Conclusions_atelectasis
advertisement

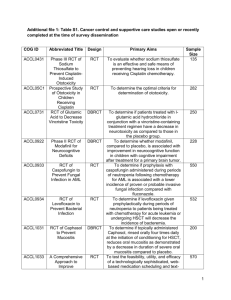
PREVENTION AND MANAGEMENT OF ATELECTASES IN INTUBATED AND VENTILATED PATIENTS RECOMMENDATIONS Recommendation 1 Post your comments on the website When volume loss is visible on CxR a CPT package of care that includes MHI; gravity assisted positioning if possible or modified position if contra indicated and suctioning might be initiated. This package should not be offered less than twice daily (Krause et al 2000) but optimally might be applied hourly for six hours (Stiller et al 1996). Post your comments Weak recommendation: Implementation of this regime provided radiographic evidence of the resolution of areas of collaps in four RCT’s (Stiller et al 1996; Krause et al 2000; Suh-Hwa Maa 2005; Crowe et al 2006). The effect of this outcome on LOS or TOV has not been established Post your comments based on low quality evidence: 4 RCT’s (Stiller et al 1996; Krause et al 2000; Suh-Hwa Maa 2005; Crowe et al 2006) providing consistent results but downgraded for imprecision and moderate risk of bias (refer to table 2). Post your comments Recommendation 2 If kinetic therapy beds are available it might be initiated routinely for unresponsive critically ill patients admitted to the unit. Post your comments Weak recommendation: The prophylactic use of kinetic beds for all patients admitted to a unit resulted in lower risk for development of ateIectasis in one RCT (Ahrens et al 2004). No effect was observed in LOS between the two groups. It is therefore unclear whether the cost of these beds can be justified in terms of savings on LOS and TOV. Post your comments based on moderate quality evidence: One RCT (Ahrens et al 2004) downgraded for moderate risk of bias (refer to table 2). Post your comments Review question: Is pulmonary physiotherapy more effective than no intervention in the prevention and or management of lobar atelectasis in intubated and ventilated patients? Following a systematic review of the literature; critical appraisal of identified studies; the following conclusions were reached: SEARCH RESULTS Six experimental studies were identified (Crowe et al 2006; Stiller et al 1996; Raoof et al 1999; Krause et al 2000; Suh-Hwa Maa 2005; Ahrens et al 2004). The interventions evaluated include a package of MHI (Crowe et al 2006; Suh-Hwa Maa et al 2005) positioning and suction (Stiller et al 1996 and Krause et al 2000) and kinetic therapy (Raoof et al 1999; Ahrens et al 2004). Five studies investigated the management of patients where atelectasis was already diagnosed (Crowe et al 2006; Stiller et al 1996; Raoof et al 1999; Krause et al 2000; Suh-Hwa Maa 2005). Only one study were identified that evaluated the prevention of atelectasis (Ahrens et al 2004) None of the studies compared the intervention to a non intervention control. SUMMARY OF EVIDENCE A package of care should include at least MHI; gravity assisted positioning (modified if contra indicated) and suctioning in patients where volume loss is visible on CxR (Stiller et al 1996; Krause et al 2000; Suh-Hwa Maa et al 2005). The addition of manual techniques in the management of atelectasis is not supported at this time (Stiller et al 1996; Raooff et al 1999) Patients should receive a minimum frequency of two treatment sessions daily (Krause et al 2000) with ideal frequency hourly for at least six hours (Stiller et al 1996). If available, kinetic therapy could be instituted for all patients admitted to a unit to prevent atelectasis (Ahrens et al 2004). Table 1 Summary of experimental studies identified Studies Internal validity (Pedro Score) 7 Sample size Population Intervention and comparison Study structure Outcome measured 35 Patients (intubated and non intubated) in ICU presenting with acute lobar atelectasis as observed on CxR. Factoral RCT Mean percentage resolution compared to first picture Raoof et al 1999 7 24 RCT Krause et al 2000 7 17 Respiratory failure & evidence of atelectasis