Orthopedic Injury Exam Questions & Answers
advertisement

37
100. A 30-year-old was involved in a rapid deceleration motor vehicle crash at street speed. He was
gripping the steering wheel tightly, and complains of pain at the MCP joint of the right thumb. On
exam there is tenderness and mild swelling of the joint on the ulnar side. X-rays are negative.
Which of the following is correct regarding the evaluation and treatment of this injury?
a. If the ulnar collateral ligament demonstrates more than 35o of laxity when compared to the
uninjured side, place a thumb spica splint and refer to orthopedics for probable surgical
management.
b. If the radial collateral ligament demonstrates any laxity, refer to orthopedics for surgical repair.
c. All gamekeepers’ thumbs need to be repaired surgically.
d. The absence of a fracture indicates that no splinting will be necessary.
e. If the ulnar collateral ligament demonstrates less than 20o laxity, apply a universal wrist splint,
and refer for surgical repair.
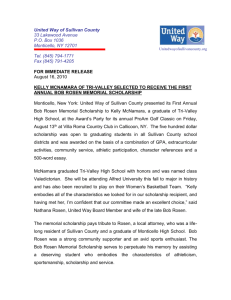
101. This x-ray shows a:
a. dorsal dislocation of the lunate.
b. volar dislocation of the lunate.
c. dorsal perilunate dislocation.
d. volar perilunate dislocation.
e. scapholunate dissociation.
Rosen 5th,
Figure 44-11
102. Elbow dislocations are associated most commonly with concomitant injuries to the:
a. ulnar nerve and radial artery.
b. ulnar nerve and brachial artery.
c. radial nerve and ulnar artery.
d. radial nerve and brachial artery.
e. median nerve and radial artery.
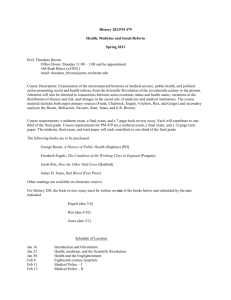
103. This child fell while rollerblading and has a tender
elbow. This x-ray (figure 169-15) is most
consistent with:
a. nursemaid’s elbow.
b. radial head fracture.
c. proximal ulnar fracture.
d. elbow dislocation.
e. supracondylar fracture
Rosen’s 5th,
Figure 169-15
104. Monteggia’s injury is a :
a. fracture of the ulnar shaft with radial head dislocation.
b. fracture of the ulnar shaft with distal radioulnar dislocation.
c. fracture of both the radius and ulna.
d. distal radial fracture with radioulnar dislocation.
e. distal radial fracture with radial head dislocation
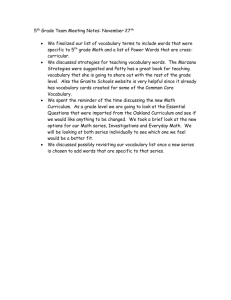
105. This x-ray (Figure 44-24) demonstrates a:
a. Colles fracture.
b. Monteggia fracture.
c. Galleazzi fracture.
d. Bennett fracture.
e. Barton fracture.
Rosen 5th,
Figure 44-24
38
100. a
th
Rosen 5 ,
Chapter 43,
p. 520
101. c
Rosen 5th,
Chapter 44,
p. 541
102. b
Rosen 5th,
Chapter 45,
p. 572
103. e
th
Rosen 5 ,
Chapter 45,
p. 564
104. a
Rosen 5th,
Chapter 44,
p. 551
105. c
Rosen 5th,
Chapter 44,
p. 552
Injury to the ulnar collateral ligament (UCL) was first described as an occupational
hazard of Scottish gamekeepers who damaged their thumbs by repeatedly twisting the
necks of hares. Skiing is now the most common cause of both acute and chronic injury
to the UCL. UCL rupture occurs ten times more often than radial collateral ligament
injury. The mechanism of injury is forced radial deviation (abduction), and the
subsequent tear usually occurs at the insertion into the proximal phalanx. Complete
and partial ruptures can usually be differentiated by clinical examination. Valgus
stress testing of the ulnar collateral ligaments is required and should be performed in
full extension and in 30% flexion to avoid the stabilizing effect of the volar plate.
More than 35% of joint laxity or 15% more laxity than is present in the uninjured
thumb is consistent with complete UCL rupture. Acute partial ruptures of the UCL can
be effectively treated by a 4-week period of immobilization in a thumb spica cast, and
full recovery is the rule. Complete ligament tear requires surgical repair because a
high number have associated soft tissue interposition from the adductor aponeurosis
(Stener’s lesion) with limited predicted healing potential.
A perilunate dislocation is best seen on the lateral view of the wrist. Although the
lunate remains in position relative to the distal radius, the capitate is dorsally
dislocated. The PA view shows overlap of the distal and proximal carpal rows and
may also demonstrate an associated scaphoid fracture or subluxation.
In patients with elbow dislocations, neurovascular complications occur in 8 to 21%, the
most frequent being injury to the ulnar nerve. Vascular complications occur in 5 to
13% of elbow dislocations, with brachial artery injury the most common.
Supracondylar injuries are extra-articular fractures which occur most commonly in
children; 95% are displaced posteriorly as a result of an extension force. The patient
will have significant swelling and tenderness at the elbow. Radiographs may reveal a
fat-pad sign in undisplaced fractures due to visualization of fat from the olecranon
fossa (posterior fat pad) as it is displaced by the hemarthrosis. In some undisplaced
fractures, the fracture line may not be seen, with the fat-pad sign being the only
evidence of injury. Treatment should be initiated as though a fracture were identified,
with splint immobilization and orthopedic consultation.
Fracture of the ulnar shaft with a radial head dislocation is often referred to as
Monteggia fracture-dislocation. It is typically a diaphyseal fracture in the proximal
third of the ulna with an anterior dislocation of the radial head (60% of cases).
Anterolateral and posterolateral dislocation of the radial head or a metaphyseal ulna
fracture are other possibilities. As a rule, the radial head normally points to the
capitellum in all radiographic views of the elbow. In a Monteggia fracture, the apex of
the ulna fracture points in the direction of the radial head dislocation.
A Galeazzi fracture involves the junction of the middle and distal thirds of the radius,
with an associated dislocation or subluxation of the distal radial-ulnar joint (DRUJ).
This rare injury accounts for only 7% of all fractures of the forearm. It occurs as a
result of a fall on the outstretched hand, with the wrist in extension and the forearm
forcibly pronated. The radial fracture causes obvious swelling and deformity on the
radial side of the forearm, and pain is localized over the fracture site. In addition, the
DRUJ is swollen and painful on palpation, and the ulnar head appears prominent when
compared with the unaffected wrist.
39
106. A 16 year old boy complains of pain and swelling in his right hand after hitting a wall with a closed
fist. You know that:
a. the neck of the metacarpal is the most frequently fractured segment.
b. metacarpal fractures of the long and index finger do not need to be reduced if there is less than
30o of angulation.
c. metacarpal fractures of the ring and small fingers do not need to be reduced if there is less than
20o of angulation.
d. most metacarpal fractures angle in a volar direction.
e. a boxer’s fracture refers to metacarpal neck fractures of the long and sometimes ring fingers.
107. A 5 year old boy falls and fractures his radius.
a. Salter-Harris Type I fractures are the most common type
b. The picture shows a Salter-Harris Type II fracture.
c. Salter-Harris Type III fractures involve the epiphyseal plate and
have a widened space between epiphysis and metaphysis.
d. Salter-Harris Type IV fractures are difficult to diagnose using
standard radiographs.
e. Salter-Harris Type I, II, and III injuries have poor prognosis despite
proper reduction and immobilization.
108. A 29 year-old man is tackled while playing football and suffers what appears to be a shoulder
dislocation. You know that:
a. the most common direction of dislocation is posterior.
b. anterior-posterior (AP) and lateral radiographs are the best views to confirm the diagnosis.
c. after reduction he should be placed in a shoulder immobilizer for 2 months.
d. infraglenoid dislocations are associated with seizures.
e. inadequate muscle relaxation is the most common reason for failed reduction.
109. A 43-year-old softball player pulled up lame stretching a single into a double. You suspect a
ruptured Achilles tendon, since you know:
a. when the soleus and gastrocnemius muscles contract, the Achilles tendon pulls up the calcaneus,
dorsiflexing the foot.
b. rupture often occurs in professional sports settings, especially in over-conditioned athletes.
c. the patient hears a popping sound and then has difficulty walking.
d. the Thompson-Doherty test is performed by squeezing the midportion of the calf while the patient
is lying in the prone position; an intact Achilles tendon is demonstrated by dorsiflexion of the
foot.
e. unbearable pain is a cardinal symptom.
110. A 23-year-old hairdresser complains of two days of increasing pain and swelling in her right index
finger pad. She has no fever. Her finger pad is tense, red, warm, and very tender. Her nail and
paronychial region are not affected. You should:
a. place her on amoxicillin / clavulanate (Augmentin®), elevation, and warm soaks.
b. perform a through-and-through incision of the pad volar to the neurovascular bundle, then
amoxicillin / clavulanate (Augmentin®), elevation, and warm soaks.
c. perform a fish mouth incision and refer to a hand surgeon.
d. perform a unilateral longitudinal incision on the ulnar side dorsal to the neurovascular bundle,
amoxicillin / clavulanate (Augmentin®), elevation, warm soaks, pain medicine, recheck in two
days.
e. remove the nail, incise the eponychium, hot soaks, pain meds, and recheck in two days.
40
106. d
th
Rosen 5 ,
Chapter 43,
p. 513
107. c
Rosen 5th,
Chapter 169,
p. 2373
108. e
th
Rosen 5 ,
Chapter 46,
p. 592-594
109. c
Rosen 5th,
Chapter 51
p.716
110. d
Rosen 5th,
Chapter 43,
p. 529-530
Fractures of the metacarpal neck are among the most common fractures in the hand.
They are usually due to a direct impaction force. A fracture of the fifth metacarpal
neck is often referred to as a boxer’s fracture. These fractures are usually unstable
with volar angulation. Angulation of less than 20° in the fourth and 40° in the fifth
metacarpal will not result in functional impairment. In the second and third
metacarpal, angulation of <15° is acceptable. These fractures should be splinted with
the wrist in 20° extension and the MP flexed at 90°. Fractures of the second or third
metacarpal that are significantly displaced or angulated require anatomic reduction and
surgical fixation.
Rosen 5th,
Table 169-1
I
II
III
IV
V
Dislocation of the glenohumeral joint is the most common major joint dislocation.
Anterior dislocations are by far the most common. Although the anteroposterior
radiograph will reveal the dislocation, the scapular Y radiograph will indicate the
direction of dislocation: anterior or posterior. Since severe pain and muscle spasms are
the norm, muscle relaxation and analgesia are paramount. Posterior glenohumeral
dislocations may occur during a fall or from violent muscle contraction from a seizure
or electric shock. In uncomplicated cases the shoulder is immobilized for 3 to 6 weeks
in younger patients and 1 to 2 weeks in older (over age 40 years) individuals.
Achilles tendon rupture usually occurs in middle-age persons during sporadic or
intermittent involvement in recreational sports. Injury mechanism is sudden
unexpected dorsiflexion, forced dorsiflexion of a plantarflexed foot, and strong pushoff of the foot with simultaneous knee extension and calf contraction (e.g., a runner
accelerating from the starting position). The diagnosis is primarily clinical. Patients
usually describe a sudden onset of pain at the back of the ankle associated with an
audible “pop” or “snap.” Although the pain may resolve rapidly, weakness in
plantarflexion persists. The classic maneuver to assess the integrity of the Achilles
tendon is the Thompson test. This is performed with the patient prone and the knee
flexed at 90o. Alternatively, the patient may kneel on a chair with both knees flexed at
90o and the feet dangling over the edge. Squeezing the calf muscles in these two
positions should cause passive plantarflexion of the foot. Absence of this motion or a
weakened response compared with the uninjured side suggests complete rupture.
A felon is a subcutaneous pyogenic infection of the pulp space of the distal finger or
thumb. The septa of the finger pad produce multiple individual compartments and
confine the infection under pressure. The patient presents with throbbing pain and a
red, tense distal pulp space. Staphylococcus aureus is the most common organism. If
the finger pad is swollen and tense, or if there is any palpable fluctuance, drainage
must be undertaken. A unilateral longitudinal approach spares the sensate volar pad
and achieves adequate drainage. Introduce a #11 blade lateral to the paronychium and
direct it in a volar direction until you find pus. Extend the incision ensure adequate
drainage, but not to the distal interphalangeal (DIP) flexor crease.
41
111. Which of the following is true of this injury?
a. This is a common wrist fracture.
b. The lunate requires immediate reduction.
c. The distal radial-ulnar ligament is disrupted and will
require surgical repair.
d. The clenched fist AP view may accentuate this finding.
e. None of the above – this is a normal x-ray.
Rosen 5th,
Figure 44-10
112. A 38-year-old man developed severe lower back pain that shoots down his right leg as he was
lifting a large box at work. He has no previous history of back problems. He has no bowel or
bladder symptoms, and denies genital numbness. On exam he has no back deformity or palpable
pain, but when he raises his leg off of the bed, a severe pain shoots down his leg to his great toe.
He has some numbness of the lower leg and web space next to the great toe. He has 4/5 strength
with dorsiflexion of the foot. His deep tendon reflexes are normal. He most likely has:
a. herniated nucleus pulposus (HNP) of L1-L2.
b. HNP of L3-L4.
c. HNP of L5-S1.
d. severe lumbar strain.
e. drug seeking behavior, since the findings are non-anatomic.
113. A 34-year-old man is ejected from a car. He has no head
Rosen 5th, Figure 48-6
injury, but complains of severe pain in his pelvis. His
airway and breathing are fine, but he is hypotensive – BP
80/40 mm Hg, heart rate 120. His workup shows multiple
abrasions and pelvic pain. His pelvis x-ray is shown. His
abdominal CT shows no intra-abdominal injury. After 4
liters of IV fluid, his blood pressure is 95/60. Of the choices
given below, your most appropriate would be to:
a. re-examine by compression and distraction of pelvic
wings.
b. transfuse fresh frozen plasma to control bleeding.
c. obtain stat vascular consult for intraoperative exploration and cauterization of vessels.
d. apply pneumatic antishock garment (PASG) to act as splint and compressive dressing.
e. arrange for hanging traction with at least 20 pounds of weights.
114. A 22-year-old man was in a head-on motor vehicle crash. His right leg is in adduction, flexion, and
internal rotation. Which is the correct statement about this injury?
a. This is likely a femoral neck fracture, so x-rays and pain relief should be given.
b. After sufficient analgesia and sedation, gentle flexion to 90o with upward traction should be
performed as soon as possible.
c. The most likely associated injury is to the femoral nerve.
d. The risk of associated acetabular fracture is minimal.
e. The risk of avascular necrosis is >50%.
115. Ankle sprains:
a. are common in young children and toddlers.
b. most commonly involve the anterior talofibular ligament.
c. most commonly occur on the medial side of the ankle.
d. require radiography to diagnosis a third-degree injury.
e. involving isolated deltoid ligament injuries are very common.
42
111. e
th
Rosen 5 ,
Chapter 44,
p. 538
112. c
Rosen 5th,
Chapter 47,
p. 617
113. d
Rosen 5th,
Chapter 48,
p. 640
114. b
Rosen 5th,
Chapter 49,
pages listed
in answer
115. b
Rosen 5th,
Chapter 51
p.714
A stage I injury, or scapholunate dissociation, results in a characteristic widening of the
scapholunate joint on the PA view, which has been called the Terry-Thomas sign, after
the British comedian with a gap between his front teeth. When a scapholunate
ligament injury is suspected clinically, additional stress views should be obtained.
Views taken with a clenched fist and ulnar deviation (the clenched fist AP view) will
accentuate widening of the scapholunate joint.
The most important test for back pain is the straight leg raise. This is done with the
patient supine and the legs extended, or with both legs slightly flexed at the hips and
knees. The symptomatic leg is passively raised, with the knee fully extended. Pain
caused by a disk herniation in L4-L5-S1 usually results in increased pain in the leg at
anywhere from 30 to 70o of elevation, as the affected nerve root is stretched. It is
important to note that back pain, probably secondary to stretching of the paravertebral
muscles as the leg is elevated, indicates absolutely nothing about radiculopathy. A
straight leg raise test is positive only if lifting the affected leg reproduces or worsens
the pain in that leg. The pain of radiculopathy is usually worse in the leg than in the
back and almost always radiates past the knee. Ninety-five percent of disk herniations
occur at L4–L5 or L5–S1. Without complaint of sciatica, or pain below the knee in a
dermatomal distribution, the chance of a herniated nucleus pulposus is 1 in 1000.
When attempts to stabilize the patient hemodynamically with crystalloid infusion and
transfusion of blood products are unsuccessful, application of a pneumatic anti-shock
garment should be discussed with orthopedic and general surgical consultants.
Although controversial, PASG can temporarily splint the fracture and tamponade
pelvic bleeding until definitive stabilization and angiography with embolization can be
performed..
The Allis maneuver (Figure 49-27) should be attempted in order to reduce a [posterior
hip dislocation as quickly as possible. The patient is placed supine the knee is
flexed and steady traction is applied in line with the deformity – the hip is brought
slowly to 90o of flexion after reduction, the hip is extended while maintaining
traction (p. 664). A patient with a femoral neck fracture presents with leg externally
rotated and shortened. A patient with a posterior hip dislocation typically holds the hip
flexed, adducted, and internally rotated (p. 662). Sciatic palsies, especially the
peroneal nerve branch, occur in 10% of patients with posterior hip dislocation (p. 662).
Acetabular fractures are common (p. 662). Avascular necrosis is reported to occur in
1% to 17% of patients with this injury (p. 665).
Most ankle sprains occur from extreme inversion and plantarflexion. Approximately
two thirds of ankle sprains are isolated anterior talofibular ligament injuries, whereas
20% involve both anterior talofibular and calcaneofibular ligament injuries. Isolated
injury of the deltoid ligament occurs in fewer than 5% of ankle sprains. A grade III
sprain involves a complete tear of the ligament with marked joint instability and severe
edema and ecchymosis, and is a clinical diagnosis.
43
116. A 75-year-old woman fell at a local flower shop and complains of
severe left hip pain. Her left leg is shortened and externally
rotated. She has strong pedal pulses and sensation is intact.
Thorough head-to-toe examination reveals no other injuries. Her
left hip x-ray is shown (Figure 49-17), so you arrange for the
patient’s admission to the orthopedic doctor on call. The patient’s
daughter, a pediatrician, wants to know about potential
complications from this injury. You tell her that, just as in
children, the most common complication is:
a. avascular necrosis.
Rosen 5th,
b. hemorrhage.
Figure 49-17
c. osteomyelitis.
d. fat embolism.
e. femoral nerve injury.
117. A 24 year-old basketball player severely twisted his left knee several hours ago and is unable to
bear weight. There is a large joint effusion. While examining his knee, you see that valgus stress at
30o flexion causes more than a centimeter of “give” without a firm endpoint. The knee is stable in
extension with valgus stress. This suggests:
a. an isolated medial collateral ligament disruption.
b. an isolated lateral collateral ligament disruption.
c. a medial collateral ligament tear with probable involvement of the cruciates and posterior capsule.
d. a lateral collateral ligament rupture with posterior cruciate tear.
e. probable anterior cruciate rupture with meniscal tear.
118. A 32-year-old man swung at a pitch while playing softball, then
collapsed due to severe knee pain. His injured leg looks like this. Your
treatment should be:
a. immobilization, x-ray, pain medicine, and examination for probable
peroneal nerve injury.
b. needle arthrocentesis of the prepatellar bursa, then ice and elevation.
c. orthopedic consult for repair of the patellar tendon.
d. gentle lateral pressure on the patella with the knee in extension.
e. examine for possible popliteal artery disruption.
119. A 35-year-old male skier fell and twisted his knee. Within five minutes, he developed severe pain
and a large joint effusion. When testing his knee stability, you know that:
a. the anterior drawer sign is highly accurate in diagnosing acute ACL injuries.
b. abduction, flexion, and internal rotation of the femur on the tibia produce injuries to the lateral
side of the knee.
c. adduction, flexion, and external rotation of the femur on the tibia produce injuries to the medial
side of the knee.
d. lateral knee injuries are far more common than medial knee injuries.
e. a negative Lachman’s test rules out ACL injury with >90% accuracy.
120. Metabolic acidosis without an anion gap is caused by:
a. cyanide poisoning.
b. renal tubular acidosis.
c. lactic acidosis.
d. ketoacidosis.
e. salicylate ingestion.
44
116. a
th
Rosen 5 ,
Chapter 49,
p. 656
117. a
Rosen 5th,
Chapter 50,
p. 678
118. d
Rosen 5th,
Chapter 50
p.688
119. e
Rosen 5th,
Chapter 50
p.677
In a patient with femoral neck fracture, avascular necrosis is the most common
complication, despite optimal treatment, because of the complex arterial anatomy. The
mortality rate during the first year after a femoral neck fracture is 14%, compared with
9% for the control population. Deep infection, in the form of osteomyelitis or septic
arthritis, is more common with femoral neck fractures because the fracture line extends
into the joint. Pulmonary embolism is the leading cause of death at 7 days postfracture in all orthopedic patients.
Abduction or valgus pressure applied to a knee in approximately 30° of flexion
determines the integrity of the medial capsular and ligamentous structures. If there is a
demonstrated laxity of greater than 1 cm without a firm end-point as compared to the
other knee, there is a complete rupture of the medial collateral ligament. If there is
laxity with a firm end-point or a laxity of less than 1 cm, an incomplete or partial tear
is present. If there is no demonstrated instability but there is pain, the patient has
suffered a strain. The patient who is unstable with the valgus test performed with 30°
of flexion should be brought into full extension, if possible, and similar maneuvers
carried out. Medial instability in full extension indicates a severe lesion involving the
cruciate ligaments and posterior capsule along with the medial ligaments.
Patellar dislocation may occur from an athletic injury caused by valgus stress
combined with flexion and external rotation. Patients may complain of the knee giving
out accompanied by pain and swelling. Inability to bear weight or to flex the knee is a
common complaint. Examination shows an anterior defect with the patella deviated
laterally. Closed reduction is accomplished through force or pressure directed
anteromedially on the lateral patellar margin while simultaneously gently extending the
leg.
A tear in the anterior cruciate ligament or intra-articular fracture usually results in an
immediate hemarthrosis and inability to continue activity. A torn meniscus may cause
an acutely locked knee but more commonly has delayed onset of swelling over 12 to
24 hours and intermittent locking associated with joint line pain. Lachman’s test is
currently the single best clinical test for determining the integrity of the ACL and one
of the only reliably performed tests in a patient with an acute hemarthrosis. Accuracy
in diagnosing ACL injury increases from 70% to 99% using Lachman’s test rather than
the anterior drawer test. The anterior drawer test is not reliable and is of little value in
diagnosing acute ACL injuries.
120. b Elevated Anion Gap
th
Rosen 5 ,
Chapter 118
p.1719
(“CAT MUD PILES”)
Carbon monoxide / Cyanide exposure
Acute alcohol intoxication / Alcoholic ketoacidosis
Toluene exposure
Methanol intoxication
Uremia
Diabetic ketoacidosis
Paraldehyde ingestion
Isoniazid (INH) / Iron intoxication
Lactic acidosis
Ethylene glycol intoxication
Salicylate intoxication
Normal Anion Gap
Gastrointestinal loss of HCO3–
Diarrhea
Enterostomy
Ureteroenterostomy
Renal loss of HCO3–
Renal tubular acidosis
Acetazolamide
Hyperalimentation
45
121. Which statement is correct concerning the entity shown in this x-ray?
a. This is a common foot injury, usually caused by inversion.
b. Associated fractures are quite common, and usually involve the base
of the 2nd metatarsal.
c. This is a pseudo-pseudo-Jones fracture.
d. Rest, ice, elevation, and ambulation as tolerated give the best longterm results.
e. You can easily reduce this injury with gentle axial traction and plantar
flexion.
Rosen 5th, Figure 51-24
122. A 35-year-old man accidentally chopped off his left index finger at the PIP joint about six hours
ago while cutting firewood at a campsite in a local state park. He stuck the amputated finger in his
pocket, hiked out of the woods, and drove to your Emergency Department. You should:
a. clean the amputated finger with Betadine® and place it in the refrigerator.
b. clean the amputated finger with hydrogen peroxide, wrapped in saline gauze, and place it on ice.
c. irrigate the amputated finger with saline, wrap it in sterile dry gauze and place it in a plastic bag,
which should be immersed in ice.
d. Irrigate the amputated finger with saline, wrap it in saline-moistened gauze and place it in a
plastic bag, which should be immersed in ice-water slurry.
e. There is no need to care for the amputated extremity as the ischemic time is too long and no
reimplantation will be possible
123. A 20-year-old college student has redness, tenderness, and swelling on the plantar surface of his
foot. Two days ago, while wearing sneakers, he stepped on a nail. You should prescribe:
a. cephalexin.
b. amoxicillin/clavulanate.
c. ciprofloxacin.
d. tetracycline.
e. erythromycin.
124. Antibiotics are clearly indicated for:
a. all dog bites.
b. all cat bites.
c. all human bites.
d. all foot puncture wounds.
e. all intraoral lacerations.
125. The acute life threats in adrenal inufficiency are:
a. hypertension and hyperglycemia.
b. hyperthermia and hypoglycemia.
c. hypothermia and hyperglycemia.
d. hypotension and hypoglycemia.
e. hyperthermia and hypertension.
126. A patient being treated for diabetic ketoacidosis develops weakness and paresthesias. The most
likely metabolic abnormality is:
a. acidosis.
b. hypokalemia.
c. hypophosphatemia.
d. hypocalcemia.
e. hypoglycemia.
46
121. b
th
Rosen 5 ,
Chapter 51,
p. 726
122. d
Rosen 5th,
Chapter 43,
p. 527
123. c
Rosen 5th,
Chapter 52,
p. 748
124. b
Rosen 5th,
Chapter 52,
p. 748
125. e
Rosen 5th,
Chapter 122,
p. 1781
126. b
th
Rosen 5 ,
Chapter 120,
p. 1753-1754
The six-bone tarsometatarsal complex is known as the Lisfranc joint. Up to 20% of
fractures at this joint are missed in the ED. The force required and the mechanisms of
injury are varied and can range from a seemingly minor rotational force to severe axial
load as seen in an automobile accident. The great majority of injuries to the Lisfranc
joint are associated with fractures, usually of the metatarsals, the cuboid, or the
cuneiforms. A fracture of the base of the second metatarsal is pathognomonic of a
disruption of the ligamentous complex. Injuries to the Lisfranc joint frequently require
open reduction and fixation or percutaneous placement of Kirschner wires and nonweight-bearing for several weeks.
The time that an amputated part can survive before reimplantation has not been
determined. As a general rule, the more proximal the amputation, the less ischemic
time the amputated part can tolerate. Warm ischemia may be tolerated for 6 to 8 hours,
but there are reports of successful replantation of digits after 30 hours of warm
ischemia. The amputated part requires minimal handling and should be cooled as soon
as possible. After wrapping in saline-moistened gauze, the part is sealed in a dry
plastic bag and placed in ice water. Ice should not come in direct contact with the
tissue because this can cause local damage. Local antiseptics, especially hydrogen
peroxide or alcohol, should not be used because they may damage viable tissues.
The infection rate for foot puncture wounds has been reported to be as high as 15%.
Most infections are due to gram-positive organisms, with Staphylococcus aureus
predominating, followed by other staphylococcal and streptococcal species.
Pseudomonas aeruginosa is the most frequent pathogen isolated post-puncture wound
osteomyelitis, particularly when foreign-body penetration occurs through the sole of an
athletic shoe. Because this organism is not detected in new shoes, it has been
postulated that the foam rubber material becomes colonized in the warm, humid
summer months. The only oral agents consistently effective against Pseudomonas are
the fluoroquinolones, including ciprofloxacin and levofloxacin.
Antibiotic prophylaxis is required for all patients with cat bites. Antibiotic prophylaxis
for dog bites is more controversial, and seven of eight randomized trails of dog bite
wounds show no benefits with antibiotics. While human bites of the hand are at a high
risk for infection, human bites of other locations appear to have no worse infection rate
than other wounds. No data suggest a benefit from prophylactic antibiotics in foot
puncture wounds. Little data suggest a clear indication for prophylactic antibiotics in
patients with intraoral lacerations, but through-and-through wounds have an infection
rate twice as high as simple mucosal injuries.
The acute life threats in adrenal insufficiency are hypotension and hypoglycemia.
Hypotension responds well to glucocorticoid replacement with IV hydration, and
hypoglycemia to IV administration of D5W.
Potassium replacement is invariably needed in DKA. The initial potassium level is
often normal or high despite a large deficit because of severe acidosis. Potassium
levels often plummet with correction of acidosis and administration of insulin.
Potassium should be administered with the fluids while the laboratory value is in the
upper half of the normal range.
47
127. According to his father, this 11-year-old boy has complained about a vague hip,
thigh, and knee pain for the past 2 weeks. He recalls no injury. There has been
no fever. The child walks with a limp and winces when his right foot hits the
ground. His x-ray demonstrates:
a. osteomalacia femoralis.
b. Osgood-Schlatter disease.
c. Legg-Calvé-Perthes disease.
Rosen 5th,
d. septic synovitis.
Figure 49-34
e. slipped capital femoral epiphysis.
128. In a patient with primary adrenal insufficiency you would expect to see:
a. hypernatremia.
b. hypokalemia.
c. hypoglycemia.
d. azotemia.
e. acidosis.
129. The most common cause of a markedly elevated serum potassium is:
a. laboratory error.
b. renal failure.
c. Addisonian crisis.
d. rhabdomyolysis.
e. acidosis.
130. Hirschsprung's disease:
a. is typically diagnosed in infancy.
b. almost always is associated with enterocolitis.
c. is more frequent in females.
d. can be diagnosed by ultrasound.
e. can best be managed pharmacologically.
131. You deliver a child at 36-weeks gestation and intestines are protruding from a defect in the
abdominal wall. On inspection, you note that the intestines lack a peritoneal covering.
a. A gastroschisis is a defect in the umbilical ring that allows the intestines to protrude out of the
abdominal cavity in a sac.
b. An omphalocele is a defect in the abdominal wall that allows the evisceration of abdominal
structures without a sac being present.
c. Gastroschisis and omphalocele are invariably fatal within hours.
d. You are twice as likely to encounter gastroschisis you are to see omphalocele.
e. Emergency department treatment gastroschisis involves gastric decompression; this same
treatment is contraindicated in omphalocele.
132. A 13-year-old male complains of acute, severe pain and swelling in his left testicle. He says that
the pain woke him from sleep. He had something silimar a week or two ago, but it got better
spontaneously. Suspecting torsion testicle, you know that:
a. absence of the cremasteric reflex is not a useful physical exam finding.
b. if this patient's symptoms have only been present for 1 hour, Doppler imaging of the testicles can
be obtained before obtaining surgical consultation.
c. relief of this pain with elevation of the scrotum indicates that epididymitis is the diagnosis.
d. torsion of the right testicle is more common due to a longer spermatic cord.
e. testicular pain may be constant or intermittent, but it is not positional.
48
127. e
th
Rosen 5 ,
Chapter 169
p.2387
128. c
Rosen 5th,
Chapter 122
p.1781
129. a
Rosen 5th,
Chapter 119,
p. 1730
130. a
Rosen 5th,
Chapter 165,
p. 2305-2306
131. d
Rosen 5th,
Chapter 9,
p. 103
132. e
Rosen 5th,
Chapter 94
p.1423
Children with a stable slipped capital femoral epiphysis have symptoms of intermittent
limp and pain for several weeks to months. Stable slips make up approximately 90%
of all cases. The pain may be localized to the hip but more commonly is poorly
localized to the thigh, groin, or knee. On AP radiographs, signs of slippage include
Klein’s line drawn along the superior margin of the femoral neck. With a normal hip,
the line intersects or falls within the epiphysis, whereas in a hip with a slipped
epiphysis, the line does not come in contact with the epiphysis.
Two thirds of patients with adrenal failure have associated hypoglycemia. The
symptoms are characteristic of hypoglycemia: perspiration, tachycardia, weakness,
nausea, vomiting, headache, convulsions, and coma. The pathophysiology is decreased
gluconeogenesis and increased peripheral glucose use secondary to lipolysis.
Electrolyte abnormalities are common. Hyponatremia is present in 88% of cases,
hyperkalemia in 64%, either hyponatremia or hyperkalemia in 92%, and hypercalcemia
in 6% to 33%.
When faced with a report of a high serum potassium level, the Emergency Physician
should first consider the possibility of laboratory error, the most common cause of
hyperkalemia. Hemolysis during phlebotomy, as may occur when blood is obtained
with a small needle or sampled in a high-vacuum tube, releases potassium into the
sample and causes a spuriously high potassium level to be measured.
Hirschsprung’s disease accounts for 20% of partial intestinal obstruction early in
infancy. It is 4 to 5 times more common in boys and can be associated with Down
syndrome or a variety of other anomalies of the GI, GU, or neurologic systems.
Neonates often present in the nursery with a failure to pass meconium. Diagnosis is
suspected on barium enema, and confirmed by biopsy. Treatment in surgical.
Gastroschisis is a defect in the abdominal wall that allows the antenatal evisceration of
abdominal structures without a sac being present. Omphalocele is a defect in the
umbilical ring that allows the intestines to protrude out of the abdominal cavity in a
sac. Gastroschisis occurs twice as frequently as omphalocele. ED treatment involved
gastric decompression and placing an occlusive plastic covering to prevent heat and
water loss.
Manual detorsion is never curative but should be attempted in most cases while
awaiting surgical treatment. Prehn's sign, or relief of pain with elevation of the
scrotum, was historically thought to be associated with epididymitis, but this
association is false and should not be used to distinguish torsion from epididymitis.
The cremasteric reflex is almost always absent in testicular torsion. The salvage rate in
testicular torsion remains high if pain has lasted less than 6 hours, but a urology
consult should be obtained as soon as the diagnosis seems likely clinically.
49
133. Concerning intraosseous lines:
a. Fat embolism is a common complication, especially in adult patients.
b. In adults, the tibia is technically easier than in children because of relative proximity to the
surface.
c. The preferred insertion site in the adult femur is the lateral surface of the trochanter.
d. Infection rates approach 20% in both adults and children.
e. Any drug which can be given intravenously can also be delivered through an intra-osseous line.
134. A 3-month-old girl is irritable, feeds poorly, and breaks into a profuse sweat whenever she takes the
nipple. She is tachypneic and pale. Her heart rate is 280 /
minute. Chest x-ray shows a large heart with alveolar
infiltrates. A rhythm strip is shown. You know that:
a. jugular venous distension and peripheral edema are
commonly found in infants with this condition.
b. volume replacement is the most essential treatment
c. heart rate is the least malleable of the cardiovascular parameters.
d. cardioversion with 0.01 watt-sec/kg is indicated for profound shock
e. a stable patient can be treated with vagal maneuvers
135. A 16-month-old child is brought to the emergency department immobilized in cervical spine
precautions. The child was an unrestrained passenger in a moderate-speed rapid-deceleration motor
vehicle collision. You are concerned about possible neck injury, keeping in mind that:
a. pseudosubluxation of C3 on C4 is common in children.
b. the small neck muscles make fractures more common than ligamentous injury.
c. the predental space should not exceed 4 to 5 mm in children younger than 10.
d. anatomic features of the cervical spine approach adult patterns at around 12 years of age.
e. if the child was ambulatory at the scene, spinal precautions are unnecessary.
136. A 2-year-old child is brought to the emergency department because of fever and pulling at his left
ear. Otitis media is best confirmed by:
a. decreased mobility of his tympanic membrane and loss of normal landmarks.
b. hyperemia of his tympanic membrane in the absence of crying.
c. retraction of his tympanic membrane accompanied by upper respiratory infection symptoms.
d. loss of the tympanic light reflex.
e. the presence of otalgia and upper respiratory infection symptoms.
137. An 18-month-old boy has fever and poor feeding. His ears look normal, but he has an exudative
pharyngitis and enlarged cervical lymph nodes. A rapid antigen detection test for Group A betahemolytic streptococcus (GABHS) is negative.
a. Rapid streptococcal tests are highly sensitive, so it is highly unlikely that this child has acute
GAS pharyngitis.
b. While GABHS is unlikely at this age, detection is important because of the significant risk of
acute rheumatic fever in untreated patients.
c. If the test had been positive, appropriate treatment would include a dose of intramuscular
procaine penicillin.
d. If the test had been positive, early institution of appropriate antibiotics would likely have
shortened the clinical course of the illness
e. Infectious mononucleosis is not a consideration because of the child’s age.
50
133. e
th
Rosen 5 ,
Chapter 8,
p. 84
134. e
Rosen 5th,
Chapter 164
p. 2290-2292
135. c
Rosen 5th,
Chapter 32,
p. 274-276
136. a
Rosen 5th,
Chapter 67,
p. 928-931
137. d
Rosen 5th,
Chapter 70,
p. 969-972
For pediatric patients up to 5 years of age, the tibia is the preferred site. In adults, the
most commonly used site is the medial malleolus. Although complications such as fat
and marrow emboli to the lungs have been reported, recent data suggest that the risk is
not increased by the use of IO access for emergent fluid and drug administration. The
tibia is technically more difficult in adults than in children because the adult bone is
thicker and the needle tends to slip off. The incidence of infection, including both
cellulitis and osteomyelitis, is less than 1%, and the potential for infection can be
minimized by limiting the duration of intraosseous infusion and avoiding hypertonic
solutions.
The predominant symptoms of congenital heart disease include poor feeding, excessive
diaphoresis, irritability or lethargy with feeding, weak cry and, in severe cases,
grunting and nasal flaring. Tachypnea is a cardinal sign. Since feeding is the infant’s
primary form of exertion, dyspnea and sweating during feeding can often be elicited in
the history. Peripheral edema, jugular venous distention, and rales are unusual and late
signs in infants. Heart rate is the most malleable of the cardiac physiologic parameters.
The common pediatric dysrhythmia is paroxysmal supraventricular tachycardia. Initial
management of unstable patients with narrow complex tachycardia consists of
immediate synchronized cardioversion at 0.5 J/kg with increases in power output to 2
J/kg as needed. In the stable patient, vagal maneuvers are the intervention of choice. If
vagal maneuvers are not successful in the stable patient, IV adenosine (0.1 mg/kg –
maximum first dose 6mg) followed by (0.2mg/kg – maximum 12mg) can be used.
On a lateral cervical spine view the distance between the anterior aspect of the
odontoid process and the posterior aspect of the anterior ring of C1, the so-called
predental space, should not exceed 5 mm in a child. Pseudosubluxation of C2 on C3
occurs in approximately 40% of children up to adolescence. Anatomic features of the
cervical spine approach adult patterns between the ages of 8 and 10 years. Compared
to adults, the child has relatively underdeveloped neck musculature and a head that is
disproportionately large and heavy compared to the body, leading to fewer fractures
and more ligamentous injuries.
The most significant sign of acute otitis media (AOM) is the loss of or decrease in
mobility of the tympanic membrane. The light reflex is of no diagnostic value. The
normal eardrum is translucent and pearly gray but may become reddened with crying.
The TM of AOM is usually opaque, hyperemic, and sometimes bulging, and bony
landmarks (long and short process of the malleus) are not easily discernible.
Early antibiotic treatment of streptococcal pharyngitis leads to a 13% earlier resolution
of symptoms and shortens the course of illness by about 1 day. GABHS is primarily a
disease of children 5 to 15 years old and occurs in winter and early spring. It is
responsible for less than 15% of pharyngitis in patients older than 15 years of age and
is rare in patients less than 3 years old. Rapid strep tests have reported specificity of
70% to 100% (with most being >95%) and sensitivity of 31% to 100% (with most
being 60% to 95%). The incidence of rheumatic fever parallels that of GABHS, with
the peak incidence in children 5 to 15 years old, less common in adults, and rare in
children less than 3 years of age. Monospot tests are positive in about 30% of children
0 to 20 months with mononucleosis.
51
138. A 3-day-old baby presents to the emergency department with purulent conjunctivitis. His mother
has a history of syphilis treated prior to this pregnancy. She had no prenatal care, but delivered in
the hospital. The infant received topical erythromycin prophylaxis in the nursery. The most likely
cause of this child’s illness is:
a. syphilis.
b. Neisseria gonorrhoeae.
c. group B streptococcus.
d. Herpes simplex.
e. Chlamydia trachomatis.
139. A 2-year-old patient has screamed inconsolably for four hours and is brought to the ED by his
frazzled parents. He is afebrile and non-toxic in appearance; initial exam shows nothing but mild
left conjunctival erythema without discharge. Your next step should be:
a. lumbar puncture.
b. Schiotz tonometry.
c. fluorescein staining of the cornea.
d. urinalysis.
e. stool for occult blood.
140. Parents bring a 6-week-old infant to the ED because of 3 days of vomiting, occurring immediately
after eager feedings. The baby is fussy, but alert. His mucous membranes are tacky. When you
feed him, he eagerly takes the bottle, but then promptly vomits. Except for the dehydration, you
find nothing else on the exam. This child will require:
a. surgical intervention.
b. intravenous hydration and observation.
c. prompt parenteral antibiotic therapy.
d. discharge with BRAT diet and parental reassurance.
e. change to a soybean-based formula.
141. Cyanosis frequently occurs with:
a. ventricular septal defect.
b. atrial septal defect.
c. patent ductus arteriosus.
d. tetralogy of Fallot.
e. hypertrophic cardiomyopathy.
142. Regarding ear infections:
a. The tympanic membrane should always appear normal in acute otitis externa.
b. Normal tympanic membrane mobility rules out acute otitis media.
c. Children with acute otitis media who are compliant with appropriate antibiotic regimens do not
require any follow-up.
d. An intense worsening of the pain usually indicates sudden tympanic membrane perforation.
e. Topical antibiotic therapy for otitis externa is ineffective unless the canal is free of debris and
cerumen.
52
138. e
th
Rosen 5 ,
Chapter 66,
p. 917
139. c
Rosen 5th,
Chapter 66
140. a
th
Rosen 5 ,
Chapter 165,
p. 2297-2301
141. d
Rosen 5th,
Chapter 164,
p.2283-2287
142. e
Rosen 5th,
Chapter 67,
p. 931-932
Neonatal conjunctivitis (ophthalmia neonatorum) occurs within the first month of life.
The chemical irritation from antimicrobial prophylaxis against bacterial infection
occurs within 1-2 days of birth. Other causes include Chlamydia trachomatis, H.
influenzae, and Streptococcus pneumoniae. Due to mandated use of erythromycin
ocular prophylaxis, Neisseria gonorrhoeae is not a major cause of neonatal
conjunctivitis in the United States. This drug, however, has not been proven effective
against chlamydia infections. Gonococcal conjunctivitis generally has its peak time of
onset between 3 and 5 days after birth. By the end of first week of life and throughout
the first month of life, chlamydia becomes the most frequent cause of conjunctivitis.
Your next step should be a fluorescein staining of the reddened eye, followed by
examination with a cobalt blue light. Corneal abrasion is a common cause of
inconsolable crying in an otherwise normal infant.
The infant with a history of nonbilious projectile vomiting must be considered to have
pyloric stenosis. Physical examination usually demonstrates a hungry infant who has
failed to gain weight over the past several weeks or has lost weight. Surgery is the
treatment of choice although there are reports of success with IV and oral atropine, a
Tetralogy of Fallot is one example of cyanotic heart disease associated with decreased
pulmonary blood flow. Transposition of the great vessels exemplifies cyanotic heart
disease with increased pulmonary blood flow. Other congenital cardiac lesions
causing cyanosis are truncus arteriosus; tricuspid atresia; and total anomalous venous
return. They are known collectively as the “terrible T’s.”
A thorough and atraumatic cleansing of the ear canal is the most important part of
therapy. For mild infections, dry mopping using a small tuft of cotton attached to a
wire applicator is sufficient and may be curative. The tympanic membrane of a child
with otitis externa may be as red and distorted as that of a child with otitis media,
although mobility of the tympanic membrane is normal or only slightly decreased in
otitis externa. Visualization of the tympanic membrane may be difficult because of
edema of the external auditory canal.
53
143. Which statement is true regarding Group A beta-hemolytic streptococcal (GABHS) pharyngitis:
a. Experienced clinicians can accurately exclude GABHS pharyngitis with the history and physical
exam alone.
b. Overuse of penicillin has resulted in emergence of resistant strains of GABHS requiring a change
in recommended first line antibiotics.
c. It is inappropriate to treat sore throat with antibiotics unless there is culture-proven GABHS.
d. Throat culture for GABHS has very few (less than 1%) false-negatives.
e. Treatment of streptococcal pharyngitis significantly shortens the course of the disease.
144. You are evaluating a 6 week-old infant for “irritability” as reported by her mother. You find an
alert but cranky infant with a rectal temperature of 95oF. The left eardrum is a little red. The baby
is fussy when held, but relatively quiet when left on the bed. Which statement is correct?
a. This infant needs lumbar puncture.
b. Since you found an otitis media, you have an explanation for the infant’s illness and an LP is not
necessary.
c. Given a reliable mother, antibiotic therapy and close outpatient follow-up is appropriate
d. It is almost impossible for an infant this young to have an otitis media.
e. If the fontanelles are flat, you can reliably rule out meningitis.
145. In a child with a chest x-ray that shows pneumonia, the most common physical finding would be:
a. rales.
b. rhonchi.
c. tachypnea.
d. asymmetric breath sounds.
e. wheezes.
146. A 4-year-old girl presents with six days of fever. You find erythema of her hands and feet,
conjunctival injection, cervical adenopathy, “strawberry” tongue, dry lips, red throat, and a
morbilliform rash. You should treat this girl with:
a. penicillin.
b. aspirin.
c. ceftriaxone.
d. amoxicillin.
e. dexamethasone.
147. A 3-year-old girl has a plastic bead stuck in her ear. She kicks and screams when you try to remove
the bead and, even after sedation, you are unsuccessful in your attempts to remove the foreign body.
Not wanting to cause injury, you give up and call the ENT surgeon, who tells you not to worry
about it; send the patient home and have Mom call the next day for an appointment. You should:
a. follow the consultant’s instructions.
b. insist that the consultant come in and see the patient.
c. call a different consultant.
d. sedate the patient even more deeply to allow successful foreign body removal.
e. turn the child upside-down and shake her vigorously.
148. Which electrical injury is correctly paired with its resultant complication?
a. low-voltage alternating current (AC) ventricular fibrillation
b. lightning ventricular fibrillation
c. high-voltage AC superficial burns
d. lightning compartment syndrome
e. high-voltage AC tetanic contraction
54
143. e
th
Rosen 5 ,
Chapter 70,
p. 971-972
144. a
Rosen 5th,
Chapter 168,
p. 2344-2350
145. c
Rosen 5th,
Chapter 163,
p. 2268-2270
146. b
Rosen 5th,
Chapter 161
p. 2238-2239
147. a
Rosen 5th,
Chapter 53
p.754-756
148. a
Rosen 5th,
Chapter 136,
p. 2010-2014
Research has clearly demonstrated the beneficial effects of early antibiotic therapy on
reduction of signs and symptoms of GABHS pharyngitis. Diagnostic accuracy on the
basis of clinical findings alone is reported at about 50 to 75% for children thought to
have GABHS and 75 to 85% for children thought not to have GABHS. There is
general agreement that clinical diagnosis alone would result in an unacceptably high
rate of misdiagnosis. GABHS is highly sensitive to penicillin, and there has been no
evidence of development of resistance in vitro despite decades of use. The rate of
false-negative results from single throat culture is about 10%. Because clinical
judgment is insufficient and rapid diagnostic tests are not always accurate and diagnose
only GABHS, this disease process is often treated empirically.
The symptoms and signs suggestive of bacteremia and serious bacterial illness most
frequently produce an overall ill appearance. Parents may note poor feeding,
decreased responsiveness, or irritability in response to attempts to console. Physical
examination findings suggestive of an ill appearance include poor eye contact and
muscle tone, including weak suck, poor head control, and indifferent response to
stimuli. The most important historical and physical findings are related to overall
appearance. Bulging fontanelle, a hallmark of an increased intracranial pressure, is
present in approximately 15% of neonatal acute bacterial meningitis.
The best physical examination finding for ruling out pneumonia in an infant or child is
the absence of tachypnea. However, tachypnea is a nonspecific symptom and may
occur secondary to fever, anxiety, metabolic disease, cardiac disease, or other
respiratory problems. Fever can increase an infant’s respiratory rate by 10 breaths per
minute for each degree centigrade of elevation. Auscultation of the lungs may reveal
localized rales, wheezing, and decreased air entry in the affected area. However,
auscultatory findings may not be reliable in children. In younger children, decreased
breath sounds, rather than rales, are often heard, since the involved areas tend to be
ventilated poorly.
Kawasaki syndrome is a vasculitis that causes a prolonged fever (more than 5 days),
usually exceeding 39.5-40°C (104° F). Clinical findings include conjunctival injection
without exudate; red, peeling lips; strawberry tongue; and pharyngitis. Early there may
be painful swelling of the hands and feet; peeling of the skin of the fingers occurs late
in the course. Cervical adenopathy in excess of 5 cm is common. Treatment is
directed toward the amelioration of symptoms and the prevention of coronary
aneurysms. Gamma-globulin 2 gm/kg intravenously should be administered over 12
hours, followed by high-dose aspirin therapy (100 mg/kg/24 hr PO given in divided
doses every 6 hours for 14 days).
If routine methods are unsuccessful or if the patient, is uncooperative or in too much
distress, the emergency physician should cease removal efforts and refer the patient to
an otolaryngologist. Primary operative intervention is frequently indicated in very
young children and in those in whom the EP and the ENT specialist believe
nonsurgical attempts unlikely to be successful. Inappropriately prolonged efforts at
foreign object removal can result in wasted time, unnecessary patient discomfort, and
high potential for complications.
Low-voltage alternating current generally produces ventricular fibrillation. Highvoltage AC that causes greater current intensity is more likely to produce asystole.
Direct current is also more likely to cause asystole. The most common arrhythmia
encountered in victims who sustain cardiac arrest from electrical injury is ventricular
fibrillation. The immediate cause of death due to a lightning strike is usually direct
current depolarization of the myocardium and sustained cardiac asystole.
55
149. A 4-year-old non-immunized child presents with sudden sore throat, stridor, drooling, and fever.
He looks sick and is sitting forward on the litter, but is alert. Pulse oximetry is 99% saturation on
room air. Your next step is to:
a. attempt to visualize his epiglottis.
b. send him to x-ray for lateral neck radiographs.
c. immediately begin bag-valve-mask ventilation.
d. immediately intubate the child nasotracheally.
e. none of the above.
150. A 3-year-old boy is brought to the emergency department after choking on a watch battery. X-rays
show that the battery is in his stomach. Appropriate management involves:
a. parental reassurance and home observation.
b. ipecac to induce expulsion of the battery.
c. cathartics to speed transit through the gastrointestinal tract.
d. admission to the hospital for observation.
e. laparotomy if the battery is still in the small bowel at 48 hours.
151. Which of the following fractures is most suggestive of child abuse?
a. 19-month-old with a supracondylar fracture after falling off a chair.
b. 22-month-old with a spiral femur fracture from a fall while running.
c. 10-month-old with linear skull fracture from a fall down stairs in an infant walker.
d. 4-month-old with a transverse fracture of the humerus from a fall out of bed.
e. 3-year-old with a tuft fracture of the distal phalanx from the finger being closed in a door.
152. A 10-year-old boy complains of mild intermittent abdominal pain and a rash. His parents have not
noted any fever. Physical examination shows a well-appearing boy with a raised purpuric rash,
most prominent on the legs. His abdominal exam is normal. Temperature = 99.8oF. The other
vital signs are normal. What is the most appropriate next step in the management of this patient?
a. Obtain blood for culture and start antibiotics.
b. Obtain abdominal radiographs.
c. Obtain a urinalysis, BUN, and creatinine.
d. Perform a skin biopsy.
e. Order liver function tests.
153. Concerning cold exposure injuries:
a. chilblains (pernio) is a painless macular rash.
b. in frostbite, the “zone of stasis” is most severely injured.
c. early surgical intervention is recommended for severe frostbite.
d. a body part previously affected by cold injury is immune from reinjury.
e. trench foot may result in irreversible damage.
154. The most common finding in a patient with a brown recluse spider bite is:
a. vomiting.
b. severe muscle cramps.
c. anaphylaxis.
d. local tissue necrosis.
e. respiratory failure.
56
149. e
th
Rosen 5 ,
Chapter 162
150. a
Rosen 5th,
Chapter 147,
p. 2118
151. d
th
Rosen 5 ,
Chapter 169,
p. 2379-2381
152. c
Rosen 5th,
Chapter 167
153. e
Rosen 5th,
Chapter 133,
p. 1974
154. d
Rosen 5th,
Chapter 55
p.796
The ideal approach is to take any patient with suspected epiglottitis to the operating
room, administer anesthesia, and examine the airway with a laryngoscope while the
patient is anesthetized. If the diagnosis of epiglottitis is made, the patient can be
intubated. If it is ruled out, the patient can be returned to the ward or the emergency
department to continue the workup, secure in the knowledge that epiglottitis is not
present.
Button batteries that have passed the esophagus need not be retrieved in the
asymptomatic patient unless the cell is not passing through the pylorus after 48 hours
of observation, in which case endoscopic retrieval is the preferred option. Ipecac has
no place in the management of button battery ingestion.
Fractures suggestive of child abuse include spiral fractures caused by torsion (twisting)
of a long bone, and metaphyseal chip fractures, especially when present in infants less
than 6 months of age. While this is the most suspicious of the fractures described, it
must be emphasized that any of these fractures could result from abuse. Abuse must
always be considered as a possibility with injuries involving young children.
Henoch-Schönlein Purpura is an immunoglobulin A mediated systemic vasculitis
involving the small blood vessels supplying the skin, gastrointestinal tract, and joints.
The hallmark is a palpable, purpuric, or petechial rash most prominent on the lower
extremities and extending to the buttocks, which is the presenting complaint in ~50%
of patients. GI complaints are present in ~65% of patients, especially periumbilical,
dull pain resulting from bleeding into the intestinal wall. 25% - 50% of children
develop a self-limiting glomerulonephritis manifested by hematuria. There are no
specific tests to confirm HSP, and the diagnosis can be difficult if the classic rash is
absent. Screening tests such as urinalysis, BUN and creatinine, CBC, and coagulation
studies may be needed to rule out other pathologic diseases.
A helpful mnemonic is ARENA:
A = Abdominal pain
R = Rash
E = Edema
N = Nephritis
A = Arthralgias / arthritis
Trench foot develops slowly over hours to days and is initially reversible but if allowed
to progress will become irreversible. Chilblains, or pernio, is characterized by mild but
uncomfortable inflammatory lesions of the skin of bared extremities caused by chronic
intermittent exposure to damp, nonfreezing ambient temperatures. The zone of stasis
is the middle ground and is characterized by severe, but possibly reversible, cell
damage. It is here that treatment is directed. Early surgical intervention is not
indicated in the management of frostbite. Premature surgery has been an important
contributor to unnecessary tissue loss and poor results in the past. Refreezing
previously frozen tissue worsens the prognosis.
Most victims of bites by the brown recluse spider do not even know they were bitten.
Pain usually develops within 3 to 4 hours, and a white area of vasoconstriction begins
to surround the bite. A bleb then forms in the center of this area, and an erythematous
ring arises on the periphery. The lesion at this stage resembles a bull’s-eye. The bleb
darkens, necroses over the next several hours to days, and continues to spread slowly
and gravitationally, involving skin and subcutaneous fat.
57
155. A 25-year-old man was playing catch with his pet rattlesnake. He now complains of pain and
swelling in his hand and forearm, with perioral numbness, and vomiting. His blood pressure is
90/60 mmHg. He will require:
a. fluid resuscitation with fresh frozen plasma.
b. administration of 2 to 4 vials of antivenin.
c. measurement of coagulation factors and platelets.
d. immediate forearm fasciotomy.
e. non-narcotic pain medication, to avoid masking of respiratory symptoms.
156. Acetazolamide acts by inhibiting the enzyme carbonic anhydrase. This in turn:
a. reduces reabsorption of bicarbonate in the kidney, leading to bicarbonate diuresis and metabolic
acidosis, which produces compensatory hyperventilation.
b. increases the blood carbon dioxide level, allowing a respiratory acidosis and compensatory
diuresis.
c. slows the sodium-potassium ATPase pump, causing a natriuretic compensation for the leftwardshifting oxygen dissociation curve.
d. causes the kidney to reabsorb more bicarbonate ions, leading to a metabolic alkalosis, which
shifts the oxygen dissociation curve to the right to compensate for lower atmospheric pressures.
e. prevents acute mountain sickness by an unknown mechanism.
157. A 55-year-old male diver complains of back pain and urinary retention which started about one
hour after ascent from a dive. He most likely has:
a. bladder barotrauma.
b. lumbar strain.
c. envenomation by coelenterate species.
d. nitrogen narcosis.
e. decompression sickness.
158. Concerning High Altitude Pulmonary Edema (HAPE):
a. it is the most lethal of the altitude illnesses.
b. women are more susceptible than men.
c. salt deprivation is a risk factor; use of a sleeping medication is somewhat protective.
d. early symptoms include a moist cough with blood-tinged sputum; rales are universally present.
e. the condition typically improves at night.
159. Choose the correct statement concerning electrical burns.
a. When tissue carbonization occurs, resistance to current flow decreases even further.
b. Contact with low voltage long distance communications lines and telephone can cause death in
certain circumstances.
c. A very narrow range exists between the threshold of perception of current and the level above
which a person becomes unable to release the current source because of muscular tetany.
d. The foot is the most common body part involved in alternating current injuries.
e. Sweating increases resistance against electricity.
160. Which of these patients requires admission to a burn-care facility?
a. A 35-year-old man with extensive partial-thickness burns on the back, shoulders, and buttocks.
b. A 60-year-old diabetic with a full-thickness burn of the entire forearm.
c. A 25-year-old woman with full-thickness burns of both hands and lower arms.
d. A 40-year-old house-fire victim with multiple, small partial-thickness burns and wheezing.
e. All of the above
58
155. c
th
Rosen 5 ,
Chapter 55,
156. a
Rosen 5th,
Chapter 138,
p. 2041
157. e
Rosen 5th,
Chapter 137,
p. 2024
158. a
Rosen 5th,
Chapter 138,
p. 2042
159. c
Rosen 5th,
Chapter 136,
p.
160. e
Rosen 5th,
Chapter 56,
p. 812, Box
56-2
Patients admitted to the hospital after poisonous snakebite should have serial
determinations of platelets, prothrombin time, and urinalysis to check for myoglobin
and hemoglobin. Daily comprehensive laboratory tests should be performed.
Fasciotomy is not usually indicated unless compartment pressures are elevated.
Antivenin (Crotalidae) polyvalent is the mainstay of therapy for poisonous snakebite;
usually 10 vials or more are required. Debridement should probably not be performed
earlier than 3 days after the bite, until the coagulopathy has resolved.
Acetazolamide is a carbonic anhydrase inhibitor that induces a renal bicarbonate
diuresis causing a metabolic acidosis, thereby increasing ventilation and arterial
oxygenation. The diuretic effects may be of benefit for the fluid retention common in
AMS. The drug also lowers CSF volume and pressure, which may play an additional
role in its therapeutic and prophylactic use.
The central nervous system is particularly susceptible to decompression illness because
of its high lipid content. The spinal cord, especially the upper lumbar area, is more
often involved than cerebral tissue. Symptoms of spinal DCS include limb weakness
or paralysis, paresthesias, numbness, and low back and abdominal pain. Bladder
symptoms, such as urinary retention, can occur, as well as fecal incontinence and
priapism.
High Altitude Pulmonary Edema (HAPE) is the most common fatal manifestation of
severe high-altitude illness. It can occur, and even be fatal, at altitudes as low as 8000
feet. Many patients have a single episode of HAPE and subsequently are able to return
to high altitude without a recurrence. Others who have had uneventful high-altitude
exposures may have HAPE develop on a future ascent.
A very narrow range exists between the threshold of perception of current (0.2 to 0.4
mA) and the let-go current (6 to 9 mA), the level above which a person becomes
unable to release the current source because of muscular tetany. When tissue
carbonization occurs, resistance to current flow increases. No deaths are recorded
from contact with low voltages associated with long distance communications lines
(24V) or telephone lines (65V). The hand is the most common site of contact via a
tool that is in contact with an AC electric source. Sweating can reduce the skin’s
resistance from 10 – 40,000 ohms to 2500-300 ohms.
1. Partial- or full-thickness burns involving >10% of body surface area (BSA) in
patients under 10 or over 50 years of age.
2. Partial- or full-thickness burns of >20% of BSA in other age groups.
3. Partial- or full-thickness burns with the threat of functional or cosmetic impairment
that involve face, hands, feet, genitalia, perineum, or major joints.
4. Full-thickness burns of >5% of BSA in any age group.
5. Electrical burns, including lightning injury.
6. Chemical burns with the threat of functional or cosmetic importance.
7. Inhalation injury with burns.
8. Circumferential burns of the extremities or chest.
9. Burn injury in patients with preexisting medical disorders that could complicate
management, prolong recovery, or affect mortality.
10. Any burn patient with concomitant trauma, such as fracture.
59
161. Concerning victims of near-drowning:
a. “dry drowning” without aspiration results from laryngospasm and glottal closure.
b. electrolyte abnormalities contribute significantly to mortality.
c. hemolysis resulting in anemia is found in more than half of fresh-water victims.
d. disseminated intravascular coagulation is a common finding.
e. postural drainage or the abdominal thrust (Heimlich maneuver) is recommended by most experts
as a way to remove water from the lungs and improve oxygenation.
162. After radiation exposure, the best predictor of hematopoietic involvement is the:
a. Absolute neutrophil count at 24 hours.
b. Absolute neutrophil count at 48 hours.
c. Absolute lymphocyte count at 24 hours.
d. Absolute lymphocyte count at 48 hours.
e. Absolute platelet count at 24 hours.
163. A 35-year-old man presents complaining of headache, weakness, nausea, and vomiting after
working with paint remover in an enclosed space. You know that:
a. a special antidote kit is required.
b. treatment must continue longer in patients with this exposure than from other sources.
c. the patient's oxygen-hemoglobin dissociation curve is shifted to the right.
d. severe metabolic acidosis may be present.
e. methylene blue may be required.
164. A 25-year-old photographer is found slumped over his workbench in the back of his store. Minutes
earlier he had complained of headache, dizziness, and weakness. Presently the patient is comatose
and apneic with a thready pulse. Cyanosis is absent. A venous blood sample drawn by paramedics
in the field is noted to be very red. Laboratory results reveal a high anion gap acidosis. Blood gas
determinations on arterial and venous blood samples reveal nearly identical pO2 values.
Carboxyhemoglobin is 5%. Although the patient is intubated and being hyperventilated with 100%
oxygen, the acidosis persists. What is the proper management?
a. administer methylene blue IV
b. administer physostigmine and hydroxocobalamin (vitamin B12a)
c. administer 2-PAM
d. administer sodium nitrite IV, then infuse sodium thiosulfate
e. transfer the patient to a facility with a hyperbaric chamber
165. In a mass casualty situation involving a large number of victims of a “dirty bomb,” the highest
priority patients are those:
a. who are critically injured and contaminated.
b. with external local body radiation only.
c. with external total body radiation only.
d. with internal contamination.
e. with external contamination.
166. A 24-year-old man was bitten on the arm by his girlfriend’s cat six hours ago. He now has warmth
and erythema at the site. The infecting organism is most sensitive to:
a. gentamicin.
b. metronidazole.
c. clindamycin.
d. penicillin.
e. fluconazole.
60
161. a
th
Rosen 5 ,
Chapter 139,
p. 2051
162. d
Rosen 5th,
Chapter 140,
p. 2058-2059
163. b
Rosen 5th,
Chapter 152,
p. 2159-2162
164. d
Rosen 5th,
Chapter 153,
p. 2166-2168
165. a
Rosen 5th,
Chapter 140,
p. 2060-2062
166. d
th
Rosen 5 ,
Chapter 54,
p. 775-776
In a small number of submersion victims, severe laryngospasm causes hypoxia,
convulsions, and death in the absence of active aspiration (“dry” drowning). Most
drowning victims do not aspirate enough fluid to cause life-threatening changes in
blood volume or serum electrolyte concentrations. Although DIC has been reported, it
is uncommon. Procedures to drain fluid from the lungs are ineffective and potentially
dangerous because of the increased risk of vomiting and aspiration. If particulate
material is obstructing the airway, the Heimlich maneuver may be of benefit but it is
not indicated for the removal of fluid.
The absolute lymphocyte count 48 hours after exposure is a good predictor of
hematopoietic involvement. If the absolute lymphocyte count is greater than 1200, it is
unlikely that the patient has received a fatal dose of radiation. If the absolute
lymphocyte count falls between 300 and 1200 at 48 hours, the possibility of exposure
to a lethal dose of radiation should be suspected. A level in this range is an indication
for hospitalization. Levels less than 300 are critical, and heroic procedures such as
bone marrow transplant and the use of hematopoietic growth factors may be
considered in individual cases.
Carbon monoxide (CO) toxicity can develop when inhaled methylene chloride vapor in
paint strippers or from leaking "bubble" electric Christmas tree lights is slowly
metabolized to produce CO. The elimination half-life of CO from methylene chloride
is about twice that of inhaled CO because it is stored in tissues and gradually released.
The binding of CO to hemoglobin transforms the oxyhemoglobin dissociation curve
from a sigmoid shape to an asymptotic shape, increasing the ability of HbCO to hold
on to oxygen at the remaining heme moiety sites. In CO toxicity, both the reduced
oxygen carriage and the transformation of oxyhemoglobin dissociation curve impair
tissue oxygen delivery. In effect, high HbCO imposes the equivalent of a sudden
“chemical” anemia in the patient.
Cyanide in its salt form (e.g., sodium or potassium) is important in the metallurgic
(e.g., jewelry) and photographic industries. Cyanide salts do not have an odor under
dry conditions. Since cyanide prevents tissue extraction of oxygen from the blood, the
oxygen content of venous blood approaches that of arterial blood. Clinically this may
appear as the “arterialization,” or brightening, of venous blood to resemble arterial
blood. Although the exact mechanism of the cyanide antidote kit is controversial, the
accepted goal of therapy is to reactivate the cytochrome oxidase system by providing
an alternative, high-affinity source of ferric ions (Fe3+) for cyanide to bind. Sodium
nitrite and sodium thiosulfate are the active ingredients in the kit.
If treatment of great numbers of radiation exposed and contaminated patients is
necessary, resuscitation and stabilization always takes precedence over
decontamination. However, health care workers must not expose themselves.
Protection of health care workers from injury takes priority over the patient's ABCs'.
Pasteurella multocida is the major pathogen found in infected cat bite wounds, isolated
in up to 80%. Infection is characterized by a rapidly developing, intense inflammatory
response, often within a few hours and rarely more than 24 hours after the bite. Pain
and swelling are prominent. The antibiotic best used to treat the major organism in this
presentation is penicillin.
61
167. Your friend has just stepped on a jellyfish while swimming. He is tearful because of the pain. You
can offer temporary relief by:
a. drying the area.
b. rinsing the site with ethanol.
c. rinsing the site with fresh water.
d. rinsing the site with milk.
e. rinsing the site with salt water.
168. The vast majority of mushroom-related fatalities in North America are due to:
a. coprine-induced disulfiram-like reaction when consumed with ethanol.
b. cyclopeptide-induced liver and renal failure.
c. monomethylhydrazine-induced seizures and hepatorenal failure.
d. muscarine-induced "SLUDGE" syndrome.
e. psilocybin-induced hallucinations and seizures.
169. A 16-year-old girl ingested an unknown plant an hour ago. Now she is tachycardic with mydriasis,
decreased bowel sounds, altered vision, and abnormal mental status. After ensuring the basic
ABCs, your next action should be:
a. intravenous atropine.
b. GI decontamination.
c. isotonic intravenous fluid administration.
d. subcutaneous physostigmine.
e. intramuscular glucagon.
170. A hiker on the Appalachian Trail is bitten on the hand by a snake, which was positively identified
as having red bands next to yellow bands. She describes mild pain at the site of the bite, but is
otherwise asymptomatic. Your recommended treatment is:
a. admission to the hospital for observation only.
b. discharge after extended observation.
c. discharge after routine wound care.
d. administration of antivenin if the patient becomes symptomatic.
e. immediate administration of antivenin.
171. Which is the typical sequence of cardiac arrhythmic deterioration in a patient whose core
temperature is below 30oC (86oF).
a. atrial fibrillationventricular fibrillationpulseless electrical activityasystole
b. sinus bradycardiaventricular tachycardiaventricular fibrillationasystole
c. sinus bradycardiaatrial fibrillationventricular fibrillationasystole
d. atrial fibrillationatrial flutterventricular fibrillationasystole
e. sinus bradycardiaatrial flutteratrial fibrillationfine ventricular fibrillation
172. A 25-year-old man notices burning pain in his arm while retrieving logs from a woodpile. Within
six hours, he has developed a necrotic area surrounded by an erythematous ring. He then notices
fever, myalgias, nausea and generalized weakness. Of those listed, the most likely cause is:
a. acute contact dermatitis.
b. brown recluse spider bite.
c. splinter from maple bark.
d. deer tick bite.
e. black widow spider bite.
62
167. e
th
Rosen 5 ,
Chapter 55,
p. 797-798
168. b
th
Rosen 5 ,
Chapter 144,
p. 2203-2205
169. b
Rosen 5th,
Chapter 144,
p. 2081-2081
Chapter 158,
p. 2199-2201
170. e
Rosen 5th,
Chapter 55,
p. 789-792
171. c
Rosen 5th,
Chapter 134,
p. 1989-1990
172. b
Rosen 5th,
Chapter 55,
p. 795-796
Jellyfish envenomation sites should be washed off with salt water from the ocean, as
fresh water is reported to worsen the pain.
Cyclopeptides such as amatoxin, found in certain amanita species, produce a threephase pattern of toxicity with early GI effects followed by a quiescent phase during
which the patient may be released from medical care. The devastating third phase
results in severe hepatic and sometimes renal toxicity. Ninety-five percent of North
American deaths from mushroom poison are due to these toxins. While
monomethylhydrazine poisoning from the Gyromitra species may have 10 – 40%
mortality, this poisoning is much less common and thus yields fewer fatalities.
Poisoning due to mushrooms containing muscarine, psilocybin, or coprine generally
responds well to supportive measures and antidotal therapy.
Anticholinergic toxicity commonly occurs with jimsonweed ingestion. This plant
contains belladonna alkaloids such as atropine, scopolamine, and ecgonine. After
assuring the ABC's, treatment includes GI decontamination with emesis or lavage,
activated charcoal, and supportive care (IV fluids, external cooling, and restraints for
patient protection). GI decontamination may be useful for up to 48 hours after
ingestion if the patient remains symptomatic. Isotonic fluid administration is the first
line treatment for hypotension. Many authorities recommend treatment of "full-blown"
anticholinergic syndrome with physostigmine, but reports of asystole, ventricular
arrhythmia, hypotension, bronchospasm, and seizures have occurred.
“Red on yellow, kill a fellow; red on black, venom lack.” This applies to women
victims, too. Anyone bitten by the Eastern coral snake (Micrurus fulvius) should be
given the antivenin even before any symptoms develop. The toxicity of this venom
has a rapid onset, and once the symptoms develop, it may be too late to reverse the
effects with antivenin. The recommended dose is three to five vials in 300 to 500 ml
of normal saline.
Patients are at risk for dysrhythmias at body temperatures below 30°C (86°F); the risk
increases as body temperature decreases. Although various dysrhythmias may occur at
any time, the typical sequence is a progression from sinus bradycardia to atrial
fibrillation with a slow ventricular response, to ventricular fibrillation, and ultimately,
to asystole.
As the name implies, the brown recluse spider is a reclusive organism. Humans
encounter this spider in attics, storage sheds, crawl spaces, and woodpiles. Encounters
with humans are uncommon. Brown recluse spiders are not aggressive and bite
humans in self-defense. The venom results in epidermal and subcutaneous necrosis.
This reaction is a local process around the bite site. About 6 to 8 h after the bite, pain
associated with a red-to-violaceous discoloration develops.
63
173. When resuscitating a hypothermic patient whose core temperature is <85oF you should:
a. administer prophylactic lidocaine.
b. move the patient as little as possible.
c. pronounce the patient dead if there is no cardiac response after rewarming to 90oF.
d. use Ringer's lactate as the intravenous fluid of choice.
e. massage extremities and apply heating blanket.
174. A diver was stung by a stingray and has severe pain, which you can relieve by:
a. applying ice packs.
b. applying vinegar.
c. immersing his leg in hot water.
d. urinating on his leg.
e. using a topical slurry of sodium bicarbonate.
175. The delayed complications of fetal hemorrhage into maternal circulation are of most concern in a
woman:
a. taking steroids.
b. who is Rh-negative.
c. with beta-thalassemia.
d. with alpha-thalassemia.
e. with sickle trait.
176. A 36-week pregnant woman presents in shock with painful vaginal bleeding and a hard, tender
uterus. She most likely has:
a. eclampsia.
b. endometritis.
c. placenta previa.
d. threatened abortion.
e. abruptio placenta.
177. A 28-year-old woman is brought to your Emergency Department by ambulance in cardiopulmonary
arrest after an automobile collision. Cardiopulmonary resuscitation was started approximately 4
minutes prior to arrival. Her husband is in the next room, crying hysterically. “She’s due with our
first baby next month.” Judging from her fundal height you estimate that the fetus is at 34-weeks
gestational age. You are the only physician in the hospital, covering a Level II trauma center. Your
most appropriate next action is:
a. page the obstetrician.
b. start a tocolytic agent and page the obstetrician.
c. pronounce the patient dead.
d. continue ACLS and page the trauma surgeon.
e. perform perimortom cesarean delivery.
178. The earliest that a serum beta-hCG test can detect pregnancy is:
a. shortly before a missed period.
b. during the time of an expected period.
c. 2-weeks after a missed period.
d. 4-weeks after a missed period.
e. 6-weeks after a missed period.
64
173. b
th
Rosen 5 ,
Chapter 134,
p. 1989-1994
174. c
Rosen 5th,
Chapter 55,
p. 797-799
175. b
Rosen 5th,
Chapter 172,
p. 2424-2425
176. e
Rosen 5th,
Chapter 172
p. 2420
177. e
Rosen 5th,
Chapter 31,
p. 264
178. a
Rosen 5th,
Chapter 171,
p. 2404-2405
The hypothermic myocardium is extremely irritable, and ventricular fibrillation may be
induced by a variety of manipulations and interventions that stimulate the heart,
including rough handling of the patient. The activity of antiarrhythmic and
cardioactive drugs is unpredictable in hypothermia, and the hypothermic heart is
relatively resistant to atropine, pacing, and countershock.
The success of therapy for stings from marine animal spines depends on rapid
initiation. Treatment is directed at combating the effects of the venom, alleviating
pain, and preventing infection. The wound should be irrigated immediately, and any
visible pieces of the spine or integumentary sheath should be removed. As soon as
possible, the wound should be immersed in hot water to tolerance [45°C (113°F)] for
30 to 90 min or until there is pain relief. During the hot-water soak, the wound should
be explored and foreign material removed.
Rh immunization occurs when an Rh-negative female is exposed to Rh-positive blood
during pregnancy or delivery. The incidence of sensitization is about 16% when the
Rh-negative woman and Rh-positive fetus are ABO-compatible and 1% to 2% if they
are ABO-incompatible. Sensitization occurs most commonly at the time of delivery,
but transplacental hemorrhage can occur during threatened miscarriage (even without
fetal loss), spontaneous miscarriage, surgery for ectopic pregnancy, and amniocentesis.
Anti-D immune globulin (RhoGAM) should be administered when these events occur.
RhoGAM is routinely administered to Rh-negative mothers (if the father is Rh-positive
or his status is unknown) at about the 28th week of gestation to protect the mother
from spontaneous sensitization, which occurs during the third trimester. RhoGAM has
also been used to prevent further deterioration of fetal anemia in Rh-D immunizations
if started before severe fetal anemia and imminent hydrops fetalis arise. Minidose
RhoGAM has been used in some patients with early miscarriage or trauma.
Abruptio placentae, or separation of the placenta from the uterine wall, accounts for
about 30% of episodes of bleeding during the second half of pregnancy. Vaginal
bleeding occurs in 80% of patients with abruptio placentae. Blood is characteristically
dark and the amount is often insignificant, although the mother may have
hemodynamic evidence of significant blood loss. Uterine tenderness or pain is seen in
about two thirds of women; uterine irritability or contractions are seen in one third.
With significant placental separation, fetal distress occurs and the maternal coagulation
cascade may be triggered causing DIC.
The need to perform perimortem cesarean delivery in cases of maternal cardiac arrest
arises extremely infrequently. The time to delivery from the onset of maternal arrest
was found to be critical to fetal survival with good neurologic outcome. Excellent
outcomes were reported when delivery took place within 5 min of maternal death.
Survival was unlikely if delivery occurred after 20 min of maternal arrest.
Consideration of perimortem cesarean delivery must be made only after immediate and
optimal advanced maternal cardiopulmonary resuscitative measures have been
instituted. Successful maternal revival following fetal delivery has been reported.
Improved venous return to the central circulation, increased maternal oxygen delivery
following removal of the high uterine demand, and decreased pooling of blood in the
uteroplacental circulation have all been suggested explanations.
The quantitative beta-hCG analysis may be very helpful. It is first detectable as early
as 9 to 11 days following ovulation (usually 24 days after the last menstrual period)
and reaches 200 IU/mL at the expected time of menses.
65
179. A 20-year-old woman is 14 weeks pregnant. She has had vaginal spotting for eight hours. Her
vital signs are normal, including orthostatic readings. Her vaginal vault is normal; her cervical os is
closed. Because she is obese, you cannot estimate uterine size or adnexal structures, but feel that
there is no tenderness. Fetal heart tones are heard with a Doppler stethoscope at a rate of 150 beats
per minute. Her hematocrit is 35%. Optimal management includes:
a. conjugated estrogen 20 mg IM and observation for eight hours.
b. emergent gynecologic consultation to admit the patient for bed rest and fetal monitoring.
c. transvaginal ultrasound followed by fetal monitoring for 12 hours.
d. type and screen, administer Rho (D) Immune Globulin if Rh-negative.
e. discharge home on bed rest with OB follow-up in 24 hours.
180. A 23-year-old G3P2 patient who is 34 weeks by dates presents with acute abdominal pain and heavy
dark vaginal bleeding. Her blood pressure is 78/32 mmHg. When the nurse draws blood and starts
an intravenous line, the patient oozes blood from the IV site. She also has a nosebleed. A DIC
panel will probably show:
a. diminished fibrin split products.
b. negative d-dimer.
c. prolonged prothrombin time.
d. elevated fibrinogen levels.
e. normal platelets.
181. A 28-year-old female insulin-dependant diabetic who is 16 weeks pregnant complains of 2 days of
vomiting, shortness of breath, and high blood sugar. She has no known allergies. Her examination
shows oral temperature 100.0oF, heart rate 130 beats / minute, respiratory rate 28 / minute, and
blood pressure 100/70 mmHg. Her breath smells like fingernail polish, and her urine dips strongly
positive for ketones. Her bedside fingerstick glucose is 287 mg/dl. You suspect diabetic
ketoacidosis, knowing that in pregnancy:
a. DKA may develop at lower glucose values.
b. hyperemesis is seldom a precipitant.
c. maternal insulin and counter-regulatory hormones cross the placenta.
d. it is more frequently seen in patients with gestational diabetes than in those with juvenile
diabetes.
e. serum pH may be deceptively low.
182. A 15-year-old female presents by ambulance, complaining of sudden abdominal pain. She is pale
and diaphoretic. She is initially afebrile with heart rate 140 beats / minute, respiratory rate 20 /
minute, and blood pressure 60/0 mmHg. Her lungs are clear, and her heart is tachycardic. Her
abdomen is soft with bowel sounds present and no masses palpable. Her stool is brown stool and
negative for blood. Pelvic exam shows blood in the vault. She has a nonfocal neurologic exam, but
she loses consciousness as you examine her. Bedside glucose is 180 mg/dl. You assure the ABCs
and start two large bore antecubital intravenous lines. She does not respond to 0.8 mg of naloxone.
Your next step is:
a. call general surgeon, transfer to OR with probable ruptured appendix.
b. call obstetrics for emergent transfer to OR, type and screen.
c. send patient to radiology for abdominal and vaginal ultrasound.
d. await results of serum pregnancy and quantitative beta-hCG.
e. stat CT scan of abdomen and pelvis.
66
179. d
th
Rosen 5 ,
Chapter 171,
p. 2403-2406
Chapter 172,
p. 2417-2419
180. c
Rosen 5th,
Chapter 116,
p.1698,
Table 116-3
181. a
Rosen 5th,
Chapter 173,
p. 2440-2441
182. b
Rosen 5th,
Chapter 172,
p. 2416-2419
In a woman with first trimester pregnancy and vaginal bleeding, you must rule out
ectopic pregnancy and threatened miscarriage. A transvaginal ultrasound is not
indicated because the presence of fetal heart tones confirms the dates. Emergent
obstetric consultation is not indicated because she is hemodynamically stable.
Estrogens are not appropriate in pregnancy. It is important to assess the woman's Rh
status and give RhoGAM if appropriate.
MOST USEFUL
Prothrombin time
Platelet count
Fibrinogen level
Prolonged
Usually low
Low
HELPFUL
aPTT
Usually prolonged
Thrombin clot time
Prolonged
Fragmented RBCs
Should be present
Feibrin split products Elevated
D-dimers
Elevated
About 10% of insulin-dependent diabetics will develop ketoacidosis at some point
during pregnancy. DKA occurs more rapidly and at lower glucose levels in pregnant
patients as compared with nonpregnant patients. Hyperemesis and noncompliance or
errors in insulin dosage are the most common precipitants. Admission is often
indicated to correct dehydration and more carefully adjust glucose control. The serum
pH may be deceptively normal in the pregnant patient, because the initial pH tends to
be higher in pregnancy due to physiologic hyperventilation. DKA is rare in patients
with gestational diabetes, and insulin and counter-regulatory hormones do not cross the
placenta.
Unstable patients suspected of ectopic pregnancy should receive resuscitation, urgent
consultation, and operative intervention. Surgery may be both diagnostic and
therapeutic if an EP is found or may reveal another cause for the patient’s condition.
When bedside ED sonography is available, it may be valuable even in unstable patients
if it does not interfere with resuscitation, consultation, and rapid transfer to the
operating room.
67
183. Concerning the diagnosis of appendicitis during pregnancy:
a. diagnosis of appendicitis is delayed because x-rays are not taken.
b. positive urinary WBC esterase and bacterial nitrite are usually seen in appendicitis.
c. the appendix rotates from McBurney's point as pregnancy progresses, ultimately lying near the
midline in the upper abdomen.
d. the incidence of appendicitis is increased in pregnancy.
e. the incidence of perforated appendix is increased in pregnancy.
184. A woman who is 30-weeks pregnant is involved in a motor vehicle crash and sustains a spiral
fracture of the right humerus. She is hemodynamically stable and has an otherwise normal physical
exam. In addition to treating her orthopedic injury, you know she needs:
a. abdominal CT scan
b. ECG
c. fetal monitoring
d. urine pregnancy test
e. urine toxicology screen
185. A 26-year-old woman has dysuria for one week. She denies fever, nausea, vomiting, and back pain.
She does admit to having a new sexual partner over the past month. Her pelvic examination shows
a small amount of whitish discharge from the cervical os but is otherwise normal. Urinalysis shows
10 WBCs, 0 RBCs, no epithelial cells, and no bacteria. Her most likely diagnosis is:
a. pyelonephritis secondary to E. coli infection.
b. cystitis secondary to E. coli infection.
c. urethritis secondary to Chlamydia infection.
d. cervicitis secondary to gonorrheal infection.
e. vaginitis secondary to candida infection.
186. You are using serial quantitative beta-hCG tests to assess the health of a fetus in a patient with first
trimester threatened abortion. You know that in a healthy pregnancy with a normal fetus the level:
a. doubles every two to three days.
b. doubles every seven days.
c. triples every two to three days.
d. triples every seven days.
e. will not change by more than 10% during the first 12 weeks of pregnancy.
187. You are arranging transportation for a 23-year-old woman who fell down some stairs and fractured
her pelvis. She is 28 weeks pregnant by bedside ultrasound. Her blood pressure is 64 palpable.
The position best for her to travel is:
a. 60o Trendelenberg.
b. tilted 15o to the left.
c. tilted 45o to the right.
d. with her head elevated 45o.
e. lying on her right side.
188. The most common manifestation of gonococcal infection in children is:
a. salpingitis.
b. cervicitis.
c. pharyngitis.
d. vaginitis.
e. conjunctivitis.
68
183. e
th
Rosen 5 ,
Chapter 172,
p. 2425-2427
184. c
Rosen 5th,
Chapter 31,
p. 262-264
185. c
Rosen 5th,
Chapter 94,
p. 1395-1396
186. a
Rosen 5th,
Chapter 172,
p. 2418
187. b
th
Rosen 5 ,
Chapter 31,
p. 256 & 264
188. d
th
Rosen 5 ,
Chapter 93,
p. 1395
Appendicitis is the most common surgical emergency in pregnancy. Appendectomy is
one of the most common laparoscopic procedures performed during pregnancy, second
only to cholecystectomy. The incidence of appendicitis in pregnancy is unchanged
from the nonpregnant state, but delays in diagnosis contribute to an increased rate of
perforation. During the first half of pregnancy, diagnostic findings are usually similar
to those in the nonpregnant female, but the clinical picture becomes less classic during
the second half. During pregnancy the appendix is displaced counterclockwise out of
the right lower quadrant so that by the last trimester, the appendix is located deep in the
right upper quadrant, superior to the iliac crest. Proximity to the ureter, and during
later pregnancy to the kidney itself, leads to an increased incidence of sterile pyuria in
the pregnant patient who has appendicitis, further confounding the diagnosis.
Fetal evaluation in the secondary survey focuses on the fetal heart rate and noting any
fetal movement. Once the presence of fetal heart tones has been confirmed,
intermittent monitoring of fetal heart rate is sufficient for the pre-viable fetus. If the
fetus is viable (i.e., 24 weeks or more), continuous external monitoring should be
initiated quickly and maintained throughout all diagnostic and therapeutic procedures.
Such monitoring can also benefit the mother because fetal hemodynamics are more
sensitive to decreases in maternal blood flow and oxygenation than are most maternal
measures. Fetal distress can be a sign of occult maternal distress. Signs of fetal
distress include an abnormal baseline rate, decreased variability of heart rate, and fetal
decelerations after contractions.
Chlamydial urethritis may be present in up to 20% of women with dysuria. The
history of a new sexual partner, the gradual onset of symptoms, the discharge from the
os, and the sterile pyuria are all consistent with chlamydial urethritis. The lack of
fever, vomiting, and back pain make pyelonephritis less likely.
Serum beta-HCG levels normally double every 1.8 to 3 days for the first 6 to 7 weeks
of pregnancy, beginning 8 to 9 days after ovulation.
For pregnant patients beyond 20 weeks of gestation who must be transported in the
supine position or in whom spinal immobilization is indicated, a wedge should be
placed under the right hip area tilting the patient toward her left side to avoid
hypotension from inferior vena cava compression by the gravid uterus.
Vaginitis is the most common gonococcal infection in children. The thin, friable
genital mucosa of the prepubescent girl is susceptible to gonococcal infection, resulting
in copious, purulent vaginal discharge. Obtain specimens from the child at the vaginal
introitus. Vaginitis, scalp infection, bacteremia, arthritis, meningitis, and endocarditis
are manifestations of gonorrhea in the newborn.
69
189. HELLP stands for:
a. hepatitis – elevated lipids – low platelets
b. hemolysis – elevated lipids – low platelets
c. hepatitis – elevated liver enzymes – low platelets
d. hemolysis – elevated liver enzymes – low platelets
e. herpes – extrophic labia – lumbar pernio
190. In a patient with genital herpes:
a. HSV-1 accounts for up to 50% of the cases of genital herpes.
b. systemic acyclovir decreases the frequency of recurrences.
c. systemic symptoms are common with the initial presentation of genital herpes.
d. Tzanck smears are positive in the majority of cases.
e. cultures of fluid obtained from herpes vesicles are positive only a third of the time.
191. In the patient with sinusitis:
a. CT scans of the sinuses are the "gold standard" for diagnosing the disease.
b. ethmoid sinusitis pain is made worse when the patient sits up.
c. maxillary sinusitis pain is made worse by placing the patient supine.
d. phenylephrine or oxymetazoline decongestants should be avoided, as they can irritate the nasal
mucosa.
e. the Water's view is most helpful in finding ethmoid sinusitis.
192. The most common agent causing infectious pharyngitis in an adult is:
a. Chlamydia trachomatis.
b. group A beta-hemolytic streptococcus.
c. Neisseria gonorrhoeae.
d. viral.
e. pneumococcus.
193. A 65-year-old woman has swelling at the base of her tongue and a "bull neck". She is an insulindependent diabetic. You find brawny induration of the floor of the mouth. She is ill appearing but
is not in any respiratory distress. You should:
a. incise and drain the area of swelling.
b. admit the patient to the ICU for close monitoring of possible airway obstruction.
c. start IV antibiotics in the ED and admit her to the general medical floor.
d. discharge home on outpatient antibiotics with ENT follow-up the next day
e. consult a dentist for probable tooth extraction.
194. Ménière’s disease is characterized by vertigo and:
a. fever.
b. hearing loss.
c. headache.
d. blurred vision.
e. facial nerve paralysis.
195. Concerning nosebleeds:
a. anterior epistaxis accounts for 75% of nosebleeds.
b. anterior epistaxis requires immediate consultation with an otolaryngologist.
c. anterior epistaxis usually originates from the turbinates of the lateral wall of the nasal cavity.
d. posterior epistaxis is less likely to require hospitalization than anterior epistaxis.
e. posterior epistaxis usually occurs from the posterior branch of the sphenopalatine artery.
70
189. d
th
Rosen 5 ,
Chapter 172,
p. 2422-2423
190. c
Rosen 5th,
Chapter 93,
p. 1392
191. a
Rosen 5th,
Chapter 70,
p. 981-984
192. d
Rosen 5th,
Chapter 70,
p. 969-971.
193. b
Rosen 5th,
Chapter 65,
895-896
Chapter 70,
p. 977-978
194. b
Rosen 5th,
Chapter 13,
p. 125-127
195. e
Rosen 5th,
Chapter 67,
p. 933-935
The HELLP syndrome (an acronym for hemolysis, elevated liver enzymes, and low
platelets) is an important clinical variant of preeclampsia that has a predilection for the
multigravid patient, in contrast to the primigravida, in whom preeclampsia is more
common. In the HELLP syndrome, the blood pressure is variable and may not be
elevated initially. This fact, combined with the usual complaint of epigastric or right
upper quadrant pain, makes it easy to mistake the HELLP syndrome for other causes of
abdominal pain, such as gastroenteritis, hepatitis, pancreatitis, cholecystitis, or
pyelonephritis.
Overall, 85 to 90% of genital herpes infections are caused by HSV-2. There may be
both local and systemic manifestations. Cultures are positive 85 to 95% of the time.
Usually, initial infection is more severe and lasts longer than do subsequent
recurrences. A Tzanck smear stained with either Wright or Giemsa stain is positive in
up to 50% of cases. Systemic antiviral agents provide partial control of the signs and
symptoms and accelerate healing of the lesions, but do not affect the frequency or
severity of recurrences.
The best method for imaging the sinuses is to perform a CT. The Waters view is a
plain x-ray that best shows the maxillary sinuses and can provide good views of the
frontal sinuses. Maxillary sinusitis is usually made worse when the patient leans
forward, while assuming the supine position exacerbates ethmoid sinusitis.
Decongestants are an important part of treatment, allowing drainage of the sinuses.
Prolonged use of these agents can cause a rebound inflammation on cessation.
Causal agents of pharyngitis include viruses, bacteria, fungi, and parasites. Most often,
viruses are the culprits. Rhinovirus and adenovirus are the most common, but EpsteinBarr virus, herpes simplex virus, influenzavirus, parainfluenzavirus, and coronavirus
are responsible for about 5% of the infections.
Cellulitis of bilateral submandibular spaces and the lingual space is called Ludwig´s
angina and is potentially life threatening. It is a rapidly spreading cellulitis that results
in brawny induration of the suprahyoid region and elevation of the tongue.
Involvement of the floor of the mouth pushes the tongue posteriorly. Epiglottic
involvement is not uncommon. As a result, airway compromise is the immediate
primary concern. The primary focus of initial management is maintenance of a patent
airway. Timely administration of high- dose penicillin and metronidazole or cefoxitin
is essential. Immediate oral and maxillofacial surgical consultation and hospitalization
for incision and drainage and intubation as indicated are necessary.
With Ménière’s disease the onset of vertigo is usually sudden, and duration ranges
from 20 minutes to 12 hours. It is associated with nausea, vomiting, and diaphoresis.
The frequency of attacks can vary from several times per week to several times per
month. Between attacks, the patient is usually well, although deafness may persist.
Other hallmarks of the diagnosis include associated symptoms such as roaring tinnitus,
diminished hearing, and fullness in one ear.
Anterior epistaxis is responsible for 90% of nosebleeds. It usually arises from the
anterior-inferior nasal septum from vessels known as Kiesselbach's plexus. Although
posterior epistaxis requires consultation with an otolaryngologist and hospitalization,
most anterior bleeds can be managed on an outpatient basis without immediate
consultation of a specialist. The most common site of posterior bleeds is the posterior
branch of the sphenopalatine artery.
