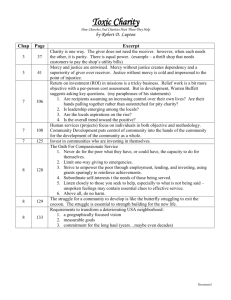
undergraduate orientation booklet
advertisement

Undergraduate Clinical Placement Orientation Manual January 2011 WELCOME Welcome to Werribee Mercy Hospital. This orientation booklet has been designed to provide you with some general information to assist you with your clinical placement. Our aim at Werribee Mercy Hospital is to provide you with the support that enables you to develop and achieve your assessment criteria. This placement will further provide the opportunities that will help facilitate the development of becoming a competent and confident registered nurse. ABOUT WERRIBEE MERCY HOSPITAL Werribee Mercy Hospital is a general community hospital comprising 200 beds and treats approximately 20, 000 inpatients annually. It is a public hospital campus that was opened in 1994 and is part of the Mercy Health & Aged Care Group. The hospital offers general surgical, general medical, maternity, neonatal, ambulatory care, palliative care services, day chemotherapy, renal dialysis, mother/baby unit, allied health services, hospital in the home and a 24 hour emergency department. There is also a large psychiatric service comprising acute care, community care and rehabilitation. The hospital is currently undergoing rapid expansion and redevelopment in order to meet the increasing demand for health services within the region. The hospital is busy, modern and provides a wide variety of current clinical experiences. Mission Statement In keeping with this statement of philosophy, Mercy health care institutions shall: Provide general and acute health care services to those who come to us in need; Design programs for the provision of acute health care services so as not to ignore the dispossessed of our times; Provide quality services with dignity and with the belief that the spirit of those rendering such services is paramount to the fulfilment of patient needs; Establish a continuing commitment to health education at all levels to meet the needs of our times. Core Values Compassion Hospitality Respect Innovation Stewardship Teamwork Ethical Guidelines in Clinical Practice Students must respect staff, patients, families and all who are welcome to Werribee Mercy Hospital regardless of their religious beliefs, nationalities and cultures. The dignity of each person must be upheld at all times. 1 FACILITIES AND AMENITIES Café Zouki offers a wide variety of hot and cold food, toasted sandwiches, salads, cappuccinos, soft drinks and cakes. Food may be eaten in the Café’s comfortable surroundings or in the outdoor eating area. Each ward also has a small kitchen area. Change Rooms Change rooms and showers are available for staff. The change rooms are located opposite the kitchen. Car Parking Car parking is available for staff members at a cost of $3 per day. ID badges must be presented at the car park booth. Public Transport The Hoppers Crossing Railway Station is located within 5 minutes walking distance of the hospital. Pastoral Care The Department of Pastoral Care aims to create a caring atmosphere through which the service of Christian ministry is made available to all people within the hospital and in particular provides support to enable patients, families and staff to call on their spiritual and/or personal resources, in meeting the events and challenges of life. Chapel Staff are welcome, to use the Chapel near the Boutique, for prayer or as a place of peace and rest. Mobile Phones Students are not permitted to carry their mobile phone on them whilst providing patient care. Mobile phones can be checked during breaks. Smoking Werribee Mercy Hospital is a totally smoke free hospital. 2 Identification Badges ID badges are a means of identifying the particular person. Students are required to wear their ID badge at chest height at all times whilst on duty. Clinical Uniform It is compulsory for students to wear the correct university uniform at all times whilst on clinical placements. Students must adhere to the uniform code outlined by the university. I f a student does not present in uniform they may be sent home from the clinical. Neat and professional attire must be maintained throughout the clinical placement including; The uniform must be clean. Long hair must be worn tied back. Nails are to be short and clean, without nail polish. Artificial / porcelain nails are not acceptable. Earrings: plain studs or sleepers should be worn. A plain wedding band may be worn. Necklaces and bracelets are not acceptable. For safety reasons, rings or studs worn in facial piercing may not be appropriate. Customer Service The Werribee Mercy Hospital values the provision of a quality service. In our working environment there is a clear relationship between the quality of care to customers and a collaborative and supportive working team. Customer satisfaction is integral to the process of ongoing evaluation. Patients are encouraged to complete a hospital questionnaire, in which their suggestions and comments are a welcome contribution to our continuous quality improvement program. All patients receive a brochure outlining their rights and responsibilities. Infection Control Infection control is an implicit component of the day to day activities of all health care workers. All staff and students will ensure that they understand the hospital’s infection control objectives and be able to articulate their role in reducing the risk of infection in the hospital environment. Standards Precautions apply to work practices which assume that all blood and body fluids are potentially infectious, and should be used as a first line approach to infection control. These precautions include good hygiene practices, particularly hand washing before and after patient contact, the use protective barriers which may include gloves, gowns, plastic aprons, masks, eye shields or goggles, appropriate handling and disposal of sharps and other contaminated or infectious waste, and use of aseptic techniques. Standard precautions are recommended for the treatment and care of all patients, regardless of their perceived infectious status, and in the handling of blood, all other body fluids, secretions, excretions, non intact skin; and mucous membranes. 3 Health Care Workers (HCWs) maybe exposed to, and transmit, vaccine preventable diseases Maintenance of immunity to such diseases helps prevent transmission of infection to and from HCWs and patients. The likelihood of contact with patients and/or blood or body substances determines vaccination recommendations. The following vaccines are recommended for all nursing staff prior to the commencement of placement programs or employment. Hepatitis B Course of three doses must be completed. Antibody levels checked after third dose. Influenza Annual vaccination is recommended for all staff Measles/Mumps/Rubella (MMR) Booster dose recommended for all persons age 18 – 30 years. Tetanus/Diphtheria/Whooping cough A single booster dose is recommended for all health care workers. Varicella (Chickenpox) If no history of infection then blood test check is recommended. If no immunity demonstrated then vaccination is required. Manuals Policy manuals are readily available in all units of the hospital, and are provided to guide staff in obtaining uniform standards of practice. It is important that students and staff become familiar with the content of these manuals. The policies are divided into three books: General Hospital Policies (white cover), Infection Control (yellow) and Emergency (orange) Mercy Intranet is also available to access the most up to date policies and procedures. 