WA Mass Casualty Aeromedical Transport Plan
advertisement
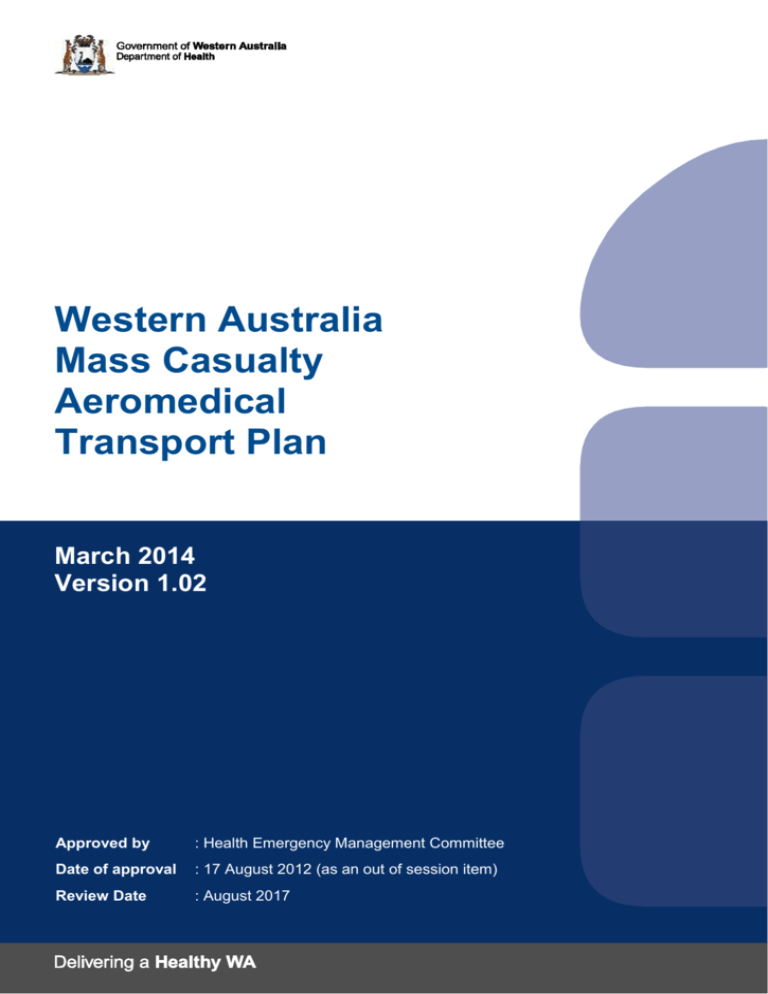
Western Australia Mass Casualty Aeromedical Transport Plan March 2014 Version 1.02 Approved by : Health Emergency Management Committee Date of approval : 17 August 2012 (as an out of session item) Review Date : August 2017 Contact officer For copies of this plan, or to provide comment, contact: Manager Disaster Preparedness & Management Unit Health Department of Western Australia Level 3C, 189 Royal St, East Perth 6004 DPMU@health.wa.gov.au AMENDMENT No. 1 1.02 DETAILS DATE INITALS September 2012 Initial Release March 2014 AMENDED BY Minor update of available resources ML SL /TS 2 Contents page Executive summary ...................................................................................................... 5 1. Authority and planning responsibility ................................................................. 6 2. Plan review and amendments .............................................................................. 6 3. Aims and objectives .............................................................................................. 6 4. Hazard definition.................................................................................................... 6 5. Legislation and related documents...................................................................... 7 6. Preparedness ......................................................................................................... 7 6.1. Responsibility for preparedness......................................................................... 7 6.2. Planning and arrangements ............................................................................... 7 6.3. Resources ......................................................................................................... 8 7. 6.3.1 WA fixed wing aeromedical assets .............................................................. 8 6.3.2 WA rotary wing aeromedical assets ............................................................ 8 6.3.3 Neighbouring interstate fixed wing aeromedical assets .............................. 9 6.3.4 Neighbouring interstate rotary wing aeromedical assets ............................. 9 6.3.5 Federal assets........................................................................................... 10 6.3.6 WA Non-commercial non-aeromedical assets .......................................... 10 6.3.7 WA commercial non-aeromedical assets .................................................. 11 Response ............................................................................................................. 11 7.1. Plan activation procedures .............................................................................. 12 7.2. Notification ....................................................................................................... 13 7.3. Strategies for a health response ...................................................................... 14 7.4. Considerations when planning an aeromedical response ................................ 14 7.4.1 Location of incident ................................................................................... 14 7.4.2 MCI exceeding WA aeromedical capability .............................................. 15 7.4.3 Bariatric aeromedical transfers.................................................................. 16 7.5. Immediate response actions ............................................................................ 17 7.6. Command and control ..................................................................................... 17 7.7. Coordination .................................................................................................... 17 7.7.1 State Health Incident Coordination Centre ................................................ 17 7.7.2 Planning cell .............................................................................................. 18 7.7.3 RFDS Western Operations Coordination Centre ....................................... 19 7.8. Health response actions .................................................................................. 19 7.9. Communications .............................................................................................. 20 7.10. 8. Financial arrangements for response ........................................................... 20 Recovery .............................................................................................................. 20 3 8.1. Responsibility for Recovery ............................................................................. 20 8.2. Stand Down and Post-Operations Report........................................................ 21 9. Acknowledgements ............................................................................................. 21 Appendix 1: Contact list – aeromedical operators................................................... 22 Appendix 2: Contact list – non-aeromedical operators ........................................... 23 Appendix 3: Contact list – key agencies................................................................... 24 Appendix 4: Indian Ocean Territories aeromedical response ................................ 24 Appendix 5: Master action card 1: Aviation Planning Officer ................................. 25 Appendix 6: Master action card 2: Aeromedical Liaison Officer (RFDS Western Operations).................................................................................................................. 26 Appendix 7: Master action card 3: Aviation Liaison Officer (WA Police Air Wing) 27 Appendix 9: Neighbouring interstate aeromedical assets ...................................... 29 Appendix 10: WA non-aeromedical assets ............................................................... 30 Appendix 11: Medical cache assets .......................................................................... 31 Appendix 12: Locations of designated airfields for each type of QANTAS commercial aircraft for WA ........................................................................................ 35 4 Executive summary The Western Australian (WA) Mass Casualty Aeromedical Transport Plan is a subplan of WESTPLAN – Health and has been developed in consultation with key aeromedical and non-aeromedical aviation stakeholders. The intent of the plan is to provide a framework for aeromedical retrievals and evacuations following a mass casualty event in the regional and remote areas of WA WA is the largest and most remote state in Australia. Additionally, all critical care infrastructure is based in Perth and as such, any casualty requiring critical care services will need to be transferred to Perth or an interstate facility offering appropriate clinical services. It is acknowledged that any mass casualty event outside of the Perth metropolitan area will provide significant logistical challenges for WA Health and other WA emergency services. The broad framework of this plan is for the State Health Coordinator to delegate the central coordination of aeromedical assets (government and private) to the Royal Flying Doctor Service – Western Operations. Non-aeromedical assets will be coordinated by the WA Police air wing. The State Health Coordinator will maintain overall control of the WA health response to a mass casualty incident. Linkages to the National Aeromedical Transport Coordination Group will be through the aviation planning cell within the State Health Incident Coordination Centre. 