project management structure
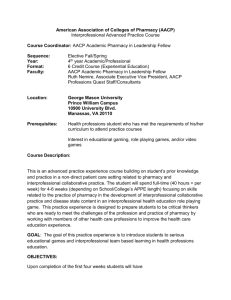
advertisement
Appendix D: Project Summary Project Title: Creating Interprofessional Collaborative Teams For Comprehensive Mental Health Services 1. Mandate of the primary applicant organization: UWO is a centre of learning with more than 60 different degree and diploma programs. Research is an integral part of the University’s mission and external support for research projects totals approximately $141.5 million per year. 2. List of partners with whom the organization will work on this project and their roles: a) Schulich School of Medicine & Dentistry (includes psychiatry), Faculty of Health Sciences, School of Social Work, and the Department of Psychology. Roles: To develop curriculum; to help students learn core concepts relating to patient-centred collaborative interprofessional (IP) teamwork through simulation and practice opportunities b) Consortium of Applied Research and Evaluation in Mental Health (CAREMH), Community University Research Alliance (CURA) on Housing and Mental Health, and Victorian Order of Nurses (VON): To guide the steering committee; to mentor and educate students and to provide community practice opportunities for student teams. 3. Objectives of the project: 1) Socialize health care faculty, students, and practitioners in client-centred IP collaborative practice, specifically focussing on comprehensive mental health services to a vulnerable population; 2) Stimulate networking and sharing of best educational approaches for collaborative client-centred practice; 3) Increase the number of educators prepared to teach from an IP collaborative client-centred perspective; 4) Increase the number of health professionals trained for collaborative client-centred practice before and after entry into practice. Longer-term goals: 5) Facilitate IP collaborative care in both education and practice settings 6) Augment the work toward provincial priorities, including: mental health care reform; care of the homeless; and development of Local Health Integration Networks (LIHNs). 4. Major activities required to achieve these objectives: 1) Half-day retreat for student leaders, community partners, consumers and faculty members 2) Development and teaching of core concepts of IP within own disciplines 3) Workshops and simulation exercises for students; online modules for self-directed problem- based learning 4) Team collaboration in community settings 5) Evaluation at different phases involving micro (at each phase) and macro approaches. 5. Expected results of the project: Creation of sustainable infrastructure and curriculum to support IP education at UWO to influence successful IP education and practice through training faculty, students and community partners. 6. Methods that will be used to evaluate both the process and the outcomes of the project: Focus groups, various assessment tools, scales and surveys. 7. List of the project deliverables with timelines: i) Increase in the number of educators prepared to teach from an IP collaborative client-centred perspective; ii) Increase the number of health professionals trained for collaborative client-centred practice before, and after entry into practice (end of project term); ( iii) Development of tools (curriculum and methods) to facilitate inter-professional collaborative care in both education and practice settings (throughout the project); iv) Evaluation of implementation and short-term outcomes (throughout the project). 8. Dissemination plan: a) To the public: Communication through UWO Communications staff; columns in regional and local newspapers and the Internet. b) To administrators and Boards of Health: web-pages linked to key sources such as Health Canada; print newsletters from CIPHER (The title of Consortium for Interprofessional Health Education and Research is being considered); conferences; booths at health fairs c) To researchers, professors and practitioners: Papers and posters at local, regional and national conferences, through project team network. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 1 6.1 PRIMARY APPLICANT ORGANIZATION The University of Western Ontario (UWO) is a vibrant centre of learning with 1,164 faculty members and almost 29,000 undergraduate and graduate students. Through its 12 Faculties and Schools, and three affiliated Colleges, the University offers more than 60 different degree and diploma programs. UWO has demonstrated ability in introducing and successfully running innovative programs: the Scholar’s program, an undergraduate interdisciplinary educational program for exceptional students; and the Transdisciplinary Understanding and Training on Research Primary Health Care (TUTOR-PHC) -- a Canadian Institutes of Health Research (CIHR) funded national program in training in primary health care research to meet the immediate need for research capacity in this field, are two examples. TUTOR's objectives are to build a critical mass of skilled, independent researchers through student opportunities and faculty (supervisor) development and to increase the interdisciplinary and transdisciplinary focus in primary health care research. The trainees include mid-career clinicians (family physicians, psychologists, nurses and social workers returning to/beginning a research career), post-doctoral fellows and graduate students in family medicine, nursing, psychology, social work, epidemiology and sociology. Project team members, Drs. Carol McWilliam (Nursing), Evelyn Vingilis (Family Medicine and Epidemiology and Biostatistics), and Graham Reid (Psychology) are mentors and educators with this program. This is not unusual. A number of UWO faculty members have cross-appointments in two or more disciplines and many also work collaboratively on research projects. UWO has excellent teaching facilities that incorporate state of the art technological design to help simulation and learning to prepare students for real practice settings. For example, the medical school has a multimedia facility that provides self instructional resources. A new clinical skills facility opened in January 2005 with 16 offices and small group meeting rooms with 2 way mirrors and videotaping capabilities. These facilities will be used in this project to encourage self-directed team based learning. The new home for the Faculty of Health Sciences, the South Valley Building, also contains a Clinical Education Suite that has meeting rooms suitable for the small group team learning activities. Research is an integral part of the University’s mission, and external support for research projects totals approximately $141.5 million per year. UWO has a reputation for leadership in patient-centred and community-oriented medical education and for innovation and excellence in research. UWO also has a strong track record in community based mental health care and research. One of the assets in this community is the existence of a Community-University Research Alliance (CURA) on Housing and Mental Health, which is funded through SSHRC and is in its fourth year of five year funding. This CURA came together as an initiative from community organizations in London, Ontario, to build the capacity of the community to create, support, and evaluate housing for psychiatric consumers/survivors. The combination of excellence in teaching, research, facilities, collaborative working arrangements and proven capabilities in administering interdisciplinary research and teaching, demonstrate UWO’s capacity to capably deliver interprofessional education for collaborative practice. This, coupled with the project team’s strong network of community partners who are willing to mentor and offer practice opportunities for students in mental health services – an area that offers plenty of opportunity for interprofessional client-centred collaborative practice for student teams comprising medical, nursing, psychology, social work, occupational and physical therapy disciplines – is a great combination which will help build the evidence for IECPCP. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 2 6.2 PARTNER ORGANIZATIONS The Schulich School of Medicine and Dentistry (SSoMD) was founded in 1912 and currently enjoys a world class reputation for its teaching and research. Its mission is to be internationally recognized for: leadership in patient-centred and community-oriented medical and dental education and for innovation and excellence in research. The SSoMD offers professional degrees in dentistry, undergraduate and postgraduate MD degrees, including psychiatry. The academic and clinical enterprise for the Department of Psychiatry spans early childhood to geriatrics, comprises acute care and psychosocial rehabilitation, general psychiatry and specialty care and is a resource for the Southwestern Ontario Region (particularly for specialized care). In addition to outstanding teaching and research, the SSoMD offers state of the art teaching and research facilities, to be discussed later. As partner in this project, faculty members from the SSoMD will serve on the Steering Committee and work with other partners in this project to develop curriculum and to train and mentor students. The SSoMD has committed to providing financial resources to ensure sustainability of this project (see budget note in Appendix A) The Faculty of Health Sciences comprises five Schools - Communication Sciences & Disorders (CSD), Kinesiology, Nursing, Occupational Therapy (OT) and Physical Therapy (PT), and two multidisciplinary degree programs - the undergraduate Bachelor of Health Sciences (BHSc) and the Doctoral Program in Rehabilitation Sciences. The Schools of Nursing, OT and PT will be involved in this project. All three have outstanding national teaching reputations. The Faculty’s graduate and graduate professional programs are among the most research-intensive in Canada. While quality and tradition are an integral part of the Faculty, innovation and change are also key to maintaining its place at the forefront of health sciences education. The Schools of Occupational and Physical Therapy have replaced their post-degree undergraduate professional programs with Master of Science (MSc[OT]) and Master of Physical Therapy (MPT) degrees respectively, and the School of Nursing has combined with London's Fanshawe College to introduce the Western-Fanshawe Collaborative Bachelor of Science in Nursing program. In addition, students in the new Compressed Time-Frame program will be invited to participate. The Faculty’s many Schools, programs, research laboratories, and community clinics dot the UWO campus, with locations in the South Valley Building, the Health Sciences Addition (Nursing), Thames Hall/3M Centre (Kinesiology), and Elborn College (CSD, OT, PT, Rehabilitation Sciences). The new South Valley Building provides state-of-the-art facilities (simulated hospital ward, simulated home care unit and virtual theatre) for collaborative teaching and research. As partner in this project, faculty members from the Faculty of Health Sciences have committed involvement in the Steering Committee, in working together with other partners in this project to develop curriculum, and facilitate the development and guidance, with project staff, for participating students. The Faculty of Health Sciences will also be providing financial resources. Together with the SSoMD, it has committed to providing sustaining funds in support of the project (see budget note in Appendix A). The School of Social Work, located within King’s University College at UWO provides a learning environment characterized by excellence in social work education. Its undergraduate and Masters level programs are directed towards developing and fostering principled and competent professional practitioners who recognize the interrelatedness of human needs, social structures and oppressive conditions in their work with diverse populations. Specific objectives ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 3 of the program include education for Social Work practice with individuals, families, groups and communities, emphasizing the social and organizational contexts of practice. Students are given opportunities to develop practical skills by participating in a variety of practicum settings, under professional supervision, throughout Southwestern Ontario. As a partner in this Interprofessional Collaborative Team, the School of Social Work is committed to involvement in planning, developing conjoint curriculum, as well as opening courses in our undergraduate and graduate program to students from other disciplines, integrating our established community placements, contacts and resources with other faculties while assisting in developing new and innovative local and international practicum opportunities. As well, faculty time will be allocated to allow for active participation in workshops, mentoring students from other fields and engaging in outcome evaluation. The Department of Psychology, in Social Sciences, offers a comprehensive undergraduate program in general psychology and has affiliations with a number of researchers in various hospital and clinical settings. The Graduate Program in Psychology may involve experimentation in the laboratory, observation in a school, agency, or other setting, or clinical internships. Graduate-level training in clinical psychology involves two types of training – a graduate program at UWO in clinical psychology at the PhD level with graduate course work and practica placements, and essentially postgraduate training (internship program for clinical graduate students). As a partner in this project, Faculty and students will participate in workshops, and advise and mentor student teams. Dr. Ian Nicholson, Professor and Director of Psychology Training and Professional Practice Leader at the London Health Sciences Centre (LHSC) will help formalize the support for collaborative teams that is now encouraged, but not structured. The Community University Research Alliance (CURA) on Housing and Mental Health focuses on building capacity and uses a participatory research approach to: evaluate existing models of supported housing; enable information sharing between community and academic partners; give voice to the consumers (residents) of supported housing; and to develop working relationships among partners in the community. This alliance taps into the collaborative resources of four universities and eight community organizations. It seeks to promote understanding of the housing situation for psychiatric survivors on an individual, community, and societal level, and through this work to promote positive change in the quality of life for psychiatric survivors. The academic director of the CURA is Dr. Cheryl