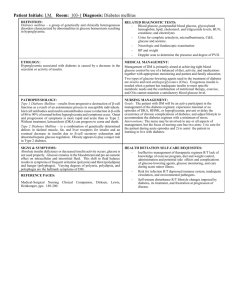
Course Outline
advertisement

Managing Diabetes and Hyperglycemia Improving Inpatient Care STATEMENT OF PURPOSE: This course consists of 7 on-line modules. Participants are asked to complete a pre-course survey and a post-test. Module 1 2 3 4 5 6 7 Topic Hyperglycemia and hospital outcomes Challenges and opportunities for care improvement Initial recognition, triaging, and management Principles of pharmacologic management: Insulin 1 Principles of pharmacologic management: Insulin 2 Review of policies and procedures Getting patients ready for discharge OBJECTIVES: After completing all 7 modules participants will: 1. Discuss the importance of controlling inpatient hyperglycemia; 2. Describe guidelines for recognizing and triaging patients with hyperglycemia; 3. Identify hyperglycemia management techniques. PREREQUISITES: None. MATERIALS NEEDED: 1. Pre-Course Survey 2. PowerPoint Presentation 3. Content Outline 4. Post Test 5. Evaluation METHOD OF PRESENTATION: Start with introduction; allow time for the pre-program survey to be completed. Review objectives, present material, provide time for post-test and evaluation to be completed. Module 3: Initial Recognition, Triaging, and Management of Hyperglycemia STATEMENT OF PURPOSE: Module 3: Module 3 is intended to provide information about phases of inpatient glucose management, how to differentiate types of hyperglycemia, and how to initiate appropriate management steps. Participants will be able to: 1. Describe the phases of inpatient glucose management 2. State the different types of hyperglycemic patients encountered in the hospital setting 3. Discuss how to initiate appropriate management steps according to type of diabetes and severity of hyperglycemia PREREQUISITES: Completion of Modules 1 and 2 MATERIALS NEEDED 1. PowerPoint Presentation 2. Content Outline 3. Post Test 4. Evaluation CONTENT Descriptions of phases of glucose management, hyperglycemic patients and initial management steps METHOD OF PRESENTATION Start with introduction. Review objectives, present material, provide time for post test and evaluation to be completed. CONTENT OUTLINE Module 3 Objectives Phases of Inpatient Hyperglycemia Care DETAIL Module 3 discusses the phases of inpatient glucose management, the types of hyperglycemic patients you will encounter in the hospital, and how to initiate appropriate glucose management. We will conceptually divide inpatient hyperglycemia care into three phases after admission. Phase 1 is the first 24 hours, Phase 2 is continued care, and Phase 3 is discharge planning. We should identify hyperglycemia as soon as possible after admission. As soon as it is identified we should initiate the treatment plan. Ongoing monitoring, education and treatment adjustment should be conducted during the continued care phase. Discharge planning starts at the time of admission. In some cases the general discharge plan will be evident (such as in the case of a newly diagnosed Type 1 or Insulin Requiring Type 2 patient who will need instruction on insulin use along with multiple other criteria during the hospital stay). In other cases the discharge plan may not be finalized until close to discharge but the patient’s instruction should be initiated as soon as possible. Begin thinking about what therapy you will prescribe for home glucose management and what follow-up care you will order. Evaluate daily the progress your patient is making in self-care skills. INSTRUCTOR’S NOTES CONTENT OUTLINE Types of Hyperglycemic Patients in the Hospital Minimum Admission Actions DETAIL INSTRUCTOR’S NOTES There are several types of hyperglycemic patients in the hospital. There are patients with pre-existing diabetes. They have a history of diabetes and may already be on pharmacotherapy. There are patients with undiagnosed diabetes. Often they have unequivocal hyperglycemia (glucose greater than or equal to 200 mg/dL) on admission. There are also patients with stress hyperglycemia. This is hyperglycemia that develops in response to the acute illness or medications. These patients require therapy during hospital stay if their blood glucose is above target range for their unit (ICU 80- Insert your hospital’s targets if 110 mg/dL, Med Surg and Peri-Op they are different. 