Dystrophia Myotonica
advertisement

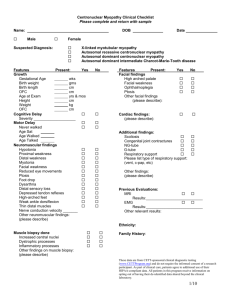
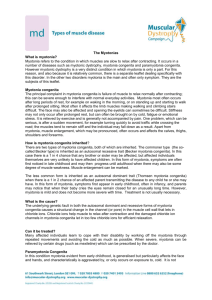
Dystrophia Myotonica Approach to Congenital Myopathies 1. Duchenne’s, Becker’s 2. Myotonia Dystrophia myotonica (fascioscapular dystrophies can mimic appearance) Congenital myotonia Hereditary paramyotonia 3. Fascioscapulahumeral dystrophies, limb-girdle dystrophies, distal myopathies Examination Examine patient’s face or hands (Can be short case of locomotor or in CNS station) Examine the hands Demonstrate difficulty opening hands after shaking Repeatedly open and close the hands Percussion myotonia of the thenar eminence (proceed with hand examination with function assessment if locomotor station) Demonstrate weakness in the forearms (especially) and hands No sensory loss Loss of reflexes Check the pulse (dysrhythmias, small volume pulse) Examine the face Myopathic facies Expressionless Triangular facies Wasting of the temporalis, masseter (palpate these muscles when patient clenches teeth) Frontal balding Bilateral ptosis Close his eyes and open Tongue for percussion myotonia Gum hypertrophy from phenytoin toxicity Swan-neck appearance with wasting of the SCM (test for weakness of SCM), weakness of flexion of the neck Nodular thyroid enlargement Request Face Cataracts - posterior subcapsular and stellate Assess Speech – slurring due to myotonia of the tongue and pharyngeal muscle Chest examination Gynecomastia Cardiovascular examination – dilated cardiomyopathy (split S1, mitral murmur, low BP and pulse volume) Testicular atrophy Urine dipstick for diabetes mellitus Lower limbs – bilateral footdrop Presentation Sir, this patient has got dystrophia myotonica as evidenced by A myopathic facies that is triangular in appearance with an expressionless look. There is wasting of the facial muscles involving the temporalis and masseter muscles associated with frontal balding and bilateral ptosis. He had difficulty opening his eyes after firm closure. There was myotonia affecting the tongue. There is also a swan-neck appearance with wasting of the sternocleidomastoid muscles with weakness of flexion of the neck. On shaking his hand, there was a delay in releasing his grip. In addition, after making a fist, he was unable to quickly open it especially after doing this repetitively. There was also presence of percussion myotonia of the thenar eminence. There is presence of proximal myopathy and wasting with involvement of the forearms and hands. There are also reduced reflexes with no sensory loss detected. Function is relatively preserved. With regards to complications His pulse is regular at 80 bpm with a small volume pulse suggesting dil CMP There was no gum hypertrophy to suggest chronic phenytoin use. There is nodular thyroid enlargement. I would like to complete my examination by Face Cataracts - posterior subcapsular and stellate Assess Speech – slurring due to myotonia of the tongue and pharyngeal muscle Chest examination Gynecomastia Cardiovascular examination – dilated cardiomyopathy (split S1, mitral murmur, low BP and pulse volume) Testicular atrophy Urine dipstick for diabetes mellitus Lower limbs – foot drop with high steppage gait (tibial nerves are affected early) Questions What are the types of muscular dystrophies you know of? 1. Duchenne’s Sex linked Pseudohypertrophy of the calves or deltoids Gower’s sign, proximal weakness Cardiomyopathy Becker’s Sex linked Later onset and less severe form of Duchenne’s 2. Limb-girdle Autosomal recessive Shoulder and pelvic girdle affected Third decade Sparing of the face and heart Fascioscapulohumeral Autosomal dominant Bilateral, symmetrical weakness of the facial and SCM with bilateral ptosis Weakness of the shoulder muscles and later the pelvic girdle muscles 3. Dystrophia myotonica Congenital myotonia Hereditary paramyotonia 4. Distal myopathies eg Welander’s myopathy What is myotonia? Continued contraction of the muscles after voluntary contraction ceases, followed by impaired relaxation. What is dystrophia myotonica? Characteristic clinical appearance with myotonia and weakness with no sensory loss Autosomal dominant with a trinucleotide (AGC) repeat disorder on chromosome 19 Anticipation – phenotypic expression worsens with each successive generation Onset in the 3rd or 4th decade Males>females In addition to the characteristic facies and musculoskeletal involvement Intellectual and personality disorder Cataracts – posterior subcapsular cataracts which are stellate type CVM – dilated cardiomyopathy and conduction defects Resp – recurrent infection from weakness of the bronchiolar musculature, hypoventilation and post-anaesthetic respiratory failure Abdomen – dysmotility and dysphagia Testicular atrophy and gynecomastia Diabetes mellitus Nodular thyroid enlargement How would you investigate? Confirm Diagnosis EMG – dive bomber pattern ie waxing and waning of the potentials Muscle biopsy shows no inflammatory changes with type 1 fibre atrophy which is characteristic but not diagnostic DNA analysis Muscle enzymes are normal Screen for Complications FPG – screen for diabetes mellitus ECG – heart blocks, small P, prolonged PR, notched QRS and prolonged QTc CXR – enlarged heart Slit-lamp examination for cataracts How would you manage? Education, genetic counselling PT/OT – eg foot orthosis for foot drop Medications – phenytoin for myotonia, other anti-myotonic medications such as quinine and procainamide should be avoided due to aggravation of cardiac conduction defects; however it is the weakness that causes disability and not myotonia Pacemaker for 3rd degree heart block or symptomatic such as syncope How would you counsel the patient’s family? Vertical Autosomal dominant, children 1 in 2 Anticipation DNA analysis is available for some families for prenatal diagnosis Horizontal Screen with clinical examination Slit-lamp examination EMG What are the other types of myotonia disorders? Myotonia congenita (Oppenheim’s disease) Autosomal dominant or recessive Presence of myotonia without other features of dystrophia myotonica Present at infancy with difficulty feeding with subsequent improvement No weakness and reflexes are preserved Herculean appearance Channelopathies Hereditary paramyotonia Autosomal dominant Cold-induced myotonia What are your differential diagnoses for dystrophia myotonica? Facies appearance – Facioscapulohumeral dystrophy Autosomal dominant, onset at age 10-40, Chr4, normal lifespan Face – ptosis, difficulty closing eyes, facial weakness and speech impaired Normal IQ Neck – wasted SCM and weakness Shoulder – winging of scapula, weakness of pectoralis, trapezius, biceps and triceps and hypertrophy of deltoids Occasionally affecting the anterior tibialis Normal CK Proximal weakness – FSH, limb-girdle, prox myopathy causes, MG Limb Girdle dystrophy (see prox myopathy) Distal weakness – Welander’s distal myopathy, nerve problem Myotonia – Congenital myotonia, hereditary paramyotonia