5 1. Authority and planning responsibility The authority to plan as a Combat Agency stems from the Western Australian Emergency Management Act (2005) Section 18 to ensure appropriate planning and response capabilities are in place to respond to disaster or emergency health requirements. The development, implementation and revision of this plan is the responsibility of the Disaster Preparedness and Management Unit, in consultation with the Health Emergency Management Committee (HEMC) and relevant stakeholders. 2. Plan review and amendments As per State Emergency Management Policy No. 2.2, the Disaster Preparedness and Management Unit (DPMU) and the WA HEMC shall ensure that review period shall not be more than five years with the review commencing 12 months prior to the review date of endorsement by the WA HEMC. The review period can be linked to any activation of the plan 3. Aims and objectives The aim of the Western Australian (WA) Mass Casualty Aeromedical Transport Plan is to provide a basis for managing the movement of a large number of casualties via air, thereby providing the best opportunity for a favourable outcome for those casualties. The objectives of this subplan are to: Identify the agency responsible for the coordination of aeromedical assets in consultation with State Health Incident Coordination Centre (SHICC). Provide the basis for the provision and coordination of aeromedical transport response during a major disaster emergency. Provide guidelines for the operation of the plan following its activation. 4. Hazard definition For the purposes of this plan, the hazard is defined as a mass casualty incident in Western Australia (WA) that requires the use of aeromedical assets to transfer the casualties to appropriate medical facilities. The following outlines the challenges facing agencies when planning or responding to an incident requiring an aeromedical response in WA: Accessibility to some regions within WA with limited landing sites and fuel availablity. The extended flight times involved and the limit imposed by Civil Aviation Safety Authority (CASA) on pilot hours. The limited number of aeromedical assets in WA that can respond to a mass casualty incident in the Indian Ocean Territories. 6 The large number of industry facilities within WA and offshore, an increase in the number of Suspected Illegal Entry Vessels (SIEV) entering Australia via the north of the state. The geographical nature of the north of the state is such that an effective response would be difficult, especially during the wet season, when accessibility from the landing site to the disaster location may be hampered. The lack of critical care facilities in regional WA necessitating the movement of all critically injured to Perth for definitive care. Response capability of sites in the north is limited by lack of specialist clinicians and these sites would need additional specialist medical team/s to be deployed in to assist depending on the nature of the incident. 5. Legislation and related documents This plan is to be read in conjunction with: Emergency Management Act 2005; Emergency Management Regulations 2006; WESTPLAN – Health; SEMP 4.1 Operational Management; Local Emergency Management Arrangements; and Relevant agency plans / procedures. 6. Preparedness 6.1. Responsibility for preparedness Organisations, both government and private, with responsibilities within this plan are to ensure strategies and operational plans are in place to support the WA Mass Casualty Aeromedical Transport Plan. Preparedness activities include: Developing agency response plans and procedures. Designing organisational structures. Implementing training programs. Developing resource management systems, ensuring 24/7 contactability. 6.2. Planning and arrangements This plan will be used to manage a mass casualty incident in WA that requires the use of aircraft to transport casualties to appropriate medical facilities. 7 Training of aeromedical services in WA is a fundamental requirement for preparedness. Aeromedical operators must understand their role within the context of the WA Mass Casualty Aeromedical Transport Plan. All aeromedical services are responsible for the identification of local training needs, and the subsequent planning and implementation of a training program. Where multiple aeromedical services are involved in a State or National aeromedical exercise then the Disaster Preparedness & Management Unit (DPMU) shall coordinate the information, dissemination and preparedness of aeromedical providers for the exercise. 6.3. Resources The principles underpinning this WA Mass Casualty Aeromedical Transport Plan are that all aeromedical assets (public and private) will be coordinated by the Royal Flying Doctor (RFDS) – Western Operations section and all non- aeromedical assets will be coordinated by WA Police Air Wing. 6.3.1 WA fixed wing aeromedical assets 6.3.1.1. Royal Flying Doctor Service Western Operations Royal Flying Doctor Service (RFDS) Western Operations has 14 Pilatus PC12 turboprop aircraft and one medically-dedicated LifeFlight jet (a Hawker 800XP) which are located in 5 bases around the state at Jandakot Airport (Perth), Kalgoorlie, Meekatharra, Port Hedland and Derby and Perth Domestic Airport (the LifeFlight Jet). Each aircraft can be staffed by a doctor and a nurse. Activation time is subject to current workload 90 minutes from base or less. All the aircraft can carry 2 stretchers and 1 sitting patient. Depending on crew configuration, 1 or 2 critical are patients can be transported at any one time. The jet can carry three stretcher patients or two stretcher patients and up to three seated patients if necessary. 6.3.1.2. CareFlight International CareFlight international have 1 jet based in Darwin and 2 based in Sydney. Activation time is 2 hours. 6.3.1.3. Aspen Medical Aspen Medical has a Citation jet based in Karratha with a doctor and ICU paramedic. Activation time is 60 minutes. This service is contracted to provide support of seven mining companies, including; Woodside, Chevron, Vermilion, BHP, Apache, Santos and Total. The aircraft can carry 1 stretcher and 1 sitting patient. 6.3.2 WA rotary wing aeromedical assets 6.3.2.1. State Emergency Rescue Helicopter The RAC Rescue helicopter is based at Jandakot airport with a critical care paramedic and doctor as requested. Activation time is 15 minutes. It has an operating range of 250-400 km depending on fuel. This aircraft can carry 1 stretcher or ICU patient and is fitted with a rescue winch, which can be used day or night and can lift up to 272kgs 8 6.3.2.2. BHP BHPB Iron Ore (BHPBIO) has a contract with Heliwest to provide 1 helicopter with limited aeromedical capability. The aircraft is based in Port Hedland. This aircraft and has the capacity to transport 1 stretcher patient and is crewed with pilots only but has the capability to carry 1 site based medical officer if required. The aircraft has limited night flying capability and is currently restricted to a 90Nm range of Port Hedland due fuel capacity and associated flight planning constraints. This helicopter has no winch capability. 