word document
advertisement

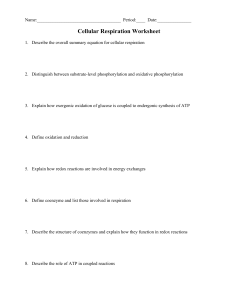
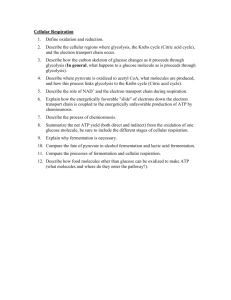
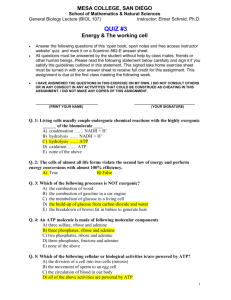
Biochemistry I *1: GenChem Review/Carbs *2: Diabetes Mellitus *3: Glycolysis *4: PDH pathway *5: TCA/Kreb’s *6: ETC Overview Outline & Notes --Midterm— *7: cytochrome p450 *8: HMP pathway *9: Cancer & Metabolism *10: Fructose Metabolism *11: Galactose Metabolism *12: Mannose Metabolism *13: Gluconeogenesis *14: Glycogenesis *15: Glycogenolysis *16: Glycosaminoglycans (GAGs) *17: Lipid Overview Enzyme Tips and Definitions: The suffix -ase is used in biochemistry to form names of enzymes. The most common way to name enzymes is to add this suffix onto the end of the substrate. Sometimes enzymes are named for the function they perform, rather than substrate. Dehydrogenase – removal of H20 (aka dehydration) Transaminase – Transfer of amino group to form Usually involved w/ NADH/NADPH alpha keto or amino form of the molecule. Usually requires pyridoxial phosphate (vit B6) Hydrogenase – add water (hydration) Synthase – makes something w/o using ATP Kinase –phosphorylates, usually ATP involved Lyase – breaks something to make double bonds Isomerase – a changing isomer Phosphorylase – Adds a Phosphate group. Involved Mutase – moving R group to another carbon. in conversion of glycogen to P + glucose Decarboxylase – removal of CO2. Carboxylase – Adding CO2; usually involves Biotin and Bicarbonate. o Those with McArdle's disease (a deficiency in phosphorylase or phosphofructokinase) have an impaired ability to utilize intramuscular glycogen as an energy substrate. Phosphatase –removes a Phosphate Group Co-enzyme/ Co-factor tips and hints: Co-enzyme – o A nonproteinaceous organic substance that usually contains a vitamin or mineral and combines with a specific protein, the apoenzyme, to form an active enzyme system. ATP – Adenosine triphosphate, o The energy “currency” of the cell. It translates low energy bonds (from food/nutrients) to high energy bonds. o Dephosphorylation liberates the energy from the ATP molecule and fuels biochemical rxns. o Whenever you see ATP, you know that you need Magnesium as well. ADP - Adenosine diphosphate o Gets recycled in the mitochondria where it is phosphorylated (“recharged”) and becomes ATP. o It is involved as a nucleotide (DNA/RNA production) and plays a role as a co-enzyme. NAD/NADH- (or NADP/NADPH) - Nicotinamide Adenine Dinucleotide o NADH is the reduced coenzyme form of vitamin B3 (niacin), while NAD is the oxidized form. Biochemistry I Guide Page 1 o o o o o NAD and NADH serve to activate various enzymes, NAD for example, activates alcohol dehydrogenase and acetaldehyde dehydrogenase which detoxify the alcohol into CO2 and H2O NADH is the first of five enzyme complexes of the electron transport chain and is involved in glycolysis and Krebs’ cycle. Each unit of NADH is capable of generating three units of ATP energy. Can be made from L-Tryptophan at the "expensive" ratio of 60mg tryptophan for 1mg B3. Taking in exogenous (from outside the body) B3 may spare the scarce amino acid tryptophan, which is the least plentiful amino in any normal diet. Tryptophan is the precursor of one of the most important antidepressant neurotransmitters, serotonin. FAD/FADH2- flavin adenine dinucleotide o FADH and FADH2 are reduced forms of FAD. FADH2 is produced in the citric acid cycle. In oxidative phosphorylation, two molecules of FADH2 typically yield 2.5 ATP. o Riboflavin is the OTC form of FAD/FADH2 *1: General Chemistry Review and Carbohydrates Learn the following general chemistry terms: *Anion , Cation, Mono, di, trivalent, R, S : chirality, Reduction, and Oxidation *Anabolism – creation of molecules by increasing number of carbons, carbon fixation *Catabolism – breakdown of molecules for the release of energy (we are net catabolic at ~30% efficiency) *Mn++ is involved in gluconeogenesis (deficiency = hypoglycemia) *Ca++ is involved in phosphorylation and at the neuromuscular junction *Ferrous (Fe++) is oxidized to Ferric (Fe+++) while Cu++ is reduced to Cu+ (a vitamin C dependent reaction) so that Transferrin transports iron out to the organs where it is reconverted and stored as Fe++ *Hemochromatosis- overstorage of iron so that it puts tissues at risk for oxidation. Allopathic treatment involves decreasing Vitamin C consumption. Yet, Vitamin C not only helps with oxidative stress occurring in the body but is also necessary for countless other vital processes. Better to decrease iron consumption. *F- : TOXIC. Binds to Mg++ (important for ADP) *HCO3-: bicarbonate ion: increases acidic conditions (important for junction b/w stomach + intestines) *HClO-: hypochlorite helps us cleave bacteria so we can present them to T-cells *NO3-, NO2-: Nitrates and Nitrites are not metabolic, can deteriorate lining of gut *Relationships in Pousilles Law Diameter is indirect to pressure and directly proportional with flow. As diameter decreases (r4), pressure increases dramatically, flow decreases *PH: physiological ph about 7. *Acid vs Base (below or over 7): Acid: proton donor, Base: Proton acceptor (More N more basic) *Covalent – sharing e- between 2 atoms. STRONG. (ex: disulfide bonds, peptide bonds) *Ionic - a chemical bond in which electrons are transferred from one atom (eg, sodium) to another (eg, chlorine) so that one bears a positive and the other a negative charge, the attraction between these opposite charges forming the bond. *VanDerWaals Forces: instantaneous dipole moment. Attractive force. *Hydrogen – between H and O. Weak. Allows for solubility property of water. *Crystal – arrangement of atoms *Exogonic – heat given off (energy releasing) *Endogonic – heat or energy requiring. Biochemistry I Guide Page 2 *Major functional groups – need to memorize A. Hydroxyl R-OH G. Methyl –CH3 B. Amino R-NH2 H. Phosphate –PO4 C. Carboxyl R-CO-OH I. Sulfhydryl -SH D. Carbonyl (any C=O) J. Alkyl E. Ketone R2-CO K. Alkene R=R F. Aldehyde R-CO-H L. Aromatic M. N. O. P. Q. R. Ester R-CO-O-R Amide R-CO-NR2 Disulfide R-S-S-R Hydroxy acid Keto acid Dicarboxylic *L, D isomers: L is active form of amino acids and D is better form for sugars *Geometric isomers are cis or trans (fatty acids are usually cis) *Organelles and functionality (major) Plasma Membrane, nucleus, nucleolus, nuclear membrane, RER, SER, MTOC (microtubule organizing center or (centrioles), Mitochondria, Cytosol (cytoplasm), Cytoplasm, Golgi Body, Vesicles, Lysosome, Microsome (involved in glycogen metabolism, involved in steroidal metabolism), Chloroplasts , cell wall, starch granules Carbohydrate Metabolism Introduction: Carbohydrates made up of carbon, hydrogen, and oxygen atoms are classified as mono-, di-, and polysaccharides, depending on the number of sugar units they contain. The monosaccharides—glucose, galactose, and fructose (and mannose)—obtained from the digestion of food are transported from the intestinal mucosa via the portal vein to the liver. They may be utilized directly for energy by all tissues; temporarily stored as glycogen in the liver or in muscle; or converted to fat, amino acids, and other biological compounds. The entry of glucose into most tissues is dependent upon the presence of the hormone insulin. Insulin controls the uptake and metabolism of glucose in these cells and plays a major role in regulating the blood glucose concentration. The reactions of carbohydrate metabolism cannot take place without the presence of the B vitamins, which function as coenzymes. Ca++, Cd++ and Zn++ are key to glucose absorption; Na+ is necessary with transport of glucose; and Mg++ is necessary for ATP>ADP in glycolysis. (phosphorous, iron, copper, and chromium are also important). Carbohydrate metabolism begins with glycolysis, which releases energy from glucose or glycogen to form two molecules of pyruvate, which enter the Krebs cycle (or citric acid cycle), an oxygen-requiring process, through which they are completely oxidized. Before the Krebs cycle can begin, pyruvate loses a carbon dioxide group to form acetyl coenzyme A (acetyl-CoA). This reaction is irreversible and has important metabolic consequences. The conversion of pyruvate to acetyl-CoA requires the B vitamins. The hydrogen in carbohydrate is carried to the electron transport chain, where the energy is conserved in ATP molecules. Complete metabolism of one molecule of glucose yields 38 molecules of ATP. The energy released from ATP through hydrolysis (a chemical reaction with water) can then be used for biological work. Under anaerobic conditions, lactate is formed from pyruvate. This reaction is important in the muscle when energy demands exceed oxygen supply. Glycolysis occurs in the cytosol of a cell and has a dual role. It degrades monosaccharides to generate energy, and it provides glycerol for triglyceride synthesis. The Krebs cycle and the electron transport chain occur in the mitochondria. Most of the energy derived from carbohydrate, protein, and fat is produced via the Krebs cycle and the electron transport system. Biochemistry I Guide Page 3 Only a few cells, such as liver and kidney cells, can produce their own glucose from amino acids, and only liver and muscle cells store glucose in the form of glycogen. Glycogenesis is the conversion of excess glucose to glycogen. Glycogenolysis is the conversion of glycogen to glucose (which could occur several hours after a meal or overnight) in the liver or, in the absence of glucose-6-phosphate in the muscle, to lactate. Gluconeogenesis is the formation of glucose from noncarbohydrate