Partnerships_Organ Systems
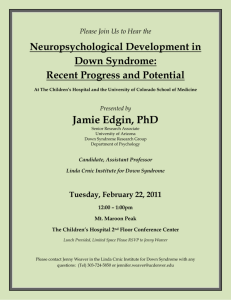
advertisement

Partnerships Lecture Partnerships: Pain for 2 hoursacute Pain for 3 monthschronic Neutrophils and yellowish sputumacute Mononuclear cells (lymphocytes, macrophages)chronic Rolling: E-selectin in context of adhesionSialyl Lewis x molecules on WBC Pavementing: LFA-1 (Leukocyte function associated antigen on WBCs) w/ ICAM-1 & VCAM (on endothelial cells) Transmigration: CD31 or PECAM Delayed separation of umbilical cordfucosyl transferase deficiency (selectin)? check CGDNBT test for this condition Partnerships reviewed by Gohara: Defective organelles trafficking Chediak Higashi (albinism, fair eyelashes & eyebrows, giant granules in neutrophils) Defective NADPH Oxidase CGD (X-linked= gp91PHOX; autosomal recessive= P47PHOX & P67PHOX) C5achemotaxis C3bopsonins Immunoglobulinsopsonins Prostaglandinscyclooxygenase pathway Prostaglandinsvasodilation NOvasodilation PECAMtransmigration Selectinrolling ECAMPavementing Mast cells histamine Plateletsserotonin MyeloperoxidaseHOCl Arachidonic acid metabolitescyclooxygenase and lipoxygenase Vasoactive aminesserotonin and histamine Leukocytes stickingintegrin Delayed separation of umbilical cordselectin deficiency/defects Kininogen + Kallikreins kinins Activated factor XII converts prekallikreins to kallikreins—cleaveHMW Kininogin to Bradykinin *Kinins are inactivated in the lung by ACE Kallikreins & PAF cleave plasminogen to plasmin cleaves C3 and activates factor XII (Cycle) Erythema nodosumsarcoidosis, Type IV hypersensitivity, unknown etiology Morphologic pattern of acute inflammation: Serous (effusion and blisters)viral infections and burns Fibrinous (proteinaceous material accumulating as a result of inflammation)Uremic pericarditis or pleura Diseases of Blood Vessels: Which of the following cells is responsible for initial lesion of atherosclerosis= endothelial cells Atherosclerosis= disease of intima (single layer of endothelial cells and minimal CT) Disease of media= Monckeberg’s sclerosis Progression of atherosclerosis= smooth muscle cells Hyalinization= (see a story about someone with high BP for long time and controlled with medications); appearance of blood vessels with benign hypertension Onion skinning (causes major medical emergencies)= malignant hypertension (hyperplastic arteriolosclerosis) Pts with diabetes= more prone to developing atherosclerosis bc always have high cholesterol and high triglycerides *very important* high sensitivity to C reactive protein= risk assessment test; if pt has high sensitivity elevated C reactive protein, at higher risk for developing MIs and strokes Hyalinization of blood vessels occur in benign hypertension and diabetes Review of Diseases of Blood Vessels: Mutation of LDL receptor= Hyperlipidemia Type IIa (Familial Hypercholesterolemia) High sensitivity C reactive protein= risk factor for ischemic heart disease and stroke Lipoprotein-a (an altered LDL) when in large quantities= risk factor for atherosclerosis Familial Homocysteinemia= premature ischemic heart disease Calification in the media= Monckeberg’s Atherosclerosis What type of patient, what type of presentation, what type of complications? What does it mean to you when you see Hyperplastic Arteriosclerosis? = malignant hypertension= onion skinning Vignette: a person with this lesion (malignant hypertension) How are they going to present? Onion skinning in arterioles, could be in microangiopathic hemolytic anemia; schistocytes on peripheral blood smear, diastolic P >120 mmHg (maybe 200/130) What complication? An older lady dies at home. Long history of hypertension and diabetes well-controlled by medication. Do an autopsy. What do you expect to see at autopsy in arterioles? Will see HYALINIZATION bc this woman most likely had benign hypertension. Both benign hypertension and diabetes cause hyalinization of the arterioles. **Smooth muscles prolif, occlude, and form fibrous cap.= point of no return once get this cap Thickened intima (genetic)= response to vascular injury We are going to choose which scenario it will be associated with: Scenario 1: a 32 year old man and he comes in to the derm clinic bc he has a lesion on his penis, it’s kind of ulcerated but not painful. He doesn’t use protection, and this lesion has been there for about 5 days. Scenario 2: the same man, but now about 2 months later, and he doesn’t have that ulcerated lesion anymore but some rash on his palms, and he just doesn’t feel right. Scenario 3: that man about 10-15 years later, comes in with dyspnea, dysphagia, and heart failure, and some neurologic manifestations (sensory loss) this one associated with thoracic aneurysms Loss of elasticity in media due to ischemia caused by inflamm of vasovasorum causes intima to wrinkle/fold. Treebark appearance of blood vessel intimal surface=Syphilis Ascending aorta aneurysm= Syphilis Medial necrosis & dissection= Marfan’s Syndrome Ripping chest pain/tearing chest pain radiating to the back and hypertension= Aortic Dissection Anything in which pain radiating to the backthink of something that perforated e.g. abdominal pain, started suddenly, 75 yo male with hypertension and atherosclerosisruptured aortic aneurysm ruptured bowel or vesselpain radiates to the back acute pancreatitis also radiates pain to the back Inflammatory Diseases of Blood Vessels: pANCAAntimyeloperoxidase (myeloperoxidase is in granules that generate free radicals) Churg Strauss, Microscopic polyangitis, Polyarteritis Nodosa (very small # of pts) cANCAAnti Proteinase 3 (proteinase 3 present in azurophilic granules)Wegener granulomatosis stiffness and pain in shoulderstemporal arteritis (inflammation of small and medium sized arteries, esp temporal arteries) Polymyalgia rheumatica treebarksyphilis medial necrosis Marfan’s cANCA- Wegener pANCA- Churg Strauss, Microscopic Polyangitis, and small % PAN polymyalgia rheumaticatemporal arteritis beefy tongue Kawasaki cold arm Takayasu smokingBuerger’s (or Thromboangiitis Obliterans) renal involvement Wegener, Microscopic Polyangitis, and PAN Partnerships reviewed: Tree barksyphilis Eosinophilia Churg-Strauss (is the main partner), the behind the scene partner is PAN Asthma Churg-Strauss cANCA (antigen= proteinase 3)Wegener Polymyalgia rheumatica temporal arteritis Branches of aortic archTakayasu (young females get) Severe leg pain and smokingBuerger’s Non-responsive high fever 5 days in a childKawasaki pANCAChurch Strauss and small percentage of PAN Hep BPAN SinusitisWegener (sinusitis, glomerulitis, pneumonitis) Ripping chest pain radiating to the backdissecting aneurysm of the aorta 2 possible causes: Marfan Severe hypertension If Marfan medial necrosis (cherish and frame it) What else could he have? Mitral valve prolapse 45 yr old pat with severe epigastric pain and hematuria and CBC eosinophiliaPAN (does not affect the lungs), affects GI, skin, and kidneys 70 year old man presents with large thoracic aortic aneurysm. What should we ask him? Syphilis! (always always always ask) Diseases of Endocardium: Clinical vignette: 8 yo boy brought in by his mother because of a swollen, red, tender left knee and right wrists. He also had a reddish rash on his chest (erythema marginatum). He has not been feeling well since he had a sore throat a couple weeks ago. PE: temp 101 degrees F, pulse 100/minute, friction rub heard on chest auscultation Dx: Rheumatic Fever Jones Criteria: Major: carditis, polyarthritis (migratory), sydenham’s chorea, E. marginatum, subcutaneous nodules Minor: fever, arthralgia, increased ESR, increased PR interval on EKG need 2 major or 1 major + 2 minor Erythema marginatumpink rash, clear center with red serpingenous margins on trunk (never on face), transient and migratory nonpruritic, nonindurated, blanches on pressure Aschoff bodies (nodules), anitschow cells (caterpillar nucleus cell, macrophage according to Robbins), aschoff cells (giant cells with owl-eye nucleus)Rheumatic Fever “bread and butter appearance” pericarditisFibrinous pericarditispost MI, Dressler Syndrome, Rheumatic Fever/Pericarditis Aschoff bodiesmyocarditis Verrucous endocarditis at line of closure of valves on side of blood flowRheumatic Fever 10 yo boy who arrived from Cambodia two months ago, presents to ER w/ fever 103F, chills, petichiaie under his nails PE tender nodules in elbows, hemorrhagic spot on retina Dx: subacute endocarditis, probably had RF in the past Subacute endocarditisoccurs on abnormal valves, less virulent microorganisms such as streptococcus viridans, indolent course (wks to mos), full recovery in most cases with tx Acute endocarditisoccurs on normal valves, highly virulent microorgs such as staph aureus, destructive and rapidly progressive, death within days to weeks, IV drug users Petechiae, splinter hemorrhages (nails), Janeway lesions (palms and soles: painless hemorrhagic lesions), Subcutaneous (Osler nodes: hemorrhagic painful), Roth spots (hemorrhage on retina) Septic infarcts and abscesses, glomerulonephritis (immune complex deposition)complications of endocarditis Marantic Endocarditissterile endocarditis associated with malignancies, Troussea sign (mucinous adenocarcinoma of the pancreas) SLE endocarditis, small vegetations on both sides of valves, hematoxylin bodies (look like naked nuclei)Libman-Sacks Disease Thick plaques in right side of heart on tricuspid valve, acid mucopolysaccharides with matrix, increased serum levels of serotoninCarcinoid Heart Disease Mid-systolic clickmitral valve prolapse, sometimes associated with Marfan’s Syndrome Elderly person with angina, CHF, and syncopecalcific aortic stenosis (commonly bicuspid valves, especially if younger person such as in 50s) pulsus paradoxicus, muffled heart soundsConstrictive pericarditis painful, modified smooth muscle cell tumors, distal digits under nails, arise from glomus body (A-V shunt in dermis)glomus tumors polyvinyl chloridehemangiosarcoma of liver cardiac myxomas (CT tumor with mucus), skin myxomas, hyperpigmentation, endocrinopathies, autosomal dominant syndromeCarney Syndrome rhabdomyoma (skeletal muscle tumor of myocardium)tuberous sclerosis adriomycindilated cardiomyopathy radiation therapyscarring, fibrosisadhesive pericarditis 18 yo man to ER with fever 104F, tachycardia 5 days after tooth extraction PE: new systolic murmur, hemorrhagic spot on retina IE: Infectious endocarditis Do Blood cultures Congestive Heart Failure: OrthopneaLeft-sided heart failure Congestion, pulmonary edemamacrophages come in to clean up hemorrhaging “heart failure cells” (have hemosiderin in them, Fe from broken down blood cells) Right heart failureliver congestionnecrosis of liver cells around central veinincreased LDH5 B-type Natriuretic Peptide (BNP)regulates BP and from the heartelevated in CHF Alcohol, peripartum, genetic, myocarditisdilated cardiomyopathy (heavy flabby heart, thin walls) Alcohol dilated cardiomyopathydirect toxicity or thiamine deficiency Increased levels of an antiangiogenic cleavage product of prolactinperipartum dilated cardiomyopathy Mutation of a dystrophin gene (main one) or alpha cardiac actin in terms of heartgenetic dilated cardiomyopathy (“put on night stands”) Adriomycin toxicity (Boo! I had this!)myocarditis Mutations in myosin binding protein, beta myosin heavy chain, troponin THypertrophic cardiomyopathyhypertrophy in septum obstructing outflow through aortic valveoften young athletes who collapse and die Hypertrophy of heart and on microscopy, sarcomeres not arranged in normal layers (disorganized appearance)Hypertrophic cardiomyopathy Cor pulmonale (long-standing lung disease)isolated right ventricle hypertrophy Glomerular Diseases: Fixed Tissue AntigensGood Pasture Syndrome anti GBM (Glomerular Basement Membrane) Nephritis Immune Complex Nephritis (immune complex circulating and depositing in basement membrane, activating complement, PMNs, lysosomal enzymes cause tissue damage) post-streptococcal glomerulonephritis + low serum complement Low serum C3 (alternative pathway-mediated) membranoproliferative glomerulonephritis Nephrotic Syndrome thickening of basement membrane