection: Every month, 18 different water samples were obtained from November 96 to October 97. The collection was made, from the following sites representing Addis Ababa's various water sources, namely, the two upstream reservoirs at Gefersa and Legedadi (both raw and treated waters), tap waters from various locations in the city, a mineral water bottled in Ethiopia, rain water, (roof-run-off from a house in Woreda 19 was collected after rain was allowed to clean the roof), two city rivers (Akaki and Bulbula) that serve as sources of drinking water for humans and animals living in rural areas east and southeast of the city, Lake Aba Samuel (a dam that receives most of the city's liquid waste), and two swimming pools in the city (Figure 1). For each water source, the sampling site was never changed. Figure 1: Map of sample collection sites Chemistry and microbiology of water 239 ──────────────────────────────────────────────────────────── Note: The numbers within Addis Ababa are code numbers of Weredas (Councills). The black dots are sampling sites. Ambo is 125km west of Addis Ababa. All samples were collected by grab method. Reservoir samples were from Addis Ababa Water and Sewerage Authority's sampling taps. Ambo Mineral Water samples were collected at official sampling taps. Samples from swimming pools, city rivers, and Aba Samuel were surface waters. Water from domestic taps of various weredas were collected after discharging about a liter of water at every sampling site. Rain water was collected by a method stated above. Methods on chemical and physical characteristics: Every month, a single 5L sample was collected per location in a plastic bottle thoroughly cleaned by detergent, hypochlorous acid, distilled water, and finally rinsed with deionized water. The samples were then filtered using Whatman's No 42 filter paper and stored at 4oC until analysis was carried out. Temperature was taken at the time of sample collection. Information on the odour, taste, and colour of each sample was obtained from five water laboratory technicians. The pH was read on calibrated Beckman's 050pH meter. Conductivity (con.) was read on microprocessor LF 2000/C conductivity meter of GmbH W. Germany, which was calibrated using 10,25,50,75, and 100mM standard KCl solutions. Both Beckman's 050pH meter and LF 2000/C possess inbuilt programmes that calculate and display readout at 25 oC. The total dissolved solids (TDS) of a sample that was evaporated by a steam bath and dried at 105oC was measured using an analytical balance. The cations (Sodium, Potassium, Magnesium, Calcium, Iron, Cadmium, Chromium, Lead and Zinc) were determined by atomic absorption spectrometer (Varian SP-20) using their respective hollow cathode lamps (15). Carbondioxide and Bicarbonate were measured by titration using phenolphthalein and methyl orange indicators, respectively(16). Since bottles of Ambo Mineral Water were opened under atmospheric pressure and 100C, reported Carbondioxide content is nearer to what is available to the consumer and not the quantity bottled by the factory, i.e., minimum values are reported. Chloride was titrated by 10mM AgNO3 to K2CrO4 endpoint(17). Fluoride was assayed by a specific ion selective electrode (18). Sulphate was determined as BaSO4 particles in a turbid solution (19). Nitrate was estimated using Varian DMS 80 spectrophotometer set at two different wave lengths. The absorption at 220nm is for nitrate and organic nitrogen whereas the absorption at 275nm is only for the latter. Optical density due to nitrate was then obtained by subtracting double the reading at 275nm from the reading at 220nm(20). Method on bacteriological characteristics: All microbial analyses were conducted within 48 hours of sample collection using portions of the 5L sample that were never subjected to Whatman's No. 42. Tests were conducted using 100mL of water aseptically filtered through a nitrocellulose filter (Gelman Sciences, Michigan, USA). The filters were then layered on endoagar. After 24 hours, the number of visible colonies were counted (21). Further tests were conducted on those membranes that had viable bacterial colonies. To do this, 10ml of Lauryl tryptose broth (35.6gm/L) was inoculated by about 10 viable colonies, and the mixture was incubated at 370 C for 24 hours. Those samples that displayed gas inclusion in tube inserts were then subjected to Brilliant Green Lactose broth at 37oC for 24 hours and the presence of gas emission was checked. Final test to identify whether the organisms were E.coli or other Enterobacter species was done using Eosin methylene blue agar's confirmatory test (21,22). Method on parasitological characteristics: Parasitological tests were conducted on samples of 100mL of water by modification of the method of Levine and Estenez (23). The samples were concentrated by centrifugation. Then one drop of the sediment was resuspended in one drop of 0.85% saline and an aliquot was applied to a slide. The preparation mentioned above was viewed under low power microscope for cyst or ova. At times iodine was added for detection of protozoan cysts. 240 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Table 1: Annual averages of physical and chemical characterisitcs of water samples collected from November 1996 to October 1997 from sites stated. Sites Analyte Akaki Bulbula Aba Samuel pH T Con TDS Na+ K+ Mg2+ Ca2+ Cr2+ Cd2+ Fe3+ Pb2+ Zn2+ CIFCO2 HCO3NO3SiO2 SO4= HBO2 Cu2+ Mn4+ 7.64 6.00 486.33 386.41 35.75 15.35 9.14 41.83 0.10 0.10 0.11 0.10 0.10 43.92 0.38 22.78 212.08 2.45 23.25 7.07 0.33 0.10 0.10 7.54 8.25 876.75 652.83 50.10 26.70 15.5 53.17 0.10 0.10 0.41 0.10 0.10 97.41 0.61 24.3 255.25 10.96 28.67 29.08 1.15 0.08 0.58 7.67 18.67 377.33 341.58 32.08 8.13 9.33 36.08 0.10 1.93 0.38 0.10 0.10 23.83 0.63 12.6 179.08 22.28 34.00 8.50 0.41 0.10 0.10 W 17 Bole 7.47 18.75 93.33 76.58 2.23 1.68 2.42 10.28 0.10 0.10 0.06 0.10 0.46 6.42 0.16 4.58 38.33 2.93 10.08 2.81 0.42 0.10 0.10 Gefersa Raw Gefersa Treated 7.12 17.25 60.25 56.00 2.33 1.42 2.06 5.62 0.10 0.10 1.93 0.10 0.10 0.87 0.08 5.58 27.33 2.41 11.50 5.06 0.39 0.10 0.10 7.16 16.33 108.25 79.75 2.29 1.07 2.08 12.35 0.10 0.10 0.11 0.10 0.13 3.25 0.06 4.17 20.50 1.20 6.83 24.5 0.34 0.10 0.10 Legedadi Raw 7.37 17.75 84.50 81.50 2.27 2.30 3.11 11.00 0.18 0.10 4.20 0.18 0.13 0.72 0.46 4.92 42.42 3.66 15.08 8.12 0.50 0.10 0.10 Legedadi Treat Nefas Silk W 18 Gulele 7.44 16.83 90.75 72.83 2.24 1.64 2.46 9.87 0.10 0.10 0.00 0.09 0.10 5.67 0.16 4.00 36.58 2.90 10.25 2.20 0.72 0.05 0.10 7.43 16.83 97.25 77.17 2.26 1.64 2.54 10.83 0.10 0.23 0.10 0.10 0.36 5.83 0.16 4.55 36.58 2.81 9.92 3.85 0.26 0.11 0.10 7.7 17.5 423.2 140.2 6.55 1.63 5.33 15.5 0.10 0.10 0.10 0.10 0.50 2.95 0.24 5.67 79.25 9.38 27.58 1.09 0.36 0.10 0.10 Chemistry and microbiology of water 241 ──────────────────────────────────────────────────────────── (Table 1 continued) Analyte Sites W 15 Kasanchis W5 Merkato Ambo Raw Ambo Treated W 15 Hilton W 21 Ghion W 23 Makanisa W 19 Rain Normal Value pH 7.41 7.19 6.41 5.82 8.0 8.56 7.22 6.33 6.5-8.5 T 8.08 17.75 31.0 22.0 35.50 27.42 19.0 12.8 - Con 92.2 95.2 1664 1653.2 2938.8 1236.6 108.9 34.0 50-1500 TDS 74.4 74.1 1415.8 1406.9 2575 1016.2 82.1 27.6 1000 Na+ 2.25 2.18 222.31 244.27 807.08 291.2 10.58 0.21 200 K+ 1.63 1.32 32.36 30.91 13.74 7.05 1.69 0.66 - 2+ Mg 5.33 2.33 44.64 40.59 1.74 2.18 2.46 0.23 50 Ca2+ 15.5 10.48 72.36 64.91 4.58 8.17 8.72 3.76 75 Cr2+ 0.10 0.11 0.10 0.10 0.10 0.10 0.10 0.10 0.05 Cd2+ 0.10 0.10 0.10 0.10 0.10 0.10 0.10 0.10 0.005 Fe3+ 0.10 0.12 0.10 0.10 0.10 0.10 0.10 0.10 0.10 Pb2+ 0.10 0.10 0.10 0.10 0.10 0.10 0.10 0.10 0.05 2+ Zn 0.50 3.22 0.10 0.10 0.10 0.10 0.68 1.11 5.00 CI 2.95 5.50 30.55 33.91 47.35 26.58 7.35 1.03 250 F0.24 0.11 0.69 0.70 22.54 7.43 0.15 0.03 1.5 CO2 5.67 4.84 582 1730 33.6 7.00 5.85 6.14 6.5-8.5 HCO379.25 28.08 1031.6 1029.27 1764.3 775.9 40.42 4.43 - NO39.38 2.04 2.40 0.55 0.53 3.31 2.06 7.67 10 SiO2 27.58 9.08 36.34 35.82 88.25 35.83 12.17 - - SO4= 1.09 7.92 0.86 0.83 53.58 26.58 1.56 2.80 400 HBO2 0.36 0.28 0.79 0.98 1.38 0.63 0.26 0.37 - Cu2+ 0.10 0.10 0.10 0.10 0.10 0.19 0.10 0.10 0.005 Mn4+ 0.10 0.10 0.16 0.24 0.10 0.10 0.10 0.10 0.10 Temperature (T) is in 0C, Total dissolved solid (TDS) and concentrations are in mg/L, conductivity (con) is in μ-mho/cm . The values given are means. Ssee References 24, 25 and 26 for normal values, conductivity of potable water is from Ref. 15 pages 2-43 to 2-48. W is wereda. -- not known Table 2: Annual mean of coliforms that were detected in sampling sites from November 96 to October 97. S ite Aba Samuel Akaki Bulbula (Gefersa Raw) Legedadi (Raw) Mean(EFU/100mL) 112 270 170 50 79 Data compilation and analysis: The chemical, physical and microbiological results were processed using the World Health Organisation's Epidemiological Computer Programme developed by CDC in 1994, i.e., Epi. info version 6.22 (Epi-6). The information collected included mean, SD, p-value, etc. The mean was based on 12 averages except for rain water which was from nine sample collections. Each average was done on triplicates of a single sample. Standard error of the mean of each average was < 5%. Results Chemical and physical characteristics: All filtered water samples were colourless. However, unfiltered water samples of Gefersa and Legadaddi were brownish yellow. None of the samples had any dectetable odour. Since Akaki, Bulbula, and Aba Samuel waters were polluted with excreta, their tastes was not determined. The raw Mineral Water had a blend of sour and bitter taste whereas the treated Mineral Water had Soda flavour. All the other samples were tasteless. Table 1 presents chemical and physical characteristics of samples from 18 different localities. Measurements collected over 12 months were processed by Epi-6 and only the mean values are displayed. Notice, conductivity and total dissolved solid of two groups of water were very high compared to that of pure water : 1. Akaki River, Bulbula River, and Lake Aba Samuel; 2. The swimming pools of Hilton and Ghion as well as Ambo Mineral Water. Furthermore, the sodium content of the mineral water under investigation was also high (244mg/L) compared to WHO's guideline value of 200mg/L (24). On the other hand, lowest conductivity and lowest total dissolved 242 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── solid were determined for rain water. Table 3: Number of Cysts or Ova detected in 100mL samples from Novermber 1996 to October 1997 from the sites stated Sites & counts/100mL Species Month Aba Akaki Bulbula Gefersa (Raw) Samuel Entamoeba Coli December’96 3 4 January’97 1 5 2 February 2 March 3 April 1 2 May 2 Etamoeba histolytica November’96 3 1 December 3 January’97 4 3 February 2 March 8 April 2 T. Trichuria November’96 3 January’97 6 - Bacteriological characteristics: Every month, for twelve months, triplicate tests were conducted for every sample. The observed, total colony forming units/100mL of E.coli and/or Enterobacter species are displayed in Table 2. All others (13 sample sites) except the five listed below gave results that were not detectable. Parasitological characteristics: Every month, for twelve months, triplicate tests were conducted for every sample. No parasite ova or cyst was detected in treated water of Legedadi and Gefersa, tap waters of Addis Abeba, raw or treated mineral waters, swimming pools, or rain water of Addis Abeba. Parasites were seen only in samples and months indicated in table 3. Even for these sites, detections were not throughout the year but were observed for a few months (Table 3). Discussion During this study, no bacteriological or parasitological organisms were seen in samples of treated water of Legedadi, Gefersa, Addis Abeba taps, rain water, and mineral waters. The concentration of various analytes were also within the normal values accepted by WHO (24,25 & 26) although conductivity, TDS, Sodium, CO2 , HCO3- concentration of the mineral waters were also high. Neverthless, the aformentioned TDS is within 150% of the normal value and is probably tolerated. Equally, the high concentration of CO2 and HCO3- is unlikely to pose any health risk since CO2 toxicity, except in suffocation, is unknown (27). Similarly conductivity, TDS, HCO 3- and fluoride (7.43 mg/L) content of the swimming pools were high. However, they do not pose any health risk, since they are not used for drinking. It is clear from the above that drinking waters of Addis Abeba are safe for health, while recreational waters of the city are acceptable for the purpose they serve. With the exception of Cr3+, Cd2+, Pb2+ and Fe3+ concentrations that were at 2 the normal values, the raw waters of Gefersa and Legedadi were within WHO's guideline values. However, occasionally parasite ova/cyst were detected in samples from those sites. Their bacterial contamination which was at less than 100CFU/100mL but higher than the maximum permissible level of 10CFU/100mL poses health risk (26). On the other hand these coli forms might be from livestock excreta and, hence, pose little health risk, particularly to local immune inhabitants. It is clear from the above rigorous effort is needed to minimize the microbial contamination of waters flowing into Legedadi and Gefersa reservoirs. One way to achieve this would be to declare the environs of these Chemistry and microbiology of water 243 ──────────────────────────────────────────────────────────── water sources to be nature's reserve. Except for Cr3+, Cd2+, Fe3+, Pb 2+, Mn 4+ and Nitrate contents all other chemicals tested in this study revealed low values for Akaki and Bulbula Rivers. Nevertheless the deleterious effect of these ions on health can not be underestimated. Likewise parasitic ova/cyst existed for most parts of the year in Akaki. Lower parasitic values that were seen in Bulbula might be attributed to the fact that samples were collected in rural area almost near the entry point of Bulbula to Aba Samuel whereas Akaki River's samples were from Saris Market to the East of Bhere-Tsege garden, i.e., one of the most polluted sections of the river. Aba Samuel samples were from the dam end of the lake, hence, parasite ova/cyst had time to settle to the bottom of the lake or adhere to the dense tuber vegetation that completely covered the lake. Further more, the rate of bulk water flow through the lake is low, hence, time is in favour of lower parasite burden of the water at the outlet of the dam. Lower parasite levels of the rivers that were registered from May to September can be attributed to the dilution effect of rain. All the same, the presence of bacteria at >100 CFU/100mL is indicative of faecal contamination making these waters a high health risk. Inspite of the above, Akaki, Bulbula and Aba Samuel waters are used to grow vegetables that are sold in Zone 3 markets, to water animals, and as drinking water of rural communities outside Addis Abeba. Recommendations In view of the pollution stated earlier and economic significance of these waters, more effort should be made to teach the local community on methods of minimizing the deleterious effects of their water supply. One approach could be drinking water from wells dug a few meters away from these bodies of water, thus benefiting from ground filtration of the polluted water. Furthermore, awareness of hygenic handling of vegetables should be introduced. In addition, the following future actions may be considered; 1. Conduct organic analysis of these sites since factories are in the habit of releasing their effluents; 2. Encourage industries on alternative method of waste disposal; 3. Conduct skin test, kidney function test, stool examination, etc. in communities that depend on these water sources using a rural community between Akaki Town and Aba Samuel, that has access to clean well water, as control. Last but not least, there is a need to draw the attention of the Water and Sewerage Authority or all concerned to consider methods of minimizing faecal pollution of Akaki, Bulbula, and Aba Samuel. Acknowledgements This study was supported by the Ethiopian Science and Technology Commission with some assistance from Addis Abeba University. The samples were collected by permission of Ethiopian Water and Sewerage Authority as well as Ambo-Mineral Water Bottling Factory. Microbiological reagents were bought through Armeur Hanson Research Laboratory. We are profoundly grateful to all institutions mentioned above. We are also grateful to many technicians who helped us to do this project, particularly Ato Kassu Desta, without whom this work was almost impossible. We are indebted to Ato Kidane Mariam G/Eyesus who did the statistical analysis. Finally we are grateful to W/o Yenesew Bekele, Biochemistry Lab assistant and W/o Haimete Abraham the Department's secretary, who put up with the numerous corrections during typing. References 1. White G. (Ed.), Water, Health and Society. Selected works by Abel Wolman. Indiana university press, 1969:3 2. Ethiopian Federal Democratic Republic's Water Resources Policy. Ministry of Water Resources, Addis Abeba, May 1997. 3. Falkenmark M.(Ed.), Rural Water and Health. Scandinavian Institute of African Studies, Uppsala, 1982;75-83. 4. Gross MG. Oceanography: A view of the earth, 4 th edition. Prentice-Hall Inc., New Jer 1987;365-67. 5. Reagen PA and Bookins-Fisher J. In: Community health in the 21st century. Water quality. Masssachussets, Allyn and Bacon, 1997;439-62. 6. Teka Gebre-Emanuel. Water Supply-Ethiopia: An introduction to environmental health practise. Addis Abeba University press, Addis Abeba, Ethiopia, 1977;16-28. 7. Ethiopian Federal Democratic Republic's National Action plan to Combat Dese-rtification, Environmental protection Authority, Addis Abeba, September 1998;1:3-8. 8. Lipp EK and Rose JB. The Role of Seafood in foodborne diseases in the United States of America. Rev Sci Tech 1997;16:620-40. 9. Griffith J Duncan RC, Riggan WB and Peltern AC. Cancer mortality in US counties with hazardous waste sites and ground water pollution. Arch Envion Health 1989;44:69-74. 10. Kryshew II, Romanov GN, Sazykina TG, Isaeva LN, Trabalka JR and Blaylock BG. Environmental Contamination and assessment of doses from radiation releases in Southern Urals. Health Phys 1998;74:687-97. 11. Pruss A. Review of Epidemiological Studies on health effects from exposure to recreational water. Int J Epidemol. 1998;27:1-9.12. 12. Demamu S; Ismail S and Yihdegu M. The nominal group technique for participating communities in analyzing rural town water and sanitation situation Ethiop J Health Dev 1997;11(1):37-42. 13. Teka Gebre-Emanuel. Environmental Health: Water supply & Sanitation Status in Ethiopia. Issues & constrains. 1991;6-10. 14. Worku Y and Ejigu S. Some Chemical Constituents of selected water Sources In and Around Addis Ababa and Ambo. Ethiop J Health Dev. 1994;8(2):97-102. 15. American Public Health, American water works Assoc., Water pollution and Control Federation. Metals by Atomic Absorption Spectrophotometry. In standard method: For examination of water and waste water. 19th Ed., Washington, American public Health Assoc., 1995;3:43-3.107. 16. Titremetric method for carbondioxide. Ibid, 4-17. 17. Cotlove E. Determination of Chloride in Biological materials. Methods of Biochemical Analysis 1964;12:277-391. 18. Oesch U. Ammann D and Simon W. Ion selective memberane electrode for clinical use. Clin Chem 1986;32: 1448-59. 19. Jackson SG and Mc Candless, E.L. Simple, Rapid, Turbidometric determination of Inorganic sulphate and/or protein. Anal Biochem 1978;90:802-8. 20. Miles DL and Epejo CK. Comparison between an Ultraviolet spectrophotometric and the 2,4-xylenol method for the determination of Nitrate in Ground waters of low salinity. Analyst 1977;102:104-9. 21. Pelczar JR MJ, Chan ESC, Krieg NR. Microbiology 2nd ed., Singapore Fong and Sons Printers Pte Ltd. 1988; 599-600. 22. Eduards PR, Ewing NH. Identification of Enterobacteriaceae. In Ewing WH. ed. Identification of Enterobacteriaceae, 3rd. ed., Minneapolis: Burgess Publishing Company, 1972;7-47. 23. Levine JA, Estenez EG. Method for Concentration of Parasites from small amounts of faeces JClin Microbiol. 1983;18:786-788. 24. WHO. Global pollution & Health: Result of health related environmental monitoring. UNEP & WHO, Global Environmental monitoring system, London 1987;12. 25. WHO. Guidelines for drinking water Quality. Recommendations, WHO, Geneva, 1984;1:6-8. 26. Ethiopian Standards Regulations No. 12/1990, Negarit Gazeta, No. 25; Addis Abeba, September 1990. 