sources, such as certain amino acids and the glycerol fraction of fats when carbohydrate intake is limited. Liver is the main site for gluconeogenesis, except during starvation, when the kidney becomes important in the process. Disorders of carbohydrate metabolism include diabetes mellitus, lactose intolerance, and galactosemia. Monosaccharides Three common sugars share the same molecular formula: C6H12O6. (6 carbons = hexose; 5 C = pentose) Although all three share the same molecular formula (C6H12O6), the arrangement of atoms differs in each case. Substances such as these three are known as structural isomers. Three common disaccharides: sucrose — common table sugar = glucose + fructose lactose — major sugar in milk = glucose + galactose maltose — product of starch digestion = glucose + glucose The two monosaccharides are bonded via a dehydration reaction (also called a condensation reaction or dehydration synthesis) that leads to the loss of a molecule of water and formation of a glycosidic bond. The glycosidic bond can be formed between any hydroxyl groups on the component monosaccharide. So, even if both component sugars are the same (e.g., glucose), different bond combinations and stereochemistry (alpha- or beta-) result in disaccharides that are diastereoisomers with different chemical and physical properties. All sugars are very soluble in water because of their many hydroxyl groups. Although not as concentrated a fuel as fats (9 kcal/gram), sugars are the most important source of energy for many cells providing the bulk of the calories (4 kcal/gram) in most diets, and starches provide the bulk of that. Disaccharide Unit 1 Unit 2 Bond Disaccharidase Sucrose (table sugar, cane sugar or beet sugar) glucose fructose Α(1→2) sucrase Lactose (milk sugar) galactose glucose Β(1→4) lactase Maltose (malt grain) glucose glucose Α(1→4) maltase Biochemistry I Guide Page 4 Maltose, the form of sugar found in malted grain, is really a disaccharide with an alpha-1,4-gylcosidic bond between carbons 1 (the anomeric carbon) and 4 of two Dglucopyranose molecules (D-glucose in the cyclic form). Lactose has a beta-1,4 glycosidic bond between carbon 1 of D-galactopyranose (D-galactose) and carbon 4 of D-glucopyranose (D-glucose). Individuals who are lactose intolerant lack the digestive enzyme required to break this specific glycosidic bond. Bacteria in the digestive system use lactose as a food source, leading to the symptoms of lactose intollerant people. Treat by ingesting some of the enzyme prior to lactose. Sucrose, table sugar, is not pure glucose, but rather a disaccharide with an alpha-1,2 glycosidic bond between carbon 1 of D-glucopyranose (D-glucose) and carbon 2 of D-fructofuranose (D-fructose). In an animal's body, the glycosidic bond of sucrose is broken, and the D-fructose is converted into Dglucose and used to supply a quick source of energy. Polysaccharides Starch The glycosidic bonds in starch are alpha-1,4 linkages. There are two types of starch: amylose and amylopectin. Amylose consists of glucose rings hooked together using alpha-1,4 linkages making hundreds of glucose rings hooked together in this way. Cellulose The glycosidic bonds in cellulose are referred to as being beta-1,4 linkages because the 1-oxygen is in the beta position. Cellulose is also not a reducing sugar and; therefore, cannot be digested (in humans). Glycogen Glycogen is the polysaccharide that is used by animals for storing glucose for future use. Like amylopectin, it also consists of a-1,4 linkages and a-1,6 branches. One of the functions of having many branches in the molecule is that it gives a lot more ends for enzymes to work on to hydrolyze the glycogen to form glucose. Thus, glucose can be released much more quickly than if there was just one end for the enzymes to work on. Digestion of Carbohydrates Mouth: o Salivary alpha amylase cleaves starch to disaccharides and oligosaccharides Cleaves the alpha-1,4 linkages b/t glucose residues yielding “dextrin” fragments Intestine: o Pancreatic alpha amylase continues glucose cleavage in the duodenum o Maltase (a1,4) and isomaltase (a1,6) on brush border of intestinal epithelium complete the conversion of starch to glucose o Sucrase: Converts sucrose to fructose and glucose o Lactase: Converts lactose to glucose and galactose by breaking beta 1,4 linkage Biochemistry I Guide Page 5 o Cellulase: a beta galactisidase that breaks beta (1,4) linkages between glucose; not in humans *2 Diabetes Mellitus Structure of Insulin Polypeptide hormone with 51 amino acids in two polypeptide chains linked by two disulfide bridges Synthesis of Insulin and Biphasic Insulin Secretion (beta cells of pancreas) (Prior to glucose arriving) Phase 1 (cephalic phase) insulin response, which lasts for ~10 min, is initiated by sight and smell of food when a lot of preformed insulin releases. This “preps” the body for glucose. The secondary, smaller rise in insulin reflects the considerable amount of newly synthesized insulin that is released immediately into circulation. This second phase is initiated by glucose entering the bloodstream via absorption by the enterocytes’ GLUT receptors or co-transportation with sodium. Glucose travels to the pancreas and stimulates the Beta cells - turning on the gene for insulin production: PREPROINSULIN. After transcription and translation, PROINSULIN is formed and secondary folding occurs by the formation of 2 disulfide bonds. Proinsulin is than cleaved to form a short and long strand of INSULIN. During cleavage, a C-peptide is formed and gets released into the blood stream along with insulin. This secondary response is slower in pseudodiabetics, leading to temporary hyperglycemia and potentially dizziness if the meal is not prolonged (shown by the glucose tolerance test). Diabetes Mellitus Overview (page 345 of Lippincott’s) Diabetes is a condition that results in hyperglycemia, and in many cases, hyperinsulemia Type 1: Insulin dependant; Does not produce insulin due to autoimmune attack on beta-cells long-term develops glucagon deficiency; making epinephrine the primary gluconeogenesis stimulant DDx test; c peptide. o If insulin is being made, there will be c peptide floating around in blood. Type 2 (NIDDM): Used to be considered “adult onset” and risks factors were age and obesity. Predisposition on chromosomes 1 and 4 Cause is thought to be a systemic infection, vasculitis, stemming from a poor diet, rich in “bad” fats o vasculitis causes a constant state of inflammation Brittle Diabetes: when glucose goes up and down, uncontrollably. Brought on by constant up and down of glucose cycle when insulin shots are involved because the excess glucose is converted to sorbitol. The eastern thought is to maintain high glucose levels if unable to permanently lower levels. 3 Tests for the degree of diabetes mellitus (both types) 1. Fasting Glucose a. Check glucose levels after fasting (>130 mg/dl) to give a daily “snapshot” 2. Fructosamine a. Urine or blood test that gives approximation of levels every 6 weeks. 3. Hb alpha 1c (glycosilated hemoglobin) a. Gives the long term look, done every 6 months b. Mechanism: glucose is sticky! When glucose is high, it begins to stick to protein (like Hb).1 c. The more heavy Hb alpha 1c present, the longer since onset. Hb-a-1c levels should drop under successful treatment. Glucose (and heavy metals) can also stick to and inhibit metallothianines needed for proliferation of B cells, thereby disengaging the immune system even in the presence of a normal B cell level. 1 Biochemistry I Guide Page 6 Why diabetes is a problem (particularly for type II) In a normally functioning cell In response to an elevation in blood glucose, insulin is secreted into the blood by the Beta cells. Insulin binds to its receptor on the cell surface and acts as a “doorman” for letting glucose into the cell. Glucose enters erythrocytes via GLUT 1 receptors (GLUT 4=skeletal muscles and adipose tissue). In the absence of insulin, GLUT1 glucose transporters are present in cytoplasmic vesicles, where they are useless for transporting glucose. Binding of insulin to receptors on such cells leads rapidly to fusion of those vesicles with the plasma membrane and insertion of the glucose transporters, thereby giving the cell an ability to efficiently take up glucose. When blood levels of insulin decrease and insulin receptors are no longer occupied, the glucose transporters are recycled back into the cytoplasm. Insulin opens the “door” to the cell and glucose (along with Na+ as a symport) rushes into the cell (and therefore out of the blood). Due to the lowering of glucose in the blood, glucagon levels rise and insulin leaves its receptor. Glucose’s cellular entry diminishes and glucose levels stabilize in blood. In Diabetes; In diabetes, there is an excessive amount of glucose in the blood, which in turn stimulates the production of excess insulin. Over time, the Beta Cells of the Pancreas cannot keep up with the demand and production goes down. Eventually the cells can stop producing insulin altogether. Insulin is that it is pro inflammatory. This can become a problem because insulin cannot remain in the blood too long without causing an inflammatory response. When insulin remains in the bloodstream for too long it begins to stimulate an immune response and can lead to the following: o Insulin begins to modify the surface protein receptor (GLUT 4) or its sensitivity and the body does not recognize/respond to insulin’s presence. o Antibodies develop and receptors become inflamed. o Glucose has an even