CHF (Handout, B. Shah, 2005)
advertisement
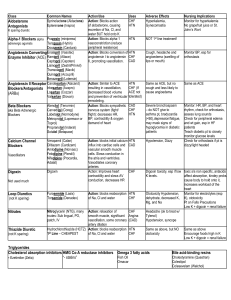
CONGESTIVE HEART FAILURE Brijen J. Shah, MD July 17, 2005 Goals: 1. 2. 3. 4. 5. To review the etiology and basic pathophysiology concepts related to congestive heart failure. To understand the difference between right and left sided heart failure To identify symptoms from the history and physical exam findings related to CHF To be able to generate the elements needed for an initial workup of CHF To outline strategies of CHF therapy as it relates to mechanism of disease A. Pathophysiology Two main entities which determine the mechanism of disease: systolic dysfunction and diastolic dysfunction. 1. Systolic dysfunction, relating to the pumping mechanism of the heart. -Decreased contractility Etiologies: MI(62%), valvular heart disease, HTN (10%), cardiomyopathy Arch Intern Med 2001 Apr 9;161(7):996-1002. -Increased afterload related to HTN -Body’s own compensation: In CHF, the heart undergoes certain changes which allow it to maintain it’s equilibrium. It’s when these mechanisms are maximized that a CHF exacerbation may occur. a. Frank-Straling curve represents the mechanical relationship between muscle fibers and volume. With regards to CHF, increased volume (end-diastolic volume due to poor systolic emptying) leads to increased stretch of myofibers/cross links which then increase contractility. b. Hypetrophy. -Increased inotropy by endogenous catecholamines. 2. Diastolic dysfunction relating to active relaxation in early diastole and passive filling. B. Right vs left heart failure Left heart failure is related to any process that effects the left side such as an left ventricular ischemic event. Right sided hear failure which is most commonly due to left sided heart failure and COPD. C. Symptoms These can be divided into symptoms of excess fluid accumulation and symptoms related to decreased cardiac output. The chronicity of these symptoms can help determine the underlying cause. Dyspnea (from vascular congestion and decreased CO), orthopnea, PND, edema (related to disequilibrium in Starling Forces), anorexia, fatigue, bowel distention, palpitations, lightheadnedd New York Heart Association classification of heart failure is based on symptoms and activity level. Class I (few symptoms at high levels of activity) to class IV (symptoms at rest). D. Physical Exam The multiple mechanisms resulting in CHF also determine the physical findings. Mechanism Decreased cardiac output Volume overload Ventricular enlargement Pulmonary HTN Physical Exam Sinus tachycardia, diaphoresis; cool, pale and cynatoic limbs, palpable dichotic notch, pulsus alternans Rales peripheral edema- ascites, hepatomegaly, splenomegaly elevated JVP S3, laterally displaced PMI Accentuated P2 E. Diagnostic Tests Blood test- CBC can reveal an anemia which could exacerbate CHF. Chemistries are important in determining treatment and baseline renal function (creatinine, potassium). LFTs can be elevated with hepatic congestion. Thyroid function as hypothyroidism and thyrotoxicosis can present as heat failure. BNP is a substance released in response to high ventricular filling and elevated values have been shown to coorelate with CHF. N Engl J Med 2002 Jul 18;347(3):161-7. ECG- Although any new finding for a patient with new CHF could lead the underlying cause, in most patients it is important to look for evidence of ischemia (ST segment changes, T wave inversions) or atrial fibrillation. Assess voltage for left ventricular hypertrophy. CXR- cardiomegaly, Kerley B lines, pulmonary effusion, vascular congestion ECHO- This 2D test can help to assess for valvular abnormalities, right ventricular size, left systolic function. Cardiac catheterization- Helpful in looking for chamber pressures, pulmonary artery hypertension, shunts, as well as flow limiting lesions for ischemia. F. Treatment Correct underlying cause, ie. valvular disease! Mechanism/Symptom Systolic Dysfunction Contractility Reducing afterload Reducing preload and LV pressure Increased catecholamines Pulmonary edema Diastolic heart failure Agents Digoxin, beta agonists (dobutamine), PDE inhibitors (milrinone, amrinone) ACEI, nitrates, hydralizine Diuretics and vasodilators Beta blocker Oxygen, furosemide, morphine, nitroprusside, intubation Diuretics, beta blocker Long term: cardiac rehabilitation, cardiac transplantation Additional Bibliography: Harrison’s Principles of Internal Medicine, 15th edition. Lilly L. et al, Pathophysiology of Heart Disease. “Congestive Heart Failure” Up to Date