Abdomen 1. Which organ is not located in the right upper quadrant
advertisement
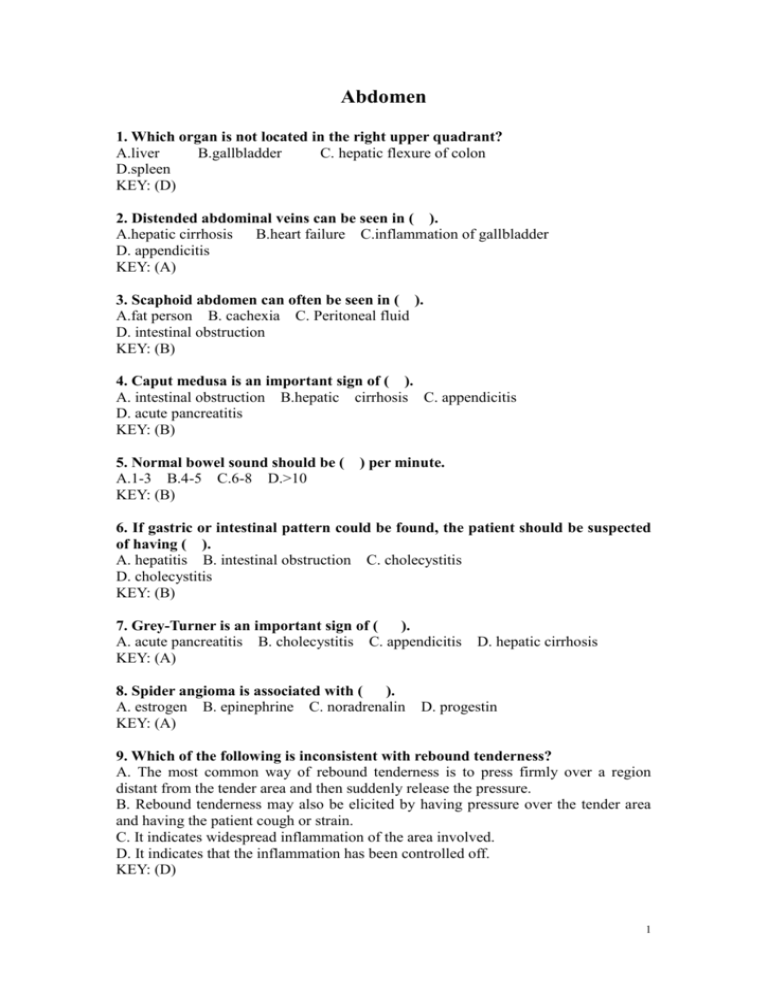
Abdomen 1. Which organ is not located in the right upper quadrant? A.liver B.gallbladder C. hepatic flexure of colon D.spleen KEY: (D) 2. Distended abdominal veins can be seen in ( ). A.hepatic cirrhosis B.heart failure C.inflammation of gallbladder D. appendicitis KEY: (A) 3. Scaphoid abdomen can often be seen in ( ). A.fat person B. cachexia C. Peritoneal fluid D. intestinal obstruction KEY: (B) 4. Caput medusa is an important sign of ( ). A. intestinal obstruction B.hepatic cirrhosis C. appendicitis D. acute pancreatitis KEY: (B) 5. Normal bowel sound should be ( ) per minute. A.1-3 B.4-5 C.6-8 D.>10 KEY: (B) 6. If gastric or intestinal pattern could be found, the patient should be suspected of having ( ). A. hepatitis B. intestinal obstruction C. cholecystitis D. cholecystitis KEY: (B) 7. Grey-Turner is an important sign of ( ). A. acute pancreatitis B. cholecystitis C. appendicitis D. hepatic cirrhosis KEY: (A) 8. Spider angioma is associated with ( ). A. estrogen B. epinephrine C. noradrenalin KEY: (A) D. progestin 9. Which of the following is inconsistent with rebound tenderness? A. The most common way of rebound tenderness is to press firmly over a region distant from the tender area and then suddenly release the pressure. B. Rebound tenderness may also be elicited by having pressure over the tender area and having the patient cough or strain. C. It indicates widespread inflammation of the area involved. D. It indicates that the inflammation has been controlled off. KEY: (D) 1 10. Murphy sign could be seen in ( ). A. acute pancreatitis B. cholecystitis C. appendicitis D. hepatic cirrhosis KEY: (B) 11. Shifting dullness could be found when patient has at least ( A.300ml B.500ml C.1000ml D.1500ml KEY: (C) ) ascites. 12. Normally the upper border of liver is located at the (B) th intercostal space along the right midclavicular line, the(D)th intercostal space along the right midaxillary line, and the (G)th intercostal space along the right scapular line. A.4 B.5 C.6 D.7 E.8 F.9 G..10 H.11 I.12 13. What does hepatojugular reflux sign mean? If you press the liver, you will find the dilated jugular vein becomes more bulged or distended, as from the enlargement of liver passive congestion resulted from right failure. 14. How to measure the spleen when splenomegaly is suspected of? We must use three lines to measure it. Line 1: The distance between left costal border and the lower edge of spleen along left midclavicular line Line 2: The distance between the crossing point of left midclavicular line and left costal border and the most remote point of the spleen Line 3: (when the spleen is extremely large and exceeds the anterior midline.) The distance between the right border of the spleen and the anterior midline. If the spleen indeed exceeds the anterior midline, The mark “+” is used to indicate “exceeding”, while “ – “ is used to indicate “not exceeding”. 15. What does Courvoisier sign refer to? This is an exceedingly valuable sign in differentiating jaundice caused by cancer of the head of the pancreas or the common bile duct from that caused by gallstones. In the presence of tumor of the common bile duct or head of the pancreas, the wall of the gallbladder is normal, and consequently the organ is capable of distending to the point that it is palpable .On the other hand, if the obstruction is caused by gallstones, the gallbladder wall is inflamed, and this diseased organ is not capable of distention. Therefore, the gallbladder will not become palpable. 16. How many types of pain are there which may be elicited by palpation? What are they? How to distinguish them? Two types of pain may be elicited by palpation. 