more difficult time entering the cell due to these malformed receptors. Once the inflammation reaches a certain point, TNF alpha (tumor necrosis factor) blocks the insulin receptors in attempt to protect the body from this inflammation. This INSULIN RESISTANCE results in hyperglycemia and hyperinsulemia. The situation would be further exacerbated by insulin injections causing further hyperinsulemia and, thereby, weight gain as well as hypercholesterolemia and possibly atherosclerosis from arterial glucose deposits. Properties of Insulin Made in Beta cells of pancreas Pro-inflammatory *** (Counter by Tx: Olimeric Proanthocyanide(?)) Secretion stimulated by: o Glucose, amino acid arginine, GI hormone secretin Secretion inhibited by: o low glucose levels In the liver: o ↓ production of glucose by inhibiting gluconeogenesis / glycogenolysis o ↑ synthesis of glycogen In the muscles: o ↑ glucose uptake o ↑ synthesis of glycogen In the adipose tissue Excess glucose has a fat-sparing effect: o Stimulates production of triglycerides o Stimulates enzyme for cholesterol production Biochemistry I Guide Page 7 o Stimulates Fatty Acid Synthesis Has a plasma half-life ~6 minutes, is degraded in liver (primarily) Properties of Glucagon A polypeptide hormone made in the alpha cells of the pancreas under the control of amylin o amylin is directly proportional to/made with insulin and inhibits glucagon Opposes insulin by preventing hypoglycemia (making glucagon a hyperglycemic action) Secretion stimulated by: o Low blood glucose, High insulin levels Secretion inhibited by: o Elevated blood glucose Activates hepatic glycogenolysis and gluconeogenesis Does not directly stimulate muscle tissue, but epinephrine does and has the same effect Favors hepatic oxidation of FAs and the formation of ketone bodies Increases uptake of amino acids by the liver causes a ↓ in plasma levels of AAs. Properties of Somatostatin Produced in delta cell of pancreas (among other places) Inhibits production of both insulin and glucagon It’s the “guard dog” – levels blood between insulin and glucagon. o Can be hypo or hyperinsulinic Amino Acid 37 (37aa) produced by gamma cells of pancreas induces feeling of satiety Sorbitol Alcohol Unmetabolized glucose is converted into the alcohol Sorbitol in cells not requiring insulin o Enzyme: Aldose Reductase Causes cellular expansion-contraction due to influx-outflux of H20 and alcohol, possibly leading to apoptosis. This apoptosis combined with the necrosis brought on by hyperglycemia permits: o peripheral neuropathy, renal failure, blindness The liver, ovaries and seminal vesicles aren’t as susceptible b/c they have sorbitol dehydrogenase, which transforms sorbitol into fructose Naturopathic treatment o Quercitin Acetate (onion): Blocks aldose reductase Ethanol inhibits the absorption of thiamine in the intestine o Thiamine deficiency causes hypoglycemia (Due to inhibited gluconeogenesis) o Thiamine is responsible for helping liver make glucose. Therefore: liver Pyruvate levels drop Inhibits lactate dehydrogenase Alcohol is oxidized by alcohol dehydrogenase (ADH) to acetaldehyde (destroying liver cells and causing a hangover) which is then oxidized to acetate by acetaldehyde dehydrogenase (AcDH). Both of these products are toxic and a side-effect of their reactions is the reduction of NAD+ to NADH, which results in a cellular imbalance of NAD+/NADH thereby disrupting glycolysis and causing an increase in hepatic lactate production. Biochemistry I Guide Page 8 *3: GLYCOLYSIS: Greek -glykos = "sweet" + "splitting" Oxidation of glucose is known as glycolysis. Glucose is oxidized to either lactate or pyruvate in the cytosol of the cell. Under aerobic conditions, the dominant product in most tissues is pyruvate and the pathway is known as aerobic glycolysis. When oxygen is depleted, as for instance during prolonged vigorous exercise, the dominant glycolytic product in many tissues is lactate and the process is known as anaerobic glycolysis. Glucose + 2 ADP + 2 NAD+ + 2 Pi -----> 2 Pyruvate + 2 ATP + 2 NADH + 2 H+ Niacin is the only vitamin required for glycolsyis as the NADH generated during glycolysis is used to fuel mitochondrial ATP synthesis via oxidative phosphorylation, producing either two or three equivalents of ATP depending upon whether the glycerol phosphate shuttle or the malate-aspartate shuttle is used to transport the electrons from cytoplasmic NADH into the mitochondria. The net yield from the oxidation of 1 mole of glucose to 2 moles of pyruvate is, therefore, either 6 or 8 moles of ATP. Complete oxidation of the 2 moles of pyruvate, through the TCA cycle, yields an additional 30 moles of ATP; the total yield, therefore being either 36 or 38 moles of ATP from the complete oxidation of 1 mole of glucose to CO2 and H2O. Step 1: The Phosphorylation of Glucose ATPADP + P Mg2+ Glucose --------------------------------------- Glucose-6-phosphate (G-6-P) Hexokinase / Glucokinase (in Liver) Note: Fl- toxicities **IRREVERSIBLE RXN The phosphorylation accomplishes two goals: First, the hexokinase reaction converts nonionic glucose into an anion that is trapped in the cell, since cells lack transport systems for phosphorylated sugars. Second, the otherwise biologically inert glucose becomes activated into a form capable of being further metabolized. Four mammalian isozymes of hexokinase are known (Types I - IV), with the Type IV isozyme being glucokinase. Glucokinase is the form of the enzyme found in hepatocytes (liver) and kidney cells. The high Km of glucokinase for glucose means that this enzyme is saturated only at very high concentrations of substrate (like after a meal). This feature helps regulate glucose use among high energy tissue cells (brain, muscles) and low energy tissue cells (liver, kidney) so that both function efficiently. Under various conditions of glucose deficiency, the liver performs gluconeogenesis. The levels of glucose produced during gluconeogenesis are insufficient to activate glucokinase, allowing the glucose to pass into the blood and sustain life. The regulation of hexokinase and glucokinase activities is also different. Hexokinases I, II, and III are allosterically inhibited by glycolysis step 1 product (G6P) accumulation, whereas glucokinases are not. The latter further insures liver accumulation of glucose stores during times of glucose excess, while favoring peripheral glucose utilization when glucose is required to supply energy to peripheral tissues. Michaelis-Menten Equation: Km= [S] where Vmax/2 determines enzyme affinity of isoenzymes Notes: 1. Km – derived under “ideal” conditions Biochemistry I Guide Page 9 2. Higher the Km = lower the affinity for substrate 3. Lower the Km = higher the affinity for substrate o takes less substrate for velocity to reach ½ max 4. Substrate must be the same for both enzymes or cannot compare the Km values Step 2: Isomerization of Glucose-6-Phosphate Glucose-6-Phosphate ----------------------------Fructose-6-Phosphate Phosphoglucose Isomerase Step 3: Phosphorylation of Fructose-6-Phosphate ATPADP + P Mg2+ Fructose-6-p -------------------------------- Fructose 1,6-bisphosphate Phosphofructokinase I (PFK-1) Note: Fl- toxicities ***RATE LIMITING STEP/ **IRREVERSIBLE RXN This reaction is not readily reversible because of its large positive free energy in the reverse direction. Nevertheless, fructose units readily flow in the reverse (gluconeogenic) direction because of the ubiquitous presence of the hydrolytic enzyme, fructose-1,6-bisphosphatase (F-1,6-BPase). The presence of these two enzymes in the same cell compartment provides an example of a metabolically futile cycle, which if unregulated would rapidly deplete cell energy stores. The activity of these two enzymes is so highly regulated that PFK-1 is considered to be the rate-limiting enzyme of glycolysis and F-1,6-BPase is considered to be the rate-limiting enzyme in gluconeogenesis. PFK-1 is inhibited by ↑ levels of ATP, which act as an “energy-rich” signal indicating an abundance of high energy compounds. ↑ levels of Citrate (an intermediary of the TCA cycle) also inhibits PFK-1. PFK-1 is activated by high concentration of AMP, which signals that the cell’s energy stores are depleted; it is activated by Fructose 2,6-bisphosphate. This compound (F-2,6-BP) also acts as an inhibitor of the enzyme Fructose 1,6-bisphosphatase ensuring that both pathways are not fully active at the same time. Biochemistry I Guide Page 10 Step 4: Cleavage of Fructose 1,6 –bisphosphate Fructose 1,6-bisphosphate--------------- PGAL + DHAP Adolase A Note: PGAL Triphosphate isomerase DHAP * interconversion occurs; but must have PGAL to continue down the glycolytic pathway Two 3-carbon products: dihydroxyacetone phosphate (DHAP) and glyceraldehyde 3-phosphate (PGAL/ or G3P). DHAP also functions as the 3-carbon backbone for fatty acids when cellular energy levels are high. The adolase reaction proceeds readily in both directions; utilized for both glycolysis and gluconeogenesis. Step 5: Oxidation of PGAL (Beginning of the Energy-Yielding Phase) NAD+ NADH (2) PGAL+ 2pi -------------------------------- (2) 1,3-bisphosphoglycerate d Arsenate toxicities PGAL dehydrogenase Vit: Niacin (2% NAD+ from tryptophan) This reaction is reversible, and the same enzyme catalyzes the reverse reaction during gluconeogenesis. The arsenate (pentevalent arsenic) prevents net ATP and NADH production by glycolysis by competing with inorganic phosphate (Pi) as a substrate for PGAL dehydrogenase , forming a complex that spontaneously hydrolyzes to form 