Original Articles
advertisement

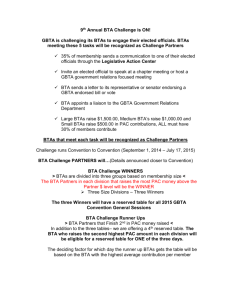
Journal of Pediatrics Volume 137 • Number 3 • September 2000 Copyright © 2000 Mosby, Inc. Original Articles An evaluation of botulinum-A toxin injections to improve upper extremity function in children with hemiplegic cerebral palsy Darcy Fehlings MD, MSc Mercer Rang MB, BS Janet Glazier BSc(OT) Catherine Steele PhD From the Division of Neurology and General Pediatrics, Department of Pediatrics and the Division of Orthopedics, Department of Surgery, Bloorview MacMillan Centre and The Hospital for Sick Children, Toronto, Ontario, Canada. Supported by the Easter Seal Research Institute (Kids Action Research). Submitted for publication Oct 13, 1999. Revision received Feb 23, 2000. Accepted Apr 28, 2000. Reprint requests: Darcy Fehlings, MD, MSc, Bloorview MacMillan Centre, 350 Rumsey Rd, Toronto, Ontario, M4G 1R8, Canada. Copyright © 2000 by Mosby, Inc. 0022-3476/2000/$12.00 + 0 9/21/108393 Objective: In a randomized, controlled, single-blind trial, to test the hypothesis that botulinum-A toxin (BTA) injections into the upper extremity of children with spastic hemiplegia improve upper extremity function. Study design: Thirty children with hemiplegia, aged 2.5 to 10 years, were randomly assigned to receive: (1) a BTA injection into 1 or more of 3 muscle groups (biceps, volar forearm muscles, adductor pollicis) plus occupational therapy or (2) occupational therapy alone. Blinded outcomes obtained at baseline and at 1, 3, and 6 months included the Quality of Upper Extremity Skills Test (QUEST), goniometry measurements, grip strength, and Ashworth scores. The caregiver completed the self-care domain of the Pediatric Evaluation of Disability Inventory. Results: Twenty-nine subjects completed the study. The QUEST demonstrated a significant improvement favoring the treatment group on a 2-way analysis of variance (F = 4.69, df = 1,83; P = .039). BTA treatment was also associated with an improvement in score on the self-care domain of the Pediatric Evaluation of Disability Inventory (F = 4.68, df = 1,82; P = .04). Conclusions: This study supports the effectiveness of BTA injections to improve upper extremity function of children with hemiplegia who have at least moderate spasticity. (J Pediatr 2000;137:331-7) ANOVA Analysis of variance BTA Botulinum-A toxin CP Cerebral palsy PEDI Pediatric Evaluation of Disability Inventory QUEST Quality of Upper Extremities Test See editorial, p. 300. Intramuscular injections of Clostridium botulinum-A toxin into spastic muscles cause a local temporary muscle paralysis associated with decreased spasticity. The biologic effects of BTA are well understood. [1] Botulinum toxin has been used therapeutically in adults over the last 25 years in neuromuscular conditions associated with focal dystonia (strabismus, torticollis).[2] The use of BTA in cerebral palsy[3] has received much interest recently because of the high prevalence of CP (1-2 in 1000 in developed countries)[4] [5] and conservative nature of the treatment. It is postulated that by decreasing spasticity, there will be improved control of movement patterns, stretching and increased excursion of shortened muscles, improved posture, and secondary strengthening of antagonistic muscles. By implication, these changes should be associated with improved motor function. Most studies to date have focused on the use of BTA injections into the lower extremity gastrocnemius muscle and have demonstrated a temporary reduction in spasticity, temporary improvement in gait, and improved range of motion.[6] [9] Minimal information is available on the impact on function of upper extremity injections in children with CP. Wall et al[10] report positive gains in function and cosmetic appearance in a prospective case series of 5 children with a "thumb in palm" deformity associated with CP treated with BTA injected into the adductor pollicis muscle and rigid splinting of the thumb.