4 NOTES Clinical Teacher: _________________________________________ Pager Number: ________________ Phone Number: _______________ Ward: __________________________________________________ Ward Phone Number: _____________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ _______________________________________________________ 5 ORIENTATION Objectives of Orientation To meet the clinical teacher and review expectations of the clinical placement and assessment criteria. Familiarize with the hospital and general practice and procedures. Understand the legal and ethical responsibilities of the undergraduate nursing student in relation to clients, their relatives and the Werribee Mercy Hospital. Identify the expected outcomes / objectives for the clinical placement that is relevant to the clinical experience to be undertaken. STUDENTS RESPONSIBILITIES Students must present a current police check on the first day of clinical placement. Students should ensure their vaccinations are up-to-date. Students are expected to work a 7 day rotational roster including night duty; this is an agreement between the hospital and the Universities. Students who are going to be absent are required to notify the unit they are working on and also the clinical teacher. Any absences must be supported with a medical certificate. The Nurses Board of Victoria (NBV) perceive clinical placement as essential to prepare nurses to be safe and competent. Therefore it is a requirement of the NBV that nursing students attend clinical placement and complete the required hours. Try to be punctual. If you are going to be late please contact the unit you are working on. Identification badges and uniforms must be worn at all times during clinical placement. Students are expected to complete all of the assessments identified by the university. Students must identify themselves to staff, patients and visitors. Students are reminded that maintaining confidentiality is paramount. Students are expected to respect and uphold the Werribee Mercy Hospital’s values whilst on clinical placement. Students are required to familiarize themselves with the Werribee Mercy Hospital policy and procedures. Students are expected to report any concerns or changes in patient state immediately to nursing staff. Students should be motivated, dedicated, show initiative and actively participate in patient care appropriate to their level of learning experience. Students are expected to care for a minimum of two acutely ill patients depending on their level and experience. Students will discuss the patients Medical/ Nursing management in detail and deliver this management appropriately to their level of learning experience. Personal belongings should be kept to a minimum. Werribee Mercy Hospital will not take any responsibility for missing belongings. 6 CLINICAL TEACHER RESPONSIBILITIES The clinical teacher / preceptor / buddy must be available for students to contact him / her. The clinical teacher will have a phone. The clinical teacher will confirm shift times and ward allocation at orientation, and assist students in the completion of the various universities requirements. The clinical teacher will provide support and supervision to each student to enhance learning and to assess his / her competence. The clinical teacher / preceptor will complete the clinical appraisal by reflecting on the evidence of the students’ performance. The clinical teacher / preceptor have a responsibility in providing ongoing feedback to each student regarding his / her progress and discuss recommendations for improvement. Any concerns regarding a students’ progress will be discussed with the universities undergraduate coordinator and subject coordinator within a timely manner and not left until the interim or final appraisal. Unsatisfactory progress of a student will require the clinical teacher to place the student on a learning program. This usually requires written objectives for the student to achieve with a maximum of three days from implementation. Failure to achieve the stated objectives, the student will be placed on a clinical challenge contract to be negotiated between the subject coordinator, clinical teacher and student. The clinical coordinator will review each student’s completion of their personal learning objectives weekly, and discuss these with the student. The clinical teacher will set aside a specific time each day to meet with the students for debriefing and discussion. ROSTERS Rosters will be developed on the first day of placement during orientation. A clinical area will be allocated to each student according to availability and previous clinical experience. Each student will have the opportunity to make some shift requests, however there is no guarantee that the hospital will be able to accommodate these. Ward Shift Times: Emergency Department Early (D) Late (E) Night (N) - Early (D) Late (E) Middle (M) 0700 - 1530 1300 - 2130 2100 - 0730 0700 -1530 1300 -2130 1000 -1830 DPU Early (D) - 0700 - 1530 Middle (0930) 0930 -1800 Late (E) 1130 - 2000 Theatre 0800 - 1630 (D) 1130 - 2000 During this time you are entitled to a 10 minute tea break and a 30 minute meal break. 7 CLINICAL DEBRIEFING / GROUP SUPERVISION CONTRACT 1. The supervisor and supervisee are both responsible for their own clinical practice. 2. Debriefing/supervision should take place in a confidential environment. 3. Confidentiality is maintained between the supervisor and supervisees unless there is a breach in codes of practice or MHAC policy. Prior to any breach of this confidentiality the issue will firstly be discussed with the supervisee. 4. The supervisor will have the option of keeping a record of clinical supervision/debriefing sessions and agrees to keep this information stored in a confidential place. This information will not be used for any other purpose apart from supervision/ debriefing. 5. The model of supervision/debriefing being used is one of support and development. Ideally the topics for discussion will have been planned in advance by both the supervisor and supervisees. 6. The time is to be used to discuss clinical issues not personal or outside issues. 7. The supervisor will ensure that the session will remain professional. It is not a venue for gossip and/or destructive criticism about other staff members or units. 8. If a session is fostering a culture of negativity or promoting discontent and blame among the wider group it is the responsibility of the supervisor to bring the group back on track with problem solving strategies or positive solutions. 9. This contract whilst needing to be adhered to is always negotiable. Date: Name of Supervisor: Signature of Supervisor: Name of Supervisee: Signature of Supervisee: 8 STUDENT PRIVACY AND CONFIDENTIALITY AGREEMENT As a student on clinical placement at Werribee Mercy Hospital I agree that I will abide by the privacy policy, privacy legislation and privacy procedures which apply to the Werribee Mercy Hospital. In particular, I agree that: a) I will read both the Mercy Health & Aged Care and the Entity’s Privacy Policy and Procedures (however named) within seven (7) days of commencing employment. b) I shall not, during my period of placement with Werribee Mercy Hospital, disclose or use any patient files, medical reports or confidential knowledge obtained through my placement with Werribee Mercy Hospital other than to perform my duties as authorised and detailed in my University guidelines for clinical placement or specifically requested by my supervisor to perform. c) Any breach of Werribee Mercy Hospital’s privacy policy or privacy legislation, caused by me, whether intentional or not, may result in disciplinary action, including immediate termination. d) I may be held personally liable for any compensation payable resulting from a breach of privacy which has been caused by me, whether intentional or not. e) The obligations contained in clauses (a) to (c) inclusive will continue even after the completion of my clinical placement with Werribee Mercy Hospital. f) Upon termination of my clinical placement with Werribee Mercy Hospital I will immediately deliver to Werribee Mercy Hospital all patient files, medical reports or other documents which are in my possession or under my control which in any