1-arcino-3-phosphoglycerate which phosphoglycerate kinase cannot recognize > stops glycolysis at 6. Step 6: Synthesis of 3-Phosphoglycerate producing ATP (2) ADP + P (2) ATP (2) 1,3-bisphosphoglyecerate -------------------- (2) 3-phosphoglycerate Arsenate toxicities Phosphoglycerate kinase *Erythrocyte Pathway The high-energy phosphate of 1,3-BPG is used to form ATP from ADP and 3-phosphoglycerate (3PG). Note that this is the only reaction of glycolysis or gluconeogenesis that involves ATP and yet is reversible under normal cell conditions. Because 2 molecules of 1,3-BPG are formed from each glucose molecule, this kinase rxn replaces the 2 ATP molecules consumed by earlier formation of G-6-P and F-1,6 –BP. This is an example of substrate-level phosphorylation. FYI: Erythrocyte Shunt Associated with the phosphoglycerate kinase pathway is an important reaction of erythrocytes. The 2,3BPG shunt operates with the net expenditure of 1 equivalent of ATP per triose passed through the shunt (i.e. no ATP is generated by the shunt, so the net ATP produced in erythrocytes equals 6). The process is not reversible under normal physiological conditions. o o o Erythrocytes (RBCs) have no mitochondria Hemolytic Anemia – first effect of Mg2+ deficiencies (differentiate w/ Flpoisoning) RBCs require glycolytic pathway as it is the only Biochemistry I Guide Page 11 o source of ATP Hemolytic Anemia of the Newborn (HAN) aka Erythroblastosis fetalis aka RH incompatibility: can be so severe that the blood pressure drops enough for the child to succumb to shock Why does this occur? Oxygen needs to be released from erythrocytes so it can be picked up by body tissues. If oxygen is released from hemoglobin and not immediately picked up it could re-bind to hemoglobin. The erythrocyte overcomes this problem with 2,3 bisphosphoglycerate. This molecule has a very similar structure that can temporarily bind to hemoglobin and lower the affinity for oxygen in exchange for diminished ATP production. Step 7: Shift of Phosphate group form the Carbon 3 to Carbon 2 position (2) 3-phosphoglycerate ------------------------- (2) phosphoglycerate Phosphoglycero mutase Step 8: Dehydration of 2PG (2) phosphoglycerate --------- (2) phosphoenol pyruvate (PEP) Enolase Note: Fl- toxicities (other halides, too) The dehydration of 2PG by enolase redistributes the energy within the 2-PG molecule, resulting in the formation of PEP, which contains a high-energy enol phosphate. The rxn is still reversible. Step 9: Formation of Pyruvate producing ATP (2) ADP + P (2) ATP (2) PEP ------------------------ (2) pyruvate Pyruvate kinase **IRREVERSIBLE RXN. The final reaction of aerobic glycolysis is catalyzed by the highly regulated enzyme pyruvate kinase (PK). In this strongly exergonic reaction, the high-energy phosphate of PEP is conserved as ATP. This is another example of substrate-level phosphorylation. Energy Yield from Glycolysis: Calculations per 1 mole of glucose Gross: 10 ATP produced Net : 8 ATP produced Controls: Stimulators of Glycolysis: 1. High I:G ratio 2. High AMP and ADP levels 3. Low Citrate levels Biochemistry I Guide Inhibitors of Glycolysis 1. Low I:G ratio 2. High ATP levels Page 12 Fate of Pyruvate: Conversion to Lactate: Anaerobic Metabolism The end product of glycolysis is pyruvate. If oxygen is limited or absent pyruvate is reduced to lactic acid using NADH which was produced during glycolysis. This is a reversible reaction. * Niacin (Vit B3) is required for this rxn. Calculations per round of anaerobic glycolysis: Net 8 ATP per mole of glucose for glycolysis - 6 ATP (-3 per/NADH) per Lactate formation (Remember 2 pyruvate) Net: 2 ATP If you do vigorous exercises then the body’s demand for ATP is very high. The lack of oxygen results in a cellular paucity of oxidized NAD+. In order to regenerate NAD+, the enzyme lactate dehydrogenase converts pyruvate to lactate while oxidizing NADH to NAD+. Oxygen can not be carried fast enough into the muscle cells to oxidize all the pyruvate, so some of it is converted to lactate or lactic acid. This is cause for sore muscles. Excessive lactic acid production can lead to lactic acidosis. Lactate may diffuse out of the cell and pass to the liver where it is transformed into glucose; glucose is then capable of passing back to peripheral cells in order to re-enter glycolysis. This process is the Cori cycle. Conversion to Acetyl CoA: Aerobic Metabolism If oxygen is present then pyruvate becomes Acetyl CoA via the enzyme pyruvate dehydrogenase. Pyruvate enters the mitochondria where it is converted to Acetyl CoA which enters another pathway called the TCA cycle. Conversion to Oxaloacetate (OAA): Pyruvate can be converted to OAA by pyruvate carboxylase, an enzyme found in tissues such as the liver and brain; but not in the muscle. This reaction serves to replenish the intermediates in the TCA cycle. Conversion to Alanine: In muscle cells, pyruvate may be transanimated to form the alpha-keto amino acid Alanine by AlanineLactate-Transaminase (ALT). This reaction requires Vit. B6 (pyridoxine). Alanine and Lactate go out into the blood, travel to the liver, and if energy is needed, will be converted back to glucose via gluconeogenesis. Regulatory Enzymes of Glycolysis: The Kinase Enzymes The names given to kinases shows the substrate which is phosphorylated by the enzyme. For example: Hexokinase - an enzyme that uses ATP to phosphorylate hexoses. Protein kinase - enzymes that use ATP to phosphorylate proteins within the cell. Phosphorylase Kinase: an enzymes that use ATP to phosphorylate the protein phosphorylase within the cell Phsophorylation in general occurs at a high rate when the insulin : glucagon ratio is LOW If a protein is phosphorylated by a kinase, the phosphate group must eventually be removed by a phosphatase through hydrolysis. If it wasn't, the phosphorylated protein would be in a constant state of either being activated or inhibited. Kinases and phosphatases regulate all aspects of cellular function. Biochemistry I Guide Page 13 The rate limiting step in glycolysis is step 3, the reaction catalyzed by PFK-1. The most important allosteric regulator of both glycolysis and gluconeogenesis is fructose-2,6-bisphosphate, F-2,6-BP, which is not an intermediate in glycolysis or in gluconeogenesis The synthesis of F-2,6-BP is catalyzed by the bifunctional dimer-enzyme PFK-2/F-2,6BPhosphatase. In the nonphosphorylated form (when insulin : glucagon is high) the enzyme is known as PFK-2 and serves to catalyze the synthesis of F-2,6-BisPhosphate from F-6-P and ATP. F-2,6-BP stimulates PFK-1 synthesis and activity while the activity of F-1,6-BPase is greatly inhibited. Under conditions where PFK-2 is active, fructose flow through the PFK-1/F-1,6-BPase reactions takes place in the direction of glycolysis, with a net production of F-1,6-BP. When the bifunctional enzyme is phosphorylated (when insulin : glucagon is low) it no longer exhibits kinase activity, but a new active site on the F-2,6-BPase side hydrolyzes F-2,6-BP to F6P and inorganic phosphate. The metabolic result of the phosphorylation of the enzyme is that allosteric stimulation of PFK-1 ceases, allosteric inhibition of F-2,6-BPase is eliminated, and net flow of fructose through these two enzymes is gluconeogenic, producing F6P and eventually glucose. The interconversion of the bifunctional enzyme is catalyzed by cAMP-dependent protein kinase (PKA), which in turn is regulated by circulating peptide hormones. Hormones such as glucagon bind to plasma membrane receptors on liver cells, activating membrane-localized adenylate cyclase leading to an increase in the conversion of ATP to cAMP. cAMP binds to the regulatory subunits of PKA, leading to release and activation of the catalytic subunits. PKA phosphorylates numerous enzymes (using ATP as the phosphate donor), including the bifunctional PFK-2/F-2,6-BPase. Under these conditions the liver stops consuming glucose and becomes metabolically gluconeogenic, producing glucose to reestablish normoglycemia. Regulation of glycolysis also occurs at step 9 when catalyzed by pyruvate kinase, (PK). This enzyme is inhibited by ATP and acetyl-CoA and is activated by F-1,6-BP when ATP is low. The inhibition of PK by ATP is similar to the effect of ATP on PFK-1. The binding of ATP to the inhibitor site reduces its affinity for PEP. The liver enzyme is also controlled at the level of synthesis. Increased carbohydrate ingestion induces the synthesis of PK resulting in elevated cellular levels of the enzyme. Genetic diseases of adult erythrocyte PK are known in which the kinase is virtually inactive. The erythrocytes of affected individuals have a greatly reduced capacity to make ATP and thus do not have sufficient ATP to perform activities such as ion pumping and maintaining osmotic balance. These erythrocytes have a short half-life, lyse readily, and are responsible for some cases of hereditary hemolytic anemia. The liver PK isoenzyme is regulated by phosphorylation, allosteric effectors, and modulation of gene expression. The major allosteric effectors are F-1,6-BP, which stimulates PK activity by decreasing its Km(app) for PEP, and for the negative effector, ATP. Expression of the liver PK gene is strongly influenced by the quantity of carbohydrate in the diet, with highcarbohydrate diets inducing up to 10-fold increases in PK concentration as compared to low carbohydrate Biochemistry I Guide Page 14 diets. Liver PK is phosphorylated and inhibited by PKA, and thus it is under hormonal control similar to that described earlier for PFK-2. Muscle