27. Trevethick RA. Environmental and Industrial Hazard. London, William Heinemann, 1973;42-43. Original article Trends in suicide, parasuicide and accidental poisoning in Addis Ababa, Ethiopia. Abdulreshid Abdullahi Bekry Abstract: Because of lack of compiled data on Suicide, Parasuicide and Accidental Poisoning (AP) in the general population and in over 15 year olds in Addis Ababa, Ethiopia, it was essential to prepare and analyze these basic data. The average crude suicide rate for over 15 year olds was found to be 12.7 and 2.45 for males and females, respectively. The difference between male and female rates is significant (P<0.002). The commonest method of committing suicide was by hanging and strangulation (70.2%). Suicide rates showed marked declines, especially in males, during exacerbation of the civil wars. The average standardized parasuicide rate was found to be 74.85 and 25.93 for males and females respectively. The difference between male and female rates is significant (P<0.002). In over 15 year olds, 83.91% of parasuicides were in the age group of 15-44 and males in this age group had the highest parasuicide rate (122.03). Trends of parasuicide rates had indicated high peaks during stressful years. The average standardized AP rate was found to be 14.17 and 8.19 for males and females respectively. The differences between male and female rates is significant ( P<0.002). In over 15 year olds, 76% of AP cases were in the age group of 15-44, but males in the age group of 45-64 had the highest AP rate (19.37). Possible reasons for changes in the trends of these three phenomena are discussed. [Ethiop. J. Health Dev. 1999;13(3):247-261] Introduction Suicide is defined as an intentional, self-inflicted death while ‘attempted suicide’ is defined as a non-fatal suicidal act. The terms ‘suicidal behavior’, which generally embraces both Suicide and ‘Attempted Suicide’, and “suicidal ideation” are extreme expressions of underlying psychopathology, not diagnoses by themselves (1, 2, 3). In a genuine suicidal act, a person having decided to end up his life, or acting on a sudden impulse to do so, kills himself, having chosen the most effective method available and having made sure that nobody interferes. The definition and categorization of ‘Attempted Suicide’ is far from simple as the outcome of a suicidal act may depend on outside intervention, irrespective of the seriousness of the suicidal behavior. The attempters usually recognize that the means are non-lethal and they have different characteristics than patients who display lethal suicidal behavior. In other words, those who attempt and those who commit suicide constitute two different groups of populations, which may overlap (1). Studies show that between 14% and 51% of adolescent attempters repeat their attempts depending partially on length of follow-up period (4). Therefore, one can not discount the importance of ‘Attempted Suicide’. Sex and age composition and the peak age for Suicides and ‘Attempted Suicides’ are different. More men than women kill themselves, but more women than men attempt Suicide. It has usually been found that the peak age for Suicides lies between 55 and 65 years and for ‘Attempted Suicide’ between 24 and 44 years (2,3). The methods and the settings are very important in the determination of the risk-to-rescue fantasy ratio. Attempters have a lower ratio than those who complete Suicide (4). ______________________________________ 1 Department of Psychiatry, Faculty of Medicine, Addis Ababa University, P.O. Box 9089, Addis Abeba, Ethiopia. Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 247 ──────────────────────────────────────────────────────────── Many people deny suicidal intentions after an act of self-damage, because they feel ashamed and guilty. They may not want to tell the truth, or their intentions may have been confused at times (1). As Kreitman has pointed out, intention can not be used as a criterion since the person’s motive may be too uncertain or too complex to ascertain readily. Therefore, more and more authors on the subject prefer the term ‘Parasuicide’ to ‘Attempted Suicide’ since it makes no reference to intention (4). The term ‘Parasuicide’ covers behaviors that can vary from suicidal gestures and manipulative attempts to serious but unsuccessful attempts to kill oneself (2,4). Hereafter, in this paper, the term ‘Parasuicide’ will be used as much as possible instead of ‘Attempted Suicide’. Suicide is certainly under-reported to some extent everywhere. If the agent responsible for certifying deaths in a country is reluctant to report death as Suicide, due to lack of clear evidence that the injury was self-inflicted and that the individual intendeds to kill himself, the most likely categories for reporting the case are ‘Undetermined Cause of Death’ or ‘Accidental Death’(1,4). Experience in Addis Ababa indicates that Suicides and Parasuicides by poisoning are also incorrectly recorded as ‘Death due to Accidental Poisoning’ and ‘Accidental Poisoning’, respectively. According to the 8th edition of the International Classification of Diseaes (5), doubtful cases of Suicide may be placed in a category of death - ‘Injury undetermined whether accidentally or purposely inflicted (E980-E989)’ which also include doubtful Homicides (6). Barraclough (7) believes that in the UK the majority of cases allocated in this category are probably equivocal Suicides, since Homicides are rare and usually obvious, and doubtful accidents will be more readily placed in the accident category. Thus, he believes that the sum of the Suicide rate and the ‘Undetermined Death’ rate may be a closer approximation to the true incidence of Suicide than Suicide rate alone. When we come to Parasuicide, which is still a legal offense in many countries, it often goes unreported unless hospital treatment has been sought. Therefore, the figures of Parasuicide are less reliable. In 1986, in the USA, Suicide was the 8th leading cause of death, affecting 30,904 people. The true incidence is believed to be far greater. Parasuicide is conservatively estimated to be 10 to 20 times more frequent than successful Suicide (4,8). Statistics of Suicide and Parasuicide show periodic changes in rates for total population and for different sex and age groups. Changes were also observed in the rate of different methods of Suicide and Parasuicide-sometimes one method is substituted for another method (5,9). Social class, religious, and ethnic groups most affected by Suicide and Parasuicide and seasonal variations of these acts have been studied well in developed countries. Crisis interventionists, social workers, and psychiatrists are familiar with methods of predictions of these acts and this has helped them to establish community based ‘Suicide Prevention Centers’. In Addis Ababa, eventhough hospital statistics on Suicide, Parasuicide, and ‘Accidental Poisoning’ are available, they have not been systematically analyzed. Clinical researches also have not been carried out. The reason was that researches on these topics have been rather discouraging because of political consequences as Suicide and Parasuicide were taken as offense against the government. This early notion about Suicide and Parasuicide in Ethiopia is probably changing now and seen as signs of acute emotional disturbance (a cry for help) or a consequence of mental illness. This paper reports the results of the analyses of the compiled data on Suicide, Parasuicide, and ‘Accidental Poisoning’ in different hospitals of Addis Ababa and related information from the Ministry of Health. The main objective was to find out the magnitudes (rates) of Suicide, Parasuicide, and ‘Accidental Poisoning’ in Addis Ababa in different age and sex groups together with seasonal and periodic (yearly) variations. If the magnitudes of these problems are found to be convincing, a proposal will be forwarded to the concerned authorities in Addis Ababa to organize ‘Suicide Prevention Services’, governmental or non-governmental, like ‘Samaritans’. These services could include public education and training within the context of mental health services together with social and psychological support system for the vulnerable groups. It is known that adults differ from children in the incidence of Suicide, Parasuicide, and ‘Accidental 248 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Poisoning’, in the methods used, reasons given, etiologic and psychodynamic factors associated with the incidences of these three phenomena. This paper deals with cases of over 15 years olds, but to have some general view of all ages, sex-specific crude or standardized rates of each category will also be presented and analyzed. Methods Data on suicide, parasuicide and accidental poisoning: Two reliable sources of data were identified in Addis Ababa. 1. All general hospitals, except Dejazmach Balcha, the Army, and the Police Hospitals, include in their monthly reports to the Ministry of Health, the number of cases of Parasuicide (E code No. 148) and ‘Accidental Poisoning’ (E code No. 140) seen at the OPD or admitted to the inpatient departments. If death occurs in the hospital it is certified by the attending physician as ‘completed Suicide’ or as ‘Death after Accidental Poisoning’ or as ‘Death Undetermined whether Accidental or Intentional’ in doubtful cases. Postmortem examination is not mandatory in such circumstances and certificates are issued to the Police Department if requested. But in doubtful cases, the dead body is usually sent to Minilik II Hospital for confirmation. 2. Minilik II hospital has a postmortem examination service carried out by a qualified Pathologist or Forensic Physician. All cases of violent death from Addis Ababa Region and a considerably large number from other regions are taken there by the Police Department to establish causes of deaths. All circumstantial evidences leading to the death are supplied by the Police Department to help the Forensic Physician to decide on the cause of the death. Certificates are issued to the Police Department, but detailed informations are kept in the record book of the Forensic Department of the Hospital. In the record books, some cases do not contain the age of the victim as it was probably difficult to know. Some other important demographic variables also were not available on the record books. The dates of the examination were written either in the E.C. or G.C. and it was difficult for the data collector to convert all the dates to either of the calendars. So the author had to restrict himself to calculating only the crude sex-specific Suicide plus ‘Undetermined Death’ rates and Suicide rates. It was confirmed that in practice a verdict of Suicide is recorded by the Forensic Physician only if there was a clear evidence that the injury was self-inflicted and that the individual intended to kill himself. Methods of committing Suicide also were specified in the record books except in cases of ‘Undetermined Death’. For the purpose of this paper, only Suicide cases and ‘Undetermined Deaths’ from Addis Ababa were included. The rest were excluded. The permission to get access to all hospital monthly reports was obtained from the Medical Directors of the respective hospitals. The general hospitals that handle cases of Parasuicide and ‘Accidental Poisoning’ and submit their monthly reports include St. Paul’s, Ras Desta, Yekatit 12th (adult and pediatrics), Minilik II, Empress Zewditu, Tikur Anbessa, and Ethio-Swedish pediatrics hospitals. The data were collected, by a psychiatric nurse, a trained data collector and by the author himself. Demographic data: The mid-year population (in medium variant) for Addis Ababa, by sex and five year age groups, from 1982 to 1996 was obtained from the 1984 (10) and the 1994 (11) Population and Housing Censuses and from the sample surveys of 1984 (10). These population data are used in calculating yearly rates (per 100,000) of Suicide, Parasuicide and ‘Accidental Poisoning’ for both sexes in the general population and in different age groups (i.e. 0-4, 5-14, 15-44, 45-64, and 65 and above) according to the standard monthly report form of the Ministry of Health. Fiscal year proclamation of 1959(12): Ethiopia follows the Julian Calendar, locally known as Ethiopian Calendar (E.C.), which consists of 12 months, of 30 days each and a 13 th month of five days or six days on leap-years. The 13th month is customarily added to the 12th month (i.e. Nehasie) to make it 35 days or 36 days on the leap-year. All morbidity and mortality statistical reports in Ethiopia traditionally follow the Fiscal Year Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 249 ──────────────────────────────────────────────────────────── Proclamation of 1959 which is fixed at a period of one year (in E.C.) from ‘Hamle’ 1st (i.e. July 8 ) to ‘Senie’ 30 th (i.e. July 7 of the following year). So, the end of the Ethiopian fiscal year coincides roughly with the mid-year of the Gregorian Calendar, the time when the size of the population is estimated. These facts are well known when morbidity and mortality rates are calculated and results obtained are taken to represent that specific Ethiopian fiscal year which covers the duration specified above in the Gregorian Calendar. To make it simple, all tables and graphs in this paper will have the corresponding years and dates in the Gregorian Calendar also. Presentation and analyses of data: Both descriptive and analytical methods are used in the presentation and analyses of data. On Suicide and ‘Undetermined Death’ data collected from the Forensic Department of Minilik II Hospital and other hospitals in Addis Ababa, yearly sex-specific crude suicide death rates and crude suicide plus ‘Undetermined Death’ rates (per 100,000) of 15 years ,from 1974 to 1988 E.C.( i.e., from 1981/’82 to 1995/’96 G.C.), were calculated. Reliable and uniform data collection was started in all civilian government hospitals of Addis Abeba in 1974 E.C. (i.e. 1981/’82 G.C.). These two sets of rates were tabulated and statistically tested whether they maintain their rank order over the 15 years. Differences between male and female rates were tested for singnificance. Two-tailed test was applied here and in all other tests for significance in this paper. Methods of committing suicide were also analyzed and changes in these methods over 15 years were commented upon. On Parasuicide data, standardized rates (per 100,000) for both sexes for the specified 15 years were calculated and tabulated. The differences between male and female Parasuicide rates were tested for significance. Age- and sex-specific Parasuicide rates were calculated for over 15 year olds and also for under 15 year olds. The trends of these age- and sex-specific rates were compared with those of the standardized rates mentioned above. The average number of Parasuicide cases reported in each Ethiopian month for the specified 15 years among those aged 15 and above were calculated. In both age groups, the difference between daily means of the peak month and the trough was tested for significance and possible reasons for these differences were discussed. Similar calculations and analyses were conducted on ‘Accidental Poisoning’ and Parasuicide data. Results Table 1 Shows the number and crude sex-specific rates (per 100,000) of Suicide plus ‘Undetermined Death’ and Suicide Deaths for Addis Abeba in those aged 15 and above from 1974 to 1988 E.C. (i.e. from 1981/’82 to 1995/’96 G.C.). The male crude Suicide Death rates have always been higher throughout the specified 15 years than those of the females. The Wilcoxon’s rank sum test on paired data has shown that these differences are highly significant (P<0.002). In males, the average crude Suicide Death rate of 15 years was 12.71 and in females, it was 2.45 (per 100,000). Thus male-to-female ratio of the average rates is 5.19:1. For both sexes combined, the average crude Suicide rate was 7.76 (per 100,000). Figure 1 demonstrates trends of the above mentioned rates for both sexes. Between 1981/’82 and 1985/ `86 G.C., no clearly apparent divergence was seen on the graph. Between 1986/’87 and 1990/’91 G.C., as more ‘Undetermined Deaths’ were reported in both sexes, slight divergences on the graph become apparent. After 1991/’92 G.C., the number of ‘Undetermined Deaths’, both in males and females, has continued to increase during successive years that the divergence of 250 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Table 1: Numbers and crude sex-specific rates (per 100,000) of suicide plus undetermined deaths and (suicide deaths) for over 15 year olds for Addis Ababa from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), Addis Ababa, 1998. Year in E.C.* Male Female Male & Female (year in G.C.) No. Rate No Rate NO. Rate *2 1974 (1981/82) 74(74) 11.48(11.48) 14(14) 2.02(2.02) 88(88) 6.57(6.57) 1975 (1982/83) 64(64) 9.6(9.6) 10(10) 1.39(1.39) 74(74) 5.35(5.35) 1976 (1983/84) 99(98) 14.36(14.22) 12(12) 1.62(1.62) 111(110) 7.76(7.69) 1977 (1984/85) 85(85) 11.81(11.81) 17(17) 2.20(2.20) 102(102) 6.84(6.84) 1978 (1985/86) 56(56) 7.46(7.46) 8(8) 1.00(1.00) 64(64) 4.12(4.12) 1979 (1986/87) 125(124) 15.99(15.86) 37(37) 4.41(4.41) 162(161) 10.01(9.95) 1980 (1987/88) 148(146) 18.17(17.93) 31(28) 3.56(3.21) 179(174) 10.61(10.44) 1981 (1988/89) 105(100) 12.35(11.76) 29(27) 3.20(2.98) 134(127) 7.62(7.51) 1982 (1989/90) 170(160) 19.07(17.95) 41(39) 4.34(4.13) 211(199) 11.50(11.39) 1983 (1990/91) 106(103) 11.36(11.06) 28(28) 2.84(2.84) 134(131) 6.98(6.98) 1984 (1991/92) 54(54) 5.55(5.55) 11(11) 1.07(1.07) 65(65) 3.24(3.34) 1985 (1992/93) 161(160) 15.85(15.74) 41(35) 3.80(3.25) 202(195) 9.65(9.36) 1986 (1993/94) 129(119) 12.60(11.63) 34(23) 3.12(2.11) 163(142) 7.71(7.19) 1987 (1994/95) 153(127) 14.55(12.08) 30(24) 2.68(2.14) 183(151) 8.43(8.15) 1988 (1995/96) 225(180) 20.59(16.47) 44(28) 3.78(2.41) 269(208) 11.93(11.65) Total 1754(1650) 11.48(11.48) 387(341) 2141(1991) Average 12.71 9.6(9.6) 2.45 7.76 *E.C. = Ethiopian or Julian Calendar, G.C. = Gregorian Calendar. Numbers in parentheses refer to suicide death & suicide death rates. M:F (crude suicide rate)=5.119:1 Kendall’s rank correlation coefficient (T) between suicide plus undetermined death rates and (suicide rates) is 0.886, P<0.001 for males and 0.905, P<0.001 for females Defference between M and F crude suicide rates is significant, P<0.002 (Wilcoxon’s rank sum test on paired data) the two sets of rates on the graph became wider and clearly apparent. But as a whole, the general trends in both sexes are obviously similar. Further more, Kendall’s rank correlation coefficient (T) between Suicide Death rates and Suicide plus ‘Undetermined Death’ rates of 15 years was found to be 0.886, P<0.001 for males and 0.905, P<0.001 for females, both showing strong positive correlation which are very highly significant. This shows that the trends in both sexes are maintained. Table 2 shows the number and percentage of methods of Suicide in Addis Ababa during the specified 15 year period. ‘Hanging and strangulation’ were the most common methods as 1502 (70.2%) victims of both sexes have used this method. The second common method was drowning which was used by 328 (15.3%). The third method of committing Suicide was by drinking poisonous liquids which was responsible for 161 (7.5%) deaths of both sexes. One hundred and fifty cases(7.%) were diagnosed as ‘Undetermined Deaths’ and their methods were not also specified in the record books. It was earlier mentioned why ‘Undetermined Deaths’ are included into Suicide statistics. Now, considering changes observed in the methods of Suicide at a five-year-intervals, it is clear as shown on Table 2, that ‘hanging and strangulation’, in both sexes, have manifested a gradual percentage reduction every five years. The drowning method of Suicide among females has not shown remarkable changes except for a small degree of successive reductions, but, among males, there was a remarkable increase, almost double, during the second five - year period just to come back almost to the previous level during the third five - year period. The percentage of drinking poison among females did not show remarkable changes during the three five-year periods, but, among males, there was a remarkable decrease from 10.58% to 2.75% during the second five- year period and then, during the third five-year period, the percentage was back almost to the previous level. The methods of committing Suicide in the ‘Undetermined Death’ were unspecified. Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 251 ──────────────────────────────────────────────────────────── Table 2: Number and percentage distribution of methods of suicides in Addis Ababa in both sexes at 5 years intervales from 1974 to 1988 E.C. (i.e 1981/82 - 1995/96 G.C.), Addis Ababa, 1998. ___________________________________________________________________________________________________________ ___________ Methods 1. Hanging/ Strangulation 2. Drowingin 3. Drinking Poison 4.Unspecified undetermined Total 1974-1978E.C (1981/82-1985/98 G.C.) Male Female No. % No. % 1979-1983 E.C. (1986/87-1990/91 G.C.) Male Female No. % No. % 1984-1988 E.C (1991/92-1995/96 G.C.) Male Female No. % No. % Total Male & Female No. 290 % 76.72 No. 49 % 88.33 No. 467 % 71.41 No. 127 % 75.51 No. 457 % 65.79 No. 94 % 58.75 No. 1502 % 70.15 47 40 2.43 0.85 8 4 3.11 6.56 148 18 22.63 2.75 20 12 12.05 7.23 89 76 12.33 10.53 16 11 10.00 6.88 328 161 15.32 7.52 1 0.26 0 10.00 21 3.21 7 4.22 82 11.36 39 24.38 150 7.01 78 100 61 100 65 100 166 100 722 100 160 100 2114 100 *Percentages are corrected to 100% In both sexes, such deaths have shown remarkable increases. In males, the percentage which was 0.26 in the first five-year period has reached 11.36 in the third five- year period. In females, the percentage has increased from 0.00 in the first five-year period to 24.38 in the third 5- year period. Table 3 shows the number of Parasuicide cases and the standardized male and female Parasuicide rates and crude Parasuicide rate (per 100,000) of combined sex in the general population for Addis Ababa for the specified 15 years. Throughout, the male rates were higher than the females and the Wilcoxon’s rank sum test on paired data has indicated that the differences between male and female standardized Parasuicide rates is very highly significant (P<0.002) in favor of the males. The average standardized Parasuicide rate was found to be 74.85 and 25.93 (per 100,000) for males and females, respectively. Thus, the male-to-female ratio of the standardized Parasuicide rate is 2.89:1.The average crude Parasuicide rate is 49.80 (per 100,000) for the specified 15 years duration. The ratio of the average crude Parasuicide rate to crude Suicide rate is 6.42:1. Figure 2 demonstrates the trends in standardized male and female Parasuicide rates in Addis Abeba in the general population during the specified 15 years. In 1981/’82 G.C., the standardize male Parasuicide rate was 99.61 and that of females was 64.83 (per 100,000). Then, there was a marked decline in the rates after two years that the male rate reached to 22.06 and that of females to 9.57. Thereafter, the rates showed only minor fluctuations until 1990/’91 G.C.. This was then followed by marked increases, more pronounced in the male than in the female Fugure 1: Suicide plus undetermined death rates and suicide death rates among males and females, 15 years and above, in Addis Ababa, from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), Addis Ababa, 1998. Table 3: Number of Parasuicide cases and standardized male and female parasuicide rates and crude parasuicide rates (per 252 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── 100,000) of the general population of Addis Ababa from 1974 to 1988 E.C.*1(i.e. 1981/82-1995/96 G.C.*1), Addis Ababa, 1998. ___________________________________________________________________________________________________________ ___________ Year Male Female Male & Female (S. Rate) No (S. Rate) No (C. Rate) No. 1974 E.C. (1981/82 G.C.) 642 99.61 450 64.83 1092 81.57 1975 E.C. (1982.83 G.C.) 764 114.65 109 15.16 873 63.07 1976 E.C. (1983/84 G.C.) 152 22.06 71 9.57 223 15.58 1977 E.C. (1984/85 G.C.) 86 11.94 24 3.11 110 7.38 1978 E.C. (1985/86 G.C.) 111 14.8 47 5.85 158 10.22 1979 E.C. (1986/87 G.C.) 159 20.34 93 11.11 252 15.57 1980 E.C. (1987/88 G.C.) 88 10.81 45 5.16 133 7.89 1981 E.C. (1988/89 G.C.) 129 15.17 64 7.06 193 10.98 1982 E.C. (1989/90 G.C.) 91 10.21 88 9.32 179 9.75 1983 E.C. (1990/91 G.C.) 148 15.9 55 5.58 203 10.58 1984 E.C. (1991/92 G.C.) 396 40.71 133 12.9 529 26.4 1985 E.C. (1992/93 G.C.) 516 50.77 100 9.28 616 29.42 1986 E.C. (1993/94 G.C.) 2015 196.89 618 56.73 2633 124.62 1987 E.C. (1994/95 G.C.) 2655 252.47 1057 88.68 3712 117.98 1988 E.C. (1995/96 G.C.) 2692 246.47 983 84.55 3675 162.99 Total Average 10644 3937 74.85 14581 25.93 49.8 ___________________________________________________________________________________________________________ ___________ E.C=Ethiopian or Julian Calendar G.C.= Gregorian Calendar S. Rate = Standardized Rate C.Rate = Crude Rates M:F of standardized Parasuicide rate = 2.89:1 Difference between male and female standardized Parasucide rates is significant, P<0.002 (Wilcoxon’s rank sum test on paired data). YEARS Figure 2: Standardized male and female parasuicide rates (per 100,000) of the general population of Addis Ababa from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), Addis Ababa, 1998. population, that it reached 252.47 (per 100,000) in males and 88.69 (per 100,000) in females in 1994/’95 G.G.. Then, in 1995/’96 G.C., there was a negligible decline in the rates both in males and females. In the age group of 15 years and above, the total number of Parasuicide cases seen during the specified 15 years in both sexes of this age group amounted to 14102. Out of these, 11833 (83.91%) were in the age group of 15-44 and Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 253 ──────────────────────────────────────────────────────────── Figure 3: Parasuicide rates (per 100,000) for Addis Ababa for the three specified age groups, 15 years and above, of both sexes from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), Addis Ababa, 1998. Table 4: Number of Accidental Poisoning (AP) cases and standardized male and female AP rates and crude AP rates (per 100,000) of the general population of Addis Ababa from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), 1998. Year 1974 E.C. (1981/82 G.C.) 1975 E.C. (1982.83 G.C.) 1976 E.C. (1983/84 G.C.) 1977 E.C. (1984/85 G.C.) 1978 E.C. (1985/86 G.C.) 1979 E.C. (1986/87 G.C.) 1980 E.C. (1987/88 G.C.) 1981 E.C. (1988/89 G.C.) 1982 E.C. (1989/90 G.C.) 1983 E.C. (1990/91 G.C.) 1984 E.C. (1991/92 G.C.) 1985 E.C. (1992/93 G.C.) 1986 E.C. (1993/94 G.C.) 1987 E.C. (1994/95 G.C.) 1988 E.C. (1995/96 G.C.) Male No. 59 93 69 56 53 99 129 208 201 136 113 92 152 197 202 (S. Rate) 9.15 13.95 10.02 7.78 7.07 12.67 15.84 25.63 22.56 15.08 11.62 9.05 14.85 18.73 18.49 Female No 33 67 35 45 14 71 65 146 162 105 69 60 71 101 111 (S. Rate) 5.05 9.33 4.72 5.84 1.74 8.49 7.46 15 17.15 10.64 6.69 5.57 6.52 9.02 9.56 Male & Female No 92 160 104 101 67 170 194 354 363 241 182 152 223 298 313 (C. Rate) 6.87 11.56 7.27 6.77 4.33 10.5 11.5 20.14 19.78 12.56 9.08 7.26 10.56 13.73 13.88 Total 1859 1155 3014 Average 14.17 8.19 11.05 E.C=Ethiopian or Julian Calendar G.C.= Gregorian Calendar S. Rate = Standardized Rate C.Rate = Crude Rates M:F = 1.73 (standardized AP rate) Difference between male and female standardized AP rate is significant, P<0.00 (Wilcoxon’s rank sum test on paired data). 75% of them (8863) were males. Those in the age group of 45-65 were 2123 (15.05% of the total) and 66% of them (1392) were male. In the age group of 65 and above, there were 146 (1.04%) cases of Parasuicide out of which 75% (110) were males. During the specified 15 years, the average annual Parasuicide rate (per 100,000) for the age group of 15-44 was 122.03 for males and 36.04 for females. For the age group of 45-64, it was 92.63 for males and 57.1 for females, and for the age group of 65 and above, it was 31.86 for males and 7.93 for female. Note that in each age group, the male group has higher average Parasuicide 254 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Figure 4: Monthly average of parasuicide cases for the Addis Ababa population, aged 15 and above, from 1974 to 1988 E.C. (i.e. 1981/82-1995/96), Addis Ababa, 1998. rate than its female counterpart and that males in the age group of 15-44 have the highest average Parasuicide rate (122.03 per 100,000). Figure 3 demonstrates the trends of Parasuicide rates (per 100,000) for the three specified age groups, 15 and above, of both sexes. Note that the graphs in figure 2 and 3 have similar patterns, i.e. they are both U-shaped. Examining the peaks on both sides of the trough in figure 3, it is clear that males in the age group of 15-44 and 45-64 and females in the age group of 45-64 have contributed more to the steep rise of the peaks than the rest of the groups. Figure 4 shows the trends of the monthly averages of Parasuicide cases for the age group of 15 and above for the specified 15 years. The monthly averages of both sexes reached their peak in the month of ‘Nehasie’ which has 35 or 36 days as mentioned earlier (see methods) and the lowest monthly average was recorded in the month of ‘Tikimt’ which has 30 days. When the daily average of ‘Nehasie’ (mean = 3.89, S.D=6.64) is compared with that of ‘Tikimt’ (mean = 1.6, S.D, - 2.48), the difference is not statistically significant (t=1.2514, P>0.1). Table 4 shows the numbers and the standardized male and female ‘Accidental Poisoning’ (AP) rates and crude AP rates (per 100,000) of both sexes in the general population for Addis Ababa for the specified 15 year period. Throughout, the male rates were higher than those of the females and the Wilcoxon’s rank sum test on paired data has indicated that the difference is very highly significant (p<0.002). Figure 5 demonstrates the trends of AP rates (per 100,000) in the general population which is similar for both sexes. Note that this graph does not have the same scale (Y-axis) as that of figure 2, which demonstrates trends of Parasuicide rates (per 100,000) in the general population. This graph has no peaks at the two ends and the peaks at the center also are comparatively exaggerated. Now, coming back to the age group of 15 and above, the number of AP cases reported in Addis Ababa during the specified 15 year period in all the three age groups of both sexes were 2075. Out of this, 1576 (75.95%) were in the age group of 15-44 and 60% of them were males. Those in the age group of 45-64 were 441 (21.25%) and again 60% them were males. In the age group of 65 and above, there were only 58 (2.8%) cases of AP and 66% of them were males. In the age group of 15-44, the average AP rate (per 100,000 ) for 15 years was found to be 15.34 for males and 8.74 for females and in the age group of 45-64, it was found to be 19.37 for males and 13.21 for females. In the age group of 65 and above, the average AP Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 255 ──────────────────────────────────────────────────────────── Figure 5: Standardised male and female accidental poisoning rate (per 100,000) of the general population for Addis Ababa from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), 1998. rate was found to be 10.26 and 4.20 for males and females, respectively. Note that in this age group, there were no reports of AP for nine years in males and for 11 years in females. Figure 6 demonstrates the trends of AP rates (per 100,000) for the three specified age bands 15 years and above, of both sexes. Note again that the general trends in this graph, except for those aged 65 and above, is similar to that of figure 5 which demonstrates the trends of standardized AP rates in the general population both for males and females. In figure 6 it is evident that all age groups of both sexes, except females aged 65 and above, have their peak rates between 1985/’86 and 1991/’92 G.C.. The pronounced increase in rates in 1995/’96 G.C. for the age group of 65 and above of both sexes needs explanation. Figure 7 demonstrates the trends of the monthly average of AP cases for the specified 15 years for the age groups of 15 and above. Note that this graph is not drawn with the same scale as that of figure 4 which demonstrates the monthly average of parasuicide cases. Note also that it does not have a predominant peak as in figure 4. However, when both sexes are combined, the highest daily average of AP (meam=0.491, S.D=0.318) was recorded for the month of ‘Yekatit’ and the lowest (mean=0.298, S.D=0.293) for the month of ‘Ginbot’. The difference between these two means is not statistically significant (t=0.6993, P>0.1). Figure 6: Accidental poisoning rates (per 100,000) for Addis Ababa for the specified age groups, 15 years and above, of both sexes from 1974 to 1988 E.C. (i.e. 1981/82-1995/96 G.C.), 1998. 256 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Figure 7: Morthly average of accidental poisoning cases for Addis Ababa population, aged 15 and above, from 1974 to 1988 E.C. (i.e. 1981/82-1995/96), 1998. Discussion Thorough investigation into the causes of violent or unexpected deaths (including autopsy), constant case definition of Suicide, and consistent ascertaining techniques render reliability to any Suicide data (13). Such procedures are being followed at Minilik II Hospital. It is inevitable, in our circumstances, that certain informations about the victims, especially the demographic variables, remain incomplete. This will certainly limit the type and the number of epidemiological and sociodemographic analyses that could be performed from the data obtained from the records of Minilik II Hospital. In Addis Ababa, as mentioned earlier, all doubtful Suicides are classified as ‘Undetermined’ whether accidentally or purposefully inflicted in accordance with the revised 8 th edition of the International Classification of Diseath. Logically, such procedures tend to underestimate further the Suicide rates (9,14,15). Hospital-based Parasuicide rates also under-estimate the true rates because many Parasuicide cases do not come to the hospital unless they are critically ill. Among those who come to the hospital, some probably present themselves as cases of ‘Accidental Poisoning’ because of the stigma and possible legal problems. This, on the other hand, led to an exaggerated rates of ‘Accidental Poisoning’ (1,4,16). With this background in mind, the important aspects of this study are discussed below. The finding that male Suicide rates were significantly higher (P<0.002) than female Suicide rates is consistent with the reported rates throughout the world. China is the only exception where women have a higher incidence of Suicide than men from youth through middle age. For example, the male-to-female ratio was 0.8:1 in China in 1989 (8). For Addis Abeba, the male-to-female ratio of the average crude Suicide rate was found to be 5.19:1 which means that men had had higher risk (over five times) of Suicide than women. For most countries the male-to-female ratio is well above 3(4). The crude Suicide rate (both sexes combined) for Addis Ababa ranged from 3.24 to 11.65 (per 100,000), the average being 7.76. Rate between 5 and 15 in considered as a midium rate and below 5 as a low rate (4). Literature on Suicides is very rare in Ethiopia. Jacobson (17), in a retrospective analysis of medical records from Nekemtie General hospital, found Suicide rates ranging from three to 11 (per 100,000) with an average of 4.5 for a duration ranging from 1966-1972, which could be described as a peaceful period. It has to be remembered that the above- mentioned rates for Addis Ababa cover 15 years duration from the early 80’s to the mid-90’s which was marked by unrest and war. The author has no any intention of comparing the Suicide rates of these two Ethiopian cities which are different in many aspects. Addis Ababa is a large capital city with a multi-ethnic population, whereas Nekemtie is a small provincial city with less social isolation and with predominantly Oromo population. More over, the two Suicide figures cover different periods. Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 257 ──────────────────────────────────────────────────────────── It is believed that the majority of the cases allocated in the ‘Undetermined’ category are probably equivocal Suicides; and the sum of the Suicide rates and the ‘Undetermined Death’ rates may be a closer approximation to the true incidence of Suicide than Suicide rate alone (7). But when we come to interpreting the trends of Suicide rates of Addis Ababa any one of the two sets of rates could be correctly used. The reason is that Kendall’s rank correlations between the Suicide Death rates and Suicide plus ‘Undetermined Death’ rates of both sexes are strongly positive and very highly significant showing that even when doubtful Suicides are included the order or the pattern is maintained. This study has shown that the most common method of committing Sucide in both sexes is ‘hanging and strangulation’ (70.2%) followed by drowning (15.3%) and poisoning (7.5%). In (7.%) of cases, the method is not specified. The fact that ‘hanging and strangulation’ is the most common means of committing Suicide in Ethiopia was also confirmed by other studies (17,18). The reported Suicide by poisoning does not give any clue about the nature of the poison (i.e. drugs, pesticides etc.) and therefore this information does not help to point to the preventive action. It is known that cultural values and social policies determine the preference for methods of Suicide (8). Suicide by firearms and explosives, cutting and piercing instruments, jumping from high places and by domestic gas, though not unheard of in Addis Ababa, were not reported in this study. The author believes that such causes are probably treated as accidents and this has to be confirmed by further investigations. Commenting on changes in methods of Suicide, care has to be taken in interpreting the apparent changes: the apparent reduction in percentage of ‘hanging and strangulation’ method is associated with successive increases in the percentage of ‘unspecified/ undetermined’ method during the three successive five - year periods. But if one considers the first three methods only, the changes in the percentage of ‘hanging and strangulation’ method become less remarkable in both males and females. The author believes that the increase in the percentage of ‘unspecified/ undetermined’ method could be due to a fall in the quality of police reports since 1991, which help, to some extent, the Forensic Physician to come to a correct decision about methods of committing Suicide. In 1991, following the overthrow of the ‘Derge’ regime, the entire police force of Addis Ababa was replaced by less experienced police force. This explanation is of course simply speculative which needs further investigation. A sudden increase in the percentage of ‘drowning’ method and a reduction in the percentage of ‘poison drinking’ method in males during the second five-year period (i.e. 1986/’871990/`91 G.C.) could partly suggest the theoretical possibilty of a substitution of one method, which is less available, by another more available method during that period. This sort of possible substitution is not apparent in females who generally prefer less violent methods of Suicide. Reasons for committing Suicide are not mentioned in the record books of Minilik II Hospital, so that there is no clue about the most frequent reason for committing Suicide in Addis Ababa. In general, risk factors are classified into societal or psychological. Other factors include physical illness, alcoholism, financial problems, interpersonal disputes, social and political protests, and general sense of meaningless in life. These factors are not mutually exclusive. Easy access to the killing agent and publicity about suicidal acts are reported to be strongly and directly related to the frequency of suicidal acts (4,8). According to E. Durkheim, each society has a collective inclination to Suicide expressed in the Suicide rate which tended to remain constant as long as the character of the society did not change (1). Fluctuations of the Suicide rates, the directions of which depend on the settings, were often manifestly associated with changes in the state of society, such as war, political upheavals, and economic crisis (1,8). From the mid-70’s to the early 90’s, Ethiopia was in a state of war and, in general, Suicide rates of this era represent war-time rates. Further more, there were specific turning points in this era which were marked by mass mobilization of the army and aggravation of catastrophic wars. Such