way relate to the business of Werribee Mercy Hospital or its patients past or present. Name: ……………………………………... Signed: ……………………… Date: …/…/… Witness Name: …………………………… Signed: ……………………… Date: …/…/ 9 Code of Conduct Policy Statement: This Code of Conduct outlines what is expected by all people employed directly or indirectly by entities comprising the Mercy Health group. It is designed to help you understand your responsibilities and obligations, and provide guidance if you are faced with an ethical dilemma or conflict of interest in your work. Policy It is expected that all employees will demonstrate the following behaviours at work: To respect and work with the Mission and Vision of Mercy Health To aspire to demonstrate the Values of Mercy Health and the associated behaviours, namely: Compassion Behaviour: Demonstrate kindness and generosity of spirit Provides support in times of need Displays a passion to serve others Hospitality All people are greeted and made comfortable Seek to provide assistance where needed Provide a consistent level of customer service, internally and externally Respect Behaviour: Recognises that each person is individual and unique Strives to be open and honest in all things, at all times Delivers good and bad news in ways that ensure people retain their sense of dignity and self respect Innovation Behaviour: Embraces change as an opportunity for renewal and improvement Seeks opportunities to try new ideas and, as Mercy people, be acknowledged for their contribution Focuses on present and future actions Stewardship Behaviour Holds in trust and builds on the tradition and spirit of Mercy Develops Mercy people to be accountable for the highest standard of performance Seeks opportunities to lead and made decisions, within agreed financial frameworks Teamwork Behaviour: Working together to serve others and provide the best possible care Communicates openly and honestly, to work as team members for the collective good Respects the need and feelings of others and actively seeks their perspective It is expected that all employees of Mercy Health will demonstrate the following behaviours at work: Policy Compliance Comply with all Mercy Health policies, procedures and relevant statutory regulations. Uniform Adhere to the specified uniform policy, or if not applicable, to present for work neatly and 10 professionally attired in a manner appropriate to the setting and context of the workplace. Position Description Comply with the organisational Position Description (PD) for their role and actively take part in regular appraisal process. Smoking Adhere to non-smoking policies with Mercy Health facilities Alcohol and Drugs Present for work at all times free from the effects of alcohol and or other drugs that affect the ability to work safely (see Risk Management Alcohol and Drug Policy). Environmental Setting Respect the workplace and its environmental setting Outside Employment Not engage in outside employment or conduct a business, trade or profession without written authority from their General Manager, Chief Executive Officer or Chairperson as appropriate. Consideration of requests to engage in outside employment would need to be established to determine whether the outside employment would give rise to an actual or perceived conflict of interest. External Committees / Boards Not participate as a member of any external Committee or Board that may cause a conflict of interest with their role at Mercy Health. A written request specifying the time and obligations of the desired membership should be provided to their General Manager, Chief Executive Officer or Chairperson as appropriate. Acceptance of Gifts and Benefits Not accept gifts or benefits for services performed in connection with their perceived duties and responsibilities, which might directly, indirectly or be perceived to comprise them in their official capacity. Conflict of Interest Not engage in activities or behaviour that causes actual or potential conflict with personal interests and employment responsibilities. Where a personal interest exists employees must openly disclose that interest to their General Manager, Chief Executive Officer or Chairman of the Board as appropriate. Intellectual Property It is a condition of employment that all employees assign to Mercy Health all intellectual property rights in the works created by them during employment with Mercy Health. The right to retain intellectual property rights of work may only be approved by their General Manager, Chief Executive Officer or Chairperson as appropriate or if it can be demonstrated that Mercy Health’s time, name, information or resources were not utilised in producing the work. Moral Rights It is a condition of employment that all employees confirm they will not exert their moral rights during their employment with Mercy Health. For example, if an employee creates artistic works, written material, computer programs etc for a facility and the facility wants to move or change the original works, it needs to be agreed that the Mercy Health facility will have rights to move or change those works. Excessive Hours To ensure sufficient sleep and rest is obtained in order to perform work duties in a safe and responsible manner. Unacceptable behaviour / serious misconduct includes, but is not restricted to: - Breach of patient/resident or staff privacy 11 - Breach of patient/resident or staff privacy Breaching Mercy Health policies/procedures Failure to report a work related accident/serious near miss Continual lateness for duty/unauthorized absence Careless action/neglect of professional conduct or duty Failure to report a criminal conviction or impending action, which in the opinion of Mercy -Health, directly relates to a risk in performing your duties Failure to disclose a prior or current conviction when requested to do so Sleeping during working hours where there is a requirement to be working Falsification of qualifications leading to employment Public misrepresentation – causing damage to the reputation or image of Mercy Health or its employees Actions which deliberately or recklessly injure other employees, patients, clients or visitors or that place their health, safety or welfare at serious risk Improper use of workplace equipment, supplies and other physical resources Breaches of this policy will be regarded as a discipline issue. Cases of unacceptable and/or serious misconduct may result in summary dismissal of employment. Employee Declaration I agree that I have read and understand the Mercy Health Code of Conduct Policy. Signature: ____________________________ Date: ___________________ Witness: _____________________________ Date: ___________________ Definitions Term Mercy Health Group Definition All facilities and entities across Mercy Health References All Mercy Health Policies AS8002: Organisational Code of Conduct 1983 Facility Staff Handbooks 12 HOSPITAL UNITS C2 – Surgical Unit C2 is a 16 bed unit that primarily cares for patients who have undergone elective and emergency surgical procedures. These types of surgical procedures include; general surgery (eg Laparoscopic Cholecystectomies, appendicectomies), gynaecology, paediatrics and adult ENT, some orthopaedic and plastic surgery procedures, and urology. The ward area also includes a four-bed Monitored Beds Area which facilitates some higher level monitoring of Postoperative Patients, as well as acutely unwell medical patients. C3 – Acute Medical Unit C3 is a 28 bed unit. This unit is dedicated predominately to care for patient with medical conditions. These include COAD, Pneumonia, Infectious Illness, cellulitis, renal failure, CVA, AMI, Diabetes, DKA, APO, IHD and Heart Failure. This clinical area will enable students to develop, consolidate and extend their skills within the area of medical nursing. C3 is set up with a security unit for wandering confused patients, which is affectionately known as the granny tracker