6.3.2.3. Royal Australian Air Force – Pearce The Royal Australian Air Force (RAAF) Pearce has 1 Sikorsky S76 or Bell 412 on rotation for maintenance. These aircraft can be configured to carry 2 stretcher patients utilizing the Inferno 71S rescue stretchers and is fitted with a rescue winch, which can be used day or night and can lift up to 272kgs. A military doctor and medic can be provided. 6.3.2.4. WA Police Air Wing WA Police Air Wing has two twin engine helicopters, a Dauphin AS365n3+ and a BK117, based at Jandakot. Police Air Wing performs standby Air Ambulance duties when the State Emergency Rescue Helicopter is unavailable. Both aircraft are multipurpose but can be quickly configured for 1 stretcher patient and a paramedic. Both aircraft can be configured to transport multiple sitting patients and are fitted with rescue winches, which can be used day or night and can lift up to 272kgs; including stretcher patients. WAPOL have fuel located strategically across Western Australia. 6.3.3 Neighbouring interstate fixed wing aeromedical assets 6.3.3.1. RFDS Central Operations RFDS Central Operations has 11 turbo prop aircraft which are located in 3 bases in South Australia and the Northern Territory. These aircraft are based in Adelaide, Port Augusta and Alice Springs. Each aircraft can be staffed by a doctor and a nurse. All the aircraft can carry 2 stretchers and 1 sitting patient. Depending on crew configuration, 1 or 2 Intensive Care Unit (ICU) patients can be transported at any one time. 6.3.3.2. CareFlight Northern Operations (Northern Territory) CareFlight Northern Operations is based in the Northern Territory and has 8 turboprop aircraft. These aircraft are based in Darwin, Katherine and Gove. 6.3.4 Neighbouring interstate rotary wing aeromedical assets 6.3.4.1. CareFlight Northern Operations (Northern Territory) CareFlight Northern Operations is based in the Northern Territory and has 2 rotary wing aircraft based in Darwin. 9 6.3.4.2. MedSTAR (South Australia) MedSTAR based in Adelaide has access to 3 rotary wing aircraft that can be staffed be a doctor, nurse or paramedic. 6.3.5 Federal assets 6.3.5.1. Australian Defence Force The Australian Defence Force (ADF) has at its disposal in the event of an Aeromedical response both turbo prop C130 and Jet C17 fixed wing aircraft operated by the RAAF. The current configuration of these aircraft allow for a maximum of 4 ICU patients to be transported in any 1 aircraft. The ADF also has access to various rotary wing aircraft operated by both the Army and Navy that can be configured for Aeromedical use. Access to these aircraft is by formal request via the Executive Officer WA State Emergency Management Committee (SEMC). 6.3.5.2. QANTAS An arrangement exists between Western Australia Police (WAPOL) Incident Control Centre and the Qantas WA regional manager. The Deputy Commissioner of Police can contact the Qantas Regional Manager directly if a Qantas asset is required. In turn, WAPOL requests are discussed with Qantas operations in Sydney and an assessment made as to whether or not assistance can be granted and then planning would occur. 6.3.6 WA Non-commercial non-aeromedical assets 6.3.6.1. West Australian Police Air Wing WA Police (WAPOL) has three fixed wing aircraft; 2 x Pilatus PC12 based at Jandakot and Karratha respectively. These aircraft can carry nine passengers and have a large cargo door to allow easy loading of cargo if required. WAPOL also have a GA8 Air Van based at Jandakot. It is capable of carrying five passengers and/or cargo. The Police Air Wing regularly charter aircraft across Western Australia to perform a variety of police tasks and maintain a database of suitable operators – both fixed wing and rotary. All operators used by WAPOL must hold a CASA approved Air Operators Certificate. 6.3.6.2. Bristow Helicopters – Ausrtralia Bristow Helicopters currently operate a number of rotary aircraft primarily based in the North West of WA. The number of available aircraft may fluctuate due to maintenance requirements. 6.3.6.3. CHC Helicopters (Australia) CHC helicopters a number of rotary aircraft primarily based in the North West of WA. The number of available aircraft may fluctuate due to maintenance requirements. 10 This number may fluctuate due to maintenance requirements. These helicopters are rated for night flying operations. 6.3.7 WA commercial non-aeromedical assets 6.3.7.1. Cobham (formerly National Jet) Cobham operate a large number of commercial turbo prop and jet aircraft based at Perth domestic airport. Cobham has in the past assisted in the aeromedical evacuation of patients from the Indian Ocean Territories. 6.3.7.2. Skippers Skippers operate a large number of commercial turbo prop and jet aircraft based at Perth domestic airport. 6.3.7.3. Air North Air North is based out of Darwin in the Northern Territory but has a comprehensive network in the Kimberley and Pilbara regions of WA. Air North operate a large number of commercial turbo prop and jet aircraft. Air North does operate a direct flight between Perth and Kununurra. 6.3.7.4. Maroomba Airlines Maroomba Airlines operate a number of commercial turbo prop and jet aircraft based at Perth domestic airport. In addition to operating and maintaining the Rio Tinto LifeFlight Hawker 800XP jet used by the RFDS, they operate a Hawker 850 jet under contract to the Department of Premier & Cabinet. This aircraft can carry seated personnel and equipment but is not configurable for stretcher transport. 6.3.7.5. Revesco Aviation Revesco Aviation operate a number of medium to large corporate jets from the Perth domestic airport. Thes include a Bombardier Challenger 601 which is configured with an RFDS LifePort system. It can carry an additional 1-2 stretcher patients configured across club seats. 6.3.7.6. Other Other commercial non-aeromedical operators are available from time to time in regional centres and in Perth but usually do not have proper medically-configurable aircraft or aeromedical crews. The RFDS regularly uses charter aircraft of opportunity in the Kimberley out of Broome, Derby or Kununurra which can be jury rigged to carry a stretcher patient. Most non-aeromedical aircraft are best used for transport of personnel and equipment freeing up dedicated aeromedical assets for patient transport. 