71
196. Necrotizing external otitis is almost always caused by:
a. group A beta-hemolytic streptococcus.
b. Staphylococcus aureus.
c. E. coli.
d. Pseudomonas aeruginosa.
e. aspergillus.
197. Central retinal vein occlusion:
a. causes brief, transient blindness or flickering vision.
b. causes a pale retina and optic disc with “boxcar” segmentation of the retinal veins.
c. is secondary to embolic phenomenon.
d. is treated with eye massage, acetazolamide, timolol, and increasing the inhaled pCO2.
e. has a wide range of clinical appearances.
198. A 4-year-old child has purulent nasal discharge from the left nostril for 4 days. She flails her arms
and shakes her head vigorously when you attempt to examine her, but you notice a bead from a toy
necklace partially occluding the left nostril. You should:
a. send her home on oral antibiotics with assurance to mom that the object will dislodge itself.
b. instill topical vasoconstrictor into the nostril and attempt blind removal with a right angle hook.
c. obtain an X-ray of the nasal bones.
d. under conscious sedation, grasp the object with a suction catheter taking precautions against
pushing the foreign body further back into the nasopharynx.
e. consult ENT for referral to the operating room.
199. An 18-year-old man presents with right ear pain and discharge. Temperature 39oC (102.2oF). You
find a perforated right tympanic membrane with purulent drainage, and a tender swelling over the
mastoid area. The most appropriate treatment is:
a. admit, culture drainage, start IV antibiotics, obtain urgent otolaryngology consultation.
b. admit patient on antibiotic ear drops with routine consult otolaryngology.
c. discharge on oral antibiotics to follow-up with an otolaryngologist in one week.
d. incise and drain mastoid area, then discharge on oral antibiotics.
e. topical sulfacetamide drops for 7 days.
200. A 32-year-old woman is struck in the left eye with a tennis ball. She complains of pain but denies
flashes of light, floaters, diplopia, or a decrease in vision. On initial evaluation her visual acuity is
20/20 vision in each eye, she has orbital emphysema, and her extraocular muscles and globe are
intact. Shortly after arrival she complains of suddenly decreased visual acuity. You should now:
a. ballotte the globe in an attempt to dislodge the clot causing the central retinal artery occlusion.
b. intraorbital needle aspiration or lateral canthotomy with cantholysis to release pressure under the
orbit.
c. ophthalmologic consult for traumatic retinal tear with vitreous hemorrhage.
d. topical cycloplegics (5% homatropine) to the affected eye for treatment of traumatic iridocyclitis
with an ophthalmologic follow-up.
e. anterior chamber paracentesis.
72
196. d
th
Rosen 5 ,
Chapter 67,
p. 932
197. e
Rosen 5th,
Chapter 66,
p. 921
198. d
Rosen 5th,
Chapter 53,
p. 756-757
199. a
th
Rosen 5 ,
Chapter 67,
p. 932-933
200. b
Rosen 5th,
Chapter 66,
p. 909
Previously known as malignant otitis externa because of its high mortality, necrotizing
external otitis is an extremely aggressive form of otitis externa. It occurs primarily in
adults with diabetes mellitus but has also been seen rarely in immunocompromised
children. Pseudomonas is the predominant pathogen, but S. aureus, S. epidermidis,
Proteus mirabilis, Klebsiella, Aspergillus, and Salmonella have all been described.
Central retinal vein occlusion (CRVO) symptoms are similar to those of central retinal
artery occlusion (CRAO) in that there is a painless loss of vision. Brief transient
blindness is uncommon. A pale retina and optic disc with boxcar segmentation are
seen in CRAO. The degree of vision loss depends on the degree of ischemia and
ranges from mild to severe. CRAO results from embolic phenomenon, but not CRVO.
No treatment is necessary acutely for CRVO other than watching for elevation of
intraocular pressure consistent with neovascular glaucoma. Eye massage,
acetazolamide, timolol, and increasing the PCO2 are all indicated treatments for
CRAO.
With conscious sedation, a majority of nasal foreign bodies can be removed. If
attempts are unsuccessful, the patient should follow-up with an otolaryngologist within
one to two days.
Mastoiditis requires admission for antibiotic therapy. Antibiotic choices include
semisynthetic penicillin combined with chloramphenicol, or a third-generation
cephalosporin such as cefuroxime (50 to 150 mg/kg/day), or ceftriaxone (50 to 75
mg/kg/day), usually for 1 week. Surgical procedures may range from myringotomy
drainage and tympanostomy tube placement to mastoidectomy and drainage for more
extensive disease progression. Mastoidectomy is required in approximately half of
mastoiditis cases.
Orbital emphysema associated with orbital fractures is usually a benign, self-limited
condition. This patient however, is complaining of a sudden decrease in visual acuity
in the traumatized eye. The emergency physician must consider that air may have built
up under pressure in the orbit, causing cessation of blood flow in the central retinal
artery. The air must be released immediately or the patient may lose her vision. This
is done by performing a lateral canthotomy with cantholysis or intraorbital needle
aspiration of the trapped air. Ballottement of the globe will not benefit this patient
because the etiology of her visual loss is not embolic occlusion of the retinal artery.
Iridocyclitis following trauma is painful but should not be associated with loss of
visual acuity.
73
201. The most common complication of acute otitis media is:
a. brain abscess.
b. facial nerve paralysis.
c. hearing impairment.
d. labyrinthitis.
e. meningitis.
202. In a patient with suspected retropharyngeal abscess, the most appropriate initial
diagnostic study is:
a. magnetic resonance angiography of the neck.
b. direct laryngoscopy.
c. indirect laryngoscopy.
d. soft tissue lateral x-ray.
e. barium swallow.
203. A 23-year-old woman noticed that her right eye was red as she was putting on her makeup. She has no pain and denies any trauma. Her past medical history is unremarkable.
Her visual acuity is 20/20 in each eye. Her pupils are reactive, and the extraocular
muscles are intact. There are several patches of bright red blood scattered across the
sclera. Funduscopic exam is normal. You know that this patient needs:
a. reassurance.
b. outpatient workup for von Willebrand’s disease.
c. STAT ophthalmologic referral.
d. inpatient stay for trabeculoplasty.
e. referral to a hematologist.
204. A 15-year-old boy was punched in the right eye during a brawl at a local basketball court.
He complains of photophobia and a dull ache in the injured eye. Physical examination
shows visual acuity of 20/80 that corrects to 20/40 with a pinhole. The right pupil is dilated
and sluggishly reactive, but extraocular movements are intact. There is scleral and ciliary
injection. Slit lamp exam shows moderate cell and flare in the anterior chamber. He has:
a. traumatic cranial nerve III palsy.
b. conjunctivitis with traumatic lens dislocation.
c. conjunctivitis with iris sphincter rupture.
d. conjunctivitis with ruptured globe.
e. traumatic iridocyclitis.
205. The 39-year-old woman shown in this picture was struck in the eye while playing
racquetball. She complains of mild pain and
decreased vision. Her visual acuity is 20/100 with
pinhole. Her eye is shown. You need to treat her
with:
a. bed rest, head elevation, avoid reading.
b. pilocarpine 1% eye drops every 4 hours for 48
hours.
c. fresh frozen plasma.
Rosen 5th Edition, Figure 66-9
d. aminocaproic acid.
e. surgical wash out of the anterior chamber.
74
201. c
th
Rosen 5 ,
Chapter 67, p.
930
202. d
Rosen 5th,
Chapter 70, p.
979
203. a
th
Rosen 5 ,
Chapter 66, p.
912
204. e
th
Rosen 5 ,
Chapter 66, p.
913
205. a
th
Rosen 5 ,
Chapter 66, p.
912-913
Almost all children with otitis media will have temporary conductive hearing loss.
Sensorineural hearing loss is less common, but may contribute to the association of otitis media
with delayed speech, language, or cognitive development. Labyrinthitis, facial nerve paralysis,
meningitis, and extradural abscesses are also complications, but are far less common,
particularly in the postantibiotic era.
Radiographs and CT scans are helpful diagnostic tools in assessing a patient for retropharyngeal
abscess. A lateral soft-tissue radiograph of the neck taken during inspiration with moderate
cervical extension demonstrates thickening and protrusion of the retropharyngeal wall.
The fragile conjunctival vessels can rupture from trauma, sudden Valsalva pressure spikes
(sneezing, coughing, vomiting, straining), hypertension, or spontaneously with no discernible
etiology. No treatment is necessary, and the hemorrhage usually resolves within 2 weeks. If
multiple recurrent episodes occur, coagulation studies and further investigation are warranted.
Blunt injury of the globe may contuse and inflame the iris and ciliary body, resulting in ciliary
spasm. Patients complain of photophobia and deep aching eye pain. Examination reveals
perilimbal conjunctival injection (ciliary flush), cells and flare in the anterior chamber
(representing white blood cells and protein), and a small, poorly dilating pupil.
Management of hyphema must be individualized for a given patient. Selected low-grade
hyphemas in reliable patients may be managed on an outpatient basis. General therapy
includes elevating the bed 30 to 45 degrees, bed rest, and limiting eye movements such as
reading. Specific treatment for hyphema with miotics, mydriatics, cycloplegics, steroids, and
antifibrinolytics (such as aminocaproic acid) will vary depending on the specific clinical
situation, and is best left to the ophthalmologist.
75
206. Regarding acute traumatic retinal detachment:
a. most detachments can be visualized on standard funduscopy.
b. examination may reveal the typical “blood and thunder” retinal bleeding pattern.
c. the patient usually reports “flashing lights” which are due to retinal neuron stimulation.
d. visual outcome depends on the extent of involvement of the optic disc.
e. sudden onset of pain is a prominent feature.
207. A 62-year-old female with a history of hypertension, diabetes, and glaucoma complains of
sudden, painless loss of vision in her right eye. Visual acuity shows only hand-motion
recognition on the affected side. There is an afferent papillary defect and absent red reflex
on the right. You are unable to visualize the fundus. Slit lamp examination is normal. Her
most likely diagnosis is:
a. acute open-angle glaucoma.
b. central retinal artery occlusion.
c. central retinal vein occlusion.
d. optic neuritis.
e. vitreous hemorrhage.
208. The patient in question #207 is best treated with:
a. anterior chamber paracentesis.
b. expectant management with delayed phototherapy.
c. intravenous prednisolone.
d. ocular massage.
e. pilocarpine, intravenous acetazolamide, and urgent laser iridectomy.
209. A 19-year-old man was assaulted and robbed outside the baseball stadium after “bat day.”
He has an obvious mid-face fracture and unstable mandible. His left eye is mildly
proptotic with severe conjunctival swelling and a large subconjunctival hemorrhage.
Visual acuity is limited to counting fingers. His pupil is fixed and mid-point. You must now:
a. begin therapy with mydriatics and cycloplegics.
b. avoid sedation and analgesia, so as not to mask intracranial injuries.
c. begin therapy with local fibrinolytic injection.
d. apply a firm occlusive eye patch and arrange outpatient follow-up.
e. perform emergent lateral canthotomy.
210. A 75-year-old woman with diabetes and hypertension complains of abrupt onset of right
eye pain, blurred vision, unilateral headache, and mild nausea. Her visual acuity is 20/200
in the affected eye, which does not correct with pinhole. She has conjunctival injection
and a cloudy, edematous cornea. Her pupil is mid-point and nonreactive to light. Slit lamp
examination shows no corneal staining. You should now:
a. order erythrocyte sedimentation rate (ESR).
b. dilate her pupil and perform direct funduscopy.
c. order orbital CT with 3-mm cuts.
d. perform tonometry.
e. order an intraocular ultrasound.
76
206. c
th
Rosen 5 ,
Chapter 66, p.
914
207. e
Rosen 5th,
Chapter 66, p.
922
208. b
Rosen 5th,
Chapter 66, p.
922
209. e
th
Rosen 5 ,
Chapter 66, p.
910
210. d
Rosen 5th,
Chapter 66, p.
919-920
Retinal tears and detachments from blunt eye trauma are common. Symptoms include floaters
from bleeding, “flashing lights” from stimulation of retinal neurons, and visual field cuts or
decreased visual acuity. Retinal tears or detachments do not cause pain. Examination may
reveal the hazy gray membrane of the retina billowing forward, but many tears are located
peripherally and cannot be seen with direct ophthalmoscopy. Visual acuity will be normal
unless the macula is involved.
Vitreous hemorrhage results from bleeding into the preretinal space or vitreous cavity. The
most common causes are diabetic retinopathy and retinal tears. Symptoms begin as floaters or
“cobwebs” in the vision and may progress to severe painless vision loss over a few hours.
Direct ophthalmoscopy reveals reddish haze in mild cases to a black reflex in severe cases.
Vitreous hemorrhage by itself will not cause an afferent pupillary defect, but this finding will be
present if there is a retinal detachment behind the vitreous hemorrhage. Initial therapy consists
of bed rest with elevation of the head of the bed. Vascular retinopathy if treated with laser
photocoagulopathy or cryotherapy.
The patient has a retrobulbar hemorrhage which is impinging on the optic nerve and retinal
circulation. Immediate ophthalmologic consultation is warranted. If intraocular pressure is
increased, begin treatment with carbonic anhydrase inhibitors, topical beta blockers, and
intravenous mannitol. A lateral canthotomy can be done in the ED as a temporizing measure
before definitive decompression.
Attacks of primary angle closure glaucoma are precipitated by pupillary dilatation, which
increases the degree of pupillary block and leads to an accumulation of aqueous humor in the
posterior chamber. Symptoms are abrupt in onset and include severe eye pain, blurred vision,
headache, nausea, vomiting, and occasionally abdominal pain. Lab studies are not necessary,
and dilating the eye with a mydriatic agent will make the problem even worse.
77
211. The most appropriate initial therapy for the patient in question #210 is:
a. parenteral steroid therapy.
b. anterior chamber paracentesis.
c. beta-blocker ophthalmologic drops.
d. tropicamide ophthalmologic drops.
e. phenylephrine ophthalmologic drops.
212. A 73-year-old man has fevers to 103oF, with a stiff neck, headache, and slurred speech.
Your exam shows a sleepy patient who arouses to sternal rub. His right hand strength is
weak. His wife mentions that he had an endoscopic sinus polypectomy three days ago.
a. The patient almost certainly has meningitis; he requires an immediate lumbar puncture.
b. The patient almost certainly has encephalitis; he requires an immediate lumbar
puncture.
c. Since most strokes are not associated with alterations in mental status, this patient
requires an immediate lumbar puncture.
d. The patient probably has a brain abscess and will require neurosurgery.
e. He requires immediate treatment with steroids, mannitol, and antibiotics.
213. A complication from using phenobarbital to control status epilepticus is:
a. an anion gap metabolic acidosis.
b. a prolonged QT segment.
c. paradoxical elevation of blood pressure.
d. poor tolerance in pediatric patients.
e. prolonged obtundation.
214. You are evaluating a 29 year-old man with a history of AIDS and HIV encephalopathy for
deterioration in his level of function. He complains of a headache, but his vital signs are
normal. He is lethargic but easily awakens when his name is called. Appropriate
management should include:
a. routine laboratory blood work; if the cell count and chemistries are normal, he can go
home.
b. brain computerized tomography (CT) scan without contrast; if normal he can go home.
c. discharge home after advising family that HIV encephalopathy is a progressive disease
and nothing can be done to alter its course.
d. brain computerized tomography (CT) scan with contrast, lumbar puncture, admit to
hospital.
e. admit on high-dose steroid therapy.
215. Which statement concerning myasthenia gravis is true?
a. Most patients have general weakness, especially of the distal extremity small muscle
groups.
b. Most patients have general weakness, especially of the neck flexors.
c. Ptosis and diplopia are the most common presenting symptoms.
d. Symptoms can fluctuate throughout the day, usually improving toward evening.
e. Sensory, reflex, or cerebellar abnormalities are also common.
216. Guillain-Barré syndrome:
a. is an autoimmune disorder of the neuromuscular junction.
b. causes impaired cough reflex, leading to frequent aspiration.
c. leads to respiratory complications in 50% of patients.
78
d. can cause respiratory muscle compromise even with mild peripheral muscle
involvement.
e. is easily treated with steroids.
79
211. c
th
Rosen 5 ,
Chapter 66,
p. 920
212. d
Rosen 5th,
Chapter 103,
p. 1528
213. e
Rosen 5th,
Chapter 96, p.
1453
214. d
Rosen 5th,
Chapter 126,
p. 1849
215. c
Rosen 5th,
Chapter 102,
p. 1523
216. d
Rosen 5th,
Chapter 101,
p. 1508-1509
Treatment for acute glaucoma involves a three-pronged attack: block aqueous production
(topical beta-adrenergic antagonist, oral carbonic anhydrase inhibitor, topical alpha-2 agonist),
reduce vitreous volume (systemic hyperosmotic agent such as oral glycerol, oral isosorbide, or
intravenous mannitol), and facilitate aqueous outflow (pilocarpine drops to pull the iris from the
iridocorneal angle). Topically administered timolol 0.5% decreases intraocular pressure in 30
to 60 minutes.
CNS abscesses may occur at any age and any time of the year, and are more common in men
than in women. CNS abscesses are associated with both local contiguous and remote systemic
infections, intravenous drug use, neurologic surgery, and cranial trauma. Brain abscess
secondary to otitis media most often presents in pediatric or older adult populations. When
associated with sinusitis, it most often presents in young adults.
Anticonvulsant therapy with phenobarbital is derived primarily from studies in the pediatric
populations. Phenobarbital is a CNS depressant that decreases both ictal and physiologic
cortical activity. Sedation and depression of the respiratory drive must be anticipated,
especially if this drug is combined with a benzodiazepine.
Cryptococcus neoformans may be seen in up to 10% of patients with AIDS and may cause
either focal cerebral lesions or diffuse meningoencephalitis. The most common initial
symptoms are fever and headache. The diagnosis depends on identifying organisms in the CSF.
Cryptococcal antigen in the CSF is nearly 100% sensitive and specific; less definitive are India
ink staining (60 to 80% sensitive), fungal culture (95% sensitive), and serum cryptococcal
antigen (95% sensitive). Treatment involves admission for intravenous amphotericin or other
anti-fungals.
Most myasthenia gravis patients have general weakness, especially of the proximal extremities
muscle groups, neck extensors, and facial or bulbar muscles. Ptosis and diplopia are the most
common presenting symptoms, but oropharyngeal symptoms (dysphagia and dysarthria) and
limb weakness also can be seen. These symptoms can fluctuate throughout the day, usually
worsening as the day progresses.
In most cases, GBS is caused by an autoimmune attack on myelinated motor nerves.
Sometimes the patient first notices numbness and tingling of the lower extremities, followed by
weakness of thighs, legs, and then arms. In classic cases, there is symmetric extremity
weakness, more pronounced in the legs. Despite subjective sensory disturbances, sensation on
examination is usually normal. The hallmark finding in GBS is the lack of deep tendon
reflexes. There may be a marked limb ataxia, and the patient may not be able to walk or stand
despite reasonable strength. In all forms of the disease, there is a chance of developing
respiratory failure and lethal autonomic fluctuations.
80
217. A 4-year-old boy has acute fever, severe headache, and projectile vomiting. He is
stuporous and resists neck flexion. On physical exam you find papilledema and a
petechial rash. Suspecting meningococcal disease, you prioritize your workup and
treatment in this order:
a. LP CT head antibiotics steroids
b. LP antibiotics CT head steroids
c. steroids antibiotics CT head LP
d. CT head LP antibiotics steroids
e. antibiotics steroids CT head LP
218. A 23-year-old woman with AIDS is brought by her mother after she
has a seizure. She is waking up, but complains of a headache.
Prior to performing a spinal tap, you do a head CT which looks like
this. Your next step is to:
a. start anti-parasitic therapy, such as pyrimethamine plus
sulfadiazine (Daraprin®).
b. start anti-fungal therapy, such as fluconazole or amphotericin.
c. start broad-spectrum antibiotic coverage with a third-generation
fluoroquinolone.
d. arrange for imaging-guided drainage of the abscess.
e. arrange for ventriculoperitoneal shunt placement.
219. A 50-year-old woman complains of fatigue, cold intolerance, and weight gain.
Temperature 94.5oF, heart rate 52 beats / minute, blood pressure 82/38 mmHg. She has
dry skin, generalized edema, and diminished reflxes. Her most immediate life threats
include:
a. metabolic acidosis, hyperglycemia, and hyperkalemia.
b. hepatorenal syndrome.
c. respiratory insufficiency, hypotension, and hypoglycemia.
d. myocardial infarction and stroke.
e. hypertension and intracranial hemorrhage.
220. A 42-year-old woman with adult T-cell lymphoma-leukemia complains of back pain,
abdominal pain, and confusion. Laboratory evaluation shows a total calcium of 15.8
mg/dl. Appropriate management of this patient should include:
a. plasmapheresis.
b. intravenous bicarbonate.
c. intravenous hypertonic saline and oral Kayexalate®.
d. intravenous normal saline and intravenous furosemide.
e. glucagon.
221. A 25-year-old insulin dependent diabetic complains of nausea, vomiting and abdominal
pain for two days. His bedside glucose is 565, and his serum bicarbonate is 8 mEq. The
anion gap is 34. Your initial treatment should include:
a. insulin by intravenous drip.
b. intravenous bicarbonate until serum pH is normalized.
c. adequate phosphorus repletion in the form of potassium phosphate.
d. judicious intravenous fluids to avoid volume overload.
e. glucagon by intravenous drip.
81
217. e
th
Rosen 5 ,
Chapter 103,
p. 2349
218. a
Rosen 5th,
Chapter 126,
p. 1849
219. c
Rosen 5th,
Chapter 122,
p. 1778
220. d
Rosen 5th,
Chapter 119,
p. 1735
221. a
Rosen 5th,
Chapter 120,
p. 1753
If a patient's presentation is an acute, fulminating, febrile illness and bacterial meningitis is the
concerning diagnosis, early initiation of antimicrobial therapy is mandatory. The role of
dexamethasone therapy for acute bacterial meningitis has long been the focus of clinical
interest, and considerable controversy exists among individuals who view the same data
differently. Consensus opinion suggests that for infants beyond 8 weeks old, dexamethasone
may improve some neurologic sequelae, particularly hearing loss with meningitis cause by H.
influenzae. Beneficial effect, if any, of dexamethasone on morbidity and mortality caused by
other bacteria is less well defined.
Toxoplasma gondii is the most common cause of focal encephalitis in patients with AIDS.
Common symptoms include fever, headache, altered mental status, and seizures. Serologic
testing is not useful as the antibody is present in the general population. Diagnosis of
toxoplasmosis is most often made by the presence of multiple subcortical lesions on CT scan.
Noncontrast CT is the initial study of choice, as addition of contrast has been shown to be of
marginal value in patients with completely normal noncontrast CT scans. In the presence of
contrast, toxoplasmosis lesions are ring-enhancing with surrounding areas of edema.
Hypoventilation and hypoglycemia are the two immediately serious metabolic abnormalities of
myxedema. ABGs may be the only indication that significant hypercapnea and respiratory
acidosis exist. An elevated serum carbon dioxide partial pressure may be seen in nearly one
third of patients with myxedema coma, and ventilator support can immediately reverse this
cause of coma. Serious hypoglycemia is unusual and is less characteristic of primary
hypothyroidism than of secondary hypothyroidism. If present, hypoglycemia can contribute to
coma, although seizures may be a more likely outcome. Patients should receive 5% dextrose in
water (D5W), and serum glucose should be monitored.
Patients with severe hypercalcemia (>14 mg/dl) require immediate treatment regardless of
symptoms. The four basic goals of therapy are (1) restore intravascular volume, (2) enhance
renal calcium elimination, (3) reduce osteoclastic activity, and (4) treat primary disorder.
Isotonic saline is the first step. Once volume has been restored, the calcium will usually have
decreased by 1.6 to 2.4 mg/dl, but hydration alone rarely leads to complete normalization.
Loop diuretics such as furosemide inhibit the resorption of calcium in the thick ascending loop
of Henle, increasing the calciuric effect of hydration. Volume expansion must precede the
administration of furosemide, however, because the drug’s effect depends on the delivery of
calcium to the distal nephron.
Rapid fluid administration is the single most important initial step in the treatment of DKA.
Fluid restores intravascular volume and normal tonicity, perfuse vital organs, improves
glomerular filtration rate (GFR), and lowers serum glucose and ketones. The average adult
patient has a water deficit of 100 mL/kg (5 to 10 L) and a sodium deficit of 7 to 10 mEq/kg. It
is generally accepted that the “ideal way” to administer insulin is by continuous infusion of
small doses of regular insulin through an infusion pump. This approach appears to be more
physiologic, helps produce a more linear fall in serum glucose and ketone bodies, and is
associated with less-severe metabolic complications (hypoglycemia, hypokalemia, and
hypophosphatemia).
82
222. Euvolemic hyponatremia is found in patients with:
a. diabetes insipidus.
b. vomiting.
c. laxative abuse.
d. SIADH.
e. decreased water intake.
223. A 27-year-old alcoholic with insulin dependent diabetes is lethargic and vomiting. He
smells heavily of alcohol. Labs show Na+ 143, K+ 4.2, Cl- 107, HC03 18, glucose 305. His
serum ethanol level is 0.128 (128 mg%). His urine dips positive for ketones. What is the
likely cause of his ketoacidosis?
a. alcoholic ketoacidosis, anion gap 36
b. diabetic ketoacidosis, anion gap 18
c. alcoholic ketoacidosis, anion gap 18
d. diabetic ketoacidosis, anion gap 36
e. diabetic ketoacidosis, anion gap 22
224. A common finding in myxedema is:
a. hypocalcemia.
b. hyponatremia.
c. hyperglycemia.
d. hypocholesterolemia.
e. hypokalemia.
225. A 48-year-old woman with a history of Graves’ disease complains of nervousness and
palpitations. Temperature 39.5oC; pulse 150 / minute; respirations 36 / minute; blood
pressure 150/70 mmHg. She is thin and very anxious. The first medication you should
give is:
a. propylthiouracil.
b. dexamethasone.
c. potassium iodide (SSKI).
d. methimazole.
e. propranolol.
226. A 48-year-old woman with a history of rheumatoid arthritis complains of profound
weakness and diffuse abdominal pain. She just returned from a two week cruise and
admits that she forgot to take her prednisone. You suspect adrenal insufficiency and
begin her treatment with:
a. potassium supplementation.
b. rapid volume replacement.
c. intramuscular mineralocorticoid.
d. subcutaneous insulin.
e. colloid volume expanders.
227. A 73-year-old man with a history of noninsulin-dependent diabetes mellitus is being
evaluated for altered mental status. Physical exam is remarkable for signs of severe
dehydration. His serum glucose level is 1283 mg/dl. You also expect to find:
a. BUN : creatinine ratio less than 20:1.
b. markedly elevated serum ketones.
c. elevated troponin.
d. hyponatremia (uncorrected).
83
e. profound acidosis.
84
222. d
th
Rosen 5 ,
Chapter 119,
p. 1724-1725
223. b
Rosen 5th,
Chapter 179,
p. 2524
224. b
Rosen 5th,
Chapter 122,
p. 1776, Box
122-9
225. e
Rosen 5th,
Chapter 122
p.1774
226. b
Rosen 5th,
Chapter 122,
p. 1781-1782
227. d
Rosen 5th,
Chapter 120,
p. 1755
The many causes of euvolemic hyponatremia include the syndrome of inappropriate secretion
of ADH (SIADH), defined as the secretion of ADH in the absence of an appropriate
physiologic stimulus. Hypovolemic hyponatremia results from the loss of water and sodium
with a greater relative loss of sodium. Typical causes include vomiting, diarrhea,
gastrointestinal (GI) suction or drainage tubes, fistulas, and “third spacing” of fluids (e.g.,
burns, intra-abdominal sepsis, bowel obstruction, pancreatitis).
The difference between the serum sodium (the contribution of potassium, largely an
intracellular ion, is usually ignored) and the sum of serum chloride and bicarbonate equals the
concentration of the unmeasured anions, or the "anion gap." Almost all patients with DKA
present with blood glucose greater than 300 mg/dL, but patients who present just after receiving
insulin or who have impaired gluconeogenesis (e.g., in alcohol abuse or liver failure) may have
lower initial serum glucose levels. In alcoholic ketoacidosis, alcohol levels are usually low or
undetectable at the time of presentation, but some patients may present with an elevated blood
alcohol level, making diagnosis more challenging. Serum glucose levels are usually less than
200 mg/dl.
In the myxedematous patient, hyponatremia occurs often and is usually mild. The mechanism
is thought to be syndrome of inappropriate secretion of antidiuretic hormone (SIADH), and
thyroid replacement therapy reverses the abnormality. Hypoglycemia is unusual and typically
mild; its correction usually does not materially affect the clinical symptoms. Hypercalcemia is
rare, mild when present, and of uncertain cause. Cholesterol levels are typically elevated, are
rarely less than 250 mg/dl, and in 86% of cases are greater than 290 mg/dl. A mild normocytic,
normochromic anemia without reticulocytosis may be present.
Treatment of thyroid storm has five goals: (1) inhibit hormone synthesis, (2) block hormone
release, (3) prevent peripheral conversion of T4 to T3, (4) block the peripheral effects of thyroid
hormone, and (5) provide general support. Blockade of the peripheral adrenergic hyperactivity
of thyroid crisis may be the most important factor in reducing morbidity and mortality.
Treatment of adrenal crisis includes replacement of fluids and sodium, administration of
glucocorticoid, correction of hypotension and hypoglycemia, reduction of hyperkalemia, and
identification and treatment of a precipitating cause of the crisis. A rapid infusion of 5%
dextrose and isotonic saline should be started immediately. This acts to correct dehydration,
hypotension, hyponatremia, and hypoglycemia.
Patients in a hyperglycemic hyperosmolar nonketotic coma have a blood glucose level greater
than 600 mg/dl and serum osmolarity greater than 350 mOsm/L. The BUN concentration is
invariably elevated. Although patients with HHNC do not have a ketoacidosis caused by
diabetes, they may have a metabolic acidosis secondary to some combination of lactic acidosis,
starvation ketosis, and retention of inorganic acids attributable to renal hypoperfusion. They
typically manifest more profound electrolyte imbalance than with DKA. Initial serum sodium
readings will be inaccurately low because of hyperglycemia.
85
228. A 25-year-old with hemophilia A has a painful swollen ankle but no history of trauma.
Appropriate treatment includes ice, immobilization, and a Factor VIII infusion of:
a. 12.5 units/kg.
b. 25 units/kg.
c. 40 units/kg.
d. 50 units/kg.
e. 100 units/kg.
229. A 4-year-old boy has fever and headache. Temperature 104°F, pulse 168 / minute,
respiratory rate 42 / minute, blood pressure 58/35 mmHg. He is lethargic and irritable, and
has a purpuric rash. You start antibiotics and steroids and perform a lumbar puncture,
which shows Gram-negative diplococci. One hour later, the nurse notes that there is
oozing from his IV site. He then has a large bloody stool and passes dark red-brown urine
which tests strongly positive for blood. You expect lab studies to show:
a. elevated fibrinogen.
b. elevated fibrin degradation products (FDP) and d-dimers.
c. diminished INR.
d. elevated platelet count.
e. shortened thrombin clot time.
230. A 72-year-old woman with a past history of congestive heart failure complains of epigastric
pain, black bowel movements, and vomiting some “coffee-ground” material. Her
hemoglobin is 6.5 mg/dL, so you order two units of packed red blood cells for transfusion.
The first unit is transfused uneventfully over a 45 minute period. Thirty minutes after the
second unit of packed red blood cells is started, she complains of a headache and
shortness of breath. Her lung exam now shows bilateral crackles. You tell the nurse to:
a. give a bolus of intravenous saline.
b. use a leukocyte reduction filter.
c. administer diphenhydramine.
d. slow the transfusion and begin diuresis.
e. stop the transfusion and report a transfusion reaction.
231. A healthy 12-year-old African-American female complains of weakness and fatigue 3 days
after starting a course of trimethoprim-sulfamethoxasole and pyridium for a urinary tract
infection. Her hemoglobin is 4.8 mg/dl, and her urine is tea-colored, but you see no red
blood cells on microscopic exam. She probably has undiagnosed:
a. hemolytic uremic syndrome.
b. G6PD deficiency.
c. idiopathic thrombocytopenic purpura.
d. thrombotic thrombocytopenic purpura.
e. sickle cell disease.
232. In methanol poisoning the most likely cause of toxicity is:
a. acetaldehyde.
b. formic acid.
c. folate.
d. ethyl methanol.
e. oxalic acid
86
228. b
th
Rosen 5 ,
Chapter 116,
p.
Treatment of nontraumatic hemarthrosis in a hemophiliac patient begins DDAVP. If not
available, Factor VIII 12.5 U/kg as a single dose is given for early or mild bleeds; most
hemophiliacs usually require 25 U/kg every 24 hours for 2 or 3 days.
Results
229. b Tests for DIC
Pathophysiology
th
Rosen 5 ,
Chapter 116,
p. 1698, Table
116-3
Peripheral smear
Low platelets, schistocytes,
RBC fragments
RBCs fragment on fibrin strands
(schiztocytes not always seen)
Platelet count
Low – usually <10,000/mm3
Consumed in clotting, reflected in
bleeding time
Prothrombin time
Prolonged
Factors II and IV consumed
Prolonged
Decreased Factor II
Activated partial
thromboplastin time
Fibrinogen level
230. d
Rosen 5th,
Chapter 5, p.
51
231. b
th
Rosen 5 ,
Chapter 115,
p. 1676-1677
232. b
Rosen 5th,
Chapter 149,
p. 2127
Low
Factor II consumed
Dependent on secondary
FDP / d-dimer
Zero to large
fibrinolysis
Chronically anemic, normovolemic elderly patients are at greatest risk for developing
congestive heart failure with the rapid infusion of blood. Taking four hours to infuse a unit and
using diuretics (if needed) should prevent this complication.
Deficiency of the red blood cell (RBC) enzyme glucose-6- phosphate dehydrogenase (G-6-PD)
is the most common human enzyme defect, affecting nearly one-tenth of the world’s
population. The RBC is unable to protect itself against oxidant stress. Acute hemolytic crises
occur that are incited by bacterial and viral infections, exposure to oxidant drugs, metabolic
acidosis (such as diabetic ketoacidosis), and ingestion of fava beans in some patients. Within 1
to 3 days following oxidant stress, the patient can develop hemoglobinuria and the potential for
vascular collapse. These hemolytic crises are generally well tolerated and self-limited because
only the older RBCs will hemolyze. The drugs most commonly associated with oxidant stress
are sulfa drugs, antimalarials, phenazopyridine, and nitrofurantoin.
Methanol itself has little toxicity, producing less CNS depression and inebriation than does
ethanol. Metabolites of the parent compound are, however, very toxic. Although small
amounts of methanol are eliminated via renal and pulmonary routes, 90% is hepatically
metabolized. Methanol is oxidized by alcohol dehydrogenase to formaldehyde, which is then
rapidly converted by aldehyde dehydrogenase to formic acid, which is the primary toxicant and
accounts for much of the anion gap metabolic acidosis ocular toxicity peculiar to methanol
ingestion.
87
233. A 5-year-old girl complains of weakness and fatigue. Two weeks ago she saw her family
doctor and was diagnosed with an upper respiratory infection. She received no medicine
at that time. Physical examination shows only a scattered petechial rash located in areas
where her clothing is snug against her skin, such as underwear elastic lines. Laboratory
studies show a white blood cell count 11,000/mm3 , Hgb 10.5 mg/dL, and platelet count of
16,000/mm3. Appropriate management of this patient should be:
a. platelet concentrate transfusion.
b. discharge home with instructions to limit contact sports.
c. admit for salicylate therapy.
d. admit for splenectomy.
e. admit for observation.
234. A 38-year-old woman has von Willebrand’s disease, Type I. She complains of bloodtinged emesis and epigastric pain. Her stool tests weakly positive for blood. Appropriate
initial therapy includes:
a. vitamin K.
b. 6 units platelet concentrate.
c. factor IX concentrate.
d. desmopressin (DDAVP).
e. plasmapheresis.
235. A 71-year-old woman takes warfarin for chronic atrial fibrillation. She complains of bloody
bowel movements. Her INR is 16.0 and her hemoglobin is 8.0 gm/dl. The first thing you
should administer is:
a. heparin.
b. fresh frozen plasma.
c. cryoprecipitate.
d. fibrinogen.
e. desmopressin (DDAVP).
236. A 32-year-old man complains of shortness of breath. He has just started trimethoprimsulfamethoxazole for chronic sinusitis. He is cyanotic. His pulse oximetry is 85% and
does not improve despite 100% oxygen. His lungs are clear. Room air arterial blood gas
shows a PaO2 of 94. Appropriate therapy for this patient would be:
a. subcutaneous epinephrine 1:1000.
b. intravenous diphenhydramine.
c. rapid sequence intubation.
d. albuterol nebulization.
e. intravenous methylene blue.
237. A 15-year-old boy with hemophilia A complains of a diffuse headache which started two
hours after he hit his head on a kitchen cabinet at home. He has a 3 cm contusion on his
left parietal scalp, but otherwise appears normal. Your first step is to:
a. give intranasal desmopressin (DDAVP).
b. give factor VIII replacement followed by brain CT.
c. order a brain CT and discharge home if normal.
d. observe for six hours in Emergency Department.
e. do a thorough neurologic exam and, if normal, discharge home.
88
233. e
th
Rosen 5 ,
Chapter 116,
p. 1693
234. d
Rosen 5th,
Chapter 116,
p. 1697
235. b
Rosen 5th,
Chapter 5, p.
50
236. e
Rosen 5th,
Chapter 180,
p. 2540
237. b
Rosen 5th,
Chapter 116,
p. 1695
Acute idiopathic thrombocytopenic purpura (ITP) is seen most often in children 2 to 6 years
old. A viral prodrome is common, usually within 3 weeks of the onset. The platelet count falls,
usually to less than 20,000/mm3. The course is self-limited, with a greater than 90% rate of
spontaneous remission. Morbidity and mortality are low, although full recovery may take
several weeks. Treatment is supportive, and steroid therapy does not alter the disease course.
The treatment of von Willebrand’s disease depends on the type of disease that is present and the
severity of bleeding. Desmopressin (DDAVP) treatment has benefit in patients with mild to
moderately severe von Willebrand’s disease, but should be given in consultation with a
hematologist. Factor VIII (cryoprecipitate) or fresh frozen plasma may be used in patients with
severe bleeding.
Warfarin has a half-life of 2.5 days in patients with normal hepatic function. Patients with
bleeding complications can be treated with fresh frozen plasma (FFP) or vitamin K1
(intravenous, intramuscular, or subcutaneous) – each has advantages and disadvantages.
Infusion of FFP can result in the rapid repletion of coagulation factors and control of
hemorrhage, but carries some risk of viral transmission and volume overload. Parenteral
vitamin K1 will reverse the warfarin effect in 12 to 24 hours. Intravenous vitamin K1 can cause
hypersensitive anaphylactic reactions, although usually 1 mg can be given intravenously safely.
Intramuscular or subcutaneous vitamin K1 is typically given in doses of 5 to 10 mg daily in
states of coagulation factor deficiency.
Most cyanotic patients improve with oxygen, whereas patients with methemoglobinemia do
not. Agents causing methemoglobinemia include nitrites, dapsone, lidocaine, aniline dyes,
sulfonamides, phenacetin, and the fluoroquinolones. Methylene blue is the treatment of choice
for patients who are symptomatic or have levels above 30%. This substance acts as a cofactor
that accelerates the reduction of methemoglobin.
Any patient with hemophilia who complains of a new headache or any neurologic symptoms
requires immediate factor VIII replacement therapy followed by immediate computed
tomographic (CT) scanning of the head.
89
238. A 40-year-old woman has a four day history of progressive confusion, fever, and mild
jaundice. Laboratory tests show a severe anemia with schistocytes and
thrombocytopenia. Her prothrombin time (PT), partial thromboplastin time (PTT),
fibrinogen, and fibrin split products are all normal. Her most likely diagnosis is:
a. acute idiopathic thrombocytopenic purpura.
b. severe autoimmune hemolytic anemia.
c. disseminated intravascular coagulopathy.
d. G6PD deficiency.
e. thrombotic thrombocytopenic purpura.
239. A 68-year-old man complains of headache, dizziness, and blurred vision. His blood
pressure is 190/118 mmHg. He has a florid face, normal fundi, and marked splenomegaly.
His hematocrit is 67%. Reasonable therapy includes:
a. 250cc salt-poor albumin.
b. intravenous nitroprusside.
c. phlebotomy.
d. plasmapheresis.
e. sublingual nifedipine.
240. As an antidote, pralidoxime (2-PAM) is:
a. used in lieu of atropine.
b. employed in poisoning due to chlorinated hydrocarbon insecticides.
c. necessary to treat carbamate insecticide toxicity.
d. effective against many of the same toxins as physostigmine.
e. necessary to reverse nicotinic effects of insecticide poisoning.
241. A 2-year-old child is found comatose in his grandfather’s barn with muscle twitching,
vomiting, diarrhea, and wheezing. He probably got into some:
a. parathion.
b. jimson weed.
c. DDT.
d. nitrate fertilizers.
e. antifreeze.
242. An 18-year-old hair salon stylist complains of abdominal pain and nausea for several
hours. She seems confused and intoxicated, but her breath does not smell of alcohol.
You begin intravenous fluids and send some lab work. One hour later, her blood pressure
drops to 60 palpable and she becomes apneic. You intubate her just as the lab results
come back. The most important clue that this may be isopropyl alcohol poisoning is:
a. bradycardia.
b. elevated creatinine with high serum acetone level.
c. fever greater than 39°C.
d. hypertension.
e. profound metabolic acidosis with elevated osmolar gap, but no anion gap.
90
238. e
th
Rosen 5 ,
Chapter 116,
p. 1693
239. c
Rosen 5th,
Chapter 115,
p. 1683
240. e
th
Rosen 5 ,
Chapter 157,
p. 2189
241. a
Rosen 5th,
Chapter 157,
p. 2187
242. b
Rosen 5th,
Chapter 149,
p. 2134
TTP is a heterogeneous clinical syndrome characterized by this classic pentad of symptoms and
signs (all five are present only in 40%):
1. Microangiopathic hemolytic anemia (MAHA) with schistocytes on the blood smear and a
reticulocytosis
2. Thrombocytopenia: platelet counts range from 5000 – 100,000 / mL
3. Renal abnormalities: azotemia, proteinuria, or hematuria
4. Fever (90%)
5. Neurologic abnormalities including headache, confusion, cranial nerve palsies, seizures, or
coma
The disease may affect patients of any age or sex, but the majority are 10 to 40 years old, and
60% of cases occur in women.
Emergency treatment of any form of symptomatic polycythemia is phlebotomy. Usually not
more than 500 ml of blood is slowly removed as the volume is replaced with a comparable
amount of normal saline.
The definitive treatment of acetylcholinesterase inhibition starts with the administration of
atropine. The second part of acetylcholinesterase inhibition treatment is the use of pralidoxime
(Protopam, 2-PAM) to break up the organophosphate-acetylcholinesterase complex and restore
cholinesterase activity at both muscarinic and nicotinic sites. The use of 2-PAM in carbamate
poisoning is controversial.
Commonly used organophosphate poisons include diazinon, orthene, malathion, parathion, and
chlorpyrifos. The accumulation of acetylcholine results in the classic cholinergic syndrome
called the DUMBELS syndrome. This stands for diarrhea, urination, meiosis, bronchorrhea,
emesis, lacrimation, and salivation. The mnemonic SLUDGE ignores bronchorrhea, the
principle cause of morbidity and mortality. This represents the general hypersecretion seen in
poisoning with this class of pesticide. Later, the effect of nicotinic hyperstimulation of skeletal
muscle determines the ultimate morbidity and mortality of acetylcholinesterase inhibitors.
Signs of skeletal muscle hyperactivity include involuntary twitches, fasciculations, and
hyperactive reflexes.
One early clue to the diagnosis of isopropanol ingestion is “pseudo renal failure” or isolated
false elevation of creatinine with a normal BUN. This results from interference of acetone and
acetoacetate by the colorimetric method of creatinine determination. The most common
laboratory abnormality is is ketosis with little or no acidosis and normal blood glucose levels.
The ketosis is from the metabolite acetone.
91
243. A 27-year-old unemployed man drank a bottle of Liquid Drano® in a suicide attempt. He
appears uncomfortable but is drooling. You know that:
a. activated charcoal will be a helpful adjunct in his treatment.
b. forcing fluids is never indicated..
c. he requires immediate decontamination with a large-bore nasogastric tube.
d. neutralization with a weak acid will be helpful.
e. barium swallow will help delineate the depth of involvement.
244. A teenage girl ingests a “handful” of over-the-counter pills. She is tachycardic,
hypotensive, and hyperthermic. Her pupils are dilated and she appears to be
hallucinating. The antidote most likely to be effective in treating her symptoms is:
a. atropine.
b. naloxone.
c. physostigmine.
d. pralidoxime.
e. propranolol.
245. A 40-year-old woman is found comatose with pulse 80 / minute, respirations 8 / minute,
and blood pressure 90/60 mmHg. An empty butalbital bottle is found nearby. Treatment
includes:
a. respiratory support, vasopressors, forced alkaline diuresis.
b. respiratory support, fluids.
c. respiratory support, immediate hemodialysis.
d. respiratory support, immediate hemoperfusion.
e. respiratory support, acid diuresis.
246. Ethylene glycol toxicity is characterized by:
a. high anion gap acidosis, osmolal gap, and elevated serum calcium.
b. high anion gap acidosis, osmolal gap, and crystals in urine.
c. high anion gap acidosis, retinal hyperemia, and crystals in urine.
d. osmolal gap, distinctive breath odor, and visual changes.
e. distinct CNS depression with acidosis, but no osmolal gap.
247. A 74-year-old man has apparently been despondent since his cardiac bypass surgery. He
took a whole bottle of his blood pressure pills. He is bradycardic, hypotensive, and
seizing. Bedside glucose is 270 mg/dl. The most effective treatment would be:
a. lidocaine 100 mg.
b. digoxin 0.25 mg.
c. dopamine 5-10 mcg/kg/min.
d. isoproterenol 0.2 mg.
e. glucagon 10 mg.
248. A 2-year-old child mistook a bottle of her uncle’s “cancer vitamins” for candy. She is
comatose, hypotensive, and bradycardic, but her skin is pink. Antidotal therapy includes:
a. sodium nitrite to induce methemoglobinemia.
b. methylene blue to induce methemoglobinemia.
c. sodium thiosulfate to produce cyanomethemoglobin.
d. sodium nitrite to bind cyanide.
e. amyl nitrite to induce a methemoglobinemia of 50%.
92
243. b
th
Rosen 5 ,
Chapter 147,
p. 2117
244. c
Rosen 5th,
Chapter 144,
p. 2085
245. b
Rosen 5th,
Chapter 159,
p. 2209
246. b
Rosen 5th,
Chapter 149,
p. 2131
247. e
th
Rosen 5 ,
Chapter 146,
p. 2112
248. a
Rosen 5th,
Chapter 153,
p. 2166
Emesis induction and activated charcoal administration have no place in the treatment of a
caustic ingestion, and forcing fluids is never indicated. Gastric and esophageal lavage is
usually not warranted. Use of an acid neutralizing agent will cause an exothermic chemical
reaction and possible severe burns. Noninvasive techniques such as barium swallow do not
gauge the depth of involvement. Corticosteroid therapy remains controversial.
The patient exhibits classic anticholinergic toxidrome (Blind as a Bat, Hot as a Hare, Red as a
Beet, Dry as a Bone, Mad as a Hen). Physostigmine reverses delirium in 96% of patients who
receive it as a first-line therapy, and has been used successfully to treat intractable seizures,
coma, severe agitation, and ventricular tachycardia. Because of potential toxicity,
physostigmine should be infused slowly in an initial dose of 1 to 2 mg for adults to control
severe anticholinergic manifestations.
The management of barbiturate intoxication is based on meticulously supporting cardiovascular
and respiratory systems, maintaining adequate renal function, and avoiding unnecessary
aggressive interventions. Gastric lavage, charcoal hemoperfusion, and hemodialysis are used in
only a small minority of cases. Alkalinizing the urine with NaHCO 3 will increase renal
clearance of long-acting phenobarbital, but does not effect clearance of short-acting barbiturates
such as butalbital.
Like methanol, ethylene glycol often causes a profound anion gap metabolic acidosis when the
metabolites glycolic acid and glyoxylic acid (and, to some extent, lactic acid) accumulate. As
with methanol toxicity, an elevated osmolal gap as measured by freezing point depression is a
clue to the diagnosis of ethylene glycol toxicity.
Toxicity with overdose of both beta-blockers and calcium channel antagonists causes lethargy,
confusion, and coma. Unlike beta-blockers, calcium antagonists rarely induce seizures.
Pulmonary effects of both include noncardiogenic pulmonary edema. While atropine can be
used to treat both hypotension and bradycardia, its effect are disappointing and short-lived.
Isoproterenol or dobutamine along may not reverse (or may even exacerbate) peripheral
vasodilation, so it is logical to add a vasopressor such as norepinephrine, metaraminol, or
phenylephrine.
Amygdalin is a cyanogenic glycoside that is found in particularly high concentrations in apricot
pits and bitter almonds. It is the principal constituent of Laetrile, a compound popular for
nontraditional cancer therapies in the late 1970s. The clinical signs and symptoms of cyanide
poisoning mimic those of hypoxia, with one exception: unless respiratory arrest has occurred,
patients are not cyanotic.
93
249. A standard 0.4 mg dose of naloxone should be sufficient to reverse an overdose from:
a. dextromethorphan.
b. fentanyl.
c. morphine.
d. pentazocine.
e. propoxyphene.
250. The diagnosis of methemoglobinemia is consistent with:
a. chocolate-colored blood which turns red upon exposure to air.
b. a normal pO2.
c. a bitter-almond breath odor.
d. a decreased calculated O2 saturation.
e. urine which turns red when left exposed to air.
251. A 60-year-old man has been taking 20 or more aspirin a day for two weeks for pain relief.
He complains of ringing in his ears, confusion and vomiting. You draw and send an
arterial blood gas, expecting to find:
a. primary respiratory alkalosis.
b. mixed respiratory alkalosis and metabolic acidosis.
c. mixed respiratory acidosis and metabolic acidosis.
d. mixed respiratory acidosis and metabolic alkalosis.
e. mixed respiratory alkalosis and metabolic alkalosis.
252. You wish to use ketamine for an adult patient who requires Procedural Sedation and
Analgesia (PSAA). You are concerned about the possible occurrence of “reimergence
phenomenon,” so you also give him:
a. midazolam.
b. morphine sulfate.
c. fentanyl
d. ketorolac.
e. nitrous oxide.
253. A 26-year-old man had an unknown ingestion in an apparent suicide attempt. He is
unresponsive with evidence of emesis. Heart rate 130 / minute; respiratory rate 26 /
minute; blood pressure: 110/70 mmHg. You intubate him for airway protection and start
intravenous fluids. The secondary exam is remarkable only for normal pupils, clinical
evidence of dehydration, active bowel sounds, and bibasilar rales. CBC is normal. Na+
142; K+ 3.8; Cl- 96; CO2 16; BUN 58. ABG shows pH 7.14; pO2 198; pCO2 30; HCO3 12,
O2sat 99% on 100% oxygen. Chest x-ray shows pulmonary edema with a normal-sized
heart. After unremarkable gastric large and activated charcoal administration, this
patient's toxicology screen returns positive only for a salicylate level of 145 mgldl. Your
next treatment is:
a. correction of serum potassium.
b. forced diuresis.
c. hemodialysis.
d. repeat activated charcoal administration.
e. urine alkalinization using intravenous sodium bicarbonate.
94
249. c
th
Rosen 5 ,
Chapter 156,
p. 2184
250. a
th
Rosen 5 ,
Chapter 180,
p. 2067, Table
141-3
251. b
th
Rosen 5 ,
Chapter 143,
p. 2077
252. e
Rosen 5th,
Chapter 183,
p. 2582
254. e
Rosen 5th,
Chapter 143,
p. 2078
Exposures to propoxyphene, fentanyl, pentazocine, or dextromethorphan may require large
doses of naloxone. Standard dose should be sufficient to reverse morphine intoxication.
The diagnosis of methemoglobinemia should be considered in all patients who present with
cyanosis, and is particularly suspect in those whose cyanosis does not improve with
supplemental oxygen. The blood of these patients has a characteristic “chocolate brown” color,
analogous to that seen in the chocolate agar used to plate gonococcus (which contains
methemoglobin).
The initial manifestations of acute salicylate toxicity include tinnitus and impaired hearing.
More clinically significant toxic manifestations include hyperventilation, vomiting,
dehydration, hyperthermia, and central nervous system (CNS) disturbances. Salicylate-induced
hyperpnea may manifest as increased respiratory depth without commensurate increase in rate
(“panting dog” respiration). Vomiting may occur 3 to 8 hours after ingestion. Signs and
symptoms of chronic intoxication include hyperventilation, tremor, papilledema, agitation,
paranoia, bizarre behavior, memory deficits, confusion, and stupor. Neurologic abnormalities
are much more common in chronic salicylate poisoning and often mislead physicians. Serious
dehydration may occur from hyperpnea, vomiting, and hyperthermia. Most often, respiratory
alkalosis is followed by metabolic acidosis.
Emergence phenomena manifested by hallucinations and nightmares occur in up to 50% of
adults (and 10% of children) receiving ketamine. A study of adult patients requiring PSAA to
facilitate a painful procedure demonstrated that a combination of midazolam and ketamine
produced safe and effective sedation and analgesia with a low incidence of emergence
phenomena.
Urinary alkalinization should be considered in patients with salicylate levels greater than 35
mg/dl, acid-base abnormalities, or rapidly increasing salicylate levels. A urine pH of 7.5 to 8.0
is necessary to increase excretion. ABG values will help determine acid-base status. Sodium
bicarbonate (1 to 2 mEq/kg) may be administered over 1 to 2 hours, with subsequent dosage
adjustment determined by urinary and serum pH.
95
254. A tobacco harvester complains of nausea, vomiting, diarrhea, and abdominal pain. His
plants have recently been sprayed with Sevin, a carbamate insecticide. Appropriate
management would include:
a. physostigmine intravenously if seizures occur.
b. pralidoxime chloride (2-PAM) 1 gram IV.
c. atropine 0.4 to 2.0 mg IV as needed until atropinization is achieved.
d. gastrointestinal decontamination.
e. intravenous rehydration and antiemetics.
255. A 25-year-old man complains of chest pain six hours after smoking crack cocaine. An
ECG shows ST elevation in leads II, III and aVF. A drug you should avoid in treating him
is:
a. diazepam.
b. morphine.
c. nitrates.
d. propranolol.
e. sodium bicarbonate.
256. A 2-year-old girl ingested an unknown liquid in her neighbor’s garage. She is comatose
and has nystagmus. Physical exam is otherwise remarkable only for the smell of alcohol.
Basic metabolic panel: Na+ 140; K+ 4.2; Cl- 107; HCO3 24; BUN 7, creatinine 0.6, glucose
92. Her urine dips positive for ketones, but negative for glucose. She probably drank
some:
a. ethanol.
b. ethylene glycol.
c. gasoline.
d. isopropanol.
e. methanol.
257. Drugs which can be dialyzed usually have:
a. high molecular weight.
b. high protein binding.
c. large volume of distribution.
d. renal metabolism.
e. water solubility.
258. Choose the correct statement.
a. Opioid agonist / antagonists do not precipitate withdrawal in the dependent patient.
b. Opioid withdrawal in adults does not cause seizures.
c. Propoxyphene overdose may result in seizures.
d. The duration of the effects of naloxone is longer than that of methadone.
e. The primary cause of death from heroin overdose is myocardial depression.
259. Choose the correct statement concerning the stages of acute iron poisoning:
a. Stage I of iron poisoning is considered the corrosive or GI stage.
b. Intestinal obstruction is the clinical sign most commonly associated with Stage II iron
poisoning.
c. Systemic toxicity characterizes stage III of iron toxicity, including shock and lactic
acidosis, with grossly elevated serum iron levels.
d. Stage IV of iron poisoning includes delayed sequelae such as gastric outlet obstruction
e. Stage V, or the hepatic stage of iron poisoning, develops 4 to 6 weeks after ingestion.
96
253. e
th
Rosen 5 ,
Chapter 158,
p. 2200
255. d
Rosen 5th,
Chapter 148,
p. 2122-2123
256. d
Rosen 5th,
Chapter 149,
p. 2134
257. e
Rosen 5th,
Chapter 141,
p. 2173
258. c
th
Rosen 5 ,
Chapter 156,
p. 2185
259. a
Rosen 5th,
Chapter 151,
p. 2151
Symptoms of nicotine toxicity begin shortly after absorption. Nausea, vomiting, salivation,
lacrimation, diarrhea, hypertension, tachycardia, diaphoresis, agitation, and fasciculation are
seen initially. More severe toxicity is manifested by seizures, respiratory depression (muscle
weakness), and hyperthermia. Treatment for ingestion is initially aimed at limiting absorption
with activated charcoal. Gastric lavage is of questionable value. Other treatments are
supportive in nature, because no specific antidote for nicotine is available. Benzodiazepines
can be used for seizures and agitation. If severe salivation and lacrimation occur, atropine may
be useful.
Beta-adrenergic antagonist therapy such as propranolol is absolutely contraindicated because
unopposed stimulation of a-adrenergic receptors may worsen coronary and peripheral
vasoconstriction, hypertension, and possibly ischemia. Although labetalol (a mixed alpha- and
beta-adrenergic antagonist) has been suggested, labetalol increased seizures and mortality in an
animal model of cocaine toxicity and does not decrease cocaine-induced coronary
vasoconstriction in humans.
The clinical features of isopropanol intoxication are similar to those seen with ethanol
intoxication except that the duration of symptoms and signs is longer and central nervous
system depression may be more profound because of the formation of acetone. Nystagmus is
usually present. Severe poisoning is marked by early onset of coma, respiratory depression, and
hypotension. Hypoglycemia may occur secondary to depressed gluconeogenesis. Isopropanol
poisoning should be suspected when the smell of rubbing alcohol is present on the breath, when
there is acidosis associated with ketonuria and ketonemia without glycosuria or hyperglycemia,
and in the presence of an elevated osmolal gap.
Lithium and the toxic alcohols are readily dialyzable because of their small molecular weight,
water solubility, and lack of protein binding.
Propoxyphene causes sodium channel blockade similar to that of type IA antidysrhythmic
agents; dysrhythmias caused by propoxyphene overdose can be treated with sodium bicarbonate
therapy. Opioid withdrawal occurs in tolerant individuals when opioid exposure is
discontinued or an antagonist is administered. Increased sympathetic discharge and adrenergic
hyperactivity are responsible for the neurologic manifestations so prominent in opioid
withdrawal, including restlessness, agitation, anxiety, and seizures. Naloxone has a half-life of
elimination of 1.1 hours, whereas methadone’s half-life of elimination varies from 15 to 40
hours. Opioids decrease both respiratory rate and tidal volume in a dose-dependent manner by
suppression of the sensitivity of the medullary respiratory center to hypercapnea.
Stage I reflects the corrosive effects of iron on the gut. Vomiting occurs within 80 minutes of
ingestion and GI bleeding is common.
Stage II represents an apparent (but not complete) recovery that lasts less than 24 hours but can
extend up to 2 days.
Stage III is characterized by recurrent GI bleeding, severe lethargy or coma, cardiovascular
collapse, anion gap metabolic acidosis, leukocytosis, and coagulopathy. Acute renal failure
may develop.
Stage IV, 2 to 5 days after ingestion, is characterized by acute hepatic failure, with jaundice,
hepatic coma, elevated transaminase and ammonia levels, hypoglycemia, and coagulation
defects. Fulminant hepatic failure generally is fatal.
Stage V is characterized by pyloric or proximal bowel scarring, sometimes associated with
obstruction.
97
260. A 33-year-old man ingested 50 of his grandfather's benztropine tablets. Rectal
temperature: 39oC; heart rate: 130 / minute; respiratory rate: 20 / minute; blood pressure:
100/60 mmHg. His skin is dry and his pupils are dilated. Since arriving, he has become
more delirious and lethargic. You consider giving an antidote, but are especially worried
about the occurrence of:
a. diarrhea.
b. hyperthermia.
c. respiratory depression.
d. seizures.
e. torsade de pointes.
261. A 29-year-old woman ingested what she thought was a Valium® tablet at a party. She
complains that she can’t swallow. Her eyes are deviated upwards and to the right, and
she cannot voluntarily move them from this position. She probably was given:
a. atropine eye drops.
b. GHB (gamma-hydroxybutyrate).
c. haloperidol (Haldol®).
d. methyl scopolamine.
e. flunitrazepam (Rohypnol®)
262. You should treat the patient in question #261 with:
a. benztropine (Cogentin®).
b. flumazenil (Romazicon®).
c. lorazepam (Ativan®).
d. naloxone (Narcan®).
e. physostigmine (Antilirium®).
263. A potentially lethal medication combination would be:
a. phenelzine (Nardil®) and ketamine.
b. imipramine (Tofranil®) and bronchodilators.
c. lithium and acetazolamide (Diamox®).
d. theophylline and high dose steroids.
e. thioridazine (Mellaril®) and cimetidine (Tagamet®).
264. You would expect bradycardia in a patient who has overdosed on:
a. angiotensin converting enzyme inhibitor.
b. hydralazine.
c. nifedipine.
d. dietary supplements.
e. verapamil.
265. A 3-year-old complains of headache and dizziness. His 5-year-old sister says he was
eating flowers in the back yard. The cardiac monitor shows frequent PVCs. Shortly after
arrival he has a generalized seizure. You subsequently identify the flowers as oleander.
Treatment should be started with:
a. activated charcoal.
b. digoxin-specific Fab fragment.
c. phenytoin.
d. hemodialysis.
e. sodium bicarbonate
98
260. d
th
Rosen 5 ,
Chapter 144,
p. 2085
261. c
Rosen 5th,
Chapter 104,
p. 1546
262. a
Rosen 5th,
Chapter 104,
p. 1546
263. a
Rosen 5th,
Chapter 145,
p. 2099-2101
264. e
Rosen 5th,
Chapter 146,
p. 2111
265. b
Rosen 5th,
Chapter 158,
p. 2200
Benztropine (Cogentin®) is an anticholinergic. Physostigmine in the management of
anticholinergic overdoses is controversial. In the absence of anticholinergic blockade,
physostigmine itself has significant toxicity. It causes seizures, muscle weakness, bradycardia,
lacrimation, salivation, bronchorrhea, and diarrhea, and it exacerbates asthma. Even in
documented anticholinergic toxicity, seizures have been reported after its rapid administration.
Acute dystonia, the most common adverse effect seen with neuroleptic agents, occurs in 1% to
5% of patients. Reactions can occur at any point during long-term therapy and up to 48 hours
after administration of a neuroleptic agent, such as haloperidol. The patient may have
protrusion of the tongue (buccolingual crisis), deviation of the head to one side (acute
torticollis), sustained upward deviation of the eyes (oculogyric crisis), extreme arching of the
back (opisthotonos), or rarely laryngospasm. Dystonic reactions should be treated with IM or
IV benztropine (Cogentin®), 1 to 2 mg, or diphenhydramine (Benadryl®), 25 to 50 mg.
Intravenous administration usually results in an almost immediate reversal of symptoms.
Patients should receive oral therapy with the same medication for 48 to 72 hours to prevent
recurrent symptoms.
Five drugs with significant monoamine oxidase (MAO) inhibition are marketed in the United
States: the antidepressants phenelzine and tranylcypromine, the antiparkinsonian agent
selegiline, the antimicrobial furazolidone, and the antineoplastic procarbazine. MAOI-drug
interaction signs and symptoms are sympathomimetic storms or the serotonin syndrome. Most
MAOI-drug interactions occur in patients who are regularly taking MAOIs long term and ingest
incompatible drugs, such as indirect-acting sympathomimetics (e.g. ketamine) , mixed-acting
(direct/indirect-acting) sympathomimetics, methylxanthines, antidepressants, opioids (e.g.,
meperidine), and other drugs that can cause the serotonin syndrome. These drugs produce
excessive concentrations of endogenous biogenic amines that are not degraded because of
MAO inhibition.
Verapamil generally causes hypotension and bradycardia as early symptoms. Other rhythm
disturbances include AV block of all degrees, sinus arrest, AV dissociation, junctional rhythm,
and asystole. Nifedipine, overdose more commonly causes reflex sinus tachycardia from
peripheral vasodilation. Calcium channel blockade has little effect on ventricular conduction,
so QRS widening is not seen early .
Nerium oleander is one of many plants that contain toxic cardiac glycosides structurally similar
to digoxin. Small ingestions (up to several leaves) are unlikely to cause serious symptoms.
However, large exposures from suicide attempts or misidentification of plants used for teas or
herbal products can lead to severe toxicity or death. The cardiac glycosides are potent sodiumpotassium adenosine triphosphatase (ATPase) inhibitors, and the symptoms they cause are
similar to those of digoxin poisoning. Measurement of an abnormal digoxin level is only
qualitative proof of exposure, because the absolute digoxin level may not correlate with serum
levels. Negative digoxin measurements do not rule out exposures, because the level of crossreactivity with different assays varies. Treatment for oleander toxicity involves digoxinspecific Fab antibodies; however, larger doses of Fab fragments will be needed than for
comparable digoxin poisonings. Initial empiric doses of 10 to 20 vials of digoxin-specific Fab
fragments have been suggested.
99
266. Which statement is true regarding the stages of ethylene glycol toxicity?
a. Stage I, the acute neurologic phase: inebriation, convulsions, decreased pupillary
reflexes, and papilledema, occurring 24 to 48 hours after ingestion.
b. Stage II, the cardiopulmonary stage: hypertension and tachycardia with development of
pulmonary infiltrates.
c. Stage III, the renal stage: hematuria, proteinuria, and dihydrate crystalluria occurring 24
to 72 hours postingestion.
d. Stage IV, the delayed neurologic sequelae stage: usually manifests as a central cord
syndrome with a stocking-glove peripheral neuritis.
e. Stage V, the hepatic stage: can first present 6 to 12 days after ingestion with fulminant
jaundice and hyperammonemia.
267. In a patient with acute salicylate toxicity, the MOST LIKELY finding will be:
a. metabolic alkalosis.
b. respiratory acidosis, metabolic alkalosis.
c. respiratory acidosis , metabolic acidosis.
d. respiratory alkalosis, metabolic acidosis.
e. respiratory alkalosis, metabolic alkalosis.
268. Of the conditions listed, the one most closely resembling strychnine poisoning is:
a. botulism poisoning.
b. puffer fish poisoning.
c. rat poison ingestion.
d. organophosphate poisoning.
e. tetanus infection.
269. Clonidine toxicity is reported to be reversed by:
a. digoxin Fab fragments.
b. calcium chloride.
c. naloxone.
d. physostigmine.
e. hypertonic saline solution.
270. Body packers :
a.are individuals who suddenly swallow the “evidence.”(i.e. drugs) in imminent law
enforcement presence.
b.are at greater risk of developing toxicity from ingested drug than “ body stuffers.”
c. have gastrointestinal placement of drugs intentionally prepared for safe swallowing and
transportation.
d.are less likely to have positive x-rays than “body stuffers”.
e.are more likely to be harboring cannabinoids or amphetamines than cocaine or heroin.
271. Glucagon is indicated in the treatment of overdose caused by:
a. iron.
b. nicotine.
c. organophosphates.
d. tricyclic antidepressants.
e. verapamil.
100
266. b
th
Rosen 5 ,
Chapter 149,
p. 2130-2131
267. d
Rosen 5th
Chapter 143,
p. 2076-2077
268. e
th
Rosen 5 ,
Chapter 123, p
1791-1793
269. c
Rosen 5th,
Chapter 156,
p. 2184-2185
270. c
Rosen 5th,
Chapter 53, p
766
271. e
Rosen 5th,
Chapter 141, p
2067
Stage I, the acute neurologic stage, occurs 30 minutes to 12 hours after ingestion. Stage II, the
cardiopulmonary stage, occurs 12 to 24 hours after ingestion. Often the patient exhibits mild
hypertension and tachycardia. Stage III consists of elements of renal failure typically occurring
24 to 72 hours postingestion. Stage IV, the delayed neurologic sequelae stage, occurs 6 to 12
days after ingestion and typically manifests as cranial neuropathy (facial auditory nerve
oxalosis). No Stage V has been described.
Salicylates stimulate the medullary respiratory center and inhibit Krebs cycle dehydrogenases.
Most frequently reparatory alkalosis is followed by metabolic acidosis.
Strychnine poisoning is similar to tetanus in that the patient develops opisthotonos while
remaining awake. Strychnine is suggested by a history of toxin ingestion and by muscle
rigidity alternating with periods of relaxation. Also in strychnine poisoning, trismus is a later
finding. Trismus is the presenting symptom in most patients with tetanus. Treatment of the
two conditions is similar, and toxicologic studies can confirm the presence of strychnine.
The clinical response to naloxone is not pathognomonic of opioid intoxication; other
intoxications may improve with naloxone therapy as well, including valproic acid, clonidine,
tramadol, captopril, and ethanol. Naloxone has been given to patients who have ingested these
agents either because of a presentation similar to opioid intoxication or suspicion of a mixed
exposure that included opioids. The mechanism of these responses to naloxone is not
established. Some of these drugs may have activity at opioid receptors.
Body packing, which entails systematic GI tract placement of previously prepared drug
packages, should be clinically differentiated from body stuffing, which denotes hurried
ingestion of hastily prepared packages in the face of imminent police presence. Body stuffers
are more likely to suffer toxicity due to the poor packaging of drugs and are less likely to have
positive plain radiography findings. Drugs most often seen with body packing or body stuffing
are cocaine and heroin, with amphetamines and cannabinoids seen less frequently.
Glucagon can be used as an antidote in patients with beta-blocker or calcium channel blocker
overdose. Recommended dose is 5–10 mg in adults, then infusion of same dose per hour.
101
272. A 2-year-old girl is transferred from a local Day Care
Center where she had two seizures shortly after her
mother dropped her off this morning. The Day Care
worker can’t get in touch with mom, but knows the child
was recently adopted from China. She was given 10 mg
diazepam IV in the ambulance, but had a third seizure
just prior to arrival. She arrives in status epilepticus.
Temperature 100oF; heart rate 140 / minute; respiratory
rate 16 / minute; blood pressure 98/65 mmHg. WBC
18,000; hemoglobin 16; Na+ 140; K+ 4.9; Cl- 100; HCO3- 7;
Rosen 5th, Figure 129-3
glucose 120; pH 6.99; pO2 112; pCO2 45. Her chest xray, done to check tube placement, is shown. You now
know that you should attempt to stop the seizures using intravenous:
a. diazepam (Valium®) 10 mg.
b. fosphenytoin (Cerebyx®) 15-20 mg/kg.
c. phenobarbital 10-20 mg/kg.
d. pyridoxine 5 g.
e. vecuronium 0.1 mg/kg.
273. The generally recognized toxic dose of acetaminophen in adults is:
a. 70 mg/kg.
b. 100 mg/kg.
c. 140 mg/kg.
d. 180 mg/kg.
e. 220 mg/kg.
274. Acetaminophen is toxic in overdose situations because
a. renal excretion is overwhelmed increasing liver excretion.
b. the toxic metabolite n-acetyl-p-benzoquinoneimine (NAPQI) exceeds glutathione supply
and binds to hepatocyte intracellular proteins.
c. it is directly toxic to the liver.
d. the cytochrome p450 system is overwhelmed and there is increased metabolism through
sulfation and glucuronidation which cause hepatotoxicity.
e. once glutathione stores are depleted, the native acetaminophen compound builds up
and causes toxicity.
275. Trans-abdominal ultrasonography can detect a normal intrauterine pregnancy at about:
a. 2 weeks gestation.
b. 4 weeks gestation.
c. 6 weeks gestation.
Rosen 5th, Figure 85-7
d. 8 weeks gestation.
e. 10 weeks gestation.
276. The use of ultrasound evaluation is currently increasing in
emergency departments. This ultrasound (Figure 85-7)
demonstrates:
a. cholelithiasis.
b. ruptured abdominal aortic aneurysm.
c. ectopic pregnancy.
d. pericardial effusion.
e. hydronephrosis.
102
272. d
th
Rosen 5 ,
Chapter 16, p.
147; Chapter
129, p. 1917;
Chapter 168,
p. 2359
273. c
Rosen 5th,
Chapter 142,
p. 2071
274. b
Rosen 5th,
Chapter 142, p.
2069-2070
fig 142-1
275. d
Rosen 5th,
Chapter 171, p.
2405
276. a
Rosen 5th,
Chapter 85, p.
1266-1267
Patients with seizures refractory to benzodiazepines should be screened for isoniazid overdose,
since the only effective pharmacological treatment is pyridoxine. A dose of 1 mg IV of
pyridoxine for each 1 mg of isoniazid ingested should be administered, or if an unknown
quantity was ingested 5 mg IV should be given.
In adults, indications for laboratory evaluation include ingestion of >4 grams (in children >75
mg/kg) acetaminophen in a 24 hour period associated with malnourishment, chronic alcohol
consumption, or chronic use of medications that induce the cytochrome P450 system.
Laboratory evaluation should also be performed for adults who ingest >7.5 grams (in children
>150mg/kg) in a 24 hour period.
Once acetaminophen (APAP) is absorbed, hepatic metabolism normally accounts for up to 90%
of its elimination. APAP is primarily metabolized in the liver through three routes: (1)
conjugation with glucuronide (40% to 67%), (2) conjugation with sulfate (20% to 46%), or (3)
oxidation via the cytochrome P450 (CYP450) mixed-function oxidase system with subsequent
conjugation. The oxidation of APAP by CYP450 subfamilies results in the formation of highly
reactive NAPQI. NAPQI rapidly combines with glutathione and other thiol-containing
compounds forming nontoxic conjugates, which are eliminated in the urine. When NAPQI
formation exceeds glutathione supply, free NAPQI binds to hepatocyte intracellular proteins,
causing toxicity.
At 6 weeks of gestation, the gestational sac can be visualized with transabdominal sonography
(TAS). At 8 weeks, the fetal pole and fetal heart activity can be visualized using
transabdominal sonography (TAS). Using transvaginal sonography (TVS) an intrauterine
gestational sac can be seen at 5 weeks gestation and this correlates with an HCG of more than
1,800 IU/L. Fetal heart motion can be detected using transvaginal sonography (TVS) at 6
weeks of gestation and correlates with an HCG level of 6,770 IU/L.
Ultrasound is the most useful test for evaluating gallbladder disease in the emergency
department It is the procedure of choice in evaluating for gallstones. Visualization of the
gallbladder without identification of stones has an extremely high negative predictive value for
cholecystitis, whereas the presence of stones, a thickened gallbladder wall, and pericholecystic
fluid has a positive predictive value in excess of 90%.
103
277. The FAST ultrasound exam:
a. is for the evaluation of ectopic pregnancy.
b. has the primary role of detecting free retroperitoneal blood after blunt trauma.
c. is sensitive for detecting subcapsular splenic injury.
d. may be false positive in a patient with ascites.
e. .is sensitive for bowel perforations.
278. Usually, the minimal amount of intraperitoneal fluid that ultrasound (US) easily detects is:
a. 10 ml.
b. 50 ml.
c. 500 ml.
d. 1,000 ml.
e. 1,500 ml.
279. An anatomic area not well visualized by CT scan is the:
a. ureter.
b. retroperitoneum.
c. aorta.
d. bladder.
e. posterior intracranial fossa.
280. You are called to the radiology suite when an outpatient having an IVP done suddenly
becomes short of breath, tachycardic, and complains of chest pain. His face is red, you
hear wheezing as you walk into the room, and the nurse tells you his blood pressure is 76
palpable. The most important treatment is:
a. diphenhydramine (Benadryl®) 50 mg IV.
b. cimetidine (Tagamet®) 300 mg IV.
c. methylprednisolone (Solu-Medrol®) 125 mg IV.
d. epinephrine 10ml of 1:100,000 dilution IV over 10 minutes.
e. albuterol by nebulizer.
281. The procedure of choice to evaluate possible aortic dissection in the unstable patient is:
a. magnetic resonance imaging. (MRI).
b. transthoracic echocardiography (TTE).
c. transesophageal echocardiography(TEE).
d. computed tomography (CT).
e. aortography.
282. MRI is the procedure of choice in the acute evaluation of:
a. spinal epidural hematoma.
b. periorbital/globe injury.
c. bladder injury.
d. traumatic bowel perforation.
e. testicular torsion.
283. A 8-month-old girl has scabies. The preferred treatment is:
a. crotamiton (Eurax®).
b. Diphenhydramine (Benadryl®).
c. lindane (Kwell®).
d. permethrin (Elimite®).
e. topical hydrocortisone.
104
277. d
th
Rosen 5 ,
Chapter 30,
p. 252-253,
Chapter 39,
p. 423-424
278. c
th
Rosen 5 ,
Chapter 39, p.
423
279. e
th
Rosen 5 ,
Chapter 34, p.
296
280. d
th
Rosen 5 ,
Chapter 113,
p. 1632
281. c
Rosen 5th,
Chapter 80, p.
1173-1174
282. a
Rosen 5th,
Chapter 36,
p. 360,363, fig
36-40
Chapter 100,
p. 1502-1503
283. d
th
Rosen 5 ,
Chapter 114,
p. 1651
Focused assessment with sonography for trauma (FAST) exam’s primary role is detecting free
intraperitoneal blood after trauma. . It cannot distinguish blood from ascites. False-negative
FAST scans commonly involve bowel perforations or solid parenchymal damage if free
intraperitoneal blood is absent as in subcapsular splenic injury.
Sensitivity in detecting as little as 100 ml and, more typically, 500 ml of intraperitoneal fluid
ranges from 60% to 95% using ultrasound.
MRI is better than a head CT in detecting posttraumatic ischemic infarctions, subacute
nonhemorrhagic lesions and contusions, and axonal shear injury, and lesions in the brainstem or
posterior intracranial fossa. MRI is not as useful as CT in detecting bony injuries or hyperacute
bleeding.
Epinephrine, with its combined - and - adrenergic agonist actions, is the first drug of choice
in the treatment of anaphylaxis. The route of administration chosen depends of the severity of
the clinical presentation. Subcutaneous epinephrine is usually effective in those situations in
which the clinical manifestations are mild and the patient is normotensive. In the patient with
diffuse, generalized uriticaria, subcutaneous absorption of epinephrine may be slow and
unpredictable, so the intramuscular route should be used. If the patient demonstrates severe
upper airway obstruction, acute respiratory failure, or shock (systolic blood pressure less than
80 mm Hg, not associated with a ventricular tachydysrhythmia), intravenous epinephrine should
be administered. The risk of supraventricular, accelerated idioventricular, and ventricular
tachydysrhythmias; accelerated hypertension; and myocardial ischemia, including the stunned
heart syndrome, is increased by using intravenous route of epinephrine. Because of these risks,
dilution and slow administration is recommended.
While CT, MRI, and aortography have all been used to diagnose aortic dissections, they all
require the patient to leave the ED. In contrast transesophageal echocardiography (TEE) may
be done at the bedside and thus when available is the primary diagnostic method for evaluating
for possible aortic dissection in the unstable patient. Transthoracic echocardiography (TTE) has
not been useful in detecting aortic dissection.
The primary advantages of MRI over other imaging modalities lie in its ability to directly image
nonosseous structures of the spinal complex. An MR scan allows noninvasive direct
visualization of intramedullary and extramedullary spinal abnormalities that potentially cause
neurologic deficit. Its major impact has therefore been in demonstrating lesions that are
potentially correctable surgically, including acute disk herniation, ligamentous injury, bony
compression, epidural and subdural hemorrhage or abscess, and vertebral artery occlusion.
Treatment options for scabies include crotamiton (Eurax®) lotion and cream, or permethrin 5%
cream (Elimite®). Lindane is no longer the preferred treatment. Patients in whom the former
treatment fails may respond to the latter. Permethrin 5% cream applied overnight once weekly
for 2 weeks over the entire body is the treatment of choice for infants and small children. It is
more effective than crotamiton in eliminating the mite, in reducing secondary bacterial
infection, and in reducing pruritus.
105
284. A 20-year-old woman complains of painful, swollen right and left knees , low grade fever,
and a pustular rash on her hands. Your next step in her evaluation is:
a. ASO titer.
b. pelvic exam.
c. knee ultrasound.
d. rheumatoid factor.
e. urinalysis.
285. A 57-year-old female complains of oozing lesions with mild swelling and slight erythema of
her face and hands after working in her garden 2 days prior. The appropriate treatment of
moderate to severe dermatitis on the face and hands from a known poison ivy exposure is:
a. dexamethasone (Decadron®) injection 0.01 mg/kg.
b. intravenous hydrocortisone (Solu-Cortef®).
c. prednisone 10 mg daily for 10 days.
d. prednisone tapered over 21 days, starting with relatively high dose.
e. topical calamine lotion.
286. A 54-year-old man has had a burning pain in
his chest for 5 days. He has no shortness of
breath, and there is no radiation. Today he
noticed this rash, which alarmed him and his
wife. You can tell them that this rash is
associated with:
a. a high mortality rate.
b. arthralgia.
c. neuralgia.
d. pruritus.
e. resolution in 48-72 hours.
Rosen 5th Figure 114-29
287. Nikolsky's sign is characteristically seen in:
a. toxic shock syndrome.
b. pemphigus vulgaris.
c. Rocky Mountain spotted fever.
d. scarlet fever.
e. erythema nodosum
288. A 17-year-old female complains of large raw, denuded areas of her skin. She also has low
grade fever and generalized malaise. She does recall seeing her doctor recently for an
upper respiratory infection. Toxic epidermal necrolysis (TEN):
a. has no association with immunizations.
b. has mucus membrane involvement .
c. has a low mortality rate, generally less than 2%.
d. is rarely caused by medications.
e. causes bullae along the cleavage plane between the dermis and the subcutaneous
tissue.
289. The treatment of contact dermatitis includes:
a. cool wet compresses of Burow´s solution.
b. topical corticosteroid ointment.
c. systemic steroids.
d. systemic antihistamines.
106
e. all of the above.
107
284. b
th
Rosen 5 ,
Chapter 110,
p. 1593
285. d
Rosen 5th,
Chapter 114,
p. 1647-1648
286. c
Rosen 5th,
Chapter 114,
p. 1656
287. b
Rosen 5th,
Chapter 114,
p. 1643,1653
Chapter 131,
p. 1946
288. b
th
Rosen 5 ,
Chapter 114,
p. 1643
289. e
Rosen 5th,
Chapter 114,
p. 1647-1648
Gonococcal arthritis begins with fever, chills, and a migratory tenosynovitis and arthralgias that
progress to arthritis, predominantly in the knee, ankle, or wrist. A characteristic rash in two
thirds of patients accompanies the tenosynovitis and arthritis—a countable number of
hemorrhagic necrotic pustules that typically first appear on the distal extremities, including the
sides of the fingers. Rarely does the patient complain of cervicitis or urethritis. Cervical,
urethral, rectal, and pharyngeal cultures are positive in 75% of cases. For best yield, all
possible sites (synovium, blood, cervix, urethra, rectum, pharynx, and skin lesions) should be
cultured. The initial diagnosis is a clinical one; it is the diagnosis to be excluded in any young
patient with a fever, migratory polyarthritis, and polytendinitis.
Oozing or vesiculated lesions caused by the Rhus species (poison ivy ,oak, and sumac) should
be treated with cool wet compresses of Burow’s solution. Topical baths, available over the
counter, may also be comforting. A course of systemic corticosteroids is often necessary.
Prednisone in a dosage of 30 to 80 mg/day (depending on the severity of involvement) should
be prescribed initially. This should be tapered over at least 10 to 14 days, and 21 days for
poison ivy.
Herpes zoster has a very low mortality rate and is rarely life threatening even when
dissemination to the visceral organs occurs. The vesicles progress to scab then crust over 10 to
12 days then the scab falls off in 2 to 3 weeks. Pain is the symptom typically reported.
Complications include CNS involvement, ocular infection, and neuralgia.
Meningoencephalitis, myelitis, and peripheral neuropathy have been reported. Postherpetic
neuralgia, pain that persists after the lesions have healed, occurs more commonly in the elderly
and immunosuppressed patients. It may last a number of months and is often resistant to
treatment with standard analgesics.
Nikolsky’s sign is the easy separation of the outer portion of the epidermis from the basal layer
(desquamation) when pressure is exerted. It is present in and characteristic of pemphigus
vulgaris. It is also found in .toxic epidermal necrolysis (TEN) and staphylococcal scalded skin
syndrome.
The main feature of nonstaphylococcal-induced toxic epidermal necrolysis (TEN), or Lyell’s
disease, is the separation of large sheets of epidermis from underlying dermis. The full
thickness of epidermis is involved. Drugs including the long-acting sulfa drugs, penicillin,
aspirin, barbiturates, phenytoin, carbamazepine, allopurinol, and nonsteroidal anti-inflammatory
drugs are an important cause of TEN. TEN has occurred after vaccination and immunization
against polio, measles, smallpox, diphtheria, and tetnus. A mortality rate of 15% to 20% is
expected with this condition. Mucus membrane involvement is the rule.
Treatment of contact dermatitis includes avoidance of the irritant or allergen and treatment of
secondary bacterial infection. Oozing or vesiculated lesions should be treated with cool wet
compresses of Burow’s solution applied for 15 minutes three or four times a day. Topical
baths, available over the counter, may also be comforting. A course of systemic corticosteroids
is often necessary. Prednisone in a dosage of 30 to 80 mg/day (depending on the severity of
involvement) should be prescribed initially. This should be tapered over at least 10-14 days,
and 21 days for poison ivy. The long, slow taper is needed to prevent rebound of the disease.
Systemic antihistamines, such as hydroxyzine and diphenhydramine, may help control pruritis.
The patient should also be counseled to wash all clothes that might have contacted the plant.
108
290. A 27-year-old male presents with the lesions
shown, but does not recall any pertinent historical
information. A linear vesicular eruption on
exposed area of the arms or legs is most likely
secondary to:
a.diabetic neuropathy.
b.mycobacterium.
c.parasite.
d.poison ivy.
e.spirochete.
Rosen 5th Fig 114-12
291. A Tzanck smear can establish a diagnosis of:
a. gonorrhea.
b. herpes.
c. syphilis.
d. staphylococcal cellulites.
e. candida.
292. A 4-year-old child presents with a patch of scaly alopecia for two weeks duration.
Recommended treatment would be:
a. clotrimazole (Lotrimin®) cream.
b. griseofulvin oral suspension.
c. mupirocin (Bactroban®) ointment.
d. systemic steroids.
e. cephalexin.
293. A 65-year old woman complains of blisters on her
face over the last two days which are quite painful.
She has no other complaints. Physical examination
reveals the rash shown here. Which of the following
examinations is also essential for appropriate
evaluation?
a. sedimentation rate
b. complete blood count
c. sinus MRI
d. lumbar puncture
e. slit lamp examination
294. Appropriate treatment of neuroleptic malignant syndrome includes:
a. antihistamines (both H1 and H2).
b. anticholinergics.
c. high-dose steroids.
d. dantrolene.
e. physostigmine.
295. Which statement about suicide is true?
a. Attempted suicide rates are equal in both sexes.
b. Completed suicide rates are equal in both sexes.
c. Marital status does not seem to have an effect on successful completion rates.
d. Older individuals are more likely to complete or succeed.
109
e. Wrist cutting is the most common attempted method of suicide.
110
290. d
th
Rosen 5 ,
Chapter 114,
p. 1647
291. b
Rosen 5th,
Chapter 93, p.
1392
292. b
th
Rosen 5 ,
Chapter 114,
p. 1635-1636
293. e
Rosen 5th,
Chapter 114,
p. 1656
294. d
Rosen 5th,
Chapter 155,
p. 2177-2178
295. d
Rosen 5th,
Chapter 109,
p. 1576
The primary lesions of contact dermatitis are papules, vesicles, or bullae on an erythematous
bed. Of the allergens, Rhus species are the most likely to cause bullous eruptions. Oozing,
crusting, scaling, and fissuring may be found, along with lichenification in chronic lesions. The
distribution of the eruption depends on the specific contactant and may be localized,
asymmetric linear, or unilateral.
HSV infections are often obvious, but if tehre is doubt or a need to confirm the diagnosis, a
simple Tzanck slide preparation helps reveal the characteristic multinucleated giant cells
approximately 50% of the time.
Tinea capitis is a dermatophyte infection of the scalp. It is most commonly seen in children,
particularly African-American children. Clinically one sees areas of alopecia with broken-off
hairs and scale at the periphery. The alopecia is patchy and usually nonscarring. Occasionally,
tinea capitis is associated with an intense inflammatory response. After a diagnosis is
established, the current first-line therapy is griseofulvin. Topical treatment alone is not
effective.
Herpes zoster, or shingles, is an infection caused by the varicella-zoster virus. It occurs
exclusively in individuals who have previously had chicken pox. Ocular complications occur in
20% to 70% of the cases involving the ophthalmic division of the trigeminal nerve. Eye
involvement produces anterior uveitis, secondary glaucoma, and corneal scarring. There is a
close correlation between eye involvement and vesicles located at the tip of the nose
(Hutchinson’s sign).
Treatment of neuroleptic malignant syndrome revolves around supportive care and
discontinuation of the offending medication. Agitation, psychomotor hyperactivity, and
muscular rigidity should be treated aggressively with intravenous benzodiazepines. Dantrolene,
which inhibits the release of calcium from the sarcoplasmic reticulum, has been advocated as an
adjunctive therapy for NMS, along with the dopamine antagonists bromocriptine and
amantadine. There is no proven benefit to any of these agents.
Suicides are highest among older individuals, particularly elderly white men. White men
commit 73% of all suicides in the United States. Whites and Native Americans are much more
likely to commit suicide than African Americans, Hispanics, or Asians. Marriage decreases the
likelihood of suicide, but separated or divorced persons have a higher rate of suicide than those
who never had a close relationship. Women attempt suicide three to four times more often than
men, whereas men are three to four times more likely to kill themselves. Men have a higher
incidence of alcoholism and tend to use more lethal methods, such as firearms. Most completed
suicides involve firearms (70%), whereas most attempted suicides involve the ingestion of
drugs or poisons (72%).
111
296. A 70-year-old male complaints of difficulty sleeping followed by periods of sleeping for
over 20 hours daily, fatigue, difficulty concentrating and forgetfulness. He denies weight
loss or new weaknesses. Upon further questioning, you find that his wife of 45 years
passed away 4 months ago. The most likely cause of these symptoms is:
a. cancer.
b. dementia.
c. depression.
d. hypothyroidism.
e. stroke.
297. Symptoms of major depression include:
a. sleep disturbances.
b. dysphoria.
c. agitation.
d. lack of concern about personal hygiene.
e. all of the above.
298. A 52-year-old schizophrenic woman has been treated with fluphenazine (Prolixin®) for
many years. Today she complains of uncontrollable movements of her face and tongue.
She is probably suffering from:
a. acute psychotic break.
b. akathisia.
c. dystonia.
d. neuroleptic malignant syndrome.
e. tardive dyskinesia.
299. The most appropriate management of a comatose patient who overdosed on his lithium is:
a. activated charcoal.
b. adenylate cyclase stimulators.
c. chelation with EDTA.
d. hemodialysis.
e. aggressive fluid replacement.
300. A 44-year-old young woman complains of the sudden onset of blindness. She was visiting
her debilitated father in the hospital. Her husband confides that she is distraught by her
father’s diagnosis of metastatic colon cancer and the sight of him distresses her greatly.
Her physical exam, including pupillary response and retinal exam is completely normal.
Which statement is true regarding her likely diagnosis?
a. The disorder usually presents with multiple complaints.
b. It is more prevalent in well educated and higher socioeconomic social status.
c. It usually involves orthopedic or neurologic complaints.
d. The patient is typically older.
e. Patients are typically very distressed by their symptoms.
112
296. c
297. e
Rosen 5th,
Chapter 105,
p. 1550-1551
298. e
Rosen 5th,
Chapter 155,
p. 2175
299. d
Rosen 5th,
Chapter 154,
p. 2173
300. c
Rosen 5th,
Chapter 107,
p. 1566
The essential features of major depression are a persistent dysphoric (sad) mood or pervasive
loss of interest in usual activities, lasting for at least two weeks. “Vegetative symptoms”
involve physiologic functioning and include loss of appetite and weight, sleep disturbance,
fatigue, inability to concentrate, and psychomotor agitation or retardation. The depression may
begin gradually or rapidly but usually will have been present for several weeks before the
patient comes for treatment.
Tardive dyskinesia is an involuntary movement disorder that is idiosyncratically associated with
chronic therapy with the typical antipsychotic agents. Symptoms classically include
involuntary, repetitive, choreoathetoid movements of the face, mouth, and tongue, and may be
mild or severe and debilitating; uncommonly, the limbs and trunk are also affected. Elderly
patients, especially those with diabetes mellitus and organic brain damage, seem to be at
increased risk. The overall incidence is approximately 5% per year of exposure to the
offending agent.
Severely lithium-poisoned patients in coma or with seizures may require urgent airway
interventions and anticonvulsant therapy with benzodiazepines, phenobarbital, and propofol as
necessary. Many of these patients will be volume depleted. Although frank hypotension is
unusual, fluid resuscitation is needed and should include normal saline. The goal of saline
administration is to restore glomerular filtration, normalize urine output, and enhance lithium
clearance. Forced diuresis does not assist in lithium clearance. Dialysis may be useful for
patients with an acute overdose who have decreased level of consciousness, seizures, or levels
greater than 4.0 mEq/L, although asymptomatic patients with higher levels have been managed
without dialysis. For chronic toxicity, dialysis is helpful in symptomatic patients with levels
greater than 2.5 mEq/L.