system. The unit works by activating an alarm on the four exits to C3. The patient at risk must wear the activation device as an anklet. If the patient wearing the devices passes through an exit once they have been activated, an alarm sounds at the desk area and a display panel indicates which exit has been passed. The alarm can be turned off once the patient has been found by turning the key twice to the left until it is line with the black marker. D3 – Medical Unit & Gabrielle Jennings Centre – Palliative Care Unit D3 and the Gabrielle Jennings Centre is an integrated unit with 10 palliative care beds and 18 medical beds. Palliative care patients are admitted for pain management, terminal care and respite. The care provided to a palliative patient is a team effort. Registered Nurses work closely alongside Medical staff, Social Workers, Physiotherapists, Occupational therapists, Speech Pathologist, Pastoral Carers, Pharmacists and volunteers to provide optimal holistic care to the patients. Ambulatory Care Unit – Day Procedure, Renal Dialysis, Hospital in the Home (HITH), Midwifery in the Home (MITH) The Ambulatory Care Department cares for patients who are having a procedure where they will be admitted and discharged on the same day or require a nursing service at home. It consists of the following units: Day Procedure: cares for patients having medical and surgical procedures or chemotherapy Renal dialysis: Provides haemodialysis for patients with end stage renal failure. Hospital in the Home: provides nursing care for acute patients in the home Midwifery in the Home: provides postnatal care in the home for women after childbirth. 13 Also managed by this department is the: Preadmission service: All patients having surgery have their health details checked by a nurse prior to the procedure. Home Oxygen: Co-ordination of oxygen for patients who require it at home. D2 – Childbirth Centre The Childbirth Unit is a busy integrated unit that provides antenatal, labour, birth and postnatal care. Other services include Pregnancy Booking Clinic, Pregnancy Day Stay, Childbirth Education, Breastfeeding Day Stay, Midwifery in the Home and Team Midwifery Program. Obstetric care is provided by consultant obstetricians and one GP Obstetrician. The current birth rate is approximately 2,000 births per year. The Special Care Nursery provides Level 2 care, and accepts babies from 32 weeks gestation. The unit can provide care for up to 12 Neonates. Emergency The Emergency Department was recently upgraded, with the new department being opened in June 2005. The new Emergency Department is currently seeing 37,000 patients per year, with that number expected to rise to 50,000 over the next two to three years. The Emergency Department has a total of 21 cubicles. Currently we are working with 10 cubicles which include 2 resuscitation bays. We also have a procedure room where minor procedures such as suturing and plastering are attended to, a dedicated eye room and a negative pressure isolation room. The new Emergency Department provides separate waiting areas for adult and paediatric patients, a triage room so patients who need privacy can be assessed quickly on arrival and a lounge room for distressed family members. There are dedicated facilities to care for the increasing number of patients presenting with mental health issues. The Crisis Assessment and Treatment Team (CATT) are based permanently in the ED. Operating Suites The Operating Suite at Werribee Mercy Hospital consists of; General Theatres 1 Endoscopy Room A seven (7) bay recovery CSSD General and gynaecological surgery are the predominant types of surgery performed in this very busy and efficient unit. Other specialties include; ENT Urology Plastics Paediatric general Oral Maxillary Basic Vascular The Endoscopy Unit (located in the Day Procedure Unit) carries out Flexible cystoscopies, bronchoscopies, ECT, colon and gastroscopies 14 Diabetes Education The Diabetes Education Unit has been operating for the past 6 years. There is a Diabetes Educator available 4 days a week. She sees both inpatients and outpatients. Hospital Admission Risk Program (HARP) 1. HARP aims to prevent avoidable hospital presentations and admissions. 2. HARP targets people with chronic disease, aged and/or complex needs that frequently use hospitals or are at imminent risk of hospitalisation and could benefit from coordinated care. 3. Health services may have people who present frequently for many different reasons. HARP specialises in managing people with diabetes, chronic respiratory disease, chronic heart failure, complex psychosocial and complex aged needs. 4. HARP provides specialist medical care and multidisciplinary services through an integrated response of hospital and community services, delivered in hospital, community and home-based settings. 5. HARP works in collaboration with other acute, community, aged care and specialist services, but does not duplicate them. 6. For clients who are acutely, psychiatrically unwell and meet the mental health eligibility criteria, referral to an area mental health service is the most appropriate response. What does HARP provide? Our HARP Care Coordination Team is multidisciplinary and includes Allied Health and Registered Nursing staff. We also utilise the services of medical specialists where appropriate. The services we provide are: Short Term Care Coordination: Outreach service: hospital, home and community visits. Comprehensive assessment. Development of a self-management care plan. Education about chronic conditions and how best to manage them. Linking in with the local health network (GP, specialists, home services, support groups, allied health and counselling). Advocating for the client’s individual needs and goals. Rehabilitation (Pulmonary and Heart Failure): Twice weekly individualised exercise sessions for 8 weeks (Pulmonary) and 10 weeks (Heart Failure). Education discussions with multidisciplinary team targeting disease education and self-management. 15 Who is eligible for HARP? Patient/Client exhibits complex care, aged or psychosocial needs, and/or unstable or complicated chronic respiratory disease, chronic heart failure, diabetes or other chronic disease AND Has had at least one (1) unnecessary or avoidable hospital presentation or admission in the past twelve (12) months AND Meets the screening criteria for each HARP care stream as follows: Chronic Obstructive Pulmonary Disease: Diagnosis of moderate to severe COPD as per Lung Function Test. No age limit. Pulmonary Rehabilitation: Diagnosis of COPD as per Lung Function Test or other chronic lung conditions (Pulmonary Fibrosis or Bronchiectasis). Excludes unstable cardiac conditions, unstable pulmonary hypertension and clients with severe physical, neurological or psychological conditions which prevent participation in exercise. Chronic Heart Failure: Diagnosis of Chronic Heart Failure (CHF) as per Echocardiography. No age limit. Heart Failure Rehabilitation: Diagnosis of Chronic Heart Failure (CHF) as per Echocardiography. Excludes medically unstable clients and clients with severe physical, neurological or psychological conditions which prevent participation in exercise. Diabetes: Diagnosis of Type 1 (T1DM) or Type 2 (T2DM) Diabetes as per Fasting Blood Glucose (FBG) pathology. High risk diabetic patient/client (i.e. psychosocial issues, poorly controlled diabetes). Excludes gestational diabetic and juvenile clients. Older People with Complex Needs: 55+ years of age. Two or more chronic diseases. Complex psychosocial issues contributing to hospitalisations (e.g. self-care, 16 limited support network, demanding care responsibilities). MEDICATION MANAGEMENT Students must be supervised at all times when preparing and administrating medications. This hospital has a double checking protocol which includes all intravenous, intramuscular, subcutaneous medications. Please familiarize yourself with the section on medications in the nursing procedures manual and the hospital protocol on double checking of medications (H005). Safe Medication Administration Principles Right Record Right Drug Right Dose Right Patient Right Route Right Time AND Check the expiry date of the medication Check the patient does not have any allergies Question the order if it is unclear or illegible. Check the labelling of the drug or ampoule. A patient has the right to refuse their medications if this occurs, report to doctor and nurse in charge. Converting Metric Units 1kg = 1000g 1g = 1000mg 1mg = 1000mcg 1L = 1000ml Administration of drugs There is one formula to calculate the amount of medication required for an injection or oral tablet. Drug to be given (Mass/ volume) Strength required = x Volume Stock strength 1 Drugs to be given: is the mass or volume of stock to be given to the patient. Strength Required is the amount of drug required for the patient. Stock Strength is the amount of drug in the stock per an amount of drug (volume of the ampoule). Volume: is the volume of the stock solution if applicable. 