First Aid and CPR notes - Tamalpais Union High School District
advertisement

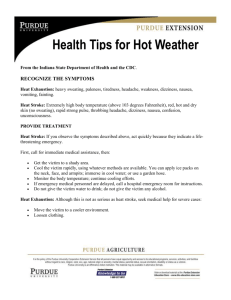
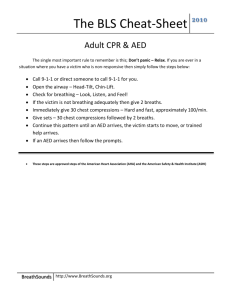
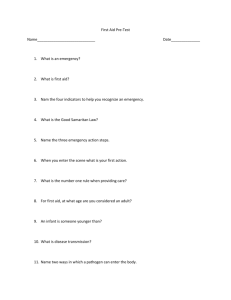
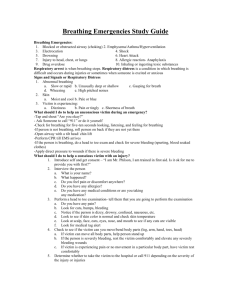
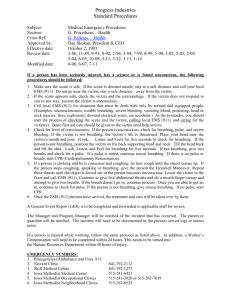
DRAKE HIGH SCHOOL PHYSICAL EDUCATION STANDARD FIRST AID LESSON ONE: INTRODUCTION Purpose of the program: The purpose of the American Red Cross First Aid course is to give individuals knowledge and skills necessary to recognize and provide basic first aid care for injuries and sudden illness until advanced medical personnel arrive and take over. Prerequisites: NONE To become certified: Attend all class sessions or make-up any missed work Demonstrate competency in all required skills Participate in all skill sessions and scenarios Correctly answer at least 80% of the questions in each section of the final written exam. LESSON TWO: RECOGNIZING EMERGENCIES 1. Emergencies can often be recognized because of unusual sights, appearances or behaviors, odors, or noises. 2. Concerning sudden illnesses: A victim may deny anything is seriously wrong. If you think something is wrong, check the victim. Ask questions. 3. Once an emergency has been recognized, be calm and follow the emergency action steps: CHECK - CALL – CARE CHECK: the scene for: 1. 2. 3. 4. Safety to find out what happened to determine the number of victims for any bystanders who may be able to help CALL: 9 - 1 – 1 CARE: for life-threatening emergencies first (Use TRIAGE) LESSON THREE: PROTECTING YOURSELF Good Samaritan Laws Enacted in U. S. to give legal protection to people who willingly provide emergency care to ill or injured persons without accepting anything in return. Enacted to encourage people to help others in an emergency. They require the “Good Samaritan” to use common sense and a reasonable level of skill, and not to exceed the scope of the individual’s training. Good Samaritan Laws vary from state to state. Obtaining Consent Before giving care to a conscious victim you must first get consent. To get permission: State your name. Tell the victim you are trained in first aid. Ask the victim if you can help. Explain what you think is wrong. Explain what you plan to do. If the victim does not give consent, do not give care, but call 9-1-1. Consent is implied in the following two instances: 1. Unconscious victim 2. Children without an adult Preventing Disease Transmission The risk of getting a disease while giving first aid is extremely rare. The following precautions can reduce the risk even further: Avoid contact with blood and other body fluids. Use gloves and breathing barriers. Wash hands with soap and water immediately after giving care. Cleaning up a Blood Spill If a blood spill occurs: Clean up the spill immediately. Use gloves when cleaning up a blood spill. Wipe up the spill with paper towels. Clean with a chlorine solution. Dispose contaminated material in a separate container. LESSON FOUR: BEFORE PROVIDING CARE 1. Check the scene For safety To see what happened To see how many victims there are To see if there are others who can help 2. Check the victim for consciousness To check for consciousness: Tap and shout, “Are you O.K?” Unconsciousness is a life -threatening emergency = immediately call 9-1-1 3. Call 9-1-1 What you might be asked during a 911 call 1. Caller’s name 2. Location: Address Main and cross streets What happened? How many victims and the condition of the victims Care being provided and your First Aid knowledge and abilities *Other than care what helpful things can you do while waiting for EMS help to arrive? 1. Crowd control/ keep scene safe 2. Meet EMS personnel and take them to the emergency scene 3. Give information to EMS: circumstances, condition of victim, care given, etc. Moving a victim It is best to not more an injured person, unless: 1) Scene is unsafe or becoming unsafe. 2) To reach another victim who may have a more serious injury. 3) Must be moved to be able to provide proper care 5 ways to move a victim 1. 2. 3. 4. 5. Clothes drag - if victim may have a head or neck injury. Two-person seat carry - to carry a victim who cannot walk (no head/back injury). Walking assist - support victims injured area. Blanket drag - lay victim down and pull. Foot drag - if victim is too large or heavy to move any other way. LESSON FIVE: PRIORITIZING CARE CARE Determine which victims need care first (triage), and what care to give. Always care for Life Threatening emergencies first. Life threatening emergencies 1. 2. 3. 4. 5. 6. 7. 