PK (M-type) is not regulated by the same mechanisms as the liver enzyme. Extracellular conditions that lead to the phosphorylation and inhibition of liver PK, such as low blood glucose and high levels of circulating glucagon, do not inhibit the muscle enzyme. The result of this differential regulation is that hormones such as glucagon and epinephrine favor liver gluconeogenesis by inhibiting liver glycolysis, while at the same time, muscle glycolysis can proceed in accord with needs directed by intracellular conditions. Enzyme Stimulation Inhibition Hexokinase *Entrance of glucose (or other Rising levels of G-6-P hexoses) into the cell (its product) *Insulin stimulation of cell. Phosphofructokinase I *High AMP levels allosterically High ATP and Citrate levels (Rate-limiting step enzyme) activate PFK-1 allosterically inhibit PFK-1 *High I:G ratio *Hepatic Fructose-2, 6-BP Low I:G ratio (as in fasting or (intracellular signal indicating starvation) glucose levels are ↑) Pyruvate Kinase Low ATP: ADP ratio High ATP: ADP *4: Pyruvate Dehydrogenase Complex (PDH pathway) - occurs on the inner surface of the outer mitochondria membrane *E1: pyruvate decarboxylase, E2: dihydrolipoyltransacetylase, E3: dihydrolipoyldehydrogenase *all require their vitamin in its active form in order to do work *Defects of E2 and E3 are common in the human population due to mitochondrial genetic defects or vitamin deficiencies. They present with high serum pyruvate and alanine concentrations, indicating the breaking down of proteins in the tissue. Pyruvate build-up allows for lactic acidocis & neurological disorders. ** Lactic Acidosis – build up of lactic acid in blood -can be caused by toxicities affecting the mitochondria thereby preventing pyruvate from moving into the PDH complex (FYI: mitochondria is very susceptible to toxins) Dx of Mitochondrial dysfunction: chronic fatigue / immune deficiency syndrome (CFIDS) WBCs also increase constantly as if infected, often misdiagnosed as Epstein Barr virus Tx: ketogenic diets (high fat-low carb diet) may stimulate lipolysis, bypassing the PDH cycle; orthomolecular doses of thiamine (helps w/ E1), lipoic acid helps w/ E2 (also used for peripheral neuropathy in diabetics); vit B12 (which keeps erythrocytes elastic to allow for high gas exchange) Steps: 1. (2) pyruvate (2) CO2 + (2) Hydroxyethyl-TPP Vit: Thiamine E1 – Pyruvate decarboxylase Active form: thiamine pyrophosphate (TPP) **pyruvate decarboxylates one of its carbons in CO2 and the other are part of Hydroxyethyl-TPP 2. (2) Hydroxyethyl-TPP (2)Acetyl-CoA + (2)H+ Vits: alpha-lipoic + Pantothenic acids E2- Dihydrolipoyl transacetylase Active forms: lipoamide + coenzyme A **2 of the carbons from pyruvate bind via a sulfide bond to make Acetyl-CoA which migrates to the matrix **alpha-lipoic acid helps alleviate the pain from neuropathy in diabetes and is used here in metabolism **the hydrogen products come off of the sulfurs in Hydroxyethyl-TPP allowing for reformation of the disulfide bond (FAD+ FADH >> NAD+NADH) 3. (2) H+ ---------------------------------------- (2) NADH Vit: Niacin + Riboflavin E3 – Dihydrolipoyl dehydrogenase Active forms: NAD+ and FAD+ **FADH is an intermediate proton donor for the second NAD+ reduction Biochemistry I Guide Page 15 Calculations: Per 1 mole of glucose: (2 molecules of pyruvate) Net: 2x CO2+6 ATP (2x NADH formed)+2x Acetyl-CoA STIMULATION THROUGH INHIBITION OF PKA2 *Based on the NADH:NAD+ ratio *E1, E2, E3 are active when de-phosphorylated Stimulated by: PDH not phosphorylated -NAD+ inhibits protein kinase A > no phosphorylation > stimulates PDH complex -Ca2+ inhibits PKA by stimulating phosphatase which breaks phosphate bonds Note: ATP and calcium are inversely related -High cortisol indirectly stimulates PDH enzymes Inhibitions: PDH phosphorylated -High NADH: NAD+ stimulates protein kinase A -High ATP: Ca2+ inhibits PDH phosphatase *5: The TCA CYCLE / The CITRIC ACID CYCLE / The KREBS CYCLE Location: Mitochondrial Matrix Starting Substrate: Acetyl CoA (from E2 of PDH or from fat bypassing the PDH) Stimulants: Low energy state. Specific enzymes have their own regulations as well. (ADP) Inhibitions: High energy state or excess product. (ATP, NADH, Succinyl CoA) 1. Citrate Synthase: Very important regulatory step!!! (OAA + Acetyl CoA >> Citrate) a. Irreversible, condensation reaction of oxaloacetate and acetyl-CoA to make citrate. b. Acetyl CoA is not the 1st step, rather the oxaloacetate made first from the citrate condensing enzyme using acetyl- CoA is the first substrate that then is converted to citrate. Epinephrine, a catecholamine synthesized from tyrosine>Dopamine>NE by Phenylethanolamine Nmethyltransferase in the adrenal medulla and stimulated by the anti-inflammatory glucocorticoid cortisol, causes increased heart rate and, thus, increased metabolic demand and stimulation of PDH. When under stress, take L-tyrosine, vit C, SAMe and copper to prevent tissue degradation especially of the pancreas. 2 Biochemistry I Guide Page 16 c. Oxaloacetate is inter-convertible with the alpha-keto amino acid Aspartate by AST, requiring Vit B6 (Pyridoxine). There is a 10-14 day lag from cell destruction to the presentation of these transaminase enzymes (AST and ALT) in the bloodstream. d. Citrate levels are a pivotal control of TCA and glycolysis. As citrate levels increase due to high carbohydrate ingestion, it moves out into the cytosol and is the precursor for fatty acid and cholesterol biosynthesis. Elevated citrate also inhibits PFK1, slowing glycolysis. 2. Cis-aconitase (isoergonic rxn) (Citrate >> Isocitrate) a. 2 steps. Dehydration, then hydration. (no net loss of H20) b. Cis-aconitase problems would also result in citrate build-up causing the same problems as 1. 3. Isocitrate dehydrogenase (Isocitrate >> alpha-ketoglutarate) a. Dehydrogenase = uses NAD+ (needs NIACIN) and produces 1 NADH=3 ATP b. The reaction is an oxidative decarboxylation, meaning loss of CO2 c. Alpha-ketoglutarate is the alpha keto amino acid form of glutamate (requires Pyridoxine) 4. Alpha-Ketoglutarate dehydrogenase (complex) (alpha-ketoglutarate >> Succinyl-CoA) a. Dehydrogenase = uses NAD+ (needs NIACIN) and produces 1 NADH=3 ATP b. Similar to PDH, so it requires Niacin, Riboflavin and Pentoic Acid just like PDH c. Oxidative decarboxylation = LOSS of CO2 5. Succinyl Thiokinase (complex) (Succinyl-CoA >> Succinate....the half-way point) a. This is a substrate level phosphorylation, not oxidative, because it takes GDP and makes GTP which then serves as the phosphate donor to make 1 ATP. This is a coupled reaction. 6. Succinate Dehydrogenase (Succinate >> Fumarate) a. A small exception to our rule. This Dehydrogenase does not use NAD, but FAD instead. b. Produces 1 FADH2 >> 2 ATP c. FAD is a derivative of Riboflavin (vitB2). FAD covalently binds to this enzyme. d. This is an oxidation reaction coupled to the reduction of FAD+ to FADH e. This enzyme has iron-sulfur centers, so it will be especially affected by deficiencies. i. Lead poisoning causes the malformation of porphyrin rings which transport iron and sulfur (from the amino acids Cysteine and Methionine) throughout the body. The 1st effect of lead poisoning is anemia causing the body to undergo splenomegaly trying to remove the anemic RBCs while the liver overworks to help replenish good RBCs and experiences hepatomegaly. Splenomegaly may be fatal. 7. Fumerase (isoergonic rxn) (Fumarate >> Malate) a. Hydration. (adds H2O) 8. Malate Dehydrogenase (isoergonic rxn but also slightly endergonic favoring reactant reformation) (Malate >> OAA) a. Control step b. Dehydrogenase = uses NAD+ (needs NIACIN) and produces 1 NADH=3 ATP c. Aspartate is the amino acid that is bidirectional with OAA Energy Yield from TCA Cycle Total: 12 ATP/cycle; 2 cycle (1 cycle/Acetyl CoA) = 24 ATP **Mitochondria makes 15 ATP (12 TCA + 3 PDH) but per glucose it’s 30 ATP theoretically **Maltose and fructose make the same amount of ATP, but are unregulated How many CO2’s are released in the mitochondria? PDH = 1; TCA = 2 Biochemistry I Guide Page 17 Total 3 CO2 released, but per glucose = 6 CO2 Anapleurotic Reactions increase the concentrations of TCA cycle intermediates (ex: some forms of amino acid metabolism: transamination of glutamate to alpha-ketogluterate or aspartate to OAA). Amphabolic Reactions are those that are bi-directional (anabolic or catabolic). *6: ELECTRON TRANSPORT CHAIN (Oxidative Phosphorylation) http://www.wiley.com/legacy/college/boyer/0470003790/animations/animations.htm Click on Oxidative Phosphorylation link. Malate Aspartate and Glycerophosphate shuttles are involved in getting the protons from glycolysis into the mitochondria for the ETC. In the Malate shuttle, the protons are bound to OAA in the cytosol to form malate which can cross the mitochondrial membrane and then be reconverted to OAA and NADH. The Glycerophosphate shuttle binds the protons to DHAP making glycerol-3-phosphate which goes across the membrane and makes FADH2. NADH and FADH2 then travel to the ETC on the inner membrane. Of the two shuttles, the glycerophosphate does not generate as much ATP as the malate aspartate shuttle and, therefore, is used when the cell is in a high-energy state. Requirements: Needs Magnesium. Oxygen acceptor. (if asked which pathway uses oxygen this is it!) Complex 1: a. Enzymes: NADH dehydrogenase or NADH Coenzyme Q reductase b. NAD enters here, then skips to 3, 4 and 5. (producing 3 ATP) c. NAD adds to Coenzyme Q making CoE Q10 a. Enzyme is FMN (flavomononucleotide) > another active form of riboflavin (like