capillaries*, proteinuria, hypoproteinemia, edema of legs, hyperlipidemia, lipiduria Nephritic Syndrome *hematuria, *RBC casts (RBCs that have taken the shape of renal tubules from sitting there for awhile), *azotemia (increase in nitrogenous waste products in the serum) proliferation of mesangial cells* and necrosis, mild proteinuria, hypertension, oliguria Hematuria Syndromevariable changes in the glomeruli Chronic Renal FailureHyalinization or sclerosis (scars) of glomeruli Collagen Type IV of basement membrane completely impermeable to albumin Nephrintransmembrane glycoprotein in the slit diaphragm that forms disulfide bridges between adjacent podocytes Nephrin and podocincrucial role in maintaining selective permeability of glomerular filtration barrier Mutations of nephrin or podocinabnormal leakage of plasma proteinsFamilial nephrotic syndrome Resident glomerular mesangial cells can initiate an inflammatory response in the glomerulus 5 year old was brought to the emergency room because the mother had noted dark urine (looks like Coca Cola or Tea). The child had a sore throat 10 days earlier. Physical Exam BP:120/80 (high for age) Urinalysis: RBCs, RBC casts, 1+ protein (not significant), CBC nl, ESR elevated, BUN elevated, Creatinine elevated (these last two are collectively referred to as azotemia) Dx: Post-Streptococcal glomerulonephritis (Immune Glomerulonephritisimmune complexes in membrane) Clinical picture: hematuria, hypertension, azotemia Lab Findings: ASO titer increased, complement (CH50, C3 & C4) low bc of classical pathway activation by immune complexes, RBCs + RBC casts in urine, elevated BUN, elevated Creatinine Morphology: Mesangial Cell Proliferation (*characteristic of nephritic syndrome) IF: Lumpy Bumpy (Coarse Granular) peripheral deposits of IgG and C3 on BM EM: Subepithelial electron dense humps Post strep glomerulonephritislow complement, increased ASO, Humps on EM (subepithelial), mesangial proliferation A 5yo boy comes to the clinic with a hx of tea color urine for 3d and a past hx of a severe skin rash with pustules 3 wks ago Infection: impetigo (caused by strep) What would you expect to see in his urine? RBCs and RBC casts What would you see on a renal biopsy? LM: mesangial cell proliferation IF: lumpy bumpy IgG and C3 EM: subepithelial humps A 35 yo male went to his physician for an annual physical. He was found to have microscopic hematuria. CBC nl and CHEM20 nl DD: Hematuria Syndrome as a result of IgA nephropathy (also known as Berger’s Disease) LM: variable IF: diffuse mesangial IgA Tx: steroids Prognosis: benign in children; can progress to renal failure or hypertension in adults; recurrence in allografts IgA Nephropathydiffuse mesangial IgA and recurrence in renal allografts (suggests a problem in immune system rather than the kidney~Wikipedia) A 12 year old girl presents with a palpable red rash on her buttocks, arthralgia, abdominal pain, and hematuria. UA: RBCs and RBC casts; BUN, creatinine, and serum IgA increased (nephritic syndrome)proliferation of mesangial cells Dx: Henoch-Schonlein purpura*GI, skin, & kidney involvement; *IgA deposits in skin and kidney; *nl bleeding time; preceding illness usually an upper respiratory tract infection A 25 yo male presents with profuse hemoptysis following a flu-like illness a week prior Physical examination: pale, tired young man Urinalysis: many RBCs, many RBC casts CBC: Hemoglobin 11 DDx: Good Pasture’s, Wegener’s hemoptysis and hematuriaGood Pasture’s and Wegener’s Good Pasture’s Syndrome*hematuria, *hemoptysis, *anti-GM (glomerular basement membrane) antibodies against *alpha 3 chain of Collagen Type IV, URI preceding symptoms LM: necrosis, crescents IF: linear peripheral Ig deposits** along glomerular BM and alveolar septa Crescentic glomerulonephritisleakage of fibrin in Bowman’s space, proliferation of parietal cells (lining Bowman’s capsule)crescent= fibrin and parietal cells lining bowman’s capsule rapidly progressing glomerulonephritis (according to website with pic below, occurs in post-strep, lupus, Good Pasture, vasculitis, and idiopathic) (Crescents are defined as the presence of 2 or more layers of cells in the Bowman space. The presence of crescents in glomeruli is a marker of severe injury. Cells and mediators from the interstitium enter the Bowman space with disruption of the Bowman capsule, which leads to development of crescents. The major participants in crescent formation are coagulation proteins, macrophages, T cells, fibroblasts, and parietal epithelial cells. Activated macrophages contribute to the crescents by proliferating and releasing procoagulant tissue factor, interleukin-1 (IL-1) and tumor necrosis factor (TNF). T cells are not prominent components, but they play an important role in glomerular injury by antigen recognition and macrophage recruitment. http://emedicine.medscape.com/article/239504-overview) http://www.pathologyatlas.ro/rapidly-progressive-crescentic-glomerulonephritis.php A 45 yo F with a three month history of epistaxis presents with cough and hematuria. Wegener GranulomatosiscANCA positive, clinical triad: sinusitis, pneumonitis (cough, hemoptysis can be present), glomerulonephritis (hematuria), see crescents under light microscoperapidly progressive glomerulonephritis (progresses to renal failure within weeks or months) A 50 yo Executive presents with recurrent abdominal pain and a skin rash. He has had a low grade fever for three months. BP 140/90, Temp 100 F (oral), UA RBCs, RBC casts, 1+ protein, CHEM 20: BUN50, Creatinine 3azotemia, CBC Eosinophilia, other tests: Hep B positive in 30% of cases, pANCA positive in small % of cases Dx is Polyarteritis Nodosa (PAN); Polyarteritis= multiple arteries inflamed, Nodosa= aneurismal dilatation in segmental fashion Polyarteritis Nodosa (PAN)*Hepatitis B (30%), *segmental arteritis, *NO lung involvement, *GI, *skin, *kidney, musculoskeletal, CNS, small % have pANCA Other info: Male:Female= 15:1, mostly occurs in 5th and 6th decades; pathogenesis is chronic immune complex with hypersensitivity (no one preceding illness to trigger) An IV drug user presents with a skin rash & hematuria DD? Hep BPAN CBCeosinophilia UAnephriticRBCs and RBC casts Hemolytic Uremic Syndrome (HUS) Vignette A 3 yo boy presents to the ER with hematuria and bloody diarrhea for 2 days following a birthday party where he ate a grilled hamburger. CBC: Hb7, BUN and creatinine high (azotemia), low platelets, schistocytes on peripheral blood smear (microangiopathic anemia) Pathogenesis: intravascular coagulationdecreased plts, increased fibrin split products CP: oliguria, renal failure, hemolytic anemia, E. Coli 0157:H7 toxins in stool HUS identical to TTP except no neurological manifestations HUSundercooked hamburger, E.coli 0157:H7, hematuria, renal failure, microangiopathic hemolytic anemia Microangiopathic hemolytic anemias (Schistocytes)HUS, Scleroderma, TTP, Vasculitis, DIC, Malignancies; low platelets; normal platelets Systemic Lupus Erythromatosis affects skin, heart, joints, kidney (ultimately kills them), lab findings: ANA increased (anti-smith antibody: the smith antigen is a complex of RNA and proteins that form small ribonucleic proteins which ultimately come together with others to form spliceosomes, which cuts out introns of pre-mRNA to mRNA), anti DNA increased, complement decreased all of them bc classical pathway (CH50 low, C3 and C4 low), hematuria, proteinuria, casts, nephrotic syndrome (First Aid says nephritic or nephrotic) IF: IgG + C’ in mesangium and tubules “full house fluorescence”* EM: subendothelial deposits* Vignette: Scleroderma AKA Progressive Systemic Sclerosis 45 yo F with hypertension* and pulmonary fibrosis* and Raynaud’s phenomenon* for 5 years presents with renal failure*. ANA 1:20,000 speckled anti SCL70 positive* Most also have dysphagia* She has thin leathery skin on her hands and face due to scars 21 yo man with gross hematuria, BUN nl, creatinine nl, BP nl, What will you see on a renal biopsy? Diffuse mesangial IgA Dx: pure hematuria Hematuria Syndrome (IgA nephropathy) (listed under Nephritic Syndrome in First Aid, but not in Dr. Gohara’s notes) 10 yo boy with a rash on face, arthralgia, and renal failure UA: RBCs and casts BUN is elevated Creatinine is elevated What would you like to ask? Infections? NO, rash palpable? NO, abdominal pain? NO What tests? ANA 1:2000 speckled, anti dsDNA++, anti Smith +++ Dx: Lupus What are you going to see in a renal biopsy? Subendothelial deposits 31 yo man IV drug user presents with severe epigastric pain and a rash on his chest. Also has hematuria. Questions to ask: Hep B? YES Dx: PAN CBC: eosinophilia Nephrotic Syndromes: Primary- Lipoid Nephrosis (Minimal Change Disease), Focal Glomerulosclerosis, Membranous Glomerulonephritis, Membranoproliferative Glomerulonephritis Secondary- Diabetes, Amyloidosis *Clinical: edema (especially in ankles due to decreased oncotic pressure), 4+ proteinuria (>3 gm ptn lost in 24 hours), hypoproteinemia due to loss of proteins in the urine, hyperlipidemia *Proteinuria due to leaky capillary basement membrane leading to frothy urine *Hyperlipidemia (unknown cause) leads to increased risk of atherosclerosis and *oval fat bodies* in the urine (tubular cells filled up with lipid) --USMLE World Qbank also said that Nephrotic Syndrome presents with thrombi/increased risk of clotting due to loss of antithrombin in the urine. 2 vignettes for Lipoid Nephrosis (AKA Minimal Change Disease): 1) a 2 yo boy with recurrent nephrotic syndrome is found to have selective proteinuria* (mostly albumin in urine)—80% of primary nephrotic syndrome in children is this. 2) a 40 yo lady with a hx of left-sided neck pain for 3 months with accompanying lymphadenopathy*, and the pain gets worse when she drinks her glass of wine* with her dinner. 10 days ago she noted swelling of her feet* and frothy urine*. *Hodgkin’s Lymphoma *Nephrotic Syndrome—30% of primary nephrotic syndrome in adults is this Pathogenesis: T cell factors damage podocytes, proteins leak out of foot processes and they then become sticky and fuse together “podocyte foot processes effacement”* Nothing on LM, EF. Just EM: fusion of foot processes* Usually no preceding illness Good response to steroids* Focal Segmental Glomerulosclerosis (FSGS) hematuria and NONselective proteinuria*, NO response to steroids*, 60% nephrotic syndrome, 30% azotemia (*mixed nephrotic and nephritic syndromes*), 25% hypertension, recurrence in renal allograft* Morphology: LM: juxtamedullary glomeruli (corticomedullary) focal necrosis which spreads superficially as the disease progresses (segments of glomeruli have scarring and focal means some glomeruli will have scarring and some will not) Types: -C1q—very poor prognosis -collapsing with HIV*partnership -collapse of the entire glomerulus—very large Bowman’s space as a result -podocyte hyperplasia associated with HIV or drugs -poor prognosis A 15 year old with a history of malignant lymphoma (Non-Hodgkin’s) presents with nephrotic syndrome. All tests negative except urinalysis: 4+ protein Dx: Membranous Glomerulonephritispartners HAVE TO KNOW: hepatitis B, tumor (Non-Hodgkin’s), poison ivy, immune complex disease (e.g. lupus), syphilis, malaria, renal vein thrombosis Pathogenesis: chronic immune complex, so slow progessing, and thus complement level is nl LM: thick basement membrane IF: fine granular subendothelial deposits (in BM) with Ig and C3 Stages (MUST KNOW) 1- epimembranous deposits sitting at periphery 2- intramembranous deposits and basement membrane spikes 3- intramembranous depisits totally surrounded by BM 4- radiolucent areas where deposits used to be NO response to steroids Hepatitis B 2 partners: 1)PAN—nephritic syndrome 2) Membranous Glomerulonephritis—nephrotic syndrome Membranoproliferative nephritis: Type I= Mesangio Capillary Disease Type II= Dense Deposit Disease Vignette for Mesangio Capillary Disease: A 5 yo F with nephrotic syndrome, hypertension, and hematuria for the last 6 mos. She has a hx of hearing problems. Her uncle died at the age of 22 with chronic renal failure. CBC: Hemoglobin 