[10] Denislic and Meh[11] injected BTA into the upper limbs of 10 children with CP and found an improvement in upper limb function in 9. A double-blind controlled study by Corry et al[12] reports mixed results on the impact on function in hemiplegic CP. Functional improvements were not found 2 weeks after injection. A small improvement was found at 12 weeks, favoring the BTA group in a grasp-and-release activity, but was not found in another grasp activity (the ability to pick up coins). We report the results of a randomized, controlled, single-blind trial of BTA injections into the involved hand or arm of 30 children with hemiplegic CP using the Quality of Upper Extremity Skills Test, a standardized measure of quality of function of the upper extremity, as our principal outcome. METHODS Participants Eligible children met the following criteria: 2.5 to 10 years of age; a diagnosis of hemiplegic CP; moderate spasticity at the elbow, wrist, or thumb with a modified Ashworth score 2[13] ; full passive range (defined in this study as elbow extension to neutral, wrist extension to 30 degrees past neutral with the fingers extended, forearm supination to 30 degrees past neutral, and thumb extension to neutral); and the ability to initiate voluntary movement of the digits. Children were excluded if they were using a rigid splint to maximize homogeneity and allow active movement in the hand. Study Design The study was approved by the Bloorview MacMillan Centre Research Ethics Review Board. The ethics board, guided by Canadian ethical standards, did not grant approval for a double-blind BTA study in which the control group would receive an intramuscular injection of saline solution because this was judged to be too painful and invasive for a placebo.[14] When the eligibility criteria were met and written informed consent was obtained, children were randomly assigned, by using a uniform random number generator, to a treatment or control group. The treatment group received an intramuscular injection of BTA (Botox, Allergan, USA), at a dosage of 2 to 6 U/kg body weight, into at least 1 of 3 muscle groups (biceps, volar forearm muscles, or adductor pollicis muscle). Two investigators (D.F. and M.R.) determined jointly which muscle groups to inject during reach-and-grasp activities of the involved hand or arm. If the child demonstrated persistent elbow flexion, the biceps was injected; for thumb adduction, the adductor pollicis muscle was injected. In the volar forearm muscles, for pronation, the pronator teres muscle was injected; wrist flexion was an indication for flexor carpi ulnaris muscle injections; and finger flexion was an indication for injection of the finger flexors. The location of the injection was determined by anatomic knowledge and muscle palpation.[15] [17] The biceps was injected in the top third of the muscle at 2 sites, the volar flexor muscle was injected at 2 sites, 2 to 3 cm below the medial epicondyle. The pronator teres was injected at one site in the upper third of the muscle, and the adductor pollicis was injected in one site in the belly of the muscle. Children in both groups were asked to continue with community-based occupational therapy at a minimum frequency of one session every 2 weeks. Research funding was not available to provide occupational therapy by research personnel. An occupational therapy manual with guidelines was developed for the study and sent to each of the participating occupational therapists. The guidelines were based on standard practice for therapy management of spastic hemiplegia and incorporated activities for upper extremity strengthening and the development of skills for activities of daily living.[18] [19] Children were seen at baseline and at 1, 3, and 6 months. A single investigator (J.G.), blinded to the subject group assignment, obtained all objective outcome measurements. The primary outcome measure was the QUEST.[20] [22] This is an objective standardized measure evaluating the quality of upper extremity function in 4 domains: dissociated movement (an isolated joint movement of the upper extremity that counters a pattern of spastic synergy), grasp, protective extension, and weight bearing. Scores for the QUEST are calculated as percentages with a maximum score of 100. The QUEST was designed with minimal developmental sequencing so that scoring reflects the severity of the disability rather than age. A caregiver completed the self-care domain of the Pediatric Evaluation of Disability Inventory to assess the child's activities of daily living.[23] The self-care domain has 73 items in 15 skill areas, such as hand washing. Raw scores can be converted to a scaled score with a 0 to 100 distribution based on Rasch scale modeling. The PEDI has been designed to measure function in children with physical disabilities and has established reliability, validity, and responsiveness.