17 Intravenous Infusion Rates Formulae: Volume = Rate x Time Time = Volume --------Rate Rate = Volume --------Time Volume is measured in units of volume (mL, L, etc). Time is measured in units of time (mins, hours, etc). Rate is measured in units of volume per time (mL/hour, L/day, etc). Intravenous Drug Doses Standard giving set: 20drops per minute = 1ml Microdrip set: 60 microdrops = 1ml drip rate = rate (mL/hr) _________ 1 x drop factor (drops/mL) __________________ 60 minutes To calculate mcg/kg/min This formula is often used to calculate inotrope and vasoactive drug dosages. mcg/kg/min = Amount required X 1000 (convert to mcg) X mls/hr (rate set) Volume 60 (convert to min) weight mls/hr = Volume X 60 (convert to min) Amount Required 1000 (convert to mcg) X mcg/min (dose required) X weight A student must never administer any type of medication unsupervised 18 COMMONLY USED MEDICATIONS SURGICAL Pethidine Tramadol Metoclopramide Prochlorperazine Panadeine Forte Kytril Dexamethasone Midazolam Metronidazole Cephazolin Ceftriaxone Ampicillin Getamicin Amoxycillin Endone Dolasetron Panadeine Forte Diflofenac Oxycodone MEDICAL Clexane Heparin Warfarin Salbutamol Atrovent Sodium Valproate Ranitidine Roxithromycin Atorvastatin Lanoxin (Digoxin) Frusemide (Lasix) Endone Ibersartin Potassium Enalapril Maleate Actrapid Levemir Magnesium Ramipril Clexane Azithromycin Protophane Metformin PALLATIVE Fentanyl Ketamine Haloperidol ANAESTHETICS Propofol Sodium Thiopentone Atracurium Atropine sulfate Vecuronium Suxamethonium Rocuronium bromide Adrenaline DOCUMENTATION GUIDELINES Always date and time all entries. Writing should be legible. Always print your name clearly after your signature. Always print clearly the designation of the author. Be objective and clearly reflect the event of the shift. Additional entries can be added if an event occurs. Entires should not be written prospectively ( or out of date / time order) Liquid paper should never be used. Errors should be initialled and a line put through them. Do not leave any spaces between previous entries and the one you are writing. Always ensure bradma labels are applied to the page you are writing on or that the patient’s details are written including name, DOB, UR number. Students must always get a registered nurse to co-sign their entries. Ensure if referring to anyone in the notes, e.g. Doctor that you use their surname and don’t just document RMO. Changes in patient care should be clearly documented with investigations and plan of treatment outlined. 19 HANDOVER GUIDELINES Handover is a process of communicating the current information and condition of the patient’s on the ward. Handover is commenced at the start of the shift and last approximately 30 minutes. There are different styles of handover throughout the hospital these include, taped handover, verbal handover and individual handover. Guidelines for Handover Be concise. Handover any abnormal results. Handover the patients Patients: Name Written on handover sheet. Age: Reason for Admission / Diagnosis: Written on handover sheet. Past History: Operation / treatment so far: Observations: Input: Output: Mobility: Hygiene: Wound Care: Pain: Emotional: Social: Plan: Written on handover sheet. Any relevant past history: - Medical past history. - Smoker, alcohol, drug use. - Allergies - Psychiatric history. Discussed. Including relevant medications / relevant blood results. Any vital signs outside of the normal limits and treatment given as a result. IV therapy: Rate and if relevant fluid. Date of the last IV site change. Diet: any restrictions. FBC Need for Dietician involvement? IDC & measurement frequency, Trail of void. Bowel activity. Drain tubes/ vaginal packs Level of mobility, any changes in mobility. Need for Physiotherapy involvement? Level of assistance. Description of the wound; type, location and size. Dressing and frequency, any changes to the wound. Skin integrity/pressure area care. Type, location, intensity, duration. What analgesia has been administered and it’s effectiveness. PCA or Epidural: Psychological/emotional status eg. Patient’s reaction to surgery, illness or treatment. Need for Pastoral Care involvement? Any issues which need to be discussed. Need for social work/ interpreter involvement? Planned procedures or treatment. Discharge planning: when, what is required, what needs to be organised, etc. 20 FLUID BALANCE CHARTS Maintaining an accurate fluid balance chart is an important aspect of nursing care that assists with fluid management therapy. Where indicated any patient who requires close observation or monitoring of fluids should be commenced on a fluid balance chart. It is advisable that you familiarise yourself with the different charts that are used in the clinical area you will be working in. It is also desirable that you will subtotal the fluid balance chart throughout the shift ensuring you maintain your patient’s fluid status. Fluid Measurements Cup Tea / Coffee 180mls Bowl of soup 210mls Carlton of Milk 140mls Tumbler of Fluid 200mls Container of Juice 110mls Jelly 120mls Ice-cream (Dixie) 150mls Icy-pole 80mls 21 EARLY TIME GUIDE 0700 Handover, allocations Intro to patient Mane tablets, IV AB’s s/c injections, Insulin 0730 0800 Name: Room: Dr: 0830 Work out time plans Look at patient’s charts, care plans Patient hygiene, beds 0900 0930 Patient hygiene, beds Morning tea 1000 Wound dressings Update & sign care plans, FBC charges, PAC 1030 1100 1130 1200 1230 1300 1330 Name: Room: Dr: Name: Room: Dr: Medications, injections QID obs Check updated info on patient BSL’s / Insulin Lunch Prepare patient for lunch Update FBC, PAC Handover Patient rest period Write nursing notes 1400 1430 TDS obs and medications 1500 Check charts Update care plans Home time 1530 Name: Room: Dr: REPORT: BSL’s <4mmol or >8mmol Urine <30ml/hr, pH, leukocytes Blood or protein Temp <35.5 or >37.5 Pulse <60 or >110 Resps <14 or >24 Systolic BP <100mmhg Sa02 <95/% PATIENT 1: PATIENT 2: NURSING NOTES: Visualise patient from head to toe Mobility, e.g. RIB, NWB Wounds, e.g. dressings, PAC Fluid balance, e.g. IDC, IVT, FBC, FWT Pain Control Medications, injections, AB’s Observations PATIENT 3: PATIENT 4: 22 LATE TIME GUIDE Name: Room: Dr: 1300 1330 Handover, allocations Intro to patient TDS obs and medications 1400 Work out time plans 1430 Look at patient’s charts, care plans 1500 1530 Afternoon tea 1600 QID Obs 1630 QID & BD Medications 1700 Check updated info on patient Name: Room: Dr: Name: Room: Dr: Name: Room: Dr: 1730 BSL’s / Insulin Prepare patient for dinner 1800 Dinner break 1830 Update FBC, PAC 1900 1930 Write nursing notes 2000 TDS, QID obs and medications 2030 Patient hygiene, dressings BSL’s, Insulin 2100 Check charts Update care plans 2130 Home time REPORT: BSL’s <4mmol or >8mmol Urine <30ml/hr, pH, leukocytes Blood or protein Temp <35.5 or >37.5 Pulse <60 or >110 Resps <14 or >24 Systolic BP <100mmhg Sa02 <95/% NURSING NOTES: Visualise patient from head to toe Mobility, e.g. RIB, NWB Wounds, e.g. dressings, PAC Fluid balance, e.g. IDC, IVT, FBC, FWT Pain Control Medications, injections, AB’s Observations PATIENT 1: PATIENT 2: PATIENT 3: PATIENT 4: 23 ROOM 0700 0800 0900 1000 1100 1200 1300 1400 1500 HANDOVER TIME PATIENT 1 PATIENT 2 PATIENT 3 PATIENT 4 PATIENT 5 1400 1500 1600 1700 1800 1900 2000 2100 2200 25 26 EMERGENCY RESPONSE CODES EMERGENCY: DIAL 3333 RED - FIRE ORANGE - EVACUATION BLUE - MEDICAL EMERGENCY PURPLE - THREATS – BOMB, ARSON, EXTORTION YELLOW - INTERNAL DISASTER BROWN - EXTERNAL EMERGENCY BLACK - HOLD UP, ASSAULT GREY - PSYCHIATRIC EMERGENCY 27 BASIC LIFE SUPPORT SUMMARY 2010 [Reference – Australian Resuscitation Council (ARC)] D R A B C D Check for danger to self/patient/bystanders. Response. If unresponsive, call for local help and call 3333 and state Code Blue and the location. Airway: - visually inspect the airway - clear the airway prn; suction is recommended - open the airway – head tilt & chin lift or jaw thrust Breathing. If not breathing normally or not at all, deliver 2 effective breaths (allowing about one second per inspiration) with a laerdal circuit connected to Oxygen flowmeter set at maximum delivery. Check for * signs of life; if no signs of life, commence chest compressions (lower half of sternum, one third the depth of the chest cavity). Aim 100 compressions per minute. Compression to ventilation ratio 30:2. Pause compressions for ventilation. Defibrillation – apply defibrillation pads (‘Multifunction Adult Defib Electrodes’) as soon as available (when there are no signs of life & the individual is over 8 years of age) and follow the audible prompts. The defibrillator should be turned on in AED mode. * Signs of Life Conscious Responsive Breathing Moving No signs of life Unconscious Unresponsive Not breathing normally Not moving Management of foreign body airway obstruction (choking): ‘…The victim with an effective cough should be given reassurance and encouragement to keep coughing to expel the foreign material’ (ARC). In the case of conscious victim with severe airway obstruction (ineffective cough), ‘…perform up to five sharp back blows with the heel of one hand in the middle of the back between the shoulder blades’ (ARC). ‘…If back blows are unsuccessful the rescuer should perform five chest thrusts. Check to see if each chest thrust has relieved the airway obstruction. To perform chest thrusts identify the same compression point as for CPR…these are similar to chest compressions but sharper and delivered at a slower rate’ (ARC). Resuscitation in late pregnancy: ‘…In the obviously pregnant woman the pregnant uterus causes pressure on the major abdominal vessels when she lies flat, reducing venous return to the heart. The pregnant woman should be positioned on her back with her shoulders flat and sufficient padding under the right buttock to give an obvious tilt to the left’ (ARC). Extra points relating to defibrillation: - apply pads firmly to bare, dry & hairless skin - avoid placing pads over ECG electrodes, any medication patches, implanted devices eg. pacemakers/CVC insertion sites - avoid having the victim in contact with metal fixtures eg. bed rails - position pads below the right collarbone & the other, below the left breast over the ribs in line with the armpit - when in AED mode, follow audible prompts if ‘shock’ is advised, loudly state ‘all clear’ & visually check that everyone is clear of the patient & bed. 28 CHECKLIST This needs to be completed on the first day of clinical placement CAN YOU PROMPTLY LOCATE: () Resuscitation Trolley Break Fire Alarms Air Viva - paediatric and adult Paediatric emergency equipment Wall oxygen and suction Portable oxygen and suction Fire Extinguishers Fire Hose Reels Red Phones Designated Evacuation Area Emergency Buzzer Duress Alarms Bomb Threat Forms Emergency Procedures Manual Practices & Procedures Manual Communication Book Incident Forms Utility Room - clean / other Storage Room Drug Room Call bell system 29 CHECKLIST Continued ARE YOU ABLE TO: () Use telephone system Contact VMO’s and RMO’s CAN YOU PROMPTLY LOCATE: Thermometers Intravenous / Blood Taking Trolley Pathology tubes, forms, plastic bags Asthma equipment: drugs, nebulisers, peak flow meters Blood Glucose Monitor Suture equipment: suture material, instruments, local anaesthetic Syringes, needles Intravenous, intra-muscular and oral medication Suppositories, antibiotics, vaccines Plaster trolley Sterile stock: gowns, drapes, dressing trays Patslide Name bands / Allergy bands 30 ABBREVIATIONS A A&B A&E A/N A/V A/W AAA Ab / Abort Abdo ABG AB's AC ADLs ADT AE A/F AF AFI AFP AIDS AK AKA ALD AMI Amp Anaes ANC Ant. AO A-P APH APO Appt APTT ARDS ARF ARM ART ASAP ASD AUM AUR AV AXR B B/F Apnoea and bradycardia Accident and Emergency Antenatal Anteverted Associated with Abdominal aortic aneursym Abortion Abdomen Arterial blood gases Antibiotics Antecibum – before meals Activities of daily living Adult diphtheria and tetanus Air entry Artificial feeding Atrial fibrillation Amniotic fluid index Alphafetoprotein Acquired immune deficiency syndrome Above knee Above knee amputation Alcoholic liver disease Acute myocardial infarction Ampoule anaesthetics Antenatal Classes anterior Admitting officer Anterior - posterior Antepartum haemorrhage Acute pulmonary oedema Appointment Activated partial thromboplastin time Adult respiratory distress syndrome Acute renal failure Artificial rupture of membranes Arterial, artery As soon as possible Atrial septal defect Associate unit manager Acute urine retention atroventricular Abdominal x-ray Breastfed 31 BA Ba Enema / Meal BBA BBB BCC BCG BD BFDS BGL BHCG BIBA Bili BKA BMI BPS BNO BO BOS BP BPD BPM BSE BSL BSO B/W Bx C c/o Ca CA125 CABG CAD CAG Cas CATT CCF CCP CCT CCU CE’s CEA CHB CHD Chol Chole CI CIN Circ CIS CLD Bowel action Barium enema / barium meal Born before arrival Bundle branch block Basal cell carcinoma Vaccination against tuberculosis Twice daily Breast Feeding Day Stay Blood glucose levels Beta Human Chorionic Gonadotrophin Brought in by ambulance Bilirubin Below knee amputation Body Mass Index Biophysical profile score Bowels not open Bowels open Base of skull Blood pressure Biparietal diameter Beats per minute Breast self examination Blood sugar level Bilateral salpingo-oopherectomy Birth weight Biopsy Complaining of Carcinoma Tumour marker for ovarian carcinoma Coronary artery bypass graft Coronary artery disease Coronary artery graft Casualty Crisis assessment triage team Congestive cardiac failure Central chest pain Controlled cord traction Community care unit Cardiac enzymes Carcino embryonic antigen Complete heart block Congenital heart disease cholesterol Cholecystectomy Coitus interruptus Cervical intraepithelial neoplasm Circumcision Carcinoma in situ Chronic lung disease 32 cm CMV CNS CO CO2 COAD CP CPAP CPD CPR Creat Creps CRF CRP CS or C/S CSF CSU CT CTG CTR CTS CVA CVC CVL CVP CVS CWMS Cx CXR D D&C D&E D&V D/C D/W DBE DD DIC DM DNA DNW DOA DOB DOM DPM Dr. DRG DT centimeter Cytomegalo virus Central nervous system Clinical Nurse Specialist Carbon monoxide Cardiac output Carbon dioxide Chronic obstructive airways disease Chest pain Continuous positive airways pressure Cephalo pelvic disproportion Cardiopulmonary resuscitation Creatinine Crepitations Chronic renal failure C reactive protein Caesarean section Cerebrospinal fluid Catheter specimen of urine Computed tomography (scan) Cardio tocograph Carpal tunnel release Carpal tunnel syndrome Cerebrovascular accident Central venous catheter Central venous line Central venous pressure Cardiovascular system Colour, warmth, movement, sensation Cervix Chest x-ray Dilatation and curettage Dilatation and evacuation Diarrhoea and vomiting Discharge Discussed with Deep breathing exercises Differential diagnosis