aggravations appear to have coincided with further declines in the Suicide rates in Addis Ababa. In Addis Ababa, there was a dramatic decline of Suicide rates in both sexes in 1985/’86 (i.e. 1978 E.C.) 258 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── following the great drought and war especially in the North of the country and in 1991/’92 (i.e. 1984 E.C.) following the overthrow of the ‘Derge’ regime. There was also another minor decline in 1988/’89 (i.e. 1981 E.C.) coinciding with the total evacuation of military from the entire Tigray province and an aborted coup d’ e`tat in Addis Ababa. In general, the pattern of trends in male and female Suicide rates are similar except that in male the rates 0fluctuated within a wide range while in female rates fluctuated within a narrow range. The decline of the Suicide rates in war time had never been explained satisfactorily, but at least three possible conditions were mentioned. These are (1): 1/- less social isolation, which means that the more strongly the individual was integrated with social groups, the smaller was the likelyhood of Suicide, 2/- directions of aggressive feelings form the threatened self against the external enemy, and 3/- decline of the value of individual life. In Addis Ababa there could be another explanation also: it appears that mass mobilization of the youth to the war front and to the resettlement areas of drought victims might have helped to reduce the vulnerable groups in the city, thus leading further to reduced Suicide rates. Now, focusing on Parasuicide in Addis Ababa, the average crude rate (per 100,000) which is 49.80 is much higher than that of Ibadan (1986) and Benin City (1978 to 1981), Nigeria, which is 2.60 and 7.00 (per 100,000), respectively (19,20). No other hospital-based rate of Parasuicide is available for Addis Ababa, but there are two community studies worth mentioning here, one in Addis Ababa and the other in ‘Butajira’. In a community survey in 1989/’90 academic calendar among Addis Ababa high school students aged 1118, Kebede and Ketsela (21) found a life-time prevalence of Parasuicide of 14.3%. In a crosssectional survey in 1997 in a rural and semi-urban community of ‘Butajira’, South Ethiopia, Alem (18) reported a life-time Parasuicide of 3.2% which is most frequent between the age of 15 and 24. Male-to-female ratio of Parasuicide for Addis Ababa which was earlier mentioned as 2.89:1 is also higher than that of Ibadan and Benin city which is 1.4:1 and 1.2:1, respectively (19,20). This shows clear preponderance of males in these three African cities which is in contrast to the findings in developed countries (4). As far as Addis Ababa is concerned, it was earlier mentioned that male standardized Parasuicide rates are significantly higher (P<0.002) than those of female rates. The ratio of the average crude Parasuicide rate to Suicide rate was mentioned earlier as 6.42:1. This is within the range reported in urban community of the U.K. and the U.S.A in 1960’s (1), but recent studies have indicated ratios as high as 20:1 (22). One possible explanation to this change could be that in these countries under-reporting of Parasuicide is decreasing as the associated stigma also is becoming less severe (22). Age-and sex-specific average Parasuicide rates have indicated that males in all the three age groups have much higher rates than their female counter-parts. The finding that most (83.91%) of those who committed Parasuicide are in the age group of 15-44 is consistent to some extent with other studies in Ethiopia (18,23). It was mentioned earlier that the peak age for Parasuicide in the West has usually been found to lie between 24 and 44 years (1). While examining the general pattern of trends of Parasuicide shown on figure 2, it is important also to identify which age and sex groups were responsible for the observed upward trends on both sides of the trough. As shown in figure 3 it is clear that males in the age band 15-44 and 45-64 and females in the age band 45-64 are mainly responsible for the observed upward trends. The author has no adequate explanations for the unusually high rates observed in the three age groups prior to 1976 E.C. (1983/’84) and after 1983 E.C. (1990/’91), but much of the risk-factors could be speculated as acute stresses or sudden critical changes of different forms related to political, social and economic changes. The Parasuicide acts could also have appealing effect or function against such changes. Between 1976 E.C. (1983/’84) and 1983 E.C. (1990/’91), the duration was marked by an aggravation of war in the northern provinces, national military services, formation of a repressive communist regime, attempt of a coup d’e`tat, extension of the war to central provinces and the final Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 259 ──────────────────────────────────────────────────────────── takeover of Addis Ababa by the Ethiopian Peoples Democratic Revolutionary Forces. It appears that the population had adapted well to a gradual accumulation of miseries and thus have manifested less parasuicidal acts. Examining the seasonal variations of the incidence of Parasuicide in Addis Ababa, the peak daily average which was recorded in “Nehasie” (Aug. 7-Sept. 10), has to be explained. The author is not aware of any study in Addis Ababa or in Ethiopia in general that establishes correlations among the incidences of Parasuicide, Suicide and other conditions. He believes that any sociological, seasonal, and weather factors peculiar to the two months, ‘Hamlie’ and ‘Nehasie’, should be carefully investigated for possible associations. Such factors could include:1. Heavy rain and cold 2. Possible lack of employment 3. School vacation and increased courting behavior of the youth and all of its related complications. 4. Failure in class and national examinations. 5. The effect of the Ethiopian new year at the end of ‘Nehasie’. Earlier, it was stated that Parasuicide is under-reported because some are possibly reported as ‘Accidental Poisoning’ (AP). But a close examination of the data on AP indicates that they do not resemble that of Parasuicide: the general trend, age-and sex-specific trend, the peak age, M:F, and the seasonal patterns of the two phenomena (i.e. Parasuicide & AP) are quite different. Therefore, it is unlikely that the data on AP provide some corroboration to believe that appreciable number of Parasuicide have been reported as AP. As shown on figure 5, the yearly AP rates for both sexes did not fluctuate to form peaks and troughs as in Parasuicide. Thus, it appears that the factors that have possibly affected the Parasuicide rates prior to 1976 E.C. (1983/’84) and after 1983 E.C (1990/’91) have not affected the AP rates. Examining figure 6, which shows AP rates for the three specific age groups of both sexes, indicates that between 1977 E.C. (1984/’85) and 1984 E.C. (1991/’92) some age groups have shown small isolated peaks which are difficult to explain. Though 75.95% of cases of AP are in the age group of 15-44, this group does not have the highest average rates. Among both males (19.37) and females (13.21) the average AP rate is the highest in the age group of 45-64. In adults AP is usually jobrelated, such as exposure to pesticide spray or to factory chemicals. Probably more males than females are employed in such jobs in Addis Ababa. In a four - year study at Tikur Anbessa Hospital in Addis Ababa, it was found that organophosphate poisoning accounts for 50% of all poisonings (24). In another study of 50 organophosphate poisoning cases in the same hospital, only three cases were due to accident while 47 had suicidal intentions (24). The trends of the monthly averages of AP for the specified 15 years do not show peaks similar to that of Parasuicide. In conclusion, this study has shown that male crude Suicide rates, standardized Parasuicide rates, and AP rates are significantly higher than those of females. Age distribution of Suicides and monthly distribution was found to be unreliable from the hospital records. These records have to be improved in the future. Remarkable fall in Suicide Death rates was observed during the exacerbation of the civil wars and, in fact, all the Suicide rates reported during the specified 15 years are war time rates. The most common means of Suicide was found to be ‘hanging or strangulation’, but the immediate reasons for Suicides are not known as they were not recorded. The study has also shown that males in the age group of 15-44 have the highest Parasuicide rate and that 83.91% of all Parasuicide cases over the age of 15 are in this age group. During stressful years, trends of Parasuicide rates have shown dramatic rises, specially in males of the age group of 15-44 and 45-64 and females of the age group of 45-64. The highest mean daily number of Parasuicide (3.89) was recorded for ‘Nehasie’ (Aug. 7-Sept. 10), but this is not significantly higher than those of other months. The ratio of the average crude Parasuicide rate to crude Suicide rate is 6.42:1. Finally, this study has shown that males in the age group of 45-64 have the highest AP rate, but 260 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── 75.95% of all AP cases over the age of 15 were in the age group of 15-45. Trends of AP rates have not shown dramatic rises during stressful years. The mean daily number of AP was the highest (0.49) for ‘Yekatit’ (Feb. 8-Mar. 9), but this is not significantly higher than those of other months and does not form a prominent peak on the graph as in Parasuicide. Because of gross under-reporting of Suicidal behaviors worldwide, the author believes that the figures reported in this paper may represent only a fraction of the prevailing problem. Prevention of Suicide is an important public health responsibility and success depends largely on early identification and adequate treatment of the high-risk population. It was earlier mentioned that suicidal act is committed frequently as a “cry for help” rather than with a clear desire to die. It appears that, regardless of local conditions, where this cry for help is answered, and the help is continued with the aim of solving the outstanding problems leading to the act, much suffering may be prevented (5). General instructions on how to prevent household and industrial poisoning should be available to the public and patterns of drug prescription and drug packaging should follow safety procedures. The need for Suicide prevention services, governmental or non-governmental, and a continuous research program for Addis Abeba is quite obvious. Acknowledgments I gratefully acknowledge the Ethiopian Science and Technology Commission for its financial assistance. I am also thankful to Dr. Kasahun Abate for his critical review of the statistical analyses and to Ato Mulugeta Wondimu, the Psychiatric Nurse, as well as to Ato Mulugeta Addeme for their help in data collection. I am also grateful to W/O. Almaz Lemma for her secretarial help. References 1. Stengle E. Suicide and Attempted Suicide. Rev. ed. Middlesex, England: Penguin Book, 1977. 2. Kreitman N. Suicide and Parasuicide. In: Kendell RE, Zeally AK, editors. Companion to Psychiatric Studies. 5th ed. Edinburgh: Churchill and Livingstone, 1983:396-411. 3. Bennetts MP. Depression and Suicide: recognition and early positive intervention. In: Matzen RN, Lang RS, editors. Clinical Preventive Medicine. St. Louis, Missouri: Mosby, 1993:163-183. 4. Diekstra RFW, Gulbinat W. The Epidemiology of Suicidal Behavior: a review of three continents. World Heath Statistics Quarterly. Geneva, 1993;46(1):52-68. 5. World Health Organization. Prevention of Suicide: Public Health Papers No.35. Geneva, Switzerland: WHO, 1968. 6. World Health Organization. Manual of International Statistical Classification of Diseases, Injuries, and Causes of Death, Vol. 1. Geneva, Switzerland: WHO, 1968. 7. Barraclough B. Differences Between National Suicide Rates. Brit J Psychiat 1973;122:95-6. 8. Desjarlais R, Eisenberg L, good B, Klienman A. World Mental Health: Problems and priorities in low-income Countries. New York: Oxford University Press, 1995. 9. Sainbury P. Validity and Reliability of Trends in Suicide Statistics. Wld Hlth Statist. Quart 1983;36:339-348. 10. Office of the Population and Housing Census Commission. The 1984 Population and Housing Census of Ethiopia: Analytical Report on Results For Addis Abeba. Addis Abeba, Ethiopia: 1987. 11. Office of The Population and Housing Census Commission, Central Statistical Authority. The 1994 population and Housing Census of Ethiopia: Results for Addis Abeba. Addis Abeba, Ethiopia: 1995. 12. The Faculty of Law, Haile Sellasie I University. Consolidated laws of Ethiopia. Addis Abeba: Artistic Printers Ldt, 1972;1:341-345. 13. World Health Organization. Suicide Statistics: the problem of comparability. WHO Chronicle 1975;29:188-193. Trends in suicide, parasuicide & accidental poisoning in Addis Ababa 261 ──────────────────────────────────────────────────────────── 14. Clarke-Finnegan M, Fahy TJ. Suicide rates in Ireland. Phychol Med 1983;13:385-391. 15. Ruzicka LT, Choi CY. Demographic and social profile of suicide mortality in Australia. Genus 1996;11(3-4):135-154. 16. Manian T. Suicide and Parasuicide in a Hill Resort of Malaysia. Brit J Psychiat. 1988;153:222225. 17. Jacobson L. Suicide and attempted suicide in a general hospital in Western Ethiopia. Acta Psychiat Scand 1985;71:596-600. 18. Alem A. Suicide attempts among adults in Butajira, Ethiopia. In: Mental health in rural Ethiopia (dissertations). Umea: Umea University, 1997. 19. Efrakeya AE. Drugs and suicide attempts in Benin-City, Negeria, Brit J Psychiat 1984;145:70-73. 20. Odejide AO, Williams AO, Ohoeri JU, Ikweson BA. The epidemiology of deliberate self harm: the Ibadan experience, Brit J Psychiat 1986;149:734-737. 21. Kebede D, Ketsela T. Suicide attempts in Ethiopia in Addis Abeba high school adolescents. Ethiop Med J 1993;31:83-99. 22. Tomb DA. Psychiatry. 5th ed. Baltimore: Williams & Wilkins, 1995. 23. Abebe M, Organophosphate pesticide poisoning in 50 Ethiopian patients. Ethiop Med J 1991;29:109-118. 24. Yemanebirhan B, Yacob F. Analysis of admissions to the Medial Intensive Care Unit of a teaching hospital in Addis Abeba. Ethiop Med J 1988;26:61-67. Original article Trends in suicide, parasuicide and accidental poisoning in Children in Addis Ababa, Ethiopia Abdulreshid Abdullahi Bekry Abstract: Due to lack of compiled data on suicide, parasuicide and accidental poisoning (AP) in under-fifteens in Addis Ababa, Ethiopia, it was essential to prepare and analyze these basic data. By using estimated mid-year population for 0-4 and 5-14 years age groups and fiscal year morbidity and mortality data reports, age and sex-specific suicide, parasuicide, and AP rates (per 100,000) are, calculated for 1981/82-1995/96. No suicide deaths or ‘undetermined’ deaths were reported in underfifteens, but 12 deaths were recorded in the two pediatrics hospitals of Addis Ababa following admissions for AP. Out of 479 reported parasuicide cases, 402(83.9%) were in the age group of 5-14 years and the average parasuicide rate for the same age group was 6.74 and 5.32 for boys and girls, respectively. The trends of the reported parasuicide rates showed small peaks initially in 1981/82 in both age groups, but after 1990/91 only the age group of 5-14 showed peaks. Out of 939 cases of AP,533 (56.8%) were in the age group of 0-4 years and the rest in the age group of 5-14. Males in the age group of 0-4 have the highest AP rate (19.91%) followed by females (12.60%) of the same age group. Possible reasons for changes in trends and preventive measure are discussed. [Ethiop. J. Health Dev. 1999;13(3):263-269] Introduction Despite generations of social concern, research and legislative actions pertaining to the health and welfare of children and adolescents, their major health and mental health needs are not yet being met world-wide. In the U.S.A, 27% of the population are under the age of 18 years, and an estimated 10% of this group are in need of mental health care (1). In Addis Ababa, currently, 31.70% (i.e.771,165) of the population are under the age of 15 years (2) and so far no such estimation of those who are in need of mental health care is available. A child is not a small adult, and the needs of children differ form those of adults. Physiologic, psychological, and cognitive growth is accompanied by new vulnerabilities to biologic, psychological, and social stresses (1). In addition to these stresses, child abuses, school problems, physical and mental illnesses, and various psychodynamic and family factors keep children under constant stress. Children and adolescents who are unable to cope with these stressful moments and periods of development may not seek or even know that help is available or needed. Thus, it is important for professionals and other adults to identify signs of emotional problems in children as early as possible and refer them for treatment; otherwise the consequences will be quite grave. Depressed hospitalized children often express suicidal thoughts either consciously (verbally) or unconsciously (on projective testing). Suicidal behavior in children under 12 is extremely rare, but after 12 it is more common and in fact suicide is one of the major causes of death in adolescents (i.e. 12-20 year olds). Suicidal gestures (superficial attempts) are made more frequently by girls than by boys, whereas true suicide attempts are made more frequently by boys(3). Although the majority of suicidal adolescents are depressed, only about 25% of them meet the DSMIII diagnostic criteria for Depressive Illness while the rest have masked depression. Behavioral ______________________________________ From the Department of Psychiatry, Faculty of Medicine, Addis Ababa University, P.O. Box 0986, Addis Ababa, Ethiopia Trend in suicide, parasuicide and accidental poisoning in Children 263 ──────────────────────────────────────────────────────────── changes also precede suicidal attempts and self-poisonings in adolescents and these too do not manifest characteristic depressive symptoms (3,4). Some authors believe that there is under-reporting of childhood suicide and it was asserted that death by suicide in childhood is often reported as accidental to avoid the stigma attached to suicide. However, Shaffer believed that this under-reporting may be true in North America, but he cited good evidences that this is not the case in England and Wales (5). In his study in England and Wales in 1974, Shaffer found an annual suicide of 1 child out of every 800,000 (i.e. 0.125 per 100,000) in the 10 to 14 year age range(5). McClure, reviewing the same phenomenon, has reported that the total number of children committing suicide in this age group (i.e.10 to 14) is little changed between 1941 to 1980(6) and between 1960 and 1990(7). However, he has indicated that the rate for males has declined and that of females has increased between 1941 and 1980(6). In 1978, in the U.S.A., Shaffer found an annual suicide of one child in 123,000 (i.e.0.8 per 100,0000), again in the age range of 10 to 14. Boys to girls ratio was more than 3:1(5). The rate (per million) of ‘undetermined’ death for 10 to 14 year old males increased from 0.6 in 1970 to 9.1 in 1990. For females aged 10 to 14 years, the increase was only from 0.6 in 1970 to 3.4 in 1990. The rate (per million) of ‘accidental’ death for 10 to 14 year-old males decreased from 36 in 1970 to 9.1 in 1990, but for females the rate remained unchanged (i.e.,4.1 per million). The summation of ‘undetermined’ and ‘accidental’ death rates shows a decrease for males and a small increase for females between 1970 and 1990. These two categories of death may contain misclassified suicides which can distort the recorded suicide statistics (i.e., obscure or accentuate actual changes) (7). In England and Wales, statistics obtained from the Office of Population Census and Surveys and Registrar General’s Statistical Review did not show any recorded suicides in children under 10 years between 1950 and 1980(6)and also between 1960 and 1990(7). The incidence of parasuicide is by far higher than that of completed suicide. But it is also much more difficult to estimate it accurately. What is clear is that the sex ratio is reversed (5). Shaffer has indicated that 7-10% of referrals to child psychiatric services were due to threatened or attempted suicide and some studies gave the incidence of 10-33% in children aged 6-12 years (8). Black et al (1982) stated that 6-8% of parasuicide occurs in the under-12 age group with the rate of admission rising sharply from the age of 12, with peaks at 16 years for females and 18 for males (8). In a 10 to 20 year follow–up, Otto (1972) found that 10% of male and 2.9% of female parasuicides have eventually committed suicide. According to Hawton, short- term prognosis for most parasuicides is relatively good, but 10-14% make a further attempt within a year (8). ‘Accidental poisoning’ (AP) among urban children under-five was studied thoroughly for five years (1977-1981) in Brisbane (Australia) by Pearn et al. They found that the current age correlated rate of AP was 392 per 100,000 per year and they came across only one fatality during the five year period. This was described as a dramatic reduction in rate compared to the previous 15 years (i.e. 1962-1976) when 13 children died form AP and two were murdered with drug. The reason for this dramatic reduction was found to be due to changes in patterns of drug prescription, safe package of drugs, and coloring blue of certain substances like kerosene, etc. (9). In Ethiopia, recently, there was a growing awareness and concern about physical illness in children, but no similar awareness and concern about their emotional problems and about the family and psychodynamic factors associated with these problems. Parasuicide and ‘accidental poisoning’ are reported monthly by the two pediatrics hospitals and general hospitals (government civilian) in Addis Ababa, but none have clearer guidelines for assessment, appropriate management, and possible modes of prevention. Clearly, there are many areas of future research in these three related phenomena, but first, the magnitudes of these problems have to be known. 