Forchuk, School of Nursing, Faculty of Health Science, University of Western Ontario and the community co-directors are Susan Ousley and Betty Edwards of Canvoice. Canvoice is a psychiatric consumer/survivor group. The CURA project operates from a Community Economic Development (CED) model that is supported and guided by a broad-based advisory committee. A community advisory group of major stakeholders (psychiatric consumer/survivors, mental health service-providers, housing providers, policy/decision-makers, income support staff and academics) and subcommittees oversee different aspects of the CURA project. Researchers from various disciplines participate on the CURA: nursing, psychology, social work, geography, law, political sciences, economics, psychiatry, and epidemiology. There are numerous opportunities for students to participate. Both nursing and social work students have participated in the community development aspect of the work as practica. Law students have had pro bono placements assisting with policy issues. Undergraduate and graduate nursing students have had research placements with the project. Medical students have also participated ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 4 through the summer research training program at UWO as well as international research exchange medical students from Spain, Greece, and Germany. Many of these students as well as media studies students participated in the annual conferences. The links between researchers/faculty and community agencies will be extended to create the opportunity for practice settings for multidisciplinary student teams for this project. CURA members will serve on the steering committee, attend workshops and help mentor and guide interdisciplinary student teams working in mental health services for disadvantaged client groups. Dr. Cheryl Forchuk is co-chair of this project. The Consortium of Applied Research and Evaluation in Mental Health (CAREMH), headed by Dr. Evelyn Vingilis, is currently funded from a CIHR Interdisciplinary Capacity Enhancement Team grant. The original purpose of CAREMH was to research psychiatric deinstitutionalization using primarily Southwestern Ontario as a "natural laboratory." To ensure this group’s work would, both – accurately describe and anticipate the impacts of mental health reforms; and be useful to, and used by, potential knowledge users – CAREMH developed strategies to encourage collaboration and knowledge translation among researchers from different disciplinary perspectives, practitioners, administrators and consumer/survivors. CAREMH embraces an interdisciplinary approach and includes the areas and disciplines of correctional services, economics, epidemiology, family medicine, law, nursing, police services, political science, psychology, psychiatry and social work. It includes researchers, service providers, administrators, and policy planners. CAREMH’s role in this project is to guide the experience of interdisciplinary teams in mental health services; to help in planning and curriculum development, and to help students find practice settings through its network of community partners. Dr. Evelyn Vingilis is director of this project. Victorian Order of Nurses (VON): VON Canada is a charity guided by the principals of Primary Health Care and works in partnership with Canadians for a healthier society through leadership in community based care, delivery of innovative, comprehensive health and social services and influence in the development of health and social policy. Since 1995 VON Middlesex Elgin site has been providing charitable nursing to the Salvation Army shelter. Five years ago, two charities – the VON and The Salvation Army – in response to identified needs formed a partnership to work together and involve the community, where possible, to improve the health and social outcomes for the most marginalized of our citizens, those who are homeless and those with mental health problems. The partnership focused on the addition of social, rehabilitation and educational resources to a small medical team of nurses and doctors working with the homeless, many of whom have been diagnosed with one or more significant psychiatric and physical illnesses. This population is growing, its needs are increasing and they need the social and rehabilitation supports on site. VON supports the need for the development of interdisciplinary teams to deliver mental health services and welcomes the opportunity to mentor and guide student teams through practice opportunities. Both VON and the Salvation Army have been active members of the CURA and will participate in workshops and serve on the Steering Committee on this project. 6.3 PATIENTS/CLIENTS & LEARNERS Patients/Clients: Table 1 (below) contains patient/client demographics based on a sample of 300 in London, Ontario. It has been compiled from data collected by the CURA on Housing and Mental Health (Nelson, Hall & Forchuk, 2003). ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 5 Table 1 Comparison of Residents of Different Types of Housing on Demographic Variables Type of Housing Demographic Variables and Psychiatric History Homes for Special Care Shelter Supportive Housing Own apartment/ house Statistic Demographic variables Age 43.1 (12.5) 41.3 (11.7) 41.1 (14.1) 38.6 (13.4) not significant Number of housing moves in past 5 2.2 (4.1) 3.4 (4.5) .8 (1.4) 2.4 (3.0) F (3,279) = 4.4a years χ2 (3) = 19.5a Gender 38 (42%) 54 (66%) 25 (60%) 27 (35%) Men 53 (58%) 28 (34%) 17 (40%) 51 (65%) Women χ2 (6) = 18.5a Marital status 7 (8%) 4 (5%) 1 (2%) 12 (15%) Married/widowed 17 (19%) 21 (26%) 11 (26%) 29 (37%) Separated/divorced 67 (73%) 57 (69%) 30 (72%) 37 (48%) Single/never married χ2 (6) = 30.5a Education 13 (14%) 14 (17%) 13 (30%) 30 (38%) University or college 53 (58%) 60 (73%) 25 (60%) 42 (54%) High school 25 (28%) 8 (10%) 4 (10%) 6 (8%) Elementary school χ2 (6) = 16.5a Employment status 21 (15%) 13 (16%) 13 (31%) 6 (8%) Employed part-time or full79 (85%) 67 (84%) 29 (69%) 72 (92%) time Not employed χ2 (9) = 58.4a Psychiatric history Primary psychiatric diagnosis (self51 (56%) 9 (11%) 20 (48%) 26 (33%) reported) 15 (17%) 40 (49%) 9 (21%) 29 (37%) Schizophrenia 20 (22%) 19 (23%) 13 (31%) 20 (26%) Mood disorder 5 (5%) 14 (17%) 0 (0%) 3 (4%) χ2 (3) = 48.1a Other Unknown 85 (93%) 46 (56%) 40 (95%) 66 (85%) Currently taking psychiatric medication 6 (7%) 36 (44%) 2 (5%) 12 (15%) Yes No a p < .01. Note that for age and number of housing moves, means and standard deviations are reported, while for the categorical variables, frequencies and percentages are reported. First Nations Arabic/West Asian Black/African Ontario N=11,285,550 188,315 (0.017%) 155,645 (0.014%) 411,095 (0.036%) White Multi-Racial Multi-Cultural Other 121,290 (0.011%) CURA N=318 (100%) 17 (5.3%) 2 (0.6%) 5 (1.6%) 249 (78%) 18 (5.7%) 4 (1.3%) 24 (7.5%) Homeless n=132 (100%) 12 (9%) 2 (1.5%) 3 (2.3%) 97 (74%) 7 (5.3%) 2 (1.5%) 9 (6.8%) LEARNERS In this project everyone is a learner – faculty members, students, community agency participants and clients -- in sharing knowledge of professions and disciplines other than one's ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 6 own, in working together and sharing expertise within interprofessional collaborative teams, whether in curriculum development, professional guidance, mentoring of student teams or taking courses. Community agency partners will contribute to the learning in workshops and conferences. Student teams’ learning will be tied to curriculum. All learners will contribute to evaluation and assessment of the learning process from the workshops to the practice settings in surveys or focus group discussions. Collectively, the experiences will help build the evidence for interprofessional education for collaborative practice that is client-centred. Making it work Informal interdisciplinary education will be promoted by publicizing, more widely, department seminars and workshops that are normally publicized only within departments, to encourage participation from other disciplines. Formal interdisciplinary education will be organized through CIPHER (the title of Consortium for Interprofessional Health Education and Research is being considered), where students from the different disciplines will be given the opportunity to take elective courses in interprofessional collaboration, which will include classroom instruction and opportunities to collaborate in interdisciplinary teams in simulated as well as real practice situations in the community. While that can be a challenge, given the differing program structures and curriculum demands, the deans and department heads agree that interprofessional collaboration should be encouraged and have given their commitment to helping make this work. In addition, most faculties currently try to encourage interprofessional collaboration in practica in various ways – this initiative will help formalize the process by enhancing training, tracking and evaluation opportunities. Below is a description of program and time commitments for students in each faculty/school to illustrate how student participation in interprofessional team collaboration could be feasible. We estimate approximately 30 student teams would avail themselves of the opportunity in a year (see also Exhibit # 2: Learning Foci for Interdisciplinary Teams – page 30). Medicine: The undergraduate Medical Program is a four year course with the first two years largely devoted to knowledge skills and attitude development delivered in a combination of lecture, and small group formats. The latter two years are composed of the clinical clerkships, clinical electives and a small return to classroom component. Class size is 133. A course titled "Community Medicine" runs through first and second year of the program and already has a community placement component which would be compatible with the module being proposed in this submission. In psychiatry, both the clerkship rotations and the residency program include added opportunities for interprofessional training and education through the didactic teaching, small group learning and psychiatric team learning. Further support of these themes would occur during the five weeks of Psychiatry and Behavioural Science teaching in Year 2. Psychology: Psychology students have very heavy curriculum demands to meet various stringent professional licensing requirements. Psychology students will be involved in this project via the Internship program (supervised by Dr. Ian Nicholson) and the Graduate program. Both programs are small – with about 6 students each admitted each year. The Internship program students may be from anywhere in America, whereas the Graduate program involves students specifically from UWO. Psychology student involvement in practica would be in settings that are overseen by a licensed supervising psychologist. Nursing: The BScN is offered in three program options: a) a four year undergraduate program offered in a collaborative partnership at two sites (UWO and Fanshawe College), and b) a 19 month compressed time-frame at the UWO site, with an enrollment of 35 students. In a) students are divided between the two sites for the first two years of the program but then merge at the ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 7 UWO site in the 3rd and 4th years. Community nursing and health promotion is offered during the 3rd year. Class size is up to 240. Community-mental health placements with interprofessional teams will be accommodated as an alternate to the traditional nursing aggregate group placements. In b) and c) students can utilize the same placements during the spring semester. Physical Therapy: The Master of Physical Therapy (MPT) is a two-year professional graduate program with 44-48 students in each year. In both years of the program, there is a required course in community-based physical therapy. Students in the second year of the MPT program will participate, with the activities forming an assignment in the Physical Therapy in Community Settings II course. Occupational Therapy: The Master of Science in Occupational Therapy MSc(OT) is a two year program which admits 48 students each year (this will increase to 50 starting next year). During the two years the students undertake 4 clinical placements. In year one, they are on placement in January and then again in either May and June or June and July. In year two they are on placement for January and February and then again in May and June. There are several community based components of the curriculum that would support this initiative. Social Work: Affiliated with the Faculty of Graduate Studies at UWO, the School of Social Work at King’s University College offers a part-time, Advanced Generalist Master of Social Work program for those who already have a Bachelor of Social Work degree, are members of the Ontario College of Social Service and Social Workers and have had formal practice experience. The MSW program is course-based with an advanced practicum which is sequenced over a three year period that permit students to maintain full-time employment; for example, evening classes and compressed courses in the summer term. 20 – 25 students are admitted each year into this program. The School of Social Work has practica in a variety of hospitals, mental health, and community social service agencies that also use other health care disciplines. An opportunity to integrate learning and bring teams together at both the school and the field exists. STEERING COMMITTEE (See Exhibit #4 – page 34) A project Steering Committee will be established at the inception of this project. This committee will be accountable for the planning, implementation, and evaluation of this project. The Steering committee will be composed of the two project co-chairs (Drs. Cheryl Forchuk and Evelyn Vingilis), 7 faculty member representatives from the participating disciplines (nursing, medicine, psychiatry, psychology, occupational therapy, physical therapy and social work), 5 student representatives (one from each participating discipline), 4 mental health community agency representatives (CURA, CAREMH, VON, Salvation Army), and 4 consumer representatives (one representing the CURA, Can-Voice, VON, and Salvation Army). The Deans from the Schulich School of Medicine and Dentistry, Faculty of Health Sciences, and the project coordinator, will be ex-officio. The Steering Committee (See Exhibit #4 for terms of reference, page 34) will have four working groups: a) the Curriculum Working Group; b) the Practice site Working Group; c) the Education Program Development Group; and d) the Evaluation Working Group. These working groups will focus on key component areas of the project and report to the Steering Committee who will in turn provide direction and guidance to their work. The major development work of (a), (b), and (c) will occur in the first half of year one of the project. Implementation of the project will be carried out through a partnership between (a), (b) and (c) and will occur during the second half of year one and into the first half of year two, as outlined in phases 3,4,5, and 6. 