Disseminated intravascular coagulopathy Diabetes mellitus Did not attend Did not wait Dead on arrival Date of birth Domiciliary midwifery service Drops per minute Doctor Diagnostic related groups Drain Tube 33 DTA DTs DU DUB DVT Dx E E.coli E/O EAR EBM ECG ECHO ECT ECTR ECV EDC EDD Eg. EMD ENT ERCP ESR ESRF ETOH ETT EUA Exac F F/S F/U FB FBC FBE FC FDIU Fe FFP FG FGM FH FHH FHR FHx FI Fib FMF FOOSH FSE Deep transverse arrest Delirium tremens Duodenal ulcer Dysfunctional uterine bleeding Deep vein thrombosis Diagnosis Escherichia coli Excision of Expired air resuscitation Expressed breast milk Electrocardiograph Echocardiogram Electro convulsive therapy Excision carpal tunnel release External cephalic version Estimated date of confinement Estimated due date Example Electromechanical dissociation Ear, nose and throat Endoscopic retrograde cannulation of pancreatic duct Endoscopic retrograde cholangiopancreatography Erythrocyte sedimentation rate End stage renal failure Alcohol (ethanol) Endotracheal tube Examination under anaesthetic exacerbation Frozen section Follow up Foreign body Fluid balance chart Full blood examination Filschie clips Fetal death in utero Iron Fresh frozen plasma French gauge Female genital mutilation Fetal heart Fetal heart heard Fetal heart rate Family history For investigation Fibula Fetal movements felt Fall on outstretched hand Fetal scalp electrode 34 FSH FTA FTSG FWB FWT Fx G G GA GAMP GBS GCS GCT GDM GIT GNC GOR(D) GP GTT GU Gutt Gynae H H&M H/O H/T Hb HCG HDU HELLP Hep A,B,C,D HITH HIV HIE HMD HNPF HNPU HOPC HOT HOV HPF HPV HR Hrly HSG Ht HVS Hx Hypo Follicle stimulating hormone Failed to attend Full thickness skin graft Full weight bearing Full ward test Fornix Gravid General anaesthetic General anaesthetic, manipulation and plaster Group B streptococcus Glasgow coma score Glucose challenge test Gestational Diabetes Mellitus Gastro intestinal tract General nursing care Gastro-oesophageal reflux (disease) General Practitioner Glucose tolerance test Gastric ulcer Eye drop Gynaecology Hematemesis and malaena History of Hypertensive Hypertension Haemoglobin Human chorionic gonadotrophin High dependency unit Haemolysis elevated liver enzymes low platelets Hepatitis A,B,C,D Hospital in the home Human immuno deficiency virus Hypoxic ischaemic encephalopathy Hyaline membrane disease Has not passed flatus Has not passed urine History of presenting condition Hands off Technique - Breast Feeding Education programme Head on view Has passed flatus Human papilloma virus Heart rate hourly Hysterosalpingogram height High vaginal swab History hypoglycaemia 35 I I/O I/P ICC ICH ICP ICS ICU IDC IDDM IF IHD II IM IMB IMI Imp Ing. INR IOL IOP IPPV IT ITP IU IUD IUGR IV IVB IVF IVH IVP IVT Ix J J JVP K K+ KCl KUB L L L/Min LA Lac LAD Insertion of Inpatient Intercostal catheter Intracranial haemorrhage Intercranial pressure Intercostal space Intensive care unit Indwelling catheter Insulin Dependent Diabetes Mellitus Iliac fossa Ischaemic heart disease Image intensifier Intramuscular Intermenstrual bleeding Intramuscular injection Impression Inguinal International normalised ratio Induction of labour Intraocular pressure Intermittent positive pressure Intrathecal Idiopathic thrombocytopaenia purpura International unit Intrauterine device Intrauterine growth restriction Intravenous Intravenous bung In vitro fertilisation Intraventricular haemorrhage Intravenous pyelogram Intravenous therapy Investigation joules Jugular venous pressure Potassium Potassium chloride Kidneys, ureter, bladder Left Litres per minute Local anaesthetic Left arm Left atrium Laceration Left anterior descending (coronary artery) 36 LAMP Local anaesthetic, manipulation and plaster Lap Lat LAVH LBBB LBO LBW LC LCM LEEP LFC LFT's LH LHF LIF LLETZ LLL LLQ LML LMO LMP LNMP laparoscopy lateral Laparoscopically assisted vaginal hysterectomy Left bundle branch block Large bowel obstruction Low birth weight Lactation consultant Left costal margin Loop electro surgical excision procedure Laparoscopic filschie clips Liver function tests Luteinising hormone Left heart failure Left iliac fossa Large loop excision transformation zone Left lower lobe Left lower quadrant Left middle lobe Local medical officer Last menstrual period Last normal menstrual period Left occipito anterior (? Midwifery term – is it used?) Loss of appetite Loss of consciousness Left occipito posterior (? Midwifery term) Left occipito transverse (? Midwifery term) Loss of weight Lumbar puncture Left salping-ooppherectomy Left upper lobe Left upper quadrant Lower uterine segment caesarean section Left ventricle Left ventricular failure Leave without Pay LOA LOC LOP LOT LOW LP LSO LUL LUQ LUSCS LV LVF LWOP M MA M, C & S M/W Mane MAP MBA MCA mcg MCHN M-C-P joint mg Mg Metered aerosol Micro, culture and sensitivity Midwife morning Mean arterial pressure Motorbike accident Motor car accident microgram Maternal & Child Health Nurse Metacarpophalangeal joint Milligram Magnesium 37 MG MI MICA MITH ml mm mmHg mmol MO MOW MR MRI MROP MRSA MS MSU MUA Multi MV MVA MVR MV regurg Mx N N/A N/CT N/O N/S N2O Na NaCl NAD NASS NBM NST NCP Neb NEC Neg, -ve NESB Neuro NFO NG NGT NICU NIDDM NIPPV NKDA NMRI Multigravida Myocardial infarction Mobile intensive care ambulance Midwifery in the Home millilitres Millimetres Millimetres of mercury Millimols Medical officer Meals on wheels Membranes ruptured Magnetic resonance imaging Manual removal of placenta Multiple resistant staphylococcus aureus Multiple sclerosis Mid stream specimen of urine Manipulation under anaesthetic Multiparous Mitral valve Motor vehicle accident Mitral valve replacement Mitral valve regurgitation Management Not applicable Nasal cautery Nil orally Nipple shield Nitrous oxide Sodium Sodium chloride Nil abnormalities detected Neonatal abstinence scoring system Nil by mouth Newborn screening test Nursing care plan Nebuliser Necrotising enterocolitis Negative Non english speaking background Neurological No further orders Nasogastric Nasogastric tube Neonatal intensive care unit Non Insulin Dependent Diabetes Mellitus Nasal intermittent positive pressure Non-invasive positive pressure ventilation No known drug allergies Nuclear magnetic resonance imaging 38 NND No. Nocte NOF NOK NP NPA NPO NSAID NST NVD NVB NVF O O O&G O/A O/E O/N O/T O2 O2 Sat OA Obs Occ OCP OD OHS OP Op OR ORIF OT Oz P P p.c. P/C P/T PA PAC PACFU Paed Palp PANDA PAP Pb PC Neonatal death Number Night Neck of femur Next of kin Nasal prong Naso-pharyngeal aspirate Nil per os (nil orally) Non-steroidal anti-inflammatory drug Non stress test Normal vaginal delivery Normal Vaginal Birth Normal vaginal flora Orally Obstetrics and Gynaecology On admission On arrival On examination Overnight Operating theatre Oxygen Oxygen saturation Osteoarthritis Observations Eye ointment Oral contraceptive pill Overdose Occupational health and safety Occipito-posterior Out patient Operation Operating room Open reduction, internal fixation Occupational therapist Ounce Parity Post cibum – after meals Presenting complaint Phototherapy Postero - anterior Pressure area care Premature atrial contraction Post acute care funding unit Paediatrics Palpation Post and Antenatal Depression Association Pulmonary artery pressure Lead Packed cells 39 PCA PCEA PCOS PD PDA PDS PDPH PE PE(T) PEA PEEP PEFR PFO PG Primip PHx PID PIH PKU PM PMB PMS PND PNx PO POC POD POP POP Pos, +ve Post PPH PPHN PR PRBC Preg Pre-med Pre-op PRN PROM Prox PT Pt PTTK PTL PTSD Patient controlled analgesia Patient controlled epidural analgesia Polycystic ovarian syndrome Peritoneal dialysis Patent ductus arteriosis Pregnancy Day Service Post dural puncture headache Pre-eclampsia Pulmonary embolus Pre-eclamptic toxaemia Pulseless electrical activity Positive end expiratory pressure Peak expiratory flow rate Patent foramen ovale Primigravida Past history Pelvic inflammatory disease Pregnancy induced hypertension Phenylketonuria Post mortem Post