10, indices normal Chem 20: BUN 20, Creatinine 3impaired renal function UA: 2+ blood, RBC casts (these two are nephritic), 4+ protein (nephrotic) LM: lobular pattern proliferation, increased mesangial matrix, thickening of BM Females>males, immune complex disease so low C3 and C4 due to Classical Complement Pathway, thick basement membrane (nephrotic) and proliferation of mesangial cells (nephritic) which cause *split basement membrane *recurs in renal graft IGA nephropathy Focal Segmental Glomerulonephropathy Membranoproliferative Glomerulonephritis Type I (Mesangio Capillary Disease) recurrence in renal allografts Dense Deposit Disease Mean age usually 16 Chronic glomerulonephritis Post infection such as strep or pneumonia Pathogenesis: alternative complement pathway*decreased C3* LM: same as mesangio capillary disease IF: discontinuous linear deposit of C3 peripherally…with antibody to C3 according to her picture on p.327…though this she did not explain in class or on her slides, also says “most patients have detectable circulating C3 nephritic factor, an IgG autoantibody” EM: ribbon-like deposits in lamina densa Systemic Diseases: Diabetes and Amyloidosis Diabetic Nodular Glomerulosclerosis (AKA Kimmelstiel-Wilson Disease)*nodular sclerosis (thick capillary loops with nodules), *hyalinization of afferent and efferent arteriolesthickened BMs of capillaries occurs in all organs, particularly in uncontrolled diabetes, leading to MI, gangrene, neuropathy, skin lesions, retinal lesions, and renal disease as a result of compromised blood flow Amyloidosis: Familial: 3rd decade Primary: 6th decade Secondary: 4th decadeassociated with multiple myeloma (back pain-lytic bone lesions, frothy urine (proteinuria), constipation (due to hypercalcemia caused by lytic bone lesions)) LM: nodular lesion, apple-green birefringence with congo red stain (little yellowgreenish fibers) EM: non-branching fibrils in BM, mesangium and vessel walls Slow downhill course to renal failure, NO response to steroids Nodular lesions: amyloidosis, diabetes, and light chain nephropathy (see later notes) Low C3: post strep, membranoproliferative type I and II, lupus Low C3 & C4: post strep, membranoproliferative type I, and lupus Review of last lecture for glom diseases: 45 yo archeologist who returns from a trip to Africa 3 weeks later he comes to the emergency room with fever, chills, and headache. These episodes of fever chills and headaches have recurred 3 times in 4 weeks. 2 weeks later he has frothy urine. What is his systemic illness and what is his renal problem? Malaria, Membranous Glomerulonephritis (nephrotic syndrome) 14 yo boy who comes in with nephrotic syndrome. He is known to have hearing problems. So what do you think his renal disease is? Mesangio Capillary Disease AKA Membranoproliferative Type I What do you think we would see on electron microscopy? Mesangialization, migration of mesangial cell in BM and this splits it, giving a tram track appearance 25 yo HIV positive male presents with nephrotic syndrome. What is his renal disease? Collapsing Focal Segmental Glomerulosclerosis If see spikes in context of glomerular disease: basement membrane protrusions in stage 2 of membranous glomerulonephritis Hepatitis C (FA also says HepB), what kidney disease is associated? Membranoproliferative Type I Which disease sometimes is familial? IgA Nephropathy, Membranoproliferative Type I, and amyloidosis Mesangialization on EMmembranoproliferative Type I Lung fibrosis and renal diseasescleroderma Apple-green birefringence in the glomerulusamyloidosis Kimmelstiel-Wilson lesionsDiabetic Nodular Glomerulonephritis Hyalinized afferent and efferent arteriolesdiabetes Selective proteinuria Minimal Change Disease (Lipoid Nephrosis) Nephrotic/Nephriticboth have blood and protein in urine: 1) Focal Segmental Glomerular Sclerosis 2)Membranoproliferative Glomerulonephritis Recurs in renal allograft: 1)IgA Nephropathy 2)Focal Segmental Glomerulosclerosis 3)Membranoproliferative Type I Palpable rashHS purpura IgA deposits in the skinHS purpura Ribbon-like deposits in lamina densa on electron microscopymembranoproliferative disease Type II (Dense Deposit Disease) Alternative Complement Pathway Activation membranoprolif Type II Non-Hodgkin’s lymphomaMembranous Glomerulonephritis Subendothelial depositslupus Urinary Tract Infections, Renal Hypertension, Tubular Necrosis (+ some other stuff Dr. Gohara threw in from previous lectures) Acute pyelonephritisWBC casts Major complication: papillary necrosis CP: sterile pyuria and severe flank pain radiating to the groin 4 causes of papillary necrosis: 1) acute pyelonephritischronic pyelonephritis and inflammation 2) Diabetes 3) Sickle cell anemia 4) Analgesic abuse Last 3 mech is ischemia Older male w/large prostateincreased risk of urinary tract infections Pulmonary endotheliumACE Fibrinoid necrosis of blood vessels malignant hypertension Hyalinizationbenign hypertension Sickle Cell Disease papillary necrosis (ischemia) Eosinophiluriaantibiotic useacute interstitial nephritis Papillary necrosis sickle cell disease, diabetes, acute pyelonephritis with obstruction, analgesic nephritis (chronic interstitial nephritis) Tubulorrhexis Ischemic tubular necrosis (can be caused by blood transfusion mismatch—get hemolysis of RBCs and resulting ischemia) Oxalate crystals in urine ethylene glycol (antifreeze) Segmental tubular damage ischemic tubular necrosis Sterile pyuriapapillary necrosis Onion skinning chronic malignant hypertension Urea splitting organismproteus (stones) Staghorn stone stone obstructing pelvis of the kidney (large) Pylonephrosis obstruction and then superimposed infection (kidney is a pocket of pus) Hepatitis C membranoproliferative Type I* Nodular lesions Diabetes, amyloid, light chain disease * Non-branching fibers on EM amyloid* Berger disease(another name is) IgA nephropathy* Light chain nephropathy multiple myeloma 17 yo male presents to the ER with hematuria, headache, and blurred vision, BP 205/130 Dx malignant hypertension Renal morphologyfibrinoid necrosis of blood vessels 55 year old lady with RA for 20 years with severe renal colic and sterile pyuria Dx: papillary necrosis What caused it: analgesics for her RA Berry aneurysmadult polycystic kidney disease Lamellation of lamina densaalport Radially arranged cystsinfantile type polycystic disease Cysts in the liveradult polycystic disease 45 yo male presents with hypertension, hematuria, and bilateral flank discomfort. His dad is 65 and has been on renal transplant list for 7 yearsadult polycystic disease A 6 yo girl has hearing problems and hematuria Dx: Alport* Pathogenesis—alpha 3 and alpha 4 chain of collagen type IV is mutated* Differentiate from Membranoprolif type I is mixed (both nephrotic (protein) and nephritic (blood))—she just has blood Congenital Familial Renal Diseases (reviewing notes) Infantile Polycystic Disease (Potter Type I)radially arranged cysts extending through cortex and medulla in the interstitium, incompatible with life bc no room for nl tissue, autosomal recessive*, oligohydramnios (little amniotic fluid) during pregnancy*, Mutation in PKHD1 gene* that codes for a membrane-receptive protein called fibrocystin (Fibrocystin is a large, receptor-like protein that is thought to be involved in the tubulogenesis and/or maintenance of duct-lumen architecture of epithelium~Wikipedia) Dysplastic Kidney (Potter Type II)sporadic and usually unilateral (if bilateral= incompatible with life), usually associated with CNS abnormalities and esophageal atresia, lots of cysts and remnants of mesenchymal tissue especially cartilage Adult Polycystic Kidney (Potter Type III)abnormality of interstitial regions and multiple small cysts initially and manifest in late 30s early 40s as cysts become larger, fill with fluid, and compress on surrounding parenchyma; also can get infection due to stagnation and urine a good nutrient broth, repeated infections lead to scarring, autosomal dominant* Clinically: hematuria due to infections (red blood cells and red blood cells casts), hypertension (due to scarring of BVs), liver cysts*, 20 % have berry aneurysm* of cerebral vessels (may not know they have disease until suddenly collapse due to leakage of aneurysm or hemorrhage), flank pain, renal stones due to repeated infections A 45 year old male executive died suddenly after collapsing in his office. He had complained of a severe headache and nausea earlier. Major autopsy findings include: massive subarachnoid hemorrhage, enlarged cystic kidneys. What is the underlying cause of his intracranial hemorrhage? Berry aneurysm What is the nature of his renal disease? Potter Type III (Adult Polycystic Disease) What is the mode of inheritance of this disease? Autosomal dominant What are other types of cystic renal disease? Infantile polycystic, dysplastic kidney, medullary cysts Adult Onset Medullary Cystic Diseaseautosomal dominant*; corticomedullary cysts*, shrunken kidneys*, scarred, salt-losing polyuria*, chronic renal failure beginning in adulthood Horseshoe kidneyfailure of kidneys to rotate and poles fuse to form a horseshoe kidney that remains in the pelvis, may be mistaken for a pelvic tumor, stagnation of urine and stone formation occur in the lower part of the U shape, repeated infections lead to scarring and hypertension and impaired renal function Associated with Turner Syndrome (USMLE World) Benign Recurrent Hematuriasporadic or familial, prognosis is good, on EM see thin capillary loops* (probably leak to cause the hematuria) Alport Syndromefemales: hematuria and mild proteinuria (autosomal recessive; can get X-linked but only manifest with mild hematuria since X-linked needs both X’s knocked out to manifest as poorly as males; females do not go into renal failure); males: autosomal recessive or more commonly X-linked, progress to renal failure; clinical manifestations: ocular problems such as cataracts and dislocated lenses and hearing problems (neurosensory loss)*Autosomal recessive defect: α3 and α4 chains of Collagen Type IV; *X-linked defect: α5 chain of type IV collagen Morphology: EM—lamellation of lamina densa (splitting of lamina densa) also called “basket woven appearance”, “moth-eaten appearance” Side note: remember α3 chain of Collagen Type IV is the antigen in Good Pasture’s Syndrome Renal Tumors (reviewing notes) Hamartomasbenign angiomyolipomas (angio=blood, myo= Sm. Muscle cells, lipoma= fat tissue)part of systemic disease called *Tubular sclerosisrhabdomyomas (benign tumor of striated muscle (skeletal muscle)) in the heart tissue, also associated with neoplasms of skin, heart, and brain Renal Adenocarcinomain proximal convoluted tubules* Predisposing factor to remember: Tobacco* (this puts people at increased risk for GI, lungs, kidney, bladder, and pancreas cancer) Most are sporadic Gene implicated is Von Hippel-Lindau (tumor suppressor gene)* in both sporadic and familial cases of clear cell carcinoma, familial type is without symptoms; the gene is lost, inactivated, or hypermethylated Hereditary papillary carcinoma: autosomal dominant*, mutation in MET protooncogene*, Trisomy 7*, usually bilateral; CP: painless hematuria*; Lab findings: polycythemia* (tumors secrete erythropoietin), hypercalcemia* (causes constipation, people act funny as causes mental issues), feel itchy all over, feel flushed all the time, very high Hbg and Hct How to differentiate Hereditary papillary carcinoma from Polycythemia rubra vera? In the latter, EPO is very low Clear cell carcinomas are the most common renal adenocarcinomas Sporadic papillary carcinoma: papillary growth pattern, *trisomy 7, 16, 17*, Loss of Y* (in male patients), mutated, inactivated MET*; chromosome 7 encompasses MET*, a protooncogene that serves as a tyrosine-kinase receptor for hepatocyte growth factor, scatter factor, which mediates growth, cell motility, and invasion (targets epithelial and endothelial cells)(on Boards), *multifocal and bilateral, spread through renal vein* Wilms Tumor - peak age 2-5 years old, the younger the child at diagnosis, the better prognosis; can be completely cured