6.4 ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 8 The Evaluation Working Group (d) will focus on the evaluation plan and ensure that all data are brought forward for of the formative evaluation during phase 7, occurring during the final 6 months of the project. The results from the formative evaluation of the project reported by (d) will be used to make revisions and recommendations to the Coordinator of CIPHER to assist in transitioning the project to regular offerings within the partnership. Since this program will be two years in length, a summative evaluation will not be feasible, as the first two years will focus on program development and implementation. The Steering Committee during the first year will also work to create a permanent structure within UWO charged with on-going evolution of interprofessional education within the health professional programs. A draft set of goals and membership is appended (Exhibit #1 – page 25). Steering Committee members will collaboratively develop CIPHER and UWO will commit to providing the funding to sustain and foster its integration into the university through appointment of a part-time director and a secretary when this project ends. Day-to-day management of this project will be provided through a full-time project coordinator hired within the first 3 months of the project’s inception (Phase 1). A full time research associate will also be hired to manage the evaluation of the project. The project coordinator and research associate will report to the project co-chairs. The research associate will chair the Evaluation Working Group and the project coordinator will chair the Education Program Working Group. PROJECT STEERING COMMITTEE CURRICULUM WORKING GROUP EDUCATIONAL PROGRAM WORKING GROUP PRACTICE SITE WORKING GROUP EVALUATION WORKING GROUP CONSORTIUM FOR INTERPROFESSIONAL HEALTH EDUCATION AND RESEARCH (CIPHER) PROJECT MANAGEMENT STRUCTURE A matrix management structure is proposed to support this project. The Secretary will be accountable to the Project Coordinator for work assignment and completion but will also provide secretarial support to the research associate and the project coordinators. The research associate will work under the direction of the project co-chairs but also with the project coordinator for the integration of the evaluation activities into the implementation of each phase of the project. PROJECT CO-CHAIRS SECRETARY PROJECT COORDINATOR RESEARCH ASSOCIATE ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 9 Co-chairs Dr. Evelyn Vingilis is Director of the Population and Community Health Unit and Professor with the Departments of Family Medicine and Epidemiology and Biostatistics in the Schulich School of Medicine and Dentistry, and the School of Nursing in the Faculty of Health Sciences, at The University of Western Ontario. Moreover, she is leading a steering committee to develop a proposal for an inter-disciplinary, multi-faculty graduate program in health studies to support inter-disciplinary education and research. She is a member of the CIHR-funded TUTOR-PHC training grant. Dr Vingilis teaches interdisciplinary courses which include students from nursing, medicine, psychology and political science. She is also Director of CAREMH and PI of a CIHR Interdisciplinary Capacity Enhancement -Team Grant. This research interdisciplinary program includes educational and mentoring components with the purpose to enhance the research and knowledge uptake in the area of mental health reform. She has received 25 research grants in the past five years and is on the editorial board of two international journals. Dr. Cheryl Forchuk's primary appointment at UWO is in the School of Nursing, Faculty of Health Sciences with a cross appointment in the Department of Psychiatry, Faculty of Medicine and Dentistry. She is involved in teaching in both the undergraduate and graduate programs in nursing and regularly has medical students work with her for research experiences. Her program of research focuses on therapeutic relationships and systems issues related to individuals diagnosed with a chronic mental illness. Her work involves participatory research approaches and she currently has a CURA on Housing and Mental Health that includes multiple partners: major housing providers, shelters, psychiatric survivors, mental health agencies, policy decision makers and researchers. The CURA involves interdisciplinary education as well as research. Dr. Forchuk also has a project funded through CIHR related to best discharge practices from psychiatric wards. That project is a collaborative endeavour with 6 Ontario hospital sites, sites in Scotland and Finland, and over 20 psychiatric consumer groups participating. She is the program leader for the Health Systems and Outcomes group at Lawson Health Research Institute (LHRI) which includes 137 researchers. Dr. Forchuk is on the editorial board of The Journal of Psychiatric & Mental Health Nursing (UK) and Archives of Psychiatric Nursing (US) as well as a reviewer for several other journals. 6.5 PROJECT DESCRIPTION a) TITLE: Creating Interprofessional Collaborative Teams For Comprehensive Mental Health Services. b) PROJECT OVERVIEW “Imagine a world where each group’s expertise is held in regard, offered, and shared as the need arises. Imagine a time when the patient can determine which kinds of practitioners he or she needs or wants, and then imagine a system that makes those professionals available.” - Carroll-Johnson, 2001, p.619 This proposed project will bring together faculty members and students from the UWO Schulich School of Medicine, including psychiatry; Faculty of Health Sciences, including Nursing, Occupational Therapy and Physical Therapy; School of Social Work, Department of Psychology; community agencies, and patients, to introduce, develop, monitor and evaluate changes in interprofessional education and interdisciplinary practice. The project will specifically focus on the provision of mental health services, creating a culture of ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 10 interdisciplinary education and practice through a phased change process: sensitization of faculty, students, community partners and clients on the need for and benefits of interprofessional collaboration (Phases 1 and 2); exploration of interprofessional education and interprofessional practice opportunities, using simulation and problem based learning tools (Phases 3, 4 and 5); intervention with student teams working in practice settings (Phase 6) and evaluation to measure short-term outcomes against objectives (Phase 7). The results will increase awareness, broaden the network, develop curriculum and get more students, faculty and communities involved in sustained education and practice of interprofessional comprehensive mental health services, including services to the homeless and other disadvantaged groups. There are two reasons for the selected focus: i) The target group has limited access to care even while suffering multiple social, mental and physical problems. Interprofessional teams are essential for provision of care to this group of persons, so student teams would have ample opportunity to get practical experience working collaboratively. ii) The UWO project team comprises considerable teaching and research expertise in mental health, homeless issues and interdisciplinary team development, and it also has strong links with community agencies which will enable placements, role models and guidance for student teams affording the foundation required to ensure project success. Rationale Health care, as currently practiced, is delivered by health professionals who work within disciplinary “silos” that usually operate within a hierarchy, with power imbalances even when groups work as teams. Such power imbalances can lead to "divisiveness and conflict … for each discipline but… even higher costs for society in duplication of effort, unnecessary conflict, energy-depleting discord, and the potential for greater risks to patients" (Fagin, 1992, p. 296). This is particularly true in the provision of mental health services, where clients suffer low access to care, and whose needs are complicated by multiple social, mental and physical problems that require coordinated medical care, psychiatric counselling, and social advocacy if they are to be fully addressed. A further power imbalance exists between the health care system and the client who is generally not consulted in the process of planning for, implementation of, and evaluation of health decisions made on his or her behalf. This is particularly so in the case of persons needing mental health services. If mental health care is delivered in a fragmented way by each profession treating the patient within his/her expertise, there is a danger that the needs of the patient may be inadequately addressed, and may be lacking continuity of care, possible duplication of effort and miscommunication of needs. In the final report of the Commission on the future of health care in Canada, Romanow1 challenged the health care professions to move towards “teamwork and interdisciplinary collaboration… from health care providers either working in primary health care organizations or participating in networks of providers” (Commission Report, p. 117). Teamwork and interdisciplinary collaboration are admirable goals, but moving to a system which understands and values interdisciplinary practice will need a change in the current culture of healthcare systems. The process of change has to begin with education of health professionals to sensitize them to the need for interdisciplinary client-centred care; to teach them tools to work in an 1 Romanow, R.J. 2002. Building of Values: The Future of Health Care in Canada. Royal Commission on the Future of Health Care in Canada. http://www.hc-sc.gc.ca/english/pdf/romanow/pdfs/HCC_Final_Report.pdf ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 11 environment that supports team work and collaboration. If successful, it could help influence practice in the long term. Interdisciplinary care provides for “a partnership between a team of health professionals and a client in a participatory, collaborative and coordinated approach to share decision-making around health issues” (Orchard & Curran, 2003). Moving towards interdisciplinary collaborative practice requires a cultural shift away from current power imbalances, competition, distrust, and underdervaluing the educational knowledge and expertise of other professions. A change to nterdisciplinary practice requires alterations in health professionals’ existing values, socialization, and workplace organizational structures. This will only be possible with encouragement of a new culture in health systems that support trust among health professionals, willingness to share in patient care decision-making, and inclusion of patients and/or relatives in discussions about their care. c) CONCEPTUAL FRAMEWORK OR LOGIC MODEL STRATEGIES ASSUMPTIONS Faculty conference to discuss strategies and develop road map. “Lab” days to enhance discussion of issues. Self-directed participatory student team projects. Prepare educators, students and practitioners for ICP* 1. Workshops 2. Simulated practice 3.Community practice 4. Self-directed problem-based learning will encourage success of team collaboration. PROBLEM OR ISSUE INFLUENTIAL FACTORS - Kirby/Romanow report calling for change. - organizational structuralism - power imbalances - role socialization - role clarification - role valuing - trusting relationships - team effectiveness - team outcomes Complexity of mental health needs requires interdisciplinary skills and integrated teams to provide range of services. Focus on patient centred care requires collaboration among interprofessional teams. Pre-and post licensure education does not currently provide training for ICP. COMMUNITY NEEDS/ASSETS 1.UWO has teaching and research programs in medicine including psychiatry, nursing, OT, PT, psychology, social work 2. CAREMH and CURA successful IDP* research collaboration. 3 Community partners. 4. Teaching modules available. 5. New clinical skills facilities 6. Standardized patient program 7. Health Zone initiative in Nursing. DESIRED RESULTS (Outputs, & Outcomes And Impact) 1.Socialize health care providers in working together. 2.Instill requisite competencies for collaborative practice 3.Promote patient centred collaborative teamwork. *IDP—Interdisciplinary practice *IPC—Interprofessional collaboration ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 12 The proposal has adopted the Kellogg Logic Model2 for program planning and development to present, in a systematic way, the relationships among the resources we have, the strategies we will use to bring about change and the outcomes we hope to achieve. The strategies focus on the educational system – the left side of the D’Amour/Oandasan model3 of Interprofessional Education for Collaborative Patient-Centred Practice. Strategies Promotion of interprofessional education for collaborative practice will require a change in management process which must address the two separate aspects which are interdependent: Interprofessional education to enhance learner outcomes4 and Collaborative practice5 to enhance client care outcomes. This proposal focuses on development of interprofessional education through a change process that creates a culture for interdisciplinary collaborative client-centred practice using Orchard’s Conceptual Framework (2005) [See Exhibit #3: Outline for Team Process Modules – page 32]. Faculty from participating disciplines as well as community agency partners will act as mentors, monitors and facilitators to guide student learning and practice6. Faculty and agency partner workshops, in addition to sensitization, will collaboratively develop a “road-map” that shows the “destination.” Thus, the conference and the workshops will have the following objectives – to discuss content, to define process, and to set common goals7. We recognize that obstacles exist to having students from different programs work collaboratively, including logistical and attitudinal factors. The coordination of interactive opportunities among the different disciplines will require creativity and commitment. All faculties/schools are deeply committed to moving this agenda forward 8. The Directors of the various academic programs recognize the need for promoting interdisciplinary collaborative client-centred care, and are committed to collaboratively supporting this initiative (see attached letters of commitment by Program Directors). A goal driven approach will be encouraged. Student teams will direct their learning through self-directed participatory teamwork9. This approach has been chosen based on the assumption that in giving students control over their time and resources it will encourage them to take ownership of their learning, driven by goals and objectives against which they can evaluate their achievement. A rapidly changing health care environment requires students to be prepared as self-directed life long learners. This approach will also enable them to see challenges as opportunities and be equipped to address these challenges faced by their clients10. Self-directed 2 W.K. Kellogg Foundation. 