11 6.4. Plan activation procedures This Plan will normally be activated in stages, however, in an impact event, these stages may be condensed with stages being activated concurrently. Stage 1 – Alert: The alert stage is activated when advice of an impending or potential emergency is received or when, following the occurrence of an event, it is unclear as to whether an aeromedical response is needed. During this stage, the situation is monitored to determine the likelihood and nature of the aeromedical response. The following actions are undertaken: On-Call Duty Officer The On-Call Duty Officer (OCDO) will receive notification of an actual or potential incident. The OCDO shall notify the State Health Coordinator (SHC) of the incident and await further instruction. As required, the OCDO may notify the State Health Incident Coordination Centre (SHICC) Coordinator to activate the Aeromedical Transport Planning Cell of preparation/response actions determined by the SHC. The OCDO will contact the relevant Regional Health Disaster Coordinator (RHDC) to inform them of the incident. The RHDC will in turn notify the most local health facility. State Health Coordinator The SHC will receive notification of the incident from the OCDO. The SHC will determine the extent of preparation or response required and authorise the OCDO to commence notification of relevant staff/organisations. As required, the SHC may advise the Director General (Health), Executive Director of Public Health and Western Australia Country Health Service (WACHS), WA SEMC Executive Officer, State Health Executive Forum (SHEF) members and the Public Affairs Department. On-Call Clinical Officer The On-Call Clinical Officer (OCCO) will usually assume the role of the Operations Cell Coordinator in the SHICC. The OCCO will liaise with the Health Commander and/or Regional Health Disaster Coordinator to gather incident information and communicate Incident Response Objectives (IROs) and Incident Action Plans (IAPs). The OCCO will coordinate with St John Ambulance WA (SJA) Liaison Officer and Aeromedical Liaison Officer regarding casualty transport arrangements. NOTE: For a comprehensive description of the OCDO, SHC and OCCO roles, please refer to SHICC SOPS, Annex D, SHICC staff role checklist. Planning Cell 12 A liaison officer from RFDS Western Operations will provide an Aeromedical Liaison Officer to the Planning Cell. A liaison officer from WAPOL Air Wing will provide an Aviation Liaison Officer to the Planning Cell (providing this does not conflict with WAPOL operations). Stage 2 – Standby: The standby stage is activated when information received is sufficient to warrant preparatory activities in readiness for a response. Depending on the situation, the following actions may be undertaken: As required, the OCDO, OCCO and SHICC Coordinator will update the SHC who may inturn update or advise the Director General (Health), Executive Director of Public Health and WACHS, SEMC/SECG, State Health Executive Forum (SHEF) members and the WA Department of Health Public Affairs Department Stage 3 – Response: The response stage is activated when a health emergency management response is required and resources are deployed accordingly. Depending on the situation, the following actions may be undertaken: The State Health Incident Coordination Centre (SHICC) is activated and staffed by pre-designated strategic and operational staff. The appropriate members of the Planning Cell and other support organisations, including the Aeromedical Liaison officer and Aviation Liaison Officer, are advised of the need for the deployment of a health response. Stage 4 – Stand Down: The stand down stage is activated when an aeromedical response is no longer required. Aeromedical services can resume their normal business. The decision to stand down a single or multiple aeromedical services from a mass casualty activation and response shall be made by the State Health Coordinator and may be effected in a graduated manner. This may include the following actions: Participating aeromedical services are informed of “stand down” by the State Health Coordinator as per the activation of the communication cascade. Organisations are stood down in accordance with relevant procedures for each organisation. Organisations are to advise the State Health Coordinator when stand down has been completed. Arrangements for debriefings are advised. 6.5. Notification Notification of personnel involved in the Planning Cell Aeromedical component of SHICC will be the responsibility of the SHICC Coordinator. 13 6.6. Strategies for a health response The location of the incident and number of casualties will determine the type of aeromedical response. In this circumstance it may be necessary to apply one or more of the following strategies. Use a combination of rotary and fixed wing aircraft to move personnel, equipment and casualties. Consider using a rural town as a base for initial triage and treatment (preferably one with medical resources available), then use a combination of turbo prop, jet and rotary wing aircraft to ferry personnel, equipment and casualties to and from the incident site. For example, for an incident in the Indian Ocean Territories, consider using a jet to transfer casualties from the Indian Ocean Territories to Karratha, then use turbo prop aircraft to transfer the casualties from Karratha to Perth. This strategy may also be implemented if crew hours are limited. For an incident in the North East of the state, consider ‘ferry runs’ to and from Darwin to assist with casualty load distribution. Consider using Northern Territory/South Australia assets to conduct routine priority 1 AME work, thereby releasing RFDS Western Operations aircraft to respond to the incident. 6.7. Considerations when planning an aeromedical response Key factors to consider when planning an aeromedical response in WA include: Incident location, including jurisdictional responsibilities. Landing strip location, accessibility, length, width, load capacity and refuelling facilities. Nearest health facility or RFDS Western Operations base. Aircraft availability (aeromedical and non-aeromedical), MOUs, duty time available and current location. Aircraft suitability (jet, turbo prop, rotary, ADF). Aircraft capacity (number of stretchers or sitters. Note that each intubated patient requires a doctor and nurse, in some cases one doctor and two nurses can care for 2 intubated patients). Non aeromedical aircraft may be required to transport large volumes of oxygen, thereby decreasing the passenger carrying capacity. Any plan must take into consideration the restrictions imposed by CASA on pilot operating duty times. Normally this is limited to 8 hours of flying time and 12 hours of duty time. As a general rule, the longer the pilots flying or duty time, the longer the break required before resuming duty. 6.7.1 Location of incident Due to the large flying distances involved in WA and the Indian Ocean Territories, fixed wing or jet aircraft may be the only practical mode of transport. The airstrip capacity at or near the incident site may only be suitable for certain types of aircraft to land. Due to terrain and weather conditions, accessability to the disaster location may be hampered as a result of flooding of the airstrip or the road linking the airstrip to the incident site. 14 6.7.1.1. Any incident in the north of the state requiring an aeromedical response from Perth will require the use of fixed wing aircraft. Considering the use of jet aircraft may be beneficial depending on the location of the incident and flying distances involved. 