meridien Post menopausal bleeding Premenstrual syndrome Postnatal depression Pneumothorax Per orally Products of conception Pouch of douglas Plaster of Paris Persistent occipito posterior Positive Posterior Post partum haemorrhage Primary Pulmonary Hypertension Persistent pulmonary hypertension of the newborn Per rectum Packed red blood cells Pregnancy Pre medication Pre operatively As required Premature rupture of membranes Proximal Prothrombin time Patient Partial thromboplastin time with kaolin Pre-term labour Post traumatic stress disorder 40 PU PUIT/ PUIB PUO PV PVC PVD Q QA QID / qid Quad R R R/O R/V R/V RA RAF RBBB RBC RBG RCM RDNS RDS Reg Rehab RFT Rh RIB RIF RLL RLQ RM RML RMO RN ROA ROM ROP ROP ROS RPAO RPOC Rpt RR Passed urine Per urethra Passed urine in toilet Passed urine in Bed Pyrexia of unknown origin Per vaginum Premature ventricular contraction Peripheral vascular disease Quality assurance Four times daily / 6 hourly Quadriplegia Right Removal of Review Review Rheumatoid arthritis Right atrium Right arm Rapid atrial fibrillation Right bundle branch block Red blood cells Random blood glucose Right costal margin Royal District Nursing Service Respiratory distress syndrome Registrar Rehabilitation Renal function test Rhesus Rest in bed Right iliac fossa Right lower lobe Right lower quadrant Registered Midwife Right middle lobe Resident Medical Officer Registered Nurse Right occipito anterior Rupture of membranes Range of movement Right occipito posterior Retinopathy of prematurity Right occipito posterior Removal of sutures/staples Routine post anaesthetic observation Retained products of conception Repeat Respiratory rate 41 RSO RSV Rt RTW RUL RUQ RV RVF RVH Rx S S&S S/B S/I S/L SA node SAH SANDS SaO2 Right salpingo - oophorectomy Respiratory syncytial virus Right Return to ward Right upper lobe Right upper quadrant Right ventricle Right ventricular failure Right ventricular hypertrophy Treatment SBE Sub-acute bacterial endocarditis SBO SBR SC SubCut SCC SCN SD SDH Se SFD SG SGA Sib SIDS SIMV Sl SLE SO SOB SOBOE SOF SOH SOL SOOB SPC SPPS SR SROM SSD cream Small bowel obstruction Serum bilirubin Signs and symptoms Seen by Sexual intercourse Sublingual Sinoatrial node Subarachnoid haemorrhage Stillborn and neonatal death society Saturation of oxygen Subcutaneous Squamous cell carcinoma Special care nursery Syringe driver Sub dural haemorrhage Serum Small for dates Specific gravity Small for gestational age Sibling Sudden infant death syndrome Synchronised intermittent mandatory ventilation Slight Systemic lupus erythematosis Salphingo-oopherectomy Short of breath Short of breath on exertion Shaft of femur Shaft of humrus Space occupying lesion Sat out of bed Suprapubic catheter Stable protein plasma solution Sinus rhythm Spontaneous rupture of membranes Silver sulphadiazine cream 42 SSF SSG ST Stat STD STI STOP Supp SVC SVD SVB SVT T T T/L T’s & A’s T1DM T2DM Tab TAC TAH TB TBG TDS Tet Tox TFI TFT THR TIA Tib TKJR TKR TKVO TLC TMJ TML To TOF TOL TOP Top. TOS TOV TPN TPR TTN TURBT TURP TVT Sacrospinous fixation Split skin graft Sinus tachycardia Immediately Sexually transmitted disease Sexually transmitted infection Suction termination of pregnancy Suppository Superior vena cava Spontaneous vaginal delivery Spontaneous Vaginal Birth Supraventricular tachycardia Term Tubal ligation Tonsils ad adenoids Type 1 diabetes mellitus Type 2 diabetes mellitus Tablet Transport accident commission Total abdominal hysterectomy Tuberculosis Total blood glucose Three times daily Tetanus toxoid Total fluid intake Thyroid function test Total hip replacement Transient ischaemic attack Tibia Total knee joint replacement Total knee reconstruction To keep vein open Tender loving care Temporomandibular joint Trachea midline Temperature Trial of forceps Tetrology of fallot Trial of labour Termination of pregnancy Topical Trial of scar Trial of void Total parenteral nutrition Temperature, pulse, respiration Transient tachypnoea of newborn Transurethral resection of bladder tumour Trans urethral resection of prostate Transvaginal tape 43 Therapy Treatment Tx U U&E U/A U/S UAC UGIT UHCG UO UR URTI Ut UTI UTV UVC V Vag VBAC VCS VE VF VT VV W WB WBC WCC WNL WPW WRIGTN Wt X x-match XR Y Yr Urea & electrolytes Urinalysis Ultrasound Umbilical artery catheter Upper gastrointestinal tract Urine human chorionic gonadotrophins Urine output Unit record Upper respiratory tract infection Uterus Urinary tract infection Unable to void Umbilical vein catheter Vaginal Vaginal birth after caesarean Victorian Cytology Service Vaginal examination Ventricular fibrillation Ventricular tachycardia Varicose veins Weight bearing White blood cells White cell count Within normal limits Wolfe-Parkinson White Wedge resection ingrown toenail Weight Cross match x-ray year Symbols < 1/24 1/52 # Less than 1 hour 1 week Fracture > 1/7 1/12 ↑ Greater than 1 day 1 Month Increased ↓ Ψ Decreased Psychiatric History / Illness Δ Change 44 Medical Emergency Team – MET Aim - To provide an early and rapid response to seriously ill patients with life threatening conditions. To offer support to nursing and medical staff in the management of critically ill patients. Process 1. Nursing and Medical staff can call a MET if the patient meets one or more of the criteria below: Airway Difficulty Speaking Threatened Airway Breathing Circulation BP < 90mmHg Systolic RR > 30/min RR < 6/min SaO2 < 90% on O2 despite treatment PR > 130 PR < 45 Neurology Altered Conscious State Fitting Respiratory Distress Other Concerned 2. Call the Emergency Department on Ext. 8651 and liaise with the Senior Medical Officer, clearly stating that it is a MET call. 3. You will be required to outline the reasons for the MET call, relevant events prior to the MET call, vital signs and any care initiated. 4. The Bed Co-ordinator or After Hours Co-ordinator (AHC) should be notified on Ext. 8529 that a MET call has been made. 5. Vital signs should be monitored and documented. The Emergency Trolley and patient notes should be readily available. A nurse must remain with the patient. 6. After a MET call has been made to the Emergency Department, a telephone or ward assessment shall be made by the Senior Medical Officer. A decision will be made to either manage the patient on the ward or to transfer the patient to the ED for stabilisation. 7. The Consultant of the patient and/or other relevant medical staff eg Anaesthetist should be notified of the situation in an appropriate time frame. 45 EVALUATION The following evaluation is designed to elicit feedback concerning your clinical placement. Your response will be useful in assisting in the future development of the undergraduate program. Please circle the response that best describes your feelings concerning the following statements and provide comments where applicable. Strongly Disagree 1 Disagree Unsure Agree 4 Strongly Agree 5 2 3 1 2 3 4 5 Hospital orientation was informative and appropriate to your learning needs. If not, please comment: How would you describe your clinical teacher? A. Professional 1 2 3 4 5 B. Approachable and conducive to professional development 1 2 3 4 5 C. Supportive 1 2 3 4 5 D. Helped me to meet my learning objectives. 1 2 3 4 5 Please comment if you disagree with the above: The clinical teacher gave regular feedback concerning my progress. 1 2 3 4 5 The debriefing sessions were appropriate to my needs. 1 2 3 4 5 If not, please comment: What aspects of this clinical placement did you like the most? What aspects of this clinical placement did you like the least? Was your preceptor / buddy nurse supportive, informative and encouraging with clinical interventions / nursing? During your clinical placement was there a preceptor / buddy nurse who has had a positive impact on your learning? YES NO If yes, please name: Additional comments: Thank you for your participation and we hope your clinical placement has been a positive and rewarding experience.