Basics of internal Medicine
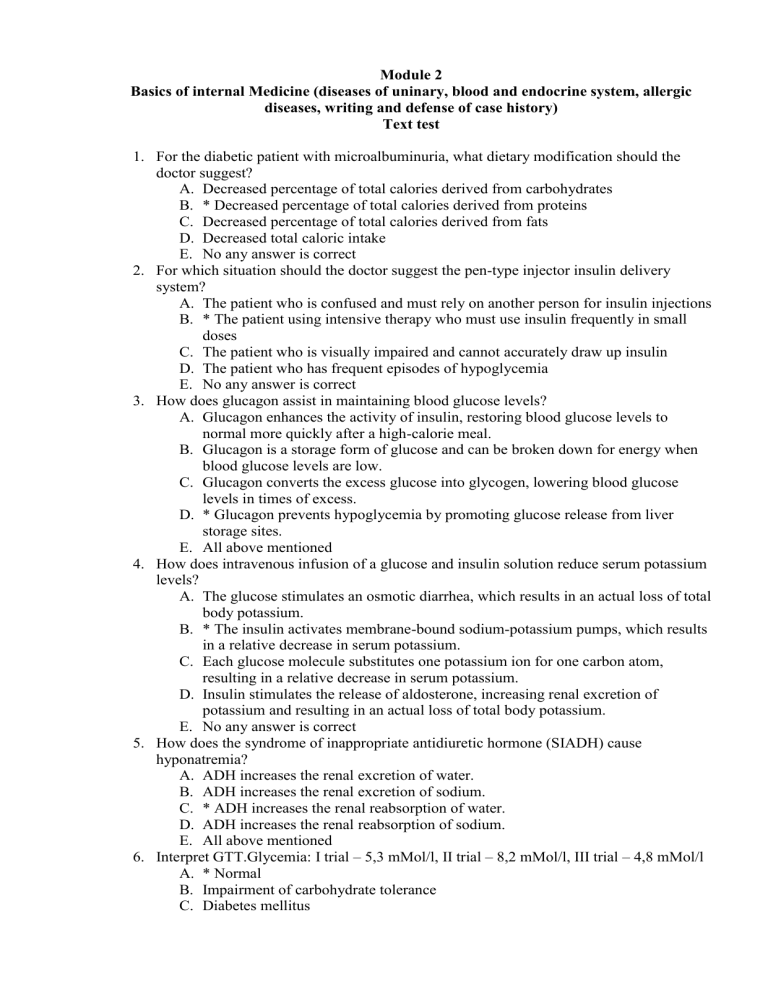
Module 2
Basics of internal Medicine (diseases of uninary, blood and endocrine system, allergic diseases, writing and defense of case history)
Text test
1.
For the diabetic patient with microalbuminuria, what dietary modification should the doctor suggest?
A.
Decreased percentage of total calories derived from carbohydrates
B.
* Decreased percentage of total calories derived from proteins
C.
Decreased percentage of total calories derived from fats
D.
Decreased total caloric intake
E.
No any answer is correct
2.
For which situation should the doctor suggest the pen-type injector insulin delivery system?
A.
The patient who is confused and must rely on another person for insulin injections
B.
* The patient using intensive therapy who must use insulin frequently in small doses
C.
The patient who is visually impaired and cannot accurately draw up insulin
D.
The patient who has frequent episodes of hypoglycemia
E.
No any answer is correct
3.
How does glucagon assist in maintaining blood glucose levels?
A.
Glucagon enhances the activity of insulin, restoring blood glucose levels to normal more quickly after a high-calorie meal.
B.
Glucagon is a storage form of glucose and can be broken down for energy when blood glucose levels are low.
C.
Glucagon converts the excess glucose into glycogen, lowering blood glucose levels in times of excess.
D.
* Glucagon prevents hypoglycemia by promoting glucose release from liver storage sites.
E.
All above mentioned
4.
How does intravenous infusion of a glucose and insulin solution reduce serum potassium levels?
A.
The glucose stimulates an osmotic diarrhea, which results in an actual loss of total body potassium.
B.
* The insulin activates membrane-bound sodium-potassium pumps, which results in a relative decrease in serum potassium.
C.
Each glucose molecule substitutes one potassium ion for one carbon atom, resulting in a relative decrease in serum potassium.
D.
Insulin stimulates the release of aldosterone, increasing renal excretion of potassium and resulting in an actual loss of total body potassium.
E.
No any answer is correct
5.
How does the syndrome of inappropriate antidiuretic hormone (SIADH) cause hyponatremia?
A.
ADH increases the renal excretion of water.
B.
ADH increases the renal excretion of sodium.
C.
* ADH increases the renal reabsorption of water.
D.
ADH increases the renal reabsorption of sodium.
E.
All above mentioned
6.
Interpret GTT.Glycemia: I trial – 5,3 mMol/l, II trial – 8,2 mMol/l, III trial – 4,8 mMol/l
A.
* Normal
B.
Impairment of carbohydrate tolerance
C.
Diabetes mellitus
D.
Necessary to repeat test
E.
Necessary to order additional laboratory tests.
7.
Macroangiopathy, as a symptom of diabetes mellitus, most often destroy vessels of:
A.
* Brain
B.
Lung
C.
Kidneys
D.
Retina
E.
Intestine
8.
The 45-year-old diabetic patient has proliferative retinopathy, nephropathy, and peripheral neuropathy. What should the doctor teach this patient about exercise?
A.
“The type of exercise that would most efficiently help you to lose weight, decrease insulin requirements, and maintain cardiovascular health would be jogging for 20 minutes 4 to 7 days each week.”
B.
“Considering the complications you already have, vigorous exercise for an hour each day is needed to prevent progression of disease.”
C.
“Considering the complications you already have, you should avoid engaging in any form of exercise.”
D.
* “Swimming or water aerobics 30 minutes each day would be the safest exercise routine for you.”
E.
No any answer is correct
9.
The patient diabetic patient asks the doctor why it is necessary to maintain blood glucose levels no lower than about 74 mg/dL. What is the doctor’s best response?
A.
“Glucose is the only fuel form used by body cells to produce energy needed for physiologic activity.”
B.
* “The central nervous system, which cannot store glucose, requires a continuous supply of glucose for fuel.”
C.
“Without a minimum level of glucose circulating in the blood, erythrocytes cannot produce ATP.”
D.
“The presence of glucose in the blood counteracts the formation of lactic acid and prevents acidosis.”
E.
No any answer is correct
10.
The patient who has used insulin for diabetes control for 20 years has a spongy swelling at the site used most frequently for insulin injection. What is the doctor’s best action?
A.
Apply ice to this area.
B.
Document the finding as the only action.
C.
Assess the patient for other signs of cellulitis.
D.
* Instruct the patient to use a different site for insulin injection.
E.
No any answer is correct
11.
The patient with diabetes is visually impaired and wants to know if syringes can be prefilled and stored for use later. What is the doctor’s best response?
A.
* “Yes, prefilled syringes can be stored for up to 3 weeks in the refrigerator in a vertical position with the needle pointing up.”
B.
“Yes, prefilled syringes can be stored for up to 3 weeks in the refrigerator, placed in a horizontal position.”
C.
“Insulin reacts with plastic, so prefilled syringes must be made of glass.”
D.
“No, insulin cannot be stored for any length of time outside of the container.”
E.
No any answer is correct
12.
The patient with diabetes who is just starting on insulin therapy wants to know why more than one injection of insulin each day will be required. What is the doctor’s best response?
A.
“You need to start with multiple injections until you become more proficient at self-injection.”
B.
* “A single dose of insulin each day would not match your blood insulin levels and your food intake patterns closely enough.”
C.
“A regimen of a single dose of insulin injected each day would require that you could eat no more than one meal each day.”
D.
“A single dose of insulin would be too large to be absorbed predictably, so you would be in danger of unexpected insulin shock.”
E.
No any answer is correct
13.
The patient with hypokalemia requires a diuretic for another health problem. Which agent should the doctor be prepared to administer?
A.
Furosemide (Lasix)
B.
Bumetanide (Bumex)
C.
Chlorothiazide (Diuril)
D.
* Spironolactone (Aldactone)
E.
No any answer is correct
14.
The patient with type 1 diabetes has a blood glucose level of 160 mg/dL on arrival at the operating room. What is the doctor’s best action?
A.
* Document the finding as the only action.
B.
Administer regular insulin.
C.
Cancel the surgery.
D.
Notify the physician.
E.
No any answer is correct
15.
Three hours after surgery, the doctor note that the breath of the patient who is a type 1 diabetic has a “fruity” odor. What is the doctor’s best first action?
A.
Document the finding as the only action.
B.
Increase the IV fluid flow rate.
C.
* Test the urine for ketone bodies.
D.
Perform oral care.
E.
All above mentioned
16.
What effect can moderate to severe hypokalemia have on digoxin therapy?
A.
Hypokalemia increases the excretion rate of digoxin; therefore, digoxin must be given twice each day.
B.
Hypokalemia increases the half-life of digoxin; therefore, digoxin must be given every other day.
C.
* Hypokalemia increases the sensitivity of excitable membranes to digoxin; therefore, toxic effects may occur with normal doses.
D.
Hypokalemia decreases the sensitivity of excitable membranes to digoxin; therefore, higher doses of digoxin are required to achieve a therapeutic effect.
E.
All above mentioned
17.
What intervention is most important to teach the patient at risk for hypercalcemia?
A.
“Avoid drinking coffee and other caffeinated beverages.”
B.
* “Be sure to drink at least 3 liters of fluids each day.”
C.
“Do not eat or drink any dairy products.”
D.
“Take at least one 2-hour nap per day.”
E.
No any answer is correct
18.
What intervention should the doctor suggest to the diabetic patient who self-injects insulin to prevent or limit local irritation at the injection site?
A.
“Do not reuse needles.”
B.
“Massage the site for 1 full minute after injection.”
C.
“Try to make the injection deep enough to enter muscle.”
D.
* “Allow the insulin to warm to room temperature before injection.”
E.
No any answer is correct
19.
What intervention should the doctor teach the patient with diabetes who uses an insulin infusion pump to prevent the complication of infection?
A.
“Test your urine daily for the presence of ketone bodies.”
B.
“Use buffered insulin to prevent crystal formation.”
C.
“Keep the insulin frozen until you fill the pump.”
D.
* “Change the needle every 3 days.”
E.
All above mentioned
20.
What is the basic underlying pathology of diabetes mellitus?
A.
A disruption of the cellular glycolytic pathway
B.
* An inability of the liver to catabolize glycogen
C.
A failure to synthesize and/or utilize insulin
D.
An inhibition of the conversion of protein to amino acids
E.
No any answer is correct
21.
What is the basic underlying pathology of diabetes mellitus?
A.
A disruption of the cellular glycolytic pathway
B.
An inability of the liver to catabolize glycogen
C.
* A failure to synthesize and/or utilize insulin
D.
An inhibition of the conversion of protein to amino acids
E.
No any answer is correct
22.
What is the physiologic basis for the polyuria manifested by individuals with untreated diabetes mellitus?
A.
Inadequate secretion of antidiuretic hormone (ADH)
B.
Early-stage renal failure causing a loss of urine concentrating capacity
C.
Chronic stimulation of the detrusor muscle by the ketone bodies in the urine
D.
* Hyperosmolarity of the extracellular fluids secondary to hyperglycemia
E.
No any answer is correct
23.
What is the priority intervention for the patient having Kussmaul respirations as a result of diabetic ketoacidosis?
A.
Administration of oxygen by mask or nasal cannula
B.
Intravenous administration of 10% glucose
C.
Implementation of seizure precautions
D.
* Administration of intravenous insulin
E.
All above mentioned
24.
What is the priority nursing diagnosis for a patient with long-standing hypocalcemia?
A.
Ineffective Breathing Pattern related to muscle weakness
B.
Risk for Infection related to immunosuppression
C.
* Risk for Injury related to bone demineralization
D.
Fatigue related to malnutrition and anemia
E.
No any answer is correct
25.
What is the priority nursing intervention for a patient with moderate to severe hypernatremia?
A.
Restricting fluid intake
B.
* Initiating seizure precautions
C.
Weighing the patient daily at the same time of day
D.
Assessing pulse oximetry and respiratory status every hour
E.
No any answer is correct
26.
What is the priority teaching intervention for the patient with chronic hypophosphatemia?
A.
Where to find the radial pulse and what qualities to note
B.
How to intersperse daily activities with periods of rest
C.
* How to select foods high in phosphorus and avoid foods with high concentrations of calcium.
D.
The importance of weighing himself or herself daily at the same time each day and wearing the same amount of clothing.
E.
All above mentioned
27.
What pathologic process is most likely occurring in a patient who has a serum sodium level of 122 mEq/L and a serum potassium level of 6.6 mEq/L?
A.
* Adrenal insufficiency
B.
Chronic renal failure
C.
Cushing’s syndrome
D.
SIADH
E.
No any answer is correct
28.
When taking the blood pressure of a very ill patient, the doctor observes that the patient's hand undergoes flexion contractions. What is the doctor’s best first action?
A.
Place the patient in the high-Fowler's position and increase the IV flow rate.
B.
* Deflate the blood pressure cuff and give the patient oxygen.
C.
Document the finding as the only action.
D.
Notify the emergency team.
E.
No any answer is correct
29.
Which action should the doctor suggest to reduce insulin needs in the patient with diabetes mellitus?
A.
Reducing intake of water and other liquids to no more than 2 L/day
B.
Eating animal organ meats high in insulin
C.
Taking two 1-hour naps daily
D.
* Walking 1 mile each day
E.
No any answer is correct
30.
Which action should the doctor suggest to the patient who has been having difficulty with hypoglycemia to decrease the rate of insulin absorption from the injection site?
A.
Massaging the injection site
B.
Exercising within 1 hour of insulin injection
C.
Injecting into muscle rather than subcutaneous tissue
D.
* Using refrigerated insulin without warming it to room temperature
E.
All above mentioned
31.
Which action should the doctor teach the diabetic patient as being most beneficial in delaying the onset of microvascular and macrovascular complications?
A.
* Controlling hyperglycemia
B.
Preventing hypoglycemia
C.
Restricting fluid intake
D.
Preventing ketosis
E.
No any answer is correct
32.
Which alteration in psychosocial functioning should alert the doctor to the possibility of hypokalemia?
A.
Anxiety
B.
Insomnia
C.
* Confusion
D.
Combative behavior
E.
All above mentioned
33.
Which assessment finding in the patient with diabetes mellitus indicates that the disease is damaging the kidneys?
A.
The presence of ketone bodies in the urine during acidosis
B.
The presence of glucose in the urine during hyperglycemia
C.
* The presence of protein in the urine during a random urinalysis
D.
The presence of white blood cells in the urine during a random urinalysis
E.
No any answer is correct
34.
Which change in clinical manifestations in a patient with long-standing diabetes mellitus alerts the doctor to the possibility of renal dysfunction?
A.
Loss of tactile perception
B.
The presence of glucose in the urine
C.
The presence of ketone bodies in the urine
D.
* A sustained increase in blood pressure from 130/84 to 150/100
E.
No any answer is correct
35.
Which patient is at greatest risk for developing hypercalcemia?
A.
The patient taking digoxin and a high-ceiling diuretic (Lasix) for heart failure
B.
The patient with long-standing osteoarthritis
C.
The patient who is pregnant with twins
D.
* The patient with hyperparathyroidism
E.
No any answer is correct
36.
Which patient is at greatest risk for hypokalemia?
A.
65-year-old with diabetes mellitus
B.
55-year-old with Addison’s disease
C.
* 45- year-old with Cushing’s disease
D.
35-year-old with diabetes insipidus
E.
No any answer is correct
37.
Which patient is at greatest risk for the development of hyperphosphatemia?
A.
* 27-year-old man undergoing chemotherapy for lymphoma
B.
45- year-old man taking Tums for chronic acid indigestion
C.
21-year-old man recovering from a fractured tibia that has been pinned
D.
36-year-old woman taking thyroid hormone replacement after a thyroidectomy
E.
No any answer is correct
38.
Which clinical manifestation in a patient with uncontrolled diabetes mellitus should the doctor expect as a result of the presence of ketoacid in the blood?
A.
* Increased rate and depth of respiration
B.
Extremity tremors followed by seizure activity
C.
Oral temperature of 102° F (38.9° C)
D.
Severe orthostatic hypotension
E.
All above mentioned
39.
Which clinical manifestation indicates to the doctor that the therapy for the patient with hyperglycemic, hyperosmolar, nonketotic syndrome (HHNS) needs to be adjusted?
A.
The patient's serum potassium level increased from 2.8 mEq/L to 3.2 mEq/L.
B.
The patient's blood osmolarity has decreased from 350 mOsm to 330 mOsm.
C.
* The patient's score on the Glasgow Coma Scale is unchanged from 3 hours ago.
D.
The patient's urine has remained negative for ketone bodies for the past 3 hours.
E.
No any answer is correct
40.
Which intervention for self-monitoring of blood glucose levels should the doctor teach the patient with diabetes to prevent bloodborne infections?
A.
“Wash your hands before beginning the test.”
B.
* “Do not share your monitoring equipment.”
C.
“Blot excess blood from the strip.”
D.
“Use gloves during monitoring.”
E.
All above mentioned
41.
Which intravenous solution should the doctor be prepared to administer to a patient with a serum sodium level of 120 mEq/L and a serum potassium level of 4.3 mEq/L?
A.
0.45% saline
B.
0.9% saline
C.
* 2% saline
D.
Ringer's lactate
E.
No any answer is correct
42.
Which nutritional group should the doctor teach the diabetic patient with normal renal function to rigidly control to reduce the complications of diabetes?
A.
* Fats
B.
Fiber
C.
Proteins
D.
Carbohydrates
E.
No any answer is correct
43.
Which nutritional problem should the doctor be more alert for in older adult patients with diabetes mellitus?
A.
Obesity
B.
* Malnutrition
C.
Alcoholism
D.
Hyperglycemia
E.
No any answer is correct
44.
Which protein source should the doctor recommend for a patient who needs to restrict dietary potassium intake?
A.
Raw broccoli
B.
Grilled salmon
C.
* Poached eggs
D.
Baked chicken
E.
All above mentioned
45.
Which question is most important for the doctor to ask the patient who has been diagnosed with hypokalemia to identify a possible cause for the imbalance?
A.
“Do you use sugar substitutes?”
B.
* “Do you use diuretics or laxatives?”
C.
“Have you or any member of your family been diagnosed with kidney disease?”
D.
“Have you noticed any changes in your pattern of bowel elimination during the last month?”
E.
No any answer is correct
46.
Which statement made by the diabetic patient who has a urinary tract infection indicates correct understanding regarding antibiotic therapy?
A.
“If my temperature is normal for 3 days in a row, the infection is gone and I can stop taking my medicine.”
B.
“If my temperature goes above 100° F (37.8° C) for 2 days, I should take twice as much medicine.”
C.
* “Even if I feel completely well, I should take the medication until it is gone.”
D.
“When my urine no longer burns, I will no longer need to take the antibiotics.”
E.
No any answer is correct
47.
Which statement regarding diabetes mellitus is true?
A.
Diabetes increases the risk for development of epilepsy.
B.
The cure for diabetes is the administration of insulin.
C.
* Diabetes increases the risk for development of cardiovascular disease.
D.
Carbohydrate metabolism is disturbed in diabetes, but protein and lipid metabolism are normal.
E.
All above mentioned
48.
Which subjective symptom reported by the patient should alert the doctor to the possibility of hypocalcemia?
A.
“I have a bowel movement only every 2 to 3 days.”
B.
* “Usually I wake up several times a night with painful cramps in my legs or feet.”
C.
“My rings and shoes are much tighter fitting at night than they are in the morning.”
D.
“I notice that my heart seems to pound whenever I climb steps or drink a cup of coffee.”
E.
No any answer is correct
49.
While assessing the patient who has had diabetes for 15 years, the doctor notes that the patient has decreased tactile sensation in both feet. What is the doctor’s best first action?
A.
Document the finding as the only action.
B.
Test sensory perception in the patient's hands.
C.
* Examine the patient's feet for signs of injury.
D.
Notify the physician.
E.
No any answer is correct
50.
Why is ketosis rare in patients with type 2 diabetes, even when blood glucose levels are very high (higher than 900 mg/dL)?
A.
Ketosis is less prevalent among obese adults.
B.
People with type 2 diabetes have normal lipid metabolism.
C.
* There is enough insulin produced by type 2 diabetes to prevent fat catabolism but not enough to prevent hyperglycemia.
D.
Oral antidiabetic agents do not promote the breakdown of fat for fuel (lipolysis), and exogenous insulin spares carbohydrates at the expense of fats.
E.
No any answer is correct
51.
With which therapy for diabetes mellitus is the patient not at risk for hypoglycemia?
A.
Regular insulin
B.
Lente insulin
C.
* Biguanides
D.
Sulfonylureas
E.
No any answer is correct
52.
Excretion of which metabolites causes hypercreatininemia?
A.
* Proteins metabolites
B.
Carbohydrates metabolites
C.
Fats metabolites
D.
All mentioned
E.
Uric acid salts
53.
What is the purpose of Nechyporenko’s test execution?
A.
to reveal which part of urinary system is the source of hematuria or leukocyturia,
B.
estimation of kidney concentration function
C.
* for calculation of formed elements (red cells, leukocytes, casts) in urine with the method of Kakovsky-Addis
D.
for determination of diuresis
E.
for determination of the amount of albumen in urine.
54.
Which is main drug for treatment of acute glomerulonephritis?
A.
Antibiotics
B.
* Glucocoricoids
C.
Immunodepressants
D.
Diuretics
E.
Calcium channel antagonists
55.
Which is main drug for treatment of acute pyelonephritis?
A.
* Antibiotics
B.
Glucocortecoids
C.
Immunodepressants
D.
Diuretics
E.
Calcium channel antagonists
56.
Which laboratory test is useful for assessment kidney concentration function?
A.
Complete blood count;
B.
ECG;
C.
Nechiporenko’s test;
D.
* Zimnicki’s test
E.
determination of daily proteinuria.
57.
According to location of pathological process chronic pyelonephritis may be:
A.
Unilateral
B.
Bilateral
C.
Pyelonephritis of a single kidney
D.
No correct answer
E.
* All enumerated
58.
Anticoagulants are prescribed in the following curse of glomerulonephritis:
A.
With uric syndrome
B.
With uric syndrome and hematuria
C.
In resistant hypertension
D.
* With nephrotic syndrome
E.
With acute nephritic syndrome
59.
For patient A., who sufers of chronic glomerulonephritis, it was found out violation of kidneys concentration function. Which pathological changes in kidneys cause renal failure in this disease?
A.
* glomerular sclerosis
B.
edema of kidney parenchyma
C.
canalicular sclerosis
D.
obstruction of canaliculi with destroyed erythrocytes
E.
collaps of tubes.
60.
For patient E., 52 years old, ill with chronic pyelonephritis for 12 yers, biochemical blood test is conducted. What changes can be when the patient has renal failure?
A.
increase of glucose level in blood;
B.
increase of bilirubin;
C.
* increase of creatinine;
D.
increase of amylaze
E.
increase of alkaline phosphatase.
61.
For patient I., 54 years old, paranephritis is diagnosed. What position does patient with paranephritis assume?
A.
* On affected side with legs bended hip and knee joints and by the leg pressed to the stomach from the side of affection
B.
Semirecumbent position with lowered legs (orthopnoe)
C.
Lying on a sick side
D.
Knee-elbow position
E.
Sitting, bending forward.
62.
Un patient I., 54 y.o., paranephritis is diagnosed. What is this?
A.
* Inflammation of tissueds surrounding the kidney
B.
Inflammation of a bladder
C.
Inflammation of kidney calicies
D.
Inflammation of kidney parenchyma
E.
Inflammation of peritoneum surrounding the kidney
63.
For the patient of 43 y.o.., in the urinalysis it is found out the changed red cells. What is appearance in urine of the changed red corpuscles related to?
A.
* acute nephritis;
B.
urolithiasis;
C.
acute cystitis;
D.
kidney amyloidosis;
E.
the cancer of urinary bladder.
64.
For treatment of primary acute pyelonephritis all the following drugs are used except of:
A.
Ampicillin
B.
Palin
C.
Biseptol
D.
Nevigramon
E.
* prednisolon
65.
For treatment of primary acute pyelonephritis sre used:
A.
* Antibiotics, sulfa drugs, uroseptics, phitodiuretics
B.
sulfa drugs, spasmolythics
C.
Antibiotics, uroseptics, hemostatics
D.
Antibiotics, spasmolythics, phitodiuretics
E.
sulfa drugs, spasmolythics, vitamina
66.
For treatment of pyelonephritis all the following drugs are used except of:
A.
Antibiotics
B.
uroseptics
C.
Preparations which improve urine outflow
D.
Nonsteroid anti-inflammatory agents
E.
* prednisolon
67.
For treatment of pyelonephritis it is necessary to prescribe:
A.
uroseptics
B.
Preparations which improve urine outflow
C.
Nonsteroid anti-inflammatory agents
D.
Antibiotics
E.
* all mentioned
68.
For what purpose Tompson’s test is performed (tree-glass test)?
A.
* for the exposure of department of the urinary system, which is the source of hematuria or leukocyturia,
B.
estimation of kidney concentration function
C.
for calculation of formed elements (red cells, leukocytes, casts) in urine with the method of Kakovsky-Addis
D.
for determination of diuresis
E.
for determination of the amount of albumen in urine.
69.
For which period of time is it necessary to prescribe a bed mode for a patient with acute glomerulonephritis?
A.
Till disappearance of uric syndrome
B.
On 1-3 days
C.
* Till disappearance of edema and normalization of blood pressure
D.
On 3-5 days
E.
On 10-14 days
70.
How is pain called caused by kidney block with a stone?
A.
* Urocolick
B.
Biliary colick
C.
Intestinal colick
D.
Spasmodic pain
E.
Dull boring pain
71.
How many nephrons for a healthy man are counted in both kidneys:
A.
200 southants.;
B.
* 3 millions.;
C.
10 millions.;
D.
2,5 millions.;
E.
1 million
72.
Hypertonic type of chronic glomerulonephritis is manifested with:
A.
Normal blood pressure (BP) and uric syndrome
B.
High BP
C.
Edema and uric syndrome
D.
* High BP and edema
E.
Total edema
73.
In a patient with disease of kidney pericardial friction sound is heard. Which condition is it typical for?
A.
Myocarditis
B.
Rheumatic attack
C.
* chronic renal failure
D.
Ischemic heart disease
E.
hypertension
74.
In acute pyelonephritis in urine sediments may be found:
A.
* Protein and erythrocytes
B.
Protein and uric acid salts crystals
C.
Leucocytes
D.
Leucocytes and hyaline casts
E.
Erythrocytes and calcium oxalatis crystals
75.
In pathogenesis of chronic glomerulonephritis the most important role belongs to:
A.
Inflammation
B.
* Authoimmune process
C.
Immune disorders
D.
Disorders of hemostasis
E.
Liver disease
76.
In patient E., 42 years old., who is ill with chronic glomerulonephritis for 8 years, complaints of headache, nausea, vomiting, itch of skin and rash on it. Creatinine level is
2,18 mmol/l. Which type of rash is typical for renal failure?
A.
* hemorrhagic (petechia and echymoses)
B.
allergic erythema
C.
papulopustular
D.
herpes zoster
E.
Sarcoma Caposhi
77.
In patient E., 42 years old., who is ill with chronic glomerulonephritis for 8 years, complaints of headache, nausea, vomiting, itch of skin and rash on it, gingival bleeding.
Creatinine level is 2,18 mmol/l. What is thr cause of bleeding?
A.
* Decreased blood coagulation because of toxic affection of bone marrow
B.
Increased permeability of vessels
C.
gingivitis
D.
stomatitis
E.
no correct answer
78.
In patient’s urianalyses there were found casts, leucocyturia, bacteriuria and proteinuria.
Which disease is this typical for?
A.
Paranephritis
B.
Acute glomerulonephritis
C.
* pyelonephritis
D.
Amyloidosis
E.
Kidney cancer
79.
In urine of the patient of 43 years old, it were found out crystals of solts . What they indicate on?
A.
acute nephritis;
B.
* urolithiasis;
C.
acute cystitis;
D.
kidney amyloidosis;
E.
cancer of urinary bladder.
80.
In which age pyelonephritis usually develop in women?
A.
In childhood
B.
In young age
C.
* In moderate age
D.
In declining years
E.
In elderly people
81.
In which disease nicturia may be present?
A.
Acute nephritis
B.
Diabetes mellitus
C.
* Chronic renal failure
D.
Chronic liver failure
E.
Diencephalic syndrome
82.
In which kidney disease may be convulsions?
A.
Urocolick attack
B.
* Renal eclampsia
C.
Kidney tuberculosis
D.
Tumor of a kidney
E.
Glomerulonephritis
83.
Indicate a disease which most often is complicated with chronic pyelonephritis:
A.
* Diabetic nephropathy
B.
Paraneoplastic nephropathy
C.
Amyloidosis
D.
Chronic interstitial nephritis
E.
Kidney polyscystosis
84.
Main laboratory sign of pyelonephritis:
A.
Large amount of casts
B.
Lipiduria
C.
* Prevalence of leucocyturia against of erythrocyturia
D.
Prevalence of erythrocyturia against of leucocyturia
E.
Proteinuria more than 2 g per day
85.
Main principle of chromic pyelonephritis:
A.
To avoid overcooling
B.
* To remove disorders of urine outflow
C.
Sanation of focci of infection
D.
To avoid sulfa drugs
E.
Usage of adequate volume of liquid
86.
Most often the causative agent of acute glomerulonephritis is:
A.
* Hemolythic streptococcus group A
B.
Viruses
C.
Staphylococci and pneumococci
D.
E. Coli
E.
Fungi
87.
Most often the causative agent of acute pyelonephritis is:
A.
* E. Coli
B.
Proteus
C.
Streptococcus
D.
Viruses
E.
Chlamidia
88.
Pathogenesis of arterial hypertension in kidney diseases is the following:
A.
* increased production of renin
B.
transformation of angiotensinogen in angiotensin II
C.
decreased production of prostaglandin
D.
replacement of natrium ions inside cells
E.
increased production of renin
89.
Patient A., 35 y.o.., handed over urine on an analysis. The table of contents of what matter in urine considerably does promote it specific gravity?
A.
Uric acid salts;
B.
oxalates;
C.
bilious pigments;
D.
* glucose;
E.
uric acid.
90.
Patient E., 38 years old, complains of attack-like pains in lumbar area, which irradiate downward. What does can this symptom testify about?
A.
acute glomerulonephritis;
B.
* urolithiasis;
C.
hypernephroma;
D.
chronic glomerulonephritis;
E.
heart attack.
91.
Patient T., 48 years old, has an attack of kidney eclampsia. What will not be characteristically for this state?
A.
Convulsions
B.
* Eyeballs are soft
C.
Swellings of neck veins
D.
Pupils are dilated and irresponsive on light
E.
Smell from a mouth
92.
Patient F., 38 years old ., developed acute pyelonephritis. What appearance of urine mis typical for the disease?
A.
red;
B.
color of «meat wastes»;
C.
color of beer;
D.
* cloudy, with white sediment
E.
straw-yellow.
93.
Primary urine appears for a healthy man:
A.
* in glomerulis;
B.
in the proximal department of tubulis;
C.
in a distal department;
D.
in the loop of Genle;
E.
in glomerulis and proximal department of tubulis.
94.
Progression of chronic glomerulonephritis is usually caused by:
A.
Infection
B.
* Hemodynamic changes in glomeruli
C.
Immune disorders
D.
disorders of urine outflow
E.
hyperurikemia
95.
Provoking factors of pyelonephritis:
A.
* severe diseases
B.
Focuses of infection in the organism
C.
Immune deficiency state
D.
Acute cystitis
E.
All mentioned
96.
Reberg’s test is performed with the purpose:
A.
to reveal which part of urinary system is the source of hematuria or leukocyturia,
B.
* estimation of kidney concentration function
C.
for calculation of formed elements (red cells, leukocytes, casts) in urine with the method of Kakovsky-Addis
D.
for determination of diuresis
E.
for determination of the amount of albumen in urine.
97.
Select complication of acute glomerulonephritis:
A.
* Acute renal failure
B.
Chronic renal failure
C.
Toxic shock
D.
Bleeding
E.
All mentioned
98.
Select complication of chronic glomerulonephritis:
A.
Acute renal failure
B.
* Chronic renal failure
C.
Toxic shock
D.
Bleeding
E.
All mentioned
99.
Select complication of chronic glomerulonephritis:
A.
Acute renal failure
B.
Chronic renal failure
C.
Toxic shock
D.
Bleeding
100.
E.
* Hypertonic crisis
Select the method of assessment of urine outflow disorders in pyelonephritis of pregnant women:
A.
Excretory urography
B.
Chromocystoscopy
C.
Ultrasound
D.
* Ultrasound, chromocystoscopy
101.
E.
Radioisotopic renography
Select the most informative method of diagnostics of acute secondary pyelonephritis:
A.
* X- ray and ultrasound
B.
Laboratory tests
C.
Ultrasound
D.
Chromocystoscopy
102.
E.
Radioisotopic renography
Sick E., 48 y.o.is ill with chronic pyelonephritis for 10 years. What changes in biochemical blood test do testify to kidney insufficiency?
A.
albuminemia;
B.
beta-lipoproteinemia;
C.
hyperbilirubinemia;
D.
* kreatiniemia
E.
dysproteinemia.
103.
Sick O., 39 years old., complains of nicturia. What pathology is this symptom typical for?
A.
acute nephritis;
B.
diabetes mellitus;
C.
* chronic kidney insufficiency;
D.
chronic cardiac insufficiency;
104.
105.
106.
107.
108.
109.
110.
111.
112.
E.
diencephalic syndrome.
The main difference between primary and secondary chronic pyelonephritis:
A.
Diabetes mellitus
B.
tonsillitis, caries
C.
chronic prostatitis
D.
decreased immune reactivity
E.
* disorders of urine outflow
The most often complication of acute pyelonephritis is:
A.
Hypotension
B.
Hypertension
C.
Acute renal failure
D.
* Paranephritis
E.
Cardiopulmonary insufficiency
The most typical symptoms in acute pyelonephritis:
A.
Proteinuria
B.
Bacteriuria
C.
Erythrocituria
D.
* Leucocyturia, bacteriuria
E.
Sternmaiber-Malbin’s cells
The most typical causes of acute secondary pyelonephritis:
A.
Stricture of a urether
B.
* Stones of kidneys and urethers
C.
Prostatic gland cancer
D.
Pregnancy
E.
Iatrogenic affection of urethers
The most typical provoking factor of primary pyelonephritis:
A.
Violation of diet
B.
Disorders in urine outflow
C.
* Decreased immune defense
D.
Hemodynamic disorders in kidney
E.
Diabetes mellitus
The most typical provoking factor of secondary pyelonephritis:
A.
Violation of diet
B.
* Disorders in urine outflow
C.
Decreased immune defense
D.
Hemodynamic disorders in kidney
E.
Diabetes mellitus
The most typical symptoms of acute pyelonephritis:
A.
Bacteriuria
B.
Chills and hectic fever
C.
Leucocyturia, pain
D.
Hematuria and leucocyturia
E.
* Lumbar pain, chills and hectic fever
The most typical triad of symptoms in acute pyelonephritis:
A.
Thirst, anorexia, nausea
B.
Vomiting, diarrhoea, abdominal pain
C.
* Chills, lumbar pain, dysuria
D.
Pain in bones, joints and muscles
The obvious condition for development of pyelonephritis:
A.
Arterial hypertension
B.
Heart failure
C.
* Disordered urine outflow
113.
D.
Increased body weight
E.
Renal failure
The plain X-ray of kidney allows to define:
A.
condition of the pyelocaliceal system;
B.
position of ureters;
C.
* sizes of kidneys;
D.
condition of glomerular apparatus of kidneys;
E.
presence of a tumor.
The plain X-ray of kidneys allows to define: 114.
115.
A.
state of the pyelocaliceal system;
B.
placing of ureters;
C.
* kidney stones;
D.
state of glomerular vehicle of kidneys;
E.
presence of tumour.
The what least of albumen in urine is characteristic for a nwphrotic syndrome?
A.
* 3,5 gr per day
B.
4,1 gr per day
C.
5,0 gr per day
D.
2,0 gr per day
E.
0,33 gr per day
To what syndrome belong edema, high proteinuria, hypoproteinemia, 116.
117.
dysproteinemia, hypercholesterolemia?
A.
To uric
B.
Nefritic
C.