6.7.1.2. Rotary wing aircraft response Consider rotary wing aircraft use in any incident where there is no facility for a fixed wing aircraft to access the incident site. The use of available rotary wing aircraft can be used to transfer medical personnel and casualties from the incident site to the nearest airstrip where the appropriate personnel can be transferred to a fixed wing aircraft if necessary. 6.7.1.4. Jet aircraft response to Indian Ocean Territories Any incident occuring in the Indian Ocean Territories will require a jet aircraft response due to the distances involved. See appendix 4. Consider that all aircraft, unless using a large jet, will need to refuel on route to the Indian Ocean Territories. This is usually completed in Learmonth. Approximate flight times using aeromedical jet aircraft are: - Perth to Learmonth 1 hour 40 minutes - Learmonth to Christmas Island 2hours 20 minutes - Learmonth to Cocos Island 3 hours Consider the need for crew to clear customs and if this can be fast tracked. Perth Airport Coordination Center may be available on 08 9478 8572 to provide assistance with customs clearance. 6.7.1.3. Fixed wing aircraft response in WA Non-aviation response Consider the use of land vehicles or marine vessels to transfer medical personnel and casualties from the the incident site to a sutiable location where aircraft can land. 6.7.2 MCI exceeding WA aeromedical capability The number of casualties at the incident may overwhelm the aeromedical capabilities in WA. In this circumstance it may be necessary to apply one or more of the following strategies. 6.7.2.1. Surge capacity In the event that aeromedical resources in WA do not meet the demand for the nominated incident, consider the adoption of the following strategies: Activation of interstate bilateral agreements. Request for assistance from the Commonwealth Government. 15 6.7.2.2. Bilateral agreements In the event that aeromedical resources within WA do not meet the demand for the nominated incident, interstate bilateral agreements may require activation. Consider the adoption of these strategies: For an event in the North of the state aeromedical services in the Northern Territory can be contacted to assist in the aeromedical response. For an event in the East of the state aeromedical services in South Australia can be contacted to assist in the aeromedical response. For an event anywhere in the state where WA aeromedical resources require assistance, both aeromedical services in South Australia and the Northern Territory can be contacted to assist in the aeromedical response. 6.7.2.3. Commonwealth request for assistance In the event that an incident excedes the capabilities of a WA and neighbouring jursidictional aeromedical response, or due to the unique location of the incident a specialist aeromedical response is required, consider the adoption of the following strategy: Activation of the The Australian Medical Transport Coordination Group (AMTCG), via the National Incident Room. The AMTCG exists to facilitate the coordination of a national aeromedical response in support of a state response. The AMCTG can request assistance from unaffected States and Territories as necessary to assist in the transfer of casualties across jursidictional or national borders. 6.7.3 Bariatric aeromedical transfers Special consideration is needed regarding the aeromedical transfer of bariatric patients. Due to the weight restrictions imposed on aeromedical equipment and accessibility to the aircraft cabin, some bariatric patients may not be able to be transferred by regular aeromedical services. RFDS Western Operations aircraft can transfer a patient with a maximum weight of 200 kilogrammes using a specialist bariatric mat. The RFDS are developing a bariatric transport system which can be retrofitted to turboprop aircraft for patients up to 300kg. Only one patient can be carried with two critical care staff. These are likely to be deployed at Derby, Port Hedland and in Perth by May 2014. The Department of Fire and Emergency Service (DFES) RAC rescue helicopter can transfer a patient with a maximum weight of 154 kilogrammes. Aeromedical jet aircraft may be unable to transfer bariatric patients due to the size of the door frame. Consider the option that some Lear Jet aircraft with larger door frames may be able to transfer bariatric patients. ADF aircraft (rotary or fixed wing) may be able to assist in the transfer of bariatric patients. A request for assistance is to be made via the ADF AME Duty Coordinator. Consider the need for additional medical equipment such as oxygen and additional batteries if transferring casualties by non aeromedical ADF assetts. 16 Consider the use of the two St John Ambulance (WA) bariatric ambulance(s) that is stationed in Perth. This vehicle has the capacity to transport a patient with a maximum weight of 500 kilogrammes. 6.8. Immediate response actions Upon activation of the SHICC the Planning Cell is responsible for gathering, interpreting and disseminating intelligence and the preparation of aeromedical evacuation plans. Due to the logistics involved in any aeromedical response the early notification of aeromedical operators is essential. An early situation report to aeromedical operators will determine availiability of assets so alternative plans can be formulated and assist in a prompt response if requested. 6.9. Command and control The State Health Coordinator (SHC) has the authority to command the coordinated use of all health resources within WA, for response and recovery from, the impacts and effects of a major emergency or disaster situation. The Royal Flying Doctor Service (RFDS) – Western Operations branch will coordinate mass casualty aeromedical transport of casualties, including non-RFDS assets, in close consultation with the SHC and the State Health Incident Coordination Centre (SHICC). The Western Australia Police Air Wing is responsible for the coordination of all nonAeromedical (AME) resources. When this plan is activated, RFDS and WA Police Air Wing will deploy liaison officers to the SHICC to assist with the coordination of Mass Casualty AME movements. 6.10. Coordination 6.10.1 State Health Incident Coordination Centre In the context of a Mass Casualty Incident, the SHICC is the focal point of strategic decision-making, operational coordination and communications for Health. Areas, roles or departments that may liaise with the SHICC include: State Health Coordinator Health Commander Regional Health Disaster Coordinators RoyalFlying Doctor Service St John Ambulance (SJA) Department of Health officials External agencies Director General for Health Minister for Health Emergency Services National, Interstate and international agencies 17 State Trauma or State Burns Directors The primary objective of the SHICC is to coordinate the WA Health System response when an incident either decreases Health service availability or increases patient load against existing service provision. 