Also known as hysterical neurosis, conversion type, the rare conversion disorder is
characterized by the sudden onset and dramatic presentation of a single symptom, typically
simulating some nonpainful neurologic disorder for which there is no pathophysiologic or
anatomic explanation. The most common ages of presentation are adolescence or early
childhood, although other age groups are also affected. The symptoms, generally conforming
to the patient’s own idiosyncratic ideas about illness, are not under the patient’s voluntary
control. The most common presentations to the ED include pseudoseizures, syncope or coma,
and paralysis or other movement disorders. Most patients are women, except for military
service and industrial accidents. Symptoms tend to be of sudden onset, waxing and waning in
response to environmental stresses. Patients may describe their conversion symptoms with a
lack of appropriate concern about their profound bodily dysfunction (la belle indifférence).
113
301. You are treating a 2-year-old boy who is in cardiac arrest. Your boss borrowed the Broselow tape
for a paramedic lecture, but that’s okay because you know that:
a. atropine is the first drug given for bradycardia in all age groups.
b. the minimum dose of atropine is 0.1 mg.
c. the initial defibrillation energy is 5 j/kg.
d. the curved Macintosh blade will be more effective than the straight Miller when you are
intubating.
e. the tidal volume necessary to ventilate children is 5 to 8 ml/kg.
302. Which statement about appendicitis in the pediatric age group is true?
a. Perforation and peritonitis are uncommon in younger children.
b. The presence of diarrhea effectively excludes appendicitis.
c. The condition most commonly mistaken for acute appendicitis is mesenteric adenitis.
d. Most abdominal x-rays in patients with appendicitis reveal a fecalith
e. The peak age of incidence in appendicitis is 6 to 10 years of age.
303. An Apt test is apt to:
a. differentiate central causes of blindness from peripheral causes.
b. confirm knee stability.
c. differentiate seizures from pseudo-seizures.
d. differentiate maternal from fetal blood.
e. determine the presence of pathogenic bacteria in stool samples.
304. A 7-year-old boy has fever, abdominal pain, and vomiting over the past 18 hours. He has pain in
his right lower abdomen when he coughs, and you find McBurney’s point to be exquisitely tender.
Suspicious that he has a perforated appendix, you page the surgeon and instruct the nurse to give
the patient:
a. ceftriaxone (Rocephin®).
b. ampicillin and gentamicin.
c. ampicillin, gentamicin, and metronidazole (Flagyl®.
d. a macrolide and a fluoroquinolone.
e. levofloxacin (Levaquin®).
305. Hirschsprung's disease:
a. accounts for 50% of intestinal obstruction in young infants.
b. requires barium enema to make the diagnosis.
c. is more frequently found in females.
d. is usually diagnosed early in infancy.
e. usually presents with a massive GI bleed.
306. The most common cause of intestinal obstruction between 3 months and 6 years of age is:
a. cystic fibrosis.
b. Hirschsprung’s disease
c. intussusception
d. Meckel’s diverticulum.
e. natal adhesions.
114
301. b
th
Rosen 5 ,
Chapter 8,
pages listed
in text
302. c
Rosen 5th,
Chapter 165,
p. 2311-2312
303. d
Rosen 5th,
Chapter 165,
p. 2307
304. c
Rosen 5th,
Chapter 88,
p. 1298
305. d
Rosen 5th,
Chapter 165,
p. 2305-2306
306. c
Rosen 5th,
Chapter 165,
p. 2304
The recommended dose of atropine is 0.02 mg/kg IV, with a minimum dose of 0.1 mg
to prevent paradoxical bradycardia (p. 89). Initially, 2 joules (watts per second)/kg
should be used for defibrillation (p. 97). Epinephrine is indicated in all cardiac arrest
settings, including asystole, pulseless electrical activity, and ventricular fibrillation
(p.84). Because of the superior and anterior position of the tracheal opening, as well as
the large tongue and relatively large floppy epiglottis, visualization of the glottic
opening can be obstructed in children less than 4 years of age if a curved blade is used.
The straight blade lifts these tissues so the glottic opening can be recognized (p. 91).
The tidal volume necessary to ventilate children is the same as that for adults: 10 to 15
mL/kg (p. 93).
The condition most commonly mistaken for acute appendicitis in children is
mesenteric adenitis. The rate of appendiceal perforation before surgery varies from
17% to 40% and is inversely related to age with higher rates in younger age groups.
The presence of diarrhea does not rule out appendicitis. An appendicolith is found in
about 10% of plain films. The peak age of incidence in appendicitis is 9 to 12 years of
age.
In young neonates an Apt test can be performed to determine if a bloody stool contains
maternal or fetal blood. Add 1% NaOH to the bloody stool. Fetal hemoglobin resists
oxidation and remains pinkish-red, whereas maternal hemoglobin changes to a dark
brown color.
Once the decision has been made to operate, prophylactic antibiotics should be given
to cover gram-negative and anaerobic organisms. Intravenous second-generation
cephalosporins, such as cefotetan of cefoxitin, provide good coverage. If the appendix
has already perforated, more complete coverage with ampicillin, gentamicin,
clindamycin, or advanced penicillin combinations such as piperacillin and tazobactam
may be preferred.
Hirschsprung's disease is usually diagnosed in infancy. Although a barium enema can
reveal a narrowed aganglionic segment with proximal dilation, which is highly
suggestive of Hirschsprung’s disease, the diagnosis is confirmed by biopsy or
manometry. It accounts for approximately 20% of cases of partial intestinal
obstruction early in infancy. It occurs at a rate of 1 in 5,000 live births and is 4 to 5
times more common in boys. Definitive therapy is surgical resection of the
aganglionic segments.
Intussusception is the most common cause of intestinal obstruction in children less
than 2 years of age, and occurs most commonly in infants between 5 and 12 months of
life. There is an estimated incidence of 1 per 2000 children under the age of 15 years
with a male predominance. Siblings of affected children have a relative risk 15 to 20
times higher than the general population. Mortality for untreated intussusception is
high.
115
307. In an infant with newly diagnosed pyloric stenosis, the classic electrolyte findings of patients with
severe symptoms is:
a. hyperchloremic, hypokalemic alkalosis.
b. hyperkalemic, hypernatremic acidosis.
c. hypernatremic, hypokalemic acidosis.
d. hypochloremic, hypokalemic alkalosis.
e. hypochloremic, hyponatremic acidosis.
308. Which of the following is correct regarding developmental milestones in children?
a. 1 month: holds head in midline
b. 4 months: rolls
c. 6 months: uses pincer response
d. 9 months: walks alone
e. 12 months: creeps up stairs
309. Sudden infant death syndrome (SIDS):
a. is most common in the neonatal period, peaking at 2 months of life, and then tapering off by 4
months.
b. is more common in countries where infants sleep supine.
c. is primarily a cardiac event.
d. does not occur more frequently in infants with apnea of prematurity.
e. means a higher risk for similar occurrence in siblings.
310. A clean wound located in a highly vascular area, such as the face, can safely be closed if the patient
presents within a maximum of:
a. 6 hours.
b. 10 hours.
c. 18 hours.
d. 24 hours.
e. 48 hours.
311. A 34-year-old man has extensive lacerations of his left ear after he disagreed with a local bartender
over the accuracy of his account. In preparing to reassemble his damaged ear, you tell the patient
that you will numb his entire ear by:
a. injecting lidocaine without epinephrine and raising a wheal about the entire base of the ear.
b. injecting lidocaine with epinephrine directly into the wound.
c. injecting lidocaine without epinephrine directly into the wound.
d. doing a hemi-facial nerve block.
e. performing conscious sedation, as there is no good way to regionally block an ear.
312. The best way to control the pain from a femoral shaft fracture is by using:
a. Buck’s traction.
b. a femoral nerve block.
c. a combination of injectable opioid and non-narcotic pain medicine.
d. a steroid injection of the trochanteric bursa.
e. high-dose intravenous narcotic injection.
116
307. d
th
Rosen 5 ,
Chapter 165,
p. 2297-2301
308. b
th
Rosen 5 ,
Chapter 160,
p. 2228
309. d
Rosen 5th,
Chapter 170,
p. 2392-2396
310. d
Rosen 5th,
Chapter 35,
p. 318
311. a
th
Rosen 5 ,
Chapter 35,
p. 321
312. b
Rosen 5th,
Chapter 49,
p. 655
Extensive and protracted vomiting in pyloric stenosis may lead to hypokalemia and
hyponatremia. More striking decreases occur in chloride concentration and an increase
in pH and carbon dioxide content. This constitutes the characteristic changes of
hypochloremic alkalosis.
A one month old can raise his head only slightly from the prone position. A 2-month
old can hold his head in midline and lift his chest off the table. A 4 month old can
roll,. At 6-months an infant can sit unsupported, but it is not until 9 months that the
pincer grasp begins and the infant starts to cruise and crawl. Walking alone typically
occurs at 1 year of age and creeping up stairs occurs at 15 months of age.
Apnea of prematurity is not a risk factor for SIDS. SIDS is rare in the first month of
life, probably because the neonate has a better anaerobic capacity for survival, and with
a gasp may be able to raise his or her arterial PO2 over 20 mmHg and continue
breathing. Victims range in age from 1 month to 1 year, with peaks at 2½ months and
at 4 months. Epidemiologic studies indicate that the incidence of SIDS is lower in
countries where infants sleep supine or in the side-down position. Death is a
respiratory rather than cardiac event, and some potential SIDS victims may be
successfully resuscitated with ventilation alone. Factors that do not appear to increase
the risk of SIDS include maternal alcohol use, recent diphtheria-pertussis-tetanus
(DPT) or other vaccine administration, being a sibling of a SIDS victim, sickle cell
disease, and bronchopulmonary dysplasia.
Although the incidence of bacterial contamination and the risk of infection increase
with injuries more than 4 hours old, clean wounds in highly vascular areas (scalp, face,
and neck) have an incidence of infection so low that primary closure may be possible
even up to 24 hours after injury.
Anesthesia of the ear is best achieved by raising a wheal with lidocaine with no
epinephrine about the entire base of the ear. This anesthetizes all but the external canal
and concha, which, if involved with the injury, require direct infiltration with plain
lidocaine.
Femoral nerve block is an effective technique for relieving pain of a femoral shaft
fracture and is useful in the multitrauma patient when minimizing narcotics is
important. The femoral nerve is lateral to the femoral artery at the inguinal ligament
and innervates the anterior thigh, the periosteum of the femur, and the knee joint.
117
313. A 74-year-old retired staff surgeon slipped on some urine while visiting his
Rosen 5th, Figure
wife, who recently had a mastectomy. His right leg is externally rotated and
49-14
shortened, and his x-ray is shown (Figure 49-14). He demands to see the
orthopedic surgeon who performed the original procedure, but you tell him
that the orthopedic doctor recently moved to Arizona because of the cost of
his malpractice insurance. He reluctantly allows you to attempt reduction.
You know the best way to get the prosthesis back is through:
a. longitudinal traction with simultaneous flexion and internal rotation, then
abduction.
b. longitudinal traction with simultaneous flexion and external rotation, then
adduction.
c. longitudinal compression with simultaneous extension and internal
rotation, then abduction.
d. longitudinal traction with simultaneous extension and external rotation, then abduction.
e. longitudinal compression with simultaneous extension and external rotation, then adduction.
314. Herpetic whitlow:
a. is usually caused by HSV-2 virus, especially in health-care workers.
b. heals more rapidly after incision and drainage.
c. is frequently painful and accompanied by axillary adenopathy.
d. usually involves several digits simultaneously.
e. clears rapidly with topical acyclovir.
315. A 27-year-old woman suffered a deep laceration of her left calf. You cannot see the base of the
wound. She tells you “it feels like there’s something in there.” You know that:
a. patients who report the sensation of “something in the wound” should be taken seriously, as their
perceptions are usually correct.
b. ultrasound is the gold standard for finding foreign bodies.
c. glass must be leaded for standard radiographs to find.
d. plain radiographs find less than 50% of foreign bodies.
e. it is not essential to find foreign bodies, as they inevitably “work their way out.”
316. The drug of choice to treat Rocky Mountain Spotted Fever in a 6 year-old girl is:
a. azithromycin.
b. chloramphenicol.
c. doxycycline.
d. cephalexin.
e. linezolid.
317. Most cases of infant botulism are caused by ingestion of:
a. well-water.
b. canned baby food.
c. inadequately prepared instant formula.
d. raw chicken.
e. raw honey.
118
313. a
th
Rosen 5 ,
Chapter 49,
p. 665-666
314. c
th
Rosen 5 ,
Chapter 43,
p. 530-531
315. a
Rosen 5th,
Chapter 53,
p. 770-771
316. b
Rosen 5th,
Chapter 128,
p. 1895
317. e
Rosen 5th,
Chapter 123,
p. 1795
Treatment for the dislocation is early closed reduction, usually under conscious
sedation. Strong, in-line traction is done with simultaneous flexion and internal
rotation. Finally, the hip is abducted once the head clears the rim of the acetabulum.
Herpetic whitlow is a primary or recurrent HSV infection of the finger. HSV-1 is seen
in health care workers who are exposed to infected oral secretions. HSV-2 is more
common among adults due to digital/genital contact in the community. The disease is
usually limited to a single digit. Herpetic whitlow is frequently painful and
accompanied by axillary adenopathy. Vesicles, which may be recognizable early in
the course of the disease, coalesce and may appear to contain pus, but actually contain
necrotic epithelial cells causing the purulent appearance. Whitlow may be
misdiagnosed as a paronychia and incised, which may delay healing or allow a
secondary infection to occur. For patients with frequent painful recurrences
suppressive therapy with systemic acyclovir may be effective. Topical acyclovir has
not been shown to be effective in either the treatment or prophylaxis of this disorder.
If a foreign body is suspected but not found during exploration of a wound, a plain film
should be ordered first, since plain radiography will detect as many as 80 to 90% of all
foreign bodies. When a foreign body is suspected but cannot be palpated or visualized,
plain films should be performed in an attempt to determine the location, size, and
number of foreign objects present. Even when the foreign body is not visualized,
radiographs may show secondary changes (e.g., pulmonary air trapping) providing
clues to foreign body presence. To assist in the localization of the object, two views—
anteroposterior (AP) and lateral—are usually necessary. Objects such as metal or
gravel, which are denser than the tissue in which they are embedded, are usually easy
to visualize on plain radiographs. However, organic material, which has a density
similar to that of human tissue, may not be seen on plain films. Besides plain
radiographs, other techniques may be useful for ED workup of foreign bodies. These
modalities include fluoroscopy, contrast studies, computed tomography (CT) scanning,
magnetic resonance imaging (MRI), and ultrasound (US).
Tetracycline or doxycycline is the antibiotic of choice to treat Rocky Mountain Spotted
Fever, but chloramphenicol can be used for patients allergic to tetracycline and in
children younger than 9 years of age. A usual course is 6 to 10 days and should
continue for 72 hours after defervescence. Sulfa drugs should be avoided, as they can
exacerbate the illness. Rickettsiae are routinely resistant to penicillins, cephalosporins,
aminoglycosides, and erythromycin.
Adults can get botulism not by bacterial infestation but by ingestion of botulinum toxin
through exposure to foods such as home-canned vegetables. Unlike adults, infants,
whose guts are not colonized fully, are susceptible to infection with viable bacteria that
elaborate toxin. Parents of infants should be questioned for possible ingestion of C.
botulinum spores, commonly transmitted by feeding honey, but occasionally reported
with corn syrup.
119
318. Synchronized intermittent ventilation (SIMV) prevents:
a. decreased renal blood flow.
b. decreased venous return to the heart and decreased cardiac output.
c. nosocomial infections of the lungs and sinuses.
d. respiratory alkalosis.
e. stacking breaths, which can lead to barotrauma.
319. A majority of acute hemolytic transfusion reactions result from:
a. antibodies in the donor's type O serum against the recipient's A or B antigen.
b. antigen-antibody reaction to the Rh factor.
c. emergent use of uncrossed matched type O-negative blood.
d. transfusion of the wrong unit of blood due to clerical error.
e. undetected leukocyte antibodies.
320. The safest place in the body for hydrocarbons is the:
a. stomach.
b. colon.
c. duodenum.
d. jejunum.
e. ileum.
321. Rhabdomyolysis is defined by:
a. end organ damage.
b. total serum creatine kinase more than five times normal.
c. total serum creatine kinase higher than 1000.
d. total serum myoglobin more than three times normal.
e. total plasma myoglobin higher than 1 mg/dl.
322. Eikenella corrodens is a worrisome bacteria found most commonly in injuries caused by:
a. cat bites.
b. foot punctures through an old sneaker.
c. lionfish spines.
d. human bites.
e. camel bites.
323. Twenty-four hours after she was exposed to an unknown amount of radiation, a 45-year-old woman
has an absolute lymphocyte count of 1500. This means she:
a. will almost certainly die, no matter what treatment you provide.
b. has a 50:50 chance of survival.
c. can survive, but only after aggressive therapy.
d. had exposure in excess of 2000 rad.
e. requires no special care, as she is expected to survive without complications.
324. An example of an ester local anesthetic is:
a. lidocaine.
b. tetracaine.
c. mepivacaine.
d. bupivacaine.
e. prilocaine.
120
318. e
th
Rosen 5 ,
Chapter 2,
p. 22
319. d
th
Rosen 5 ,
Chapter 5,
p. 50
320. a
Rosen 5th,
Chapter 152,
p. 2162
321. b
th
Rosen 5 ,
Chapter 121,
p. 1766
322. d
th
Rosen 5 ,
Chapter 54,
p. 781
323. e
Rosen 5th,
Chapter 140,
p. 2059-2060
324. b
Rosen 5th,
Chapter 182
p.2571
Synchronized intermittent ventilation (SIMV) supports a patient's spontaneous breath
at a preset rate that prevents a mechanical breath being delivered at the same time as a
spontaneous breath (stacking). The other choices are all potential adverse effects of
positive-pressure ventilation.
Acute intravascular hemolytic transfusion reactions are immediate and life threatening.
They are usually the result of ABO incompatibility, most often due to clerical error
(e.g., mislabeling of blood product, misidentification of patient). Because RBCs of
type O do not have A or B antigens on their surface, they are not agglutinated or
hemolyzed by anti-A or anti-B antibodies. Less severe and more common febrile
transfusion reactions are due to antileukocyte and antiplatelet antibodies, seen in
multiply transfused patients.
The aphorism, “the safest place in the body for hydrocarbons is the duodenum,” holds
true for most hydrocarbons regardless of the volume ingested. There is a high toxicity
to the lungs, but low systemic toxicity to the gastrointestinal track, with low potential
for GI absorption.
A specific creatine kinase level cannot define rhabdomyolysis. In general, however, a
creatine kinase level greater than five times normal is diagnostic, but levels as high as
several hundred thousand have been reported.
Eikenella corrodens, a facultatively anaerobic gram-negative rod harbored in human
dental plaque, is found in 25% to 29% of human closed fist injury infections. It acts
synergistically with aerobic organisms, most frequently streptococci, and is thought to
account for greater morbidity in these wounds. E. corrodens is susceptible to
penicillin, ampicillin, second- and third-generation cephalosporins, carbenicillin,
tetracycline, and the fluoroquinolones.
The lymphocyte count 24 hours postexposure is useful in predicting the patient’s
clinical course. If the lymphocyte count is maintained above 1200/mL, it is unlikely
the patient has received a lethal dose of radiation and no clinical support is required. If
the absolute lymphocyte count falls between 300 and 1200 at 48 hours, the possibility
of exposure to a lethal dose of radiation should be suspected. Levels less than 300 are
critical and require heroic measures.
Local anesthetic agents are chemical compounds that consist of an aromatic and an
amine group separated by an intermediate chain. The class that has an ester link
between the intermediate chain and aromatic portion are called amino esters; procaine,
chloroprocaine, and tetracaine are the only ones in use today. Amides have an amide
link and are more commonly used; lidocaine, mepivacaine, prilocaine, bupivacaine,
and etidocaine are examples (Notice that they all have two ‘i’s). Esters are unstable in
solution and are metabolized in the body by the plasma enzyme cholinesterase.
Enzymes in the liver destroy the amides after absorption.
121
325. The LD50 from exposure to ionizing radiation is defined as the dose of penetrating ionizing
radiation that will result in the deaths of 50% of the exposed population within 60 days. In humans
who receive aggressive post-exposure therapy, this number is generally accepted to be:
a. 0.5 Gy (50 rad).
b. 1.0 Gy (100 rad)
c. 4.5 Gy (450 rad).
d. 6.0 Gy (600 rad)
e. 10.0 Gy (1000 rad).
326. Hyperbaric oxygen therapy is contraindicated in the patient with:
a. acute sinusitis.
b. pregnancy.
c. disulfiram (Antabuse®) therapy.
d. epilepsy.
e. metallic prostheses.
327. Chondromalacia patellae:
a. is a traumatic syndrome of the patella ligament.
b. is caused by patellofemoral malalignment, leading to excessive lateral pressure on the articular
cartilage.
c. is most common in adolescent male athletes
d. causes joint effusion and generalized knee pain.
e. is made worse with descending stairs and squatting down.
Rosen 5th, Figure 50-9
328. Several young men coveted the jacket previously worn by the
patient whose x-ray is shown here (Figure 50-9). He refused to
relinquish this valued possession, having worked long and hard
at a menial position in order to earn the money to honestly
purchase it. After forcefully removing the aforementioned
jacket, the assailants jumped up and down on his leg a few times.
The nerve most likely to be affected is the:
a. peroneal.
b. superficial femoral.
c. deep femoral.
d. tibial.
e. sciatic.
329. A normal reticulocyte count is:
a. 0.5 – 1.5%
b. 2.0 – 5.0%
c. 6.0 – 7.5%
d. 7.5 – 10.0%
e. >10%
122
325. c
th
Rosen 5 ,
Chapter 140,
p. 2059
326. c
th
Rosen 5 ,
Chapter 194,
p. 2700
327. b
Rosen 5th,
Chapter 50,
p. 688-689
328. a
Rosen 5th,
Chapter 50,
p. 689
329. a
Rosen 5th,
Chapter 115,
p. 1665
The median lethal whole body dose (i.e., the dose that is lethal for 50% of test
subjects)for human beings is estimated to be about 4.5 Gy if victims are hospitalized
and receive aggressive care. With whole-body exposure of more than 10 Gy, mortality
is nearly 100% unless bone marrow transplantation is performed.
Very few absolute contraindications to HBO therapy exist. Treatment with
doxorubicin, cisplatin, bleomycin, disulfiram, and mafenide acetate is considered a
contraindication to HBO therapy because of potentially toxic effects when combined
with HBO. An untreated pneumothorax is an absolute contraindication because of the
concern that it may progress to a tension pneumothorax, particularly during
decompression.
The patellofemoral pain syndrome refers to the clinical presentation of anterior knee
pain related to changes in the patellofemoral articulation. The term chondromalacia
has been used imprecisely to define this syndrome, but this is a pathologic term that
refers to softening of the articular cartilage. A typical presentation is nonspecific
anterior knee discomfort that is nonradiating and occurs in a teenage girl. The knee is
more painful with prolonged flexion, and the discomfort is typically accentuated by
stair climbing and kneeling.
The popliteal neurovascular bundle, composed of the popliteal artery, popliteal vein,
and common peroneal nerve, runs posteriorly behind all bony and ligamentous
structures in the popliteal fossa. The popliteal artery is fixed in the fibrous tunnel of
the adductor magnus hiatus proximally and traverses the fibrous arch of the soleus and
interosseous membrane distally. In essence, it is tethered to both the femur and tibia,
and its inherent immobility renders it susceptible to injury during dislocation. At that
time, the popliteal artery may be stretched, lacerated, or contused. Because of the
parallel course of the popliteal vein and peroneal nerve, they are vulnerable to a similar
injury.
When the late normoblast extrudes its nucleus, it still contains a ribosomal network,
which identifies the reticulocyte. The reticulocyte retains its ribosomal network for
about 4 days, of which 3 are spent in the bone marrow and 1 in the peripheral
circulation. The red blood cell matures as the reticulocyte loses its ribosomal network
and circulates for 110 to 120 days. The erythrocyte is then removed by macrophages
that detect senescent signals. Thus at any given time, approximately 1% of circulating
erythrocytes can be identified as reticulocytes.
123
330. A 56-year-old man was found unconscious in a nearby wooded area. Medics report that his dog
was lying dead next to him. As you undress him for
examination, you see these skin findings and realize
the cause of his coma is exposure to:
a. cyanide.
b. hydrofluoric acid.
c. herbicide aerial spray.
d. lightning.
e. carbon tetrachloride.
331. Metformin:
a. is more appropriately termed an antihyperglycemic than a hypoglycemic agent.
b. decreases peripheral sensitivity to insulin.
c. suppresses exogenous glucose uptake.
d. stimulates insulin secretion.
e. causes profound hypoglycemia if taken in error by a non-diabetic.
332. A 63-year-old woman developed acute left-sided weakness and garbled speech about 40 minutes
prior to arrival. Her head CT is unremarkable and she has no contraindications, so you choose to
treat her with:
a. low-molecular weight heparin, 1 unit/kg subcutaneously.
b. recombinant tissue plasminogen activator, 0.9 mg/kg, maximum 90 mg; first 10% administered as
bolus, with remaining amount infused over 60 minutes.
c. recombinant tissue plasminogen activator 90 mg IV bolus.
d. streptokinase IV.
e. nothing has been shown effective in this scenario.
333. A comatose 19-year-old man is brought from his college dormitory room. His roommate found
him at the end of classes today, but did not accompany him to the hospital. Fortunately he is
wearing a Medic Alert bracelet that identifies him as diabetic. He also smells like fingernail polish
remover. His bedside glucose is too high to be read, so you empirically start an intravenous with
normal saline solution after blood work is sent to the laboratory. You get a call several minutes
later with some “panic values:” Na+: 129, K+: 3.8; HCO3- : 12, glucose: 745. You know that the
corrected sodium is actually:
a. 119
b. 129
c. 134
d. 139
e. 145
334. A 47-year-old diabetic woman complains of a severe headache, fever, and a green-black nasal
discharge. She has generalized left facial swelling and redness, but does not have proptosis. You
see necrosis of the inferior turbinate, and a black spot on the soft palate. You know that she will
require aggressive treatment with intravenous:
a. vancomycin.
b. gentamicin.
c. cyclosporine.
d. dexamethasone.
e. amphotericin B.
124
330. d
th
Rosen 5 ,
Chapter 136,
p. 2014
331. a
th
Rosen 5 ,
Chapter 120,
p. 1759
332. b
Rosen 5th,
Chapter 95,
p. 1440-1441
333. d
Rosen 5th,
Chapter 119,
p. 1724
334. e
Rosen 5th,
Chapter 70,
p. 982, 983
Feathering burns are not true burns because there is no damage to the skin itself. They
seem to be caused by electron showers induced by the lightning that make a fern
pattern on the skin. These fern patterns are called Lichtenberg figures and are
pathognomonic for lightning.
Metformin works by decreasing hepatic glucose output, leading to decreased insulin
resistance and lower blood glucose. Used alone, metformin does not cause
hypoglycemia; it is contraindicated in patients with renal insufficiency and metabolic
acidosis, and must be used with caution in patients with hypoxemia, liver compromise,
and alcohol abuse.
To date, the Food and Drug Administration (FDA) have approved only the use of
intravenous tPA for treatment of patients with acute ischemic stroke. These
recommendations were based on the results of the National Institutes of Neurological
Disorders and Stroke (NINDS) trial. The total dose of rt-PA is 0.9 mg/kg, with a
maximum dose of 90 mg; 10% of the dose is administered as a bolus, with the
remaining amount infused over 60 minutes. Heparin is frequently prescribed for
patients with acute ischemic stroke or TIAs, but its value is unproved. Streptokinase is
not recommended for use in patients with acute ischemic strokes.
745 – 100 = 645 / 1.6 = 10.3 + 129 = 139.
Redistributive hyponatremia is caused by osmotically active solutes in the extracellular
space that draw water from the cell, diluting the serum sodium concentration.
Common situations causing such hyperosmolar states include hyperglycemia (e.g.,
diabetic ketoacidosis) and parenteral administration of mannitol or glycerol for the
management of intracranial hypertension or glaucoma. The measured serum sodium in
patients with hyperglycemia can be corrected by adding approximately 1.6 mEq/L for
every 100-mg/dl rise in the serum glucose over 100 mg/dl.
Invasive fungal sinusitis is an aggressive opportunistic rhinocerebral infection that
affects immunocompromised hosts. Mucormycosis (Rhizopus) is usually associated
with fever, localized nasal pain, and cloudy rhinorrhea. On examination, the affected
tissue (usually the turbinates) appears gray, friable, anesthetic, and nonbleeding
because of infarction caused by mucormycotic angioinvasion. In advanced cases the
tissues are necrotic and black, and the infection spreads beyond the sinus. Acute
fulminant fungal sinusitis requires emergent consultation and admission for IV
antifungal therapy and aggressive surgical debridement.
125
335. This 56-year-old woman was started on a new medication
last week after she visited a walk-in clinic. Today she is
toxic in appearance, and large sheets of skin are peeling
from her back (Figure 114-8). The old chart is not
available, and the patient only remembers that her “face
hurt.” You recognize that the most likely culprit is:
a. prednisone for Bell’s palsy.
b. doxycycline for Lyme-induced Bell’s palsy.
c. clindamycin for dental abscess.
d. carbamazepine for trigeminal neuralgia.
e. cephalexin for erysipelas.
Rosen 5th, Figure 114-8
126
335. d
th
Rosen 5 ,
Chapter 114,
p. 1643
The main feature of nonstaphylococcal-induced toxic epidermal necrolysis (TEN), or
Lyell’s disease, is the separation of large sheets of epidermis from underlying dermis.
The full thickness of epidermis is involved. The two conditions are easily
histologically distinguishable with a skin biopsy. A mortality rate of 15% to 20% is
expected with this condition. Drugs including the long-acting sulfa drugs, penicillin,
aspirin, barbiturates, phenytoin, carbamazepine, allopurinol, and nonsteroidal antiinflammatory drugs are an important cause of TEN.
127
Abdominal and Gastrointestinal Disorders
336. In adults the most common source of upper gastrointestinal bleeding is:
a. Mallory-Weiss tear.
b. peptic ulcer disease.
c. esophageal varices.
d. esophagitis.
e. gastric erosions.
337. Melana is:
a. present in 95% of upper gastrointestinal bleeds.
b. from blood that has been in the GI tract for at least 24 hours.
c. present in approximately one-third of lower gastrointestinal bleeds.
d. may occur from as little as 10 mls of blood in the GI tract.
e. stool that will remain black and tarry for no more than 24 hours after bleeding stops.
338. Antiemetic drugs work by:
a. suppressing the vomiting center in the brain.
b. depressing the chemoreceptor trigger zone.
c. inhibiting impulses to the chemoreceptor trigger zone from the vestibular apparatus.
d. inhibiting impulses to the vomiting center from peripheral receptors.
e. all of the above.
339. In adults the most common cause of nausea and vomiting is:
a. cholecystitis.
b. medication.
c. kidney stones.
d. migraine headache.
e. myocardial infarction.
340. A patient is sent to the emergency department by his primary doctor to rule out gastric outlet
obstruction. After talking to him, you also believe that gastric outlet obstruction is the most likely
diagnosis given his symptom of:
a. emesis that is both bilious and bloody.
b. abdominal distention with normoactive bowel sounds.
c. vomiting during meals.
d. vomiting made worse by lying supine.
e. vomiting of material eaten more than 12 hours previously.
341. The most common cause of neuromuscular swallowing dysfunction is:
a. stroke.
b. myasthenia gravis.
c. poliomyelitis.
d. polymyositis.
e. tetanus.
128
336. b
th
Rosen 5 ,
Chapter 23,
p. 194-195
337. c
th
Rosen 5 ,
Chapter 23,
p. 195
338. e
Rosen 5th,
Chapter 21,
p. 179
339. b
Rosen 5th,
Chapter 21
p. 178
340. e
th
Rosen 5 ,
Chapter 21,
p. 180-181
341. a
th
Rosen 5 ,
Chapter 84,
p. 1245
In adults the most common causes – in descending order – of upper gastrointestinal
bleed are: peptic ulcer disease , gastric erosions, varices, and Mallory-Weiss tears.
The top three account for approximately three fourths of adult patients with upper GI
bleed..
Melena, or black tarry stool, occurs from approximately 150-200 ml of blood in the GI
tract. Melena is present in approximately 70% of upper GI bleeds and 33% of lower
GI bleeds. Black nontarry stool may result from as little as 60ml of blood. Blood from
the jejunum or duodenum must remain in the GI tract for at least 8 hours before turning
black. Stool may remain black and tarry for several days after bleeding has stopped.
The chemoreceptor trigger zone area is rich in dopamine D2 receptors, which are
antagonized by drugs such as prochlorperazine, metoclopramide, and droperidol. The
serotonin receptor has been found widely in the area postrema and the GI tract. It may
act both directly and through the release of dopamine. Serotonin receptor antagonists
(ondansetron, alosetron, granisetron) have been shown to be effective in preventing
chemotherapy-induced nausea and vomiting. Concentrations of cholinergic and
histamine receptors are found in the lateral vestibular nucleus and are important in
motion sickness. Meclizine, diphenhydramine, and scopolamine act by antagonizing
these receptors.
In adult medicine, nausea and vomiting are most often caused by medications. The
most common causes of nausea and vomiting are acute gastroenteritis, febrile systemic
illnesses, and drug effects. Acute viral gastroenteritis is the most common GI disease
in the United States.
Vomiting of material eaten more than 12 hours previously is pathognomonic for outlet
obstruction. Bilious emesis essentially rules out a gastric outlet obstruction. Highpitched bowel sounds suggest a gastric outlet obstruction.
Neuromuscular diseases cause approximately 80 % of oropharyngeal dysphagias.
Strokes are probably the most common cause of neuromuscular dysphagia, and
pharyngeal muscle weakness is often the mechanism. The second most common cause
of neuromuscular dysphagia is polymyositis or dermatomyositis. These disorders are
characterized by inflammatory and degenerative changes that produce weakness of the
palate, pharynx, and upper esophagus.
129
342. A 25-year-old man complains of a severe intermittent substernal chest pain. It started suddenly
while he was lying in bed. He admits to several months of difficulty swallowing solids and liquids,
and he occasionally has to stand when he eats to help food pass into his stomach. Physical
examination reveals an underweight male with no abnormal findings. His 12-lead ECG is normal.
His probable diagnosis is:
a. gastroesophageal reflux.
b. achalasia.
c. nutcracker esophagus.
d. spontaneous esophageal perforation (Boerhaave’s syndrome).
e. duodenal ulcer.
343. In distinguishing chest pain caused by gastroesophageal disease from that caused by coronary
disease, the most helpful historical point is probably:
a. pain made worse by postural changes and swallowing.
b. pain precipitated by high emotional state.
c. pain which is almost always relieved by antacids.
d. pain precipitated by exercise and relieved by rest.
e. radiation of pain into the neck or the jaw.
344. The majority of esophageal perforations are:
a. spontaneous.
b. iatrogenic.
c. traumatic.
d. caused by caustic ingestion.
e. idiopathic.
345. One of the most common etiologies of peptic ulcer disease is:
a. dietary indiscretion.
b. Helicobacter pylori infection.
c. idiopathic.
d. increased parietal cell mass.
e. Zollinger-Ellison syndrome.
346. The description of abdominal pain may be helpful in its evaluation. For instance:
a. pain from ulcer disease is often described as colicky.
b. acute gastric volvulus is likely to present with mild pain.
c. peptic ulcer pain is classically described as a burning or gnawing quality.
d. pain from iatrogenic esophageal perforation always occurs immediately after the procedure.
e. pain from a perforated duodenal ulcer is usually appreciated in the epigastrium only and rarely
becomes generalized.
347. Treatment of choice for acute gastric volvulus is:
a. watchful waiting.
b. endoscopic decompression.
c. combined Trendelenberg / left lateral decubitus position.
d. attempted reduction by barium swallow.
e. surgery.
130
342. b
th
Rosen 5 ,
Chapter 84,
p. 1246
343. a
Rosen 5th,
Chapter 84,
p. 1238, 1240
344. b
Rosen 5th,
Chapter 38,
p. 406-409
Chapter 84,
p. 1236
345. b
th
Rosen 5 ,
Chapter 84,
p. 1241
346. c
th
Rosen 5 ,
Chapter 84,
p. 1236,
1242-1244
347. e
Rosen 5th,
Chapter 84,
p. 1244
Achalasia is a disorder in which there is a marked increase in the resting pressure of
the lower esophageal sphincter and absent peristalsis in the body of the esophagus.
Dysphagia is common. Odynophagia, from esophageal spasm may be seen early in the
course of the disease. Symptoms often worsen with rapid eating and stress. A dilated
esophagus with air-fluid levels may be seen on chest x-ray.
Esophageal pain is more likely to be positional and related to swallowing. Radiation
of pain is an inconstant finding in both esophageal and cardiac chest pain.
Precipitation of pain by exercise and relief by rest may occur in pain from reflux or
ischemic heart disease. Emotional precipitation of pain occurs in reflux, although it is
also seen in coronary artery disease. Relief of chest pain from reflux by antacids is a
key point in the history, however the emergency physician should not place too much
weight upon this point as evidence against a cardiac etiology. The relief is often short
lived, and may recur in a short time.
Spontaneous esophageal perforation accounts for only 15% of cases, with iatrogenic
injuries accounting for most of the remainder. These usually occur as a complication
of upper endoscopy, dilation, sclerotherapy, or other GI procedures.
Peptic ulcer disease is considered to have two main etiologies: Helicobacter pylori
infection and NSAID use. Only about 1% of PUD is caused by increased levels of
circulating gastrin from gastrin-secreting tumors (Zollinger-Ellison syndrome). These
patients have increased parietal cell mass and hypersecretion of acid.
Colicky pain is rarely gastric or duodenal in origin. Classically ulcer pain is described
as nonradiating epigastric pain of a burning or gnawing quality. Primary volvulus may
present with the sudden onset of severe pain. Pain from an iatrogenic perforation may
not appear until several hours after the procedure. Pain from a perforated duodenal
ulcer is usually appreciated first in the epigastrium but becomes generalized within a
short time
Treatment of an acute gastric volvulus is surgical. Acutely, one should attempt
passage of a nasogastric tube, as this may occasionally reduce the volvulus. There
have also been reports of reductions of volvulus using endoscopy, but this is best
reserved for patients who cannot tolerate surgery or who have no evidence of vascular
compromise.
131
348. A patient with a known exposure to hepatitis B presents with right upper quadrant abdominal pain
and scleral icterus. You know that her serum bilirubin must be at least:
a. 1.5 mg/dl.
b. 2.0 mg/dl.
c. 2.5 mg/dl.
d. 3.0 mg/dl.
e. 3.5 mg dl.
349. Of the tests listed, the one MOST ACCURATE in predicting a fulminant course of disease in a
patient with hepatitis is:
a. prolonged prothrombin time.
b. bilirubin higher than 10 mg/dl.
c. AST several times higher than ALT.
d. alkaline phosphatase more than 5 times normal.
e. lactate dehydrogenase more than 10 times normal.
350. A newly hired housekeeper is stuck with a hollow needle while picking up trash in a room recently
vacated by a patient known to have chronic hepatitis B. She has not yet started her primary
hepatitis prophylaxis series. You decide to:
a. send antibody levels (HBSAg) on the employee and determine treatment based on the results.
b. give her hepatitis B immune globulin (HBIG) 0.06 ml/kg and start the hepatitis B vaccine series,
with the first shot in the buttock.
c. give her hepatitis B immune globulin (HBIG) 0.06 ml/kg and start the hepatitis B vaccine series,
with the first shot in the deltoid.
d. give her hepatitis B immune globulin (HBIG) 0.6 ml/kg and start the hepatitis B vaccine series,
with the first shot in the buttock.
e. give her hepatitis B immune globulin (HBIG) 0.6 ml/kg and start the hepatitis B vaccine series,
with the first shot in the deltoid.
351. Ascites occurs as a consequence of:
a. portal hypertension.
b. impaired hepatic lymph flow.
c. hypoalbuminemia.
d. renal salt retention.
e. all of the above.
352. The organism which causes the majority of spontaneous bacterial peritonitis is:
a. Streptococcus pneumoniae.
b. Escherichia coli.
c. Klebsiella pneumoniae.
d. Staphylococcus aureus.
e. Pseudomonas abdominus
353. In children, the majority of acute esophageal obstructions are caused by:
a. balloons.
b. coins.
c. food.
d. strictures.
e. surgical procedures.
132
348. c
th
Rosen 5 ,
Chapter 85,
p. 1253
349. a
th
Rosen 5 ,
Chapter 85,
p. 1253
350. c
Rosen 5th,
Chapter 85,
p. 1256
351. e
Rosen 5th,
Chapter 85,
p. 1259
352.b
Rosen 5th,
Chapter 85,
p, 1261
353. b
Rosen 5th,
Chapter 84,
p. 1234
Scleral icterus usually is not clinically apparent, even to the most astute observers,
until serum bilirubin is above 2.5 mg/dl. Muddy sclera, commonly found among
African-American patients, may obscure or confuse this finding. An alternative in this
setting is examination of sublingual or subungual surfaces.
Prothrombin time (PT) is a useful test to assess the degree of hepatic synthetic
dysfunction. Elevation of the PT may be the first clue of a complicated course. The
white blood count (WBC) generally is not useful because values range from low
overall counts with a lymphocytic predominance to marked polymorphonuclear
leukocytosis. The typical case is associated with elevations (tenfold to 100-fold) of
serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT), with
ALT generally elevated in excess of AST. Bilirubin may be moderately increased (5 to
10 mg/dl) and occasionally is markedly elevated (15 to 25 mg/dl). Alkaline
phosphatase and lactate dehydrogenase may be elevated but are rarely more than two
to three times normal.
HBV immune globulin (HBIG) is recommended for immediate passive immunization
in individuals not previously immunized but exposed to potentially infective material.
HBIG alone diminishes the risk of HBV infection by 75%. Unvaccinated, exposed
people should receive HBIG 0.06 ml/kg intramuscularly (IM) in addition to the HB
vaccine. Centers for Disease Control and Prevention (CDC) data suggest that optimal
immunologic response results from deltoid injection.
Ascites occurs as a consequence of portal hypertension, impaired hepatic lymph flow,
hypoalbuminemia, and renal salt retention. Although ascites generally causes little
more than unsightly abdominal distention and discomfort, it can become massive and
lead to respiratory compromise.
E. coli account for approximately 47% to 55% of spontaneous bacterial peritonitis
infections, Streptococcus sp 18%-26%, Klebsilla sp 11%, and Streptococcus
pneumoniae 8%-26%. Polymicrobial and anaerobic infections have been reported but
are not common. A third-generation cephalosporin such as cefotaxime is considered to
be a drug of choice with a demonstrated cure rate of 85%. An alternative would be an
ampicillin sulbactam combination. Ampicillin and an aminoglycoside is a rational and
effective combination but somewhat less desirable due to the risk of renal toxicity.
Eighty percent of foreign body ingestions occur in the pediatric age group, with coins
being the most commonly impacted object. In adults, most impactions are due to
pieces of food, particularly meat and bones.
133
354. Drug-induced liver injury usually causes damage by hepatocellular necrosis or cholestasis. A
commonly used drug which causes hepatonecrotic changes is:
a. amiodarone.
b. anabolic steroids.
c. chlorpromazine.
d. erythromycin estolate.
e. haloperidol.
355. The most likely cause of massive lower GI bleed in a child under two years of age is :
a. duodenal atresia.
b. gastric ulcer.
c. Mallory-Weiss tears.
d. Meckel’s diverticulum.
e. variceal bleeding secondary to portal hypertension.
356. The most common cause of massive lower GI bleed in adults is:
a. diverticular disease.
b. inflammatory bowel disease.
c. internal hemorrhoids.
d. left colon carcinoma.
e. right colon carcinoma.
357. Post-transfusion hepatitis is usually due to:
a. hepatitis A.
b. hepatitis B.
c. hepatitis C.
d. hepatitis D.
e. hepatitis E.
358. An ill-appearing, 47-year-old man complains of severe epigastric pain and vomiting. Lab studies
show a markedly elevated lipase. He is not a drinker. The cause is probably:
a. biliary tract disease.
b. cimetidine therapy.
c. hyperlipidemia.
d. indomethacin therapy.
e. infection.
359. The second most common cause of small bowel obstruction in the United States:
a. abscess.
b. congenital abnormality.
c. Crohn’s disease.
d. hernia.
e. regional enteritis.
360. Epigastric pain which is relieved by food, but which returns between meals is typical for:
a. sliding hiatal hernia.
b. esophagitis.
c. peptic ulcer.
d. pancreatitis.
e. Zollinger-Ellison syndrome.
134
353. a
th
Rosen 5 ,
Chapter 85,
p. 1261-1262
355. d
Rosen 5th,
Chapter 23,
p. 194-195
356. a
Rosen 5th,
Chapter 23,
p. 194-195
357. c
th
Rosen 5 ,
Chapter 85,
p. 1252
358. a
Rosen 5th,
Chapter 86,
p. 1273
359. d
Rosen 5th,
Chapter 87,
p. 1284
360. c
Rosen 5th,
Chapter 84,
p. 1242
Although specific agents tend to cause damage characterized by a particular pattern of
injury, there is considerable overlap. Cellular necrosis is commonly associated with
anesthetic agents (e.g., halothane), the antifungals amphotericin and ketoconazole, or
the antidysrhythmic amiodarone. A cholestatic picture is characteristic of
chlorpromazine, haloperidol, anabolic or oral contraceptive steroids, and erythromycin
estolate.
Esophagitis, gastritis, peptic ulcer disease, esophageal varices, and Mallory-Weiss tears
are common causes of upper GI bleeding in children . In children under the age of 2
years, massive LGIB is most often a result of Meckel’s diverticulum or
intussusception. Anal fissure, infectious colitis, inflammatory bowel disease, and
polyps are other causes of LGIB in children.
At all ages rectal abnormalities are the most common cause of minor LGIB The most
common etiology of significant LGIB in adults is diverticulosis followed by
angiodysplasia .
Although hepatitis C has been most prominently associated with transfusions, only
10% of patients with this disease report a previous history of having received blood or
blood products. The historic risk of hepatitis in patients receiving blood transfusions
was about 0.45% per unit transfused. The screening of donor blood for surrogate
markers (aminotransferases) and antibody to hepatitis C has decreased this risk to
0.03% per unit.
Eighty percent of pancreatitis is caused by either gallstones (about 45%) or alcoholism
(about 35%). The exact mechanism of biliary pancreatitis is not clear. Either a stone
within the bile duct applies transmural pressure on the pancreatic duct or a stone in the
common channel of the pancreatic duct and common bile duct causes obstruction.
Obstruction or pressure on the pancreatic duct causes bile reflux or increased pressure
of pancreatic secretions. Either mechanism leads to the activation of pancreatic
enzymes setting off the cascade of pancreatitis. Many cases that were presumed to be
idiopathic are actually due to small stones, sludge, or crystals that are too small to be
seen by ultrasound examination but may be noted on endoscopic retrograde
cholangiopancreatography (ERCP).
In developed countries, postoperative adhesions are responsible for more than 50% of
all small bowel obstruction. It is estimated that as many as 15% of abdominal
surgeries will eventually result in small bowel obstruction from adhesion. A
particularly high incidence of small bowel obstruction is found after gynecologic or
intestinal surgeries, as well as in those patients who have previously undergone surgery
in the presence of peritonitis or significant abdominal trauma. Other important causes
of small bowel obstruction include hernias and neoplasms, each with an incidence of
approximately 15%. Hernias can be either external or internal.
The most common symptom of PUD is abdominal pain, occurring in 94% of patients
with an ulcer. Classically, ulcer pain is described as nonradiating epigastric pain of a
burning or gnawing quality, although pain in the chest, back, or other areas of the
abdomen may be noted. Relief of pain after eating is a feature of gastric or duodenal
ulcer. Pain usually occurs 2 to 3 hours following a meal or at night.
135
361. You are evaluating a 57-year-old woman with epigastric discomfort, and suspect pancreatitis. You
know that:
a. endocrine products produced by the pancreas include amylase, lipase, trypsin, and other enzymes.
b. in patients with chronic pancreatitis, the degree of pain diminishes with the decreasing amount of
remaining pancreatic tissue.
c. the bile duct, portal vein, splenic vein, vena cava, aorta, and superior mesenteric artery all lie
posterior to the pancreas.
d. pancreatic tumors are usually painful and rapidly progressive.
e. the most common pancreatic disorder is pancreatitis.
362. The pain of uncomplicated small bowel obstruction is frequently:
a. a poorly localized, crampy abdominal pain.
b. a constant and severe abdominal pain.
c. associated with peritoneal signs.
d. mild in proximal intestinal obstructions.
e. associated with explosive profuse diarrhea.
363. A 6-year-old boy is brought by his frantic mother because she found blood on the toilet paper. You
know that the most common cause of this complaint in this age group is:
a. anal fissure.
b. cryptitis.
c. external hemorrhoid.
d. internal hemorrhoid.
e. perirectal abscess.
364. Which of these conditions may be drained appropriately in the emergency department?
a. “horseshoe” abscess.
b. intersphincteric abscess.
c. postanal abscess.
d. perianal abscess.
e. supralevator abscess.
365. Painful anorectal vesicles are most commonly caused by:
a. Chlamydia trachomatis.
b. Herpes simplex.
c. Neisseria gonorrhea.
d. papillomavirus.
e. Treponema pallidum.
366. The most prevalent parasite in the United States is:
a. Cyclospora cayetanensis.
b. Entamoeba histolytica.
c. Enterobius vermicularis.
d. Giardia lamblia.
e. Plasmodium vivax.
136
361. c
th
Rosen 5 ,
Chapter 84,
p. 1272, 1281
362. a
Rosen 5th,
Chapter 87,
p. 1285
363. a
Rosen 5th,
Chapter 23,
p. 195
Chapter 91,
p.1347
364. d
th
Rosen 5 ,
Chapter 9,
p. 1348-1349
365. b
th
Rosen 5 ,
Chapter 91,
p. 1353-1354
366. c
th
Rosen 5 ,
Chapter 89,
p. 1318
The pancreas has both essential exocrine and endocrine functions. Exocrine products
include amylase, lipase, trypsin, chymotrypsin, elastase, carboxypeptidase,
phospholipase, and other enzymes. The endocrine functions of the pancreas are
managed by insulin, glucagon, pancreatic polypeptide, and somatostatin. Advances in
care have decreased hospital mortality from pancreatitis from 25% to 30% to as low as
6% to 10% over the past 30 years. Anterior to the pancreas from right to left is the
transverse colon, the lesser sac of the omentum, and the stomach. Posteriorly lies the
bile duct, portal vein, splenic vein, vena cava, aorta, and superior mesenteric artery.
The presentation of pancreatic cancer is variable because progression of the disease is
indolent. Diabetes is the most common disorder of the pancreas, followed by
pancreatitis.
Patients with small bowel obstruction typically complain of regularly recurrent bouts
of poorly localized abdominal pain lasting from seconds to minutes. Several hours of
severe colicky pain in association with bilious vomiting and mild abdominal distension
is typical of proximal intestinal obstruction, whereas a day or two of progressively
worsening pain and more prominent abdominal distention is typical of distal
obstruction. A change in the description of the pain from intermittent and colicky to
constant and severe may signal the development of complications, such as intestinal
ischemia or perforation. The presence of peritoneal signs usually indicates late
obstruction with complications including strangulation. Patients with complete
obstruction eventually develop obstipation, while those with early or partial
obstruction may continue to pass stool or flatus.
The most common cause of lower GI bleeding in children is an anal fissure. It is also
the most common anorectal problem in the pediatric patient.
Perirectal and perianal abscesses are the most common (40% - 45%) and can be incised
and drained in the Emergency Department in the absence of complicating factors.
In herpes proctitis single or coalesced vesicles and ulcerations occur in the perianal
area and rectum. Syphilis (Treponema pallidum) may form a perianal ulcer or chancre.
Chlamydia may form a perianal ulceration .Gonorrhea may form proctitis with a thick
discharge. HPV (human papillomavirus)may form perianal warts.
Enterobius vermicularis, also known as pinworm or seatworm, is perhaps the most
prevalent parasite in the United States. It is estimated that 20% to 30% of all children
are infected with pinworms, and a total of 30 to 40 million persons are infected.
137
367. In differentiating a patient with cholangitis from one with simple cholecystitis, the most helpful
finding is:
a. fever.
b. hyperlipasemia.
c. jaundice.
d. Murphy’s sign.
e. elevated serum aminotransferases.
368. A 27 year-old man complains of fever and right upper quadrant pain. He is not jaundiced, and his
urine shows only trace bilirubin when dipped. Both ALT and AST are 50 to 60 times the norm.
You suspect:
a. hemolysis.
b. pancreatic disease.
c. biliary disease.
d. liver disease.
e. stomach cancer.
369. The most sensitive and specific test for diagnosing acute cholecystitis is:
a. Nuclear scintigraphy with technetium-99m-labeled IDA (iminodiacetic acid)
b. ultrasound.
c. oral cholecystogram.
d. non-contrast CAT scan of abdomen.
e. oral and intravenous contrast CAT scan of abdomen.
370. The test of choice for detecting the presence of gallstones is:
a. IDA scan.
b. non-contrast CAT scan of abdomen.
c. oral and intravenous contrast CAT scan of abdomen.
d. oral cholecystogram.(OCG)
e. ultrasound.(US)
371. Lipase:
a. hydrolyzes triglycerides.
b. exists only in the pancreas.
c. in acute pancreatitis peaks in 3 hours and levels fall over 24-48 hours.
d. degree of elevation can be used as a marker of pancreatitis disease severity.
e. is definitely an inferior test to amylase levels for pancreatitis.
372. This process in a 2-year-old child may be associated with:
a. celiac sprue.
b. Crohn’s disease.
c. cystic fibrosis.
d. Hirschsprung’s disease.
e. intussusception.
373. The predominant symptom in a patient with diverticulitis is:
a. abdominal pain.
b. bloody stools.
c. constipation.
d. diarrhea.
e. tenesmus.
Rosen 5th,
Figure 91-13
138
367. c
th
Rosen 5 ,
Chapter 85,
p.1267, 1269
368. d
Rosen 5th,
Chapter 85,
p. 1253
369. a
Rosen 5th,
Chapter 85,
p. 1267
370. e
th
Rosen 5 ,
Chapter 85,
p. 1266
371. a
Rosen 5th,
Chapter 86,
p. 1276
372. c
Rosen 5th,
Chapter 91,
p. 1356
373. a
Rosen 5th,
Chapter 90,
p. 1330
Although patients with cholangitis , in general, will have a higher fever and appear
more ill than those with cholecystitis, there can be considerable variability and overlap.
The presence of jaundice is the clinical sign most helpful in differentiating these two
disorders. An elevated bilirubin is characteristic of cholangitis and uncommon in
cholecystitis. Elevated serum aminotransferases may be found in both conditions.
The typical patient with hepatitis has elevations (tenfold to 100-fold) of serum
aspartate aminotransferase (AST) and alanine aminotransferase (ALT), with ALT
generally elevated in excess of AST. Bilirubin may be moderately increased, but
typically emerges several days to a week or more after the onset of clinical symptoms.
Alkaline phosphatase and lactate dehydrogenase may be elevated but are rarely more
than two to three times normal.
Nuclear scintigraphy using technetium-99m-labeled iminodiacetic acid (IDA) is
generally considered the most sensitive and specific test for cholecystitis. Ultrasound
imaging is the most useful test in the ED setting.
Ultrasound is the procedure of choice for investigating the gallbladder. US imaging
can be performed rapidly, does not require the overnight delay necessary with an oral
cholecystogram, is at least as sensitive, and provides the added use of permitting
evaluation of surrounding structures. Oral cholecystogram remains an option for the
patient with clinical suspicion of cholelithiasis in the uncommon circumstance when
US imaging has failed to identify the gallbladder.
Lipase is a pancreatic enzyme that that hydrolyzes triglycerides. Lipase, like amylase,
exists in other tissue. In the presence of pancreatic inflammation it peaks at 24 hours
and the levels fall over 8 to 14 days. The degree of elevation of amylase or lipase is
not a marker of disease severity. Several expert authors recommend using lipase over
amylase when seeking the diagnosis of pancreatitis.
Rectal prolapse, or procidentia, is a disease of the extremes of age. In children,
procidentia may herald the presence of malnutrition or cystic fibrosis, and occurs
during the first 2 years of life. Boys are more commonly affected than girls. Children
usually have a mucosal prolapse. The parent reports protrusion during defecation with
small amounts of mucus or blood. In adults complete procidentia is most common in
older women with a history of excessive straining. The cause is a laxity of attachment
structures and it is often accompanied by uterine prolapse or a cystocele.
The predominant symptom in patients with classical sigmoid diverticulitis is persistent
abdominal pain . Initially the pain may be vague and generalized, but it quickly
becomes well localized to the left lower quadrant. Low grade fever, malaise, and a
change in bowel habits, usually constipation, are common.
139
374. A 48 year-old man has severe abdominal pain that began suddenly as he was driving to work this
morning. He also complains of vomiting, which you see is not bilious. He has diffuse tenderness
on exam. His WBC count is 14,300 / mm. You suspect this is a surgical process rather than
medical because:
a. he has a fever.
b. his pain is diffuse.
c. his white blood cell count is elevated.
d. the pain started before the vomiting.
e. the vomiting started before the pain.
375. A 22 year-old homosexual male complains of rectal itching and a purulent discharge. Anoscopy
shows a proctitis. You suspect the causative organism to be:
a. Campylobacter.
b. Chlamydia.
c. Giardia.
d. N. gonorrhoeae.
e. Herpes simplex.
376. Which statement is correct concerning the patient with a small bowel obstruction?
a. increase in intraluminal pressure result in capillary and lymphatic obstruction.
b. early bowel distention decreases epithelial secretory activity and decreases the amount of fluid in
the bowel lumen.
c. even with aggressive treatment, there is little change in the mortality of patients with small bowel
obstruction.
d. peristalsis decreases during the early stages of the disease process.
e. all complete small bowel obstructions require emergent surgery.
377. The most common clinical manifestation of cholelithiasis is:
a. gallbladder carcinoma.
b. biliary colic.
c. cholecystitis.
d. cholangitis.
e. pancreatitis.
378. Traveler’s diarrhea is most commonly caused by :
a. Shigella.
b. Campylobacter.
c. Giardia lamblia.
d. rotavirus.
e. enterotoxigenic E. coli.
379. Acute mesenteric ischemia is most commonly caused by:
a. arterial thrombosis.
b. arterial embolus.
c. venous occlusion.
d. hypercoagulable state.
e. nonocclusive vascular disease.
140
374. d
th
Rosen 5 ,
Chapter 22,
p. 192
375. d
Rosen 5th,
Chapter 91, p. 1353
Surgical causes of abdominal pain are more likely to present with pain first, followed
by nausea and vomiting, rather than the converse. Diffuse pain is generally
nonsurgical, but may represent the early visceral component of a surgical process.
Fever does not accurately predict significant surgical pathology. Serial white blood
cell counts have failed to discriminate surgical versus nonsurgical conditions.
Gonorrhea causes proctitis that results from anal intercourse or autoinoculation from
vaginal secretions after a 5- to 7-day incubation period. Proctitis may cause bloody or
purulent rectal discharge , tenesmus and pruritus ani.
As intraluminal pressure increases it causes capillary and lymphatic obstruction with
subsequent bowel wall edema. Early bowel distension stimulates epithelial cell
Rosen 5 ,
secretory activity. Mechanical small bowel obstruction stimulates peristalsis.
Chapter 87,
Aggressive treatment has decreased mortality from approximately 60% in 1900 to less
p. 1283,
1284, & 1287 than 5 % today. Up to 35 % to 50% of patients with complete obstruction will have
resolution of symptoms with non-surgical intervention.
377. b Although cholelithiasis is associated with cholecystitis, cholangitis, gallbladder
carcinoma, and pancreatitis, its most common clinical manifestation is biliary colic.
Rosen 5th,
Chapter 85,
p. 1265
378. e Approximately 80 % to 85% of traveler’s diarrhea is caused by bacteria. An estimated
45%-50% is caused by enterotoxigenic E. coli, 8%-12% by Shigella and 7%-9% by
Rosen 5th,
Campylobacter. Rotavirus accounts for 5%-10% and Giardia lamblia accounts for
Chapter 89,
p. 1321,1323 4%-5%.
379. b Although acute mesenteric ischemia may be caused by mesenteric arterial thrombosis,
nonocclusive mesenteric ischemia, mesenteric venous thrombosis and hypercoagulable
Rosen 5th,
states (causing a venous thrombosis), the most common cause is an arterial embolus.
Chapter 87,
p. 1288-1289
376. a
th
141
380. The most predictive finding for appendicitis is:
a. pain for more than 48 hours.
b. migration of initial periumbilical pain to the right lower quadrant.
c. diffuse abdominal pain.
d. lack of abdominal rigidity.
e. history of similar episodes.
381. Cecal volvulus is most common in:
a. infants.
b. young children.
c. institutionalized teenagers.
d. age 25 to 35 years.
e. the elderly.
382. Regarding nasogastric(NG) tubes and lavage:
a. NG tubes do not aggravate hemorrhage from varices or Mallory-Weiss tears.
b. Iced water lavage is recommended in patients with upper GI bleeding.
c. Sterile fluid must be used as an irrigant.
d. Gastric lavage has been shown to reduce blood loss in patients with upper GI bleeding.
e. Gastric lavage has been shown to be completely safe with no serious complications reported.
383. Vomiting secondarily to Bacillus cereus is almost always from eating contaminated:
a. raw oysters.
b. poultry.
c. dairy products.
d. raw fish.
e. fried rice.
384. Meperidine (Demerol®) :
a. has a longer duration of action than morphine.
b. has a metabolite that may cause CNS toxicity.
c. has no significant interaction with MAO inhibitors.
d. has been conclusively shown to be superior to morphine for treating biliary colic.
e. can be used repeatedly in the elderly without undue concern.
385. When considering abdominal pain:
a. somatic pain is dull, constant and poorly localized.
b. somatic pain is intense, intermittent and poorly localized.
c. somatic pain is intense, constant and well localized.
d. visceral pain is dull, intermittent and well localized.
e. visceral pain is intense, constant and well localized.
386. In children, gastroenteritis accompanied by seizures should suggest infection with:
a. Campylobacter.
b. E. coli 0157:H7.
c. Giardia.
d. Salmonella.
e. Shigella.
142
380. b
th
Rosen 5 ,
Chapter 88,
p. 1294
381. d
th
Rosen 5 ,
Chapter 90,
p. 1335
382. a
th
Rosen 5 ,
Chapter 23,
p. 197
383. e
Rosen 5th,
Chapter 89,
p. 1309
384. b
th
Rosen 5 ,
Chapter 182,
p. 2562-2563
385. c
Rosen 5th,
Chapter 22,
p. 190
386. e
Rosen 5th,
Chapter 89,
p. 1304-1305
Three findings that are highly predictive of appendicitis: right lower quadrant pain,
rigidity, and migration of initial periumbilical pain to the right lower quadrant.
Volvulus of the cecum occurs in all ages but is most common in persons 25 to 35 years
of age. Unlike in sigmoid volvulus, severe, chronic constipation is not an underlying
factor, and there is no association with psychiatric or neurological diseases.
No evidence exists that gastric tube placement aggravates hemorrhage from varices or
Mallory-Weis tears. Gastric lavage does not reduce blood loss in patients with UGIB,
and iced lavage is not recommended. The irrigant need not be sterile. Gastric tubes are
safe in most patients but pharyngeal and esophageal perforation, cardiac arrest,
ethmoid sinus fracture with brain trauma and bronchial intubation have all been
reported.
The emetic form of Bacillus cerus illness is almost always caused by the ingestion of
contaminated fried rice.
Meperidine’s duration of action is no longer than morphine’s and most studies have
not shown it to be of a marked advantage for use in biliary tract disease or pancreatitis.
It may have a fatal interaction with MAO inhibitors. It has a CNS toxic metabolite that
is renally excreted and that also has a longer half-life in the elderly.
Visceral pain results from stimulating autonomic nerves invested in the visceral
peritoneum surrounding internal organs. It is often the earliest manifestation of a
particular disease process This discomfort is poorly characterized and difficult to
localize. If the involved organ is affected by peristalsis, the pain is often described as
intermittent, crampy, or colicky. Somatic pain occurs with irritation of the parietal
peritoneum. Somatic pain is often described as intense ,constant and better localized
In children it is common for shigellosis to cause convulsions.
143
387. You have just seen 4 adolescents from the same 7th grade class school with apparent appendicitis –
right lower abdominal pain, anorexia, nausea, and low-grade fever. You suspect they may actually
be infected with:
a. Bacillus cereus.
b. E. coli 0157:H7.
c. Isosporidiosis.
d. epidemic Bunyavirus.
e. Yersinia enterocolitica.
388. A preferred oral therapy for antibiotic-induced pseudomembranous enterocolitis is:
a. a 2nd or 3rd generation fluoroquinolone.
b. ampicillin.
c. chloramphenicol.
d. metronidazole.
e. Pepto-Bismol®.
389. Lactulose is useful in patients with hepatic encephalopathy because it:
a. acidifies the fecal stream, resulting in the trapping of ammonia as ammonium in the stool.
b. causes ammonia to be transmitted to the intracellular region through the sodium-potassium
membrane pump; once there, it is safely used in the Kreb’s cycle.
c. forces renal excretion of sodium bicarbonate, leading to compensatory hyperpnea and respiratory
alkalosis, which keeps ammonia nontoxic.
d. provides an alternative calorie source to ammonia, preventing its digestion and the subsequent
metabolic ketoacidosis.
e. works in a manner as yet undescribed.
390. A 47-year-old man complains of right upper quadrant pain, vomiting after meals, and dark urine.
Laboratory studies show AST 420, ALT 198. This is highly suggestive for:
a. obstructive biliary disease.
b. pancreatitis.
c. hepatitis B.
d. hepatitis C.
e. alcohol related liver disease.
391. From an Emergency Practitioner’s perspective, the most acutely devastating complication of
ulcerative colitis is:
a. carcinoma.
b. fistula formation.
c. hepatorenal syndrome.
d. malabsorption and electrolyte abnormalities.
e. toxic megacolon.
392. A 72 year-old bedridden patient is sent for evaluation of vomiting. On physical exam you find
several well-healed scars, a distended tympanic abdomen, quiet bowel sounds, and an empty rectal
vault. The plain film radiograph of the abdomen shows a markedly dilated single loop of colon on
the left side suggestive of a sigmoid volvulus. You need to consult a:
a. surgeon for laparotomy, detorsion, and reattachment of the sigmoid in the left lower quadrant.
b. surgeon for sigmoidoscopy, decompression and detorsion.
c. surgeon for hemicolectomy.
d. surgeon for sigmoid colectomy.
e. surgeon for total colectomy.
144
387. e
th
Rosen 5 ,
Chapter 89,
p. 1305
388. d
Rosen 5th,
Chapter 89,
p. 1312-1313
389. a
th
Rosen 5 ,
Chapter 85,
p. 1260
390. e
Rosen 5th,
Chapter 85,
p. 1258
391. e
Rosen 5th,
Chapter 90,
p. 1338
392. b
Rosen 5th,
Chapter 87,
p. 1334
The initial clinical picture of Yersinia enterocolitis resembles that of infection by other
invasive intestinal organisms: fever; colicky abdominal pain; watery, greenish, and
sometimes bloody diarrhea; and constitutional symptoms of anorexia, vomiting, and
malaise. A substantial number of patients with yersiniosis, in particular adolescents
and young adults, develop an ileocecitis. In these cases, lower abdominal pain with
little or no diarrhea predominates and may perfectly mimic acute appendicitis. Large
gastrointestinal outbreaks have been traced to contaminated milk, largely because
physicians noticed an extraordinary jump in the number of negative appendectomies.
Many cases of antibiotic-associated colitis are self-limited, provided that the offending
agent is discontinued. When antibiotic treatment for C. difficle is warranted, oral
metronidazole is typically used unless the patient is significantly ill and merits IV
therapy.
Lactulose is a poorly absorbed sugar metabolized by colonic bacteria yielding lactic
acid. The salutary effects of this agent are related both to the acidification of the fecal
stream, resulting in the trapping of ammonia as ammonium in the stool, and to its
cathartic action. The usual dosage of lactulose is 15 to 30 ml orally three or four times
daily or in a quantity sufficient to result in several loose bowel movements daily. The
principal adverse effect is excessive diarrhea, with resultant fluid and electrolyte
imbalance.
In alcoholic liver disease serum transaminases aspartate aminotransferase (AST) and
alanine aminotransferase (ALT) are moderately elevated. Values in excess of 10 times
normal are unusual and a relative predominance of AST to ALT is expected. Bilirubin
is commonly elevated with a wide range of possible values.
Toxic megacolon occurs in up to 5% of cases of ulcerative colitis , usually during the
initial acute episode. The patient will appear septic, apathetic, and lethargic, with high
fever, chills, tachycardia, and progressive abdominal pain, tenderness, and distention.
The cause of toxic dilation is unknown, but precipitating factors may include use of
antidiarrheal agents, vigorous use of cathartics or enemas, or barium enema
examinations. Toxic dilation occurs predominantly in the transverse colon, probably
because in the supine position air collects in the transverse colon.
Once the diagnosis of sigmoid volvulus is made, a surgeon should be consulted. The
therapy of choice for a nonstrangulationg sigmoid volvulus is decompression and
detorsion, using a rectal tube via the sigmoidoscope. Success is achieved in 85% to
95% of patients.
145
393. The two most common causes of diarrhea in AIDS patients are:
a. Cryptospiridium and Cytomegalovirus (CMV).
b. Giardia and Rhodococcus equi.
c. Salmonella and Campylobacter.
d. Cyclospora and Strongyloides stercoralis.
e. Toxoplasma gondii and Shigella.
394. A 70-year-old female presents with increasing constipation for the last few months. You complete
her history and physical exam and become worried that she may have a serious disorder. You are
most concerned about her:
a. age greater than 60.
b. rectal bleeding.
c. abdominal distention.
d. flatulence.
e. depression.
395. A 28 year-old woman received a liver transplant 10 days ago. Tonight she complains of low-grade
fever and body aches. Which of the following is true concerning liver post-transplant rejection?
a. Rejection often begins 1 to 2 weeks post-op.
b. Leukocytosis may occur.
c. Fever may occur.
d. Right upper quadrant pain may occur.
e. All of the above are true
396. The most common cause of acute food poisoning in the United States is:
a. Bacillus cereus.
b. Clostridium perfringens.
c. Escherichia coli 0157:H7.
d. Staphylococcal organisms.
e. Yersinia.
397. A 51 year-old businessman ate sushi several hours before he started vomiting and having crampy,
explosive diarrhea. He requires intravenous rehydration and anti-emetics. He now feels better and
asks for ice chips. You notice he spits them out, explaining, “They burn my mouth, and my teeth
feel loose.” He is probably suffering from:
a. ciguatera poisoning.
b. scombroid poisoning.
c. tetrodotoxin psychosis.
d. E. coli 0157:H7 poisoning.
e. disulfiram (Antabuse®) reaction.
398. You can tell the suffering gentleman with the condition described in question #397 that he:
a. will probably require psychiatric counseling.
b. must wait for the antidote to be delivered from Japan.
c. can expect rapid improvement.
d. must avoid alcohol, as it can worsen his symptoms.
e. will need high-dose steroid therapy.
146
393. a
th
Rosen 5 ,
Chapter 89,
p. 1319
394. b
th
Rosen 5 ,
Chapter 2,
p. 210
395. e
th
Rosen 5 ,
Chapter 178,
p. 2508
396. b
th
Rosen 5 ,
Chapter 89,
p. 1308
397. a
th
Rosen 5 ,
Chapter 89,
p. 1311
398. d
Rosen 5th,
Chapter 89,
p. 1311
Cryptosporidium and cytomegalovirus (CMV) infections are the most causes of
diarrhea in AIDS patients. The incidence of each is 15% to 40%.Chronic persistent
diarrhea is most often from one coccidia, Cryptosporidium or Isospora belli
The most concerning symptoms associated with constipation are rectal bleeding and
change in the caliber of the stool. These are warning signals suggesting possible
colorectal cancer.
Rejection often occurs 1 to 2 weeks after surgery, with fever, right upper quadrant
pain, and elevated bilirubin and transaminases. Leukocytosis may occur but is
nonspecific.
Clostridium perfringens is probably the most common cause of acute food poisoning
in the US, constituting almost one fourth of all bacteria-associated food-borne illnesses
and usually occurring in large outbreaks caused by ingestion of meat or poultry dishes.
Classically, patients with ciguatoxin develop both GI and neurological symptoms. The
GI symptoms (e.g., nausea, vomiting, profuse watery diarrhea, crampy abdominal pain,
and diaphoresis) tend to appear earlier. The panoply of neurological symptoms
consists largely of dysesthesias and paresthesias around the throat and the perioral
area; “burning feet,” which may resemble alcoholic peripheral neuropathy; “loose,
painful teeth”; and sometimes CNS changes, such as ataxia, weakness, vertigo, visual
hallucinations, and even confusion and coma. One symptom highly suggestive of
ciguatera fish poisoning is sensory reversal dysesthesia, in which cold objects are
perceived to be warm and vice versa. Patients describe such distortion of temperature
perception very vividly. Another classic feature is either a return or a worsening of the
symptoms after ingestion of alcohol. Ciguatera poisoning lasts an average of 1 to 2
weeks, but at least half of its victims are still symptomatic at 8 weeks. The
neurological symptoms, particularly the paresthesias and dysesthesias, tend to persist
longer than the GI symptoms and have been reported up to years later.
147
399. When assessing a patient for acute appendicitis, which of the following describes the obturator
sign?
a. pain produced by internal rotation of the flexed right hip.
b. pain produced by external rotation of the flexed right hip.
c. pain produced by extension of the right hip with the patient in the left lateral decubitus
position.
d. sensation of pain in the right lower quadrant with palpation of the left lower quadrant.
e. pain produced by the patient coughing.
400. A type of hemorrhoid that requires emergent surgical consultation is:
a. thrombosed external hemorrhoid.
b. second –degree internal hemorrhoid.
c. third-degree internal hemorrhoid.
d. nonthrombosed fourth degree internal hemorrhoid
e. thrombosed or gangrenous fourth degree internal hemorrhoid.
148
399. a
th
Rosen 5 ,
Chapter 88,
p. 1294
400. e
Rosen 5th,
Chapter 91,
p. 1347
The obturator sign is the elicitation of pain as the right hip is flexed and internally
rotated. Other clinical signs of acute appendicitis include the psoas sign (increase of
pain when the psoas muscle is stretched as the patient is asked to extend his/her right
hip), and Rovsing's sign ( referred right lower quadrant pain with palpation on the left
lower quadrant).
Patients with acute, gangrenous, fourth-degree internal hemorrhoids should be referred
for emergent hemorrhoidectomy. Nonthrombosed fourth-degree hemorrhoids require
nonemergent hemorrhoidectomy. Acutely thrombosed external hemorrhoids can be
excised in the ED for pain relief. Second- and third- degree internal hemorrhoids
require referral for elective surgery.
149
4.0 – Cutaneous Disorders
502. A 25-year-old woman is worried about some patches on her back that did not tan this
summer. She probably has:
a. pityriasis rosea.
b. seborrheic dermatitis.
c. tinea versicolor.
d. vitiligo.
e. xerosis.
503. A 27-year-old woman has several dozen small, scaly, slightly itchy lesions on her back.
She also points out a 3-cm lesion that she noticed a few days before the above rash. You
can tell her that:
a. she may get some lesions in her mouth.
b. the rash is likely to reoccur every year or two.
c. chronic low-dose griseofulvin will be curative.
d. its cause is unknown.
e. topical hydrocortisone will shorten the course of the disease.
504. A wheal is:
a. an elevated skin lesion >0.5 cm in diameter and depth.
b. a nodule filled with expressible material.
c. a blister >0.5 cm in diameter filled with clear fluid.
d. a blister filled with cloudy or purulent fluid.
e. a papule or plaque of dermal edema; often with central pallor and irregular borders.
505. A 54-year-old woman recently started trimethoprim-sulfamethoxazole for a sinus infection.
She complains of low-grade fever, lethargy, loss
of appetite, and this rash (Figure 114-13). She
has similar lesions in her mouth.
a. She requires intravenous broad-spectrum antibiotic
coverage to prevent progression to toxic shock
syndrome.
b. This is Kaposi’s sarcoma; she probably has AIDS.
c. The severe form of this disease is called a StevensJohnson syndrome.
d. Systemic steroids will shorten the course of the
disease.
e. It is caused almost exclusively by viral infections
Rosen 5th, Figure 114-13
506. A 3-year-old boy has had several days of yellow crusting lesions on his forehead and chin.
They are itchy but not painful. The child is afebrile and nontoxic.
a. Group A streptococcus is the most common causative organism.
b. Systemic antibiotics have a higher cure rate than topical agents.
c. These lesions are not contagious.
d. Systemic antibiotics will prevent later occurrence of glomerulonephritis.
e. Without treatment, the lesions heal within 3 to 6 weeks.
150
502. c
th
Rosen 5 ,
Chapter 114,
p. 1637
503. d
Rosen 5th,
Chapter 114,
p. 1638
504. e
Rosen 5th,
Chapter 114,
p. 1636
505. c
Rosen 5th,
Chapter 114,
p. 1648
506. e
Rosen 5th,
Chapter 114,
p. 1639
Tinea versicolor is a superficial yeast infection caused by Pityrosporum ovale.
Superficial scaling patches occur mainly on the chest and trunk but may extend to the
head and limbs. As the name implies, lesions can be a variety of colors including pink,
tan, or white. The disease may be associated with pruritus, but medical care is often
sought because the spots do not tan. On physical examination, a fine subtle scale is
noted that may appear hypopigmented. A KOH preparation reveals short hyphae
mixed with spores (“chopped spaghetti and meatballs”).
Pityriasis rosea is a mild skin eruption predominantly found in children and young
adults. The lesions are multiple pink or pigmented oval papules or plaques 1 to 2 cm
in diameter on the trunk and proximal extremities. Mild scaling may be present. The
lesions are parallel to the ribs, forming a Christmas tree–like distribution on the trunk.
Oral lesions are rare. In children, papular or vesicular variants of the disease may
occur. In half the cases, the generalized eruption is preceded by a week by the
appearance of a “herald patch.” This is a larger lesion, 2 to 6 cm in diameter, that
resembles the smaller lesions in other respects. The eruption is usually asymptomatic,
although pruritus may be present. Pityriasis rosea is self-limited, resolving in 8 to 12
weeks. Its cause is unknown, although a virus is suspected. Treatment is usually
unnecessary, except for symptomatic alleviation of bothersome pruritus.
Macule: Flat, color differs from surrounding skin
Patch: A macule with surface changes (i.e., scale or wrinkling)
Papule: Elevated skin lesion <0.5 cm in diameter
Plaque: Elevated skin lesion >0.5 cm in diameter; without substantial depth
Nodule: Elevated skin lesion >0.5 cm in diameter and depth
Cyst: Nodule filled with expressible material
Vesicle: Blisters <0.5 cm in diameter filled with clear fluid
Bullae: Blisters >0.5 cm in diameter filled with clear fluid
Pustule: Vesicle filled with cloudy or purulent fluid
Crust: Liquid debris that has dried on the skin surface
Scale: Visibly thickened stratum corneum; usually white
Lichenification: Epidermal thickening characterized by visible and palpable skin
thickening and accentuated skin markings
Induration: Dermal thickening that feels thick and firm
Wheal: Papule of dermal edema; often with central pallor and irregular borders
Erythema: Red appearance of skin caused by vasodilatation of dermal blood vessels
Erythema multiforme is an acute, usually self-limiting disease precipitated by a variety
of factors. It is characterized by the sudden appearance of skin lesions that are
erythematous or violaceous macules, papules, vesicles, or bullae. Their distribution is
often symmetrical, most commonly involving the soles and palms, the backs of the
hands or feet, and the extensor surfaces of the extremities. Treatment should begin
with a search for the underlying cause. Mild forms resolve spontaneously in 2 to 3
weeks. Systemic steroids are commonly used and provide symptomatic relief, but are
of unproven benefit in influencing the duration and outcome.
Impetigo is a slowly evolving pustular eruption, most common in preschool children.
Currently, Staphylococcus aureus is the most common pathogen, with Group A
streptococcus a distant second. Both systemic and topical therapy is equally successful
in treating impetigo. Lesions are very contagious among infants and young children
and less so in older children and adults. There is no evidence, however, that systemic
antibiotics prevent the development of acute glomerulonephritis. Without treatment,
impetigo heals within 3 to 6 weeks.
151
507. A 21-year-old man has fever and a urethral discharge. He also complains of a swollen
painful left knee and this rash.
a. He can be treated as an outpatient with oral antibiotics.
b. This condition occurs more in men than in women.
c. If the lesions are cultured, they are usually positive for the
organism.
d. The tick serves as a vector for this disease.
e. You expect the rash to be pustular rather than petechial and
hemorrhagic.
508. The most common medication-related cause of
erythema nodosum is:
a. sulfa-based drugs.
b. non-steroidal anti-inflammatory agents.
c. oral contraceptives.
d. penicillin.
e. fluoroquinolones.
509. The most common skin eruption due to drugs is:
a. bullae.
b. macules.
c. papules.
d. striae.
e. urticaria.
510. A 25-year-old woman had an abortion five days ago. She now has fever and a flu-like
syndrome. Today she started vomiting and got confused. Oral temperature 103.4°F,
heart rate 120 / minute, blood pressure 80/40 mmHg. You also notice diffuse eryhtema.
You know that:
a. mucous membrane involvement would indicate this is not toxic shock syndrome.
b. you can also see pharyngitis, a “strawberry tongue,” conjunctivitis, and vaginitis with this illness.
c. supportive care and high-dose penicillin is the appropriate treatment.
d. desquamation tends to spare the hands and feet.
e. the skin rash may take several weeks to dissipate.
511. Nikolsky’s sign is often found in patients with:
a. acanthosis nigrans.
b. bullous pemphigoid.
c. hidradenitis suppurativa.
d. Rocky Mountain spotted fever.
e. toxic epidermal necrolysis.
512. Erysipelas is usually caused by:
a. Neisseria gonorrhoeae.
b. Coxsackievirus.
c. Bartonella tularensis.
d. Group A streptococcus.
e. Staphylococcus epidermidis.
152
507. e
th
Rosen 5 ,
Chapter 114,
p. 1640
508. c
Rosen 5th,
Chapter 114,
p. 1653
509. e
Rosen 5th,
Chapter 114,
p. 1640
510. b
Rosen 5th,
Chapter 114,
p. 1644
511. e
Rosen 5th,
Chapter 114,
p. 1643
512. d
Rosen 5th,
Chapter 131,
p. 1946
About 2% of patients with mucosal gonococcal infection will develop disseminated
GC infection. Hospitalization is recommended for patients in whom the diagnosis is
uncertain and for those who have septic arthritis, meningitis, or endocarditis. It affects
women primarily. Fever and migratory polyarthralgias commonly accompany the skin
lesions. The rash of disseminated gonococcemia is pustular rather than obviously
petechial and hemorrhagic, as are the lesions of Rocky Mountain spotted efevr and
meningococcemia.
A number of underlying conditions produce erythema nodosum: tuberculosis,
sarcoidosis, coccidioidomycosis, histoplasmosis, ulcerative colitis, regional enteritis,
pregnancy, infections with streptococci, Yersinia enterocolitica, and chlamydia. As
with erythema multiforme, many cases of erythema nodosum are idiopathic. Oral
contraceptive agents are the leading cause of drug-induced cases. The differential
diagnosis includes traumatic bruises and subcutaneous fat necrosis.
A given drug can produce a skin eruption of a different appearance in different patients
or a different appearance in the same patient on different occasions. The most
common eruptions are urticaria (hives) and morbilliform rashes. Drug reactions tend
to appear within a week after the drug is taken, with the exception of reactions to
semisynthetic penicillins, which commonly occur later. Skin lesions may appear after
a drug has been discontinued and may worsen if the drug or its metabolites persist in
the system. Special note should be made of penicillin because it is the most common
cause of drug reaction. Serum sickness and urticaria are the most common
manifestations of penicillin allergy.
In toxic shock syndrome, the rash is typically diffuse, blanching, macular
erythroderma. Accompanying nonexudative mucous membrane inflammation is
common. Pharyngitis, sometimes accompanied by a “strawberry tongue,”
conjunctivitis, or vaginitis may be seen. As a rule, the rash fades within 3 days of its
appearance. This is followed by a full-thickness desquamation, most commonly
involving the hands and feet. Initial treatment of TSS consists of IV fluid replacement,
ventilatory support, pressor agents, penicillinase-resistant antibiotics, and drainage of
infected sites. Corticosteroids reduce the severity of illness and duration of fever if
initiated within 2 to 3 days after the onset of illness.
Nikolsky’s sign is epidermal shearing following lateral pressure on unblistered skin.
The extension of a blister following application of pressure to its roof has earned the
eponym Asboe-Hansen’s sign. Nikolsky's sign is most commonly found in scalded
skin syndrome (also called Ritter disease), toxic epidermal necrolysis, and pemphigus
vulgaris.
Erysipelas is an acute superficial cellulitis characterized by a sharply demarcated
border surrounding skin that is raised, deeply erythematous, indurated, and painful. It
usually involves the dermis, lymphatics, and most of the superficial subcutaneous
tissue. Erysipelas most often occurs in the very young and those age 50 to 60 years; it
is associated with small breaks in the skin, nephrotic syndrome, and postoperative
wounds. Patients usually appear toxic with a prodrome of fever, chills, and malaise
preceding the eruption of a bright red cellulitis predominantly on the lower extremities
or on the face. Group A Streptococcus, other streptococcal species, and S. aureus are
the involved pathogens.
153
513. A positive Hutchinson sign is found in patients with:
a. herpes zoster ophthalmicus.
b. Lyme disease.
c. measles.
d. mumps.
e. Rocky Mountain spotted fever.
514. Physical findings of patients with scarlet fever and Kawasaki disease are similar. The
finding most likely to make you think of scarlet fever would be:
a. ‘strawberry’ tongue.
b. cervical adenopathy.
c. fever.
d. generalized erythematous rash.
e. circumoral pallor.
515. There is an outbreak of head lice in the local school district, and the local school nurse
calls for advice. You tell her that:
a. household contacts require treatment.
b. involvement of the interdigital web spaces is typical.
c. nits are seen more frequently than the adult louse form.
d. pediculosis capitis is more common in adults.
e. the organism is a mite.
516. Oral acyclovir is recommended for the treatment of an initial episode of:
a. genital herpes simplex.
b. herpes zoster.
c. oral herpes simplex.
d. varicella.
e. vaccinia.
517. Roseola infantum:
a. causes a high fever followed in several days by a desquamating rash.
b. frequently is a precursor to encephalitis.
c. generally occurs in school-age children.
d. is also called fifth disease.
e. is caused by a herpes virus.
518. A pinkish maculopapular rash that first appears on the face and associated with
generalized lymphadenopathy including suboccipital and postauricular nodes is most
typical of:
a. measles
b. Rocky Mountain spotted fever.
c. roseola.
d. rubella.
e. rubeola.
519. The primary lesions of pemphigus vulgaris are:
a. bullae.
b. macules.
c. nodules.
d. papules.
154
e. wheals.
155
513. a
th
Rosen 5 ,
Chapter 66,
p. 918
514. e
Rosen 5th,
Chapter 123,
p. 1804-1805
Chapter 114,
p. 1646
515. c
Rosen 5th,
Chapter 114,
p. 1649
516. a
Rosen 5th,
Chapter 124,
p. 1819
517. e
th
Rosen 5 ,
Chapter 114,
p. 1822
518. d
Rosen 5th,
Chapter 114,
Chapter 128,
pages listed
in text of
answer
519. a
Rosen 5th,
Chapter 114,
p. 1653-1654
Herpes zoster keratoconjunctivitis occurs as a result of activation of the virus along
ophthalmic division of the trigeminal nerve. The rash follows dermatomal patterns,
involves the forehead and upper eyelid, and produces significant pain. Involvement of
the nasociliary nerve, manifested by zoster lesions on the tip of the nose (Hutchinson’s
sign), is associated with a 76% risk of ocular involvement vs. 34% risk if the nerve is
not involved.
Kawasaki disease, or mucocutaneous lymph node syndrome (MLNS) is a disease of
unclear etiology found predominantly in children less than 9 years of age. The
diagnosis of this disorder is based on a prolonged fever associated with at least four of
the following: (1) conjunctivitis, (2) rash, (3) lymphadenopathy, (4) changes in the
oropharynx consisting of injection of the pharynx and lips with prominent papillae of
the tongue (strawberry tongue), and (5) extremity erythema and edema. Patients with
scarlet fever can have the erythematous rash, strawberry tongue, lymphadenopathy,
and fever, but also have facial flushing with circumoral pallor.
Only occasionally are the adult lice forms found, looking like blue or black grains.
The nits often attach to the base of the hair shafts, appearing as white dots. Any sexual
contacts should be treated; household contacts should be examined, and if uninfected,
no treatment is necessary. Scabies involves the interdigital web spaces and is a mite
infestation.
Acyclovir is not routinely recommended for oral herpes, herpes zoster, or varicella
infections unless the patient is immunocompromised. Acyclovir reduces the duration
of viral shedding and accelerates healing. It does not prevent recurrent episodes.
Roseola infantum is the most common exanthem of children younger than 2 years of
age and occurs most often at about 1 year of age. The illness begins abruptly with the
acute onset of fever, often as high as 41o C, lasting three to five days. Despite the
fever, the child usually remains active and alert. A fine, evanescent, rose-colored
maculopapular rash then appears on the trunk after lysis of the fever, which may last
for 1 or 2 days. The rash may spread to the face and extremities.
This is a typical picture of rubella (German measles), particularly the involvement of
the postauricular nodes. It is important to recognize rubella in order to avoid maternal
exposure that can result in severe birth defects (p. 1825). Roseola infantum is
described in question #517 (p. 1822). Rocky Mountain spotted fever is manifested by
the abrupt onset of fever, headaches, chills, and malaise; rash develops on the second
to fourth day, with blanching erythematous macules around the wrists and ankles.
They may become petechial (p. 1891-1896). Rubeola (measles) is a febrile illness,
with rash that starts on the face and spreads to the trunk on the third to fifth day of
illness. Koplik's spots-bright red spots with bluish centers opposite the molars-occur
early in the course of the measles (p. 1827).
Pemphigus vulgaris (PV) is an uncommon, but important, dermatologic disorder. The
mortality rate before the use of steroids was approximately 95%. PV is a bullous
disease, affecting both sexes equally, and is most common in patient 40 to 60 years of
age. Nikolsky’s sign is present and characteristic of the disease.
156
520. Hidradenitis suppurativa:
a. begins as a painful deep erythematous nodule usually in the axilla or groin.
b. begins in childhood.
c. is easily treated with 10-days of a long-acting tetracycline.
d. is more common in men.
e. should never be drained in the emergency department.
157
520. a
th
Rosen 5 ,
Chapter 114,
p. 1639
Hidradenitis suppurativa affects the apocrine sweat glands. Recurrent abscess
formation in the axillae and groin resembles localized furunculosis. The condition
tends to be recurrent and may be extremely resistant to therapy. It is treated with
drainage of abscesses, but antistaphylococcal antibiotics are useful if administered
early and for a prolonged period.
158
5.0 – Endocrine, Metabolic, Nutritional Disorders
521. The most common cause of coma in a patient with diabetes is:
a. alcohol intoxication.
b. diabetic ketoacidosis.
c. hypoglycemia.
d. sepsis.
e. stroke.
522. In a hypoglycemic patient who has known adrenal insufficiency , you should consider
giving intravenous:
a. ACTH.
b. amiodarone.
c. hydrocortisone.
d. sodium bicarbonate.
e. thyroxin.
523. The only agents capable of stimulating hepatic glucose production (glycogenolysis) within
minutes are:
a. glucagon and epinephrine.
b. glucagon and insulin.
c. glucagon and norepinephrine.
d. insulin and epinephrine.
e. insulin and norepinephrine.
524. In patients with hypoglycemia, signs of CNS dysfunction are common. The next most
common physical sign would be:
a. seizures.
b. focal weakness.
c. hypotension
d. tachypnea.
e. sweating.
525. The only anabolic hormone is:
a. adrenaline.
b. cortisol.
c. glucagon.
d. insulin.
e. testosterone.
526. In a patient with diabetic ketoacidosis, the primary reason for mental status change is the:
a. elevated blood sugar.
b. metabolic acidosis.
c. respiratory alkalosis.
d. hypoxemia.
e. elevated osmolarity.
159
521. c
th
Rosen 5 ,
Chapter 120,
p. 1748
522. c
th
Rosen 5 ,
Chapter 120,
p. 1781
523. a
th
Rosen 5 ,
Chapter 120,
p. 1745
524. e
Rosen 5th,
Chapter 120,
p. 1748
525. d
th
Rosen 5 ,
Chapter 120,
p. 1745
526. e
Rosen 5th,
Chapter 120,
p. 1750
The most common cause of coma associated with diabetes is hypoglycemia, due to an
excess of administered insulin with respect to glucose intake. Hypoglycemia may be
associated with significant morbidity and mortality. Severe hypoglycemia is usually
associated with a blood sugar below 40 to 50 mg/dl and impaired cognitive function.
Steroid administration should be considered for hypoglycemia that is either resistant to
aggressive glucose replacement therapy or associated with the signs of adrenal
insufficiency. The dose is 100 to 200 mg hydrocortisone IV in adults.