FAD). b. FMN only works in the ETC. d. GTP makes CoE Q (which is species specific to humans and cannot be easily absorbed by digestion, better to do sublingual absorption or give an IV) Complex 2: a. Enzyme: Succinate dehydrogenase or succinate coenzyme Q reductase b. FADH2 enters here, then skips to 3, 4 and 5 (producing 2 ATP) c. Complex 2 does not release a proton, hence only complexes 3 and 4 work on FADH2 Complex 3: a. Cytochrome C – coenzyme Q oxidoreductase Complex 4: this one is the most tested on. a. Enzyme: Cytochrome oxidase b. Copper dependant; Iron and sulfur needed for porphyrin ring c. Production of water by cytochrome c oxidase, without this step we acidify due to excess protons. Complex 5: a. Enzyme: ATP synthase b. Site of ATP formation, for every pair of protons > 1 ATP + (2) H2O c. It has a rachet formation. It turns with every pair of protons. a. Whenever H+’s go through the core (gamma region) of the rachet, it is called coupling. b. Whenever the H+ are diverted away from this region, it is uncoupling. c. Importance? A lot of toxins cause uncoupling (like the diet pill 2,4 dinitrophenol) COMPLEX 4 is the most affected. All complexes are affected by insecticides, barbiturates, some antibiotics (making the ETC very susceptible), but Complex 4 is also inhibited by H2S, Azide (HIV meds), Carbon Monoxide, Cyanide (almond smell, results in sever acidosis, Tx by infusion of thiosulfate which binds CN+do ventilation with 100% O2+give sodium bicarbonate). Biochemistry I Guide Page 18 Midterm Review liver (and kidney) cells can do gluconeogenesis liver and muscle can do glycogenesis and glycogenolysis disaccharides: polysaccharides: o sucrose: alpha-1,2 o starch: alpha-1,4 o lactose: beta-1,4 o cellulose: beta-1,4 o maltose: alpha-1,4 o glycogen: alpha-1,4 w/ alpha-1,6 branches pancreatic alpha-cells: glucagon (epinephrine does glucagon’s job in muscle) o beta-cells: insulin and amylin o delta-cells: somatostatin o gamma-cells: amino acid 37 sorbitol: made from excess glucose via aldose reductase; block via quercitin acetate alcohol blocks thiamine, allowing for hypoglycemia and increases hepatic lactate levels Glycolysis occurs in the cytosol of the cell (see drawing) o Glucose + 2ADP + 2NAD+ + 2 Pi >> 2 Pyruvate + 2 ATP + 2 NADH + 2H+ o Niacin (VitB3) for NAD+ is the only vitamin required for glycolysis (2% from tryptophan) o Mg++ is the required cofactor for ATP metabolism o 6-8 ATP/glucose in glycolysis o Toxicities Fl-, halides, arsenate (stops at step 6-phosphoglycerate kinase) o Glycolysis deficiencies manifest as hemolytic anemia (RH incompativility/Erythroblastosis foetalis) – Mg++ or PK deficiencies may be involved allowing for blood pressure to drop o glycolysis: gross 10 ATP net 8 ATP gross 4 ATP directly made (net 2) gross 6 ATP indirectly made (3/NADH+H+) anaerobic gross 8 net 2 o RBCs only produce 6 ATP 3 ATP / NADH both ATP made in step 9 make up for the 2 used earlier o Alanine (present in muscles) is the alpha-keto-amino acid form of pyruvate o pyruvate can go directly into mitochondria, but has to be changed immediately inside PDH pathway occurs on the inner surface of the outer mitochondrial membrane o defects of E2+E3 are more common and present with high serum pyruvate and alanine levels and can lead to lactic acidosis (Dx: CFIDS and/or high WBC count; misdiagnosed as Epstein Barr virus; Tx: ketogenic diet to bypass PDH complex altogether) o pathway occurs twice (once per pyruvate) o E1: pyruvate decarboxylase gives off CO2; thiamine (vitB1) as TPP o E2: transacetylase produces Acetyl CoA; alpha-lipoic acid as lipoamide & pantothenic acid (vitB5) as coenzyme A o E3: dehydrogenase produces NADH; Niacin as NAD+ & Riboflavin as FAD+ o stimulants: epinephrine (indirect) due to cortisol stimulation (L-tyrosine, vit C, SAMe and Cu help prevent tissue degradation due to excessive cortisol) NAD+ by blocking PKA keeps PDH active Ca++ by stimulating phosphatase turns PDH on o inhibitors NADH by stimulating PKA turns off PDH ATP by inhibiting phosphatase turns off PDH (ATP is indirectly prop. to Ca++) TCA/Kreb’s occurs in the mitochondrial matrix and is amphibolic o aspartate is the alpha-AA form of OAA; alpha-ketogluterate is the alpha-AA of glutamate Biochemistry I Guide Page 19 o o citrate, which increases alongside ATP, is a precursor to FA and cholesterol biosynthesis Steps 3 (IDH) and 4 (alpha-KGDH) release CO2 and NADH while making succinyl-CoA this step makes the total CO2 released in the mitochondria equal to 6 o Step 5 (succinyl thiokinase; thio is the sulfur) takes succinyl-CoA and temporarily makes GTP which makes ATP while the substrate is made into succinate o o o o o o o o o o o Step 6 (Succinate DH) has Iron-Sulfur porphyrin rings which transfer from Cysteine and Methionine and are affected by deficiencies causing first splenomegaly as the spleen removes anemic RBCs and then as hepatomegaly as the liver tries to replenish the RBCs the only dehydrogenase covered that makes FADH2 (2ATPs) instead of NADH FADH2 requires riboflavin (vitB12) A : Acetyl CoA Crazy : Citrate Idiot : Isocitrate Ass : Alpha-ketogluterate aSs: succinyl CoA asS : succinate F’d : fumerate Me : Malate Over : OAA Total yield: 12 ATP/cycle (2 cycles/glucose) Anapleurotic Reactions increase the concentrations of TCA cycle intermediates (ex: some forms of amino acid metabolism: transamination of glutamate to alpha-ketogluterate or aspartate to OAA). ETC on the inner membrane of the mitochondria o MALATE > 1 (ATP) > 3 > 4 (H2O) > 5 (1 ATP/2H+ + 2H2O) (yields 3 ATP) o Glycerophosphate > 2 > 3 > 4 > 5 (yields 2 ATP) o “4” is cytochrome oxidase and is Cu and Fe dependent for its porphyrin rings as well as easily toxicated (H2S, Azide, CO, Cyanide) leading to body acidification o coupling – H+ goes through the gamma region of “5” uncoupling – it doesn’t go through o cofactors of ETC FMN is another active form of riboflavin. NAD adds to Coenzyme Q to make CoE Q10. copper, iron and sulfur needed for complex 4 (cytochrome oxidase) well fed vs. fasting effects (1:6 ratios and enzymes) o NADH (well-fed):NAD (fasting) ratios Biochemistry I Guide Page 20 *7: CYTOCHROME p450 and Detox Cytochrome p450 proteins are involved in hydroxylation reactions and are drug metabolizing enzymes that are used to make cholesterol, steroids and other important lipids (ex: prostacyclins and thromboxane A2 from arachidonic acid). Production of cytochrome p450 is stimulated by ACTH, peroxisome proliferators, aromatic hydrocarbons or ethanol among others. These can convert procarcinogens into carcinogens under certain conditions. The enzyme works by oxidation (phase I), conjugating the drug (phase II) and transferring electrons via NADPH cytochrome p450 reductase in the ER or Ferredoxin in the mitochondria in order to break oxygen-oxygen bonds. conjugation: the process of adding amino acids (esp. taurine (from N-acetyl-cysteine) and glycine) to a hydrophobic substance in order to make it more water soluble; the other possibilities include adding oxygen or methyl groups which accomplish the same thing; occurs during detox diets FYI: glutamine, a major carrier of nitrogen in the blood that can be prescribed during detox to alleviate headaches, can cause GI problems when taken directly (we normally consume protein with glutamine) *Bioflavinoids quench the extra free radicals from causing damage >> detox supplement and effective Down’s Snydrome treatment. drug enhancer: two substances that compete for the same site forcing one to remain more in the blood circulation, thereby increasing the effect of the drug by prolonging its efficaciousness. An enhancer is an inhibitor (antagonist) of the site. *8: Hexose Manophosphate Pathway (HMP)/Pentose Phosphate Pathway3 -Operates mostly in cytoplasm of liver and adipose cells -Purpose: (1) Generates NADPH for reductive biosynthesis reactions within cells. (NADPH is used in cytosol for fatty acid synthesis.) (2) Produces ribose-5-phosphate (R5P) for the synthesis of the nucleotides and nucleic acids. (3) Metabolizes dietary pentose sugars derived from the digestion of nucleic acids as well as rearranges the carbon skeletons of dietary carbohydrates into glycolytic/gluconeogenic intermediates. G6PD deficiency is an X-linked disease. -Process: Two oxidative processes followed by five non-oxidative steps, but the needs (and checkpoints) vary. *Step 2: 6-phosphogluconate dehydrogenase is the only step to give off CO2 (decarboxylation). *Steps 5 and 7 are transketolases that require thiamine. The products interact with glycolysis as they are in fact intermediates of that cycle. *Step 6: Phosphopentose isomerase converts ketose to aldose Note the importance of G6PD in the production of reduced G-SH, ribose, and NADPH... There are other metabolic pathways that can generate NADPH, except in red blood cells. RBCs are therefore less stable and especially sensitive to oxidative stresses. This is why G6PD deficient individuals are not prescribed Glutathione is a tripeptide of glycine, cysteine and glutamine that acts as a proteolytic/reducing enzyme important in movement of amino acids across cellular membranes. It is also an antioxidant and, when acetylated, the body does not brake it down making it stay in the blood longer when IV’d or taken orally as Recancostat (coated w/proanthocyanions). 