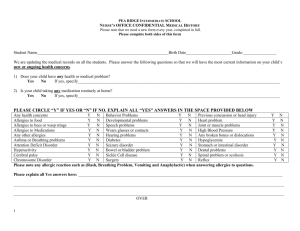
New Patient Information Sheet
advertisement

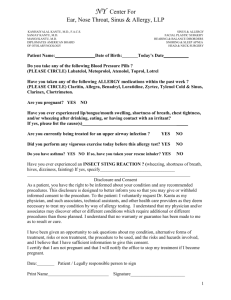
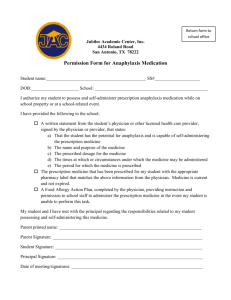
TODAY’S DATE:___________________________ Patient Name: ______________________________ MRN: ___________________________ Social Security #: ____________________________ Date of Birth: _____________________ Occupation: ____________________________________________________________________ Who has referred you for this visit? __________________________________________________ Referring Physician address: _______________________________________________________ What is the reason for your visit today? ______________________________________________ ALLERGIES: Please list any medication, for or other allergy and type of reaction. Allergy Description of Reaction MEDICATIONS: Please list current prescription and non-prescription drugs/dosage you are taking. Medication Circle Prescription (P) or Dosage Non- Prescription (N) P N Do you take aspirin or any blood-thinning medications? P N P N P N Y N Name/Dose: _________________________ SURGERIES: Please list past surgical procedures (date and reason for surgery) Date Reason Patient Name: ________________________________ Date of Birth: _________________ MEDICATION LIST ALERGIES/REACTION ACTIVITIES OF DAILY LIVING Do you have difficulty with any physical movement that might affect the way we provide your care? ____Y ______N If yes, please circle all applicable: Talking Eating/Swallowing Speech Standing Walking Transfers Do you have a hearing or speech impairment? _______Y _______N Hearing? Speech? Is English your primary language? ___Y ____N If no, what is your primary language______________ What is your preferred learning style? Can you read? ___Y ____N Written Verbal Can you write? ____Y ____N Demonstration What is your highest level of education? DIET How is your appetite? Good Fair What is your normal diet? Regular Or Pediatric: Bottle Breast Poor Soft Liquid Tube Low Sodium Diabetic Table Food Do you take any nutritional supplements? ____Y ____N If yes, what kind____________ How many glasses of water do you drink per day? ____________________________________________ Without wanting to, have you lost or gained 10 or more pounds in the past 6 months? ____Y ____N *If yes, Gained? Lost? ________ #of Pounds Lost or Gained Do you weigh more than 350 pounds? _____Y ______N Do you have any metal implants, devices, pacemaker, etc? _____Y ____N If so, specify:____________ HABITS: Do you currently use tobacco products? ______Y ______N *If yes, please circle all that apply: Cigarettes, Cigar, Pipe, Smokeless Tobacco (snuff, chew, dip) How much per day_______________________ How many years___________________ *If no, have you ever smoked? _____Y _____N If yes, how many years did you use tobacco ______________ When did you stop___________ *Does anyone around you at home smoke? _____Y _____N Do you use Alcohol? _____Y _____N If yes, how many drinks per day? ______ Per Week?_________ How many cups/glasses of caffeinated beverage do you drink per day? ___________________________ FAMILY HISTORY Alcoholism Asthma Bleeding disorder Cancer Diabetes Heart Disease Thyroid Disease Other: ____________ PARENT _________ _________ _________ _________ _________ _________ _________ _________ SIBLING _________ _________ _________ _________ _________ _________ _________ _________ GRANDPARENT ________________ ________________ ________________ ________________ ________________ ________________ ________________ ________________ Please check all that apply to the patient: Yes _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ Health conditions for which you see another physician: No _______ Appetite Change _______ Bad Breathe _______ Blurry vision related to sinus Infection _______ Breathing difficulties _______ Claustrophobic _______ Cough _______ Decreased taste or smell _______ Dizzy Spells _______ Ear infections, frequent _______ Ear Pain _______ Facial/sinus pain _______ Fatigue _______ Fevers _______ Headache _______ Pain in facial area _______ Hearing Loss _______ Injury to facial bone _______ Meniere’s Disease _______ Nasal congestion _______ Other pain in head or neck _______ Post Nasal Drip _______ Previous injury to nose When/Where___________ _______ Reflux/Heartburn _______ Ringing/buzzing in ears _______ Sinus Disease _______ Tonsillitis, frequent ________________________________________ Patient Signature Yes _______ _______ _______ No _______ Allergies _______ Allergy Shots _______ Arthritis _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ _______ Asthma _______ Blood Sugar _______ Bronchitis _______ Cancer _______ Diabetes _______ Endocrine disorder _______Gastrointestinal disease _______ Hay fever _______ Heart Problems _______ High Blood Pressure _______ Immunotherapy _______ Join/bone Disease _______Kidney/bladder Disease _______ Liver Disease _______Mental Disorder _______ Neurologic Disorders _______ Pregnant _______ Seizures _______ Skin Changes _______ Stroke _______Thyroid Disease _______ Tuberculosis (family?) _______Ulcers I have reviewed and confirm the Review of Systems, Past History, Family History, and Social History as completed herein by the patient. ________________________________________ Guardian, if applicable ________________________________________ Relationship to Patient _______________________________________ Physician Signature Date