Causes - Villanova University
advertisement
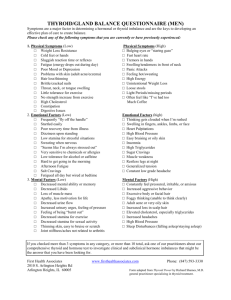
VILLANOVA UNIVERSITY COLLEGE OF NURSING NUR 3112 NURSING CARE OF ADULTS RELATED TO ENDOCRINE FUNCTION Hormones Of Anterior And Posterior Pituitary ANTERIOR HYPERPITUITARISM Cause: Pituitary adenoma Symptoms related to: 1. increase in hormone release 2. space occupying lesion Increase in Hormone Release Anterior Pituitary Acromegaly GH (Growth Hormone/Somatotropin) Giantism in children ACTH (Adrenocorticotropic Hormone) Symptoms of Cushing’s Syndrome TSH (Thyroid Stimulating Hormone) Symptoms of Hyperthyroidism Dx: Serum tests reveal elevated hormone levels Urine tests reveal elevated hormone levels CAT Scans or MRI confirm presence and size of adenoma Acromegaly also Dx’ed with Radioimmunassay or enzyme linked immunoabsorbent assay for GH level Treatment Radiation Medications: Bromocriptine (Parlodel) Octreotride acetate (Sandostatin) Transphenoidal Hypophysectomy “Moustache Dressing” / Packing Teach not to blow nose, sneeze, bend over Neuro Checks Visual Acuity,Visual Fields Need for Frequent Monitoring of Urine Output (Diabetes Insipidus) Fluid Replacement if Diabetes Insipidus Use of vasopressin (Pitressin), desmopressin acetate (DDAVP) Hormone Replacement POSTERIOR HYPOPITUITARISM - DIABETES INSIPIDUS Causes: Pituitary Tumor or Post-op anterior Hypophysectomy or Trauma Symptoms (Related to Decreased ADH) Excessive Urine Output Low urine specific gravity Dehydration/ Vascular Collapse Treatment Correct the underlying condition Fluid Replacement ADH vasopressin (Pitressin) desmopressin acetate (DDAVP) Replacement of ANTERIOR HYPOPITUITARISM Causes: Developmental Disorders, Vascular Lesions, Trauma, Tumor Symptoms related to decrease in hormone release GH (Growth Hormone/Somatotropin) Adult: No Change in Stature Children: Deficits in Growth ACTH (Adrenocorticotropic Hormone) Symptoms of Addison’s Disease TSH (Thyroid Stimulating Hormone) Symptoms of Hypothyroidism Gonadotropins Sexual and Reproductive Disorders Dx: Serum tests reveal decreased hormone levels Urine tests reveal decreased hormone levels CAT Scans or MRI confirm presence of lesions/tumors Treatment Hormone Replacement HGH Corticosteroids Hormones Correct the Underlying Condition if Possible Thyroid Sex POSTERIOR HYPERPITUITARISM - SYNDROME OF INAPPROPRIATE (INCREASED) ADH SECRETION Causes: Trauma, CNS Surgery, Oat Cell CA of Lung, Other Diseases Symptoms Related to Increased ADH: ***Fluid Retention*** EDEMA Cerebral Edema (Water Intoxication) Altered LOC Weakness/Lethargy Coma Serum hypo-osmolarity (dilutional hyponatremia) Oliguria / Concentrated Urine (High urine specific gravity) Hypertension 2 Treatment (SIADH usually self-limiting) ***Water/Fluid RESTRICTION*** Diuretics & Hypertonic Saline if condition severe Neuro Checks Demeclocycline (DMC) THYROID GLAND SECRETES: T3 T4 Thyrocalcitonin HYPERTHYROIDISM Thyrotoxicosis/Grave’s Disease/Toxic Nodular Goiter CAUSES: Autoimmune Familial Tendency Females 5-6 X’s > Males 30 - 50 year olds (Grave’s most in 40’s) Emotional shock, stress, infection SYMPTOMS: Grave’s Triad: 1.Goiter (& Thrill / Bruit) 2. Cardiac Symptoms 3. Exopthalamos Increased BMR - Increased Temp. Increased Cardiac ( Pulse, Cardiac Output, Pulse Pressure, Small Increase in Systolic BP) Atrial Fibrillation CHF Respiratory Stimulation Increased Sympathetic Adrenergic Activity Increased GI Peristalsis – Diarrhea Hyperactive Skin moist, increased oil Amenorrhea Osteoporosis & Fractures