* Nefrotic
D.
To hypertension
E.
To hypotension
Typical peculiarities of renal edeme:
A.
Appear in the evening
B.
First appear on legs
C.
First appear on arms
118.
D.
* Appearance on face in the morning
E.
Early appearance of anasarca
Urinary syndrome was found out in a patient. What amount of albumen in urine is
119.
it typical for urinary syndrome?
A.
* less than 3,5 g/day;
B.
to 4,5 g/day;
C.
to 5,5 g/day;
D.
to 6,5 g/day;
E.
to 9,5 g/day.
What amount of urine is selected by kidneys for a healthy man?
A.
* 1 liter/day;
B.
2,5 liter/day;
C.
3,5 liter/day;
120.
D.
5,0 liter/day;
E.
7,0 liter/day
What are casts?
A.
Mucus, which changed its consistency in acid urine
B.
* Protein molds from renal canaliculi
C.
Accumulation of bacteria
D.
Thrombocytes pressed together
E.
Salt corks
121.
122.
123.
124.
125.
126.
127.
128.
129.
What are the signs of chronic latent nephritis?
A.
Slow progressive course
B.
Malignant course
C.
* Hidden course
D.
Quick progression course
E.
Fast development of renal failure
What can not be assessed on plane X-ray of kidneys?
A.
Form of kidneys
B.
Size of kidneys
C.
Location of kidneys
D.
Presence of concrements
E.
* Presence of crystals of salts
What can not be reason of edema at the diseases of kidneys?
A.
* Growth of level of albumen is in blood
B.
Increase of permeability of wall of capillaries
C.
Diminishing of oncotic pressure of plasma of blood
D.
A delay is in blood and fabrics of ions of sodium
E.
Sharp delay of selection urine by buds
What can not be the reason of edema in kidney diseases?
A.
* Increased hydrostatic pressure in lower limbs
B.
Increase of permeability of capillary wall
C.
Diminishing of oncotic pressure of blood plasma
D.
Accumulation of sodium ions in blood and tissues
E.
Acute delay of selection of urine by kidneys
What can not be assessed at plain X-ray examination of kidneys?
A.
Form of kidneys
B.
Size of kidneys
C.
Location of kidneys
D.
Presence of concrements
E.
* kidney exretion function
What does belong to contrast X-ray examination of kidney
A.
* Excretory urography
B.
Radionuclide renogram
C.
Scintigraphy
D.
Radiocistography
E.
All mentioned above
What does not belong to radionuclide diagnostics of diseases of kidneys?
A.
* Excretory urography
B.
Radionuclide nephrography
C.
Plain X-ray
D.
Radiocystography
E.
No any one
What does not belong to radionuclide diagnostics of kidney diseases
A.
* Excretory urography
B.
Radionuclide renogram
C.
Scintigraphy
D.
Radiocistography
E.
All mentioned above
What edema are characteristic for kidney patients:
A.
edema are on lower limbs.
B.
edema are on the lumbar region
C.
* edema under eyes, later - edematousness of whole the body.
130.
131.
132.
133.
134.
135.
136.
137.
D.
accumulation of liquid in abdominal region (hydroperitoneum)
E.
edema are on overhead extremities.
What is ishuria:
A.
absence of urination because of affection of kidney excretory function
B.
* absence of urination because of impossibility to discharge urine from the bladder
C.
increase of amount of urine more than 2 liters per day
D.
decrease of amount of urine less than 1 liter per day
E.
amount of urine excreted per day is 0-30 ml per day because of affection of kidney excretory function
What is anuria:
A.
absence of urination because of affection of kidney excretory function
B.
absence of urination because of impossibility to discharge urine from the bladder
C.
increase of amount of urine more than 2 liters per day
D.
decrease of amount of urine less than 1 liter per day
E.
* amount of urine excreted per day is 0-30 ml per day because of affection of kidney excretory function
What is location of edema in initial stages of kidney affection?
A.
* Below eyes
B.
On lower limbs
C.
On upper limbs
D.
In lumbar region
E.
In abdominal cavity
What is not typical for acute pyelonephritis:
A.
Leucocyturia
B.
proteinuria
C.
* edema
D.
Leucocytosis
E.
Increased ESR
What is oliguria:
A.
frequent urination
B.
increase of amount of urine more than 2 liters per day
C.
* decrease of amount of urine less than 1 liter per day
D.
increase of specific gravity of urine
E.
lowering of specific gravity of urine
What is oligutia:
A.
excretion of 200 ml of urine per day
B.
excretion of 300 ml of urine per day
C.
* excretion of 500 ml of urine per day
D.
excretion to 700 ml per day
E.
excretion is to 1000 ml per day.
What is Pasternatsky’s symptom?
A.
Pain in palpation of lumbar region in the area of projection of kidneys
B.
Appearance of pain in lumbar region in rotation of a trunk
C.
* Appearance of pain at tapping lumbar region in the area of kidneys
D.
Appearance of pain in the lumbar area at coughing
E.
Appearance of pain in the projection of ureter at passing of stone from a kidney
What is pathogenesis of kidney eclampsia?
A.
* Brain edema
B.
Affection of peripheral nerves
C.
Brain stroke
D.
Increased nerve irritation
E.
All mentioned
138.
What is pathological mechanism of urocolick?
A.
* Obstruction of urine outflow from the kidney
B.
Inflammaltion of kidney parenchyma
C.
Inflammaltion of kidney calicies
D.
Inflammaltion of paranephral tissues
E.
No correct answer
139.
140.
141.
What is pollakiuria:
A.
urination 3-4 times per day
B.
urination 4-7 times per day.
C.
* urination 8-11 times per day
D.
absence of urination
E.
urination 1-2 times per day.
What is polyuria:
A.
frequent urination
B.
* increase of amount of urine more than 2 liters per day
C.
decrease of amount of urine less than 1 liter per day
D.
increase of specific gravity of urine
E.
lowering of specific gravity of urine.
What is stranguria:
A.
urination 3-4 times per day
B.
* painful urination .
C.
urination 8-11 times per day
D.
absence of urination
E.
urination 1-2 times per day.
What is the main principle of diet in acute pyelonephritis? 142.
A.
Restriction of proteins (beans) and water
B.
* Restriction of proteins (beans), spicy food
C.
Restriction of fats
D.
Restriction of products containing uric acid
E.
Increased caloric supplement
143.
144.
What is the main principle of diet in chronic renal failure?
A.
* Restriction of proteins (beans) and water
B.
Restriction of proteins (beans), spicy food
C.
Restriction of fats
D.
Restriction of products containing uric acid
E.
Increased caloric supplement
What is the origin of destroyed erythrocites in urianalyses?
A.
* Acute glomerulonephritis
B.
Urolithiasis
C.
Paranephritis
145.
D.
Acute cystitis
E.
pyelonephritis
What is the origin of destroyed erythrocites in urianalyses?
A.
* Acute glomerulonephritis
B.
Urolithiasis
C.
Paranephritis
D.
Acute cystitis
E.
pyelonephritis
146.
What is the sourse of leucocyturia if leucocites are mainly present in I portion of urine in Tompson’s test?
A.
* Urethra
B.
Kidney
C.
Urethers
D.
A bladder
E.
rectum
147.
What is the sourse of leucocyturia if leucocites are mainly present in II portion of urine in Tompson’s test?
A.
Urethra
B.
* Kidney
C.
A bladder
D.
Urethers
E.
rectum
148.
What is the sourse of leucocyturia if leucocites are mainly present in III portion of urine in . Tompson’s test?
A.
Urethra
B.
Kidney
C.
* A bladder
D.
Urethers
E.
rectum
149.
What is typical for nephritic syndrome in acute glomerulonephritis?
A.
Gross proteinuria
B.
Hypoproteinemia
C.
Hyperlipidemia
D.
* All enumerated
E.
No correct answer
150.
151.
What may be revealed in urinalyses of patient with acute pyelonephritis within first 48 hours of the disease/
A.
* Bacteriuria, proteinuria
B.
Pyuria
C.
Pyuria, erythrocyturia
D.
Casts
E.
Hematuria, proteinuria
152.
Which criteria of nephrotic syndrome do you know?
A.
* edema, high proteinuria, hypoproteinemia, dysproteinemia, hypercholesterolemia
B.
high proteinuria, hyperproteinemia, hyperestrogenemia
C.
edema, high proteinuria
D.
hypoproteinemia, dysproteinemia, hypercholesterolemia
E.
edema, high proteinuria, hypoproteinemia, dysproteinemia
What may be the consequence of gross prolonged loss oprotein with urine?
A.
Development of uric syndrome
B.
Development of nephritic syndrome
C.
Development of hematuric syndrome
D.
* Development of nephritic syndrome
E.
Development of hypertensive syndrome
153.
What pains are characteristic for nephrocolic:
A.
dull, aching pain in lumbar region
B.
intensive permanent pain in lumbar region
C.
* intensive sharp attack-like pain in lumbar region from one side irradiating downward to the internal surface of the shin and perineum.
D.
intensive sharp attack-like pain in lumbar region from the right side irradiating upward to the right shoulder and scapula.
E.
pain at the bottom of a stomach
154.
155.
156.
What pains are characteristic for a nephrocolic:
A.
dull, aching pain is in small of the back
B.
sharp permanent pain is in small of the back
C.
* very sharp attack-like pain in small of the back from one side.
D.
pain at the bottom of stomach
E.
permanent pain is in small of the back.
What pathology of kidney cramping pain is typical for?
A.
* In the attack of nephrocolic
B.
In kidney eclampsia
C.
Tuberculosis of kidneys
D.
Tumour of kidneys
E.
Glomerulonephritis
What pathology of kidney muscular cramps and convulsions are typical for?
A.
At the attack of nephrocolic
B.
* To the kidney eclampsia
C.
Tuberculosis of buds
D.
To the tumour of buds
E.
Glomerulonephritis
157.
What pathology of the urinary system does result in sudden sharp very intensive pain in lumbar region from one side?
A.
Paranephritis
B.
Kidney ptosis
C.
Acute pyelonephritis
D.
Acute glomerulonephritis
158.
E.
* thrombosis of renal artery
What pathology of urinary system is manifested with attack-like crumping pain in lumbar region from one side?
A.
Paranephritis
B.
Nephroptosis
C.
Acute pyelonephritis
D.
Acute glomerulonephritis
159.
E.
* Renal colic.
What position does patient with urocolick assume?
A.
On affected side with legs bended hip and knee joints and by the leg pressed to the stomach from the side of affection
B.
Semirecumbent position with lowered legs (orthopnoe)
C.
Lying on a sick side
D.
* Restless
160.
E.
Sitting, bending forward.
What results of Zimnitsky’s test do testify about violation of concentration function of kidneys?
A.
* prevalence of night diuresis above daily one
B.
Increased relative gravity of urine in separate portions.
C.
presence even one portion of urine with a relative gravity is below 1010
D.
monotonous high relative gravity of urine is in all of portions.
E.
an increase of amount of albumen is in urine.
161.
What syndrome the following signs: edema, high proteinuria, hypoproteinemia, dysproteinemia, hypercholesterolemia - are typical for?
A.
Uric syndrome
B.
Nephritic one
C.
* Nephrotic syndrome
D.
Hypertensive syndrome
162.
E.
Renal eclampsia.
What type of a disease is acute glomerulonephritis?
A.
* Immunoallergic
B.
Allergic
C.
Authoimmune
D.
Infectious
E.
Dysthrophic
163.
164.
What type of a disease is acute pyelonephritis?
A.
Immunoallergic
B.
Allergic
C.
Authoimmune
D.
* Infectious
E.
Dysthrophic
When does deformation of calicies and thin renal parenchyma of kidneys appear
165.
on excretory urogram?
A.
* In chronic diffuse nephritis
B.
In the case of polycystosis
C.
In chronic kidney insufficiency of the II stage.
D.
In uncomplicated urolithiasis
E.
In hydronephrosis.
When does the displacement of one kidney appear on plane X-ray?
A.
In diffuse nephritis
B.
In the case of polycystosis
C.
In chronic kidney insufficiency of the II stage.
166.
D.
* In nephroptosis
E.
In hydronephrosis.
When does the enlargement of one kidney appear on plane X-ray?
A.
In diffuse nephritis
B.
In the case of polycystosis
C.
In chronic kidney insufficiency of the II stage.
D.
In uncomplicated urolithiasis
167.
E.
* In hydronephrosis.
When does the enlargement of both kidneys appear on plane X-ray?
A.
In nephritis
B.
In the case of hypertrophy
C.
In the case of diabetic nephropathia
D.
* In the case of polycystosis
E.
In chronic kidney insufficiency of the II stage
168.
When does the increase of shade of both kidneys appear at plain X-ray?
A.
At a nephroncus
B.
In the case of hypertrophy
C.
In the case of diabetic nephropathy
D.
* In the case of polycystic degeneration
E.
At chronic kidney insufficiency
169.
170.
When does the decrease of shade of one kidney appear on X-ray?
A.
Acutediffuse nephritis
B.
In the case of polycystic degeneration
C.
* At chronic pyelonephritis
D.
At an urolithiasis
E.
At presence of hydronephrose
When in pyelonephritis th mass of affected kidney decreases?
A.
In acute serous inflammation
171.
B.
In kidney carbuncul
C.
In fat dystrophy
D.
* In sclerosis of the kidney
E.
In pyonephrosis
Which antibiotics used for treatment of glomerulonephritis are nephrotoxic?
A.
* Hentamycin
B.
Penicillin
C.
Phthorchynolones
D.
Macrolides
E.
Cephalosporines
Which changes in biochemical blood study are possible if the patient suffers from 172.
173.
chronic pyelonephritis for 10 years?
A.
Hypoproteinemia
B.
Hyperpliporoteinemia
C.
Hyperbilirubinemia
D.
* hypercreatininemia
E.
Dysproteinemia
Which changes in complete blood count are the most often presented in acute pyelonephritis?
A.
Increased ESR
B.
Leucocytosis
C.
Decreased hemoglobin content
D.
Thrombocytopenia
E.
* Shift on the left
174.
Which changes of kidney concentration function are typical for chronic pyelonephritis?
A.
* hypoisosthenuria
B.
isosthenuria
C.
hypersthenuria
D.
hyposthenuria
E.
oliguria
175.
176.
177.
178.
Which clinical sign is not typical for the beginning of pyelonephritis?
A.
Febril fever
B.
Lumbar pain
C.
Dysuria
D.
* Arterial hypertension
E.
chills
Which cnahges in urianalyses are typical for chronic glomerulonephritis?
A.
Active leucocytes
B.
Protein in urine less than 1 %
C.
Leucocytes cover all vision field
D.
* Erythrocytes till 30 in one vision field
E.
Bacteria till 100 in one vision field
Which data of urianalyses are typical for acute glomerulonephritis?
A.
* increased protein, erythrocytes and hyaline and wax casts
B.
increased protein, and hyaline casts
C.
leucocyturia, granular casts
D.
Crystals of uric acid salts in urine
E.
No correct answer
Which data of urianalyses are typical for acute pyelonephritis ?
A.
increased protein, erythrocytes and hyaline and wax casts
B.
* protein in low concentration leukocyturia, bacteriuria
179.
C.
leucocyturia, granular casts
D.
Crystals of uric acid salts in urine
E.
No correct answer
Which degree of nephroptosis is present if it is possible to palpate all the kidney in
180.
iliac region, it is easly displaceble, move to the opposite side of the body?
A.
I
B.
II
C.
* III
D.
IV;
E.
total nephroptosis.
Which degree of nephroptosis is present if it is possible to palpate the lower
181.
kidney pole, it is not displaceble,?
A.
* I
B.
II
C.
III
D.
IV;
E.
total nephroptosis.
Which degree of nephroptosis is present is it is possible to palpate all the kidney, it is easly displaceble, but does not move to the opposite side of the body?
A.
I
B.
* II
C.
III
D.
IV;
E.
total nephroptosis.
182.
Which examination should you prescribe for a patient if you revealed erythrocytes, protein and casts in his urine?
A.
Renography
B.
Chest X-ray
C.
* Ultrasound examination of kidneys
D.
Renal scintigraphy
E.
Duodenal probing
183.
184.
185.
186.
Which irradiation is typical for urocolick?
A.
* Downward to internal surface of thighs and perineum
B.
Upward to the right scapula
C.
Toward the neck
D.
Toward the navel
E.
No irradiation
Which laboratory test is useful for assessment kidney concentration function?
A.
Complete blood count;
B.
Nechyporenko’s test;
C.
* Canalicular reabsorption
D.
Clearance by endogenous creatinine (glomerular filtration)
E.
determination of daily proteinuria.
Which laboratory test is useful for assessment kidney filtration function?
A.
Complete blood count;
B.
Nechyporenko’s test;
C.
Canalicular reabsorption
D.
* Clearance by endogenous creatinine
E.
determination of daily proteinuria.
Which level of protein in urine is typical for acute glomerulonephritis?
A.
0,03 g/l
B.
0,03-1 g/l
187.
188.
C.
1-2 g/l
D.
2-3 g/l
E.
* More than 3 g/l
Which level of protein in urine is typical for acute pyelonephritis?
A.
No protein in urine
B.
* 0,03-1 g/l
C.
1-2 g/l
D.
2-3 g/l
E.
More than 3 g/l
Which main sign of chronic renal failure is the main criterion of its severity?
A.
Hypertension
B.
* Serum creatinin
C.
Degree of anemia
D.
Proteinuria
E.
Heart failure
Which microorganism is the causative agent acute glomerulonephritis? 189.
A.
* Beta-hemolythic streptococcus, type A
B.
Pneumococcus
C.
Mycoplasma
D.
Influenza virus
E.
Multiple bacterial microflora
190.
Which process in pyelonephritis is manifested with chills?
A.
Infection contamination of urinary ducts
B.
Fever
C.
* Appearance of bacteria in perypheric blood
D.
disorders of urine outflow
E.
disorders of kidney filtration function
Which results of excretory urography are typical for secondary chronic 191.
pyelonephritis?
A.
Uneven shadows of kidneys
B.
Decreased sizes of kidneys, asymmetrically decreased secretion and excretion of
193.
raduipaque preparation
C.
* Deformation of calicies and caliculi system, asymmetrically decreased secretion and excretion of raduipaque preparation
D.
Dilataion of calicies and caliculi system
192.
E.
Increased secretion of raduipaque preparation, decreased sizes of kidneys
Which results of ultrasound examination should be expected in acute glomerulonephritis?
A.
Thin kidney parenchyma because of sclerosis on both sides symmetrically
B.
Thin kidney parenchyma because of sclerosis on one side
C.
Stones in calicies
D.
Ellarged calicies
E.
* Swelling of kidney parenchyma on both sides symmetrically
Which results of ultrasound examination should be expected in chronic
194.
glomerulonephritis?
A.
* Thin kidney parenchyma because of sclerosis on both sides symmetrically
B.
Thin kidney parenchyma because of sclerosis on one side
C.
Stones in calicies
D.
Ellarged calicies
E.
Swelling of kidney parenchyma
Which results of ultrasound examination should be expected in chronic right-sided pyelonephritis/
195.
196.
197.
198.
199.
200.
201.
202.
A.
Thin kidney parenchyma because of sclerosis on both sides symmetrically
B.
* Thin kidney parenchyma because of sclerosis on right side
C.
Stones in calicies
D.
Ellarged calicies
E.
Swelling of kidney parenchyma
Which sign is a criterium of pathological process activity in glomerulonephritis?
A.
Hyerptension
B.
Hyaline casts
C.
Hematuria
D.
Creatitinemia
E.
* Nephrotic syndrome
Which syndrome a gross loss of albumеn with urine is typical for?
A.
Urinary syndrome
B.
Nephritic syndrome
C.
Hematuria
D.
* Nephrotic syndrome
E.
Hypertensjon.
Which syndrome is nit typical for pyelonephritis
A.
Uric
B.
* Nephrotic
C.
Pain
D.
Intoxication
E.
Dysuric
Which syndrome is not typical for chronic pyelonephritis?
A.
Asthenic
B.
Pain
C.
Hypertension
D.
Dyspeptic
E.
* cachexia
Which test is useful in assessment of kidney function?
A.
Complete blood count;
B.
ECG;
C.
Nechyporenko’s test;
D.
* Zimnicki’s test
E.
determination of dailyglucousuria.
Which test is useful in diagnostics of pyelonephritis?
A.
Biochemical blood study;
B.
ECG;
C.
* Nechyporenko’s test;
D.
Zimnicki’s test
E.
determination of daily proteinuria.
Which types of acute pyelonephritis do you know?
A.
Focal
B.
Asymptomatic
C.
Fast progressing
D.
Latent
E.
* Focal and latent
Which way of infection contamination is typical for primary pyelonephritis?
A.
Through the urether (in bladder-urether reflux)
B.
Along the urether walls
C.
* Hematogenic
D.
Lymphogenic
E.
No correct answer
203.
Which way of infection contamination is typical for secondaty pyelonephritis?
A.
* Through the urether (in bladder-urether reflux)
B.
Lymphogenic
C.
Along the urether walls
D.
Hematogenic
E.
No correct answer
204.
Which changes will be in biochemical blood analysis of a patient with B12 deficiency anemia?
205.
A.
* Increased bilirubin
B.
Increased amylase
C.
Increased kreatinine
D.
Increased ALT and AST
E.
All mentioned
Which factor is leading in chronic posthemorrhagic anemia?
A.
Hemolysis
B.
Vit. B12-deficiency
C.
Intoxication
D.
* Blood loss
E.
Folic acid deficiency
A blood test was prescribed to a patient with iron-deficiency anemia for 206.
determination of iron. Specify, what amount of iron of whey of blood is in a norm
(mkmol/l)
A.
1,5-3,5
B.
3,5-6,5
C.
7,5-11,7
D.
* 12,5-30,4
E.
32,2-35,9
207.
A fever at pernicious anemia is caused by:
A.
Massive disintegration of leucocytes;
B.
* Disintegration of red corpuscles;
C.
Infectious complications;
D.
General intoxication;
E.
Hyperglobulinemia.
208.
A patient with chronic gastritis finished treatment of iron-deficiency anemia.
What should be prophylaxis of the disease?
A.
* Iron preparations per os within 1 month twice a year
B.
Proper diet
C.
Vit. B12 i/v during a year
D.
Hemotransfusions 1 time per month
E.
All mentioned above
209.
At general blood analysis in patient with B12 deficiency anemia all the signs are determined except for:
A.
decreasing hemoglobin and erythrocytes amount
B.
macrocytosis
C.
increasing of CI more than 1,1
D.
* decreasing of CI less then 0.8
E.
bodies of Zholli, rings of Kebota in erythrocytes
210.
At the blood analysis of patient A. was determined the level of haemoglobin – 92 gr/l. Specify, what level of haemoglobin is normal for women.
A.
150-160
B.
140-160
211.
C.
130-150
D.
* 120-140
E.
100-120
At the blood analysis of patient A. was determined the level of haemoglobin – 92
212.
gr/l . Specify degree of severity of the disease:
A.
* Mild
B.
Moderate
C.
Severe
D.
Critical
E.
No any of them
At the blood analysis of patient A. was determined the level of haemoglobin – 80
213.
gr/l . Specify degree of severity of the disease:
A.
Mild
B.
* Moderate
C.
Severe
D.
Critical
E.
No any of them
At the blood analysis of patient A. was determined the level of haemoglobin – 48 gr/l . Specify degree of severity of the disease:
A.
Mild
B.
Moderate
C.
* Severe
D.
Critical
E.
No any of them
214.
215.
Botkin-Humpreht’s shadows are found in bone marrow smear in:
A.
Tbc
B.
Chronic myeloleucosis
C.
Subleukaemic myelosis
D.
Lymphogranulomatosis
E.
* Chronic lympholeucosis
Duration of prophylactic treatment of anemia with iron preparations:
A.
7 weeks
B.
* 4 weeks
C.
5 weeks 6 weeks
216.
D.
9 weeks
E.
No correct answer
During auscultation of neck vessels in patients with anemia it is heard:
A.
Rhythm of quail
B.
Diastolic murmur
C.
Intensification of I sound
D.
Intensification of II sound
E.
* Nunt’s murmur
217.
During heart auscultation in patients with anemia is heard:
A.
Rhythm of quail
B.
Bradycardia
C.
Intensification of I sound on apex
D.
Intensification of II sound above aorta
E.
* Systolic murmur on apex
218.
During the routine inspection of teenager a blood test was made, in which was found shift on the left. Which cells percentage will be increased in this case?
A.
Segmentonuclear neutrophils
B.
Young neutrophils in usual quantity
C.
Stab neutrophil in usual quantity
D.
* Juvenile and stab neutrophils quantity is increased, may be found myelocytes, promyelocites
E.
Juvenile and stab neutrophils quantity is decreased
219.
During the routine inspection of teenager a blood test was made, in which was found shift on the right. Which cells will be in CBC in this condition?
A.
Segmentonuclear neutrophils
B.
Young neutrophils in usual quantity
220.
C.
Stab neutrophil in usual quantity
D.
Juvenile and stab neutrophils quantity is increased, may be found myelocytes, promyelocites
E.
* Juvenile and stab neutrophils quantity is decreased
Early criteria of efficiency of vitamin B12-deficiency anemia treatment:
A.
Increased level of vit. B12 in blood serum
B.
* Reticulocytosis
C.
Anysocytosis
D.
Increase of Hb content
E.
Normalisation of CI
221.
Enlarged liver and especially spleen, which lower border may be found even in pelvic region, is typical for:
A.
Tbc
B.
* Chronic myeloleucosis
C.
Subleukaemic myelosis
D.
Lymphogranulomatosis
222.
E.
Chronic lympholeucosis
For what disease CI is more than 1,05?
A.
Iron-deficiency anemia
B.
Posthemorrhagic anemia
C.
* B12 deficiency anemia
D.
Hemolytic anemia
E.
Acute leucosis
223.
224.
225.
226.
For what disease color index is more than 1,05?
A.
Iron-deficiency anemia
B.
Posthemorrhagic anemia
C.
* folic acid deficiency anemia
D.
Hemolytic anemia
E.
Acute leucosis
For which anemia such findings like anysocytosis and poikilocytosis are typical?
A.
* Iron-deficiency
B.
Vitamin B12-deficiency
C.
Congenital hemophilic
D.
Acquired hemophilic
E.
Aplastic
For which anemia such findings like Jollie bodies and Kebot’s rings are typical?
A.
Iron-deficiency
B.
* Vitamin B12-deficiency
C.
Congenital hemophilic
D.
Acquired hemophilic
E.
Aplastic
For which conditions thrombocytosis is not typical?
A.
All mentioned
B.
For polycythemia
227.
228.
C.
For patients with malignant new formations
D.
For patients with rheumatism
E.
* For patients with diabetes mellitus
For which disease “Hunter’s glossitis” is typical:
A.
* Pernicious anemia
B.
Iron-deficiency;
C.
Hemolytic anemia;
D.
Acute leucosis;
E.
Erythremia.
For which disease “tabes dorsalis” is typical:
A.
* Pernicious anemia
B.
Iron-deficiency;
C.
Hemolytic anemia;
D.
Acute leucosis;
E.
Erythremia.
For which disease alveolar pyorrhea is typical: 229.
230.
A.
Pernicious anemia;
B.
* Iron-deficiency;
C.
Hemolytic anemia;
D.
Acute leucosis;
E.
Erythremia.
Functional murmurs in anemia are often:
A.
* systolic;
B.
diastolic;
C.
protodiastolic;
D.
presystolic;
E.
systolodiastolic;
How complication of acute leukemia is called when the patient develops 231.
symptoms of brain affection?
A.
Migrain
B.
Meningitis
C.
Encefalopathy
D.
Hypertension
E.
* Neuroleukemia
232.
233.
How many classes of haemopoetic cells there are?
A.
* 6
B.
4
C.
7
D.
5
E.
3
How the anemia called if CI is less than 0,85?
A.
* Hypochromic anemia
B.
Hypoerchromic anemia
C.
Megalochromic anemia
234.
D.
Normochromic anemia
E.
Microchromic anemia
How the anemia called if CI is more than 0,95?
A.
Hypochromic anemia
B.
Hypoerchromic anemia
C.
Megalochromic anemia
D.
* Normochromic anemia
E.
Microchromic anemia
235.
236.
How the anemia called if CI is more than 1,05?
A.
Hypochromic anemia
B.
* Hypoerchromic anemia
C.
Megalochromic anemia
D.
Normochromic anemia
E.
Microchromic anemia
How the specific elements on skin of patient with acute leukemia are called which
237.
indicate on prolipheration of malignant cells in the skin?
A.
* Leukaemids
B.
Purpura
C.
Ecchymoses
D.
Scares
E.
Erythema
In a patient with iron-deficiency anemia hemoglobin content in CBC is 95 g/l.
238.
What is severity of the disease?
A.
* Mild
B.
Moderate
C.
Severe
D.
Very severe
E.
There is no anemia in the patient
In a patient with iron-deficiency anemia hemoglobin content in CBC is 88 g/l.
239.
What is severity of the disease?
A.
Mild
B.
* Moderate
C.
Severe
D.
Very severe
E.
There is no anemia in the patient
In a patient with iron-deficiency anemia hemoglobin content in CBC is 76 g/l.
What is severity of the disease?
A.
Mild
B.
*Moderate
C.
Severe
D.
Very severe
E.
There is no anemia in the patient
240.
In patient T., 30 y.o., was found iron-deficiency anemia, confirmed by laboratory blood test. Specify the most typical complaints for iron deficiency.
A.
Loss of tactile sensation
B.
Graying of hair
C.
* Fragility of nails
D.
Labial fissure
E.
Anosmia
241.
In patient T., 30 y.o., was found iron-deficiency anemia, confirmed by laboratory blood test. Specify the most typical complaints for iron deficiency:
A.
Loss of tactile sensation
B.
Graying of hair
C.
* Deranged appetite and desire to eat cholck
D.
Labial fissure
E.
Anosmia
242.
In patient T., 30 y.o., was found iron-deficiency anemia, confirmed by laboratory blood test. Specify the most typical complaints for iron deficiency:
A.
Loss of tactile sensation
B.
Graying of hair
243.
C.
* Skin dryness and hair loss
D.
Labial fissure
E.
Anosmia
In patient T., 30 y.o., was found vit. B12-deficiency anemia, confirmed by
244.
laboratory blood test. Specify the most typical complaints for this disease:
A.
Loss of tactile sensation
B.
Graying of hair
C.
* Pierching sensations in the tongue
D.
Labial fissure
E.
Anosmia
In patient with leucaemia there were found 82% of blast cells in sterna punctuate.
245.
What should be the following examination?
A.
Tests for activity of inflammation
B.
Serum bilirubin
C.
Fibrinogen
D.
No correct answer
E.
* Cytochemic investigation of blast cells
In patients with leukemia there are 82% of blast cells in CBC. Which examination is it necessary to prescribe?
A.
* Sternal puncture
B.
Trepanobiopsy
C.
Puncture of lumph node
D.
Puncture of a spleen
E.
Puncture of a liver
246.
In which disease Beresovsky-Sternberg’s cells may be found in lymph node bioptat?
247.
248.
A.
AIDS
B.
Lupus erythematodus
C.
* Lymphogranulomatosis
D.
Tbc
E.
Chronic lympholeucosis
In which disease is nunt’s murmur present?
A.
* Iron-deficiency anemia
B.
Vit. B12-deficiency anemia
C.
Hemolythic anemia
D.
Aortal incompetence
E.
Mitral incompetence
In which disease may be found high blast cells in CBC ?
A.
Pernicious anemia
B.
Chronic myeloleucosis;
C.
Chroniclympholeucosis;
D.
Hemolytic anemia;
E.
* Acute leucosis;
In which disease may be found high quantity of immatured myelocytes and 249.
250.
myelocytes in CBC ?
A.
Pernicious anemia
B.
* Chronic myeloleucosis;
C.
Chroniclympholeucosis;
D.
Hemolytic anemia;
E.
Acute leucosis;
In which disease may be found high quantity of immatured lymphocytes in CBC ?
A.
Pernicious anemia
251.
252.
253.
257.
In which disease may be found shift on the right?
A.
* Pernicious anemia
B.
Iron-deficiency;
C.
Hemolytic anemia;
D.
Acute leucosis;
E.
Erythremia.
In which disease you can find angular stomatitis in the patient?
A.
Chronic lympholeukosis
B.
* Iron-deficiency anemia
C.
Folic acid deficiency anemia
D.
Hemolytic anemia
E.
Lymphogranulomatosis
In which parts of digestive system the main part of iron is absorbed?
A.
In a stomach
B.
* In a duodenum and initial part of thin colon
C.
In a sigmoid colon
D.
In a caecum
254.
E.
Along the whole length of digestive tract
Parestesia in pernicious anemia is caused by:
A.
* Toxic affection of nerve myelin coats by malonic and methylmalonic acids
B.
Toxic affection of nerve myelin coats by cetone bolies
C.
Disintegration of red blood cells;
D.
Infectious complications;
E.
General intoxicatION
255.
Patient 40 yo., has periodical uterine bleedings. During inspection the signs of hypochromic anemia were found. Which research is specific for diagnostics?
A.
ESR
B.
Blood proteins
C.
Reticulocyte
D.
Form of erythrocytes
256.
E.
* Serum iron
Patient P, a woman, complains of dizziness, faintness, dyspnea. Data of inspection: skin is pale with yellow tint. What data will prove diagnosis “anemia”?
A.
Paleness of the tongue.
B.
Increased skin moistness.
C.
Reddness of conjuntive.
D.
* Paleness of conjuntive.
E.
Pulsation of carotide arteries
Select typical signs of acute leucaemia:
A.
Skin pallor, dyspnoe
B.
Skin redness, paresthesia in limbs
C.
* Necrotic pharyngitis
D.
Skin dryness, fragidity of nails
E.
Gigantic liver and spleen, jaundice
258.
B.
Chronic myeloleucosis;
C.
* Chronic lympholeucosis;
D.
Hemolytic anemia;
E.
Acute leucosis;
Select typical signs of anemic syndrome:
A.
* Skin pallor, dyspnoe
B.
Skin redness, paresthesia in limbs
C.
Necrotic pharyngitis
259.
D.
Skin dryness, fragidity of nails
E.
Gigantic liver and spleen, jaundice
Select typical signs of chronic lympholeycosis:
A.
Skin redness, paresthesia in limbs
B.
Necrotic pharyngitis
C.
Skin dryness, fragidity of nails
D.
Gigantic liver and spleen, jaundice
E.
* Enlarged and solid lymph nodes of all groups
Select typical signs of chronic myeloleycosis: 260.
A.
Skin pallor, dyspnoe
B.
Skin redness, paresthesia in limbs
C.
Necrotic pharyngitis
D.
Skin dryness, fragidity of nails
E.
* Gigantic liver and spleen, jaundice
261.
262.
263.
Select typical signs of erythremia:
A.
Skin pallor, dyspnoe
B.
* Skin redness, paresthesia in limbs
C.
Necrotic pharyngitis
D.
Skin dryness, fragidity of nails
E.
Gigantic liver and spleen, jaundice
Select typical signs of syderopoenic syndrome:
A.
Skin pallor, dyspnoe
B.
Skin redness, paresthesia in limbs
C.
Necrotic pharyngitis
D.
* Skin dryness, fragidity of nails
E.
Gigantic liver and spleen, jaundice
Signs of deficit of iron:
A.
Psilosis
B.
Fragility of nails
C.
Distortion of taste
D.
Koylonychia
264.
E.
* All mentioned
Specify which indexes of leucocytes in blood are normal?
A.
2,0-5,0 · 109/l
B.
* 4,0-9,0 · 109/l
C.
9,0-11,0 · 109/l
D.
11,0-13,0 · 109/l
E.
13,0-14,0 · 109/l
265.
The 37-year-old male patient has a hemoglobin level of 22.1 g/dL. What is the doctor’s best action?
A.
Document the report as the only action.
B.
Institute infection precautions.
C.
Institute bleeding precautions.
D.
* Prescribe transfusion of compatible blood
E.
All above mentioned
266.
The doctor should instruct the patient to eat which of the following foods to obtain the best supply of vitamin B12?
A.
Whole grains
B.
Green leafy vegetables
C.
* Meats and dairy products
D.
Broccoli and brussels sprouts
E.
All above mentioned
267.
The patient being discharged home after a bone marrow transplantation for leukemia asks why protection from injury is so important. What is the doctor’s best response?
A.
“The transplanted bone marrow cells are very fragile and trauma could result in rejection of the transplant.”
B.
* “Trauma is likely to result in loss of skin integrity, increasing the risk for infection when you are already immunosuppressed.”
C.