3 Biochemistry I Guide Page 21 oxidative drugs because the red blood cells in these individuals are not able to handle this stress and would risk hemolysis. *9: CANCER AND METABOLISM Myeloperoxidase System: NADPH from the HMP pathway allows for production of a super oxide which super oxide dismutase can turn into hydrogen peroxide, with NADPH acting as the proton donor. These protons may also bind with chloride ions forming hypochlorite, which is very oxidative and acts as a cleaver. In Major Histo-Compatibility complexes, both H2O2 and HOCl present alongside interleukens (IL2 & ILa) initiating T-cell programming at the receptor site. B-cells may then be programmed by T-cells to function as memory B-cells that circulate as plasma B-cells in case of a future infection. Copper and Zinc are necessary cofactors for the immune system. Cancer and Vit C: Up to 46% of cancer patients have scurvy or absolute lack of Vitamin C, most affecting tissues rich in collagen, which is a fiber resistant to tumor penetration. Because proline and lysine residues are not hydroxylated, collagen molecules are unstable; characterized by bleeding gums, loose teeth, skin lesions, and weakened blood vessel walls. Dx: Test for phagocytosis Normal in vitro levels of 40%-70% engulfing of yeast cells. Many cancer patients 1%-2%. After Vitamin C Therapy back up to typical phagocytosis. Vitamin C induces large amounts of Hydrogen Peroxide, which normal cells produce adequate catalases to remove, but which can kill tumor cells. The amounts of Vit C needed may be between 25-150 grams, which is more than may be ingested because it would cause severe diarrhea. The stress cancer patients undergo also demands Vit C as dopamine-beta-hydroxylase consumes Vit C in the production of epinephrine, which is stimulated by cortisol. CAUTION: With G6PD deficiency Vitamin C therapy could destroy erythrocytes. (TEST FIRST) Tx: Dendritic Cell Stimulation and Anti-angiogenesis o Dendritic cells stimulate production of natural killer cells. These are low in number in cancer patients. o Angiogenesis is an increase in vascularization. AE-941 from shark cartilage is theorized to stop angiogenesis, leading to starving of the tumor...but a large quantity would need to be consumed. Other therapies: o Beta 1,3 and Beta 1,6D-Glucans o Alpha Lipoic Acid > reduces Vit. C requirement o Bioflavinoid Quercetin has been shown to induce tumor apoptosis This is why smoking isn’t pretty…The left displays mouth cancer resulting from prolonged smoking. The right displays gangrene which results primarily from decreased blood flow through an area, allowing for accumulation of infection. W library.thinkquest.org/.../mouth_cancer_cr.jpg Biochemistry I Guide Page 22 *10: FRUCTOSE METABOLISM *Fructose is a relatively uncontrolled sugar in body that is NOT co-transported with Na+. (unlike glucose). *Insertion point is AFTER PFK1 > Metabolically not regulated; however, energy yield is still 38 ATP *Fructose blocks break down of glycogen in the liver (leads to hypoglycemia) (not good for diabetics) *Tissues not affected by sorbitol effectively break it down into fructose, which goes through this pathway: STEPS one>>two: Fructose + Mg+ + ATP ADP + Fructose-1-P Glyceraldehyde + DHAP Fructokinase Aldolase B (splitter) STEP 3: Glyceraldehyde + NADH NAD + Glycerol alcohol dehydrogenase Glyceraldehyde4 + Mg+ + ATP ADP + Glyceraldehyde-3-P (PGAL) Glyceraldehyde Kinase Insertion points into Glycolysis: 1. Fruc Fruc 6 P. >> glycolysis step 2 (not the most common way. Usually used in gluconeogenesis.) 2. DHAP (step 2) PGAL (triose Isomerase) >> glycolysis step 4 3. Glyceraldehyde PGAL (step 3) >> glycolysis step 4 Step 1 Genetic defect: Essential fructosuria. Defect of fructokinase. Pathway is hindered, not eliminated. Dx: High Fructose concentration in urine, otherwise a benign condition. Tx: Lower fructose intake Step 2 Genetic defect: hereditary fructose intolerance. MAJOR PROBLEM. Autosomal recessive defect in Aldolase B allows the body to “sequester phosphate” as Fructose-1-P in the liver, kidney and small intestine. Epidemiology: 1/40,000 Dx: urinary F-1-P, very hypoglycemic, fatigue, vomiting, jaundice, hemorrhaging and hepatic failure o Phosphates removal from the body results in hypophosphatemia, allowing more ADP and AMP to be broken down to uric acid, which causes gout as uriate crystals form in the joints. Tx: elimination of fructose and sucrose from diet Pathophysiology: hypophosphatemia, hypermagnesia, hyperuricemia, hypoglycemia o Phosphate is vital for metabolism, particularly in AMP and ADP conversions to ATP. o Magnesium also relies on phosphate by attaching to it to make it available to AMP and ADP. o Phosphate removal results in increased levels of “unbound”/“free” magnesium o As magnesium rises in the blood, parathyroid hormone facilitates calcium release from bone in order to maintain a 1:1 ratio of calcium:magnesium. o In HFI, as hypermagnesia ensues, parathyroid hormone is inhibited by the elevated Mg++. o The kidneys then respond to low phosphate levels in the blood as a result of urine Fruc-1-P by releasing active Vitamin D in order to substitute for the role of parathyroid hormone. Vitamin D must travel inactively from the skin>liver>kidney, and only at the kidney is it made active so that it can work to raise serum calcium levels Continued depletion of bone calcium leads to calcium imbalances & osteoporosis o This becomes a huge yo-yo cycle as vitamin D, PTH and Mg++ continue to feedback on each other, constantly dropping and raising calcium in the blood. 4 Glyceraldehyde can also be used as the backbone for Fatty Acids Biochemistry I Guide Page 23 *11: GALACTOSE METABOLISM AND LACTATION *Galactose is important in connective tissue development. UDP molecule Requires aspartate, glutamine PRPP is enzyme that adds ribose (from HMP pathway) to Uritolate. o A thiamine deficiency will affect this process, as it is needed for HMP’s transketolases, and need HMP to make UDP for galactose metabolism Why go through all this? Hexokinase cannot see UTP. Since both reactions take place in the cytosol, the body separates them by attaching UTP to the molecule to force down this pathway. More on Galactosemia: *Galactose, being part of lactose, makes up 20% of the energy source of a typical infant's diet. Three enzymes are required to convert galactose into glucose-1-phosphate. Each of these three enzymes is encoded by a separate gene. If any of these enzymes fail to function, a galactosemia results. Thus, there are three types: Galactosemia I (also called classic galactosemia), the first form to be discovered, is caused by defects in both copies of the gene that codes for galactose-1-phosphate uridyl transferase (GALT). USA Epidemiology: 1/50,000-70,000 births. o Sx: normal until given milk for the first time > then vomiting, diarrhea, lethargy, low blood glucose, jaundice, enlarged liver, protein and amino acids in the urine, and susceptibility to infection, especially from gram negative bacteria. Cataracts can appear within a few days after birth. People with galactosemia frequently have symptoms as they grow older even Biochemistry I Guide Page 24 though they have been given a galactose-free diet (speech disorders, cataracts, ovarian atrophy and infertility in females, learning disabilities, and behavioral problems) Galactosemia II is caused by defects in both copies of the gene that codes for galactokinase (GALK). Epidemiology: 1/100,000-155,000 births. o Sx: less harmful than galactosemia I. Babies will develop cataracts at an early age unless they are given a galactose-free diet. Do not generally suffer from liver or neurological damage. Galactosemia III is caused by defects in the gene that codes for uridyl diphosphogalactose-4epimerase (GALE). This form of galactosemia is very rare. o There are two forms of galactosemia III, a severe form, which is exceedingly rare, and a benign form. The benign form has no symptoms and requires no special diet. However, newborns with galactosemia III, including the benign form, have high levels of galactose-1phosphate that show up on the initial screenings for elevated galactose and galactose-1phosphate. Further tests showing normal levels of GALT and GALK allow people affected by the benign form of galactosemia III to enjoy a normal diet. Galactosemia Diagnosis o Almost all states require that all newborns be tested. Blood from a baby who is two to three days old is usually first screened for high levels of galactose and galactose-1-phosphate. If needed, further tests are performed to pinpoint the enzyme lacking (GALT, GALK, GALE) o In the case when galactose is removed from diet just to be safe, or for babies refusing milk or vomiting, tests to measure enzyme levels must be given Galactosemia Treatment o Galactosemia I and II are treated by removing galactose (and lactose) from the diet. Other foods like legumes, organ meats, and processed meats also contain considerable galactose and must be avoided. Soy-based and casein hydrolysate-based formulas are recommended for infants with galactosemia. Galactosemia Prognosis o It is critically important that all newborn babies be tested for galactosemia because the prognosis for any baby with galactosemia I who doesn't start a galactose-free diet within the first five days of life is tragic. About 75% of the untreated babies die within their first two weeks. On the other hand, with treatment, a significant proportion of people with galactosemia I can lead nearly normal lives, although speech defects, learning disabilities, and behavioral problems are common. In addition, cataracts due to galactosemia II can be completely prevented by a galactose-free diet. Lactation: UDP-galactose + glucose –loss of UDP Lactose Sight or sound of infant or suckling stimulates