[23] [26] Secondary outcome measures included manual goniometric measurements of passive range of motion[27] ; modified sphygmomanometer measurements of grip strength[28] ; and the modified Ashworth score of spasticity at elbow extension, wrist extension, forearm supination, and thumb extension.[13] Test-retest reliability for passive goniometry measurements and grip strength was evaluated before the study in children with upper extremity spasticity and was found to be high, with correlation coefficients ranging from 0.58 to 0.97.[29] Statistical Analyses The analyses were conducted by using the SAS microcomputer-based package. [30] The following tests were used. 1. A preliminary analysis included a thorough check of the data (review of outliers and missing data), a descriptive summary, and plots of each variable. 2. Chi-square and unpaired t tests were used to check the comparability of the BTA treatment and control groups at baseline for age, sex, involved side, and baseline Ashworth, QUEST, and PEDI scores. 3. A 2-way analysis of variance was computed to detect differences between the BTA treatment and control groups during the study period in the QUEST, the PEDI, grip strength, Ashworth scores, and passive goniometry measurements. To account for baseline effects, the differences between baseline and 1 month, baseline and 3 months, and baseline and 6 months were used. Statistical significance was set a priori at P < .05 for the 2 functional outcomes, the QUEST and the PEDI, and set at P < .01 for the secondary outcomes to account for the multiple testing. 4. A post hoc Wilcoxon rank sums test was performed to examine the significance of group differences at 1, 3, and 6 months for variables that demonstrated statistical significance on the ANOVA. RESULTS Participant Characteristics Fifty children were screened; 20 did not meet the eligibility criteria (13 had an Ashworth score <2, 6 had an inability to initiate voluntary movement in the involved hand, and 2 had fixed contractures). Thirty children were recruited into the study and randomly assigned to the treatment (n = 15) and control (n = 15) groups. Thus 29 children completed the study, with one child in the treatment group dropping out before the 1-month assessment. Table I outlines the comparability of the 2 groups at baseline. Table I. Baseline comparability of the treatment and control groups* Treatment group (n = 14) Control group (n = 15) P value 68 ± 31 64 ± 28 .71 Gender (M/F) 10/5 10/5 1.00 Involved side (right/left) 10/4 7/8 .17 Modified Ashworth score* 2.3 ± 0.75 2.2 ± 0.59 .89 QUEST baseline 19.2 ± 15.1 27.6 ± 19.0 .41 PEDI baseline 50.2 ± 11.1 52.2 ± 15.4 .25 56.40 ± 16.59 53.38 ± 21.33 .46 Characteristic Age (mo) Grip strength (mm Hg) Values are expressed as means ± SD. *Represents the mean of Ashworth measurements for elbow and wrist extension, forearm supination, and thumb extension. No significant differences were found. Table II outlines the BTA treatment for each child with respect to dosage and location. Table II. Dosage and location of injection for each participant in the BTA treatment group Muscle injected (U/kg) BTA (U/kg) QUEST change (to 1 mo) Volar flexors Pronator teres muscle Adductor pollicis muscle Biceps 1 4 36.67 -- 4.0 -- -- 2 4 4.48 -- 4.0 -- -- 3 2 19.36 2.0 -- -- -- 4 4 12.19 -- 4.0 -- -- 5 4 8.53 -- 4.0 -- -- Subject No. Table II. Dosage and location of injection for each participant in the BTA treatment group Muscle injected (U/kg) BTA (U/kg) QUEST change (to 1 mo) Biceps Volar flexors Pronator teres muscle Adductor pollicis muscle 6 4 23.90 -- 1.3 1.3 1.3 7 5.2 -1.97 -- 3.6 1.6 -- 8 3.8 21.37 -- 2.9 -- 1.0 9 4.3 2.21 3.2 1.1 -- -- 10 2.7 0.78 -- 1.8 -- 0.9 11 3.3 -9.71 -- 2.2 -- 1.1 12 3.6 30.18 1.8 -- -- 1.8 13 6.6 14.29 -- 4.9 -- 1.6 14 3.4 Dropout -- 1.1 1.1 1.1 15 6.3 12.79 1.6 3.2 -- 1.6 Subject No. Both groups received occupational therapy in the community at a recommended frequency of once every 2 weeks. The treatment group received a mean of 11.93 (SD 6.89) treatment sessions, and the control group received a mean of 16.07 (SD 7.60) treatment sessions over the 6-month period of the study. This difference favored the control group but was not statistically significant (P = .74). Main Results The total score for the involved side on the QUEST, the primary outcome measure, demonstrated a statistically significant improvement favoring the BTA treatment group on the ANOVA (F = 4.69, df = 1,83; P = .039). The time-group interaction was not significant (P = .50). Post hoc testing with the Wilcoxon rank sum test showed significant differences between the treatment and control