“Platelet recovery is slower than white blood cell recovery and you remain at risk longer for bleeding than you do for infection.”
D.
“The medication regimen after transplantation includes drugs that slow down cell division, making healing after any injury more difficult.”
268.
E.
All above mentioned
The patient has anemia and all the following clinical manifestations. Which manifestation indicates to the doctor that the anemia is a long-standing problem?
A.
Headache
B.
* Clubbed fingers
C.
Circumoral pallor
D.
Orthostatic hypotension
269.
E.
All above mentioned
The patient with leukemia asks his doctor why he is so susceptible to infection when his white blood cell count is so high. What is the doctor’s best response?
A.
“The number of white blood cells is falsely high because of the severe dehydration that accompanies leukemia.”
B.
* “Even though you have a lot of white blood cells, they are immature and not able to prevent or fight infection.”
C.
“Your white blood cells have been poisoned by chemotherapy and are now nonfunctional.”
D.
“It is the platelets, not the white blood cells, that protect you from infection.”
270.
E.
All above mentioned
The patient with pernicious anemia has periodical increased temperature to
37,40С. What is the reason of temperature rise?
271.
A.
Intoxication
B.
* Destruction of erythrocytes
C.
Infectious complications
D.
Development of hepatitis
E.
Destruction of leucocytes
The patient’s face with Adison-Birmer anemia is:
272.
A.
Pale, diffusely edematic;
B.
* «waxen doll»;
C.
Cyanotic, edematic;
D.
Pale, exhausted;
E.
Moonlike.
Treatment in erythraemia:
A.
* Periodical blood letting or erythrocytophoresis
B.
Bone marrow transplantation
C.
Cytostatics
D.
Hypotensive drugs
E.
Erythropoetin
273.
Treatment of patients with congenital mycrospherocytosis?
A.
Iron preparations
B.
Cyancobalamin
C.
Hemotransfusions
274.
D.
* Splenectomy
E.
Glucocorticoids
Treatment of patients with vitamin B12-deficiency anemia:
A.
Iron preparations
B.
* Cyancobalamin
C.
Hemotransfusions
D.
Splenectomy
E.
Glucocorticoids
Treatment of pernicious anemia: 275.
276.
277.
282.
A.
* Vit. B12 parenterally
B.
Iron preparations
C.
Na nucleinatis
D.
Glucocorticoids
E.
Erythropoetin
What is «pica chlorotica»?
A.
Inacidity and achylia for patients with iron-deficiency anaemia
B.
* Patients have distortion of taste with iron-deficiency anaemia
C.
Decline of taste qualities
D.
Heartburn is on a proglossis
E.
pallor with a greenish tint for patients with chronic iron-deficiency anaemia
What is anisocytosis:
A.
* erythrocytes of different size
B.
appearance of red corpuscles of different form
C.
appearance of leucocytes of different form
278.
279.
E.
appearance of leucocytes of different size
What day's requirement of the grown man in iron is needed for the erythrocytes synthesis?
A.
* 20-25 mg
B.
30-35 mg
280.
C.
10-15 mg
D.
5-10 mg
E.
1-2 g
What is “pica chlorotica”?
A.
Increased
B.
Decreased
C.
Absent
D.
* Desire to eat unusual things like chalk
E.
Abstinence of food intake
281.
D.
appearance of leucocytes of different size
E.
appearance of thrombocytes of different size
What anyschromia of erythrocytes:
A.
* appearance of red blood cells with different intensity of red colour
B.
appearance of red blood cells of different size
C.
appearance of red blood cells of different form
D.
appearance of leucocytes of different form
What is shift on the left in leucocyte formula?
A.
Appearance in blood of increased amount of lymphocytes
B.
Appearance in blood of increased amount of leucocytes
C.
Appearance in blood of increased amount of monocytes
D.
Appearance in blood of increased amount of erythrocytes
E.
* Appearance in blood of increased amount of stab and juvenile neutrophils
What is shift on the right in leucocyte formula?
A.
Appearance in blood of increased amount of lymphocytes
B.
Appearance in blood of increased amount of leucocytes
C.
Appearance in blood of increased amount of monocytes
D.
Appearance in blood of increased amount of erythrocytes
E.
* Appearance in blood of decreased amount of stab neutrophil and juvenile neutrophils
283.
284.
What is normal spleen longitudinal diameter assessed by percussion?
A.
4-6 сm
B.
2-4 сm
C.
* 6-8 сm
D.
8-10 сm
E.
10-12 сm
What is normal spleen transverse diameter assessed by percussion?
A.
* 4-6 сm
B.
2-4 сm
C.
6-8 сm
D.
8-10 сm
E.
10-12 сm
285.
What is not typical for a patient with iron-deficiency anemia?
A.
Dryness and shelling of skin
B.
Hair fragility
C.
Concavity of nail plates
D.
* "Tabes dorsalis"
E.
Parodontosis, darkening of teeth
286.
287.
288.
What is not typical for a patient with iron-deficiency anemia?
A.
Dryness and shelling of skin
B.
Hair fragility
C.
Concavity of nail plates
D.
* Subicteritiousness of skin and mucous membrane
E.
Parodontosis, darkening of teeth
What is nunt’s murmur?
A.
Systolic murmur at the heart apex in Iron-deficiency anemia
B.
* Systolic murmur at carotid arteries is Iron-deficiency anemia
C.
Systolic murmur at jugular veins is Iron-deficiency anemia
D.
Systolic murmur at femoral artery in aortal incompetence
E.
Systodiastolic murmur at femoral artery in aortal incompetence
What is the cause of geographic tongue in pernicious anemia?
A.
* Papillar athrophy
B.
Fungal infection
C.
Bacterial infection
D.
Edema of the tongue
289.
E.
Papillar hyperhrophy
What is the pathologic mechanism involved in aplastic anemia?
A.
Decreased intake of iron
B.
Increased rate of red blood cell lysis and destruction
C.
* Decreased bone marrow production of red blood cells
D.
Increased (excessive) cellular metabolic oxygen demand
E.
All above mentioned
290.
What is the prior problem for the patient with aplastic anemia who is being treated with a combination of prednisone and cyclophosphamide.
A.
Risk for Activity Intolerance
B.
* Risk for Infection
291.
292.
293.
294.
295.
296.
297.
298.
C.
Risk for Injury
D.
Constipation
E.
All above mentioned
What is the prior problem for the patient with polycythemia vera?
A.
Adult Failure to Thrive related to increased energy demands
B.
Ineffective Thermoregulation related to excessive heat loss
C.
* Risk for Injury related to thrombus formation
D.
Constipation related to dehydration
E.
All above mentioned
What is the type of aplastic anemia?
A.
Hyperchromic, megaloblastic
B.
Hypochromic, syderopoenic
C.
* Normochromic, normocytic
D.
Hyperchromic, mactocytic
E.
Normochromic, megaloblastic
What is the type of folic acid-deficiency anemia?
A.
Hyperchromic, megaloblastic
B.
Hypochromic, syderopoenic
C.
Normochromic, normocytic
D.
* Hyperchromic, macrocytic
E.
Normochromic, megaloblastic
What is the type of hemolitic anemia?
A.
Hyperchromic, megaloblastic
B.
Hypochromic, syderopoenic
C.
* Normochromic, normocytic
D.
Hyperchromic, mactocytic
E.
Normochromic, megaloblastic
What is the type of iron-deficiency anemia?
A.
Hyperchromic, megaloblastic
B.
* Hypochromic, syderopoenic
C.
Normochromic, normocytic
D.
Hyperchromic, mactocytic
E.
Normochromic, megaloblastic
What is the type of vit. B12-deficiency anemia?
A.
* Hyperchromic, megaloblastic
B.
Hypochromic, syderopoenic
C.
Normochromic, normocytic
D.
Hyperchromic, mactocytic
E.
Normochromic, megaloblastic
What koilonychia?
A.
Transversal strakes on the nails
B.
A bulge of nails is as sentinel скелець
C.
* Spoon-shaped form of nails
D.
Fragility of nails
E.
discoloration nails
What poikilocitosis:
A.
* appearance of red corpuscles of different size
B.
appearance of red corpuscles of different form
C.
appearance of leucocytes of different form
D.
appearance of leucocytes of different size
E.
appearance of thrombocytes of different form
299.
When a person's hemoglobin is deficient in iron, which assessment finding is expected?
A.
Cherry red lips and mucous membranes
B.
* Increased respiratory rate
C.
Slow capillary refill
D.
Bradycardia
E.
All above mentioned
300.
301.
Where do lymphocites develop?
A.
* In lymphatic nodes and in all lymphoid organs.
B.
In red bone marrow
C.
In a thymus
D.
In a spleen
E.
In kidneys
Where do red cells develop?
A.
In lymphatic knots
B.
In a spleen
C.
In thymus
D.
* In red marrow
302.
E.
In a liver
Where do white cells appear?
A.
In lymphatic knots
B.
In a spleen
C.
In thymus
D.
* In red marrow
E.
In a liver
Where is the best site to assess capillary refill on an 88-year-old patient? 303.
A.
* Fingernails
B.
Forehead
C.
Toenails
D.
Lips
E.
All above mentioned
304.
Which assessment finding alerts the home care doctor to the possibility of infection in the patient with sickle cell disease who is recovering from a crisis episode?
A.
Oral temperature of 37.8o C (100o F)
B.
* Diminished breath sounds unilaterally
C.
Firm, nodular texture to the liver on palpation
D.
Darkened areas of skin on the lower extremities
E.
All above mentioned
305.
Which cells do not belong to the reticular stroma of bone marrow?
A.
Fibroblasts
B.
* Erythroblasts
C.
Fatty cells
D.
Osteoblasts
E.
Endothelial cells
306.
Which changes may be expected in sterna punctate of a patient with Vit. B12deficiency anemia?
A.
* Prevalence of megaloblasts
B.
Increased amount of syderoblasts
C.
Erythroid bone marrow steam hyperplasia
D.
Blast cells
E.
Prevalence of lymphoid tissue
307.
Which clinical manifestation is common for all types of anemia regardless of cause or pathologic mechanism?
A.
Jaundiced sclera and roof of the mouth
B.
Hypertension and peripheral edema
C.
* Tachypnoe
D.
Increased PaCO2
E.
All above mentioned
308.
Which clinical manifestation is common for all types of anemia regardless of cause or pathologic mechanism?
A.
Jaundiced sclera and roof of the mouth
B.
Hypertension and peripheral edema
C.
* Skin paleness
D.
Increased PaCO2
E.
All above mentioned
309.
Which clinical manifestation is common to all types of anemia regardless of cause or pathologic mechanism?
310.
311.
A.
Jaundiced sclera and roof of the mouth
B.
Hypertension and peripheral edema
C.
* Tachycardia at basal activity levels
D.
Increased PaCO2
E.
All above mentioned
Which compliant is typical for “Hunter’s glossitis” in Vit.B12-deficiency anemia?
A.
Patients like such smell as benzin and others unusual strong smells
B.
* Perching sensations in a tongue
C.
Bitter taste in the mouth
D.
Heart burn
E.
Foul smell from the mouth
Which complication is possible in bone marrow aplasia?
A.
Vascular thrombosis
B.
* Infections
C.
Pancreatitis
312.
D.
Hepatitis
E.
Myocardial infarction
Which complication is possible in bone marrow aplasia?
A.
Vascular thrombosis
B.
* Hemorrhagic syndrome
C.
Pancreatitis
D.
Hepatitis
313.
E.
Myocardial infarction
Which complication of chronic myeloleukosis present if patient’s spleen is enlarged, pulsating, and painful in palpation, there is muscular defence in this area?
314.
A.
Acute appendicitis
B.
* Infarction of a spleen
C.
Acute pancreatitis
D.
Reflectory splenomegaly
E.
Acute hepatitis
Which disease “pica chlorotica” is typical for?
A.
* Iron-deficiency anemia
B.
Vit. B12-deficiency anemia
C.
Aplastic anemia
D.
Hemolytic anemia
E.
Leukemia
315.
316.
317.
318.
319.
320.
321.
322.
323.
Which disorders of appetite is typical for iron-deficiency anemia?
A.
Increased
B.
Decreased
C.
Absent
D.
* Desire to eat unusual things like chalk
E.
Abstinence of food intake
Which drug is prescribed in pernicious anemia complicated with polyneuropathy?
A.
Vit. B12 200-300 γ i/v per day
B.
* Vit. B12 1000 γ i/v per day
C.
Folic acid 0,5 mg/day
D.
Phenobarbital
E.
Neuromidin
Which examination is important for diagnosis of plasma cells myeloma?
A.
* Bence-Jones protein determination in urine
B.
C-reactive protein
C.
Lymph node puncture
D.
Coagulogram
E.
Common protein and its fractures
Which examination is important for diagnosis of plasma cells myeloma?
A.
* X-ray of a chest and skull
B.
C-reactive protein
C.
Lymph node puncture
D.
Coagulogram
E.
Protein in urine
Which examination method is necessary fro diagnostics of myeloleucosis
A.
Immunogram
B.
Coagulogram
C.
X-ray of bones
D.
Proteinogram
E.
* Myelogram
Which factor is leading in anemia secondary to chronic severe infectious disease?
A.
Hemolysis
B.
Vit. B12-deficiency
C.
* Intoxication
D.
Blood loss
E.
Folic acid deficiency
Which factor is leading in anemia secondary to chronic enterocolitis?
A.
Hemolysis
B.
Vit. B12-deficiency
C.
Intoxication
D.
Blood loss
E.
* Folic acid deficiency
Which factor is leading in pathogenesis of acquired hemolytic anemia
A.
Deranged differentiation of erythroid cells
B.
* Intravascular hemolysis
C.
Demaged hemoglobin synthesis
D.
Deranged transport of iron from reticuloendotelial depot
E.
Depression of hemopoesis
Which factor is leading in pathogenesis of aplastic anemia?
A.
Deranged differentiation of erythroid cells
B.
Intravascular hemolysis
C.
Demaged hemoglobin synthesis
324.
D.
Deranged transport of iron from reticuloendotelial depot
E.
* Bone marrow aplasia
Which factor is leading in pathogenesis of congenital microspherocytosis?
A.
Deranged differentiation of erythroid cells
B.
* Deranged intracellular hemolysis
C.
Deranged hemoglobin synthesis
D.
Depression of hemopoesis
E.
No correct answer
Which factor is leading in pathogenesis of iron-deficiency anemia? 325.
A.
Deranged differentiation of erythroid cells
B.
Intravascular hemolysis
C.
Deranged transport of iron from reticuloendotelial depot
D.
* Deranged hemoglobin synthesis
E.
Depression of hemopoesis
326.
327.
Which factor is leading in pathogenesis of vitamin B12-deficiency anemia?
A.
* Deranged differentiation of erythroid cells
B.
Intravascular hemolysis
C.
Deranged hemoglobin synthesis
D.
Deranged transport of iron from reticuloendotelial depot
E.
Depression of hemopoesis
Which factor is leading in pernicious anemia?
A.
Hemolysis
B.
* Vit. B12-deficiency
C.
Intoxication
D.
Blood loss
E.
Folic acid deficiency
328.
Which feature is characteristic of vitamin B12 deficiency anemia but not characteristic of folic acid deficiency anemia?
A.
Weight loss
B.
Smooth, beefy-red tongue
C.
Macrocytic red blood cells
329.
D.
* Paresthesias of the hands and feet
E.
All above mentioned
Which from objective symptoms are typical for anemia?
A.
* Paleness of skin and mucous membranes
B.
Petechias
C.
Cyanosis
D.
Edema
330.
E.
Rash
Which intervention should the doctor teach the patient who has IgM-mediated immunohemolytic anemia?
331.
A.
Use an electric shaver.
B.
Avoid crowds and sick people.
C.
Wear socks and gloves in cool weather.
D.
* Do not take aspirin or aspirin-containing products.
E.
All above mentioned
Which iron is absorbs the best?
A.
That which is the part of plants
B.
* That, which is the part of albumens which contain haem (veal)
C.
That which is the part of dietary sorts of meat (rabbit, chicken)
D.
That which is received with groats
E.
Any iron is absorbed inspite of valency and amount
332.
333.
Which iron is absorbs the best?
A.
From the part of plants
B.
* From meat, fish
C.
From egg protein
D.
That which is received with groats
E.
Any iron is absorbed inspite of valency and amount
Which laboratory value alerts the doctor to the possibility that the patient is
334.
chronically losing small amounts of blood?
A.
* Reticulocyte count of 7%
B.
Bleeding time of 3 minutes
C.
Hemoglobin level of 14.0 g/dL
D.
Negative indirect Coombs’ test
E.
All above mentioned
Which medical preparation will you prescribe for a patient with chronic hepatitis
335.
and megalocytic anemia?
A.
* Folic acid
B.
Ferroplex
C.
Prednisolon
D.
Ferrum-lek
E.
Vit. B12
Which medical preparation will you prescribe for a patient with chronic
336.
enterocolitis and megalocytic anemia?
A.
* Folic acid
B.
Ferroplex
C.
Prednisolon
D.
Ferrum-lek
E.
Vit. B12
Which medical preparation will you prescribe for a patient with chronic irondeficiency anemia which developed as a result of stomach resection?
A.
Folic acid
B.
* Ferrolec pro injections
C.
Tardiferon-retard
D.
Prednisolon
E.
Vit. B12
337.
Which menu selection made by the patient with vitamin B12 deficiency anemia demonstrates adequate understanding of dietary management for this problem?
A.
* Boiled liver and onions, orange juice, spinach salad
B.
Baked chicken breast, boiled carrots, glass of white wine
C.
Eggplant Parmesan, cream-style cottage cheese, iced tea
D.
Whole-grain pasta with cheese, apple sauce, glass of red wine
E.
All above mentioned
338.
Which method of examination is important in verification of diagnosis of macrocitic anemia except of CBC?
A.
* Sternal puncture
B.
Endoscopic examination of a stomach
C.
Stomach X-ray
D.
Erythrocytes osmotic resistance
E.
Serum iron
339.
Which method of examination is important in verification of diagnosis of anemia which arises after usage of aspirin or exposure to cold?
A.
Sternal puncture
B.
Endoscopic examination of a stomach
340.
C.
Stomach X-ray
D.
* Erythrocytes osmotic resistance
E.
Serum iron
Which of the following assessment findings is a late symptom of polycythemia
341.
vera?
A.
Headache
B.
Dizziness
C.
* Pruritus
D.
Shortness of breath
Which organ does product erythropoietin?
A.
Lymphatic knots and all lymphoid organs.
B.
Red bone marrow
C.
Thymus
D.
A spleen
342.
E.
* Kidneys
Which other symptoms except of deranged appetite belong to “pica chlorotica” in iron-deficiency anemia?
A.
* Patients like such smell as benzin and others unusual strong smells
B.
Perching sensations in a tongue
C.
Bitter taste in the mouth
D.
Heart burn
343.
E.
Foul smell from the mouth
Which patient is at greatest risk for development of acute leukemia?
A.
* 50-year-old being treated with cyclophosphamide (Cytoxan) for a chronic autoimmune disease
B.
55-year-old with diabetes mellitus type 1 who has received insulin injections for
43 years
C.
20-year-old with cystic fibrosis who has been on continuous enzyme replacement
344.
therapy since age 3 months
D.
38-year-old who has used combination oral contraceptives without a break for 15 years
E.
All above mentioned
Which patient is most at risk for hematologic problems?
A.
48-year-old man who had a myocardial infarction 5 years ago
B.
62-year-old woman with diabetes mellitus on insulin therapy
C.
* 55-year-old man with chronic alcoholism
D.
27-year-old woman taking oral contraceptives
E.
All above mentioned
345.
Which question is appropriate when exploring the risk factors for the patient newly diagnosed with acute leukemia?
A.
“How many packs of cigarettes do you smoke per day and for how many years have you smoked?”
B.
“Have you ever been treated for a sexually transmitted disease?”
C.
* “Have you ever worked around radioactive materials?”
D.
“How old was your mother when you were born?”
346.
E.
All above mentioned
Which symptoms arise up in patients with acute leucosis?
A.
Disuria
B.
Angina pectoris
C.
Low body temperature
D.
* Often pain during swallowing
E.
All above
347.
348.
349.
Which symptoms arise up in patients with acute leucosis?
A.
General weakness
B.
Pain in joints and muscles
C.
High body temperature
D.
Often pain during swallowing
E.
* All above
Which symptoms arise up in patients with acute leucosis?
A.
Disuria
B.
* Pain in joints and muscles
C.
Angina pectoris
D.
Disgust to meat
E.
All above mentioned
Which symptoms arise up in patients with acute leucosis?
A.
Disuria
B.
Angina pectoris
C.
* High body temperature
D.
Disgust to meat
E.
All above
350.
Which symptoms arise up in patients with acute leucosis?
A.
Disuria
B.
* Pain in throat
C.
Angina pectoris
D.
Disgust to meat
E.
All above
351.
352.
Which symptoms arise up in patients with acute leucosis?
A.
Disuria
B.
* Gingival bleeding
C.
Angina pectoris
D.
Disgust to meat
E.
All above
Which symptoms arise up in patients with acute leucosis?
A.
Disuria
B.
* Marked sweating
C.
Angina pectoris
D.
Disgust to meat
E.
All above
353.
Why is the patient with polycythemia vera at an increased risk for a myocardial infarction?
A.
The rapid synthesis of cells greatly increases metabolism.
B.
The abnormal hemoglobin in the erythrocytes inadequately oxygenates the myocardium.
C.
* The increased number of erythrocytes increases blood viscosity and the workload of the heart.
D.
The disease is most prevalent among men in their 60s and 70s who have other
354.
conditions that damage the heart.
E.
All above mentioned
Why patients with iron-deficiency anemia develop trophic changes of skin?
A.
* Because of lack of intracellular respiratory enzymes containing iron
B.
Because of collagen atrophy
C.
Because of hypoxia
D.
Because of bed absorption of vitamins in intestine
E.
All mentioned
355.
356.
357.
Yellow tint of skin in pernicious anemia is caused by:
A.
* Mild hemolysis
B.
Disintegration of red corpuscles;
C.
Infectious complications;
D.
General intoxication;
E.
Hyperglobulinemia.
A fever at pernicious anemia is caused by:
A.
Massive disintegration of leucocytes;
B.
* Disintegration of red corpuscles;
C.
Infectious complications;
D.
General intoxication;
E.
Hyperglobulinemia.
A hemorragic syndrome arises up as a result of all of reasons, except for:
A.
Decreasing of thrombocytes amount
B.
Functional deficiency of thrombocytes
C.
Deficit of coagulation factors in plasma
D.
Damage of vascular wall of immune character
E.
* Decreasing of erythrocytes amount and level of hemoglobin
358.
A hemorrhagic syndrome arises up as a result of all of reasons, except of:
A.
Decreasing of thrombocytes amount
B.
Functional deficiency of thrombocytes
C.
Deficit of coagulation factors in plasma
D.
Damage of vascular wall of immune character
359.
E.
* Decreasing of erythrocytes amount and level of hemoglobin
A student should assess patient’s facial expression. Which pathological condition
“Facies Basedovica” is typical fo?
A.
kidney pathology;
B.
infectious diseases;
C.
cardiac insufficiency;
D.
anaemia;
E.
* toxic goitre.
360.
At general blood analysis in patient with B12 deficiency anemia all the signs are determined except of:
A.
decreasing hemoglobin and erythrocytes amount
B.
macrocytosis
C.
increasing of CI more than 1,1
D.
* decreasing of CI less then 0.8
E.
bodies of Zholli, rings of Kebota in erythrocytes
361.
Falling of hairs out of external part of eyebrows is observed at:.
A.
unstable angina pectoris.
B.
Myocardial infarction
C.
Hypertension
D.
Rheumatism
E.
* Hypothyreosis.
362.
For which patient with hyperthyroidism is radioactive iodine therapy contraindicated?
A.
18-year-old man with asthma
B.
* 28-year-old woman who is pregnant
C.
48-year-old man with type 2 diabetes mellitus
D.
68-year-old woman with mild congestive heart failure
E.
All the above
363.
For which disease alveolar pyorrhea is typical:
A.
Pernicious anemia;
B.
* Iron-deficiency;
C.
Hemolytic anemia;
D.
Acute leucosis;
364.
E.
Erythremia.
For which patient with hyperthyroidism is radioactive iodine therapy contraindicated?
A.
18-year-old man with asthma
B.
* 28-year-old woman who is pregnant
C.
48-year-old man with type 2 diabetes mellitus
D.
68-year-old woman with mild congestive heart failure
365.
E.
All above mentioned
Hemorrhages in the form of small dots are named:
A.
* petechia
B.
purpura
C.
ecchympses
D.
roseola
E.
papula
366.
Hemorrhagic syndrome arises up as a result of all of reasons, except of:
A.
diminishing of amount of thrombocites
B.
functional inferiority of thrombocites
C.
a deficit of factors of rolling up is in plasma
D.
damage of vascular wall of immune character
E.
* decline of amount of red corpuscles and haemoglobin
367.
368.
Hoarse voice is observed in:
A.
* Aortic aneurism
B.
Hypertension
C.
Rheumatic heart disease
D.
Nephritis
E.
Hepatitis
How is it needed to take away blood for determination of thrombocytes?
A.
Into place of puncture inflict the drop of iodine
B.
Into place of puncture inflict the drop of alcohol
C.
Into place of puncture inflict a drop марганцевокислого potassium
D.
* Into place of puncture inflict the drop of a 14% solution of magnesium of sulfate
369.
370.
E.
Into place of puncture inflict the drop of a 25% solution of magnesia
How many levels of thrombotest are determined?
A.
* 7
B.
6
C.
4
D.
8
E.
5
How the I-st phase of blood coagulation activity is determined?
A.
* By determination of time of plasma recalcification and test of prothrombin
371.
consumption.
B.
By determination of prothrombin index
C.
By determination of fibrinogen concentration
D.
By a thrombotest level
E.
By determination of plasma tolerance to the heparin
In collaboration with the dietician, what dietary modification should the doctor suggest for the patient with hyperthyroidism?
A.
Decrease calories and proteins and increase carbohydrates.
B.
Eliminate carbohydrates and increase proteins and fats.
C.
* Increase calories, proteins, and carbohydrates.
D.
No dietary modification is needed.
372.
E.
All above mentioned
Patient was prescribed determination of blood haematocrite. Specify, what level of haematocrite is normal for men?
A.
29-36
B.
36-42
C.
* 40-48
D.
48-54
373.
E.
more than 54
Patient was prescribed determination of blood haematocrite. Specify, what level of haematocrite is normal for men?
A.
29-36
B.
36-42
C.
* 40-48
D.
48-54
374.
E.
more than 54
Rash in the form of small red spots is named:
A.
* peteshia
B.
purpura
C.
echymoses
D.
roseola
375.
E.
papula
The patient is at risk for a urinary tract infection. Which of the following beverages is the patient encouraged to drink?
A.
Carbonated beverages
B.
Citrus juices
C.
Milk
D.
* Tomato juice
376.
E.
All the above
The patient is receiving an antithyroid medication to treat hyperthyroidism. Which of the following should be included in patient education regarding the initiation of this therapy?
A.
* “Increased need for sleepy or not tolerating cold like you used to can occur when taking this medication. If it does, notify your physician.”
B.
“Nausea and vomiting are serious complication of the medication you are taking.”
C.
“Take your pulse every day, as you were taught. If it is too fast, call your doctor.”
D.
“This medication may cause dyspnea or vertigo. Notify your health care provider if this occurs.”
E.
No correct answer
377.
The patient scheduled to have a thyroid scan asks the doctor how long she will be radioactive after the scan. What is the doctor’s best response?
A.
“No radiation is used for the thyroid scan.”
B.
“Only external beam radiation is used so you are not radioactive.”
C.
* “The dose of radiation is so low and is excreted by the kidneys in just a few days, so you are not considered radioactive.”
D.
“The radiation used is taken up by your thyroid gland, so only your thyroid is considered radioactive. Because it is not excreted to the outside of the body, no precautions are needed.”
E.
No correct answer
378.
The patient with hyperthyroid symptoms is having hormone studies done to confirm the diagnosis. Which set of values indicates non–Graves’ disease hyperthyroidism?
A.
* Elevated T3, elevated T4, high TSH levels
B.
Elevated T3, normal T4, low TSH levels
C.
Elevated T3, low T4, low TSH levels
D.
Low T3, normal T4, high TSH levels
379.
E.
No correct answer
The patient with hyperthyroidism is taking lithium carbonate to inhibit thyroid hormone release. Which of the following patient reports alerts the doctor to side effects of this therapy?
A.
Blurred vision
B.
* Increased thirst and urination
C.
Increased sweating and diarrhea
D.
Decreased attention span and insomnia
E.
No correct answer
380.
The patient with hypothyroidism as a result of Hashimoto’s thyroiditis asks the doctor how long she will have to take thyroid medication. What is the doctor’s best response?
A.
“You will need to take the thyroid medication until the goiter is completely gone.”
B.
“The thyroiditis will be cured with antibiotics, and then you will no longer need the thyroid medication.”
C.
* “You will need thyroid replacement hormone therapy for the rest of your life because the thyroid gland function will not return.”
D.
“When your thyroid function studies indicate a normal blood level of thyroid hormones, you will be able to discontinue the medication.”
E.
No correct answer
381.
The patient is receiving an antithyroid medication to treat hyperthyroidism. Which of the following should be included in patient education regarding the initiation of this therapy?
A.
* “Increased need for sleepy or not tolerating cold like you used to can occur when taking this medication. If it does, notify your physician.”
B.
“Nausea and vomiting are serious complication of the medication you are taking.”
C.
“Take your pulse every day, as you were taught. If it is too fast, call your doctor.”
D.
“This medication may cause dyspnea or vertigo. Notify your health care provider if this occurs.”
E.
All above mentioned
382.
The patient scheduled to have a thyroid scan asks the doctor how long she will be radioactive after the scan. What is the doctor’s best response?
A.
“No radiation is used for the thyroid scan.”
B.
“Only external beam radiation is used so you are not radioactive.”
C.
* “The dose of radiation is so low and is excreted by the kidneys in just a few days, so you are not considered radioactive.”
D.
“The radiation used is taken up by your thyroid gland, so only your thyroid is
383.
considered radioactive. Because it is not excreted to the outside of the body, no precautions are needed.”
E.
All above mentioned
The treatment of Grave’s disease usually include
A.
* Antagonists of thyroid hormones
B.
Antidepressants
C.
Narcotic analgesics
D.
Diuretics
E.
Sulfonylureas
384.
Twelve hours after a total thyroidectomy, the patient develops stridor on exhalation. What is the doctor’s best first action?
A.
Reassure the patient that the voice change is temporary.
B.
Document the finding as the only action.
C.
Hyperextend the patient's neck.
D.
* Call for emergency assistance.
E.
No correct answer
385.
Twelve hours after a total thyroidectomy, the patient develops stridor on exhalation. What is the doctor’s best first action?
A.
Reassure the patient that the voice change is temporary.
386.
B.
Document the finding as the only action.
C.
Hyperextend the patient's neck.
D.
* Call for emergency assistance.
E.
All above mentioned
What are the goals of the Healthy People 2010 campaign?
A.
To provide culturally congruent care across the life span
B.
* To increase years of healthy life while eliminating health disparities
C.
To eliminate all chronic and acute diseases affecting the population
D.
To provide specific population-focused health care delivery across the life span
387.
E.
All above mentioned
What are the goals of the Healthy People 2010 campaign?
A.
To provide culturally congruent care across the life span
B.
* To increase years of healthy life while eliminating health disparities
C.
To eliminate all chronic and acute diseases affecting the population
D.
To provide specific population-focused health care delivery across the life span
E.
No correct answer
388.
What assessment data should be collected first from a patient admitted to the emergency department with a lacerated radial artery from a lawn mower accident?
A.
Information regarding next of kin to notify in case the patient dies
B.
* History about what medications the patient is currently taking
C.
Measurement of blood pressure, pulse, and capillary refill time
D.
Assessment of rate and depth of respiration to ensure that the airway is patent
389.
E.
All above mentioned
What assessment data should be collected first from a patient admitted to the emergency department with a lacerated radial artery from a lawn mower accident?
A.
Information regarding next of kin to notify in case the patient dies
B.
* History about what medications the patient is currently taking
C.
Measurement of blood pressure, pulse, and capillary refill time
D.
Assessment of rate and depth of respiration to ensure that the airway is patent
390.
E.
No correct answer
What factor has influenced the growth and acceptance of home care in the United
States?
A.
* The lower cost of home care as compared to institutional care
B.
A cultural shift away from traditional nursing home care
C.
The increasing numbers of terminally ill individuals
D.
The recent nursing staff shortages
391.
E.
All above mentioned
What factor has influenced the growth and acceptance of home care in the United
States?
A.
* The lower cost of home care as compared to institutional care
B.
A cultural shift away from traditional nursing home care
C.
The increasing numbers of terminally ill individuals
D.
The recent nursing staff shortages
E.
No correct answer
392.
What information obtained by observation or interview is considered part of cultural assessment?
A.
The home is neat and clean.
B.
The patient is underweight for his or her height.
C.
The skin tone of all family members is similar.
D.
* The wife corrects the husband's response to the question of how old his parents are.
E.
All above mentioned
393.
What information obtained by observation or interview is considered part of cultural assessment?
A.
The home is neat and clean.
B.
The patient is underweight for his or her height.
C.
The skin tone of all family members is similar.
D.
* The wife corrects the husband's response to the question of how old his parents
394.
are.
E.
No correct answer
What intervention should the doctor use to prevent injury in the patient with
395.
hyperparathyroidism?
A.
Instruct the patient to place both hands behind the neck when moving.
B.
* Use a lift sheet to assist the patient with position changes.
C.
Instruct the patient to use a soft-bristled tooth brush.
D.
Strain all urine.
E.
All above mentioned
What intervention should the doctor use to prevent injury in the patient with
396.
hyperparathyroidism?
A.
Instruct the patient to place both hands behind the neck when moving.
B.
* Use a lift sheet to assist the patient with position changes.
C.
Instruct the patient to use a soft-bristled tooth brush.
D.
Strain all urine.
E.
No correct answer
What is «pica chlorotica»?
397.
A.
Inacidity and achilia for patients with iron-deficiency anaemia
B.
Patients have distortion of taste with iron-deficiency anaemia
C.
Deranged taste
D.
Burning sensations on a tongue
E.
* Pallor with a greenish tint for patients with chronic iron-deficiency anaemia
What is anisocytosis:
A.
* erythrocytes of different size
B.
appearance of red corpuscles of different form
C.
appearance of leucocytes of different form
398.
D.
appearance of leucocytes of different size
E.
appearance of thrombocytes of different size
What is coagulation time by Ly-White?
A.
* 5-10 min
B.
3-5 min
C.
6-12 min
D.
1-3 min
E.
12-13 min
399.
400.
What is coagulation time by Ly-White?
A.
* 5-10 min
B.
3-5 min
C.
6-12 min
D.
1-3 min
E.
12-13 min
What is it found out during the review of oral cavity for a patient with acute
401.
leucosis?
A.
* Ulcerative and necrotic tonsillitis and stomatitis
B.
Gingival bleeding
C.
Plural chronic focuses of infection
D.
Enlarged tongue and imprints of teeth is on it
E.
Salivation is increased
What is the cause of ostealgia in patients with chronic leucosis?
A.
Secondary infection
B.
* Hyperplasia of myeloid tissue
C.
Intoxication syndrome
D.
Increased production of lymphocites in bone marrow
402.
E.
Systemis enlargement of lymphatic knots
What is the priority problem for the patient newly diagnosed with hyperthyroidism?
403.
404.
A.
* Decreased cardiac output related to tachycardia
B.
Disturbed Body Image related to weight loss
C.
Hyperthermia related to hypermetabolism
D.
Fatigue related to energy depletion
E.
No correct answer
What is the priority problem for the patient in thyroid crisis?
A.
* Potential for Ineffective Breathing Pattern
B.
Risk for Imbalanced Body Temperature
C.
Risk for Decreased Cardiac Output
D.
Activity Intolerance
E.
No correct answer
What is the priority nursing diagnosis for the patient with hypothyroidism?
A.
Hypothermia
B.
Disturbed Body Image
C.
* Disturbed Thought Processes
D.
Imbalanced Nutrition: More than Body Requirements
E.
No correct answer
405.
What is the priority nursing diagnosis for the patient newly diagnosed with hyperthyroidism?
A.
* Decreased cardiac output related to tachycardia
B.
Disturbed Body Image related to weight loss
C.
Hyperthermia related to hypermetabolism
D.
Fatigue related to energy depletion
E.
All above mentioned
406.