264 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── In paper I (10) the author has tried to show the trends of suicide, parasuicide and AP in the general population in Addis Ababa during, 1981/82-1995/96 with special emphasis on those aged 15 years and above. The main objectives of this paper are to find out the magnitudes (rates) of suicide, parasuicide and AP in Addis Ababa from 1981/82 to 1995/96 in both sexes aged below 15 years. The trends and seasonal variations of the magnitudes of these phenomena will be commented upon. Methods For the collection of data on demography, suicide, parasuicide, and AP and for the statistical analyses refer back to the methods of paper (10). Results In part I (10), it was already mentioned that, at Minilik II Hospital, the data collector on suicide did not come across any victim who is below the age of 15 years. As shown in Table 1, death due to AP among children below the age of 15 years, was recorded both in the Ethio-Swedish and in the Yekatit 12 pediatrics Hospitals, but not in other hospitals. Out of 939 victims registered as cases of ‘accidental poisoning’, only 12 (1.28%) died in the two pediatrics hospitals during the 15 years period. The kind of poison ingested by the victims is not mentioned on any of the monthly inpatient morbidity and mortality reports. Also, the author did not come across any death registered as ‘undetermined’ whether accidentally or deliberately inflicted. The reported number of parasuicide cases and age and sex specific parasuicide rates for the under15 year olds for the specified 15 years are as follows. The total number of parasuicide cases reported in the two age groups is 479. Out of these, only 122(25.5%) were seen in the two pediatrics hospitals. The remaining 357(74.5%) were seen in general Table1: Age distribution of deaths due to ‘accidental poisoning’ in two pediatrics and other hospitals in Addis Ababa during 1981/82-1995/96, Ethiopia . Hospitals Age Yekatit 12 Under 1Yr 0 1-4yrs 1 5-14yrs 7 Total 8 Ethio-swedish All other hospitals Total 0 0 0 1 0 2 3 0 10 4 0 12 *Sex of the victims is not recorded in the monthly inpatient mortality reports. hospitals (government civilian) and are in the age group of, 0-4 nearly 75% of whom are males. Those in the age group of 5-14 are 402(83.9%) of whom 55.5% are males. In the age group of 0-4, the reported yearly parasuicide rates (per 100,000) ranged from 0.00 to 29.36 for boys, the average being 3.75 and from 0.00 to 12.25 for girls, the average being 1.49. Zero annual rate was the dominant rate in both sexes during the Trend in suicide, parasuicide and accidental poisoning in Children 265 ──────────────────────────────────────────────────────────── Figure 1: Reported parasuicide rates (per 100,000) of specified age sgroups, under-15, of both sexes, in Addis Ababa, 1981/’82-1995'96 G.C., Addis Ababa, 1998. Figure 2: Monthly average of reported parasuicide cases for the Addis Ababa population, under 15 years, from 1974 to 1988 E.C. (i.e. 1981/82-1995/’96 G.C.), Addis Ababa, 1998. 266 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── specified 15 years. In the age group of 5-14, the reported yearly parasuicide rate (per100,000) ranged from 0.47 to 30.18 for boys, the average being 6.74, and from 0.00 to 35.02 for girls, the average being 5.39. Figure 1 demonstrates the trends of the reported parasuicide rates (per 100.000) for the two specified age groups below 15 years. Note that all age groups of both sexes had their peaks in 1981/82, followed by sudden drops in rates the next year and in the subsequent years. This was then followed by the appearance of small peaks after 1990/91 in the age group of 5-14 of both sexes. But in the age group of 0-4 the rate of the reported parasuicide remained very low. Figure 2 demonstrates the trends of monthly average of the reported parasuicide cases, during the specified 15 years, in under-15 Year olds. Males and females combined had their highest monthly (11.7) and daily (0.33) averages during Aug. 7-Sept. 10 which has 35 or 36 days as mentioned in paper I (see methods). The lowest monthly (0.9) and daily (0.03) averages were recorded Oct. 11-Nov. 10 and Nov. 11-Dec. 9. The difference between the highest and lowest monthly averages is not statistically significant (t=0.9615,p>0.1). The number of AP and age and sex-specific AP rates for Addis Ababa for under 15 year olds during the specified 15 years are as follows. The total number for both age and sex groups amounted to 939 cases. Out of this, 929(98.9%) were seen in the two paediatrics hospitals, Yekatit 12 and EthioSwedish. The remaining 10(1.1%) were seen in the general hospitals mentioned earlier (see ’Method’ section of part 1). Out of 939, 533(56.8%) were in the age group of 0-4 and about 60% of them were boys. Those in the age group of 5-14 were to 406(43.2%) and 67% of them were boys. In the age group of 0-4, the yearly AP rate (per 100,000) ranged from 4.83 to 45.42 for boys and from 1.00 to 25.21 for girls, the average rate being 19.91 and 12.60 for boys and girls, respectively. In the age group of 5-14, the yearly AP rate (per 100,000) ranged from 1.84 to 16.94 for boys and from 0.47 to 9.38 for girls, the average rate being 8.05 and 3.96 for boys and girls, respectively. Figure 3 demonstrates the trends of AP rates (per 100,000) for both sexes of the two specified age groups under 15. Note that the age group of 0-4 show higher rates than the age group of 5-14 throughout the 15 years except in 1985/86, when boys aged 0-4 show a lower rate. The peaks in the age group of 0-4, especially in boys, are more prominent after 1990/91, but after 1994/95 G.C. all age and sex groups started to show down ward trends in rates. Figure 3: Accidental poisoning rates (per 100.000) of under- 15, of both sexes, in Addis Ababa, 1981/’82-1995/’96, G.C, Addis Ababa1998. Figure 4 demonstrates the trends of the monthly averages of AP during the specified 15 years among those aged under 15 years. It reaches the highest peak (6.7) in ‘Tikimt’ (Oct. 11-Nov.10) which is significantly higher (t=2.4490,p<0.050) than that of ‘Senie’ (June 8-July 7) (3.1). It was also singificantly higher (t=2.2094,P<0.05)than that of ‘Meskerem’ (Sept.11-Oct.10) (3.5). Trend in suicide, parasuicide and accidental poisoning in Children 267 ──────────────────────────────────────────────────────────── Discussion There were no recorded suicides in children under 15 at Minilik II Hospital in Addis Ababa during the specified 15 years period. The reported ‘accidental’ deaths in the two pediatrics hospiatls, though small in number, have to be examined carefully as it may contain misclassified suicides, especially in those aged 10-14 years. Suicide in the age group of 10-14 is known to occur in western countries like England and Wales, but there have been no recorded suicides in children under 10 years between 1950 and 1990 (6, 7, 11). Out of the 10 cases of death due to ‘accidental poisoning’ in the age group of 5-14, it was not possible to identify from the records the number of cases in the age group of 10-14 (see Table 1). The type of poisons involved were not also found in the records. Further study is required to identify the poisons involved in order to design specific preventive measures. Coming back to the reported parasuicides in children, the author is of the opinion that the figures are misclassified. It was mentioned earlier that in the age group of 0-4 years, 77 cases of parasuicide were reported during the specified 15 years and that the average annual rate(per 100,000) was found to be 3.75 and 1.49 for boys and girls, respectively. These figures are not acceptable as children of this age lack conceptual maturity to apply suicidal or parasuicidal acts to solve their psychodynamic or family problems. Mistakes in classification may arise when there are difficulties in distinguishing ‘accidental poisoning’, ‘suicidal behaviors’, and ‘ a form of child abuse’. Sometimes mistakes may be comitted when the responsible pediatrician fails to fill in the diagnostic number and this duty is left to other health workers. The reported 402 cases of parasuicide in the age group of 5-14 years and rates (per 100,000) of 6.74 (for boys) and 5.39(for girls) also have to be taken cautiously. To the younger cases, especially to those under 10 years of age, the same analogy applies. But to those between 10 and 14 years, though their exact number is not known in this study, the term parasuicide could be applied as in other countries. However, there is a need to confirm this by other studies. In figure 1 it is clear that the peaks at the two ends are comparatively too small to deserve similar comments. However, it is apparent that the age group of 5-14 years is mostly responsible for these peaks. The reason for not accepting the diagnosis of Figure 4: Monthly average of accidental poisoning cases of the Addis Ababa population, under 15, 1981/’82-1995/’96, Addis Ababa, 1998. parasuicide in children under 10 was already mentioned. Examining the monthly variation of the average number of parasuicides in under-15 year olds (Figure 2), the trends are similar to that of over-15 year olds. Figure 4 shows monthly trends of the same phenomena in over 15 year olds. Both age groups have their highest monthly and daily average numbers of parasuicides in ‘Nehasie’ (Aug.7-Sept.10). Out of 479 reported cases of parasuicides during the specified 15 years in under-15 year olds, 175(36.5%) were seen in the month of ‘Nehasie’. In over-15 year olds, out of 14102 cases of parasuicides reported during 15 years, 2058 (14.6%) were seen in the month of ‘Nehasie’ (10). These findings emphasize the need for a careful investigation of possible association of parasuicide with factors peculiar to the month of ‘Nehasie’. Such factors were already discussed (10). Now, comparing figures of AP’s with those of parasuicides among children under 15. More cases of 268 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── AP(939) were reported than parasuicides (479) during the specified 15 years. On the other hand, in the age group of 15 years and above, more parasuicide cases (14102) were reported than AP (3014) during the same period (10). This shows the relative importance of the two phenomena in under- fifteens and in over-fifteens. In under-fifteens, the younger age group of 0-4, both in males and females, have higher rates of AP than the older age group (ie. 5-14). Infact, males aged (0-4) have the highest average AP rate (19.91 per 100,000) of all age groups of both sexes and females in the same age group have the second highest rate( 12.60 per 100,000). This indicates that children of both sexes in the age group of 0-4 are in general highly vulnerable to AP. It is known that accidents involving household poisons, especially in children under five years of age, are attributable to three main factors: (1)improper storage, (2) poor lighting, and (3) human factors, including failure to return poison to its proper place, failure to read the lable properly, and failure to recognize the substance as poisonous (12). In the U.S.A., non-fatal poisnings are 100-200 times as frequent as fatal poisonings. Medicines account for about 50% of all cases of poisoning (aspirin 20%); cleaning and poisoning products, 17%; pesticides, 10%; and petroleum products, 10% (12). Eventhough it is not known what types of household poisons are responsible in Addis Ababa, general instructions on how to prevent household poisoning are best given to parents repeatedly and regularly with each visit to the M.C.H. clinic and booklets should be available for distribution. If there is an older child in the family, the parents may be warned that it is common for an older child to feed a younger one a poisonous material (12). The visible increase rates of AP after 1990/91 (see Figure 3), specially in the age group 0-4 could be due to easy availability of household poisons in the market, including in the hands of the street vendors or due to parental preoccupation with their own stresses (political, social, and economic) which brought about factors of AP mentioned above. The trends of the monthly averages of AP in under fifteens (Figure 4) has no single predominant peak similar to that of parasuicide (Figure 2). It is rather marked by three troughs with monthly averages of 3.1, 3.5, and 3.7. The first two troughs corresponding to ‘Senie’ (June 8-July 7) and Meskerem’ (Sept. 11-Oct. 10) are significantly lower than the average of ‘Tikimt’ (Oct. 11 - Nov. 10)which has the highest monthly average (6.67). The reason for this, whether it depends on the seasonal availability of house-hold poisons or parental and other factors, needs further investigation. In conclusion, this retrospective study of 15 years data on suicide, parasuicide and AP has its own short-comings. 1. Some of the recordings of data, especially on suicide, are incomplete. 2. The age groups used in the report forms of the Ministry of Health are not suitable for tabulating suicidal behaviors; for example, using age groups of 5-14 for suicide and parasuicide which are not reported below the age of 10 years is quite unacceptable. 3. Possible lack of proper knowledge of case definitions and carelessness in tabulation, which lead to the wrong diagnosis and mis-classification. With these limitations in mind, it could be concluded, from the data collected from Minilik II Hospital, and the two pediatrics and other hospitals mentioned, that suicide for under-15 years was not reported so far in Addis Ababa even though 10 deaths were reported due to AP during 15 years in the age groups of 5-14 years. Seventy seven reported cases of parasuicide in the age group of 0-4 years have to be considered as misclassifications. Similar mis classifications are also believed to exist among some of the 402 reported cases of parasuicide in the age group of 5-14 years showing relatively small peaks at the two ends of the graph as in over-fifteens. The mean monthly/daily number of parasuicide also has a single remarkable peak for the month of ‘Nehasie’ (Aug. 7 - Sept. 10), similar to that of over-fifteens. It appears that the magnitude of misclassification has not apparently affected the general trends of the mean monthly/daily numbers. The number of AP cases reported in under- fifteens is almost twice that of parasuicides indicating Trend in suicide, parasuicide and accidental poisoning in Children 269 ──────────────────────────────────────────────────────────── that this group is more vulnerable to AP. In fact, boys in the age group of 0-4 years have the highest AP rate, as mentioned earlier, followed by girls in the same age group. There are no remarkable changes in the trends of AP rates during the 15 years indicating that factors which had some effect on parasuicide rates did not show any effect on AP rates. But the trends of mean monthly number of AP have manifested three troughs, two of which are significantly lower than that of the month of ‘Tikimt’ (Oct. 11 - Nov. 9) which has the highest mean. The real reason for this needs further investigation . Acknowledgements I gratefully acknowledge the Ethiopian Science and Technology Commission for the financial assistance. I am thankful to Dr. Kassahun Abate for his critical review of the statistical analysis and to Ato Mulugeta Wondimu, the Psychiatric Nurse, and Ato Mulugeta Ademe for their help in data collection. I am also grateful to W/o Almaz Lemma for her secretarial help. References 1. Binger CM. Child and Adolescent Psychiatry. In: Goldman HH, editor. Review of General Psychiatry. California: Lange Medical publications, 1984:642-648. 2. Office of the Population and Housing Census Commission, Central Statistical Authority. The 1994 population and Housing Census of Ethiopia, results for Addis Ababa. Addis Ababa, august 1995, volume 1, statistical Report. 3. Floher LM, Philips I. Mental Disorders of Childhood and Adolescence. In: Goldman HH, editor. Review of General psychiatry. California: Lange Medical publications, 1984:488-513. 4. Taylor EA, Stansfeld SA. Children who poison Themselves. Brit J Psychiat 1984; 145,127-135. 5. Barker P. Basic Child psychiatry. 4th ed. London: Granada publishing Ltd,1983. 6. Mc Clure GMG. Recent Trends in Suicide Amongst the Young. Brit J psychiat 1984:144,134-138. 7. Mc Clure GMG. Suicide in Children and Adolescents in England and Wales 19601990.Brit.J.Psychiat. 1994;165,510-514. 8. Brooksbank DJ. Suicide and Parasuicide in Childhood and Early adolescence. Brit J Psychiat 1985;146,459-463. 9. Pearn J et al. Accidental Poisoning in Childhood: Five year urban population study with 15 year analysis of mortality. BMJ.1984; 288:44-46. 10. Addullahi A. Trends of Suicide, parasuicide and accidental poisoning in the general population and in over 15 year olds in Addis Ababa, Ethiopia. Ethiop J Health Dev 1999;13(3): 11. Mc Clure GMG. Trends in suicide for England and Wales 1975-80. Birt J Psychiat 1984;144,119126. 12. Silver HK, Kempe CH and Bruyn HB. Handbook of pediatrics. 