2001. Logic Model Development Guide: Using Logic Model to Bring Together Planning, Evaluation, & Action. Chapter 3. Program Planning Template. p 33. http://www.wkkf.org/Programming/ResourceOverview.aspx?CID=281&ID=3669 3 Health Canada. (2004) Interdisciplinary Education for Collaborative Patient-Centred Practice. Research and Findings Report. February 20, 2004. Project leader: Ivy Oandasan. Framework P 64. D'Amour, Oandasan Model – Teaching factors: Learning context → learner outcomes D'Amour, Oandasan Model – Organizational factors → patient outcomes 6 D'Amour, Oandasan Model – Structuring clinical care 7 D'Amour, Oandasan Model – Sharing goals/vision 8 D'Amour, Oandasan Model – Institutional factors: leadership resources 9 D'Amour, Oandasan Model – Sense of belonging → Professionals satisfaction, well-being 10 D'Amour, Oandasan Model – Patient: task complexity → Patient quality of care/satisfaction 4 5 ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 13 educational approaches are formed around case based discussions that are student driven and related to the learning needs identified by the students (Woods, 1994). Students determine which problems they will address and when they have reached a satisfactory conclusion to their discussion11. Throughout this, and other related processes, students are encouraged to identify learning needs and research these needs thus promoting divergent thinking. In addition students are required to identify a solution to a problem or situation posed in the case promoting convergent thinking (Woods, 1994). Throughout a health based curriculum there is opportunity for self-evaluation and the expectation that the students will utilize their strengths in order to develop areas in which they are less accomplished. This process echoes the one the students will be required to apply in practice (School of Occupational Therapy, 2004). Before students set up their teams, they will be required to attend introductory workshops to sensitize them to the issues related to working in teams with clients needing mental health services (See Exhibit #3: Outline of Team Process Modules – page 32). Early in the project there will be simulated learning – student teams will conduct an interview with a Can-voice12 member to learn first hand, the range of problems experienced by consumer mental health survivors13. Students will be given as much as one year to set up, work at, and evaluate their efforts against the objectives they set at the outset. Assumptions The strategies we have chosen ---to enhance student team learning through self-directed, problem based learning, and to focus on mental health services, are based on the following assumptions: 1) That the workshops will bring together a diverse community of faculty, students, community leaders and clients to provide a sensitization to the issues of interprofessional collaboration in mental health services and will help us define and refine the infrastructure and supports and processes. That the Consortium for InterProfessional Health Education and Research (CIPHER14) will be adopted and given a structure and purpose. 2) That simulated practice, using the advanced learning tools we have to offer our students, will achieve its goal in helping students understand the principles of team dynamics and mental health services and prepare them for practice in the community15. 3) That the community practice settings available through our partners will give students good opportunities to put their learning in the classroom to good use with the help and support of faculty and community mentorship16. D'Amour, Oandasan Model – Learning context → Learner outcomes; competencies Can-voice is a psychiatric consumer/survivor Community support service. Can-voice is one of the partners in the CURA on Mental Health and Housing. 13 D'Amour, Oandasan model: Patient: sharing goals/vision → Patient quality of care. 14 D'Amour, Oandasan model: Institutional factors: leadership/resources: administrative processes 15 D'Amour, Oandasan model: Teaching factors: structuring clinical care 16 D'Amour, Oandasan model: Organizational factors: structuring clinical care: interactional factors → patient provider outcomes 11 12 ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 14 4) That the Council of Ontario Universities (COU) online learning modules will be available through a project initiated by Dr. Carole Orchard17 that has been funded by Health Canada in the first phase of this call. 5) That self-directed problem-based learning will achieve the goals of helping students work collaboratively in teams by giving them ownership of their learning in an enabling environment18. Influential Factors Conflict exists between the traditional role that consumers of services play in shaping their receipt of services and the value which health professionals place in a client-centred system of service delivery (Orchard & Curran, 2003). There is no area of health care that is affected more than the mental health sector. The recent Romanow Commission (2002) and Kirby (2002) reports stress the need for Canada’s Health System to move towards a primary health care model. This model of care has also been proposed by the World Health Organization (WHO). Such a model, however, requires a significant change in the organizational structure of the system, in the power relationships among the health disciplines, and the patterns of socialization of health professionals and consumers of health services19. The health care system has become very complex over the past number of decades, largely because of the rapid progress of medical science and the accompanying emergence of medical and health care specialists from multiple disciplines (Drinka, 1996). This has led to consultation being the hallmark of current practice. This consultation and specialization has resulted in a fragmented level of care and dwindling opportunities for interdisciplinary exchange. Problem or Issue Mental illness is a common health condition that leaves few families untouched. The best epidemiological estimate from the World Health Organization (2001) is that one in five persons suffer from a diagnosable mental disorder in any one year. Moreover, findings from the largescale Global Burden of Disease study, conducted by the World Health Organization, the World Bank and Harvard University, indicate that mental illness is in second position among disease burdens in developed economies (Murray & Lopez, 1996). The estimated economic burden of mental illness in Canada in both direct and indirect costs in 1993 was $7.8 billion (Moore et al., 1997). More recent work, addressing some limitations of the previous research, found that in 1998 the direct and indirect cost estimates of total economic burden of mental health problems was $14.4 billion (Stephens & Joubert, 2001). Because of this high prevalence and economic burden, the mental health care system has been under exceeding pressure to deliver services of high quality against fiscal restraints. Mental health care reform and the de-institutionalization movement has been underway in Europe and North America for a number of years. Three factors, relating to monetary and ethical issues, have been driving this movement. First, the economic burden of mental health care is extremely high. For example, in Canada mental illness has been ranked as second highest 17 IECPCP Project: Institute of Interprofessional Health Sciences Education. Related to teaching factors in D'Amour Oandasan model: learning context; faculty development → competencies. 18 D'Amour, Oandasan model: competencies: sense of belonging. 19 D'Amour, Oandasan model. Organizational Factors. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 15 in hospitalization costs only surpassed by cardiovascular illness (Wigle et al., 1986). Over half of hospital days have been in the psychiatric hospital system, in which a small number of people with chronic mental illness experience lengthy hospitalizations (Randhawa & Riley, 1996). Clearly the discovery of medications that manage the symptoms of many psychiatric illnesses provided a major stimulus for reform and de-institutionalization as persons with mental illness could now function in the community. A second driving force has been humanitarianism, where we have moved from a silo approach to mental health to a more community based, humane manner of providing services. The third force has been consumer advocacy. The consumer advocacy movement has focussed on rights of individuals and pressing for different practice approaches which helped providers recognize the need for reform. Mental health reform and de-institutionalization have major implications for how we educate health care professionals. The reality of mental health reform and de-insitutionalization is that society is creating a “virtual” hospital, where the needs of persons with serious mental illness are more likely to be met outside of hospital walls. However, the development and management of a virtual hospital and community-based care poses challenges because of the need to: (a) coordinate the multiple health service functions and (b) coordinate other non-health care functions. This first challenge relates to the integration of multiple functions of assessment, treatment and rehabilitation, which previously was provided within hospital walls. As services are moved to community-based treatment, the services that used to be provided by a number of different components within a service system may no longer be as accessible. The challenge occurs because of the increased complexity of the service system, where the person providing the assessment, for example a family physician or nurse in a family practice centre, may also need to be delivering some of the treatment, or rehabilitation functions that would have been provided by specialized mental health care providers in psychiatric and other hospitals. This highlights the need for interprofessional education and knowledge. The second challenge relates to coordination of added functions that are not specifically health care services, such as income support, appropriate housing and nutrition, recreation and leisure activities, legal advice, etc. This further complicates what used to happen in a hospital in a fairly integrative way, as it was easier to co-ordinate and integrate those functions for people who were all together and across the hall from one another, where the meals came on the food tray, recreational activities were in the common room and most other services were available in situ. The new approach to community-based care requires interdisciplinary skills and integrated teams to provide a full range of health and other services to persons with mental illness. Moreover, since small core groups of specialized mental health professionals are no longer working in provincial hospitals and providing the majority of care to persons with mental illness, there is a fundamental need to develop programs for interprofessional education for collaborative care that focus on the unique issues and needs of persons with mental illness (client-centred care). Client-centred practice is an important concept in many health professions including medicine, nursing, occupational therapy and physical therapy but limited research has been done to elucidate the implications for clients with a mental illness (Bishop 2001). It is important to understand how the concepts within a client-centred approach can be effectively applied to enable patients affected by deinstitutionalization to thrive outside of the hospital. Research has shown that clients can be engaged in meaningful community lives and that client-centred practice facilitates this success (Krupa & Clark, 2004). Additional research has also shown that ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 16 clients in mental health programs value a client-centred approach and the opportunity to be at the centre of the intervention enhances their potential for rehabilitation. (Corring & Cook, 1999; Rebeiro, 2000; Sumsion 2004). A client-centred approach does not negate the importance of the professional’s expertise but it does enable clients with a mental illness to explain their goals and plans and to seek meaning in their lives. Health practitioners aim to empower clients and facilitate a sense of control and fulfillment through the application of this approach (Dressler & MacRae, 1998). Client-centred practice supports the concept of recovery, which enables people to become actively involved in their communities despite the presence of pervasive and continuous mental illness (Krupa & Clark, 2004). Therefore, it is important to investigate opportunities to enhance the application of client-centred practice in order to address the rising costs of mental illness. Community Needs/Assets In developing a culture of interprofessional collaboration, there are multiple needs for appropriate teaching tools, mentors to guide and practice settings to support learners. Development of education for interprofessional client-centred collaboration will need a number of adjustments to the traditional methods of teaching and working. Fortunately, at UWO, there are a number of assets in place already that can be drawn upon or adapted to a wider purpose. i. Specialized Learning Resources20 Learning Resource Centre (LRC): The Schulich School of Medicine and Dentistry has a multimedia facility which provides self-instructional resources. The resources available within the Centre include: 80 networked computer workstations (34 of these located in the computer based learning centre (CLBC)), nine laptop ports, three laser printers, scanner, information desk, clinical skills room, mannequins for practicing various physical exam and procedure skills, videotapes, reference books, radiographs, pathology specimens, anatomical models, and the LRC website at http://www.fmd.uwo.ca/cblc/. The LRC computer network provides Internet and WebCT access, a variety of office software and medical education software. The Schulich School of Medicine has just completed the building of a set of physician office learning units that are designed to assist in teaching/learning assessment and interviewing skills. Located within the LRC is a teaching facility, the CLBC, available for instructional and examination purposes. The CBLC may be reserved for class use in the programs of medicine, dentistry and nursing. It is also available on an individual basis by medical, dental and nursing students when not reserved for teaching. The South Valley Building (SVB, that opened in January 2005, is home to the Faculty of Health Sciences. This state-of-the-art four-storey 80,000 square foot structure houses six general use classrooms - with seating capacities of 50 (2), 150 (3), and 500 (1) students - and three 50seat general use student computer labs/classrooms on its first and second floors. Two uniquely designed facilities in the building place the Faculty and its programs at the forefront of clinically-based education. A clinical education suite, located on the building's third floor, incorporates a nine-bed simulated hospital, and is equipped with programmable simulated mannequins, a bachelor-apartment style simulated home unit, four computer-based learning pods, one small group learning area, and a unit charting station. A further simulated learning laboratory will be available in the School of Nursing in September 2005. These learning facilities will provide a resource for interprofessional student groups working within intranets, on 20 D'Amour, Oandasan model. Institutional Factors: Leadership/Resources. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 17 case studies, to develop their teamworking skills in sharing their knowledge and skills in arriving at client-centred care decision-making. These new facilities will improve and enhance the current clinical instruction studios in the Schools of Nursing, Occupational Therapy and Physical Therapy, and in combination with the Speech and Hearing clinics in the School of Communication Sciences and Disorders, will further strengthen the Faculty's profile for on-site clinical education. Additionally, the SVB's third floor will be the Faculty's virtual reality theatre. This 50seat facility will offer state-of-the art instruction in the study of anatomy to students in all of the Faculty's Schools and Programs, and will open the door to more creative and imaginative approaches to the study of health care. It will facilitate collaborative and interprofessional learning and research that will take place amongst and between students and faculty, will lead to generations of better educated health care professionals, and by extension, a more healthy and prosperous Canada. The standardized patient (SP) program: in the Schulich School of Medicine & Dentistry simulates an actual patient; not just the history, but the body language, the physical findings, and the emotions and personality characteristics as well. SPs are laypeople who may or may not have any medical knowledge. Some SPs are actors, but most are not. SPs are from all walks of life, of all ages and educations. The common thread among all our SPs is an interest in helping others. The SP offers a readily available and standardized tool for teaching new skills, refining old skills and evaluating learner performance. This allows for teaching and assessment of skills in an experiential and problem based manner. UWO’s current Standardized Patient base exceeds 200 Standardized Patients, ages 12 - 90. On previous studies of Dr. Forchuk, Can-Voice members, who are mental health consumer survivors, have acted as standardized patients. This is a resource we can draw upon for this project. The School of Nursing has an innovative program called “The Health Zone” – a primary care initiative funded by the T.R. Meighan Foundation and the Nursing Alumni, started in September 2004. The UWO School of Nursing, Merrymount Children’s Centre and the Middlesex-London Health Unit formed a collaborative partnership to guide the development of this initiative. This program within the initiative of The Community Nursing Resource Centre (CNRC) is an accessible, community-based nurse-managed health centre with three interdependent components - research, education and service. Dr. Carole Orchard, is a co-chair of the IECPCP funded project through the Council of Ontario Universities, entitled “Institute of Interprofessional Health Sciences Education.” In this role, she will develop a set of modules for team process development that UWO will utilize (See Exhibit #3, p. 32): 1) Awareness of the realities of clinical practice and its limitations to interprofessional collaborations; 2) Helping groups re-conceptualize the way they wish to view and enact interprofessional practice; 3) Developing norms for interdisciplinary collaborative teams and their practice; and 4) Creating means for testing the model with patient groups, which will be available for this project. ii. Interdisciplinary research and programs21 UWO has a strong track record in community based mental health care and research. As mentioned before (in section 6.2 – page 2) one of the assets in this community is the existence of a CURA on Housing and Mental Health. The links between researchers/faculty and community agencies can be extended to create the opportunity for placements for multidisciplinary student 21 D'amour , Oandasan model. Health professional/learner outcomes: Patient/provider outcomes. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 18 teams. The shift in curriculum is that these placements would focus on the process of interdisciplinary teams as well as the content of mental health and housing. CAREMH. headed by Dr. Evelyn Vingilis, is another resource at UWO whose expertise and community contacts can be drawn upon for this project. CAREMH has experience in encouraging collaboration and knowledge translation among researchers from different disciplinary perspectives, practitioners, administrators and consumer/survivors. The successes of both CURA and CAREMH result from fostering interprofessional collaboration through creating interprofessional collaborative teams for comprehensive mental health services and/or research. Together, these formalized alliances afford an infrastructure upon which we can build a sustainable interprofessional education program for collaborative client-centred practice in community-based mental health care. UWO has a legacy of innovative and successful interdisciplinary training programs. For example, Transdisciplinary Understanding and Training on Research - Primary Health Care (TUTOR-PHC) is a CIHR funded national program in training in primary health care research to meet the immediate need for research capacity in this field. The teaching methods developed and used and experiences garnered to enhance interdisciplinary learning in TUTOR will provide much shared learning to the proposed interprofessional education program. This program has educated 36 clinical researchers from more that eight professions from across Canada. The team of 18 co-investigators represent six professions and have created symposia, workshops, interdisciplinary lab discussion groups and transdisciplinary concept papers to enhance interprofessional education of future researchers. Additionally, an on-going UWO initiative is to develop an interdisciplinary health studies graduate program which will include departments and schools in the Faculty of Health Sciences, the Schulich School of Medicine and Dentistry, and the Faculty of Social Sciences, headed by Dr Evelyn Vingilis. This initiative has the support of many Faculties across UWO, including faculty, schools and departments listed within this proposal. The strategies and successes obtained in this initiative can inform and support the proposed program. Desired Results, Outputs, and Short-term Outcomes See 6.6 for a listing of project objectives and Exhibit #5 (page 36) that presents a table linking objectives to process outputs, workplan/implementation and evaluation and assessment. 6.6 PROJECT OBJECTIVES The objectives of this project are to: 1) Socialize health care faculty, health professional students, and practitioners in working together, with shared problem solving and decision making, toward enhancing benefits for people receiving community-based health services; 2) Stimulate networking and sharing of best educational approaches for collaborative clientcentred practice; 3) Increase the number of educators prepared to teach from an interprofessional collaborative client-centred perspective; 4) Increase the number of health professional students trained for collaborative clientcentred practice before, and after entry into practice; Longer term goals: 5) Facilitate inter-professional collaborative care in both education and practice settings; ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 19 6) Augment the work toward provincial priorities, including: mental health care reform; care of the homeless; development of Local Health Integration Networks (LIHNs) and Family Health Teams. 6.7 WORK PLAN AND TIMELINES (see Exhibit #6 – page 39) A rough outline of the structure under which this project will operate is presented in Exhibit # 1 (p. 29). The actual structure will be decided upon at the first workshop involving faculty, community members, students and clients. CIPHER is using a team-development model (Forming, Storming, Norming, Performing) originally developed by Tuckman (1965) and used extensively in business and educational environments (e.g. The Stanford Center for Innovations in Learning, 2002; The University of Queensland, 2002; University of Alaska Anchorage, 2004) to realize the work plan and timelines. Sensitization Phase 1: Development of Infrastructure (January – April, 2006) Steps: Officially launch the UWO Interprofessional Education and Research Group Hire a coordinator and secretary * Create the Steering Committee Organize a half-day retreat for health professional student leaders, community partners, consumers, faculty members to consolidate a shared vision and common expectations. Create a permanent CIPHER and refine its functioning, interprofessional education structure and membership. Phase 2: Sensitization and Integration of Leaders and Mentors (April 2006 through project end) Steps: Organize a workshop for facilitators (community partners and faculty members) to “train the trainers,” to expose each to the elements of inter-disciplinary practice, to discuss their application within each specific organization. Build in sustainability of partners by assisting community agencies in the capacity to participate and collaborate. Phase 3: Community Experiences (June 2006-March 2007) [See Exhibit #2 – page 30] Steps: Building on the work already done by the Applied Health Science Education Task Team (1995) and the current informal interdisciplinary activities organized by the different faculties and schools, the leaders and mentors will formalize interdisciplinary opportunities for students within the different practica, internship and residency settings. Student teams will interface with patients in the community. The length of the community experience will depend on the specific goals set out in the learning contract (1-3 visits would allow assessment of progress towards a trusting relationship). Faculty mentors will meet with student teams for consolidation of learning regarding interprofessional team practice. Phase 4 Development of Integrating Components (April 2006- end) Steps: A number of faculties/schools/departments are undergoing or have recently undergone curriculum renewal. Informed by the respective curriculum renewal committees, CIPHER will identify learning and curriculum module needs and develop knowledge modules of use for the ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 20 various committees. Thus, the following steps are flexible so that CIPHER can be responsive to the needs of the different curriculum renewal groups. Working groups develop and support placement of core knowledge modules online (communication skills; ethics; team dynamics, incorporating use of COU online team development modules (see Exhibit #3). Use expertise from the UWO Faculty Development Centre and the various curriculum renewal groups to develop online problem based learning modules specific to mental health services. Planning committees determine selection of participants and assignments into interprofessional teams and development and testing of case studies in conjunction with curriculum renewal committees, consumers and community partners. Role Clarification, Trusting Relationships, Shared Decision-Making Phase 5: Development of Student Teams (September-December 2006) Steps: Curriculum steering committee (comprising student members as well as faculty) prepares self-directed learning modules in WEBCT, so students who elect to do this can work at their own pace in September. Elements of interprofessional collaboration will be introduced into lectures and discussions when relevant. For example, in medicine, in 2005/2006, Year 1 students will have a lecture on the mental health team. Department seminars relevant to interdisciplinary interest publicized more widely to encourage participation from other disciplines and professions. Teaching methods & tools for Phases 1, 2, 3, 4: Presentations, small group discussion, online learning modules. Parties responsible: Co-chairs of project; project coordinator; working groups; faculty in individual disciplines; community agencies to present realities; steering committee to guide; student leaders; CURA & CAREMH to share learning relating to inter-disciplinary research teams, some of which could apply to practice. Exploration Phase 6: Further Development of Student Teams Using Peer Support (January 2007) Steps: Standardized patient exercise Problem based learning – communication skills and practice, evidence based practice, ethical practice, relationship based practice. Development of common format/guidelines for learning contract with student teams, faculty mentor and community partner Intervention All activities done in the 2 years, including planning and steering committee work. Teaching methods & tools for phases 5, 6: Learning by doing: a) simulation and role-playing (see above); two way mirror interviewing/clinical skills development, b) working in teams with real patients in practice settings, c) consultations with faculty and community mentor. Parties responsible: Student teams, student mentors, faculty mentors, community mentors, patients, steering committee ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 21 Evaluation Phase 7: Evaluation of site visits & CQI (on-going) [See Exhibit #2 – page 30 and Exhibit #5 – page 36] Steps: Evaluation of community experience Analysis of evaluative data Formulation of findings against desired results Make recommendations for curriculum or organizational improvement Tools: See section 6.8 Evaluation will be ongoing throughout the project. In phase 7, evaluation will be of site visits to enable continuous quality improvement (CQI). See section 6.8 for more. Parties responsible: As in phase 6 above. 