Thyroid Storm - Hyperthyroidism in the Nth Degree Severe Tachycardia Heart Failure Shock Fever (105 F) Agitation / Delirium / Coma Nausea & Vomiting Diarrhea DIAGNOSIS: Decreased TSH, Increased T4 (F T4) Primary Hyperthyroidism = Increased T3 & T4 but decreased trh & decreased TSH Thyroid Scan (6 or 24 hr radioactive iodine uptake) ECG Treatment: Antithyroid Medications: Propylthiouracil (PTU) Methylthiouracil (methimazole) Inderal (propanalol) to Rx tachycardia Radioactive Iodine (131I) 3 Tapazole Nursing Care: Vital Signs Assessment (Cardiac Assessment / meds. PRN) Clothing/ Light Blankets/ AC Eye Care Calm Approach Light THYROIDECTOMY Subtotal (5/6ths removed) Get patient euthyroid pre-op POST-OP THYROIDECTOMY Position Patient –Semifowlers Neck in alignment Prevent Hyperextension Vital Signs Assess for Hemorrhage Check for choking sensation / Sensation of dressing tightness Check for injury to parathyroids (Decreased Serum Calcium Positive Chvostek’s and Trousseau’s Signs Numbness and Tingling Laryngospasm) Have Calcium Gluconate and Tracheostomy Kit on hand Teach about Medications (Thyroid Replacement)Teach about the need to monitor for signs & symptoms of Hypo and Hyperthyroidism HYPOTHYROIDISM Myxedema in adults; Cretinism = Congenital CAUSES: Most Common = Surgical or Radiative Destruction of the Gland Idiopathic/Congenital Deficiency/Iodine Deficiency/ Drug Females > 50 years old SYMPTOMS: Decreased BMR (Cold Intolerance Weight Gain Hair Loss) Decreased Cardiac(CHF) Increased Cholesterol (Atherosclerosis & CAD) Slowed Intellectual Functioning/Sleepiness/ Coma Decreased Sympathetic Adrenergic Activity Decreased GI Peristalsis – Constipation Anemia & Bruising Menorrhagia & Infertility DIAGNOSIS: *TSH, T4 (Increased TSH, Decreased T4 ) Primary Hypothyroidism = Decreased T3 & T4 Thyroid Scan (6 or 24 hr radioactive iodine uptake) CT, MRI, Ultrasound Goal: Euthyroid TREATMENT: Lifelong Replacement of deficient Thyroid Hormone Synthroid = Drug of Choice NursingCare: Vital Signs Assessment Cardiac Assessment /Meds. For CHF prn Need for Decreased Calories Warm Clothing / Blankets / Use of Heat Care related to constipation Need for low intellectual level (Patient Teaching Considerations) Nursing Care Related to Medications: Administer all Meds. With Caution AVOID SEDATIVES Teach symptoms of Hypo & Hyperthyroidism Cardiac - Thyroid replacement increases O2 demands which can lead to angina (related to CAD) 4 PARATHYROID GLANDS Secrete PTH (Parathyroid Hormone) Maintain Serum Calcium & Phosphorus Levels HYPOPARATHYROIDISM Causes: After thyroid or parathyroid surgery Symptoms: Neuromuscular Irritability Tetany Laryngeal Stridor Cardiac Disrhythmias Idiopathic Chvostek’s Sign, Trousseau’s Sign Treatment: Calcium Gluconate Vitamin D and Supplementary Dietary & Elemental Calcium Teach Signs of Calcium Deficiency HYPERPARATHYROIDISM Causes: Benign Adenoma Symptoms: Pathologic Fractures Renal Calculi GI Symptoms Mental Changes Treatment: Surgical Removal of 3/4 of Parathyroids Correction of Electrolyte Imbalance IV & p.o. Fluids Diuretic Mithramycin Dietary Restriction of Calcium Prevention of Injury Assess for and teach the patient signs & symptoms of calcium excess and deficiency The Adrenal Glands Adrenal Medulla Produces: Epinephrine Norepinephrine Effects: Stress Response Cardiac Status, Vascular Resistance Respirations Urine Output, Glucose Metabolism ADRENAL MEDULLA HYPOFUNCTION No symptoms - Handled by Sympathetic Nervous System ADRENAL MEDULLA