release of oxytocin from the paraventricular nucleus of the hypothalamus via the neurohypophysis. Oxytocin causes contraction of the myoepithelial cells of the breast in order to release milk. Simultaneously, prolactin is released via the adenohypophysis to synthesize new milk. Prolactin’s action is stimulated by PRH enzyme and inhibited by PRIH (and/or dopamine). *12: MANNOSE METABOLISM Mannose is necessary for glycoproteins. ATPADP Mannose Mannose-6-Phosphate Fructose-6-Phosphate 1. Hexokinase 2. Phosphomannose Isomerase Fructose-6-phosphate then inserts into glycolysis at the PFK1 reaction. This will yield the same energy as glucose (38 ATP). Biochemistry I Guide Page 25 *13: CORI CYCLE, GLUCOSE ALANINE CYCLE, GLUCONEOGENESIS Cori Cycle Purpose: involves the utilization of lactate, produced by glycolysis (in muscle primarily) as a carbon source for gluconeogenesis. The liver converts the byproduct of anaerobic glycolysis—lactic acid—back into glucose for re-use or to contribute to glycogen stores. Glucose Alanine Cycle Pyruvate can be transaminated to alanine, which can be shuttled to the liver for gluconeogenesis. o req: vit B6= pyridoxyl phosphate/pyridoxine The MAIN purpose of this cycle is to deliver the amino portion of amino acids to the liver for excretion as urea. The Alanine can be converted back into pyruvate by ALT and used in gluconeogenesis. o The liver’s uric cycle eliminates the nitrogen byproduct GLUCONEOGENESIS An anabolic pathway occurring mainly in the liver, but can occur in intestine and kidney as well. o Is not the mere reversal of glycolysis b/c of energetics Does NOT occur in muscle (Cori Cycle and Glucose-Alanine Cycle are used instead) Substrates: pyruvate, lactate, amino acids (and TCA intermediates) and glycerol (forms DHAP). o Fatty acids cannot be used b/c they only yield acetyl-coA, which goes through TCA It is not high levels of pyruvate and lactate that stimulate GNG, it’s the high Glucagon:insulin ratio. Upon arrival of pyruvate to inner surface of the outer mitochondria membrane, the cell makes a choice as to what it’s needs are. If the tissue is lacking energy (low acetyl CoA/low ATP/low NADH) then PDH works. Otherwise, GNG occurs... 1. Pyruvate Oxaloacetate a. Enzyme: Pyruvate Carboxylase (PDH complex in glycolysis) b. Req. 1st: Biotin, Mg 2nd: Mn, Bicarbonate(for CO2) i. Anytime CO2 is added, Biotin is involved b/c it links to lysine (biocytin). c. Acetyl CoA is an allosteric activator d. 2 ATP consumed (1ATP/pyruvate) 2. Oxaloacetate Malate Oxaloacetate a. Enzyme: Mitochondric > Cytosolic Malate dehydrogenase b. Important side reaction since oxaloacetate cannot cross the inner mitochondrial membrane, so it is temporarily converted to Malate 3. OAA PEP + CO2 (released prior to cytosol entrance) a. PEP carboxykinase (pyruvate kinase) b. High energy demands: Decarboxylation is favorable, plus 2 GTP consumed (Req: Mg) Biochemistry I Guide Page 26 4. PEP 2-Phosphoglycerate 3-Phosphoglycerate 5. 3 Phosphoglycerate 1,3 bisphosphoglycerate a. 2 ATP consumed (1ATP/pyruvate) 6. 1,3 bisphosphoglycerate fructose 1,6, bisphosphate a. Thermodynamically favorable (negative delta G) in the liver b. 2 NADHNAD+ (Niacin, VitB3) 7. fructose 1,6 bisphosphate fructose 6 phosphate a. fructose 1,6 bisphosphatase (PFK 1) b. Allosterically stimulated by citrate and inhibited by F-2,6-BP and AMP 8. fructose-6-phosphate glucose-6-phosphate 9. glucose-6-phosphate glucose a. glucose-6-phosphatase (hexokinase) i. present in the ER of the liver and kidneys, hence GNG occurs here b. under substrate level control c. the ER ships glucose to plasma membrane via exocytosis TOTAL: -4 ATP directly + -8 ATP indirectly = -12 ATP (anabolic, only 8 ATP returned in glycolysis) Regulation of Gluconeogenesis When glucagon binds to the receptor and stimulates cAMP and protein Kinase A to phosphorylate PFKII, it will turn OFF glycolysis, but turn ON gluconeogenesis. Inhibited by: PFKII not phosphorylated (making F-2,6-BP) o Low Glucagon : Insulin o NAD+ inhibits protein kinase A > no phosphorylation > stimulates PFK1 o Ca2+ inhibits PKA by stimulating phosphatase which breaks phosphate bonds Note: ATP and calcium are inversely related o High cortisol indirectly inhibits o Acute hepatitis, HIV infections with high viral load Stimulated by: PFKII phosphorylated (acting as F-2,6-BPase) o High Glucagon : Insulin o High ATP : AMP o High citrate o High NADH : NAD+ stimulates protein kinase A o High ATP: Ca2+ inhibits PDH phosphatase o Epinephrine Biochemistry I Guide Page 27 *14: GLYCOGENESIS - anabolic General information in regards to glycogen (animal starch): 1. Storage form of glucose that is optimized to deliver quick energy 2. Mostly found in the liver and muscle tissue (in muscle tissue glucagon metabolism is uncontrolled) 3. Linear alpha(1,4) glycosidic bonds, branching alpha(1,6) glycosidic bonds Reactions Initially: glucose-6-P--------------------- glucose-1-P Phosphoglucomutase * Glycogenesis depends on sugar nucleotide formation 1. Glucose-1-phosphate + UTP ------------------------------- UDP-glucose + 2Pi UDP-glucose pyrophosphorylase * GP is allosterically activated by AMP and inhibited by ATP, glucose-6-P and caffeine 2. UDP-glucose + glycogenin ------------------------ glucose-glycogenin + UDP Glycogen initiator synthase *Glycogenin is a protein that forms the core of a glycogen particle. Glycogenin has the unusual property of catalyzing its own glycosylation, attaching C-1 of a UDP-glucose to a tyrosine residue on the enzyme. The attached glucose is believed to serve as the primer required by glycogen synthase. 3. glucose-glycogenin + UDP-glucose ------------------- (glucose)2-Glycogenin + UDP Glycogen synthase (forms the α1,4 bonds) **repeats until 12th glucose added * Glycogen synthase is active when there is a high I:G ratio. It is subject to covalent modification and depicted in two forms: a and b. Glycogen synthase a is the unphosphorylated form and the most active. Glycogen synthase b is the phosphorylated and glucose-6-p-dependent form. DAG encourages Ca++ release from the ER and, thereby, PKC activation, thereby phosphorylating this enzyme to its b form. Dephosphorylation is carried out predominately by protein phosphatase-1 (PP-1), the same phosphatase involved in dephosphorylation of glycogen phosphorylase. Glycogen synthase is also under allosteric control and stimulated by high ATP and Caffeine. 4. (glucose)12-Glycogenin ------------------------------ alpha(1,6) glucose-(glucose)8-Glycogenin amylo-(1,4 - 1,6)-transglycosylase, (Branching enzyme) *Branching enzyme takes off the distal 4 glucose molecules and adds the alpha(1,6) glycosidic linkage onto the 8th glucose molecule in the chain. Glycogen synthase can then add onto the branch and linear chain another 12 glucose molecules each and repeat the branching process again. Biochemistry I Guide Page 28 *15: GLYCOGENOLYSIS - Catabolic * In regular digestion, glycogenolysis is unregulated and proceeds via alpha-amylase (α1-4) and debranching enzymes (α1-6). Reactions 1. Glycogen + Pi ------------------------ glucose-1-P + remainder of glycogen Glycogen phosphorylase * Glycogen phosphorylase is active when there is a low I:G ratio. It exists in two conformational states: active R form and inactive T. T form is phosphorylated to be phosphorylase a (inactive). R form is dephosphorylated to be phosphorylase b (active). Phosphorylase b is stimulated by: High ADP/AMP, epinephrine + glucagon (acting on PKA), and High Ca2+. 2. Glucose-1-P ---------------------------------- glucose-6-P >> glycolysis (9 ATP b/c it skips hexokinase) Phosphoglucomutase DISORDERS of Glycogenesis and Glycogenolysis (all are RARE) 1. McArdle’s Syndrome (Type V) -Problem with Glycogen breakdown (skeletal glycogen phosphorylase deficiency) -skeletal muscle is affected while liver enzyme is normal -Sx: Patients often have cramps after exercise (but no rise in lactate during strenuous exercise) 2. Pompe’s Disease (Type II) -Problem with Glycogen breakdown (lysosomal α -1,4-glucosidase deficiency) leading to glycogen sequestering in cytosolic vacuoles and severe cardiomegaly -Problem is generalized to liver, heart and skeletal muscle tissue -very serious, fasting can kill the patient -Ssx: infantile form = death by 2; juvenile form = myopathy; adult form = muscular dystrophy-like Type Ia: von Gierke's IIIa: Cori's/Forbe's IV: Anderson's VI: Her's VII: Tarui's XI: Fanconi-Bickel Table of Some Other Glycogen Storage Diseases Enzyme Affected Primary Organ Manifestations hepatomegaly, kidney failure, glucose-6-phosphatase Liver thrombocyte dysfunction liver and muscle liver, muscle infant hepatomegaly, myopathy debranching enzyme branching enzyme liver, muscle hepatosplenomegaly, cirrhosis hepatomegaly, mild hypoglycemia, hyperlipidemia liver phosphorylase liver and ketosis, improvement with age muscle PFK-1 muscle, RBC's like V, also hemolytic anemia glucose transporter-2 failure to thrive, hepatomegaly, liver (GLUT-2) rickets, proximal renal tubular Biochemistry I Guide Page 29 dysfunction *16: GLYCOSAMINOGLYCANS (GAGs) *Some examples of glycosaminoglycan uses in nature include heparin as an anticoagulant, hyaluronate as a component in the synovial fluid lubricant in body joints, and chondroitins which can be found in connective tissues, cartilage and tendons. Types of GAGs *17: LIPID OVERVIEW Saturated FA -Raise Good and Bad Cholesterol Monounsaturated FA -Raise HDLs and Lower LDLs Polyunsaturated FA -Maintain HDLs and Lower LDLs Trans fatty acids -Lower HDLs and Raise LDLs Biochemistry I Guide Page 30