9th ed. California: LMP 1971:582604. Original article Breast milk intake measured by deuterium kinetics in mother-infant pairs in Addis Ababa Zewditu Getahun1, Rachel Elsom 2, Hailemichael G/sellasie 1, Leslie John Charles Bluck 2, Yonas Taffese1, Anthony Wright 2, Graham Jennings 2 Abstract: The accurate determination of breast-milk intake of infants is essential in order to estimate energy intake and nutrient requirement during infancy and lactation. The deuterium dilution technique was employed for measuring breast-milk intake in exclusively breast-fed Ethiopian infants. This method is convenient for field conditions rather than the commonly used test-weighing procedure. In addition, the feasibility of using the less specialised, more efficient and considerably cheaper instrument, Fourier Transform Infrared (FTIR), was evaluated in the Ethiopian setting. The results obtained were compared to that of Isotope Ratio Mass Spectrometer (IRMS). Ten mother-infant pairs were recruited from two government subsidised health centres, namely Ledeta and Semen. Mothers received a pre-weighed 30g oral dose of D2O. Maternal and infant saliva samples, and breast milk samples were collected over a 14-day period following dose administration. Anthropometric data were also collected. Saliva and deffated milk samples were analysed for deuterium enrichment by Infrared Spectroscopy and Mass Spectrometry and the data were fitted into two-compartment model. Infant weights were compared with a 12 months breast-fed infant-pooled data set. Comparison of these infants with 12 months breast-fed pooled data set showed that weight for age Z-scores were below the mean. There was no significant difference between initial and final Z-scores (p>0.05) during the experimental period although all of the infants showed some catch-up growth. Mean ± SD breast milk intake was 850±120ml/day and 880±120ml/day measured using FTIR and IRMS, respectively. The study has demonstrated that it is feasible to measure breast milk intake using deuterium dilution technique in the Ethiopian setting and Infrared spectroscopy could be used for the purpose. It also confirmed that Ethiopian mothers have comparable or higher milk output than privileged communities. These findings have important implications for future research. [Ethiopia. J. Health Dev. 1999; 13(3): 271-279] Introduction In recent years, attention has been given to the length of time for which breast-milk alone is adequate to support normal infant growth. In most cases the age at which supplementary food should be given is the age at which breast-milk production falls below the requirement. The amount of milk transferred to the infant affects the infant's energy intake and the mother’s energy requirement. The energy requirement of an individual is the level of energy intake from food that will balance energy expenditure when the individual has body size, composition, and level of physical activity consistent with long term good health (1). For exclusively breast-fed infants, energy requirement is solely based on energy intakes from maternal milk. The accurate estimation of breast-milk intake of infants is essential to the estimation of nutrient requirements during infancy and lactation (2). The most widely used method for measuring milk intake is the test-weighing procedure in which the infant is weighed before and after each feeding. In this method milk intake is usually underestimated by approximately 1% to 5% (3). The method is ______________________________________ 1 From Ethiopian Health and Nutrition Research Institute, P.O. Box 1242, Addis Ababa, Ethiopia; 2 Dunn Nutrition Unit, Medicial Research Council, Cambridge, UK. Breast milk and deuterium kinetics 271 ──────────────────────────────────────────────────────────── technically simple, requires minimal equipment and training of personnel but prone to measurement errors (4). Another method is the mechanical extraction of breast-milk, which is also prone to measurement error (5). It is especially difficult to use the test weighing method in Ethiopia as it requires full co-operation and knowledge of the mother for taking accurate measurements which complicates the matter as most mothers in Ethiopia can not read and write and, as a result, leads to omitting feeds. Therefore, the method of choice is the deuterium dilution technique as test-weighing method is not suitable for field conditions. The measurement of breast-milk intake by use of the deuterium dilution technique was first introduced by Coward et.al. (6). In the original method deuterium oxide is administered to the infant. This resulted in overestimation of the infant total body water and also unreported water intake from other sources other than human milk (6,7). An improved version of this method, where the dose of deuterium is given to the mother, avoids these problems. The isotope dilution method does not interfere with feeding behaviour and is therefore suitable for longitudinal studies in developing countries (9). In this study Infrared Spectroscopy was used for measurement of breast-milk intake and the results were validated against the gold standard Mass Spectrometric measurement. The application of this non-invasive, convenient method is tested in the Ethiopian setting. This study was done as part of a large-scale study designed to measure the breast-milk intake of exclusively breast-fed infants in Addis Ababa, Ethiopia. Methods Ten women of low socio-economic status were recruited from two government subsidised health centres, namely Semen and Ledeta Health Centers, immediately after the birth of the infant. All infants were full-term and the appropriate size for gestational age. At the time of the study all infants were aged less than four months, exclusively breast-fed, and free from infection. Ethical approval for the study was obtained from the Ethiopian Health and Nutrition Research Institute’s Ethical Committee. Written informed consent was obtained from all participating mothers. On study day “0”, a pre-weighed 30g dose of neat deuterium oxide was administered orally to each mother irrespective of body weight, following the collection of the pre-dose samples and anthropometric data. This was in agreement with an earlier study by Caballero(10). The use of a fixed isotope dose simplified the procedure, bypassing the need to know each subjects weight before preparing individual doses, and is acceptable provided an accurate record of each mother’s weight is made on day “0”. Samples of breast-milk, maternal and infant saliva were collected over a 15 day period, (day’o’ through day ‘14’), commencing with a pre-dose sample on day ‘o’ to determine background enrichment, followed by sampling, on days 1,2,3,4,13 and 14 after dose administration. Breast-milk samples (approximately 10-20ml) were obtained by manual expression. Saliva samples of between 3-5 ml were collected by having the mothers expectorate into clean plastic tubes. To obtain infant saliva, foam mouth swabs were cut down to approximately 1.5cm cubes, and rolled around the infant’s mouth until saturated. The foam was then squeezed into 5ml sterlin plastic tubes. At least 30 minutes had to elapse between the last feed and the collection of the sample to avoid contamination by residual breast milk. All samples were placed in a cool bag on collection in the field. Later samples were stored at-70o C. On day ‘0’ of the study, mothers were weighed to the nearest 100g using a standard clinical scale (TEFAL, sensitive computer, 130kg/100), and their height was measured to the nearest 0.1cm. Mid upper arm circumference was determined and triceps, biceps, sub-scapular, and superailiac skinfold thickness were measured in triplicate using Lange Callipers (Holtazan Ltd, Cry Mych, UK). Infants were weighed naked to the nearest 100g using an electronic baby scale (Mod. 727-SECA, CMS Weighing equipment Ltd). Length was measured using a portable length board (Pedobaby, Brussels, 272 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Belgium). These measurements were repeated on the last day of the study. The growth of these infants was compared with the new international growth reference prepared by WHO based on children who are fed according to WHO recommendations, which entail exclusive breast-feeding for the first 4-6 months of life. Infant weights were plotted on growth charts derived from pooled 12-month growth data for breast-fed children (11). Weight-for-age Z-scores were calculated and a paired t-test applied for significant change in Z score over the experimental period. Laboratory procedures: Approximately 1.5ml of breast-milk and maternal saliva were centrifuged at 13000 rpm for five minutes, as required. The deffated milk samples were transferred to clean tubes, as was the supernatant obtained from each saliva sample. The whole sample was centrifuged at 13000 rpm for five minutes. The sample was recovered after FTIR analysis to be reused in later analysis by isotope Ratio Mass Spectro-meter. The Fourier Transform Infrared (FTIR) Spectrometer was used to determine the 2H enrichment of saliva and breast-milk samples. This method is based on the detection of the vibrational band produced by deuterated water between 2400 and 2600cm-1,in the infrared region of the spectrum. Predose samples were used as a reference against which the corresponding post-dose samples were read. These measurements were made in duplicate, while measurements of the standard against distilled water were made in triplicate at least three times a day in order to calibrate the instrument. Measurements are expressed in parts/million (ppm) excess that is above background enrichment. Mass Spectrometric analysis was performed by using a Sira 10 (Vacuum Generators Ltd, Middlewich, Cheshire, UK). The saliva samples were centrifuged prior to equilibration to remove solids, but tests on centrifuged and non-centrifuged breastmilk indicated that the results were not influenced by centrifugation and so this step was not performed. Samples were measured in duplicate and calibrated by the inclusion of two references of differing isotopic composition in each loading list to allow SMOW/SLAP corrected values to be obtained. Data analysis and modelling: To estimate the agreement between deuterium enrichment measurements obtained for breast milk with those for maternal saliva, the mean values obtained for milk and saliva were plotted against the difference between the values at each data point, (12). Breastmilk intake was estimated from a two-compartment model, describing the monoexponential decay curve of deuterium in the mother’s milk and multi-exponential curve of deuterium appearance in the infant’s saliva(9). The model does not include a time delay. A spreadsheet devised in Microsoft Excel was used to calculate the various parameters of water kinetics. Each mother-infant pair was modelled individually using values obtained from the analysis of infant and maternal saliva. The infants total body water (TBW) was calculated from the equation of Butte et al. (8). Single estimate of body water was considered inappropriate since the infants showed a weight increase over the two-week period during which samples were taken. Estimates were made from the baby’s initial and final weights, and intermediate values calculated by linear interpolation. Maternal total body water pool was calculated as the hydrogen distribution volume divided by a factor of 1.04 to account for non-aqueous exchangeable hydrogen. From this the weight of lean tissue was estimated, assuming it to be 73% hydrated, and the amount of fatty tissue calculated as the difference between the mothers total and lean tissue weights. Statistical analysis: A paired t-test was carried out to discover whether the final z-scores were significantly different from the initial Z-scores. Bland and Altman plot was made to see the agreement between breast-milk and saliva measurements on FTIR(12). Breast milk and deuterium kinetics 273 ──────────────────────────────────────────────────────────── Table 1: Maternal anthropometric characteristics Subject Age Height Weight (yrs) (m) (kg) BMI (kgm-2) MUAC (cm) Sum skinfolds (cm) Predicted body fat (%) 1 2 3 4 5 6 7 8 9 10 Mean SD 18.47 19.04 23.32 23.44 20.82 21.76 24.60 18.96 20.75 21.19 21.2 2.1 22.00 23.75 29.70 25.35 26.30 25.00 25.55 23.40 24.50 24.30 24.9 2.0 54.90 87.20 80.80 59.60 53.60 51.70 76.10 47.13 53.53 52.70 61.7 14.1 27.79 34.34 34.34 28.72 27.33 26.87 32.45 27.33 29.18 27.33 29.57 2.83 20 22 30 28 22 23 26 31 38 22 26 6 1.62 1.65 1.77 1.62 1.64 1.54 1.59 1.55 1.51 1.56 1.61 0.07 48.40 51.80 73.00 61.40 56.00 51.60 62.30 45.50 47.00 51.50 54.8 8.5 Results Age, weight, height and skinfold-thickness of the mothers are presented in Table 1. The BMI values for the mother range from 18.5 to 24.6 showing that none of them ware malnourished (13). The mean mid-upper arm circumference 24.99 was 90% of the standard of WHO reference (14), indicating that maternal body fat stores are adequate for breast-feeding. Skinfold measurements were converted to an equivalent fat percentage using the equation developed by Durnin and Womersley (15) to predict body density, from which body fat content can be predicted using Siri’s equation (16). Mean ± SD initial infant weight was 4.46 ± 0.75kg and mean ±SD final weight was 4.99 ± 0.83kg, with an average increment of 0.53 ± 0.28kg. Comparison of these infants with a “12 month breast-fed pooled data set” Table 2: Infants characteristics Subject Sex Age (d) 1 2 3 4 5 6 7 8 9 10 Mean SD M F M M F F M M F M 25 31 41 31 45 63 45 35 45 101 46 22 Initial Weight(kg ) 3.77 3.85 4.95 4.35 4.30 4.00 5.61 3.90 4.00 5.85 4.46 0.75 ZScore Age(d) 0.50 -1.00 1.00 -0.50 -1.50 -2.00 0.00 -1.00 -2.00 -0.50 -0.70 1.01 39 45 55 45 59 77 59 49 59 115 60 22 Final Weight(kg ) 4.50 3.94 5.09 4.95 4.65 4.50 6.40 4.40 4.95 6.50 4.99 0.84 ZScore 0.00 -2.00 -1.00 -1.00 -1.00 -2.00 1.50 -2.00 0.00 -0.50 -0.80 1.11 Change Weight(kg ) 0.73 0.09 0.14 0.60 0.35 0.50 0.79 0.50 0.95 0.65 0.53 0.28 ZScore 0.50 1.00 2.00 0.50 -0.50 0.00 -1.50 1.00 -2.00 0.00 0.10 1.20 274 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── Table3: Summary of the data obtained from the Mass Spectrometric and Infra-red methods. In each case the results are quoted as the mean of the ten subjects with the standard deviations following in parentheses. MOTHER age weight D space Lean Mass Body fat fat% wat intake BABY Age Start weight Final weight Start ext water final ext water KINETIC Mass SpecS FTIR 26(6) 54.9(8.5) 30.4(5.3) 0.0(6.9) 4.9(3.3) 7.1(4.5) 26(6) 54.9(8.5) 29.8(5.0) 39.3(6.6) 15.6(3.6) 28.3(4.7) Years kg (dm)3 kg kg 3.87(0.68) 3.82(0.66) (dm)3day-1 46(22) 4.5(0.8) 5.0(0.8) -0.03(0.05) 0.0.8(0.02) 46(22) 4.5(0.8) 5.0(0.8) .00(0.07) .08(0.01) days kg kg kg.day1kg.day1-1 k(mm)=0.128(0.013) k(bb)= 0.267(0.031) k(bm)=0.025(0.003) F(bm)=0.76(0.10) Milk vol 0.88(0.12) 0.129(0.015) 0.270(0.035) 0.025(0.004) 0.74(0.10) 0.85(0.12) day1 day1 day1 kg.day1 kg.day1 show that the mean initial Z-score was 0.7 ± 1.01 and the mean final Z-score was 0.10 ± 1.20 (Table2). Eventhough 90% of the infants had weight-for-age Z score below the mean, none of the infants were observed to have weight for age Z-scores below – 2SD. There was no significant difference between initial and final Z-scores (p>0.05) although all of the infants had shown some catch-up growth. Figure 1: Bland and Altman analysis of the Mass Spectrometric results obtained from maternal saliva versus breast-milk. Breast milk and deuterium kinetics 275 ──────────────────────────────────────────────────────────── Figure 2: Modelled elimination curve for a representative mother-infant pair. The Bland and Altman plot (Fig.1) for saliva and breast-milk showed that results from the two fluids, breast-milk and maternal saliva, were therefore not significantly different. Without exception, saliva data showed greater precision than that obtained from breast milk. Table 3 summarises the parameters of water kinetics for the 10 subjects analysed. The mean steady state transport of water to the infant from the mother (Fbm) was 0.760 ± Figure 3: Weight-for-age of girls in the “12-month breast-feed pooled data set” 0.10, using Mass Spectrometric measurements and was 0.74 ± 0.10 on FTIR, assuming 87% of human milk consists of water. It was necessary to calculate the deuterium dilution space (D space) for both the initial and final measurements as the infants were in an extremely dynamic phase of growth. Generally, it is considered sufficient to measure the initial deuterium dilution space alone and, from this, calculate the final space, (17). The deuterium enrichments and modelled elimination rate curves for a representative mother-infant pairs are shown in Fig.2. After calculating Fbm, which represents 276 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── only the free water of milk and does not include the water obtained from the oxidation of milk solids, milk output was calculated as M=Fbm/0.87. Therefore, the average milk output was 880 ml/d using measurements on MS and 850 ml/d using FTIR. There is no significant difference between milk output measured by the two methods. Figure 4: Weight-for-age of boys in the “12-month breast-fed pooled data set” Discussion The results of the study support previous studies (8,9,17) that it is possible to conduct investigations into breast-milk intake using the deuterium dilution technique in underprivileged populations in developing countries, in this case Ethiopia. Concerns had been expressed that the fixed dose of 30g D2 0 would not achieve adequate isotopic enrichment in the saliva samples towards the end of the elimination period for detection by the less sensitive Infrared Spectroscopy method. However, not only was the Infrared Spectrometer able to detect enrichment at values of less than 200ppm, the precision as estimated by the coefficient of variation, was well below the accepted limit of 5%. The measurements obtained by FTIR were validated against IRMS and the results for all kinetic parameters and breast-milk output were comparable. Therefore, it is feasible to use Infrared Spectroscopy in the analysis of samples; thus corroborating the study carried out by Caballero et al. (10) in Indonesia. There is a very wide range in milk intake among healthy, exclusively breast-fed infants. In industrialised countries, milk intakes average approximately 750 to 800ml/d in the first four to five months, but range from approximately 450 to 1,200ml/day (18,19,20,21). Most of these studies used the test weighing method, which tend to underestimate milk production when compared to the deuterium dilution technique. Data from developing countries indicate a similar mean level of intake when a rigorous methodology for measuring milk volume is used (22). Several studies indicate that potential milk production in humans is considerably higher than the average milk intake by a single infant. In two separate studies, milk production increased by 15% to 40% when breast pump was used to remove additional milk after feedings (23,24). Previous study done on breast-milk composition of Ethiopian and Swedish mothers reveals that milk volume was 769 ± 354 and 808 ± 225ml/day for underprivileged and privileged Ethiopian mothers, respectively (25). This was done by using a rigorous methodology of emptying both breasts by using an electrical pump. Using the safe and non- Breast milk and deuterium kinetics 277 ──────────────────────────────────────────────────────────── invasive method of deuterium dilution, breast milk intakes of the Ethiopian infants in this study were similar to or exceeds those commonly reported for exclusively breast-fed infants in privileged and underprivileged populations (8,26). Human milk intakes (648.0±63.1ml/d) of priveileged breast-fed infants from huston (27), and of 23 Papua New Guinean infants (mean ± sd: 606 ± 100ml/d at one month; 734 ± 164ml/d at two months) receiving minimal supplementation (9), are lower than those estimated using the same D20 dose-to-mother method as in this study where the milk intake for 10 infants (mean age, 60 days) was 880±120ml/d using Mass Spectrometric method and 850±120ml/day using the Infrared method. The fact that most of these mothers were from low socio-economic class does not seem to affect milk production. The most important variable behind lactation failure in poor women, namely milk volume, does not not seem to be dependent on food intake, but the combined stress of maternal disease and undernutrition. The mothers in this study were healthy and with adequate fat stores which may have contributed to high milk output. The dose-to-mother method for measuring breast-milk output is non-invasive simple and safe, and involves minimal disruption to feeding behaviour. In the original deuterium dilution technique developed by Coward (6), the dose was given to the infant and not to the mother. However, this method demands longer fasting periods for the infant immediately preceeding sample collection, and more significantly, is based on the assumption that the only water source presented to the infant is breast-milk, (28,2). If this is not the case, all food and water consumed from sources other than breast milk must be recoreded quantitatively (27). The revised method of dose administration to the mother (28) obviates these difficulties. Milk-water volume is calculated using the compartmental model, from which it is possible to estimate the amount of supplemental water intake (Fbo), thus enhancing the accuracy of estimates for milk intake. Comparison of these infants with the 12-month breast-fed pooled data set (11) revealed that 90% of these infants were below the mean (Fig 3&4). However,this is not necessarily indicative of undernutrition, but may instead illustrate the non-transferable nature of reference data between populations, particularly when applying figures based on affluent populations to those in deprived areas. Contrary to the high breast-milk intake and considering the mean