9. Comprehensive Nursing Home, pain, poor nutrition, decubitis
advertisement

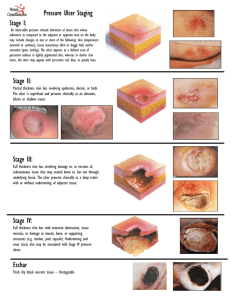
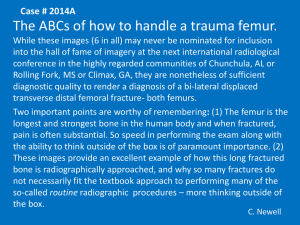
Comprehensive Nursing Home, pain, poor nutrition, decubitis ulcer, parotitis TC is a 98-year-old Caucasian, widowed, female resident in nursing home since July 1990. Cognitive status is compromised due to pain and Alzheimer’s dementia. Source of the history is exclusively from the client’s chart and nursing home staff. CHIEF COMPLAINT Client has 4 current problems to be addressed. 1. Pain. Client atraumatically fractured her right distal femur 10/05/95. She was evaluated at Hospital and a right AKA was suggested. Her family decided against it and TC was returned to the nursing home on 10/08/95. She continuously moans and screams out with turns. Demerol 25 IM q 4 hours provides 1-3 hours of relief. 2. Nutritional impairment. Client has been decreasing her oral intake since July 1995. According to nursing home staff and dietary records, she has only taken in approximately 500 cc/shift of clear liquids in the past 72 hours. Prior to the femur fracture, she was taking in approximately 1500 calories/day for the past 2 weeks. 3. Stage II decubitis ulcer right gluteal fold lateral to the sacral bone. Ulcer is 5mm x 5mm, round, present for 3 weeks and has not improved with current treatment of bacitracin and telfa. 4. Parotiditis left parotid gland present 10/06/95, unknown etiology. PAST HISTORY General state of health: According to staff and records, TC has been slowly deteriorating since July 95. She is uncomfortable since returning from the hospital. Childhood illnesses: Measles, mumps – dates unknown. Adult illnesses: Hypertension 1980. Duodenal ulcer and gastritis 1985. Alzheimer’s dementia 1991. Accidents and injuries: Right femur fracture 1995. Hospitalizations/Surgeries: Cholecystectomy 1965. Psychiatric illnesses: Depression 1986. CURRENT HEALTH STATUS Allergies: Penicillin 9hives). Immunizations: Td 1993. Pneumovax 1993. Flu shot 1994. PPD 1993. Screening: Mammogram 1980, annual dental and eye exams 4/95. Pap 1993. Safety measures/Environmental hazards: Bed rest. Side rails up at all times while in bed. Exercise and leisure activities: No exercise since femur fracture. Attended nursing home activities prior to fracture. Sleep patterns: Bed rest. Rests intermittently between turns and pain injections. Diet: As tolerated. Taking only H2O the past 16 hours. Current Medications: - Prednisone 30 mg po q day x 7 days (10/08/95 – 10/15/95) for parotiditis - Zantac 150 mg p.o. bid while on prednisone. - Rocephin 1 gm IM q 24 hours x 5 days (10/08/95 – 10/13/95) for parotiditis. - Pamelor 30 mg PO q hs for depression. - Prilosec 20 mg PO q day for ulcer prophylaxis. - Maxide I PO bid for hypertension. - ES Tylenol 1000 mg qid prn. - Ativan .25 mg PO prn anxiety. Tobacco/Alcohol/Illicit drug use: Never, according to records. FAMILY HISTORY TC is widowed and has no children of her own. Her nephew is her power of attorney and 2 nieces remain active in their concern. TC was born in Iowa. She worked for her parents in their general store. She was educated through high school and married her only spouse when she was 25. Her father died of heart failure in his 50s and her mother lived until 94, dying of natural causes. One of her 2 sisters is deceased from ovarian cancer in her 60s and the other is alive in her 90s with Alzheimer’s as well. PSYCHOSOCIAL HISTORY TC is a permanent resident of this facility since 1993. She is Lutheran. She had been active in the facility most recently with declining involvement in the past 6 weeks. Her nieces visit weekly. Her sister hasn’t visited in several months due to declining health. TC is a DNR/DNI. Her nephew has decided against IVs, tube feedings, antibiotics, and further hospitalizations. Comfort measures only. Nieces are in agreement and very supportive. REVIEW OF SYSTEMS Unobtainable. Patient only moans and doesn’t answer specific questions. PHYSICAL EXAM General survey: TC is a pale, elderly, uncomfortable woman in bed. BP 138/62, RR 24, HR 88, T 100.8 Ht. 5’2” Wt. 158 lbs. WBC 12,000 10/07; Hgb 9.9 10/07. Right femur x-ray, displaced distal supracondylar femur fracture. Skin: Pale, warm and dry. Poor turgor, multiple ephelides and nevi on chest and back, nails short and clipped. 5mm x 5mm round, open pressure sore on right gluteal fold stage II; edges pink with small moist white center. Head: Hair is white, thin, dry. Scalp and skull without masses. Eyes: PEERLA, sclera white without discharge, eyes and brows symmetrical. Ears: Pale, smooth, canals clear, drums negative. Nose/Sinuses: Mucosa pale without discharge. Mouth: Edentulous, mucosa pale but intact, gums without swelling; edema left inner cheek at parotid gland, tender to touch, warm. Neck/Lymph glands: Trachea midline, left parotid gland enlarged to golf ball size, with subsequent enlargement of right and left submandibular lymph glands, other nodes negative. Breasts: Without masses or discharge, axillary nodes negative. Thorax/Lungs: Thorax symmetrical, lungs clear, no adventitious sounds. Peripheral vascular: 3+ radial and 1+ left pedal pulse. No palpable pedal or post-tibial pulse palpable on right leg; bilateral feet cool, right foot eccymotic on posterior surface with small stage 1 ulcer on right heel. Cardiac: Regular apical pulse at 5th ICS; no lifts, heaves, thrills, gallops, or murmurs; negative carotid bruit. Abdomen: Large, round, soft; bowel sounds active x 4 quads; liver and spleen nonpalpable. Musculoskeletal: Obvious deformity right leg above knee, hallux valgus with hammer toes bilateral feet, kyphotic spine, generalized pain with any movement. Genitalia: Indwelling foley catheter, pelvic not performed due to pelvic 1993 and discomfort of patient. Rectum: Rectum without masses or stool, small external hemorrhoids. Neurological: Lethargic, oriented to self only, unable to follow commands to examine cranial nerves II-XII, sensation grossly intact throughout, bicep reflexes 1+ bilaterally.