90-140 mg/dL). Patient with diabetes or hyperglycemia, or patient who are at risk of developing hyperglycemia (For example, transplant patients, patients starting steroids, patients experiencing extreme stress) should have the following at admission as a minimum: Bedside glucose monitoring before meals, bedtime and 3AM if eating or every 6 hours if not eating. A1C if none available from past 60 days Documentation in admission note about the presence or risk of hyperglycemia Therapeutic strategy outlined Remember to include the problem CONTENT OUTLINE Initial Management Decisions Triaging Patient Without Known Diabetes DETAIL of diabetes/hyperglycemia in your problem list! Initial management decisions should be based on the type of diabetes and severity of hyperglycemia. Half of the patients with diabetes are undiagnosed. Patients without a known diagnosis of diabetes but who exhibit hyperglycemia on admission are likely to have diabetes and should be treated as such. Upon admission patients may fit into groups. The first group to consider is the one including DKA, Hyperglycemic Crisis, and Labor and Delivery. Care for these patients should include: Obtaining a recent A1C Beginning IV Insulin Protocol Hourly blood glucose monitoring Another group would include patients with no previous Diabetes diagnosis but their blood glucose is greater than or equal to 200 mg/dL. Care for these patients should include: Obtaining a recent A1C Beginning blood glucose monitoring Correction of any BG greater than 140 mg/dL with rapid acting insulin. This group may be triaged into further therapy as follows: Start basal-bolus insulin protocol and consult the diabetes education team for patients who experience INSTRUCTOR’S NOTES CONTENT OUTLINE Triaging Patients Without Known Diabetes (continued) DETAIL two consecutive bedside glucose results greater than or equal to 140 mg/dL. Continue to monitor and start correction insulin for patients who occasionally experience glucose levels 140 to 199 mg/dL. Consider basal-bolus insulin in patients such as cardiac patients. The third group includes patients with unequivocal hyperglycemia. Blood glucose levels are greater than or equal to 200 mg/dL but they do not have DKA, hyperglycemic crisis or labor. Initial Management for Patients With Known Diabetes Care for these patients should include: Obtaining a recent A1C Beginning glucose monitoring Initiation of scheduled insulin therapy Remember, all insulin deficient patients, especially Type 1 diabetes, must have insulin! First determine if the patient is insulin requiring. Type 1 or Insulin Requiring Type w or Gestational patients should be considered for this group. Treatment should include: Obtaining recent A1C Start blood glucose monitoring Continue and adjust insulin regimen Patients with non-insulin requiring Type 2 diabetes or patients with diet controlled Gestational Diabetes would be included in the other group. INSTRUCTOR’S NOTES CONTENT OUTLINE Case Scenario DETAIL If the patient was taking oral agents prior to admission, consider discontinuing them at admission if acutely ill. Obtain a recent A1C Start blood glucose monitoring Start insulin if needed Patients with no previous pharmacotherapy should have orders for: Obtaining a recent A1C Blood glucose monitoring Initiation of insulin if needed A 75 year old, lean, woman, with a five year history of diabetes is admitted for elective knee replacement. She has always needed insulin to control hyperglycemia. She is currently on short acting insulin with meals and a long acting insulin in the evening. You place her only on a sliding scale (correction) insulin program. Her blood glucoses start to rise pretty quickly into the 300’s and 400’s, and you desperately call the Endocrine service. What went wrong? She has Type 1 Diabetes and needs a basal-bolus insulin program. Not every person who develops diabetes in older years has Type 2 diabetes. Be certain to correctly classify your patient’s diabetes and never withhold basal insulin from someone with Type 1 diabetes. INSTRUCTOR’S NOTES CONTENT OUTLINE When a patient with preexisting diabetes is admitted to the hospital… Module Summary DETAIL When a patient with pre-existing diabetes is admitted to the hospital determine if the patient is insulin requiring. Type 1 Diabetes patients ALWAYS need a long acting (basal) insulin even if they are fasting. They also need meal bolus insulin based on the carbohydrate they consume at each meal. If patients are already on outpatient insulin, chances are they were on it because they needed it. At the very least keep them on basal insulin until you are sure they don’t need it. 1. Hyperglycemic inpatients are diverse. 2. Be sure you know who you are managing. 3. Identify hyperglycemic patients early. 4. Apply appropriate therapy early. INSTRUCTOR’S NOTES