What level of serum iron is typical for chronic iron-deficiency anaemia?
A.
20-30 gr/l
B.
12-20 gr/l
C.
* 6-12 gr/l
D.
2-6 gr/l
E.
1-2 gr/l
407.
What precaution should be given to a person who will be taking warfarin
(Coumadin) for 6 months?
A.
“Decrease your intake of sodium.”
B.
“Sleep with the head of your bed elevated.”
C.
* “Avoid aspirin and aspirin-containing drugs.”
D.
“Avoid taking walks or performing any physical activity.”
E.
All above mentioned
408.
What sign may be found during inspection of skin of a patient with chronic lympholeukosis?
A.
Systemic increase of peripheral lymphatic nodes, they are painless and not connected with skin
B.
Enlargement of a spleen
C.
Mild enlargement of a liver
D.
Dryness of skin, psoriasis elements. Appearance of violetblue knots on the skin (
409.
leukemides).
E.
* All above mentioned
Whatever sign does confirm the diagnosis of thrombocytopenic purpura?
A.
Diminishing in peripheral blood of maintenance of thrombocytes
B.
* Negative symptom of plait and nip *
C.
Time of hemopexis mostly is not changed
D.
Bleeding time is prolonged to 15-20 хв
410.
E.
Retrakciya of bloody clot is broken
Which action should the doctor implement to prevent pressure ulcer formation in a bedridden patient?
A.
* Assessing serum albumin and transferrin levels
B.
Measuring the ulcer diameter and depth every shift
C.
Changing the gauze dressing whenever drainage is observed
D.
Applying antibiotic ointment to all excoriated skin areas
411.
E.
All above mentioned
Which action should the doctor implement to prevent pressure ulcer formation in a bedridden patient?
A.
* Assessing serum albumin and transferrin levels
B.
Measuring the ulcer diameter and depth every shift
C.
Changing the gauze dressing whenever drainage is observed
D.
Applying antibiotic ointment to all excoriated skin areas
E.
No correct answer
412.
Which activity by the doctor would be appropriate in caring for a patient using complementary therapies as a supplement to traditional treatment for cancer?
A.
* Instruct the patient to make a follow-up appointment with the health care provider after using alternative treatments to assess the patient’s response to the treatment.
B.
Instruct the patient never to use alternative or complementary treatments for serious illnesses.
C.
Explain to the patient that physicians and doctors are not prepared to recommend and monitor alternative treatments.
D.
Explain to the patient that physicians and doctors do not incorporate such treatments into their practice.
E.
All above mentioned
413.
Which activity by the doctor would be appropriate in caring for a patient using complementary therapies as a supplement to traditional treatment for cancer?
A.
* Instruct the patient to make a follow-up appointment with the health care provider after using alternative treatments to assess the patient’s response to the treatment.
B.
Instruct the patient never to use alternative or complementary treatments for serious illnesses.
C.
Explain to the patient that physicians and doctors are not prepared to recommend and monitor alternative treatments.
D.
Explain to the patient that physicians and doctors do not incorporate such treatments into their practice.
E.
No correct answer
Which activity or situation helps meet the goals of Healthy People 2010 with 414.
regard to culture?
A.
Ensuring accurate recording of a patient's race and/or ethnicity in the medical record
B.
* Hiring physicians and doctors from culturally diverse backgrounds
C.
Providing magazines written in more than one language in waiting areas of clinics
D.
Translating HIV prevention guidelines into multiple literacy and language forms
E.
All above mentioned
415.
Which activity or situation helps meet the goals of Healthy People 2010 with regard to culture?
A.
Ensuring accurate recording of a patient's race and/or ethnicity in the medical record
B.
* Hiring physicians and doctors from culturally diverse backgrounds
C.
Providing magazines written in more than one language in waiting areas of clinics
D.
Translating HIV prevention guidelines into multiple literacy and language forms
E.
No correct answer
416.
Which activity plan would best conserve a patient's energy without compromising the patient's physical or mental health?
A.
Reducing hygiene activities and restricting visitors
B.
Ensuring that the patient toilets before and after any other planned activity
C.
* Scheduling energy-intensive activities at the time of day when the patient has higher energy levels
D.
Scheduling as many activities as possible within a small block of time to allow the patient a longer, uninterrupted rest period
E.
No correct answer
417.
Which activity plan would best conserve a patient's energy without compromising the patient's physical or mental health?
A.
Reducing hygiene activities and restricting visitors
B.
Ensuring that the patient toilets before and after any other planned activity
C.
* Scheduling energy-intensive activities at the time of day when the patient has higher energy levels
D.
Scheduling as many activities as possible within a small block of time to allow the patient a longer, uninterrupted rest period
E.
All above mentioned
418.
Which patient is at greatest risk for hyperparathyroidism?
A.
28-year-old patient with pregnancy-induced hypertension
B.
* 45-year-old patient receiving dialysis for end-stage renal disease
C.
55-year-old patient with moderate congestive heart failure after myocardial infarction
D.
60-year-old patient on home oxygen therapy for chronic obstructive pulmonary disease
E.
No correct answer
419.
Which patient is likely to require transitional subacute care before being discharged home?
A.
The patient with stable human immunodeficiency virus infection
B.
The patient with a progressive neurologic disease
C.
* The patient requiring deep wound management
420.
D.
The patient who is ventilator dependent
E.
No correct answer
Which clinical manifestation alerts the doctor to the possibility of Graves’ disease as the cause of hyperthyroidism?
A.
Weight loss
B.
* Exophthalmos
C.
Menstrual irregularities
D.
Increased heart rate and blood pressure
E.
All above mentioned
421.
Which clinical manifestation indicates to the doctor that treatment for the patient with hypothyroidism is effective?
A.
The patient is thirsty.
B.
The patient’s weight has been the same for 3 weeks.
C.
The patient’s total white blood cell count is 6000 cells/mm3.
D.
* The patient has had a bowel movement every day for 1 week.
E.
All above mentioned
422.
423.
Which from objective symptoms are typical for anemia?
A.
* Paleness of skin and mucous membrane
B.
Petechias
C.
Cyanosis
D.
Edema
E.
Rash
Which hematologic problem would the doctor expect the patient with liver failure to have?
A.
* Prolonged bleeding after IM injections
B.
Elevated blood pressure from hypercellularity
C.
Increased formation of thromboses in deep veins
D.
Spontaneous bleeding from the gums and mucous membranes
E.
All above mentioned
424.
425.
Which indexes characterizes the II phase of blood coagulation?
A.
By determination of time of plasma recalcification
B.
* By determination of prothrombin index
C.
By determination of fibrinogen concentration
D.
By a thrombotest level
E.
By determination of plasma tolerance to the heparin
Which indexes characterizes the II phase of blood coagulation?
A.
By determination of time of plasma recalcification
B.
* By determination of prothrombin index
C.
By determination of fibrinogen concentration
D.
By a thrombotest level
E.
By determination of plasma tolerance to the heparin
426.
Which information gathered during assessment is considered to be subjective data?
A.
The patient’s urine is dark and foul-smelling.
B.
The patient’s total 24-hour urine output is 1800 mL.
C.
* The patient indicates that pain and burning are present when urinating.
D.
The patient has been treated for urinary tract infections in the past.
E.
No correct answer
427.
Which laboratory test result indicates to the doctor that the factor VIII cryoprecipitate therapy for the patient with hemophilia is effective?
428.
A.
Hematocrit of 43%
B.
Platelet count of 200,000/mm3
C.
Prothrombin time of 15 seconds (INR of 1.3)
D.
* Activated partial thromboplastin time of less than 30 seconds
E.
All above mentioned
Which levels of thrombotest correspond to hypocoagulation?
A.
III-IV
B.
* I-III
C.
IV-V
D.
VI-VII
E.
II-I
429.
430.
Which levels of thrombotest correspond to hypocoagulation?
A.
III-IV
B.
* I-III
C.
IV-V
D.
VI-VII
E.
II-I
Which manifestation of Graves’ disease is unaffected by medical treatment for the
431.
hyperthyroidism?
A.
Thinning hair
B.
* Exophthalmos
C.
Weight loss
D.
Tachycardia
E.
All above mentioned
Which medication should the doctor be prepared to administer to a patient with bradycardia as a result of hypothyroidism?
A.
Atropine sulfate
B.
* Levothyroxine sodium
C.
Propranolol
D.
Epinephrine
E.
All above mentioned
432.
433.
Which of the following statements regarding thyroid disorders is true?
A.
The presence of a “goiter” always indicates hypothyroidism.
B.
* The effects of thyroid dysfunction are found in all body tissues and organs.
C.
The hormones synthesized by the thyroid gland are not essential for life.
D.
The effects of hypothyroidism are less serious than those of hyperthyroidism.
E.
No correct answer
Which patient is at greatest risk for hyperparathyroidism?
A.
28-year-old patient with pregnancy-induced hypertension
B.
* 45-year-old patient receiving dialysis for end-stage renal disease
C.
55-year-old patient with moderate congestive heart failure after myocardial infarction
D.
60-year-old patient on home oxygen therapy for chronic obstructive pulmonary disease
E.
All above mentioned
434.
the highest priority for instruction of the patient going home with thrombocytopenia?
A.
“Drink at least 3 liters of fluid each day.”
B.
“Avoid flossing your teeth until platelets return to normal.”
435.
C.
“Avoid drinking alcoholic beverages until your CBC is normal.”
D.
“Avoid the use of salt substitutes that contain potassium chloride.”
E.
* All above mentioned
Which statement made by the patient alerts the doctor to the possibility of hypothyroidism?
A.
“My sister has thyroid problems.”
B.
“I seem to feel the heat more than other people.”
C.
“Food just doesn't taste good without a lot of salt.”
D.
* “I am always tired, even when I get 10 or 12 hours of sleep.”
E.
Men experience more disability than women, but women experience a higher incidence of chronic illness than men.
436.
Which statement regarding platelet function in hemostasis is true?
A.
Platelets are required for erythrocyte aggregation.
B.
Platelets aggregation is dependent on adequate amounts of all clotting factors.
C.
* Platelets aggregation helps maintain blood vessel integrity during tissue trauma.
D.
Platelets aggregation prevents the extension of clot formation beyond the area of injury.
E.
All above mentioned
437.
Which statement, made by the patient who is taking warfarin (Coumadin) daily to prevent blood clots from forming in deep veins, indicates a need for further discussion regarding this therapy?
A.
“I have been eating more salads and other green, leafy vegetables to prevent constipation.”
B.
“I have two pairs of antiembolic stockings so that one pair can be washed each day.”
C.
“Instead of a safety razor, I have been using an electric shaver to shave.”
D.
* “On hot days, I make sure I drink at least two quarts of water.”
E.
* All above mentioned
Situations real-life
1.
The patient with hypokalemia requires a diuretic for another health problem. Which agent should the doctor be prepared to administer?
A.
Furosemide (Lasix)
B.
Bumetanide (Bumex)
C.
Chlorothiazide (Diuril)
D.
* Spironolactone (Aldactone)
E.
No any answer is correct
2.
A 33-year-old lady has been suffering from DM for 5 years. The last 3 years she has taken more than 100 units of insulin per day. Body weight has increased up to 10 kg.
Fasting blood glucose is 13 mmol /L, glucoseuria - 3\%. Generalized microangiopathy.
By increasing the dose of insulin the parameters of glycemia do not change. The diagnosis is:
A.
* DM 1st type, severe form, decompensation, insulin resistant
B.
DM 2nd type, severe form, decompensation
C.
DM 1st type, severe form, subcompensation, Somoji phenomenon
D.
DM 2nd type, moderate form, Zabrodi phenomenon
E.
DM 1st type, severe form, decompensation, allergic response on insulin
3.
A patient who has long-standing diabetes mellitus and severe, burning pain in the feet and hands as a result of peripheral neuropathy asks the doctor why an antidepressant has been prescribed. What is the doctor’s best response?
A.
“Many people experiencing chronic pain become depressed.”
B.
* “The antidepressants may counteract the chemicals causing your pain.”
C.
“You are less likely to become addicted from using antidepressants than you are from using other types of pain killers.”
D.
“The antidepressants also have strong anti-inflammatory properties and can reduce the pain you have from inflammation.”
E.
No any answer is correct
4.
A patient of 62 years with DM-2. Diabetes is being compensated by diet and Maninilum.
Pаtient has to undergo an operation for inguinal hernia. What should be tactics of hypoglycemic therapy?
A.
* Prescribe the drugs of an insulin of short activity
B.
Give Glurenorm in place of Maninilum
C.
To continue with the current therapy
D.
Prescribe the drugs of insulin of long activity
E.
Prescribe guanyl guanidines
5.
The 30-year-old woman whose mother has type 2 diabetes mellitus asks the doctor what her chances are of developing diabetes because of her mother's disease. What is the doctor’s best response?
A.
“You have a greater susceptibility for developing the disease, with a 1 in 20 to a 1 in 50 chance.”
B.
“Your risk is the same as the general population, because there is no genetic risk for development of type 2 diabetes.”
C.
“Type 2 diabetes is inherited in an autosomal dominant pattern. Therefore, your risk for becoming diabetic is 50%.”
D.
* “Children of people with type 2 diabetes have a 15% chance of developing the disease, but environmental factors, such as obesity, also influence your risk.”
E.
All above mentioned
6.
The patient at risk for continuing hyperkalemia is going home and says that she really enjoys fruit. She will miss having fruit each day but understands that she must restrict her intake of potassium. What is the doctor’s best response?
A.
“You are correct. Fruit is very high in potassium. I am glad you understand your dietary needs.”
B.
“If you cook the fruit before eating it, the total amount of both potassium and sodium in it will be reduced.”
C.
* “Some fruit is high in potassium, but berries, cherries, apples, and peaches are low in potassium and you can eat them.”
D.
“Some vegetables, such as potatoes and avocados, can be substituted for fruit, so you can still enjoy the texture of raw food.”
E.
No any answer is correct
7.
The patient getting ready to engage in a 30-minute, moderate-intensity exercise program performs a self-assessment. Which data indicate that exercise should be avoided at this time?
A.
* Ketone bodies in the urine
B.
Blood sugar level of 155 mg/dL
C.
Pulse rate of 66 beats/min
D.
Weight 1 pound higher than the week before
E.
No any answer is correct
8.
The patient is a 28-year-old man newly diagnosed with type 1 diabetes mellitus. He wears glasses for myopia and asks the doctor how frequently he should see his ophthalmologist now. What is the doctor’s best answer?
A.
“At your age, you do not need to change your usual patterns for visiting the ophthalmologist.”
B.
“See your ophthalmologist whenever you have a vision problem and yearly after you are 40 years old.”
C.
“Your vision will change more quickly now, and you should see the ophthalmologist whenever you find that your glasses are not strong enough to allow you to read comfortably.”
D.
* “The disease increases your risk for cataracts, glaucoma, and retinal blood vessel changes, so you should see the ophthalmologist yearly, even when you do not have a new vision problem.”
E.
No any answer is correct
9.
The patient is receiving amikacin, an aminoglycoside antibiotic, for treatment of a systemic infection. Which clinical manifestation is a probable response to an electrolyte imbalance induced by this therapy?
A.
Decreased systolic blood pressure
B.
Hyperactive bowel sounds and diarrhea
C.
Lethargy progressing to somnolence
D.
* Positive Trousseau's and Chvostek's signs
E.
No any answer is correct
10.
The patient newly diagnosed with type 1 diabetes mellitus has just learned to measure urine ketone bodies. She asks the doctor when this should be done. What is the doctor’s best response?
A.
“Daily, just before you take your insulin.”
B.
“Whenever you test your blood for glucose.”
C.
* “Whenever you are ill or your blood sugar is consistently higher than 300 mg/dL.”
D.
“Whenever you participate in vigorous exercise or experience a change in your daily activity level.”
E.
No any answer is correct
11.
The patient newly diagnosed with type 2 diabetes tells the doctor that since he has increased his intake of fiber, he is having loose stools, flatulence, and abdominal cramping. What is the doctor’s best response?
A.
“Decrease your intake of water and other fluids.”
B.
* “Decrease your intake of fiber now and gradually add high-fiber foods back into your diet.”
C.
“You must have allergies to high-fiber foods and will need to avoid them in the future.”
D.
“Taking an antacid 1 hour before meals or 2 hours after meals should reduce the intensity of your bowel problems.”
E.
No any answer is correct
12.
The patient on an intensified insulin regimen consistently has a fasting blood glucose between 7,0 and 8,0 mmol/L, a postprandial blood glucose level below 20,0 mmol/L, and a hemoglobin A1c level of 5.5%. What is the doctor’s interpretation of these findings?
A.
The patient is at increased risk for developing hypoglycemia.
B.
The patient is at increased risk for developing hyperglycemia.
C.
The patient is demonstrating signs of insulin resistance.
D.
* The patient is demonstrating good control of blood glucose.
E.
No any answer is correct
13.
The patient tells the doctor that he enjoys having a glass of wine on Saturdays when dining out with friends. He asks if having type 1 diabetes will prohibit him from this activity. What is the doctor’s best response?
A.
“Insulin activity is dramatically reduced under the influence of alcohol and drinking even one glass of wine will increase your insulin requirements.”
B.
“Diabetics have decreased kidney function and should avoid ingesting alcohol in all forms at all times.”
C.
“You shouldn't drink any alcohol because it is likely to increase your sense of hunger and make you overeat.”
D.
* “One glass of wine can be ingested with a meal and is counted as two fat exchanges.”
E.
No any answer is correct
14.
The patient with type 1 diabetes mellitus is switching from an animal-source regular insulin to a synthetically derived human regular insulin. Which precaution should the doctor explain to this patient?
A.
“Human insulin should only be administered in the umbilical area.”
B.
“Do not mix human regular insulin with any other type of insulin.”
C.
* “Adjustments in insulin timing may be needed with the human regular insulin.”
D.
“You may notice the need to increase the dose to achieve the same level of glucose control.”
E.
No any answer is correct
15.
The patient with type 2 diabetes had been taking the oral antidiabetic agents glyburide and metformin. These medications have been discontinued and he has now been prescribed to take Glucovance. He asks why he only needs one medication. What is the doctor’s best response?
A.
“Glucovance is more effective than glyburide and metformin.”
B.
* “Glucovance contains a combination of glyburide and metformin.”
C.
“Glucovance is a new oral insulin and replaces all other oral antidiabetic agents.”
D.
“Your diabetes is improving and you now only need one drug for blood glucose control.”
E.
No any answer is correct
16.
The patient with type 2 diabetes is prescribed to take the antidiabetic agent nateglinide.
Which statements made by the patient indicates correct understanding of this therapy?
A.
“I'll take this medicine with my meals.”
B.
* “I'll take this medicine 15 minutes before I eat.”
C.
“I'll take this medicine just before I go to bed.”
D.
“I'll take this medicine as soon as I wake up in the morning.”
E.
No any answer is correct
17.
The diabetic patient has severe peripheral neuropathy, resulting in numbness and reduced sensation. Which intervention should the doctor teach the patient to prevent injury as a result of this complication?
A.
“Examine your feet daily.”
B.
“Rotate your insulin injection sites.”
C.
“Wear white socks instead of colored socks.”
D.
* “Use a bath thermometer to test water temperature.”
E.
No any answer is correct
18.
The home care doctor administers a cup of orange juice to the patient with diabetes who is experiencing symptoms of a mild hypoglycemic episode. The patient's clinical manifestations have not changed 5 minutes later. What is the doctor’s best next action?
A.
* Administer an additional a cup of orange juice.
B.
Document the finding as the only action.
C.
Administer 10 units of regular insulin.
D.
Notify the physician.
E.
No any answer is correct
19.
The home care doctor administers a cup of orange juice to the patient with diabetes who is experiencing symptoms of a mild hypoglycemic episode. The patient's clinical manifestations have not changed 5 minutes later. What is the doctor’s best next action?
A.
* Administer an additional ? cup of orange juice.
B.
Document the finding as the only action.
C.
Administer 10 units of regular insulin.
D.
Notify the physician.
E.
No any answer is correct
20.
What instruction should the doctor emphasize when teaching the diabetic patient about how to alter diabetes management during a period of illness that includes nausea and vomiting.
A.
“Continue your prescribed exercise regimen.”
B.
“Avoid eating or drinking to reduce vomiting.”
C.
“Do not use insulin or take your oral antidiabetic agent.”
D.
* “Monitor your blood glucose levels at least every 4 hours.”
E.
No any answer is correct
21.
A 54-year-old woman complains of increasing fatigue and easy bruising of 3 weeks’ duration. Physical findings included pale, scattered ecchymoses and petechiae and mild hepatosplenomegaly. CBC\: RBC – 2.550.000/mcL; Hb – 73 g/L; HCT 20\%; PLT –
23.000/mcL; and WBC – 162.000/mcL with 82\% blasts, that contained Auric rods; peroxidase stain was positive; What is the most probable diagnosis?
A.
* Acute leukemia
B.
Chronic leukemia
C.
Thrombocytopenia
D.
Hemolytic anemia
E.
Megaloblastic anemia
22.
A 60-year-old man complains of fever, significant weight loss, bone and joint pain, and bleeding gums. On exam, paleness, lymphadenopathy, hepato- and splenomegaly. CBC\:
WBC – 270•109/L with 13\% lymphocytes, 1\% monocytes, 21\% basophiles, 29\% neutrophils, 9\% blasts, 12\% promyelocytes, 12\% myelocytes, 2\% metamyelocytes,
1\% eosinophils. ESR – 22 mm/h. Name the drug for treatment
A.
* Myelosan
B.
Prednisolone
C.
Cytosar
D.
Blood transfusion
E.
Vinblastine
23.
A client is scheduled for a mastectomy as part of her treatment for breast cancer. As she is about to receive the preoperative medication, she tells the nurse that she does not want to have her breast removed but wants a lumpectomy. Which response indicates that the nurse is acting as a client advocate?
A.
Telling the client that her surgeon is excellent and knows what is best for her condition
B.
* Calling the surgeon to come and explain all treatment options to the client
C.
Holding the client’s hand and offering to pray with her for a good outcome to the surgery
D.
Arranging to have the client be visited after surgery by a person who has had a successful mastectomy and is a long-term survivor of cancer
24.
A client with an aortic valve replacement is taking a daily dose of warfarin to prevent clot formation. The client states that he is also taking ginkgo biloba to improve his memory and concentration. What would be the nurse’s best response?
A.
Inform the client that memory problems following valve replacement surgery are common, but temporary.
B.
* Instruct the client that ginkgo biloba interacts with anticoagulant drugs and then check for bruising or bleeding.
C.
Inform the client that this drug combination is most effective if the ginkgo biloba is taken twice daily.
D.
Instruct the client to keep a record of episodes of forgetfulness or memory disturbances to monitor effectiveness.
25.
A patient is scheduled for a mastectomy as part of her treatment for breast cancer. As she is about to receive the preoperative medication, she tells the doctor that she does not want to have her breast removed but wants a lumpectomy. Which response indicates that the doctor is acting as a patient advocate?
A.
Telling the patient that her surgeon is excellent and knows what is best for her condition
B.
* Calling the surgeon to come and explain all treatment options to the patient
C.
Holding the patient’s hand and offering to pray with her for a good outcome to the surgery
D.
Arranging to have the patient be visited after surgery by a person who has had a successful mastectomy and is a long-term survivor of cancer
E.
All above mentioned
26.
A patient of 32 complains of severe weakness, tremor of extremities. Objective examination: body weight loss, wet & warm skin. The thyroid gland is enlarged up to the
3rd degree, painless, elastic. Pulse: 108. BP- 160\55 mmHg. Everything else is normal.
The diagnosis is:
A.
* Diffuse toxic goiter of the 3rd degree, thyrotoxicosis of the average degree
B.
Diffuse euthyroid goiter of the 3rd degree.
C.
Chronic autoimmune thyroiditis, hypertrophic type
D.
Chronic fibrous thyroiditis
E.
Toxiferous adenoma of the thyroid gland
27.
A patient of 32 complains of severe weakness, tremor of extremities. Objective examination\: body weight loss, wet & warm skin. The thyroid gland is enlarged up to the
3rd degree, painless, elastic. Pulse\: 108. BP- 160\55 mmHg. Everything else is normal.
The diagnosis is\:
A.
* Diffuse toxic goiter
B.
Diffuse euthyroid goiter
C.
Hypothyreosis
D.
Chronic fibrous thyroiditis
E.
Vegetovascular dystonia
28.
A patient with an aortic valve replacement is taking a daily dose of warfarin to prevent clot formation. The patient states that he is also taking ginkgo biloba to improve his memory and concentration. What would be the doctor’s best response?
A.
Inform the patient that memory problems following valve replacement surgery are common, but temporary.
B.
* Instruct the patient that ginkgo biloba interacts with anticoagulant drugs and then check for bruising or bleeding.
C.
Inform the patient that this drug combination is most effective if the ginkgo biloba is taken twice daily.
D.
Instruct the patient to keep a record of episodes of forgetfulness or memory disturbances to monitor effectiveness.
E.
All above mentioned
29.
A patient’s warfarin (Coumadin) therapy was discontinued 3 weeks ago. Which laboratory test result indicates that all effects of the warfarin have been eliminated?
A.
* International normalized ratio (INR) of 0.9
B.
Total white blood count of 9000/mm3
C.
Serum ferritin level of 350 ng/mL
D.
Reticulocyte count of 1%
E.
All above mentioned
30.
A student should assess patient’s facial expression. The patient’s face is amimic, edematous, external parts of eyebroves are lost. Which pathological condition this facial expression is typical for?
A.
toxic goitre;
B.
* hypothyreosis;
C.
lepra;
D.
Kushing’s syndrome;
E.
peritonitis.
31.
An African American client’s health history includes hypertension, diabetes, and heart disease. What major factor accounts for the increase in these diseases among some populations?
A.
* Lack of access to health care
B.
Medical insurance that fails to cover drug treatment
C.
Religious beliefs that conflict with health promotion activities
D.
Inconsistent adherence to medical regimens by African Americans
32.
An African American patient’s health history includes hypertension, diabetes, and heart disease. What major factor accounts for the increase in these diseases among some populations?
A.
* Lack of access to health care
B.
Medical insurance that fails to cover drug treatment
C.
Religious beliefs that conflict with health promotion activities
D.
Inconsistent adherence to medical regimens by African Americans
E.
All above mentioned
33.
During the routine inspection of teenager a blood test was made, in which were foun the foloowing data of leucocytes formula: young – 3 %, stab neutrophil – 10 %. Which cells of granulocytic row are normally in the perypheric blood flow?
A.
Young
B.
* Stab neutrophil
C.
Myelocytes
D.
Promielocites
E.
Metamyelocyte
34.
In patient T., 30 years old iron-deficiency anemia was found, confirmed by laboratory blood test. Specify the most typical complaints for iron deficiency.
A.
Loss of tactile sensation
B.
Graying of hair
C.
* Fragility of nails
D.
Labial fissure
E.
Anosmia
35.
On the second postoperative day after a subtotal thyroidectomy, the patient tells the doctor that he feels numbness and tingling around the mouth. What is the doctor’s best first action?
A.
Offer mouth care.
B.
Loosen the dressing.
C.
* Notify the physician.
D.
Document the finding as the only action.
E.
All above mentioned
36.
On the second postoperative day after a subtotal thyroidectomy, the client tells the nurse that he feels numbness and tingling around the mouth. What is the nurse’s best first action?
A.
Offer mouth care.
B.
Loosen the dressing.
C.
* Notify the physician.
D.
Document the finding as the only action.
37.
On the second postoperative day after a subtotal thyroidectomy, the patient tells the doctor that he feels numbness and tingling around the mouth. What a doctor may suspect in the patient?
A.
Thyrotoxic crisis.
B.
Hypothyreoid coma
C.
* Disfunction of parathyroid glands
D.
Brain stroke
E.
Hypertonic crisis
38.
Patient 40 years old has massive uterine bleeding. During inspection the signs of hypochromic anemia were found. Which research is specific for the assessment of treatment efficiency and regeneration function of the bone marrow?
A.
ESR
B.
Blood proteins
C.
Reticulocyte
D.
Form of erythrocytes
E.
* Serum iron
39.
Patient I. 40 years old, 5 years ago carried the resection of stomach concerning ulcerous illness. The expressed general weakness, shortness of breath, appeared lately. Blood test: er. 3,1x1012/l, Hb 60 grammes/l, CI 0,6, leukocytes 4,5x1012/l, eosynophiles 2%, stub
3%, segm. neutr. 5%, lymph. 32%, mon. 8%, ESR 5 mm/hour. What method of inspection will help in clarification of diagnosis?
A.
level of bilirubin
B.
level of glucose
C.
* level of serum iron
D.
level of kreatinine
E.
level of amylase
40.
Patient L., 46 years old, a woman, is inspected by a doctor. Data of inspection: the face is of intensive red colour, round (like Moon), hair growth is present on patient's chin and under the upper lip. Which disease this facial expressionis typical for?
A.
* Itsenko-Kushing's syndrome
B.
Thyrotoxicosis
C.
Mixedema
D.
Sclerodermia
E.
No any answer is correct.
41.
Patient S. 40 years old, is on the long-standing treatment in endocrinologial department.
Data of inspection: the face is puffy, amimic, eye slits ate narrowed, hair is abcent on the external parts of eyebroves, the nose and lips are enlarged, skin is pallid. Which disease is this facial expression typical for?
A.
Thyrotoxicosis
B.
Quinke's edema
C.
Acromegalia
D.
* Hypothyreosis
E.
No any answer is correct.
42.
Patient В.45 years old, a woman, was admitted to a hospital with complaints on palpitation, tremor of her hands. Data of examination: expression of fair on patient's face, eye sleats are widened, eyes are protruded. Which facial expression is observed in the patient?
A.
facies mitralis
B.
facies Hippocraticа
C.
* facies Basedovica
D.
facies febrilis
E.
No any answer is correct
43.
The client in a rehabilitation program has been using the bladder training techniques of the Valsalva and Crede maneuvers. When a nurse catheterizes this client immediately after voiding, the residual volume is 50 mL. What is the nurse’s best action?
A.
Notify the physician.
B.
Insert an indwelling catheter.
C.
* Document the finding as the only action.
D.
Modify or extend the bladder-training program.
44.
The client is scheduled for a functional assessment using the Functional Independence
Measure (FIM). He asks the nurse, “What is the purpose of the FIM?” What is the nurse’s best response?
A.
“It is a tool that is used to determine your level of independence.”
B.
“It measures how you should be able to perform various tasks.”
C.
* “It is a tool to measure the severity of your disability.”
D.
“It is a test the nurse manager uses to determine staffing patterns.”
45.
The client scheduled for a partial thyroidectomy for hyperthyroidism asks the nurse why she is being given an iodine preparation before surgery. What is the nurse’s best response?
A.
“To make the surgery as sterile as possible.”
B.
“To stimulate storage of thyroid hormones for use after surgery.”
C.
“To replace the thyroid hormones that will be eliminated as a result of the surgery.”
D.
* “To decrease the blood vessels in the thyroid and prevent excessive bleeding during surgery.”
46.
The client who is a paraplegic is scheduled to participate in a rehabilitation program. She tells her nurse, “I don't understand why I should do rehabilitation. After all, my paralysis will not go away nor will it get better.” What is the nurse’s best response?
A.
“Your doctor, one of the best in the specialty, ordered rehabilitation, and he does know what is best for you.”
B.
“When new discoveries are made regarding paraplegia, people in rehabilitation programs will benefit first.”
C.
* “Rehabilitation will teach you how to maintain the functional ability you have.”
D.
“You are right. I will cancel the orders for rehabilitation.”
47.
The client, a Jehovah’s Witness scheduled for surgery, has expressed concern that she might receive blood products, an act condemned by her religion. What is the nurse’s best response?
A.
“You should allow the health care professionals to do whatever is needed to save your life.”
B.
“If you are worried about contamination, the blood supply in this country is the safest in the world.”
C.
“I will have the hospital chaplain come and interpret the Bible for you to show you that there really is nothing unacceptable in a blood transfusion.”
D.
* “Transfusions are not routine and now there are good alternatives to transfusions if you should lose an excessive amount of blood.”
48.
The doctor has just completed an interview and physical examination of a newly admitted patient. What sources of information should this doctor use in formulating expected outcomes for the patient?
A.
* Identified nursing diagnoses and collaborative problems
B.
The goals for the patient as set by family members
C.
The medical history and laboratory test results
D.
Patient goals as set by the nursing staff
E.
All above mentioned
49.
The doctor is performing passive range-of-joint motion exercises on a semiconscious patient and meets resistance while attempting to extend the right elbow more than 45 degrees. What is the doctor’s best action?
A.
Splint the joint and continue the passive range of motion to the shoulder only.
B.
Progressively increase the joint motion 5 degrees beyond the resistance each day.
C.
Apply weights to the right distal extremity before initiating any joint exercise.
D.
* Move the joint only to the point at which resistance is met.
E.
All above mentioned
50.
The doctor notes that the reddened area on the heel of a bedridden patient is smaller 24 hours after placing a padded booty on the heel. What phase of the nursing process is reflected in the doctor’s action?
A.
Analysis
B.
Planning
C.
Implementation
D.
* Evaluation
E.
All above mentioned
51.
The nurse has just completed an interview and physical examination of a newly admitted client. What sources of information should this nurse use in formulating expected outcomes for the client?
A.
* Identified nursing diagnoses and collaborative problems
B.
The goals for the client as set by family members
C.
The medical history and laboratory test results
D.
Client goals as set by the nursing staff
52.
The nurse is performing passive range-of-joint motion exercises on a semiconscious client and meets resistance while attempting to extend the right elbow more than 45 degrees. What is the nurse’s best action?
A.
Splint the joint and continue the passive range of motion to the shoulder only.
B.
Progressively increase the joint motion 5 degrees beyond the resistance each day.
C.
Apply weights to the right distal extremity before initiating any joint exercise.
D.
* Move the joint only to the point at which resistance is met.
53.
The nurse notes that the reddened area on the heel of a bedridden client is smaller 24 hours after placing a padded booty on the heel. What phase of the nursing process is reflected in the nurse’s action?
A.
Analysis
B.
Planning
C.
Implementation
D.
* Evaluation
54.
The patient asks his doctor why he was told to avoid aspirin and other salicylates for 2 weeks before surgery. What is the doctor’s best response?
A.
“These drugs can counteract the effects of certain anesthetics.”
B.
* “These drugs decrease platelet aggregation and increase your risk for excessive bleeding.”
C.
“These drugs are toxic to white blood cells and increase your risk for developing an infection.”
D.
“These drugs inhibit the bone marrow from making new blood cells and increase your risk for anemia.”
E.
All above mentioned
55.
The patient in a rehabilitation program has been using the bladder training techniques of the Valsalva and Crede maneuvers. When a doctor catheterizes this patient immediately after voiding, the residual volume is 50 mL. What is the doctor’s best action?
A.
Notify the physician.
B.
Insert an indwelling catheter.
C.
* Document the finding as the only action.
D.
Modify or extend the bladder-training program.
E.
All above mentioned
56.
The patient is scheduled for a functional assessment using the Functional Independence
Measure (FIM). He asks the doctor, “What is the purpose of the FIM?” What is the doctor’s best response?
A.
“It is a tool that is used to determine your level of independence.”
B.
“It measures how you should be able to perform various tasks.”
C.
* “It is a tool to measure the severity of your disability.”
D.
“It is a test the doctor manager uses to determine staffing patterns.”
E.
All above mentioned
57.
The patient scheduled for a partial thyroidectomy for hyperthyroidism asks the doctor why she is being given an iodine preparation before surgery. What is the doctor’s best response?
A.
“To make the surgery as sterile as possible.”
B.
“To stimulate storage of thyroid hormones for use after surgery.”
C.
“To replace the thyroid hormones that will be eliminated as a result of the surgery.”
D.
* “To decrease the blood vessels in the thyroid and prevent excessive bleeding during surgery.”
E.
All above mentioned
58.
The patient who is a paraplegic is scheduled to participate in a rehabilitation program.
She tells her doctor, “I don't understand why I should do rehabilitation. After all, my paralysis will not go away nor will it get better.” What is the doctor’s best response?
A.
“Your doctor, one of the best in the specialty, ordered rehabilitation, and he does know what is best for you.”
B.
“When new discoveries are made regarding paraplegia, people in rehabilitation programs will benefit first.”
C.
* “Rehabilitation will teach you how to maintain the functional ability you have.”
D.
“You are right. I will cancel the orders for rehabilitation.”
E.
All above mentioned
59.
The patient with hyperthyroidism is taking lithium carbonate to inhibit thyroid hormone release. Which of the following patient reports alerts the doctor to side effects of this therapy?
