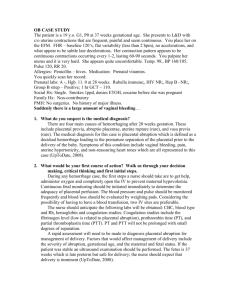
OB CASE STUDY
advertisement

OB CASE STUDY The patient is a 19 y.o. G1, P0 at 37 weeks gestational age. She presents to L&D with c/o uterine contractions that are frequent, painful and seem continuous. You place her on the EFM. FHR – baseline 120’s, flat variability (less than 2 bpm), no accelerations, and what appear to be subtle late decelerations. Her contraction pattern appears to be continuous contractions occurring every 1-2, lasting 60-90 seconds. You palpate her uterus and it is very hard. She appears quite uncomfortable. Temp. 98., BP 160/105, Pulse 120, RR 20. Allergies: Penicillin – hives. Medication: Prenatal vitamins. You quickly scan her record: Prenatal labs: A -, Hgb. 11. 0 at 28 weeks. Rubella immune;, HIV NR;, Hep B –NR;, Group B strep – Positive; 1 hr GCT – 110. Social Hx: Single. Smokes 1ppd, denies ETOH, cocaine before she was pregnant Family Hx: Non-contributory PMH: No surgeries. No history of major illness.. Suddenly there is a large amount of vaginal bleeding… 1. What do you suspect is the medical diagnosis? Placental abruption secondary to preeclampsia or cocaine use. 2. What would be your first course of action? Walk us through your decision making, critical thinking and first initial steps. Notify provider of situation. The provider will come and assess the pt. They may do a vaginal exam to see if a vaginal birth is eminent. Position pt on her left side, give oxygen, maintaining optimal perfusion to the baby. Prepare for a cesarean birth if vaginal birth is not imminent. The FHTs are flat and show that baby is not getting perfused effectively and is losing the ability to compensate. Furthermore, there are late decels which are an ominous sign.The mother’s vital signs are also not stable and need to be assessed by the care provider. These two things lead me to be believe that a cesarean birth is needed. A large amount of vaginal bleeding does not give an accurate idea of the degree of placental abruption. Place two large bore IVs, in preparation for surgery and the possible need for transfusion due to hemorrhage secondary to the poor ability of the uterus to contract after birth. Draw labs, ABO cross match, preeclampsia labs and OB panel. Have matching units of blood on hand in case a transfusion is needed. Insert a Foley catheter, collect urine for UA for protein and urine tox screen. Take history of present illness, noting s/s of preeclampsia (RUQ pain, blurred vision, HA, brisk reflexes, facial or generalized edema) or recent use of cocaine. Give bicitra, prep abdomen (if applicable), and take to OR. 3. What is the pathophysiology of this condition? Placental abruption is the abnormal premature separation of the placenta from the uterine wall that can be caused by trauma, hypertension, and coagulopathy. However, most often the cause of placental abruption is unknown. These factors precipitate the avolution of the anchoring placental villi from the lower uterine segment. Bleeding from this separation fills the decidual basalis and the uterus. Women present with bright red vaginal bleeding , abdominal or back pain, and a large and tense uterus that does not relax between contractions, abnormal premature contractions and fetal distress. The situation is a medical emergency as the associated perinatal mortality rate is 12%. In cases in which the placenta is nearly completely separated from the uterus the infant mortality rate is 100%. 4. What would you anticipate the medical orders to be? Stat cesarean birth IV bolus infusion of NS. Labs Foley Catheter Continuous EFM Oxygen NPO Rhogam Possibly a blood transfusion, have four units cross matched and ready. 5. What medications might be used? Bicitra Rhogam Possibly antibiotics for GBS positive status based on GBS sensitivity tests (this is less of a priority if cesarean birth is ordered). If no sensitivity tests are available, follow CDC guidelines for antibiotics to be used for GBS for a pt with penicillin allergy. Magnesium sulfate postpartum (?)