on X-rays Intubated patients lobar atelectasis as observed on CxR MHI; suction compared to MHI; MPD position; vibration and suction compared to MHI; MPD position; suction compared to MHI; MPD position; suction hourly for 6 hours compared to MHI; MPD position; suction once daily Kinetic therapy compared to two hourly manual turn and percussion PD position; vibration; suction compared to modified PD position; vibration; suction Ahrens et al 2004 Suh-Hwa Maa 2005 Crowe et al 2006 8 234 4 23 multicenter RCT multicenter RCT 7 20 Kinetic therapy compared to two hourly turn by nursing MHI and standard CPT (MPD position;vibration;suction) compared to standard CPT MHI (Breath stacking) and standard CPT (MPD position;vibration;suction) compared to standard CPT (MPDposition;vibration;suction) Extent of Atelectasis vissible on CxR segmental; lobar etc Number of treatments needed for complete resolution of atelectasis vissible on CxR Atelectasis vissible on CxR (Yes or No) Improvement vissible on CxR (Yes or No) Stiller et al 1996 Intubated GCS <11; PaO2:FiO2 <250 >40 intubated > 7 days clinical diagnosis atelectasis Intubated with unilateral or bilat CxR diagnosis of atelectasis RCT RCT mean radiology score based on predetermined score SUMMARY OF THE QUALITY OF THE EVIDENCE All the studies included in this review accepted that some intervention (physiotherapy or positional changes) is indicated for the management of intubated patients in ICU. A modified postural drainage position (MPD) was used in four RCT’s evaluating specific CPT techniques (Crowe et al 2006; Stiller et al 1996; Krause et al 2000; Suh-Hwa Maa 2005). One RCT reported a more rapid resolution when using a gravity assisted drainage position compared to the standard (Krause et al 2000). The quality of this evidence is downgraded to low quality due to methodological quality and imprecision of data and sample (refer to table 2). The addition of MHI to a standard protocol of position and suction was specifically investigated in 3 RCT’s (Crowe et al 2006; Stiller et al 1996; Suh-Hwa Maa 2005). Data could not be pooled because different outcomes had been measured. The addition of MHI improved radiological evidence of atelectases in two RCT’s (Stiller et al 1996; Suh-Hwa Maa 2005) and had no effect in one study (Crowe et al 2006). The quality of the evidence (from the two studies) is downgraded to low quality evidence due to poor methodological quality and imprecision of data and sample (refer to table 2). The frequency of the physiotherapy intervention used in two RCT’s was twice daily (Crowe et al 2006; Krause et al 2000). An increased frequency of hourly intervention for 6 hours compared to a once daily intervention reported a significant improved resolution on CxR (Stiller et al 1996). The quality of this evidence is downgraded to low quality due to methodological quality and imprecision of data and sample (refer to table 2). One study multicentre RCT reported a significant reduction in the incidence of atelectasis (Ahrens et al 2004). The quality of this evidence is downgraded to moderate quality for methodological quality (refer to table 2). Table 2 Factors considered in determining the quality of the evidence Experimental Studies Risk of bias Heterogeneity Directness of evidence Concealed allocation LTFO Stiller et al 1996 No Raoof et al 1999 Precision ITT Intervention investigated Sample investigated Publication Bias Data Sample Yes No Yes NA Yes Yes Yes Krause et al 2000 No Yes Yes Yes Yes NA Ahrens et al 2004 Suh-Hwa Maa 2005 No Yes Yes Yes Yes NA No No No Yes NA Crowe et al 2006 Yes Yes Yes Yes No (pt intubated > 7 days Yes Insufficient data to calculate size of treatment effect No OR 8.57(CI0.8387.83) Insufficient data to calculate size of treatment effect Yes OR 0.44 (CI 0.23 – 0.85) No OR 10.5 (CI 0.83 – 87.83) No Yes No (included intubated and non intubated pt) Yes Insufficient data to calculate size of treatment effect No Lost to follow up NA NA No No Yes No