A.
Blurred vision
B.
* Increased thirst and urination
C.
Increased sweating and diarrhea
D.
Decreased attention span and insomnia
E.
All above mentioned
60.
The patient, a Jehovah’s Witness scheduled for surgery, has expressed concern that she might receive blood products, an act condemned by her religion. What is the doctor’s best response?
A.
“You should allow the health care professionals to do whatever is needed to save your life.”
B.
“If you are worried about contamination, the blood supply in this country is the safest in the world.”
C.
“I will have the hospital chaplain come and interpret the Bible for you to show you that there really is nothing unacceptable in a blood transfusion.”
D.
* “Transfusions are not routine and now there are good alternatives to transfusions if you should lose an excessive amount of blood.”
E.
All above mentioned
61.
What instruction should be given to a client with decreased cardiac output from an old myocardial infarction who now needs to engage in a rehabilitation program after a total knee replacement?
A.
“You must take prophylactic antibiotics just before engaging in the planned exercise.”
B.
* “You must take prophylactic nitroglycerin just before engaging in the planned exercise.”
C.
“You must take prophylactic analgesics just before engaging in the planned exercise.”
D.
“You must take prophylactic potassium chloride just before engaging in the planned exercise.”
62.
What instruction should be given to a patient with decreased cardiac output from an old myocardial infarction who now needs to engage in a rehabilitation program after a total knee replacement?
A.
“You must take prophylactic antibiotics just before engaging in the planned exercise.”
B.
* “You must take prophylactic nitroglycerin just before engaging in the planned exercise.”
C.
“You must take prophylactic analgesics just before engaging in the planned exercise.”
D.
“You must take prophylactic potassium chloride just before engaging in the planned exercise.”
E.
All above mentioned
63.
When taking the blood pressure of a client after a parathyroidectomy, the nurse notes that the client's hand has gone into flexion contractions. What is the nurse’s interpretation of this observation?
A.
Hypokalemia
B.
Hyperkalemia
C.
Hyponatremia
D.
* Hypocalcemia
64.
When taking the blood pressure of a patient after a parathyroidectomy, the doctor notes that the patient's hand has gone into flexion contractions. What is the doctor’s interpretation of this observation?
A.
Hypokalemia
B.
Hyperkalemia
C.
Hyponatremia
D.
* Hypocalcemia
E.
All above mentioned
65.
A patient complains of gingival bleedings,incraesed body temperature till 38`C,marked general weakness.He feels himself sick for the recent 2weeks.Data of objective examination,petectnia on the skin,by palpation enlarged submandibular axillary and femoral lymph nodes.Data of CBC: thrombocytes-120000/l, Le-18,6 .10`9/l, blast cels-
80%, ESR-36 mm/hr. Acute leucaemia is diagnosed. What is the main treatment for this disease?
A.
corticosteroides
B.
radiotherapy
C.
* chemiotherapy
D.
surgical therapy
E.
immunostimulators
66.
A patient complains of gingival bleedings,incraesed body temperature till 38`C,marked general weakness.He feels himself sick for the recent 2weeks.Data of objective examination,petectnia on the skin,by palpation enlarged submandibular axillary and
femoral lymph nodes.Data of CBC: thrombocytes-120000/l, Le-18,6 .10`9/l, blast cels-
80%, ESR-36 mm/hr. Acute leucaemia is diagnosed. Which symptoms indicate on hemorrhagic syndrome?
A.
* petectnia,gingival bleeding,low account of thrombocytes
B.
general weakness,fever
C.
enlarged lymph nodes,decreased amount of RBC,thrombocytes,blast cells in CBC
D.
all mentioned
E.
no correct answer.
67.
A patient complains of gingival bleedings,incraesed body temperature till 38`C,marked general weakness.He feels himself sick for the recent 2weeks.Data of objective examination,petectnia on the skin,by palpation enlarged submandibular axillary and femoral lymph nodes.Data of CBC: thrombocytes-120000/l, Le-18,6 .10`9/l, blast cels-
80%, ESR-36 mm/hr. Acute leucaemia is diagnosed. Which symptom indicate an intoxication syndrome?
A.
petechnia, gingival bleeding, low account of thrombocytes
B.
* general weakness,fever
C.
enlarged lymph nodes,decreased amount of RBC,thrombocytes,blast cells in CBC
D.
all mentioned
E.
no correct answer.
68.
A patient complains of gingival bleedings,incraesed body temperature till 38`C,marked general weakness.He feels himself sick for the recent 2weeks.Data of objective examination,petectnia on the skin,by palpation enlarged submandibular axillary and femoral lymph nodes.Data of CBC: thrombocytes-120000/l, Le-18,6 .10`9/l, blast cels-
80%, ESR-36 mm/hr. Acute leucaemia is diagnosed. Which symptoms indicate a malignant proliferation?
A.
petechnia, gingival bleeding, low account of thrombocytes
B.
general weakness,fever
C.
* enlarged lymph nodes,decreased amount of RBC,thrombocytes,blast cells in
CBC
D.
all mentioned
E.
no correct answer.
69.
A patient complains of pain in the lumbar region, dark urine, weakness, dizziness. These symptoms arise after usage of aspirin and ampicillin. Data of objective examination: skin pallor, subicteric sclera. Ps-90 per min, liver +2cm, spleen +3cm, painful in palpation.
Data of CBC :er-2,2.10 9/l, Hb-60g/l.CI-0,5, Le-9,4.10`9/l,basophil-0,5%,e-3%,stub-
6%,lymph-25%,mon-7%, ESR-38mm/hr, reticulocytes-24%. Biochemical blood study: bilirubin common-38mmol/l. Which preparation is it necessary to prescribe to prevent renal failure?
A.
Isotonic saline solution
B.
* 4% sodium solution
C.
glucose solution
D.
7% potassium solution
E.
transfusion of blood.
70.
A patient suffers of peptic ulcer for more than 5 years. The last exacerberation starts
1week ago.Since the last evening the patient has noticed dissappearance of pain. Data of examination:moderate severity,skin is pale and covered with cold sweat. BP is 105/70mm of Hg. PS-105 per min. Which hematologic problem may arise in the patient in 3days?
A.
* acute posthemorrhagic anaemia
B.
chronic iron-defficiency anaemia
C.
chronic vitamin B12-defficiency anaemia
D.
hemolypic anaemia
E.
aplastic anaemia
71.
A patient suffers of peptic ulcer with exacerbations in autumn and spring seasons for more than 5 years. The last exacerberation starts 2 month ago withn periodical tarry stools. Data of examination:moderate severity,skin is pale and covered with cold sweat.
BP is 105/70mm of Hg. PS-105 per min. Which hematologic problem developed in the patient?
A.
acute posthemorrhagic anaemia
B.
* chronic iron-defficiency anaemia
C.
chronic vitamin B12-defficiency anaemia
D.
hemolypic anaemia
E.
aplastic anaemia
72.
A 25-year-old woman complained of fatigue, hair loss, and brittle nails. On exam, pallor of skin, PR of 94/min, BP of 110/70 mm Hg. On blood cell count, Hb of 90 g/L, RBC
3.5·1012/L, color index of 0.7, ESR of 20 mm/h. Serum iron level was 8.7 mcmol/L. what treatment would you initiate?
A.
* Ferrous sulfate orally
B.
Iron dextrin injections
C.
Vitamin B12 intramuscularly
D.
Blood transfusion
E.
Packed RBCs transfusion
73.
A 32 -year-old welder complains of weakness and fever. His illness started as tonsillitis a month before. On exam, BT of 38.9°C, RR of 24/min, HR of 100/min, BP of 100/70 mm
Hg, hemorrhages on the legs, enlargement of the lymph nodes. CBC shows Hb of 70 g/L,
RBC of 2.2·1012/L, WBC of 3.0·109/L with 32\% of blasts, 1\% of eosinophiles, 3\% of bands, 36\% of segments, 20\% of lymphocytes, and 8\% of monocytes, ESR of 47 mm/h. What is the cause of anemia?
A.
* Acute leukemia
B.
Chronic lympholeukemia
C.
Aplastic anema
D.
Vitamin B12 deficiency anemia
E.
Chronic hemolytic anemia
74.
A 54-year-old woman complains of increasing fatigue and easy bruising of 3 weeks’ duration. Physical findings included pale, scattered ecchymoses and petechiae and mild hepatosplenomegaly. CBC: RBC – 2.550.000/mcL; Hb – 73 g/L; HCT 20\%; PLT –
23.000/mcL; and WBC – 162.000/mcL with 82\% blasts, that contained Auric rods; peroxidase stain was positive; What is the most probable diagnosis?
A.
* Acute leukemia
B.
Chronic leukemia
C.
Thrombocytopenia
D.
Hemolytic anemia
E.
Megaloblastic anemia
75.
A male 23 y.o used sulfanilamides per. os. In last 2 days before examination he noticed marked weakness, high body temperature, nausea, vomiting, abdominal pain, discharge of dark urine . Data of objective examination: jaundice of skin and mucosa, splenomegaly
.Data of CBC: Hb 50g/l reticulocites 25percents, erythrocytes contain Haintz-Erlish’s bodies. Besides it was revealed glucose-6-phosphat dehydrogenates deficiency in erythrocytes. Which disease is it possible to suspect?
A.
congenital iron –deficiency anemia
B.
congenital myerospherocytosis
C.
* congenital hemolytic anemia
D.
talassemia to 0.6p deficiency
E.
circle-cell anemia
76.
A male 23 y.o used sulfanilamides per. os. In last 2 days before examination he noticed marked weakness, high body temperature, nausea, vomiting, abdominal pain, discharge of dark urine . Data of objective examination: jaundice of skin and mucosa, splenomegaly
.Data of CBC: Hb 50g/l reticulocites 25percents, erythrocytes contain Haintz-Erlish’s bodies. Besides it was revealed glucose-6-phosphat dehydrogenates deficiency in erythrocytes. Conginetal hemolytic anemia is diagnosed. Where actually hemolysis develops in this disease?
A.
* in liver and spleen
B.
in lymph nodes
C.
in vascular bed
D.
in bone marrow
E.
in kidney
77.
A male 23 y.o used sulfanilamides per. os. In last 2 days before examination he noticed marked weakness, high body temperature, nausea, vomiting, abdominal pain, discharge of dark urine . Conginetal hemolytic anemia is diagnosed. Which organ affection with followed failure most often develops in acute hemolysis?
A.
* kidneys
B.
liver
C.
spleen
D.
stomach
E.
lungs
78.
A patient complains of gingival bleedings,incraesed body temperature till 38`C,marked general weakness.He feels himself sick for the recent 2weeks.Data of objective examination,petectnia on the skin,by palpation enlarged submandibular axillary and femoral lymph nodes.Data of CBC: erythrocythes-2,1.10 9/l,Hb-80g/l, thrombocytes-
120000/l, Le-18,6 .10`9/l, l%,stub-2%,segm-9%, lymph-5%, mon-3%, blast cels-80%,
ESR-36mm/hr.Which disease has developed in the patient:
A.
* acute leukaemia
B.
chronic leukaemia
C.
hemolytic anaemia
D.
vitamin B12-deficiency anaemia
E.
symptom of dysseminated hypercoagulation
79.
A patient complains of gingival bleedings,incraesed body temperature till 38`C,marked general weakness.He feels himself sick for the recent 2weeks.Data of objective examination,petectnia on the skin,by palpation enlarged submandibular axillary and femoral lymph nodes.Data of CBC: erythrocythes-2,1.10 9/l,Hb-80g/l, thrombocytes-
120000/l, Le-18,6 .10`9/l, l%,stub-2%,segm-9%, lymph-5%, mon-3%, blast cels-80%,
ESR-36mm/hr.Which data of CBC directly proves diagnosis of acute leucaemia?
A.
erythocytes 2,1.10`12/l
B.
thrombocytes-120000/l
C.
leukocytes 18,6.10`9/l
D.
ESR-36mm/hr
E.
* blast cells 80%
80.
A patient complains of pain in the lumbar region, dark urine, weakness, dizziness. These symptoms arise after usage of aspirin and ampicillin. Data of objective examination: skin pallor, subicteric sclera. Ps-90 per min, liver +2cm, spleen +3cm, painful in palpation.
Data of CBC :er-2,2.10 9/l, Hb-60g/l.CI-0,5, Le-9,4.10`9/l,basophil-0,5%,e-3%,stub-
6%,lymph-25%,mon-7%, ESR-38mm/hr, reticulocytes-24%. Biochemical blood study: bilirubin common-38mmol/l. Which complication developed in the patient?
A.
* acquired autoimmune hemolytic anaemia
B.
congenital hemolytic anaemia
C.
vitamin B12-defficiency anaemia
D.
toxic hepatitis
E.
urolithiasis
81.
A patient had stomach resection a year ago. He complains of general weakness, giddiness. Blood count: Er 2,6 g/L, Hb 80 g/L, C.ind 0.7, L – 3.7 g/L, reticulocytes 1\%, segm 56\%, lymp 34\%, mon. 6\%, ESR 17 mm/hour. Erythrocytes are hypochromic; there are anisocytosis & poikilo-cytosis. Fe of serum 5 mkmol/L. Diagnosis is:
A.
* Iron-deficiency anemia
B.
B12-deficiency anemia
C.
Сhronic myeloleukosis
D.
Aplastic anemia
E.
Chronic lymphoid leukosis
82.
A patient suffers of peptic mucous disease for more than 5 years. The last exacerberation starts 1week ago.Since the last evening the patient has noticed dissappearance of pain.
Data of examination:moderate severity,skin is pale and covered with cold sweat. BP is
105/70mm of Hg. PS-105 per min. Which examination is necessary to prescribe for verification of diagnosis?
A.
* analysis of faeces for scant/hidden blood
B.
ionogram
C.
coagulation
D.
CBC
E.
ECG
83.
A patient who suffers from postheamorrhagic anemia was treated with tardiferon. within five weeks. Now erythrocytes and hemoglobin contents correspond to norm. Is it necessary to continue treatment?
A.
no
B.
* yes if serum iron and indexes from metabolism are lower than normal
C.
yes but choose another drug
D.
all answers are wrong
E.
it is necessary to check other criteria’s of cbc
84.
A patient who suffers from postheamorrhagic anemia was treated with tardiferon. within five weeks. Now erythrocytes and hemoglobin contents correspond to norm. which criteria of lab test are necessary to check to ensure that it is possible to check treatment?
A.
erythrocyte count
B.
hemoglobin content
C.
CI and ESR
D.
* serum iron and indexes of its metabolism
E.
serum bilirubin
85.
A patient who suffers from postheamorrhagic anemia was treated with tardiferon. Now erythrocytes and hemoglobin contents are normal. How long treatment with iron preparation should last?
A.
11-5 months
B.
3-4 weeks
C.
5-6 weeks
D.
* 2-3 months
E.
7-8 months
86.
A patient, 26yrs old, noticed periodical jaundice within her life. After severe exercises, she felt pain in muscles and upper part of abdomen. Next day usually moderate jaundice developed, dark feces and urine. Data of objective examinations: moderate enlargement of liver and spleen. Data of CBC: erythrocytes-2,8.1012/l, Hb-80g/l, Ci-0,9, reticulocytes-15%, leucocytes-9,5.109/l, ESR-20mm/hr, thrombocytes-230.109/l,
Bilirubin 60micmol/l, direct bilirubin-8micmol/l. Which disease is present?
A.
* hemolytic anemia
B.
calculous cholecystitis
C.
Leptospirosis
D.
Iron-deficiency anemia
E.
Chronic hepatitis
87.
A patient, 26yrs old, noticed periodical jaundice within her life. After severe exercises, she felt pain in muscles and upper part of abdomen. Next day usually moderate jaundice developed, dark feces and urine. Data of objective examinations: moderate enlargement of liver and spleen. Data of CBC: erythrocytes-2,8.1012/l, Hb-80g/l, Ci-0,9, reticulocytes-15%, leucocytes-9,5.109/l, ESR-20mm/hr, thrombocytes-230.109/l,
Bilirubin 60micmol/l, direct bilirubin-8micmol/l. Which type of anemia is present?
A.
iron-deficiency anemia
B.
vitamin B12 deficiency anemia
C.
* congenital hemolytic anemia
D.
acquired hemolytic anemia
E.
no correct answer
88.
A patient, 35yrs old, complains of weakness, palpitation, flickering before eyes, dizziness. He has peptic ulcer in anamnesis. Data of examination: skin palor, vesicular breathing in lungs, systolic murmur at heart apex, pulse rate-100/min, BP-100/70 mm of
Hg. Data of CBC: erythrocytes-3,2.1012/l, Hb-75g/l CI-0,7. Which type of anemia is present?
A.
posthemorrhagic anemia
B.
sideroblastic anemia
C.
thalassemia
D.
* iron-deficiency anemia
E.
hyperchromic anemia
89.
A patient, 35yrs old, complains of weakness, palpitation, flickering before eyes, dizziness. He has peptic ulcer in anamnesis. Data of examination: skin palor, vesicular breathing in lungs, systolic murmur at heart apex, pulse rate-100/min, BP-100/70 mm of
Hg. Data of CBC: erythrocytes-3,2.1012/l, Hb-75g/l CI-0,7. What is probable cause of anemia in this case?
A.
decreased iron absorption
B.
* periodical blood loss
C.
invasion of helmints
D.
newgrows
E.
Poor iron content in diet
90.
A patient, 40yrs old, complains of weakness, fragility of nails, loss of hair. He has duodenal ulcer in anamnesis. Data of fibrogastroscopy: duodenal deformation because of scars. Data of CBC: erythrocytes-3,6.1012/l, Hb-90g/l, CI-0,7, serum iron-8,7micmol/l.
What is the pathogenesis of anemia in this case?
A.
increased iron consumption
B.
increased excretion of iron
C.
* permanent loss of iron
D.
deranged transport of iron
E.
decreased absorption of iron
91.
A patient, 40yrs old, complains of weakness, fragility of nails, loss of hair. He has duodenal ulcer in anamnesis. Data of fibrogastroscopy: duodenal deformation because of scars. Data of CBC: erythrocytes-3,6.1012/l, Hb-90g/l, CI-0,7, serum iron-
8,7micmol/l.What treatment is necessary to prescribe?
A.
* enteral administration of iron preparations
B.
parenteral administration of iron preparations
C.
vitamin B12 parenterally
D.
folic acid
E.
ascorbic acid
92.
A patient, 48yrs old, suffers from prolonged menses with severe discharge of blood. Last
3months she complained of general weakness, dizziness, attacks of palpitation, flickering before eyes. Data of examinations: skin pallor, fragility of nails. On ECG, extrasystoly is recorded. Data of CBC: erythrocytes-2,8.1012/l, Hb-76g/l, CI-0,7, anisocytosis, poikilocytosis. ESR-4mm/hr. What is diagnosis?
A.
hemophilia
B.
* iron-deficiency anemia
C.
myocarditis
D.
hemolytic anemia
E.
cardioneurosis
93.
A patient, 48yrs old, suffers from prolonged menses with severe discharge of blood. Last
3months she complained of general weakness, dizziness, attacks of palpitation, flickering before eyes. Data of examinations: skin pallor, fragility of nails. On ECG, extrasystoly is recorded. Data of CBC: erythrocytes-2,8.1012/l, Hb-96g/l, CI-0,7, anisocytosis, poikilocytosis. ESR-4mm/hr. What is the cause of anemia?
A.
* blood loss
B.
poor iron consumption in diet
C.
poor iron absorption
D.
increased iron excretion with urine
E.
helminthic invasion
94.
A patient, 55yrs old, complains of pain in sternal bone and in ribs. 6 months ago he had pathological fracture of the left shin. Data of lab tests: protein-110g/l, positive Mgradient. Bence Jones protein is present in urine. Which disease is present?
A.
radiculitis
B.
proteinuria
C.
* plasma cell myeloma
D.
osteochondrosis
E.
angina pectoris
95.
A patient, 55yrs old, complains of pain in sternal bone and in ribs. 6 months ago he had pathological fracture of the left shin. Data of lab tests: protein-110g/l, positive Mgradient. The patient is suspected plasma cell myeloma. Which rest is necessary to prescribe?
A.
CBC
B.
Biochemical blood study
C.
* Determination of Bence Jones protein in urine
D.
X-ray of ribs
E.
CT of the chest
96.
A patient, 60yrs old, complains of general weakness, fatigue, parestesia in limbs. He had resection of stomach 3years ago because of peptic ulcer. Data of examination: the tongue is of raspberry colour and smooth, the patient is not stable in Romberg’s position. Data of
CBC: erythrocytes-2,5.1012/l, Hb-88g/l CI-1,3, macrocytosis. What disease is present?
A.
* vitamin B12 deficiency anemia
B.
iron-deficiency anemia
C.
hemolytic anemia
D.
hypochromic anemia
E.
hyperchromic anemia
97.
A patient, 60yrs old, complains of general weakness, fatigue, parestesia in limbs. He had resection of stomach 3years ago because of peptic ulcer. Data of examination: the tongue is of raspberry colour and smooth, the patient is not stable in Romberg’s position. The patient is diagnosed vitamin B12 deficiency anemia. How do you explain parestesia?
A.
affection of central nervous system
B.
* affection of perypheral nervous system
C.
dystension of skin
D.
affection of subcutaneous fat
E.
all mentioned
98.
A patient,35yrs old, who suffers of autoimmune gastritis and vitamin B12-deficiency anemia, presents signs of funicular myelosis. Data of CBC: erythrocyte-2,2.1012/l, Hb-
80g/l, LC-2,4.109/l, ESR-40mm/hr, direct bilirubin-8,6micmol/l, indirect bilirubin-
27micmol/l. What is probable reason of funicular myelosis?
A.
prolonged hypoxia of nervous system
B.
increased bilirubin content in blood serum
C.
* accumulation of propionic and methylmalonic acids n blood serum
D.
infection contamination due to leukaemia
E.
malnutrition due to gastritis
99.
A patient,35yrs old, who suffers of autoimmune gastritis and vitamin B12-deficiency anemia, presents signs of funicular myelosis. Data of CBC: erythrocyte-2,2.1012/l, Hb-
80g/l, LC-2,4.109/l, ESR-40mm/hr, direct bilirubin-8,6micmol/l, indirect bilirubin-
27micmol/l. What is funicular myelosis?
A.
* demyelinization of posteriolateral columns of spinal cord
B.
demyelinization of anterior columns of spinal cord
C.
affection of brain cortex
D.
demyelinization of peripheral nerves of lower limbs
100.
E.
no correct answer
A patient,35yrs old, who suffers of autoimmune gastritis and vitamin B12deficiency anemia, presents signs of funicular myelosis. Data of CBC: erythrocyte-
2,2.1012/l, Hb-80g/l, LC-2,4.109/l, ESR-40mm/hr, direct bilirubin-8,6micmol/l, indirect bilirubin-27micmol/l. Which substance is not produced with patient’s gastric mucosa responsible for vitamin B12 absorption in intestine?
A.
full hydrochloric acid
B.
combined hydrochloric acid
C.
pepsin
D.
* gastromucoprotein
101.
E.
lactic acid
A wonan, 38 y.o. suffers from menorrhagias. She complains of flickering before eyes, dizziness, skin dryness, loosing of hairs. Data of ovjective exaiation: paleness of skin and mucosa . Pulse is 100 per min , rrhythmic . Liver and spleen are not enlarged .
Data of CBC: Hb 90 g / l , er . 3,3х10 9/ l , CI - 0,7, reticulocites .1,2%, leuc .4,8х10 9/l , eosyn .2%, stub 3%, segmented 70%, lymphocites 25%, monocites 10%. Serum iron 4,2
102.
mkmol / l . Which treatment is it necessary to prescribe?
A.
Folic acid
B.
* Iron preparations
C.
Vitamin B12
D.
Glucocorticoids
E.
All mentioned
During assessment of a patient at risk for hematologic problems, the doctor palpates the patient's spleen just below the ribs on the left side. What is correct interpretation of obtained results?
A.
Norm
B.
* Splenomegaly
C.
Decreased sizes of spleen
D.
This is not spleen but the left kidney
E.
This is not spleen but descending colon
103.
During the routine inspection of teenager a blood test was made, in which were found leucocytes: young – 3 %, stab neutrophils – 10 %. Which cells of granulocytic row are normally in a blood flow?
A.
Young
B.
* Stab neutrophil
C.
Myelocytes
D.
Promielociti
104.
E.
Metamyelocyte
In a patient, 17yrs old, congenital spherocytosis anemia (Minkorwsky-Shauffard’s disease) was diagnosed. What is the mechanism of hemolysis?
A.
* membranopathy
B.
hemoglobinopathy
C.
autoimmune affection
D.
immunopathy
105.
E.
bone marrow hypoplasia
In a patient, 17yrs old, congenital spherocytosis anemia (Minkorwsky-Shauffard’s disease) was diagnosed. Which type of anemia is it?
A.
macrocytic
B.
megaloblastic
C.
* microspherocytic
D.
normocytic
106.
E.
no correct answer
In a patient, 30yrs old, aplastic anemia was diagnosed. What is pathogenesis of anemia?
A.
membranopathy
B.
hemoglobinopathy
C.
autoimmune affection of erythrocytes
D.
affection of erythrocytes by immune complexes
107.
E.
* bone marrow affection
In patient B 46 y.o whos suffers of chronic obstructive pulmonary disease for 15 years, in CBC it was revealed that erythrocytes account is equal to 4,5 .1012/l. there are no other changes in CBC and bone marrow punctate. What is the correct interpretation of obtained results?
A.
normal RBC level
B.
absolute erythrocytosis( erythramia)
C.
number of RBCis increased, because of increased circulating blood volume.
D.
*This is relative erythrocytosis for compensation of chronic hypoxia
E.
All answers are correct
108.
In patient B 46 y.o who suffers of chronic obstructive pulmonary disease for 15 years, in CBC it was revealed that erythrocytes account is equal to 4,5 .1012/l. there are no other changes in CBC and bone marrow puncture. Select the main mechanism of
109.
erythrocytosis in chronic hypoxia in patients with bronchopulmonary diseases:
A.
.intensified erythropoyesis
B.
increased hemopoyetic function of kidneys
C.
increased blood viscosity
D.
* erythrocytes enter perypheric circulation from depot
E.
dilution of blood.
In patient M, 32yrs old, acquired hemolytic anemia had developed after usage of aspirin. What is the mechanism of hemolysis?
A.
membranopathy
B.
hemoglobinopathy
C.
autoimmune affection of erythrocytes
D.
* affection of erythrocytes by immune complexes
E.
bone marrow affection
110.
In patient S, 20yrs old, glucose-6-phosphate dehydrogenase deficiency anemia was diagnosed. What is the cause of hemolysis?
A.
membranopathy
B.
* haemoglobinopathy
C.
autoimmune affection
D.
immunopathy
E.
bone marrow hypoplasia
111.
In patient S, 20yrs old, glucose-6-phosphate dehydrogenase deficiency anemia was diagnosed. Which type of anemia is it?
A.
macrocytic
B.
megaloblastic
C.
microspherocytic
D.
* normocytic
E.
no correct answer
112.
In patient S, 42yrs old, who suffers fro scleroderma for 15years, anemia was diagnosed. What is the pathogenesis?
A.
membranopathy
B.
hemoglobinopathy
C.
* Autoimmune affection
113.
D.
affection of erythrocytes by immune complexes
E.
bone marrow affection
In patient who suffers for duodenal ulcer complains of general weakness, dyspnoe in insignificant physical load and desire to eat a chalk. Data of objective examination: skin paleness, throphic changes of skin. CBC: erythrocytes 3,3.1012/l Hb 90g/l Ci-0,75, reticulocytes-2%, serum iron-5,6 micmol/l. Which pathological condition takes place?
A.
erythremia
B.
hemolytic anemia
C.
* iron-deficiency anemia
D.
aplastic anemia
114.
E.
vitamin B12 deficiency anemia
In patient who suffers for duodenal ulcer complains of general weakness, dyspnoe in insignificant physical load and desire to eat a chalk. Data of objective examination: skin paleness, throphic changes of skin. CBC: erythrocytes 3,3.1012/l Hb 90g/l Ci-0,75, reticulocytes-2%, serum iron-5,6 micmol/l. Which diet will you prescribe for the patient?
A.
low fat diet
B.
* enriched with meat and fruits
C.
enriched with milk products
D.
enriched with vegetables
E.
restriction of salt intake
115.
In complete blood count (CBC) of a patient it was found out that the concentration of haemoglobin is 92 gramm/l, CI 0,8. A patient is undergone treatment concerning irondefficiency anaemia. Which other changes are characteristic in CBC in this disease?
A.
Presence of microcytes and megalocites
B.
Toxic grittiness of leucocytes
C.
Blast cells
D.
* Anisocytosis, poikylocytosis, microcytosis
116.
E.
Changes will not be
Older adult patient is receiving the third unit of packed red blood cells that have been administered in the last 8 hours. One hour into the third transfusion, a doctor
observes the patient to have distended neck veins in the sitting position. What is the doctor’s best first action?
A.
* Slow the infusion rate.
B.
Discontinue the transfusion.
C.
Document the observation as the only action.
D.
Check the type of infusing blood with the patient's blood type.
E.
All above mentioned
117.
Patient 38 y.o., complains on weakness, dizziness, dyspnea, burning of tongue.
During examination there were found the signs of folic acid-deficiency anemia. What kind of tongue does this patient have?
A.
* Geographical
B.
coated with yellow tint
C.
Coated with grey fur
D.
Clean
118.
E.
Swollen
Patient 38 years old, who suffers of pernicious anemia for 20 years, complains on weakness, dizziness, dyspnea, burning of tongue. What kind of tongue does this patient
119.
have?
A.
Coated with yellow tint
B.
* Brilliant and smooth
C.
Coated with grey fur
D.
Clean
E.
Swollen
Patient 38 years old complains on weakness, dizziness, dyspnea, burning of tongue. During examination were found the signs of folic acid-deficiency anemia. In which diseases usually this type of anemia develops?
A.
* Chronic liver diseases
B.
Chronic kidney diseases
C.
Diseases of a stomach
D.
Affection of bone marrow
E.
Infectious diseases
120.
Patient 38 years old complains on weakness, dizziness, dyspnea, burning of tongue. During examination were found the signs of folic acid-deficiency anemia. In which diseases usually this type of anemia develops?
A.
* Chronic diseases of intestine
B.
Chronic kidney diseases
C.
Diseases of a stomach
D.
Affection of bone marrow
121.
E.
Infectious diseases
Patient 43 y.o, complains of increased body tempreture till 36.6oC, sweating,skin itching. By palpation there were revealed enlarged lymph nodes; neck, axillary, inguinal; they are of 1-2 cm in diameter, solid, painless, movable. Data of CBC; erythrocytes –
4,0.1012/l, hb 136 g/l, Lc 10.10 g/l, basophiles 0%, eosinophiles 6%, stub neutrophiles
10% segmented 65%, lymphocytes 14%, monocytes 3%, ESR 58 mm/hr. Which
122.
pathological condition is present?
A.
mediastinitis
B.
* lymphogranulomatosis
C.
chronic lympholeucosis
D.
acute leukemia
E.
sepsis
Patient 43 y.o, complains of increased body tempreture till 36.6oC, sweating,skin itching. Enlarged liver and spleen, jaundice of skin and mouth. The lower spleen border
is 3cm below the nevel. The lymph nodes are not enlarged. In CBC there are a lot of immature granulocytes( juvenile, plasma cells). Blast are absent in peripheral blood.
Which pathological condition is present?
A.
acute leukemia
B.
* chronic myloleucosis
C.
hronic lympholeucosis
D.
lympogranulomatosis
123.
E.
liver cirrhosis.
Patient B, 25yrs old complains of weakness, dizziness, hemorrhagic rash on the skin. She is ill for the last month. Data of CBC: erythrocytes- 1,0. 1012/l, Hb-30g/l, CI-
0,9, LC-1,2.109/l, thrombocytes-42.109/l. How to make interpretation of these results/
A.
depression of red cells stem
B.
depression of white cells stem
C.
depression of thrombocytes
D.
decreased Hb content in erythrocytes
E.
*depression of all bone marrow stems
124.
Patient B, 25yrs old complains of weakness, dizziness, hemorrhagic rash on the skin. She is ill for the last month. Data of CBC: erythrocytes- 1,0. 1012/l, Hb-30g/l, CI-
0,9, LC-1,2.109/l, thrombocytes-42.109/l. Which examination method is the most informative in verification of diagnosis?
A.
lymph node biopsy
B.
* sternal puncture
C.
biopsy of spleen
D.
biopsy of liver
125.
E.
pleurocentesis
Patient B. has fallen sick at the usage of biseptol. He developed disuria, jaundice with skin pallor, splenomegaly. Data of CBC: er-2,2.10`12/l, HB-60g/l, CI- 0,82, Le-
14.10`9/l, retinolocytes-24%. Indirect serum bilirubin-35mmol/l. Urine and feces are dark, contain increased concentration of stercobilin. What is prescribed diagnosis?
A.
iron-deficiency
B.
* hemolytic anaemia
C.
toxic hepatitis
D.
acute leukaemia
E.
vitamin B12 defficiency anaemia
126.
Patient B. has fallen sick at the usage of biseptol. He developed disuria, jaundice with skin pallor, splenomegaly. Data of CBC: er-2,2.10`12/l, HB-60g/l, CI- 0,82, Le-
14.10`9/l, retinolocytes-24%. Indirect serum bilirubin-35mmol/l. Urine and feces are dark, contain increased concentration of stercobilin. What is the mechanism of hemolysis?
A.
membranopathy
B.
hemoglobinopathy
C.
* immune-allergic reaction
D.
tone marror hypoplasia
E.
all mentioned
127.
Patient I., 40 y.o., 5 years ago carried the resection of stomach concerning ulcerous illness. Now he has developed exacerbation. The expressed general weakness, shortness of breath, appeared lately. Iron-deficiency anemia is diagnosed. What way of introduction of preparations of iron is most acceptable in this case?
A.
per os
B.
per rectum
C.
* parenterally
D.
inhalation
E.
through a skin
128.
Patient I., 40 y.o., 5 years ago carried the resection of stomach concerning ulcerous illness. The expressed general weakness, shortness of breath, appeared lately.
Blood test: erythr. 3,1x1012/l, HB 60 gramms/l, CI 0,6, Leuk. 4,5x109/l, e 2%, stab 3%, segmented 5%, lymph. 32%, mon. 8%, ESR 5 mm/hr. What method of inspection will help in clarification of diagnosis?
A.
level of bilirubin
B.
level of glucose
C.
* level of serum iron
D.
level of kreatinine
E.
level of amylase
129.
Patient, 62yrs old, is hospitalized with complaints of enlargement of neck, subclavian and axillary lymph nodes, general weakness, increased sweating, subfebrile body temperature within the last 3months. Data of CBC: LC-64.109/l, lymphocytes-72%.
130.
Which examination method is necessary for diagnosis?
A.
computer tomography
B.
* myelogram
C.
Lymphography
D.
Lymphosintigraphy
E.
X-ray
Patient, 62yrs old, is hospitalized with complaints of enlargement of neck, subclavian and axillary lymph nodes, general weakness, increased sweating, subfebrile body temperature within the last 3months. Data of CBC: LC-64.109/l, lymphocytes-72%.
Blast cells 1-2%. Which disease is possible to suspect?
A.
vitamin B12-deficiency anemia
B.
plasma cell myeloma
C.
* acutre leukaemia
D.
chronic leukaemia
131.
E.
mononucleosis
Patients P., a female, feels general and muscular weakness,dyspnoe, dizziness, fragidity of hair and nails, desire to eat chalk, She had uterine fibromyoma in the past.
Data of CBC :2,8.10`12/l, HB-105g/l, CI-0.78, anisocytosis, poikilocytosis, serum iron-
10mmmol/l. Which diagnosis is prescribed?
A.
talassemia
B.
aplastic anaemia
C.
* iron-defficiency anaemia
D.
vitamin B12-defficiency anaemia
E.
autoimmune hemolytic anaemia
132.
The patient is receiving a unit of packed red blood cells. Fifteen minutes into the infusion, the patient is cyanotic and complains of chest pain. What is the doctor’s best first action?
A.
Administer oxygen.
B.
* Stop the transfusion.
C.
Call the emergency team.
D.
Increase the infusion flow rate.
E.
All above mentioned
133.
The patient who has been diagnosed with Hodgkin's lymphoma is scheduled for numerous tests. The patient asks if these tests are really necessary, because the exact type of cancer has already been established. What is the doctor’s best response?
A.
“You may be eligible for new and experimental therapy. These tests will determine whether or not you would qualify for such treatment.”