The first defense against the development of hypoglycemia is a decrease in insulin
secretion, but both glucagon and epinephrine are also important for the acute protection
against hypoglycemia. Both of these counterregulatory hormones are the only agents
capable of stimulating hepatic glucose production within minutes of their release into
circulation, primarily via glycogenolysis—the release of glucose from its intracellular
storage-depot glycogen.
A depressed sensorium is most common. Described less frequently are seizure activity
and focal neurologic findings. Sweating is common.
Insulin is the only anabolic hormone and is responsible for the metabolism and storage
of carbohydrates, fat, and protein. Counterregulatory hormones include glucagon,
catecholamines, cortisol, and growth hormone.
Mental confusion and coma are much more likely with serum osmolarity 340 mOsm/L
or higher. If the serum osmolarity is <340 mOsm/L in a comatose patient, another
cause of the coma should be sought.
160
527. Urine dipstick for ketones uses a nitroprusside reaction, which measures:
a. acetoacetate.
b. beta-hydroxybutyrate.
c. insulin levels.
d. ketones.
e. lactic acids.
528. The lab values most consistent with a diagnosis of DKA are:
a. glucose >350 mg/dL, bicarbonate >20 mEq/L, arterial pH <7.3, severe ketonuria
b. glucose >250 mg/dL, bicarbonate >15 mEq/L, arterial pH >7.3, moderate ketonemia
c. glucose >250 mg/dL, bicarbonate <20 mEq/L, arterial pH <7.0, moderate ketonuria
d. glucose >350 mg/dL, bicarbonate <15 mEq/L, arterial pH <7.3, moderate ketonemia
e. glucose >700 mg/dL, bicarbonate >15 mEq/L, arterial pH >7.3, moderate ketonuria
529. The single most important initial treatment for the patient in diabetic ketoacidosis is:
a. oxygen therapy.
b. rapid bicarbonate administration.
c. rapid fluid administration.
d. rapid insulin administration.
e. rapid potassium replacement.
530. In a patient with diabetic ketoacidosis, the preferred method of insulin administration is:
a. intramuscular.
b. intravenous bolus – high dose.
c. intravenous bolus – low dose.
d. intravenous constant drip– weight-based.
e. subcutaneous.
531. During treatment of diabetic ketoacidosis, the most potentially life-threatening electrolyte
abnormality is:
a. hypercalcemia.
b. hyperkalemia.
c. hypokalemia.
d. hypernatremia.
e. hyponatremia.
532. Concerning the use of sodium bicarbonate in the treatment of diabetic ketoacidosis, it has
been shown to:
a. rapidly improve the hypokalemia
b. improve the central nervous system acidosis.
c. improve intracellular acidosis.
d. assist oxyhemoglobin dissociation.
e. do none of the above – don’t use it.
533. Common presenting symptoms in a patient with alcoholic ketoacidosis include:
a. blurred vision.
b. delirium tremens.
c. dehydration
d.
e.
bloody diarrhea.
fetid breath odor.
161
527. a
th
Rosen 5 ,
Chapter 120,
p. 1748
528. d
Rosen 5th,
Chapter 120,
p. 1752
529. c
th
Rosen 5 ,
Chapter 120,
p. 1752
530. d
Rosen 5th,
Chapter 120,
p. 1752-1753
531. c
Rosen 5th,
Chapter 120,
p. 1754
532. e
th
Rosen 5 ,
Chapter 120,
p. 1754
533. b
Rosen 5th,
Chapter 179,
p. 2524
Urine ketone dipsticks use the nitroprusside reaction, which is a good test for
acetoacetate but does not measure beta-hydroxybutyrate. Although the usual
acetoacetate / beta-hydroxybutyrate ratio in diabetic ketoacidosis is 1:2.8, it may be as
high as 1:30, in which case the urine dipstick does not reflect the true level of ketosis.
When ketones are in the form of beta-hydroxybutyrate, the urine ketone dipsticks may
infrequently yield negative reactions in patients with significant ketosis.
Although the exact definition of DKA is variable, most experts agree that a blood
glucose greater than 350 mg/dL, bicarbonate level less than 15 mEq/L, and an arterial
pH of less than 7.3 with moderate ketonemia constitute the disease.
Rapid fluid administration is the single most important initial step in the treatment of
DKA. Fluid helps restore intravascular volume and normal tonicity, perfuse vital
organs, improve glomerular filtration rate, and lower serum glucose and ketones. The
average adult patient has a water deficit of 100 mL/kg (5 to 10 L) and a sodium deficit
of 7 to 10 mEq/kg. NS is the most frequently recommended fluid for initial
rehydration even though the extracellular fluid of the patient is initially hypertonic.
High dosages of insulin have potentially harmful effects, including a greater incidence
of iatrogenic hypoglycemia and hypokalemia. Because the half-life of regular insulin
is 3 to 10 minutes, IV insulin should be administered by constant infusion rather than
by repeated bolus. The current therapy of choice is regular insulin infused at 0.1
U/kg/hr up to 5 to 10 U/hr, mixed with the IV fluids. Regular insulin, 10 to 20 U/hr,
administered IM accomplishes similar effect but subjects the patient to repeated painful
injections. In theory, IM insulin may accumulate at a poorly perfused administration
site, failing to enter the systemic circulation in a timely manner.
The development of severe hypokalemia is potentially the most life-threatening
electrolyte derangement during the treatment of DKA. This complication is avoidable
if the pathophysiology is understood and the effects of therapy frequently monitored.
To date, not a single study clearly demonstrates improved clinical outcome using
bicarbonate in the treatment of DKA. Acidotic patients routinely recover from DKA
without alkali therapy. Routine use of supplemental bicarbonate in the treatment of
DKA is not recommended.
Presenting symptoms of alcoholic ketoacidosis
Nausea 76%
Vomiting 73%
Abdominal pain 62%
Shortness of breath 20%
162
534. Initial treatment of the patient with alcoholic ketoacidosis should begin with:
a. intravenous bicarbonate.
b. intravenous D5NS.
c. intravenous insulin.
d. intravenous Ringer’s lactate.
e. subcutaneous insulin.
535. In comparing patients with diabetic ketoacidosis (DKA) to those with hyperglycemic
hyperosmolar nonketotic coma (HHNC), those with DKA have:
a. greater fluid and electrolyte deficits.
b. higher serum glucose levels.
c. lower anion gaps.
d. more profound acidosis.
e. slower onset.
536. Na+ 136 mEq/L; K+ 4.1 mEq/L; Cl- 108 mEq/L; NaHCO3- 12 mEq/L; glucose 600 mg/dL;
arterial pH 7.10
a. The anion gap is 26.
b. The corrected potassium is 2.3 mEq/L.
c. The corrected potassium is 5.9 mEq/L.
d. The corrected sodium is 126 mEq/L.
e. The corrected sodium is 152 mEq/L.
537. In rehydrating the patient with hyperosmolar hyperglycemic coma, you should use:
a.D5NS.
b. hypertonic saline.
c.hypotonic saline.
d. isotonic saline.
e.Ringer’s lactate.
538. When fixing a patient’s fluid and electrolyte imbalances, they should be corrected in this
order:
a. sodium and chloride > volume > pH > potassium, calcium, and magnesium
b. volume > pH > potassium, calcium, and magnesium > sodium and chloride
c. potassium, calcium, and magnesium > volume > pH > sodium and chloride
d. pH > potassium, calcium, and magnesium > sodium and chloride > volume
e. volume > potassium, calcium, and magnesium > sodium and chloride > pH
539. The most common cause of metabolic acidosis in children is:
a. cystic fibrosis.
b. diabetes.
c. febrile seizure.
d. nephrotic syndrome.
e. prolonged diarrhea.
540. Common precipitating factors in the development of hyperglycemic hyperosmolar
nonketotic syndrome include:
a.fever.
b. prolonged bedrest.
c.hypokalemia
d. myocardial ischemia.
163
e.use of a salt substitute.
164
534. b
th
Rosen 5 ,
Chapter 179,
p. 2524
535. d
Rosen 5th,
Chapter 120,
p. 1752
536. b
Rosen 5th,
Chapter 120,
p. 1752
537. d
Rosen 5th,
Chapter 120,
p. 1756
538.b
Rosen 5th,
Chapter 119,
p. 1753-1754
539. e
th
Rosen 5 ,
Chapter 118,
p. 1718
540. c
Rosen 5th,
Chapter 120,
p. 1756
Treatment of alcoholic ketosis is volume replacement with normal saline, glucose,
thiamine, and correction of hypokalemia. This can be accomplished with 5% dextrose
in normal saline and either 30 mEq of potassium chloride or 30 mEq of oral potassium.
Bicarbonate is seldom necessary for the uncomplicated case but may be considered in
the rare patient who has a pH of less than 7.1. If no serious complicating illness is
present, the ketosis will reverse in 12 to 24 hours with this treatment.
The prodrome for HHNC is significantly longer than that of DKA. The patient
typically manifests more profound electrolyte imbalance and dehydration than those
with DKA. A patient with HHNC does not have a ketoacidosis caused by diabetes but
may have a lesser degree of metabolic acidosis. The mortality rate is much higher for
HHNC as most patients are elderly and have underlying cardiac and renal disease.
The reported serum sodium is often misleading in DKA. The true value of sodium
may be approximated by adding 1.6 mEq/L to the reported value for every 100 mg/dl
of glucose over the norm. Acidosis and dehydration contribute to high measured
serum potassium despite total body deficits. Correction for acidosis can be made by
subtracting 0.6 mEq/L from the laboratory value for every 0.1 decrease in pH below
7.4.
Most authors agree that the use of isotonic saline (0.9% NaCl) is the most appropriate
initial crystalloid for the replacement of intravascular volume. It is hypotonic to the
patient’s serum osmolarity and will more rapidly restore plasma volume. Once
hypotension, tachycardia, and urinary output improve, half- normal saline (0.45%
NaCl) can be used to replace the remaining free water deficit.
When fluids and electrolytes are altered, they should be corrected in the following
orderly fashion: volume > pH > potassium, calcium, and magnesium > sodium and
chloride. Equilibrium of fluid, electrolytes, and pH depends on adequate tissue
perfusion and often corrects spontaneously with resolution of the underperfused state.
Metabolic acidosis can be caused by one of three mechanisms: (1) increased
production of acids, (2) decreased renal excretion of acids, or (3) loss of alkali. The
etiologies of metabolic acidosis can be clinically divided into those that create an
elevation in AG and those that do not. In the pediatric age group, dehydration from
prolonged diarrhea is the most common cause of metabolic acidosis.
Usually some precipitating event causes a patient to develop an insidious state of
progressive hyperglycemia and hyperosmolarity, which goes unchecked. By far, acute
infection is the most common precipitating cause of HHNS. Urinary tract infection
and pneumonia are most common, though uremia, viral illness, and a host of metabolic
and iatrogenic causes have been identified. Similarly, several drugs may predispose or
contribute to hyperglycemia, volume depletion, or other effects leading to HHNS,
especially diuretics, glucocorticoids, lithium, phenytoin, neuroleptics, beta-blockers,
mannitol, didanosine, and calcium-channel blockers.
165
541. It is well known that vomiting leads to hypokalemia. The reason for this is:
a.direct loss of potassium from stomach contents.
b. hypovolemia from volume loss leads to increases in aldosterone secretion, causing the kidney to
preserve sodium and bicarbonate in exchange for potassium, resulting in alkalosis which causes
potassium to shift into cells in exchange for hydrogen ions.
c.vomiting causes hyperventilation, leading to respiratory alkalosis and compensatory extracellular to
intracellular potassium shifts.
d. with the loss of hydrogen ions after a first episode of vomiting, the gastric parietal cells secrete
potassium, which is lost in further vomiting.
e.unknown.
542. An 86-year-old woman from a local nursing home presents in hyperosmolar hyperglycemic
coma. She was recently hospitalized for pyelonephritis and bacteremia. When you look at
her medication list, you suspect that her current condition is more than likely caused by:
a.
aspirin.
b.
levofloxacin.
c.
thyroid replacement.
d.
omeprazole (Prilosec®).
e.
hydrochlorothiazide.
543. In treating the patient mentioned in Question #542, you know that insulin
a is contraindicated.
b. should be given in higher doses than when treating DKA.
c. can safely and effectively be used intramuscularly.
d. can precipitate vascular collapse if it is given prior to volume expansion.
e. can cause a potentially lethal hyperkalemia if given too rapidly.
544. The patient in Question #542 has received 2000 cc of normal saline solution and 12 units
of regular insulin. Her repeat bedside glucose is 245 mg/dL. Your third liter of fluid should
be:
a.0.9% saline.
b. 0.45% saline.
c.Ringer’s lactate.
d. dextrose / 0.9% saline.
e.5% dextrose / 0.45% saline.
545. The most common cause of hyperthyroidism in the United States is:
a.Graves’ disease.
b. multinodular goiter.
c.pituitary adenoma.
d. thyroid cancer.
e.thyroiditis.
546. A 40-year-old woman complains of palpitations. Temperature 100.8oF, heart rate 140 /
minute, respiratory rate 22 / minute, blood pressure
148/80 mmHg. Her eyes are shown in this picture. You
immediately suspect:
a.amphetamine toxicity.
b.lithium overdose.
c.myxedema coma.
d.pheochromocytoma.
166
e.thyroid storm.
167
541. e
th
Rosen 5 ,
Chapter 120,
p. 1755
542. b
Rosen 5th,
Chapter 119,
p. 1728
543. d
Rosen 5th,
Chapter 120,
p. 1756
544. e
Rosen 5th,
Chapter 120,
p. 1756
545. a
th
Rosen 5 ,
Chapter 173,
p. 2441
546. e
Rosen 5th,
Chapter 122,
p. 1771
Several drugs may predispose or contribute to hyperglycemia, volume depletion, or
other effects leading to HHNS, especially diuretics, glucocorticoids, lithium,
phenytoin, neuroleptics, beta-blockers, mannitol, didanosine, and calcium-channel
blockers.
The hypokalemia associated with vomiting has very little to do with the actual K+ lost
in the vomitus and much more to do with the metabolic alkalosis that follows. The
hypovolemia from volume loss leads to increases in aldosterone secretion, which acts
on the kidney to preserve Na+ and bicarbonate in exchange for K+. The resultant
alkalosis also causes K+ to shift into cells in exchange for H+.
Initial volume replacement should always precede the initiation of an insulin drip in
HHNS. If insulin is utilized prior to rehydration, intravascular volume may be further
depleted. Insulin will cause a shift of osmotically active glucose into the intracellular
space, bringing free water with it. This will further deplete the intravascular
compartment and may precipitate vascular collapse. Another relative contraindication
to the early use of insulin in HHNS is hypokalemia. Insulin promotes transport of
potassium into cells and it should be withheld until the potassium level is known and
hypokalemia has been treated.
Once serum glucose decreases to less than 300 mg/dL, the intravenous solution should
be changed to D5W 0.45 percent NaCl and the insulin infusion should be reduced to
half or 0.05 (units/kg)/h.
Graves’ disease is by far the most common cause, accounting for more than 80% of
cases of hyperthyroidism in the United States. Toxic multinodular and toxic
(adenoma) nodular goiters are the next most frequent causes. Less common causes of
hyperthyroidism are thyroiditis, pituitary tumors, metastatic thyroid cancer, and
dermoid tumors or teratomas of the ovary.
Common symptoms of thyroid storm include palpitations, dyspnea, and chest pain.
Fever is often present, but the tachycardia may be elevated out of proportion to the
height of fever. The manifestations of ophthalmopathy include upper-lid retraction,
staring, lid lag (Graefe’s sign), exophthalmos, and extraocular muscle palsies.
168
547. The most important treatment for the reduction of morbidity and mortality in thyroid storm
is:
a.inhibit hormone synthesis.
b.block hormone release.
c.prevent peripheral conversion of T4 to T3
d.block the peripheral effects of thyroid hormone.
e.provide general support.
548. A drug to avoid in a patient in thyroid storm is:
a. acetaminophen.
b. aspirin.
c. calcium chloride.
d. calcium gluconate.
e. insulin.
549. You are treating a patient in thyroid storm. You have given propranolol two mg
intravenously. An appropriate follow-up regimen would be:
a.intravenous methimazole followed by rapid intravenous sodium iodide.
b. intravenous propylthiouracil (PTU) followed by slow intravenous sodium iodide.
c.oral propylthiouracil followed by slow intravenous sodium iodide.
d. oral sodium iodide followed by intravenous methimazole.
e.oral sodium iodide followed by intravenous propylthiouracil.
550. Secondary hypothyroidism is usually caused by panhypopituitarism and initially leads to:
a. thyroglobulin deficiency.
b. thyroid releasing hormone deficiency.
c. thyrotropin (thyroid stimulating hormone) deficiency.
d. thyroxin deficiency.
e. triiodothyrinine deficiency.
551. A 70-year-old patient is sent by her family doctor because
“She’s just not acting right.” Rectal temperature 95.2oF, heart
rate 48 / minute, blood pressure 102/72 mmHg. She is slow
to respond. You notice periorbital edema and a thick tongue.
Her EKG shows sinus bradycardia and low voltage, but no
ischemia. Her general appearance is as shown here. In
addition to abnormal thyroid function testing, you would also
expect to find:
a. hyperchloremia.
b. hyperglycemia.
c. hypocarbia.
d. hypomagnesemia.
e. hyponatremia.
552. Concerning the patient in Question #551, you will need to begin therapy using intravenous:
a. high-dose steroids and a diuretic.
b. levothyroxine and hydrocortisone.
c. thyroglobulin and ACTH.
d. thyrotropin and insulin.
e. triiodothyrinine and a beta-blocker.
169
547. d
th
Rosen 5 ,
Chapter 122,
p. 1774
548. b
Rosen 5th,
Chapter 122,
p. 1774
549. c
Rosen 5th,
Chapter 122,
p. 1774
550. c
Rosen 5th,
Chapter 122,
p. 1778
551. e
Rosen 5th,
Chapter 122,
p. 1778
552. b
Rosen 5th,
Chapter 122,
p. 1778-1779
Initial treatment of thyroid storm consists of stabilization, airway protection,
oxygenation, intravenous fluids, and monitoring. Blockade of the peripheral
adrenergic hyperactivity of thyroid crisis may be the most important factor in reducing
morbidity and mortality. Beta-blockade is currently the method of choice for
staunching the peripheral manifestations of thyroid storm. Propranolol can reduce
dysrhythmias, hyperpyrexia, tremor, palpitations, restlessness, anxiety, and perhaps
myopathy.
Hyperpyrexia of thyroid storm should be treated aggressively with acetaminophen.
Aspirin should not be used because it displaces thyroid hormone from thyroglobulin,
thus theoretically increasing the pool of metabolically active hormone. Ice packs and
hypothermia blankets may also be used.
Thioamides, including propylthiouracil (PTU) and methimazole, inhibit thyroidal
peroxidase, thereby preventing hormone synthesis. PTU is generally preferred over
methimazole because it has the additional minor effect of inhibiting peripheral
conversion of T4 to T3. PTU is given in an initial dose of 600 to 1000 mg by mouth
(PO) or by nasogastric (NG) tube, followed by 200 to 250 mg every 4 to 6 hours.
Further organification of iodine will be blocked within 1 hour of PTU administration,
but the drug should be continued for several weeks while the hyperthyroidism is
brought under control. Because preformed T4 and T3 are stored in the thyroid colloid,
release of hormone can occur for weeks despite synthesis inhibition. Thus prevention
of colloid hormone release is the second goal of therapy. Both iodine and lithium can
inhibit thyroid hormone release. Lithium is not generally used because it can be
difficult to titrate the dose, and toxic effects are common. Thioamides should be given
at least 1 hour before iodine therapy to prevent organification of the iodine. Lugol’s
iodine solution, 30 drops per day in 3 to 4 divided doses PO or by NG tube; potassium
iodide (SSKI), 5 drops every 6 hours PO or by NG tube; or sodium iodide, 1 g slow
intravenous (IV) drip every 8 to 12 hours, is acceptable.
Regulation of synthesis and release of thyroid hormone is under the control of the
anterior pituitary gland via thyroid-stimulating hormone (TSH), or thyrotropin.
Regulation of TSH in turn is by hypothalamic thyrotropin-releasing hormone (TRH)
and also by means of a feedback loop to the pituitary gland by circulating thyroxine
(T4) and triiodothyrinine (T3) levels. Thyroid hormone production depends on
adequate iodine intake and synthesis of thyroglobulin.
Laboratory evaluation of patients with suspected myxedema coma may reveal anemia;
hyponatremia; hypoglycemia; elevated transaminases, creatine phosphokinase, and
lactate dehydrogenase levels; hypercholesterolemia; and arterial blood- gas
abnormalities (decreased PO2 and increased PCO2). The electrocardiogram may
demonstrate sinus bradycardia, prolongation of the QT interval, and low voltage with
flattening or inversion of T waves.
Specific therapy includes intravenous levothyroxine; an initial intravenous bolus is
administered, followed by a reduced daily dose until the patient can take oral
medication. This has the advantage of repleting the T4 pool and allowing the hormone
to enter tissues slowly. Stress dosages of corticosteroids, such as 300 mg of
hydrocortisone IV followed by 100 mg IV every 6 to 8 hours, are also routinely given
because myxedema may be either a manifestation of panhypopituitarism or a
coexisting condition with primary adrenal failure.
170
553. The most common precipitating factor for myxedema coma is:
a. barbiturates.
b. depression.
c. diuretics.
d. infection.
e. trauma.
554. A 62-year-old man presents with classic symptoms of hypothyroidism – mild hypothermia,
bradycardia, hoarse voice, and bilateral carpal tunnel syndrome. You find no signs of
infection. He has an extensive cardiac history, including an automatic internal defibrillator,
and is on a waiting list for heart transplant. He takes many medications, but the one you
suspect is probably causing his thyroid malfunction is:
a. amiodarone (Cordarone®).
b. bumetinide (Bumex®).
c. enalapril maleate / felodipine (Lexxel®).
d. lovastatin (Mevacor®).
e. sotalol (Betapace®)
555. The most common cause of acute adrenal insufficiency and adrenal crisis is
a. hypothalamic infarct.
b. fuunctional, from exogenous glucocorticoid administration.
c. non-adrenal catecholamine-secreting tumors.
d. post-partum panhypopituitarism (Sheehan’s syndrome).
e. Waterhouse-Friderichsen syndrome.
556. Aldosterone is the primary mineralocorticoid. It is regulated by the renin-angiotensin system and
acts to:
a. change the osmotic “set-point” in the hypothalamus.
b. decrease potassium excretion.
c. decrease water retention.
d. increase calcium reabsorption.
e. increase sodium reabsorption.
557. Common laboratory findings in a patient with adrenal insufficiency include:
a. high sodium, high potassium, high glucose.
b. high sodium, low potassium, low glucose.
c. low sodium, high potassium, low glucose.
d.
e.
low sodium, low potassium, high glucose.
low sodium, low potassium, low glucose.
558. A 28-year-old woman has just returned from a 10-day cruise. She forgot to bring her prednisone,
which she uses to treat her rheumatoid arthritis. She started vomiting yesterday and now appears
quite dehydrated. Pulse 120 / minute, blood pressure 84/42 mmHg. The best way to treat her
hypotension is:
a. corticosteroids.
b. intravenous fluids and corticosteroids.
c. intravenous fluids and pressor agents.
d. intravenous fluids.
e. pressor agents.
171
553. d
th
Rosen 5 ,
Chapter 122,
p. 1778
554. a
Rosen 5th,
Chapter 122,
p. 1775
555. b
th
Rosen 5 ,
Chapter 122,
p. 1779
556. e
Rosen 5th,
Chapter 122,
p. 1781
557. c
Rosen 5th,
Chapter 122,
p. 1781-1782
558. b
Rosen 5th,
Chapter 122,
p. 1781
A patient suspected of presenting with myxedema coma commonly has a prior history
of primary hypothyroidism or previous thyroid surgery. Medication noncompliance or
coexisting stressors such as cold exposure, severe infection, or the addition of new
medications may precipitate the onset of myxedema coma. By far, infection is the
most common cause.
The many complex effects of iodine-rich amiodarone on thyroid physiology may lead
to asymptomatic abnormalities of thyroid hormone levels, including an elevated TSH,
as well as clinically relevant hypofunction of the thyroid gland. Hypothyroidism has
been estimated to occur in 1% to 32% of patients taking amiodarone.
The most common cause of tertiary adrenal insufficiency and adrenal crisis is
functional, from exogenous glucocorticoid administration. Rapid withdrawal of
steroids from patients with adrenal atrophy secondary to chronic steroid use may result
in collapse and death, especially under circumstances of increased stress.
The major mineralocorticoid is aldosterone. The renin-angiotensin system and plasma
potassium concentration regulate aldosterone through negative feedback loops.
Aldosterone acts to increase sodium reabsorption and potassium excretion, primarily in
the distal tubules of the kidneys.
The usual laboratory findings in patients with primary adrenal insufficiency include
hyponatremia, hyperkalemia, hypoglycemia, and azotemia. Hyponatremia is present in
88% of cases and is usually mild to moderate; severe hyponatremia (<120 mEq/L) is
rare. Hyperkalemia is present in 64% of cases, usually mild; the potassium level rarely
exceeds 7 mEq/L. Two-thirds of patients with adrenal failure have hypoglycemia and
the glucose levels are less than 45 mg/dl; the pathophysiology is decreased
gluconeogenesis and increased peripheral glucose use secondary to lipolysis.
Several mechanisms produce hypotension. Cortisol deficiency, even in the presence of
normovolemia, can lead to hypotension by directly depressing myocardial contractility.
Responsiveness to catecholamines is also reduced. If aldosterone deficiency coexists,
sodium wasting can lead to hypovolemia. Volume deficits are greater in primary than
in secondary adrenal insufficiency. Elevations in renin-angiotensin function and ADH
secretion are seen and partially compensate for the relative or absolute hypovolemia
present. Understandably, response to pressors is poor, to volume replacement better,
and to volume plus corticosteroids best.
172
559. You are seeing a young man whom you believe to have adrenal insufficiency. You have started
intravenous fluids and arranged for admission. Because of his hypotension, you wish to start
appropriate replacement therapy, but you know that he will need an ACTH stimulation test
performed to confirm your diagnosis. Therefore you choose to give:
a. cortisone acetate.
b. dexamethasone phosphate.
c. fludrocortisone acetate (Florinef®).
d. hydrocortisone sodium succinate.
e. hypertonic 3% saline solution.
560. Adrenal crisis is an acute, life-threatening emergency that must be suspected and treated based upon
clinical impression. The primary treatment of choice for a patient known to have adrenal failure is:
a. cortisone acetate
b. dexamethasone phosphate
c. fludrocortisone acetate (Florinef)
d. hydrocortisone hemisuccinate
e. hypertonic 3% saline solution
561. The most important blood protein buffer is:
a. albumin.
b. fibrinogen.
c. glucose-6 phosphatase.
d. hemoglobin.
e. myoglobin.
562. The most common acid-base disorder seen in the seizing patient is:
a. metabolic acidosis.
b. metabolic alkalosis.
c. mixed respiratory / metabolic acidosis.
d. respiratory acidosis.
e. respiratory alkalosis.
563. You are treating a patient with diabetes whom you suspect to be in ketoacidosis. She has
a fruity smell on her breath and she is taking deep, rapid respirations. Which statement is
True?
a. DKA occurs most often in type II diabetics
b. The occurrence of DKA in Type II patients is extremely rare
c. DKA can be caused by any condition that reduces insulin availability or activity or that decreases
glucagons
d. DKA can be induced by emotional or physical stressors
e. In DKA, decreased lipolysis resulting in the breakdown of free fatty acids, leads to production of
ketoacids.
564. Choose the correct match.
a. acute respiratory acidosis increased PaCO2, decreased pH, normal HCO3–
b. chronic respiratory acidosis increased PaCO2, decreased pH, increased HCO3–
c. acute respiratory alkalosis decreased PaCO2, increased pH, normal plasma HCO3–
d. chronic respiratory alkalosis decreased PaCO2, increased pH, decreased plasma HCO3–
e. all of the above are correct.
173
559. b
th
Rosen 5 ,
Chapter 122
p.1782
560. d
Rosen 5th,
Chapter 122,
p. 1782
561. d
th
Rosen 5 ,
Chapter 118,
p. 1714-1715
562. d
Rosen 5th,
Chapter 118,
p. 1717
563. d
Rosen 5th,
Chapter 118,
p. 1715
564. e
Rosen 5th,
Chapter 118,
p. 1716-1722
If the diagnosis of adrenal failure is unconfirmed, dexamethasone phosphate, 4 mg IV
every 6 to 8 hours, is the corticosteroid replacement that should be used while an
ACTH stimulation test is performed. Dexamethasone is approximately 100 times more
potent than cortisol, and this amount of dexamethasone will not factitiously elevate
serum cortisol determinations. Replacement with hydrocortisone could confound
interpretation of serum cortisol determinations.
For a patient known to have adrenal failure, 100 mg of hydrocortisone hemisuccinate
IV every six to eight hours should be used. If IV access cannot be obtained, cortisone
acetate, 100 mg IM every six to eight hours, may be used, but its absorption is erratic
and not as reliable as the IV route.
Many protein buffers in blood are effective in maintaining acid-base homeostasis. The
most important is hemoglobin, which can buffer large amounts of H+, preventing
significant changes in the pH. If hemoglobin did not exist, venous blood would be 800
times more acidic than arterial blood, circulating at a pH of 4.5 instead of the normal
venous pH of 7.37.
Transient respiratory acidosis is the most common acid-base disorder seen acutely in
the seizure patient. Treatment centers on control of the seizure activity and assisted
ventilation if required. Intravenous bicarbonate is not recommended because these
patients resolve their acid-base disorder with return of spontaneous ventilation.
DKA presents clinically as a triad: hyperglycemia (usually >200 mg/dl), ketonemia
(>1:2 dilutions) and academia (pH <7.3). DKA can be caused by any condition that
reduces insulin availability or activity or that increases glucagons. DKA occurs most
often in type I diabetic patients with little or no endogenous insulin; however, its
occurrence in type II patients, particularly obese African-Americans, is not as rare as
once thought. Increase lipolysis, resulting in the breakdown of free fatty acids, leads to
production of ketoacids. Precipitating events usually include infections, surgery, and
emotional and physical stressors.
All are correct.
174
565. Treatment for patients with saline responsive metabolic alkalosis might include:
a. intravenous mineral acids (i.e. arginine monohydrochloride)
b. normal saline solution.
c. acetazolamide.
d. dialysis.
e. all of the above.
566. Choose the correct statement about lactic acidosis:
a. The body does not have a mechanism to break down lactic acid, accounting for its
toxicity.
b. Most lactic acidosis is associated with normal tissue perfusion.
c. The liver converts about 20% of lactate into glucose.
d. Pyruvate metabolism does not affect the fate of lactic acid.
e. Since most lactic acid is cleared by the kidneys, its excretion is enhanced by using
intravenous bicarbonate.
567. When considering electrolytes:
a. calcium is primarily intracellular.
b. magnesium is primarily extracellular.
c. phosphorus is primarily extracellular.
d. potassium is primarily intracellular.
e. sodium is primarily intracellular.
568. Daily maintenance fluid requirements for an average-sized patient with a fever of 101oF is
about:
a. 1000 – 1500 cc.
b. 1500 – 2500 cc.
c. 2000 – 3000 cc.
d. 3000 – 4000 cc.
e. 4000 – 5000 cc.
569. The most common cause of redistributive hyponatremia is:
a. diuretic use
b. hyperglycemia
c. laxative abuse
d. protein-wasting nephropathy
e. water intoxication
570. In patients with symptomatic chronic hyponatremia, correction must take place in a
controlled fashion. Overaggressive saline administration can lead to:
a. acute renal failure.
b. ARDS.
c. coma, seizures, and quadraparesis.
d. fulminant hepatic failure.
e. life-threatening cardiac dysrhythmias.
571. The only known mechanism for hypervolemic hypernatremia is:
a. overdose on mercurial diuretics.
b. licorice ingestion.
c. salicylate toxicity.
d. excess sodium intake.
175
e. laxative abuse.
176
565. a
th
Rosen 5 ,
Chapter 118,
p. 1721
566. d
Rosen 5th,
Chapter 118,
p. 1119-1120
567. d
Rosen 5th,
Chapter 119
568. d
Rosen 5th,
Chapter 119
569. b
Rosen 5th,
Chapter 119,
p. 1724
570. c
Rosen 5th,
Chapter 119,
p. 1726
571. d
Rosen 5th,
Chapter 119,
p. 1726-1727
In a patient with saline responsive alkalosis, treatment is directed toward correcting the
urinary excretion of HCO3-. Administration of NaCl and KCl suppresses both renal
acid excretion and HCO3- excretion. In patients who are severely volume depleted,
administration of IV mineral acids (e.g., arginine monohydrochloride) may be
necessary. In edematous states for which saline therapy may be contraindicated,
acetazolamide will increase the excretion of HCO3-, treating both the alkalosis and the
edema.
Lactic acidosis is a marker of hypoperfusion and ongoing shock. A product of
anaerobic metabolism, lactic acidosis develops when an imbalance exists between
lactic acid production and subsequent conversion by the liver and kidney. Pyruvic acid
is metabolized aerobically into CO2 and H2O or anaerobically to lactic acid. Lactic
acid is then buffered by HCO3-, forming lactate. The liver converts 80% of lactate into
CO2 and H2O and 20% to glucose. This reaction regenerates HCO3- in the process and
balances the acid-base balance.
Electrolytes are classified according to electronic charge, cations (positively charged
ions) and anions (negatively charged ions). The principal cations in the intracellular
compartment are K+ and Mg2+, whereas the principal anions are PO4- and proteins. In
the plasma and interstitial fluids, which together make up the extracellular fluid space,
Na+ is the predominant cation, while Cl- and HCO3- are the major anions.
To maintain balance, an average normal adult requires approximately 2000 to 3000 mL
intake of water per day. This accounts for the volume of water lost in a day due to
insensible and urinary losses. The insensible loss can accelerate dramatically in the
setting of fever (500 mL per 1°C fever), sweating (up to 1500 mL), and gastrointestinal
losses.
Hyponatremia with an increase in osmotically active solutes occurs when there is an
accumulation of large quantities of solutes restricted primarily to the ECF space. In
this setting, there is a net movement of water from the ICF to the ECF, thereby
effectively diluting the ECF [Na+]. The most common cause of this is hyperglycemia.
Each 100-mg/dL increase in plasma glucose decreases the serum [Na+] by 1.6 to 1.8
mEq/L.
Acute hyponatremia may be corrected at rates of up to 1 to 2 mEq/L/hr, and chronic
hyponatremia should be corrected at a rate not greater than 0.5 mEq/L/hr. In general
the serum sodium should not be corrected to above 120 mEq/L or increased by more
than 10 mEq/L in a 24-hour period. Hypertonic saline should be administered through
a controlled intravenous (IV) infusion, with careful attention to fluid input and output
and frequent assessment of serum electrolytes. The approximate required dose of
hypertonic saline can be calculated with the following formula:
(desired [Na+] – measured [Na+]) x (0.6) (weight in kg) = mEq [Na+] administered
Overaggressive correction of the serum sodium may have serious consequences.
Central pontine myelinolysis (CPM), also known as cerebral demyelination, involves
the destruction of myelin in the pons and is thought to result from rapid elevation of
the serum sodium. Patients may develop cranial nerve palsies, quadriplegia, or coma.
CPM is more likely to occur in patients with chronic hyponatremia than in those with
acute hyponatremia.
Excessive sodium intake, accidentally, intentionally, or iatrogenically, may cause
hypernatremia in the absence of corresponding intake of water. Because the kidney
can usually excrete an increased sodium load effectively, most cases are seen in
patients with renal insufficiency.
177
572. An elderly woman is found unconscious in her non-air conditioned apartment during a July
heat spell. Heart rate 125 / minute, blood pressure 70/palpable. Her serum sodium is 170
mEq/L, so you make sure that the intravenous which is running contains:
a. 0.9% saline.
b. 0.45% saline.
c. 0.225% saline.
d. 5% dextrose.
e. 5% dextrose / 0.9% saline.
573. In a patient with a potassium level of 7.6 mEq/L and this
rhythm strip, the medication which should be given first is:
a. calcium gluconate 5 – 10 mEq intravenously to stabilize
cardiac membranes.
b. furosemide 40 mg intravenously to promote renal K+
excretion.
c. glucose 50 gm intravenously to move K+ to the
intracellular space.
d. sodium bicarbonate 50 mEq intravenously to assist in K+ redistribution.
e. sodium polystyrene (Kayexalate®) 15 to 50 gram orally or rectally to bind K+ for rectal
excretion.
574. In the absence of acute shifts caused by acid-base disturbances, a decrease of the serum
potassium by 1.0 mEq/L may reflect what deficit of potassium?
a. 80 mEq/L
b. 150 mEq/L
c. 225 mEq/L
d. 300 mEq/L
e. 370 mEq/L
575. If you were to inadvertently rapidly bolus a liter of 0.45% saline into a normovolemic
osmotically balanced patient, the first change you might notice is:
a. contraction of both extracellular fluid and intracellular fluid.
b. contraction of extracellular fluid, expansion of intracellular fluid.
c. expansion of both extracellular fluid and intracellular fluid.
d. expansion of extracellular fluid, contraction of intracellular fluid.
e. expansion of extracellular fluid, no change in intracellular fluid.
576. In a patient with diabetes insipidus:
a. fluid restriction is essential.
b. hypernatremia is the rule.
c. intranasal vasopressin may be helpful.
d. there is an osmolar gap.
e. urine specific gravity is high.
577. A patient is found to have a serum calcium level of 4.5 mEq. You expect most of her
symptoms to be related to the:
a. central nervous system.
b. pulmonary system.
c. cardiovascular system.
d. neuromuscular system.
e. gastrointestinal system.
178
572. a
th
Rosen 5 ,
Chapter 119,
p. 1727p.
573. a
th
Rosen 5 ,
Chapter 119,
p. 1731
574. c
Rosen 5th,
Chapter 119,
p. 1729
575. b
th
Rosen 5 ,
Chapter 119,
p. 1727
576. c
th
Rosen 5 ,
Chapter 119,
p. 1726
577. d
Rosen 5th,
Chapter 119,
p. 1733
The primary goals in the emergency management of hypovolemic hypernatremic
patients are to restore volume deficits and to maintain organ perfusion. Treatment
should begin with an infusion of isotonic solution (0.9% NaCl). Once the patient is
hemodynamically stable, the remaining free water deficits can be replaced.
Treatment of hyperkalemia involves three processes: membrane stabilization
(especially cardiac tissue), shifting potassium from extracellular to intracellular, and
removing excess potassium from the body. Membrane stabilization is achieved with
calcium gluconate or calcium chloride. This is indicated in any patient with unstable
dysrhythmias or hypotension. Several ampules of calcium ( 10 ml or 10% solution)
may be required. Because of the brief duration of action (approximately 20-40
minutes), other measures should also be instituted promptly.
In the absence of acute shifts caused by acid-base disturbances, a decrease
of the serum potassium by 1.0 mEq/L may reflect a 370 mEq deficit of total
potassium.
Hypotonic saline infusion will lower the extracellular fluid osmotic strength, which
will then cause a shift of extracellular fluid into the cells until the osmolalities are
equalized.
Diabetes insipidus (DI) results in loss of large amounts of dilute urine because of the
loss of concentrating ability in the distal nephrons. DI can be central (lack of ADH
secretion from the pituitary) or nephrogenic (lack of responsiveness to circulating
ADH). Patients are usually able to maintain near-normal serum levels as long as
access to water is maintained. Patients will have a low urine specific gravity (<1.005)
and low urine osmolality. Those with central DI require the administration of
parenteral or intranasal vasopressin.
The clinical manifestations of hypocalcemia depend not only on the serum level but
also on the rapidity with which it declines. Although the signs and symptoms of
hypocalcemia are numerous, the effects on neuromuscular function predominate. A
declining serum calcium level is associated with progressive neuromuscular
hyperexcitability.
179
578. The most common cause of symptomatic hypokalemia is:
a. hyperemesis.
b. diuretic therapy.
c. beta-agonist therapy.
d. diabetes insipidus.
e. SIADH.
579. Patients who have undergone prolonged starvation and are suddenly fed can develop:
a. hypocalcemia.
b. hypoglycemia.
c. hypokalemia.
d. hyponatremia.
e. hyperphosphatemia.
580. In an adult patient with tetany and a positive Trousseau sign 5 days after thyroidectomy,
an appropriate treatment would be:
a. 10 ml of 10% calcium chloride IV bolus.
b. 100 ml of 10% calcium gluconate IV slow drip.
c. 25 ml of intravenous calcium biphosphonate.
d. 50 ml of sodium bicarbonate, then 200 mcg intravenous PTH.
e. fresh frozen plasma 4U.
581. A 61-year-old man complains of
weakness, numbness around his
mouth, and no appetite. When the
nurse checks his blood pressure she
notes this finding. You send serum
calcium, expecting it to be low. You
also order an EKG, expecting to find:
a. frequent PVCs.
b. prolonged QT interval.
c. second or third degree heart block.
d. shortened PR interval.
e. tachycardia.
582. More than 90% of cases of hypercalcemia are associated with:
a. adrenal insufficiency.
b. dietary indiscretion.
c. malignancy and primary hyperparathyroidism.
d. sarcoidosis and other granulomatous diseases.
e. vitamin A or D toxicity.
583. A 54-year-old woman who is being treated for breast cancer complains of fatigue, malaise,
and loss of appetite. Clinically she is mildly dehydrated. Her serum calcium is 14.3 mg/dl.
You begin treatment in the Emergency Department, realizing that:
a. glucocorticoids are contraindicated.
b. hypotonic saline administration will lead to normalization more than half the time.
c. the side effects of digoxin are accentuated in the presence of hypercalcemia.
d. simultaneously occurring hypermagnesemia must be recognized and treated.
e. thiazide diuretics are preferred over loop diuretics.
180
578. b
th
Rosen 5 ,
Chapter 119,
p. 1728
579. c
Rosen 5th,
Chapter 119,
p. 1728
580. a
Rosen 5th,
Chapter 119,
p. 1733
581. b
Rosen 5th,
Chapter 119,
p. 1733
582. c
Rosen 5th,
Chapter 119,
p. 1734
583. c
th
Rosen 5 ,
Chapter 119,
p. 1735
Diuretic therapy, the most common cause of hypokalemia in clinical practice, increases
sodium delivery to the distal tubule, promoting potassium excretion. Associated
volume depletion and high levels of aldosterone cause K+ and H+ excretion and may
worsen hypokalemia. In addition, alkalosis from H+ excretion promotes cellular
potassium uptake, further lowering the serum potassium. Other disorders can cause
significant renal potassium loss. These include osmotic diuresis, high
mineralocorticoid states, magnesium depletion, and high urinary concentrations of
anions such as penicillin. Intrinsic renal causes of potassium loss include renal tubular
acidosis (RTA), chronic interstitial disease, and drugs that affect tubular potassium
reabsorption. RTA type 1 is caused by a defect in H+ secretion in the distal tubule,
and RTA type 2 is associated with a similar defect in the proximal tubule.
Hypokalemia resulting from decreased dietary intake is rare. However, when poor
intake is combined with other factors (e.g., vomiting or diarrhea, high insulin or
aldosterone levels), severe hypokalemia may result. Patients suffering from prolonged
starvation may become hypokalemic when they are fed because insulin secretion and
increased cellular uptake cause potassium to move into cells.
Two different calcium formulations are readily available in most Emergency
Departments: (1) 10-ml ampules of 10% calcium chloride, which contain 360 mg of
elemental calcium, and (2) 10-ml ampules of 10% calcium gluconate, which contain 93
mg of elemental calcium. For the adult patient the recommended initial dose is 100 to
300 mg of elemental calcium given as calcium chloride or calcium gluconate. This
dose of calcium will increase the serum ionized calcium for only a short time (1 to 2
hours) and should be followed by repeated doses or an infusion at a rate of 0.5 to 2
mg/kg/hr.
Severe hypocalcemia causes a decrease in myocardial contractility and rarely
bradycardia, hypotension and symptomatic CHF. Patients with preexisting cardiac
dysfunction and those taking digoxin or diuretics are especially at risk. The ECG may
demonstrate QT prolongation and an inverse relationship exists between the serum
calcium and the QT interval. However, the ECG is a poor predictor of hypocalcemia
and should not be used to rule in or rule out this disorder.
Hypercalcemia is a relatively common entity. It is defined as a total calcium level
exceeding 10.5 mg/dL or an ionized calcium level exceeding 2.7 mEq/L. Over 90% of
occurrences are associated with hyperparathyroidism or malignancy.
Calcium potentiates the action of digoxin, and the side effects of digoxin are
potentiated when hypercalcemia is present. The administration of isotonic saline is the
first step in the management of severe hypercalcemia. Once the intravascular volume
has been restored to normal, the serum calcium will usually have decreased by 1.6 to
2.4 mg/dl, although hydration alone rarely leads to complete normalization. Loop
diuretics such as furosemide inhibit the resorption of calcium in the thick ascending
loop of Henle, increasing the calciuric effect of hydration. Volume expansion must
precede the administration of furosemide. Thiazide diuretics should not be used
because they enhance distal absorption of calcium and may worsen hypercalcemia.
Glucocorticoids are useful in patients with sarcoidosis, vitamin A or D intoxication,
multiple myeloma, leukemia, or breast cancer. They work by inhibiting bone
resorption and gastrointestinal absorption of calcium.
181
584. The most likely EKG finding in a patient with severe magnesium depletion is:
a. bradycardia.
b. PVCs and other ventricular dysrhythmias.
c. prolonged QT interval.
d. second or third degree heart block.
e. shortened PR interval.
585. Clinically significant hypermagnesemia is encountered almost exclusively in patients with:
a. adrenal insufficiency.
b. exogenous magnesium administration, like antacids.
c. impaired renal magnesium excretion.
d. rhabdomyolysis.
e. tumor lysis syndrome.
586. You are treating a pregnant woman for pre-eclampsia while awaiting emergent delivery.
She shows signs of iatrogenic hypermagnesmeia. After infusing isotonic saline and giving
a loop diuretic, you can reverse her respiratory depression and hypotension by giving:
a. 20 ml of 10% calcium chloride IV bolus.
b. 25 ml of intravenous potassium phosphate.
c. 40 mEq potassium chloride intravenously over two hours.
d. 50 – 100 mEq IV sodium bicarbonate.
e. methotrexate.
587. A 45-year-old man complains of myalgias and severe weakness. You have treated him in
the past for alcohol-related diseases. You suspect he is suffering from:
a. hypercalcemia.
b. hyperchloremia.
c. hyperkalemia.
d. hyponatremia.
e. hypophosphatemia.
588. A 68-year-old man complains of shortness of breath. He takes digoxin for chronic atrial
fibrillation. You listen to his heart and find an irregular rhythm. You know that digitalisinduced dysrhythmias can be made worse by:
a. hypocalcemia.
b. hypoglycemia.
c. hyperkalemia.
d. hypomagnesemia.
e. hypophosphatemia.
589. The most common cause of hyperphosphatemia is:
a. adrenal insufficiency.
b. exogenous phosphorus administration.
c. renal failure.
d. rhabdomyolysis.
e. tumor lysis syndrome.
182
584. b
th
Rosen 5 ,
Chapter 119,
p. 1738
585. c
Rosen 5th,
Chapter 119,
p. 1738
586. a
th
Rosen 5 ,
Chapter 119,
p. 1739
587. e
Rosen 5th,
Chapter 119,
p. 1740
588. d
Rosen 5th,
Chapter 119,
p. 1738
589. c
th
Rosen 5 ,
Chapter 119,
p. 1741
Dysrhythmia is the most common cardiovascular manifestation of hypomagnesemia.
A number of studies demonstrate an increased incidence of supraventricular
dysrhythmias (atrial fibrillation, multifocal atrial tachycardia, paroxysmal
supraventricular tachycardia) and ventricular dysrhythmias (PVCs, ventricular
tachycardia, torsade de pointes, ventricular fibrillation) in patients who are magnesium
deficient. Digitalis-induced dysrhythmias are also more likely in the presence of
hypomagnesemia. Because magnesium is an essential cofactor for the Na+-K+
ATPase pump that is inhibited by digitalis, hypomagnesemia typically worsens the
manifestations of digitalis toxicity.
Clinically significant hypermagnesemia is encountered almost exclusively in the
setting of renal insufficiency. Serum magnesium levels rise as the creatinine clearance
falls below 30 ml/min and typically reach approximately 2.5 mEq/L as renal function
nears zero.
Patients with severe hypermagnesemia should receive IV calcium. Calcium directly
antagonizes the membrane effects of hypermagnesemia and reverses respiratory
depression, hypotension, and cardiac dysrhythmias. For life-threatening
manifestations of hypermagnesemia, 100 to 200 mg of calcium, as either 10% calcium
gluconate (93 mg calcium per ampule) or 10% calcium chloride (360 mg calcium per
ampule), is a reasonable dose.
Although diabetic ketoacidosis is an important cause of hypophosphatemia, decreased
phosphate intake and impaired intestinal phosphate absorption are other causes of
hypophosphatemia. Up to 50% of alcoholics are hypophosphatemic. Increased renal
excretion and decreased intake are the proposed mechanisms. Hypophosphatemia may
be exacerbated when glucose-containing solutions are administered because these
cause phosphate to shift from the serum into cells.
Hypomagnesemia, like hypokalemia and hypercalcemia, will worsen the
manifestations of digitalis toxicity. Digitalis-induced dysrhythmias are more likely in
the presence of hypomagnesemia.
Renal failure is the most common cause of hyperphosphatemia. The serum phosphate
typically remains normal until the creatinine clearance falls below 30 ml/min.
Hyperphosphatemia is usually mild unless an exogenous phosphate load is given
183
6.0 – Environmental Disorders
590. Which statement is true concerning the physiology of cold exposure?
a. Just as with heat exposure, humans develop physiologic adaptation to the cold.
b. During cold stress, peripheral vasodilation limits radiant heat loss.
c. Cutaneous blood flow plays a minimal role in maintaining heat homeostasis.
d. The unsheltered and homeless remain the group most likely to suffer cold-related injury.
e. Peripheral cooling of the blood activates the preoptic anterior hypothalamus, which then
orchestrates temperature regulation.
591. The ultimate determinant of progressive tissue damage from cold-exposure appears to be
injury to the:
a. clotting cascade.
b. complement cascade.
c. microvasculature.
d. platelets.
e. red blood cells.
592. Predisposing factors to the development of frostbite include:
a. anhidrosis.
b. hypertension.
c. loose clothing and boots.
d. overeating.
e. vasoconstrictors and vasodilators.
593. The most common presenting symptom of frostbite is:
a. burning pain.
b. gnawing pain.
c. numbness.
d. sharp pain.
e. tingling and other dysesthesias.
594. Some studies suggest that chilblains (pernio) can be both treated and prevented with:
a. beta-agonists (terbutaline, albuterol).
b. beta-blockade.
c. naloxone (Narcan®).
d. nifedipine (Procardia®).
e. steroid burst.
595. When treating an Emergency Department patient who has experienced frostbite:
a. a common error is “overshoot” rewarming, resulting in a heat damage to the tissues.
b. gentle, passive rewarming is less destructive to damaged tissues than aggressive
warming.
c. rapid rewarming can lead to hypokalemia and severe metabolic alkalosis.
d. rethawing is essentially a painless procedure.
e. rewarming should be continued until the part feels pliable and you see distal erythema.
184
590. e
th
Rosen 5
Chapter 133,
p. 1972
591. c
Rosen 5th
Chapter 133,
p. 1973
592. e
Rosen 5th
Chapter 133,
p. 1974
593. c
Rosen 5th
Chapter 133,
p. 1973
594. d
th
Rosen 5
Chapter 133,
p. 1974
595. e
th
Rosen 5
Chapter 133,
p. 1975
The preoptic anterior hypothalamus is the central thermostat. Cutaneous blood flow in
the euthermic 70 kg human averages 200 to 250 ml/min. Heat stress causes
vasodilatation that can increase this amount to 7000 ml/min. In contrast, extreme coldinduced vasoconstriction reduces flow tenfold to less than 50 ml/min. In contrast to
heat exposure, humans do not appear to display significant physiologic adaptation to
the cold. The unsheltered and the homeless are no longer the most likely group at risk.
Most cases of civilian frostbite now result from routine exposure to cold by individuals
who have not given due consideration to risk factors for cold injury, such as
participants in outdoor recreational activities that produce exposure to unanticipated
drastic climatic changes.
The ultimate determinant of progressive tissue damage appears to be injury to the
microvasculature. Endothelial cells are the tissue most susceptible to freezing injury.
After thawing, the vasculature is only patent temporarily. Platelet and erythrocyte
aggregates promptly clog and distort the vasculature. Intense vasoconstriction coupled
with arteriovenous shunting occurs at the interface between normal and damaged
tissue. The injured viable vasculature remains distorted. Local arteritis, medial
degeneration, and intimal proliferative thickening are seen.
Predisposing factors to cold injury include:
Physiologic – genetic, core temperature, previous cold injury, ±acclimatization,
dehydration, overexertion, trauma: multisystem, extremity, dermatologic diseases,
physical conditioning, diaphoresis, hyperhidrosis, hypoxia
Mechanical – constricting or wet clothing, tight boots, vapor barrier, inadequate
insulation, immobility or cramped positioning
Psychological – mental status, fear, panic, attitude, peer pressure, fatigue, intense
concentration on tasks, hunger, malnutrition, intoxicants
Environmental – ambient temperature, humidity, duration of exposure, wind chill
factor, altitude, ± associated conditions quantity of exposed surface, area heat loss:
conductive, evaporative aerosol propellants
Cardiovascular – hypotension, atherosclerosis, arteritis, Raynaud syndrome, anemia,
sickle cell disease, diabetes, hypovolemia, shock, vasoconstrictors, vasodilators
The symptoms of frostbite usually reflect the severity of the exposure. The most
common presenting symptom is numbness, present in more than 75% of patients. All
patients will have some initial sensory deficiency in light touch, pain, or temperature.
Anesthesia is produced by intense vasoconstrictive ischemia and neurapraxia.
Management of chilblains is supportive. The affected skin should be rewarmed, gently
bandaged, and elevated. Some European studies support the use of nifedipine, at a
dose of 20 mg tid, as both prophylactic and therapeutic.
Rewarming should be continued until the part feels pliable and distal erythema is
noted. Frozen or partially thawed tissue should be rapidly and actively rewarmed by
immersion in gently circulating water that is carefully maintained at a temperature of
37° to 40° C by thermometer measurement. A common error is premature termination
of rewarming, which results in a partial thaw. The acute thawing of large amounts of
distal musculature extinguishes peripheral vasoconstriction, resulting in the sudden
return of cold, hyperkalemic, acidotic blood to the central circulation. This produces
“core temperature after-drop,” which is dysrhythmogenic.
185
596. Hypothermia can cause many physiologic changes. Which statement is true.
a. Osborn J waves are both diagnostic and prognostic. The size of the J wave is related to
the arterial pH.
b. Atrial fibrillation is rarely seen as a rhythm of hypothermia. Its presence should clue you
to seek a primary cardiac pathology.
c. Asystole and VF occur spontaneously when the core temperature falls below 25° C.
d. The “core afterdrop” phenomenon is an interesting finding in the laboratory, but of little
clinical significance.
e. Cerebral metabolism increases 6% to 7% for each 1°C decline in temperature.
597. Blood gas analyzers warm the blood to 37°C (99°F), which increases the partial pressure
of dissolved gases. This results in an ABG report showing incorrect values, especially:
a. higher oxygen, higher carbon dioxide levels, higher pH.
b. higher oxygen, higher carbon dioxide levels, lower pH.
c. higher oxygen, lower carbon dioxide levels, lower pH.
d. lower oxygen, higher carbon dioxide levels, lower pH.
e. lower oxygen, lower carbon dioxide levels, lower pH.
598. Which statement is true concerning laboratory findings in a hypothermic patient?
a. A patient’s hematocrit may be deceptively low.
b. Acute hypothermia initially elevates blood sugars, but if hyperglycemia persists during
rewarming, you should suspect hemorrhagic pancreatitis or diabetic ketoacidosis.
c. BUN and hematocrit must be closely followed to determine volume status.
d. Extracellular plasma potassium level is highly temperature dependent.
e. White blood cell counts and platelet counts tend to remain normal.
599. In treating a hypothermic patient with a Bair Hugger, you are heating the patient by:
a.convection.
b.conduction.
c.evaporation.
d.transmission.
e.radiation.
600. Administering warm, humidified oxygen via mask or endotracheal tube to a hypothermic
patient:
a. helps prevent the inevitable rewarming dehydration.
b. is an excellent method for rapid rewarming.
c. serves as a heat “sump.”
d. works best by minimizing heat loss from the lungs.
e. works to promote oxygen use and prevent carbon dioxide retention.
601. The physiology of heat-related disease has been very well described. For instance, we
know that:
a. in a warm environment, convection is the most important mechanism of heat dissipation.
b. skin temperature changes correlate well with changes in rate of heat loss.
c. sweating occurs because of core temperature changes.
d. the major mechanisms of accelerating heat loss are sweating and peripheral vasodilation
e. wind at a velocity of 10 m/sec cools twice as much as wind at velocity 5 m/sec.
186
596. c
th
Rosen 5
Chapter 134,
p. 1981
597. b
Rosen 5th
Chapter 134,
p. 1985
598. b
Rosen 5th
Chapter 134,
p. 1985
599. a
Rosen 5th
Chapter 134,
p. 1991
600. d
th
Rosen 5
Chapter 134,
p. 1991
601. d
th
Rosen 5 ,
Chapter 135,
p. 1998
Asystole and VF occur spontaneously when the core temperature falls below 25°C. J
waves are potentially diagnostic but not prognostic. They may appear at any
temperature less than 32°C. The size of the J wave is not related to arterial pH but
does increase with temperature depression. An analysis of ECGs of accidental
hypothermia patients commonly notes atrial fibrillation when the core temperature is
less than 32°C. Core temperature afterdrop is a clinically relevant consideration when
treating patients with a large temperature gradient between the core and the periphery.
Cerebral metabolism decreases 6% to 7% for each 1°C decline in temperature.
Blood gas analyzers warm the blood to 37°C (99°F), which increases the partial
pressure of dissolved gases. This results in an ABG report showing higher oxygen and
carbon dioxide levels and a lower pH than the patient’s actual values. Optimal ABG
levels in the setting of hypothermia have not been determined, and current literature
concludes that correction of ABGs for temperature is unnecessary as a guide to
therapy.
A patient’s hematocrit may be deceptively high as the result of a decreased plasma
volume. Splenic, hepatic, and splanchnic sequestration in hypothermia decreases
leukocyte and platelet counts. Acute hypothermia initially elevates blood sugar levels
through catecholamine-induced glycogenolysis, diminished insulin release, and
inhibition of cellular membrane glucose carrier systems. When hyperglycemia persists
during rewarming, one should suspect hemorrhagic pancreatitis or diabetic
ketoacidosis. The plasma potassium level is independent of the primary hypothermic
process. Because of hypothermic fluid shifts the hematocrit and BUN levels are poor
indicators of a patient’s actual fluid status.
The Bair Hugger uses hot forced air circulated through a blanket. The air exits
apertures on the patient side of the cover, which allows a convective transfer of heat.
Inhalation rewarming provides a fairly small heat gain and is not effective for rapid
rewarming. It does, however, minimize heat loss from the lungs, a potential loss of up
to 30% of the total metabolic heat production.
Temperature-sensitive structures are located both peripherally in the skin and centrally
in the body. Skin temperature changes correlate poorly with changes in rate of heat
loss. The skin temperature effects heat loss since a person resting in a warm
environment initiates sweating, even though the core temperature remains constant.
Sweating and peripheral vasodilation are the major mechanisms by which heat loss
may be accelerated. In a warm environment, evaporation of sweat from the skin is the
most important mechanism of heat dissipation. The major effect of wind is attained at
a velocity of 0.5 to 5 m/sec; higher velocities do not appreciably increase cooling.
187
602. Acclimatization is defined as "a constellation of physiologic adaptations that appear in a
normal person as the result of repeated exposures to heat stress." Daily exposure to work
and heat for 100 min/day results in near-maximal acclimatization in 7 to 14 days. This is
characterized by:
a. a later onset of sweating at a higher core temperature.
b. diminished plasma volume.
c. diminished sweat volume to prevent dehydration.
d. increased sweat electrolyte concentration to preserve homeostasis.
e. lower heart rate with higher stroke volume.
603. The most critical variable to prevent heat stroke in young, healthy individuals is:
a. ambient temperature.
b. fluid intake.
c. relative humidity index.
d. sodium intake.
e. sweat sodium level.
604. Patients suffering from heat cramps invariably display:
a. hyperchloremia.
b. hyperkalemia.
c. hypernatremia.
d. hypokalemia.
e. hyponatremia.
605. The main difference between heat exhaustion and heat stroke is:
a. heart rate and blood pressure
b. height of temperature.
c. level of CNS dysfunction.
d. serum transaminases elevations.
e. sweating.
606. Concerning exertional vs. classic heat stroke:
a. classic heat stroke occurs in young people with increased heat production.
b. hypoglycemia is more frequently found in exertional heatstroke.
c. sweating is profuse in classic heatstroke.
d. the absolute height of core temperature is the most important prognostic factor.
e. the distinction between the two is important, as treatment varies depending on the cause.
607. Of methods listed, the preferred treatment to rapidly lower core temperature in heatstroke
is:
a. cooling blanket.
b. evaporative cooling using large circulating fans and skin wetting.
c. gastric lavage.
d. ice packs to axillae and groin.
e. peritoneal dialysis.
608. Lightning is:
a. direct current.
b. alternating current.
c. a combination of both direct and alternating current.
d. neither direct nor alternating current, but a unidirectional current impulse.
188
e. a voltage phenomenon.
189
602. e
th
Rosen 5 ,
Chapter 135,
p. 1998
603. b
Rosen 5th,
Chapter 135,
p. 2004
604. e
th
Rosen 5 ,
Chapter 135,
p. 2001
605. c
Rosen 5th,
Chapter 135,
p. 2004
606. b
Rosen 5th,
Chapter 135,
p. 2004
607. b
Rosen 5th,
Chapter 135,
p. 2006
608. d
Rosen 5th,
Chapter 136,
p. 2012
Acclimatization is characterized by an earlier onset of sweating (at a lower core
temperature), increased sweat volume, and lowered sweat electrolyte concentration. It
is hastened by modest salt deprivation and delayed by high dietary salt intake. As
acclimatization proceeds, the sweat sodium concentration drops from approximately 65
mEq/L to as low as 5 mEq/L. The cardiovascular system plays a major role in both
acclimatization and endurance training, largely resulting from a 10% to 25% expansion
of plasma volume that occurs in both situations. Heart rate is lower and associated
with a higher stroke volume.
Exertional heat stroke is most likely to occur in young, healthy people involved in
strenuous physical activity. Fluid intake is the most critical variable. Dehydration
may be minimized by education on work-rest cycles and fluid consumption, and
through provision of cool, pleasantly flavored fluids.
Heat cramps appear to be related to salt deficiency. Several steel mills virtually
eliminated heat cramps in their employees by encouraging salt consumption.
Anecdotal reports from Germany and England indicate that laborers salt their beer to
successfully prevent heat cramps. Heat cramp victims exhibit hyponatremia,
hypochloremia, and low urinary sodium and chloride levels.
Mild heat exhaustion and full-blown heat stroke represent extremes of the spectrum of
heat illness, and intermediate cases may prove difficult to differentiate. Heat
exhaustion should not be diagnosed in the presence of major CNS dysfunction
(seizures, coma) or severe hyperthermia (greater than 40.5°C).
The distinction between exertional and nonexertional heatstroke is moot, because
signs, symptoms, and management are the same. The primary factor that contributes to
the morbidity and mortality of heat illness is the severity of underlying disease and not
the absolute height of the core temperature. Sweating is totally absent in the majority
of classic heatstroke patients. Hypoglycemia in exertional heatstroke may occur as the
result of increased glucose use and hepatic damage resulting in impaired
gluconeogenesis.
Evaporative cooling is the most widely used cooling method. Immersion in ice water
results in a rapid reduction of core temperature to less than 39°C within 10 to 40
minutes. Application of ice packs is commonly used; although technically easier to
perform than cold water immersion, this method sacrifices the conductive cooling
power of water immersion, resulting in slower cooling. Cooling blankets may be a
useful adjunct but will not produce rapid cooling if used exclusively. Peritoneal
dialysis with cold fluids, successful in dogs, remains untested in humans. Cold-irrigant
gastric or rectal lavage will not provide significant heat exchange if used as the
primary cooling modality.
Lightning is neither a direct current nor an alternating current. At best, it is a
unidirectional massive current impulse. Therefore lightning is classed as a current
phenomenon, rather than a voltage phenomenon.
190
609. A 79-year-old woman is brought from her non-air conditioned apartment when neighbors
had not seen her for more than two days. She is comatose with a rectal temperature of
41.6oC (106.8oF). Her heart rate is 46 and her blood pressure is 70 palpable. You begin
rapid cooling techniques and address the other vital sign abnormalities by giving:
a. atropine 1 mg by intravenous bolus.
b. isoproterenol by intravenous drip.
c. norepinephrine by intravenous drip.
d. normal saline solution 2000 cc wide open.
e. nothing initially – the vital signs should all normalize as the patient cools down.
610. Which statement concerning the physiology of electrical injuries is true?
a. Direct current exposure to the same voltage tends to be three times more dangerous than
alternating current.
b. The thorax is the most common site of contact with an AC electric source.
c. The higher the resistance of a tissue to the flow of current, the less likely is transformation of
electrical energy to thermal energy.
d. Tissue resistance remains constant throughout length of exposure to current.
e. Tetany occurs when muscle fibers are stimulated at 40 to 110 cycles per second.
611. A “kissing burn” occurs:
a. at extensor surfaces in electrical exposure when the current causes flexion at a joint, protecting
that area but leaving the exposed extensor surfaces at greater risk for damage.
b. at flexor surfaces in electrical exposure when the current causes flexion at a joint, and the
moisture in the flexor crease leads to an arc burn and extensive deep tissue damage.
c. when a child “sucks” an electrical outlet.
d. when a child bites an electrical cord.
e. when lightning “kisses” the skin, leaving a typical fernlike pattern.
612. The paramedics are calling for medical command. They are on their way to a local golf
course where a tournament was interrupted by an unexpected thunderstorm. Their initial
report from the scene says there are 10 victims of a lightning strike, two of whom are
apparently dead, with no signs of breathing or heartbeat. Three victims are comatose but
breathing, and another was reported to be seizing but is now awake and confused. The
other four have flash burns and thermal burns where their clothing caught fire, but these
fires have been extinguished. You tell the medics that they should:
a. be careful when approaching these victims, as they may still be electrically charged.
b. treat the comatose victims first, just as in any mass casualty situation.
c. treat the apparently dead victims first, as there is a good chance they can be resuscitated.
d. bring the seizure patient first, as he will require rapid loading with phenytoin or fosphenytoin in
order to avoid going into status epilepticus.
e. preemptively countershock the comatose patients before they go into fibrillation.
613. Many victims of electrical injury have extensive burns. Their intravenous fluid needs
should be calculated by:
a. using the Parkland formula.
b. using the Brooke formula.
c. using the Edison formula.
d. serial BUN and creatinine.
e. maintaining urine output of 1 ml/kg/hr or greater.
191
609. e
th
Rosen 5 ,
Chapter 135,
p. 2007
610. e
Rosen 5th,
Chapter 136,
p. 2010
611. b
Rosen 5th,
Chapter 136,
p. 2014
612. c
Rosen 5th,
Chapter 136,
p. 2016
613. e
Rosen 5th,
Chapter 136,
p. 2017
Hypotension is common in heat stroke and is usually caused by peripheral vasodilation
resulting in high-output cardiac failure, in addition to dehydration. Blood pressure
usually rises with cooling. If this does not occur, or if the patient monitored invasively
has a low central venous or pulmonary capillary wedge pressure, a fluid challenge of
250 to 500 ml of 0.9% saline should be given rapidly. The use of alpha-adrenergic
agents such as norepinephrine is not recommended because they promote
vasoconstriction without improving cardiac output or perfusion, decrease cutaneous
heat exchange, and may enhance ischemic renal and hepatic damage. The role of
isoproterenol, dopamine, or dobutamine is unclear. Atropine and other anticholinergic
drugs that inhibit sweating should be avoided.
Alternating current exposure to the same voltage tends to be three times more
dangerous than direct current. Continuous muscle contraction, or tetany, can occur
when the muscle fibers are stimulated at between 40 and 110 times per second.
Electrical transmission frequency used in the United States is 60 cycles per second.
The hand is the most common site of contact via a tool that is in contact with an AC
electric source. The higher the resistance of a tissue to the flow of current, the greater
the potential for transformation of electrical energy to thermal energy at any given
current. As the tissue breaks down under the energy of the current flow, its resistance
may change markedly, making it difficult to predict the amperage for any given
electrical injury.
A peculiar type of burn associated with electrical injury is the “kissing burn,” which
occurs at the flexor creases. As the current causes flexion of the extremity, the skin of
the flexor surfaces at the joints touches. Combined with the moist environment that
often occurs at the flexor areas, the electric current may arc across the flexor crease,
causing arc burns on both flexor surfaces and extensive underlying tissue damage.
Traditional rules of mass casualty triage do not apply to lightning victims. In the
absence of cardiopulmonary arrest, victims are highly unlikely to die of any other
cause. Thus triage of lightning victims should concentrate on those who appear to be
in cardiorespiratory arrest. Cardiopulmonary resuscitation should be started on those
who have no pulse or respirations. When multiple victims are involved, the evaluation
of those who are breathing may be delayed because they are likely to survive the
incident.
Fluids should be administered at a rate sufficient to maintain a urine output of at least
0.5 to 1.0 ml/kg/hr in the absence of heme pigment in the urine and 1.0 to 1.5 ml/kg/hr
in its presence.
192
614. The mother of this 2-year-old boy heard him crying and
found him with this lesion. You find no other sign of
injury, and the child is hemodynamically stable. You
have consulted the oral surgeon and the trauma
surgeon. The child easily takes liquids, and he stops
crying after an appropriate dose of acetaminophen with
codeine. Appropriate disposition would be to:
a. admit to a monitor bed.
b. admit to a burn center.
c. admit to a floor bed for observation.
d. discharge home with careful instructions to parents.
e. 12-hour overnight observation in Emergency Department or Short-Stay Unit.
615. Which statement is true concerning dysbarism?
a. A diver needs to descend only 33 feet in seawater to double the atmospheric pressure.
b. Barotrauma of ascent is also called “squeeze.”
c. If a diver ascends too rapidly to the surface, carbon dioxide comes out of solution, forming gas
bubbles in the tissues and blood.
d. The greatest risk for barotrauma is in deep water.
e. The solubility of gases is affected by temperature: the lower the temperature, the lower the
solubility.
616. The most common medical complaint of SCUBA divers is:
a. the bends.
b. inner ear squeeze.
c. middle ear squeeze.
d. nitrogen narcosis.
e. swimmer’s ear.
617. External ear barotrauma:
a. occurs during ascent if water is trapped in the external auditory canal, causing a relative positive
pressure.
b. is more common than middle ear barotrauma.
c. is diagnosed clinically, as there are no physical findings.
d. can be prevented by use of earplugs or a tight fitting wetsuit hood.
e. becomes painful as the tympanic membrane bulges outward.
618. The most severe form of pulmonary over-pressurization syndrome (POPS) is:
a. alveolar hemorrhage.
b. arterial gas embolism.
c. pneumomediastinum.
d. pneumothorax.
e. subcutaneous emphysema.
619. The most important physiologic change occurring during high-altitude acclimatization is:
a. compensatory tachycardia and hypertension.
b. diminished pulmonary compliance and resistance.
c. increased hemoglobin.
d. increased minute ventilation.
e. renal excretion of bicarbonate.
193
614. d
th
Rosen 5 ,
Chapter 136,
2018
615. a
Rosen 5th,
Chapter 137,
p. 2021
616. c
Rosen 5th,
Chapter 137,
p. 2022
617. e
Rosen 5th,
Chapter 137,
p. 2022
618. a
Rosen 5th,
Chapter 137,
p. 2025
619. d
Rosen 5th,
Chapter 138,
p. 2036
Pediatric patients with oral burns may generally be safely discharged if close adult care
is assured. There is no evidence that an isolated oral burn correlates with cardiac
injury or myoglobinuria. In general, these patients require surgical and dental
consultation for oral splinting, eventual debridement, and occasionally reconstructive
surgery. After appropriate consultation, if hospitalization is not deemed necessary, the
child’s parents should be warned about the possibility of delayed hemorrhage and
receive instructions to apply direct pressure by pinching the bleeding site and to
immediately return to the ED.
Although a mountain climber would need to ascend to 18,000 feet to reduce
atmospheric pressure by 50%, a diver needs to descend only 33 feet in seawater to
double atmospheric pressure. The solubility of gases is affected by temperature: the
lower the temperature, the higher the solubility. Barotrauma results when a diver is
unable to equalize the pressure within air-filled structures to the ambient pressure of
the environment during ascent or descent. Proportionally, changes in volume are
greater as a diver approaches the surface. Thus, the greatest risk for barotrauma is in
shallow water. Barotrauma of descent, or “squeeze,” as it is known in common diving
parlance, results from the compression of gas in enclosed spaces as ambient pressure
increases with underwater descent. If a diver ascends too rapidly to the surface,
nitrogen comes out of solution, forming gas bubbles in the tissues and blood.
Middle ear barotrauma, (barotitis or “ear squeeze,”) is the most common complaint of
scuba divers, experienced by 30% of novice scuba divers and 10% of experienced
divers. The middle ear is an air-filled space with solid bony walls except for the
tympanic membrane. The Eustachian tube is the only anatomic passage to the external
environment. As the diver descends, each foot of water exerts an additional 23 mmHg
pressure against the intact tympanic membrane. Ear squeeze occurs when a negative
differential pressure is created within the middle ear because the diver could not
“equalize” to ambient pressure, leading to pain. If equilibration of middle ear pressure
does not occur, the floppy medial third of the Eustachian tube collapses shut, making
any further attempts at equalization futile. Further pressure increases can cause the
TM to rupture.
When a diver is submerged, the external ear canal usually fills with water. If the
external ear canal is occluded (e.g., by cerumen, foreign bodies, exostoses, or
earplugs), water entry is prevented, and compression of the enclosed air with descent
will have to be compensated for by tissue collapse, outward bulging of the tympanic
membrane, or hemorrhage. This is typically manifested by pain or bloody otorrhea.
The most severe form of POPS is arterial gas embolism. AGE is the second leading
cause of mortality of sport divers after drowning, accounting for approximately 30% of
diving-related deaths. Typically it results when air bubbles are forced across the
alveolar-capillary membrane, escape into the pulmonary venous circulation, and
proceed through the left atrium and ventricle and into the arterial circulation. Clinical
symptoms and signs are in part the result of mechanical obstruction by gas bubbles.
AGE can also result from a right-to-left shunt of venous bubbles, such as in a diver
with a PFO.
The most important physiologic change that occurs during acclimatization to high
altitudes is an increase in minute ventilation, causing a decrease in the partial pressure
of carbon dioxide in arterial gas (PaCO2). The alveolar gas equation states that, as the
PaCO2 decreases, a corresponding increase in PaO2 occurs, thereby increasing arterial
oxygenation. Thus the level of ventilation determines alveolar oxygen for a given
inspired oxygen tension.
194
620. You are practicing in an emergency department near an international airport. A 23-yearold woman has just flown back from the Caribbean, where she had gone on her
honeymoon. Despite the signs posted at the resort, she took “one last dive” an hour
before going to the airport. When she got off the airplane, she complained of limb
weakness, paresthesias, numbness, and low back and abdominal pain. The leg
symptoms started on the flight as a distal prickly sensation that advanced proximally,
followed by progressive sensory or motor loss. You suspect Type II decompression
sickness. You also know:
a. ground ambulance to a hyperbaric facility is the preferred method of transportation; air
transportation must be avoided.
b. hyperbaric treatment must start within 12 hours or it will not be beneficial.
c. if she’s pregnant, decompression sickness should not affect the developing fetus.
d. more than half of all decompression sickness patients have delayed symptoms occurring 12 or
more hours after surfacing.
e. the goals of recompression therapy are to reduce the washout of nitrogen by decreasing the tissueblood nitrogen gradient, and to increase oxygen delivery to ischemic tissue.
621. Concerning the epidemiology of acute mountain sickness:
a. high-altitude illness is uncommon under 10,000 feet, even with rapid ascent.
b. most serious altitude illness occurs above 18,000 feet.
c. above 18,000 feet, complete acclimatization takes 50% longer than acclimatization at 12,000 feet.
d. the partial pressure of oxygen in the atmosphere decreases as altitude rises, but remains a constant
20.93% of the barometric pressure.
e. it has been well-demonstrated that children have a lower incidence of acute mountain sickness
than adults.
622. The most common fatal manifestation of severe high-altitude illness is:
a. high-altitude cerebral edema.
b. high-altitude pulmonary edema.
c. acute mountain sickness.
d. pulmonary embolism.
e. dehydration.
623. In high-altitude pulmonary edema (HAPE):
a. most cases occur within 24 hours of ascent.
b. marked dyspnea on exertion, fatigue with minimal to moderate effort, and dry cough are early
manifestations.
c. the symptoms of AMS preclude the development of HAPE.
d. paradoxically, the lungs remain clear to auscultation until the end stages of the condition.
e. hypothermia is a common finding.
624. The most effective therapy for high-altitude pulmonary edema is:
a. acetazolamide.
b. descent, rest, and oxygen.
c. dexamethasone.
d. furosemide.
e. morphine sulfate.
195
619. a
th
Rosen 5 ,
Chapter 137,
p. 2028
620. d
Rosen 5th,
Chapter 138,
p. 2035
622. b
Rosen 5th,
Chapter 138,
p. 2042
623. b
th
Rosen 5 ,
Chapter 138,
p. 2042
624. b
Rosen 5th,
Chapter 138,
p. 2043
Ground transport to a hyperbaric facility is preferred over air transportation, if at all
feasible, as an increase in altitude will lower the ambient pressure and allow
microbubbles to expand. The goals of recompression therapy are to reduce the
mechanical obstruction of air bubbles, to facilitate the washout of nitrogen by
increasing the tissue-blood nitrogen gradient, and to increase oxygen delivery to
ischemic tissue. More than half of all DCS patients will become symptomatic in the
first hour after surfacing, with most of the rest experiencing symptoms within six
hours. DCS may be particularly dangerous to a developing fetus in the womb of a
scuba diving mother because the majority of fetal circulation bypasses the pulmonary
bed through the foramen ovale and the ductus arteriosis. Patients can obtain some
benefit from recompression even if treatment is initiated more than 24 hours after the
dive.
High-altitude illness is common with rapid ascent above 8200 feet. Most serious
altitude illness occurs between 10,000 and 18,000 feet. Above 18,000 feet, complete
acclimatization generally is not possible and long visits above this level result in
progressive deterioration. The partial pressure of oxygen (PO2) in the atmosphere also
decreases as altitude rises, but it remains a constant 20.93% of the barometric pressure.
Limited data suggest that children probably have the same incidence of acute mountain
sickness as adults.
High-altitude pulmonary edema is the most common fatal manifestation of severe
high-altitude illness.
The initial symptoms of HAPE usually begin insidiously 2 to 4 days after arrival at
high altitude. Most cases occur during the second night, but HAPE may develop
rapidly, with early symptoms apparent after just a few hours at high altitude. Marked
dyspnea on exertion, fatigue with minimal to moderate effort, and dry cough are early
manifestations of the disease. These symptoms may be subtle but noticeable when
comparing the victim with others in the group. The symptoms of AMS usually occur
concurrently with the development of HAPE. The physical examination reveals a few
rales in mild HAPE usually found in the region of the right middle lobe, progressing to
unilateral or bilateral rales, then diffuse bilateral rales and audible rhonchi and gurgles
that can be heard without the stethoscope. Elevated temperatures are common.
If HAPE is recognized early and treated properly, death usually can be avoided.
Descent to a lower altitude, bed rest, and supplemental oxygen are the most effective
methods of therapy.
196
625. The most sensitive physical finding for the recognition of high-altitude cerebral edema is:
a. cerebellar ataxia.
b. inability to do reverse serial sevens.
c. loss of deep tendon reflexes.
d. nystagmus.
e. tinnitus.
626. When considering victims of drowning or near-drowning:
a. freshwater immersion leads to hypotonicity in a majority of victims.
b. salt water immersion leads to hypertonicity in a majority of victims.
c. most near-drowning victims require therapy for electrolyte abnormalities.
d. cerebral hypoxia is the final common pathway in all drowning victims.
e. All of the above statements are true.
627. It is now known that the most important factor(s) to correct in treating the near-drowning
victim is/are:
a. acidosis and volume overload.
b. blood volume and tonicity.
c. cardiovascular function.
d. pulmonary injury and hypoxia.
e. serum electrolyte concentrations.
628. A 25-year-old man was pulled comatose from the bottom of a private swimming pool.
Immersion time was unknown. His pupils were dilated, and his breathing was agonal.
CPR was initiated at the scene, and the paramedics intubated him at once. On arrival in
the Emergency Department his heart rate is 42 and his blood pressure palpable at 66
mmHg. You know that:
a. he will be hyperkalemic because of hypotonic cell lysis.
b. he will have dilutional hypokalemia.
c. he will have dilutional hyponatremia.
d. he will have dilutional anemia.
e. his odds of surviving neurologically intact are higher than his odds of dying.
629. Optimal treatment for patients with hypoxemic brain injury after near-drowning includes:
a. barbiturate coma.
b. continuous positive airway pressure
c. corticosteroids.
d. hypothermia.
e. neuromuscular blockade.
630. A three-year-old boy was pulled from an icy river. His estimated time underwater was 15
minutes. He is without spontaneous vital signs, but you know that there is a chance for
recovery. Aggressive measures are instituted and should be maintained until:
a. barbiturate coma is induced
b. core temperature reaches 30° to 35°C.
c. emergent dialysis is arranged.
d. high-dose steroids are give intravenously.
e. naloxone has been administered.
197
625. a
th
Rosen 5 ,
Chapter 138,
p. 2045
626. d
th
Rosen 5 ,
Chapter 139,
p. 2051
627. d
Rosen 5th,
Chapter 139,
p. 2052
628. e
Rosen 5th,
Chapter 139,
p. 2052
629. e
Rosen 5th,
Chapter 139,
p. 2054
630. b
Rosen 5th,
Chapter 139,
p. 2054
The finding of cerebellar ataxia is the most sensitive test for early recognition of
HACE. This early appearance of ataxia reflects the particular sensitivity of the
cerebellum to hypoxia. Ataxia alone is an indication for immediate descent.
Pathophysiologic differences between freshwater and seawater aspirations have
traditionally been emphasized. In freshwater aspiration, hypotonic fluid passes
through the lungs into the pulmonary and systemic vasculature. Blood volume
increases within 3 to 4 minutes after aspiration, and the concentrations of most serum
electrolytes decrease. A rise in the serum potassium level may occur from the lysis of
red blood cells as a result of the effects of hypotonic freshwater or hypoxemia.
Conversely, aspirated saltwater, which is 3 to 4 times more concentrated than plasma,
leads to the development of an osmotic gradient across the alveolar membrane;
protein-rich fluid from the capillaries moves into the alveoli and interstitium, leading
to pulmonary edema. Blood volume decreases, and serum electrolyte concentrations
increase. Although these differences are demonstrated in experimental animal studies,
most victims of drowning or near-drowning do not aspirate enough fluid to cause lifethreatening changes in blood volume or serum electrolyte concentrations.
The early literature on submersion incidents emphasized changes in serum electrolyte
concentrations, blood volume, and cardiovascular function. It is now clear that
pulmonary injury and hypoxia are the factors of primary importance in the neardrowning victim. The CNS injury seen in near-drowning victims is also a hypoxicischemic event. Acidosis is often a prominent feature, developing from
hypoventilation, hypoxia, and poor perfusion.
Of near-drowning victims who are comatose, 44% survive neurologically intact, 17%
to 24% survive with severe neurologic damage, and 27% to 39% die. Decreased serum
bicarbonate is common and indicates tissue hypoxia (as well as elevated lactic acid
levels). The other electrolytes are usually normal on presentation. Similarly, the
complete blood count levels are often normal, with the exception of leukocytosis.
The optimal treatment for patients with anoxic brain injury remains unclear. The
classic protocol of neuromuscular blockade, barbiturate coma, dehydration,
hyperventilation, hypothermia, and corticosteroids (HYPER therapy), has been
abandoned because it did not demonstrate improved outcomes. Supportive care
without barbiturates, steroids, induced hypothermia, routine intracranial pressure
monitoring, or muscle paralysis is the standard in many intensive care centers.
The safest guideline is to continue resuscitation efforts until the core temperature
reaches 30° to 35°C. Cerebral death cannot be accurately diagnosed in the
hypothermic patient with core temperatures below this level.
198
631. Africanized honeybees (“killer” bees) cause fatalities because of:
a. aggressiveness of the swarms, leading to multiple stings.
b. increased human sensitivity to the venom.
c. increased venom toxicity.
d. the relative insensitivity of its victims to epinephrine (adrenalin).
e. their propensity to sting near the face and throat, leading to rapid airway compromise.
632. The insect from the hymenoptera family with the most dangerous venom is thought to be
the:
a. fire ant (Solenopsis invicta).
b. honey bee (Apis mellifera).
c. hornet (Vespula maculata).
d. wasp (Chlorion ichneumerea).
e. yellow jacket (Vespula maculiforma).
633. Dapsone may be helpful in the management of the local effects of envenomation by the:
a. black widow spider.
b. brown recluse spider.
c. fire ant.
d. golden orb weaver spider.
e. pickled herring.
634. Care of a presumed black widow spider bite in a stable, asymptomatic ED patient
includes:
a. broad spectrum antibiotics including anaerobic coverage
b. immediate admission to an intensive care unit.
c. incision and drainage at the site.
d. intermittent tourniquet application proximal to the site.
e. tetanus immunization.
635. A 4-year-old child started screaming after tried to pet his mother’s boyfriend’s pet
tarantula. He has probably been exposed to this arthropod’s:
a. alkali saliva in the eye, as the beast is an excellent spitter.
b. cardiotoxin through a sting.
c. irritating abdominal hairs, which the creature can throw several feet like a javelin.
d. neurotoxin through a bite.
e. pinchers.
636. The part of the United States with the highest reported incidence of venomous snake bites
is the:
a. Midwest.
b. Northeast.
c. Northwest.
d. South.
e. West Coast.
637. In using antivenin to treat the victim of snakebite, it is important to remember that:
a. dosing is weight-based.
b. if intravenous access cannot be obtained, the antivenin can be given intramuscularly.
c. pregnancy is a contraindication.
d. the first vial should be injected around the site of envenomation.
199
e. the need for doses beyond the first several vials is based on clinical response.
200
631. a
th
Rosen 5 ,
Chapter 55,
p. 793
632. b
Rosen 5th,
Chapter 55,
p. 793
633. b
Rosen 5th,
Chapter 55,
p. 796
634. c
Rosen 5th,
Chapter 55,
p.794
635. c
Rosen 5th,
Chapter 55,
p. 796
636. d
Rosen 5th,
Chapter 55,
p. 787
637. e
th
Rosen 5 ,
Chapter 55,
p. 791
Envenomations from these aggressive arthropods are most dangerous to very young or
elderly patients and those with concomitant medical conditions. Killer bees have
colonized northern Mexico and now have moved into the southern United States,
including California, Arizona, and Texas, where the mean high temperatures are at
least 60° F. This type of bee is not more toxic, only more aggressive.
The signs and symptoms of bee and wasp stings vary, depending on the degree, type,
and location of envenomation as well as the characteristics of the victim. Bee and
wasp venom can cause serious injuries other than allergic types of reactions, depending
on the number of stings, the species of insect, the size and previous health of the
victim, and the anatomic area stung. For example, a sting in the tongue or throat may
quickly compromise the airway. Honeybee venom causes a much greater release of
histamine per gram than other hymenopteran venom and thus is more dangerous.
Certain species of honeybee release a pheromone, isoamylacetate, when the ovipositor
is pulled from the abdomen after stinging a victim. This pheromone attracts other bees
to the victim and thus incites multiple stings.
Dapsone, 50 to 200 mg/day, has been shown to be helpful in preventing the local
effects of the venom. However, dapsone may cause methemoglobinemia and
hemolysis in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency.
Hyperbaric oxygen has been shown to decrease lesion size in animals. Analgesics and
antibiotics should be used as indicated during the course of the disease, although
infection is not common.
The ED care consists of obtaining a history of the circumstances surrounding the bite, a
description of the appearance of the spider, any significant past medical history,
medications, and allergies to insect bites, horses, or horse serum. The wound site
should be inspected for fang marks and cleansed with soap and water. Tetanus
immunization should be instituted. The patient should be observed for about 4 hours.
If the patient does not develop any symptoms and the spider was not positively
identified as a black widow, the patient may be discharged with instructions to return
to the ED if any symptoms develop.
Tarantulas are popular pets in the United States, and most native species are relatively
nontoxic. Tarantulas are unusual in that the abdominal hairs can be thrown by the
spider and embedded in human skin and the eye. These hairs can cause allergic
reactions and severe conjunctivitis and must be removed. A recent import from
Thailand, the cobalt blue tarantula, Haplopelma lividum, is a very aggressive spider
with a toxic venom.
The incidence of reported venomous snakebites is greatest in the southern United
States, which has the largest number of venomous snakes. States having the highest
death rates were North Carolina, Arkansas, Texas, and Georgia.
The smaller the body of the patient, the larger is the relative initial dose required; a
bitten child usually receives more venom in proportion to body weight and thus
requires more antivenin to neutralize it. All antivenin should be given intravenously.
Pregnancy is not a contraindication to antivenin therapy. Administration of antivenin
at or around the site of the bite is not recommended. The need for subsequent doses is
based on the clinical response.
201
638. The greatest number of envenomations by marine animals are caused by the:
a. cephalopods, like the blue-ringed octopus.
b. coelenterates, like the Portuguese man-of-war.
c. gastropods, like coneshells and nudibranches.
d. echinoderms, like starfish and sea urchins.
e. scorpaenidae, like the zebrafish and stonefish.
639. 5% acetic acid (vinegar) is used to neutralize nematocysts from the marine animal:
a. box jellyfish
b. saltwater catfish.
c. sea urchin.
d. stingray.
e. zebrafish.
640. The symptom most consistently associated with pit viper bites is:
a. anaphylaxis.
b. compartment syndrome.
c. immediate burning pain
d. petechiae.
e. purpura.
641. A 35-year-old woman was intoxicated at a picnic and passed out in a mound of fire ants.
She has evidence of hundreds of bites, including in her ear canals. Treatment consists of:
a. a bicarbonate slurry to neutralize the ant acid.
b. high-dose steroids.
c. intubation and barbiturate coma for 24-hours until the pain has subsided.
d. symptomatic care.
e. warm soaks to neutralize the heat-labile toxin.
642. Narcotic analgesics should not be used when treating the sting from a:
a. Africanized killer bee.
b. bark scorpion.
c. Portuguese man-of-war.
d. puss caterpillar.
e. stingray.
643. When seeing a patient who has ingested poisonous mushrooms, you know that:
a. the earlier the symptoms start, the more likely an ingestion is lethal.
b. coprine-containing mushrooms like the “inky cap” can cause an Antabuse®-type reaction if
consumed with alcohol.
c. the majority of mushroom fatalities in the USA occur from ingesting gyromitrin-containing
mushrooms.
d. amatoxins are used as an abortifacient.
e. psilocybin is structurally related to phencyclidine (PCP).
202
638. b
th
Rosen 5 ,
Chapter 55,
p. 797
639. a
th
Rosen 5 ,
Chapter 55,
p. 799
640. c
th
Rosen 5 ,
Chapter 55,
p. 789
641. d
th
Rosen 5 ,
Chapter 55,
p. 793-794
642. b
th
Rosen 5 ,
Chapter 55,
p. 797
643. b
Rosen 5th,
Chapter 158,
p. 2203
Because of their large numbers, coelenterates account for the greatest number of
envenomations by marine animals. This includes the Portuguese man-o-war, true
jellyfish, fire corals, stinging hydroids, sea wasps, sea nettle, and anemones. Most of
these organisms are sessile, but some are free floating.
Nematocyst injuries are treated by first removing the nematocysts without allowing
them to discharge. Tentacles should be removed with a gloved hand or forceps. The
remaining nematocysts should be fixed by pouring vinegar over the wound area. Fresh
water should not be used because it may stimulate continued nematocyst discharge.
Immediate burning pain is characteristic of pit viper bites. This differentiates it from
other snakebites. Petechiae may occur, as well as anaphylaxis if there is an immune
response. These do not occur as consistently. Compartment syndrome has not been
reported despite severe edema.
Treatment of fire ant stings consists of local wound care. If there is evidence of
systemic reaction, give the usual treatment for anaphylaxis. Desensitization should be
directed to any person exhibiting a potentially life-threatening reaction to these
arthropods.
For Centruroides exilicauda (box scorpion) envenomations that occur in Arizona,
antivenin is available from the Antivenom Production Laboratory of Arizona State
University. Narcotic analgesics and barbiturates have been reported to increase the
toxic effects of the venom and should be avoided.
The “inky-cap” or “shaggy mane” contains coprine and can cause a typical disulfiram
reaction if washed down with alcohol. In general, if toxicity begins within 2 hours of
ingestion of a mushroom, the clinical course will most likely be benign. If symptoms
begin 6 hours or later after ingestion, however, in general the clinical course will be
more serious and potentially fatal. Nearly all fatalities in the United States occur from
the ingestion of the Amanita species (Amanita phalloides, Amanita virosa, and
Amanita verna). Amatoxin does not cross the placental barrier. Psilocybin is
structurally related to lysergic acid diethylamide (LSD).