1. Visceral—This is pain that arises from an organic lesion or functional disturbance within an abdominal viscus. For example, it is the type seen in an obstructive lesion of the intestine in which there is a buildup of pressure and distention of the gut. This type of pain has several characteristics: it is dull, poorly localized, and difficult for the patient to characterize. 2. Somatic—This is similar to the distress noted in painful lesions of the skin. It is sharp, bright, and well localized. It is sharp, bright, and well localized. It is not caused 2 primarily by involvement of the viscera; rather it indicates involvement of one of the somatic structures, such as the parietal peritoneum or the abdominal wall itself. It should be pointed out that an inflammatory process originating in a viscus will produce visceral pain that may extend to involve the peritoneum. Inflammation of the peritoneum would then result in somatic pain. 17. When one can palpate an abdominal mass, how to describe it? How to make difference between abdominal wall mass and intra-abdominal mass? It should be characterized as to size , location ,consistency, contour, mobility , and tenderness. Masses in the abdominal wall may be distinguished from those of visceral origin by palpation during voluntary tensing of the muscles. When the patient lifts his head from the examining table, abdominal wall masses will remain palpable and even may become more evident as they are elevated by the tensed muscle. In contrast, intra-abdominal masses will be more difficult to discern after the wall is tensed. 18. How many ways in that we ma detect ascites? What are they and how to do the examinations? This may be detected by several maneuvers(1) fluid wava, (2)shifting dullness , and (3) elbow-knee position. Fluid wave. With patient lying on his back, the examiner’s left hand is placed against the patient’s right flank. An assistant or the patient places the ulnar edge of one hand lightly against the middle of the abdomen to prevent the transmission of any wave through the tissues of the abdominal wall. The examiner’s right hand then lightly taps the left flank of the patient. In the presence of a siguificant amount of ascites, a wave will be transmitted through the fluid that will be felt against the examiner’s left hand as a sharp impulse. This finding is present only when there is a reasonably large amount of fluid. Shifting dullness. When the patient with ascites lies on his back, the fluid will migrate into the flanks, producing dullness laterally. At the same time the midabdomen is tympanitic because of the underlying bowel. When dullness is found in the flanks, a mark is made on the skin at the appropriate level. The patient is then rolled onto his right side, and the percussion is aagain carried out toward each flank. In the presence of ascites, the fluid will gravitate toward the midline and that the bowel, which has been displaced upward by the fluid, results in a tympanitic note in the upper flank. This is repeated after rolling the patient to his left side. By this means, an estimate of the amount of free fluid can be made. Elbow-knee position. The presence of small amounts of fluid may be readily detected by placing the patient in an elbowknee position and percussing from the flanks toward the most dependent portion of the abdomen. Free fluid, if present, will run from the pelvis into the most dependent area, which, if the patient is in the proper position , is located in the periumbilical region. The finding of dullness in this area indicates the presence of ascitic fluid. This technique is more sensitive for detecting small amounts of fluid than are the previously described methods. 3
![Lymphatic problems in Noonan syndrome Q[...]](http://s3.studylib.net/store/data/006913457_1-60bd539d3597312e3d11abf0a582d069-300x300.png)