B.
* “It is best to determine how healthy your major organs are before undergoing the strenuous and uncomfortable therapies for cancer.”
C.
“Different treatments are used depending on where the cancer is, so it is first necessary to determine the exact sites.”
D.
“The doctors want to be very sure, because it is possible to have two different kinds of cancer at the same time.”
E.
All above mentioned
134.
The patient with lymphoma asks his doctor why his disease treatment regimen includes radiation and surgery as well as chemotherapy, when his 16-year-old female cousin only had chemotherapy for leukemia. What is the doctor’s best response?
A.
“Radiation is not used as therapy in girls and women so as not to disrupt their childbearing ability.”
B.
* “Lymphomas can form discrete tumors that can be removed by surgery or treated locally with radiation, but leukemic cells are more widespread.”
C.
“Your disease is probably more widespread and advanced than your cousin's was, requiring additional types of intensive therapy for cure.”
D.
“Lymphomas can be cured using multiple therapies and leukemia cannot be cured, only controlled with lifelong injections of chemotherapy.”
E.
All above mentioned
135.
Within the last year, a patient complained of weakness, fatigue, sweating, dry cough. 1month ago, he had severe herpes infection. Data of present examination:enlarged lymph nodes in the neck, in axillary region. The lymph nodes are slightly dense and painless. Data of CBC: leucocytes-4,0.109/l, lymphocytes-80%. Which examination should be performed in first line?
A.
biochemical blood study
B.
biopsy of enlarged lymph nodes
C.
blood immunogra
D.
chest x-ray
136.
E.
* sternal puncture
Within the last year, a patient complained of weakness, fatigue, sweating, dry cough. 1month ago, he had severe herpes infection. Data of present examination:enlarged lymph nodes in the neck, in axillary region. The lymph nodes are slightly dense and painless. Data of CBC: leucocytes-4,0.109/l, lymphocytes-80%. Chronic lympholeucosis was diagnosed. Which properties of lymph nodes are typical for this disease?
A.
mild, elastic, painful
B.
mild, elastic, painless
C.
* solid, painful
D.
solid, painless
137.
E.
not enlarged
A 20- year-old patient with a history of preceding streptococcal infection complains of malaise, headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of 100/min, RR of 20/min, the urinalysis showed increased protein, red cell casts and hyaline casts. What is your diagnosis?
A.
* Acute glomerulonephritis
B.
Acute pyelonephritis
C.
Rheumatic fever
D.
Essential hypertension
E.
Bacterial endocarditis
138.
A 20- year-old patient with a history of preceding streptococcal infection complains of malaise, headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of 100/min, RR of 20/min. Acute glomerulonephritis is diagnosed. Which data of urianalyses are typical for the disease?
A.
* increased protein, erythrocytes and hyaline and wax casts
B.
increased protein, and hyaline casts
C.
leucocyturia, granular casts
D.
Crystals of uric acid salts in urine
139.
E.
No correct answer
A 20- year-old patient with a history of preceding streptococcal infection complains of malaise, headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of 100/min, RR of 20/min. Acute glomerulonephritis is diagnosed. Which level of protein in urine is typical for the disease?
A.
0,03 g/l
B.
0,03-1 g/l
C.
1-2 g/l
D.
2-3 g/l
E.
* More than 3 g/l
140.
A 20- year-old patient with a history of preceding streptococcal infection complains of malaise, headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of 100/min, RR of 20/min. Acute glomerulonephritis is
141.
diagnosed. What is the type of the disease according to its pathogenesis?
A.
* Immunoallergic
B.
Allergic
C.
Authoimmune
D.
Infectious
E.
Dysthrophic
A 20- year-old patient with a history of preceding streptococcal infection complains of malaise, headache, anorexia, subfebrile fever. On exam, mild generalized edema, BP of 150/90 mm Hg, HR of 100/min, RR of 20/min. Acute glomerulonephritis is diagnosed. Which is main in treatment of the disease?
A.
Antibiotics
B.
* Glucocortecoids
C.
Immunodepressants
D.
Diuretics
142.
E.
Calcium channel antagonists
A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating, aching pain in lumbar area, a discomfort in urination, and frequent voiding. Pasternatsky’s sigh is positive in both sides. On lab exam, WBC of 20.000/mcL; on urinalysis protein of 0.6g/L, leukocyturia, bacteriuria. Your preliminary diagnosis.
A.
* Acute pyelonephritis
B.
Exacerbation pf chronic pyelonephritis
C.
Acute glomerulonephritis
D.
Acute cystitis
E.
Nephrolithiasis
143.
A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating, aching pain in lumbar area, a discomfort in urination, and frequent voiding. Pasternatsky’s sigh is positive in both sides. Acute pyelonephritis is diagnosed.
144.
Which data of urianalyses are typical for the disease?
A.
increased protein, erythrocytes and hyaline and wax casts
B.
* protein in low concentration leukocyturia, bacteriuria
C.
leucocyturia, granular casts
D.
Crystals of uric acid salts in urine
E.
No correct answer
A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating, aching pain in lumbar area, a discomfort in urination, and frequent
voiding. Pasternatsky’s sigh is positive in both sides. Acute pyelonephritis is diagnosed.
Which level of protein in urine is typical for the disease?
A.
No protein in urine
B.
* 0,03-1 g/l
C.
1-2 g/l
D.
2-3 g/l
E.
More than 3 g/l
145.
A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating, aching pain in lumbar area, a discomfort in urination, and frequent voiding. Pasternatsky’s sigh is positive in both sides. Acute pyelonephritis is diagnosed.
What is the type of the disease according to its pathogenesis?
A.
Immunoallergic
B.
Allergic
C.
Authoimmune
D.
* Infectious
E.
Dysthrophic
146.
A 29-year-old woman is critically ill. The illness was manifested by high fever, chills, sweating, aching pain in lumbar area, a discomfort in urination, and frequent voiding. Pasternatsky’s sigh is positive in both sides. Acute pyelonephritis is diagnosed.
Which is main in treatment of the disease?
A.
* Antibiotics
B.
Glucocortecoids
C.
Immunodepressants
D.
Diuretics
147.
E.
Calcium channel antagonists
A 40-year-old man complained of headache in occipital area. On physical examination, the skin was pale; there was face and hand edema, blood pressure of
170/130 mm Hg. On EchoCG, there was concentric hypertrophy of the left ventricle.
Ultrasound examination of the kidneys revealed thinned cortical layer. Urinalysis showed proteinuria of 3.5 g/day. What is the diagnosis?
A.
* Chronic glomerulonephritis.
B.
Essential arterial hypertension.
C.
Chronic pyelonephritis.
D.
Polycystic disease of the kidneys.
E.
Cushing’s disease.
148.
A 40-year-old man complained of headache in occipital area. Chronic right-sided pyelonephritis was diagnosed. Ultrasound examination of the kidneys was performed.
149.
Which results should be expected?
A.
Thin kidney parenchyma because of sclerosis on both sides symmetrically
B.
* Thin kidney parenchyma because of sclerosis on right side
C.
Stones in calicies
D.
Swelling of kidney parenchyma
E.
Polycystosis
A 40-year-old man complained of headache in occipital area. On physical examination, the skin was pale; there was face and hand edema, blood pressure of
170/130 mm Hg. Acute glomerulonephritis was diagnosed. Ultrasound examination of the kidneys was performed. Which results should be expected?
A.
Thin kidney parenchyma because of sclerosis on both sides symmetrically
B.
Thin kidney parenchyma because of sclerosis on one side
C.
Stones in calicies
D.
* Swelling of kidney parenchyma on both sides symmetrically
E.
Polycystosis
150.
A 40-year-old man complained of headache in occipital area. On physical examination, the skin was pale; there was face and hand edema, blood pressure of
170/130 mm Hg. Acute glomerulonephritis was diagnosed. Which complication of the disease may develop?
A.
* Acute renal failure
B.
Chronic renal failure
C.
Toxic shock
D.
Bleeding
E.
All mentioned
151.
A 40-year-old man complained of headache in occipital area. On physical examination, the skin was pale; there was face and hand edema, blood pressure of
170/130 mm Hg. Chronic glomerulonephritis was diagnosed. Ultrasound examination of the kidneys was performed. Which results should be expected?
A.
* Thin kidney parenchyma because of sclerosis on both sides symmetrically
B.
Thin kidney parenchyma because of sclerosis on one side
C.
Stones in calicies
D.
Ellarged calicies
E.
Swelling of kidney parenchyma
152.
A 40-year-old man complained of headache in occipital area. On physical examination, the skin was pale; there was face and hand edema, blood pressure of
170/130 mm Hg. Chronic glomerulonephritis was diagnosed. Which complication of the
153.
disease may develop?
A.
Acute renal failure
B.
* Chronic renal failure
C.
Toxic shock
D.
Bleeding
E.
All mentioned
A 40-year-old man complained of headache in occipital area. On physical examination, the skin was pale; there was face and hand edema, blood pressure of
220/130 mm Hg. Acute glomerulonephritis was diagnosed. Which complication of the disease may develop?
A.
Acute renal failure
B.
Chronic renal failure
C.
Toxic shock
D.
Bleeding
E.
* Hypertonic crisis
154.
A man, aged 25, presents with facial edema, moderate back pains, body temperature of 37,5 С, BP 180/100 mmHg, hematuria [ up to 100 in v/f], proteinuria [2,0 g/L], hyaline casts - 10 in v/f., specific gravity -1020. The onset of the disease is probably connected with acute tonsillitis 2 weeks ago. The most likely diagnosis is:
A.
* Acute glomerulonephritis
B.
Acute pyelonephritis
C.
Cancer of the kidney
D.
Urolithiasis
E.
Chronic glomerulonephritis
155.
A man, aged 25, presents with facial edema, moderate back pains, body temperature of 37,5 С, BP 180/100 mmHg, hematuria [ up to 100 in v/f], proteinuria [2,0 g/L], hyaline casts - 10 in v/f., specific gravity -1020. The onset of the disease is probably connected with acute pharyngitis 2 weeks ago. Which microorganism is the causative agent of the disease?
A.
* Beta-hemolythic streptococcus, type A
B.
Pneumococcus
156.
C.
Mycoplasma
D.
Influenza virus
E.
Multiple bacterial microflora
At sick E., 42 y.o.., what is 8 years ill with chronic glomerulonephritis, complains
157.
of head pains, nausea, vomit, itch of skin. What changes will be in blood?
A.
Increases bilirubin;
B.
* increased kreatinine;
C.
decline of ESR;
D.
increase of cholesterol
E.
increase of transaminases.
At sick E., 52 y.o., what is ill with chronic pyelonephritis, biochemical blood test
158.
is conducted. What changes can be?
A.
increase of level of glucose in blood;
B.
increase of bilirubin;
C.
* increase of kreatinine;
D.
decline of alfa-amylase
E.
increase of alkaline phosphatase.
?During palpation of kidneys the following was revealed: it is possible to palpate all the kidney, it is easly displaceble, but does not move to the opposite side of the body.
Which degree of nephroptosis is present?
A.
I;
B.
* II;
C.
III;
D.
IV;
159.
E.
total nephroptosis.
During palpation of kidneys the following was revealed: it is possible to palpate all the kidney in iliac region, it is easly displaceble, move to the opposite side of the
160.
body. Which degree of nephroptosis is present?
A.
I
B.
II
C.
* III
D.
IV;
E.
total nephroptosis.
During palpation of kidneys the following was revealed: it is possible to palpate all the kidney, it is easly displaceble, but does not move to the opposite side of the body.
Which degree of nephroptosis is present?
A.
I;
B.
* II;
C.
III;
D.
IV;
E.
total nephroptosis.
161.
During palpation of kidneys the following was revealed: it is possible to palpate the lower kidney pole, it is not displaceble, but does not move to the opposite side of the body. Which degree of nephroptosis is present?
A.
* I
B.
II
C.
III
D.
IV;
162.
E.
total nephroptosis.
During research of patient’s urine the faoolwing findings were revealed: 5-6 leucocytes are found in 1 vision field, single fresh red corpuscles in 1 vision field. What research must be appointed a patient for clarification of diagnosis?
A.
Complete blood count;
B.
ECG;
C.
* Nechiporenko’s test;
D.
Zimnicki’s test
163.
E.
determination of daily proteinuria.
For a patient A., 30 years old., urine is taken for analysis. There found out a lot of changed red cells in the urine (1/2 of every vision field). What is the possible cause of
164.
their origin in the urine?
A.
* acute glomerulonephritis;
B.
Uncomplicated urolithiasis;
C.
acute cystitis;
D.
paranephritis;
E.
cancer of urinary bladder.
For a patient E., 38 y.o.., there are attack-like pains in a counter-clockwise lumbar
165.
area, which irradiate downward. About this what disease can testify?
A.
acute glomerulonephritis;
B.
* urolithiasis;
C.
hypernephroma;
D.
chronic glomerulonephritis;
E.
heart attack.
For a patient E., 38 y.o.., there are attack-like pains in the left lumbar area, which
166.
irradiate downward to internal surface of thighs and perineum. How is this pain called?
A.
* Urocolick
B.
Biliary colick
C.
Intestinal colick
D.
Spasmodic pain
E.
Dull boring pain
For patient A., who sufers of acute glomerulonephritis, it was found out violation of kidneys concentration function. Which pathological changes in kidneys cause renal failure in this disease?
A.
glomerular sclerosis
B.
tubular sclerosis
C.
* edema of kidney parenchyma
D.
obturation of tubuli with destroyed erythrocytes
167.
E.
No correct answer
For patient E., 52 years old, ill with chronic pyelonephritis for 12 years, biochemical blood test is conducted. Increased creatinine is found. Excretion of which
168.
metabolites is affected to produces intoxication in renal failure?
A.
* Proteins metabolites
B.
Carbohydrates metabolites
C.
Fats metabolites
D.
Uric acid salts
E.
All mentioned
In 34-year-old woman acute pyelonephritis is diagnosed. What should be the main
169.
principle of her diet?
A.
Restriction of proteins (beans) and water
B.
* Restriction of proteins (beans), spicy food
C.
Restriction of fats
D.
Restriction of products containing uric acid
E.
Increased caloric supplement
In 34-year-old woman chronic renal failure is diagnosed. What should be the main principle of her diet?
A.
* Restriction of proteins (beans) and water
B.
Restriction of proteins (beans), spicy food
C.
Restriction of fats
D.
Restriction of products containing uric acid
170.
E.
Increased caloric supplement
In patient A. chronic pyelonephritis was diagnosed. Which laboratory test is useful for assessment kidney filtration function?
A.
Complete blood count;
B.
Nechyporenko’s test;
C.
Canalicular reabsorption
D.
* Clearance by endogenous creatinine
171.
E.
determination of daily proteinuria.
In patient A. chronic renal failure was diagnosed. Which laboratory test is useful for assessment kidney concentration function?
A.
Complete blood count;
B.
Nechyporenko’s test;
C.
* Canalicular reabsorption
D.
Clearance by endogenous creatinine (glomerular filtration)
172.
E.
determination of daily proteinuria.
In patient A. a chronic pyelonephritis was diagnosed. Which laboratory test is useful for assessment kidney concentration function?
A.
Complete blood count;
B.
ECG;
C.
Nechiporenko’s test;
D.
* Zimnicki’s test
173.
E.
determination of daily proteinuria.
In patient E., 38 y.o.., hypercreatininemia was revealed. Reberg’s test is performed for him. What is the purpose of its execution?
A.
to reveal which part of urinary system is the source of hematuria or leukocyturia,
B.
* estimation of kidney concentration function
C.
for calculation of formed elements (red cells, leukocytes, casts) in urine with the method of Kakovsky-Addis
174.
D.
for determination of diuresis
E.
for determination of the amount of albumen in urine.
In patient E., 38 y.o.., leucocyturia was revealed. Tompson’s test is performed
(tree-glass test) for him. What is the purpose of its execution?
A.
* to reveal which part of urinary system is the source of hematuria or leukocyturia,
B.
estimation of kidney concentration function
C.
for calculation of formed elements (red cells, leukocytes, casts) in urine
D.
for determination of diuresis
175.
E.
for determination of the amount of albumen in urine.
In patient E., 38 y.o.., leucocyturia was revealed. Tompson’s test is performed
(tree-glass test) for him. What is the sourse of leucocyturia if leucocites are mainly present in I portion of urine?
A.
* Urethra
B.
Kidney
C.
A bladder
D.
Urethers
E.
rectum
176.
In patient E., 38 y.o.., leucocyturia was revealed. Tompson’s test is performed
(tree-glass test) for him. What is the sourse of leucocyturia if leucocites are mainly present in II portion of urine?
A.
Urethra
B.
* Kidney
C.
A bladder
D.
Urethers
177.
E.
rectum
In patient E., 38 y.o.., leucocyturia was revealed. Tompson’s test is performed
(tree-glass test) for him. What is the sourse of leukocyturia if leucocites are mainly present in III portion of urine?
A.
Urethra
B.
Kidney
C.
* A bladder
D.
Urethers
178.
E.
rectum
In patient E., 38 y.o.., leukocyturia was revealed. Nechyporenko’s test is performed for him. What is the purpose of its execution?
A.
to reveal which part of urinary system is the source of hematuria or leukocyturia,
B.
estimation of kidney concentration function
C.
* for calculation of formed elements (red cells, leukocytes, casts) in urine with the method of Kakovsky-Addis
D.
for determination of diuresis
E.
for determination of the amount of albumen in urine.
179.
In patient I., 54 years old, urocolick is diagnosed. What position does patient with urocolick assume?
A.
On affected side with legs bended hip and knee joints and by the leg pressed to the stomach from the side of affection
B.
Semirecumbent position with lowered legs (orthopnoe)
C.
Lying on a sick side
D.
* Restless
180.
E.
Sitting, bending forward.
In patient I., 54 years old, urocolick is diagnosed. Which irradiation is typical for this type of pain?
A.
* Downward to internal surface of thighs and perineum
B.
Upward to the right scapula
C.
Toward the neck
D.
Toward the navel
181.
E.
No irradiation
In the complete blood count of a patient it was found that the concentration of haemoglobin is 92 g/l, CI 0,8. A patient treats himself concerning of iron-deficiency
182.
anaemia. What changes are characteristic in the complete blood count in this disease?
A.
Presence of microcytes and megalocites
B.
Toxic grittiness of leucocytes
C.
Blast cells
D.
* nisocytosis, poikilocytosis, microcytosis
E.
Changes are abcent
Patient A., 35 years old, is troubled with appearance of sediment in his urine which make the urine cloudy but disappear in an hour. Appearance of what matter in urine can you suspect?
A.
* Salts;
B.
protein;
C.
bilious pigments;
D.
glucose;
E.
urinary acid.
183.
Patient A., 35 years old, is troubled with appearance of sediment in his urine which make the urine cloudy and don’t disappear in an hour. Appearance of what matter in urine can you suspect?
A.
Salts;
B.
* protein;
C.
bilious pigments;
D.
glucose;
E.
urinary acid.
184.
Patient A., 35 years old, is troubled with increased amount of urine excreted per day. During exami ation is was revealed that urine specific gravity is increased.
Appearance of what matter in urine makes its gravity increased?
A.
Salts;
B.
protein;
C.
bilious pigments;
D.
* glucose;
185.
E.
urinary acid.
Patient E. 48 years old., is ill with chronic pyelonephritis for 10 years. What changes in biochemical blood test do indicate on kidney insufficiency?
A.
albuminemia;
B.
beta-lipoproteinaemia;
C.
hyperbilirubinemia;
D.
* creatininemia
E.
dysproteinemia.
186.
Patient E. has renal failure. By physical examination it was revealed swelling of subcutaneous tissue of whole the body. Accumulation of liquid in subcutaneous fat tissue on whole the body is called:
A.
Ascites
B.
* Anasarca
C.
Hives
D.
Pleurisy
E.
Pericarditis
187.
Patient E. has terminal stage of renal failure. By physical examination it was revealed swelling of subcutaneous tissue of whole the body. What is location of edema in initial stages of kidney affection?
A.
* Below eyes
B.
On lower limbs
C.
On upper limbs
D.
In lumbar region
188.
E.
In abdominal cavity
Patient E., 38 y.o. has urocolick: there are attack-like pains in the left lumbar area, which irradiate downward to internal surface of thighs and perineum. How is this pain
189.
called? What is pathological mechanism of this pain?
A.
* Obstruction of urine outflow from the kidney
B.
Inflammaltion of kidney parenchyma
C.
Inflammaltion of kidney calicies
D.
Inflammaltion of paranephral tissues
E.
No correct answer
Patient M. experiensed pyelonephritis. What laboratory sign is the most characteristic for this pathology?
A.
* active leucocytes in urine;
B.
considerable proteinuria;
C.
uraturia;
D.
oxalaturia;
E.
glucosuria.
190.
Patient M., 27 years old, entered clinic with complaints on edema under eyes, increase of body temperature up to 37,8 degree of Сelsium, discoloration of urine. 2
191.
weeks ago he had quinsy. What research must be conducted?
A.
ECG;
B.
* General analysis of urine;
C.
Chest X-ray;
D.
Ultrasound of a heart
E.
Esophagogastroduodenoscopy.
Patient M., 27 years old, is ill for 7 years with chronic glomerulonephritis. Kidney insufficiency was diagnosed in him 2 years ago. Name possible changes of cardiovascular system?
A.
Systolic murmur on teh apex;
B.
weakening of II heart sound above an aorta;
C.
* heart sounds are weakened, possibly appearance of pericardial friction
D.
breaking up I heart sound on an apex
E.
“gun tone of Strazhesko”.
192.
Patient M., 52 years old., experienced edema. Acute glomerulonephritis was diaghnosed. What is the pattern of edema in this disease?
A.
appear in the evening;
B.
first appear on lower extremities;
C.
first appear on overhead extremities;
D.
* appear on face in the morning;
E.
Early development of anasarca.
193.
Patient O., 26 years old, complains of appearance of edema in the morning, it is located mainly on her face (eyeleads). Which pathology is present in this case?
A.
ardiovascular
B.
Neurological
C.
* Urinary system pathology
D.
Respiratory system pathology
194.
E.
No right answer
Patient P., 38 y.o.., was fallen ill with nephritis. What color of urine must be in this sick?
A.
red;
B.
* color of «meat wastes»;
C.
color of beer;
D.
sulphur
195.
E.
straw-yellow.
Patient R. who suffers of chronic glomerulonephritis for 2 years complains of headache, weakness, fever, discharge of cloudy urine. Which test is useful in diagnostics?
A.
Biochemical blood study;
B.
ECG;
C.
* Nechyporenko’s test;
D.
Zimnicki’s test
196.
E.
determination of daily proteinuria.
Patient R. who suffers of chronic glomerulonephritis for 2 years complains of poliuria, headache, weakness. Which test is useful in assessment of kidney function?
A.
Complete blood count;
B.
ECG;
C.
Nechyporenko’s test;
D.
* Zimnicki’s test
E.
determination of daily proteinuria.
197.
Patient S., 38 years old, grumbles about the unpleasant feelings in lumbar region, edema under eyes in the morning. She was fallen ill sharply 3 days before. 2 weeks ago the patient had viral respiratory infection. What inspection must be conducted?
A.
ECG;
B.
Ultrasound of a heart
C.
* general analysis of urine;
D.
determination of cholesterol in blood
198.
E.
Chest X-ray.
Patient T., 48 years old, has an attack of kidney eclampsia. What is pathogenesis of this condition?
A.
* Brain edema
B.
Affection of peripheral nerves
C.
Brain stroke
D.
Increased nerve irritation
199.
E.
All mentioned
Patient., 38 y.o. Research results of urine show 5-6 leucocytes in a vision field, single fresh red cells in a vision field. What research must be appointed for a patient for
200.
clarification of diagnosis?
A.
total blood count;
B.
ECG;
C.
* Nechiporenko's test
D.
Zimnicky's test
E.
determination of daily proteinuria.
Sick I., 26 y.o.., entered clinic with complaints on edema under eyes, increase of body temperature to 37,8 degree, discoloration of urine. 2 weeks ago he was ill with quinsy. What research must be conducted for assessment of kidney function?
A.
ECG;
B.
urinalysis;
C.
Chest X-ray;
D.
Ultrasound of a heart
201.
E.
* Biochemical blood study
Sick M., 27 y.o., is ill 7 years with chronic glomerulonephritis. Kidney insufficiency is diagnosed 2 years before. Name possible signs of pathological changes in
202.
cardiovascular system?
A.
Diastolic murmur on heart apex;
B.
weakening of second heart sound at aorta;
C.
* arterial hypertension
D.
intensified I heart sound at an apex
E.
gun tone of Strazhesko.
Sick N., grumbles about the unpleasant feelings in small of the back, oedematousness under eyes in the morning. Was fallen ill sharply 3 days back. 2 weeks ago he had influenza. What inspection must be conducted?
A.
ECG;
B.
Ultrasound of a heart;
C.
* total blood count;
D.
determination of cholesterol in blood
E.
X-ray of thorax.
Questins to pictures
1.
Fig.56. In which disease osmotic resistance of erythrocytes is reduced?
A.
*Minkovsky-Shoffar’s anaemia
B.
Hyperchromic anemia
C.
Hypochromic anemia
D.
Pernicious anemia
E.
Agranulocytosis
2.
Fig.59. In which anemia may be revealed enlargement of organ presented on the picture?
A.
Iron deficiency anemia
B.
*B12-deficiency anemia
C.
Normochromic anemia
D.
Hypochromic anemia
E.
Aplastic anemia
3.
Fig.56 What does the presence of the patient's blood count of red blood cells 12 mcm diameter indicate on?
A.
Leukemoid reactions
B.
*Megaloblastic anemia
C.
Acute leukemia
D.
Hemolytic anemia
E.
Aplastic anemia
4.
Fig.56 What is the most likely diagnosis in the patient with the size of red blood cells 12 microns?
A.
*B12-deficiency anemia
B.
Aplastic anemia
C.
Congenital hemolytic anemia
D.
Acquired hemolytic anemia
E.
Iron deficiency anemia
5.
Fig.56 What method of treatment of anemia is most appropriate in a patient with the size of red blood cells 12 microns?
A.
*Vitamin B12
B.
Iron preparations
C.
Blood
D.
Prednisolone
E.
Dysferal
6.
Fig.56 Appointment of which of the following drugs is most appropriate in a patient with the size of red blood cells 12 microns?
A.
Globiron
B.
Feroplex
C.
Prednisolone
D.
*Cyanocobalamin
E.
Lipoic acid
7.
Fig.56 What is the most likely diagnosis in the patient with the size of red blood cells 5 microns?
A.
Macrocytosis
B.
Normotsytois
C.
*Mikrotsytosis
D.
Poikilocytosis
E.
Fig.69 Anisocytosis
8.
At what anemia the presented on the picture organ is enlarged?
A.
*Hemolytic anemia
B.
Iron-deficiency anemia
C.
Folic acid deficiency anemia
D.
No correct answer
E.
Hypochromic anemia
9.
Which organ does the physician palpate in Figure 31?
A.
The right kidney
B.
The left kidney
C.
Pancreas
D.
*Spleen
E.
Stomach
10.
Where normally is it possible to palpate the organpresented in Figure 31?
A.
1 cm below the costal arch
B.
*It is not palpable innorm
C.
At 3 cm below the costal arch
D.
At 2 cm below the costal arch
E.
In the costal arch
11.
Palpation of which part of colon is shown in Figure 32?
A.
Caecum
B.
*Descending colon
C.
Transverse
D.
Ascending colon
E.
Sigmoid
12.
What is presented in Figure 32?
A.
*Palpation of the descending colon
B.
Palpation of the small intestine
C.
Palpation of the pancreas
D.
Percussion sigmoid
E.
Palpation of the sigmoid colon
13.
What method of examination is shown in Figure 33?
A.
sphygmogram
B.
Ultrasound of the heart
C.
Coronary angiography
D.
*Electrocardiography
E.
Phlebotonometry
14.
For the purpose to reveal pathology of some systems method of examination shown in
Figure 33 is commonly used. Which method is that?
A.
respiratory
B.
hepato-biliary
C.
urinary
D.
endocrine
E.
*Cardiovascular
15.
What changes can be revealed in the examination shown in Figure 33?
A.
Cardiac arrhythmia
B.
Signs hipertrofii vddiliv heart
C.
Conduction
D.
signs of cardiac ischemia myscul
E.
*All of the above
16.
Which number in Figure 34 shows the location of the pain in stomach ulcers?
A.
1
B.
3
C.
5
D.
6
E.
*2
17.
Which number in Figure 34 shows the location of the pain in duodenal ulcer?
A.
1.3
B.
2.6
C.
1.2
D.
7.8
E.
*4.5
18.
Which number in Figure 34 shows the location of the pain in chronic colitis?
A.
1.3
B.
2.7
C.
4.5
D.
1.2
E.
*6.9
19.
Which number in Figure 34 shows the location of the pain in chronic pancreatitis?
A.
2.6
B.
4.5
C.
1.2
D.
7.8
E.
*2.3
20.
Which number in Figure 34 shows the location of the pain in acute appendicitis?
A.
6
B.
5
C.
1
D.
8
E.
*7
21.
Which number in Figure 34 shows the location of the pain in cystitis?
A.
7
B.
5
C.
6
D.
2
E.
*8
22.
Which number in Figure 34 shows the location of the pain in hepatitis?
A.
2,3,5,6
B.
4,5,7,8
C.
5,6,8,9
D.
2,5,8,7
E.
*1,2,4,5
23.
What method of examination is shown in Fig. 35?
A.
Percussion
B.
Auscultation
C.
Inspection
D.
Instrumental
E.
*Palpation
24.
What research is conducted by a doctor (see Fig. 35)?
A.
*Determination of the upper border of the heart
B.
Determination of the right border of the heart
C.
Determination of the left border of the heart
D.
Determination of the width of vascular bundle
E.
Determination of width of Kroenig’s area
25.
Where in the norm is relative cardiac dullness border located, which is determined by the physician in Figure 35?
A.
At the level of the 2nd rib on the left side
B.
*At the level of the 3rd rib on the left side
C.
At the level of the 4th rib on the left side
D.
At the level of the 5th rib on the left side
E.
At the lower edge of the left clavicle
26.
Where in the norm is absolute cardiac dullness border located, which is determined by the physician in Figure 35?
A.
At the level of the 2nd rib on the left side
B.
At the level of the 3rd rib on the left side
C.
*At the level of the 4th rib on the left side
D.
At the level of the 5th rib on the left side
E.
At the lower edge of the left clavicle
27.
What forms the relative cardiac dullness border, which is determined by the physician in
Figure 35?
A.
Right atrium
B.
Pulmonary trunk
C.
Left ventricle
D.
*Left atrial auricle
E.
Right ventricle
28.
Which research method is shown in Figure 36?
A.
Inspection
B.
Sternal puncture
C.
Acupuncture
D.
Lumbar puncture
E.
*Pleurocentesis
29.
Manipulation presented in Figure 36 is used in the case of:
A.
Dry pleurisy
B.
Pneumothorax
C.
Bronchitis
D.
Emphysema
E.
*Pleural effusion
30.
Figure 36As the result of presented on the picture manipulation hemorrhagic fluid is obtained. What is the most likely diagnosis?
A.
Pulmonary hemorrhage
B.
Pneumothorax
C.
Chronic bronchitis
D.
Focal pneumonia
E.
*Lung tumor
31.
What is the diagnostic value of the research shown in Figure 36?
A.
Lets to determine the amount of accumulated fluid.
B.
Lets to evacuate free pleural cavity of fluid.
C.
Lets to assess the character of pleural contents
D.
Lets to calculate the number of blood form elements
E.
*All answers are correct
32.
Select the best place for manipulation presented in Figure 36.
A.
On the upper edge of the underlying rib in the V intercostal space.
B.
On the upper edge of the underlying rib in III intercostal space.
C.
*On the upper edge of the underlying rib in VI intercostal space
D.
On the upper edge of the underlying rib in VIII intercostal space
E.
On the upper edge of the underlying rib in VII intercostal space
33.
What complication may develop as a result of manipulation, shown in Figure 36?
A.
Pulmonary embolism
B.
Hydrothorax
C.
Lung abscess
D.
*Damage to the vascular nerve bundle
E.
Respiratory failure
34.
What research is conducted by a doctor shown in Fig. 37?
A.
Determination of the upper border of the heart
B.
*Determination of the right border of the heart
C.
Determination the left border of the heart
D.
Determination the width of vascular bundle
E.
Determination of Kroenig’s area width
35.
Where is the relative cardiac dullness border located in the norm, which determines the physician in Figure 37?
A.
In the second intercostal space along the right edge of the sternum
B.
In the fourth intercostal space 1 - 1.5 cm from the right edge of the sternum
C.
*In the third intercostal space along the right edge of the sternum
D.
In the fourth intercostal space on the left edge of the sternum
E.
In the fifth intercostal space along the right edge of the sternum
36.
Where is the absolute cardiac dullness border located in the norm, which determines the physician in Figure 37?
A.
In the second intercostal space along the right edge of the sternum
B.
In the fourth intercostal space 1 - 1.5 cm from the right edge of the sternum
C.
In the third intercostal space along the right edge of the sternum
D.
*In the fourth intercostal space on the left edge of the sternum
E.
In the fifth intercostal space along the right edge of the sternum
37.
What forms the relative cardiac dullness border, which is determined by the physician in
Figure 37?
A.
*The right atrium
B.
Pulmonary trunk
C.
Left ventricle
D.
Left atrial auricle
E.
Right ventricle
38.
What research is conducted by a doctor shown in Fig. 38?
A.
Determination of the upper border of the heart
B.
Determination the right border of the heart
C.
*Determination the left border of the heart
D.
Determination the width of vascular bundle
E.
Determination of width of Kroenig’s area
39.
Where is the relative cardiac dullness border located in the norm, which determines the physician in Figure 38?
A.
In the second intercostal space on the left edge of the sternum
B.
In the fourth intercostal space 1 - 1.5 cm from the left midclavicular line
C.
*In the fifth intercostal space 1 - 1.5 cm in the middle of the left midclavicular line
D.
In the fourth intercostal space on the left edge of the sternum
E.
In the sixth intercostal space in the left midclavicular line
40.
Where is the absolute cardiac dullness border located in the norm, which determines the physician in Figure 38?
A.
In the second intercostal space on the left edge of the sternum
B.
In the fourth intercostal space 1 - 1.5 cm from the left midclavicular line
C.
*In the fifth intercostal space 2-2,5 cm medially from the left midclavicular line
D.
In the fourth intercostal space on the left edge of the sternum
E.
In the sixth intercostal space in the left midclavicular line
41.
What forms the relative cardiac dullness border, which is determined by the physician in
Figure 38?
A.
Right atrium
B.
Pulmonary trunk
C.
*Left ventricle
D.
Left atrial auricle
E.
Right ventricle
42.
The examination presented in Figure 39 is indicated in patients with COPD (chronic obstructive pulmonary disease) in the case .of..
A.
Bronchopulmonary bleeding
B.
Sanation of the tracheobronchial tree
C.
Differentiation of COPD and possible tumor
D.
Taking smears of bronchial content for research
E.
*All enumerated
43.
Which examination is presented in Figure 39?
A.
Esophagogastroduodenoscopy
B.
Artificial lung ventilation
C.
assessment of external respiratory function
D.
All enumerated
E.
*Bronchoscopy
44.
The examination presented in Figure 39 in patients with bronchial asthma is indicated in the case of ...
A.
Necessity to clarify the nature of the allergen
B.
Differentiation of COPD and possible tumor
C.
Improving lungs ventilation
D.
All enumerated
E.
*Sanatiion of the tracheobronchial tree and intrabronchial administration of bronchodilators
45.
Which of presented below states are contraindications to the examination shown in
Figure 39?
A.
Tumors of the bronchi
B.
Foreign body of airways
C.
Anomalies of bronchial development
D.
Bronchiectatic disease
E.
*Acute respiratory failure
46.
What examination is conducted with the device presented in Figure 40?
A.
*Endoscopic
B.
Ultrasound
C.
Computer
D.
Radiological
E.
There is no correct answer
47.
Which organs of gastrointestinal tract is it not possible to examine by the study shown in
Figure 40?
A.
*Stomach
B.
Esophagus
C.
Liver, spleen, gallbladder
D.
Small intestine
E.
Colon
48.
Which of presented below diseases is the indication for the examination shown in Figure
40?
A.
Ulcerative colitis
B.
Acute pancreatitis
C.
Calculous cholecystitis
D.
*Peptic ulcer
E.
Enterocolitis
49.
What is indicated with number 1 on Figure 41?