groups at 1 month (P = .01) but not at 3 (P = .13) or 6 months (P = .14). These results are outlined in the Figure. Figure. Mean change from baseline in the QUEST total scores. Changes in scores were analyzed with 2way ANOVA. Post hoc Wilcoxon rank sums test was done at 1, 3, and 6 months. Asterisk indicates P < .05 on post hoc testing. On the 4 subtests of the QUEST, the subtest "weight bearing" (P = .009) showed a significant improvement favoring the treatment group. On the other 3 subtests, results favored the treatment group but were not statistically significant: "dissociated movement" (P = .63), "grasp" (P = .33), and "protective extension" (P = .55). The results of the PEDI and secondary outcomes are listed in Table III. Table III. Results of the 2-way ANOVA for the secondary outcome measures Change from baseline One month Three months Six months P value* BTA group 2.00 ± 5.99 3.85 ± 5.11 6.77 ± 5.82 .04 Control group -1.93 ± 5.78 1.13 ± 5.19 2.64 ± 5.75 BTA group 2.57 ± 6.91 2.78 ± 3.72 5.50 ± 4.54 Control group -1.51 ± 4.07 1.09 ± 4.07 3.30 ± 6.05 BTA group -7.60 ± 14.57 -6.86 ± 13.06 2.00 ± 12.74 Control group 1.50 ± 18.76 3.83 ± 22.81 -0.27 ± 20.77 BTA group -0.29 ± 0.47 -0.23 ± 0.48 -0.38 ± 0.46 Control group -0.20 ± 0.62 -0.37 ± 0.44 -0.29 ± 0.51 BTA group -0.43 ± 0.43 -0.31 ± 0.38 -0.35 ± 0.43 Control group -0.36 ± 0.44 -0.33 ± 0.45 -0.25 ± 0.55 BTA group -0.32 ± 0.42 -0.35 ± 0.38 -0.27 ± 0.60 Control group -0.20 ± 0.49 -0.20 ± 0.53 -0.18 ± 0.58 BTA group -0.31 ± 0.48 -0.25 ± 0.40 -0.33 ± 0.39 Control group -0.28 ± 0.57 -0.29 ± 0.54 -0.27 ± 0.48 BTA group 0.07 ± 6.62 5.46 ± 11.74 2.84 ± 6.69 Control group -0.80 ± 6.62 3.00 ± 12.83 0.79 ± 9.32 BTA group 3.43 ± 9.00 5.15 ± 8.10 3.00 ± 12.08 Control group 1.67 ± 5.63 1.67 ± 6.28 0.64 ± 6.62 PEDI (raw score) PEDI (scaled score) .08 Grip strength (mm Hg) .34 Ashworth/elbow .89 Ashworth/wrist .81 Ashworth/forearm .51 Ashworth/thumb .90 Elbow extension .11 Forearm supination Wrist extension .34 Table III. Results of the 2-way ANOVA for the secondary outcome measures Change from baseline One month Three months Six months P value* BTA group 4.08 ± 7.35 4.58 ± 11.92 2.00 ± 15.02 .55 Control group 0.67 ± 8.78 1.27 ± 9.91 2.07 ± 11.49 BTA group 2.14 ± 5.91 1.46 ± 8.52 2.77 ± 8.12 Control group 1.00 ± 7.97 -0.60 ± 10.01 1.21 ± 6.96 Palmar thumb abduction .48 Values are expressed as means ± SD. *P value refers to the significance of overall differences between the BTA group and control group on the ANOVA. Goniometry measurements. A statistical difference was found in the raw scores of the parent-completed self-care domain of the PEDI (F = 4.68, df = 1; P = .04). The time-group interaction was not significant (P = .84). Post hoc testing with the Wilcoxon rank sums test approached significance at 1 month (P = .08) and 6 months (P = .06). The corresponding ANOVA evaluating the PEDI scaled scores approached significance (F = 3.22, df = 1; P = .08). No significant differences between the treatment and control groups were found in grip strength, Ashworth scores, or passive goniometry measurements. The injections in the treatment group were well tolerated. Aside from the discomfort of the injection, only one child (Table II, subject 1) reported temporary decreased grip strength lasting 2 weeks. No other side effects were noted. DISCUSSION This controlled clinical trial provides evidence to support the use of intramuscular BTA injections to improve both quality of functional movement of the upper extremity and functional capability in children with hemiplegic CP. A clinical and statistically significant improvement in quality of function was found at 1 month. Children in the BTA group improved from 19.2% on the QUEST at baseline to 32.5% at 1 month compared with a 1.7% change in the control group. Moderate improvements were maintained up to 6 months after injection. This is clinically important because the effect of the BTA injection on function lasts longer than the neuromuscular blockade, which disappears, on average, at 3 months.