by surgery, radiation, and chemo - Associated with 3 syndromes o WAGR Syndrome: Wilms Tumor, Aniridia (no iris in eyes), Genital Anomalies, Mental Retardation; deletion of 11p13 tumor associated gene WT1 o Denys-Drash Syndrome: gonadal dysgenesis, diffuse mesangial sclerosis (mesangial cells are specialized smooth muscle cells around blood vessels in the kidney that help to modulate blood flow)renal failure, gonadoblastoma (tumors of gonads), Wilms Tumor o Beckwith-Wiedeman Syndrome: organomegaly, macroglossia (unusual enlargement of the tongue), hemihypertrophy (enlargement of one side of the body) - Sporadic cases associated with mutation of *β catenin gene* (in adherin junctions and connects to actin skeleton) - Cells of embryonic origin are displaced in kidney and grow and differentiate into various types of tissue - Lab findings: erythropoietin levels are elevated (used to monitor therapy, recurrence, metastasis) - Micro: epithelial abortive glomeruli* (non-functional), stromal rhabdosarcoma* (stromal malignant skeletal muscle cells), embryonal* Assessment of Renal Function (reviewing notes) Urinanalysis (know these): - colorless: dilute urine (if not bc well-hydrated, think tubular disease* as cause of not reabsorbing a lot of water), low specific gravity - red: hemoglobin, myoglobin (blood) - black: melaninmetastatic melanoma Specific gravity: Low specific gravity diabetes insipidus and tubular diseases High specific gravity diabetes mellitus and dehydration *pH variable with diet: pH of 7 or less, uric acid crystals will be present* Nitritesbacteruria (infection)* partner Proteinuria (per 24 hours): MUST KNOW THESE 1+: 250-500 mg 2+: 500-1000 mg 3+: 1000-2000mg 4+: >2000mg –nephrotic syndrome Microscopic Examination: Casts: -RBCs Acute Nephritic Syndrome -WBCsAcute Pyelonephritis -Granular (broken RBCs)Acute Nephritic Syndrome -HyalineChronic Renal Disease -TubularAcute Tubular Necrosis -Oval Fat Bodies (tubular cells filled with lipid)nephrotic syndrome Obstructive Pulmonary Diseases Dyspneacommon feature of obstructive pulmonary diseases Cigarette smokingbronchitis and emphysema Paroxysmal reversible obstructionasthma Mucous gland hyperplasia, hypersecretion, tobacco smoke, productive coughchronic bronchitis Alveolar dilation, scarring bc of severe or chronic infections, cough, purulent sputum, feverbronchiectasis Smooth muscle hyperplasia, excess mucous, inflammation, episodic wheezing, cough, dyspneaasthma Air space enlargement and alveolar wall destruction, acinus involvement, tobacco smoke, dyspneaemphysema inflammatory scarring/obliteration of bronchioles, tobacco smoke, air pollutants, cough, dyspnea Small-airway disease bronchiolitis (beginnings of emphysema) persistent cough with sputum production present for at least 3 months per year and for at least 2 consecutive yearsclinical diagnosis of chronic bronchitis increased Reid Index (thickness of mucous gland layer/thickness of wall between epithelium and cartilage)Chronic Bronchitis Cor Pulmonale with heart failureChronic bronchitis In class review: Cyanosischronic bronchitis Smokingemphysema and chronic bronchitis Pizzalpha 1 antitrypsin deficiency Liver cirrhosisalpha 1 antitrypsin Wheezingobstructionasthma (a lot +++++) and chronic bronchitis (++) Barrel chestemphysema Pneomonectomycompensatory hyperinflation Viral infectionintrinsic asthma Eosinophils spiutmasthma Increased reid indixchronic bronchitis Hyperplasia of the submucous glandschronic broncthitis and asthma Curshmann spiralsasthma Charcot leyden crystals-->asthma Hypertrophy of sm masthma Emphysema <40yoalpha 1 antitrypsin deficiency ADAM33 polyasthma YKL40chitinaseasthma InfertilityCF Steatorhhea and increased NaCl in sweat and repeated respiratory infectionsCF Fouls smelling sputumbronchiectasis Metalloproteinase familyADAM33 Increase IgEatopic asthma Cor pulmonale-->chronic bronchitis (+++++) emphysema (++) Diffuse infiltrative lung diseases: Dyspnea, crackles (rales), no wheezing, reduced total lung capacity, x ray: honey comb lung (end stage), fibrosis of lung: pulmonary hypertension and cor pulmonale (end stage) Alveolitisearliest manifestation of diffuse infiltrative lung disease (restrictive lung disease) Egg shell calcifications of lymph nodesSilicosis Increased risk for tuberculosissilicosis Amphibole asbestosmesothelioma Amiodorone (an antiarrhythmic drug)Pulmonary fibrosis, microvesicular steattosis of the liver, and hypothyroidism Radiationalveolitisrestrictive lung diseases Diffuse interstitial lung disease partnership review in class Alveolitisrestrictive lung diseases Caplan syndromeRA and pneomoconiosis Amiodarone (an antiarrhythmic)lung fibrosis, hypothyroidism, microvesicular steatosis (small tiny fat droplets) of the liver *Know all of them—check TSH before putting pt on this drug Macrovesicular steatosisalcohol associated (big fat globs) Reticular nodule lesions consistent with Honeycomb lungend stage of restrictive lung disease Amphibole fibersbrittle, straight, short asbestos fibers (break and scatter and cause damage)pathogenic for mesothelioma TBsilicosis (silica suppressed cell mediated immunity and inhibits ability of macrophages to kill ingested microbacteria) Hypercalcemiasarcoidosis (that we’ve talked about so far—will have another tomorrow) Anti GM-CSFalvelor proteinosis Genetic is a mutation in the same factor (GM-CSF) Quartzsilicosis Impaired surfactant clearancealveolar proteinosis Egg shell calcifications in lymph nodes on x-raysilicosis (online also said CWP) Chitinasesasthma (YKL40 tells about prognosis) Metalloproteinases in asthma ADAM 33 polymorphism Mucous plugs asthma (curschmann) Pleural plugsasbestos Raynaud’s phenomenen and shortness of breathscleroderma, fibrosis of lungs A shipyard worker 65 yo comes in with dyspnea and fatigue for 6 monthsasbestosis (do chest x rays and find asbestos fibers) A 35 yo lady comes in with painful nodules on her legs for 3 months. Also her eyes have been itchy and watery. She also has recurrent viral infectionssarcoidosis, recurrent viral infections bc no CD4 bc consumed in the granulomas, check ACE and do a chest x ray. Atelectasis of the lung, acute lung injury, and diseases of vascular origin lecture review in class: Hyaline membrane (fibrin) in alveoliARDS UremiaARDS Hypoxia refractory to oxygen*ARDS Sepsis a cause ofARDS Fracture femurfat embolism Criminal abortionair embolus Lines of Zahn*premortem clot (2 lines: 1 line of fibrin (light pink) and 1 line of RBCs (dark red) Increased LD3pulmonary infarct wedge shapepulmonary infarct Brown induration (severe congestion)mitral stenosis BMPR2 mutationprolif of sm m in pulmonary vasculatureprimary pulmonary hypertension* Normal BMR2 inhibits prolif of sm. Mm. Necrotizing granulomaswegeners NSAIDsasthma Pizzalpha antirrypsin Blue bloaterschronic bronchitis Pink puffersemphysema Vignettes: 65 yo lady with a hx of RA develops silicosis after retiring from a glass factory Dx: Caplan Syndrome * 70 yo male presents with dyspnea for 6 months, chest x-ray reveals honeycomb lung* Dx: end-stage restrictive lung disease* Pathogenesis: alveolitis* 8 yo boy playing with marbles with his cousin. His cousin pushes him. 2 days later develops he develops dyspnea auscultation reveals markedly diminished breath sounds Dx: obstructive atelectasis X ray: mediastinum shifted toward affected lung 35 yo F with progressive dyspnea, leg edema, hemoptysis and discomfort in rt upper quadrant Dx:primary pulmonary htn, cor pulmonale as a result Pathogenesis: mutation of BMPR2* 65 yo construction worker with chest pain, recurrent pleural effusion* and dyspnea* for 3 months chest x ray reveals pleural opacities Dx: mesothelioma *pleural plugs alone do not cause these Bx of pleura reveals malignant cells Partnership Reviews in Class: A young African American woman comes in because she has had recurrent renal colic (sharp pain in the lower back that radiates to the groin) and hematuria. Now she also reports shortness of breath. No rash No hemoptysis No scleroderma DDx: Sarcoidosis, bc lung and kidney involvement but no hemoptysis The reason she has colic is because she has high calcium and thus calcium calculi in the kidney. Pts don’t always have to have constipation. X ray: in the lungs, nodular lesions In mediastinum, see hilar lymph nodes If biopsy, will see non-caseating granulomas A 60 yo male heavy smoker presents with left eye ptosis and dry skin on the left side of his face Dx: Horner’s Syndrome Pathogenesis: Lung cancer invading sympathetic ganglia Check: Do chest x ray to find a mass A 55 yo male presents with htn, recent onset diabetes, and a round swollen face. He has been smoking for 30 years. Dx: Cushing’s Syndrome Underlying problem: elevated ACTH coming from small cell carcinoma A 26 yo man presents with productive cough for 4 months. The sputum is mucinous. Dx: Bronchioalveolar carcinoma Bx: a papillary tumor lined up by tall columnar cells A 55yo man presents with flushing, diarrhea, and a new murmur consistent with tricuspid valve damage. Dx? Carcinoid Syndrome EM? Bx of tumor will show neurosecretory granules A 75 yo male dies suddenly after a surgery for a broken femur. Dx: Fat embolism A 22 yo tall slender man presents with sudden onset of dyspnea and chest pain. Chest exam reveals decreased breath sounds. X ray reveals a collapsed left lower lobe. The trachea is pushed away from the collapsed lung. Dx: Spontaneous pneumothorax, secondary to peripheral emphysema that occurs in young people called Paraseptal Emphysema Some new and old partnerships… Endothelial injury ARDS SIADH paraneoplastic syndrome of small cell carcinoma Gelatinous sputumalveolar proteinosis*GMCSF mutation or loss caused by antibodies* Deep leg veinsthromboembolismcan cause a PE Air fluid levelabscess Lambert EatonautoAbs against neuronal Ca2+ channels and they have muscle weakness that improves when use the muscles (in contrast with Myasthenia Gravis where the muscle weakness gets worse when you use the muscle) Virchow nodesupraclavicular node invaded by gastric or lung cancer cannot be resectedsmall cell carcinoma Dexamethasone suppression testdifferentiates between ectopic cancer producing ACTH (doesn’t suppress) and pituitary cancer causing Cushing Syndrome where it does suppress the ACTH Elevated Reid IndexChronic Bronchitis Peripheral tumor of the lungadenocarcinoma Sharp chest painpleuritis Shortness of breathpleural effusion Lines of Zahnpremortem clot Erythema nodosumsarcoidosis Lamellar bodies in the sputumalveolar proteinosis Head and Neck Pathology Make enamel resistant to degradationfluoroapatite (from fluoride) Chronic alcoholics, homeless, bacillus fusiformis, poor dental hygienerisk factors for gingivitis Hyperplastic gums (swollen gums)phenytoin and AML5 (monoblastic leukemia) Periodontitis (inflammation of periodontal ligament, cementum, and bone)actinobacillus and actinomycetes Periodontitisimmune system impairment: e.g AIDS, Leukemia, Diabetes, Neutropenia Periodontitis can cause infective endocarditis, pulmonary abscess, and brain abscess An erythematous, hemorrhagic, exophytic mass on the gingival mucosa of a pregnant womanpyogenic granuloma (pygogenic granuloma looks like granulation tissue (not granuloma—no giant cells) under the microscope. Reminder that granulation tissue consists of neovascularization, fibrosis, and lymphocytic infiltrates) A single painful ulceration of the mouth mucosa with an erythematous halo surrounding a yellowish fibrinopurulent membrane in a woman who is stressedapthous ulcer (canker sore) Beefy red tongueglossitis B12 deficiency (e.g. Pernicious Anemia), Celiac Sprue, Kawasaki Disease, PlummerVinson SyndromeGlossitis http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001984/ (reminder of Kawasaki) Macroglossia (large tongue)children (Cretinism—congenital hypothyroidism; and Pompe Disease—Acid Maltase deficiency, a lysosomal storage disease) and Adults: Cmyloid (Amyloidosis—kidney problems: nephrotic syndrome manifesting as edema of legs and foamy urine; heart failure: dyspnea and leg edema) Herpes Simplex virus, recurrent vesicular lesionscold sores White