A.
Point of auscultation of aortic valve
B.
Point of auscultation of tricuspid valve
C.
Point of auscultation of pulmonary trunk valve
D.
Point of auscultation of left ventricle
E.
*Point auscultation mitral valve
50.
What is indicated with number 2 on Figure 41
A.
*Point of auscultation of aortic valve
B.
Point of auscultation of tricuspid valve
C.
Point of auscultation of pulmonary trunk valve
D.
Point of auscultation of left ventricle
E.
Point auscultation mitral valve
51.
What is indicated with number 1 on Figure 41
A.
Point of auscultation of aortic valve
B.
Point of auscultation of tricuspid valve
C.
*Point of auscultation of pulmonary trunk valve
D.
Point of auscultation of left ventricle
E.
Point auscultation mitral valve
52.
What is indicated with number 1 on Figure 41
A.
Point of auscultation of aortic valve
B.
*Point of auscultation of tricuspid valve
C.
Point of auscultation of pulmonary trunk valve
D.
Point of auscultation of left ventricle
E.
Point auscultation mitral valve
53.
How is the point of heart sounds auscultation called which is presented on the picture 41 with number 51?
A.
Zacharyin – Hed’s point
B.
apical point
C.
Central point
D.
Krenig’s point
E.
*Botkin’s point
54.
See on the lower lung border position located along the line under No. 2 in Figure 42. At which level in normostenics is this border located in norm?
A.
In 4 intercostal space
B.
In 6 intercostal space
C.
In 5 intercostal space
D.
*At the level of the 6th rib
E.
At the level of 8-rib
55.
See on the lower lung border position located along the line under No. 1 in Figure 42. At which level in normostenics is this border located in norm?
A.
In 4 intercostal space
B.
In 6 intercostal space
C.
*In 5 intercostal space
D.
At the level of the 6th rib
E.
At the level of 8-rib
56.
See on the lower lung border position located along the line under No. 6 in Figure 42. At which level in normostenics is this border located in norm?
A.
In 4 intercostal space
B.
In 6 intercostal space
C.
In 5 intercostal space
D.
At the level of the 6th rib
E.
*At the level of 8-rib
57.
See on the lower lung border position located along the line under No. 8 in Figure 42. At which level in normostenics is this border located in norm?
A.
In 4 intercostal space
B.
In 6 intercostal space
C.
In 5 intercostal space
D.
*At the level of the 10th rib
E.
At the level of 8-rib
58.
See on the lower lung border position located along the line under No. 5 in Figure 42. At which level in normostenics is this border located in norm?
A.
In 4 intercostal space
B.
In 6 intercostal space
C.
In 5 intercostal space
D.
*At the level of the 7th rib
E.
At the level of 8-rib
59.
See on the lower lung border position located along the line under No. 7 in Figure 42. At which level in normostenics is this border located in norm?
A.
In 4 intercostal space
B.
In 6 intercostal space
C.
In 5 intercostal space
D.
*At the level of the 9th rib
E.
At the level of 8-rib
60.
Figure 43 marked area of kin sensitivity in pancreatitis. What number on the figure indicates on Shoffar’s zone?
A.
*1
B.
2
C.
3
D.
4
E.
1, 2
61.
331. Figure 43 marked area of skin sensitivity in pancreatitis. What number on the figure indicates on Huberhryts-Skulsky’s zone?
A.
1
B.
*2
C.
3
D.
4
E.
1.2
62.
332. Figure 43 marked area of skin sensitivity in pancreatitis. What number on the figure indicates on Desjardins point?
A.
1
B.
2
C.
*3
D.
4
E.
1.2
63.
Figure 43 marked area of skin sensitivity in pancreatitis. What number on the figure indicates on Mayo-Robson’s point?
A.
1
B.
2
C.
3
D.
*4
E.
1.2
64.
In which among the enumerated below diseases may be observed pain in areas indicated on Figure 43?
A.
*Pancreatitis
B.
Cholecystitis
C.
Peptic ulcer
D.
Liver cirrhosis
E.
Gastritis
65.
What complications of hypertension can be detected in the examination shown in Figure
44?
A.
Horner’s symptom
B.
Greffe’s symptom
C.
Mobius’s symptom
D.
Dalrimpl’s symptom
E.
*Salus’s symptom
66.
Which among the enumerated below changes is it possible to reveal in arterial hypertension with the method presented on the Figure 44?
A.
Narrowed and tortuous retinal artery
B.
Hemorrhages in the retina
C.
Swelling of the optic nerve papilla
D.
Degenerative retinal areas
E.
*All of the above
67.
Which research is the proper to reveal positive Salus’s symptom (see Figure 44)?
A.
Encephalography
B.
Electrocardiography
C.
Echocardiography
D.
Tonometry
E.
*Examination of eye fundus
68.
What is the test name which is shown in Figure 45?
A.
Assessment of vocal fremitus
B.
*Palpation apical beat
C.
Palpation heart beat
D.
Determination of elasticity of the chest
E.
Research of pulsation of vessels
69.
What is the test name which is shown in Figure 46?
A.
Electrocardiography
B.
Rheography
C.
*Spirometry
D.
No correct anwer
E.
Encephalography
70.
What is the reason for the research shown in Figure 46?
A.
For registration of the heart function
B.
*To study the function of the lungs
C.
To investigate the function of kidney
D.
For the magnetic therapy
E.
For sonography
71.
What indexes are defined with the method, shown in Fig. 46?
A.
Respiratory volume
B.
Lung capacity
C.
Forced vital capacity of the lungs
D.
Volume forced expiratory volume in 1 sec
E.
*All of the above
72.
Look at picture 46. What a pathological syndrome is it possible to diagnose using this method?
A.
intoxication syndrome
B.
Syndrome of cavity in the lungs
C.
Syndrome of accumulation of fluid in the pleural cavity
D.
Pulmonary hyperventilation syndrome
E.
*Respiratory insufficiency syndrome
73.
Which organ is the physitian palpating in Figure 47?
A.
*The right kidney
B.
The left kidney
C.
Pancreas
D.
Spleen
E.
Stomach
74.
Which organ is the physitian palpating in Figure 48?
A.
The right kidney
B.
*The left kidney
C.
Pancreas
D.
Spleen
E.
Stomach
75.
Which of these diseases characterized by organ damage presented in Figure 49?
A.
Pneumonia
B.
Rheumatism
C.
Hypotension
D.
Bronchitis
E.
*Hypertension
76.
Figure 49. In patient with arterial hypertension it was found positive Salus ‘s symptom.
Changes in which organ is it typical for?
A.
1
B.
3
C.
4
D.
5
E.
*2
77.
Figure 49. In patient with arterial hypertension it was found increased serum creatinine.
Changes in which organ is it typical for?
A.
1
B.
2
C.
4
D.
5
E.
*3
78.
Indicate affection of which organs will be in patients with hypertension (see Figure 49)?
A.
1.2
B.
3.4
C.
1.5
D.
2.4
E.
*1,2,3,4,5
79.
Determining of which symptom is presented in Figure 50?
A.
*Pasternatsky’s symptom
B.
Vasylenko’s symptom
C.
Ortner’s symptom
D.
Blumberg’s symptom
E.
Kehr’s symptom
80.
Determination of symptom shown in Figure 50 is conducted in pathology of the following organ ..
A.
*Kidney
B.
liver
C.
musculoskeletal system
D.
Pancreas
E.
Colon
81.
Fig. 82 Where to determine pulse in kidney diseases?
A.
In the vessels of the neck
B.
*The radial artery
C.
At temples
D.
At the foot arteries
E.
At various arteries
82.
Fig.85 What is the presented on the picture 85 symptom typical or?
A.
*Glomerulonephritis
B.
Pyelonephritis
C.
Urolithiasis
D.
Respiratory failure
E.
Heart failure
83.
Fig.85 What symptom in patients with kidney disease is shown in Figure 85?
A.
Facies hippocratica
B.
*Facies nephritica
C.
Korvizar’s facce
D.
Botkin’s face
E.
Humpreht’s face
84.
Fig.80 In which kidney disease the layer labeled with the number 1 is affected?
A.
*Glomerulonephritis
B.
Pyelonephritis
C.
Urolithiasis
D.
Renal failure
E.
Amyloidosis of kidneys
85.
Fig.80 In which kidney disease the layer labeled with the number 2 is affected?
A.
Glomerulonephritis
B.
*Pyelonephritis
C.
Urolithiasis
D.
Renal failure
E.
Amyloidosis of kidneys
86.
Fig. 83 How in the apparatus for blood pressure measuring called shown in Figure?
A.
Ghenc’s apparatus
B.
Bobrov’s apparatus
C.
Strazhesko’s apparatus
D.
*Korotkov’s apparatus
E.
Riva Rocchi’s apparatus
87.
Fig. 83 Korotkov’s apparatus in nephrological patients is used to measure:
A.
Pulse pressure
B.
Venous pressure
C.
*Arterial pressure
D.
Vascular pressure
E.
Vascular resistance
88.
Fig. 80 What is indicated by arrows in figure 7?
A.
*Ureter
B.
renal poles
C.
renal artery
D.
renal vein
E.
renal tubules
89.
Fig. 80 What is indicated by arrows in figure 13?
A.
renal poles
B.
renal artery
C.
renal vein
D.
renal tubules
E.
*Cortical substance
90.
Fig. 80 What is indicated by arrows in figure 14?
A.
*Medulla
B.
renal artery
C.
renal vein
D.
renal tubules
E.
cortical substance
91.
Fig. 80 What is indicated by arrows in figure 8?
A.
*Renal pelvis
B.
renal artery
C.
renal vein
D.
renal tubules
E.
cortical substance
92.
Fig. 80 What is indicated by arrows in figure 12?
A.
*Kidney capsule
B.
renal artery
C.
renal vein
D.
renal tubules
E.
cortical substance
93.
Fig. 81 What is indicated by arrow 1 in the figure?
A.
*Upper segment of the kidney
B.
upper anterior segment of the kidney
C.
lower anterior segment of the kidney
D.
lower segment of the kidney
E.
posterior segment of the kidney
94.
Fig. 81 What is indicated by arrow II in the figure?
A.
upper segment of the kidney
B.
*Upper anterior segment of the kidney
C.
lower anterior segment of the kidney
D.
lower segment of the kidney
E.
posterior segment of the kidney
95.
Fig. 81 What is indicated by arrow III in the figure?
A.
upper segment of the kidney
B.
upper anterior segment of the kidney
C.
*Lower anterior segment of the kidney
D.
lower segment of the kidney
E.
posterior segment of the kidney
96.
Fig. 81 What is indicated by arrow IY in the figure?
A.
upper segment of the kidney
B.
upper anterior segment of the kidney
C.
lower anterior segment of the kidney
D.
*Lower segment of the kidney
E.
posterior segment of the kidney
97.
Fig. 81 What is indicated by arrow Y in the figure?
A.
upper segment of the kidney
B.
upper anterior segment of the kidney
C.
lower anterior segment of the kidney
D.
lower segment of the kidney
E.
*Posterior segment of the kidney
98.
Fig. 83 Patient S., 48 years old, is treated about kidney disease in a hospital. He has high blood pressure, as shown in Fig. What pathological condition may be suspected?
A.
Angina pectoris
B.
Hypertonic disease
C.
Vascular dystonia
D.
*Nephrogenic hypertension
E.
Cirrhosis
99.
Fig. 86. Patient B., 64 years old, who is treated because of the end-stage of kidney disease, suddenly developed changes in the skin, the localization of which is shown in
100.
Fig. How is this syndrome called?
A.
renal failure
B.
eclampsia
C.
skin-muscular syndrome
D.
*Hemorrhagic syndrome
E.
spider angiomata
Fig. 87 How is the element called presented in the figure?
A.
glomeruli
B.
tubules
C.
bowls
D.
Kidney cells
101.
E.
*Nephron
Fig. 84 Which symptom is shown in Figure?
A.
ascites
B.
lymphostasis
C.
venostaz
D.
*Edema
E.
hydrothorax
102.
Fig. 88 What is the name of the symptom find out in the patient with end-stage renal disease?
A.
Watch glasses
B.
Club-shaped fingers
C.
*Drum stick rodes
D.
Sclerodactyly
103.
E.
Koylonihiya
Fig. 89 How is the method of kidney visualization presented on the picture called?
A.
*Scintygraphy
B.
Radionefrography
C.
Ultrasound
D.
X-ray examination
E.
Tomonefrography
104.
Fig. 89 The most fine method of renal parenchyma assessment is presented on the
Figure 89. How is it called?
A.
*Scintygraphy
B.
Radionefrography
C.
Ultrasound
D.
X-ray examination
E.
Tomonefrohrafiya
105.
Fig. 89 Glomerulonephritis was confirmed by kidney research, shown in Figure
89. How is this study called?
A.
Radionefrography
B.
Ultrasound
106.
C.
. X-ray examination
D.
Tomonefrohrafiya
E.
*Scintygraphy
Fig. 85 For which renal disease is the most typical symptoms presented on the
107.
picture?
A.
pyelonephritis
B.
urolithiasis
C.
tumor of the kidney
D.
*Glomerulonephritis
E.
nephrogenic hypertension
Fig. 88 Drum stick rodes presented in Figure 88, may take place at ...
A.
pyelonephritis
B.
urolithiasis
C.
Hyperthyreosis
D.
*Renal failure
E.
Nephrogenic hypertension
108.
Fig. 84 For which renal disease is the most typical symptoms presented on the picture?
A.
urolithiasis
B.
renovascular hypertension
C.
*Glomerulonephritis
109.
110.
111.
D.
nephrogenic hypertension
E.
pyelonephritis
Fig.85 The patient has glomerulonephritis. What is presented in Figure 85?
A.
Facies hippocratica
B.
*Facies nephritica
C.
Korvizar’s face
D.
Botkin’s face
E.
Humpreht’s face
Fig. 84 What pathology is the presented on the picture symptom typical for?
A.
vascular insufficiency
B.
renovascular hypertension
C.
Hypothyroidism
D.
Hyperthyroidism
E.
*Renal failure
Fig. 84 Facies nefritica is the most typical symptom of the following isease:.
A.
vascular insufficiency
B.
renovascular hypertension
C.
hypovolemia
D.
*Renal failure
E.
pyelonephritis
112.
113.
Fig.86 The patient has glomerulonephritis. What is presented in Figure 86?
A.
vascular insufficiency
B.
eclampsia
C.
skin-muscular syndrome
D.
*Hemorrhagic syndrome
E.
spider angiomata
Fig.83 The patient has glomerulonephritis. What has a doctor found (shown in
Figure) in the patient?
A.
vascular insufficiency
B.
eclampsia
C.
renal syndrome
D.
*Hypertension syndrome
E.
hypotension syndrome
114.
Fig.85 The patient has glomerulonephritis. What has a doctor found (shown in
Figure) in the patient?
A.
vascular insufficiency
B.
*Renal failure
C.
renal syndrome
D.
hypertension syndrome
E.
hypotension syndrome
115.
Figure 88 shows the symptom of drumsticks rodes. What pathology of kidney is this symptom most typical for?
A.
pyelonephritis
B.
urolithiasis
C.
*Renal failure
116.
D.
glomerulonephritis
E.
nephrogenic hypertension
What disease is presented on the picture 73 symptom typical for?
A.
*Hemophilia
B.
Angina pectoris
C.
Bronchial asthma
D.
Angioedema
117.
E.
Hypothyroidism
What disease is presented on the picture 73 symptom typical for?
A.
*Hemophilia
B.
Pneumonia
C.
Chronic pyelonephritis
118.
D.
Diabetes
E.
Diffuse toxic goiter
Fig.73 shows a patient with hemophilia. What condition is dangerous for patient’s life in this disease?
A.
*Hemorrhagic syndrome
B.
Intoxication syndrome
C.
Bronchial obstruction syndrome
D.
Edema
119.
E.
Dyspeptic syndrome
Fig.73 shows a patient with hemophilia. In what category of patients is this disease manifested?
A.
*Men
B.
Women
C.
Equally in men and women
D.
Elderly people
120.
E.
medial age people
Which character of bleeding is shown in fig.79?
A.
*Hematomic
B.
Vasclitic
C.
Petechial
D.
Angiomatous
E.
Mixed
121.
Fig.71 shows changes of the skin characteristic for hemorrhagic diathesis. The disease is more commonly appears ...
A.
*In young age, mostly in women
B.
In young age, mostly in men
122.
C.
In anyone aged, mostly in men
D.
In anyone age in men and women
E.
Since childhood, mostly in men
Fig.90 presents knee of a patient with hemophilia. How is this disease
123.
transmitted?
A.
*To grandchildren through healthy daughters
B.
To grandchildren through sick daughters
C.
To grandchildren through sick sons
D.
To grandchildren through healthy sons
E.
Is not transmitted
Fig.90 presents the knee patient with hemophilia. How is this symptom called?
A.
*Hamartrosis
B.
Hematoma
C.
Edema
D.
Angioedema
E.
There is no right answer
124.
In fig.90 it is presented the knee of a patient who has hematologic disease. What is this disease?
A.
*Hemophilia
B.
Leukemia
C.
Thrombocytopenic purpura
125.
D.
Lymphogranulomatosis
E.
Myeloleukosis
In fig.90 it is presented the knee of a patient with hemophilia. In what age is this
126.
disease manifested?
A.
*From the first years of life
B.
Up to 10 years
C.
In middle age
D.
In elderly age
E.
In anyone age
Fig.71 shows increased bleeding. What disease is it typical for?
A.
*thrombocytopenic purpura (Verlgof’s disease)
B.
Myeloma
C.
Iron deficiency anemia
127.
128.
D.
Chronic lymphocytic leukemia
E.
Lymphogranulomatosis
What type of eruption shown on fig.71?
A.
Angiomatous
B.
Vasculitic
C.
*Petechial
D.
Hematomic
E.
Mixed
What type of eruption is shown on fig.71?
A.
Papulous- hemorrhagic
B.
*Petechial
C.
Hematomic
D.
Erythematous
E.
Ecchymosis
129.
In fig.71 it is shown petechial type of bleeding. For what disease is it typical?
A.
Hemophilia
B.
*Thrombocytopenic purpura
C.
Hemorrhagic vasculitis
130.
D.
Anemia
E.
Lymphogranulomatosis
In fig.71 it is shown the type of bleeding, which is typical for ...
A.
Hemophilia
B.
Leukosis
C.
*Thrombocytopenic purpura
D.
Lymphogranulomatosis
E.
Liver cirrhosis
In fig.71 it is shown the type of bleeding, which is typical for ... 131.
A.
*Hemorrhagic diathesis
B.
Liver disease
C.
Diseases of cardiovascular system
D.
Allergic disease
E.
Endocrine disease
132.
133.
134.
138.
How often is the part of body affected shown in fig.75 in hemophilia?
A.
Not affected
B.
*Very rare
C.
Often
D.
Always is affected
E.
Affected if other joints are not impaired
What determines the affection of the body in hemophiliacs shown in fig.75?
A.
Food
B.
Heredity
C.
*The severity and frequency of injuries
D.
Sedentary lifestyle
E.
Never affected
What may be the cause of body affection in hemophiliacs shown in fig.75?
A.
Hematomas
B.
*Hemarthrosis
C.
Increased pressure in the large circulation
D.
Increased pressure in the pulmonary circulation
135.
136.
What determines the affecting of the knee joint in Fig. 76 in patients with hemophilia?
A.
Food
B.
Heredity
C.
*Injuries
D.
Never affected
E.
Sedentary lifestyle
137.
E.
Never affected
How often is body part affected in hemophiliacs presented in fig.76?
A.
Not affected
B.
Hardly ever
C.
*Often
D.
Affected if other joints are no changed
E.
Always affected
What is presented in Fig.76 in patient with hemophilia?
A.
Hematoma
B.
Fracture
C.
*Hemarthrosis
D.
Erythema
E.
No changes were detected
In Fig.76 it is shown hemarthrosis. For what disease is it typical?
A.
*Hemophilia
B.
Gout
C.
Rheumatic diseases
D.
Rheumatoid arthritis
139.
E.
Liver cirrhosis
In Fig.76 it is shown hemarthrosis. Repeated hemarthrosis lead to the development .of..
A.
*Contracture
B.
Fractures
C.
Neoplasm
D.
Lypodystrophy
140.
E.
Chalk-stones (tophuses)
What is presented in Fig.76 in patient with hemophilia?
A.
Fracture
B.
Contracture
C.
*Hemarthrosis
D.
Tumor
E.
Chalk-stone (tophus)
141.
What is presented in Fig.76 in patient with hemophilia?
A.
Lipodystrophy
B.
Hematoma
C.
Tumor
D.
*Hemarthrosis
E.
Erythema nodosum
142.
143.
144.
What is shown in Fig.79?
A.
Hemarthrosis
B.
Erythema nodosum
C.
*Hematoma
D.
Chalk-stone (tophus)
E.
Angioedema
In Fig 79 in a patient with hemophilia after travma at his knee it is shown ...
A.
*Hematoma
B.
Lipodystrophy
C.
Angioedema
D.
Rheumatoid nodule near the elbow joint
E.
Chalk-stone (tophus)
In Fig.79 it is presented the following type of bleeding ...
A.
Anhiomatous
B.
*Hematomic
C.
Vaskulitic
D.
Petechial
145.
E.
Mixed
Fig.79 shows changes of the skin that are characteristic for...
A.
Urticaria
B.
Angioedema
C.
*Hemophilia
D.
Rheumatic disease
E.
Rheumatoid arthritis
146.
In a healthy person during damage of blood vessels the special formation occurs immediately with proteins and blood cells as it is shown schematically in Fig.74.
Consequently, the bleeding stops. In which disease this mechanism doesn’t work?
A.
Iron deficiency anemia
147.
B.
*Hemophilia
C.
B12-deficiency anemia
D.
Hypertension
E.
Peptic ulcer (complicated by bleeding)
Looking at Fig.72 it is possible to say that hemophilia is ...
A.
*Blood disease
B.
Vascular disease
C.
Disease of the lymphatic system
D.
Metabolic disorder
E.
There is no right answer
Looking at Fig.77 it is possible to say that for rapid coagulation in trauma the 148.
necessary factors are clotting factors and enough platelets. What pathological changes will be in hemophilia?
A.
Insufficient number of platelets produced by bone marrow
B.
*Lack of blood factors involved in the formation of plasma thromboplastin
C.
Proliferation of young (blast) cells of blood
D.
Affected small capillaries
E.
Mature and maturing, but functionally disable lymphocytes
149.
In Fig.78 it is shown the knee joint of the patient .with..
A.
*Hemophilia
B.
Leukemia
C.
Liver cirrhosis
D.
Rheumatic diseases
E.
Rheumatoid arthritis
150.
In Fig.78 it is presented the knee joint in a patient with hemophilia. What pathological finding can you see?
A.
Fracture
B.
*Hemarthrosis and contracture
C.
Chalk-stone
D.
Neoplasm
E.
Hematoma
151.
How does the increased production of iodine hormones of the endocrine gland shown in Figure 21 (number 2) influence on the cardiovascular system?
A.
Leads to increase in minute and systolic volumes of a heart
B.
Leads to increase in circulating blood volume and blood flow velocity
C.
Causes the increase in systolic and reduction of diastolic blood pressure, increased pulse pressure
D.
Causing tachycardia and paroxysmal atrial fibrillation.
E.
*All of the above
152.
How does the increased production of iodine hormones by the endocrine gland shown in Figure 21 (tsyfra2) influence on the digestive tract?
A.
Increases appetite
B.
increases secretion of gastric juice
C.
Increases peristalsis.
D.
*Provides all of the effects
E.
No effect
153.
What pituitary hormone regulates the function of the endocrine gland, shown in
Fig. 21 (number 2)?
A.
Corticotropin (ACTH);
B.
*Thyroid stimulating hormone (TSH);
C.
Follicle stimulating hormone (FSH);
D.
prolactin (lactogenic hormone);
E.
somatotropin (STH).
154.
What are the possible dysfunction of the endocrine gland, shown in Fig. 21
(number 2)?
155.
A.
Hyperfunction;
B.
hypofunction;
C.
dysfunction
D.
*Hyper-and hypofunction
E.
All of the above
Glands, shown in Fig. 21 (figure 2) produces:
A.
*Triiodothyronine, thyroxine
B.
insulin
C.
epinephrine, norepinephrine
D.
Oxytocin
E.
parathyroid hormone
156.
157.
Fig. 22 What method of examination is shown?
A.
*Palpation of the thyroid gland
B.
Palpation of the cervical lymph nodes
C.
Detection of neck swelling
D.
Determining the degree of subcutaneous fat development
E.
All numbered
Fig. 22. To what degree of thyroid gland enlargement is it possible to include the
158.
option when the gland is not palpable (according to the WHO classification, 2001).?
A.
*0 degree .
B.
1 degree.
C.
4 degree.
D.
2 degree.
E.
3 degree.
Fig. 22. After palpation of the thyroid gland a doctor concluded that it is 0 degree of enlargement (according to the WHO classification, 2001). This means that:
A.
*No goiter (sizes of the gland do not exceed the dimensions of the distal phalanx of the thumb)
B.
Goiter is palpable but is invisible in normal neck position
C.
Goiter is visible with upturned head
D.
Goiter is visible at a distance
159.
E.
Goiter is clearly visible in the normal position the neck
Fig. 22. After palpation of the thyroid gland a doctor concluded that it is I degree of enlargement (according to the WHO classification, 2001). This means that:
A.
No goiter (sizes of the gland do not exceed the dimensions of the distal phalanx of
160.
the thumb)
B.
*Goiter is palpable but is invisible in normal neck position
C.
Goiter is visible with upturned head
D.
Goiter is visible at a distance
E.
Goiter is clearly visible in the normal position the neck
Fig. 22. To what degree of thyroid gland enlargement is it possible to include the option when sizes of the gland do not exceed the dimensions of the distal phalanx of the thumb (according to the WHO classification, 2001).?
A.
*0 degree.
B.
1 degree.
C.
4 degree.
D.
2 degree.
E.
3 degree.
161.
Fig. 23. What disease may be suspected?
A.
*Diffuse toxic goiter
B.
Hypothyroidism
C.
Itzenko-Cushing sundrome
D.
Acromegaly
162.
E.
Diabetes.
Fig. 23. What ocular symptoms may be characteristic for the disease shown in this figure?
A.
Graefe’s sign
B.
Mobius’s sign
C.
Delrympl’s sign
D.
Kocher’s sign
163.
E.
*All of the above
Fig. 23. For the disease shown in this figure, may be characteristic all the symptoms, except:
A.
Graefe’s sign
B.
Mobius’s sign
C.
Delrympl’s sign
D.
Kocher’s sign
E.
*Ortner’s sign
164.
Fig. 23 What belongs to the most dangerous complication of the disease presented on the picture?
A.
Thyrotoxic myocardiodystrophy
B.
*Thyrotoxic crisis
C.
Rapidly progressing hypotension
D.
Atrophy of eye muscles, obfuscation of cornea
E.
Compression of the neck organs with swallowing difficulties
165.
Fig. 23. What medication may be used for treatment of the disease of thyroid gland (as it is presented on the picture)?
A.
mercazolil
B.
metoprolol
C.
prednisolone
166.
D.
retabolil
E.
*All answers are correct
Fig. 23. Production of which hormonesis increased in patients with this disease?
A.
*Triiodothyronine (T3) and thyroxine (T4).
B.
Parathhormone
C.
Estradiol
D.
Thyrotropin
167.
E.
Aldosterone
Fig. 24. Manifestation of which disease may be pretybial myxoedema?
A.
Diffuse toxic goiter
B.
*Hypothyroidism
C.
Euthyroid goiter
D.
Acromegaly
E.
Itzenko-Cushing syndrome
168.
Fig. 24. The patient, in addition to these changes in the legs, presents exophthalmos, tachycardia, enlargement of the thyroid gland. What disease is it possible to suspetct?
A.
*Diffuse toxic goiter
B.
Hypothyroidism
C.
Euthyroid goiter
D.
Acromegaly
E.
Thyroiditis
169.
Fig. 25. What are the main reasons for these changes in the eyes of patients with hyperthyroidism?
A.
Accumulation of acid mucopolysaccharides in the retrobulbar tissue, which consequently intensivly binds water, and its volume increases, pushing to the eyeball the front;
B.
varicose dilatation of orbital veins with the accumulation of adipose tissue in the
170.
orbita;
C.
pathological changes (hyalinosis, fibrosis) of muscle fibers of the external eye muscles;
D.
influence of exophthalmic factor.
E.
*All of the above
Fig. 25.These changes of eyes are typical for:
A.
diabetes mellitus;
B.
*Hyperthyroidism;
C.
myxedema;
D.
acromegaly.
E.
Addison’s disease
171.
Fig. 26. The picture presents a patient before and after successful treatment with
L-thyroxine. What kind of illness you can think about?
A.
Diffuse toxic goiter
B.
*Hypothyroidism
C.
Acromegaly
D.
Adisson’s disease
172.
E.
Itzenko-Cushing syndrome
Fig. 26. What changes in the cardiovascular system are characteristic for patients with hypothyroidism?
A.
Expanding of heart borders;
B.
weakening of heart sounds,
C.
rare and empty pulse;
D.
normal or slightly lowered blood pressure, sometimes symptomatic sclerotic hypertension develops.
E.
*All of the above
173.
Fig. 27. What is the degree of enlargement of the thyroid gland in Figure
(classification WHO, 2001)?
A.
0 degree.
B.
4 degree.
C.
1 degree..
D.
*2 degree.
E.
3 degree.
174.
Fig. 27. Patient has 2 degree of thyroid gland enlargement (WHO classification,
2001). This means that:
A.
sizes of the gland do not exceed the dimensions of the distal phalanx of the thumb
B.
The gland is palpable but invisible in normal neck position
C.
No goiter
D.
*Goiter is clearly visible in the normal position the neck
E.
All answers are wrong
175.
Fig. 27. Which disease is manifested with such a facial expression?
A.
*Thyrotoxicosis
B.
Hypothyroidism
C.
Euthyroid goiter
176.
D.
Acromegaly
E.
Itzenko-Cushing syndrome
Fig. 27. Such changes are typical forl:
A.
*thyroid gland hyperfunction
B.
Hypothyroidism
C.
Euthyroid goiter
D.
Pituitary hyperfunction
E.
Adrenal hyperfunction
Fig. 27. Production of which hormone increases in patients with this disease? 177.
A.
*Triiodothyronine (T3) and thyroxine (T4).
B.
PTH
C.
Tyreocacitonine
D.
Thyrotropin
E.
Aldosterone
178.
Fig. 27. Pathogenetically the development and progression of this are disease caused by:
A.
*Excess amount of thyroid hormones
B.
Normal thyroid hormones content
C.
Reduction of thyroid hormones content
D.
Increased content of thyreoliberyn
E.
Deficiency of thyroid hormones
179.
180.
181.
182.
Fig. 27. This disease is most common in people aged:
A.
*20-50 years
B.
1-10 years
C.
10-20 years
D.
60-70 years
E.
70 years
Fig. 27. Etiological factors of the disease are:
A.
Psychic trauma
B.
infection
C.
heredity
D.
overheating in the sun
E.
*All answers are correct
Fig. 27. What changes in blood pressure are characteristic of the disease?
A.
increase in systolic and diastolic
B.
*Increase in systolic and reduction of diastolic
C.
reduction in diastolic and systolic
D.
reduction in systolic and increase in diastolic
E.
decrease in pulse pressure
Fig. 28. What disease is presented?
A.
Diffuse toxic goiter
B.
*Nodular goiter
C.
Euthyroid goiter
D.
Lymphadenopathy
E.
Myxedema
183.
184.
Fig. 29. The figure shows:
A.
Radiographs of the thyroid gland
B.
Ultrasonography of the thyroid gland
C.
Basal metabolism assessment
D.
Termogram of the thyroid gland
E.
*Scanogram of the thyroid gland
Fig. 30. The figure shows:
185.
A.
Scanogram of the thyroid gland
B.
*Ultrasound exmination of the thyroid gland
C.
CT scan of the thyroid gland
D.
Termogram of the thyroid gland
E.
No correct answer
Fig. 30. Indications for conducting of this research method are:
A.
Thyroid gland formations found on palpation
B.
The presence of mass in the anterior neck
C.
Complaints of suffocation, increased irritability, causeless cough
D.
Monitoring the effectiveness of treatment for diseases of the thyroid gland
E.
*All numbered
186.
13.)?
Which of the following diseases is presented with such a body built (see Figure
A.
*Itzenko-Cushing's syndrome
B.
Acromegaly
C.
Hypothyroidism
D.
Addison's disease
E.
Diffuse toxic goiter
187.
16.)?
Which of the following diseases is presented with such a body built (see Figure
A.
Acromegaly
B.
Hypothyroidism
C.
*Itzenko-Cushing's syndrome
D.
cachexia
188.
E.
alimentary obesity
Which of the following diseases is presented with such changes (see Fig. 12)?
A.
Itzenko-Cushing's syndrome
B.
*Acromegaly
C.
Hypothyroidism
D.
Addison's disease
E.
Diffuse toxic goiter
189.
Which of the following diseases presented on the Fig. 20 is manifested with such changes of skin color?
A.
Hepatitis
B.
Acromegaly
C.
Iron deficiency anemia
D.
*Addison's disease
E.
Diffuse toxic goiter
190.
What changes in the skin are presented in Fig. 18?
A.
Increased body mass index
B.
Rash
C.
*Striae
D.
Skin cancer.
E.
Scabies.
191.
What disease is characterized by skin changes, presented on Fig.18?
A.
*Itzenko-Cushing's syndrome
B.
Acromegaly
C.
Hypothyroidism
D.
Addison's disease
E.
Diffuse toxic goiter
192.
Patient A., 29, complains of general weakness, weight loss, nausea, recurrent vomiting. Objectively: hypotension, hyperpigmentation of the skin and mucous membranes (Fig. 20). What is preliminary diagnosis?
A.
Cushing’s syndrome
B.
Acromegaly
C.
Hypothyroidism
D.
*Addison's disease
193.
E.
neurogenic anorexia
Patient A., 60 years old, a few weeks ago, was treated in hospital because of tuberculosis/ Now he complains of general weakness, weight loss, diarrhea. Objectively: hypotension, hyperpigmentation of the skin, especially the folds (Fig. 20). Which test
194.
should be used?
A.
examination of feces fro helmints ova
B.
The level of glycemia
C.
Ultrasonography of the abdomen
D.
*The level of cortisol and ACTH
E.
Electrocardiogram.
Where the pathological process is located in patients with Cushing's syndrome
(Fig. 18)?
A.
Adenohypophysis
B.
Neurohypophysis
C.
Hypothalamus
D.
*Adrenal cortex
E.
Adrenal medulla
195.
except:
All of the presented below symptoms are typical for Addison's disease (Fig. 20),
A.
hyperpigmentation
B.
hypotension
C.
*Hyperglycemia
D.
Increased serum potassium
E.
dyspepsia
196.
197.
198.
199.
What disease is characterized by changes presented in Fig. 14?
A.
Cushing’s syndrome
B.
*Acromegaly
C.
Hypothyroidism
D.
Addison's disease
E.
Diffuse toxic goiter
Where the pathological process is located in patients with acromegaly (Fig. 14)?
A.
*Adenohypophysis
B.
neurohypophysis
C.
hypothalamus
D.
adrenal cortex
E.
adrenal medulla
Where the pathological process is located in patients with acromegaly (Fig. 12)?
A.
*Adenohypophysis
B.
neurohypophysis
C.
hypothalamus
D.
adrenal cortex
E.
adrenal medulla
Complaints of patients with acromegaly (Fig.12):
A.
Increased body weight and size of shoes and gloves
B.
Change of facial pattern
200.
201.
202.
203.
204.
205.
206.
207.
C.
Impaired vision
D.
Women - amenorrhea, men - decreased sexual potency
E.
*All answers are correct
Complaints of patients with acromegaly (Figure 14):
A.
Increased body weight and size of shoes and gloves
B.
Change of facial pattern
C.
Impaired vision
D.
Women - amenorrhea, men - decreased sexual potency
E.
*All answers are correct
What laboratory signs characteristic of acromegaly (Fig. 12)?
A.
Hyperglycemia and glycosuria
B.
Hyperlipidemia
C.
Increased blood alkaline phosphatase
D.
Elevated levels of growth hormone
E.
*All answers are correct
What laboratory signs characteristic of acromegaly (Fig. 14)?
A.
Hyperglycemia and glycosuria
B.
Hyperlipidemia
C.
Increased blood alkaline phosphatase
D.
Elevated levels of growth hormone
E.