HYPERFUNCTION - Pheochromocytoma 5 ADRENAL CORTEX Adrenal Cortex Produces Mineralocorticoids Effects: Intravascular Volume Na & K reabsorption/excretion Increased Mineralocorticoids: Increased Na Retained So increased H2O Retained Increased Blood Volume Increased Blood Pressure Decreased K Retained (Increased K Excreted) Decreased Mineralocorticoids: Increased Na Excreted (Decreased Na Retained) So increased H2O Excreted Decreased Blood Volume Decreased Blood Pressure Decreased K Excreted (Increased K Retained) Adrenal Cortex Produces Androgen Effects: Mostly Same as Male Sex Hormones Adrenal Cortex Produces Glucocorticoids Effects: Glucose Metabolism Fat Metabolism HCl Secretion Inflammatory Response Bone Demineralization Cartilage Development Mental Status ADRENAL CORTEX HYPERFUNCTION 6 CAUSES: CHRONIC CORTICOSTEROID THERAPY Causes Cushing’s Syndrome Cushing’s Disease can also be caused by increased ACTH, adenoma or carcinoma of cortex CUSHINGS SYNDROME/DISEASE SYMPTOMS Related to Increased Mineralocorticoids: Hypernatremia, Hypokalemia Fluid Retention (Moon Face, Buffalo Hump) Truncal Obesity Hypertension Related to Glucocorticoids: Hyperglycemia Fatigue & Muscle Weakness Osteoporosis/Pathologic Fractures Child: Impaired Growth Increased Risk of Infection Altered Moods Capillary Fragility GI Ulcers Related to Androgens: Hirsuitism Mild Acne Menstrual Irregularities DIAGNOSIS Increased Plasma Cortisol Increased Serum Glucose, Na Decreased K 24 hour urines for: Increased 17 ketosteroids Increased 17 hydroxyketosteroids Serum ACTH (Increased if Hyperpituitarism) ACTH Suppression Test NURSING: ForvHyperglycemia Accuchecks Increased Insulin May be Needed onset of Diabetes Mellitus - Insulin (or Oral Meds) may be needed Can cause For Hypernatremia, Hypokalemia & Fluid Retention:Monitor fluids &electrolytes Replace PRN Daily Weights Hypertension:Frequent Monitoring Medicate PRN Notify MD PRN For Increased Risk of Infection Need for antibiotics for Rx &/or prophylactic purposes Protect from infected persons For Altered Moods Support/education/consults For Capillary Fragility Osteoporosis/Pathologic Fractures Fatigue&Muscle Weakness Safety issues. Patient protection/education Child: Impaired Growth To Prevent GI Ulcers Need for antiulcer meds. (Pepcid, Zantac, Mylanta, etc.) 7 ADRENAL CORTEX HYPOFUNCTION CAUSES: Abrupt D/C of high dose corticosteroids Life Threatening Bilateral Adrenalectomy Addison’s Disease: Congenital, Secondary to hemorrhage or infection, idiopathic, autoimmune SYMPTOMS Related to Increased ACTH & Increased MSH: Hyperpigmentation (Bronze-like) Related to Decreased Mineralocorticoids Hyponatremia, Hyperkalemia Increased BUN Fluid Loss Hypotension - Shock / Circulatory Collapse Related to Decreased Glucocorticoids: Altered Moods Lymphocytosis Hypoglycemia Intolerance to Stress Related to Decreased Androgens: Decreased Hair Decreased Sex Drive in Females Decreased Appetite DIAGNOSIS 8 hour IV ACTH Test / Cosyntropin Stimulation Test Decreased Plasma Cortisol Decreased Serum Glucose, Na Increased K 24 hour urines for: Decreased 17 ketosteroids Decreased 17 hydroxyketosteroids NURSING Need for life-long replacement hormones: Florinef May get testosterone for protein anabolic effect. Corticosteroids: Hydrocortisone, Prednisone, Decadron (dexamethasone) Assess F & E (I & O, Daily Weights, labs.) Electrolyte Replacements Monitor Glucose Levels, BP Emotional Support Teach that PRIOR TO ANY STRESSORS - NEED INCREASED MEDICATION BE:1/03 8