lesion that can be scraped and goes away with tx; associated with immunosuppression, diabetes, and AIDScandida albicans (Thrush) White thickening of the epithelium that cannot be scraped, precancerousleukoplakia Raspberry tongueScarlet fever Strawberry tongueScarlet fever Koplik spotsMeasles Dirty white suppurative membrane over tonsilsDiptheria Red vesicular lesions in mouth after antibioticerythema multiforme (Stevens-Johnson Syndrome) Ludwig angina (cellulitis of the neck)pancytopenia that leads to gingivitis, pharyngitis, and tonsillitis Enlargement of the gingivamonocytic leukemia (AML5) Striking fibrous enlargement of the gingivaephenytoin (Dilantin) ingestion Multiple congenital aneurysmal telangiectasis beneath mucosal surfaces of the oral cavity and lipsRendu-Osler-Weber Syndrome Smoking, Alcohol, and HPVrisk factors for Squamous cell carcinoma of the mouth Mutations that cause hyperplasia/hyperkeratosis + mutation of p53 causing dysplasiasquamous cell carcinoma of the mouth Necrotizing lesions of the nasal cavity and sinusitisWegener’s granulomatosis Sinusitis in diabeticsmucormycosis HPV 6, 11squamous papilloma of the nasopharynx Virus found in nasopharyngeal cancerEBV Tx for nasopharyngeal cancerradiotherapy (50-70% 3-year survival, undifferentiated, unkeratinized the most sensitive) H. influenzae, β-hemolytic Strep, parainfluenzalaryngoepiglottitistrouble breathing and barking cough (croup) Hoarseness of voice in a singersinger’s nodules Tobacco use, persistent hoarseness, later dysphagia, pain and hemoptysissquamous cell carcinoma of the larynx, keratinizing Swelling of the parotid glandMumps (an RNA virus) In children, no sequelae from Mumps Pancreatitis and Orchitissequelae from Mumps in adults Sialolithiasisbacterial sialadenitis Anti-SSA (anti-RO) and Anti-SSB (anti-La), dry eyes and mouth, risk for lymphomaautoimmune Sjogren Syndrome Anti-RO (anti-SSA)intrauterine heart block of fetus Mixture or epithelial cells and myxoid connective tissue that forms a benign tumor of the parotid glandPleomorphic adenoma Most common benign tumor of the parotid glandpleomorphic adenoma Tumor comprising of glands and lymphocytesWarthin tumor (papillary cystadenoma lymphomatosum) Second most common benign salivary gland tumorWarthin tumor (papillary cystadenoma lymphomatosum) Most common malignant salivary gland tumor with squamous cells, mucus-secreting cells, and intermediate cells of varying differentiation (majority in parotid)Mucoepidermoid carcinoma parainfluenza virus croup [epiglottitis] EBV nasopharyngeal carcinoma HPV oral cancer, laryngeal papillomas GlossitisB12 deficiency, Kawasaki, Plummer-Vinson, celiac sprue Mumpsorchitis P53 mutationoral cancer Mucormycosisdiabetes Facial palsymalignant tumor, parotid gland, resection of benign parotid tumor Macroglossiachildren (cretinism/Pompe), adult (amyloid) Vignette: A young vagrant with foul gums: a 19 year old male, a homeless vagrant, is seen in the ED in a drunken state. He is bleeding from the mouth but has no history of trauma. On examination there is acute sloughing and ulceration of the gums surrounded by an inflamed red mucosa w/ many areas of bleeding. The breath is foul & the teeth are dirty, with a large build up of plaque & calculus. A smear from the ulcerated areas shows numerous fusiform & spirochaetal organisms Diagnosis: gingivitis Predisposing factor: poor oral hygiene Organisms: Bacillus fusiformis Long-term complications: ulceration of mouth, necrosis Vignette: A 72 y/o retired bookbinder is referred by his dentist because of an area of white thickening of the buccal mucosa. On examination, there is an ill-defined thick white patch on the buccal mucosa on the left (cannot be scraped off) Diagnosis: leukoplakia Why biopsy: to rule out cancer (this is a precancerous lesion) Vignette: A retired doctor aged 74 - area of white thickening on lateral border of anterior third of tongue; smoked many years, alcohol. Describes lesion as slowly enlarging thick white patch present for many months Diagnosis: carcinoma Biopsy: squamous cell carcinoma Spread: will go to cervical lymph nodes Vignette: 57 y/o woman w/ smooth enlarging mass at angle of jaw on left side. Has been present for some years, no trouble but slowly enlarged & now disfiguring. Her daughter fears cancer & lump can no longer be disguised; appears to be in parotid gland Diagnosis: pleomorphic adenoma Precautions during surgery: facial nerve Vignette: "Singer w/ hoarse voice" Diagnosis: singer's nodule Vignette: An old man w/ loss of voice: 68 M, pig farmer, heavy smoker, has had hoarse voice for as long as can remember; complete loss of voice 1 month; left vocal cord replaced by large white friable mass Diagnosis: squamous cell carcinoma of larynx Pathology of the Esophagus Upper esophageal webs, iron deficiency anemia, glossitis, and cheilosisPlummer-Vinson Syndrome Risk of post-cricoid carcinomaPlummer-Vinson Syndrome Vignette: a 30 yo man comes in tired, pale, bothered by dry, cracked lips. CBC shows iron deficiency anemia (microcytic anemia), red beefy tongue (glossitis), upper endoscopy shows esophageal webs Dx: Plummer-Vinson Syndrome Zenker (Pharyngeoesophageal) Diverticulumdiverticula immediately above the UES; associated with accumulation of food in diverticula and regurgitation, dysphagia, a neck mass, and aspiration pneumonia Diverticulum located above LES, nocturnal regurgitation of massive amounts of food when lie downEpiphrenic Diverticulum Longitudinal treats at the esophagogastric junction or gastric cardia, commonly seen in alcoholics in binge drinking with severe retching or vomiting, severe pain and vomiting blood bc tore mucosaMallory-Weiss Syndrome Pain to back and vomit bloodBoerrhaave syndrome (perforated GI tract, esophagus) Prolonged or severe portal hypertensionblood diverted through coronary veins of stomach and submucosal venous plexusincreased pressure in plexusvarices Alcoholic cirrhosisesophageal varices (if rupture, massive hematemesis and up to 50% die in first bleeding episode) Heartburn, dysphagia, in severe cases: hematemesis and melenareflux esophagitis Ulceration, stricture, Barrett espophagus, bleedingbad clinical outcomes of reflux esophagitis Metaplastic change in which squamous epithelium of esophagus is replaced by columnar epithelium with goblet cells (intestinal metaplasia)Barrett Esophagus Long-standing GERDBarrett Esophagus Barrett Esophagus is single most important risk factor for? esophageal carcinoma Squamous cell carcinoma of esophagus risk factorsin US, alcohol and tobacco; in other countries, fungi and nitrosamines Dysphagia predominant sign with weight lossadenocarcinoma Insidious onset with late development of dysphagia, obstruction, cachexia, debilitationsquamous cell carcinoma of esophagus Review: EBVnasopharyngeal carcinoma Koplik spotsMeasles Ludwig angina (severe inflammation of buccal mucosa with cellulitis (severe swelling) of the neckpancytopenia (see in patients on chemo) Bacillus fusiformis (poor hygiene, alcoholics)gingivitis Pregnancypyogenic granuloma Dirty membrane on tonsils, fever, difficulty breathingdyptheria Plummer-Vinson Syndromecheilosis, upper esophageal webs, iron deficiency anemia Nocturnal regurgitation of large amt of fluidepiphrenic diverticulum Barrret esophagusintestinal metaplasia of the lower esophagus; associated with adenocarcinoma of the esophagus HPVnasopharyngeal papilloma (benign lesions) Stressaphthous ulvers Diabetesmucormycosis especially of sinuses Chaga’s diseaseachalasia Singer’s nodulereactive nodule (another name) Esophageal varices portal hypertension Coronary veinsesophageal submucosal venous plexusvarices (pathway of blood from liver to esophagus) Longitudinal mucosal tear of the esophagusMallory-Weiss Syndrome Vignette: binge drinking and then vomit forcibly and mucosa tears up; if also pain in back, they ruptured their esophagus Boerrhaave Boerrhaaverupture esophagus Parainfluenza viruscroup (epiglottitis)—cannot breathe and seems to be choking (Haemophilis inf also, but not as common) Kawasakiglossitis Orchitismumps in adults Most common tumor in salivary glandspleomorphic adenoma (myxoid stroma) Intrauterine fetal heart blockanti-Ro with Sjogren syndrome in mother Pathology of the stomach Antiparietal cell antibodiesautoimmune gastritis Congenital hypertrophic pyloric stenosisOlive like mass, projectile vomiting, 2-3 wks old, Turner Syndrome, visible peristalsis Pernicious anemiaautoimmune gastritis NSAIDSdecreased prostaglandinsacute gastritis and peptic ulcers and chronic interstitial nephritis NSAIDS, excessive alcohol consumption, heavy smokingacute gastritis Pathogenesis of acute gastritis: Increased acid secretiondecreased HCO3-decreased blood flowdisruption of mucous layer + direct mucosal injuryacute gastritis Massive hematemesis in alcoholicsesophageal varices, acute gastritis, Mallory-Weiss Syndrome Antral chronic gastritisHelicobacter pylori (90%) Autoimmune gastritisantibodies to parietal cells, gastrin receptor, intrinsic factor, and H+K+ ATPaseachlorhydria, pernicious anemia, atrophy of the mucosaHIGHER risk for gastric carcinoma if pernicious anemia present Chronic gastritislymphocytes and plasma cell infiltrates; if neutrophils present, there is active inflammation Chronic gastritis due to H. pylorihypochlorhydria, not achlorhydria bc not all parietal cells are destroyed Autoimmune gastritishypergastrinemia H. pyloririsk of chronic gastritis, peptic ulcer, gastric carcinoma, MALT lymphoma Prostaglandin synthesis by mucosal cells (COX inhibitors remove these protective effects)increased mucus and bicarbonate production, vasodilation and improved mucosal blood flow, inhibits acid secretion by parietal cells Antral type gastritis caused by H. pyloriincreased acid production and increased risk of duodenal ulcer Pangastritis caused by H. pyloriatrophy Zollinger-Ellison Syndromemultiple peptic ulcers in the stomach, duodenum, and jejunum due to excess gastrin secretion by a tumor (gastrinoma) Curling ulcersassociated with severe burns or trauma Cushing ulcersassociated with intracranial injury, operations or tumors Intracranial injurydirectly stimulate vagal nuclei, leading to increased acid production Phytobezoarsconcretions of plant matter in the stomach Trichobezoars “hairballs” in the stomach Menetrier’s disease (a type of Hypertrophic Gastropathy)males in the 4th-6th decades, hyperplasia of mucous cells, with atrophy of glandsexcessive mucous causes loss of protein in feces and thus hypoproteinemia Hyperplastic polypsno malignant potential Adenomasmalignant potential Nitrites, smoked and salted foods, pickled vegetables, deficiency of fresh fruits and vegetables, cigarette smokinggastric carcinoma Mutations in CDH1E-cadherinrisk for gastric cancer Loss of E-cadherindiffuse gastric carcinoma BRCA2 mutationsdiffuse gastric carcinoma Large portion of gastric wall or entire stomach infiltrated with malignancy, “leather bottle” appearanceLinitis Plastica Intestinal type histologymutations in β cadherin and APC Gastric type histologyinfiltrating pattern of poorly differentiated cells with “signet ring” conformation (cells full of mucus with nucleus pushed to the side) Virchow’s node (supraclavicular node)lump in neck due to mets from gastric or lung carcinoma Krunkenberg Tumorsmets to ovaries from gastric cancer Sister Mary Joseph nodulemetastatic nodule that appears in paraumbilical region MALT Lymphoma (lymphoma of mucosa-associated lymphoid tissue)11;18 translocation Gastrointestinal stromal tumormutation of the gene encoding tyrosine kinase (cKIT) Gastrointestinal Carcinoid Tumors -most common in the jejunum/ileum -patients typically in 50s-60s -all secrete serotonin -in stomach, MEN-1 mutation -in proximal duodenumCCK (cholecystokinin) causes biliary obstruction and abdominal pain; also associated with Zollinger-Ellision Syndrome and NF-1 (neurofibromatosis-1) -in jejunum/ileumpolypeptide YY also secreted which causes constipation; aggressive behavior -in appendixmostly an incidental finding bc asymptomatic, benign behavior Crohn’s Skip lesions Transmural granulomas fistulas and strictures