pdr tmj evaluation - Minnesota Occupational Therapy Association
advertisement

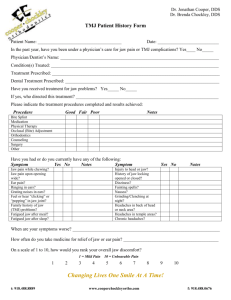
PDR TMJ EVALUATION Name: _______________________________________ Date:____________________ History & Symptoms: History______________________________________________________ _________________________________________________________________________________ Hx of blow to head or face ____________________________________________________________ Head & Jaw Symptoms: Jaw Pain (0-10) ___________ Right / Left / Bilateral: _______________ Frequency ______________________________ TMJ Noise: None / Clicking / Popping / Grinding / Cracking / Other:________ TMJ Locking: None / Open / Closed / Tightness: __________________ HA: Yes No Frequency: _________________________________ Neck Pain right/Left ________________________________________________ Ear Pain/Stuffiness Right/Left Dizziness/vertigo _______________________ Teeth Pain _____________Other:_____________ ___________ Symptoms relieved with: Heat / Ice / Rest / Soft diet / Massage / Relaxation / Exercise / Medication / Other: ___________________________________ Previous Treatment: ____________________________ Current Medications __________________ Appliance Yes No Type: ________________ Pertinent Medical History / Surgeries / Contraindications ____________________________________________________________________________ Contributing Factors: Clenching / Bruxism / Gum / Leaning on Chin / Sleep Position / Phone / Biting Habits / Jaw Thrust / Tongue Thrust/ Chewing Functional Limitations Sleep is reduced by none / ¼ / ½ / ¾ of pre-injury level. Hours __________ Waking _________ Pain level _______ Sleep Position: prone / sup / side (R/L) Surface & Pillow support: ______________________________________ Sx in am: ____________________ Sitting Tolerance: NA / 1 hr / ½ hr / 10 min / avoids ______________________ Pain Level____________________ Required: _______________ Sustained Head Position Tolerance: NA / 10 min / ½ hr / 1 hr/ 2 hr / avoids_________Pain Level____________________ Required: _______________ Jaw Activities: Talking Tolerance _____________________ P level:________ Dental Tolerance: ______________________ P level:________ Oral Hygiene Tolerance _____________________ P level:________ Yawning Tolerance: ______________________ P level:________ Laughing Tolerance ________________________ P level:________ Chewing Tolerance_______________________ P level:________ Work / Other Functional Limitations:___________________________________________________________________________________________ Current overall ability to perform self-cares and HH tasks < 3/10: _______% Current ability to perform job tasks < 3/10 : __________% Systems Review: General Behavior & Affect: flat / calm / acute distress / cooperative / non-cooperative / other: ______________________ Communication & Cognition: normal / impaired / difficulty staying on task / symptom magnification / neurological issues / ESL / Translator Present Anxiety / Stress ____________________________________________ General Health: _________________________________________________ Postural: FHP / FSP Lips:Open / Closed / Tense Tongue: Up / Down / Thrust Breathing Pattern: Mouth / Nose / Shallow/ Diaphramatic Tests, Measures,& Palpation AROM: Active Incisal Opening ___________mm (Normal 40-60mm) Lateral Excursion Right _________ mm Left __________ mm (Normal > 7mm) Passive Incisal Opening ____________mm (Normal 42-62mm) Protrusion ___________ mm (Normal > 7mm) R__________________________L Quality of Motion: Smooth / Rigid / Jerky / Guarded / Fasciculation / Thrusting ______________ TMJ Translation: R=L R<L R > L __________________________________________________________ TMJ Noise: Right: Opening Click / Closing Click / Reproducible / None Quality: Soft / Loud Crepitus: Fine / Course Left: Opening Click / Closing Click / Reproducible / None Quality: Soft / Loud Crepitus: Fine / Course PDR TMJ EVALUATION Name: _______________________________________ Palpation: + Pain, -- Pain Free, * Duplicates Pain Right _________ _________ _________ _________ _________ _________ _________ _________ _________ Left Temporalis ________ Masseter ________ Medial Pterygoid ________ Anterior Digastric ________ Internal Lateral Pterygoid ________ Internal Medial Pterygoid ________ Internal Temporalis Tendon________ Internal Anterior Masseter ________ Capsule ________ Cervical Screen: Forward Flexion _________________________________________ Protrusion _________________________________________ Left Sidebend _________________________________________ Left Rotation _________________________________________ Examiner/Date:_________________ Special Tests: Max Clench (30 sec) R: ________ L: ________ S=Same side O=Opposite side -- Pain Free Weight Bearing –loading joint + Pain, -- Pain Free, *Duplicates Click Opening R: _______ L: _______ Deviation R: _______ L: _______ Protrusion R: _______ L: _______ Joint Distraction Anterior/Medial Glide R=L R=L R>L R>L R < L _________________ R < L _________________ Extension ___________________________________________________ Retraction ____________________________________________________ Right Sidebend ___________________________________________________ Right Rotation ____________________________________________________ Palpation: (tender/spasm): Right: SO, CEXT, SCAL, UT, LS, SCM, PECMAJ, PECMIN Left: SO, CEXT, SCAL, UT, LS, SCM, PECMAJ, PECMIN Other: ______________________________________ __________________________________ Evaluation Summary: _______ Subjective Impairments _______ Severe/ Moderate/ Mild Pain in ________________________________________________________________________ _______ Headaches / Dizziness ______________________________________________________________________________ _______ Extremity Sx _______________________________________________________________________________________ _______ Objective Impairments _______ Pain Medication Reliance _____________________________________________________________________________ _______ Postural Dysfunctions: _______________________________________________________________________________ _______ TMJ Dysfunction: _____ Myofascial Pain (R / L ) _____ Disc Disorder ( R / L ) _____ Subluxation/Hypermobility ( R / L ) ______Arthritis (R / L ) _____ Capsulitis (R / L ) _______ Vertebral Mobility Dysfunction (MET): ___________________________________________________________________ _______ Myofascial / Palpatory Dysfunction: _____________________________________________________________________ _______ Fair / Poor AROM in R / L Upper Extremity / JAW ________________________________________________________ _______ Fair / Poor MMT strength in R / L SCAP/ Upper Extremity __________________________________________________ Functional Limitations / Impairments: _____ SLEEP: Inability to achieve quality sleep. Limited due to pain; sleep reduced by > 25%, waking several > 3 x night, and/or waking in > 3/10 P. _____ SITTING: Inability to sit normal duration ( 1- 2 hours) to complete educational, desk, and/ or dining activities. _____ HEAD POSITIONS: Prolonged head positions (30 min – 2 hrs) creates fatigue and / or >3/10 pain with reading, and/or overhead activities. _____ JAW ACTIVITIES: _____ Inability to tolerate conversation due to jaw pain > 3/10 _____ Inability to tolerate dental work due to jaw pain >3/10 ______Inability to tolerate oral hygiene due to jaw pain > 3/10 _____ Inability to tolerate yawning due to jaw pain > 3/10 ______Inability to tolerate laughing due to jaw pain > 3/10 _____ Inability to tolerate opening mouth to eat or chew due to jaw pain > 3/10 _____ SELF CARES: Inability to complete self cares and oral hygiene efficiently independently, and/or due to pain > 3/10, currently __________% able _____ WORK: Inability to complete following work and / or specific daily requirements: currently __________% able _____ Inability to sit required duration of ________________________________________________________________________ _____ Inability to perform: ___________________________________________________________________________________ _____ HEALTH:Inability to engage in physical exercise due to pain > 3-5/10, putting patient at risk for medical issues associated with sedentary lifestyle. _____ SOCIAL: Inability to engage in wellness, family, or social activities due to fatigue and exhaustion created from pain interference in daily life. _____ FLARE UPS: Patient does not demonstrate any measurable functional limitations as of today; however suffers from periodic, recurrent flare-ups that significantly impair functional levels on a regular basis & demonstrates objective impairments ______Others:_____________________________________________________________________________________________________________ Prognosis: Patient demonstrates EXCELLENT/ GOOD/ FAIR/ POOR motivation to improve functional status and reach established goals. Prognosis for this patient is EXCELLENT/ GOOD/ FAIR/ POOR based upon above orthopedic and functional problems, chronicity of symptoms, and/or co-morbidities, to achieve program goals. TMJ REHABILITATION PLAN OF CARE Name: _______________________________________ Examiner/Date:_________________ Rehabilitation Goals: (circle those that apply) 1. 