8. Unconscious victim Persistent or constant chest pain Not breathing or difficulty breathing No pulse Severe bleeding Severe or long seizures Choking Shock Checking a CONSCIOUS victim Check the scene Obtain consent Ask questions of any conscious victims (What happened?, Where does it hurt?, Do you have any allergies?, Are you taking any medications?, etc.) Check for life threatening conditions Give head to toe evaluation (Toe to head evaluation on children) Give care Be calm and reassuring Minimize the risk of shock SHOCK = A life-threatening condition in which not enough blood is being delivered to all parts of the body. It is likely to develop in any serious injury or illness, including severe bleeding, serious internal injury, severe allergic reaction, or significant fluid loss. This condition needs immediate attention as the body’s systems are beginning to fail. Minimize the effects of shock and monitor the ABC’s. SIGNS OF SHOCK: 1. Restlessness or irritability 2. An altered level of consciousness 3. Pale, cool, moist skin 4. Nausea or vomiting 5. A blue tinge to lips and nail beds 6. Rapid breathing 7. Rapid pulse CARING FOR SHOCK: 1. Make sure 9-1-1 has been called 2. Monitor ABC’s 3. Control external bleeding 4. Keep the victim from getting chilled or overheated 5. Elevate the legs about 12 inches and keep the victim comfortable 6. Comfort and reassure the victim until advanced medical personnel arrive 7. Do not give food or drink to the victim Checking an UNCONSCIOUS victim When you discover someone who is unconscious, you must immediately determine if they show signs of life. 1. Check the scene 2. Check the victim for consciousness (Tap and shout, Are you OK?) 3. Call 911 (if the victim is unconscious) If the victim is face down, support the head and neck and roll him/her over) 4. Check ABC’s. Open the airway (head tilt/chin lift), and check for breathing and pulse for “NO MORE THAN 10 SECONDS”. ABC’s A = Airway Perform a “Chin Lift” maneuver by lifting the victim’s chin with one hand while stabilizing the victim’s head with the other hand on the forehead (tilt the head back slightly). Use the “Jaw Thrust” maneuver if there is a suspected neck or back injury. While kneeling at the top of the victim’s head, place both thumbs on the victim’s cheeks and lift the jaw up with the index fingers. Breathing and circulation are the “Signs of Life”. B = Breathing Put your ear close to the victim’s mouth and look, listen, and feel for breathing and pulse Look - to see if the victim’s chest is rising and falling Listen - for breathing noises Feel - for air hitting your cheek and for the pulse. Assuming the victim is not breathing, perform two rescue breaths. These are slow, full breaths of air. If the person is not breathing, scan the body for severe bleeding and prepare to give CPR. If the person is breathing, place in “recovery position” and monitor the ABC’s. Rescue Breaths Step 1: Tilt head back, lift chin forward, and pinch nose shut. Step 2: Take a breath in and form a complete seal over the person’s mouth. Step 3: Blow into the mouth for 1 second to make the chest clearly rise. If breaths go in, give CPR If breaths do not go in, try the breaths again and then give care for an unconscious choking victim C = Circulation Assuming the victim is not breathing, find the carotid artery on the same side of the victim’s neck that you are positioned. Using two fingers (facing down), check the pulse for “no more than ten seconds”. LESSON SIX: CONSCIOUS CHOKING VICTIM PROTOCOL (ADULT) Choking can lead to death. Common causes of choking are: swallowing large pieces of food, too much alcohol before and during meals, exercising while eating, dentures, and laughing while eating. CONSCIOUS CHOKING PROTOCOL 1. Obtain consent 2. Encourage coughing 3. When coughing stops, CALL 911 4. Position yourself slightly behind the person, place one arm across the victim’s chest and lean the person forward. Firmly strike the person’s back between the shoulder blades with the heel of your hand 5 times (5 back blows). 5. Find landmark (just above belly button) and place thumb side of fist against the middle of the abdomen. Grasp the fist with your other hand and give 5 abdominal thrusts (each thrust is a separate action) 6. Repeat steps 5 and 6 until object is dislodged, the victim can cough or breathe, or the victim becomes unconscious Exceptions (where you would use chest compressions instead)—same thrusts but on the sternum Pregnant women Obese victims People in wheelchairs LESSON SEVEN: CARDIAC EMERGENCIES AND UNCONSCIOUS CHOKING Signs of a HEART ATTACK Both men and women experience chest pain or discomfort. Women are more likely to experience Pain in the arm, trouble breathing, and vomiting (nausea). Women also delay recognizing the signs and tend to delay telling others. 1. Persistent chest pain or discomfort lasting more than 3-5 minutes or that goes away and comes back again. 