6.8 EVALUATION PLAN (See Exhibit #5 – page 36) The steering committee will appoint an evaluation-working group composed of representatives from each of the health disciplines, partnering agencies and student representatives at the outset of the project. Although this group will oversee the evaluation procedures, including qualitative and quantitative data collection, analyses and knowledge translation, the evaluation will inform program development and implementation for continuous quality improvement. A Research Assistant will be assigned to the committee chair to assist with all components of the evaluation. Ethics review of the evaluation plan will be submitted to the UWO Health Sciences Ethics Review Board. The University of Western Ontario will provide office space to support the work of this group and also a repository for secured storage of all data. This office will be equipped with high-speed computers, a scanner, printer and lockable file cabinets. Formative evaluation will include assessment of program processes, using quantitative and qualitative measures. Summative evaluation of program outcomes will not be possible in the nineteen month duration of this proposal, as only one cycle of student teams will go through the program in that time. Whenever possible, data collection for the project evaluation will be integrated with assessment of learning by participants in the various project activities. In this very short time frame for program development and implementation, only shorter term outcomes and impacts can be reasonably expected. All data will be collected in conjunction with the appropriate phases of the project (as outlined below). Evaluation results will be brought to the attention of the project Steering Committee by the Evaluation Working Group (EWG) at the completion of each component of the evaluation. This committee will determine if changes in actions or materials are needed for subsequent phases. If changes are required, the Steering Committee will direct the appropriate working group to take action. A final evaluation report of the project will be prepared to present to the Steering Committee for final approval and then forwarded to Health Canada and all the project partners. Phase 1-4: Using instruments selected to measure the project outputs and outcomes, all as specified in Section 6.7, baseline data (T1 outputs and outcomes) will be obtained from student leaders (n = 75), community partners (n=40), consumers (n=15), faculty members (n=30) who agree to participate in the half-day retreat. Exhibit #5 presents a table of these instruments, complete with descriptions and details regarding source, validity and reliability. However, as this program is in development, program changes may necessitate the use of other instruments. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 22 However, care will be taken to ensure that valid and reliable measures are used. Demographic data on all participant groups will also be collected to facilitate sub-analyses, as appropriate. Members of the EWG will also conduct focus groups involving participants from each of the participant groups (n=15). Semi-structured focus group guides will be developed in consultation with Steering Committee Members to obtain qualitative formative evaluation data on: (a) what constitutes interdisciplinary collaborative practice; (b) attitudes toward interprofessional learning about health teams; and (c) barriers, facilitators and strategies for achieving practice within interdisciplinary collaborative teams. Focus groups will be taperecorded and transcribed verbatim and the data analyzed to identify themes and patterns that may inform sensitization and role clarification endeavours. Phase 4 - 6: Student team experiences will be captured (n=15) using a mix of focus group sessions and a reflective summary of team experiences. The Team Climate Inventory, an instrument developed for use in the TUTOR-PHC project will be adapted for use with these student teams to capture pre-and post collaborative data. Areas for reflection will include: understanding of the nature of the collaboration; expectations related to roles/responsibilities; experience with collaborating; and personal feelings about participation in project. Phase 7: All participating institutions will be asked to retain annual records of measures of impact, including: numbers of faculty participating in the project; numbers of students participating in the project; numbers of clients served by the interprofessional collaborative practice teams; self-directed learning materials and forums developed; workshop and conference agendas and participation rates; and documents reflecting the contributions of the project to mental health reform and the development of the local Health Integration Network. These numerical data will afford measures of project impact in the longer term. A maximally varied purposive sample of students (ensuring a representative sample across the participating health professions), mentors, and leaders will be selected to participate in taped focus group interviews (approximately 5 – 7 learning/teaching teams) to discuss the meaning of their interprofessional learning and interdisciplinary practice experiences. Qualitative data transcripts will be analyzed for themes and patterns affording insights into how best to promote success in the sustained interprofessional collaborative educational program and service delivery. 6.9 KNOWLEDGE TRANSFER, NETWORKING AND DISSEMINATION The introduction of interdisciplinary practice requires re-orientation to the way the public accesses and uses health professionals. We will implement, through the UWO communications staff, a consistent communication plan to educate the public about this form of practice and provide frequent reminders through updates highlighting successes. Administrators and Boards of health agencies equally will need to be convinced that movement into interdisciplinary practice will not cost the system more and at the same time provide higher quality of service outcomes. Hence, we will utilize multiple means to communicate messages that are appropriately formulated at key literacy levels and to integrate cultural awareness. Communication would include web-pages linked to key sources such as Health Canada; internet public education programs on interdisciplinary practice; newsletters; public service columns in regional and local newspapers; regular programming on community TV channels; annual public conferences on functioning interdisciplinary teams and their benefits; booths at health fairs, etc. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 23 Faculty collaborators associated with this project will present papers and posters at local, regional, and national conferences on the process. We hope Health Canada will host annual conferences ‘showcasing’ interdisciplinary practice models and outcomes once models and results of outcomes begin to emerge. Knowledge transfer is a complex process that has explicit methods of dissemination, but it has a tacit component that is difficult to define or to measure. This project has both the explicit and tacit communication built into knowledge translation because of the involvement and exchange between professionals, academics, students from different disciplines, clients and community agencies. External transmittal of knowledge and addressing the tacit knowledge issues in this domain will be addressed through inviting student alumni, professional practice leaders from hospitals and community agencies affiliated with UWO, and policy makers from local, provincial and national levels to serve on an Advisory Committee to CIPHER. This will have the benefit of having knowledgeable input from those working in the field, while informing them (and their affiliated organizations) of developments in CIPHER that may have wider benefit and application. Drs. Carole Orchard and Carol Herbert are UWO representatives on the Management Structure in the Canadian Interprofessional Health Network (CHIN), a national network for interprofessional health practice, led by the University of British Columbia, which has recently applied for funding to the National Centres of Excellence-NI call for proposals. If funded, this would be yet another valuable knowledge dissemination and knowledge sharing opportunity. 6.10 SUSTAINABILITY PLAN At UWO, there has already been considerable investment in state of the art learning resources, like the “standardized patient program,” the new clinical skills facilities, and computer resources that encourage collaborative and self-directed problem based learning. The Deans of the Faculty of Health Sciences and the Schulich School of Medicine and Dentistry have additionally pledged support for the project, beyond the 2 year term, in the amount of $53,000 each. These funds will contribute towards the ongoing administrative needs of CIPHER, which should have moved beyond the time and resource intensive start up stage into a maintenance phase. We expect that evaluation and active knowledge dissemination and transfer will increase buy-in to CIPHER and help to leverage additional funding to accommodate more practice sites and include more students, faculty and community agencies. Sustainability will also be built in through the Advisory Committee (mentioned above), and especially through having alumni who have graduated from CIPHER active in guiding and learning in a continual relationship with CIPHER, as well as participation in the NCE-NI national collaboration, if funded. 6.11 DETAILED PROJECT BUDGET i) Administration: In keeping with the stipulations of the collective agreement, the co-chairs of the project will be paid $10,000 each per annum, or they will be given an alternate workload and the Schools will use the $10,000 for teaching buy-out. A project coordinator will be hired for the duration of the project with a salary of $70,000 ($50,000 plus benefits). A secretary will be hired to help with administration of the project, at a cost of $40,000 per annum ($35,000 plus benefits). A full-time research associate will be hired at a cost of $70,000 ($50,000 plus benefits) to manage the evaluation of the project. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 24 ii) Workshops and Retreats: Two half-day workshops will be held per year. All the workshops will give faculty, student leaders, and community agency members a chance to attend. We estimate that on average, 30 faculty members and 40 community members may attend in addition to student leaders and client representatives. In the first year the workshops will encourage sharing of view points on interprofessional client-centred care and mental health services and to collaborate on the structure and mandate of CIPHER. In year 2, the workshops will include evaluation and encourage sharing ideas on improving the program. Steering committee retreats include those held by the 4 working groups. The workshop and retreat costs include rental of a facility, materials, and compensation for community member participants' time. iii) Mentors: The budget for community agencies includes supervision, mentoring and paperwork in connection with student team visits. It also includes a budget for a community agency member’s workshop attendance or steering committee retreat participation. Many community agencies have very few staff to spare. If a staff member is away, the office must either close for the duration or employ a replacement person for that time. Since community agency participation is a very important component of this project, the budget factors in those costs. A rough calculation is $2,000 per community agency member per year and the total is based on 40 members participating per year. These are start-up costs when commitments for participation in workshops will be higher. iv) Teaching resources: The consultant fee ($2,000) is allowed for a programmer or student research assistant to help create and maintain online learning modules. The annual standardized patient budget is based on putting 15 students groups through the simulated training exercise, estimating 8 hours per group, at $100 per hour). The same amount would be paid for Can-voice members or the UWO standardized patient program. The budget estimates that six faculty members from each of the disciplines will serve as leaders and mentors to students. Stipends for 6 faculty leaders’ time in Phase 4 activities are budgeted at $3,500 per faculty member, for a total of $21,000. 6.12 ETHICS REVIEW Curricular modifications are not usually sent for approval to the Ethics Review Board (ERB), but because this represents a new teaching model which we intend to assess and write about, we will seek ethics review of the evaluation plan, which will be submitted to the UWO Health Sciences Ethics Review Board. A key element in having students work in community practice settings is the degree to which patients need to be informed and agree to their involvement in a teaching enterprise. For that we will follow the procedures we use for clinical placements. The University of Western Ontario will provide office space to support the work of this group and also a repository for secured storage of all data. This office will be equipped with high-speed computers, a scanner, printer and lockable file cabinets. CONCLUDING REMARKS We hope that encouragement and formalization of interdisciplinary education and collaborative practices between faculties and departments at UWO will influence practice post licensure. In focussing on the needs of mental health clients and in promoting self-directed learning, we hope interprofessional teams will have the opportunity and motivation to learn together. Our leaders think this approach of sufficient importance to commit financial and in-kind resources to this proposal. We thank Health Canada for supporting this important initiative. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 25 References Anderson,N. & West,M.A. (1998). Measuring climate for work group innovation: development and validation of the team climate inventory. Journal of Organizational Behaviour, 19, 235-258. Baggs, J.G. (1994). Development of an instrument to measure collaboration and satisfaction about care decisions. Journal of Advanced Nursing. 20, 176-182. Carroll-Johnson, R.M. (2001). Redefining interdisciplinary practice. Oncology Nursiing Forum, 28(4), 619. Community Mental Health Evaluation Initiative. 2004. Making a Difference. Ontario’s Community Mental Health Evaluation Initative. Downloaded November 27, 2004. http://www.ontario.cmha.ca/cmhei/images/report/Making_a_Difference.pdf Corring, D. J., & Cook, J. (1999). Client-centred care means that I am a valued human being. Canadian Journal of Occupational Therapy, 66, 71-82. Dressler,J., & MacRae, A. (1998). Advocacy, partnerships and client centred practice in California. Occupational Therapy in Mental Health, 14, 35-43. Drinka, T.J.K., & Clark, P.G. (2000). Healthcare Teamwork: Interdisciplinary practice and teaching. Westport, Conn: Auburn House. Eisenberger, R., Cummings, J,. Armeli, S., & Lynch, P. (1997). Perceived organizational support, discretionary treatment, and job satisfaction. Journal of Applied Psychology, 82(5), 812-820. Eisenberger, R., Huntington, R., Hutchsion, S. & Sowa, D. (1986). Perceived organizational support. Journal of Applied Psychology, 71(3, 500-507. Elwyn, G., Edwards, A., Wensing, M., Hood, K, Atwell, C., & Grol, R. (2003). Shared decisionmaking: Developing the OPTION scale for measuring patient involvement. Qualitative Saf Health Care , 12, 93-99. Fagin, C.M. (1992). Collaboration between nurses and physicians: No longer a choice. Academic Medicine, 67(5), 295-303. Golin, A.K, & Ducanis, A.J. (1981). The interdisciplinary team: A handbook for the education of exceptional children. Rockvill, MD: Aspen, 1981 Hojat, M., Gonnella, J.S., Nasca, T.J., Fields, et. al. (2003). Comparisons of American, Israeli, Italian and Mexican physicians and nurses on the total and factor scores of the Jefferson scale of attitudes toward physician-nurse collaborative relationships. International Journal of Nursing Studies, 40, 427-435. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 26 Krupa, T., & Clark, C. (2004). Occupational therapy in the field of mental health: Promoting occupational perspectives on health and well-being. The Canadian Journal of Occupational Therapy, 71, 69-74. Luecht, R.M, Madsen, M.K, Taugher, M.P. & Petterson, B.J. (1990) Assessing professional perceptions: Design and validation of an interdisciplinary education perception scale. Journal of Allied Health, Spring181-191. Moore, R, Mao,Y, Zhang, J. and Clarke, K. (1997) Economic burden on illness in Canada, 1993. Health Canada http://www.hc.sc.gc.ca/pphb-dgpsp/publicat/edic-femc93/index.html Nelson, G., Hall. B., & Forchuk, C. (2003) Current and Preferred Housing of Psychiatric Consumer/Survivors. Canadian Journal of CommunityMental Health. 22 (1), 5-19. O’Connor, A.M. (1995). Validation of a decisional conflict scale. Medical Decision Making, 15, 25-30. Orchard, C.A., Curran, V., & Kabene, S. (2005). Creating a culture for interdisciplinary collaborative practice. Medical Education online [serial online], 10(11), 1-13. http://www.meded-online.org Orchard C.A. & Curran, V. (2003). Centres for Excellence in Interdisciplinary Collaborative Professional Practice. Funded by the Office of Nursing Policy, Health Canada. Randhawa, J. and Riley, R. (1996) Mental health statistics 1982-83 ro 1993-94. Health Reports 7(4), 55-61. Reberio, K. L. (2000). Client perspectives on occupational therapy practice: Are we truly clientcentred? Canadian Journal of Occupational Therapy, 67, 7-14. Rizzo, J.R., House, R.J., Lirtzman, S.I. (1970). Role conflict and ambiguity in complex organizations. Administrative Schience Quarterly, 15(2), 150-163. School of Occupational Therapy (2004) Self Study Accreditation Document. The University of Western Ontario, Standard 2.2. Stephens, T., & Joubert, N. (2001) The Economic Burden of Mental Health Problems in Canada Chronic Diseases in Canada 22, 18-23 Strasser, D.C., Falconer, J.A., & Matrino-Saltzmann, d. (1994). The rehabilitation team: Staff perceptions of the hospital environment, the interdisciplinary team environment, and interprofessional relations. Archives of Physical Medicine Rehabilitation, 75, 177-182. Sumsion,T. (2004). Pursuing the client’s goals really paid off. British Journal of Occupational Therapy, 67, 2-9. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 27 Temkin-Greener, H., Gross, D., Hunitz, S.J., & Mukamel, D. (2004). Measuring Interdisciplinary team performance in a long-term care setting. Medical Care, 42(5), 472-481. Thames Valley Family Practice Research Unit (June 2004). Pretest Study of a Teambuilding Intervention for Interdisciplinary Primary Health Care Teams. Final Report to Ontario Family Health Network, Ministry of Health and Long-term Care. The Stanford Center for Innovations in Learning, (2002) Learning communities/collaborative learning http://sll.stanford.edu/projects/tomprof/newromprof/posting. accessed 12/9/2004 The University of Queensland (2002) Forming-storming-norming-performing-mourning. http://www.catalyst.uq.edu.au/designsurfer/team_stages.html. accessed 12/9/2004 Tuckman, B.W.(1965) Developmental Sequence in Small Groups, Psychological Bulletin, 63, 384-399. University of Alaska Anchorage (2004) Student leadership. http://www.uaa.alaska.edu/studentleadership/group.cfm. accessed 12/9/2004. Wigle, D.T, Mao, Y, Wong, T. & Lane, R. (1986) Economic burden of illness in Canada, 1986. In L. J. Anderson & K. Wilkins (Eds) Chronic Diseases in Canada: Supplement to Volume 12(3), 1-37. Woods. D.R. (1994). Problem-based learning: How to gain the most from PBL. Hamilton, ON: Author. World Health Organization (WHO) (2001) Mental Health: New Understanding, New Hope. http://www.who.int/whr/2001/main/en/index.htm/ ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 28 EXHIBIT 1: Proposed Structure For Consortium For Interprofessional Health Education And Research (CIPHER) The Consortium for Interprofessional Health Education and Research is an affiliation of Schools and Departments in the University of Western Ontario with an interest in interdisciplinary education and research including: Medicine & Dentistry (which includes psychiatry), Nursing, Occupational Therapy, Physical Therapy, Communication Sciences and Disorders, Social Work and Psychology. The goals of the CIPHER are: 1) To provide a forum for fostering interprofessional education and practice among health professional students; 2) To provide a forum for faculty to discuss health issues that relate to interprofessional study; 3) To support development of interprofessional curricular modules for the undergraduate and graduate levels for health sciences students; 4) To provide workshops to assist faculty wishing to teach interprofessional practice in the university 5) To facilitate development of practice areas both on the campus and in the community in support of interdisciplinary collaborative professional practice; 6) To sponsor continuing education offerings on interdisciplinary professional practice topics for practicing health professionals in the southern Ontario area; 7) To provide a means for educating the public in the southern Ontario area on the benefits of interdisciplinary collaborative professional practice; 8) To support studies related to evaluation of interdisciplinary collaborative professional practice in the community; 9) To support student projects using interdisciplinary collaborative practice approaches; 10) To provide a forum for discourse around the merits of interdisciplinary collaborative practice. Membership: All faculty in the affiliating schools are eligible for membership in the CIPHER. All students admitted to programs in the affiliated schools are eligible to be student members of CIPHER. Programs: (suggested examples) Orientation to the conceptual underpinnings for interdisciplinary collaborative professional practice Interprofessional course teaching strategies for faculty Learning in an interprofessional collaborative environment for students Practicing in an interdisciplinary collaborative team Funding: An agreed upon sharing from each of the participating faculties will be provided on an annual basis to support the functioning of the CIPHER Organizational Structure: The CIPHER will be managed initially by one of the project coChairs and after the project period by an appointed Director. The Director will report to a council composed of one faculty member and one student member from each of the affiliated Schools/Departments.. The council will have a representative from each of the affiliated community agencies and consumer representatives. Strategic Planning: The CIPHER Council will develop a strategic plan for interdisciplinary health education and research initially focusing on undergraduate health professional and continuing professional education. Inclusive in this plan will be development of a program logic model for evaluation of actions taken. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 29 Exhibit 2: Learning Foci for development of inter-disciplinary practice applied to mental health services in the community (Adapted from Orchard & Curran, 2003) Health Promotion Health Focus Setting Settings will include emergency shelters, emergency rooms, homes for special care and subsidized housing provided by the following agencies and through project partner CURA and CAREMH community links including: Issues Social (housing, income) Behavioural Medical (nutrition, oral, physical hygiene, AIDs, Hepatitis, other illnesses and disorders) Learning Mission Services, London Prevention Homes for Special Care Salvation Army Intervention London Health Sciences Centre, Mental Health Care Program Women’s Community House St. Joseph’s Health Care, Regional Mental Health Care, London Counselling/ working with client and families to address social issues. Evaluating strategies to promote compliance with medical regimes prescribed to prevent clients readmitting to hospitals or on the street. Locating accommodation or other special services Counselling client/families Treatment for physical problems Determination of Cultural issues Identification of Community political issues Identification of health status of community members Identification of environment within the community (water, food, air) Assessment of determinants of health within setting Identification of issues impacting on determinants of health Working within community groups Development of plan, in consultation with community leaders, to address issues leading to problems in meeting determinants of health Setting of indicators to measure impacts of interventions Evaluation of indicator achievement Assessment of health problems within a community setting through use of existing data bases. Exploration within inter-disciplinary group of all aspects associated with the development of the health problem Identification of aspects leading to development of health problem Selection of strategies that can reduce incidence of health problem within community Development of action plan to implement strategies identified Identification of indicators to assess success of implementation plan Evaluation of outcome of interventions over time. Identification of health promotion needs within community to support alleviation of health problem. Communication skills with patients Counselling skills with patients Health/physician assessment skills with patients Social assessment with patients and families Environmental assessment with patients and families Patient teaching with patients and families ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 30 Restoration Health Focus Setting London Mental Health Crisis Centre Issues Learning Evaluation of outcomes of interventions Revision of intervention plans of care Patient teaching with clients and families around prevention of recurrence of problem(s) Counselling on wellness approaches to restore appropriate levels of health Rehabilitation Emergency Rooms Evaluation of progression towards outcome goals Revision of plan of care and expected short-term goals based on evaluation Patient teaching with clients and families toward next set short-term goal Counselling regarding impact of recovery phase on family, and normal roles ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 31 Exhibit 3: Outline for Team Process Modules (1) Awareness of the realities of clinical practice and its limitations to interprofessoinal collaborations This module will focus on three broad barriers to interprofessional collaborations: organizational structuralism, power imbalances, and role socialization. In the sub-unit on organizational structuralism learners will explore how organizations are seen to be just; in particular how health professionals view both distributive and procedural justice and expand this to the extent that patients’ have the right to selfdetermination. Finally, learners will explore the extent to which organizations share power with patient and health professionals. In the sub-unit on power imbalances learners will explore four groups of conflicts: role, goal, between health professional and others, and among health professionals. They will discuss accountability issues, role overload, and role ambiguity that lead to role conflicts, then health professionals’ dissimilar philosophies, beliefs, and professional socializations that cause goal conflicts. Further discussion will focus on group differing values, work styles, personality traits that can lead to conflicts between health professionals and other. Finally, learners will explore how professional isolation within each health discipline and approaches to assessing clients can lead to conflicts among health professionals. In the third sub-unit leaders will explore how they have been socialized into each of their health professions. They will focus on their patterns of practice that are shaped by their occupational knowledge (patterns of language, modes of dress, demeanor, norms of behaviour) and their occupational orientation (e.g. views regarding leadership, authority, collegialism, preference or working within organizational structures). (2) Helping groups re-conceptualize the way they wish to view and enact interprofessional practice. Sub-units will address the questions: (a) Whose knowledge and skill is it anyway – boundaries of practice; and (b) What value does each health professional bring to interdisciplinary practice? Learners will begin by working on role clarification within their own health profession developing a clear understanding of their own roles and expertise, gaining confidence in own abilities, recognizing boundaries of their own discipline, committing to the values and ethics of their own profession, and gaining knowledge of their own disciplinary practice standards. Whose knowledge and skill is it anyway – Boundaries of practice? Learners will explore the boundaries that control their practice that arise from various sources including: between professional groups, inter-agency, between health and social care, between responsibility of service users and health care professionals, between proximal and distal knowledge What value does each health professional bring to interdisciplinary practice? ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 32 Learners will discuss how to show respect for knowledge and contributions all members bring to the group, including development of clear understandings of unique contributions each will bring, and then how each will share self, ideas, responsibilities, aspirations, disagreements. They will further explore how to effectively negotiate within a team while ensuring that the contributions of all members are valued through openness, respect, safe expression of opinion and feelings without retribution. (3) Developing norms for interdisciplinary collaborative teams and their practice Learners, working in teams will establish their norms for functioning that facilitate power sharing based on individual’s knowledge and expertise, including how to ensure that trusting relationships guide functioning including: how to cooperate and share responsibility for patients’ care from planning to decision-making. Teams will consider how they will work collaboratively in: assessing patients, exploring options for care/services, selecting choices from among alternatives, processes for implementing the plan, and acceptance of individual responsibility for the plan. Finally, learners will create operational procedures that reflect team effectiveness including: setting a shared vision, goals, roles among professionals, management of decision making; creating patterns of functioning around task accomplishment, leadership, goals settings, influencing, role negotiating, trust building, problem solving problem setting; inter-group communications including information around meetings, and other methods, and handling (managing) of disagreements and conflicts including acceptance of disagreements, identifying issues that are likely to cause dissent, and developing methods for dealing with conflict. (4) Creating means for testing the model with patient groups (e.g. assessing outcomes in interdisciplinary practice – health professionals and patients perspectives). Learners will explore how to set results for each patient group including improvement in their health outcomes and satisfaction with their involvement in their care and assess achievement as well. Both learners and patient groups will be asked to assess their empowerment through interprofessional practice. Teams will explore various instruments available to measure outcomes of their practice and how to track the continuity of actions in support of agreed upon plan of care/services for patients. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 33 Exhibit 4: Project Steering Committee Purpose: To provide ongoing collaborative input to and decision making for project activities including monitoring of phase planning, implementation, evaluation and creation of a permanent sustainable structure for interprofessional education and research. Structure: There will be an overall Steering Committee with four working groups: (a) the Curriculum Working Group; b) Practice Site Working Group; (c) Education Program Development Group; and d) Evaluation Working Group. Each working group will have a member of the Steering Committee who will either act as chair or participate to provide a communication linkage between the Project Steering Committee and the work within each working group. Reporting relationships: The Steering Committee is accountable to the Deans of the Faculty of Health Sciences and the Schulich School of Medicine & Dentistry of the University of Western Ontario (principal applicant). Specifically: 1. To plan, develop, implement, and evaluate learning opportunities that will socialize health care providers’ interprofessional education and practice among health professional students; 2. To provide for faculty and health professionals to discuss health issues that relate to interprofessional study and practice; 3. To support development of interprofessional curricular models, at pre-licensure and post-licensure levels for health professional students; 4. To provide workshops to assist faculty wishing to develop interprofessional teaching/learning strategies in the educational settings; 5. To facilitate collaborative development of practice areas, simulated and actual, on the university campus and in participating community agencies that support clientcentred interdisciplinary collaborative professional practice; 6. To sponsor continuing education offerings on client-centred interdisciplinary professional practice topics for practicing health professionals in partnering agencies 7. To provide a means for educating the partnering agencies about their role involvement in interdisciplinary collaborative practice; 8. To support studies related to evaluation of client-centred interdisciplinary collaborative professional practice; 9. To support student and health professional projects using client-centred interdisciplinary collaborative practice approaches; 10. To provide health professional students, faculty and practitioners for an opportunity for discourse around the merits of interdisciplinary collaborative practice; 11. To review and approve reports prepared for the funders and partners in this project as agreed to in the project plan. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 34 Members 2 project Co-chairs 5 faculty members (each representing a participating health professional group) 5 students (each representing a participating health professional group) 4 community health agency representatives (from partnering agencies) 4 consumer representatives (from partnering agencies) 1 Project coordinator (ex-officio) 1 Research Associate (ex-officio) 1 Dean Faculty of Health Sciences (ex-officio) 1 Dean Faculty of Medicine & Dentistry (ex-officio) Meetings: During the first 6 months of the project the Steering Committee will meet monthly and then bi-monthly throughout the duration of the project. Documentation and decision-making: Summaries of all meeting discussions and decisions will be recorded as minutes by the project coordinator. Decision making will be arrived at through consensus of all participants. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 35 Exhibit 5: Monitoring & Formative Evaluation #1 Socialize health care faculty, students, and practitioners in working together, with shared problem solving and decision making, toward enhancing benefits for people receiving community-based health services. OBJECTIVES PROCESS OUTPUTS Sensitization of faculty and students to the issues, disciplinary norms, administrative structures and power imbalances that undermine IP client cenrred practice Role Clarification, Trusting Relation-ships and Shared decision-making in planning and implementing IP self-directed teams learning contracts. WORKPLAN/ IMPLEMENTATION Phases 1,2,3,4 (T1, T2)* - Appoint steering committee - Development of infra-structure. - Launch and develop structure of CIPHER - Workshop for leaders/ mentors/ students/ community partners. - Development of curriculum Phase 4,5 – Development of Learners (T1, T2)* - Core concepts of IP introduced within own disciplies - Train mentors - Online modules: conflict resolution, critical appraisal, communicaton skills, ethical practice - Simulation. Standardized patient exercise [SP] - Clinical skills facility - self-directed problem based learning skills - Development of learning contract with learner teams, faculty mentor and community partner. EVALUATION/ASSESSMENT [Reliability and Validity Indices] For Leaders, Mentors & Learners Focus Group Semi structured Interviews Faculty set criteria for evaluation of learning contracts. Focus groups addressing facets of collaboration and sharing that are necessary for teams offering mental health services and clients; visions, roles, approaches, and contributions needed to improve team collaboration for mental health care. TUTOR – PHC Team climate inventory (adapted: [Thames Valley Family Practice Research Unit (June 2004)] based on [Anderson, N. & West, M. A. [1998]); administered pre- and post- collaboration. [The 5 factor 38-item summarized version, as reported by Anderson et al. demonstrated robust psychometric properties, with acceptable measure of reliability and validity. Alpha coefficients range 0.84 and 0.94 indicating acceptable levels of internal homogeneity and reliability for all factors] Evaluation of workshop experience through post workshop reaction sheets. Focused interviews of learners, community leaders and mentors to assess process outcomes indicating progress toward trusting relationships (i.e. rapport, feeling of caring/being cared about, experience of hope for a better service). ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 36 #4: Increase the number of health professionals trained for collaborative client-centred practice before, and after entry into practice #3: Increase the number of educators prepared to teach from an inter-professional collaborative client-centred perspective. #2: Stimulate networking and sharing of best educational approaches for collaborative client-centred practice OBJECTIVES PROCESS OUTPUTS Networking amongst faculty, students, agencies and consumers of health and social services Activities to promote collaborative IP client-centred education for mental health care and practice for mental health services delivery WORKPLAN/ IMPLEMENTATION EVALUATION/ASSESSMENT [Reliability and Validity Indices] Phases 1,2,3,4,5,6 (T1, T2)* This will be done in all phases through workshops, knowledge dissemination strategies and utilizing faculty, students, clients and community agencies to mentor and advise. For Learners Focus Group interviews, with, purposefully selected, 5- 7 learning/teaching teams, containing both learners and mentors/leaders to discuss the meaning of their interprofessional learning to discover what each learned about roles that other health discipline professionals can provide within mental health services; what increase in personal learning exposure to this training; how it will further professional practice? In addition to implementation as outlined in Phases 1,2,3,,4 and 5 above, Phase 6 will involve student practice teams experience of working with clients in a community setting. Analysis of reflective summary of experiences recorded by participants. Phase 7 (T1, T2, T3)* Evaluation of site visits Evaluation of process For Educators/Health Professionals Interprofessional Education Perception Scale (Ducanis & Golin, 1981) [Content validity established by direct nature of questions. Reliability established through test-retest procedure over three weeks. Exact agreement ranged from 72% to 86%.] Interprofessional Team Performance Scale (Temkin-Greener et. al, 2004) [Reliability range from .76 to .89 (Cronbach’s ); construct validity demonstrated through results of regression analysis] Make recommendations for curriculum or organizational improvement. For Organizers/Administrators Data on health outcomes as established by partner agencies Data on client safety identified in collaboration with Steering Committee ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 37 LONGER TERM GOAL: #6: Augment the work toward provincial priorities, including: mental health care reform; care of the homeless; development of Local Health Integration Networks (LHINs) LONGER TERM GOAL #5: Facilitate inter-professional collaborative care in both education and practice settings OBJECTIVES PROCESS OUTPUTS WORKPLAN/ IMPLEMENTATION System: Incorporate learning of mental health care practical knowledge gained in community to classroom, to refine practice definitions. Sharing in workshops, labs. Transfer learning to student groups, steering committee for development of future teams. Changes in mental health care service provision. Phase 7, (T1, T2, T3)* As well as ongoing knowledge dissemination and transfer strategies involving, via various communication means, all stakeholders and decision-makers to increase impact on system EVALUATION/ASSESSMENT [Reliability and Validity Indices] Varied purposeful sample of learners, mentors, and leaders will be selected to participate in taped focus group interviews to discuss the meaning of their interprofessional learning and interdisciplinary practice experiences. Qualitative data transcripts will be analyzed for themes and patterns affording insights into how best to promote success in the sustained interprofessional collaborative educational program and service delivery. All participating institutions will be asked to retain annual records. The following will afford measures of impact: - numbers of faculty participating in the project; - numbers of students participating in the project; - numbers of clients served by the interprofessional collaborative practice teams; - self-directed learning materials and forums developed; - workshop and conference agendas and participation rates; and - documents reflecting the contributions of the project to mental health reform and the development of the local Health Integration Network *[T1 =Baseline data, T2 = post simulated learning data, T3 = post practice data] ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 38 Exhibit 6: WORKPLAN TIMELINE ACTIVITY 2006 2007 JAN FEB MAR APR MAY JUN JUL AUG SEP OCT NOV DEC JAN FEB MAR APR MAY PHASE 1: Infrastructure Development (CIPHER) PHASE 2: Workshop (which begins the formal process of sensitization of leaders and mentors that will continue throughout the project) Sensitization of leaders and mentors continues to the end using feedback from focus groups and other feedback. PHASE 3: Community experiences PHASE 4: Development of integrating components PHASE 5: Development of student teams (Role clarification, trusting relationships, shared decision-making PHASE 6: Further development of student teams (Where students play a major role in developing and driving the process) PHASE 7: Evaluation of site visits and CQI NOTE: While evaluation in Phase 7 refers to site visits and related CQI, evaluation will be part of every phase. ________________________________________________________________________ UWO, Creating Interprofessional Collaborative Teams for Comprehensive Mental Health Services 39