*All answers are correct
What examination is presented in Fig. 17?:
A.
Ultrasonography
B.
*Computer tomography
C.
Radiography
D.
Electrocardiography
E.
Electrorenceohalohraphy
Which hormone excess production develops in acromegaly (Figure 12)?:
A.
Progesterone
B.
estrogen
C.
*Somatotropin
D.
insulin
E.
aldosterone
Which hormone excess production develops in acromegaly (Figure 14)?:
A.
Progesterone
B.
estrogen
C.
*Somatotropin
D.
insulin
E.
aldosterone
What changes (presented in Fig. 19) are typical for acromegaly?
A.
*Diastema
B.
Caries
C.
There is no right answer
D.
Ulceration of oral mucosa
E.
Herpetic eruptions
What disease the following changes in the teeth are typical for (Figure 19)?
A.
Itzenko-Cushing's syndrome
B.
*Acromegaly
C.
Hypothyroidism
D.
Addison's disease
E.
Diffuse toxic goiter
208.
Where the pathological process is located in patients with Cushing's syndrome
(Fig. 16)?
A.
Adenohypophysis
B.
Neurohypophysis
C.
Hypothalamus
D.
*Adrenal cortex
E.
Adrenal medulla
209.
Where the pathological process is located in patients with Cushing's syndrome
(Fig. 13)?
A.
Adenohypophysis
B.
Neurohypophysis
C.
Hypothalamus
D.
*Adrenal cortex
E.
Adrenal medulla
210.
211.
212.
213.
What disease is manifested with such a high growth (Figure 15)?
A.
Itzenko-Cushing's syndrome
B.
Pituitary dwarfism
C.
Hypothyroidism
D.
Addison's disease
E.
*Gigantism
Which hormone excess production leads to the high growth (Fig. 15)
A.
*Somatotropin
B.
insulin
C.
estrogen
D.
cortizol
E.
no right answer
In which organ pathological changes occur that lead to gigantism (Fig. 15)?
A.
*Pituitary gland
B.
thyroid gland
C.
hypothalamus
D.
adrenal cortex
E.
adrenal medulla
What disease is manifested with such a high growth (Figure 11)?
A.
Itzenko-Cushing's syndrome
B.
Pituitary dwarfism
C.
Hypothyroidism
D.
Addison's disease
E.
*Gigantism
214.
Which hormone excess production leads to the high growth (Fig. 11)
A.
*Somatotropin
B.
insulin
C.
estrogen
D.
D. cortisol
E.
no right answer
215.
216.
In which organ pathological changes occur that lead to gigantism (Fig. 11)?
A.
*Pituitary gland
B.
thyroid gland
C.
hypothalamus
D.
adrenal cortex
E.
adrenal medulla
What disease is manifested with such low height (Figure 15)?
A.
Itzenko-Cushing's syndrome
217.
B.
*Pituitary dwarfism
C.
Hypothyroidism
D.
Addison's disease
E.
Giantism
Which hormone low production leads to the low growth (Fig. 15)
A.
*Somatotropin
B.
insulin
C.
estrogen
D.
Cortisol
E.
no right answer
In which organ pathological changes occur that lead to pituitary nanizmu (Fig. 218.
219.
15)?
A.
*Pituitary
B.
thyroid
C.
hypothalamus
D.
adrenal cortex
E.
adrenal medulla
Laboratory findings characteristic of pituitary dwarfism (Rys15.)
A.
*All answers are correct
B.
Reduced levels of growth hormone, TSH, corticotropin, gonadotrophins;
C.
Increased cholesterol
220.
D.
Hypoglycemia
E.
Anemia
The main method of diagnosis of pituitary adenoma is presented in Fig. 17. How
221.
is it called?
A.
Electrocardiography
B.
*Computer tomography
C.
Radiography
D.
Ultrasonography
E.
Electrorencephlohraphy
Fig.62 Which nodes will be primarily affected in leukemia:
A.
*Cervical, submandibular, axillary, inguinal lymph node groups
B.
Neck, palate, axillary, popliteal lymph node groups
C.
Cervical, submandibular, elbow of lymph nodes
D.
Generally not affected
E.
All answers are correct
222.
Fig.62 How many percent of patients will experience an increase cervicalsupraclavicular lymph node groups in leukemia::
A.
*60-70%
B.
10-20%
C.
70-90%
223.
D.
50-60%
E.
There is no correct answer
Fig.62 How many percent of patients will experience an increase inguinal lymph
224.
node groups in leukemia:
A.
*6-10%
B.
10-30%
C.
60-70%
D.
80-90%
E.
There is no correct answer
Fig.62 diagnosis of lymphoma is established:
A.
*On the basis of lymph nodes biopsy materials examination
B.
On the basis of brain tissue biopsy materials examination
C.
On the basis cornea biopsy materials examination
D.
On the basis of subcutaneous fat tissue biopsy materials examination
E.
On the basis of gastric mucosa biopsy materials examination
225.
226.
227.
228.
Fig.64 Which cells will prevail in the peripheral blood in leukemia:
A.
*Blast cells
B.
Macrophages
C.
Platelets
D.
Young leukocytes
E.
Eosinophils
216. Fig.66 Which cells predominate in the picture:
A.
Neutrophils
B.
Basophils
C.
Segmented
D.
*Blasts
E.
Eosinophils
What disease is presented on the Fig.70?
A.
*Lymphoma
B.
Goiter
C.
Sarcoma
D.
Mumps
E.
Limphadenitis
Fig.63 Which organ is affected on the picture?
A.
*Lymph nodes
B.
Thyroid gland
C.
Trachea
D.
Esophagus
E.
Parathyroid glands
229.
What is presented on the Fig.61?
A.
*Sternal puncture
B.
Lumbar puncture
C.
Puncture knee
D.
Collection of blood
E.
Putting blood substitute
230.
231.
Fig.61 At what level is sternal puncture conducted?
A.
*Level of III-IV ribs
B.
At level of II-III cervical vertebra
C.
At level of III-IV thoracic
D.
At the of level I and II ribs
E.
At level of VII ribs
Fig.61. How is device for sternal puncture called?
A.
*Kassyrsky’s needle
B.
Trocar
C.
All answers are correct
D.
Deschan’s needle
E.
Dufo’s needle
232.
Fig.62 Which groups of lymph nodes will be affected in chronic lymphoid leukemia?
A.
Inguinal
B.
Abdominal
C.
Mediastinum
D.
Inguinal
E.
*All answers are correct
233.
Fig.62. How many stages is distinguished in chronic lymphoid leukemia?
A.
2
B.
3
C.
*4
234.
by?
D.
5
E.
There is no right answer
Fig.62 Stage IV of Hodgkin's disease (lymphogranulomatosis) is characterized
A.
Liver metastases
B.
Lung metastases
C.
*Affection of lymph nodes on both sides of the diaphragm
D.
All answers are correct
E.
No right answer
235.
236.
237.
238.
Fig.67. The onset of acute leukemia is accompanied with?
A.
Flu
B.
*Tonsillitis
C.
Stomatitis
D.
Gingivitis
E.
There is no correct answer
What is presented on the picture 65 (patient with acute leukemia)?
A.
*Gingivitis
B.
stomatitis
C.
mumps
D.
There is no correct answer
E.
angina
What is typical for I period of acute leukemia (presented on Fig.65)?
A.
candidiasis
B.
catarrhal stomatitis
C.
chronic hypertrophic gingivitis
D.
acute herpetic stomatitis
E.
*All answers are correct
What agents in leukemia may cause such affections (Fig.65)?
A.
*Candida fungus
B.
Actinomycetes
C.
fungi of the genus Fusarium
D.
Fungi of the genus Psilotsibum
E.
Fungi of the genus Aspergillus
239.
240.
241.
What is presented on Fig.68?
A.
Insulin syringe
B.
Deschamp’s needle
C.
*Kassyrsky’s needle
D.
Dufo’s needle
E.
Trocar
Fig.68. Which manipulation is this tool necessary for?
A.
Collection of blood
B.
Venipuncture
C.
*Sternal puncture
D.
Celiocentesis
E.
There is no correct answer
Fig.69. Which genetic abnormality occurs in chronic myelogenous leukemia?
A.
Trisomy of chromosome 9
B.
22 izohromosoma
C.
*Philadelphia chromosoma
D.
Deletion of chromosome 9
E.
There is no correct answer
242.
243.
244.
245.
Fig.69. What the Philadelphia chromosoma?
A.
*Translocation between 22-th and 9-th chromosomas
B.
Inversion between 22-th and 9-th chromosomas
C.
Trisomy of chromosome 22
D.
Deletion of chromosome 9
E.
There is no correct answer
Fig. 69 What the chromosomal aberration is shown in Figure?
A.
*Transfer of land chromosome to another
B.
recurrence plots chromosome
C.
changing the order of genes on chromosome areas on reverse one
D.
There is no correct answer
E.
removal plots chromosome
What is presented on Fig.70?
A.
*Lymphoma
B.
Adenoma
C.
Shvanoma
D.
All answers are correct
E.
Goiter
What formation is presented on Fig.70?
A.
*Hodgkin's Lymphoma
B.
Burkitt’s Lymphoma
C.
Skin Lymphoma
D.
Follicular lymphoma
E.
There is no correct answer
246.
247.
Fig.70 Which cells are present in Hodgkin lymphoma?
A.
*Sternberg cells
B.
Stem Cells
C.
Leydig cells
D.
Cells Betz
E.
There is no right answer
Fig.66 What stages in the course of acute leukemia do you know?
A.
Initial
B.
Expand clinical
C.
Terminal
D.
There is no right answer
E.
*All answers are correct
Fig.64 In cytochemical study of acute leukemia the following reaction is 248.
249.
conducted:
A.
*Peroxidase
B.
Catalase
C.
Lactase
D.
Amylase
E.
All answers are correct
Fig.66 What color will be in a positive Schick reaction?
A.
*Red
B.
Green
C.
Blue
D.
Colorless
250.
E.
Yellow
Fig.70 How many syndromes are in chronic lymphatic leukemia:
A.
*2
B.
3
C.
4
D.
0
E.
5
251.
252.
Fig.70. Which syndromes in chronic lymphocytic leukemia do you know:
A.
lymphoproliferative
B.
Syndrome of complications
C.
anaemic
D.
*A and B are correct
E.
All answers are correct
Fig.62 One of the manifestations of the leukemic cell proliferation syndrome in
253.
acute leukemia is:
A.
*Lymph nodes enlargement
B.
Fever
C.
Sweats
D.
Stuffiness
E.
Weight loss
Fig.64 Which of these formed elements not normally found in the peripheral
254.
blood?
A.
Reticulocytes
B.
All cells can occur in the peripheral blood.
C.
*Lymphoblasts.
D.
Neutrophil metamyelocytes.
E.
Eosinophilic metamyelocytes.
Fig.66. In which disease in complete blood count there are blast cells and is
"hiatus leucemicus"?
A.
Chronic myelogenous leukemia
B.
Chronic lymphocytic leukemia
C.
Lymphogranulomatosis
D.
Multiple myeloma
E.
*Acute leukemia
255.
Fig.64 The clinical diagnosis of acute leukemia is put as well as treatment begins only on the basis of:
A.
Typical general clinical signs
B.
Morphological examination of peripheral blood
C.
Morphological examination of bone marrow
D.
Biopsy lymph nodes, liver and other tissues
E.
*Cytochemical study
256.
Fig.51 Which syndrome is the presented finger appearance characteristic for:
A.
Asthenic
B.
Vegetative
C.
Dysplastic
D.
*Syderopenic
E.
Syderoahrestychnyy
257.
Fig.51 To clarify the diagnosis in a patient, whose finger is shown in the figure, the necessary additional examination should be prescribed:
A.
Lipidogram
B.
Determination of total protein
258.
C.
Determination of electrolytes
D.
*Determination of serum iron
E.
Determination of glucose
Fig.51 Prescribe the treatment for the patient with anemia, whose finger is shown
259.
in the picture:
A.
Vitamins
B.
Corticosteroids
C.
Antibiotics
D.
*Iron preparations
E.
Antiviral drugs
Fig.52 Which of the products presented on the picture contain more iron?
A.
Citric
B.
*Veal
C.
Pork
D.
Vegetables
E.
Corn
260.
Fig.52 Which among the presented in Figure products is recommended for iron deficiency anemia in the first place:
A.
Citric
B.
Corn
C.
Vegetables
261.
D.
Pork
E.
*Veal
Fig.53 Specify normal size of erythrocytes:
A.
1-2 microns
B.
3-4 microns
C.
6.5 microns
D.
*7.8 microns
262.
E.
11.10 microns
Fig.58 What changes of erythrocytes are presented in the picture?
A.
Spherocytosis
B.
Microspherocytosis
C.
Macrocytosis
D.
Normocytosis
263.
E.
*Circle shape
Fig.58 What disease is manifested with presented in Figure erythrocyte shape changes?
A.
Iron deficiency anemia
B.
Microcytic anemia
C.
Normocytic anemia
D.
All listed.
264.
E.
*Anemia due to hemoglobinopathies
Fig.58 What causes changes in erythrocytes prseneted in this picture?
A.
Iron deficiency
B.
Deficiency of folic acid
C.
*Hemoglobinopathies
D.
Membranopatiya
E.
Fermentopathy
265.
Fig.54 The picture presents the tongue of bright red color with smooth papillae.
Which disease is it typical for?
A.
Hypoplastic anemia
B.
Hemolytic anemmiya
266.
C.
Hemorrhagic anemia
D.
Iron deficiency anemia
E.
*Pernicious anemia
Fig.54 Patient’s tongue became bright red and papillae become smooth. What type
267.
of anemia may a doctor suspect?
A.
*Pernicious anemia
B.
Hipoblastychna anemia
C.
Hemorrhagic anemia
D.
Iron deficiency anemia
E.
All answers are correct
Fig.54 During inspection a doctor examined patient’s tongue and revelaled the following changes: a bright red color and smooth papillas. What form of anemia is presents in a patient?
A.
Hypoplastic anemia
B.
Hemolytic anemia
C.
Iron deficiency anemia
D.
*Pernicious anemia
E.
All answers are correct
268.
Fig.54. The presented changes the tongue indicate on:
A.
Hemolytic anemia
B.
Hypoplastic anemia
C.
Iron deficiency anemia
D.
*Pernicious anemia
E.
All answers are correct
269.
Fig.55 The patient has blue tint of sclera. In which type of anemia is a symptom present?
A.
*Iron deficiency anemia
B.
Hypoplastic anemia
C.
Pernicious anemia
D.
All answers are correct
E.
No right answer
270.
Fig.55 On examination the doctor noticed yellow color of sclera in the patient and suspected anemia. Help the doctor to determine the type of anemia in this patient.
A.
Iron deficiency anemia
B.
*Hemolytic anemia
C.
Hypoplastic anemia
D.
Hyperplastic anemia
E.
There is no correct answer
271.
Fig.55 What disease is characterized by decreased amounts of iron in the body, resulting in disturbed heme synthesis and synthesis of proteins that contain iron?
A.
Hypoblastdc anemia
B.
Pernicious anemia
C.
*Iron deficiency anemia
D.
Hyperblastsc anemia
E.
There is no correct answer
272.
Fig.56 Increased diameter of erythrocyte (macrocytosis) is observed in:
A.
There is no right answer
B.
Refractory anemia
C.
Severe anemia
D.
Mild form of anemia
E.
*B12 - and folic acid deficiency anemia
273.
Fig.56 Macrocytosis is observed at?
274.
A.
There is no right answer
B.
folic acid deficiency anemia
C.
*All answers are correct
D.
Hyperchromic anemia
E.
Megaloblastic anemia
Fig.57 What type of anemia is usually caused by diseases of the digestive tract?
A.
Thalassemia
B.
Hemolytic anemia
C.
*Iron deficiency anemia
D.
Aplastic anemia
E.
There is no correct answer
275.
body?
Fig.57 Which of the presented organ is is responsible for iron absorption in the
A.
Liver
B.
Colon
C.
*Stomach and small intestine
D.
Esophagus
E.
There is no correct answer
276.
Fig.57 At what anemia iron absorption in the body is impaired?
A.
Hypoplastic anemia
B.
Pernicious anemia
C.
*Iron deficiency anemia
D.
Hyperblastsc anemia
E.
There is no correct answer
277.
Fig.57 The patient has chronic gastritis. What type of anemia can occur in the patient?
A.
Hypoplastic anemia
B.
Pernicious anemia
C.
*B12 - deficiency anemia
278.
for?
D.
Hyperblastsc anemia
E.
There is no correct answer
Fig.56 In patient’s blood microspherocites are found. What disease is it typicsl
A.
*Congenital hemolytic anemia
B.
Acquired hemolytic anemia
C.
Iron deficiency anemia
279.
D.
folic acid deficiency anemia
E.
Agranulocytosis
Fig.56 In patient’s blood microspherocites are found. What test can help to confirm the diagnosis?
A.
*Research of erythrocytes osmotic resistance
B.
Research of hematocrit
C.
Research of bleeding time
D.
Research of coagulogram
E.
Studies of proteolytic activity
280.
What isindicated on the. Fig. 91?
A.
Tatoo
B.
Work injury
C.
*Allergic prick-tests
D.
Indications with the marker for the surgeon.
E.
Insects bites.
281.
in…
On the picture 91 you can see conduction of allergic prick-test. It is indicated
A.
*Determination of hypersensitivity to different drugs
B.
For specific treatment of allergy
C.
For prophylactic vaccination of allergy
D.
For differential diagnosis of different diseases
E.
All mentioned.
282.
In the case of positive allergic test on the certain drug (see Fig. 91) the patient is advised…
A.
To use ? of this drug for treatment
B.
To decrease the dosage of the drug twice
C.
*Do not use the drug.
D.
To administer the drug under the control af antihistamine preparations.
E.
All mentioned.
283.
284.
What is presented on the Fig. 92?
A.
The mushroom
B.
The turtle
C.
A helmet
D.
*Domestic mite
E.
A spider
On the picture 92 you can see zoomed domestic mite. It may be the reason of…
A.
*Atopic allergy
B.
Dermatomycosis
C.
Viral hepatitis
285.
286.
D.
COPD
E.
Myocarditis
On the picture 92 you can see zoomed domestic mite. It may be the reason of…
A.
*Atopic bronchial asthma
B.
Infectious-depending bronchial asthma
C.
Epidemic parotitis
D.
COPD
E.
Pneumonia
On the picture 92 you can see zoomed domestic mite. It may be the reason of…
A.
Acute bronchitis
B.
Infectious-depending bronchial asthma
C.
Hemopthysis
D.
COPD
E.
*Atopic bronchial asthma
287.
On the picture 92 you can see the process of biting of a human by a bee. What is the most dangerous consequence of this process?
A.
Hypertension
B.
Innoculation with hepatitis virus
C.
Hemopthysis
D.
Development of COPD
E.
*Anaphylactic shock
288.
On the picture 92 you can see the process of biting of a human by a bee. What is the most dangerous consequence of this process?
A.
*Anaphylactic shock
B.
Myocardial infarction
C.
Hemopthysis
D.
Virus hepatitis
E.
No correct answer
289.
On the picture 92 you can see the process of biting of a human by a bee. What actions should be conducted in first aid?
A.
To pull the stinger out
B.
To squeeze out the poison from the wound
C.
To apply the cold compress
D.
To administer antihistamines and glucocorticoids
E.
*All mentioned
290.
On the picture 92 you can see the process of biting of a human by a bee. What actions should be conducted in first aid?
A.
To take for the patient 25 drops of valeriana decoction
B.
To apply the turniquett for 2 hrs on the forearm
C.
To treat the wund with brilliant green
D.
To apply the sterile bandage
E.
*All answers are wrong
291.
292.
What is presented on the picture 94?
A.
Facies mitralis
B.
Facies nefritica
C.
Facies Hippocratica
D.
Myxoedematous face
E.
*Quincke’s edema
What is presented on the picture 94?
A.
Diabetic face
B.
Thyrotoxic face
C.
Face in hypercorticism
D.
Myxoedematous face
293.
E.
*No correct answer
On the Fig. 94 you can see the face of a patient with Quinke’s edema. What is the cause of its appearance?
294.
295.
A.
*Marked accumulation of mediators of inflammation in the skin or mucosa
B.
Antithrombin defficiency
C.
Congenital deficiency of alfa-2-macroglobulin
D.
Marked accumulation of angiotensine II in the skin or mucosa
E.
Dfficiency of natural killers.
On the picture 95 it is presented the face of a human …
A.
Of mongoloid race
B.
With acute glomerulonephritis
C.
With chronic pyelonephritis
D.
With hypothyreosis
E.
*With Quincke’s edema
On the picture 95 it is presented the face of a human …
A.
With anasarca
B.
With chronic renal failure
C.
With chronic pyelonephritis
D.
With hypothyreosis
E.
*With Quincke’s edema
296.
On the picture 95 it is presented the face of a human with Quincke’s edema. What is the most danger for patient’s life may develop in this disease?
A.
*Asphyxia
B.
Pneumonia
C.
Angina pectoris
D.
Hypothyreosis
E.
Е. Hypertension
297.
On the picture 95 it is presented the face of a human with Quincke’s edema. What is the most danger for patient’s life may develop in this disease?
A.
*Anaphylactic shock
B.
Antritis
C.
Pulmonary artery thromboembolism
D.
Hyperthyreosis
E.
Hypotension
298.
299.
Clinical manifestation of which disease is presented on the picture Fig. 96?
A.
*pollinosis
B.
Scute viral conjunctivitis
C.
Sun burn of eye conjunctiva
D.
Trauma of the eye
E.
No correct answer
Clinical manifestation of which disease is presented on the picture Fig. 96?
A.
*Exogenic atolic allergy
B.
Acute respiratory viral infection
C.
Sun burn of eye conjunctiva
D.
Chemical affection of an eye
300.
301.
E.
No correct answer
Clinical manifestation of which disease is presented on the picture Fig. 96?
A.
*pollinosis
B.
Acute conjunctivitis
C.
Sun burn of eye conjunctiva
D.
Chemical affection of an eye
E.
No correct answer
Clinical manifestation of which disease is presented on the picture Fig. 96?
A.
*hay-fever
B.
Acute conjunctivitis
C.
Sun burn of eye conjunctiva
D.
Chemical affection of an eye
E.
No correct answer
302.
303.
What I presented on the picture 97?
A.
Application of piper plaster
B.
Application of antiseptic patch
C.
*Application allergic test plaster
D.
Application of mustard plaster
E.
No correct answer
On the picture 97 you can see conduction of application skin allergic test. In
304.
which case is it indicated?
A.
*In external usage of medicines
B.
In usage of medicines in inhalations
C.
In enteral usage of medicines
D.
In parenteral usage of medicines
E.
No correct answer
On the picture 98 you can see the hand of a patient with…
305.
A.
Malignant tumor
B.
Local overdevelopment of fat tissue
C.
*Rheumatoid arthritis
D.
Gout
E.
No correct answer
On the picture 98 you can see the hand of a patient with rheumatoid arthritis.
What lies in the basis of this disease?
A.
Degenerative and dysthrophic processes
B.
Dysmetabolic processes
C.
Infectious and allergic processes
D.
*Processes of autoimmune agression
306.
E.
No correct answer
On the picture 98 you can see the hand of a patient with rheumatoid arthritis.
Which symptom is present on the picture?
A.
Degenerative and dysthrophic processes
B.
Dysmetabolic processes
C.
Infectious and allergic processes
D.
Urticaria
307.
E.
*Ulnar deviation of the wrist
On the picture 99 you can see X-ray film of the patient with rheumatoid arthritis.
Which symptom of this disease is presented?
A.
Neoplastic processes
B.
Dysmetabolic processes
C.
Infectious and allergic processes
D.
Urticaria
308.
E.
*Ulnar deviation of the wrist
Look at the picture 99. In the lower right corner you can see results of blood test for rheumatoid factor. What is rheumatoid factor?
A.
*Special autoantibodies to immunoglobulins class G
B.
Antigens to cartilages
C.
Antigens to bone tissue
D.
Complexes of uric acid
E.
No correct answer
309.
Look at the picture 99. In the lower right corner you can see results of blood test for rheumatoid factor. Where does it occur?
A.
In lymphocites
B.
In monocites
C.
In erythrocites
310.
D.
*In the cavity of affected joint
E.
No correct answer
On the fig. 100 you can see the transverse section of a kidney. Which factors
311.
cause functional insufficiency of this organ?
A.
Disorders of renal hemodynamics (shock, collapse)
B.
Exogenic intopxications (sublimate, bіsmut, poisoning mushrooms etc)
C.
Infectious diseases (leptospirosis)
D.
Acute kidney diseases
E.
*All enumerated
On the fig. 100 you can see the transverse section of a kidney. Which factors
312.
cause functional insufficiency of this organ?
A.
Obstruction of urinary tract
B.
Arterial hypertension
C.
Eclampsy in pregnancy
D.
Malignant tumors
E.
*All enumerated
On the fig. 100 you can see the transverse section of a kidney. Which factors are the first to cause functional insufficiency of part 1 of this organ?
A.
Obstruction of urinary tract
B.
*Acute glomerulonephritis
C.
Acute cystitis
D.
Diseases of prostatic gland
E.
All enumerated
313.
On the fig. 100 you can see the transverse section of a kidney. Which factors are the first to cause functional insufficiency of part 2 of this organ?
A.
*Calculous pyelitis
B.
Acute glomerulonephritisт
C.
Acute cystitis
D.
Diseases of prostatic gland
E.
All enumerated
314.
On the fig. 100 you can see the transverse section of a kidney. Which factors are the first to cause functional insufficiency of parts1 and 2 of this organ?
A.
*Acute pyelonephritis
B.
Acute glomerulonephritis
C.
Acute cystitis
315.
D.
Diseases of prostatic gland
E.
All enumerated
Fig.1 Indicate on the skin affection typical for lipid metabolism changes:
A.
Diabetic rubeosis
B.
Dermopathy
C.
Lipoid necrobiosis
D.
*Xanthomatosis
316.
E.
Granuloma annulare
Fig.1 Presented on the picture skin affection in diabetes mellitus occur due to the disorder of:
A.
Carbohydrates metabolism
B.
Protein metabolism
C.
Mineral metabolism
D.
*Lipid metabolism
317.
318.
E.
Pigment metabolism
Fig.1З. On the picture you can see skin affection typical for:
A.
Diabetes mellitus I type
B.
*Diabetes mellitus I type
C.
Gout
D.
Hepatitis
E.
Diabetic dermopathy
On the Fig.1З there are skin affections. How are they called?
A.
Furunculosis
B.
Erythema
C.
Pustula
D.
Roseola
E.
*Xanthelasmas
319.
Fig.2 A dentist examined the woman with complaints on feeling of loose teeth, bad breath in the mouth, taste perversion, jam of food in the interdental spaces, hyperesthesia of naked necks of the teeth. From her history it is known that the woman was suffering from diabetes mellitus. What is the pathological condition found during the inspection of the oral cavity?
A.
Caries
B.
Paradontitis
C.
Pulpitis
D.
Periodontitis
E.
*Paradontosis
320.
Fig.2 A dentist has examined the woman with complaints of thirst, dry mouth, increased tooth sensitivity. On examination of the oral cavity dentist revealed signs of periodontal disease. What kind of pathological condition of the patient can he think of?
A.
Shogren’s syndrome
B.
Anaemia
C.
Hypothyreosis
D.
Stomatitis
321.
E.
*Diabetes mellitus
Fig.2. A dentist has examined a woman sick with diabetes mellitus. On examination of the oral cavity dentist showed signs of periodontal disease. What changes may a doctor find?
A.
Dryness of oral cavity mucosa
B.
Naket necks and roots of teeth
C.
Atrophy of the tops of papillas and gingiva
D.
Wedge-shaped defects
E.
*All enumerated
322.
Fig.2. A dentist has examined a woman sick with diabetes mellitus. On examination of the oral cavity dentist showed signs of periodontal disease. Which among presented below signs are typical for periodontal disease?
A.
Dryness in the mouth
B.
naked necks and roots of the teeth
C.
Atrophy of the tops of papillas and gingiva
D.
Wedge-shaped defects
E.
*Edema and gingival hyperemia
323.
Fig.3 Glucose concentration in blood plasma of a health individual is equal to:
A.
*3,5-5,5 mmol/l
B.
4,4 – 6,6 mmol/l
C.
4,4 – 5,5 mmol/l
D.
3,3 – 6,6 mmol/l
E.
4,4 – 5,5 mmol/l
324.
Fig.3 What may be used in diagnostics of diabetes mellitus for assessment of its compensation?
325.
A.
Glucosied hemoglobin
B.
Postprandial glycaemia,
C.
Glycaemia before sleep
D.
*All enumerated
E.
Cholesterol and arterial hypertension
Fig.3 For evaluation of glycaemia level may be used …
A.
Photometer
B.
Pulseoxymeter,
C.
Tonometer
D.
*Glucometer
E.
Glucose tolerance test
326.
Fig.3 Glucose concentration in the blood on fasting stomach in compensated diabetes mellitus II type is in the limits:
A.
*5-6 mmol/l
B.
6,1-6,5 mmol/l
C.
>6,1 mmol/l
D.
3,3 – 6,6 mmol/l
E.
4,4 – 5,5 mmol/l
327.
Fig.3 Glucose concentration in the blood on fasting stomach in subcompensated diabetes mellitus II type is in the limits:
A.
5-6 mmol/l
B.
*6,2-7,8 mmol/l
C.
>6,5 mmol/l
D.
3,3 – 6,6 mmol/l
E.
4,4 – 5,5 м mmol/l
328.
Fig.3 Glucose concentration in the blood on fasting stomach in decompensated diabetes mellitus II type is in the limits:
A.
5-6 mmol/l
B.
6,1-6,5 mmol/l
C.
*>7,8 mmol/l
D.
3,3 – 6,6 mmol/l
E.
4,4 – 5,5 mmol/l
329.
330.
Fig.4 How is insulin administered for the patient with diabetes mellitus:
A.
With intramuscular injection
B.
*With subcutaneous injection
C.
With intravenous drop infusion
D.
With intradermal injection
E.
With intravenous drop infusion slowly
Fig.4 A doctor is examining a pregnant woman with diabetes mellitus. Which treatment is probable in diabetes with pregnancy?
A.
*prolonged types of insulin combined with short action insulin
B.
short action insulin
331.
C.
biguanides
Fig.4 Intensifies insulin therapy was prescribed for a patient with diqbetes mellitus. What does it mean?
A.
*Single injection of long-acting insulin and on this background the simple insulin in necessary dosage before each meal;
B.
Injections of the required dose of insulin before each meal;
C.
Single injection of long-acting insulin;
D.
Administration of medial-acting insulin twice a day;
E.
Combination of metformin and simple insulin in necessary dosage before each meal;
332.
333.
334.
Fig.4 Where to inject insulin for the diabetic patient:
A.
External quadrant of buttoxk region
B.
*In paraumbilical region
C.
Into internal surface of forearm
D.
Intradermally
E.
In intravenous drop infusion
Fig.4 Short-cating insulines are injected in such a way:
A.
*30 хв. before meals which contains carbohydrates
B.
60 хв. before meals which contains carbohydrates
C.
15 хв. before meals which contains carbohydrates
D.
During eating food which contains carbohydrates
E.
After eating food which contains carbohydrates
Fig.4 How many units of insulin is present in 1 ml of syinge:
A.
*100 UN of insulin in 1 ml.
B.
50 UN of insulin in 1 ml.
C.
10 UN of insulin in 1 ml.
D.
45 о UN of insulin in 1 ml л.
E.
150 UN of insulin in 1 ml.
335.
336.
337.
Fig.4 How many units of insulin is present in 1 ml of syinge:
A.
*40 UN of insulin in 1 ml.
B.
50 UN of insulin in 1 ml.
C.
10 UN of insulin in 1 ml
D.
45 UN of insulin in 1 ml.
E.
150 UN of insulin in 1 ml
Fig.5 Which complication of diabetes mellitus is indicated with number 1:
A.
*Diabetic retinopathy.
B.
Diabetic central polyneyropathy.
C.
Diabetic peryphefar polyneyropathy.
D.
gaucoma
E.
Cataract
Fig.5 Which complication of diabetes mellitus is indicated with number 2:
A.
*Diabetic macroangiopathy.
B.
Diabetic central polyneyropathy.
C.
Diabetic peryphefar polyneyropathy.
D.
Diabetic microangiopathy.
E.
Metabolic cardiopathy
338.
339.
Fig.5 Which complication of diabetes mellitus is indicated with number 4:
A.
*Diabetic foot.
B.
Diabetic central polyneyropathy.
C.
Diabetic peryphefar polyneyropathy.
D.
Ateroslerotic affection of lower limbs.
E.
Asteoarthropathy
Fig.5 Which complication of diabetes mellitus is indicated with number 3:
A.
*Diabetic nephropathy.
B.
Diabetic central polyneyropathy.
C.
Diabetic peryphefar polyneyropathy.
D.
Diabetic microangiopathy.
E.
Metabolic lipodystrophy
Fig.6 What among the indexes of glycaemia is the most informative in conduction 340.
341.
of oral glucose tolerance test?
A.
*in 120 min. after glucose intake
B.
Glucaemia after supper
C.
Glucaemia on fasting stomach
D.
in 30 min after glucose intake
E.
in 30 min after glucose intake
Fig.6 Glucose tolerance test is conducted for the purpose:
A.
*Diagnostics of diabetes mellitus.
B.
Diagnostics компенсації цукрового діабету.
C.
Diagnostics of compensation within the last 3 month.
342.
D.
Diagnostics of insulin needs.
E.
Diagnostics of pancreas functional state.
Fig.6 Impaired glucose tolerance test is established if glucose level in 2 hrs after
343.
its intake per os is elevated within the limits:
A.
*7,8-11,0 mmol/l.
B.
below 7,8 mmol/l
C.
above 11,0 mmol/l л.
D.
3,5-5,5 mmol/l
E.
4,5-6,6 mmol/l.
Fig.6 Manifested diabetes mellitus is diagnosed if glucose level in 2 hrs after its intake per os is elevated within the limits:
344.
A.
7,8-11,0 mmol/l.
B.
below 7,8 mmol/l
C.
*above 11,0 mmol/l л.
D.
3,5-5,5 mmol/l
E.
4,5-6,6 mmol/l.
Fig.7 Which complication of diabetes mellitus is presented on the picture?
A.
Diabetic rubeosis
B.
Dermatopathy
C.
Lipoid necrobiosis
D.
Erytema annulare
E.
*Diabetic foot
345.
Fig.7 In the pathogenesis of presented on the picture complication of diabetes mellitus the leading place belongs to:
A.
Diabetic retinopathy
B.
Diabetic nephropathy
C.
Diabetic angiopathy of lower limbs
D.
Diabetic polyneuropathy
E.
*Diabetic polyneuropathy and microangiopathy
346.
Fig.8 Which risk factor of II type diabetes mellitus among the presented below is most important in progression of diabetis nephropaty?
A.
Smocking
B.
*High blood pressure
C.
Sedentary lifestyle
D.
High cholesterol level in food
347.
E.
Overweight
Fig.8 Which risk factor of diabetes mellitus among the presented below is most important in progression of insulin resistance?
A.
Smocking
B.
High blood pressure
C.
Sedentary lifestyle
D.
High cholesterol level in food
348.
E.
*Overweight
Fig.9 Which disease is the presented changes of eye fund typical for?
A.
*Diabetes mellitus
B.
Thyrotoxicosis
C.
Addison’s siasease
D.
Arterial hypertension
E.
Aterosclerosis
349.
Fig.9 Which diabetes mellitus complication causes changes presented on the picture?
A.
*Diabetic microangiopathy
B.
Diabetic macroangiopathy
C.
Diabetic polyneuropathy
D.
Diabetic micro- and macroangiopathy
E.
Diabetic polyneuropathy з microangiopathy
350.
Fig.10 How are short-acting insulines administered:
A.
Intramuscullary into external quadrant of buttock region
B.
*subcutaneously in paraumbilical region
C.
Intravenously in fast drop infusion
D.
subcutaneously into upper site of forearm
E.
Intravenously in slow drop infusion
351.
Fig.10 In which case action of insulin is faster:
352.
A.
In subcutaneous injection into external quadrant of buttock region
B.
*In subcutaneous injection in paraumbilical region
C.
In subcutaneous injection into external surface of the tigh
D.
Intradermally
Fig.10 Specify complication of insulin therapy?
A.
insulin edema
B.
syndrome of chronic overdose of insulin (Somoji’s syndrome)
C.
Insulin lipodystrophy
D.
Hypoglycaemia
E.
*All enumerated