2. Pain in either arm, discomfort or pressure that spreads to the shoulder, arm, neck, or jaw and back 3. Nausea or vomiting 4. Shortness of breath, or trouble breathing 5. Sweating and changes in skin appearance 6. Dizziness, lightheadedness, fainting, or going unconscious 7. Pale, ashen, or bluish skin CARDIAC CHAIN OF SURVIVAL 1. Early recognition and early access—the sooner 9-1-1 is called, the better 2. Early CPR—helps circulate blood that contains oxygen to vital organs 3. Early defibrillation (AED)—electric shock to start the heart—each minute defibrillation is delayed reduces the chance of survival by about 10 percent 4. Early advanced life support—given by trained medical personnel ADULT CPR PROTOCOL 1. 2. 3. 4. 5. Check the scene (it is safe) Check for consciousness (victim is unconscious) Call 911 Check for signs of life for “no more than ten seconds” (there are none) Perform 30 chest compressions in 18 seconds Position yourself for CPR Hands in center of chest over breastbone Your shoulders should be directly over the hands Compressions should be smooth to a depth of at least 2 inches 6. Give two rescue breaths (the air goes in) 7. Continue CPR (repeat steps 5-7) until: See signs of life An AED is ready Too exhausted to continue Trained responder arrives Scene becomes unsafe AED ADULT AED re-establishes a defective rhythm. If there is no electricity in the heart at all, the machine will tell you NOT to shock, but do CPR instead. Turn on the machine and follow the verbal instructions Warnings Do not touch the victim when analyzing Do not touch the victim or the device when it is defibrillating Do not use alcohol on device—it is flammable Do not defibrillate near flammable materials (alcohol, O2) Do not use in a moving vehicle Do not use adult pads on a child under 88 pounds Do not use if victim has a nitroglycerin patch Do not use electronic devices within 6 feet (interrupts analysis) Adult and child pads are placed above and below the heart, while you put one infant pad on the chest, and one infant pad on the back UNCONSCIOUS CHOKING VICTIM PROTOCOL 1. Check the scene 2. Check responsiveness (Tap and shout) 3. Call 9-1-1 4. Open airway and check for breathing for signs of life “no more than ten seconds” (victim is not breathing) 5. Give 30 chest compressions in 18 seconds (rate of 100 per minute) 2 inches deep (keep your shoulders over your hands and your elbows locked) 6. Perform a finger sweep if you see a foreign object 7. Give two rescue breaths while pinching nose closed (the air does not go in) Repeat steps 5-7 LESSON EIGHT: SUDDEN ILLNESS Concerning sudden illnesses: A victim may deny anything is seriously wrong. If you think something is wrong, check the victim. Ask questions. There are many types of sudden illness. Some are: Diabetic emergency Type 1: The pancreas creates little to no insulin. This used to be called “juvenile diabetes” because 70% of diagnosis happened before the age of 30. However, it can affect people of all ages. Type 2: The body either resists the effects of insulin or doesn’t produce enough insulin to maintain a normal blood sugar level. In other words, the body cannot use the insulin it has efficiently. 90% of people who have diabetes have Type 2 diabetes. This used to be called “adult onset diabetes”, but this is no longer true as in has become a big problem with younger people in the United States in the past twenty years. 80% of people with Type 2 Diabetes are overweight. Seizure Stroke (F.A.S.T) Allergic reaction Poisoning To determine if a person has had a stroke, use the letters F. A. S. T. F A S T = = = = Face: Ask the person to smile Arms: Ask the person to raise their arms over their head Speech: Ask victim questions so they have to speak Time: Write down the time when you first recognize stroke symptoms Severe Allergic Reactions: Call 9-1-1 Provide care for life-threatening conditions. Victims of poisoning: Call 9-1-1 Call the local poison control center. Usually the 9-1-1 operator can connect you directly. Look for any containers (pill boxes, etc.) and give them to the EMS personnel. Do not have the victim try to vomit unless instructed to by the poison control center! LESSON NINE: WOUNDS Controlling external bleeding 1. Direct pressure: Wear gloves, apply sterile dressing to wound, do not remove dressing 2. Elevate wound (above the heart) 3. Pressure Points: Cut off circulation to the wounded area by applying pressure to the artery above the wound 4. * Tourniquet: Only use in drastic situations in which the limb must be sacrificed to save the victim’s life Severed body parts Control bleeding Wrap body part in gauze, put in a plastic bag, put the bag on ice Care for shock Be sure the body part goes with the victim to the hospital Pregnancy (delivering a baby) Call 9-1-1 Calm the pregnant woman Layer newspaper covered with towels or blankets under the woman Control the scene so that the woman will have privacy Position the woman on her back with her knees bent, feet flat, and legs apart Let the birth happen naturally Catch the slippery baby carefully Keep