203
644. Intractable seizures can occur after ingestion of:
a. aloe (Aloe barbadensis).
b. amanita phalloides.
c. Lily of the Valley (Convallaria majalis).
d. pyracantha (firethorn).
e. water hemlock (Cicuta maculata).
645. Physostigmine may be needed to treat the toxic effects of:
a. dieffenbachia (dumbcane).
b. jimsonweed (Datura stramonium).
c. poinsettia (Euphorbia pulcherrima).
d. pokeweed (Phytolacca americana).
e. fava beans and Chianti.
646. Patients who ingest large amounts of dieffenbachia experience symptoms of calcium
oxalate crystal ingestion, including:
a. burning and irritation of the mouth.
b. generalized urticaria.
c. hypertension and tachycardia.
d. hypotension and bradycardia.
e. vomiting and diarrhea.
647. The radiation that penetrates all layers of the body and is the primary cause of acute
radiation syndrome is:
a. alpha rays.
b. beta rays.
c. gamma rays.
d. neutrons.
e. photons.
648. You are evaluating a patient 48 hours after a major radiation injury. He had severe
nausea and vomiting, but is feeling better now. His absolute lymphocyte count is 1200,
about 50% of normal. He should be triaged to the:
a. "expectant" death group.
b. "impending" death group.
c. survival improbable group.
d. survival possible group.
e. survival probable group.
204
644. e
th
Rosen 5 ,
Chapter 158,
p. 2199
645. b
th
Rosen 5 ,
Chapter 158,
p. 2200
646. a
Rosen 5th,
Chapter 158,
p. 2200
647. c
Rosen 5th,
Chapter 140,
p. 2057
648. d
th
Rosen 5 ,
Chapter 140,
p. 2061
The water hemlock contains the neurotoxin cicutoxin. Seizure activity in severe
exposure occurs in the first hour after ingestion and has resulted in high fatality rates.
Jimsonweed's effects are most frequently seen when leaves are dried and smoked for
their hallucinogenic effects. Jimsonweed seeds contain potent anticholinergic agents,
and ingestion may result in the anticholinergic syndrome typified by fever, tachycardia,
thirst, urinary retention, decreased secretions, and mydriasis. For severe cases
physostigmine may be useful.
Dieffenbachia spp. has over 30 different species including the dumbcane, mother-inlaw’s tongue, dumb plant, and tuft root. Some of these names refer to the inability to
talk that can occur after biting into parts of this plant. Typically the mucous
membranes of the mouth are immediately affected with severe pain, swelling, and the
sensation of biting into glass. These effects are due to calcium oxalate crystals,
packaged into bundles known as raphides, which are found in cellular structures known
as idioblasts. These idioblasts also contain proteolytic enzymes that are ejected out of
the idioblasts with the oxalate crystals when plant parts are chewed. Treatment is
aimed at pain relief and local supportive measures, typified by eating ice cream.
Gamma rays are the form of radiation that penetrate tissues deeply and interact with
every layer of tissue. They are emitted from radioisotopes after beta decay, and are the
primary cause of the acute radiation syndrome.
The survival possible group includes those in whom nausea and vomiting are relatively
brief, lasting 24 to 48 hours, followed by an asymptomatic period. After the initial
symptoms, these patients exhibit thrombocytopenia, granulocytopenia, and
lymphopenia. The severity of these changes depends on individual susceptibility and
the level of the initial radiation dose. These patients should be admitted for fluid and
electrolyte therapy if vomiting is severe. Antiemetics may be given as needed for
nausea and vomiting, but they may be ineffective. Also, protective isolation
precautions are indicated, particularly if the absolute lymphocyte count at 48 hours is
lower than 1200 or 50% of the baseline value.
205
7.0 – Head, Ear, Eye, Nose and Throat Disorders
649. You are examining a 5 year-old girl who knocked out her two upper central incisors in a fall
at a local amusement park. She is visiting her aunt, who does not know whether these are
her primary teeth. You know that:
a. normal primary dentition consists of 12 mandibular and 12 maxillary teeth.
b. the upper central incisors are the first teeth to erupt at approximately 10 months of age
c. all primary teeth should be present by 3 years of age.
d. permanent dentition does not begin to erupt until 7 to 8 years of age.
e. incisors are the first permanent teeth to erupt.
650. Trismus is caused by irritation of the:
a. buccinator muscle.
b. external pterygoid muscle.
c. masseter muscle.
d. platysma muscle.
e. temporalis muscle.
651. A 64-year-old woman complains of fever, neck pain and swelling, and difficulty swallowing.
She has a toxic appearance, and her neck is thicken, red, and tender. The bacteria most
likely responsible for this infection is:
a. Bacteroides fragilis.
b. hemolytic streptococcus.
c. Klebsiella.
d. Pseudomonas aeruginosa.
e. Staphylococcus aureus.
652. A 29-year-old woman complains of a toothache. She is afebrile and there is no facial
swelling, but she has very poor dentition and evidence of gingivitis. You drain her
periapical abscesses and then prescribe:
a. cephalexin.
b. ciprofloxacin.
c. an antifungal.
d. tetracycline.
e. trimethoprim-sulfamethoxazole.
653. A 22-year-old college student complains of severe mouth pain three days after removal of
two impacted mandibular molars. She looks very uncomfortable, but has normal vital
signs. Her exam shows probable “dry sockets” (post-extraction alveolar osteitis). You can
offer her best relief of her symptoms by:
a. having her hold an ice cube on the socket.
b. packing the socket with gauze impregnated with penicillin.
c. packing the socket with gauze soaked in 4% lidocaine.
d. packing the socket with gauze soaked in eugenol (oil of cloves).
e. suturing the gum over the exposed socket.
206
649. d
th
Rosen 5
Chapter 65,
p. 892
650. c
Rosen 5th
Chapter 65,
p. 898
651. b
th
Rosen 5
Chapter 65,
p. 898
652. e
Rosen 5th
Chapter 65,
p. 898
653. d
Rosen 5th
Chapter 65,
p. 899
The normal primary or deciduous dentition consists of 10 mandibular and 10 maxillary
teeth. The primary dentition is important for mastication, cosmetics, growth, and
development and functions as a “physiologic space maintainer.” Starting at the midline
and moving posteriorly in any quadrant, the normal dentition consists of a central
incisor, lateral incisor, canine, and two primary molars. The lower central incisor is
the first tooth to erupt, at approximately 6 months of age; all primary teeth should be
present by 3 years of age. If not, further investigation for developmental or endocrine
abnormalities is warranted. The permanent dentition begins to erupt at approximately
5 to 6 years of age with the appearance of the first molar.
Any irritation of the internal pterygoid or masseter muscles results in trismus. Trismus
results in the ability to open the mouth only a few millimeters, limiting visualization of
the pharynx and making diagnosis of lateral or retropharyngeal space involvement
difficult.
Ludwig’s angina is a bilateral board-like swelling involving the submandibular,
submental, and sublingual spaces with elevation of the tongue. The most serious
immediate sequela is airway obstruction. A characteristic brawny induration is
present; there is no fluctuance for incision and drainage. Hemolytic streptococcus is
most commonly responsible for the infection, although a mixed staphylococcalstreptococcal flora is not uncommon, and both may lead to an overgrowth of anaerobic
gas-producing organisms, including Bacteroides fragilis.
Pain from a periodontal abscess or swelling of the gingiva occurs when food or pus
becomes trapped in a “pocket.” Treatment consists of a small conservative stab
incision at the most fluctuant point to establish drainage, saline rinses, and antibiotic
coverage. Using tetracycline for patients more than 8 years of age is preferable
because it provides better coverage for the gram-negative and anaerobic organisms
found in the gingival pocket.
Acute alveolar osteitis or dry socket may occur 3 to 4 days after an extraction. The
patient has a pain-free interval followed by sudden onset of excruciating pain
associated with a foul odor. The pathophysiology involves premature loss of the
healing blood clot from the socket with a localized infection of the bone. Treatment of
consists of an anesthetic nerve block, gentle irrigation of the socket, and packing the
socket with iodoform gauze saturated with a medicated dental paste such as “SedaDent,” or barely dampened with eugenol (oil of cloves), giving almost immediate
relief.
207
654. A 27-year-old homeless man complains of fever, malaise, bad breath, and a feeling of
“wooden” and loose teeth. You examine him and find submandibular and anterior cervical
chain nodes. You also expect him to:
a. be culture-negative for anaerobic organisms.
b. have petechiae elsewhere on his body.
c. have the worst lesions in the location shown and near the posterior molars.
d. not be toxic in appearance.
e. respond poorly to antibiotics, as this is a surgical condition.
655. A 12-year-old boy was accidentally struck in the mouth with a baseball bat and has a
“chipped tooth” (see picture). The missing fragment is soaking in milk. You gently wipe
the tooth with some dry gauze and see a drop of blood. You should now:
a. arrange urgent follow-up with dentist or endodontist.
b. pack the pocket with gauze impregnated with penicillin.
c. pack the pocket with gauze soaked in 4% lidocaine.
d. pack the pocket with gauze soaked in eugenol (oil of cloves).
e. glue the fragment back into place using cyanoacrylate glue.
656. A 32-year-old camper avulsed his upper medial incisors three hours ago when his hatchet
ricocheted into his mouth while he was setting up his tent. He put his teeth into his shirt
pocket, hiked out of the woods, and drove to see you. You need to:
a. gently rinse the teeth and reimplant them, as there is an excellent chance they will
“take.”
b. gently rinse the teeth and reimplant them, but refer the patient to an endodontist and
warn him that the teeth will probably not survive.
c. scrub the teeth thoroughly to remove tissue and contaminants, then reimplant them.
d. soak the teeth in a povidone-iodine solution (Betadine®) and call the dentist.
e. soak the teeth in normal saline and call the dentist.
657. Herpangina and hand-foot-and-mouth disease both:
a. are winter diseases.
b. improve rapidly with acyclovir.
c. are caused by Coxsackie virus group A.
d. can lead to overwhelming sepsis in the asplenic patient.
e. cause generalized lymphadenopathy.
658. A 26-year-old woman was yawning and now cannot close her mouth. You should:
a. consult oral surgery for surgical repair.
b. inject both temperomandibular joints with local anesthetic / steroid.
c. intubate to control the airway.
d. order Panorex® or Panellipse® radiograph.
e. reduce the dislocation, using conscious sedation if necessary.
659. A 47-year-old workman accidentally splashed an unknown chemical in his right eye. He
complains of a burning sensation and blurred vision. On arrival in the Emergency
Department your protocol calls for the triage nurse to:
a. check the pH; if acid, irrigate with a bicarbonate solution; if alkali, irrigate with boric acid
or another weak acid.
b. check visual acuity.
c. determine what chemical caused the injury and begin irrigation.
d. emergently consult ophthalmology.
208
e. immediately irrigate his eye with a liter of neutral solution.
209
654. c
th
Rosen 5
Chapter 65,
p. 898
655. a
Rosen 5th
Chapter 65,
p. 902
656. b
Rosen 5th
Chapter 65,
p. 903
657. c
Rosen 5th
Chapter 65,
p. 1830
658. e
Rosen 5th,
Chapter 65,
p. 906
659. e
Rosen 5th
Chapter 66,
p. 910
Acute necrotizing ulcerative gingivitis (ANUG) is a periodontal lesion in which
bacteria actually invade nonnecrotic tissue. ANUG lesions are commonly
accompanied by systemic manifestations of fever, malaise, and regional
lymphadenopathy. The lesions can involve any part of the gingiva but are more
common in the anterior incisor and posterior molar regions. Anaerobic bacteria such
as Treponema, Selenomonas, Fusobacterium, and Prevotella are uniformly identified.
Antibiotics provide dramatic relief within 24 hours, as do dilute (3%) hydrogen
peroxide rinses.
A drop of blood indicates a pulpal exposure, a true dental emergency (Ellis Class II or
III). A general dentist, pedodontist, or endodontist should be notified immediately if
possible, or follow-up instructed for the next working day. If no dentist is available, a
piece of moist cotton can be placed over the exposed pulp and covered with a piece of
dry foil or sealed with a temporary root canal sealant (e.g., Cavet).
It has been known since the mid-1960s that an avulsed tooth can be successfully
replanted if it is returned to its socket within 30 minutes of the avulsion. A 1% chance
of successful replantation is lost for every minute that the tooth is outside of its socket;
the worst situation is to allow the tooth to be transported in a dry medium. Storage in
plain water is not much better. Teeth that have been avulsed for longer than 30
minutes will invariably require endodontic therapy.
Herpangina is caused by coxsackievirus group A, types 1–6, 8, 10, and 22 most
commonly. Most commonly occurring in the summer and autumn, herpangina
presents with a sudden onset of high fever, sore throat, headache, and malaise followed
by eruption of oral vesicles 1 to 2 mm in size within 24 to 48 h. The disease lasts 7 to
10 days and is treated symptomatically. Coxsackievirus type A16, and occasionally
types A4, A5, A9, and A10, are associated with hand, foot, and mouth disease. Fever
is usually of short duration, and the disease lasts 5 to 8 days. Treatment is palliative.
Reduction may be attempted in closed anterior dislocations without fracture. Most
attempts are made easier with analgesia.
A short-acting intravenous muscle relaxant (e.g., midazolam) helps to decrease muscle
spasm. Appropriate airway and hemodynamic monitoring is required. A systemic
analgesic (e.g., narcotic) may also be considered. Conscious sedation has also been
used successfully.
Treatment should begin at the scene with immediate irrigation using copious amounts
of water. Irrigation should continue for at least 30 minutes before any attempt to
transport the patient to the hospital. Any particles should be removed from the
fornices using a cotton swab. Upon hospital arrival, irrigation should continue.
Topical anesthetics and manual lid retraction may be needed for proper irrigation.
Irrigation is needed until the pH of the tear film is neutral as tested by Nitrazine paper
dipped into the inferior conjunctival fornix.
210
660. An apprentice welder complains of foreign body sensation and severe photophobia in both
eyes, eight hours after finishing a full day of welding. He gets good pain relief from
instillation of tetracaine drops, and fluorescein-enhanced slit lamp exam shows diffuse
punctate keratitis. Appropriate treatment is:
a. systemic antibiotics, topical anesthetic drops, systemic steroids.
b. topical and oral antimicrobials for infection prophylaxis, topical anesthetic drops for pain
relief.
c. topical antimicrobials for infection prophylaxis, topical anesthetic drops for pain relief.
d. topical antimicrobials for infection prophylaxis, topical short-acting cycloplegics for pain
relief, oral narcotics for breakthrough pain.
e. topical antimicrobials for infection prophylaxis, topical steroid drops, oral narcotics for
pain relief.
661. The major short-term complication from hyphema is:
a. cataract.
b. hypopyon.
c. glaucoma.
d. rebleeding.
e. vitreous hemorrhage and “floaters.”
662. A 23-year-old gentleman had a disagreement with an under-employed boxer at a local
entertainment establishment. During their discussion, he became punched in the eye.
After visiting his lawyer, he came to the Emergency Department complaining of pain. You
find him to be photophobic, with a midposition, poorly reactive pupil. You choose to treat
him with:
a. acetazolamide orally.
b. beta-blocker eye drops.
c. homatropine methylbromide 5%.
d. pilocarpine 4% drops.
e. topical antibiotic and an eye patch, with rapid follow-up.
663. A college basketball player complains of double vision “just in my right eye” after he was
elbowed in the face during a scrimmage. You suspect:
a. cataract.
b. hyphema.
c. malingering.
d. stroke
e. subluxed lens.
664. Scleral rupture:
a. can occur with normal visual acuity.
b. causes a bulging anterior chamber.
c. is best diagnosed by gentle palpation of the globe.
d. is confirmed by a negative Seidel test.
e. occurs most frequently at the limbus and insertion points of extraocular muscles.
665. You are examining a teen-age girl who was struck in the left eye by a batted softball. She
tells you she saw “showers of sparks,” which have now resolved. You suspect a possible
retinal tear, which:
a. always causes diminished visual acuity.
b. can be diagnosed with direct ophthalmoscopy and a slit lamp.
211
c. causes anterior chamber cell and flare and a mid-position poorly reactive pupil.
d. requires urgent ophthalmologist follow-up for best results.
e. rarely involves the macula.
212
660. d
th
Rosen 5
Chapter 66,
p. 911
661. d
Rosen 5th
Chapter 66,
p. 913
662. c
Rosen 5th
Chapter 66,
p. 913
663. e
Rosen 5th
Chapter 66,
p. 913
664. e
th
Rosen 5
Chapter 66,
p. 913
665. d
Rosen 5th
Chapter 66,
p. 914
Ultraviolet light from sun lamps, tanning booths, high-altitude environments, or
welder’s arc results in direct corneal epithelial damage. After a latent period of 6 to 10
hours, patients develop a foreign body sensation, tearing, intense pain, photophobia,
and blepharospasm. Examination reveals decreased visual acuity, injected conjunctiva,
and diffuse punctate corneal lesions, often with a discrete lower border defining the
cornea protected by the inferior lid. Treatment consists of a short-acting cycloplegic
and a topical broad-spectrum antibiotic ointment. Eye patching may be used for
patient comfort on the more affected eye. Oral narcotics are commonly needed.
Patients should never be prescribed topical anesthetics because frequent use retards
healing and can lead to corneal ulcer formation. Patients should have ophthalmologic
follow-up in 24 hours.
The major complication of hyphema is rebleeding, which occurs after 2 to 5 days when
the initial clot retracts and loosens. Rebleeding is more common in those with visual
acuities of 20/200, initial hyphema covering more than one third of the anterior
chamber, medical attention delayed more than 1 day after injury, and elevated
intraocular pressure at the initial examination. Other complications include corneal
bloodstaining, acute or chronic glaucoma, and anterior or posterior synechia formation.
Blunt injury of the globe may contuse and inflame the iris and ciliary body, resulting in
ciliary spasm. Patients complain of photophobia and deep aching eye pain.
Examination reveals perilimbal conjunctival injection (ciliary flush), cells and flare in
the anterior chamber, and a small, poorly dilating pupil. These symptoms indicate
white blood cells and protein as a result of the inflammation. Treatment consists of
paralyzing the iris and ciliary body with a long-acting cycloplegic agent, such as
homatropine methylbromide 5%, given four times daily for 7 to 10 days. Prednisolone
acetate 1% may be given to help relieve the inflammation if there is no improvement
after 5 to 7 days, but should be avoided in patients with a corneal epithelial defect.
Resolution occurs within 1 week.
Patients complain of monocular diplopia or visual distortion with lens subluxation and
marked visual blurring with lens dislocation.
Blunt trauma causes scleral rupture by suddenly elevating intraocular pressure.
Ruptures are most common at the insertions of the intraocular muscles or at the limbus,
where the sclera is the thinnest. Clues to a ruptured globe or intraocular foreign body
include shallow anterior chamber, hyphema, irregular pupil, significant reduction in
preinjury visual acuity, and poor view of the optic nerve and posterior pole on direct
ophthalmoscopy. If aqueous humor is leaking from the corneal wound, it will appear
as streaming fluorescent dye surrounded by an orange pool of solution on slit-lamp
examination (Seidel test).
Tears and detachments from blunt trauma are common. Symptoms include floaters
from bleeding, “flashing lights” from stimulation of retinal neurons, and visual field
cuts or decreased visual acuity. Retinal tears or detachments do not cause pain.
Examination may reveal the hazy gray membrane of the retina billowing forward, but
many tears are peripherally located and not seen with direct ophthalmoscopy. Visual
acuity may be normal unless the macula is involved. Indirect ophthalmoscopy is
warranted if historic clues to the presence of retinal tears are present. Ophthalmologic
consultation is warranted in all cases of suspected or proven retinal detachment.
213
666. A good antibiotic eyedrop for a patient with bacterial conjunctivitis is:
a. gentamicin.
b. neomycin.
c. sulfacetamide.
d. trimethoprim + polymyxin b (Polytrim®).
e. erythromycin.
667. There is frequently confusion about the difference between periorbital and orbital cellulitis.
In a patient with orbital cellulitis,
a. a frequent cause is spread from sinus infection, especially the ethmoid sinuses.
b. high-dose steroids may be necessary.
c. the globe itself is not at risk.
d. the most likely cause is a gram-negative rod.
e. The infection usually starts as an allergic reaction to an insect bite.
668. Corneal abrasions associated with contact lens wear should be treated with:
a. fluoroquinolone ointment + patch.
b. patch + fluoroquinolone drops+ steroid drops.
c. patch + topical anesthetics + systemic antibiotics.
d. tobramycin ointment.
e. topical anesthetics + tobramycin drops.
669. Central retinal artery occlusion causes vision loss that is:
a. gradual and painful.
b. gradual and painless.
c. intermittent.
d. sudden and painful.
e. sudden and painless.
670. The most common ocular motor palsy involves the:
a. 2nd cranial nerve.
b. 3rd cranial nerve.
c. 4th cranial nerve.
d. 6th cranial nerve.
e. 8th cranial nerve.
671. The ophthalmologic condition considered to be a surgical emergency is:
a. hyphema.
b. hypopyon.
c. retrobulbar hemorrhage.
d. rust ring from metallic foreign body.
e. vitreous hemorrhage.
672. An indication that an eyelid laceration has penetrated the orbital septum is:
a. Bell’s phenomenon.
b. fat in the wound.
c. negative Seidel’s test.
d. ptosis.
e. subconjunctival hemorrhage.
214
666. d
th
Rosen 5
Chapter 66,
p. 917
667. a
Rosen 5th
Chapter 66,
p. 909
668. d
Rosen 5th
Chapter 66,
p. 920
669. e
Rosen 5th
Chapter 66,
p. 925
670. d
Rosen 5th
Chapter 66,
p. 925
671. c
Rosen 5th
Chapter 66,
p. 910
672. b
Rosen 5th
Chapter 66,
p. 915
Treatment of acute bacterial conjunctivitis includes warm compresses and topical
ophthalmic antibiotics. In uncomplicated acute bacterial conjunctivitis, topical
trimethoprim and polymyxin is a good initial selection. Neomycin ophthalmic
solutions should be avoided because of the high incidence of hypersensitivity
reactions. Medications should be continued for 7 days. Corticosteroids and eye
patching should be avoided.
Orbital cellulitis is an orbital infection; therefore it is deep to the orbital septum. This
is a serious ocular infection that has the potential to be life threatening.
Staphylococcus aureus is the most common pathogen; however, Haemophilus
influenzae should be considered in young children and mucormycosis in diabetics and
immunocompromised patients. Polymicrobial infection is common. Orbital extension
of paranasal sinus infection (especially ethmoid sinusitis) is the most frequent source.
Abrasions related to the wearing of soft contact lenses pose a risk of Pseudomonas
infection and likewise should not be patched. These patients should be treated with
tobramycin ointment QID, followed by a fluoroquinolone (Ciloxan®, Ocuflox®) drop
or tobramycin drop QID once the epithelial defect starts to close.
The first branch off the internal carotid artery is the ophthalmic artery, which supplies
the central retinal artery, which, in turn, provides the blood supply to the inner retina.
If the central retinal artery becomes occluded, the retina will infarct and become pale,
less transparent, and edematous.
The sixth cranial nerve has a long and tortuous course, and defects of this nerve are the
most commonly reported ocular motor palsies. Patients with sixth cranial nerve palsies
have an esotropia that is worsened by lateral gaze and will often turn their heads
laterally toward the paretic side to compensate. Sixth-nerve palsy is caused by a
variety of diseases. Aneurysm, vascular disease (diabetes, hypertension,
atherosclerosis), trauma, neoplasm, multiple sclerosis, meningitis, thyroid eye disease,
and increased intracranial pressure may all cause dysfunction.
An orbital hematoma or retrobulbar hemorrhage can occur after blunt trauma. It can
result in a significant elevation in intraorbital pressure within the enclosed space,
resulting in compression of the optic nerve and central retinal artery. Symptoms
include proptosis, visual loss, and increased intraocular pressure. Any compromise in
the retinal blood supply is an indication for emergent surgical decompression.
There is no subcutaneous fat in the eyelids themselves; protrusion of orbital fat into the
wound indicates penetration of the orbital septum. Ptosis indicates injury to the levator
muscle or aponeurosis of the upper lid. Subconjunctival hemorrhage results from
rupture of small subconjunctival vessels, and by itself is benign. Bell's phenomenon is
the normal upward rotation of the globe with reflex blinking. Seidel’s test to use to
check for globe rupture.
215
673. Middle ear aspirates from patients with bullous myringitis usually grow:
a. Chlamydia trachomatis.
b. Escherichia coli.
c. Mycoplasma pneumoniae.
d. nothing.
e. Streptococcus pneumoniae.
674. The most common complication of acute otitis media is:
a. bacteremia.
b. hearing loss.
c. mastoiditis.
d. meninigitis.
e. sinusitis.
675. The most common intracranial complication of acute otitis media is:
a. lateral venous sinus thrombosis.
b. encephalitis.
c. epidural abscess.
d. meningitis.
e. subdural abscess.
676. Otitis externa:
a. can be life-threatening in an immunocompromised patient.
b. can easily be confused with a Ramsay-Hunt syndrome.
c. can initially be treated using any mildly acid solution (boric acid, acetic acid, etc.).
d. is a disease of fall and winter.
e. is usually caused by streptococcus group A.
216
673. e
th
Rosen 5
Chapter 67,
p. 929
674. b
th
Rosen 5
Chapter 67,
p. 930
675. d
Rosen 5th
Chapter 67,
p. 930
676. a
th
Rosen 5
Chapter 67,
p. 931
Although we are taught to think about “atypical bacteria” in a patient with bullous
myringitis, middle ear aspirates in this condition usually grow S. pneumoniae and H.
influenzae. Mycoplasma pneumoniae is uncommon.
Hearing impairment is the most common complication in otitis media. Almost all
children with OM will have a temporary conductive hearing loss; sensorineural deficit
occurs less commonly, probably as a spread of infection through the round window.
This may contribute to the association of OM with decreased or delayed speech,
language, or cognitive development.
Meningitis is the most common intracranial complication, more from hematogenous
spread than direct invasion. The symptoms include headache, meningismus, fever,
nausea, emesis, irritability, lethargy, and altered mental status.
Necrotizing external otitis is an extremely aggressive form of otitis externa, which can
lead to invasive disease and death. The most common bacterial causes of external
otitis are Pseudomonas aeruginosa and S. aureus. It occurs most often in the summer
and is common in the tropics. Herpes zoster oticus, also known as the Ramsay Hunt
syndrome, is a viral manifestation of disease affecting the auricle, with resulting facial
paralysis that may involve multiple cranial nerves. Acetic acid possesses antibacterial
and antifungal properties that are more important than its acidifying properties.
217
8.0 – Hematologic Disorders
677. A patient with anemia, thrombocytopenia, renal failure, normal coagulation tests and a
clear sensorium probably has:
a. (ITP) idiopathic thrombocytopenic anemia.
b. (TTP) thrombotic thrombocytopenic purpura.
c. (HUS) hemolytic-uremic syndrome.
d. (DIC) disseminated intravascular coagulation.
e. autoimmune hemolytic anemia.
678. The viral agent implicated in an aplastic crisis of patients with sickle cell disease is:
a. adenovirus (atypical).
b. herpes simplex.
c. parvovirus.
d. coxsackie virus.
e. HTLV-IV.
679. The etiologic agent implicated in hemolytic uremic syndrome is:
a. giardia.
b. Escherichia coli O157:H7.
c. scombroid toxin.
d. atypical enterovirus / poliovirus.
e. Enteromoeba histolytica.
680. The most helpful lab study in diagnosing disseminated intravascular coagulation is the:
a. D-dimer, which is elevated.
b. partial thromboplastin time (PTT), which is decreased.
c. fibrinogen level, which is elevated.
d. prothrombin time, which is prolonged.
e. fibrin degradation products (FDP), which are diminished.
681. Hemolytic-uremic syndrome is most commonly seen in:
a. neonates.
b. infants and children 6 months to 4 years of age .
c. adolescents.
d. women age 30 to 50.
e. both sexes, over age 75.
682. The initial dose of factor VIII required for a 60-kg male with severe hemophilia A in whom
you suspect a ruptured spleen is:
a. 1,500 units
b. 2,850 units
c. 3,000 units
d. 6,000 units
e. 5,700 units
218
677. c
th
Rosen 5
Chapter 116,
p. 1692-1693
678. c
th
Rosen 5
Chapter 161,
p. 1823
679. b
Rosen 5th
Chapter 167,
p. 2341-2342
680. d
Rosen 5th
Chapter 116,
p. 1697-1698
Table 116-3
681. b
Rosen 5th
Chapter 167,
p. 2341
682. c
th
Rosen 5
Chapter 116,
p. 1695
ITP generally presents with isolated thrombocytopenia. TTP causes neurologic
symptoms in addition to the other symptoms. DIC will have abnormal coagulation
studies. Autoimmune hemolytic anemia may cause severe rapid anemia, which may
present with angina or congestive heart failure.
Aplastic crises can be precipitated by viral infections (particularly parvovirus B19),
folic acid deficiency, or the ingestion of bone marrow toxins such as phenylbutazone.
Bone marrow erythropoiesis is slowed or stopped. The hematocrit falls to as low as
10%, and the reticulocyte count falls to as low as 0.5%. The white blood cell count
and platelet counts usually remain stable.
In children, the development of HUS often follows a prodromal infectious disease,
usually diarrhea or an upper respiratory infection. Diarrhea, particularly that
associated with Escherichia coli serotype 0157:H7, as well as with Shigella, Yersinia,
Campylobacter, and Salmonella, may be antecedent.
MOST USEFUL:
HELPFUL:
Prothrombin time – prolonged Activated partial thromboplastin time – usually
Platelet count – usually low
prolonged
Fibrinogen level – low
Thrombin clot time – prolonged
Fragmented red blood cells – should be present
Fibrin degradation products and D-dimers – elevated
Hemolytic-uremic syndrome (HUS) is a disease mainly of infancy and early childhood,
with a peak incidence between 6 months and 4 years of age. Mean age at presentation
is 3 years, and it is rare after age 5 years.
A 60-kg patient with a life threatening hemorrhage who requires 100% correction will
need 50 mL/kg = 3000 units of factor VIII. Formula: FactorVIII (units) = Kg./2 X
Activity Desired
219
683. A 44-year-old woman with a history of TTP, in remission for 30 days, presents to the ED
complaining of lethargy. Laboratory results would likely show:
a. elevated LDH, elevated reticulocyte count, elevated red blood cell count.
b. elevated LDH, elevated reticulocyte count, elevated creatinine.
c. decreased platelet count, decreased red blood cell count, decreased reticulocyte count.
d. decreased platelet count, decreased reticulocyte count, decreased LDH.
e. none of the above.
684. A 54-year-old woman complains of back pain for several months. She now has two days
of urine and stool incontinence and ‘numbness’ when she wipes with toilet paper. You
suspect spinal cord compression, which:
a. commonly occurs as a presenting symptom in a patient with a previously unsuspected
malignancy.
b. is always associated with back pain, but not tenderness.
c. usually responds to aggressive chemotherapy.
d. usually causes asymmetric motor or sensory defects.
e. can usually be diagnosed by plain radiographs, with CT or MRI adding little.
685. In a patient with hemolytic anemia from any cause, you would expect to find:
a. decreased haptoglobin, increased LDH, increased indirect bilirubin, decreased reticulocytes.
b. decreased haptoglobin, increased LDH, increased indirect bilirubin, increased reticulocytes.
c. increased haptoglobin, decreased LDH, decreased indirect bilirubin, increased reticulocytes.
d. increased haptoglobin, increased LDH, increased direct bilirubin, increased reticulocytes.
e. increased haptoglobin, increased LDH, increased indirect bilirubin, increased reticulocyte.
686. You are evaluating a patient whom you suspect to be severely anemic. You know that:
a. pallor is present only with chronic anemia.
b. the RBC distribution width (RDW) is useful in differentiating iron deficiency anemia from
thalassemia.
c. purpura, petechiae, and jaundice usually indicate an acute anemia.
d. orthostasis represents a chronic anemia.
e. retinal hemorrhages indicate an acute anemia.
687. The most helpful laboratory study to differentiate poor red blood cell production from
increased red cell destruction is the:
a. sedimentation rate.
b. sideroblast level.
c. serum iron level.
d. total to direct bilirubin ratio.
e. reticulocyte count.
688. Choose the correct pairing.
a. hypochromic microcytic anemia – hypothyroidism
b. chronic disease – hyperchromic anemia
c. macrocytic anemia – lead poisoning
d. myelodysplastic anemia – cells may be large or normal size, seen in toxins and renal failure
e. megaloblastic anemia – impaired RNA synthesis
220
683. b
th
Rosen 5
Chapter 116,
p. 1693
684. a
Rosen 5th
Chapter 100,
p. 1504
685. d
Rosen 5th
Chapter 115,
p. 1676
686. b
Rosen 5th
Chapter 115,
p. 1667
687. e
Rosen 5th
Chapter 115,
p. 1665
688. d
Rosen 5th
Chapter 115,
p. 1667
Thrombotic thrombocytopenic purpura is classically seen as the constellation of
thrombocytopenic purpura, microangiopathic hemolytic anemia, fluctuating neurologic
symptoms, renal disease, and fever. However, only 40% of cases present with the
classic pentad. The platelet count ranges from 10,000/mm3 to 50,000/mm3, and
generalized purpura and bleeding complaints are common. Anemia is universal, with
hematocrit commonly less than 20%. The hemolysis may cause jaundice or pallor, and
the blood smear characteristically contains numerous schistocytes and fragmented red
blood cells.
Spinal cord tumors produce neurologic symptoms by compression, invasion, or
destruction of myelinated tracts. The resulting neurologic symptoms are directly
related to both the growth rate and location of the tumor. Most tumors of the spinal
cord are metastatic in origin. Approximately 5% to 10% of patients ultimately
diagnosed with cancer first present with a spinal metastasis. Most metastases occur in
the thoracic spine, and nearly 20% will have disease at multiple levels. In 95% of
patients with spinal neoplasm, the initial complaint is pain, either in the back at the
level of the tumor or in a radicular distribution. Nighttime pain that is severe is
characteristic of spinal neoplasm.
Haptoglobin binds hemoglobin on a molecule-for-molecule basis. Its absence implies
saturation and degradation after binding with hemoglobin and is an early finding in
hemolysis. It has a normal range of 40 to 180 mg/ml, is decreased in hepatic failure,
and increases as an acute-phase reactant. After haptoglobin is bound, hemoglobin
binds with hemopexin, transferrin, and albumin before circulating in its free form.
LDH is released when the RBC is broken down peripherally or in the marrow. It is
elevated in hemolytic, thalassemic, sideroblastic, and megaloblastic anemias. It may
also be seen in cases of uremia, polycythemia vera, and erythroleukemia. Bilirubin is
often delivered to the liver faster than the conjugating mechanism can handle it.
Conjugated or indirect bilirubin may rise as high as 4 to 5 mg/dl even with normal liver
function. Higher levels connote some degree of underlying hepatic insufficiency.
The RBC distribution width (RDW) is a measure of the homogenicity of the RBCs
measured. It is automatically calculated as the standard deviation of the MCV divided
by the MCV multiplied by 100. A normal RDW is 13.5% + 1.5%. It is useful in
differentiating iron deficiency from thalassemia.
The reticulocyte retains its ribosomal network for about 4 days, of which 3 are spent in
the bone marrow and 1 in the peripheral circulation. The red blood cell matures as the
reticulocyte loses its ribosomal network and circulates for 110 to 120 days. Under
steady state conditions, the rate of red blood cell production equals the rate of
destruction. Red blood cell mass remains constant as an equal number of reticulocytes
replace the destroyed, senescent erythrocytes during the same period.
RBC indices are useful in classifying production deficit anemias. The mean
corpuscular volume (MCV) is a measure of RBC size. Decreases and increases reflect
microcytosis and macrocytosis, respectively. The mean corpuscular hemoglobin
(MCH) value incorporates both the RBC size and hemoglobin concentration.
It is influenced by both and is the least helpful of the indices. The MCH concentration
is a measure of hemoglobin concentration (MCHC). Low values represent
hypochromia. High values are noted only when decreased cell membrane relative to
cell volume exists, such as in spherocytosis.
221
689. The most common inherited bleeding disorder is:
a. hemophilia A.
b. hemophilia B.
c. von Willebrand’s disease
d. hereditary DIC.
e. Christmas disease.
690. Your patient is profoundly anemic and you believe she would benefit from a blood
transfusion. In weighing the benefits against the risks, you tell her that the most common
adverse effect is:
a. hepatitis C transmission.
b. hepatitis B transmission.
c. human immunodeficiency virus (HIV) transmission.
d. febrile nonhemolytic reaction.
e. graft versus host reaction.
691. The anemia in adult sickle-cell disease is due to:
a. poor marrow production.
b. abnormal protein-binding capacity.
c. increased red-cell destruction.
d. overactive antibody-antigen response.
e. sequestration.
692. Long-term effects of sickle-cell disease can include:
a. strokes.
b. liver failure.
c. renal failure.
d. bone infarcts.
e. all of the above.
693. In a patient with sickle-cell disease, infectious crises are primarily due to:
a. leukopenia.
b. marrow shutdown.
c. poor antibody production.
d. functional asplenia.
e. antibiotic resistance.
694. A 12-year-old girl with sickle cell disease is brought by her mother after she passed out
twice. She was kept home from school the last few days for a “cold.” When you ask the
child to stand, you must catch her to prevent her from falling to the ground. This is
suspicious for:
a. salmonella sepsis.
b. sequestration crisis.
c. acute chest syndrome.
d. aplastic crisis.
e. hemolytic crisis.
695. In a patient with sickle cell disease who is having a typical vaso-occlusive crisis:
a. oral hydration is seldom sufficient.
b. jaundice is a sign of serious disease.
c. oxygen is always helpful.
222
d. exchange transfusions are becoming the treatment of choice.
e. morphine is preferred over meperidine as the pain medication of choice.
223
689. c
th
Rosen 5
Chapter 116,
p. 1697
690. d
th
Rosen 5
Chapter 5,
p. 50
691. c
Rosen 5th
Chapter 115,
p. 1678
692. e
Rosen 5th
Chapter 115,
p. 1679,
Table 115-7
693. d
th
Rosen 5
Chapter 115,
p. 1678-1679
694. b
Rosen 5th
Chapter 115,
p. 1678
695. e
Rosen 5th
Chapter 115,
p. 1679
Von Willebrand’s disease is the most common hereditary bleeding disorder, with an
estimated prevalence of 1%. The disease occurs in 5 to 10 persons per million
population as an autosomal dominant trait with a variable penetrance pattern. A rare
X-linked inheritance has been described.
This most common and least serious transfusion reaction is characterized by fever,
chills, and malaise. Reactions are frequently related to antileukocyte and antiplatelet
antibodies and seen in multiply transfused patients. Treatment is symptomatic with an
analgesic/antipyretic and an antihistamine. If recurrent febrile reactions occur in a
patient, leukocyte-poor RBCs (washed, frozen-thawed-deglycerolized, filtered) should
be considered. If a febrile reaction occurs in a first-time transfusion, it should be
treated the same as an extravascular hemolytic reaction until proved otherwise.
Although most of the diagnostic and therapeutic problems of sickle cell disease are
related to vasoocclusive crises, other serious complications must be anticipated. Sickle
cell disease is a chronic hemolytic state with reasonably compensated hematocrit
values in the 20% to 30% range and elevated reticulocyte counts. This compensated
balance may be disrupted by a rare iron deficiency or more commonly a folate
deficiency. A potentially life-threatening aplastic crisis may be seen with an acute
postinfectious or folate deficiency suppression of erythropoiesis. This aplastic
condition is suspected when the hemoglobin level falls 2 g/dl or more from previous
stable levels, and the reticulocyte count remains low (< 2%).
Long-term effects of sickle cell disease are protean and devastating. Space prohibits
listing them here.
Adults with fever require a careful evaluation and laboratory assessment, including
appropriate cultures. Early institution of appropriate antibiotics is necessary in those
patients with a discernible source of infection. In children and adults, Staphylococcus
and Pneumococcus species and Haemophilus influenzae are particularly common. An
increased incidence of Salmonella osteomyelitis also occurs. The origin of this related
immunologic deficiency is believed to be multifactorial, with functional asplenia,
poorly migrating neutrophils, and decreased opsonin production as contributors.
Children with sickle cell disease may have an acute splenic sequestration syndrome.
This syndrome involves acute splenic enlargement from increased intrasplenic sickling
and obstruction. The child may have lassitude and be in shock.
Present therapies are directed toward symptomatic relief and attempts to stop the cycle
of deoxygenated sickling and intravascular sludging. These include rest, adequate
nutrition, hydration, oxygenation, analgesia, transfusion, and therapy for infection.
Most patients with sickle cell anemia are mildly dehydrated because of urineconcentrating difficulties. Fluid replacement can be oral or IV. Oxygen through a
nasal cannula at 2 to 4 L/min may help hypoxic patients and may be given to any
patient with HbSS as a low-risk treatment modality with potential benefit. No standard
pain management exists for sickle cell disease. The most important aspect of pain
management in these patients is a consistent, thorough, and attentive approach that
offers true pain relief. Rarely, transfusions are given for control of bony or visceral
crises. This is not an ED procedure and is considered only after hematologic
consultation. Prophylactic transfusions to dilute HbS levels are also recommended in
pregnancy and before major surgery.
224
696. The laboratory tech calls to tell you that she sees Howell-Jolly bodies on the peripheral
smear of one of your patients. You tell her that you suspected as much, since the patient:
a. has a G6PD deficiency.
b. has a history of malaria.
c. is asplenic.
d. is HIV positive.
e. is named Howell and is very jolly.
697. Obstetric causes of disseminated intravascular coagulation (DIC) include:
a. placental abruption
b. amniotic fluid embolism
c. acute fatty liver of pregnancy
d. eclampsia
e. all of the above.
698. The cornerstone of Emergency Department management of DIC is:
a. hemodynamic stabilization and treatment of the underlying disorder.
b. rapid correction of thrombocytopenia.
c. aggressive resuscitation with colloid.
d. pan-culture and broad-spectrum antibiotic coverage.
e. rapid intubation and hyperventilation.
699. Heparin has selective use in the treatment of DIC when fibrin deposition and thrombosis
dominate the pathologic picture. An example of such a condition is:
a. meningococcemia.
b. purpura fulminans.
c. abruptio placentae.
d. severe liver disease.
e. trauma.
700. Heparin-induced thrombocytopenia:
a. does not occur with low molecular weight heparins.
b. requires a minimum number of units, so a heparin “flush” is always safe.
c. can paradoxically cause thrombosis, ischemia, and amputation.
d. never occurs during the first 24 hours of infusion.
e. is easily treated with warfarin and fresh-frozen plasma.
225
695. c
th
Rosen 5
Chapter 177,
p. 2500
697. e
th
Rosen 5
Chapter 175,
p. 2481
698. a
th
Rosen 5
Chapter 116,
p. 1698
699. b
th
Rosen 5
Chapter 116,
p. 1698
700. c
Rosen 5th
Chapter 116,
p. 1692
The presence of Howell-Jolly bodies on a peripheral blood smear indicates functional
or true absence of a spleen.
Events during pregnancy which can lead to disseminated intravascular coagulation
include placental abruption, amniotic fluid embolus, septic abortion, intrauterine fetal
death (chronic DIC); women can also get DIC in HELLP syndrome.
The goals of emergency care in cases of DIC include initial suspicion, aggressive
diagnostic pursuit, understanding of potential life-threatening complications, and only
rarely, initiation of therapy.
Heparin has selective use in the treatment of DIC when fibrin deposition and
thrombosis dominate the pathologic picture. Certain disease states are more associated
with fibrin deposition, in which case heparin therapy should be considered. Examples
include purpura fulminans, retained dead fetus before delivery, giant hemangioma, and
acute promyelocytic leukemia. Heparin therapy is of little benefit in cases of
meningococcemia, abruptio placentae, severe liver disease, and trauma. Low doses of
heparin (300 to 500 U/hour) as a continuous infusion are currently recommended.
Low-molecular-weight heparin may also be used instead of unfractionated heparin.
A number of drugs have been associated with thrombocytopenia of immunologic
origin. Because of its relatively high frequency, heparin is an important cause of druginduced thrombocytopenia in hospitalized patients. Platelets are activated by the
formation of an IgG-heparin complex. Low-molecular-weight heparin may be
associated with less thrombocytopenia than standard, unfractionated heparin; however,
both forms of heparin have cross-reactivity. Heparin-induced thrombocytopenia can
occasionally lead to the “white clot” syndrome, causing impaired peripheral
circulation, gangrene, and amputation.
226
9.0 – Immune System Disorders
701. An important step in the work-up of arthritis is determining whether it is monoarticular or
polyarticular. Classification by number of joints involved can help narrow the diagnosis. Which
pairing below is correct?
a. gout polyarticular arthritis
b. Lyme disease monoarticular arthritis
c. pseudogout polyarticular arthritis
d. Reiter’s syndrome monoarticular arthritis
e. rheumatoid disease polyarticular arthritis
702. A 22-year-old female with no prior medical history presents with joint pain and swelling. When
evaluating a patient with a complaint of nontraumatic joint pain, you know that:
a. arthritis in the first carpometacarpal joint implies rheumatoid disease.
b. bursitis causes a diffuse joint pain.
c. fever is unusual in a patient with arthritis which is not a septic joint.
d. gonococcal arthritis tends to cause migratory oligoarticular symptoms.
e. true arthritis causes pain on active motion, but not on passive motion.
703. In evaluating a patient with acute arthritis, which laboratory study may be of any value in
determining the underlying etiology?
a. CPK.
b. platelet count.
c. sedimentation rate.
d. serum protein level.
e. uric acid level.
704. A 38-year-old man complains of an isolated swollen knee joint. He is afebrile and nontoxic. After
appropriate explanation and preparation, you perform arthrocentesis and obtain 55 ml of somewhat
cloudy, straw-colored joint fluid. You know that:
a. absolute cell counts can be used to rule out a septic etiology.
b. arthrocentesis is contraindicated if infection of any kind covers the joint.
c. most of the WBCs in septic arthritis are PMNs, whereas eosinophils predominate in inflammatory
arthritis.
d. synovial fluid glucose, lactic acid, viscosity, mucin clot, and total protein can all help differentiate
the etiology of the arthritis.
e. two red-topped tubes should be sufficient for any studies which need to be done.
705. You suspect a patient may have rheumatoid arthritis, so you order an EKG, thinking that you might
find:
a. bigeminy.
b. left anterior hemiblock.
c. prolonged PR interval.
d. right ventricular hypertrophy.
e. shortened QT interval.
227
701. e
th
Rosen 5 ,
Chapter 110,
p. 1585
702. d
Rosen 5th,
Chapter 110,
p. 1585
703. c
Rosen 5th,
Chapter 110,
p. 1586
704. b
Rosen 5th,
Chapter 110,
p. 1587
705. c
Rosen 5th,
Chapter 110,
p. 1589
Of the listed arthritides, only pseudogout typically presents as monoarticular arthritis.
Other monoarticular arthritides are osteoarthritis, septic arthritis, and gout. In addition,
trauma and hemarthrosis usually produce monoarticular symptoms. Besides those
listed other diseases that produce polyarticular symptoms include rubella, rheumatic
fever, Reiter's syndrome, and serum sickness. See Table 110-1, page 1585.
Gonococcal arthritis tends to occur in two or three joints (oligoarticular). True arthritis
produces generalized joint pain, warmth, swelling, and tenderness. Discomfort
increases with both passive and active motion of the joint because the inflamed
synovium is exquisitely sensitive to stretching, and because all parts of the joint are
involved in the inflammatory process. Periarticular inflammation (bursitis, tendinitis,
or localized cellulitis) tends to be focal. Tenderness and swelling do not occur
uniformly across the joint, and pain is produced only with certain movements. Patients
with any inflammatory arthritis may have low-grade fever. The first carpometacarpal
joint is frequently involved in osteoarthritis
Laboratory tests other than synovial fluid analysis are of limited diagnostic value for
evaluating acute arthritis in the ED. The two most general screening tests are a
complete blood count and an erythrocyte sedimentation rate, which is elevated in
almost all cases of inflammatory arthritides. The serum uric acid level is not helpful in
diagnosing acute gouty arthritis; in the acute phase of the disease, the serum uric level
may be normal.
Emergent arthrocentesis is contraindicated if infection of any kind covers the area to be
punctured. Most of the WBCs in both septic and severe inflammatory arthritis are
PMNs. Prediction rules regarding cell count and the likelihood of septic arthritis are
common, but are in no way absolute, and cell counts should not be used to rule out a
septic etiology. Rather, bacterial cultures should be obtained if there is any suspicion
of infection. Other tests (i.e., synovial fluid glucose, lactic acid, viscosity, mucin clot,
and total protein) have limited utility in ruling out infection and are no longer routinely
recommended. Specimens for cellular analysis should be submitted in tubes with
ethylenediaminetetraacetic acid (EDTA) anticoagulant (lavender top), whereas
specimens for crystal analysis should be transported in tubes with liquid heparin (green
top). Chemical analysis, serology, and viscosity should be analyzed on fluid submitted
in a red top tube.
ECG is indicated for patients with arthritis who have a history of chest pain or
complaints that might be related to the heart, or physical examination findings of a new
or changing heart murmur, evidence of congestive heart failure, or cardiomegaly. In
carditis, prolongation of the P-R interval is the most common finding, and if
pericarditis is present, acute diffuse ST segment elevations may be noted.
228
706. The most common bacterial cause of septic arthritis is:
a. Gram negatives.
b. group A streptococcus.
c. Haemophilus influenzae.
d. Neisseria gonorrhoeae.
e. Staphylococcus aureus.
707. The joint which most frequently becomes septic is the:
a. ankle.
b. hip.
c. knee.
d. shoulder.
e. wrist.
708. Concerning the treatment of gout:
a. allopurinol increases uric acid elimination and is useful during an acute attack.
b. colchicine should not be used prophylactically.
c. if NSAIDs are contraindicated, intramuscular injections of ACTH are useful.
d. probenecid lowers uric acid by diminishing production.
e. response to colchicine is diagnostic for the disease.
709. Pseudogout differs from gout in that:
a. indomethacin is contraindicated.
b. the attack is more severe.
c. the crystals cannot be identified using microscopy.
d. the knee is the most commonly involved joint.
e. the typical patient is younger.
710. The two viruses that most commonly cause arthritis are:
a. coxsackievirus and hepatitis A.
b. Epstein Barr virus and enteroviruses.
c. hepatitis C and parvovirus.
d. mumps and adenoviruses.
e. rubella and hepatitis B.
711. The most common stool pathogen implicated in Reiter’s syndrome is:
a. Campylobacter spp.
b. Chlamydia trachomatis.
c. Salmonella typhi.
d. Shigella flexneri.
e. Yersinia enterocolitica.
229
706. e
th
Rosen 5 ,
Chapter 110,
p. 1590
707. c
Rosen 5th,
Chapter 110,
p. 1591
708. c
Rosen 5th,
Chapter 110,
p. 1592
709. d
Rosen 5th,
Chapter 110,
p. 1592
710. e
Rosen 5th,
Chapter 110,
p. 1593
711. d
Rosen 5th,
Chapter 110,
p. 1595
The microbiology of septic arthritis has remained fairly constant over time. Overall,
Staphylococcus aureus is still the most common cause of septic arthritis.
Staphylococci, streptococci, gram-negative organisms, and anaerobes in relatively
constant proportions cause the remaining cases of monoarthritis. N. gonorrhoeae
accounts for ~20% of cases of monoarticular septic arthritis, but it is a more common
pathogen in patients with polyarthritis, which is the usual presentation.
Typically, infectious arthritis affects a single joint, with the most common joints
infected being the knee (40% to 50%), hip (13% to 20%), shoulder (10% to 15%),
wrist (5% to 8%), ankle (6% to 8%), elbow (3% to 7%), and the small joints of the
hand or foot (5%). In approximately 20% of cases, several joints may be involved at
the same time. Even in septic polyarthritis, however, the knees are the most common
sites of infection.
Colchicine is effective for gout, pseudogout and other crystal arthritides, so it cannot
be used to make the specific diagnosis of gout. Long-term therapy of gout is designed
to decrease serum uric acid levels either by decreasing production (allopurinol) or
increasing excretion (probenecid). ACTH is also recommended for those patients with
contraindications to NSAIDs. The dose of ACTH is 40 IU to 80 IU given IM. Uric
acid lowering agents should not be started during an acute attack. Colchicine may be
given prophylactically for 6 to 12 months to suppress flare-ups.
In a patient with pseudogout, the knee is the joint most commonly involved, followed
by the wrist, ankle, and elbow. The average attack is not as severe as acute gout. In
general, these patients are between the sixth and eighth decades that have a previous
history of arthritic attacks. Joint fluid examination shows the weakly positive
birefringent crystals of calcium pyrophosphate dihydrate. The crystals appear
rhomboidal on regular light microscopy. Treatment for an acute attack is similar to the
therapy for acute gout: NSAIDs or oral colchicine, although the latter is not as
effective as with gout.
The two viruses that most commonly cause arthritis are rubella and hepatitis B, but
arthritis can also occur with mumps, adenoviruses, Epstein-Barr virus, and
enteroviruses. The pathophysiology of arthritis in the viral diseases appears to be
deposition of soluble immune complexes in the synovium with resultant inflammation.
Patients with rubella arthritis often are young women.
Reiter’s syndrome represents the clinical manifestation of a reactive arthritis that
occurs in genetically susceptible hosts after infection with Chlamydia trachomatis in
the genitourinary tract, or Salmonella, Shigella, Yersinia, or Campylobacter organisms
in the GI tract. Salmonella enteritis leads to reactive arthritis in up to 4% of cases;
Shigella flexneri is the most common stool isolate causing Reiter’s syndrome.
230
712. The triad of fever, joint pain, and rash in a woman of childbearing age should suggest the diagnosis
of systemic lupus. You also know that:
a. bundle branch block is the most common cardiac manifestation, reported in 30% of patients.
b. exudative pleural effusions are relatively common.
c. persistent hematuria is seen in approximately 50% of patients.
d. neurologic presentations, such as seizures, stroke, psychosis, migraines, and peripheral
neuropathies, are frequently the first signs of disease.
e. unlike rheumatoid arthritis, the inflammation of the hands is asymmetric.
713. A 77-year-old woman complains of headache, low-grade fever, malaise, myalgias, intermittent
blurred vision, and other nonspecific symptoms. You suspect giant cell arteritis, knowing that:
a. absence of temporal artery tenderness would eliminate the possibility of this condition.
b. elevated C-reactive protein level may be a helpful diagnostic clue.
c. polycythemia is a common finding.
d. sedimentation rate will be two or three times the normal rate.
e. steroids must be withheld until arterial biopsy can be done.
714. The hallmark physical finding (as opposed to most common finding) of Behçet’s syndrome is:
a. green sclera.
b. hypopyon uveitis.
c. intracranial hypertension with a multiple sclerosis–like syndrome.
d. iritis and optic neuritis.
e. recurrent, painful genital aphthous ulcers.
715. Henoch-Schönlein purpura primarily effects:
a. arterioles and capillaries in children.
b. veins and venules in adults.
c. arteries and venules in children.
d. arterioles and veins in adults.
e. capillaries and venules in children.
716. You are evaluating a 35-year-old with a history of systemic lupus. She complains of chest pain.
You know that:
a. Libman-Sachs vegetations are infectious excrescences on the aortic valve, representing bacterial
endocarditis.
b. lupus pericarditis requires high-dose steroid therapy.
c. pericardial effusions are found in more than half of lupus patients.
d. pericarditis is the most common cardiac manifestation of SLE.
e. SLE patients have no increased risk of coronary artery disease.
717. Acute HIV syndrome is characterized by nonspecific symptoms such as fatigue, weight loss,
diarrhea, pharyngitis, and adenopathy, seen:
a. within 24 hours of exposure.
b. 1 week after exposure.
c. 2 to 6 weeks after exposure.
d. 12 to 24 weeks after exposure.
e. 4 to 6 months after exposure.
231
712. b
th
Rosen 5 ,
Chapter 112,
p. 1609
713. b
Rosen 5th,
Chapter 112,
p. 1613
714. b
Rosen 5th,
Chapter 112,
p. 1615
715. a
Rosen 5th,
Chapter 112,
p. 1616
716. d
th
Rosen 5 ,
Chapter 112,
p. 1609
717 .c
Rosen 5th,
Chapter 126
p. 1845
Pleural effusions, seen in 12% of SLE patients, are usually exudative in nature. Like
rheumatoid arthritis, the inflammation of the hands, specifically the proximal
interphalangeal and the metacarpophalangeal joints, is symmetric. Clinical nephritis,
defined as persistent proteinuria, is seen in approximately 50% of patients. Nervous
system manifestations are varied and include seizures, stroke, psychosis, migraines,
and peripheral neuropathies, but are rarely the initial sign. Pericarditis is the most
common cardiac manifestation of SLE, reported in 30% of patients.
Temporal or giant cell arteritis is most common in branches of the carotid artery but
may involve any large or medium artery. The disease is most commonly seen in
women in the sixth and seventh decades of life. The classic symptoms of TA are
consistent with ischemia to the organs fed by branches of the internal and external
carotid artery: visual loss in one eye, temporal artery tenderness, and jaw claudication.
Patients may complain of nonspecific, vague symptoms such as malaise, weight loss,
and fever. Headache may be the initial complaint. Although the diagnosis is made
clinically, helpful laboratory findings include elevated ESR (usually greater than 100
mm/hr on a Westergren blot), elevated C-reactive proteins, and anemia. The definitive
diagnosis is made by temporal artery biopsy. Most patients are extremely sensitive to
glucocorticoids, and treatment should be started for any patient with a high clinical
suspicion of TA. The steroids do not significantly change the results of the biopsy and
may prevent progression to visual loss.
Recurrent, painful aphthous ulcers that involve the oral mucosa and genitals are
clinically predominant, but the hallmark of Behçet’s, a hypopyon uveitis, is seen
rarely. Other eye involvement includes iritis, uveitis, and optic neuritis, all of which
can lead to blindness. CNS vasculitis, resulting in meningoencephalitis, intracranial
hypertension, or a multiple sclerosis–like syndrome, can also occur
Henoch-Schönlein purpura (HSP) affects mainly the arterioles and capillaries, with
peak incidence between 4 and 11 years of age, although adults may also be affected.
The syndrome occurs most often in the spring following a viral upper respiratory
infection. Other inciting agents associated with HSP include insect stings and drugs.
Pericarditis is the most common cardiac manifestation of SLE, reported in 30% of
patients. Signs and symptoms include fever, tachycardia, chest pain, and transient
rubs. Pericardial effusions, however, are found in only 20% of patients. Purulent
pericarditis associated with Staphylococcus aureus and tuberculosis has occurred in
patients taking steroids. Pericarditis in SLE is usually self-limited. Libman-Sachs
vegetations on the mitral valve are noninfectious and related to autoimmune
deposition. SLE patients with hypertension and hypercholesterolemia are at a
markedly increased risk of coronary artery disease. Myocarditis is clinically apparent
in only 10% of patients; however, it is present in 40% at autopsy.
Acute HIV syndrome usually occurs 2 to 6 weeks after initial exposure and is
characterized by multiple nonspecific symptoms such as fever, fatigue, adenopathy,
diarrhea, pharyngitis, weight loss, and rash. These symptoms may last up to 3 weeks
and usually resolve without the patient seeking medical advice.
232
718. A 24-year-old man with AIDS complains of headache, fever, stiff neck, and confusion. You
suspect cryptococcal meningitis, knowing that the most accurate diagnostic study will be:
a. CSF cryptococcal antigen.
b. CSF fungal culture.
c. CSF India ink stain.
d. Serum cryptococcal antigen.
e. Serum cryptococcal antibody.
719. In an AIDS patient who complains of diarrhea, the pathogen most likely to lead to a bacteremia is:
a. Campylobacter jejuni.
b. enteroadherent E. coli.
c. Isospora spp.
d. Salmonella spp.
e. Shigella spp.
720. Kaposi’s sarcoma is:
a. commonly found on the palms and the soles.
b. highly lethal.
c. more common in HIV-positive women, due to the estrogen effect.
d. painful, blanching raised brown-black or purple papules and nodules.
e. the second most common manifestation of AIDS.
721. The treatment of Kawasaki Syndrome is intended to prevent:
a. coronary artery aneurysms.
b. fistula formation from the draining lymph nodes.
c. fulminant liver failure.
d. meningoencephalitis.
e. paraplegia or quadriplegia.
722. A middle-aged woman is brought from a local shopping mall by ambulance. She is confused and
profusely diaphoretic, and can answer no questions. The medics only report that she was
hypotensive and bradycardic, but she did not respond to 1 mg of intravenous atropine. As you
examine the patient you note a large well-healed midchest scar and a Medic Alert bracelet stating
“Heart Transplant Patient.” You know you should treat her bradycardia with:
a. dobutamine.
b. dopamine.
c. epinephrine.
d. higher doses of atropine.
e. isoproterenol.
233
718. a
th
Rosen 5 ,
Chapter 126,
p. 1849
719. d
th
Rosen 5 ,
Chapter 126,
p. 1852
720. e
Rosen 5th,
Chapter 126,
p. 1852
721. a
Rosen 5th,
Chapter 161,
722. e
Rosen 5th,
Chapter 178,
p. 2508
Of the diagnostic tests for cryptococcus, identifying cryptococcal antigen in the CSF is
100% sensitive and specific. India ink has a 60% to 80% sensitivity; fungal culture
and serum cryptococcal antigen have a 95% sensitivity for identifying cryptococcus.
Salmonella is a particular problem in patients with HIV, often producing recurrent
bacteremia and other significant clinical disease. Campylobacter infection usually
causes a proctocolitis. Isospora and Cryptosporidium are protozoal infections that
produce a chronic watery diarrhea. Cytomegalovirus is a viral opportunistic infection
that is associated with diarrhea and other gastrointestinal disease (such as
hepatobiliary) in HIV patients.
Kaposi´s sarcoma is the second most common manifestation of AIDS and appears
more often in homosexual men than in other risk groups. Clinically, it consists of
painless, raised brown-black or purple papules and nodules that do not blanch.
Common sites are the face, chest, genitals, and oral cavity; however, widespread
dissemination involving internal organs may occur. Since cutaneous Kaposi´s sarcoma
is not generally associated with significant rates of morbidity or mortality, therapy is
indicated only for extensive, painful, or cosmetically disfiguring lesions.
The treatment of Kawasaki syndrome is directed toward the amelioration of symptoms
and the prevention of coronary aneurysms. Gamma-globulin 2 gm/kg intravenously
should be administered over 12 hours, followed by high-dose aspirin therapy (100
mg/kg/24 hr PO given in divided doses every 6 hours for 14 days). Low-dose aspirin
therapy (3 to 5 mg/kg/24 hr PO) should continue until acute phase reactants return to
normal over 3 to 5 months. A pediatric cardiologist should follow children to monitor
cardiac status.
Exogenous pressor drugs work well in the transplanted heart. Upregulation of Betaadrenergic receptors appear to occur in the graft, with a slightly increased response to
norepinephrine and isoproterenol.
234
10.0 – Systemic Infectious Disorders
723.A 22-year-old sexually active female complains of dull bilateral lower abdominal pain and dysuria.
She denies fever, chills, nausea or vomiting. She also denies vaginal discharge. Urinalysis
confirms a urinary tract infection. Urine pregnancy test is negative. Her last normal menstrual
period was 2 days ago. Pelvic examination demonstrates no cervical motion tenderness or adnexal
pain on either side. You should still have a high index of suspicion for:
a. appendicitis.
b. an ovarian cyst.
c. ectopic pregnancy.
d. mittelschmerz.
e. a sexually transmitted disease.
724.You are evaluating a 20-year-old man who returns 10 days after being treated for STD. He was
given ceftriaxone 125 mg IM and azithromycin 1 gm orally. He now complains of dysuria and
mild testicular pain. He is afebrile, and has a normal cremasteric reflex and a positive Prehn's sign.
You suspect resistant chlamydia, and confirm your suspicion with:
a. blood culture and CBC.
b. ELISA or DNA probe of urethral secretions
c. testicular ultrasound
d. urethral culture.
e. urine dipstick for nitrates/leukocytes.
725.You are treating a 19-year-old woman for salpingitis. You also tell her that she should:
a. advise her partner to be treated.
b. undergo HIV counseling and testing through her family doctor or a public health clinic.
c. avoid douching, as this has been implicated in salpingitis and cervicitis.
d. not resume normal sexual activity for at least one week.
e. all of the above are true
726.The STD-causing organism which usually produces a characteristic skin lesion is:
a. Chlamydia trachomatis.
b. Gardnerella vaginalis.
c. Neisseria gonorrhoeae.
d. Treponema pallidum.
e. Trichomonas vaginalis.
727.A 23-year-old woman complains of "vaginal pimples.” She has not had sex for 3 months. You
examine the patient and suspect genital warts. The best treatment is:
a. acyclovir 400 mg five times daily for two weeks.
b. famciclovir 500 mg three times daily for two weeks.
c. metronidazole 2 grams oral once.
d. oseltamivir 250 mg twice daily for five days.
e. podofilox 0.5% solution or gel.
235
723. e
th
Rosen 5 ,
Chapter 93,
p. 1394
724. b
Rosen 5th,
Chapter 93,
p. 1413
725. e
Rosen 5th,
Chapter 93,
p. 1393
726. d
Rosen 5th,
Chapter 93,
p. 1393
727. e
Rosen 5th,
Chapter 93,
p. 1394
Many patients who present to the Emergency Department complaining of vague
abdominal pain and/or dysuria are diagnosed with a urinary tract infection, treated and
discharged. However, more than half of these patients also have positive cultures for a
sexually transmitted disease. Therefore, the clinician must have a high index of
suspicion for diagnosing an STD, especially in a young sexually active patient. Many
of these diagnoses are delayed or missed completely. The patient just had her last
menstrual period 2 days prior, has a negative urine HCG and clinical presentation
inconsistent with an ectopic pregnancy or ovarian cyst.
The clinical examination of the patient appears to indicate a urethritis and possible
mild epididymitis. The best lab test would be polymerase chain reaction (PCR) or
enzyme immunoassay techniques (ELISA). The urinalysis may be helpful, but
oftentimes lacks the sensitivity/specificity to verify this diagnosis. A CBC and blood
culture would not be considered useful in this patient.
Patients who have contracted an STD are at higher risk for acquiring HIV, therefore, it
is advisable that they seek counseling and testing for HIV. They should also refrain
from sexual activity until they are no longer capable of spreading or potentially "pingponging" the disease between themselves and their partner. Their partner should also
be evaluated and treated.
Syphilis, caused by the spirochete, Treponema pallidum usually causes a painless
chancre with indurated borders on the shaft of the penis during the primary stage of the
disease. Chlamydia trachomatis is an intracellular organism and has not been reported
to cause a characteristic lesion. Neisseria gonorrhoeae and Trichomonas vaginalis
also do not cause an obvious, characteristic lesion.
The current recommended treatment for HPV is podofilox 0.5% solution or gel applied
to the affected area twice daily for three days, followed by four days of no therapy,
with the cycle repeated up to four times. Podofilox is similar to podophyllum but
because it is less concentrated, it can be self-applied. Another potential treatment is
imiquimod 5% cream applied three times a week at bedtime for up to 16 weeks. Some
physicians may do cryotherapy in their offices, but not in the ED.
236
728. Dark field microscopy may be helpful in laboratory diagnosis of:
a. crab lice (Pediculosis pubis).
b. genital warts..
c. HSV-II infections.
d. Treponema pallidum.
e. Trichomonas vaginalis.
729. An 18-year-old male complains of severe dysuria and difficulty urinating to the point of modest
urinary retention. He has a several, painful, vesiculopustular lesions on his glans penis. You make
a smear of fluid from one of the lesions and successfully demonstrate large intranuclear inclusions.
Your treatment regimen should include:
a. famcyclovir.
b. metronidazole.
c. nystatin.
d. penicillin G.
e. podofilox.
730. An antibiotic category considered safe for use at any time in pregnancy is the:
a. aminoglycosides.
b. fluoroquinolones.
c. penicillins.
d. sulfonamides.
e. tetracyclines.
731. A 27-year-old woman returns 4 days after having nasal packing placed for a nosebleed. Her oral
temperature is 102.9oF, and blood pressure is 86/48 mmHg. She is still oozing blood from around
the packing, and has a diffuse red rash, especially on her palms and soles. You should treat this
patient with:
a. a glucose-containing intravenous fluid, with 2 ampoules of bicarbonate added.
b. antibiotics, being certain to cover for both streptococcal and staphylococcal infection.
c. high-dose glucocorticoids.
d. platelet transfusions and fresh-frozen plasma.
e. subcutaneous epinephrine and intramuscular diphenhydramine.
732. A 37-year-old man complains of fever and blurred vision. He is HIV positive with a CD4 count of
<50. He probably has:
a. cataracts.
b. central retinal vein occlusion.
c. CMV retinitis.
d. glaucoma.
e. iritis.
733. A 2½-week-old baby is visiting with his mother; they are from an underdeveloped section of
Africa. Mother says that the baby can’t suckle. The child has a low-grade fever, increased heart
rate, and irritability. The umbilical cord stump looks red and infected. The baby probably has:
a. botulism.
b. meningitis.
c. polio.
d. rabies.
e. tetanus.
237
th
Dark field (or darkfield) microscopy is used to assist in the laboratory diagnosis of
syphilis, caused by the spirochete, Treponema pallidum. Trichomonas is diagnosed by
plain microscopy. The other conditions listed can usually be diagnosed clinically.
th
This patient appears to have herpes simplex urethritis. The Tzanck cytology test
demonstrated evidence of a viral infection, most likely HSV-II. The appropriate
treatment is an antiviral agent, such as acyclovir, famcyclovir, or valicyclovir.
728. d
Rosen 5 ,
Chapter 93,
p. 1393
729. a
Rosen 5 ,
Chapter 93,
p. 1392
730. c
th
Rosen 5 ,
Chapter 174,
p. 2449
731. b
Rosen 5th,
Chapter 131,
p. 1947
732. c
Rosen 5th,
Chapter 126,
1853
733. e
Rosen 5th,
Chapter 123,
p. 1792
Penicillins as a group are generally believed to be the antibiotics that are safest to use
during pregnancy.
Aminoglycosides – gentamicin is category C, streptomycin is category D.
Fluoroquinolones – category C, should be avoided during pregnancy, possible
detrimental effects on cartilage and joint development.
Sulfonamides as a class are category B, but trimethoprim and Bactrim® are
category C
Tetracyclines – category D, should not be used during pregnancy unless no other
alternatives are available.
This patient had a “tampon” placed in her nares. She now has fever, hypotension and
erythroderma, hailing the onset of toxic shock syndrome. She will most likely need
hemodynamic support in the form of pressors and fluids, and antibiotics to treat both
streptococcal and staphylococcal infections.
CMV retinitis occurs in 10% to 30% of HIV-infected patients and is the most common
cause of blindness in patients with AIDS. With advances in HAART, reduced
incidences of CMV retinitis have been observed, but discontinuation of HAART may
result in intraocular inflammation. CMV retinitis typically produces severe necrotic
vasculitis and retinitis. When present, it may be asymptomatic or cause diminished
visual acuity, photophobia, scotoma, redness, or pain. It is diagnosed by its
characteristic appearance on indirect ophthalmoscopy of fluffy white retinal lesions,
often perivascular. Differential diagnosis includes toxoplasmosis, syphilis, HSV
infection, HZV infection, and TB.
Neonatal tetanus is a form of generalized tetanus that occurs almost exclusively in
underdeveloped countries, where maternal immunization is inadequate and
contaminated material is used to cut and dress the umbilical cords. The incubation
period is short, with symptoms beginning during the first week of life. Early clinical
manifestations include irritability and poor sucking and swallowing.
238
734. Although Clostridium tetani is sensitive to many antibiotics, the antibiotic of choice to treat a
patient suffering from tetanus is:
a. penicillin.
b. linezolid.
c. a third-generation cephalosporin.
d. tetracycline.
e. a third- or fourth-generation fluoroquinolone.
735. In a patient with cephalic tetanus, the cranial nerve most likely to be involved is the:
a. ocular nerve.
b. olfactory nerve.
c. facial nerve.
d. trigeminal nerve.
e. vagus nerve.
736. In the United States, the animal most likely to infect a human with rabies is the:
a. raccoon.
b. squirrel.
c. rat.
d. guinea pig.
e. chipmunk.
737. A 36-year-old camper was the victim of an unprovoked attack by a fox, which bit her several times
and then ran away. She has not received any pre-exposure prophylaxis to rabies, so she now needs:
a. administration of HDVC, scrubbing the wound with virucidal agent, and waiting for the
authorities to determine if the animal in question is rabid before administering HRIG because of
the risk of anaphylaxis.
b. irrigation and scrubbing of the wound only as this is a low-risk exposure.
c. irrigation of the wound with saline and administration of a mixture of HRIG and HDVC into the
area surrounding the wound.
d. irrigation with sterile water and administration of human diploid cell vaccine (HDCV).
e. scrubbing and irrigation with a virucidal agent (e.g., povidone-iodine), followed by
administration of HDVC and human rabies immune globulin (HRIG) at separate anatomic sites.
738. A stray dog bites your hospital’s CEO. Her family doctor calls for your advice on rabies treatment,
so you tell him that:
a. bites on the head and neck have a shorter incubation period than those on the extremities.
b. the incubation time in humans cannot exceed 5 years.
c. the usual incubation time from bite to disease is 10 to 14 days.
d. the virus replicates locally and spreads via lymphatic channels.
e. mortality following an inoculation is equal regardless of the bite location.
739. Your CEO wants rabies post-exposure prophylaxis, so you begin the series after counseling her
that:
a. if pregnant, she will probably abort.
b. if she is taking steroids, she should stop during the time she is receiving the shots.
c. rabies antibody levels should be checked at 30 and 90 days after receiving PEP.
d. HRIG is contraindicated if she has an allergy to eggs or horse serum.
e. tetanus booster must be delayed for at least two weeks following HRIG administration.
239
734. b
th
Rosen 5 ,
Chapter 123,
p. 1793
735. c
Rosen 5th,
Chapter 123,
p. 1792
736. a
Rosen 5th,
Chapter 125,
p. 1834-1836
737. e
Rosen 5th,
Chapter 125
p.1839
738. a
Rosen 5th,
Chapter 125
p.1837
739. b
Rosen 5th,
Chapter 125,
p. 1839
Toxin production is eliminated by treatment of C. tetani infection. Because surgical
care and antibiotic use can cause a transient release of tetanospasmin, the EP should
consider delaying these measures until after the antitoxin has been administered. The
wound should be debrided and cleansed, and foreign bodies should be removed.
Penicillin, tetracycline, erythromycin, and metronidazole are all effective against C.
tetani. Most references recommend penicillin G, 10 to 24 million U per day IV in
divided doses in adults (for pediatrics, use 100,000 U/kg/day in divided doses) for 10
to 14 days. Doxycycline 100 mg IV every 12 hours is an alternative. Metronidazole
(500 mg orally every 6 hours) may have greater efficacy than penicillin.
Cephalic tetanus is manifested by trismus plus cranial nerve palsies. Cephalic tetanus
is rare, accounting for 1% to 3% of all tetanus cases. Most of these cases occur after
facial trauma or otitis media. Patients develop trismus and palsies of cranial nerve III,
IV, VII, IX, X, or XII ipsilateral to the site of local infection. The most commonly
involved cranial nerve is the facial nerve (VII). The clinical course is variable. In one
third of cases, resolution of symptoms is complete. Two thirds of these cases progress
to generalized tetanus.
In the 1960s and 1970s, the majority of wildlife rabies was found in skunks in the
United States. However, in the late 1970s, an epizootic among raccoons began in the
mid-Atlantic states and spread north and south to cover the entire Eastern seaboard;
now the majority of wildlife rabies in the United States is attributable to raccoons. The
source of this epizootic appears to be the inadvertent translocation of rabid raccoons
from the southeastern states to the mid-Atlantic region to stock the area for hunting.
This determination was based on the fact that the raccoons first seen in the midAtlantic states, and now along the entire east coast, carry the same antigenic variant as
those in the southeastern states. Although the total number of rabid raccoons appears
to have peaked, the population continues to spread geographically north and westward.
Prophylaxis consists of three steps: wound care, passive immunization, and active
immunization. No step in this treatment should be omitted. Rabies is easily killed by
sunlight, soap, or drying, and experimental studies have shown that scrubbing and
flushing the wound with benzalkonium chloride, 20% soap solution, or Ivory soap was
nearly 100% protective when performed within 3 hours of inoculation of virus. Rabies
immunoprophylaxis requires both passive immunization with antibody (immune
globulin) and active immunization with vaccine.
Although the incubation time for rabies is generally from 30 to 90 days, it has been
documented to take as long as 7 years. The virus replicates locally and travels along
peripheral nerves at a rate between 8 and 20 mm/day. For this reason, head and neck
bites have a shorter incubation period and higher mortality (with treatment) compared
to lower extremity bites. The risk of developing rabies is between 5% and 80%,
depending on the animal, the size of the bite/severity of exposure, and location on the
body.
Prophylaxis, including both passive and active immunization, given during pregnancy
does not result in an increase in fetal wastage, congenital defects, or side effects and
should not be withheld when indicated. Corticosteroids, antimalarials, and other
immunosuppressives can interfere with the development of active immunity and
should be withheld during the course of treatment if possible. Patients with
immunosuppressive illnesses should be monitored for antibody response.
240
740. Treatment of choice for a patient with falciparum malarium is:
a. chloroquine.
b. pyrimethamine-sulfadoxine.
c. quinine plus doxycycline.
d. rapid-infusion intravenous quinine.
e. primaquine.
741. Acute Plasmodium vivax can cause:
a. disseminated intravascular coagulation.
b. headache.
c. hypoglycemia.
d. pulmonary edema.
e. renal failure.
742. The best diagnostic test to support the diagnosis of malaria is:
a. abnormally low sedimentation rate.
b. complete blood count revealing microcytosis, schistocytes, and rouleaux.
c. microscopic urinalysis showing trophozoites.
d. peripheral blood smear showing parasites.
e. polymerase-chain reaction (PCR) DNA testing.
743. A 24-year-old entomologist was camping in New Hampshire a week ago and pulled off some deer
ticks (Ixodes dammini), so he took 200mg of oral doxycycline to prevent Lyme disease. Now he
complains of malaise, high fevers, headache, and dark urine. On his physical exam you see no rash,
but find hepatosplenomegaly. His CBC shows pancytopenia, and his urine looks quite dark. You
should now treat him with:
a. 3rd or 4th generation fluoroquinolone.
b. clindamycin and quinine.
c. one month of intravenous ceftriaxone.
d. two weeks of amoxicillin / clavulanate.
e. two weeks of doxycycline.
744. A pathognomonic finding for Chagas’ disease (Trypanosoma cruzi) is:
a. Kerley C lines on chest x-ray.
b. Romaña’s sign, painless unilateral periorbital edema.
c. spontaneous rhabdomyolysis and hematuria.
d. trifascicular heart block without cardiomegaly.
e. urine which turns green when left in a cool dark room.
745. The best way to prevent hookworm infection is to:
a. avoid raw fish.
b. avoid swimming in brackish water.
c. cook wild game thoroughly before eating.
d. wash hands frequently.
e. wear shoes.
241
740. c
th
Rosen 5 ,
Chapter 127,
p. 1869
741. b
Rosen 5th,
Chapter 127
p.1869
742. d
Rosen 5th,
Chapter 127
p.1869
743. b
Rosen 5th,
Chapter 127
p.1869
744. b
Rosen 5th,
Chapter 127
p.1874
745. e
Rosen 5th,
Chapter 127
p.1871
In the past, chloroquine phosphate was the treatment of choice for acute,
uncomplicated attacks of malaria. Resistance to chloroquine has been steadily
increasing, and now the drug should be used only in regions of known chloroquine
sensitivity. Quinine and doxycycline given together are the drugs currently
recommended for the treatment of falciparum malaria. Quinine can be given orally or
parenterally for more serious and life-threatening infections. When given
intravenously, too rapid infusion of quinine can cause profound hypoglycemia.
Irregular fevers are the hallmark of malaria. Other symptoms may include anemia,
headache, nausea, chills, lethargy, abdominal pain, and upper respiratory complaints.
Acute falciparum infection can have the following complications: cerebral malaria,
hypoglycemia (especially in children), metabolic acidosis, severe anemia, renal failure,
pulmonary edema, disseminated intravascular coagulation (DIC), and death.
Thick and thin blood films are the gold standard for the diagnosis of malaria. Viewing
several slides may be necessary if the parasite burden is not overwhelming. Giemsa or
Wright’s stains are both adequate for this purpose when used with ordinary light
microscopy. The diagnosis often can be made in a simply equipped laboratory. Even
if the parasite is not visualized, the physician should still treat for malaria if clinically
suspected.
Babesiosis is a malaria-like illness that is becoming increasingly prevalent in the
northeastern United States (Babesia microti), the northwestern United States (B.
gibsoni), and Europe (B. divergens). The organism is a protozoan similar in structure
and life cycle to the plasmodia. It is transmitted by the deer tick, Ixodes dammini, the
vector of Lyme disease. Patients develop fatigue, anorexia, malaise, myalgia, chills,
high spiking fevers, sweats, headache, emotional lability, and dark urine. They have
hepatosplenomegaly, anemia, thrombocytopenia, leukopenia, elevated liver enzyme
levels, and signs of hemolysis with hyperbilirubinemia and decreased haptoglobin.
The treatment of choice is quinine and clindamycin.
The vector for Chagas’ disease is the reduviid, or “kissing bug,” which inhabits the
walls and roofs of thatched dwellings built adjacent to forest in South America. The
reduviid bites the patient, often in the periorbital region, and excretes feces containing
the trypomastigote of T. cruzi. The trypanosome enters the inflamed bite wound or
other mucosal or conjunctival surfaces, causing local swelling, called a chagoma.
Romaña’s sign, painless unilateral periorbital edema, is pathognomonic but rarely seen.
Hookworm infection has been recognized as a major cause of anemia worldwide. The
larvae penetrate human skin, usually through the feet. Adult worms penetrate into
intestinal mucosa and feed, causing significant ongoing luminal blood loss. Eggs
defecated in the soil mature through a rhabditiform larval form to the infective
filariform larva.
242
746.A 39 year-old woman complains of a severe headache, high fever, stiff neck, and photophobia. She
appears toxic and cannot touch her chin to her chest. Her left arm also drifts downward when held
at full extension. You must now:
a. start antibiotic, do spinal tap, do head CT.
b. do spinal tap, start antibiotic if positive, do head CT.
c. start antibiotic, do head CT, spinal tap if CT negative.
d. start antibiotic, do head CT; don’t bother with spinal tap since already treating.
e. do head CT, do spinal tap, start antibiotic if indicated.
747.Babesiosis is a:
a. bacterium spread by the bite of a flea.
b. fungus spread by the bite of a flea.
c. protozoa spread by the bite of a tick.
d. spirochete spread by the bite of a rat.
e. virus spread by the bite of a tick.
748.In a patient with Babesiosis, the pathognomonic finding is:
a. abnormal hemoglobin-hematocrit ratio (>>1:3).
b. green urine which fluoresces with Woods’ lamp.
c. intraerythrocytic parasite on blood smear ('Maltese cross' formation).
d. oval liver-abscess on ultrasound.
e. spirochetal invasion of platelets.
749.The hallmark of a patient with Cat Scratch Disease is:
a. anorexia, emesis, weight loss, thinning of hair.
b. chronic tender lymphadenopathy.
c. headache, lace-like rash on chest and abdomen.
d. malaise or fatigue with splenomegaly.
e. severe pharyngitis with normal-looking throat and negative cultures.
750.An immunocompetent patient with Cat Scratch Disease can be treated with:
a. outpatient intravenous antivirals.
b. inpatient intramuscular antibiotics.
c. oral antibiotics.
d. oral antivirals.
e. watchful waiting.
751.A 43-year-old woman has uncontrollable watery diarrhea. You ask her about food intake and recent
travel in an effort to determine the correct etiology, such as:
a. giardia from home-canned vegetables.
b. salmonella from backpacking and stream water.
c. scombroid poisoning from red snapper.
d. staphylococcus from potato salad.
e. Vibrio parahemolyticus from fried rice.
243
746. c
th
Rosen 5 ,
Chapter 103,
p. 1532
747. c
Rosen 5th,
Chapter 127,
p. 1869
748.c
Rosen 5th,
Chapter 127,
p. 1869
749. b
750. e
Rosen 5th,
Chapter 54,
p.777
751. d
Rosen 5th,
Chapter 89
p.1308
Patients with a markedly depressed sensorium that precludes careful neurologic
examination, or those with a focal neurologic deficit, papilledema, seizures, or
evidence of head trauma must be considered to be at risk for a herniation syndrome
that may be exacerbated by an LP. If the presentation is an acute, fulminating, febrile
illness and bacterial meningitis is the concerning diagnosis, early initiation of
antimicrobial therapy is mandatory because of the association of prognosis and time to
treatment. The algorithmic alternatives are therefore (1) immediate LP, followed by
initiation of antibiotic treatment before obtaining the results or (2) initiation of
antibiotic treatment, followed by a cranial CT scan and then an LP. This latter choice
of empiric treatment with antibiotics is now the routine in many institutions. This
reflects the efficacy of current methodologies of ’ means other than bacteriologic
cultures.
Babesiosis is a malaria-like disease with the etiologic agents being protozoan parasites:
Babesia microti and Babesia equi. The major zoonotic reservoirs are domesticated
mammals, rodents, and deer. Ixodes ticks functions as the principal vector. Blood
transfusions have been implicated in the transmission of babesiosis. Laboratory tests
often show evidence of hemolysis, liver dysfunction, anemia, thrombocytopenia, and
renal failure. Approximately 20% of the patients with babesiosis have a concurrent
infection with Lyme disease. Diagnosis is made by finding intraerythrocytic ring
forms on a Giemsa-stained peripheral blood smear, though false-negative results can
occur when the level of parasitism is low.
Cat scratch disease most often occurs in young (80% less than 21 years of age)
immunocompetent hosts. The initial site develops a transient erythematous papule or
pustule for which the patients do not often seek medical attention. They usually come
after the development of persistent regional lymphadenopathy in an area of the body
draining lymph from the scratch or bite, usually 7 to 12 days after the injury.
Symptomatic lymphadenopathy usually resolves spontaneously in 2 to 4 months. The
bacterium is sensitive to many antibiotics.
Staphylococcal-related food poisoning is caused by the multiplication of an
enterotoxin-forming strain of Staphylococcus organisms in the food before ingestion.
Contamination of food with Staphylococcus organisms is extremely common because
the organism can be grown from the hands of approximately 50% of persons. Most
protein-rich foods will support the growth of staphylococci, especially ham, eggs (even
hard boiled), custard-filled pastries, mayonnaise, and potato salad.
244
752. Two weeks ago, a 65 year-old woman cut her hand while gardening. She vigorously washed the
wound and observed for infection. Today she complains of a painful arm and jaw. She has no
fever, but practically bites the thermometer in half when the hospital fire alarm rings. You know
that:
a. her condition is caused by an anaerobic, gram-positive bacillus, which is nonencapsulated and
forms spores.
b. the mortality rate from this disease is more than 50% in the United States.
c. the spatula test will be negative.
d. patients presenting early after exposure to the bacterium have a better prognosis.
e. broad-spectrum antibiotics are the hallmark of treatment.
753. Choose the true statement about cellulitis.
a. Blood cultures are usually positive.
b. Dicloxacillin is a good antibiotic choice for treatment.
c. Temperature is usually elevated and there is a “left shift” in the white blood cell count.
d. The most common sites are face, then upper extremities, then lower extremities.
e. The patient usually remembers a break in the skin.
754. Impetigo is the most common skin infection seen in the emergency department.
a. The prevalence is greatest in homeless, alcoholics, and others with poor immune systems.
b. Fever and malaise are usually present.
c. Regional lymphadenitis is present in virtually every case.
d. Treatment is combined oral and topical antibiotic therapy.
e. In bullous impetigo, Nikolsky’s sign is negative.
755. A six-year-old non-immunized boy has fever, sore throat, difficulty swallowing, and malaise. His
throat exam shows an adherent gray pseudo-membrane. His treatment must include antitoxin
therapy plus:
a. active immunization.
b. antiviral therapy.
c. active immunization and antibiotics.
d. passive immunization and an antiviral.
e. active immunization and steroids.
756. A 42-year-old immigrant laborer stepped on a nail protruding from a 2 x 4 while he was helping
tear down an old barn. He is not certain whether he has ever had a tetanus shot. He should get:
a. tetanus toxoid only, as this is not a “tetanus prone” wound.
b. tetanus toxoid and tetanus immunoglobulin initially, with referral for rest of immunization.
c. tetanus toxoid and tetanus immunoglobulin, even if he had been immunized in last 5 years, since
this is a tetanus-prone wound.
d. tetanus toxoid now, withhold tetanus immune globulin until he can check his immunization
status; otherwise, TIG given too soon after prior immunization greatly increases the probability of
adverse reactions.
e. tetanus immunoglobulin, with second dose in 24 hours because of short half-life.
757. The most common CNS complication of pertussis is:
a. encephalitis.
b. encephalopathy.
c. intracerebral hemorrhage.
d. seizure.
e. vasculitis and stroke.
245
752. a
th
Rosen 5 ,
Chapter 123,
p. 1791
753. b
Rosen 5th,
Chapter 131,
p. 1944-1945
754. e
Rosen 5th,
Chapter 131,
p. 1949
755. c
Rosen 5th,
Chapter 123,
p. 1787
756. b
Rosen 5th,
Chapter 123,
p. 1793
757. d
Rosen 5th,
Chapter 123
p.1789
Trismus is the presenting symptom in most patients with tetanus and is caused by
increased masseter muscle tone. Patients may complain of lockjaw and present to a
dentist or oral surgeon. As the other facial muscles become involved, the characteristic
sardonic smile (risus sardonicus) appears. Other early symptoms include irritability,
weakness, myalgia, muscle cramps, dysphagia, hydrophobia, and drooling. The muscle
rigidity increases as the disease progresses. The time from an initial symptom to the
first muscle spasm is called the onset period. A shorter onset period is predictive of a
poorer prognosis. In the most severe form of tetanus, muscle rigidity becomes
generalized and reflex muscle spasms may be precipitated by external stimuli (noise,
light, touch) or occur spontaneously.
In addition to being caused by trauma or breaks in the skin layer, cellulitis may also be
secondary to hematogenous and lymphatic dissemination. Fever is not commonly seen
in cellulitis. Without systemic involvement WBC counts are normal or only slightly
elevated without left shift. Blood cultures are rarely positive. Staphylococcus and
streptococcus cause cellulitis most commonly on the lower extremities, then the upper
extremities, and 3rd the face.
Impetigo is the most common skin infection seen in the emergency department. The
prevalence is greatest in young children, particularly those under the age of 6 years.
Impetigo may occur sporadically or, occasionally, in epidemics. There are no
associated systemic manifestations such as fever or malaise. Regional lymph nodes
may be minimally enlarged. The treatment of impetigo is oral antibiotic therapy or an
appropriate topical antibiotic for limited eruptions. A first generation oral
cephalosporin or erythromycin provides effective oral therapy. Mupirocin is the only
topical agent with proven efficacy. Combination topical and systemic therapy is
unnecessary.
Equine serum diphtheria antitoxin should be administered promptly after the clinical
diagnosis of respiratory diphtheria. Antitoxin can be obtained by contacting the CDC.
The size and location of the membrane, the duration of illness, and the patient’s overall
degree of toxicity determine the dosage of antitoxin. The Committee on Infectious
Diseases of the American Academy of Pediatrics (AAP) recommends 20,000 to
40,000 U for pharyngeal or laryngeal involvement of 48 hours’ duration, 40,000 to
60,000 U for nasopharyngeal lesions, and 80,000 to 100,000 U for extensive disease of
3 or more days’ duration or for diffuse swelling of the neck. In addition to antitoxin
therapy, antibiotics should be administered for 14 days. Erythromycin, 40 to 50
mg/kg/day (up to 2 g) IV or orally in divided doses; intramuscular (IM) aqueous
crystalline penicillin, 100,000 to 150,000 U/kg/day in four divided doses; or procaine
penicillin, 25,000 to 50,000 U/kg/day in two divided doses for 14 days given IM every
12 hours is acceptable.
Patient with no known history of tetanus immunization should be given tetanus
immunoglobulin and tetanus toxoid in two different locations in body in ED and
referred to receive the rest of the immunization. Any patient with known history of
adequate immunization within last 5 years does not need to have tetanus toxoid or
immunoglobulin even if the wound is contaminated. Tetanus immunoglobulin (TIG)
does not need to be repeated since the half-life of TIG is 25 days.
CNS complications of pertussis include seizures (3%), encephalopathy (0.9%), and
intracerebral hemorrhage. The mechanisms may include hypoxia, a toxin, or
secondary infection by neurotropic viruses. CNS hemorrhages may occur as a
consequence of the increased cerebral vascular pressures generated during the
paroxysm of coughing and whooping.
246
758. In a patient with pertussis, the severity and duration of cough can be lessened by using:
a. a macrolide antibiotic.
b. non-narcotic cough suppressants.
c. narcotic-based cough suppressants.
d. pertussis immune globulin.
e. antihistamines.
759. A 27-year-old woman complains of weakness, lightheadedness, dry mouth, difficulty speaking, and
double vision. She was at a family gathering yesterday where her aunt had served some homecanned foods. You suspect botulism, knowing that:
a. distal muscles are weaker than proximal muscles.
b. lower extremity muscles more affected than those of the upper extremity.
c. ocular signs include ptosis, extraocular palsies, and pinpoint pupils.
d. the gag reflex should be normal.
e. the patient with botulism is usually alert and afebrile.