2. RECOVERY: Pt will report a total recovery (0-10) rating of >7/10; and reduction of all pain, HA and jaw symptoms by 75% PAIN/MEDS: Pt will demonstrate knowledge in pain management strategies (icing, self treatment techniques) as instructed by therapists; decreasing pain levels by >75%, and/or decreasing reliance for pain medications by >75%. 3. HEADACHES: Pt will report > 75% reduction in headaches and demonstrate indep in headache pain management / therapeutic ex program. 4. SLEEP: Pt will be educated in good sleep postures & report that their typical duration of sleep is restored, sleep is uninterrupted by pain, and/or pt is waking with pain < 3/10 5. POSTURE: Pt will improve posture and postural habits, and postural strength to: a. ______ SITTING: ability to sustain improved postural habits in sitting and standing to improve sitting & standing tolerance by 75% b. ______ HEAD POSITIONS: tolerate prolonged reading and/or overhead activ (30 min– 2 hrs), with mild fatigue and/or P < 3/10 c. ______ OTHER: ___________________________________________________________________________________________ 6. JAW ROM: Pt will improve jaw AROM to WNL (40-60mm) of opening and (7mm) of lateral excursion with pain level < 3/10. 7. JAW FUNCTION: Pt will demonstrate WNL / mild / moderate dysfunction in AROM / strength impairments to allow a. ______ ability to tolerate conversation with < 2/10 pain b. ______ ability to tolerate pain free yawning with < 2/10 pain c. ______ ability to tolerate pain free laughing with < 2/10 pain d. ______ reduce jaw pain with chewing, with < 2/10 pain after prolonged use e. ______ reduced jaw pain with oral hygiene and/or dental work activities with < 2/10 pain f. ______ other: _____________________________________________________________________________________________ 8. SELF CARES/HH: Return to >85% ability to do all self and household requirements at tolerable level of <3/10 pain. 9. WORK: Return to >85% ability to do all work related requirements at tolerable level of <3/10 pain. 10. HEALTH/HEP: Demonstrate independence with home exercise program (stretching, CV, and strengthening exercise) prescribed by therapists with good technique and without verbal cues, engaging in regular exercise with pain < 3/10 to promote active lifestyle, and continued wellness. 11. HABITS: Pt will demonstrate understanding of contributing factors to dysfunction and make lifestyle modifications to prevent flare-ups. 12. OTHER:__________________________________________________________________________________________________________ _________________________________________________________________________________________________________________ Duration & Frequency: __________ X WEEK FOR __________ VISITS ________________________________________ Treatments & Interventions: Interventions & Treatments provided by PT, OT, PTA, or COTA in accordance to practice acts & scope of practice MedX equipment strength & AROM therapeutic exercise in-clinic; goal resistance set to body weight comparisons IF ORDERED & INDICATED Stretching & Mobility Home Exercise Prescription (see PLAN OF CARE FLOW SHEET) Patient Education (see PLAN OF CARE FLOW SHEET) Strength & Stability Home Exercise Prescription (see PLAN OF CARE FLOW SHEET) Exercise & Education Perscription: SEE TMJ/TMD PROGRAM PLAN OF CARE FLOW SHEET Discharge Planning PT, OT, and doctor will formally re-assess patient at least every 8 visits to establish progress, re-evaluate subjective and objective goals, and make appropriate changes to the rehab plan. These changes will be indicated in the Doctor PT/OT Order Form, daily SOAP note, Internal Progress Note, and on the Protocol Flow Sheet. Patient will undergo formal discharge evaluations by PT, OT, and Doctor at the completion of their treatment program. Please refer to this documentation in the patient chart as the complete medical record. I certify that this treatment plan’s nature, scope, and duration, is medically necessary & reasonable to reach the therapy goals for patient’s illness/injury. _______________________________________ Physical/Occupational Therapist Signature & Date PER MEDICARE GUIDELINES: Per Medicare guidelines, as a supervising physician, please sign that you have certified that this plan of care is medically necessary and will reasonably diagnose or improve the functioning of the patient. Supervising Physician Signature: ______________________________________________________________________________________________