age for these infants (60days), it can not be concluded that they were not growing very well. Furthermore, the aetiology of infant growth faltering in underprivileged populations is not fully understood (8). It was shown that early growth faltering is not attributable to breast-milk intake. Despite human-milk intakes of 885±145 and 869±150ml/day at four and six months, respectively, growth faltering was evidenced by a significant decline in growth velocities and NCHS scores. Similarly, in this study despite the high breast milk intake, the growth of the infants was below the mean for exclusively breast-fed infants(11). Therefore, growth faultering, is unlikely, however, to be solely due to inadequate lactation (29,30). This suggests that there may be other factors, besides nutritional, for the growth failure in breast-fed infants in developing countries. Infection, genetics, and altitude, are all factors that may modify the physical growth of children, and it is highly probable that deficits of nutrients other than energy have growth limiting effects. It is too early to see whether the infants in the study are suffering from growth faltering, but data from the Ethiopian Statistical Authority (30) have shown that 56.5% of Ethiopian children aged 6-11 months, and a staggering 64% of those under five, are stunted. Growth faltering tends to appear at about six months when breast-milk intake starts to become insufficient to meet the growth and development requirements of the child (8,29). It could therefore, be argued that conducting a largescale survey into the breast milk intakes of infants aged less than four months is not targeting the group most at risk. A better use of resources perhaps, would be to determine the intakes of babies 4-12 months of age, and on the basis of this information, formulate public health policies concerned with the optimum time for introduction of weaning foods. There is, however, a huge amount of evidence supporting the adequacy of breast- milk as the sole source of nutrition for at least the first four months 278 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── of life, (32,33,34). Indeed, it may be that in underprivileged environments where the introduction of supplementary foods and fluids of poor nutritional quality, in unsanitary conditions, is associated with a heightened risk of malnutrition and infection, exclusive breast-feeding should be promoted. To conclude, the study has demonstrated that it is feasible to measure breast milk intake using the deuterium dilution technique in the Ethiopian setting. It also confirmed that lactating Ethiopian mothers have comparable or higher milk output than privileged communities. These findings have important implications for future research. Acknowledgements We would like to thank the mothers who participated in the study for their co-operation and hospitality. Our sincere thanks to the International Atomic Energy Agency for funding the project and the EHNRI for logistical support. References 1. FAO/WHO/UNU Expert consultation: Energy and protein requirements. WHO Technical report series. Geneva: WHO. 1985;724. 2. Butte NF, Garza C, Smith EO & Nichols BL. Evaluation of the deuterium dilution technique against the test-weighing procedure for the determination of breast milk intake. Am J Clin Nutr. 1983;37:996-1003. 3. Brown KH, Black RE, Robertson AD, Akhtar NA, Ahmed G and Becker S. Clinical and field studies of human lactation: methodological considerations. Am J Clin Nutr. 1982;35:745-756. 4. Michael KF, Larsen PS, Thomson BL, Samuelson G. The Copenhagen cohort study on infant nutrition and Growth:breast milk intake, human milk macronutrient content, and influencing factors. Am J Clin Nutr. 1994;59:600-11. 5. Brown KH, Black RE, Robertson AD, Naheed Ahmed Akhtar; Giashuddin Ahmed;Beeker.S. clinical and field studies of human lactation:methodological considerations. Am J Clin Nutr. 1982;35:745-756. 6. Coward, WA, Sawyer MB, Whitehead RG, Prentice AM & Evans J. New method for measuring milk intakes in breast-fed babies. The Lancet. 1979;13-14. 7. Butte NF. Wong WW, Patterson BW, Gaza C, Klein PD. Human-milk intake measured by administration of deuterium oxide to the mother: a comparison with the test-weighing technique. Am J Clin Nutr. 1988;47:815-821. 8. Butte NF,Wong WW,Gaza C. prediction equations for total body water during early infancy.Acta paediatr. 1992;81:264-5. 9. Orr-Ewing AK, Heywood PF, Coward WA. Longitudinal measurments of beast milk output by a 2 H20 tracer technique in rural Papua New Guinean women. Human Nutrition: Clinical Nutrition 1986;40c: 451-467. 10. Caballero B, Novotny JA, Conway JM, Kjolhede C, Dibley, Sadijimin T, Fjeld CR. Breast milk intake in infants measured by deuterium oxide dilution and infrared spectroscopy:a field study in rural Indonesia. Am J Clin Nutr. 1997;(in print). 11. WHO: WHO working Group on Infant Growth an Evaluation of infant growth. Nutrition Unit, WHO,Geneva. 1994. 12. Bland JM, Altman DG. Statistical methods for assessing Agreement between two methods of clinical measurement. The Lancet 1986;1:307-310. 13. James WPT, Ferroluzzi A, waterlow JC. Definition of chronic energy deficiency in adults-report of a working party of the international-dietary-energy consultative-group. European Journal of Clinical Nutrition 1988;42(12):969-981. 14. Jelliffe D. The assessment of the Nutritional status of the community. Geneva, WHO. 1966. 15. Durnin JVGA, Womersley J. Body fat assessed rom body density and its estimation from skinfold thickness:measurement on 481 men and women from 16 to 72years. Br J Nutr. 1974;32:77-97. 16. Siri WE. Univ. Calf Radiat. Lab. Publication No. 3349. 1956. 17. Fjeld CR, Brown KH, Schoeller DA. Validation of the deuterium oxide method for measuring average daily milk intake in infants. Am J Clin Nutr. 1988;48:671-679. 18. Butte NF, Gaza C, Smith EO, Nicholas BL. Human milk intake and the growth in exclusively breast-fed infants J. Pediatr. 1984b;104:187-195. 19. Dewey KG, Lonnerdal B. Milk and nutrient intake of breast-fed infants from 1 to 6 months:relation to growth and fatness.J.Paed. Gastroen. & Nutr. 1983;2:497-506. 20. Hofvander Y, Hagman U, Hjillervik C, Sjolin S. The amount of milk consumed by 1-3 months old breast or bottle-fed infants. Acta paediatr. Scand. 1982;71:953-958. 21. Neville MC, Keller R, Seacat J, Lutes V, Neifert M, Casey C, et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr. 1988;48:1375-1386. 22. Brown KH, Akhtar NA, Robertson AD, and Ahmed MG. Lactational capacity of marginally nourished mothers:relationships between maternal nutritional status and quantity and proximate composition of milk. Paediartics 1986b;78:909-919. 23. Dewey KG, Lonnerdal B. Infant self-regulation of milk intake. Acta paediatr. Scand.1986;75:893898. 24. Neville M, Oliva-Rasbach J. Is maternal milk production limiting for infant growth during the first year of life in breast-fed infants? pp.123-133 in A.S.Goldman, Atkinson, and L.A.hanson, Eds. Human lactation 3: The effects of Human Milk on the recipient infant. Plenum Press, New york. 1987. 25. Svanbeg U, Gebre-Medlin M, Ljungqvist B, Olsson M. Breast-milk composition of Ethiopian and swedish mothers. III. amino acids and other nitrogenous substances. Am J Clin. Nutr. 1977;30:499-507. 26. Jelliffe DB, Jelliffe FC. Humsn Milk in the Modern world. Oxford: Oxford University Press. 1978. 27. Butte NF, Wong WW, Patterson BW, Garza C, Klein PD. Human-milk intake measured by administration of deuterium oxide to the mother: a comparison with the test-weighing technique. Am J Clin. Nutr. 1988;47:815-821. 28. Coward WA, Cole TJ, Swayer MB, Prentice AM. Breast milk intake measurement in mixed-fed infants by administration of deuterium oxide to their mothers. Human Nutrition: Clinical Nutrition 1982;36C:141-148. 29. Cohen RJ, Brown KH, Canahuati J, Rivera LL, Dewey KG. Effects of age of introduction of complementary foods on infant breast milk intake, total energy intake, and growth: a randomised intervention study in Honduras. The lancet 1994;344:288-293. 30. Duncan B, Schaefer C, Sibley B, Marques FN. Reduced growth velocity in exclusively breast-fed infants. An J. diseases in childhood 1984;138:309-313. 31. Authority CS. Rural National Nutrition Survey, Ethiopia. 1992. 32. Borresen HC. Rethinking current recommendations to introduce solid food between four and six months to exclusively breastfeeding infants. Journal of Human Lactation 1995;11(3):201-204. 33. Whitehead RG. for how long is exclusive breast-feeding adequate to satisfy the dietary energy needs of the average young baby? Paediatric Research 1995;37(2):239-243. 34. Whitehead RG, Paul AA, Cole TJ. How much breast milk do babies need?acta Paediatrica Scandinavia supplement. 1982;299:43-50. Brief communication Conforming to the international classification of diseases: A critique on health information reporting system in Ethiopia Daniel Fekadu1, Abebaw Fekadu2, Atalay Alem2 Abstract: Even though updating the health information system of a nation and conforming to international standards is essential for health development, it appears that very little attention is being paid to brace up the gap between the international disease taxonomy and that of Ethiopia. With the intention of appraising the existing local state of affairs with regard to the adoption of a national nosology of diseases, a review of current classification methods of diseases in Ethiopia was done and was compared with recent international developments. The World Health Organization (WHO) that took over the responsibility of revisions of the International Classification of Diseases (ICD) in 1946 with the 6th edition has recently come up with the 10th edition which is adopted world wide. Ethiopia is one of the users of the ICD system but, in disparity with the current changes, it still employs the intermediate list of ICD-6 that was supposed to be compatible with the then developing countries’ health manpower. The conditions that dictated the use of WHO’s intermediate list of causes of morbidity and mortality in the 1950’s are no longer compelling. Our review has made us realise that the persistent use of the outdated classification makes our health information system different from the rest of the world. Putting ICD-10, the latest revision, in place, is highly recommended. [Ethiop. J. Health Dev. 1999;13(3):281-283] Historical background One of the methods of relaying health information is through a standard and uniform collection of data on morbidity, mortality, and other conditions using the accepted set of classified lists (1). Through such lists, the varied disease phenomena could be clustered into a well-defined set of categories. The need to use is international classification to report diseases materialised only a century or so ago (2). Careful description of clinical phenomena that lies at the heart of clinical medicine helped to delineate the distinct syndromes in the earliest developments of medical sciences. Those recognised symptoms and syndromes were the basis for the first classification systems until they were more or less replaced by anatomical and then by etiological classification. Although etiological classification is the best way to classify diseases for well-recognised reasons, syndrome and anatomical disease classifications are still in use due to the incomplete comprehension of causes of diseases. The initial driving force behind the development of a classification system was the need for collecting statistical information on causes of death. If we go back to the 17th century where we find the inception of more practical and uniform grouping of disease phenomena, John Graunt was the _______________________________________ Maudsley Hospital, Denmark Hill, SE 5 8AZ, London; 2Amanuel Psychiatric Hospital, P.O. Box 1971, Addis Ababa, Ethiopia 1 first to start the statistical study of disease in under-six children with the intention of tabulating the causes of death (2). A subsequent attempt to classify diseases was made by Francois Bossier de Lacroix and William Farr (2). The facilitation of nosological uniformity began receiving international backing, as it wouldnaturally deserve, in the 19th century. Of much interest would be the introduction of the ICD system and especially the 6th revision that was produced by the WHO in 1948 (2) extending its list to include non-fatal conditions which evidently implied the inclusion of other categories like mental illnesses. The 7th revision of the ICD was made in 1955, while the 8 th and 9th revisions took place in 1965 and 1975, respectively. The latest revision, i.e., ICD-10, was released in 1992 (3). It is composed of 10 alphanumeric groups (4), one or more alphabets representing every chapter. Each alphabet stands for a similar group of diseases, disorders or conditions while two digits follow the alphabet. The next two digits after the dot designate subdivisions. For instance, the ICD-10 designates the letter ‘F’ for mental and behavioural disorders. ‘F20’ would represent the severe mental illness, schizophrenia. To add a specifier would require additional codes. Thus a paranoid type of schizophrenia with continuous course would be coded as ‘F20.00’(3). It should also be noted that the ICD has varying details for different users. There are other methods of classification for local use. Among these the American Psychiatric association has a well developed one called Diagnostic and Statistical Manual of Mental Disorders (DSM). This manual first appeared in 1952, shortly after WHO’s ICD-6. The last edition, DSM-IV (7), came into use in 1994. It is multi-axial and has been adopted by many countries. National nosological model In order to assess the national classification system and health reporting system, we visited statistics departments at various levels ranging from health stations to the Ministry of Health, talked with a number of concerned and responsible officials, and collected all necessary materials and information. We reviewed relevant literature and sufficiently browsed the archives at Amanuel Hospital. We assessed various ICD version codes and collected reporting formats from various health institutions to find out which version is in use currently in Ethiopia. This showed us that Ethiopia uses the intermediate list of ICD-6 while the rest of the world uses 9th or 10 th revisions. The WHO intermediate list of 150 entities for tabulation of morbidity and mortality, the ‘A’ list, was probably adopted by the Ministry of Health during 1948-1950 (8). This list was originally a modification of ICD-6 and was provided for developing countries that needed a classification system for documentation and uniform reporting but apparently lacked enough skilled manpower at that time. Ethiopia was obligated to use the list, which is still uses, because of the then existing low manpower level. In 1970, for example, there were 352 doctors in Ethiopia and only 16(17%) were nationals (9). Currently, however, the marked development in the global health information status makes the use of the old intermediate list for any reason non-compelling. Moreover, the man power level at present is much higher than it was then. At Amanuel Psychiatric Hospital it was agreed three years ago to use the DSM-IV classification which has over 400 entities. Similar models are also used in other psychiatric units in the country. However, the current Ethiopian official statistical format provides only six codes, including a code for healthy people. The origin of these six codes (7) for psychiatric disorders in this country seems obscure. According to the existing records of Amanuel Hospital (8), the first report was made by an expatriate psychiatrist in 1956. The list was made of ‘A’ code with two digits for each, and where necessary, for a lump of disorders grouped in a class. Almost all personnel in charge of health information units at all levels of health institutions are not trained in medical statistics. Invocation for a more accommodative Model Despite some degree of inconvenience and inflexibility, classification of diseases has several advantages (2). Primarily it facilitates the deduction of general principles. Secondly, it promotes the collection of clinical information, communication, and research. Thirdly, it is a basic tool for health policy and planning. Finally, it helps as a useful educational tool and may further serve in the evaluation of medical care, hospital indexing, and medical audit systems. Despite the consensus to use the DSM-IV classification system in the psychiatric domain, the national health statistics reporting system’s requirement to still use the intermediate list of ICD-6 impedes practitioners from taking advantage of the more informative DSM-IV or ICD-10. The six codes of the national list are far too short to record and report the vast majority of cases we encounter in clinical practice and we have been forced to pigeonhole the divers class of disorders into broad and ambiguous clusters. We believe the current pigeonholing is incorrect, leads to faulty information gathering, and is a handicap in communicating with colleagues in the rest of the world. Our search has led us to appreciate the inconveniences the existing system must have caused to other medical fields as well. We believe that it is timely to seek for ways of revising the old list of morbidity. The low skilled manpower level which obligated the use of the old 150 intermediate list cannot be a sufficient reason presently. Based on our observation, we suggest that the constricted reporting of psychiatric morbidity has to expand and conform to ICD-10 while taking every precaution in the national adaptation. Similar experiences pointed out that adjusting the ICD might result in significant changes and cause reversal of instructions in the manuals, thus mystifying exchange of comparable data among countries (10). Other sister disciplines should follow suit. We also suggest that the Ministry of Health should organise a workshop on this critical issue. The Ministry of Health should also attempt to solicit ideas from different disciplines and concerned offices, like the WHO representative here. A system should be designed for effective and flexible reporting. Due attention should be paid to familiarise undergraduate and postgraduate students on updated classification issues. Finally we propose that an arrangement should be made to constantly upgrade the medical knowledge of statisticians and those working in health statistics departments. References: 1. Kendell RE. Diagnosis and classification. In: RE Kendell, AK Zealley eds. Companion to psychiatric Studies 5th ed. Edinburgh, Churchill Livingstone, 1993:277-294 2. WHO. Manual for international Classification of diseases, 8 th revision, Geneva, 1965. 3. WHO. Manual for International Classification of diseases and health related Problems, 10th revision, Geneva, 1992. 4. Sartorius N, et al, Progress toward achieving a common Language in Psychiatry, results from the field trial of the clinical guidelines Accompanying the WHO classification of mental and Behavioural disorders in ICD-10. Arch Gen Psychiartry 1993;50:115-124. 5. Ministry of Health. Summary report on Outpatient Visits 1983, Planning and Programming Department, May 1993. 6. Alem A, Desta M and Araya M. Mental health in Ethiopia. Ethiop J Health Dev. 1995;9:47-62. 7. American Psychiatric Association: Diagnostic and statistical manual of mental disorders, 4th ed. Washington, DC, American psychiatric association, 1994. 8. Amanuel Psychiatric Hospital Records, 1948-1998. 9. Ministry of Health Manpower Study in Ethiopia, Addis Ababa, United Printers, 1980;36-42. 