6.10.2 Planning cell 6.10.2.1. Aviation Planning Officer The role of the Aviation Planning Officer is assumed by a member of DPMU staff and draws upon the expertise of the aeromedical liaison officer and aviation liaison officer to enable SHICC to plan for a suitable aeromedical response as requested by the State Health Coordinator. See appendix 5. 6.10.2.2. Aeromedical Liaison Officer The role of the Aeromedical Liaison Officer is assumed by a clinical coordinator from RFDS and provides expert advice to the Aviation Planning officer in coordinating of all aeromedical resources in the event of a mass casualty incident requiring the use of aeromedical services. The Aeromedical Liaison Officer is to be located at the SHICC when requested. Upon activation of the AMTCG, the Aeromedical Liasion Officer will be the nominated Aeromedical Coordinator for the state and should be available for meetings every 3 hours during critical phases of activation. See appendix 6. 6.10.2.3. Aviation Liaison Officer The role of the Aviation Liaison Officer is assumed by a member of the WA Police Air Wing and provides expert advice to the Aviation Planning Officer in the coordination of all non aeromedical aviation resources in the event of a mass casualty incident. This role includes but is not limited to sourcing none aeromedical aircraft to transport personnel to the incident site and procure additional non aeromedical aircraft as needed for the success of the operation. The Aviation Liaison Officer is located at the SHICC when requested. See appendix 7. 18 On Call Duty Officer State Health Coordinator On Call Duty Officer SHICC Coordinator Assistant to the SHC Principal Media Coordinator Assistant to the SHICC Coordinator SJA Liaison Officer WACHS Liaison Officer WAPOL Liaison Officer FESA Liaison Officer Health Liaison Officer to WAPol Health Liaison Officer to FESA Deployed Officers Operations Cell Coordinator Planning Cell Coordinator Functions: Casualty Allocation Casualty Allocation Registry Casualty Registry Hospital Operations Liaison Hospital Service Continuity Incident Site Liaison Metropolitan Bed Management Operations Cell Assistant Team Deployment Transport Liaisons Functions: Agency Liaison Data Expert Advisors External Communications GIS Planning / Intelligence Planning Cell Assistant Planning Log Review Administration Cell Coordinator Logistics Cell Coordinator Functions: Biomedical Engineering Deployable Team Resources Health Service Resources Logistic Cell Assistant Procurement Security Warehousing Functions: Administration Cell Assistant Administrative Services Finance Human Resources ICT Safety Officer SHICC Setup Switchboard WebEOC Aviation - Aviation Officer - RFDS Liaison Officer - WA Police Air Wing Liaison Operations Cell Officers Planning Cell Officers Logistics Cell Officers Administration Cell Officers Operations Cell Planning Cell Logistics Cell Administration Cell Figure 1 State Health Emergency Command and Control 6.10.3 RFDS Western Operations Coordination Centre Upon activation of the WA Mass Casualty Aeromedical Transport Plan 2010, the RFDS Western Operations Coordination Centre shall coordinate all aeromedical assets involved in the mass casualty incident. In addition to their normal duties the RFDS Western Operations Coordination Centre shall coordinate all WA aeromedical services involved in a mass casualty incident. Additional services and personnel that will liaise with the RFDS Western Operations Coordination Centre in the event of a mass casualty incident include: Aeromedical Liaison Officer WA Aeromedical service aircraft activated by the WA Mass Casualty Aeromedical Transport Plan 2011 The primary objective of the RFDS Western Operations Coordination Centre is to coordinate a state-wide aeromedical response. This involves the coordination of all WA aeromedical assets used in a mass casualty incident. 6.11. Health response actions On receipt of advice that an incident has occurred, the State Health Coordinator will liaise with the WA Police Air Wing Duty Officer and the Incident Controller and determine: 19 a. b. c. d. e. f. g. Designated Level of Response i.e. Level 1, 2 or 3 incident; Location of incident; Number and status of casualties; Determine the nearest suitable airstrip; Determine the distance between the nearest suitable airstrip and the incident site; Determine the nearest available fuel – including quantity; Determine the most appropriate aviation response, taking into account all aviation resources available; h. Liaise with RFDS Operations to delegate the coordination of aeromedical response in conjunction with the Incident Controller and Incident Management team; i. Activate the SHICC and request that Liaison Officers from WA Police Air Wing and RFDS attend the SHICC. j. Consider the activation of Hospital Response Teams and / or AUSMAT medical teams (including medical equipment) as early as possible. k. In consultation with aviation planners, consider where the medical hub could be for patients to be evacuated to. This could be a regional centre or at least an area where commercial aircraft could land (refer to appendix 12). 6.12. Communications The primary point of contact for any event that will involve the aeromedical transfer of multiple casualties is the On Call Duty Officer (OCDO) on 08 9328 0553. When the SHICC is activated the primary contact number is 08 9222 4444. The main contact in the SHICC is the Aviation Planning Officer located in the Planning Cell who can be contacted on the above number. 6.13. Financial arrangements for response Detailed information in relation to the financial responsibilities of participating organisations is outlined in SEMP 4.2 – Funding for Emergencies. The authority to engage and task any aviation provider is to be obtained from the State Health Coordinator prior to engagement and tasking by RFDS Western Operations or WA Police Air Wing coordinating non-aeromedical assets on behalf of WA Health. The State Health coordinator should be advised of the approximate cost of engaging a provider prior to authority for tasking being sought. Agencies are advised to track their individual costs incurred during the response phase of a mass casualty event. 7. Recovery 7.1. Responsibility for Recovery Recovery management is the coordinated process of supporting “emergency affected communities in the reconstruction and restoration of physical infrastructure, the environment and community, psychosocial, and economic wellbeing”. (Emergency Management Act 2005) 20 Local government are responsible for the coordination of community recovery at a local level. Where recovery activities are beyond the capacity of the local community, State support may be provided through the State Recovery Coordinator as detailed in the State Recovery Plan [WESTPLAN –Recovery Coordination]. 