the baby warm Do not pull on the baby! Embedded Objects 1. Place several dressings around the object to keep it from moving 2. Bandage the dressings in place around the object 3. * Do not remove the object if at all possible! It can do more damage coming out. It can help control the bleeding when in place. Eye Injuries Place victim in a comfortable position Do not remove any object embedded in the eye Place a sterile dressing around the object and stabilize the object. Apply a bandage over BOTH eyes Never apply direct pressure to the eyeball. Common teeth/nose injuries Knocked out tooth: Apply sterile dressing to vacant tooth and bite down to apply pressure. Preserve tooth in a closed container of cool milk (water is 2nd choice) Get victim to a dentist as soon as possible. Bloody Nose: Lean forward and pinch the nostrils together DEGREES OF BURNS 1. First Degree: Superficial burns (least severe) 2. Second Degree: Partial thickness burns 3. Third Degree: Full thickness burns (most severe) TREATMENT OF BURNS 1. Call 9-1-1: For 2nd and 3rd degree burns, for burns that cover more than one limb, for burns that lead to breathing difficulties, and for burns on children or the elderly. 2. Flush the burned area with large amounts of cool, running water There are exceptions, as in the case of a powder chemical burn and electrical burns when you would not use water. 3. Cover the burned area with a dry, sterile dressing to help prevent infection. Do not wrap, but rather drape loosely. In burn cases, DO NOT: 1. Put ointment on a burn. It may seal in heat and does not relieve pain. 2. Use home remedies such as butter or petroleum jelly. 3. Use ice instead of water on a burn except small, superficial burns. Ice causes body heat loss and may also make the burn deeper. 4. Remove any clothing that is sticking to the victim. LESSON TEN: INJURIES TO MUSCLES, BONES, & JOINTS Four types of injuries to muscles, bones, and joints 1. Fractures = breaks 2. Dislocations/Separations = removed from socket 3. Sprains = stretched ligaments 4. Strains = stretched muscles and tendons The care is the same for muscle, tendon, and ligament injuries: R I C E = = = = Rest Immobilize Cold Elevate Elevate only for sprains and strains! SPLINTS (to immobilize and injured area) 1. Anatomical = using another body part as the splint 2. Soft = using a pillow or blanket as a splint 3. Rigid = using a piece of wood or metal as the splint Applying a SLING (for an injured arm) Support the injured area above and below the site of the injury Check for feeling, warmth, and color below the injured area Place a triangular bandage under the injured arm and over the uninjured shoulder to form the sling Tie the ends of the sling at the side of the neck (a pad may be placed under the knot) Secure the arm to the chest with a folded triangular bandage Re-check the injured area for feeling, warmth, and color LESSON ELEVEN: HEAT AND COLD RELATED INJURIES Heat Related Emergencies 1. Heat Cramps: painful muscle spasms that usually occur in the legs and abdomen (least severe of the heat related emergencies). 2. Heat exhaustion: early indicator that the body’s cooling system is becoming overwhelmed (more severe than heat cramps). Indicators are: cool, moist, pale or flushed skin headache, nausea, dizziness weakness, exhaustion 3. Heat Stroke: the body’s systems are overwhelmed by heat and stop functioning (lifethreatening condition). Indicators are: change in the level of consciousness high body temperature red, hot skin that can be either dry or moist uncharacteristically rapid or weak pulse rapid or shallow breathing Care for Heat Related Injuries 1. 2. 3. 4. 5. Get the victim out of the heat. Move the victim to a cool place. Cool the victim with water. Check and monitor the ABC’s. Provide care for shock. It is OK to give a heat cramps or heat exhaustion victims small amounts of sports drinks as long as they are conscious. However, cool water is the best option. Cold Related Emergencies 1. Frostbite: the freezing of body tissue that has been exposed to the cold. Never rub a frostbitten part—this can cause extensive, painful tissue damage. Indicators are: loss of feeling or sensation in the affected area discolored, waxy skin appearance severe frostbite may include blisters and blue skin Care for Frostbite 1. Soak the affected area in warm water 2. Put dry clothes on to keep the affected area warm 2. Hypothermia: the entire body cools because its ability to keep warm fails. Victim may die if not given proper care. Indicators are: shivering slow, irregular pulse numbness impaired judgement loss of muscle control or loss of consciousness (in late stages or hypothermia) Care for Hypothermia 1. Move the victim to a warm place. 2. Remove any wet clothing. 3. Warm the victim of hypothermia slowly, using dry clothing or blankets. 4. Provide care for shock.