760. Treatment of the patient in Question #759 should include:
a. antibiotics to prevent further toxin release.
b. antitoxin to neutralize both circulating and bound toxin.
c. intubation if forced vital capacity goes to less than 50% of predicted.
d. magnesium-containing cathartics.
e. saline enemas to cleanse the GI tract of residual toxin.
761. Clinical criteria for sepsis include:
a. heart rate >110 beats/minute.
b. more than 20% immature (band) forms of WBCs.
c. respiratory rate >24 breaths/minute.
d. temperature >38°C (100.4oF) or <36°C (96.8oF)
e. WBC count greater than 15,000/mm3.
762. Patients with asplenia (post-surgical) or inadequate splenic function (as occurs in sickle cell
disease) may develop a fulminant type of pneumococcemia termed overwhelming postsplenectomy infection (OPSI), which is characterized by
a. meningitis, DIC, and hemorrhagic pancreatitis.
b. pituitary infarct, hemorrhagic thyroiditis, and asterixis.
c. septic shock, adrenal hemorrhage, and DIC.
d. septic shock, coronary artery occlusion, and fulminant hepatitis.
e. shock, rotatory nystagmus, and hemorrhagic hepatitis.
763. You are seeing a 16-year-old girl with flu-like symptoms. She is about 14 hours into the illness.
Your rapid screening test shows she has influenza type B. Her parents are insistent that you have to
“give her something.” The only medicine which might help this illness and has been approved for
this age group is:
a. amantadine.
b. famcyclovir.
c. oseltamivir.
d. rimantadine.
e. zanamivir.
247
758. d
th
Rosen 5 ,
Chapter 123
p.1789-1790
759. e
Rosen 5th,
Chapter 123
p.1796
760. e
Rosen 5th,
Chapter 123
p.1797
761. d
Rosen 5th,
Chapter 123
p.1798
762. c
Rosen 5th,
Chapter 123
p.1799
763. e
th
Rosen 5 ,
Chapter 124
p.1813, 1817
Antibiotics are indicated but may not alter the severity or duration of illness when
initiated after the catarrhal phase of illness. Corticosteroids, especially in infants, may
reduce the severity and course of illness, and beta2-adrenergic agonists may reduce the
frequency and severity of the paroxysmal coughing episodes. Early clinical trials with
pertussis immune globulin have shown significant improvement in lymphocytosis and
paroxysmal coughing in infants. This may be a useful treatment for very ill patients in
the future. Standard cough suppressants and antihistamines are ineffective.
The patient with botulism is usually alert and is afebrile unless secondary infection is
present. Postural hypotension may be present. Ocular signs are prominent and include
ptosis, extraocular palsies, and markedly dilated and fixed pupils. The absence of
ocular abnormalities does not exclude the diagnosis. Dryness of the mouth, tongue,
and pharynx leads to a red, dry appearance of the mucous membranes. The gag reflex
is depressed or absent. Muscle weakness is usually present but varies from mild to
severe. Neck muscles are often weak. Upper extremity muscles are more affected
than those of the lower extremity. Proximal muscles are weaker than distal muscles.
Deep tendon reflexes may be normal, symmetrically decreased, or absent. Sensory
examination is normal.
A decrease in vital capacity to less than 30% of predicted is a standard criterion
mandating mechanical ventilation. Saline enemas and cathartics have been
recommended to cleanse the GI tract of residual toxin. Magnesium-containing
cathartics should be avoided because magnesium can exacerbate muscle weakness.
Antitoxin neutralizes only circulating toxin and has no effect on bound toxin.
Antibiotics are not currently recommended for food-borne botulism, as they may
increase cell lysis and promote toxin release.
Sepsis is the systemic response to infection, manifested by two or more of the
following: (1) temperature greater than 38°C or less than 36°C; (2) heart rate >90
beats/min; (3) respiratory rate >20 breaths/min or PACO2 less than 32 mm Hg; and (4)
WBC count greater than 12,000/mm3, less than 4000/mm3, or greater than 10%
immature (band) forms.
Patients with asplenia (post-surgical) or inadequate splenic function (as occurs in sickle
cell disease) may develop a fulminant type of pneumococcemia termed overwhelming
post-splenectomy infection (OPSI), which is characterized by septic shock, adrenal
hemorrhage, and DIC.
Amantadine and rimantadine are effective in preventing and treating influenza A, but
have no activity against influenza B. Zanamivir and oseltamivir act by inhibiting the
activity of neuraminidase, an enzyme involved in the release of viral progeny from
infected cells. Influenza strains are identified by their hemagglutin and neurominidase
composition (e.g., H1N3, H2N4, etc.) Zanamivir is approved for the treatment of
influenza A and B, administered by inhalation, and is approved for use in patients older
than 12 years of age. Oseltamivir is approved for the treatment of influenza A and B,
an oral medication approved for patients older than 18.
248
764. Virtually all patients with meningococcemia have:
a. fever.
b. meningitis.
c. petechiae.
d. seizures.
e. Waterhouse-Friderichsen syndrome.
765. The most common exanthem of immunized children less than 2 years of age is:
a. erythema infectiosum.
b. roseola.
c. rubella.
d. rubeola.
e. varicella.
766. Parvovirus:
a. has been implicated in aplastic crisis in children with sickle cell disease.
b. has been implicated in hemolytic crisis in children with sickle cell disease.
c. has been implicated in sequestration crisis in children with sickle cell disease.
d. has been implicated in vaso-occlusive crisis in children with sickle cell disease.
e. has been implicated in equestrian crisis in children with sickle cell disease.
767. The correct match is:
a. varicella = first disease
b. rubella = third disease
c. scarlet fever = fourth disease
d. exanthem subitum = fifth disease.
e. erythema infectiosum = sixth disease
768. Flaviviruses, such as the West Nile virus, are spread to humans through the vector of:
a. bats.
b. fleas.
c. mites.
d. mosquitoes.
e. ticks.
769. Mycobacterium tuberculosis:
a. affects almost one-fifth of the world’s population.
b. can be found in greatest abundance in immigrants from Africa and Eastern Asia.
c. has been on the decline since emergence of better antibiotics in the 1980s.
d. is especially problematic in nursing home patients, as these patients are a primary reservoir for
disease.
e. is the second leading infectious cause of death worldwide.
770. Choose the true statement:
a. Hemoptysis in tuberculosis occurs early and is usually copious.
b. In children with pulmonary tuberculosis, the most common radiographic findings are hilar
adenopathy, mediastinal lymphadenopathy, and consolidated pneumonia.
c. Fewer than 5% of patients with tuberculosis have extrapulmonary manifestations.
d. Night sweats and weight loss are the most common symptoms of pulmonary tuberculosis.
e. Shortness of breath is common and is not predictive of severity.
249
764. a
th
Rosen 5 ,
Chapter 123,
p. 1801-1802
765. b
Rosen 5th,
Chapter 124,
p. 1822
766. a
Rosen 5th,
Chapter 124,
p. 1823
767. b
Rosen 5th,
Chapter 124,
p. 1825
768. d
Rosen 5th,
Chapter 124,
p. 1825
769. d
Rosen 5th,
Chapter 129,
p. 1903
770. b
Rosen 5th,
Chapter 129,
p. 1906
Table 129-1
An elevated temperature is present in 71% to 89% of cases of meningococcemia, and
hypothermia is present in 4% of cases. Although skin lesions are present in 71% of
cases, petechiae, or purpura, are present in only 49% of cases. Shock occurs in 42%
of patients, arthritis in 8%, and seizures in 8%. The Waterhouse-Friderichsen
syndrome occurs in 10% to 20% of patients with meningococcal disease and is
characterized by extreme severity and rapid clinical deterioration, including
vasomotor collapse and shock.
Roseola infantum is the most common exanthem of children younger than 2 years of
age and occurs most often at about 1 year of age. The illness begins abruptly with the
acute onset of fever, often as high as 41°C, lasting 3 to 5 days. Despite the fever, the
child usually remains active and alert.
Parvovirus B19 has a propensity for attacking and causing a marked reduction in
erythroid cell precursors and has been established as a cause of transient aplastic crisis
in patients with chronic hemolytic anemia. Recovery is associated with reappearance
of reticulocytes in the peripheral smear 7 to 10 days after their disappearance. Rare
cases of encephalitis and pneumonia have been reported.
The rash associated with rubella (“third disease”) is one of the classic common
exanthems of childhood. It may be similar to the rash of measles (rubeola, or “first
disease”), scarlet fever (“second disease”), a variant of scarlet fever or toxin-producing
staphylococcal disease (“fourth disease”), erythema infectiosum (“fifth disease”), and
roseola (exanthem subitum, or “sixth disease”).
More than 60 flaviviruses have been identified, with more than 20 causing human
disease. Three of the most common, all transmitted to humans via a mosquito vector,
are the agents of yellow fever, dengue, and St. Louis encephalitis. The West Nile virus
has recently been reported in numerous areas of the United States, including Louisiana
and the East Coast.
Tuberculosis is the world's leading cause of infectious death. Over one third of the
world's population is infected, and each year over 3 million people die from the
disease. Currently in the United States, elderly people with dormant infections are the
main reservoir of TB reactivation. The largest numbers of people with TB originate
from Mexico, the Philippines, and Vietnam.
Cough is the most common symptom of pulmonary tuberculosis. Hemoptysis is
usually minor but often indicates extensive involvement. Shortness of breath from
parenchymal lung involvement is unusual, and if present, indicates extensive
parenchymal disease or tracheobronchial obstruction. While the majority of cases of
tuberculosis are pulmonary, up to 15% of cases will have extrapulmonary
manifestations. In children with TB, The most common radiographic findings include
hilar adenopathy, mediastinal lymphadenopathy, or consolidated pneumonia.
250
771. Multi-Drug Resistant Tuberculosis (MDRTB) is defined as resistance to:
a. ethambutol.
b. rifampin.
c. streptomycin.
d. isoniazid.
e. two or more first-line anti-tuberculosis drugs.
772. The most common complication of cavitary pulmonary tuberculosis is:
a. bacteremia.
b. empyema.
c. endobronchial spread.
d. pericardial effusion.
e. pneumothorax.
773. Risks for acquiring TB may also be stratified by age. We know that:
a. infants and toddlers have a much lower incidence of TB than adults.
b. children 5 to 10 years of age are relatively resistant to TB.
c. infants and toddlers only rarely have extrapulmonary disease
d. young adults rarely develop cavitary lesions
e. the elderly are most likely to manifest “classic” disease of cough, hemoptysis, and cavitary
lesions.
774. Concerning the use of anti-tuberculosis drugs, you know that:
a. ethambutol is the preferred treatment in small children and infants,
b. fluoroquinolones are becoming first-line agents.
c. oral streptomycin is a second-line agent.
d. pyrazinamide works in the acid environment of the macrophage.
e. rifampin causes blue-green discoloration of blood, sweat and tears.
775. Hantavirus infections are usually spread by:
a. being bitten by an infected flea.
b. being bitten by an infected mosquito.
c. being bitten by an infected tick.
d. drinking contaminated water.
e. inhaling aerosolized contaminated mouse droppings.
776. Patients with the hantavirus pulmonary syndrome:
a. are treated with chloramphenicol and ampicillin.
b. can develop a paradoxical metabolic alkalosis.
c. develop bradycardia as an early sign of systemic illness.
d. have a 50 to 70% mortality rate.
e. have an annoying “brassy” paroxysmal cough.
777. The most common source of infection in the septic patient is the:
a. central nervous system.
b. gastrointestinal system.
c. integumentary system.
d. respiratory system.
e. urogenital system.
251
771. b
th
Rosen 5 ,
Chapter 129,
p. 1919
772. c
th
Rosen 5 ,
Chapter 129,
p. 1907
773. b
Rosen 5th,
Chapter 129,
p. 1906
774. d
Rosen 5th,
Chapter 129
p.1917
775. e
776. d
Rosen 5th,
Chapter 124,
p. 1829
777. d
Rosen 5th,
Chapter 132,
p. 1961
Multi-drug resistance tuberculosis is defined as resistance to two or more first-line
antituberculous agents. Multidrug resistance may occur when a single drug is added to
a failing regimen, an intervention equivalent to giving monotherapy.
Endobronchial spread is the most common complication of cavitary disease. It is seen
on x-ray examination as 5- to 10-mm poorly defined nodules clustered in dependent
portions of the lungs. Empyema is rare (1% to 4%) and is more common in patients
with extensive, progressive parenchymal disease. Pericarditis may result from the
anatomic relationship of the mediastinal lymph nodes to the pericardial sac. Rupture
of lymph nodes into the pericardium may lead to pericardial tamponade.
Pneumothorax is seen in less than 5% of patients.
Risks for acquiring TB may also be stratified by age. Infants and toddlers have poorly
developed cell-mediated immunity, so they have a much higher incidence of TB than
adults. Children 5 to 10 years of age are relatively resistant to TB. Infants and
toddlers commonly have extrapulmonary disease and acute lower and midlung
bronchopneumonia that rarely progresses to cavitary disease. Young adults show the
adult pattern of apical pulmonary disease, including cavity formation, suggesting
reactivation. Because of decreased immunocompetence, the elderly tend to manifest
the disease similar to young children.
Rifampin causes orange discoloration of urine, tears, and sweat. Pyrazinamide works
in the acid environment of the macrophage. Visual acuity and red-green color
perception should be measured when using ethambutol. Because of the difficulty in
visual testing in small children and infants, ethambutol should be avoided in these
populations. Streptomycin must be given parenterally. Fluoroquinolones have a
limited role; they are less effective than first-line agents and are used mainly in the
treatment of drug-resistant disease. If used singly, resistance may quickly develop.
Hantaviruses cause a hemorrhagic fever with renal syndrome. Rodents carry the
agents, and the virus is transmitted via aerosols infected from rodent urine. More than
100,000 cases occur in Asia and Europe, and the mortality rate is approximately 6%.
In 1994, a previously unknown hantavirus was found to cause a pulmonary syndrome
associated with tachypnea, hemoconcentration, thrombocytopenia, and leukocytosis.
Cases occurred predominantly in the southwestern United States, were associated with
a mortality rate higher than 50%, and were believed to have been transmitted from the
deer mouse, Peromyscus maniculatus. The virus has been named the Muerto Canyon
or Sin Nombre virus.
The respiratory system is the most common focus of infection in the septic patient.
History of a productive cough, fevers, chills, upper respiratory symptoms, and throat
and ear pain should be elicited. Examination should include detailed evaluation,
looking for focal infection such as exudative tonsillitis, sinus tenderness, tympanic
membrane injection, and crackles or dullness on lung auscultation. Also, pharyngeal
thrush should be noticed as a marker of an immunocompromised state.
252
778. You have just intubated a 70-year-old man who presented with fever, cough, confusion, and
respiratory failure. Even with a non-rebreather mask you were unable to get his oxygen saturation
above 85%. Your next priority should be to:
a. keep his hemoglobin above 10 g/dl.
b. keep his oxygen saturation above 96%.
c. keep his positive end-expiratory pressure to less than 8 cm of water.
d. keep his systolic blood pressure below 170 mm hg.
e. keep his transalveolar pressures (plateau pressures) below 35 cm of water.
779. Pseudomonas bacteria are responsible for bone and joint infections in three main settings. The first
is in puncture wounds to the foot. The other two are:
a. children with cystic fibrosis and alcoholics with peri-articular puncture wounds.
b. diabetics with eye prostheses and patients with Gram-negative toxic shock syndrome.
c. patients with implanted orthopedic devices and IV drug users, who may develop hematogenous
osteomyelitis, often in the spine.
d. pediatric patients with glycogen storage deficiency disease and under-treated patients with
Pseudomonas endocarditis.
e. sickle cell patients with avascular necrosis and AIDS patients with long-time steroid use for PCP
treatment.
780. Bone scanning is a very useful test in diagnosing osteomyelitis. The radionuclide with the highest
sensitivity, approaching 90%, is:
a. 111In.
b. 127Ne.
c. 23SkDu.
d. 67Ga.
e. 99mTc MDP.
253
778. e
th
Rosen 5 ,
Chapter 132,
p. 1962-1963
779. c
Rosen 5th,
Chapter 130,
p. 1928
780. e
Rosen 5th,
Chapter 130,
p. 1930
There are no specific recommendations in the acute setting of trying to lower blood
pressure below 170 mm Hg. Positive end-expiratory pressure is an effective way to
increase arterial oxygen delivery. This pressure may need to be increased well above 8
cm H2O in the acute setting. Most experts believe that transfusion is only warranted
once the hemoglobin drops below 8 g/dL. Keeping plateau pressures below 35 cm
H2O has been shown to reduce the incidence of ventilator-induced lung injury.
Pseudomonas bacteria are responsible for bone and joint infections in three main
settings. The first is in puncture wounds to the foot. Pseudomonas does not appear to
grow on puncture objects, but rather is intimately associated with shoe gear that may
be inoculated into the wound and produce soft-tissue infection and osteomyelitis.
Patients in whom prosthetic devices are implanted during orthopedic surgery are at risk
for Pseudomonas bone and joint infection. IV drug users may develop hematogenous
osteomyelitis, often in the spine, from Pseudomonas bacteria.
The technetium methylene diphosphonate (99mTc MDP) scan is a sensitive test for
osteomyelitis in patients who have no existing bone abnormalities. Most series report
a sensitivity of greater than 90% with the three-phase scan. Additional testing with
gallium citrate 67Ga and indium oxine. 111In is often used to compensate for the limited
specificity of the technetium-99m scans.
254
11.0 – Musculoskeletal Disorders (Nontraumatic)
781. Normal compartment pressures are:
a. near 0 mmHg
b. 10-20 mmHg
c. 20-40 mmHg
d. 40-60 mmHg
e. 60-80 mmHg
782. Carpal tunnel syndrome is characterized by:
a. improvement with repetitive motion.
b. negative Tinel sign.
c. positive Finkelstein’s test.
d. positive Phalen’s test.
e. radial nerve palsies.
783. Which cervical nerve root innervates the thumb?
a. C2
b. C4
c. C6
d. C8
e. T2
784. The small finger is innervated by the:
a. palmar cutaneous branch of median nerve.
b. dorsal cutaneous branch of ulnar nerve.
c. median nerve.
d. radial nerve.
e. ulnar nerve.
785. To test the motor branch of the ulnar nerve, ask the patient to
a. abduct the fingers.
b. extend the fingers.
c. extend the wrist.
d. flex the fingers.
e. flex the wrist.
786. A boutonnière or swan neck deformity
a. always involves a fracture.
b. present with DIP flexion.
c. is the same as a mallet finger.
d. presents with PIP flexion and DIP extension.
e. requires emergent surgical repair.
255
781. a
th
Rosen 5 ,
Chapter 42,
p. 479
782. d
Rosen 5th,
Chapter 44,
p. 548-549
783. c
Rosen 5th,
Chapter 36,
p. 347,
Figure 36-22
784. e
th
Rosen 5 ,
Chapter 43,
p. 505,
Figure 43-25
785. a
Rosen 5th,
Chapter 43,
p. 505
786. d
th
Rosen 5 ,
Chapter 43,
p. 523,
Figure 43-52
Normal compartment pressure is 0 mm Hg. Blood flow to the microcirculation is
generally impaired when tissue pressures reach 30 mm Hg or more; however, some
patients can tolerate much higher compartment pressures without compartment
syndrome developing. Controversy exists over attempts to define compartment
syndromes on the basis of specific tissue pressure. The tolerance to tissue ischemia
varies among individuals because of shock, compensatory hypertension, altered tone in
resistance vessels, and other unknown factors. Inadequate perfusion and relative
ischemia begin when the tissue pressure within a closed compartment rises to within
10 to 30 mm Hg of a patient’s diastolic pressure.
The most sensitive provocative test to diagnose carpal tunnel syndrome is the wrist
flexion test, or Phalen’s test (sensitivity 76%, specificity 80%). The patient fully
flexes the wrists for 60 seconds while the forearms are held in a vertical position. The
test is positive if paresthesias or numbness develops in the median nerve distribution.
Another test, Tinel’s sign, is positive if light tapping or percussion over the median
nerve at the wrist produces pain or paresthesias in the median nerve distribution.
Finkelstein's test is positive in de Quervain’s tendonitis.
C2 Occiput
C7 Index finger
L2–L3 Medial thigh
C3 Thyroid cartilage
C8 Small finger
L4 Knee
C4 Suprasternal notch
T4 Nipple line
L5 Lateral calf
C5 Below clavicle
T10 Umbilicus
S1 Lateral foot
C6 Thumb
L1 Femoral pulse
S2–S4 Perianal region
FIGURE 43–25. Cutaneous
nerve supply of the hand.
M, median
R, radial
U, ulnar
PCM, palmar cutaneous
branch of median nerve
DCU, dorsal cutaneous
branch of ulnar nerve.
The dorsal interosseous muscles abduct the fingers away from the midline. The ulnar
nerve innervates them. Wrist and finger extension is under control of the radial nerve,
while the median nerve controls flexion.
A boutonnière deformity is a disruption of the extensor hood near the PIP that presents
with PIP flexion and DIP extension. Initial treatment is by splinting the PIP in
extension. A mallet finger is a disruption of the extensor tendon at the DIP.
Boutonnière deformities are also seen in patients with rheumatoid arthritis
256
787. A felon:
a. can be treated by the emergency physician using incision and drainage followed by antibiotics.
b. is most commonly caused by group A streptococcus.
c. is the same as a paronychia.
d. requires hospital admission.
e. requires nail bed removal.
788. Patients with flexor tenosynovitis:
a. almost never recall a precipitating event.
b. have a negative Kanavel’s sign.
c. have exquisite pain with finger flexion.
d. have no pain when the proximal tendon sheath is palpated.
e. present with diffuse fusiform swelling.
789. Volkman’s contracture
a. is associated with child abuse.
b. is associated with supracondylar fractures
c. is caused by a brachial nerve injury.
d. takes weeks to develop.
e. usually presents with a pulseless extremity.
790. Legg-Calvé-Perthes disease is caused by:
a. a hip joint infection, most commonly due to Staphylococcus aureus.
b. a genetic bone matrix defect.
c. degeneration of the acetabulum.
d. avascular necrosis of the femoral head.
e. repetitive microtrauma to the articular cartilage of the knee.
791. A 3-year-old child is diagnosed with a septic arthritis of the hip. The organism which is most likely
causing his infection is:
a. Enterobacter.
b. Neisseria gonorrhoeae.
c. Pseudomonas aeruginosa.
d. Staphylococcus aureus.
e. Streptococcus pneumoniae.
792. A 14-year-old boy complains of pain in his groin, which sometimes goes to his thigh and knee. The
pain is dull, vague, intermittent or continuous, and is exacerbated by physical activity. He walks
with his leg in external rotation, and has an antalgic gait. You strongly suspect the child has:
a. Legg-Calvé-Perthes disease.
b. Osgood-Schlatter disease.
c. septic arthritis.
d. slipped capital femoral epiphysis.
e. transient toxic synovitis.
257
787. a
th
Rosen 5 ,
Chapter 43,
p. 529-530
788. e
Rosen 5th,
Chapter 43,
p. 531
789. b
Rosen 5th,
Chapter 45,
p. 565-566
790. d
Rosen 5th,
Chapter 49,
p. 643
791. d
Rosen 5th,
Chapter 169,
p. 2384,
Table 169-6
792. d
Rosen 5th,
Chapter 169,
p. 2387
A felon is a subcutaneous pyogenic infection of the pulp space of the distal finger or
thumb. The patient presents with marked throbbing pain and a red, tense distal pulp
space. Staphylococcus aureus is the most common organism, but Streptococcus species,
anaerobes, and gram-negative organisms are also encountered. Most felons can be
drained adequately with a limited incision and drainage procedure. Most felons have
significant associated cellulitis that should be treated with oral antibiotics. A firstgeneration cephalosporin or antistaphylococcal penicillin should be prescribed for 7 to
10 days or until the infection has abated.
Flexor tenosynovitis is a surgical emergency that must be diagnosed promptly by the
examining physician and managed aggressively by both the emergency physician and
the hand surgeon. Recognizing the classic clinical findings described by Kanavel makes
the diagnosis. The four cardinal signs are tenderness over the flexor tendon sheath,
symmetric swelling of the finger, pain with passive extension, and a flexed posture of
the involved digit at rest.
Ten percent of children with supracondylar fracture lose the radial pulse temporarily,
most often as a result of swelling and not direct brachial artery injury. Reducing the
fracture, avoiding flexing the elbow more than 90 degrees, and elevating the arm help
prevent secondary obstruction to arterial flow. Compartment syndrome, or Volkmann’s
ischemic contracture as a result of prolonged ischemia of the forearm, is a dreaded
complication but fortunately is rare in this era, with a reported incidence of less than
0.5%.
Perthes’disease is the name given to avascular necrosis of the pediatric femoral head. It
has also been called Legg-Calvé-Perthes’ and Calvé-Perthes’ disease. It occurs at a
younger age than SCFE does—between the ages of 2 and 10. Its peak incidence is at 6
years and it occurs 5 times more often in boys than in girls. The disease affects both
hips in 15% of patients.
The most common organism implicated in acute septic arthritis is Staphylococcus
aureus. Acute septic arthritis occurs in all age groups but is more common in children:
70% of cases occur in children less than 4 years old, and the peak incidence is between
6 and 24 months. Boys are affected twice as frequently as girls. Predisposing factors
include preceding viral infection, trauma, immunodeficiency, hemoglobinopathy,
hemophilia with recurrent hemarthroses, diabetes, intravenous drug abuse, rheumatoid
arthritis, and intra-articular injections or operations. A total of 75% of septic arthritis
cases involve the joints of the lower extremity, with the knee being most commonly and
the hip second most commonly involved.
Children with a stable slipped capital femoral epiphysis have symptoms of intermittent
limp and pain of several weeks’ to months’ duration. Stable slips make up
approximately 90% of all cases. The pain of SCFE may be localized to the hip but more
commonly is poorly localized to the thigh, groin, or knee. With continued slippage,
internal rotation, flexion, and abduction are lost; and parents and children may note
progressive external rotation and shortening of the involved lower extremity with
subsequent difficulty in daily activities such as tying shoes. On examination, children
initially experience a slight loss of internal rotation and experience pain only at the
extremes of motion. The gait is antalgic and muscle atrophy is minimal. As the slip
becomes more severe, the gait becomes more antalgic, internal rotation is lost, abduction
and flexion of the hip increase, thigh and gluteal muscle atrophy is more pronounced,
and leg length discrepancy develops.
258
793. Carpal tunnel syndrome
a. is associated with ulnar nerve compression.
b. is ruled out with a negative Tinel’s sign.
c. presents with ulnar and dorsal hand numbness.
d. is reliably diagnosed with nerve conduction velocity studies.
e. Produces symptoms that worsen when the hands are placed in a dependent position.
794. In a patient with suspected acute cervical disc herniation:
a. axial load frequently relieves the symptoms.
b. the disease is more common in women than in men.
c. it tends to occur more in the upper vertebra.
d. the disc usually bulge in a direct posterior direction.
e. Valsalva’s maneuver frequently replicates the symptoms.
795. A complaint of bilateral shoulder pain without history of trauma should raise the suspicion of:
a. C4 radiculopathy.
b. C5 radiculopathy.
c. C5 myelopathy.
d. C6 radiculopathy.
e. C6 myelopathy.
796. Chance fractures:
a. are usually at the thoracic spine level.
b. are associated with airbag deployment.
c. involve only the anterior and posterior columns.
d. involve only the middle and posterior columns.
e. are easily misdiagnosed as compression fractures.
797. The key sign of spinal stenosis is:
a. genital numbness and stool incontinence.
b. hyperreflexia and a negative anal “wink.”
c. hyporeflexia and a negative cremasteric reflex.
d. lower extremity pain exacerbated with walking and relieved with sitting.
e. urinary incontinence and stocking anesthesia.
798. Concerning the rotator cuff of the shoulder:
a. All four rotator cuff muscles originate on the scapula, traverse the glenohumeral joint, and insert
on the proximal humerus.
b. It consists of four muscles: the supraspinatus, the infraspinatus, the teres major, and the deltoid.
c. The infraspinatus muscle initiates arm elevation and abducts the shoulder.
d. The supraspinatus is an abductor of the humerus.
e. The rotator cuff muscles contribute little to the power of the upper extremity, providing less than
10% of the power in abduction and 20% percent in external rotation.
799. The muscle of the rotator cuff which is injured most frequently is the:
a. infraspinatus.
b. subscapularis.
c. supraspinatus.
d. teres minor.
e. teres major
259
793. a
th
Rosen 5 ,
Chapter 47,
p. 547-549
794. e
Rosen 5th,
Chapter 47,
p. 606-608
795. d
Rosen 5th,
Chapter 47,
p. 609
796. e
th
Rosen 5 ,
Chapter 42,
Table 42-1
797. d
Rosen 5th,
Chapter 47,
p. 616
798. a
Rosen 5th,
Chapter 46,
p. 600-601
799. c
Rosen 5th,
Chapter 46,
p.601
Carpal tunnel syndrome is a neuropathy of the median nerve at the wrist that occurs as a
result of compression of the median nerve within the carpal tunnel. The classic symptoms
include a gradual onset of numbness, paresthesia, and pain in the thumb, index finger, and
long finger. These symptoms are often bilateral and are worse during the night and after
strenuous activities. Typically, symptoms improve when the hands are shaken or held in a
dependent position. On physical examination the most sensitive provocative test is the
wrist flexion test, or Phalen’s test (sensitivity 76%, specificity 80%), performed by asking
the patient to fully flex the wrists for 60 seconds while the forearms are held in a vertical
position. The test is positive if paresthesias or numbness develops in the median nerve
distribution. Another test, Tinel’s sign, is positive if light tapping or percussion over the
median nerve at the wrist produces pain or paresthesias in the median nerve distribution.
Tinel’s sign is not as helpful as Phalen's test (sensitivity 64%, specificity 55%). Nerve
conduction studies have recently been used to confirm the diagnosis, with reports of a
sensitivity as high as 90%.
Cervical disk disease occurs most commonly in those aged 35-55 years, and frequently
with a prior history of trauma. Lateral to posterolateral is the usual direction of herniation
with directly posterior being rare. It occurs most commonly in the lower cervical
vertebrae, C4-C7. Axial load and Valsalva’s maneuver both aggravate the symptoms.
C6 lesions are frequent and may cause pain along the upper neck, down the biceps, along
the lateral forearm, and into the dorsal radial aspect of the hand. Motor weakness usually
involves the biceps or wrist extensors, making elbow flexion and wrist extension difficult.
Chance’s fracture is a vertebral fracture, usually lumbar, involving the posterior spinous
process, pedicles, and vertebral body. Caused by simultaneous flexion and distraction
forces on the spinal column, usually associated with use of lap seatbelts. The anterior
column fails in tension along with the middle and posterior columns. It may be
misdiagnosed as a compression fracture.
Spinal stenosis complaints usually come from older patients. Pain is diffuse, usually
involves the back, and often radiates down one or both legs, associated with paresthesias.
It is usually resolved by rest, although it takes longer to resolve than true vascular
claudication. Patients also note pain relief with back flexion. A typical story involves the
patient who is able to walk uphill without pain but develops pain walking downhill when
the back is extended. Impotence and incontinence may be present with spinal stenosis.
The supraspinatus, infraspinatus, and teres minor insert into facets of the greater
tuberosity, whereas the subscapularis inserts into the lesser tuberosity. All originate on the
scapula and traverse the glenohumeral joint, and serve as a dynamic stabilizer of the
glenohumeral joint. The acromioclavicular joint itself has only 5 to 8 degrees of
movement, but allows for 40 to 50 degrees of clavicular rotation. Due to its unique bony
structure, it is the most highly mobile yet least stable joint in the body. The supraspinatus
provides most of the first 30o of extension, while the infraspinatus is an external rotator.
Most rotator cuff tears involve the dominant arm and occur in men over age 40 years. The
occupational history is significant for strenuous work requiring overhead activity. Most
tears occur near the attachment of the supraspinatus and can extend anteriorly into the
subscapularis or posteriorly into the infraspinatus. Tears can be classified according to
their size, completeness, pattern location, or duration. A clinically useful system is to
divide tears into acute or chronic types.
260
800. Slipped capital femoral epiphysis:
f. affects girls more than boys.
g. frequently presents with gradual onset of knee pain.
h. is most common under age 10 years.
i. is treated conservatively.
j. usually has normal x-rays.
801. Failure to mobilize the shoulder after a stroke is a major risk factor for:
a. adhesive capsulitis.
b. biceps tendonitis.
c. carpal tunnel syndrome.
d. deltoid dawn syndrome.
e. rotator cuff disease.
802. Patients with bicipital tendonitis have intense pain, especially against resistance, when they attempt
to:
a. extend the elbow.
b. extend the wrist.
c. flex the elbow.
d. pronate the forearm.
e. supinate the forearm.
803. Transient toxic synovitis is
a.
a diagnosis of exclusion
b.
an uncommon cause of hip pain
c.
associated with high fever and laboratory abnormalities.
d.
caused by trauma
e.
treated with antibiotics
804. A 27-year-old athletic woman complains of right knee pain. She has no history of significant
trauma. There is no effusion on exam, but there is swelling and tenderness in the popliteal fossa
and in the calf. A lower extremity ultrasound is interpreted as normal. The most likely diagnosis
is:
a. anterior cruciate ligament injury
b. Baker’s cyst
c. deep venous thrombosis.
d. Osgood-Schlatter disease
e. patellar dislocation
805. Osgood- Schlatter Disease:
a. classically has no reproducible tenderness
b. is another name for patellar tendon apophysitis
c. is far more common in boys than in girls.
d. presents with acute pain.
e. requires surgery.
261
800. b
th
Rosen 5 ,
Chapter 169,
p. 2387
801. a
th
Rosen 5 ,
Chapter 46,
p. 603
802. e
th
Rosen 5 ,
Chapter 46,
p. 602
803. a
Rosen 5th,
Chapter 169,
p. 2382
804. b
Rosen 5th,
Chapter 50,
p. 697
805. c
Rosen 5th,
Chapter 50,
p. 699-700
Slipped capital femoral epiphysis is most common in obese adolescent males ages 1017. It is rare before age 10. The etiology is unclear. It often presents with gradual
onset of pain referred to the knee. The x-rays have a characteristic “melting ice cream
cone” appearance. It is treated surgically with open reduction internal fixation.
Although the cause of adhesive capsulitis remains unknown, any condition associated
with prolonged dependency of the arm can result in capsular contraction. This
includes voluntary immobilization after calcific tendinitis, rotator cuff injury,
mastectomy, or a distal upper extremity injury (Colles’ fracture).
On examination of a patient with bicipital tendinitis, there is tenderness over the biceps
tendon as it passes through the bicipital groove. This is best demonstrated with the
arm in abduction and external rotation. Active range of motion is limited by pain, but
the passive range remains intact. Supination against resistance (Yergason’s test) with
the arm adducted and the elbow flexed to 90 degrees reproduces the pain.
Transient synovitis is the most common cause of hip pain in childhood. It is a selflimited inflammatory condition caused by a nonpyogenic inflammatory response of the
synovium. Although it has been reported in children as young as 3 months and it
occasionally occurs in adults, its peak incidence is between 3 and 6 years of age.
Transient synovitis of the hip affects boys more commonly than girls and has a slight
predilection for the right side. The cause is unknown, and the diagnosis is one of
exclusion. Treatment is conservative – rest and antiinflammatories.
A Baker’s, or popliteal, cyst is a herniation of the synovial membrane through the
posterior aspect of the capsule of the knee, or it may occur through escape of fluid
through the normal communication of an anatomic bursa adjoining the
semimembranosus or gastrocnemius. It is usually the result of an internal knee
derangement with recurrent synovitis caused by a torn meniscus, loose body,
instability, degenerative change, or other factors. It generally causes a mass of varying
size occupying the posteromedial corner of the knee and often produces pressure, pain,
and limitation of range of motion. Rupture of the bursa with resultant escape of fluid
into the calf may produce a clinical picture similar to thrombophlebitis. Differentiation
from other clinical entities may require aspiration, ultrasound, or an MRI scan..
Tibial tubercle apophysitis was first described by Osgood and Schlatter in 1903. It is
believed to be caused by repeated traction to the anterior portion of the developing
ossification center of the tibial tuberosity. Past reports have suggested a large male
predominance for the development of Osgood-Schlatter disease, but as more girls and
young women have joined competitive sports, no significant sex differences have been
found. The disease is characterized by painful swelling over the tibial tubercle that is
exacerbated by activity, relieved by rest, and usually of several months’ duration.
Surgery may be required if the conservative treatment fails, but it cannot be
implemented until the epiphysis is closed, at which time the problem is usually
resolved.
262
806. Concerning pelvic fractures:
a. when present, they usually have associated bladder or urethral disruption.
b. they are usually seen in association with blunt lower urinary tract injury.
c. urethral disruption is more common in women than men.
d. they have no relation to thoracic aortic injury.
e. the first treatment is application of MAST garments.
807. Coccygeal fractures:
a. usually require an x-ray to diagnose.
b. they can be well evaluated by a rectal exam.
c. when displaced, reduction should be attempted.
d. occur more often in men than women.
e. usually heal rapidly and with minimal discomfort.
808. Plantar fasciitis:
a. causes pain and tenderness localized to the medial aspect of the heel.
b. causes pain that is worse in the evening and better after exercising.
c. eventually will require surgery.
d. is always associated with heel spurs.
e. is improved by avoiding Achilles tendon stretching and by walking barefoot on hard surfaces.
809. The tarsal tunnel syndrome:
a. causes pain on the dorsal foot near the first metatarsophalangeal joint.
b. causes tenderness over the tip of the lateral malleolus.
c. involves the anterior tibial nerve.
d. usually requires surgery.
e. can be diagnosed by the aid of selective nerve block.
810. Morton’s neuroma is found most frequently in women age 25 to 50, and causes a severe,
lancinating, debilitating pain in the:
a. ankle.
b. foot.
c. knee.
d. thumb.
e. wrist.
263
806. b
th
Rosen 5 ,
Chapter 48,
p. 627-628
807. b
Rosen 5th,
Chapter 48,
p. 632
808. a
Rosen 5th,
Chapter 51,
p. 733
809. e
Rosen 5th,
Chapter 51,
p. 733
810. b
Rosen 5th,
Chapter 51,
p. 733
The overall incidence of bladder or urethral disruption associated with pelvic fracture
ranges from 7% to 25%; however, more than 80% of patients with lower urinary tract
injury after blunt trauma have a pelvic fracture. Urethral disruption is less common in
women, but it does occur. There is a well-documented association between pelvic
fracture and injury to the thoracic aorta. This is presumably the result of the enormous
forces required to produce either injury. In particular, anteroposterior (AP)
compression fractures are associated with an 8 times greater incidence of aortic rupture
than is seen in the overall blunt trauma population. Initial treatment is fluid
resuscitation followed by considerations for stabilization and possibly embolization.
Radiographic confirmation of a coccygeal fracture is not always necessary. Displaced
fractures are often seen on the lateral view, but the diagnosis is evident on rectal
examination. Attempts at reduction are not recommended. Undisplaced fractures may
be difficult to demonstrate radiographically. The physician must decide whether the
knowledge gleaned from x-ray studies will alter the therapy to a degree that warrants
radiation exposure to the pelvis, especially considering that most of these fractures
occur in women. Because of muscle action on the fragment, healing is slow and
patients must be cautioned that discomfort may be prolonged.
The plantar fascia is a tough layer of the sole that is functionally significant during foot
strike and the early stance phase of walking. Plantar fasciitis, an overuse injury of
insidious onset, usually begins with pain on first weight bearing in the morning or after
prolonged sitting. This progresses to persistent pain during gait. Pain and tenderness
are localized to the medial aspect of the heel. Plantar fasciitis accounts for 9% of
running injuries and is particularly common in cavus feet. It is associated with heal
spurs about 50% of the time. Treatment is usually conservative with surgery rarely
required.
Compression of either the abductor digiti quinti nerve or the posterior tibial nerve (the
“tarsal tunnel syndrome”) can cause subcalcaneal heel pain. Diagnosis of these
conditions is difficult and is sometimes facilitated by assessing the impact of selective
nerve block with local anesthesia. Initial treatment of these conditions is similar to that
for plantar fasciitis, although local steroid injections or surgical release may be
required.
An important cause of unilateral metatarsalgia is a perineural fibrosis of the
intermetatarsal plantar digital nerve, more commonly known as a Morton’s neuroma.
This neuropathy of unknown cause was first described in 1876 and usually involves
the second-third or third-fourth interspace, causing lancinating pain with weight
bearing. The pain may be associated with paresthesias and can radiate into the toes. In
addition, “after burn” pain may persist during rest. The pain of a Morton’s neuroma is
reproduced when the affected interspace is pinched or when the metatarsal heads are
compressed together. Hence, pain may occur intermittently with tight-fitting footwear
(e.g., rock climbing shoes or ski boots). Crepitus or a nodule may be palpable.
Treatment usually involves surgical excision or neurolysis.
264
12.0 – Nervous System Disorders
811. The 30-day mortality rate for patients experiencing a stroke is:
a. less than 5%.
b. 10%.
c. 20 to 25%.
d. about 35%.
e. more than 50%.
812. A 74-year-old man has a history of hypertension and high cholesterol. He complains of sudden
painless blindness in his left eye. You suspect embolic stroke, with the origin of the clot being the:
a. anterior cerebral artery.
b. carotid artery.
c. circle of Willis.
d. heart.
e. middle cerebral artery.
813. An 82-year-old man is brought by his family after sudden onset of one-sided weakness, falls, and
an inability to speak. He can follow simple commands using the non-weak side. This localizes his
stroke to the:
a. anterior cerebral artery, dominant cortex.
b. anterior cerebral artery, nondominant cortex.
c. brainstem.
d. middle cerebral artery, dominant cortex.
e. middle cerebral artery, nondominant cortex.
814. Lacunar infarcts are:
a. commonly associated with chronic hypertension.
b. uncommon in African-Americans.
c. primarily located in the cerebellum.
d. frequent causes of cognitive defects, aphasia, and memory impairment.
e. rarely subcortical.
815. A 54-year-old male with a long history of smoking and hypertension says his right hand felt “dead”
for about 20 minutes this morning, and he was dragging his right foot. He dropped his coffee mug
and had a hard time lacing his shoes. He states he now feels “100% normal.” You examine him
and find no focal deficits. You discuss your findings with him, explaining:
a. 20% of patients with TIA will experience a stroke within 5 years.
b. a CT will show no evidence of an infarction.
c. carotid artery territory TIAs uniformly demonstrate arterial disease on angiography.
d. most TIAs last less than 30 minutes.
e. patients with resolved new-onset TIAs can safely be discharged from the Emergency Department
if they have a normal exam and negative CT scan.
265
811. c
th
Rosen 5 ,
Chapter 95,
p. 1433
812. b
Rosen 5th,
Chapter 95,
p. 1434
813. d
Rosen 5th,
Chapter 95,
p. 1436
814. e
Rosen 5th,
Chapter 95,
p. 1434
815. d
Rosen 5th,
Chapter 95,
p. 1435
Stroke is the third leading cause of death in the United States and the leading cause of
adult disability. It afflicts over 700,000 patients per year, with an in-hospital mortality
of almost 15% and a 30–day mortality of 20% to 25%. Even among survivors, over
half are left with a permanent disability and one third need assistance in the activities
of daily living.
Blood is supplied to the brain by the anterior and posterior circulation. The anterior
circulation originates from the carotid system and perfuses four fifths of the brain,
including the optic nerve, retina, and frontoparietal and anterotemporal lobes. The first
branch off the internal carotid artery is the ophthalmic artery, which supplies the optic
nerve and retina. As a result, the sudden onset of painless monocular blindness
(amaurosis fugax) identifies the stroke as involving the anterior circulation
(specifically the carotid artery) at or below the level of the ophthalmic artery.
Aphasia is important to recognize because it usually localizes a lesion to the dominant
(usually left) cerebral cortex in the middle cerebral artery distribution. Aphasia may be
expressive, receptive, or a combination of both. Wernicke’s aphasia occurs when the
patient cannot process sensory input such as speech and thus fails to understand verbal
communication (receptive aphasia). Broca’s aphasia refers to the inability to
communicate verbally in an effective way, even though understanding may be intact
(expressive aphasia). Aphasia should be distinguished from dysarthria, which is a
motor deficit of the mouth and speech muscles; the dysarthric patient articulates poorly
but understands words and word choices.
Lacunae or small-vessel strokes involve small terminal sections of the vasculature and
more commonly occur in African Americans and patients with diabetes and
hypertension. A history of hypertension is present in 80% to 90% of patients who have
lacunae strokes. The subcortical areas of the cerebrum and brainstem are often
involved. The infarctions range in size from a few millimeters to 2 cm and occur most
commonly in the basal ganglia, thalamus, pons, and internal capsule. They may be
caused by small emboli or by a process termed “lipohyalinosis,” which occurs in
patients with hypertensive cerebral vasculopathy. Although nearly 20 lacunae
syndromes have been described, the most common of these are pure motor strokes,
pure sensory strokes, or ataxic hemiparesis. Because they are subcortical and well
localized, lacunae strokes do not cause cognitive defects, aphasia, simultaneous
sensorimotor findings, and loss of consciousness or memory impairment.
The majority of TIAs last less than 30 minutes. Up to 50% of patients who experience
a TIA will go on to develop a stroke within 5 years. At least 50% of patients with TIA
in the carotid distribution do not have angiographically demonstrated arterial disease.
Although clinical deficits of TIAs resolve within 24 hours, studies have shown that up
to 64% of patients have CT evidence of infarction. Current standard is that a patient
with a new TIA requires hospital admission. The exception is a patient with only
minimal anterior circulation symptoms who has had a complete ED evaluation
including CT scan, carotid Doppler or MRA, and an echocardiogram if indicated.
Close neurologic follow up must be arranged.
266
816. A 76-year-old man had sudden onset of nausea and vomiting, and then became quite lethargic. His
exam shows poor pain and temperature perception on the right face and on the left arm and leg.
These symptoms are characteristic of a stroke in the distribution of the:
a. anterior cerebral artery.
b. middle cerebral artery.
c. posterior communicating artery.
d. anterior communicating artery.
e. vertebral basilar system.
817. The standard brain imaging study for a patient with presumed acute stroke is:
a. contrast-enhanced CT scan.
b. gadolinium-enhanced MRI.
c. magnetic resonance angiography.
d. noncontrast MRI.
e. noncontrast CT scan.
818. An 84-year-old woman has an acute ischemic stroke. She presents within 30 minutes of symptom
onset and her head CT shows only atrophy. She has no contraindication to fibrinolytic therapy, as
described in the National Institute of Neurologic Disorders and Stroke criteria. She weighs 50 kg,
so you choose to treat her using:
a. 10 mg bolus, 50 mg infusion over 30 minutes.
b. 10 mg bolus, 90 mg infusion over 60 minutes.
c. 100 mg bolus.
d. 5 mg bolus, 45 mg infusion over 60 minutes.
e. 50 mg bolus.
819. A 70-year-old man has a large hemorrhagic stroke. His blood pressure is 240/160 mm Hg, even
after he has received supplemental oxygen and comfort measures in the two hours you have been
caring for him. You should manage his blood pressure by giving him:
a. intravenous labetalol.
b. intravenous nitroprusside.
c. more time.
d. sublingual nifedipine.
e. transdermal clonidine patch.
820. The metabolic condition most frequently mistaken for stroke is:
a. Addisonian crisis.
b. hyperglycemia.
c. hypocalcemia.
d. hypoglycemia.
e. thyroid storm.
821. The patient who has had a classic tonic-clonic (grand mal) seizure:
a. has good recall for events leading up to and during the seizure.
b. invariably has post-ictal confusion and lethargy.
c. is usually able to avoid self-injury.
d. may experience an aura lasting a minute or two before the actual seizure.
e. may have side-to-side head thrashing, rhythmic pelvic thrusting, and clonic alternating extremity
motions
267
816. e
th
Rosen 5 ,
Chapter 95,
p. 1436
817. e
Rosen 5th,
Chapter 95,
p. 1438
818. d
Rosen 5th,
Chapter 95,
p. 1440-1441
819. b
th
Rosen 5 ,
Chapter 95,
p. 1442
820. d
th
Rosen 5 ,
Chapter 95,
p. 1438
821. b
th
Rosen 5 ,
Chapter 96,
p. 1446-1447
Unlike anterior circulation strokes, patients with posterior circulation stroke can
present with loss of consciousness, and they frequently have nausea and vomiting.
Visual agnosia, the inability to recognize seen objects, may occur, as well as alexia, the
inability to understand the written word. A third nerve palsy may occur, and the
patient may experience homonymous hemianopsia. One of the more curious facets of
this syndrome is that the patient may be unaware of any visual problem (visual
neglect). Vertigo, diplopia, visual field defects, weakness, paralysis, dysarthria,
dysphagia, syncope, spasticity, ataxia, or nystagmus may occur with vertebrobasilar
artery insufficiency. One of the key features is that the sensory findings such as
deficits in pain and temperature perception occur on one side of the face and on the
opposite side of the body.
An emergency noncontrast cranial CT is the standard imaging technique for evaluating
a patient with a potential stroke in the ED. It can quickly differentiate an ischemic
stroke from intracerebral hemorrhage and other mass lesions. It can identify almost all
parenchymal hemorrhages greater than 1 cm and up to 95% of all subarachnoid bleeds.
The majority of ischemic strokes do not have gross signs of infarction on routine CT
scan for at least 6 to 12 hours, depending on the infarct’s size. However, subtle, ultraearly changes have been noted in up to one third of stroke patients evaluated by CT
within 3 hours of symptom onset.
The total dose of rtPA for treating acute ischemic stroke is 0.9 mg/kg, with a maximum
dose of 90 mg; 10% of the dose is administered as a bolus, with the remaining amount
infused over 60 minutes. Blood pressure and neurologic checks should be assessed
every 15 minutes for 2 hours after starting the infusion.
Nitroprusside is the agent most commonly recommended because one can obtain a
rapid and consistent lowering of the blood pressure to the desired level and
adjustments can be made rapidly. It has rapid onset, it can be titrated, and has no effect
on mental status.
Hypoglycemia is often responsible for an altered mental status and is a well-known
cause of sustained focal neurologic findings that persist for several days.
By definition, patients lose consciousness in a generalized seizure, and no aura is
present. Some patients may experience a brief, vague prodrome or dysphoric state just
before the ictal event. Convulsive generalized seizures are typified by the grand mal
seizure in which the patient loses consciousness; stiffens with generalized muscular
hypertonus; and then rhythmically, violently contracts multiple, bilateral, and usually
symmetric muscle groups. A generalized convulsive seizure is followed by a postictal
state, headache, and drowsiness that may persist for hours.
268
822. Seizure is a common presenting symptom in an acute overdose of the anti-seizure medication:
a. carbamazepine (Tegretol®)
b. gabapentin (Neurontin®).
c. phenobarbital.
d. topiramate (Topamax®).
e. valproic acid (Depakene®)
823. Posttraumatic seizures (PTS):
a. are caused by epidural and intracerebral hematomas, but not subdural and traumatic subarachnoid
hemorrhages.
b. are more common in adults than children, especially in the early post-trauma stage.
c. are much more common if the dura is violated.
d. extinguish quickly, so that by one year after significant head trauma, the incidence of seizures is
the same as that of the general population.
e. occur in blunt head trauma as the result of increased intracranial pressure; thus, penetrating head
trauma does not usually cause seizures.
824. The most common cause of new onset seizures in geriatric patients is:
a. dehydration.
b. drug-drug interaction.
c. metastatic brain tumors.
d. primary brain tumors.
e. strokes.
825. A basic transport unit brings you a disheveled middle-aged man who has been seizing for about 10
minutes. As you start an intravenous line you ask the nurse to bring you a parenteral
benzodiazepine so you can stop the seizure. She asks you which one you prefer. You answer:
a. any of the three will do, as comparison studies have not demonstrated one drug to be clearly
superior.
b. diazepam, as it can be given intramuscularly if the intravenous line fails.
c. lorazepam, as it has clearly been demonstrated as the most efficacious.
d. lorazepam, diazepam, and midazolam, as the combination of all three drugs has been shown
especially efficacious in stopping status epilepticus.
e. midazolam, as it can be given endotracheally if the intravenous line fails.
826. A 24-year-old college student with a known seizure disorder failed to take any phenytoin for the
last week because of final exams. He had three seizures today and was brought by his roommate
for treatment. The patient weighs about 220 pounds, and his serum phenytoin level is 0. You need
to give him a loading dose of about:
a. 800 mg.
b. 1000 mg.
c. 1200 mg.
d. 1500 mg.
e. 1800 mg.
827. The most common recurrent head pain syndrome is:
a. cluster headache.
b. migraine headache.
c. temporal arteritis.
d. tension headache.
e. trigeminal neuralgia.
269
822. a
th
Rosen 5 ,
Chapter 96,
p. 1448-1449
823. c
Rosen 5th,
Chapter 96,
p. 1449
824. e
Rosen 5th,
Chapter 96,
p. 1449
825. a
Rosen 5th,
Chapter 96,
p. 1452
826. e
Rosen 5th,
Chapter 96,
p. 1452,
Table 96-1
827. d
Rosen 5th,
Chapter 97,
p. 1460
The most common drug- and toxin-associated seizures occur in conjunction with illicit
drugs such as cocaine, amphetamines, and phencyclidine; with overdoses of
anticholinergic agents such as cyclic antidepressants and antihistamines; as a
manifestation of withdrawal from ethyl alcohol and sedative-hypnotics; and with toxic
levels and deliberate overdoses of diverse medications such as aspirin, theophylline,
isoniazid, lithium, and the anticonvulsants phenytoin and carbamazepine.
Posttraumatic seizures (PTS) can occur as an acute result of blunt or penetrating head
trauma and as posttraumatic sequelae. Epidural, subdural, and intracerebral
hematomas and traumatic subarachnoid hemorrhages can all be acutely ictogenic,
particularly as the intracranial pressure rises. Immediate PTS are more common in
children than in adults. Within the first year after significant head trauma, the
incidence of seizures is at least 12 times that of the general population. The incidence
of seizures after injury with neurologic deficit without dural violation is 7% to 39%;
when the dura is disrupted, the incidence is 20% to 57%.
Ischemic or hemorrhagic stroke is the cause of new-onset seizures in 54% of elderly
patients. The overall incidence of seizures with stroke ranges from 4% to 15%; more
than half occur within the first week after stroke. The incidence of epilepsy after
stroke is 4% to 9%. Seizures that occur acutely with stroke are thought to result from
local metabolic alterations in the CNS; these events are transient and the seizures are
often focal and self-limited. Seizures that develop later are more likely to be
generalized.
Pertinent differences among benzodiazepines are the efficacy of diazepam when
administered rectally, endotracheally, or intraosseously; a relatively longer duration of
seizure suppression with lorazepam; and efficacy of the rectal and intramuscular routes
of administration for midazolam. In comparison studies, no one drug is clearly
superior. All three may be used in patients of all ages, all have relatively short
duration of anticonvulsant action, and all can cause sedation, hypotension and
respiratory depression.
Phenytoin is the primary drug used in the management of status epilepticus after initial
benzodiazepine therapy. It may also be used as primary therapy for patients whose
seizures are less frequent. The recommended loading dose is 18 to 20 mg/kg IV, in
this 100 kg patient a dose of 1800 to 2000 mg is appropriate. Infusion should be
limited to 50 mg/min due to the cardiotoxicity of the diluent. Patient should be on a
cardiac monitor.
Tension headache is the most common recurrent pain syndrome, affecting more than
75% of the population. Women are affected more frequently than men, and most
patients are middle aged. The headaches do not cause significant disability, and
patients are able to continue with their normal daily activities. The median frequency
of headaches is six per month, and stress and lack of sleep are implicated as triggering
factors. The average duration of the headache is 4 to 13 hours, with a maximum of 72
hours.
270
828. You are seeing a young man in whom you have suspicion of a possible subarachnoid bleed. His CT
was negative, so you did a spinal tap. The cerebrospinal fluid looks a bit pink, but the tap was
difficult and you are worried about a possible “traumatic tap.” You ask the lab to centrifuge a tube
of fluid so you can look for xanthochromia, as the patient has had the headache for long enough you
might see this finding. The amount of time it takes for xanthochromia to develop is about:
a. 4 hours.
b. 8 hours.
c. 12 hours.
d. 16-18 hours.
e. 20-24 hours.
829. Chromatographic studies on the supernatant spinal fluid of the patient in Question #828 show that it
was, indeed, a traumatic tap. You ask the patient to lie flat for two hours before sending him home
with appropriate analgesia. Twenty-seven hours later he returns, saying he has an even worse
headache than before. You suspect postdural puncture headache (PDPH).
a. An autologous blood patch will relieve the headache in a majority of patients with this condition.
b. The headache is from a hyperstimulatory overproduction of cerebrospinal fluid and can be
relieved by a second tap with removal of more fluid.
c. This is an uncommon complication, occurring in less than 10% of patients.
d. You had correctly used a large needle to minimize the amount of time needed to remove fluid,
and this should have prevented the headache.
e. You realize you should have had him stay flat for at least two more hours to avoid this
complication.
830. The treatment of choice for the pain of trigeminal neuralgia is:
a. dental referral for oral orthotic.
b. local steroid injections.
c. oral carbamazepine.
d. oral nimodipine.
e. transdermal fentanyl.
831. The majority of cases of delirium are caused by
a. electrolyte disturbances.
b. hypoxemia.
c. liver failure.
d. recreational and prescribed drugs.
e. sepsis.
832. The most common metabolic disorder causing acute organic brain syndrome is:
a. hyperglycemia.
b. hypernatremia.
c. hyperthyroidism.
d. hypoglycemia.
e. hyponatremia.
833. Brain tumor can present acutely as delirium, especially if the growth is located in the:
a. brainstem.
b. frontal lobe.
c. occipital lobe.
d. parietal lobe.
e. temporal lobe.
271
828. c
th
Rosen 5 ,
Chapter 97,
p. 1461
829. a
th
Rosen 5 ,
Chapter 97,
p. 1464
830. c
Rosen 5th,
Chapter 97,
p. 1465
831. d
Rosen 5th,
Chapter 98,
p. 1468-1469
832. d
Rosen 5th,
Chapter 98,
p. 1470
833. b
Rosen 5th,
Chapter 98,
p. 1471
To differentiate a traumatic lumbar puncture from SAH, the patient’s cerebrospinal
fluid should be spun and the supernatant observed for xanthochromia. The yellowish
pigmentation is secondary to the metabolism of hemoglobin to pigmented molecules of
oxyhemoglobin and bilirubin, a process that takes approximately 12 hours to occur.
Post Dural Puncture Headache (PDPH) is the most common complication of lumbar
puncture, occurring in up to 40% of patients. The amount of time a patient remains
recumbent after lumbar puncture does not appear to affect the incidence of headache.
Certain factors have been implicated as causes of PDPH, including the size or diameter
of the spinal needle, the orientation of the bevel during the procedure, and the amount
of fluid withdrawn. Smaller-diameter needles will cause less leakage, and it is
postulated that inserting the needle with the bevel up (i.e., bevel pointing up when the
patient is in the lateral position) will minimize damage to the dural fibers. Using
atraumatic needles or pencil-point needles (e.g., Whitaker or Sprotte) has also been
shown to significantly reduce the incidence of PDPH. Most PDPH headaches resolve
spontaneously within a few days with bed rest and mild analgesics. For severe
headaches lasting more than 24 hours, an epidural blood patch (autologous blood clot)
will relieve the headache in the majority of patients.
Trigeminal neuralgia is characterized by paroxysms of severe unilateral pain in the
trigeminal nerve distribution lasting only seconds, with normal findings on neurologic
examination. There is no pain between paroxysms. Treatment can be medical or
surgical. Carbamazepine is a very effective treatment. If it fails, the patient is unlikely
to have trigeminal neuralgia.
Delirium can be defined as acute cognitive dysfunction secondary to some underlying
medical condition. Terms that have been used interchangeably with delirium include
acute organic brain syndrome, acute confusional state, reversible cerebral dysfunction,
metabolic encephalopathy, toxic encephalopathy, and febrile delirium. The word
delirium is derived from the Latin delirare, which literally means “to go out of the
furrow” (lira, Latin “furrow”), but is used figuratively to mean crazy or deranged.
Recreational and prescribed drugs are responsible for most cases of acute delirium.
Among the elderly, medications are the most common cause of delirium, accounting
for 22% to 39% of cases.
The most common metabolic disorder causing acute organic brain syndrome is
diabetes mellitus. Hypoglycemia is the most common and readily reversible cause of
acute confusion in the diabetic patient. Other causes of acute cognitive impairment in
the diabetic patient are hyperglycemia, hyperosmolarity, and acid-base abnormalities.
Acute delirium occasionally can be the first manifestation of an intracranial spaceoccupying lesion such as a subdural hematoma, tumor (especially frontal lobe), or
hydrocephalus. The size and location of the lesion determine whether focal neurologic
findings are present.
272
834. One of the hallmarks of acute delirium is:
a. auditory, but not visual, hallucinations.
b. inability to “catnap” during the day.
c. paucity of emotions.
d. remote memory impairment.
e. short-term memory impairment.
835. In a patient with delirium, the EEG:
a. is helpful in less than 50% of cases.
b. is almost never normal, showing diffuse bilateral slowing.
c. is useless.
d. may show rapid focal spikes.
e. shows sleep abnormalities, but is normal during wakefulness.
836. In a patient with Alzheimer’s dementia, the cortical atrophy is most prominent in the:
a. cerebellum.
b. frontal lobes.
c. occipital lobes.
d. parietal lobes.
e. temporal lobes.
837. The drug of choice to treat agitated dementia is:
a. chlorpromazine (Thorazine®).
b. diazepam (Valium®).
c. haloperidol (Haldol®).
d. hydroxyzine (Atarax®).
e. lorazepam (Ativan®).
838. A 57-year-old has progressive dementia and loss of balance. He smells of urine and is incontinent
as you examine him. He most likely has:
a. bovine spongioform encephalopathy (Mad Cow Disease).
b. Creutzfeldt-Jakob disease.
c. normal pressure hydrocephalus.
d. senile dementia, Alzheimer's type.
e. Wernicke-Korsakoff syndrome.
839. Current recommended treatment for Bell’s palsy is:
a. acyclovir 400 mg five times per day for 10 days.
b. cold packs.
c. prednisone 1 mg/kg/day for 5 days and then tapered over the next 5 days and acyclovir 400 mg
five times per day for 10 days.
d. prednisone 1 mg/kg/day for 5 days, with or without taper.
e. surgical ablation.
840. Concerning the cranial nerves:
a. cranial nerve III injury causes a dilated pupil due to loss of parasympathetic nerve fiber supply.
b. cranial nerve III injury will result in diplopia on attempted lateral gaze.
c. cranial nerve IV supplies the lateral rectus muscle.
d. cranial nerve V injury causes deafness.
e. cranial nerve VI damage will often lead to head tilt.
273
834. e
th
Rosen 5 ,
Chapter 98,
p. 1471
835. b
Rosen 5th,
Chapter 98,
p. 1475
836. e
Rosen 5th,
Chapter 98,
p. 1477
837. c
Rosen 5th,
Chapter 98,
p. 1483
838. c
Rosen 5th,
Chapter 98,
p. 1481-1482
839. c
Rosen 5th,
Chapter 99,
p. 1489
840. a
Rosen 5th,
Chapter 99,
p. 14861487, Table
99-1
One of the hallmarks of delirium is impairment in short-term memory, with inability to
learn and assimilate new information. Remote memory, or memory of past events, is
usually preserved. Thought processes and speech may be disorganized. The delirious
patient has a reduced capacity to modulate fine emotional expression and may
demonstrate emotional lability. Characteristically, the sleep-wake cycle is reversed
because patients sleep during the day and are awake throughout the night. The
delirious patient may experience visual, auditory, tactile, gustatory, or olfactory
hallucinations, in contrast to patients with acute functional psychosis, who typically
experience only auditory hallucinations.
Although rarely practical in the emergency setting, the EEG can be a valuable
diagnostic tool in determining the presence of delirium. A normal EEG result is
incompatible with severe delirium; bilateral diffuse symmetric abnormalities are a
relatively consistent feature. In most cases the EEG abnormality consists of relative
generalized slowing with or without superimposed fast activity.
On a broad scale there is cortical atrophy most prominent in the temporal and
hippocampal regions, caused by progressive synaptic and neuronal loss in the cerebral
gray matter. This is generally followed by loss of white matter (subcortical atrophy).
Atrophy secondary to neuronal death is an important manifestation of Alzheimer’s
disease.
Occasionally medications are needed for symptomatic treatment of agitation, sleep
disturbance, and depression. These patients typically do not improve with anxiolytics.
Agitation can be controlled with a small dose of the butyrophenone haloperidol
(Haldol®). The cardiovascular toxicity of this drug is minimal, and it is well tolerated
in elderly patients.
The classic triad of progressive dementia, ataxia, and urinary incontinence (Wacky,
Wobbly, and Wet) occurs in patients with NPH, which affects younger patients than
does primary degenerative dementia. More than half of the reported cases involve
individuals less than 60 years of age. Hydrocephalus secondary to prior head trauma
or infection has a more favorable prognosis than primary hydrocephalus.
Treatment of Bell’s palsy is controversial but most practitioners use prednisone for
anti-inflammatory effect at 60 mg PO daily or 1 mg/kg/day for 5 days and then tapered
over the next 5 days, along with acyclovir 400 mg five times per day for 10 days and
follow-up with either ENT or neurologic consultation. The prognosis is generally
good for total recovery, but patients with total paralysis are at increased risk of longterm or permanent paralysis and should be seen in follow-up within 2 to 3 days, and
patients with incomplete paralysis instructed to return if the weakness becomes total
paralysis.
Cranial nerve III (oculomotor nerve) controls all function of extraocular muscles
except the superior oblique (CN IV, trochlear nerve) and the lateral rectus (CN VI,
abducens nerve). CN III also controls pupillary constriction via parasympathetic
innervation and upper lid elevation by the levator palpebrae. Patients will often
compensate for CN IV compression by head tilt. Memory device for ocular nerves
LR6SO4 all others 3.
274
841. You are attempting to clinically differentiate an acoustic neuroma from Ménière’s disease. The
finding more suggestive for an acoustic neuroma is:
a. asymmetric hearing loss.
b. balance problems.
c. intermittent ringing in the ears.
d. vertigo.
e. vomiting.
842. The primary pathology in a patient who refluxes fluid through the nose when he tries to swallow is:
a. CN V.
b. CN VII.
c. CN X.
d. CN XI.
e. CN XII.
843. You are evaluating a 36-year-old woman for a complaint of visual disturbance and “colors looking
funny.” Her eye examination is completely normal until you show her the bottle-top on a
cycloplegic agent. With her right eye, she says it is “bright red.” With her left eye, she says it
looks like it’s “covered with wax.” You are certain she has optic neuritis, so arrange for:
a. emergent double-contrast brain CT.
b. high-dose intravenous immunoglobulin therapy.
c. continuous mannitol infusion.
d. hyperbaric oxygen therapy.
e. urgent neurologic and ophthalmologic follow-up.
844. The most consistent finding in patients with a cauda equina syndrome is:
a. absent anal wink.
b. absent bulbocavernosus reflex.
c. low back pain.
d. urinary incontinence.
e. urinary retention.
845. Spinal subarachnoid hemorrhage:
a. can present like an intracerebral subarachnoid bleed.
b. cannot be diagnosed with lumbar puncture, as the bleed is extradural.
c. causes a painless paraplegia.
d. is best diagnosed using contract CT scan.
e. is usually the result of a patient being placed on anticoagulants.
846. Guillain-Barré syndrome is the most common cause of demyelinating polyneuropathies. It is
usually recognized through the findings of progressive symmetric:
a. distal motor weakness and hyperreflexia.
b. lower extremity weakness more than upper extremity weakness and hyperreflexia.
c. proximal and distal musculature weakness worse in the lower extremities, and hyporeflexia.
d. proximal motor weakness and hyperreflexia.
e. upper extremity weakness more than lower extremity weakness and hyporeflexia.
275
841. b
th
Rosen 5 ,
Chapter 99,
p. 1491
842. c
Rosen 5th,
Chapter 99,
p. 1486,
Table 99-1
843. e
th
Rosen 5 ,
Chapter 181,
p. 2553
844. e
Rosen 5th,
Chapter 100,
p. 1499
845. a
Rosen 5th,
Chapter 100,
p. 1502
846. c
Rosen 5th,
Chapter 101,
p. 1508
Asymmetric sensorineural hearing loss has few causes other than acoustic neuroma.
Ménière’s disease may present a diagnostic dilemma because it can be asymmetrical.
Ménière’s disease may be differentiated from acoustic neuroma in that the tinnitus of
Ménière’s disease is usually intermittent, while the tinnitus of acoustic neuroma is
typically continuous. In addition, patients with Ménière’s disease typically describe
true vertigo, whereas patients with an acoustic neuroma are more likely to describe
imbalance or dysequilibrium.
Injury to the vagus nerve causes unilateral loss of palatal elevation: Patients complain
that on drinking liquids the fluid refluxes through the nose.
Approximately 30% of patients presenting with acute optic neuritis will develop
multiple sclerosis within 5 years. In an initial study of patients with acute optic
neuritis, treatment with a 3-day course of IV methylprednisolone reduced the rate of
development of multiple sclerosis over a 2-year period. However, 5-year follow-up of
this same patient cohort revealed no significant differences among treatment groups in
the development of multiple sclerosis. Use of oral steroids for hastening optic neuritis
is controversial. The Optic Neuritis Study Group had shown an increased risk of optic
neuritis recurrences in those patients treated with oral prednisone. However, a recent
randomized and controlled study of high-dose oral methylprednisolone in acute optic
neuritis showed improved recovery from optic neuritis at 1 and 3 weeks, but no effect
at 8 weeks or on subsequent attack frequency. Long-term visual outcome is no
different than observation alone.
The cauda equina (“horse’s tail”) is the name given to the lumbar and sacral nerve
roots that continue on within the dural sac caudal to the conus medullaris. The
etiology of the cauda equina syndrome is usually a ruptured, midline intervertebral
disk, most commonly occurring at the L4-L5 level. Tumors and other compressive
masses may cause the syndrome as well. Patients generally present with progressive
symptoms of fecal or urinary incontinence, impotence, distal motor weakness, and
sensory loss in a saddle distribution. Muscle stretch reflexes may also be reduced.
The presence of urinary retention is the single most consistent finding, with a
sensitivity of 90%. Low back pain may or may not be present.
Patients with spinal subarachnoid bleed present with the paroxysmal onset of
excruciating back pain at the level of the hemorrhage. This pain may also be in a
radicular distribution or into the flank. Patients may complain of headache and exhibit
cervical rigidity if the blood migrates into the intracranial subarachnoid space
simulating an intracranial subarachnoid hemorrhage. The diagnostic study of choice is
the MRI. Lumbar puncture also confirms the diagnosis of blood in the CSF.
The majority of patients seek treatment days to weeks after resolution of a respiratory
or gastrointestinal illness and present in the ED with progressive, symmetric weakness
of proximal and distal musculature. Signs and symptoms are worse in the lower
extremities and are associated with diminution or loss of deep tendon reflexes, variable
sensory findings, and sparing of the anal sphincter. Urinary retention from autonomic
dysfunction may occur, contributing to a clinical picture easily mistaken for a spinal
cord lesion or conus medullaris syndrome.
276
847. You are seeing a 67-year-old man in whom you suspect Guillain-Barré syndrome. His vital
capacity is adequate at 3 liters. Another way to monitor impending respiratory failure is to follow
his:
a. anal wink.
b. biceps strength.
c. bulbocavernosus reflex.
d. neck muscle extensors.
e. triceps strength.
848. Patients with distal symmetric polyneuropathies:
a. get numbness in their fingertips before lower extremity numbness reaches their knees.
b. get numbness on the tops of their feet before numbness reaches the plantar surface.
c. have weak foot dorsiflexion as their first motor sign.
d. improve transiently with non-steroidal anti-inflammatory treatment.
e. lose their ankle-jerks before they develop footdrop.
849. Select the correct pairing for the cause of upper extremity mononeuropathies:
a. Bridegroom’s palsy = ulnar nerve.
b. Guyon’s canal = median nerve.
c. LOAF weakness = median nerve.
d. Saturday night palsy = ulnar nerve.
e. Tardy palsy = radial nerve.
850. The most striking feature of a complete common peroneal mononeuropathy is:
a. dorsal foot fasciculations.
b. footdrop.
c. great toe gangrene.
d. loss of ankle jerk.
e. total foot paresthesias.
851. The combination of weakness and sensory changes is found in patients with:
a. amyotrophic lateral sclerosis (ALS).
b. Guillain-Barré syndrome.
c. Lambert-Eaton myasthenic syndrome.
d. myasthenia gravis.
e. poliomyelitis.
852. Which statement is true concerning the edrophonium test, used in helping to differentiate
myasthenic crisis from cholinergic crisis.
a. A maximum dose of 5 mg can be given intravenously.
b. An intravenous test dose of 1 to 2 mg followed by muscle fasciculations and respiratory
depression demonstrates an allergic reaction and further edrophonium administration is
contraindicated.
c. Dramatic improvement of symptoms within 90 seconds is proof of cholinergic crisis.
d. The test is “graded” by measuring the distance between the upper eyelid and lower eyelid in the
most severely affected eye before and after intravenous edrophonium.
e. Edrophonium is a short-acting acetylcholinesterase stimulator.
277
847. d
th
Rosen 5 ,
Chapter 101,
p. 1509
848. a
th
Rosen 5 ,
Chapter 101,
p. 1510
849. c
Rosen 5th,
Chapter 101,
p. 1513
850. b
Rosen 5th,
Chapter 101,
p. 1517
851. b
Rosen 5th,
Chapter 101,
p. 15081509, 1518
Chapter 102,
p. 1522, 1523
852. d
Rosen 5th,
Chapter 102,
p. 1523
In patients with possible Guillain-Barré Syndrome who have normal pulmonary
function, extensor neck strength can be monitored to predict impending ventilatory
failure.
Distal symmetric polyneuropathies are the most common type of peripheral neuropathy
seen in emergency practice, with the preponderance of cases occurring in diabetics. As
the process advances, the plantar surfaces of both feet will become dysesthetic before
the dorsum of either foot is involved. Weakness of dorsiflexion of the big toe is
usually the first motor sign, followed by weakness of foot dorsiflexion, foot drop, loss
of ankle jerks, and later a “steppage gait.” Sensory loss continues to move proximally,
and before it reaches the knees, the fingertips are usually involved.
Most radial mononeuropathies are due to so-called “Saturday night palsies,” derived
from the association of improper positioning of the arm during deep, commonly
inebriated sleep. Consequently, the radial nerve is trapped for a prolonged period
between the humeral shaft and some firm surface, causing an external compression
mononeuropathy. “Bridegroom’s palsy” is another eponym for radial
mononeuropathy, so named because the bride’s head resting on the bridegroom’s arm
during sleep may compress the radial nerve. A relatively unique feature of the ulnar
nerve is its propensity to develop “tardy ulnar palsy” occurring years after a traumatic
event. Compression of the ulnar nerve within Guyon’s canal is rare, but when it
occurs, it will affect all of the ulnar intrinsics and all the interossei. Median nerve
motor involvement in carpal tunnel syndrome is confined to the median intrinsics,
which innervate the Lumbricals (flexion of the MCP joints), and power thumb
Opposition, Abduction, and Flexion, therefore known as the LOAF muscles.
The most striking feature of a complete common peroneal mononeuropathy is foot
drop caused by weakness of foot dorsiflexion. At testing, the everters of the foot are
also weak, but the inverters, which are innervated by the tibial nerve, remain strong.
This may be the single most reliable feature distinguishing sciatic from common
peroneal mononeuropathy.
Guillain-Barré syndrome is a sensorimotor polyneuropathy. Amyotrophic lateral
sclerosis results from a degeneration of the motor neuron without sensory involvement.
Poliomyelitis affects the anterior horn cells and results in lower motor neuron disease
without sensory involvement. Muscular weakness and fatigability are the hallmarks of
myasthenia gravis, but there are no sensory losses. The Lambert-Eaton myasthenic
syndrome affects both nicotinic and muscarinic receptors. With repeated stimulation
the amount of ACh in the synaptic cleft increases, leading to an increase in strength,
the opposite of that seen with MG.
The edrophonium (Tensilon®) test is performed by measuring the distance from the
upper to the lower eyelid in the most severely affected eye before and after intravenous
administration of the short-acting AChE blocking agent edrophonium. An IV test dose
of 1 to 2 mg is given first. Muscle fasciculations and respiratory depression within a
few minutes suggests that the muscle weakness is related to a cholinergic crisis, and
further edrophonium administration is contraindicated. If no adverse reaction is found,
and the patient does not dramatically improve in 30 to 90 seconds, a second dose of 3
mg is given. If there is still no response, a final dose of 5 mg is given for a total
maximum dosage of 10 mg in order to demonstrate benefit in the face of a presumed
myasthenic crisis.
278
853. Classic features of botulism would include:
a. ascending paralysis.
b. bowel and bladder incontinence
c. difficulty swallowing.
d. pinpoint pupils.
e. sore throat.
854. You are performing lumbar puncture on a 29-year-old woman with the “worst headache of her
life.” She is in the left lateral decubitus position. You recognize that:
a. a normal CSF protein is up to 45 mg/dl.
b. a normal opening pressure is 200 to 300 mmH2O.
c. an abnormal closing pressure must be accounted for.
d. normal CSF contains as many as 10 WBCs / mm3.
e. the CSF to serum glucose ratio is normally 0.4 to 1.
855. When peripheral cell counts are normal, the cerebrospinal fluid from a traumatic lumbar puncture
should contain around 1 WBC per:
a. 400 RBCs.
b. 500 RBCs.
c. 700 RBCs.
d. 1000 RBCs.
e. 1200 RBCs.
856. The vast majority of aseptic meningitis in the United States is caused by:
a. adenovirus.
b. arbovirus.
c. cytomegalovirus.
d. enterovirus.
e. herpes virus.
857. Your hospital’s infection control nurse notifies you that the infant you admitted with meningitis is
growing meningococcus from both blood and cerebrospinal fluid cultures. You know that
prophylaxis with rifampin should be mandatory for:
a. daycare personnel where the child spent 6 hours, 2 days prior to presentation.
b. emergency department nursing personnel,
c. paramedics who performed mouth-to-mouth prior to intubating the child.
d. the resident who performed the spinal tap.
e. all of the above.
858. Surgery for intracerebral hemorrhage is generally not indicated, although it has been reported to be
life saving in selective cases of bleeding in the:
a. brainstem.
b. cerebellum.
c. pons.
d. putamen,
e. thalamus.
279
853. c
th
Rosen 5 ,
Chapter 102,
p. 1525
854. a
th
Rosen 5 ,
Chapter 103,
p. 1534
855. c
Rosen 5th,
Chapter 103,
p. 1533
856. d
th
Rosen 5 ,
Chapter 103,
p. 1528
857. c
th
Rosen 5 ,
Chapter 103,
p. 1538
858. b
Rosen 5th,
Chapter 95,
p. 1443
The classic feature of botulism is a descending symmetric paralysis. Dysphagia,
diplopia, and dysarthria occur early. The toxin inhibits cholinergic output, leading to
constipation and urinary retention. There is no pain. Pupils are often dilated and
nonreactive.
The normal CSF protein in adults ranges from 15 to 45 mg/dL. An elevated CSF
protein, usually higher than 150 mg/dL commonly occurs with acute bacterial
meningitis. CSF glucose is normally in a ratio of 0.6 to 1 to the serum glucose, except
with marked systemic hyperglycemia, when the ratio is closer to 0.4 to 1. The normal
CSF pressure in an adult varies from 50 to 200 mm H2O. This may increase severalfold when in the sitting position. Normal adult CSF contains no more than 5
leukocytes/mm3 with at most one granulocyte (PMN). Closing pressure is not
necessary.
When peripheral cell counts are normal, the CSF from a traumatic lumbar puncture
should contain around 1 WBC per 700 RBCs.
Viral meningitis may likewise be caused by a variety of etiologic agents.
Enteroviruses are statistically encountered most commonly. Unfortunately, precise
definition of the etiologic agent is often impossible.
Health care workers are not at any increased risk for the disease and do not require
prophylaxis unless they have had direct mucosal contact with the patient’s secretions,
as might occur during mouth-to-mouth resuscitation, endotracheal intubation, or
nasotracheal suctioning. The general rule is 2 hours within 2 feet of a clinically ill
patient to require prophylaxis.
Surgery is not beneficial in most cases of intracerebral hemorrhage. Surgery is more
efficacious in patients with cerebellar hemorrhage. The clinical course in cerebellar
hemorrhage is notoriously unpredictable. Patients with minimal findings may
deteriorate suddenly to coma and death with little warning. For this reason, most
neurosurgeons will consider emergency surgery for patients with cerebellar
hemorrhage within 48 hours of onset.
280
859. The ascending reticular activating system (ARAS) is located in the:
a. cerebellum.
b. hippocampus.
c. hypothalamus.
d. pons.
e. thalamus.
860. Coma preceded by delirium suggests:
a. alcohol intoxication.
b. endogenous toxins, such as ammonia.
c. hypoglycemia.
d. hypoxemia.
e. stroke.
861. The paramedics have brought you a 43-year-old man who is completely unresponsive and smells
heavily of fermented beverage. The recommended method of noxious stimulus to arouse him is:
a. inserting a cotton swab into his posterior nasopharynx.
b. pinching his nipples.
c. squeezing his fingernail beds.
d. twisting his eyebrows.
e. yelling in his ears
862. Dysconjugate gaze in the vertical plane generally results from:
a. alcohol intoxication.
b. barbiturate intoxication.
c. hypoglycemic coma.
d. hypoxemia.
e. pontine or cerebellar lesions.
863. The cardinal sign of inner ear disease is:
a. abnormal nystagmus.
b. ataxia.
c. dizziness.
d. dysdiadochokinesis.
e. hearing loss.
864. A feature that is characteristic of central vertigo is:
a. brief duration.
b. gradual onset.
c. hearing loss.
d. severe intensity, especially with head movement.
e. tinnitus.
865. An 84-year-old woman with a history of coronary artery disease complains of new onset of brief
episodes of dizziness, dysarthria, ataxia, and double vision. She has a very ataxic gait, but an
otherwise nonfocal exam. Her most likely diagnosis is:
a. benign positional vertigo.
b. cerebellar hemorrhage.
c. Ménière’s disease.
d. purulent labyrinthitis.
e. vertebrobasilar insufficiency.
281
859. d
th
Rosen 5 ,
Chapter 15,
p. 137
860. a
Rosen 5th,
Chapter 15,
p. 140
861. a
th
Rosen 5 ,
Chapter 15,
p. 141
862. e
th
Rosen 5 ,
Chapter 15,
p. 141
863. a
Rosen 5th,
Chapter 13,
p. 125
864. b
Rosen 5th,
Chapter 13,
p. 125
865. e
Rosen 5th,
Chapter 13,
p. 127
The ascending reticular activating system (ARAS) is the neuroanatomic structure
responsible for arousal. It is located in the pons. The ARAS acts as a gateway for
sensory and somatic stimuli to the cerebral cortex and as a trigger for arousal from
sleep. When the ARAS is dysfunctional, coma occurs because the cerebral cortex
cannot be aroused.
Coma preceded by delirium suggests alcohol intoxication, sedative withdrawal, toxic
psychosis, or encephalitis. Coma preceded by confusion without delirium suggests
hypoglycemia, endogenous toxins, or drug overdose.
A variety of noxious stimuli have been used, but perhaps the best stimulus is to tickle
the posterior nasopharynx with a cotton swab. This is not harmful or painful, does not
leave a mark, and can be reproduced accurately by subsequent examiners.
Dysconjugate gaze in the vertical plane, called skew deviation, generally results from
pontine or cerebellar lesions. Dysconjugate gaze in the horizontal plane is normally
observed in drowsiness and in various sedated states including alcohol intoxication,
with parallel ocular axes reemerging when the patient awakens or slips deeper into
coma.
Abnormal nystagmus is the cardinal sign of inner ear disease and the principal
objective evidence of abnormal vestibular function. The abnormal jerk nystagmus of
inner ear disease consists of slow and quick components. The eyes slowly move in the
direction of the diseased, hypoactive ear and then quickly jerk back to the midline.
Nystagmus caused by vestibular disease tends to be unidirectional and
horizontorotatory. If the nystagmus is vertical, a central lesion (either brainstem or
cerebral) is usually the cause.
The main features of central vertigo are gradual onset; mild intensity; duration of
weeks to months; horizontal, rotatory, or vertical nystagmus (different directions in
different positions); little change with head position; associated with more than one
position; associated neurologic findings; and absence of auditory findings.
Vertebrobasilar insufficiency (VBI) should be considered in any patient of advanced
age who has isolated new-onset vertigo without an obvious cause. The diagnosis is
more likely in patients with a history of atherosclerosis. Initial episodes usually last
seconds to minutes. Headache may be present. Neurologic symptoms may include
dysarthria, ataxia, weakness, numbness, and double vision. Tinnitus and deafness are
uncommon. Neurologic deficits are usually present but initial neurologic examination
may be normal. Because of the possibility of progression of new-onset VBI in the first
24–72 hours, hospital admission and consideration of early MRA are probably
warranted even in the stable patient.
282
13.0 Obstetrics and Gynecology
866. There is an increased risk of candidal vaginitis in a woman:
a. with diabetes.
b. with frequent bladder infections.
c. who is menstruating.
d. who has gone through menopause.
e. who has multiple sex partners.
867. You have just diagnosed a 23-year-old woman with trichomonas vaginitis and wish to treat her with
oral metronidazole. You know also know that:
a. concomitant ingestion of ethanol inactivates the medication.
b. her partner requires treatment.
c. oral metronidazole is contraindicated if she has a near-term pregnancy.
d. there are thus far no reports of trichomonas being resistant to metronidazole.
e. trichomonas can become very aggressive during pregnancy.
868. Chlamydial infections:
a. are best treated with ceftriaxone (Rocephin®).
b. are easily diagnosed because of copious discharge.
c. are frequent causes of infertility.
d. present exclusively as cervicitis or pelvic inflammatory disease.
e. should not be treated unless infection has been proven by culture or assay.
869. Which statement about pelvic inflammatory disease (PID) is true?
a. Symptoms usually begin just before the patient’s menstrual period.
b. PID is common in pregnancy.
c. Chronic PID is nearly always due to Neisseria gonorrhoeae.
d. Successful outpatient treatment of PID involves ceftriaxone (Rocephin®) 125mg IM and twicedaily doxycycline for 7 days.
e. Irregular bleeding is reported in about 40% of women diagnosed with PID.
870. Uterine fibroids are associated with:
a. Caucasian race.
b. frequent episodes of cystitis.
c. IUD use.
d. menorrhagia.
e. unexplained fevers.
871. A 37-year-old woman complains of a single genital ulcer for three days.
a. Absence of vaginal discharge reliably rules out granuloma inguinale.
b. Herpes can easily be ruled out with a negative Tzanck prep.
c. Lyme disease must be in your differential.
d. Non-treponemal antibody tests (VDRL and RPR) are often negative at this stage, so you cannot
reliably rule out syphilis.
e. The borders of the ulcer are ragged and the inguinal nodes are tender and swollen, so you can rule
out chancroid.
283
866. a
th
Rosen 5 ,
Chapter 93,
p. 1396
867. b
th
Rosen 5 ,
Chapter 174,
p. 2449
868. c
th
Rosen 5 ,
Chapter 93,
p. 1395
869. e
Rosen 5th,
Chapter 93,
p. 1397-1398
Table 93-4
870. d
Rosen 5th,
Chapter 28,
p.
871. d
Rosen 5th,
Chapter 93,
p. 1394
Candida albicans, a yeast-like organism, is probably the most common cause of
vaginitis. Predisposing factors include antibiotic administration, pregnancy, oral
contraceptives, steroid administration, restrictive clothing, and diabetes.
Metronidazole (Flagyl®) is a Category B drug in pregnancy, and contraindicated in
first trimester, but can be used in later trimesters if the benefits outweigh the risk.
Trichomonas is rarely aggressive during pregnancy.
Chlamydia trachomatis is an obligate, intracellular parasite that has the features of both
a virus and a bacterium. It is now the most common of all STDs and is one of the
principal causes of infertility in women. An estimated 1 in 10 adolescent girls and 1 in
20 women of reproductive age are infected. In addition to causing LGV, acute urethral
syndrome, and PID, the organism causes mucopurulent cervicitis that is difficult to
clinically distinguish from that caused by N. gonorrhoeae. Chlamydia causes
nongonococcal urethritis and epididymitis in men. Men may also be asymptomatic
carriers of the infection. Azithromycin, 1 g orally in a single dose, is the preferred
treatment. Chlamydial infections also respond to doxycycline, 100 mg orally twice a
day for 7 days; or an erythromycin base 500 mg orally four times daily for 7 days.
Typically, acute PID is manifested by an increased vaginal discharge, pelvic pain, or
symptoms of urethritis, beginning 3 to 5 days after menstruation. A history of
antecedent irregular bleeding is elicited in 40% of cases. N. gonorrhoeae and
Chlamydia organisms together account for approximately 80% of all cases of PID.
Treatment: ceftriaxone, 250 mg IM OR cefoxitin, 2 g IM, + probenecid 1 g po AND
doxycycline, 100 mg po bid for 10–14 days OR ofloxacin 400 mg po bid for 14 days
AND EITHER clindamycin 400 mg po qid for 14 days OR metronidazole 500 mg po
bid for 14 days.
Leiomyomas (fibroids) are benign tumors of muscle cell origin and are the most
frequently occurring pelvic tumor. They are found in one of four white women and in
one of two black women. They decrease in size during menopause, and enlargement is
seen early in pregnancy and, in some cases, oral contraceptive use. Up to 30% of
patients with leiomyomas experience pelvic pain and abnormal bleeding.
Pain and the puttylike consistency of the ulcers distinguish chancroid from other
causes of genital ulcers. A painful unilateral inguinal bubo develops in 50% of
patients. In primary syphilis, a small papule develops at the site of inoculation 10 to 90
days after exposure, which then becomes a painless, indurated ulcer, the classic
chancre, which heals spontaneously in 4 to 5 days. Serologic tests are often negative at
this stage. Tzanck slide preparation reveals the characteristic multinucleated giant
cells of herpes only about 50% of the time.
284
872. A 19 year-old college student presents with a first episode of Herpes genitalis.
a. Counseling should involve warnings about increased risk of PID.
b. Early treatment with acyclovir will prevent future outbreaks.
c. Famcyclovir intravenously will successfully prevent recurrences.
d. Systemic analgesics may be needed.
e. Systemic antibiotics are mandatory to prevent generalized dissemination.
873. A woman with pyelonephritis can safely be treated at home unless she:
a. has a prior history of hospitalization for pyelonephritis.
b. has an allergy to sulfa.
c. has ureteral obstruction due to stone.
d. is over age 45.
e. lives alone.
874. A previously healthy 56 year-old perimenopausal woman presents with dysfunctional uterine
bleeding. Her pregnancy test is negative, and pelvic examination reveals no pathology. Ultrasound
shows no structural abnormality.
a. Anovulatory bleeding is usually heavy, with long intervals between menstrual periods.
b. Coagulopathy screen (PT, aPTT, bleeding time) is mandatory.
c. Fallopian carcinoma still needs to be ruled out.
d. NSAIDs should be avoided, as they tend to worsen bleeding.
e. Pap smear should reveal the cause of bleeding.
875. Chlamydial organisms cause:
a. chancroid.
b. condyloma accuminata
c. granuloma inguinale.
d. lichen sclerosis et atrophicus.
e. lymphogranuloma venereum.
876. A 17 year-old female complains of vaginal itching. She has never been sexually active. She has
some mild redness around the introitus. Pregnancy test, wet mount, and KOH prep are negative.
a. Environmental exposures, such as douches, soaps, and body creams, should be eliminated.
b. Gynecologic consultation is mandatory.
c. She requires broad-spectrum antibiotic coverage for presumed occult infection.
d. She should stop drinking grapefruit juice, as she is developing an allergic dermatitis.
e. You can reassure the patient there is no pathology and let her go home.
877. For “Morning after” pills to be successful in preventing pregnancy, they must be taken within what
period of time after intercourse?
a. 12 hours
b. 24 hours
c. 36 hours
d. 72 hours
e. 7 days
285
872. d
th
Rosen 5 ,
Chapter 93,
p. 1392
873. c
Rosen 5th,
Chapter 94,
p. 1410
874. a
Rosen 5th,
Chapter 28,
p. 229
875. e
Rosen 5th,
Chapter 93,
p. 1393
876. a
Rosen 5th,
Chapter 93,
p. 1397
877. d
Rosen 5th,
Chapter 61,
p. 860
Box 61-3
Treatment is not curative. Multiple antiviral agents and regimens are available.
Systemic antiviral agents provide partial control of the signs and symptoms and
accelerate healing of the lesions, but do not affect the frequency or severity of
recurrences. Topical therapy is not effective. Patients with severe disease may need
hospitalization and intravenous therapy.
Outpatient therapy for selected patients with pyelonephritis (young, otherwise healthy,
able to keep down fluids and antibiotics) is as safe and effective, and considerably less
expensive, than comparable patients treated on an inpatient basis. Hospitalization is
required in the presence of (1) clinical toxicity, (2) inability to take oral medications,
(3) an immunocompromised state, (4) pregnancy, or (5) urologic abnormalities.