7.2. Stand Down and Post-Operations Report The SHC will determine when stand-down of this subplan will occur and ensure that all agencies involved in the response conduct debriefs with their staff. The SHC will ensure that operational debriefing is conducted for all Health staff and other personnel involved in the response. The SHC will ensure that all agencies involved in the response event complete a postoperations report, and enable staff to have the opportunity to contribute information to the post-operations report. Post Operation Reports shall be provided to SEMC in accordance with SEMC Policy Number 4.3. 8. Acknowledgements The DPMU would like to acknowledge the following agencies in the development of this plan: WA Police Air Wing Royal Flying Doctor Service – Western Australian operations section All aeromedical and non-aeromedical providers mentioned in this plan. 21 Appendix 1: Contact list – aeromedical operators ORGANISATION ADDRESS CONTACT NUMBER BUSINESS HOURS CONTACT NUMBER AFTER HOURS (08) 9334 1226 (08) 9334 1226 (24/7) Jandakot Airport WA RAC Rescue Helicopter Aspen Medical Australia BHP Billiton Iron Ore Air Ambulance – Port Hedland Care Flight – Northern Operations Care Flight – International MedSTAR Suite 17C 2 King Street 1800 599 339 1800 599 339 Deakin, ACT 2600 Polar Aviation Hanger Port Hedland Airport 6 Fenton Court, Waton, NT 0820 0458 111 659 or 0477 310 256 or 0458 111 659 0400 700 944 TITLE WA Health Manager State Contract Ambulance Operations Pending Project Manager No (08) 8928 9777 (08) 8944 8007 (24/7) Pending Logistics Coordinator Cnr Redbank Rd & Barden St Northmead, NSW 2152 (02) 9893 7683 1300 655 855 (24/7) Pending Coordinator 16 James Schofield Drive Adelaide Airport, SA 5950 (08) 8154 4201 Pending Emergency Operations Coordinator 13 78 27 (24/7) RFDS Western 3 Eagle Drive Operations Jandakot, WA 6164 RFDS Central 71 Henley Beach Operations Road Mile End, SA 5031 RAAF Pearce MOU Gt Northern Highway, Bullsbrook, WA 6084 Coordination WACHS Centre Health (Clinical & Contract Operations Coordination Staff) (9417 6364) (9417 6364) (08) 8648 9555 08 8648 9555 (08) 9571 7120 0408 427 195 DACC Pearce SARO (Defence (Search and Assistance Rescue to the Civil Officer) Community) Pending 22 Appendix 2: Contact list – non-aeromedical operators ORGANISATION ADDRESS Air North 4 Lancaster Rd, Marrara, NT 0812 Bristow Helicopters 130 Fauntleroy Australia Avenue Redcliffe, WA 6104 CHC Helicopters Australia 1060 Hay St West Perth, WA 6005 Cobham 3 Valentine Road, Perth Domestic Airport, WA, 6104 CONTACT NUMBER BUSINESS HOURS CONTACT NUMBER AFTER HOURS MOU (08) 8920 4000 1800 779677 or 0439 234056 Pending (08) 9478 3388 08 9478 3388 NO (08) 9480 0695 0400 868 246 Pending (08) 9479 9700 (08) 9479 9712 Pending (08) 9478 3850 0400 600 Pending TITLE Maroomba Airlines Fauntleroy Avenue, Perth Airport, WA 6105, Australia 193 QANTAS Skippers N/A N/A Valentine Road, Redcliffe, WA 6105 (08) 9478 3989 0407 724 416 (24/7) (Conact via WAPOL police incident control centre) NO Activation Duty Officer 0417 988 562 Pending 23 Appendix 3: Contact list – key agencies ORGANISATION ADDRESS CONTACT NUMBER BUSINESS HOURS CONTACT NUMBER AFTER HOURS Canberra (02) 6128 4869 0420 979 164 Canberra (02) 6128 4333 (02) 6128 4333 Australian Maritime Safety Authority (AMSA) 82 Northbourne Avenue, Braddon, ACT 2612 (02) 6279 5000 1800 815 257 Northern Territory (NT) Health 87 Mitchell Street, Darwin, NT 0800 (08) 8999 2400 (08) 8999 2400 (08) 8226 6000 (08) 8226 6000 (08(0() 9225 (08) 9225 4104 (08) 9334 1226 (08) 9334 1226 (08) 9411 7222 0407 724 416 Northern Command HQ Darwin ADF AME Duty Coordinator ADF Joint Operations Coordination Centre (JOCC) South Australia (SA) Health Citi Centre Building 11 Hindmarsh Square Adelaide South Australia 5000 State Emergency Maylands Police Management Committee Complex, (SEMC) – Executive Officer 2 Swan Bank Road, Maylands RFDS Western Operations 3 Eagle Drive Jandakot, WA 6164 SJA (WA) Operations 209 Great Eastern Highway Belmont WA 6104 Western Australia Police Air 18 Compass Road Wing Jandakot, WA 6164 24 Appendix 4: Indian Ocean Territories aeromedical response RFDS–1xJet = 2xstretchers & 3xseated & 2 health staff OR 2xICU & 4 health staff with44cccrewcrew WA Aeromedical ASPEN–1xJet = 1xstretcher & 1xseated & 2 health staff OR 1xICU & 2 health staff Jet Capability CARE FLIGHT–1x Jet based in Darwin = 1xstretcher & 3xseated & 2 health staff OR 1xICU & 2 health staff Are these aircraft available? NO Activate BILATERAL AGREEMENTS YES Does the number of casualties exceed the capability of WA operators? YES SA – MedSTAR Potentially 3 x Jets available but not always based in Adelaide NO Use WA assets NT – CARE FLIGHT YES 1 x Jet based in Darwin Are these aircraft available? NO Does the number of casualties exceed the capability of WA and bilateral aeromedical operators? YES Request COMMONWEALTH ASSISTANCE / AMTCG activation NO Consider using ADF Use SA and NT assets 24 Appendix 5: Master action card 1: Aviation Planning Officer The Aviation Planning Officer is the WA Health contact in the SHICC for any matters relating to aeromedical evacuation and aviation generally. Initial duties 1. If applicable, receive hand over from On Call Clinical Officer (OCCO)/On Call Duty Officer (OCDO) on any aeromedical activities already commenced 2. Advice the SHIC coordinator of the need to request Liaison Officers from RFDS and WA Police Air Wing to attend the SHICC. 3. Login to WebEOC as the Aviation Planning Officer 4. Familiarise the Aeromedical Liaison Officer and Aviation Liaison Officer with the SHICC systems and procedures 5. In collaboration with the Aeromedical Liaison Officer and Aviation Liaison Officer, commence contacting organisations and establish the following: availability of Aircraft/Configuration of Aircraft availability and configuration of Medical Teams estimated times – ready to depart and flight time to the incident area Ongoing duties 1. Coordinate the reporting of aeromedical and aviation information to the Planning Cell Coordinator, and to the SHICC Executive Group (SEG) 2. Review current Memoranda of Understanding (MOU) and quotes in collaboration with the aeromedical and aviation services prior to tasking to determine the most suitable operator regarding operational requirements and costing 3. Assist the Aeromedical Liaison Officer and Aviation Liaison Officer with any problems pertaining to the SHICC systems and procedure 4. Act as a liaison between aeromedical and aviation experts and the SEG 5. Other duties as directed by Planning Cell Coordinator 25 Appendix 6: Master action card 2: Aeromedical Liaison Officer (RFDS Western Operations) The Aero Medical Liaison Officer coordinates all aeromedical resources in the event of a mass casualty incident. Ongoing duties 1. Provide information and advice on the most appropriate methods for procuring aeromedical assets to assist in the aeromedical response to a mass casualty incident 2. Coordinate all aeromedical assets in the event of a disaster involving mass casualties 3. In collaboration with the RFDS Western Operations Coordination Centre, determine the most appropriate method of transferring casualties using aeromedical assets 4. As requested by the State Health Coordinator (SHC) or the SHICC coordinator, act as the Aeromedical Evacuation Coordinator