[1] In the control group a gradual improvement in quality of function was found over the 6-month period of the study. The positive change in function in the control group may reflect both the impact of the occupational therapy intervention and developmental improvements with time; and this highlights the importance of including a control group when studying changes in child development. The improvement in the control group and low statistical power (16%) may explain the lack of statistical significance at the 6-month testing. Within the subtests of the QUEST, weight-bearing activities demonstrated the most change. For children receiving the BTA injections, the parents also reported small positive functional change in the children's self-care skills (eg, dressing, eating). This supports carry-over of functional change into the children's regular environments and daily activities. Grip strength declined at 1 and 3 months in the BTA group but normalized by 6 months after injection. This finding was expected because BTA blocks conduction at the neuromuscular junction, which reduces spasticity but also causes muscle weakness. Though the grip was weaker after BTA, function improved. Differences in the modified Ashworth score of spasticity favored the BTA group but were not significantly different. Both groups showed a decline in spasticity throughout the period of the study. It is interesting to speculate on the reason for the decline in spasticity within the control group. This may be secondary to developmental improvements in spasticity with time, familiarity with the test, the impact of the occupational therapy, or measurement variation. The ideal dosage of BTA for upper extremity spasticity requires further research. It is hard to predict the functional impact of higher dosing. Increasing the dosage will result in a greater decline in spasticity but will also lead to greater reductions in grip strength, which in turn may have a negative impact on functional outcome. Passive range of motion also did not show a significant change between the BTA and control groups. This reflects the excellent baseline flexibility of the selected subjects who had full range in the majority of joint measurements assessed. It is important to note that the positive effects on upper-extremity function observed after BTA injection are generalizable to children who are clinically similar to the subjects selected for the study. Many children with a clinical diagnosis of spastic hemiplegic CP have Ashworth spasticity scores <2 or poor distal voluntary muscle control. This clinical trial excluded both of these groups of children. Further research is required before results are generalized to these subgroups. A limitation of the study is the single-blind design. Both the children and their parents knew whether they were in the treatment or the control group. This could have an impact on the parent-completed PEDI. A single objective evaluator who was blinded to the group assignment completed all other outcome measurements, including the QUEST. The large number of subjects assessed and the similarity of changes in Ashworth score between the 2 groups prevented the unintentional unblinding of this evaluator, minimizing the impact of the single-blind design on the primary results of this study. Botulinum toxin injections were given without electromyographic guidance. This has the advantage that conscious sedation is not required, which has fewer side effects and allows the use of BTA in ambulatory and rehabilitation settings. Evaluation of the individual responses of subjects showed that the BTA injection was successful (positive change >5% on the QUEST) in 9 of 14 subjects. However, 5 subjects (33%) received a BTA injection but did not show improvement in function. One potential explanation for this is that the intended muscle groups were not targeted accurately. There is some support for improved accuracy of BTA injections with electromyographic guidance in the literature.[31] Continued research is required to evaluate the dose response and the impact on function of repeated BTA upper-extremity injections. We thank the children and families who participated in the study. We also thank Allergan for providing the botulinum-A toxin for the study. REFERENCES 1. De Paive A, Meunier FA, Molgo J, Aoki KR, Dolly JO. Functional repair of motor endplates after botulinum neurotoxin type A poisoning: biphasic switch of synaptic activity between nerve sprouts and their parent terminals. Proc Natl Acad Sci U S A 1999;96:3200-5. Abstract 2. Jankovic J, Brin MF. Therapeutic uses of botulinum toxin. N Engl J Med 1991;324:1186-94. Citation 3. Gordon N. The role of botulinum toxin type A in treatment--with special reference to children. Brain Dev 1999;21:147-51. Abstract 4. Kuban K, Leviton A. Cerebral palsy. N Engl J Med 1994;330:188-95. Citation 5. Murphy CC, Yeargin-Allsopp M, Decoufle P, Drews CD. Prevalence of cerebral palsy among ten-year