In nonpregnant patients, most vaginal bleeding is related to dysfunctional
(anovulatory) uterine bleeding. This is usually managed with estrogen
supplementation in consultation with a gynecologist. Other causes, such as neoplasm,
suspected endometriosis, or ovarian cysts, are referred to a gynecologist. Before
discharge, it is important to assess the patient’s tolerance of the hemorrhage by
measuring vital signs, including orthostatics. A baseline hemoglobin/hematocrit is
recommended. Finally, other medical causes, such as hypothyroidism, hemostasis
disorders, or anticoagulant therapy, must be considered.
Lymphogranuloma venereum (LGV) is an uncommon STD caused by C. trachomatis.
The initial lesion is a small, shallow, painless, evanescent vesicle, pustule, or ulcer that
occurs on the labia, cervix, or penis 7 to 21 days after exposure. The patient usually
does not notice the lesion. Two to 12 weeks after exposure, localized inguinal lymph
nodes develop that can enlarge, coalesce, and ulcerate impressively. The “groove
sign” may appear to be created by the proliferation of inguinal lymphadenopathy
superior and inferior to the inguinal ligament.
Chemical irritant vaginitis commonly occurs after the use of feminine hygiene
deodorants, douches, or medications not intended for the vagina. Diagnosis is by
history. Stopping the use of the offending agent usually is sufficient treatment.
Pregnancy prophylaxis must be initiated within 72 hours of the sexual encounter in
order to be most effective. Currently accepted therapy is the birth control pill Ovral
(norgestrel plus ethinyl estradiol) 2 tablets orally initially and 2 tablets 12 hours later.
Commercial preparations, called Preven® and Plan B®, are also available.
286
878. A 25 year-old woman presents with pelvic pain and mucoid vaginal discharge. Her most recent
period ended 7 days ago. Examination shows right upper quadrant tenderness. She probably has:
a. non-infectious hepatitis.
b. cholecystitis.
c. concurrent right lower lobe pneumonia.
d. Fitz-Hugh-Curtis syndrome.
e. tubo-ovarian abscess.
879. An appropriate treatment for primary syphilis is:
a. ceftriaxone, 250 mg IM, daily for 5 days
b. doxycycline, 100 mg PO BID for 7 days
c. erythromycin, 500 mg PO QID for 7 days
d. levofloxacin 250 mg PO BID for 3 days.
e. penicillin G benzathine, 2.4 million units IM, as a single dose
880. Choose the correct statement:
a. Untreated bacteriuria in pregnancy is associated with a higher incidence of fetal morbidity.
b. Pregnancy causes increased peristalsis throughout the collecting system.
c. The prevalence of bacteriuria in women increases with pregnancy.
d. Asymptomatic bacteriuria in a pregnant woman can be observed.
e. Treatment with trimethoprim-sulfamethoxazole is contraindicated.
881. A sexually transmitted disease whose lesions have been reported to turn malignant, especially in
HIV-positive men, is:
a. chancroid.
b. condyloma accuminata.
c. gonorrhea.
d. granuloma inguinale.
e. syphilis.
882. Absolute contraindication to Emergency Department speculum and manual pelvic examination is:
a. active labor.
b. delivery less than one week prior to exam.
c. possible septic abortion.
d. third trimester bleeding.
e. vaginal discharge.
883. Choose the correct statement concerning urinary tract infection:
a. Bacteria most often enter the urinary tract via hematologic seeding.
b. UTIs in men generally begin to appear with the onset of prostatic hypertrophy.
c. A single catheterization in an outpatient setting carries a risk of infection of 5% to 10%.
d. About 10% of women with sterile bladder urine will grow 1000 to 100,000 bacterial colony
forming units (CFU) per milliliter from a midstream clean-catch specimen.
e. In men the sterility of the specimen is significantly affected by lack of cleansing.
884. Mammary thrombophlebitis (Mondor’s syndrome) is commonly associated with:
a. abscess and/or fistula.
b. cystic breast disease.
c. multiparity.
d. recent breast surgery.
e. menarche.
287
878. d
th
Rosen 5 ,
Chapter 93,
p. 1398
879. e
Rosen 5th,
Chapter 93,
p. 1393
880. a
th
Rosen 5 ,
Chapter 94,
p. 1406
881. b
Rosen 5th,
Chapter 91,
p. 1354-1355
882. d
Rosen 5th,
Chapter 175,
p. 2741
883. b
th
Rosen 5 ,
Chapter 94,
p. 1401-1403
884. d
Rosen 5th,
Chapter 83,
p. 1217
Fitz-Hugh-Curtis syndrome (gonococcal perihepatitis) is an inflammation of the liver
capsule that results in band-like adhesions between the liver and the anterior abdominal
wall. Typically the patient has a sudden onset of severe, pleuritic, sharp, right upper
quadrant pain that occurs days to weeks after symptoms of acute PID. Examination
usually reveals profound tenderness over the liver, some lower abdominal tenderness,
cervicitis, and culture evidence of PID. Laparoscopy may be required in diagnosis and
lysis of adhesions.
Benzathine penicillin G 2.4 (Rosen says “2–4”, an obvious typographical error) million
units IM in a single dose has remained the standard of care for primary syphilis.
Doxycycline 100 mg PO bid for 2 weeks may be used for allergic individuals.
Untreated bacteriuria in pregnancy is associated with a higher incidence of prematurity
and fetal morbidity. Maternal complications include a 20% to 40% incidence of acute
pyelonephritis and an increased incidence of postpartum chronic pyelonephritis. The
physiologic changes that occur within the urinary tract of pregnant women include
ureteral and renal pelvis dilatation and reduced peristalsis throughout the collecting
system. The prevalence of bacteriuria in women does not change with pregnancy.
However, in contrast to bacteriuria in nonpregnant females, bacteriuria in pregnant
women, even if they are asymptomatic, must be treated. Reasonable antibiotic choices
include amoxicillin, cephalexin, and nitrofurantoin. Some authors recommend
trimethoprim-sulfamethoxazole if used before the third trimester.
Condylomata acuminata are most often found in homosexual men but can be seen in
heterosexual men, women, and children. Because one half of HIV-positive patients
have anal warts, HIV testing is recommended. The pink-to-gray warts are a result of
hyperplastic epithelial growth and appear as vegetative papilliform growths. They may
coalesce to form a massive patch that obscures the anal verge. Squamous cell
carcinoma should be considered if the lesions are indurated. Progression to
intraepithelial neoplasia has been reported to be related to the level of
immunosuppression.
In a patient with third trimester placenta previa, instrumentation, digital examination of
the cervix, and speculum examination can provoke severe, exsanguinating hemorrhage,
and are therefore contraindicated.
Bacteria most often enter the urinary tract via ascent through the urethra and into the
collecting system. UTIs in men generally begin to appear at age 50 years, concomitant
with the onset of prostatic hypertrophy. A single catheterization in an outpatient
setting carries a risk of infection of 1% to 3%. Up to 50% of women with sterile
bladder urine grew 1000 to 100,000 bacterial colony forming units per milliliter from a
midstream clean-catch specimen. In men, the specimen is not affected significantly by
lack of cleansing or by the timing of specimen collection.
Mondor’s disease of the breast is a superficial phlebitis of the veins in the
subcutaneous tissue of the breast. This condition may occur postoperatively or after
minor trauma. The patient presents complaining of a painful induration across the
costal margin. A cord may be present. The phlebitis may be tender for several weeks.
No treatment other than analgesia is required, but spontaneous fibrosis of the vessel
often leads to retraction of subcutaneous tissues, with puckering and hardening of one
quadrant of the breast. Follow-up evaluation with a surgeon is indicated. Mondor’s
disease of the penis has also been described.
288
885. A 15 year-old woman tells you that she is 7 weeks pregnant and her boyfriend recently tested
positive for Chlamydia and she wants to be treated. She plans on carrying the pregnancy to term.
She can’t afford single-dose azithromycin, so you:
a. give her a prescription for 1 week of doxycycline 100 mg bid.
b. give her a prescription for 1 week of erythromycin 500 mg qid.
c. give her a prescription for 1 week of ofloxacin 300 mg bid.
d. refer her to a public health clinic.
e. refuse to treat her because of her age.
886. A 21 year-old woman is brought by ambulance from her dormitory room at a nearby college. She
appears ill, has a fever of 102.3oF, and a blood pressure of 74/38 mmHg. The palms of her hands
are peeling skin. She refuses a pelvic exam because “My period is on and I have a tampon.” The
organism which is MOST LIKELY causing her illness is:
a. Chlamydia trachomatis.
b. Staphylococcus aureus.
c. Streptococcus pyogenes.
d. Streptococcus viridans.
e. Yersinia enterocolitica.
887. A 28 year-old woman G5P1112 whose last period was more than 4 months ago presents with
cough, flank pain, and low-grade fever. You would expect to find which of the following as a
result of her presumed pregnancy?
a. increased blood pressure
b. decreased heart rate
c. increased temperature
d. protein, glucose, and ketones in the urine
e. mild anemia
888. A 21-year-old woman G1P0 whose last period was 36 weeks ago presents with dysuria. There is
no sign of pyelonephritis. Your most appropriate antibiotic for treatment is:
a. ampicillin.
b. ciprofloxacin.
c. doxycycline.
d. erythromycin estolate.
e. trimethoprim-sulfamethoxazole.
889. Placenta previa is characterized by:
a. high fever.
b. painful vaginal bleeding.
c. right upper quadrant fullness.
d. tender, tense uterus.
e. third trimester bleeding.
890. You begin magnesium administration in a woman with third trimester pre-eclampsia. You must
monitor her closely for signs of toxicity, which include:
a. fever.
b. hyperreflexia.
c. hypotension.
d. respiratory depression.
e. tachycardia.
289
884. b
th
Rosen 5 ,
Chapter 172,
p. 2430
885. b
Rosen 5th,
Chapter 131,
p. 1399
887. e
th
Rosen 5 ,
Chapter 171,
p. 2400-2401
888. a
th
Rosen 5 ,
Chapter 171,
p. 2430
889. e
Rosen 5th,
Chapter 175,
p. 2471
890. d
Rosen 5th,
Chapter 172,
p. 2430
Clinical diagnosis is difficult during pregnancy because cervical mucus is usually
cloudy and contains WBCs. Routine Chlamydia screening during pregnancy is
important to prevent complications of preterm labor and postpartum endometritis, both
of which are more common in patients who have chlamydial cervical infections.
Chlamydial conjunctivitis has become epidemic among infants born to mothers with
chlamydial cervical infections. In addition, neonatal pneumonia caused by Chlamydia
is common. Recommended treatment during pregnancy or breastfeeding is a 7-day
course of erythromycin or amoxicillin.
Toxic shock syndrome often occurs in menstruating women who use vaginal tampons.
Staphylococcus aureus is isolated more than 90% of the time.
The hemoglobin decreases slightly in pregnancy. The Centers for Disease Control and
Prevention defined anemia in pregnancy as less than 11 g/dl during the first and third
trimesters and less than 10.5 g/dl during the second trimester.
Pregnant women with UTI are at increased risk for pyelonephritis, and pyelonephritis
is a risk factor for preterm labor and low birth weight, as a result of hydroureter,
dilatation of the renal pelvis, and consequent urinary stasis. Pregnant patients with
asymptomatic bacteriuria identified on microscopic analysis should have a urine
culture performed and be treated if the culture is positive. Untreated, 25% will develop
symptomatic infection, while treatment will decrease the incidence of symptomatic
UTI by 80 to 90%. Symptomatic UTI requires a urine culture and antibiotic therapy.
Only 7-day regimens are recommended during pregnancy, including nitrofurantoin
(one tablet bid), ampicillin; or cephalexin. Trimethoprim-sulfamethoxazole is
relatively contraindicated in the first trimester because of anti-folate properties of
trimethoprim, and sulfonamides are contraindicated in the third trimester due to risk of
fetal hyperbilirubinemia.
The classic symptom of placenta previa is painless bright red vaginal bleeding in the
third trimester. The uterus remains soft and fetal lie is often abnormal. The initial
bleeding is often self-limited and not lethal. This bleeding usually occurs as cervical
effacement exposes the placenta. The earlier in the effacement process the bleeding
begins, the lower the placenta lies.
Magnesium administration should always be accompanied by clinical observation for
loss of reflexes (which occurs at about 10 mg/dl) or respiratory depression (which
occurs at levels over 12 mg/dl, although actual serum magnesium levels are rarely
monitored). The infusion should be stopped if signs of hypermagnesemia are seen;
such patients may require assisted ventilation. Calcium gluconate, 1 g given slowly
into a secure vein, will reverse the adverse effects of hypermagnesemia.
290
891. A 16-year-old woman G2P0020 complains of intermittent crampy right lower abdominal pain. She
thinks her last period was about 3 weeks ago, but is not certain. Her vital signs are normal. Urine
pregnancy test is positive, and quantitative beta-HCG is 1123 mIU. Transvaginal ultrasound shows
an intrauterine gestational sac, a fluid-filled cyst in the right adnexa, and a small amount of fluid in
the cul-de-sac. Your next step should be to:
a. administer RhoGAM and consult gynecology for emergent laparotomy.
b. check Rh status and discharge patient on methotrexate therapy, since she is stable.
c. refer for prenatal care; history and findings are consistent with intrauterine pregnancy and a
corpus luteum cyst.
d. obtain type and screen, CBC, and start a large-bore intravenous line in preparation for emergent
laparotomy.
e. obtain type and screen, CBC, and consult gynecology; you cannot rule out an ectopic pregnancy
based on available information.
892. A 24 year-old G2P1 female in her 39th week of pregnancy says she had a “a gush of water from my
vagina” about one hour ago. Her cervix is closed to your fingertip, but there is fluid in her vaginal
vault. Which test can verify the presence of amniotic fluid?
a. Look under a microscope at a spun specimen – white blood cell presence confirms amniotic fluid.
b. Place a drop of the fluid on filter paper or a paper towel – if a ‘halo’ appears around the drop, this
is amniotic fluid.
c. Put a drop of the fluid on a Dextrose measurement stick – if less than 60 mg/dL, this is amniotic
fluid.
d. Use a strip of nitrazine paper – pH >7.0 indicates presence of amniotic fluid.
e. Use a urine dipstick – if positive for protein, amniotic fluid is present.
893. A 35 year-old woman with a history of pregnancy-induced hypertension presents after rupture of
membranes and regular uterine contractions. She is 32-weeks pregnant by dates and size. You can
help suppress premature labor by using:
a. oxytocin.
b. prostaglandin synthase inhibitors.
c. beta-blocking agents.
d. steroids.
e. terbutaline.
894. The HELLP syndrome includes:
a. HE = hepatosplenomegaly.
b. H = hypotension.
c. EL = elevated liver enzymes
d. LL = low liver enzymes
e. LP = low protein.
895. Ectopic pregnancy:
a. can occur in normal fallopian tubes.
b. does not occur after tubal ligation.
c. is the leading cause of second trimester maternal death.
d. usually causes pain before vaginal bleeding.
e. usually causes symptomatic presentation during the first 4 weeks of gestation.
291
891. e
th
Rosen 5 ,
Chapter 172,
p. 2418
892. d
Rosen 5th,
Chapter 175,
p. 2470
893. e
th
Rosen 5 ,
Chapter 175,
p. 2469,
Table 175-4
894. c
th
Rosen 5 ,
Chapter 172,
p. 2422
895. a
Rosen 5th,
Chapter 172,
p. 2416
No single diagnostic test or combination of laboratory tests is currently considered to
have sufficient negative predictive value to completely rule out ectopic pregnancy or
abnormal intrauterine pregnancy or positive predictive value to definitively diagnose
them. Ruptured ectopic pregnancies requiring surgery have been reported with very
low or absent levels of HCG. As a result, it is risky to assume a benign course on the
basis of a low HCG level.
Nitrazine paper testing will reveal a pH of 7.1 to 7.3 typical of amniotic fluid (normal
vaginal pH in pregnancy is 3.5 to 6.0).
Tocolytic agents
Magnesium sulfate: 4–6 g bolus over 30 min, 2–4 g/hr infusion
Terbutaline: 2.5–5.0 mg PO q2–4h, 0.25–0.50 mg SC, 0.010–0.080 mg/min IV
Ritodrine: 10–20 mg PO q4h, 0.050–0.350 mg/min IV
Isoxsuprine: 20 mg PO q4h
The HELLP syndrome (an acronym for hemolysis, elevated liver enzymes, and low
platelets) is an important clinical variant of preeclampsia that has a predilection for the
multigravid patient, in contrast to the primigravida, in whom preeclampsia is more
common.
Ectopic pregnancy can occur in normal fallopian tubes and after tubal ligation. It
remains the leading cause of maternal death in the first trimester of pregnancy and is
the second leading cause of maternal mortality overall. Amenorrhea of 4 to 12 weeks
is reported in approximately 70% of cases.
292
896. A 36 year-old woman in her 28th week of pregnancy complains of swollen hands and face. Her
blood pressure is 146/90 mmHg, her BUN is 12 mg/dL, and urine protein is >1 g/L. She has:
a. acute renal failure.
b. chronic hypertension of pregnancy.
c. eclampsia.
d. gestational hypertension.
e. preeclampsia.
897. Perimortem cesarean section is recommended only when:
a. an obstetrician is available to perform the procedure.
b. fetal heart sounds are fading.
c. resuscitation of the mother has stopped.
d. the fetus is at 26 weeks of gestation or greater.
e. volume resuscitation on the mother is completed.
898. The most common cause of death in a pregnant patient with toxemia is:
a. cardiogenic shock
b. cerebral hemorrhage.
c. disseminated intravascular coagulation.
d. renal failure.
e. sepsis.
899. A woman in third trimester of pregnancy with painful, dark vaginal bleeding probably has:
a. abruptio placenta.
b. molar pregnancy.
c. placenta previa.
d. pre-eclampsia.
e. uterine rupture.
900. The most common cause of blunt abdominal trauma in pregnant women is:
a. unknown.
b. domestic violence.
c. falls.
d. motor vehicle crashes.
e. self-inflicted.
901. Expected cardiovascular changes in pregnancy include:
a. heart rate, central venous pressure, blood pressure until it normalizes at term.
b. heart rate, central venous pressure, blood pressure which normalizes near term.
c. heart rate, central venous pressure, blood pressure.
d. heart rate, central venous pressure, blood pressure which normalizes near term.
e. heart rate, central venous pressure, blood pressure which normalizes near term.
902. Initial management of the hypotensive third-trimester trauma patient should include:
a. inflation of MAST garment.
b. left lateral decubitus position.
c. right lateral decubitus position.
d. semi-Fowler’s positions when cervical spine cleared.
e. Trendelenberg position.
293
896. e
th
Rosen 5 ,
Chapter 172,
p. 2422
897. d
Rosen 5th,
Chapter 31,
p. 264
898. b
Rosen 5th,
Chapter 171,
p. 2407
899. a
th
Rosen 5 ,
Chapter 172,
p. 2420
900. d
Rosen 5th,
Chapter 31,
p. 257
901. d
th
Rosen 5 ,
Chapter 171,
p. 2401
902. b
Rosen 5th,
Chapter 171,
p. 2401
The patient with mild preeclampsia has no evidence of organ damage aside from
proteinuria and mild systolic or diastolic blood pressure elevation. Mental status
assessment, testing of reflexes, abdominal examination, liver function studies, and
coagulation studies should all yield normal results. Edema is often difficult to assess,
because pregnancy is normally associated with excess extracellular fluid and
dependent edema. The edema of preeclampsia is usually generalized, involves the face
and hands, and persists throughout the day.
Perimortem cesarean section in the ED should be performed if uterine size exceeds the
umbilicus and fetal heart tones are present. Bedside US may also be used to quickly
assess the presence of a fetal heart rate. No time should be wasted obtaining consent
for delivery. Time since maternal circulation ceased is the critical factor in fetal
outcome. Reports show that 70% of children who survive perimortem cesarean
sections are delivered in less than 5 minutes of ED arrival. Accordingly, 4 minutes are
allowed in starting the procedure. The extra minute is used for actual delivery time.
Cerebral hemorrhage is the most common cause of death in toxemia. It occurs in 60%
of patients who die after becoming eclamptic.
Vaginal bleeding occurs in 80% of patients with abruptio placentae. Blood is
characteristically dark and the amount is often insignificant, although the mother may
have hemodynamic evidence of significant blood loss. Uterine tenderness or pain is
seen in about two thirds of women; uterine irritability or contractions are seen in one
third.
The most common cause of blunt abdominal trauma is motor vehicle crash, accounting
for up to 70% of acute injuries. This is followed by falls and direct assault in
decreasing order of frequency.
Arterial blood pressure and vascular resistance decrease overall during normal
pregnancy. Arterial blood pressure decreases during the second trimester and slowly
rises during the third trimester. Cardiac output at rest in the lateral recumbent position
steadily increases during pregnancy. The changes in blood pressure and cardiac output
during pregnancy reflect the physiologic balance of the decreasing blood pressure and
vascular resistance concurrent with the increase in blood volume, maternal weight, and
basal metabolic rate.
Arterial blood pressure is lowest in the lateral recumbent position and highest when
sitting. Usually the blood pressure in the supine position is somewhere between these
two levels. Some pregnant women become hypotensive in the supine position, referred
to as the supine hypotensive syndrome. Thus a supine pregnant woman with a normal
or hypotensive brachial pressure may have an even lower uterine blood pressure.
Accurate vital signs are best obtained with the patient in the left lateral decubitus
position.
294
17.0 – Toxicologic Disorders
1001. Profound ketonuria without acidosis is caused by poisoning with:
a. ethylene glycol.
b. isoniazid.
c. isopropanol.
d. methanol.
e. salicylates.
1002. A 2 year-old male presents two hours after ingesting an unknown quantity of his mother’s
prenatal vitamins. He is vomiting and has diarrhea. You should:
a. administer a dose of activated charcoal.
b. immediately administer fluid challenges and IV deferoxamine.
c. obtain an x-ray of the abdomen.
d. obtain serum iron level.
e. obtain WBC and serum glucose studies.
1003. A 21-year-old female with a history of depression was found unconscious and brought to
the emergency department. She is comatose without focal findings, has been intubated,
and is receiving mechanical ventilation. Temperature 99.0oF; heart rate 140/min;
respiratory rate 14 (assisted); BP 80/40 mmHg. Pupils are midposition and reactive and
axillae are dry. An ECG shows sinus tachycardia with a QRS interval of 0.15 seconds.
Arterial blood gas: pH 7.42; pCO2 37, pO2 106. Your next step should be to administer:
a. glucagon.
b. physostigmine.
c. propranolol.
d. sodium bicarbonate.
e. verapamil.
1004. Police bring you a 19-year-old man who is agitated, combative; and seems to be
hallucinating. Temperature 101.4oF, heart rate 120/min, respiratory rate 24/min, BP
130/85 mmHg. His pupils are dilated and he is drenched in sweat. He has most likely
ingested:
a. diphenhydramine.
b. jimson weed.
c. methamphetamine.
d. propoxyphene.
e. Thorazine®.
1005. A 22-year-old intravenous drug abuser complains of heroin withdrawal. You would expect
to find:
a. lacrimation, miosis, yawning.
b. restlessness, hallucinations, tachycardia .
c. restlessness, rhinorrhea, vomiting.
d. seizures, miosis, piloerection.
e. seizures, mydriasis, piloerection.
295
1001. c
th
Rosen 5 ,
Chapter 149,
p. 2134
1002. b
Rosen 5th,
Chapter 151,
p. 2152
1003. d
Rosen 5th,
Chapter 145,
p. 2089-2093
1004. c
Rosen 5th,
Chapter 148,
p. 2124
1005. c
Rosen 5th,
Chapter 156,
p. 2183
Isopropanol, when metabolized, forms acetone. Acetone is a ketone but not an acid.
Isopropanol poisoning produces an elevated osmolar gap and ketonuria. Isopropanol
poisoning does not produce metabolic acidosis and does not produce an elevated anion
gap. Poisoning by ethylene glycol, isoniazid, methanol, and salicylates all produce
metabolic acidosis and an elevated anion gap.
This patient is experiencing signs and symptoms of moderate iron poisoning and
should be treated with intravenous fluid challenges and the antidote deferoxamine.
Activated charcoal does not bind to iron and should not be administered. Abdominal
x-rays are occasionally helpful, especially in cases of an unknown ingestion. Patients
who experience clinical signs and symptoms of moderate to severe signs iron
poisoning need to be treated aggressively. Treatment is not based on serum iron levels,
WBC counts, or serum glucose studies.
This patient is displaying signs and symptoms of tricyclic antidepressant poisoning
(anticholinergic toxicity, sodium channel blockade, hypotension). The antidote for
tricyclic antidepressant poisoning is sodium bicarbonate. Glucagon is an antidote used
for beta-blocker and calcium channel blocker toxicity. Physostigmine is an antidote
for anticholinergic poisoning but should not be given to patients suffering from sodium
channel blockade as asystole may result.
This patient is displaying signs and symptoms of sympathomimetic poisoning.
Methamphetamine is the only sympathomimetic agent among the five choices.
Diphenhydramine and Jimson weed are anticholinergic agents. Anticholinergic
poisoning is very similar to sympathomimetic poisoning. The major difference
between these two poisonings is that anticholinergic poisoning produces dry skin while
sympathomimetic poisoning produces diaphoresis.
Heroin is an opioid. The typical signs and symptoms of opioid withdrawal are
restlessness, yawning, mydriasis, rhinorrhea, vomiting, abdominal pain, and
piloerection.
296
1006. A comatose 32 year-old woman is brought from home. Her Glasgow Coma Score is 5,
and the paramedics have successfully intubated her. They tell you that she has bipolar
disease, and show you an empty prescription bottle labeled “lithium carbonate 300mg.”
The prescription was filled three days ago for 120 tablets. Your most appropriate
management is:
a. activated charcoal.
b. hemodialysis.
c. physostigmine.
d. sodium bicarbonate.
e. syrup of ipecac.
1007. The clinical presentation of strychnine poisoning most closely resembles:
a. botulism poisoning.
b. brown recluse spider bite.
c. organophosphate poisoning.
d. scombroid poisoning.
e. tetanus infection.
1008. The treatment most likely to be successful in the management of beta-adrenergic blocker
toxicity is:
a. dialysis.
b. emesis with syrup of ipecac.
c. esmolol.
d. glucagon.
e. theophylline.
1009. Digoxin:
a. decreases cardiac automaticity.
b. increases intracellular potassium concentration.
c. decreases vagal tone.
d. decreases cardiac contractility.
e. inhibits the Na+-K+ ATPase pump.
1010. A 64-year-old woman inadvertently overdosed on her quinidine sulfate. You expect her
EKG to show:
a. QRS prolongation.
b. QT shortening.
c. ST segment depression.
d. ST segment elevation.
e. T wave inversion.
1011. Bradycardia can be seen in patients with toxic ingestion of:
a. captopril.
b. enalapril.
c. hydralazine.
d. nitroprusside.
e. verapamil.
297
1006. b
th
Rosen 5 ,
Chapter 154,
p. 2172-2173
1007. e
th
Rosen 5 ,
Chapter 123,
p. 1792-1793
1008. d
th
Rosen 5 ,
Chapter 146,
p. 2110
1009. e
Rosen 5th,
Chapter 146,
p. 2104
1010. a
Rosen 5th,
Chapter 74,
p. 1059
1011. e
th
Rosen 5 ,
Chapter 146,
p. 2111
The indications for hemodialysis for lithium patients poisoned are: clinical signs of
severe poisoning, deteriorating clinical condition (e.g., seizures, coma, ventricular
dysrhythmias), decreasing urine output, renal failure, and lack of expected drop in
serum lithium level (20% in 6 hours). Lithium does not bind to activated charcoal.
Strychnine poisoning and tetanus infection are similar clinically because both illnesses
have a negative effect on glycine neurotransmission. Strychnine produces its toxicity
by blocking glycine receptors. Tetanus, an infection caused by Clostridium tetani,
causes its toxicity by preventing the release of glycine from pre-synaptic neurons.
Glucagon is widely accepted as first-line therapy for beta-blocker toxicity. It enhances
myocardial performance by increasing cAMP concentrations in a manner identical to
that of catecholamines but is thought to act via its own receptor. Thus, glucagon may
bypass the blocked beta-receptor. Clinical experience with this antidote has generally
produced favorable results, often after other treatments have failed. A limited number
of animal models directly comparing glucagon to other therapies support the use of
glucagon.
Digoxin and the other cardiac glycosides produce their therapeutic effects by inhibiting
the Na+ - K+ ATPase pump. Other pharmacologic effects associated with digoxin
include increased cardiac automaticity, decreased intracellular potassium
concentration, increased vagal tone, and increased cardiac contractility.
Toxicity with Class 1A antidysrhythmics (quinidine, procainamide, disopyramide)
typically produces a prolonged QRS interval by blocking myocardial sodium channels.
Class 1A antidysrhythmics also have the potential to produce a prolonged QT interval.
Calcium channel antagonists block the slow calcium channels in the myocardium and
vascular smooth muscle, leading to coronary and peripheral vasodilation. They also
reduce cardiac contractility, depress SA nodal activity, and slow AV conduction. In
overdose, verapamil has the deadliest profile, combining severe myocardial depression
and peripheral vasodilation. Hypotension and bradycardia occur early, and other
rhythm disturbances include AV block of all degrees, sinus arrest, AV dissociation,
junctional rhythm, and asystole. Nifedipine overdose more commonly causes reflex
sinus tachycardia from peripheral vasodilation. Calcium channel blockade has little
effect on ventricular conduction, so QRS widening is not seen early on. Hydralazine
poisoning typically causes hypotension and reflex tachycardia.
298
1012. The syndrome of anticholinergic poisoning includes:
a. hyperactive bowel sounds.
b. hypothermia.
c. miosis.
d. salivation.
e. seizures.
1013. A 21-year-old man is brought to the emergency department by his family. He is restless
combative, and vomiting. His mother hands you a suicide note she found at his bedside.
Temperature 102.1oF, heart rate 120, respiratory rate 30, blood pressure 120/76 mmHg.
HEENT exam is unremarkable. Lungs are clear, but he has Kussmaul respirations. Heart
exam shows only tachycardia. His abdomen is soft and non-tender. His neurologic exam
shows an agitated, combative patient, but is non-focal. He has most likely ingested:
a. digoxin.
b. diphenhydramine.
c. organophosphate pesticides.
d. salicylate.
e. tricyclic antidepressants.
1014. A 75 year-old man took a handful of digoxin tablets in a suicide attempt. An indication for
using the digoxin-specific Fab fragments (Digibind®, DigiFab®) would be:
a. a serum digoxin level of 5.5 ng/ml.
b. a serum potassium of 5.8 mEq/l.
c. altered mental status.
d. hepatic insufficiency.
e. renal insufficiency.
1015. Carbon monoxide poisoning causes:
a. decreased affinity of hemoglobin for oxygen.
b. decreased oxygen carrying capacity of hemoglobin.
c. oxidative phosphorylation uncoupling.
d. methemoglobinemia.
e. stimulation of the tissue cytochrome oxidase system.
1016. Acetaminophen:
a. does not bind to activated charcoal.
b. is metabolized by the cytochrome P-450 system.
c. serum levels should be plotted on the Done nomogram.
d. overdose causes acidosis and tinnitus.
e. should not be given in combination with aspirin.
1017. A patient who has ingested a large amount of methanol will probably present with:
a. confusion, stupor, coma, and seizures.
b. crystalluria and renal failure.
c. an elevated osmolar gap but a normal anion gap.
d. hypochloremia and hypotension.
e. severe hypoglycemia and severe hyponatremia.
299
1012. e
th
Rosen 5 ,
Chapter 144,
p.2083
1013. d
Rosen 5th,
Chapter 143,
p. 2077
1014. b
Rosen 5th,
Chapter 146,
p. 2107, Box
146-4
1015. b
Rosen 5th,
Chapter 153,
p. 2169
1016. b
Rosen 5th,
Chapter 142,
p. 2069
1017. a
Rosen 5th,
Chapter 149,
p. 2128
The diagnosis of acute anticholinergic poisoning is suggested by characteristic physical
signs that constitute the anticholinergic syndrome or toxidrome. Mydriasis, dry
mucous membranes, the absence of axillary sweat, flushed skin, fever, tachycardia,
decreased or absent bowel sounds, and bladder distention constitute peripheral
evidence of muscarinic blockade. The presence of only one or two of these findings
does not exclude the diagnosis of an anticholinergic poisoning. The patient is often
alert and may be silly, agitated, violent, or incoherent. Visual hallucinations are
common. Central motor effects may manifest as myoclonus or choreoathetoid
movements in adults and children. Children seem more sensitive to the CNS stimulant
effects than adults and are more likely to have seizures, typically preceded by signs of
CNS irritability or depression.
This clinical scenario is most consistent with a salicylate overdose. Salicylate
poisoning causes nausea, vomiting, dehydration, hyperthermia, respiratory alkalosis,
and metabolic acidosis. The metabolic acidosis subsequently causes the Kussmaul
respirations.
Recommendations for Administration of Digitalis Antibody Fragments in Adults
Severe ventricular dysrhythmias
Progressive and hemodynamically significant bradydysrhythmias unresponsive to
atropine
Serum potassium greater than 5 mEq/L
Rapidly progressive rhythm disturbances or rising serum potassium
Coingestion of cardiotoxic drug as beta-blockers, calcium channel blockers, or
tricyclic antidepressants
Ingestion of plant known to contain cardiac glycosides plus severe dysrhythmias
(rare)
Acute ingestion greater than 10 mg plus any one of factors 1 through 6 above
Steady-state serum digoxin greater than 6 ng/ml plus any one of factors 1 through 6
above
Carbon monoxide binds to hemoglobin with an affinity 250 times that of oxygen.
Carbon monoxide poisoning causes reduced oxyhemoglobin saturation, a decreased
hemoglobin-to-oxygen carrying capacity, and inhibition of the cytochrome oxidase
system.
Acetaminophen is primarily metabolized in the liver. About 90% of a therapeutic dose
is converted to the inactive glucuronide and sulfate conjugates. Less than 4% is
excreted as unchanged Acetaminophen, and a similar fraction is conjugated with
glutathione by hepatic cytochrome P450 mixed function oxidases. Activated charcoal
does bind acetaminophen. Serum levels are plotted on the Rumack-Matthews
nomogram; the Done nomogram is used to plot serum salicylate levels. Salicylate
poisoning typically produces tinnitus and acidosis.
The methanol-toxic victim may be confused or, in severe cases, comatose. There may
be complaints of headache or vertigo, and seizures may occur. Visual disturbances are
seen in approximately 50% of patients. These include diplopia, blurred vision,
decreased visual acuity, photophobia, descriptions of “looking into a snow field,”
constricted visual fields, and blindness. The clinician may find nystagmus, fixed and
dilated pupils, retinal edema, and optic atrophy or hyperemia of the optic disk.
300
1018. A 30-year-old man is found slumped over his workbench in the back of his jewelry store.
Minutes earlier he had complained of headache, dizziness, and weakness. Now he is
comatose and apneic with a thready pulse. There is no cyanosis. Basic Metabolic Panel
shows a high anion gap acidosis. Blood gas determinations on arterial and venous blood
samples show nearly identical pO2 values. The carboxyhemoglobin is 5%. Although the
patient is intubated and being hyperventilated with 100% oxygen, the acidosis persists.
Your next step is to:
a. administer intravenous atropine and pralidoxime (2-PAM).
b. administer intravenous methylene blue.
c. administer intravenous physostigmine and hydroxocobalamin (vitamin B12a).
d. administer intravenous sodium nitrite, then infuse sodium thiosulfate.
e. transfer the patient to a facility with a hyperbaric chamber.
1019. Drugs which can be removed by dialysis:
a. have a high molecular weight.
b. are highly protein bound.
c. have a large volume of distribution
d. are lipophilic
e. are water soluble
1020. A 35-year-old HIV positive man with a history of Pneumocystis carinii pneumonia presents
to the awake and alert, but markedly cyanotic. Paramedics report finding the patient in a
bed in a local hospice with a suicide note and pills on the bedroom floor. The patient's
cyanosis persists despite 100% oxygen via mask. The patient is wearing a “sulfur allergy”
alert bracelet. The most likely etiology for his cyanosis is:
a. ethylene glycol poisoning.
b. hemolysis secondary to a trimethoprim/sulfamethoxazole (Bactrim®) overdose.
c. methemoglobinemia secondary to medication overdose.
d. pulmonic stenosis from endocarditis associated with atrial septal defect.
e. severe hypoxemia due to recurrence of Pneumocystis carinii pneumonia.
1021. Pralidoxime (2-PAM) reverses the toxicity of organophosphate insecticides by:
a. a direct beta-agonist effect which offsets bradycardia.
b. enhancing acetylcholine release from nerve endings.
c. enhancing norepinephrine release from nerve endings.
d. inducing metabolism of organophosphate insecticides.
e. reversing the inhibition of acetylcholinesterase.
1022. Hypocalcemia is a common finding in poisoning by:
a. acetaminophen.
b. diphenhydramine.
c. ethylene glycol.
d. iron.
e. methamphetamine.
1023. Which of the following uncouples oxidative phosphorylation?
a. acetaminophen
b. carbon monoxide
c. ethylene glycol
d. isoniazid
e. salicylates
301
1018. d
th
Rosen 5 ,
Chapter 153,
p. 2168
1019. e
Rosen 5th,
Chapter 154,
p. 2173
1020. c
1021. e
Rosen 5th,
Chapter 157,
p. 2190
1022. c
Rosen 5th,
Chapter 149,
p. 2131
1023. e
Rosen 5th,
Chapter 143,
p. 2076
This patient is most likely suffering from cyanide poisoning. Cyanide poisoning
typically causes headache, dizziness, and weakness followed by convulsions and coma.
Metabolic acidosis occurs without evidence of cyanosis or hypoxia, and an abnormally
elevated venous oxygen pressure also is seen. Cyanide is used in many industries,
including ore extraction, metal polishing, and electroplating. Sodium nitrite and
sodium thiosulfate are found in the cyanide antidote kit. Atropine and pralidoxime use
antidotes used for organophosphate poisoning. Methylene blue is an antidote that
reverses methemoglobinemia. Physostigmine is an antidote occasionally used for
anticholinergic poisoning. Hyperbaric oxygen is used to treat carbon monoxide
poisoning.
Hemodialysis is generally reserved for specific toxins that must be both potentially life
threatening and amenable to removal by this method. The benefits include the ability
to remove toxins that are already absorbed from the gut lumen, removal of substances
that do not adhere to activated charcoal, and the ability to remove both the parent
compound and the active toxic metabolites. Hemodialysis is much less effective where
the toxin ingested has a large volume of distribution, has a large molecular weight, or
is highly protein bound.
This patient most likely ingested dapsone, a medication used to treat Pneumocystis
pneumonia for patients allergic to sulfur. Dapsone toxicity can produce significant
methemoglobinemia and a resulting cyanosis that does not reverse with oxygen. Other
agents that can cause methemoglobinemia include lidocaine, aniline dyes,
sulfonamides, phenacetin, and the fluoroquinolones.
The second part of acetylcholinesterase inhibition treatment is the use of pralidoxime
(Protopam, 2-PAM) to break up the organophosphate – acetylcholinesterase complex
and restore cholinesterase activity at both muscarinic and nicotinic sites. Pralidoxime
can also combine with unbound organophosphates and prevent their subsequent
binding to nerve terminals.
Poisoning by ethylene glycol can produce hypocalcemia secondary to the precipitation
of calcium oxalate crystals. Hypocalcemia may be severe enough to cause tetany and
prolongation of the QT interval. Two forms of urinary calcium oxalate crystals may be
identified on microscopic examination of the urine: dihydrate (octahedral) form and
monohydrate (monoclinic) form).
Salicylates enhance lipolysis, inhibit various enzymes involved in energy production
and amino acid metabolism, and uncouple oxidation phosphorylation. Because
oxidative phosphorylation is a major buffer of hydrogen ions, impairment of oxidative
phosphorylation by salicylate results in metabolic acidosis. Carbon monoxide inhibits
electron transport.
302
1024. Which of the following inhibits electron transport?
a. chlorine gas
b. cyanide
c. dapsone
d. hydrofluoric acid
e. isopropanol
1025. A 3-year-old boy is brought to the ED because of lethargy. He is difficult to awaken and
slightly diaphoretic. Temperature 97.6oF; heart rate 22; respiratory rate 12; blood pressure
60/30 mmHg. ECG shows sinus bradycardia with a QRS interval of 0.1 s and peaked T
waves. The serum potassium level is 8.2. This child has ingested:
a. captopril.
b. clonidine.
c. digoxin.
d. propranolol.
e. verapamil.
1026. Acute inorganic mercury and arsenic poisoning share many clinical features. Which of the
following suggests the presence of acute inorganic mercury salt poisoning over acute
inorganic arsenic poisoning?
a. Delayed onset of peripheral neuropathy
b. Hemorrhagic gastroenteritis
c. Radio-opaque substance noted on KUB
d. Rapid onset of renal failure
e. Shock
1027. A 5-year-old boy presents with lethargy. His heart rate is 30 bpm, and blood pressure is
50/30 mmHg. On ECG, the QRS complex is narrow. He has probably ingested:
a. clonidine.
b. doxepin (Sinequan®).
c. jimson weed.
d. phenylpropanolamine.
e. thioridazine.
1028. A 32-year-old woman complains of vomiting, hematemesis, and abdominal pain. Vital
signs: temperature 99.oF; heart rate 130/min; respiratory rate 44/min, blood pressure
111/80 mm Hg. She is diaphoretic. Laboratory studies reveal: Na+ 150, K+ 4.8, Cl- 110,
CO2 12, pH 7.35, pCO2 18, pO2 104, urine ketones 3+. After fluid challenge, your next
step should be:
a. gastric lavage and deferoxamine.
b. fomepizole (4-MP) and hemodialysis.
c. intravenous ethanol and hemodialysis.
d. intravenous sodium bicarbonate and hemodialysis.
e. n-acetylcysteine and activated charcoal.
1029. In a patient suffering from serotonin syndrome, it is reasonable to give:
a. benztropine (Cogentin®).
b. bromocriptine (Parlodel®).
c. cyproheptadine (Periactin®).
d. L-dopa.
e. ondansetron (Zofran®).
303
1024. b
th
Rosen 5 ,
Chapter 153,
p. 2167
1025. c
th
Rosen 5 ,
Chapter 146,
p. 2107
1026. d
Rosen 5th,
Chapter 151,
p. 2155, 2157
1027. a
1028. d
Rosen 5th,
Chapter 143,
p. 2077, 2078
1029. c
Rosen 5th,
Chapter 145,
p. 2096
Cyanide is a potent inhibitor of the electron transport chain. Inhibition of the electron
transport chain leads to anaerobic metabolism and metabolic acidosis, as the body
tissues cannot utilize oxygen. Carbon monoxide and hydrogen sulfide also inhibit the
electron transport chain.
This scenario is most consistent with acute digoxin (cardiac glycoside) poisoning.
Acute digoxin (cardiac glycoside) poisoning typically causes lethargy, confusion,
bradyarrhythmias or supraventricular tachydysrhythmias, hyperkalemia, and nausea
and vomiting. Unless ventricular escape rhythms occur, the QRS complex typically
stays narrow (less than 0.12 s). Poisoning by clonidine, propranolol, and verapamil
can produce a similar presentation; however, hyperkalemia is NOT typical. Captopril
poisoning does not typically produce cardiovascular compromise.
Acute inorganic mercury and arsenic poisoning can produce hemorrhagic
gastroenteritis, shock, and delayed onset of peripheral neuropathy. In addition, both
inorganic arsenic and mercury are radio-opaque on an x-ray. Acute inorganic mercury
poisoning typically causes rapid onset of renal failure (within 24 hours) secondary to
acute tubular necrosis.
Clonidine (an imidazoline) poisoning typically produces bradycardia, hypotension, and
CNS depression. Unlike the tricyclic antidepressants (e.g., doxepin) and the
phenothiazines (e.g., thioridazine), clonidine and other imidazolines do NOT block
myocardial sodium channels and do NOT prolong the QRS complex. Jimson weed is a
plant with anticholinergic properties; jimson weed poisoning typically produces
tachycardia. Phenylpropanolamine was available as an over-the-counter diet
preparation and poisoning typically produced hypertension and cerebrovascular
complications. For safety reasons, the FDA recalled all products containing
phenylpropanolamine in the year 2000.
This scenario is most consistent with acute salicylate poisoning. Acute salicylate
poisoning causes nausea, vomiting, dehydration, hyperthermia, respiratory alkalosis,
and metabolic acidosis. The metabolic acidosis subsequently causes the Kussmaul
respirations. Abdominal pain and hematemesis can occur. The treatment for severe
salicylate poisoning includes fluid resuscitation, alkalinization of the serum and urine,
and hemodialysis.
Serotonin syndrome occurs when there is an excess of the neurotransmitter serotonin at
the receptor. This syndrome typically occurs with the concomitant use of two
serotonergic drugs. Overdoses of a single serotonergic agent may also produce
serotonin syndrome. Serotonin syndrome typically produces neuromuscular
symptoms, cognitive-behavior symptoms, and dysfunction of the autonomic nervous
system. Several investigators have reported successful treatment of serotonin
syndrome with the serotonin receptor antagonist cyproheptadine.
304
1030. A 34-year-old man is brought by ambulance with refractory seizures and a heart rate of
104/min. The rhythm strip shows a QRS complex of 0.08 seconds. He has probably
ingested:
a. gamma-butyrolactone (GBL).
b. gamma-hydroxybutyrate (GHB).
c. isoniazid (INH).
d. nortriptyline.
e. quinidine.
1031. A 62-year-old man is lethargic two hours after undergoing outpatient bronchoscopy. Heart
rate 120/min, respiratory rate 26/min, blood pressure 160/90 mmHg. He is cyanotic and
diaphoretic. Laboratory studies show: pH 7.28; pCO2 28, pO2 88; Hgb 12 g/dL. The oncall intensivist inserts a Swan-Ganz catheter, and the reading show a cardiac output of 5
L/min, oxygen consumption 330 ml/min (normal), and mixed venous pCO2 20 mmHg.
Your most appropriate action is:
a. check for osmolar gap and consider dialysis.
b. check pulse oximetry.
c. exchange transfusion.
d. intravenous methylene blue.
e. intravenous sodium thiosulfate and sodium nitrite.
1032. A 22 year-old woman ingested an unknown substance two hours ago. She is vomiting
and has diarrhea. Her vital signs are normal. Lab studies show pH 7.4; pCO2 40; pO2 95;
Na+ 136, K+ 4.0, Cl- 110, HCO3 24, acetaminophen level 0, salicylate level 0. Over the
next 8 hours she develops confusion, rigidity, and convulsions. ECG shows first-degree
heart block. She probably ingested:
a. acetaminophen.
b. ciprofloxacin.
c. lithium carbonate.
d. oil of wintergreen.
e. salicylate.
1033. The oxyhemoglobin dissociation curve shifts to the right in:
a. acidosis.
b. alkalosis.
c. carboxyhemoglobin.
d. methemoglobin.
e. hypothermia.
1034. Alcohol dehydrogenase metabolizes:
a. disulfiram.
b. gamma-hydroxybutyrate (GHB).
c. gyrometra mushrooms.
d. isopropanol.
e. Rohypnol.
1035. A 22-year-old woman is brought from her dormitory room, where her roommate found her
comatose. Heart rate 95/min; respiratory rate 18/min; BP 180/95 mmHg. Physical
examination shows muscular rigidity and rotary nystagmus. She has probably ingested:
a. amphetamine.
b. ecstasy.
305
c. phencyclidine.
d. phenobarbital.
e. diazepam.
306
1030. c
th
Rosen 5 ,
Chapter 118,
p. 1719
1031. d
Rosen 5th,
Chapter 182,
p. 2574
1032. c
th
Rosen 5 ,
Chapter 154,
p. 2172
1033. a
1034. d
Rosen 5th,
Chapter 149,
p. 2134
1035. c
th
Rosen 5 ,
Chapter 180,
p. 2541
Poisoning by all these agents may produce seizures. Gamma-butyrolactone (GBL) and
gamma-hydroxybutyrate (GHB) do NOT typically cause refractory seizures.
Nortriptyline and quinidine block myocardial sodium channels. Severe poisoning by
nortriptyline and quinidine may produce seizures but usually do so when the QRS
complex is prolonged (greater then 0.10 s). Isoniazid poisoning blocks the production
of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) and causes
seizures that are refractory to conventional therapy (e.g., benzodiazepines,
barbiturates). The antidote for isoniazid poisoning is pyridoxine (vitamin B6).
This clinical scenario is typical for acquired methemoglobinemia, with the source
being the local anesthetic (e.g., benzocaine) used during the bronchoscopy. The
treatment for symptomatic methemoglobinemia is methylene blue.
Acute lithium poisoning typically produces nausea, vomiting, and diarrhea. Lithium
poisoning also produces central nervous system toxicity (lethargy, confusion,
spasticity, rigidity, convulsions, etc.) and cardiovascular toxicity (ECG conduction
defects, bradycardia, ST-T wave changes, ventricular arrhythmias). Because of
lithium’s prolonged absorption and distribution period, presentation of the CNS and
cardiovascular toxicity may be delayed. Oil of wintergreen (methyl salicylate) is an
extremely toxic form of salicylate.
The following factors shift the oxyhemoglobin dissociation curve to the left:
methemoglobinemia, carboxyhemoglobinemia, alkalosis, hypothermia. The following
factors shift the oxyhemoglobin dissociation curve to the right, inhibiting the release of
oxygen at the tissue level: acidosis, hyperthermia, and elevations in 2,3diphosphoglycerate concentration.
Isopropanol, the main ingredient found in rubbing alcohol, is metabolized by alcohol
dehydrogenase to acetone. Disulfiram (Antabuse®) inhibits the enzyme aldehyde
dehydrogenase.
Phencyclidine, a dissociative anesthetic agent, is a common agent of abuse. Mild to
moderate intoxication with phencyclidine typically causes agitation, confusion,
hallucinations, delusions, ataxia, rigidity, rotary nystagmus, and coma. Severe
phencyclidine toxicity causes hypertension and tachycardia. Amphetamine and ecstasy
(sympathomimetics) poisoning typically cause tachycardia. Phenobarbital and
diazepam (sedative hypnotics) poisoning typically causes muscular relaxation.
307
1036. A patient poisoned with cyanide will have:
a. convulsions.
b. cyanosis.
c. garlic odor to breath.
d. metabolic alkalosis.
e. rotten egg odor to skin.
1037. A 44-year-old male ingests an unknown substance. In less than 10 minutes he collapses
in convulsions. He probably ingested:
a. Amanita phylloides mushrooms.
b. insulin.
c. phenobarbital.
d. salicylates.
e. strychnine.
1038. An elevated methemoglobin fraction may be seen in:
a. aldehyde dehydrogenase deficiency.
b. gastroenteritis in a newborn.
c. glucose-6-phosphate deficiency (G6PD).
d. isoniazid overdose.
e. thiamine deficiency.
1039. Centrilobular hepatic necrosis is seen in poisoning with:
a. Percocet®.
b. jimson weed.
c. ecstasy.
d. Nerium oleander.
e. theophylline.
1040. Regarding gastrointestinal decontamination after overdose:
a. Activated charcoal is the recommended gastrointestinal decontamination procedure of choice.
b. Activated charcoal prevents absorption of substances such as lithium and iron supplements.
c. In an overdose, the stomach should be emptied by both ipecac and gastric lavage.
d. Lavage is most effective if performed within 6 hours of ingestion of large quantity of pills.
e. Multidose charcoal is most useful to enhance elimination of a life-threatening dose of medication.
1041. A 37-year-old man says he took a “handful” of over the counter pain medicine yesterday
morning. In addition to an acetaminophen concentration, the lab test most sensitive in
detecting possible liver injury is:
a. acid phosphatase.
b. alkaline phosphatase.
c. aspartate aminotransferase (AST or SGOT).
d. bilirubin.
e. lactated dehydrogenase (LDH).
1042. The cut-off time for using N-acetylcysteine in a patient presenting after acetaminophen
overdose is:
a. 8 hours.
b. 24 hours.
c. 36 hours.
d. 2 days.
308
e. none.
309
1036. a
th
Rosen 5 ,
Chapter 153,
p. 2167-2168
1037. e
th
Rosen 5 ,
Chapter 123,
p. 1792-1793
1038. b
1039. a
Rosen 5th,
Chapter 142,
p. 2069
1040. a
Rosen 5th,
Chapter 141,
p. 2066
1041. c
Rosen 5th,
Chapter 142,
p. 2071
1042. e
Rosen 5th,
Chapter 142,
p. 2074
Cyanide poisoning typically causes headache, dizziness, and weakness followed by
convulsions and coma. In addition, metabolic acidosis occurs without evidence of
cyanosis or hypoxia. Garlic odor is characteristic of arsenic and organophosphate
poisoning. Rotten egg odor is characteristic of hydrogen sulfide poisoning.
Strychnine competitively blocks the glycine receptor. Glycine is an inhibitory
neurotransmitter released by the postsynaptic inhibitory neurons in the spinal cord. By
blocking the glycine receptor, strychnine causes increased neuronal excitability, which
results in generalized seizure-like contraction of the skeletal muscles. Strychnine is
absorbed rapidly following ingestion. Salicylate poisoning can produce seizures but
not in such a rapid time frame. Insulin, when ingested, is metabolized before
absorption and typically does not cause hypoglycemia.
Neonates have reduced levels of the endogenous enzyme used to reduce
methemoglobin back to its normal state. When neonates are exposed to oxidant stress
(e.g., viral induced gastroenteritis) they are at risk for developing elevated levels of
methemoglobin. Isoniazid poisoning causes seizures refractory to standard therapy.
Thiamine deficiency can lead to Wernicke’s encephalopathy, Korsakoff’s syndrome, or
Beriberi. Patients with glucose-6-phosphate deficiency (G6PD) are not predisposed to
methemoglobinemia.
Percocet® (oxycodone/acetaminophen) may produce opioid toxicity but also liver
toxicity secondary to the acetaminophen. Jimson weed typically causes anticholinergic
poisoning. Ecstasy causes sympathomimetic toxicity. Nerium oleander is a plant with
cardiac glycoside properties, and poisoning with this plant resembles poisoning seen
with digoxin. Theophylline is a phosphodiesterase-inhibitor that does not typically
produce liver damage in an overdose setting.
Activated charcoal is the procedure of choice for GI decontamination. Complications
of gastric emptying procedures, such as aspiration, are avoided with activated charcoal.
In such an overdose, whole bowel irrigation may be considered. Gastric emptying
does not require both ipecac and gastric lavage. If performed within one hour of
ingestion, gastric lavage may be useful. Multidose charcoal may be useful in removing
drugs already absorbed, not to enhance elimination.
Once potential risk has been established, determine acetaminophen concentration
([APAP]) 4 hours after the ingestion, or as soon as possible after 4 hours. In many
cases [APAP] alone will be adequate to establish risk. When the physical findings are
consistent with hepatic injury, or the timing of the ingestion cannot be established,
aspartate transaminase (AST) should also be measured to establish the presence or
absence of hepatic injury. Those at risk for APAP-induced hepatotoxicity on the basis
of [APAP], or with evidence of hepatic injury, should be treated with NAC.
All durations of NAC administration are effective when started early, indicating that
shorter courses of treatment are appropriate when NAC is used for its preventive
actions. In contrast, protocol comparisons and series involving late NAC
administration suggest that a longer duration of treatment may be needed when treating
established liver injury. Rather than a single duration of therapy for all patients, it may
be appropriate to use different treatment protocols on the basis of clinical course or
other markers. No definitive “cut-off” point for beginning therapy has been described.
310
1043. Choose the true statement concerning non-steroidal anti-inflammatory overdose:
a. Because of a high volume of distribution and slow metabolism, urinary alkalinization,
hemodialysis, or hemoperfusion can enhance NSAID elimination.
b. Children with ingestions of less than 300 mg/kg of ibuprofen do not require medical evaluation.
c. Because of zero-order kinetics, elimination half-lives are substantially prolonged in overdose.
d. NSAIDs can cause lethal dysrhythmias.
e. Overdose with mefenamic acid (Ponstel®) is associated with seizures, which can occur several
hours after ingestion.
1044. You are seeing a 23-year-old graduate student who overdosed on a bottle of over-thecounter sleeping pills. He is poorly responsive, delirious, and irritable, with frequent
myoclonic jerks. His mucous membranes are dry and pupils dilated. In an attempt to
prevent seizures, you decide to give the appropriate antidote:
a. 1 to 2 mg rapid IV push.
b. 1 to 2 mg slow IV push over 2 to 4 minutes.
c. 5 mg IM.
d. 5 mg rapid IV push.
e. 5 mg slow IV push over 2 to 4 minutes.
1045. The most significant toxicity which can be seen with bupropion (Wellbutrin®, Zyban®) is:
a. neuroleptic malignant syndrome.
b. orthostasis.
c. seizures.
d. serotonin syndrome.
e. torsade de pointes.
1046. In a patient who has overdosed on tranylcypromine (Parnate®), you should know that:
a. asymptomatic patients need 24 hours of observation.
b. bradycardia and hypotension are early findings.
c. bretylium is the drug of choice for ventricular dysrhythmias.
d. hemodialysis should be considered for severe overdoses.
e. symptoms usually start within 1 to 2 hours of ingestion.
1047. Caustic gastrointestinal burns are possible after ingestion of:
a. cigarettes.
b. furniture polish.
c. hair relaxer.
d. rodenticides.
e. rubbing alcohol.
1048. In a patient with massive topical exposure to white phosphorus, you might expect to see
a. severe metabolic alkalosis.
b. fulminant pulmonary edema.
c. intractable seizures.
d. hypocalcemia and prolonged QT on ECG.
e. severe disseminated intravascular coagulopathy.
311
1043. e
th
Rosen 5 ,
Chapter 142,
p. 2079
1044. b
Rosen 5th,
Chapter 143,
p. 2085
1045. c
Rosen 5th,
Chapter 145,
p. 2097
1046. a
Rosen 5th,
Chapter 145,
p. 2100
1047. c
Rosen 5th,
Chapter 147,
p. 2115
1048. d
Rosen 5th,
Chapter 57,
p. 818
NSAIDs are not known to be primary causes of dysrhythmias, but fluid and electrolyte
abnormalities may place patients at risk for cardiac dysrhythmias. Children with
ingestions of less than 100 mg/kg of ibuprofen do not require medical evaluation.
Because of high protein binding and rapid metabolism, urinary alkalinization,
hemodialysis, or hemoperfusion does not enhance NSAID elimination. Elimination
half-lives are not substantially prolonged in overdose.
Physostigmine antagonizes the effects of anticholinergic medications by inhibiting
acetylcholinesterase and thereby increasing the concentration of acetylcholine in the
synaptic space. In the absence of a significant anticholinergic overdose, however,
physostigmine may exacerbate asthma and may produce seizures, bradycardia,
salivation, diarrhea, and bronchorrhea. It should therefore be used with caution and
never as a first-line drug. The proper dose is 1 to 2 mg slow IV push in adults and 0.5
mg slow IV push in children. Doses may be repeated as needed. Rapid infusion, even
with significant anticholinergic toxicity, may produce seizures.
Seizures may occur not only with bupropion overdose but also when the maximum
daily dose is exceeded. Bupropion-induced seizures should be treated with
benzodiazepines. Phenobarbital should be used to treat patients with recurrent seizures
or status epilepticus. Hypotension, neuroleptic malignant syndrome, and serotonin
syndrome do not occur unless other medications are coingested.
Signs and symptoms of MAO-I overdose are usually not apparent during the first 6 to
12 hours following ingestion. For this reason, all patients with MAO-I overdose
should be admitted for 24 hours. This is in contrast to patients with suspected or
known MAO-I interactions with food, beverages, and drugs. These patients will have
onset of symptoms within minutes to hours of ingestion and may be discharged if they
remain asymptomatic for 6 hours. Bradycardia and hypotension are late findings with
MAO-I toxicity. Hemodialysis, hemoperfusion, and forced diuresis do not enhance
elimination. Lidocaine is the drug of choice for ventricular dysrhythmias. Bretylium
is contraindicated because it releases biogenic amines.
Ingestion of base-containing substances produces significant injury because bases
cause liquefactive necrosis, which allows deep penetration of the caustic material.
Such substances include lye (NaOH and KOH), ammonia (NH4OH4), hair relaxers, hair
straighteners, and electric dishwasher soaps.
Metabolic derangements have been identified after white phosphorus burns. Serum
electrolyte changes consist of decreased serum calcium and increased serum
phosphorus. ECG abnormalities include prolonged QT interval, bradycardia, and STsegment-T-wave changes, which may explain the sudden death occasionally seen in
patients with apparently inconsequential white phosphorus burns.
312
1049. The most appropriate initial treatment for a chemical burn is:
a. bleach soaks.
b. copious irrigation with water.
c. ice packs.
d. pain management.
e. silver sulfadiazine dressings.
1050. There are reports of perforated aorta, left atrium, and bronchial artery in patients who did
not completely wash down the commonly-prescribed medication:
a. potassium chloride
b. cephalexin.
c. ibuprofen.
d. codeine.
e. nitroglycerin.
313
1049. b
th
Rosen 5 ,
Chapter 57,
p. 814
1050. c
th
Rosen 5 ,
Chapter 147,
p. 2115-2116
Injury will continue as long as there is contact between the offending agent and the
skin. Contaminated clothes should be removed, but irrigation should be initiated
immediately and continued while the clothing is removed.
More than 70 different pills may cause damage when in contact with esophageal mucus
for prolonged periods. Patients who take medications in the supine position, or who
take pills without water, are at higher risk. Pills most likely to adhere are doxycycline,
tetracycline, potassium chloride, and aspirin. Potassium chloride is particularly
dangerous and has caused penetration into the aorta, left atrium, and bronchial artery.
314
18.0 – Traumatic Disorders
1051. In treating a patient with traumatic brain injury, the ideal cerebral perfusion pressure is:
a. 40 mmHg or greater.
b. 50 mmHg or greater.
c. 60 mmHg or greater.
d. 70 mmHg or greater.
e. 80 mmHg or greater.
1052. Uncal transtentorial herniation would typically result in:
a. ipsilateral fixed and dilated pupil, ipsilateral hemiparesis
b. ipsilateral fixed and dilated pupil, contralateral hemiparesis
c. contralateral fixed and dilated pupil, ipsilateral hemiparesis
d. contralateral fixed and dilated pupil, contralateral hemiparesis
e. bilateral fixed / dilated pupils with quadriparesis
1053. Epidural hematoma is most often associated with a skull fracture that tears the:
a. external carotid artery.
b. internal carotid artery
c. middle meningeal artery
d. middle meningeal vein
e. subarachnoid bridging veins
1054. A 14-year-old boy was knocked out when struck on the head with a golf ball. He now
opens his eyes when stimulated, moans in pain, and pulls away from noxious stimuli. His
Glasgow Coma Score is:
a. 14
b. 12
c. 10
d. 8
e. 6
1055. Mannitol reduces intracranial pressure by:
a. diuresis
b. pH elevation
c. pH reduction
d. vasoconstriction
e. vasodilation
1056. A 94-year-old woman is sent from a local nursing home after falling from her wheelchair.
Her transfer note asks you to “rule-out subdural.” You know that:
a. blood collects in the subdural space more quickly than in an epidural hematoma.
b. infants and toddlers rarely develop subdural hematomas.
c. most subdural hematomas are due to penetrating head injury.
d. the risk of developing a subdural hematoma decreases with age.
e. the usual mechanism is a sudden acceleration-deceleration of brain parenchyma and tearing of
bridging veins.
315
1051. d
th
Rosen 5 ,
Chapter 34,
p. 288
1052. b
th
Rosen 5 ,
Chapter 34,
p. 290
1053. c
Rosen 5th,
Chapter 34,
p. 307
1054. d
Rosen 5th,
Chapter 34,
p. 292
1055. a
th
Rosen 5 ,
Chapter 34,
p. 295
1056. e
Rosen 5th,
Chapter 32,
p. 273
Chapter 34,
p. 308
Cerebral perfusion pressure (CPP) is estimated as MAP minus ICP. Cerebral blood
flow (CBF) is dependent on CPP. As CPP drops below 60mm Hg, the autoregulation
of CBF is lost, CBF declines, and the resultant tissue ischemia critically affects
cerebral metabolism.
The most common traumatic herniation syndrome is uncal herniation, The classic signs
and symptoms are caused by compression of the ipsilateral uncus of the temporal lobe
on the edge of the tentorium cerebelli as the brain is forced through the tentorial hiatus.
As compression of the uncus begins, the third cranial nerve is compressed; anisocoria,
ptosis, impaired extraocular movements, and a sluggish pupillary light reflex develop
ipsilateral to the expanding mass lesion. As herniation progresses, compression of the
ipsilateral oculomotor nerve eventually causes ipsilateral pupillary dilation and
nonreactivity. Contralateral hemiparesis develops as the ipsilateral peduncle is
compressed against the tentorium. With continued progression of the herniation,
bilateral decerebrate posturing eventually occurs. In up to 25% of patients the
contralateral cerebral peduncle is forced against the opposite edge of the tentorial
hiatus. Hemiparesis is then detected ipsilateral to the dilated pupil and the mass lesion.
This is termed Kernohan’s notch syndrome and causes false-localizing motor findings.
Epidural hematomas (EDHs) are blood clots that form between the inner table of the
skull and the dura. Eighty percent are associated with skull fractures across the middle
meningeal artery and are therefore located in the temporoparietal region. The
incidence of skull fractures in children with EDH is lower than in adults because the
elasticity of the skull during childhood permits it to spring back to its original position
instead of breaking after a significant impact.
The GCS assesses a patient's best eye, verbal, and motor responsiveness. The score
ranges from 3 (unresponsive) to 15. This patient receives a 2 for eye response: opens
eyes in response to pain; a 2 for verbal response: moaning, no recognizable words; and
a 4 for motor response: pulls away from pain in flexion.
The timely administration of mannitol can be lifesaving. Mannitol (0.25 to 1 g/kg)
effectively reduces cerebral edema by osmotic diuresis, producing an osmotic gradient
that prevents further cellular edema and draws tissue water into the vascular space.
This reduces brain volume and provides increased space for an expanding hematoma
or brain swelling. The osmotic effects of mannitol occur within minutes and peak
about 60 minutes after bolus administration. The ICP-lowering effects of a single
bolus may last for 6 to 8 hours.
Subdural hematomas (SDHs) are blood clots that form between the dura and the
arachnoid. SDHs are caused by movement of the brain relative to the skull, as is seen
in acceleration-deceleration injuries. They are common in patients with brain atrophy,
such as alcoholic or elderly patients where superficial bridging vessels traverse greater
distances, and are thus more prone to rupture with rapid movement of the head. The
slow bleeding of venous structures in SDHs delays the development of clinical signs
and symptoms. SDHs are common in patients less than 2 years of age.
316
1057. The oculocephalic response (doll’s eyes maneuver) tests the integrity of the:
a. cerebellum.
b. hippocampus.
c. hypothalamus.
d. occipital visual fields.
e. pons.
1058. You have just received by ambulance a comatose 19-year-old college student with severe
midface fractures following a collision with a lamppost. Medics were unsuccessful in field
intubation, so you prepare to do rapid sequence intubation, knowing that:
a. thiopental can raise both systemic and intracerebral blood pressure.
b. etomidate is contraindicated.
c. ketamine reduces intracerebral pressure, but may cause severe laryngospasm.
d. pretreatment with lidocaine is not indicated.
e. succinylcholine should be avoided unless a defasciculating dose of a nondepolarizing agent has
first been given.
1059. You are looking at skull x-rays on a child who was dropped on his head onto a concrete
surface. You are trying to differentiate possible skull fracture from normal suture lines,
knowing that:
a. fractures are less lucent than vascular grooves and sutures.
b. fractures are most commonly seen in the temporal region.
c. fractures are narrowest at the ends and widest at the middle.
d. fractures are rarely more than 3 mm wide.
e. most fractures are visible only on one view.
1060. Rapid rises in the ICP can lead to the Cushing reflex of
a. disconjugate gaze, Cheyne-Stokes breathing, and tachycardia.
b. hypertension, bradycardia, and respiratory irregularities.
c. hypotension, frequent PVCs, and decerebrate posturing.
d. upgoing toes, diminished deep tendon reflexes, and Kussmaul respirations.
e. wandering nystagmus, pulsus alternans, and tardive dyskinesia.
1061. You have thoroughly examined a patient who fell off scaffolding. You found only a basilar
skull fracture and clear CSF rhinorrhea. This patient needs:
a. a lumbar puncture.
b. admission for prophylactic intravenous antibiotics.
c. outpatient observation only.
d. outpatient therapy with oral prophylactic antibiotics.
e. serial head CTs.
1062. Most head injuries seen in the Emergency Department are classified as mild and
moderate. Concerning this group:
a. patients with an initial GCS of 9 or greater who later deteriorate to a GCS of 8 generally have a
good prognosis.
b. less than 10% of moderately head-injured patients have an abnormal CT scan.
c. most moderate head trauma patients become asymptomatic within two weeks of injury.
d. signs and symptoms of concussion usually are completely resolved by 6 hours.
e. the most common complaint after concussion is headache.
317
1057. e
th
Rosen 5 ,
Chapter 34,
p. 293
1058. e
Rosen 5th,
Chapter 1,
p. 13
Chapter 34,
p. 295
1059. c
Rosen 5th,
Chapter 34,
p. 305
1060. b
Rosen 5th,
Chapter 34,
p. 290
1061. c
Rosen 5th,
Chapter 34,
p. 305
1062. d
Rosen 5th,
Chapter 34,
p. 297, 300
In the acute setting, brainstem activity is assessed by the patient's respiratory pattern,
pupillary size, and eye movements. The oculocephalic response (doll's eyes maneuver)
tests the integrity of the pontine gaze centers. This response cannot be tested until
cervical spine fractures have been ruled out. The oculovestibular response (cold water
calorics) assesses the brainstem.
In general the agents used for RSI in the head-injured patient are the same as those for
other patients, although attention must be given to the increased ICP that can occur
with any physical stimulation of the respiratory tract. Lidocaine (1.5 to 2 mg/kg IV
push) effectively attenuates the cough reflex, hypertensive response, and increased ICP
associated with intubation. Thiopental may also be effective but should not be used in
hypotensive patients. If succinylcholine is used, premedication with a subparalytic
dose of a nondepolarizing agent should be considered if time permits, since
fasciculations produced by succinylcholine may increase ICP. The degree of ICP
elevation and its clinical significance are unclear, however, and must be balanced
against the need for rapidly establishing an airway. Etomidate (0.3 mg/kg IV), a shortacting sedative-hypnotic agent, has beneficial effects on ICP by reducing cerebral
blood flow and metabolism. While ketamine is exceptionally hemodynamically stable,
it increases ICP and should not be used in head-injured patients.
In general on skull x-rays, fractures are more lucent than vascular grooves and sutures.
Sutures are usually less than 2 mm wide in adults; fractures are often 3 mm or greater
in overall width and tend to be widest in the midportion and narrow at each end.
Linear fractures are most common in the temporoparietal, frontal, and occipital regions
of the skull and can usually be visualized on more than one radiographic view.
Progressive hypertension associated with bradycardia and diminished respiratory effort
is a specific response to acute, potentially lethal rises in ICP. This response is called
the Cushing reflex, or Cushing's phenomenon, and its occurrence indicates that the ICP
has reached life-threatening levels. The full triad of hypertension, bradycardia, and
respiratory irregularity is seen in only one third of cases of life-threatening increased
ICP.
Most CSF leaks spontaneously resolve without complications in 1 week. Therefore, in
general, antibiotics are not given prophylactically during the first week of CSF
rhinorrhea. If a patient with a previously diagnosed CSF leak returns to the ED later
with fever, the diagnosis of meningitis should be strongly suspected and appropriate
workup and antibiotic treatment initiated immediately.
Patients with an initial GCS of 9 or greater who later deteriorate to a GCS of 8 or less
have a poorer outcome than those who originally presented with a GCS less than 8.
Approximately 40% of moderately head-injured patients have an abnormal CT scan,
and 10% lapse into coma. Most moderate head trauma patients remain symptomatic
for extended periods after head injury. At 3 months after trauma, up to 70% are unable
to return to work, 90% have memory difficulties, and more than 90% complain of
persistent headaches. Almost 50% are left with a permanent disability that interferes
with their previous daily activities. A wide spectrum of transient neurologic symptoms
may occur with concussion; the most common complaints are confusion and amnesia
for the traumatic event. Adults may complain of seeing stars or feeling nauseated,
dizzy, or disoriented for a brief period. A brief LOC may last for seconds up to several
minutes, but many patients report no LOC. In children, acute symptoms of concussion
differ from adults and may include restlessness, lethargy, confusion, or irritability. On
presentation, they may be vomiting, be tachycardic, or appear pale. These signs and
symptoms usually are completely resolved by 6 hours.
318
1063. The clinical picture most suggestive for a central cord syndrome is:
a. paralysis below the level of C4.
b. sensory loss below C4.
c. complete motor paralysis with loss of pain and temperature sensation distal to the lesion.
d. ipsilateral paralysis and loss of proprioception and vibratory sensation plus loss of pain and
contralateral loss of pain and temperature sensation.
e. weakness more pronounced in arms than legs and worse in hands than in the proximal upper
extremity.
1064. The maximum neurologic deficit following spinal cord injury is seen:
a. at the time of injury.
b. within hours of initial injury.
c. in the first days after injury.
d. in the first two weeks after injury.
e. six months after injury.
1065. The cervical spine injury most likely to be stable is:
a. bilateral facet dislocation.
b. burst fracture of C1 (Jefferson’s).
c. clay shoveler fracture.
d. hangman’s fracture.
e. rotary dislocation C1 on C2.
1066. Penetrating neck injury is defined as any wound that violates the:
a. digastric muscle
b. trachea
c. platysma
d. sternomastoid muscle
e. omohyoid muscle
1067. The “gold standard” for evaluating penetrating trauma to the neck is:
a. angiography.
b. color Doppler ultrasound.
c. contrast CT scan.
d. magnetic resonance imaging.
e. trans-esophageal echocardiography.
1068. A 22-year-old man walks into your Emergency Department. He is covered in blood and
pointing to his throat, where you see a large laceration and a hematoma that is displacing
his trachea. His voice is hoarse and stridorous. You must immediately:
a. consult ENT for emergent tracheostomy.
b. do a cricothyrotomy.
c. insert a laryngeal mask airway (LMA).
d. perform nasotracheal intubation.
e. perform rapid sequence intubation.
319
1063. e
th
Rosen 5 ,
Chapter 36,
p. 349
1064. b
Rosen 5th,
Chapter 36,
p. 345
1065. c
Rosen 5th,
Chapter 36,
p. 331
1066. c
Rosen 5th,
Chapter 37,
p. 372
1067. a
Rosen 5th,
Chapter 37,
p. 377
1068. e
Rosen 5th,
Chapter 37,
p. 373
Central cord syndrome is a hyperextension injury often seen in patients with
degenerative arthritis of the cervical vertebrae. The ligamentum flavum buckles into
the cord, resulting in a concussion or contusion of the central portion of the cord. This
injury affects the most central portions of the pyramidal and spinothalamic tracts.
Since nerve fibers that innervate distal structures are located in the periphery of the
spinal cord, these patients have a greater neurologic deficit in the upper extremities
than in the lower extremities.
The maximum neurologic deficit after blunt spinal cord trauma often is not seen
immediately but rather seems to progress and extend over many hours. The ultimate
extent of spinal cord injury can also be affected by reversible and preventable factors,
such as hypoxia, hypotension, hyperthermia, hypoglycemia, and mishandling by
medical personnel.
Fractures involving C1 and C2 are generally considered anatomically unstable because
of their location and the relative paucity of ligamentous and muscle support. In
assessing the stability of spinal injuries below C2, it is helpful to think of the spine as
consisting of two columns. The anterior column is formed by alternating vertebral
bodies and intervertebral disks held in alignment by the anterior and posterior
longitudinal ligaments. The posterior column, which contains the spinal canal, is
formed by the pedicles, transverse processes, articulating facets, laminae, and spinous
processes. If both columns are traumatically disrupted, the spine moves as two
separate pieces. Such a lesion is considered mechanically unstable, and the likelihood
of a spinal cord injury resulting from even a slight motion is great. On the other hand,
if only one column is disrupted, the other column resists further movement. Bilateral
facet dislocation is an extremely unstable condition that is often associated with spinal
cord injury. The clay shoveler's fracture is an oblique fracture of the base of the
spinous process of one of the lower cervical segments. Because this injury involves
only the spinous process, it is stable and not associated with neurologic involvement.
The hangman's fracture occurs when the cervicocranium is thrown into extreme
hyperextension as a result of abrupt deceleration. Bilateral fractures of the pedicles of
the axis occur with or without dislocation. This lesion is unstable.
The platysma muscle, sandwiched between the superficial and deep cervical fascia,
covers the anterolateral neck. It has clinical significance because of its superficial
location and proximity to vital structures. If the platysma muscle is violated, injury to
these structures should be suspected.
To date, arteriography remains the gold standard for diagnosing vascular injuries.
Despite a sensitivity and specificity of nearly 100% and a complication rate of less
than 2% for arteriography, other, less invasive diagnostic tests have been evaluated for
accuracy, speed, cost, and efficacy. Duplex ultrasonography has been used to exclude
cervical vascular injury in patients with both penetrating and blunt trauma. Despite
clinical success, limitations of ultrasonography include the risk of missing zone I and
III injuries and the lack of 24-hour availability at many centers.
Recent literature supports orotracheal RSI by in trauma patients with blunt or
penetrating neck injuries, and it should be considered the first-line airway technique
unless contraindications exist. Concerns over sedative-induced muscle relaxation
leading to airway distortion, although possible, have not been validated. Orotracheal
RSI is often successful even after neck trauma with airway distortion. RSI also has
been shown to be superior to intubation without paralytics. If the cervical spine must
remain immobilized, an assistant should maintain in-line stabilization of the head and
neck..
320
1069. Clinical findings of infraorbital anesthesia and inability to gaze vertically suggest:
a. zygomatic arch fracture
b. orbital wall fracture
c. orbital floor fracture
d. LeFort I fracture
e. LeFort II fracture
1070. Typical components of a tripod fracture are:
a. central maxillary fracture, orbital floor fracture, zygomatic arch fracture.
b. infraorbital rim fracture, zygomatico-frontal suture diastasis, zygomatico-temporal disruption.
c. orbital wall, pterygoid plate, nasal septum.
d. supraorbital rim fracture, zygomatico-frontal suture diastasis, zygomatico-temporal disruption.
e. zygomatico-frontal suture diastasis, zygomatico-temporal disruption, zygomatic arch fracture.
1071. In a dyspneic chest trauma patient with distended neck veins, hypotension, tracheal
deviation to the right and absent breath sounds on the left, the correct approach is:
a. confirm hemothorax with chest radiograph, place chest tube.
b. confirm simple pneumothorax with chest radiograph, place chest tube.
c. confirm tension pneumothorax with chest radiograph, place chest tube.
d. convert tension pneumothorax to simple pneumothorax with insertion of 14 gauge cannula in left
chest.
e. treat suspected cardiac tamponade with emergency pericardiocentesis.
1072. In a dyspneic chest trauma patient with distended neck veins, hypotension, midline
tracheal and equal breath sounds, the correct approach is:
a. confirm cardiac tamponade with chest radiograph, administer normal saline, perform
pericardiocentesis.
b. confirm cardiac tamponade with echocardiogram, administer normal saline, perform
pericardiocentesis.
c. suspect cardiac tamponade, administer normal saline, perform pericardiocentesis.
d. suspect bilateral tension pneumothoraces, perform bilateral needle decompression.
e. suspect bilateral simple pneumothoraces, place bilateral chest tubes.
1073. In a hypotensive chest trauma patient with unilateral absent breath sounds and a chest
radiograph showing a massive fluid collection, the ED approach involves:
a. immediate tube thoracostomy.
b. immediate thoracotomy.
c. fluid resuscitation to a systolic BP greater than 90, followed by operative repair.
d. early administration of O negative blood followed by tube thoracostomy.
e. early administration of fresh frozen plasma followed by tube thoracostomy.
321
1069. c
th
Rosen 5 ,
Chapter 35,
p. 324, 325
1070. b
Rosen 5th,
Chapter 35,
p. 324
1071. d
Rosen 5th,
Chapter 38,
p. 388, 391
1072. c
Rosen 5th,
Chapter 38,
p. 400
1073. a
Rosen 5th,
Chapter 38,
p. 391
Patients with orbital floor fractures may have impaired
upward gaze, diplopia due to entrapment of the inferior
rectus muscle within the fracture fragments, and
infraorbital hypoesthesia. Radiographic evaluation may
show the "hanging drop" sign of herniated contents into
the maxillary sinus depression of bony fragments into the
maxillary sinus, or emphysema of the orbit. Clouding of
a maxillary sinus on the side of the trauma must be
assumed to be an orbital fracture until proved otherwise.
Figure 35-9 Appearance of eyes and
limitation of motion typically present
in blowout fracture. Fracture of right
orbit is shown here.
The zygoma has two major components: the body or malar eminence and the
zygomatic arch. Two common fractures of this bone are (1) depression of the malar
eminence, with fracture lines usually at the zygomaticotemporal suture, at the
zygomaticofrontal suture, and through the infraorbital foramen (the so-called trimalar
or tripod fracture), and (2) depression of the zygomatic arch. Clinical signs of a tripod
fracture include flatness of the cheek, anesthesia in the distribution of the infraorbital
nerve, diplopia or change in consensual gaze, or a palpable step defect.
This description is classic for tension pneumothorax. It occurs when the injury acts
like a one-way valve and leads to a progressive increase of intrapleural pressure. Air
enters on inspiration but cannot exit with expiration, which compresses the vena cava
and distorts the cavoatrial junction, leading to decreased diastolic filling of the heart
and subsequent decreased cardiac output. These changes result in the rapid onset of
hypoxia, acidosis, and shock. When the diagnosis of tension pneumothorax is
suspected clinically, the pressure should be relieved immediately with needle
thoracostomy, which is performed by inserting a large-bore (16-or 18-gauge) through
the second or third interspace anteriorly or the fourth or fifth interspace laterally on the
involved side.
This patient has all the clinical signs of cardiac tamponade. Although an
echocardiogram would confirm the diagnosis, there may not be time do so in a
hemodynamically unstable patient. When the patient arrives in the ED, volume
expansion with crystalloid solution via two or three large-bore (14-or 16-gauge)
catheters should be established immediately. Aspiration of as little as 5 to 10 ml of
blood by pericardiocentesis may result in dramatic clinical improvement. Reducing
the total intrapericardial volume to just below the critical level allows compensatory
mechanisms to maintain adequate hemodynamics. Whenever possible,
pericardiocentesis should be performed under sonographic guidance because this
approach will increase success rate and decrease the incidence of complications.
This patient has a massive hemothorax. Treatment consists of restoring the circulating
blood volume, controlling the airway as necessary, and evacuating the accumulated
blood. Tube thoracostomy allows constant monitoring of the blood loss as well as
reexpansion of the lung. A large-bore tube (36 to 40 French) should be inserted in the
fifth interspace at the anterior axillary line and connected to underwater-seal drainage
and suction. Although small hemothoraces may be observed in stable patients, a
moderate hemothorax or any hemothorax in an unstable or symptomatic patient
requires tube thoracostomy. Severe or persistent hemorrhage requires thoracotomy.
322
1074. The child at moderate risk for intracranial injury would be the one with:
a. loss of consciousness for less than 5 minutes.
b. headache.
c. impact seizure.
d. vomiting.
e. seizure more than 20 minutes after impact.
1075. Concerning the Emergency Department management of facial lacerations:
a. beveled lacerations should be debrided parallel to the lacerated edges to preserve orientation with
the opposite side and allow for improved closure.
b. debris embedded in a traumatic abrasion should be removed by a consulting plastic surgeon 3 to 4
days after the accident to allow easier removal and facilitate a better cosmetic outcome.
c. dog bite puncture wounds to the face should be copiously irrigated, explored for deep tissue
injury, and closed primarily.
d. relatively clean facial wounds may be repaired up to 24 hours after injury.
e. cosmetic quality of the final result is apparent at 3 months.
1076. Loss of cerebral autoregulation leads to:
a. cerebral blood flow which varies with arterial pressure
b. compensatory hyperventilation
c. drastically decreased intracranial pressure
d. epidural hematoma
e. profound constriction of cerebral resistance vessels
1077. The most common CT scan abnormality found after severe closed head injury is:
a. cerebral contusion.
b. epidural hematoma.
c. intracerebral hemorrhage.
d. subdural hematoma.
e. traumatic subarachnoid hemorrhage.
1078. In children, the most commonly injured intra-abdominal structure is:
a. pancreas.
b. liver.
c. small bowel.
d. spleen.
e. kidney.
1079. Maternal death is the most common cause of fetal death in pregnant trauma patients.
What is the next most common cause?
a. placenta previa.
b. placental abruption.
c. fetal head injury.
d. fetal cardiac injury.
e. fetal organ rupture.
323
1074. e
th
Rosen 5 ,
Chapter 32,
p. 272
1075. d
Rosen 5th,
Chapter 35,
p. 318, 319
Chapter 54,
p. 778
1076. a
Rosen 5th,
Chapter 34,
p. 289
1077. e
th
Rosen 5 ,
Chapter 34,
p. 310
1078. d
Rosen 5th,
Chapter 32,
p. 279
1079. b
th
Rosen 5 ,
Chapter 31,
p. 258
The prognostic significance of vomiting after pediatric head trauma presents the
clinician with many challenges. There is no adequate study defining an acceptable
time frame in which vomiting after head injury is benign in nature. The development
of seizures after head trauma, in contrast to vomiting, has been well studied. A brief
seizure that occurs immediately after the insult (with rapid return of normal level of
consciousness) is commonly called "an impact seizure" and is usually unassociated
with intracranial parenchymal injury and in no way mandates the institution of
anticonvulsant therapy. Seizures that occur later (longer than 20 minutes after the
insult) portend the greater possibility of both internal injury and the development of
seizures at a later date. Patients who experience seizures later in the course of the
posttraumatic event are best evaluated by the neurosurgical service.
Beveled lacerations should have their edges debrided to convert to perpendicular
edges. Any embedded material in a traumatic abrasion should be carefully removed.
A delay in treatment may cause permanent discoloration (tattoo). Puncture wounds
from any species should not be closed. A wound up to 24 hours old may be closed on
the face, but this must be tempered by the mechanism of injury (e.g., severe crushing)
and the degree of contamination (e.g., animal bite). Patients with facial wounds should
be told that the final result of treatment cannot be evaluated until 6 to 12 months after
the injury, when maximum scar resorption and softening will have occurred.
With the loss of autoregulation, massive cerebral vasodilation occurs. Systemic
pressure is transmitted to the capillaries, and the outpouring of fluids into the
extravascular space can contribute to vasogenic edema and thus further increase ICP.
Traumatic subarachnoid hemorrhage (TSAH) is defined as blood within the CSF and
meningeal intima and probably results from tears of small subarachnoid vessels.
TSAH is detected on the first CT scan in up to 33% of patients with severe traumatic
brain injury and has an incidence of 44% in all cases of severe head trauma. It is
therefore the most common CT scan abnormality seen after head injury.
Injuries to the spleen are in the largest proportion of pediatric abdominal trauma. The
liver is the second most commonly injured solid organ in the pediatric patient with
abdominal trauma.
The leading causes of traumatic fetal death include maternal death, maternal shock and
hypoxia, placental abruption, and direct fetal injury. Abruption occurs in 2% to 4% of
minor accidents and in up to 38% of major injuries. Placental position does not appear
to affect the incidence of abruption. Fetal mortality in abruption cases approaches
54%. Classic clinical findings of abruption may include vaginal bleeding, abdominal
cramps, uterine tenderness, amniotic fluid leakage, maternal hypovolemia (up to 2 L of
blood can accumulate in the gravid uterus), or a change in the fetal heart rate. The
most sensitive indicator of placental abruption is fetal distress. Hence, prompt fetal
monitoring is very important in trauma during pregnancy. There is also a close linkage
of abruption to uterine activity. Pearlman et al find if there are 12 or more contractions
in any hour of a 4-hour cardiotocographic monitoring period, the risk of abruption is
14%.
324
1080. A 20-year-old cyclist hit a bump and was thrown over his handlebars at a speed of
approximately 20 mph. He has gross hematuria, severe abdominal pain, an elevated
lipase, and absent bowel sounds. The best approach to diagnosing his injuries is:
a. FAST exam.
b. diagnostic peritoneal lavage.
c. serial physical exams.
d. IVP.
e. CT with contrast.
1081. A 34-year-old man was the unrestrained driver in a high-speed rapid deceleration car
crash. He is transported with cervical spine precautions by a Basic Life Support unit. His
Glasgow Coma Scale score is 7, and there are no obvious signs of trauma. His breathing
is shallow, his pulse is thready, and his skin is cool. Prior to intubation, you should:
a. clear the lateral cervical spine x-ray
b. do a brief neurologic examination, including reflexes and Babinski.
c. give four good breaths with 100% oxygen using the bag-valve mask device.
d. obtain a complete set of vital signs.
e. perform chin lift to open the airway.
1082. A 19-year-old male was shot in the back, just lateral to the fifth thoracic vertebra, with a
small caliber handgun. Paramedics phone you with a blood pressure palpable at 90
mmHg, heart rate of 110, and a respiratory rate of 30 per minute. On arrival in your ED,
he has received 800cc of 0.9% saline, but his vital signs are unchanged. He is agitated
and sweaty. His neck veins are not distended, but you’re not certain about his heart tones
because of noise. Soon after arrival, his blood pressure starts to fall and his breathing is
more labored, but he is still conscious and oriented. Your next step should be:
a. bedside cardiac ultrasound.
b. blood transfusion.
c. needle decompression of the left chest.
d. pericardiocentesis.
e. thoracotomy.
1083. Select the true statement:
a. Motor vehicle collisions account for most pediatric head injuries.
b. Because of their smaller body surface are, hypothermia is less common in children than in adults.
c. Head injury is the most frequent cause of traumatic death in children.
d. Initial assessment and management of an injured child differs from that of an adult.
e. Maintenance requirement for .
1084. A distraught mother brings her 3-month-old for evaluation after she accidentally dropped
him from his changing table onto the wooden floor. You would be most concerned about
major head injury if you found that the child:
a. had a tonic-clonic seizure lasting 20 seconds immediately after the fall.
b. has been lethargic since the fall.
c. is hypotensive.
d. threw up once almost immediately after the fall.
e. was pale and sweaty for a few minutes after the fall.
325
1080. e
th
Rosen 5 ,
Chapter
1081. c
Rosen 5th,
Chapter 30,
p. 246, 248
1082. a
Rosen 5th,
Chapter 38,
p. 398
1083. c
Rosen 5th,
Chapter 32,
pp. 268, 272,
267
1084. c
Rosen 5th,
Chapter 32,
p. 274
Chapter 34,
p. 300
Compared with other modalities, numerous advantages of CT are cited. It is
noninvasive and has the potential to define the injured organ and the extent of the
pathologic condition. It is most accurate for solid visceral pathology and is often
capable of discerning the presence, source, and approximate quantity of intraperitoneal
hemorrhage. It evaluates the retroperitoneum, an area not sampled by DPL, as well as
the vertebral column and can be readily extended above or below the abdomen to
visualize the thorax or pelvis. It is helpful in the evaluation of hematuria and, if used
early enough, in determining renal artery injury. The primary role of FAST is
detecting free intraperitoneal blood after blunt trauma. IVP only visualizes the renal
parenchyma, and serial exams only suggest an improving or worsening clinical
situation.
This patient requires immediate intubation and ventilation. Securing the airway,
maintaining ventilation, controlling hemorrhage, and treating shock are first priorities
because of their crucial importance for survival. The evaluation of neurologic
function, the cardiac examination, and the status of the abdomen and musculoskeletal
systems are in the second echelon of priorities and should be addressed only after the
more critical ones. For patients who need immediate intubation, head-stabilized oral
intubation with rapid sequence induction is recommended before obtaining cervical
spine radiographs.
It is unclear whether this patient has pericardial tamponade, a tension pneumothorax,
or hemorrhagic shock. The physical findings of pericardial tamponade are
hypotension, distended neck veins, and, rarely, distant or muffled heart tones. This so
called Beck's triad is sometimes difficult to demonstrate clinically, especially in the
midst of a major resuscitation with concomitant hypovolemia. The most reliable signs
of pericardial tamponade are an elevated CVP (>15 cm H2O) with hypotension and
tachycardia. When this triad is present, the diagnoses of acute pericardial tamponade
and tension pneumothorax, should be considered. Ultrasound enables rapid, accurate,
and noninvasive diagnosis of pericardial tamponade. It can be performed at the
bedside in the ED during the initial resuscitation of the patient. The sonographic
definition of tamponade is the simultaneous presence of pericardial fluid and diastolic
collapse of the right ventricle or atrium.
Falls account for 37% and MVCs for 18% of pediatric head trauma. The
proportionately large surface area of an infant or child relative to weight predisposes
them to large amounts of heat loss as a result of evaporation. Head trauma is the
leading cause of death among injured children and is responsible for 80% of all trauma
deaths. The initial assessment and management of children is similar to adults.
Trauma accounts for approximately 30% of infant deaths.
Many children experience a brief impact seizure at the time of relatively minor head
injury. By the time the child is evaluated, he or she is at baseline neurologic function.
Following minor head trauma, children may demonstrate anorexia, lethargy, vomiting,
or pallor soon after the insult followed by a rapid recovery to baseline. Hypotension
from intracranial bleeding can occur in children less than 1 year of age with a large
linear skull fracture and an underlying large epidural hematoma, which is associated
with major head injury.
326
1085. You are evaluating a 22-year-old woman who was the restrained driver in a head-on
motor vehicle collision. She is immobilized on a long board with a hard collar in place.