cancer+ Ulcerative colitis Continuous –rectum then up mucosal crypt abscess cancer+++ superficial Review in class: Krunkenberg tumormetastatic signet ring gastric tumor to ovary AdhesinsH.pylori Multiple gastric ulcersZollinger-Ellison Syndromevery increased gastrin Protein-losing gastropathy, diarrheaMenetrier’s Disease Linitis plasticainfiltration of all layers by gastric carcinoma Head injuryCushing ulcer Burnscurling ulcer Pain boring to backperforated peptic ulcer Blood group Acarcinoma of stomach Urea breath testH. pylori Zenker Diverticulumupper esophagus NSAIDSpeptic ulcers Pathology of small intestine Contains all 3 layers of normal bowel wall (true diverticulum)Meckel Diverticulum Osmotic diarrhea (osmolality exceeds that of the plasma)lactasae deficiency (lactose intolerance) Several bowel movements, bulky, fat, foul-smelling, floats, weight loss, anorexiaMalabsorption Celiac Sprue, Crohn’s Disease, pancreatic insufficiencyMalabsorption syndrome Rotavirusoutbreaks of infectious enterocolotis in infants Norwalk virusesoutbreaks in school children and adults Adenovirusesoutbreaks in infants Astrovirusesoutbreaks in children Vibrio choleraewater borne enterotoxinsecretory diarrhea S. aureusquick onset, food-poisoning (pre-formed toxin), e.g. egg salad at party and everyone who ate it became sick Salmonella and shigellainvasive bloody diarrhea Typhoid feverdiarrhea or constipation Giardia lambliamalabsorptionsteattorhea Entamoeba histolyticadysentery (pain, blood, low volume) Radiationendothelial cell injuryischemic fibrosis and stricture Clinical Vignette: 31 yo male with an itchy vesicular rash on extensor surfaces, such as the elbow. The rash has been there for 2 weeks. On further questioning, he reports diarrhea for 6 months (steatorrhea) and 15 lb weight loss. Dx: Celiac Sprue Tests: Anti-gliaden and anti-endomysial antibodies (IgA immunoglobulins, some IgG; have to look for IgG immunoglobulins if also have IgA deficiency); Bx Tx: improves on withdrawal of wheat gliadens and related grain proteins from diet Pathology: Cytotoxic T-cell mediated hypersensitivity, release cytokines which damage intestinal wall Morphology: grossly, mucosa appears flat or scalloped, or even normal Microscopically, diffuse enteritis with marked atrophy or total loss of villi and increased intraepithelial lymphocytes Hypersensitivity to wheat gluten and gliadenHLA-DQ2 and DQ8 HLA-DQ8Hashimoto’s Thyroiditis, Grave Disease, IgA Nephropathy Clinical features: diarrhea and failure to thrive in infants but may not present with malabsorption until adults Dermatitis herpetiformisgranular IgA deposit in dermal papillae in response to gluten ingestion; is characterized by intensely itchy, chronic papulovesicular eruptions, usually distributed symmetrically on extensor surfaces (buttocks, back of neck, scalp, elbows, knees, back). (Dermatitis herpetiformis from Wikipedia) Clinical Complications: risk of *non-Hodgkin’s lymphoma, small intestinal adenocarcinoma, and esophageal SCC Tropical Sprue= celiac-like malabsorption syndrome in people visiting the tropics or people of the tropics, no specific causal agent found, but enterotoxigenic organisms implicated, responds to antibios, changes similar to Celiac, not associated with lymphoma Whipple Disease= a rare systemic disease primarily of the intestines, joints, and CNS, caused by gram-positive actinomycete Tropheryma whippelii; usually affects white males (suspect associated with occupations, such as farming), lamina propria is laden with distended macrophages, containing tiny rod-shaped bacilli that are PAS positive*; presents with malabsorption syndrome, polyarthropathy/polyarthritis, lymphadenopathy and hyperpigmentation of skin in >50%; cardiac and neurologica signs can also be present, responds to broad spectrum antibiotics Disaccharidase cleaves lactose: Disaccharide deficiencyincreased lactose in gut lumen,osmotic diarrhea and malabsorptionbacterial fermentation of unabsorbed lactoseincreased hydrogen production and gaseous symptoms Abetalipoproteinemia: autosomal recessive disorder in which there is mutated MTTP gene; “The MTTP gene provides instructions for making a protein called microsomal triglyceride transfer protein, which is essential for creating beta-lipoproteins. These lipoproteins are both necessary for the absorption of fats, cholesterol, and fat-soluble vitamins from the diet and necessary for the efficient transport of these substances in the bloodstream” (Wikipedia) ; deficiency is betalipoproteinsdecreased LDL and VLDL and chylomicrons (betalipoproteins needed to transport VLDL and chylomicrons)defective cell lipid membranesacanthocytes (Burr cells) Decreased synthesis of apoproteins leads to increased TGscell vacuolization of enterocytes seen on biopsy/microscopy -deficiency of fat soluble vitamins (ADEK) and decreased ability to absorb fat -infancyfailure to thrive, diarrhea, and steatorrhea http://en.wikipedia.org/wiki/Abetalipoproteinemia Ischemic Bowel Disease -usually old people with atherosclerosis or young people with hypercoagulability -can be restricted to either the small or large intestine or both -infarctions seen with acute occlusion of celiac, superior, and inferior mesenteric arteries -etiologies: thrombosis, embolism, non-occlusive (cardiac failure, shock, etc.), radiation therapy, volvulus, stricture -symptoms: severe, intolerable pain and bleeding in stoolbright red blood in stool -50-75% death rateshort time between symptoms and perforation -Transmural infarcts: sudden, severe abdominal pain and tenderness, can have nausea and comiting and bloody diarrhea, shock and vascular collapse within hours, diminished peristalsis; due to sudden occlusion of major vessels; bowel becomes swollen and gangrenous and perforates in few days -Mucosal and mural infarcts: may not be fatal if cause corrected, mostly due to hypoperfusion, non-specific abdominal complaints and intermittent bloody diarrhea that may progress to infarction and sepsis -Chronic ischemia infarcts: mucosal atrophy, ulcerations, mural fibrosis, but not a medical emergency; insidious with intermittent bloody diarrhea, resembling inflammatory bowel disease Hernias= weakness in peritoneal cavity wall results in protrusion of a pouch-like, serosalined sac of peritoneum, commonly in inguinal and femoral canals, umbilicus, and areas of surgical scars -segments of viscera may protrude and become trapped, resulting in ischemia -incarceration: permanent trapping of bowel loop due to edema from impaired venous drainage -strangulation: compromised arterial supply and venous drainageinfarction -incarceration and strangulation need immediate surgery Adhesions -due to inflammation (peritonitis) from surgery, infection, radiation, and endometriosisas healing occurs, get adhesions between bowel loops, bowel wall, and surgical site -twisting around adhesions can cause strangulation and obstruction Intussusception -one segment of bowel telescopes into another, and peristalsis further wedges this segment further, resulting ins ischemia -infants—no underlying cause or can be associated with rotavirus*, usually in children -Adults—usually an intralumenal mass or neoplasm is also present Symptoms: pain, currant jelly stool, bleed Tx: barium enema to push one segment out of the other or can go away on its own Volvulus -complete twisting of a bowel loop about its mesenteric baseobstruction and infarction -most commonly in large redundant loops of sigmoid colon and small intestine Pathology of Large Intestine Blood supply (on Boards): Superior mesenteric arteryascending and proximal transverse colon Inferior mesenteric arteryremainder of colon to rectum Superior hemorrhoidal branch of inferior mesenteric arteryupper rectum Hemorrhoidal branches of iliac or internal pudendal arterylower rectum Congenital Aganglionic Megacolon: Hirschsprung Disease -absence of ganglion cells (in Auerbach’s (myenteric) and Meissner’s (submucosal) plexi)) in a portion of the intestinal tract -due to problems with neural crest cell migration or early death of ganglion cells -leads to functional obstruction (constipation) and massive intestinal dilatation proximal to the aganglionic segment -complications include enterocolitis and perforation of the colon or appendix with peritonitis -manifests in newborns as failure to pass meconium and constipation Acquired Megacolon -results from Chagas disease, obstruction by neoplasm or inflammation, and as complications of inflammatory bowel disease -Chagas disease -Pseudomembranous colitis -Inflammatory Bowel Disease (broad term for Ulcerative Colitis and Crohn Disease) Pseudomembranous colitis -Clostridium difficile -Toxins A and B cause host cell apoptosis (look for toxins/spores in stool) -usually occurs secondary to broad spectrum antibiotic use for a couple of weeksdiarrhea and dilation of colon -may occur without antibiotic therapy: after surgery or debilitating illnesses -plaque-like adhesions of fibrinopurulent-necrotic debris and mucus Idiopathic Inflammatory Bowel Disease—can cause toxic megacolon by destruction of neural plexi -collective term for Crohn Disease and Ulcerative Colitis -results from inappropriate and persistent activation of the mucosal immune system -Crohn disease (AKA terminal ileitis, regional enteritis, and granulomatous colitis): noncaseating, granulomatous (50%) and can be found from esophagus to anus, most often intestine and colon; transmural; skip lesions (segmental), granular serosa with “creeping fat” and thick wall, mesentery also thickened and edematous; “string sign” on x ray from narrowed gut lumen; early lesions are apthous ulcers in mucosacoalesce into linear ulcerscobblestones; complications include fistula formation between loops of bowel, bladder and skin, strictures, and malabsorption and protein-losing enteropathy; intermittent attacks of diarrhea, fever, and abdominal pain separated by asymptomatic weeks to months; may be caused by periods of physical and emotional stress; may have occult blood loss, leading to anemia, may have severe right lower quadrant pain; extraintestinal manifestations: migratory polyarthritis, sacroilitis, ankylosing spondylitis, erythema nodosum, primary sclerosing cholangitis, clubbing of fingers -Ulcerative Colitis: nongranulomatous, confined to colon and rectum, and superficial; continuous, slightly more common, associated with nonsmoking, particularly exsmokers; crypt abscesses lead to ulcerations that are linear and broad-based, leaving a raw, exposed muscularis propria; dysplasia noted to give rise to adenomas or invasive carcinoma; relapsing bouts of bloody, mucoid diarrhea, persisting for days, weeks or months, usually accompanied by lower abdominal pain and cramps, relieved by defecation, attacks precipitated by physical or emotional stress; complications: increased risk for carcinomas, often infiltrative w/o obvious masses, toxic megacolon and extraintestinal lesions, extraintestinal lesions: ankylosing spondylitis, primary sclerosing cholangitis, erythema nodosum, pyoderma gangrenosum -both have extraintestinal inflammatory processes associated HLA-DR2Ulcerative Colitis HLA-B27pts with IBD and ankylosing spondylitis (is a chronic, inflammatory arthritis and autoimmune disease.[1] It mainly affects joints in the spine and the sacroiliac joint in the pelvis, and can cause eventual fusion of the spine.)