representing WA Health at the Australian Medical Transport Coordination Group 5. Review the current Memoranda of Understanding (MOU) with the aeromedical service providers prior to tasking, and determine the most suitable operator regarding operational requirements and costing 26 Appendix 7: Master action card 3: Aviation Liaison Officer (WA Police Air Wing) The Aviation Liaison Officer coordinates all aviation resources (non aeromedical) in the event of a mass casualty incident. Ongoing duties 1. Provide information and advice on the most appropriate methods for procuring non aeromedical aviation assets to assist in the aeromedical response to a mass casualty incident 2. Coordinate all aviation (non aeromedical) assets in the event of a deployment 3. Liaise closely with the Logistics Cell to coordinate movement of resources 4. Procure aviation assets to transfer health personnel and/or other emergency services staff and equipment to the incident site as directed 5. Act as a liaison between WAPOL officers at the airstrip/landing site and the Aero Medical Evacuation Planning Officer 6. Provide expert knowledge and obtain aviation information necessary for the response 7. Review the current Memoranda of Understanding (MOU) with the aviation services prior to tasking, and determine the most suitable operator regarding operational requirements and costing 27 Appendix 8: Aeromedical assets in WA Aeromedical Service Rotary Wing Aircraft Turbo Prop Aircraft Jet Aircraft RFDS Western Operations 0 13 1 Capacity Turbo prop Seated 1 AND Stretcher 2 Jet Seated 3 AND Stretcher 2 AND 2 Health Staff Seated Aspen 0 0 1 1 AND Stretcher 1 AND 2 Health Staff Seated State Emergency Rescue Helicopter BHP Aeromedical Helicopter 1 1 0 0 0 0 OR Stretcher 1 Seated 2 OR Stretcher TOTALS 2 13 2 1 2 28 Appendix 9: Neighbouring interstate aeromedical assets Aeromedical Service Careflight International Darwin Rotary Wing Aircraft Turbo Prop Aircraft Jet Aircraft Capacity Seated 0 0 1 3 AND Stretcher 1 AND 2 Health Staff Careflight – Northern Operations (NT) 2 4 0 Seated AND Stretcher MedSTAR – South Australia 3 0 0 RFDS Central Operations 0 11 0 2 TBC Seated 1 AND Stretcher TOTALS 1 5 15 2 1 29 Appendix 10: WA non-aeromedical assets Air Service Rotary Wing Aircraft Turbo Prop Aircraft Jet Aircraft Capacity Bristow HelicoptersAustralia 23 (number changes due to relocation and servicing of aircraft) 0 0 TBD CHC Helicopters (Australia) 3 0 0 TBD Cobham (National Jet) 0 2 20 TBD 0 23 0 TBD 0 4 1 Skippers TBD Maroomba TBD Airnorth 0 8 3 WAPOL 2 2 0 Seated 1 AND Stretcher TOTALS 28 39 1 24 30 Appendix 11: Medical cache assets a) SJA (WA) Mass casualty kit and disaster management oxygen equipment Location Comments/Status Neann Multi-Casualty Oxygen Kit Metropolitan Central Career version Yes Fremantle Career version Yes Gosnells Career version Yes Jandakot Career version Yes Joondalup Career version Yes Midland Career version Yes Morley Career version Yes Osborne Park Career version Yes Rockingham Career version Yes Two Rocks Career version Yes Albany Career version Yes Broome Career version Yes Bunbury Career version Yes Busselton Career version Yes Collie Career version Yes Geraldton Career version Yes Kalgoorlie x 3 Career version Yes (3) Kununurra Career version Yes Mandurah Career version Yes Norseman Career version Yes Northam Career version Yes Pinjara Career version Yes Port Hedland Career version Yes Serpentine Career version Yes Belmont Spare Belmont Spare Career Country 31 Location Comments/Status Neann Multi-Casualty Oxygen Kit Volunteer Country Bridgetown Volunteer version No Canarvon Volunteer version No Cue Volunteer version No Cunderdin Volunteer version No Dalwallinu Volunteer version No Denmark Volunteer version No Dunsborough Volunteer version No Esperance Volunteer version No Eucla Volunteer version No Exmouth Volunteer version Yes Harvey Volunteer version No Jurien Volunteer version No Karratha Volunteer version Yes Kojonup Volunteer version No Lake Grace Volunteer version No Leinster Volunteer version No Manjimup Volunteer version No Moora Volunteer version No Narrogin Volunteer version No Newman Volunteer version No Sandstone Volunteer version No Shark Bay/Denham Volunteer version No Southern Cross Volunteer version No NOTE: The contents of each SJA (WA) Mass Casualty Kits are able to treat approximately 20 casualties. 32 Dimensions and Weights – SJA Mass Casualty Kits Tub Dimensions Career Version Volunteer Version Weight Weight Admin Tub 645cm x 413cm x 276cm 18kg 18kg Burns Tub 645cm x 413cm x 276cm 11kg 11kg Water 2 x 10l containers 24kg (filled) 24kg (filled) Cannulation / IV Fluid Tub 645cm x 413cm x 276cm 16kg 18kg Oxygen Tub 645cm x 413cm x 276cm 10kg 8kg Mass Cas Neann Kit Trauma Tub 6.7kg 645cm x 413cm x 276cm 10kg 10kg 14.5kg 14.5kg 103.5kg 110.2kg Stretcher Pack TOTAL b) Health facilities with disaster response kits Health Facilities with two kits – Perth Royal Perth Hospital Fremantle Hospital Princess Margaret Hospital Joondalup Health Campus Sir Charles Gairdner Hospital Health facilities with two kits – country Albany Hospital Kalgoorlie Hospital South West Health Campus (Bunbury) Geraldton Hospital Broome Health Service Port Hedland Hospital Health facilities with one kit - Perth Armadale Health Service Rottnest Island Nursing Post Peel Health Campus Rockingham-Kwinana Hospital St John of God Hospital Murdoch Swan District Hospital 33 Health facilities with one kit - country Busselton Hospital Nickol Bay Hospital Northam Hospital Esperance Hospital Kununurra Hospital Warren District Hospital Merredin Hospital Moora Hospital Narrogin Hospital Collie Hospital Carnarvon Hospital Newman Hospital Derby Health Service Meekathara Hospital Morawa - Perenjori Health Service Katanning Hospital Margaret River Hospital Ravensthorpe Hospital Exmouth Hospital Tom Price Hospital Halls Creek Health Service Fitzroy Valley Health Service Learmonth Airport Dimensions and weights – health service disaster response kits Bag Dimensions Weight Airway 35cm x 35cm x 21cm 4.5kg Breathing 64cm x 46cm x 23cm 7.0kg Circulation 62cm x 51cm x 22cm 7.0kg Pharmaceutical 30cm x 36cm x 16cm 2.7kg Comfort 52cm x 37cm x 18cm 4.5kg TOTAL 25.7kg Note in addition to the above, each team member will carry a personal “bum bag” Personal 19cm x 33cm x 15cm 2.0kg 34 Appendix 12: Locations of designated airfields for each type of QANTAS commercial aircraft for WA AIRCRAFT MAIN A380 PERTH ALTERNATE ADEQUATE EMERGENCY LEARMONTH BROOME PEARCE Max 450 passengers A330 PERTH Max 299 passengers PORT HEDLAND KALGOORLIE B767 PERTH Max 254 passengers LEARMONTH BROOME PORT HEDLAND PEARCE CURTIN KALGOORLIE B733/734 Max 150 passengers PERTH ALBANY ARGYLE BROOME GERALDTON PEARCE PORT HEDLAND MEEKATHARRA KARRATHA PARABURDOO NEWMAN LEARMONTH KALGOORLIE CURTN CANARVON KUNNUNURRA B737 800 Max 168 passengers PERTH GERALDTON ARGYLE PARABURDOO BROOME LEARMONTH CURTIN MEEKATHARRA PORT HEDLAND KUNNUNURRA PEARCE KARRATHA NEWMAN KALGOORLIE 35 This document can be made available in alternative formats on request for a person with a disability. © Department of Health 2014 2012