You know that:
a. in a neurologically normal patient, lack of midline tenderness can safely exclude a cervical spine
injury
b. a lateral cervical spine film is adequate when all 7 vertebrae are visualized
c. approximately 25% of patients with head injuries also have spinal injuries.
d. sedation of the patient may be necessary because of the discomfort of immobilization.
e. if you decide to order cervical spine x-rays, you must see a lateral, odontoid, and AP view before
you can radiographically clear the cervical spine.
1086. People over age 65 years:
a. are more cautious about their balance and therefore fall less frequently than younger people.
b. are more likely to die in a car crash than from any other traumatic injury.
c. have generally been spared from the increased occurrence in assaults and other person-on-person
crimes.
d. rarely are injured in falls which occur where someone is nearby, such as a nursing home.
e. usually sustain multiple orthopedic fractures after a fall.
1087. A 75-year-old man comes to the ED with his son, who tells you
the patient is “not acting right.” A head CT shows a large
collection of blood, with slight midline shift. You know that:
a. brain atrophy should make him less susceptible to this type of
bleed.
b. if the injury is acute, the possibility of the patient leaving the
hospital alive is less than 25%.
c. mortality from this injury in the elderly is less than half that in
younger patients.
d. the patient is probably a victim of abuse, as this is an uncommon
injury without major trauma.
e. this injury is usually caused by tearing of the middle meningeal
artery.
1088. An 82-year-old man complains of neck pain after falling and striking his head on the
refrigerator as he was bending over to retrieve his glasses from the floor. You have
ordered cervical spine radiographs, knowing the most common injury in this age group is:
a. Jefferson’s fracture.
b. odontoid fracture, Type II.
c. rotary subluxation.
d. spinal cord injury without radiographic abnormality (SCIWORA).
e. unilateral facet subluxation.
1089. Which of the following is true regarding metatarsal fractures:
a. metatarsal fractures are 5-10% of foot fractures
b. nondisplaced first metatarsal fractures should be treated with casting for 4 to 6 weeks
c. the most common metatarsal base fractures occur at the first metatarsal.
d. fifth metatarsal shaft stress fractures are uncommon.
e. metatarsal shaft fractures are rarely unstable
327
1085. e
th
Rosen 5 ,
Chapter 30,
p. 250
Chapter 36,
p. 346
1086. b
Rosen 5th,
Chapter 33,
p. 281
1087. b
Rosen 5th,
Chapter 33,
p. 283
1088. b
Rosen 5th,
Chapter 33,
p. 283
1089. b
Rosen 5th,
Chapter 52,
p. 725, 728,
729
A spinal injury can be safely excluded only when the patient has normal mental status,
absence of neck pain or tenderness, lack of new neurologic signs or symptoms, and
lack of a distracting painful injury. A cervical spine film is not adequate unless all
seven cervical vertebrae and the top of the first thoracic vertebra are visualized.
Significant forms of head or facial trauma have a 5% to 10% incidence of associated
cervical spine injuries. Sedation is reserved for patients with known or probable spinal
injuries who pose a danger to themselves because of excessive movement.
Falls are the most common mechanism of injury in the elderly, accounting for 40% of
trauma in patients older than 65 years of age. Most falls occur at home and are
ground-level falls. The most common injuries sustained in falls are fractures,
occurring in 5% of fall victims. Overall, the mortality rate from falls in elderly patients
approaches 12%. While MVCs are the second most common cause of trauma in the
elderly, the overall fatality rate among elderly MVC victims is as high as 21%.
Head injuries are the most common cause of mortality in elderly trauma patients. The
most common mechanism of significant head injury in the elderly is falls. Epidural
hematomas are rare because of the adherence of the dura mater to the inside of the
skull. Cerebral contusions, however, occur in up to one third of head-injured elderly
patients. Subdural hematomas become more common with age because of the
stretching of the fragile bridging veins as the brain atrophies. The mortality from
subdural hematoma in the elderly is 4 times higher than in younger patients. In acute
subdural hematomas only 1 in 5 elderly patients will survive to discharge.
The most common mechanism likely to cause a spinal injury in an older person is a
fall. Because of the relative immobility of the cervical spine related to DJD, the most
common level of cervical spine injury in the elderly occurs at C1 to C3, higher than in
younger patients. The most common fracture of the cervical spine in the elderly is a
type 2 odontoid fracture, which necessitates adequate visualization of this area of the
cervical spine and may require CT scans with reconstructions.
Phalangeal fractures are the most common forefoot fracture. Most undisplaced
metatarsal shaft fractures of the second through fifth metatarsal may be treated in a
below-knee walking cast for 2 to 4 weeks. The great toe metatarsal requires more
aggressive management because of its biomechanical role and the stresses imposed on
it during gait. Nondisplaced first metatarsal fractures should be treated with casting for
4 to 6 weeks. Atleast the first 3 weeks of this immobilization, if not the entire period,
should be non-weight bearing. The most commonly encountered metatarsal base
fractures occur at the fifth metatarsal. The third metatarsal is the most commonly
fractured, and metatarsal shaft stress fractures are common. Navicular fractures,
although rare, are the most common midfoot fracture.
328
1090. Which of the following measurements of Boehler’s angle would indicate a compression
fracture of the calcaneus?
a. 45 degrees
b. 40 degrees
c. 30 degrees
d. 25 degrees
e. 15 degrees
1091. Identify the fracture on the accompanying radiograph and choose the
correct emergency management.
a. bimalleolar fracture; cast and crutches in ED; referral to ortho in 48
hours
b. bimalleolar fracture; posterior splint in ED; referral to ortho in 48 hours
c. bimalleolar fracture; posterior splint; orthopedic consult in ED; admit to
ortho
d. trimalleolar fracture; cast and crutches in ED; referral to ortho in 48 hours
e. tibiotalar dislocation; posterior splint in ED; ortho consult in ED; admit to
ortho
1092. According to the Ottawa ankle guidelines, which patient does not need an ankle
radiograph?
a. 25-year-old man, inversion mechanism, could not bear weight at the scene of injury; point
tenderness at tip of lateral malleolus; could not bear weight in the ED
b. 35-year-old runner, inversion injury; finished last mile of his normal 3 mile run, then came to ED
with swollen, tender ankle.
c. 22-year-old woman, uncertain mechanism, possible eversion of ankle playing basketball, carried
off court due to inability to bear weight; point tenderness over medial malleolus.
d. 12-year-old Little League baseball player, turned ankle sliding into second base, walked off field;
pain over both malleoli.
e. 50-year-old construction worker, jumped off scaffold, landed on irregular dirt pile, turned ankle,
carried from site to ambulance; marked bilateral malleolar tenderness, swelling.
1093. Radiographs indicate a spiral fracture of the distal 1/3 of the tibia in a young athlete who
was injured when he made a sharp turn while wearing cleated shoes in a football game.
An associated injury that should be sought is a fracture of the:
a. contralateral tibia
b. ipsilateral 5th metatarsal
c. ipsilateral femur
d. ipsilateral proximal fibula
e. patella
1094. The typical physical finding in intertrochanteric hip fracture is a(n)
a. shortened, internally rotated lower extremity
b. flexed, abducted lower extremity
c. shortened, externally rotated lower extremity
d. externally rotated lower extremity of equal length with the opposite leg
e. lower extremity that is in the normal anatomic position
329
1090. e
th
Rosen 5 ,
Chapter 51,
p. 724, 725
1091. c
Rosen 5th,
Chapter 51,
p. 712
1092. b
Rosen 5th,
Chapter 51,
p. 709
1093. d
Rosen 5th,
Chapter 50,
p. 702
1094. c
Rosen 5th,
Chapter 49,
p. 656
Boehler’s angle is measured on the lateral view of the
angle between two lines: one between the posterior
tuberosity and the apex of the posterior facet, and the
other between the apex of the posterior facet and the
apex of the anterior process. An angle of less than 20
degrees suggests a compression fracture, and comparison
measurement of the uninjured side is helpful in
Fig. 51-22
questionable cases.
Bimalleolar fractures involve the disruption of at least two elements of the ankle ring
and therefore are unstable. These fractures result from adduction or abduction forces,
although the latter is more common. Rotational injuries also can cause bimalleolar
fractures as well as trimalleolar fractures if the posterior malleolus is involved. All
bimalleolar fractures require orthopedic consultation in the ED. Controversy exists
about whether such injuries should be treated closed or surgically.
The Ottawa Ankle Rules (OAR) state that an ankle radiographic series is required if
there is pain in the malleolar region and any one of the following findings: bone
tenderness at the posterior edge of the distal 6 cm of the lateral malleolus, at posterior
edge of the distal 6 cm of the medial malleolus, at the navicular bone, at the fifth
metatarsal, or if the patient is unable to bear weight for at least four steps both
immediately after the injury and at the time of evaluation. The OAR have a sensitivity
approaching 100% in detecting malleolar zone ankle fractures and midfoot zone
fractures. The OAR do not apply for subacute or chronic injuries.
This is a Maisonneuve's fracture, which is a proximal fibula fracture with an associated
ankle fracture or deltoid ligament tear. The mechanism resulting in the Maisonneuve's
fracture is often an external rotatory force applied to the ankle that results in partial or
complete syndesmotic disruption. Palpation of the proximal fibula should be
performed whenever significant ankle injury is present to assess for a Maisonneuve's
fracture.
The fracture line of intertrochanteric fractures extends between the greater and lesser
trochanter of the femur. They are considered extracapsular fractures. The fracture line
extends through cancellous bone and has an excellent blood supply. The hip's short
external rotators remain attached to the proximal femoral neck and the internal rotators
are attached to the distal femur, explaining the position the leg assumes with this
fracture.
330
1095. The abnormality depicted in this radiograph
a. fifth metatarsal base fracture
b. tarsometatarsal joint disruption (Lisfranc)
c. tibio-talar dislocation
d. talar neck fracture
e. fracture first proximal phalanx
is
1096. Ankle radiographs of a young athlete who landed on a plantar flexed foot reveal anterior
displacement of the talus without a corresponding fracture. Choose the correct
emergency management of this dislocation.
a. Air Cast, discharge with instructions on partial weight-bearing, orthopedic referral in 48 hours
b. stirrup splint, crutches, referral to orthopedics in 48 hours
c. procedural sedation / analgesia, reduction in ED, observation for neurovascular compromise
d. procedural sedation / analgesia, reduction in ED, post-reduction radiographs, observation for
neurovascular compromise
e. posterior splint, arrangements for orthopedics to take patient to OR for open reduction
1097. The most appropriate Emergency Department management of an acute Achilles tendon
rupture is:
a. Ace bandage to ankle, referral to orthopedics
b. posterior splint in plantar flexion, crutches, referral to orthopedics in 1 week
c. posterior splint in dorsiflexion, crutches, referral to orthopedics in 1 week
d. immediate circular casting by the ED physician, crutches, orthopedic referral
e. emergency orthopedic consultation
1098. You are monitoring a woman who is in her third trimester of pregnancy and was involved
in a minor “fender-bender.” You have cleared the mother medically and have attached her
to a fetal monitor so you can check the fetus. You know that:
a. beat-to-beat variability of fetal heart rate during a uterine contraction is abnormal and ominous.
b. fetal heart rate should not vary at all during a contraction after trauma.
c. late decelerations are a sign of fetal hypoxia.
d. late heart rate decelerations after trauma are a favorable physiologic response to stress.
e. variable decelerations are normal.
1099. The term “greenstick fracture” refers to:
a. avulsion of ischial tuberosity in an athlete.
b. buckle fracture of a long bone in a child.
c. fracture that is not visible on standard radiographs, but visible on bone scan.
d. incomplete angulated fracture of a long bone in a child.
e. stress fracture in a child.
1100. A 10 year old has suffered a supracondylar humerus fracture. During exam you find that
the child cannot extend his fingers after wrist extension. The nerve which has probably
been injured is the:
a. anterior interosseous.
b. brachioradialis.
c. median.
d. radial.
e. ulnar.
331
1095. b
th
Rosen 5 ,
Chapter 51,
p. 726, 727
1096. d
Rosen 5th,
Chapter 51,
p. 722
1097. e
Rosen 5th,
Chapter 51,
p. 716
1098. c
Rosen 5th,
Chapter 31,
p. 262
1099. d
Rosen 5th,
Chapter 42,
p. 169
1100. d
Rosen 5th,
Chapter 169,
p. 2374
Chapter 45,
p. 566
Chapter 101,
p. 1511
This is a Lisfranc injury diagnosed by stepoff at the base of the second metatarsal and
middle cuneiform and widening between the bases of the first and second metatarsals.
In homolateral injuries, all five metatarsals are displaced in the same direction. In
divergent injuries, the metatarsals are splayed outward in both the medial and lateral
directions. These usually occur between the first and second metatarsals because of
their lack of an intermetatarsal connection. The clinical presentation varies with the
extent of injury and displacement. Severe pain in the midfoot and inability to bear
weight, particularly on the toes, usually occur. Paresthesias are occasionally present,
and examination usually reveals edema and ecchymosis.
The treatment of major talar fractures is controversial. Any significantly displaced
fracture, particularly if associated with neurovascular or cutaneous compromise, should
have an early attempt at closed reduction in the ED. With neurovascular or cutaneous
compromise, reduction should not be delayed by waiting for radiographs or
consultation. After appropriate analgesia or conscious sedation, reduction is performed
by grasping the hindfoot and midfoot and applying longitudinal traction with plantar
flexion. This is followed by realignment of the foot as reduction is achieved. Posterior
slab immobilization and postreduction radiographs should then follow.
The choice of operative versus nonoperative management is controversial. Surgical
repair has a lower incidence of rerupture (1.4% versus 13.4% in nonoperative
management), less muscle atrophy, and earlier resumption of activities. Nonoperative
therapy, which involves a series of casts changed in 2-to 4-week intervals, avoids
operative complications and decreases hospitalization and sick leave time. Emergency
orthopedic referral of patients with Achilles tendon rupture is recommended.
The loss of beat-to-beat and long-term variability warns of fetal central nervous system
depression and reduced fetal movement caused by fetal distress. Late decelerations are
an indication of fetal hypoxia. These decelerations are relatively small in amplitude
and occur after the peak or conclusion of a uterine contraction. By comparison, early
decelerations are larger, occur with the contraction, and recover to baseline
immediately after the contraction. Early decelerations may be vagally mediated when
uterine contractions squeeze the fetal head, stretch the neck, or compress the umbilical
cord. Variable decelerations are large, occur at any time, and are possibly caused by
umbilical cord compression.
Bones of children are necessarily soft and resilient and therefore sustain a number of
incomplete fractures. Greenstick fractures are incomplete angulated fractures of long
bones. The periosteum and and cortex are disrupted on the convex side; the
periosteum on the fracture's compression side remains intact. This fracture may need
to be completed to achieve an anatomic reduction.
In all cases of supracondylar fractures, it is important to carefully assess the distal
neurovascular status. Nerve injuries occurred in 7% of 4520 fractures compiled from
31 major reported series. The radial, median, and ulnar nerves are all commonly
involved. Most deficits seen at the time of injury are neurapraxias that resolve with
conservative management. Motor function returns within 7 to 12 weeks, whereas
recovery of sensation may take more than 6 months. The radial nerve controls
extension of the fingers, thumb, wrist, and elbow.
332
1101. An 8-year-old girl fell on her outstretched hands at the local playground. Her exam shows no
swelling or deformity, but she is tender when you palpate her distal radius. Her x-ray shows a
small “buckle” in the radial cortex, with no angulation. The correct ED management includes:
a. Ace bandage, ice / elevation, early mobilization.
b. immediate orthopedic consult for casting.
c. none – films are normal.
d. preparation for immediate operative management.
e. volar or sugar-tong splint, ice / elevation, referral to family doctor or orthopedics.
1102. A 25-year-old male arrives with several softball teammates after he injured his shoulder during a
headfirst slide into third base. His hand is behind his head, and he is in severe pain. His humerus is
fully abducted and his elbow is flexed. He has probably incurred:
a. anterior glenohumeral dislocation
b. distal clavicle fracture
c. inferior shoulder dislocation (luxatio erecta)
d. posterior glenohumeral dislocation
e. proximal humerus fracture
1103. Which statement regarding pediatric trauma is correct?
a. Splenic lacerations are usually treated operatively.
b. Abdominal trauma is the most common cause of unrecognized fatal injury in children..
c. Blunt force mechanisms cause 70% of pediatric abdominal trauma.
d. Chance fractures occur in about 25% of restrained children involved in MVCs.
e. Children have proportionally smaller organs than adults.
1104. A patient with a C8 cervical radiculopathy will have difficulty with:
a. arm abduction.
b. elbow extension.
c. elbow flexion.
d. hand grasp.
e. wrist extension.
1105. An adult patient has a full thickness burn of the left arm and leg, with a complete facial burn,
sparing the posterior head. Genitalia and right arm and leg are spared. Half of the torso anteriorly
is burned. The estimated percentage of burn is:
a. 36%.
b. 41%.
c. 45%.
d. 51%.
e. 54%.
1106. With injuries caused by a fall, the Emergency Physician should be aware of the correlation between
the severity of an injury and the height from which the fall took place. Using 12 feet as an average
floor or story, the estimated heights lethal to 50% of the population is:
a. 4 floors.
b. 5 floors.
c. 6 floors.
d. 7 floors.
e. 9 floors.
333
1101. e
th
Rosen 5 ,
Chapter 169,
p. 547, 2370
1102. c
Rosen 5th,
Chapter 46,
p. 595-599
1103. b
Rosen 5th,
Chapter 32,
p. 276-279
1104. b
Rosen 5th,
Chapter 101,
p. 609
1105. b
Rosen 5th,
Chapter 56,
p. 806-807
1106. e
Rosen 5th,
Chapter 30,
p. 244
There are three types of fractures of the radial metaphysis. This patient has a torus
fracture which results in a buckling of the radial cortex without cortical disruption. Due
to the strong periosteum, these fractures are not typically associated with severe
angulation, displacement, or rotational abnormalities, and the emergency physician can
competently manage most. Reduction techniques are rarely, if ever, necessary. These
fractures are initially treated with immobilization in a volar or sugar-tong splint with
conversion to a short arm cast on orthopedic follow-up. Healing usually occurs over 2
to 3 weeks, and complications are rarely seen. Analgesia requirements in the immediate
days after the injury are usually minimal after proper immobilization.
Although much less common than anterior and posterior shoulder dislocations, most
Emergency Physicians will see an inferior dislocation during their careers. Mechanism
of injury usually involves a hyperabduction force that levers the humeral neck against
the acromion. Then, the inferior capsule tears and the humeral head dislocates
inferiorly. Clinically the patient has the arm locked overhead in 110 to 160 degrees of
abduction. The elbow is usually flexed, and the forearm typically rests on top of the
head. The shoulder is fixed in this position, and any attempts at movement will result in
significant pain. The inferiorly displaced humeral head may be palpable along the
lateral chest wall. A thorough neurovascular examination is essential, and if possible,
orthopedic consultation should be obtained before attempting closed reduction. ED
reduction involves upward and outward traction, accentuating the long axis in which the
humerus is already found. A second person applies countertraction. Brachial plexus
injuries are very common and rotator cuff injuries are almost always associated with this
injury. Thrombosis of the axillary artery has also been associated with luxatio erecta;
adhesive capsulitis is a common long-term complication.
Because of the desire to maintain immunocompetency in childhood, the spleen is often
left in place as long as the patient can be adequately resuscitated with crystalloid and
blood products. Abdominal trauma is the most common cause of unrecognized fatal
injury in children. Pediatric abdominal trauma results from blunt causes in 85% of
cases, and penetrating trauma accounts for the remaining 15%. Blunt trauma related to
MVCs causes more than 50% of the abdominal injuries in children, and lap-belt injury,
including small bowel injury and Chance fractures occurs, in approximately 5% to 10%
of restrained children involved in MVCs. Children have proportionally larger solid
organs, less subcutaneous fat, and less protective abdominal musculature than adults,
and therefore relatively more solid organ injuries from both blunt and penetrating
mechanisms.
Cervical Nerve Root
Motor Findings
Decreased forearm flexion and hand extension, decreased
C6
shoulder adduction, weak biceps reflex
Weak triceps and finger extension; weak triceps reflex
C7
Weak hypothenar and hand flexors; weak elbow extension
C8
9% for arm
18% for leg
5% for face
9% for torso
With injuries caused by a fall, the Emergency Physician should be aware of the
correlation between the severity of an injury and the height from which the fall took
place. Using 12 feet as an average floor or story, the estimated heights lethal to 50%
and 90% of the population (LD50 and LD90) for falls are four and seven floors,
respectively.
334
1107. Criteria for transport to a trauma center include:
a. respiratory rate of 32 per minute.
b. fall from greater than twice patient’s height.
c. gunshot to extremity distal to elbow or knee.
d. motor vehicle crash with deformity of 12 – 18 inches.
e. motor vehicle crash with intrusion into passenger compartment of 8 – 10 inches.
1108. Estimated fluid and blood loss is made based upon certain physiologic criteria. Assuming that the
patient is a healthy, non-athletic, 40-year-old male, who takes no medication, has no pacemaker,
and has no other complicating medical issues, the findings or vital signs most consistent with a
class III hemorrhage would be:
a. normal blood pressure.
b. pulse rate of 110.
c. increased pulse pressure.
d. measured blood loss of 1750 cc.
e. pulse rate of 152.
1109. A physical finding which might help differentiate cardiac tamponade from a tension pneumothorax
would be:
a. absent breath sounds.
b. agitation.
c. distended neck veins.
d. hypotension.
e. muffled heart sounds.
1110. Match the Glasgow Coma Scale finding with its correct numeric value.
a. abnormal extension: 3
b. abnormal flexion: 4
c. disoriented but converses: 3
d. eye opening to pain: 1
e. eye opening to verbal command: 3
1111. The leading cause of traumatic death in children over 1 year of age is:
a. burns.
b. chest trauma.
c. head trauma.
d. infection after trauma.
e. multi-system failure.
1112. Which of the following is correct concering pediatric head trauma?
a. Sutures provide pliability to the pediatric skull that protects not only the skull, but also the brain
parenchyma from injury.
b. The pediatric brain is well myelinated.
c. Seizures that occur later (longer than 20 minutes) after the insult) portend the greater possibility
of both internal injury and the development of seizures at a later date.
d. Impact seizures are associated with intracranial parenchymal injury.
e. Subdural hematomas in children are almost always associated with the presence of overlying
fractures.
335
f.
1107. a
th
Rosen 5 ,
Chapter 30,
p. 243-244
1108. d
Rosen 5th,
Chapter 30,
1109. a
Rosen 5th,
Chapter 38,
p. 389-390
1110. e
Rosen 5th,
Chapter 34,
p. 292
1111. c
1112. e
Rosen 5th,
Chapter 32,
p. 272-274
Abnormal vital signs (GCS < 14 or systolic BP < 90) (respiratory rate < 10 or >29)
Multiple-system trauma
Penetrating wound to: 1) Head, neck, or torso; 2) Gunshot wound(s) to extremities
proximal to elbow and knee; 3) An extremity with neurovascular compromise
CNS injury (head, spine)
Suspected pelvic fracture
Mechanism of injury: Intrusion into passenger compartment greater than 12 inches or
major vehicular deformity greater than 20 inches
Ejection
Entrapment
Falls greater than three times the patient’s height
Fatality in same passenger compartment
Rapid deceleration
Auto-pedestrian / auto-bicycle injury with impact >5 mph
Vehicular rollover
Exposure to blast / explosion
Class I
Class II
Class III
Class IV
Up
to
750
750
–
1500
1500
–
2000
>2000
Blood Loss (mL)
15 – 30%
30 – 40%
>40%
Blood loss (%) Up to 15%
100 – 120
120 – 140
>140
Pulse rate <100
Normal
Decreased
Decreased
Blood pressure Normal
Decreased
Decreased
Decreased
Pulse pressure Normal or increased
Beck's triad for pericardial tamponade (hypotension, distended neck veins, and, rarely,
distant or muffled heart tones) is sometimes difficult to demonstrate clinically,
especially in the midst of a major resuscitation with concomitant hypovolemia. The
most reliable signs of pericardial tamponade are an elevated CVP (15 cm H2O) in
association with hypotension and tachycardia. Pulsus paradoxus may also be present.
The cardinal signs of tension pneumothorax are tachycardia, jugular venous distention,
and absent breath sounds on the ipsilateral side. They are dyspneic, agitated, restless,
cyanotic, tachycardic, and hypotensive and display decreasing mental activity. Absent
breath sounds are the key to clinically differentiating these two conditions.
abnormal extension: 2
abnormal flexion: 3
disoriented but converses: 4
eye opening to pain: 2
Head injury is the most frequent cause of trauma death in children over age 1 year.
There are some important anatomical differences between children and adults that play a
role. The child's cranial vault is larger and heavier in proportion to the total body mass.
This predisposes the child to high degrees of torque generated by any forces along the
cervical spine. The sutures in the child's skull are both protective and detrimental
regarding head injury in these patients. The cranium is more pliable and resistant to
skull fractures, but forces are generated internally that can damage the brain
parenchyma without fracturing the skull. The pediatric brain is less myelinated,
predisposing it to shearing forces and further injury. A brief seizure that occurs
immediately after the insult (with rapid return of normal level of consciousness) is
commonly called an impact seizure and is unassociated with intracranial parenchymal
injury. However, seizures that occur longer than 20 minutes after the insult indicate
greater possibility of both internal injury and the development of seizures at a later date.
336
1113. An 8 month old infant is brought to you for evaluation after falling off the bed. The child will open
her eyes when you shout, withdraws and grunts to pain. What is the GCS score?
a. 8
b. 9
c. 10
d. 11
e. 12
1114. The most common form of shock in children is:
a. cardiogenic.
b. hypovolemic.
c. hypoxic.
d. neurogenic.
e. septic.
1115. In children, one may need a GCS system that is age oriented. A simple modification includes the
AVPU system. The correct matching for the AVPU system is:
a. A - the child is able to Ask for something
b. V - the child is able to Visually track the questioner
c. P - the child is able to Point to specific people
d. U - the child is Uncooperative when asked to move an extremity
e. P - the child responds to Painful stimuli
1116. After head trauma in a child, a high-risk finding which mandates CT evaluation is:
a. alcohol / drug intoxication.
b. dizziness.
c. focal neurologic findings.
d. headache.
e. persistent vomiting 8 hours after injury.
1117. The most common cause of lethal hemorrhage in the pediatric population is injury to the:
a. Spleen.
b. Liver.
c. Kidney.
d. Small intestine.
e. Large intestine.
1118. Which of the following children should be referred to a pediatric burn center?
a. 12-year-old girl with chemical burns of her chest
b. 10-year-old boy with second degree circumferential burns of his left thigh
c. 6-year-old boy with first degree burns of his hands, feet, or genitalia
d. 10-year-old girl with 8% TBSA second degree burns
e. 12-year-old boy with 5% TBSA third degree burns of his arm
337
1113. b
th
Rosen 5 ,
Chapter 32,
p. 269
1114. b
th
Rosen 5 ,
Chapter 32,
p. 269-270
1115. e
th
Rosen 5 ,
Chapter 32,
p. 268
1116. c
th
Rosen 5 ,
Chapter 32,
p. 274, 298,
302
1117. b
th
Rosen 5 ,
Chapter 32,
p. 279
1118. b
th
Rosen 5 ,
Chapter 56,
p. 812, Box
56-2
The infant scores 3 for eye opening to verbal command, 4 for withdrawing to pain, and
2 for grunting to pain for a total of 9. (Table 32-2)
Hypovolemic shock is the most common form of shock in children. Recognizing the
subtle early signs of shock can be daunting even for experienced emergency
physicians. Children can maintain an adequate blood pressure, even in the face of
severe blood loss, but other signs of shock will be apparent.
In the AVPU system the child’s consciousness is rated as: Alert, responds to Verbal
stimuli, responds to Painful stimuli, or Unresponsive. (Box 32-2)
CT scan should be obtained for the presence of neurologic deficits, GCS 14 or lower,
or injury patterns that are the result of major forcible insults. For children less than
one year of age, CT scan is recommended for any loss of consciousness, protracted
vomiting, irritability, poor feeding or suspicion of abuse.
The liver is the second most commonly injured solid organ in the pediatric patient with
abdominal trauma, after the spleen. It is, however, the most common cause of lethal
hemorrhage, carrying a mortality rate of 10% to 20% in severe liver injury.
Burn center referral criteria include 2°/3° burns more than 20% BSA (or >10% BSA in
child under 10 years of age or involving face, hands, feet, or genitalia), 3° burns over
10% BSA, 2°/3° circumferential burns, electrical/lightning/inhalational burns,
chemical burns on face, feet, hands or genitalia, patients with burns and pre-existing
medical disorders that affect burn management, or inability/inexperience with pediatric
burn management at referring center.
338
1119. The best way to manage a patient whose foreskin is caught in a zipper is:
a. stat consult urology.
b. decompress the swollen tissue with an ice pack and wiggle the skin free of the zipper.
c. split the median zipper bar with a wire cutter.
d. use local anesthetic with epinephrine, then excise the skin and refer for a patch skin graft.
e. use a ring cutter on the zipper teeth at the level of attachment.
1120. The most common source of blunt abdominal injury in pregnant women is:
a. aggravated assault.
b. falls.
c. motor vehicle collisions.
d. self-inflicted.
e. spousal violence.
1121. Which physiologic changes of pregnancy can affect interpretation of vital signs in the pregnant
victim of trauma?
a. Blood pressure normally increases by 10 – 15 mmHg in the 3rd trimester.
b. Blood volume begins to expand at week 10, and may increase by 50%.
c. Cardiac output begins to decrease at week 10, and may reduce by 25%.
d. Heart rate decreases by 10 – 20 beats per minute during the 2nd trimester.
e. The diaphragm is lowered by as much as 4 cm and tidal volume increases by 40% as residual
volume increases by 25%.
1122. In the injured pregnant patient, a test which may help verify mixing of fetal and maternal blood
cells is the:
a. Bowling-Greene pathway.
b. Fels-Naphtha assessment of pH for ferning.
c. Hurling index.
d. Kleihauer-Betke assay.
e. Rimsky-Korsakov suite.
1123. Of listed radiographic studies, the one giving greatest radiation exposure to a viable fetus is:
a. abdominal film.
b. cervical spine film.
c. head CT scan.
d. lumbar spine film.
e. pelvis film.
1124. Which of these represents a correct chance of survival for perimortem cesarean delivery?
a. Gestational age 22 weeks, survival 8%
b. Gestational age 23 weeks, survival 12%
c. Gestational age 24 weeks, survival 40%
d. Gestational age 25 weeks, survival 50%
e. Gestational age 26 weeks, survival 75%
339
1119. d
th
Rosen 5 ,
Chapter 167,
p. 2328
1120. c
th
Rosen 5 ,
Chapter 31,
p. 257
1121. b
Rosen 5th,
Chapter 31,
p. 256
1122. d
Rosen 5th,
Chapter 31,
p. 260
1123. d
Rosen 5th,
Chapter 31,
p. 259, Table
31-2, 31-3
1124. e
th
Rosen 5 ,
Chapter 31,
p. 262, Table
31-5
Zipper entrapment of the foreskin can occur in children, especially those between 2
and 6 years of age. The zipper can be removed with bone or metal cutters to cut the
median bar of the zipper (see Figure 167-2)l The zipper falls apart and the foreskin is
freed.
The most common cause of blunt abdominal trauma in pregnant women is the motor
vehicle crash, which accounts for up to 70% of acute injuries. The major problem
centers on one third to one half of all pregnant women not using seat belts or not using
them properly. The reasons most often cited include discomfort, inconvenience, a
habit of never using seat belts, or fear of hurting the baby. However, unbelted women
are 2.3 times more likely to give birth within 48 hours of a crash and 4.1 times more
likely to experience fetal death. Improper placement of the lap belt over the pregnant
abdomen causes a threefold to fourfold increase in force transmission through the
uterus. Pregnant crash test dummy tests show that the lowest force transmission
readings through the uterus occur when a three-point seatbelt is used properly.
Maternal blood volume begins to expand at approximately week 10 of gestation and
peaks at 45 to 50% increase from baseline at week 28, resulting in a state of
hypervolemia. Red cell mass increases to a lesser extent, leading to the relative
physiologic anemia of pregnancy. Cardiac output is increased by 1.0 to 1.5 L/min at
week 10 of pregnancy and remains elevated until the end of pregnancy. Heart rate in
the mother is generally increased by 10 to 20 beats per minute in the second trimester,
accompanied by decreases in systolic and diastolic blood pressures of 10 to 15 mmHg.
The diaphragm is raised by as much as 4 cm and tidal volume increases by 40% as
residual volume diminishes by 25%.
The Kleihauer-Betke test of maternal blood has been used to detect fetal cells in the
maternal circulation. Unfortunately, the test is difficult to perform, not immediately
available in most emergency labs, and only sensitive enough to detect 5 ml of fetal
cells in the maternal circulation. Because only 0.1 ml of fetal cells is required to
sensitize the mother, routine immune globulin administration has been recommended
in situations likely to result in sensitization. In instances of significant blunt trauma to
the uterus, the Kleihauer-Betke test should be ordered to detect the rare large fetal
transfusions that may require specific fetal blood therapy or administration of
additional immune globulin to the mother. The standard dose of anti-D immune
globulin (RhoGAM 300 mcg) is sufficient to prevent maternal immunization for fetal
transfusions of up to 15 ml of red blood cells or 30 ml of whole blood.
Radiation exposure from various procedures:
X-ray lumbar spine: 204-1260 mrad
X-ray abdomen and pelvis: 190-357 mrad
X-ray cervical spine: <1 mrad
CT head (1 cm slices): <50 mrad
Estimated perimortem cesarean delivery survival rates:
22 weeks – 0 % survival
23 weeks – 15% survival
24 weeks – 56% survival
25 weeks – 79% survival
340
1125. More than 1.5 million traumatic brain injuries (TBI) occur annually in the US, with about 25%
hospitalization rate, and over 3% fatality rate. Which of the following statements concerning brain
injuries is true?
a. Ethanol-intoxicated individuals have at least a 50% greater chance of sustaining a head injury
than sober individuals.
b. The leading cause of traumatic brain injury death in the over-65 age group is motor vehicle
crashes.
c. The leading cause of TBI deaths in the 15 – 24 year old age group is motor vehicle crashes.
d. The group most commonly incurring TBI is young adult males.
e. The estimated costs for both acute and chronic TBI is upwards of $40 billion annually, in the
United States.
1126. The cerebral perfusion pressure (CPP) is a pressure gradient against which cerebral perfusion must
work, and is the result of the mean arterial pressure minus the intracranial pressure. Under normal
conditions, ICP is 0 to 10 mmHg. Patients with traumatic brain injury lose the ability to
autoregulate CPP. The true and pertinent statement is:
a. the MAP should be maintained at 120 mmHg or greater
b. the ICP should be kept at 28 mmHg or greater
c. hyperventilation should be used prophylactically to keep pCO2 below 28 mmHg.
d. if despite appropriate ICP and MAP determinations the patient continues to deteriorate, CSF
drainage by ventriculostomy is appropriate.
e. CPP should be maintained at 65 mmHg or lower.
1127. Which of the following is true regarding patients with severe traumatic brain injury?
a. The overall mortality is almost 25%.
b. Of the adults who survive severe head trauma, 30% will have moderate disability or good
outcome.
c. Field intubation has been shown to improve survival to the hospital.
d. Children have a poorer prognosis compared with adults.
e. Steroids administered within 6 hours of head injury improve outcome.:
1128. The most commonly seen brain herniation after traumatic brain injury is:
a. anti herniation of the parietal lobe through the tentorium
b. central transtentorial herniation involving frontal or occipital lobes
c. cerebellotonsillar herniation through the foramen magnum
d. uncal herniation of the temporal lobe through the tentorium
e. upward transtentorial herniation through the posterior fossa.
1129. Common findings in uncal herniation include:
a. bilateral pupillary dilatation.
b. compression of the oculomotor nerve, usually causing ipsilateral dilated and fixed pupil (may be
contralateral at times).
c. conjugate downward gaze and pinpoint pupils.
d. initial bilateral pinpoint pupils, followed by fixed midpoint pupils.
e. rotatory nystagmus.
341
1125. d
th
Rosen 5 ,
Chapter 34,
p. 286
1126. d
Rosen 5th,
Chapter 34,
p. 288
1127. e
Rosen 5th,
Chapter 34,
p. 294
1128. d
Rosen 5th,
Chapter 34
1129. b
Rosen 5th,
Chapter 34
The costs for treatment of both acute and chronic TBI have been estimated to be $4
billion dollars annually. The group most commonly incurring TBI is young adult
males. The elderly and young children are also at greater risk because of underlying
anatomic and physiologic factors. In addition, alcoholics are at an increased risk for
TBI; ethanol-intoxicated individuals have a 40% greater chance of sustaining a head
injury than sober individuals. The causal agent for TBI mortality varies greatly by age
and other demographic factors. For example, the leading cause of TBI-related deaths
in the 15- to 24-year-old age group is gunshot wounds, while for those over 65 years it
is falls.
CPP should be maintained at 70 mmHg or greater. To achieve this, two things must
occur: the MAP must be 90 mmHg or greater (which would mean a SBP of 120 to 140
mmHg) and the ICP no greater than 20 to 25 mmHg. Under these guidelines, any
patient with severe TBI must have a MAP >90 mmHg maintained. If this is achieved
and the patient exhibits progressive neurologic deterioration or evidence of herniation
not attributable to extracranial sources, then the ICP is most likely elevated and CPP
decreased. In this situation, CSF drainage by ventriculostomy is the best intervention,
followed by mannitol given as a bolus. Hyperventilation should not be used
prophylactically due to potentially serious side effects from decreased CBF. If it is
used prophylactically, then a PaCO2 of 30 to 35 mmHg should be maintained.
Up to 25% of patients with major head trauma patients will have lesions requiring
neurosurgical evacuation, and the overall mortality of severe head trauma is almost
40%. Mortality for children is lower. Adult survivors of severe head trauma are
usually severely disabled; currently, only 7% will have moderate disability or good
outcome. Children older than 1 year who survive a severe closed head injury have a
better outcome than adults. Field intubation in patients with severe head injury has
been shown to improve survival to the hospital. Despite their popularity in the past; no
evidence indicates that steroids are of benefit in head injury. They do not lower ICP or
improve outcome and are therefore no longer recommended.
There are four major brain herniation syndromes: uncal, central transtentorial,
cerebellotonsillar and upward posterior fossa. The most common site of herniation
occurs when the uncus of the temporal lobe is displaced inferiorly through the medial
edge of the tentorium. This is usually due to an expanding lesion in the temporal lobe
or lateral middle fossa. Uncal transtentorial herniation leads to compression of the
third (oculomotor) nerve, causing an ipsilateral fixed and dilated pupil. Further
herniation compresses the pyramidal tract leading to contralateral motor paralysis. In
up to 25% of patients the contralateral cerebral peduncle is forced against the opposite
edge of the tentorial hiatus. Hemiparesis is then detected ipsilateral to the dilated pupil
and the mass lesion. This is termed Kernohan's notch syndrome and causes falselocalizing motor findings.
342
1130. Mild traumatic brain injury traditionally includes patients with a Glasgow Coma Scale (GCS) of 13
or greater. Which statement is correct?
a. More than 75% of patients with traumatic brain injury and a GCS of 13 have abnormalities on CT
scan.
b. In patients with minor head trauma, those with clinical signs of a basilar skull fracture have a
30% increased incidence of intracranial lesions.
c. About 6-9% of patients with GCS of 15 and history of LOC will have an intracranial lesion.
d. Mild traumatic brain injury represents more than 95% of head injured patients seen in the ED.
e. At least 10% of patients with mild traumatic brain injury may “talk and deteriorate” within 48
hours of their injury.
1131. Moderate traumatic brain injury, defined as an initial GCS of 9 to 13, is associated with:
a. a mortality rate >25%.
b. a morbidity rate of >45%.
c. a positive CT scan in >50%.
d. a higher neurosurgical intervention rate than mild TBI.
e. an admission rate ten-fold higher than in mild traumatic brain injury.
1132. Severe traumatic brain injury, defined as an initial GCS < 9, is associated with:
a. a surprisingly low need for operative intervention.
b. a mortality approaching 40%, with death usually occurring within 48 hours
c. a relative lack of co-morbidities and other injuries.
d. an intracranial bleed rate of less than 20%.
e. less than 20% long-term disability.
1133. Which dose is considered correct when performing rapid sequence intubation:
a. fentanyl 6 – 12 mcg/kg.
b. lidocaine 5 mg/kg.
c. succinylcholine 2.5 mg/kg.
d. thiopental 3 mg/kg (if normotensive).
e. vecuronium or pancuronium 1 mg/kg.
1134. The agent implicated in development of truncal and jaw rigidity is:
a. fentanyl.
b. lidocaine.
c. succinylcholine.
d. thiopental.
e. vecuronium.
1135. An agent which can precipitate bronchospasm in a patient with reactive airway disease is:
a. midazolam.
b. etomidate.
c. ketamine.
d. propofol.
e. methohexital.
343
1130. c
th
Rosen 5 ,
Chapter 34,
p. 297-299
1131. b
Rosen 5th,
Chapter 34,
p. 297-299
1132. b
Rosen 5th,
Chapter 34,
p. 293
1133. d
Rosen 5th,
Chapter 1,
p. 15
1134. a
Rosen 5th,
Chapter 183,
p. 2580
1135. e
th
Rosen 5 ,
Chapter 183,
p. 2581
Most authors now include patients with a GCS of 13 in the moderate traumatic brain
injury (TBI) group rather than the mild group. Mild TBI accounts for 75 to 80% of all
patients with head injuries seen in the emergency department. About 3% of patients
with mild traumatic brain injury may talk and deteriorate; unexpectedly. Less than 1%
will have surgically significant lesions. Patients with clinical signs of basilar skull
fracture have a 50-90% increased incidence of intracranial lesions associated with their
minor head trauma. About 6-9% of patients with GCS of 15 and history of LOC will
have an intracranial lesion. Thus, these patients should be considered high-risk minor
head trauma patients.
Moderate TBI accounts for approximately 10% of patients with head injuries.
Mortality rates for patients with isolated moderate TBI is less than 20%, but long-term
disability is as high as 50%. Overall, 40% of moderate TBI patients have a positive
CT scan and 8% require neurosurgical intervention, the same percentage as in mild
TBI. Approximately 10% of all moderate TBI patients will deteriorate due to
secondary brain injury and progress to severe TBI. Most patients with moderate TBI
should be admitted because of the potential for deterioration. Those with an initial
GCS of 13 who return to normal, who remain intact after a 6-12 hour observation
period, and who have a normal CT, can be discharged to family.
Severe TBI accounts for approximately 10% of all emergency department patients with
TBI. The mortality of severe TBI approaches 40% with deaths usually occurring
within 48 hours. Long-term disability is common, with only about 10% making even a
moderate recovery. There are frequently associated injuries, metabolic problems, and
co-morbid factors. More than 80% have CT evidence of bleeding, (1% epidural, 30%
subdural, 30 – 40% traumatic subarachnoid hemorrhage, 20 – 30% contusion), and
emergent neurosurgical intervention can be life saving in epidural, subdural, and
subarachnoid hemorrhage.
succinylcholine 1 - 1.5 mg/kg
lidocaine 1.5 mg/kg
fentanyl 3 – 5 micrograms/kg
vecuronium or pancuronium 0.01 mg/kg
Truncal and jaw muscle rigidity are rare side effects of fentanyl that can lead to
impaired ventilation. This rigidity most often occurs at high doses >10-15 µg/kg) and
may be reversed by parenteral naloxone. If naloxone is unsuccessful, paralysis and
endotracheal intubation may be necessary.
Methohexital is an ultra-short-acting barbiturate that provides sedation and amnesia for
short, invasive procedures. Barbiturate administration may precipitate bronchospasm
in patients with moderate to severe reactive airway disease, thus limiting its use in
those patients. There is some evidence that ketamine may have a mild, transient
bronchodilatory effect.
344
1136. A 32-year-old man stepped on a large piece of broken glass while walking barefoot. He has a 10
cm cut on the medial plantar right foot. Prior to repair, you would want to do a peripheral block of
the:
a. deep peroneal nerve.
b. posterior tibial nerve.
c. saphenous nerve.
d. superficial peroneal nerve.
e. sural nerve.
1137. A 17-year-old softball player takes a bad bounce in her face and has a complex stellate cut on her
lower lip that crosses the vermilion border. Anesthesia is best achieved by performing:
a. inferior alveolar nerve block.
b. infraorbital nerve block.
c. local infiltration with 1% lidocaine with epinephrine.
d. local infiltration with 1% lidocaine without epinephrine.
e. mental nerve block.
1138. You are giving medical command to a prehospital team, which is at the scene of a bus turnover.
The driver has an obvious femur fracture and the paramedics wish to apply a femoral traction splint
(Hare traction). A contraindication to the use of this device is:
a. open femur fracture.
b. angulated femur fracture.
c. prior hip surgery.
d. severe head trauma.
e. shock.
1139. You have just delivered a premature infant who weighs 1150 grams. You do not have inpatient
neonatal capabilities at your hospital, so arrange for transfer to a specialty care center. The
appropriate intravenous fluid to use is:
a. lactated Ringers.
b. 5% dextrose in water.
c. 10% dextrose in water.
d. 0.9% saline.
e. 0.45% saline.
1140. The cornerstone of aviation physiology is:
a. Dalton’s law.
b. Henry’s law.
c. Cole’s law.
d. Boyle’s law.
e. Ellay law.
1141. Which of the following is true regarding injury to the kidney?:
a. Renal pedicle injuries typically have a salvage rate of 30-40%.
b. Major renal lacerations represent 25% of all renal injuries.
c. Minor renal lacerations are the most common injuries to the kidney.
d. Patients will typically have more life threatening blood loss from renal vein injury than renal
artery injury.
e. Even in the absence of extension to the renal medulla or collecting system and no evidence of
urine extravasation, most renal lacerations require operative repair
345
1136. b
th
Rosen 5 ,
Chapter 51,
p. 719
1137. e
Rosen 5th,
Chapter 35,
p. 316
1138. a
Rosen 5th,
Chapter 49,
p. 487, 654
1139. c
Rosen 5th,
Chapter 9, p.
1140. b
Rosen 5th,
Chapter 187,
p. 2625
1141. d
Rosen 5th,
Chapter 40,
p. 450
The posterior tibial nerve innervates the sole of the foot. To perform a peroneal nerve
block, inject 1% lidocaine into the subcutaneous tissue lateral to the posterior tibial
artery at the upper border of the medial malleolus. None of the other nerves listed
supply the plantar surface of the foot. The saphenous nerve provides sensation to the
skin over the medial malleolus. The sural nerve supplies the lateral foot and fifth toe.
The superficial peroneal nerve innervates the dorsum of the foot and the other toes,
except the adjacent sides of the first and second toes, which derive sensation from the
deep peroneal nerve.
A regional block is preferred for a complex lower lip laceration because it preserves
tissue planes and landmarks, facilitating anatomically correct repair. The mental nerve
supplies the skin and mucus membranes of the lower lip. The mental foramen is
located inside the lower lip at its junction with the lower gum, just posterior to the first
premolar tooth. To avoid nerve injury, 1% lidocaine with epinephrine is injected close
to, but not into, the mental foramen. The inferior alveolar and lingular nerves do not
supply the lower lip and thus would not be effective in this patient.
The femoral traction splint is the preferred device for immobilization of femur
fractures. Traction is applied by using a hitch on the ankle that encounters resistance
when the splint impinges proximally on the pelvis. Contraindications to using this
device include open fracture with exposed bone or suggestion of neurologic
involvement.
Because of the risk of hypoglycemia, all neonates should receive glucose-containing
fluids in preparation for and during transport. D10% should be used in infants with a
birth weight greater than 1000 g. D5% is safer in smaller infants because of the risk of
hyperglycemia with the more concentrated solution.
The cornerstone of aviation physiology is Boyle’s law, which states that the volume of
a unit of gas (a specific number of molecules) is inversely proportional to the pressure
on it. In concrete terms, Boyle’s law means that as altitude increases (and atmospheric
pressure decreases), air volume expands. With descent (increasing atmospheric
pressure), air volume contracts.
Renal vein injuries are more common than renal artery avulsions or intimal tears. Both
injuries are often associated with rapid deceleration events. As expected, a venous
injury can potentially contribute more to a patient's unstable hemodynamic status than
an arterial injury. The protective secondary vasospasm following arterial disruption
does not occur with venous injuries. Pedicle injuries rarely occur alone. Most often
they are associated with other life-threatening, non-urologic injuries that require
immediate surgical intervention. The salvage rate at best for a life-sustaining
functioning kidney approaches only 15% to 20%. An IV contrast-enhanced helical CT
scan will identify most renal artery disruptions, whereas renal vein injuries must be
indirectly diagnosed by the presence of a normal-appearing kidney in association with
a large hematoma disproportionate to the rest of the radiographic study. Major renal
lacerations represent approximately 2% to 4% of all renal injuries, and by definition
are associated with renal fractures extending deep into the renal medulla and collecting
system. They also are readily diagnosed by an IV contrast-enhanced helical CT scan.
This injury is in sharp contrast to minor renal lacerations (8% to 15%) and renal
contusions (85% to 92%) that do not extend into the renal medulla or collecting
system, are not associated with extravasation of urine, and heal spontaneously. These
latter two injuries can be managed expectantly and rarely, if ever, require initial or
subsequent operative intervention.
346
1142. The anterior humeral line is most helpful in detecting:
a. elbow dislocation.
b. olecranon fracture.
c. radial head fracture.
d. radioulnar dislocation.
e. supracondylar fracture.
1143. Radial head subluxation:
a. has a long recovery period.
b. has a typical presentation of the arm held in flexion and pronation.
c. is common among high-school athletes.
d. is diagnosed radiographically by a posterior fat pad sign.
e. is usually caused by fall on an outstretched hand.
1144. A 34-year-old woman complains of shortness of breath after a moderate-speed motor vehicle crash
in which she was a restrained front seat passenger. Her upright anteroposterior chest x-ray is
normal, but you detect a 2-mm pneumothorax on chest CT. You would place a thoracostomy tube
if she:
a. developed symptoms of cardiac contusion.
b. developed symptoms of pulmonary contusion.
c. had a paO2 <80 mmHg.
d. had one or more rib fractures.
e. required intubation and mechanical ventilation.
1145. Concerning trauma to the pancreas:
a. complications are infrequent and of little consequence.
b. concomitant injuries are rare.
c. diagnostic peritoneal lavage (DPL) is highly sensitive.
d. penetrating injuries are more common than blunt injuries.
e. serum amylase is almost always elevated.
1146. Which of the following is true of clinicians regarding forensics:
a. Clinicians should describe gunshot wounds as entrance or exit wounds.
b. The ED physician should make an educated speculation regarding the caliber of the bullet.
c. Wounds should be described according to standard anatomic position with the arms to the side
and palms up.
d. The term 'powder burn' should be used to describe the carbonaceous material associated with
close-range wounds. .
e. The physician must record the manner of a gunshot wound victim's death in the medical
record as homicide, suicide, or accidental.
347
1142. e
th
Rosen 5 ,
Chapter 169,
p. 559
1143. b
Rosen 5th,
Chapter 169,
p. 573
1144. e
th
Rosen 5 ,
Chapter 72,
p. 1004
1145. d
Rosen 5th,
Chapter 39,
p. 420
1146. c
Rosen 5th,
Chapter 59,
p. 828-829
The anterior humeral line is helpful in diagnosing supracondylar fractures.
Hyperextension forces that occur with a fall onto the arm typically displace the distal
fracture fragment posteriorly. The anterior humeral line is drawn down the anterior
aspect of the humerus on the lateral elbow film. Normally this line will transect the
middle of the capitellum. With a supracondylar fracture, the line usually passes
anterior to the capitellum or through the anterior third.
Radial head subluxation (AKA nursemaid's elbow) is often caused by traction on a
young child's arm, usually under the age of 4 years. The most common position to
find the child in is in flexion and pronation. It is not associated with abnormal x-rays.
The child will often start using the extremity within minutes of reduction.
Treatment of a simple pneumothorax depends on its cause and size. Most advocate
treating a traumatic pneumothorax with a chest tube to correct any respiratory
compromise and because treatment with a chest tube is generally thought to be safer
than observation in these patients. Small pneumothoraces, whether spontaneous or
traumatic, have been treated with hospitalization and careful observation if the patient
is otherwise healthy, symptom free, does not need anesthesia or positive pressure
ventilation, and the size of the pneumothorax is not increasing.
Pancreatic injury is more common with penetrating trauma. It may also occur as a
result of a crushing injury that divides the pancreas over the vertebral column. It may
also occur as a result of a crushing injury that divides the pancreas over the vertebral
column. Examples include steering wheel or bicycle-handlebar injuries.
Unrecognized, this injury has considerable morbidity and mortality. DPL is usually
negative, and the serum amylase is usually normal. Neither serum amylase nor lipase
is useful when obtained routinely. Normal levels do not exclude a major pancreatic
injury, and elevated values may be caused by any of an assortment of reasons in
addition to an injured pancreas. The use of serum amylase isoenzymes has not
appreciably improved accuracy. Non-traumatic causes of hyperamylasemia include
several diseases and the use of alcohol, narcotics, and various other drugs. Amylase or
lipase may also be elevated with pancreatic ischemia produced by the systemic
hypotension that often accompanies trauma. Clearly these enzymes are neither highly
specific nor sensitive for pancreatic injuries. Elevated lavage amylase levels are less
specific and sensitive for pancreatic trauma. Rising levels in serial lavages and clinical
correlation may provide more suggestive evidence of a pancreatic injury.
Documentation of gunshot wounds should include the location, size, shape, and
characteristics of the wound. Clinicians should not describe wounds as entrance or
exit, but should document a detailed description of the appearance and location of a
wound without speculating on an interpretation or the caliber of the bullet. Exit
wounds are not always larger than the entrance wound. The term soot rather than
powder burns, should be used to describe the carbonaceous material associated with
close-range wounds. Powder burns are literally the burns associated with the
coincidental ignition of clothing by the flaming black powder used in muzzleloaders,
antique weapons, and blank cartridges. This does not occur with the smokeless
powder used in modern commercial ammunition. Powder burns, therefore, is an
obsolete and potentially misleading expression. It is unnecessary to write in the
medical record, the manner of a gunshot victim's death. The determination of whether
a death is accidental, suicidal, or homicidal is the responsibility of the coroner or
medical examiner and only after a detailed investigation of the scene and
circumstances of the incident.
348
1147. The amount of blood contained in an acute pericardial tamponade after penetrating cardiac injury is
approximately:
a. 10 mL.
b. 50 mL.
c. 200 mL.
d. 500 mL.
e. 1000 mL.
1148. Hamman's sign suggests:
a. pericarditis.
b. pneumomediastinum.
c. pneumothorax.
d. pulmonary embolism.
e. status asthmaticus.
1149. Regarding blunt tracheobronchial injuries:
a. Blunt cervical tracheal injuries usually occur proximal to the tracheal cartilage.
b. Common signs and symptoms include dyspnea, hemoptysis, subcutaneous emphysema,
Hamman's sign, and sternal tenderness.
c. Concurrent esophageal injuries occur in fewer than 5% of cases.
d. Injuries to the major bronchi are usually caused by elevated intraabdominal pressure.
e. Most lower tracheobronchial injuries occur 5 cm or more from the carina.
1150. The most commonly injured structure in the genitourinary (GU) tract is the:
a. bladder.
b. kidney.
c. penis.
d. ureter.
e. urethra.
349
1147. c
th
Rosen 5 ,
Chapter 38,
p. 398-401
1148. b
Rosen 5th,
Chapter 38,
p. 408, 1137,
1237
1149. b
th
Rosen 5 ,
Chapter 38,
p. 375
1150. b
Rosen 5th,
Chapter 40,
p. 449
In a previously normal pericardium, 200 mL of blood will create sufficient
intrapericardial pressure to restrict venous filling of the heart and cause tamponade.
Although it may be detected by bedside ultrasound, this amount is too small to be
reliably visible on chest x-ray. Removal of as little as 5 to 10 mL of blood can be life
saving by augmenting venous filling and dramatically improving stroke volume.
With pneumomediastinum, a crunching sound known as Hamman's sign can be heard
during systole secondary to mediastinal air surrounding the heart. The diagnosis of
pneumomediastinum is most easily confirmed on CT but can sometimes be made with
plain films. Subcutaneous emphysema in the neck is another suggestive physical
finding.
Cervical tracheal injuries occur most frequently at the junction of the cricoid cartilage
and the trachea, usually after striking the anterior neck against the dash of a car. Most
lower tracheobronchial injuries occur within 2 cm of the carina. Lower
tracheobronchial injuries are caused by rapid deceleration and shearing of mobile
bronchi from fixed structures. Concurrent esophageal injuries occur in 25% of
patients.
In one case series, 67% of all GU injuries were to the kidney. The bladder is the
second most commonly injured structure. Kidney injuries include contusions,
lacerations, ruptures, pedicle injuries, and renal pelvis ruptures.
350
Pharmacology
1151. A 32 year old male with an unknown past medical history is brought to the ED after successful
prehospital resuscitation. He is intubated and normotensive but remains poorly perfused. The most
appropriate pressor agent to use in this situation is:
a. epinephrine at 0.05 to 1.0 mcg/kg/min.
b. dobutamine at 5 to 20 mcg/kg/min.
c. dopamine at 5 to 10 mcg/kg/min.
d. dopamine at 2 to 5 mcg/kg/min.
e. norepinephrine at 4 mcg/kg/min.
1152. While using ketamine for adult patients requiring PSAA (Procedural Sedation and Analgesia) in the
Emergency Department, you can minimize the “emergence phenomena” of hallucinations and
nightmares by also treating with:
a. midazolam.
b. morphine sulfate.
c. fentanyl.
d. intravenous ketorolac
e. nitrous oxide.
1153. Probably the best indication for antibody (Fab) treatment in a patient with digitalis toxicity is:
a. tachydysrhythmias.
b. severe bradycardia.
c. advance AV block.
d. intractable nausea and vomiting.
e. hyperkalemia.
1154. A 27 year old female was found unconscious by her mother, who does not know how long she may
have been this way. The paramedics recovered a suicide note and an empty bottle of the mother’s
high blood pressure medications. The patient is profoundly hypotensive with a heart rate of 27.
The medication which she most likely ingested is:
a. hydrochlorothiazide.
b. enalapril.
c. irbesartan.
d. metoprolol.
e. verapamil.
1155. You are treating a 37 year-old woman who has an oral infection. She tells you that she has a
history of myasthenia gravis. You can safely use:
a. tetracycline
b. clindamycin.
c. doxycycline.
d. amoxicillin/clavulanate.
e. a topical preparation containing polymyxin.
351
1051. a
th
Rosen 5 ,
Chapter 8,
p. 98
1052. a
th
Rosen 5 ,
Chapter 183,
p. 2582
1053. e
Rosen 5th,
Chapter 146,
p. 2106
1054. e
Rosen 5th,
Chapter 146,
p. 2111
1055. d
Rosen 5th,
Chapter 102,
p. 1523, Box
102-2
Dobutamine may be an effective agent in the normotensive post-arrest patient who
remains poorly perfused. Dobutamine tends to decrease systemic vascular resistance
(SVR), which is not helpful in the hypotensive patient.
Emergence phenomena manifested by hallucinations and nightmares occur in up to
50% of adults and up to 10% of children receiving ketamine. A study of adult ED
patients requiring PSAA to facilitate a painful procedure demonstrated that a
combination of midazolam and ketamine produces safe and effective sedation and
analgesia with a low incidence of minor emergence phenomena.
The chief disadvantage of Fab fragment treatment is expense. Because the average
charge to the patient per vial is about $600, it is recommended for life-threatening
toxicity rather than for routine or prophylactic treatment but certainly before pacing,
which carries significant risk. Probably the best indication for antibody treatment in
acute poisoning I hyperkalemia.
Calcium channel antagonists block the slow calcium channels in the myocardium and
vascular smooth muscle, leading to coronary and peripheral vasodilation. They also
reduce cardiac contractility, depress SA nodal activity, and slow AV conduction. In
overdose, verapamil has the deadliest profile, combining both severe myocardial
depression with peripheral vasodilation.
Drugs that may exacerbate myasthenia gravis:
Cardiovascular: beta-blockers, calcium channel blockers, quinidine, lidocaine,
procainamide
Antibiotics: aminoglycosides, tetracyclines, clindamycin, lincomycin, polymyxin B,
colistin
Other: phenytoin, neuromuscular blockers, thyroid replacement
352
1156. Prophylaxis is required for patients with cat bites, as they tend to be deep puncture wounds that are
difficult to irrigate adequately. The antibiotic of choice is:
a. cephalexin.
b. amoxicillin with clavulanate.
c. dicloxacillin.
d. clindamycin.
e. erythromycin.
1157. A 67 year old woman with a long-standing history of asthma presents in severe respiratory distress.
She is anxious, hyperactive and diaphoretic. She also has a history of hypertension and her BP is
210/140 mm Hg. Her heart beat is 190 / minute. It is apparent she will require rapid sequence
intubation soon, so you begin gathering the appropriate medications, including:
a. lidocaine 1.5 mg/kg IV.
b. rapacuronium 1.5 mg/kg IV.
c. etomidate 0.3 mg/kg IV.
d. rocuronium 1.0 mg/kg IV.
e. fentanyl 3 mcg/kg IV.
1158. A 69 year old female complains of fever; crampy abdominal pain; and explosive severe watery /
bloody diarrhea. She recently took clindamycin for an intraoral infection. She is sick enough to
require admission to the hospital, and your first drug of choice to treat he should be:
a. Lomotil® 1 tablet after each loose bowel movement.
b. metronidazole 250 mg po daily for 7 days
c. metronidazole 500 mg IV tid for 10 to 14 days.
d. vancomycin 125 mg po qid for 10 to 14 days
e. vancomycin 250 mg IV bid for 7 to 10 days
1159. A 62 year old male with history of Zollinger-Ellison syndrome presents with severe epigastric pain,
vomiting with “coffee-ground” emesis. He has been doing relatively well on H2 blockers. The
appropriate dosage of proton pump inhibitor to treat this condition is:
a. omeprazole 60 mg/day.
b. rabeprazole 20 mg/day.
c. lansoprazole 15 mg/day.
d. pantoprazole 40 mg/day.
e. omeprazole 20 mg/day.
1160. A 27 year old female complains of a bright red rash on both of her cheeks; she also says her joints
are sore. When you examine the list of medications she is presently taking, you see that these
symptoms could be explained by her use of:
a. depo shots.
b. fluoxetine.
c. isoniazid.
d. albuterol.
e. naproxen.
1161. A commonly used, effective yet inexpensive topical ophthalmic anesthetic is:
a. tetracaine (Pontocaine).
b. adrenaline.
c. lidocaine.
d. bupivicaine.
e. benzocaine.
353
1056. b
th
Rosen 5 ,
Chapter 52,
p. 748
1057. e
Rosen 5th,
Chapter 1,
p. 14
1058. c
Rosen 5th,
Chapter 89,
p.
1059. a
Rosen 5th,
Table 84-2,
p. 1248
1060. c
Rosen 5th,
Table 112-1,
p. 1611
1061. a
Rosen 5th,
Chapter 182,
p. 2574
The organisms found in cat bites include Staphylococcus species, and most often,
Pasteurella multocida. P. multocida is usually found in cat bite wounds and is present
in the normal oral flora of up to 70% of all cats. P. multocida is still sensitive to
penicillin, but the infection is often polymicrobial. In addition, P. multocida is
resistant to dicloxacillin, cephalexin, and clindamycin, with many erythromycinresistant strains. Amoxicillin with clavulanate is the current recommendation for
antibiotic prophylaxis for cat bites.
In patients at risk from acute blood pressure elevation, administration of fentanyl 3
mcg/kg, during the pretreatment phase of RSI attenuates the HR and BP rise. The full
sympatholytic dose of fentanyl; is 5 or 6 mcg/kg, but if this dosage is administered as a
single pretreatment bolus, hypoventilation or apnea can occur. The administration of 3
mcg/kg is safer and can be supplemented with an additional 3 mcg/kg immediately
after the succinylcholine if full sympathetic blockade is desired or if hypertension and
tachycardia ensue.
Vancomycin is generally not effective if given intravenously because it does not reach
effective intraluminal concentrations. Because vancomycin is much more expensive
than metronidazole and both seem to be equally effective, oral vancomycin is reserved
for patients who do not respond to metronidazole therapy or for those who are
extremely ill at the time of presentation.
Proton pump inhibitors are indicated for the short-term treatment of active duodenal
ulcer and severe erosive esophagitis and in the treatment of symptomatic GERD that
has not responded to therapy with H2 blockers. They are used in significantly higher
dosages in patients with Zollinger-Ellison syndrome. Omeprazole 60 mg/day and
lansoprazole 60 mg/day are the two currently recommended therapies.
Numerous medications can cause a lupus-like syndrome.
High risk: procainamide, quinidine, hydralazine, methyldopa, reserpine, Dpenicillamine
Moderate risk: isoniazid, penicillin, sulfonamides, streptomycin, tetracycline,
nitrofurantoin, phenytoin, ethosuximide, and primidone
Low risk: propylthiouracil, chlorpromazine, lithium carbonate
Tetracaine is a potent ester used for surface anesthesia of the cornea and is a
component of TAC solution.
354
1162. A 62 year old female with a longstanding history of rheumatoid arthritis takes several nonopioid
analgesics; she was recently diagnosed with essential hypertension. The most appropriate antihypertensive medication for her is probably:
a. hydralazine.
b. atenolol.
c. nifedipine.
d. clonidine.
e. hydrochlorothiazide.
1163. The generally acknowledged opioid of choice for Procedural Sedation and Analgesia (PSAA) in the
Emergency Department is:
a. meperidine.
b. morphine.
c. fentanyl.
d. hydromorphone.
e. ketorolac.
1164. A 66 year old female presents to the ED with new onset of symptoms highly suggestive for
uncomplicated gastritis. She is has been taking NSAIDs for a number of years. Your initial
therapy should begin with:
a. an H2 antagonists.
b. a proton pump inhibitor.
c. bismuth subsalicylate.
d. misoprostol.
e. an aluminum-containing antacid
1165. The antidysrhythmic which has characteristics of all four Vaughan-Williams classes is:
a. lidocaine.
b. procainamide.
c. quinidine.
d. amiodarone.
e. bretylium.
1166. Hypoxia and ischemia can lead to interstitial accumulation of adenosine in the myocardium. A
competitive antagonist of adenosine is:
a. atropine.
b. magnesium sulfate.
c. aminophylline.
d. bretylium.
e. epinephrine.
1167. Calcium chloride 4 mg/kg (0.04 ml/kg of 10% solution) may be beneficial in attempting to
resuscitate a patient known to have
a. hyperkalemia
b. hypernatremia.
c. hypophosphatemia.
d. hypermagnesemia.
e. cyanide toxicity.
355
1162. c
th
Rosen 5 ,
Chapter 182,
p. 2569
1163. c
th
Rosen 5 ,
Chapter 183,
p. 2563
1164. a
Rosen 5th,
Chapter 84,
p. 1241
1165. d
th
Rosen 5 ,
Chapter 7,
p. 79
1166. c
th
Rosen 5 ,
Chapter 7,
p. 79-80
1167. d
Rosen 5th,
Chapter 7,
p. 80
Nonopiod analgesic agents may interfere with the antihypertensive actions of
numerous drugs, and calcium channel blockers may be the antihypertensive agents of
choice when used with a NNA.
When given IV, fentanyl rapidly crosses the blood-brain barrier, producing analgesia in
as little as 90 seconds. Serum fentanyl levels rapidly decline from peak concentrations
because of extensive tissue uptake, producing a serum half-life of 90 minutes and
duration of action of 30 to 40 minutes. The combination of potency and short half-life
permits the administration of multiple small doses that can be titrated easily to the
desired clinical effect. It is an ideal agent for brief procedures such as incision and
drainage of abscesses or reduction of joint dislocations.
Treatment of presumptive gastritis can be started in the ED. H2 antagonists have been
shown to improve symptoms of dyspepsia in patients taking NSAIDs. Dosages should
begin at the low end and be tapered up as necessary. Patients with persistent
symptoms should be referred to a gastroenterologist for further diagnostic evaluation.
Amiodarone is considered a class III antidysrhythmic agent but has characteristics of
all four Vaughan-Williams classes.
Hypoxia and ischemia lead to the interstitial accumulation of adenosine in the
myocardium. Adenosine is known to depress automaticity of the sinus node. AV
junction. His bundle, and Purkinje fibers, as well as conduction through the AV node.
Aminophylline is a competitive antagonist of adenosine. Aminophylline (250 mg IV)
given to patients who failed ACLS with more than 2 mg of epinephrine and 2 mg of
atropine resulted in ROSC in 11 of 15 patients.
Calcium administration is likely to be beneficial in cases of hyperkalemia,
hypocalcemia, or calcium channel blocker toxicity. If required, 4 mg/kg of calcium
chloride (0.04 ml/kg of 10% solution may be administered every 10 minutes.
356
1168. Although SaO2 is maintained for up to ___ in untreated ventricular fibrillation, this rapidly falls to
hypoxic range within two minutes of chest compressions without ventilation.
a. 5 minutes
b. 10 minutes
c. 15 minutes
d. 30 minutes
e. 45 minutes
1169. The single most useful drug currently available for the treatment of cardiac arrest is:
a. epinephrine.
b. amiodarone.
c. lidocaine.
d. atropine.
e. calcium.
1170. A 68 year old female with a history of end-stage renal disease requires rapid sequence intubation.
You wish to use a neuromuscular blocking agent which is not excreted by the kidneys, so choose:
a. atracurium.
b. d-tubocurarine.
c. vecuronium.
d. pancuronium.
e. cisatracurium.
1171. A 35 year old woman presented to the Emergency Department in status asthmaticus and required
rapid sequence intubation. She is now starting to waken; she is restless and “bucking” the
ventilator. An appropriate drug, dose, and route to use is:
a. diazepam 0.2 mg/kg IV.
b. lorazepam 1 mg/kg IV.
c. phenobarbital 120 mg IM.
d. ketamine 1 to 2 mg/kg IM.
e. etomidate 0.3 mg/kg IV.
1172. The preferred induction agent for use in a patient with status asthmaticus or a head-injured patient
with normal blood pressure is:
a. diazepam 0.2 mg/kg IV.
b. lorazepam 1 mg/kg IV.
c. phenobarbital 120 mg IM.
d. ketamine 1 to 2 mg/kg IM.
e. etomidate 0.3 mg/kg IV.
1173. A 57 year old woman presents to the ED in apparent septic shock. She has no history of renal
insufficiency, but her urine output remains low despite a 20 ml/kg of normal saline solution and a
dopamine intravenous drip at 15 mcg/kg/min. Your next step should be to:
a. increase the dopamine to 20 mcg/kg/min.
b. start dobutamine at 5 mcg/kg/min; increase as needed to 20 mcg/kg/min to maintain urine output.
c. start norepinephrine at 0.1 mg/kg/min.
d. start milrinone at 5 to 10 mcg/kg/min.
e. start amrinone at 0.5 mcg/kg/min.
357
1168. d
th
Rosen 5 ,
Chapter 7,
p. 80
1169. a
th
Rosen 5 ,
Chapter 7,
p. 78
1170. a
th
Rosen 5 ,
Chapter 1,
p. 12
1171. a
th
Rosen 5 ,
Chapter 1,
p. 13
1172. d
Rosen 5th,
Chapter 1,
p. 13
1173. b
th
Rosen 5 ,
Chapter 4.
p. 43
Although SaO2 is maintained for up to 30 minutes in untreated ventricular fibrillation,
this rapidly falls to hypoxic range within two minutes of chest compressions without
ventilation.
Epinephrine is the single most useful drug currently available for the treatment of
cardiac arrest. The most important mechanism of action of epinephrine during CPR is
to increase peripheral vascular resistance through direct alpha-adrenergic activity on
arteriolar smooth muscle.
Atracurium is the competitive neuromuscular blocking agent for use in patients with
renal failure because its excretion is completely independent of renal function.
After intubation, longer paralysis is usually desired for patient control and to permit
mechanical ventilation. In most cases, one agent is comparable to another, and cost
may be a consideration. Longer term neuromuscular blockade must not be undertaken
without attention to appropriate sedation of the patient. An adequate dose of a
benzodiazepine, such as diazepam 0.2 mg/kg IV, is often the best initial choice for
sedation accompanying use of longer-acting neuromuscular blocking agents,
The principle use of ketamine in emergency airway management is for the induction of
patients with asthma and hemodynamically unstable trauma patients without head
injury.
Septic shock refractory to volume restoration requires vasopressor support. Dopamine
is a rational first-line therapy at 5 to 15 mcg/kg/min and titrated to urine output greater
than 1 ml/kg/hr. If urine output remains low with high doses of dopamine, dobutamine
should be started at 5 mcg/kg/min to increase cardiac output and increased to 20
mcg/kg/min to maintain urine output.
358
1174. A 57 year old man presents to the ED in cardiogenic shock with an extensive acute anterior wall
myocardial infarction. Despite maximal doses of dobutamine and dopamine with incremental fluid
challenges, he remains hypotensive. Your next step should be to add:
a. epinephrine at 0.1 mg/kg/hr IV.
b. amiodarone at 25 mg/kg/hr IV after a 300 mg bolus.
c. norepinephrine at 0.1 mg/kg/min.
d. milrinone at 5 to 10 mcg/kg/min after an IV bolus of 0.75 mg/kg.
e. amrinone at 5 to 10 mcg/kg/min after an IV bolus of 0.75 mg/kg.
1175. A 71 year-old gardener presents in apparent anaphylactic shock after being stung by several yellow
jackets. He has a Medic Alert bracelet which states “Allergy to Bees; Heart Condition.” Your
initial therapy should include:
a. dobutamine 5 mcg/kg/min IV.
b. ketamine 0.1 mg/kg IV.
c. epinephrine 1 ml of 1:10,000 (100 mcg) slow IV.
d. diphenhydramine 5 mg/kg IV.
e. hydrocortisone 30 mg/kg IV.
1176. A 3 week old female presents lethargic, somnolent, ashen and with a very poor suck. You suspect
acute bacterial meningitis and begin empiric therapy with:
a. ampicillin 100 mg/kg IV plus cefotaxime 50 mg/kg IV or ceftriaxone 100 mg/kg IV.
b. ampicillin 100 mg/kg IV plus cefotaxime 50 mg/kg IV or gentamicin 2.5 mg/kg IV.
c. cefotaxime 50 mg/kg IV or ceftriaxone 100 mg/kg IV and vancomycin 15 mg/kg IV.
d. nafcillin 25 mg/kg IV.
e. ticarcillin 50 mg/kg IV.
1177. Of the benzodiazepines, the one best suited as an induction agent is.
a. alprazolam.
b. diazepam.
c. lorazepam.
d. midazolam.
e. triazolam.
1178. Naloxone is a pure opioid antagonist. It is the most commonly used agent for reversal of opioidinduced sedation and respiratory depression. The dose for complete reversal is:
a. 0.1 to 2 mg IV.
b. 0.8 mg IV.
c. at least 2 mg.
d. 0.16 mg.
e. 0.01 mg/kg.
1179. The sedative-hypnotic which must be given in a continuous intravenous infusion is:
a. propofol.
b. ketamine.
c. midazolam.
d. alprazolam.
e. phenobarbital.
359
1174. e
th
Rosen 5 ,
Chapter 4,
p. 45
1175. c
Rosen 5th,
Chapter 4,
p. 45
1176. b
Rosen 5th,
Table 168-3,
p. 2350
1177. d
Rosen 5th,
Chapter 1,
p. 13
1178. c
th
Rosen 5 ,
Chapter 183,
p. 2583
1179. a
th
Rosen 5 ,
Chapter 183,
p. 2582
To improve myocardial contractility, dobutamine and dopamine are agents of choice in
cardiogenic shock. For refractory hypotension and shock, amrinone or milrinone may
improve cardiac output. These drugs exhibit little tachyphylaxis with no measurable
increase in myocardial oxygen consumption. A loading dose of 0.75 mg/kg for
amrinone or 50 mcg/kg for milrinone is necessary, followed by a titrated constant
infusion for either drug (5 to 10 mcg/kg/min for amrinone and 0.5 mcg/kg/min for
milrinone).
In the treatment of anaphylactic shock, epinephrine should be administered
intravenously in patients with hypotension, even in the presence of coronary artery
disease. Initially 1 ml of 1:10,000 epinephrine (100 mcg) can be injected slowly and
the response monitored. Afterward 5 mg of epinephrine can be diluted in 500 ml of
saline, with a starting infusion rate of 10 ml/hr (about 0.02 mcg/kg/min) and titrated to
maintain perfusion.
Empiric antibiotics for acute bacterial meningitis
0 – 4 weeks: ampicillin 50-100 mg/kg IV plus gentamicin 2.5 mg/kg or cefotaxime 50
mg/kg IV
4 weeks – 3 months: ampicillin 50-100 mg/kg IV plus cefotaxime 50 mg/kg IV or
ceftriaxone 100 mg/kg IV or chloramphenicol 25 mg/kg IV
>3 months: cefotaxime 50 mg/kg IV or ceftriaxone 100 mg/kg IV and vancomycin 15
mg/kg IV.
Of the benzodiazepines, only midazolam is well suited to use as an induction agent,
with a recommended dose of 0.1 to 0.3 mg/kg IV. In a dose of 0.2 mg/kg IV,
midazolam produces loss of consciousness in about 30 seconds and has a clinical
duration of 15 to 20 minutes.
The dose of naloxone for adults is 0.1 to 2 mg IV; for complete reversal, at least 2 mg
should be given. If the procedure has not been completed, but the patient becomes
overly sedated or experiences respiratory depression, partial reversal may be achieved
by using incremental doses of 0.1 to 0.4 mg.
Propofol is an ultra-short-acting sedative hypnotic that produces dose-dependent levels
of sedation ranging from light sedation to general anesthesia. Its short duration of
action makes titration simple, but also requires the drug to be given via continuous
intravenous infusion. Sedation is usually achieved by administering a constant infusion
of 25 to 125 mcg/kg/min.
360
1180. An 8 year old male complains of severe pain and gross deformity of his elbow after falling from the
“monkey bars” at a local playground. He denies any other injury. His x-ray shows posterior elbow
dislocation. Your orthopedic surgeon will be occupied in the operating room for the next few
hours, so you wish to reduce this as soon as possible. You want to use an agent with rapid onset of
sedation with a short duration of unconsciousness, so you choose:
a. thiopental.
b. chloral hydrate.
c. methohexital.
d. secobarbital.
e. phenobarbital.
1181. Emergence phenomena are a common side effect of ketamine, occurring in up to 50% of adults and
10% of children. Risk factors include:
a. age less than 10 years.
b. male gender.
c. intramuscular administration.
d. simultaneous use of nitrous oxide.
e. a patient who normally has frequent dreams.
1182. The dose of ketamine to obtain the dissociative state is:
a. 1 to 2 mg/kg IM.
b. 4 to 5 mg/kg IM.
c. 1 mg/kg single IV dose.
d. 2 mg/kg single IV dose.
e. 0.05 to 0.1 mg/kg/min IV.
1183. A 6 year old male has an obviously deformed left forearm after falling off a bed while jumping with
a sibling. He is anxious and apprehensive, and the parents are adamant about not causing any more
pain with an intravenous line. The last time the child received ketamine, he developed severe
laryngospasm. An appropriate drug which can be administered rectally is:
a. nitrous oxide.
b. ketamine.
c. morphine sulfate.
d. methohexital.
e. lorazepam.
1184. The competitive neuromuscular blocking agent that neither releases histamine nor exhibits cardiac
muscarinic blockade is:
a. vecuronium.
b. pancuronium.
c. d-tubocurarine.
d. rocuronium.
e. metocurine.
361
1180. c
th
Rosen 5 ,
Chapter 183,
p. 2581
1181. e
Rosen 5th,
Chapter 183,
p. 2582
1182. b
th
Rosen 5 ,
Chapter 183,
p. 2582
1183. d
th
Rosen 5 ,
Chapter 183,
p. 2585-2586
1184. a
th
Rosen 5 ,
Chapter 1,
p. 12
Methohexital has a rapid onset of action, producing unconsciousness, sleeplike state in
less than 1 minute. It also has a brief duration of action, with most patients awake in
less than 10 minutes. The elimination half-life is 3.9 hours. Rapid onset and short
duration of unconsciousness make methohexital an excellent agent for short procedures
such as cardioversion, bone or joint reduction, and CT scan in children. It should be
noted that although methohexital causes profound amnesia, it does not provide
significant analgesia. Consequently, some physicians coadminister small doses of an
opioid for extremely painful procedures.
Risk factors for emergence phenomena associated with ketamine use include age
greater than 10 years, female gender, intravenous administration (especially when
given rapidly), prior personality disorders, and patients who normally have frequent
dreams.
The IV dose of ketamine to obtain the dissociative state is 1 to 2 mg/kg given at a rate
of 0.5 mg/kg/min. For short procedures, particularly in children, the IM route is simple
and effective. A dose of 4 to 5 mg/kg IM is required to consistently achieve the
dissociative state; larger doses offer no additional benefit.
When IV access is not possible or not required, the use of rectal methohexital offers
high success rates, easy administration, and high patient and parent acceptance for
children requiring sedation for procedures.
Vecuronium neither releases histamine nor exhibits cardiac muscarinic blockade, so it
has become popular despite its higher cost and the inconvenience of reconstituting it
from powder with each use.
362
1185. A 27 year male lost control of his motorcycle and collided with an “18-wheeler” at approximately
60 mph. He has a severe open head injury and significant blunt chest and abdominal trauma. The
paramedics were unable to establish an airway. The patient is posturing with severe teeth
clenching. His respirations are shallow at a rate of 8 / minute, his blood pressure is 60/p and his
heart rate is 170 / minute. Your most appropriate induction agent is:
a. thiopental.
b. etomidate.
c. lorazepam.
d. ketamine.
e. methohexital.
1186. A 37 year old male with a long-standing history of intravenous drug use is brought by a friend; the
patient is unconscious, diaphoretic, and has shallow respirations at 6 / minute. The friend says that
the patient had been hoarding his methadone and took an 8-day supply about 30 minutes ago. An
appropriate antidote and dosage would be:
a. nalmefene 0.5 – 1.5 mg IV.
b. naloxone 0.2 mg IV.
c. flumazenil 0.5 mg/kg IV.
d. pentazocin 25 mg IV.
e. clonidine patch.
1187. A synthetic opioid which is highly lipid soluble and easily absorbed through mucous membranes is:
a. fentanyl.
b. hydrocodone.
c. hydromorphone.
d. meperidine.
e. morphine.
1188. 72 year old female inadvertently took several doses of her digoxin and complains of palpitations;
her ECG shows 2:1 atrial flutter. An antidysrhythmic though to be safe in this setting is:
a. bretylium.
b. isoproterenol.
c. phenytoin.
d. procainamide.
e. quinidine.
1189. In patients who have suffered from Clostridium difficile colitis, a novel therapy which has been
shown to decrease recurrence is:
a. amoxicillin 500 mg tid for 14 days.
b. clarithromycin 500 mg bid for 7 days.
c. minocycline 250 mg tid for 10 days.
d. nitazoxanide 100 mg daily for 5 days.
e. saccharomyces boulardii 500 mg bid for 4 weeks.
1190. The local anesthetic you should avoid when treating a patient with coronary artery disease is:
a. benzocaine.
b. tetracaine.
c. lidocaine.
d. cocaine.
e. chirocaine.
363
1185. b
th
Rosen 5 ,
Chapter 1,
p. 13
1186. a
Rosen 5th,
Chapter 156,
p. 2185
1187. a
th
Rosen 5 ,
Chapter 182,
p. 2563
1188. c
Rosen 5th,
Chapter 146,
p. 2106
1189. e
Rosen 5th,
Chapter 89,
p. 1313
1190. d
Rosen 5th,
Chapter 182,
p. 2573
Because etomidate is able to decrease intracerebral pressure, cerebral blood flow, and
cerebral metabolic rate without adversely affecting systemic mean arterial blood
pressure and thus cerebral perfusion pressure, it is an excellent induction agent for
patients with elevated intracerebral pressure, even with hemodynamic instability. The
induction dose of etomidate is 0.3 mg/kg IV.
In contrast to naloxone, nalmefene, another opioid antagonist, has a long half-life (8 to
11 hours) and duration of clinical effect. The initial intravenous dose is 0.5 to 1.5 mg.
Once a clinical response has been achieved, repeated doses or continuous infusions are
generally not required.
In children, oral transmucosal fentanyl citrate may be used when IV access is not
feasible. A fentanyl-impregnated, sweetened matrix in lozenge form on a holder
(fentanyl lollipop) allows transmucosal delivery and a rapid onset of action because
direct absorption into the systemic circulation avoids first-pass metabolism by the
liver. It has been shown to produce sedation and relieve pain 12 to 30 minutes after
administration.
Phenytoin and lidocaine are believed to be the safest of the antidysrhythmic drugs for
controlling tachydysrhythmias in the setting of digitalis intoxication. Most other
cardiac drugs, such as isoproterenol, procainamide, and bretylium, may worsen
dysrhythmias or depress AV conduction.
Adding the yeast Saccharomyces boulardii, 500 mg PO bid for 4 weeks, to antibiotic
treatment dramatically decreases the number of recurrences of C. difficile-associated
disease in patients with previous episodes. However, no benefit results when S.
boulardii is given to patients with an initial episode. No serious adverse reactions have
occurred with the use of S. boulardii.
Cocaine should not be used in patients with known coronary artery disease because it
may cause coronary artery vasoconstriction. Cocaine is also a component in TAC
(tetracaine, epinephrine, and cocaine).
364
1191. A 10 year old boy fell while riding his skateboard and chewing on a Popsicle stick. He sustained a
complex intraoral laceration. You repair the wound and decide to start him on:
a. azithromycin.
b. clindamycin.
c. erythromycin.
d. penicillin.
e. trimethorpim-sulfamethoxazole.
1192. A 42 year old man fell while playing basketball and appears to have a fracture-dislocation of his
elbow. You wish to perform regional anesthesia, but cannot find any lidocaine without
epinephrine. A safe alternative would be:
a. benzocaine.
b. cocaine.
c. dubicaine.
d. prilocaine.
e. tetracaine.
1193. The best method to achieve effective dosing for relief of moderate to severe pain is:
a. intramuscular bolus followed by intravenous maintenance.
b. intravenous bolus followed by oral maintenance.
c. repeat intravenous bolus.
d. repeat oral administration.
e. slow intravenous titration.
1194. An 87 year old man complains of severe weakness and dizziness. He is bradycardic and
hypotensive. The medicine most likely causing his symptoms is:
a. atenolol.
b. clopidogrel.
c. HCTZ.
d. isosorbide.
e. metformin.
1195. A 27 year woman complains of severe diarrhea. Yesterday she eloped from another local hospital
where she had been treated for diarrhea and dehydration. You call the hospital’s lab and determine
that stool cultures were positive for salmonella. Your therapy should start with:
a. ciprofloxacin or trimethoprim/sulfamethoxazole.
b. ivermectin.
c. metronidazole.
d. tetracycline or doxycycline.
e. vancomycin.
1196. A first line agent for both streptococcal and staphylococcal toxic shock syndrome is:
a. clindamycin.
b. ticarcillin.
c. doxycycline.
d. erythromycin.
e. amoxicillin.
365
1191. d
th
Rosen 5 ,
Chapter 52,
p. 748
1192. a
Rosen 5th,
Chapter 182,
p. 2574
1193. e
Rosen 5th,
Chapter 182,
p. 2561
1194. a
th
Rosen 5 ,
Chapter 146,
p. 2109
1195. a
th
Rosen 5 ,
Table 89-2,
p. 1303
1196. a
Rosen 5th,
Chapter 123,
p. 1809
Lacerations of the oral mucosa involve bacteria-rich oral secretions and may become
infected slightly more than other wounds. Although little data suggest a clear
indication for prophylactic antibiotics, one study showed that patients benefit from
antibiotics if they are compliant with their regimen. Rates of infection for complex
through-and-through lacerations may be twice those for simple mucosal lacerations. It
may be reasonable to limit antibiotic use to complex lacerations. Penicillin is an
appropriate choice of antibiotic.
The intravenous regional anesthesia procedure, also called a Bier block, is an effective
and rapid technique to anesthetize extremities for fracture reduction or repair of
extensive wounds. The method involves the IV injection of a local anesthetic agent
into a previously exsanguinated limb. This procedure has been adapted for use in the
ED in the form of a minidose of 100 mg of lidocaine. A safe alternative is to use the
relatively nontoxic local anesthetic agent, prilocaine.
The proper way to achieve the effective dosage for moderate to severe pain is to use a
slow IV titration. Some patients require greater than 25 mg of morphine for relief,
whereas others become comfortable at substantially lower doses.
The most common initial sign of beta-blocker ingestion remains bradycardia, which
should draw attention to the possibility of cardiac drug overdose. Hypotension and
unconsciousness are the second and third most common signs, respectively.
The following antibiotics are the drugs of choice in the pathogens listed below:
Salmonella and Shigella: ciprofloxacin, TMP/SMX
Vibrio parahaemolyticus: tetracycline or doxycycline
Clostridium difficile: metronidazole, vancomycin
Giardia lamblia: metronidazole, furazolidone
Strongyloides stercoralis: ivermectin
For both staphylococcal and streptococcal toxic shock syndrome, most clinicians
recommend clindamycin as a first-line agent. Clindamycin is a potent suppressor of
bacterial toxin synthesis; it also facilitates phagocytosis streptococci and has a longer
postantibiotic effect than the beta-lactams.
366
1197. A 29 year old woman who is seven months pregnant went camping about 3 weeks ago. Shortly
after returning she developed generalized weakness, lethargy, and a temperature of 40oC which
lasted about 3 days. Her family doctor and obstetrician both felt she had a viral illness. Now she
again feels weak and feverish, but not as bad as the first time. She should be treated with:
a. oral tetracycline 500 mg qid for 5 to 10 days.
b. intravenous ticarcillin 1 mg intravenous.
c. oral doxycycline 100 mg bid for 7 days.
d. oral erythromycin 500 mg qid for 5 to 10 days.
e. oral ampicillin 1 gram daily for 10 days.
1198. In patients with tick-induced relapsing fever, as many as one third of patients may experience a
Jarisch-Herxheimer-type reaction characterized by an increased temperature, severe rigors, a drop
in leukocyte and platelet counts and hypotension. Suggested treatment for this reaction includes
intravenous volume expansion and:
a. dopamine.
b. vitamin B6.
c. diphenhydramine.
d. naloxone.
e. meptazinol.
1199. The drug of choice to treat Lyme disease in men, nonpregnant and nonlactating women, and
children older than 8 years of age is:
a. amoxicillin.
b. clindamycin.
c. doxycycline.
d. erythromycin.
e. ticarcillin.
1200. The drug of choice to treat Lyme disease in pregnant women, and children younger than 8 years of
age is:
a. amoxicillin.
b. clindamycin.
c. doxycycline.
d. erythromycin.
e. ticarcillin.
1201. A 3 year old girl presents with frequent paroxysms of coughing. The mother says the child coughs
“at least 50 times a day”. She is noted to cough repeatedly in short exhalations, and after 10 to 15
coughs, he inhales forcibly. She is nontoxic appearing and has a low-grade temperature. With
strict isolation for 7 days and erythromycin at 50 mg/kg/day in four divided doses she can be
managed on an outpatient basis, but close contacts should be treated with:
a. amoxicillin.
b. ciprofloxacin.
c. doxycycline.
d. erythromycin.
e. rifampin.
367
1197. d
th
Rosen 5 ,
Chapter 128,
p. 1890
1198. c
th
Rosen 5 ,
Chapter 128,
p. 1890
1199. c
Rosen 5th,
Chapter 128,
p. 1887
1200. a
Rosen 5th,
Chapter 128,
p. 1887
1201. d
th
Rosen 5 ,
Chapter 123,
p. 1790
Relapsing fever is treated effectively with tetracycline or erythromycin. Tetracycline
should be avoided in children younger than 8 years old and in pregnant women.
As many as one third of patients may experience a Jarisch-Herxheimer-type reaction
after treatment with antibiotics. The reaction may be severe, especially with louseborne relapsing fever. This phenomenon may be related to administration of cytokine
intermediaries or endogenous opioids. Approximately 4 hours after antibiotic
treatment and coinciding with the clearance of spirochetes from the blood, the patient
usually experiences an increase in temperature, severe rigors, a drop in leukocyte and
platelet counts, and hypotension. Anticipation of the reaction is crucial because IV
volume expansion with saline solution may be required to maintain the blood pressure;
the reaction may be more threatening than the disease itself. Meptazinol, an opioid
antagonist with agonist properties, has been proposed for use in treatment of this
reaction.
Prompt antibiotic therapy is essential in early Lyme disease because it generally
shortens the duration of the rash and associated symptoms and, more important,
prevents later illness in most patients. Some patients with severe early disease,
however, develop later stages despite courses of antibiotics. The drug of choice for
men, nonpregnant and nonlactating women and children older than 8 years of age is
doxycycline. Pregnant or lactating women and children less than 8 years old should
receive amoxicillin. For patients who cannot tolerate tetracyclines and are allergic to
penicillins, erythromycin is recommended but is probably less effective.
Pertussis patients without significant complications may be managed as outpatients and
advised of the potential complications. The patient should be strictly isolated for 7
days and erythromycin prescribed to limit the spread of infection. Erythromycin
should also be prescribed for any unimmunized person or partially immunized infant
with a history of significant exposure to the index case. Adults who will come in close
contact with susceptible children should also take erythromycin prophylaxis.