~wikipedia Angiodysplasia= tortuous dilations of submucosal and mucosal blood vessels in cecum or right colon, vascular degenerative changes normal distention and contraction of wall may occlude the submucosal veinsfocal dilatation (elderly); manifested as variable bleeding (some massive and severe)hematochezia (bright red blood) Chronic constipation and straining, pregnancy (venous stasis), liver cirrhosis and htnhemorrhoids Focal wall weakness + increased intralumenal pressureDiverticular disease Diets low in fiber reduce stool bulk, increase peristalsisdiverticular disease Nipple-like protrusions into lumen of colonhyperplastic polyps Benign tumors of blood vessels and mesenchymal tissue in children less than 5yoJuvenile Polyps Potentially malignant juvenile polypsautosomal dominant juvenile polyposis syndrome Multiple hamartomatous polyps of mucosa, lamina propria, and muscularis mucosa throughout GI tract + melanotic mucosal and cutaneous pigmentation around oral mucosa, lips, face, genitalia, and palmar surface of hands + risk of intussusceptionPeutz-Jeghers Syndromeincreased risk of carcinoma of pancreas, breast, lung, ovary, and uterus (polyps no malignant potential) Most common adenomas of colontubular adenomas Villous adenomas of rectum and rectosigmoidless common but precancerous, hypokalemia, big bulky cauliflower like structures, very tall villi Innumerable adenomatous polyps, autosomal dominant, mutation of adenomatous polyposis coli (APC) gene on chromosome 5, 100% progress to adenocarcinomafamilial adenomatous polyposis (FAP) Variation of FAP with osteomas of mandible, skull, and long bones, epidermal cysts, and fibromatosisGardner syndrome Turcot syndromeademonatous colonic polyposis + CNS tumors Players in Familial adenomatous polyposis: APC= a tumor suppressor gene that suppresses β-catenin β-catenin= causes cell proliferation K-RAS= proto-oncogeneif becomes oncogene, cells don’t undergo apoptosis P53tumor suppressor gene Telomerase (an enzyme that adds DNA sequence repeats ("TTAGGG" in all vertebrates) to the 3' end of DNA strands in the telomere regions, which are found at the ends of eukaryotic chromosomes. This region of repeated nucleotide called telomeres contains non-coding DNA material and prevents constant loss of important DNA from chromosome ends)~wikipedia Pathological progression of FAP: -Hit 1= mutated APC allele inherited -Hit 2= loss of normal APC allele -Hit 3= K-RAS mutation -Hit 4= loss of p53 -Hit 5= Telomerase mutation Lynch Syndrome= hereditary non-polyposis colorectal cancer due to DNA mismatch repair Adenocarcinoma= most common cancer of colon Etiology: -excess caloric intake -low unabsorbable vegetable fiber -large quantities of refined carbohydrates -red meat -decreased intake of protective micronutrients: vitamins A, C, E If >55 yo and iron-deficiency anemiathick cecal cancerneed colonoscopy Adenocarcinoma of the colon metastasizes to liver (#1 that goes to the liver) (regional lymph nodesliver, lungs and bone) Carcinoid tumor -appendix most common side, followed by small intestine, rectum, stomach, and colon -solid, yellow tan appearance -many asymptomatic, may obstruct, may be functional e.g. hyperinsulinema, Cushing Syndrome, Zollinger-Ellison Syndrome -May have carcinoid syndrome due to elevated serotonin: flushing, diarrhea, asthma -may metastaze to liver -5 year survival 90% (50% if small bowel tumor and liver mets), wide spread disease usually results in death RLQ pain, vomiting, fever, rebound tenderness in RLQ, CBC shows leukocytosis w/ left shiftacute appendicitis Obstruction by fecolithgs, gallstones, tumors or parasitesacute appendicitis Neutrophils in the muscularis of appendixacute appendicitis Mucinous cystadenocarcinomas of appendix implant peritoneummucin= pseudomyxoma peritoneii (seeding of peritoneum by mucus secreting cells from ruptured intestine or ovary) Dermatitis herpetiformisceliac sprue Osmotic diarrhealactose intolerance Malabsorption and skin hyperpigmentationWhipple Disease Lynch Syndromehereditary colon cancer non-APC, DNA mismatch repair IgA Deposits in dermal papillaedermatitis herpetiformisCeliac Disease True DiverticulumMeckel’s Divirticulum Anti-gliaden antibodyCeliac sprue Clostridium difficilePseudomembranous colitis Transmural inflammationCrohn’s Disease Steatorrheamalabsorption Crypt abscessesUlcerative colitis PAS positive macrophages in lamina propriaWhipple Disease AntibioticsC. diffpseudomembranous colitis Juvenile colon polyps + hyperpigmentation of oral mucosaPeutz-Jeghers Syndromehereditary pancreatic & ovarian carcinomas Pancreatic diseases: Epigastric pain boring to back with vomitinglook at vomitus, if has blood, think of perforation of peptic ulcer; if vomitus is biliousacute pancreatitis Boerrhavesubmediastinal pain that bores to back (not in epigastic area, a little higher) SPINK1 (serine protein inhibitor kazal 1)hereditary pancreatitis syndrome D-xylose testdistinguishes between pancreatic or intestinal causes of malabsorption: if pancreatic disease, d-xylose test will be normal, if intestinal disease, d-xylose test is abnormal (give pt known quantity and check for it in urine, if intestine is NOT diseased, will show in the urine. D-xylose absorption NOT dependent on pancreatic enzymes) Painless SEVERE obstructive jaundice (direct bilirubin >5, Alkaline phosphatase >500)extrahepatic obstructionpancreatic carcinoma of the head of the pancreas; could also have Trousseau’s signmigratory thrombophlebitis and hypercoagulability Liver tests: Transaminases (AST, ALT), when elevated mean necrosis (intracellular enzymes have leaked out of damaged cells) Level of elevation tells you about pathology If severe, in the 1000s—hepatitis (severe inflammation of liver and release of large quantities of transaminases) If mild damage, in the 100s—congestion of liver due to congestive heart failure In between is moderate—in cirrhosis of liver LDH5 elevationnecrosis of liver cells LDH1heart and red cells LDH3pulmonary infarction Bilirubindirectobstruction (intra or extrahepatic) Bilirubinindirect impaired conjugation OR hemolysis Proteins made in liver: Albumin and Coagulation factors (PT and PTT) Increased ammonia levelscomplete liver failuremusty odor antiLKM (liver, kidney, microsomes)autoimmune hepatitis hepatitis C liver morphologyfatty change fatal in pregnant womenHep E antibodies to HBsAg w/o any other antigens or Abseffective immunization Low hepcidinhemochromatosis Low ceruloplasminWilson’s Disease High alphafetoproteinHepatocellular carcinoma Oral contraceptiveshepatic adenoma Vinyl chlorideangiosarcoma of the liver Target cells on peripheral smear, microcyticcirrhosis of the liver Miscrovesicular steatosispregnancy, amiodarone, tetracycline toxicity, Reyes Syndrome High ammoniahepatic failure, hepatic encephalopathy Mallory bodiesalcoholic hepatitis DsDNA virusHepatitis B PAS positive intra1hepatic inclusionsalpha-1 anti-trypsin deficiency Metastatic liver tumorsprimary is colon Crypt abscessulcerative colitis Signet ring cellsdiffuse carcinoma of the stomach Krukenberg tumor when above mets to ovaries Upper esophageal webPlummer Vinson Syndrome Anti H+K+ ATPaseautoimmune gastritis FistulasCrohn’s Osmotic diarrhealactose intolerance GastrinomaZollinger-Ellison Syndrome (multiple ulcers and diarrhea) EBVnasopharyngeal carcinoma Budd Chiari + anemiaPNH HHHHemochromatosis, HFE, Hepcidin Colonic polyps + osteomasGardner Syndrome Juvenile colon polyps, familial ovarian cancer + hyperpigmentation of oral mucosaPeutz Jeugher AST>ALTalcoholic liver disease Vignette: a tattoo artist presents to her PCP with malaise and dark urine for 5 days. She also says she felt tired for the last 4 weeks. DD Hep B, Tests HBsAg, HBeAg (no Abs yet bc too early) Risk factorsneedles ComplicationsChronic hepatitisCirrhosisHepatocellular carcinoma (3 Cs are complications) Vignette: 15 yo male presents with difficulty concentrating and he reports that he has been falling down frequently when he climbs stairs. His right upper quadrant feels funny. DD: Wilson Disease Tests: preliminary tests: ceruloplasmin will be low, confirmatory test: copper in the liver (how much copper per gram liver weight) Vignette: 6 yo girl presents to ER with stupor & vomiting for 12 hours. She has a strep throat 5 days ago with fever. Then Mom gave her aspirin to get her fever down. Dx: Reyes Syndrome Tests: ALT = 500, ammonia elevated, blood glucose low; liver biopsy finding= microvesicular steatosis Vignette: 72 yo woman presents with diarrhea and muscle weakness for 3 months. Stool exam reveals large amounts of mucin. DD: villous adenoma of the colon; hypokalemia is cause of muscle weakness Colonoscopy Vignette: 35 yo actress presents to her PCP very concerned about severe dryness around her lips, which she cannot mask with make up. She also reports she has been very tired lately. On PE, her tongue is unusually red DD Plummer Vinson Test iron deficiency (Fe+ CBC) What to do next: endoscopy to see esophageal webs Vignette: Grandma Smith brings in little Jack (6 months). She is worried he had six loose stools in the last 24 hours. What organism: Rotavirus Vignette: 24 yo male presents with mild jaundice and a slightly enlarged liver. He reports that his uncle died at age 35 with some kind of lung disease. The patient also reports that he runs out of breath when he climbs stairs to his 4th floor apt. PE: hyperresonant chest, RR 22; labs AST and ALT are both elevated (>250); bilirubin 4, split 50/50 DD: alpha-1-antitrypsin deficiency What would you see on chest xray: emphysema On liver biopsy: PAS positive intrahepatic inclusions 32 yo male with a known history of ulcerative colitis presents with recurrent rt upper quadrant and fever and what he calls a funny color to his skin. PE: tender right upper quadrant very slight jaundice test very increased IgM (hypergammaglobulinemia)—starts as an acute inflammation, which is why IgM is increased Dx: primary sclerosing cholangitis Inflammation and fibrosis that obliterates intrahepatic and extrahepatic bile ducts. Segmental constriction of ducts gives beaded appearance to barium columns on x ray Morphology: onion skin fibrosis around the ducts= primary sclerosing cholangitis Anomalies of the biliary tree Von Meyenberg complexes Polycystic kidney disease 45 yo Norwegian lady with rt upper quadrant pain radiating to her scapula. She has been hospitalized 10 times when she had her 10 babies one year apart PE tenderness, guarding, rebound 5 Fs are risk factors: Female, fat, fertile, forty, fair Hemolytic anemias (chronic) would be associated with gall stones GI Summary Partnerships: White plaques in mouth that can be scraped offthrush White plaques in mouth that cannot be scraped offleukoplakia EBVnasopharyngeal carcinoma Chronic Hep B& hematemesisesophageal varices due to portal htn Diarrhea in babiesRotavirus Diarrhea in childrenNorwalk virus Explosive diarrheaLactose intolerancelactase (disaccharidase) Fatty diarrheamalabsorption Watery diarrheaVIPoma HypokalemiaVIPoma and Villous Adenoma HyperkalemiaDKA Onion skin fibrosis of bile ductsprimary sclerosing cholangitis HemochromatosisHFE mutation and loss of proper Hepcidin expression SPINK1 mutationsHereditary pancreatitis syndrome Clinical Lab Medicine Partnerships: A 44 yo lady presents with severe right upper quadrant pain for 2 hours (pain= 10/10). She has also had a history of chronic normocytic anemia for as long as she can remember. Dx: PNH (chronic normocytic anemia), pain is most likely Budd-Chiari (thrombosis of hepatic vein) Test: Flow Cytometry for CD55 and CD59 (cells should be negative for these) 55 yo African American lady presents with malar rash and photosensitivity for 2 weeks. She has a hx of htn for 3 years. ANA is 1:80 homogeneous pattern, low titer Dx: Drug-induced Lupus—she has hypertension, so should ask if she has been on hydrochlorothiazide; If she had autoimmune lupus, the ANA pattern would have been speckled or peripheral and the titer would have been much much higher. Homogeneous pattern is anti-histone. Tests: dsDNA—negative; skin bx—no specific changes; UA—normal A patient and tell them not to eat bananas bc we are running a certain test carcinoid tumor test (bananas increase serotonin) Abstain from onions for testthey decrease insulin response to glucose Increased gamma GTalcohol Increased osmotic fragilitycongenital spherocytosis Autosplenectomysickle cell Bite cellsG6PD deficiency Dry tapaplastic anemia, hairy cell leukemia, megaloblastic anemia Pure red cell aplasiathymoma Teardrop cells on peripheral bloodmyelofibrosis Heat stabile alkaline phosphataseliver 6 yo boy is brought to ER by grandma who was babysitting for him. He is lethargic, he is vomiting, and Grandma said he had a fever 5 days ago, and she did not have Tylenol, so she gave him baby Aspirin. Dx: Reyes Syndrome Tests: ALT (↑), Ammonia (↑), and blood glucose (hypoglycemic) 55 yo male presents with gynecomastia, slight jaundice and ascites. AST 350, ALT 150, AP 200. Dx: Alcoholic cirrhosis (AST more than double the ALT) Caffeine increases catecholamines, triglycerides, and serum gastrin and decreases cholesterol High CEAGI cancer, smoker, chronic hepatitis, chronic pancreatitis Thiazideshypokalemia and induction of SLE +ANA anti-histone (drug-induced lupus) Newbornhigh Hb, lymphocytes, bilirubin, low glucose (low glycogen reserves) CPK higher in blacks Albumin higher in whites Lipids lower in Asians Conjugated hyperbilirubinemiasRotor syndrome and Dubin-Johnson Syndrome Mutations in UGT promoter, decreased UDP glucoronyl transferase, impaired conjugation, auto recessive, usually asymptomaticGilbert Syndrome Absent UGTCrigler Najar Type Ikernicterus and death in infants Decreased UGT, managed by barbituratesCrigler Najar Type II Continue later on p.234 Dermatopathology: WhealHive (edematous erythematous dermal swelling)type I hypersensitivity reaction (IgE mediated mast cell degranulation)urticaria Granular IgG and C3 at dermal epidermal junctionSLE or Discord LE Linear IgG at the dermal epidermal junctionBullous pemphigoid IgA at Dermal PapillaeDermatitis herpetiformis (see in Celiac Sprue) Intercellular IgG in the basal layer of the epidermispemphigus vulgaris Munro abscesspsoriasisIBD Koebner phenomenonrecurrence of the lesion at the site of the original injury Elastosissenile or actinic (UV damage) Suprabasilar vesicles or bullaepemphigusintercellular IgG at the dermal-epidermal junction Subepidermal bulla at tip of dermal papillaDermatitis herpetiformisIgA at dermal papillae Aging changes: Atrophy of epidermisincreased shear force injury (senile purpura) Decreased langerhans cellsdecreased immunityincreased risk of malignancy UV radiationpyrimadine dimers in DNA of keratinocytes, proliferation of melanocytes for increased melanin (can lead to melanoma), decreased langerhan cell function (decreased immunity), abnormal elastin production (solar (actinic) elastosis) Spongiotic (eczematous or contact) dermatitisAg contacts epidermisLangerhans cell/CD4+ T cell mediatededema into epidermis, spongiosis +/- vesicles Erythema multiformehypersensitivity reaction to medication, herpes simplex virus, mycoplasma, collagen vascular diseases, lymphomas, carcinoma Erythema multiforme, skin involvement onlyHSV (usually) Erythema multiforme, skin and mucous membranes, feverSteven Johnson Syndrome (usually due to drugs) Erythema multiforme, total skin sloughage like a burn patientToxic epidermal necrolysis (TEN) (usually due to drugs) Lichen planusthought to be delayed hypersensitivity reaction resulting in damage to basal keratinocytes, acanthosis, hypergranulosis, and hyperkeratosis, vacuolar basal layer damage (hydropic degeneration), eosinophilic necrosis of keratinocytes, band-like lymphocytic infiltrate*, Koebner phenomenon*, thick purplish lesions Systemic LEskin and other organs Subacute LEskin +/- other organs Discoid LElocalized to skin Lulpus Erythematosusautoimmune rxn to basal keratinocytes (+/- organs) hydropic degeneration and eosinophilic necrosis On IGF: granular IgG and C3 along DE junctionLE In DLE: IF positive in lesional skin only In SCLE, SLE: IF positive in lesional and non-lesional skin Keratinocytes proliferate at twice the normal rate, resulting in acanthosis with elongated rete ridges and dermal papilla (look like test tubes)psoriasis vulgaris PMNs migrate into epidermis and stratum corneumMunro’s microabscessespsoriasis vulgaris White scales and Koebner phenomenonpsoriasis vulgaris IgG binds to intercellular desmoglein 3 (cadherin)intercellular IgG between spinous keratinocytesacantholysis (loss of intercellular connection)suprabasilar vesiclePemphigus vulgaris (potentially fatal due to infection) *Nikolsky sign (pressure on edge of blister causes blister to expand)Pemphigus vulgaris IgG+C3 bind to hemidesmosomes at DE junctionsubepidermal blisterlinear IgG and C3 along DE junction on IFBullous pemphigoid (usually self-limited, middle aged to elderly, at sites of friction)tensa bulla (subepidermal) filled with clear fluid, heal w/o scarring IgA to anchoring fibrils in BMgranular IgA at tips of dermal papillasubepidermal bulla at tips of dermal papillaDermatitis herpetiformis (pruritic vesicles with red base)Celiac Disease association and HLA B8 SclerodermaCD4+ T cells release cytokines and cause collagen formation and fibrosis, CD8+ T cells damage endothelium by granzyme A leading to periadventitial fibrosisAnti-Scl70 (DNA topoisomerase; specific), anti-centromere ab (more common in limited scleroderma)CREST syndrome (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) Erythema nodosumidiopathic, early there are PMNs and edema, late there are giant cells and fibrosispainful, indurated subcutaneous nodules over anterior lower legs3040 yo females, usually self-limitedassociated with Strep throat, inflammatory bowel disease, TB, fungi, drugs, sarcoidosis, malignancy Hypersensitivity vasculitis, Type II hypersensitivity reaction (immune complexes deposit in vessel walls), leukocytoclastic vasculitisdrugs, infection, collagen vascular diseases (SLE, RA, Pernicious Anemia, Wegener’s) Palpable purpuraHenoch Schoenlein (immune complex vasculitis)triad of purpura, arthritis (ankles, knees, elbows), and abdominal pain; 40% have kidney involvement (minor loss of protein and blood) Acral melanomaunder nails, palms, solesvery aggressive Breslow thickness (depth of invasion in mm)melanomamost important prognostic indicator Clark levelhistologic level of invasion Moh’s procedure (frozen sections until clear margins)Basal cell carcinoma Sezary SyndromeT cell leukemia with T cell lymphoma of the skin Mycosis fungoidesT cell lymphoma skin Pautrier abscessMycosis fungoides Proliferation and death of infected keratinocytesmolluscum contagiosum Umbilicated lesions (center is deeper than surrounding, depressed in center)molluscum contagiosum Lymphocytes with cerebriform (convoluted) nucleiSezary Syndrome Dermatomal rashshingles Abnormal elastic fiberssenile or actinic Rodent ulcer (erodes surrounding tissue)basal cell carcinoma HHV8Kaposi Sarcoma Subcorneal lesions (right under keratin) and honey-colored crustimpetigo (strep infection) Scabies (left out of handout and told to add) -Scabere= latin for “to scab” -Mitesarcoptes scabeibury into skinallergic itching -close contact transmission -linear streaks (forms tunnels in skin) -responds to landin lotion Human papilloma virus (usually types 2 and 4)incorporated in host DNApapulespapillomatous on microscopyverruca vulgaris (common wart on hands, arms, etc.) NO risk of malignant transformation (vacuoles—koilocytes— cytopathic effect) condyloma acuminatum (genital wart)HPV types 6,11 (low risk types) sometimes 16,18 (high risk types)verrucous papulesubtle cytopathic effect Infected keratinocytes undergo cell deathHerpes Virus family (Herpes Simplex Virus, Varicella Zoster, Herpes-Zoster) Cold soreHSV 1 HSV 2genital infection (painful, erythematous clustered vesicles) Dewdrops on a rose petal vesiclesVaricella Zoster Stress, immunosuppression, illness + prior infection with VZVdermatomal rashshingles Member of pox viridae that causes both proliferation and destruction (death) of keratinocytesMolluscum Contagiosum Pink, grouped papules with central umbilicationMolluscum Contagiosum Vesicles/erosions with honey-colored crust, subcorneal lesionsimpetigostaph aureus and group A streptococcus Trichophyton and Microsporumringworm Benign, exophytic, greasy verrucous papule/plaque with keratin plugsSeborrheic keratosis (may be mistaken for melanoma) Scaly, erythematous papules/plaques arising on sun-exposed areas with a sandpaper texture (due to a lot of keratin)premalignant lesion called actinic keratosis Squamous cell carcinoma in situ (Bowen’s Disease)full thickness dysplasia of keratinocytes in sun-exposed areas, especially lips, mucosal surfaces, genitalialarger erythematous, scaly plaques Cup-shaped invagination of squamous epithelium with keratin-filled center, which enlarges rapidly and can regress; may be a squamous cell carcinomakeratoacanthoma Basaloid keratinocyte nodular or nested growth (and pallisading), most common nonmelanoma skin cancer, called rodent ulcer because erodes surrounding skin, rarely metastasizesbasal cell carcinoma Moh’s surgeryused for Basal cell carcinoma: keep doing frozen sections until clear margins Keratin pearls and invasive skin cancer, keratotic nodule with dermal induration, erythematous, irregular bordersSquamous cell carcinoma Tumor like growth of granulation tissue in pregnant woman, red papule with or w/o ulcerationPyogenic granuloma Kaposi’s sarcoma two types: acral sites (classic) in elderly (lower limbs due to venous stasis) or widespread HIV-associated hemorrhagic patches or plaques due to HHV-8 virus Growth of spindled peripheral nerve fibers in fascicles (whorls), café-au-lait spots, associated with MEN2b syndromeNeurofibroma (benign) Von Recklinghausen’s syndrome= malignant transformation of of neurofibroma T-cell lymphoma (aka mycosis fungoides)= most common presentation of NonHodgkin’s lymphoma of the skin=itchy, red, scaly raised plugs (may be mistaken for eczema) Sezary Syndrome= T-cell lymphoma of a large amount of skin + leukemic phase (more serious than just skin) Pautrier microabscess= small aggregate of malignant lymphocytes in skinT-cell lymphoma (Mycosis fungoides) Lymphocytes with cerebriform nuclei on peripheral blood smearSezary Syndrome Increased melanocytes in linear pattern along basal layerlentigodark brown macule Nests of melanocytes at DE junction, at tips of rete ridgesjunctional nevusdark brown macule Compound nevusnests of melanocytes in both epidermis and dermisdark brown to tan papule Intradermal nevusnests of melanocytes in the dermistan to flesh-colored papule ABCD of premalignant tumors: Asymmetry Border Irregularity Color variability Diameter > or = 6mm Dysplastic nevusatypical nevusClark’s nevus *familial type results in hundreds of lesions with high risk for melanomajunctional or compound melanocyte distribution Risk factors for malignant melanoma in situ= fair complexion, severe childhood sunburns, history of dysplastic nevi, history of melanoma in primary relative Atypical melanocytes proliferating within the epidermismalignant melanoma in situ (appears a little darker than dysplastic nevi and looks nodular) Lentigo maligna melanomaface of elderly Superficial spreading melanomasun-exposed areas, radial growth, then vertical growth Nodular melanomamore aggressive melanoma and invades deep Acral lentiginous melanomaacral sites, often deep at time of dx, non-sun-exposed areas such as fingers, palms, soles, under nailsaggressive Acanthosis Nigricans (black discoloration in axilla, neck, groin)Type I (rapidly progressing sudden onset on face, palms, trunk) GI malignancy, Type II (not associated with malignancy, family auto dominant), Type III (most common, slow onset)obesity, type II diabetes (check fasting blood sugar and will be high) Erythema chronicum migransLyme Disease Necrobiosis Lipoidica= yellow plaques, atrophic centers, on shinsDiabetes Mellitus Eruptive Xanthomas= yellow papules on extensor surfacesDiabetes Mellituscheck fasting blood sugar and serum triglycerides Granuloma Annulare= annular plaque on dorsal hands or feetDiabetes Mellituscheck fasting blood sugar and KOH (to rule out tinea) Xanthelasma= yellow plaques on eyelidsHyperlipidemia (order lipid profile) Psoriasis=well demarcated erythematous plaques with silver scales on elbows, knees, buttocksHyperlipidemia (check lipid profile, CAD risk factors) Systemic LupusErythematous plaques, bilateral cheeksANA, Anti-ro/la, AntidsDNA, Anti-smooth muscle Pagets Diseaseerythematous patch/plaque breastmammogram, ultrasound, MRI Erythema Nodosum= tender nodules, erythematous nodules on anterior shinsdo strep culture/ASO, CXR (Sarcoidosis), Stool cultures, Colonoscopy (Crohn’s/UC), Medication History (OCP) Chronic Urticaria do CBC (increased WBC, viral), ANA (lupus), TSH, CXR (lymphoma), UA