old children in metropolitan Atlanta, 1985 through 1987. J Pediatr 1993;123:S13-S20. Abstract 6. Cosgrove AP, Corry IS, Graham HK. Botulinum toxin in the management of the lower limb in cerebral palsy. Dev Med Child Neurol 1994;36:386-96. Abstract 7. Koman LA, Mooney JF III, Smith BP, Goodman A, Mulvaney T. Management of spasticity in cerebral palsy with botulinum-A toxin: report of a preliminary, randomized, double-blind trial. J Pediatr Orthop 1994;14:299-303. Abstract 8. Calderon-Gonzalez R, Calderon-Sepulveda R, Rincon-Reyes M, Garcia-Ramirez J, Mino-Arango E. Botulinum toxin A in management of cerebral palsy. Pediatr Neurol 1994;10:284-8. Abstract 9. Sutherland DH, Kaufman KR, Wyatt MP, Chambers HG. Injection of botulinum A toxin into the gastrocnemius muscle of patients with cerebral palsy: a 3-D motion analysis study. Dev Med Child Neurol Suppl 1995;73:17-8. 10. Wall SA, Chait LA, Temlett JA, Perkins B, Hillen G, Becker P. Botulinum A chemodenervation: a new modality in cerebral palsied hands. Br J Plast Surg 1993;46:703-6. Abstract 11. Denislic M, Meh D. Botulinum toxin in the treatment of cerebral palsy. Neuropediatrics 1995;26:24952. Abstract 12. Corry IS, Cosgrove AP, Walsh EG, McClean D, Graham HK. Botulinum toxin A in the hemiplegic upper limb: a double-blind trial. Dev Med Child Neurol 1997;39:185-93. Abstract 13. Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 1987;67:206-7. Abstract 14. Medical Research Council of Canada. Guidelines on research involving human subjects. Ottawa, Ontario, Canada: Ministry of Supply and Services Canada; 1987. 15. Russman BS, Tilton A, Gormley ME. Cerebral palsy: a rational approach to a treatment protocol, and the role of Botulinum toxin in treatment. Muscle Nerve Suppl 1997;6:S181-S193. Abstract 16. Thompson 17. Brash JS. Core textbook of anatomy. Philadelphia: Lippincott; 1977. JC, editor. Text-book of anatomy. 9th ed. London: Oxford University Press; 1951. 18. Boehme R. Improving upper body control: an approach to assessment and treatment of tonal dysfunction. Tucson: Therapy Skill Builders; 1988. 19. Exner CE. Development of hand skills. In: Pratt PN, Allen AS, editors. Occupational therapy for children. 3rd ed. St Louis: Mosby; 1989. p. 268-306. 20. DeMatteo C, Law M, Russell D, Pollock N, Rosenbaum P, Walter S. Quality of Upper Extremity Skills Test. Hamilton, Ontario (Canada): Neurodevelopmental Clinical Research Unit; 1992. 21. DeMatteo C, Law M, Russell D, Pollock N, Rosenbaum P, Walter S. The reliability and validity of the Quality of Upper Extremity Skills Test. Phys Occup Ther Pediatr 1993;13:1-18. 22. Law M, Cadman D, Rosenbaum P, Walter S, Russell D, DeMatteo C. Neurodevelopmental therapy and upper extremity inhibitive casting for children with cerebral palsy. Dev Med Child Neurol 1991;33:379-87. Abstract 23. Haley SM, Coster SJ, Ludlow LH, Haltiwanger JT, Andrellos PJ. Pediatric evaluation of disability inventory (PEDI): development, standardization, and administration manual. Boston: New England Medical Center and PEDI Research Group; 1992. 24. Haley SM, Ludlow LH, Coster WJ. Pediatric Evaluation of Disability Inventory: clinical interpretation of summary scores using Rasch rating scale methodology. Phys Med Rehabil Clin North Am 1993;4:52940. 25. Reid DT, Boschen K, Wright V. Critique of the Pediatric Evaluation of Disability Inventory. Phys Occup Ther Pediatr 1993;13:57-87. 26. Wright V, Boschen KA. 2nd National Rehabilitation Research Conference: outcome assessment in rehabilitation. The Pediatric Evaluation of Disability Inventory (PEDI): validation of a new functional assessment outcome instrument. Can J Rehabil 1993;7:41-2. 27. Trombly CA, Scott AD. Occupational Therapy for physical dysfunction. Baltimore: The Williams and Wilkins Company; 1977. 28. Helewa A, Goldsmith CH, Smythe HA. The modified sphygmomanometer--an instrument to measure muscle strength: a validation study. J Chronic Dis 1981;34:353-61. Citation 29. Glazier JN, Fehlings DL, Steele C. Test-retest reliability of upper extremity goniometric measurements of passive range of motion and of sphygmomanometer measurement of grip strength in children with cerebral palsy and upper extremity spasticity. Dev Med Child Neurol Suppl 1997;75:33-4. 30. SAS Institute Inc. SAS STAT user's guide, version 6. 4th ed. Cary (NC): SAS Institute Inc; 1989. 31. Ajax T, Ross MA, Rodnitzky RL. The role of electromyography in guiding botulinum toxin injections for focal dystonia and spasticity. J Neurol Rehabil 1998;12:1-4.