10. Jansson B, Johansson LA, Rosen M, Svanstrom L. National adaptation of ICD rules for classification- a Problem in the evaluation of Cause-of death Trends. J Clin Epidemilo 1997;50(4):367-375. Brief communication Maternal energy and macronutrient insecurity in an ensete-corn staple village of Southern Ethiopia Samson Taffesse1, Maria Grazia2, Woldemariam Girma1 Abstract: Thirty three rural women from Shafina, a Sidama village, aged 25-48 years, were followed longitudinally for their dietary intake for eight rounds from april 1986 to march 1987. Food consumption was measured by the weighed food record technique. The mean habitual daily energy intake was 1833±563 kcal/day, 94% adequate compared to WHO recommendations. Carbohydrate provided 88% of the total daily energy which was 15% higher than the reference upper limit. Total fat intake was critically low contributing only 6.9% of the total daily energy, 54% lower than the lower reference limit reccomended for optimal nutritional health. Protein provided 5.7% of the total daily energy with unmet animal-origin protein requirement amounting to about 78%. Foods of ensete origin provided the largest proportion of the daily energy (46%) followed by cereals, mainly corn, (39.7%). Legumes and tubers provide 3.7% and 2.0% of the total daily energy, respectively. Intakes of all macronutrients and energy were relatively higher during the post-harvest months of December through February compared to the pre-harvest months of June through November. The results from this study indicate that maternal macronutrient and energy nutriture of the study population is both chronically and seasonally insecure. Moreover, the diet is characterised by very high carbohydrate, very low fat and low animal origin protein, which is not consistent with the recommended balance for optimal long term good health, productivity, and reproductive performance. Alleviation of the adverse consequences requires emphasis on the nutrition dimension by the education, health, agricultural, industrial, and other policy sectors within the country. [Ethiop. J. Health Dev. 1999;13(3):285-290] Background Mothers living in developing countries are often exhausted by the combination of pregnancy and child birth which can end in the loss of their lives. Low birthweight and/or immature and malnourished infants born to such women are vulnerable to life-threatening diseases and nutritional problems(1). Moreover, the productivity potential of women is critically hampered by undernutrition(2). The causes of maternal malnutrition are many ranging from inadequate food supply to food taboos and the physiological drain of child bearing and inequitable intra-household food distribution with the women generally eating last and least. In many developing countries, especially in Africa, where climatic seasonality govern agricultural production, food availability is not constant throughout the year. These subsistence farming communities experience various food-insecure periods during each production year. Such seasonal variations in food production and fluctuations in prices of foods could be considered as contributing to transitory food insecurity of poor households, which over time, escalate into chronic food insecurity and nutritional deterioration(3). ______________________________________ 1 Ethiopian Health and Nutrition Research Institute, P.O. Box 5654, Addis Ababa, Ethiopia; 2Italain National Institute of Nutrition Research 284 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── In Ethiopia poor maternal nutritional status and high incidence of infection among mothers cause high perinatal and neonatal mortality. These problems are also responsible for low birth-weights which account for 10% of all live births(4). Chronic as well as transient forms of energy deficiency have also been reported to prevail among the Sidama in Southern Ethiopia (5,6). Although this varies with seasons, food stock, in the Sidama area is highest in December and lowest in July(8). However, there is lack of information as to the actual patterns of maternal macronutrient intakes. Macronutrients are broadly defined as those food components which are present in quantities of one gram or more in the daily diet, and which generally provide energy. They, therefore include protein, fat, carbohydrates,and most dietary fibers and alcohol. Such an information is useful to health, nutrition, and agricultural policies of Ethiopia. The aim of this study was to investigate the extent of maternal macronutrient and energy insecurity in an ensete-corn staple zone of Ethiopia. Methods Thirty-three women who were non-pregnant but lactating, with a parity of 2-8, were randomly selected from a larger list of logistically potential subjects. These were followed from April 1986 to March 1987 (European Calendar) for a total of eight rounds. Dietary intake was monitored at about 45 day intervals by the weighed food record technique using an electronic balance (Terrailon digital scales, 5kg max., ± 5kg accuracy). Scales were regularly calibrated using standard weights. All food consumed was weighed by trained local girl-enumerators who followed the subjects for five consecutive days during each period. Food intake was converted to nutrient intakes using nutrient values from the Food Composition Table for use in Ethiopian (9). Habitual intakes are represented by the overall means. Body weight was measured using digital adult scales. Height was measured by Holtain stadiometer. Percent body fat was calculated from four skinfolds using the equations of Durnin & Womersley (10). Data entry and analysis was performed using the SPSS/PC software (11). One way ANOVA with the tukey HSD test was employed to examine the significance of differences between means of different groups. Results Energy and macronutrient intakes: Table 2 summarizes energy, protein, fat, and carbo-hydrate intakes of the group during different periods. The mean total daily energy intake was 1833±563. ANOVA revealed an overall statistically significant difference p<0.05, between energy intakes during the various months. The difference between the maximum energy intake, 2015±585 kcal/day recorded during the post-harvest season of January/February and the minimum mean daily energy intake, 1694±543 kcal/day, recorded during the pre-harvest months of June/July was statistically significant (P<0.05). Maternal energy and macronutrient insecurity in an enset-corn staple 285 ──────────────────────────────────────────────────────────── Table 1: Anthropometric characeteristics of subjects Mean±SD Age (yrs) 36±7 Weight (kg) 45.0±4.0 Height (m) 1.57±5.7 Body mass index (kg/m2) 18.4±1.6 Mid upper arm circumference(cm) 23.8±1.1 Biceps skinfold (mm) 3.4±0.8 Triceps skinfold (mm) 8.9±2.3 Subscapular skinfold (mm) 10.4±4.2 Suprailliac skinfold (mm) 8.6±3.4 Percent fat 21.6±3.8 The habitual mean daily protein intake was 34.5±14.4 g/day. There was a statistically significant seasonal difference with a maximum of 43.0±15.8 g/day, during the month of December. This value was signifcntly higher than the minimum protien intake, 29.5±10.7 g/day, observed during the preharvest months of June/July. The overall mean daily total fat intake was 16.8±9.5 g/day. Total fat intake also showed seasonal variability with the mean highest fat intake, 19.8±8.1 g/day, during the month of December, which was significantly higher than the lowest mean fat intake recorded during the pre-harvest months of June/July, 15.0±9.5 g/day (p<0.05). Table 2: Mean quantitative macronutrient and energy intakes, by months of observation Months Energy (Kcal/day) Protein (g/day) Apr/May Jun/Jul Jul/Aug Sep/Oct Oct/Nov December Jan/Feb March Mean±SD P * lowest intake 1871±566 37.0±15.3 1694±543* 29.5±10.7* 1847±573 32.7±10.2 1704±541 31.9±10.1 1808±442 32.4±10.9 1895±507 43.0±15.8* 2015±585** 38.8±18.0 1833±589 30.9±14.3 1833±563 34.5±14.4 0.000 0.000 ** highest intake Total fat (g/day) 18.7±11.4 15.0±09.5 18.0±10.4 14.0±06.7 18.0±09.5 19.8±08.1** 17.4±09.1 13.5±08.4* 16.8±9.5 0.000 Total carbohydrate (g/day) 361±109 335±106* 375±113 360±119 365±091 350±095 382±114** 355±113 360±133 0.018 286 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── The overall mean total daily carbohydrate intake was 360±113 g/day which varied between a maximum of 382±114 g/day during the months of January/February and a minimum of 335±106 g/day during the months of June/July (p<0.05). Contribution of macronutrients to total calorie intake: Table 3 sumarizes the contributions of various macronutrients to total daily energy intake during various months of observation. On average, total fat contributed about 6.5% of the total daily energy. The average contribution of protein to total energy was 5.4% ranging from 2.8% during July/August to a maximum of 7.8% in December. Total carbohydrate contributed 83% (December) to 94% (July/August) of the total daily energy intake, with the average being about 88.1±7.1%. Total fat provided Table 3: Mean percentage energy contribution of macronutrients, by months of observation Months Protein Fat Carbohydrate Apr/May 6.6±2.7 8.6±7.1 84.8±6.5 Jun/Jul 5.6±2.4 7.1±4.7 87.3±6.4 Jul/Aug 2.8±2.6 3.0±03.4 94.2±5.3 Sep/Oct 3.0±2.2 2.6±2.7 94.4±4.4 Oct/Nov 4.8±2.1 7.8±4.6 87.3±6.2 December 7.8±3.6 9.5±4.7 82.8±6.7 Jan/Feb 6.6±3.2 6.5±4.0 86.9±5.8 March 6.0±3.0 6.7±4.4 87.3±6.2 Mean±SD 5.4±3.2 6.5±4.9 88.1±7.1 P 0.000 0.001 0.047 2.6% (September/October) to 9.5% (December) of the total daily energy intake. Calorie contribution of various food sources: Table 4 presents the contribution of various food groups to total daily energy intake in various periods. The overall average indicates that the two major sources of energy were ensete and corn contributing 46% and 39.7% of the total daily energy intake, respectively. Legumes and nuts provide about 3.7% while animal food sources, including milk, butter, eggs, and meats contribute only about 2% of the total calorie. Ensete provided the highest proportion of energy (62.6%) during the months of June/July while cereals served as a major source, providing 49.9% of the total daily energy during September/October. The lowest proportion of energy from ensete, 36.6%, was contributed during September/October while the lowest cereal energy contribution, 22.2%, was recorded during June/July. Energy from tubers was practically absent during April/May and highest during July/August and September/October (6.6%). Milk and butter provided their highest energy contribution during June/July and December, (1.9%) and lowest during January/February. Table 4: Mean energy contribution (%) of various food groups, by months of observation Month Cereal Ensete Tubers Legumes/nuts Milk/butter Apr/May ‘86 36.8 48.6 0.0 2.9 1.5 Jun/Jul ‘86 22.2 62.6 0.2 3.7 1.9 July/Agu ‘86 48.1 39.4 6.6 0.3 1.5 Sep/Oct ‘86 49.9 36.6 6.6 0.6 0.7 Oct/Nov ‘96 44.1 43.5 4.5 0.9 0.8 December ‘86 40.1 42.8 1.1 6.7 1.9 Jan/Feb ‘87 33.0 48.7 1.1 7.6 1.0 March ‘87 30.1 55.3 0.2 6.9 1.5 Mean 39.7 46.0 2.0 3.7 1.5 Meat/poultry 0.7 0.0 0.4 0.5 0.3 1.1 0.1 0.2 0.4 Discussion The average maternal BMI categorizes the group to chronic energy deficiency Grade I. The mean upper arm circumference is 5% higher than the minimum recommended (12). However, the mean bodyweight lies 1% below the minimum prepregnancy weight (13) associated with increased risk of delivering a small-for-gestational-age (SGA) infant. Hence, generally maternal nutritional status Maternal energy and macronutrient insecurity in an enset-corn staple 287 ──────────────────────────────────────────────────────────── appear to be poor compared to international standards. The major food items included in the diet are corn and ensete with their relative proportion varying with seasons. Overall, ensete is served as a major component of the diet and as a source of energy followed by cereals. This is consistent with a previous report on sidama population (14). Minor components of the diet include legumes and tubers which were not reported in the later study. The habitual energy intake apeared to be relatively sufficient, about 94%, compared to the recommended energy requirement (15). This was 3% lower compared to the Southern Beninese study (16). However, there was a considerable seasonal fluctuation in the adequacy of maternal energy intake ranging from 85% adequacy during June/July to 101% during the months of January/Februray. Similar studies among the Arsi Oromos (17) indicate that energy adequacy varied seasonally in a range of 55-100% from the hungry to the harvest seasons. For predominantly mixed vegetable diets in developing countries it is suggested that protein should contribute 10-12% since protein needs should be corrected for lower digestibility and an increased incidence of diarrhoeal diseases (18). Maternal protein intake among the present study population contributed much below the recommendations. The contrbution of animal protein was 78% lower than the lower recommended range. A previous report for an adjacent population (14) indicated that protein contributed 39% lower to total daily energy. Compared to figures reported for Southern Beninese women (16), the contribution of protein to total daily energy was 46% higher than the present study. These findings suggest that both quality and quantity of protein were below the standard recommended for optimal protein nutriture. There was also a significant seasonal trend in absolute protein intake. Recommendations for fat vary depending, inter alia, on the prevalence of protein energy malnutrition and diet related non- communicable diseases (NCD). For the former, promoting increased consumption of fat is usually desirable while, for the latter decreasing it may be in order (18). Compared to the WHO recommendations, maternal fat intake among our subjects was critically low especially for pregnant and lactating mothers who have had marginal levels of nutritional status. The overall mean shows that the contribution of fat to the daily energy intake was 57% lower than what is recommended for women of child bearing age (17). The contribution of fat to total calories (6% vs. 6.5%) was consistent with those reported for an adjacent population (14). This finding might have implications for intervention work, such as vitamin A supplementation which requires relatively proper fat nutriture for the physiological effectiveness of the supplement. Studies among Beninese women (16) reported 70% higher contribution of the daily energy compared to this study. A significant seasonal trend has also been revealed for maternal fat intakes. Fat intakes were not lowest during the pre-harvest months of June/July unlike energy and the other macronutrients. This was due to the increased proportion of cereal-ensete ratio augumented by improved food variety and a relatively higher availability of milk and butter. Carbohydrate intake was relatively high. The dietary energy contributed from carbohydrates was 17% higher than the upper limit of WHO recommendations (18) and 10% lower than those reported for Sidma adults (14). This indicates that carbohydrates remain to be the dominant source of energy. However, it probably tend to exhibit secular trends as cropping changes from ensete monocrop to ensete-cereal corpping. The Beninese study (16) reported 47% lower contribution of carbohydrate compard to the present study. This study has demonstratd that there exist considerable chronic and seasonal macro-nutrient and energy insecurity. The seasonal deficiency probably has pulled down the mean annual intake which represented the habitual intakes of mothers in the study area. Such a low intake of fat and protein is not consistent with what is recommended for optimal long term good health. The study indicates that the quality of protein is substandard with very low animal protein intake which probably fails to fulfil the essential aminoacid requirements. In our study macronutrient and energy requirements for reproductively inactive women were used as references. This indicates that maternal intakes of protein 288 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── and fat were too low to allow for normal reproductive demads. Complementing the dominant ensete diet with increased animal products, leguminous crops, and vegetables in a more consitent rather than seasonal fashion would be worthwhile to eliminate the likely harmful nutritional consequences. Multisectoral efforts are required to alleviate overall nutritional problems in the country. Nutritional security could only be attained with the involvement of the educational, health, and agricultural sectors as well as others. Production should be increased to cover for the annual requirements of households so that seasonal fluctuation of dietary intake is controlled. Not only quantitative production but also food diversity should be the objective of intervention activities such as agricultural extension efforts. Efforts to impove the energy density of the overall dietary habit should be given due emphasis as the impacts of nutritional insecurity have both current and intergenerational dimensions. Crop diversity with small-scale animal husbandury, rather than monoculture, should be encouraged to fulfil protein and fat requirements. Women should also be empowered and educated to look after their diet and the diet of their off-springs. Moreovr, generation of scientific information and research outputs which create awareness to policy makers should be encouraged by all concerened bodies. Acknowledgments We wish to thank the European Economic Commission for supporting the study financially and the Italian National Institute of Nutrition for introducing the techniques to the ENI. We would like to thank all the girl- enumerators who managed to do a meticulous job. We would also like to thank the former ENI director, Dr. Zewdie W/Gabriel, for his facilitation role. References 1. UN ACC/SCN. Women and ntrition. ACC/SCN symposium report nutrition policy discussion paper no.6. October 1990. 2. Phillip P & Lipton M. How third world rural households adapt to dietary energy stress: The evidence and issues. Food policy review. International Food Policy resarch Institute. 1994. 3. Samson T. The effect of seasonal variatio of nutritional status on the physical work capacity of Ethiopian rural adults and the implication for productivity. Proceedings of the african regional conference on genetic Resources and rural Centered Development for African survival. Institute for Sustainable Development. Addis Ababa. August 1996. 4. Chambers R, Longhurst R, Pachey A editors. Seasonal dimensions to rural poverty. U.S.A. Frances printer Ltd. 1981. 5. UNICEF. Children and women in Ethiopia: a situation report. UNICEF. 1993. 6. Ferro-Luzzi A, Scaccini C, Taffesse S, Bekele A, Demeke T. Seasonal energy deficiency in Ethiopian rural women. Eur J Clin Nutr 1990;44 (suppl.1) 7-18. 7. Branca F, Pastore G, Demissie T, Ferro-Luzzi A. The nutritional impact of seasonality in children and adults of rural Ethiopia. Eur J Clin Nutr 1993;47:851-862. 8. Pastore G, Branca F, Demissie T, Ferro-Luzzi A. Seasonal energy stress in an Ethiopian rural community: an analysis of the impact at the household level. Eur J clin Nutr 1993;47:840-850 9. Food composition table for use in Ethiopia I. Ethiopian Nutrition Institute. 1968. 10. Durnin JVGA, Womersley J. Body fat assessed from body density and its estimation from skinfold thickness. Brit J nutr 1974;32: 77-97. 11. Statistical Package for Social Sciences (SPSS). MS-DOS version. 1990. 12. James WPT, Mascie-Taylor GCN, Norgan NG, Bistrian BR, Shetty PS, Ferro-Luzzi A. The value of arm circumference measurements in assessing chronic energy deficiency in third world adults. Eur J clin Nutr 1994;48:883-894. 13. Berklow R. editor. The Merck manual of diagnosis and therapy. U.S.A. Merk & Co. INC. 1992. Maternal energy and macronutrient insecurity in an enset-corn staple 289 ──────────────────────────────────────────────────────────── 14. Selinus R, Gobezie A, Vahlquist B, dietary studies in Ethiopia III. Dietary patterns among the Sidama ethnic group. Acta Soc med upsal 1971;76:158-178. 15. Diet, nutrition and the prevention of chronic diseases. Tehnical Report Series 797. WHO, Geneva. 1990. 16. Chultnik WJ, Klaver W, Van Wijk H, Van Raaij JMA, and Hautvast JGAG. Body weight changes and basal metabolic rates of rural Beninese women during seasons with different energy intakes. Eur J Clin Nutr 1990;44 (suppl.1)31-40. 17. Selinus R, Gobezie A, Knutsson RE, vahlquist B. Dietary studies in Ethiopia: dietary studies among the rift valley Arsi Oromo. Am J Clin Nutr 1971;24:365-377. 18. WHO/FAO. Preparation of and use of food-based dietary guidelines. Report of a joint FAO/WHO consultation Nicosia, Cyprus. WHO Geneva. 1996. 290 Ethiop.J.Health Dev. ──────────────────────────────────────────────────────────── News Ethiopian Journal of Health Development with the assistance of University of Bergen in Norway is now available on the Internet at http://www.cih.uib.no/journals/EJHD. Go to http://www.cih.uib.no/, then click on journals and then Ethiop J Hlth Dev.

![[SENDER`S ADDRESS]](http://s3.studylib.net/store/data/007552927_2-f74ba3398a02c0a6fcf578f457395e63-300x300.png)