template - Alliance for Advancing Nonprofit Health Care
advertisement

California Hospital Medical Center
Community Benefit Report 2008
Community Benefit Plan 2009
TABLE OF CONTENTS
Executive Summary
3
Mission Statement
CHW Mission Statement
CHMC Mission Statement
13
13
Organizational Commitment
14
Community
Definition of Community
Community Needs and Assets Assessment Process
17
21
Community Benefit Planning Process
Developing the Hospital’s Community Benefit Report and Plan
Planning for the Uninsured/Underinsured Patient Population
34
94
Plan Report and Update including Measurable Objectives and Timeframes
95
Program Digests
Type 2 Diabetes Prevention, Screening, and Intervention Program
Hope Street Family Center Early Head Start Program
Hope Street Family Center Family Literacy Program
Health Ministry Program
Healthy Eating Lifestyle Program
Para Su Salud
Hope Street Family Center School Readiness Program
Community Benefit and Economic Value
Report – Classified Summary of Unsponsored Community Benefit Expense
Communication Plan
97
104
112
120
124
127
130
138
Attachments
Charity Care Policy
Community Needs Index, Map of the Community
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
2
EXECUTIVE SUMMARY
Primary Service Area:
City of Los Angeles, including downtown, central and
south Los Angeles
Facility Type:
Not for profit
Total Licensed Beds:
316
Number of Employees:
1,186 (meets community requirements for Major Employer)
Year Established:
1887
Ethnic Mix of Patients:
67% Hispanic; 20% African American;
6% Caucasian; 6% Asian; 1% other
Payer Mix of Patients:
65.7% Medi-Cal, 14.3% Medicare; 16.3% HMO/PPO;
5% Self-Pay
Annual Emergency Services
Statistics:
48,708 Emergency Services visits
33% Medi-Cal Emergency Services visits
20% Indigent Care Emergency Services visits
President:
Mark A. Meyers
(213) 742-5778 (phone) | (213) 765-4078 (fax)
Senior Vice President
Business Development:
David Mauss
(213) 742 5693 (phone) | (213) 742 6405 (fax)
City Council Representative:
County Supervisor:
Assembly Member:
State Senator:
Congressional Representative:
Jan Perry, Council District 9
Gloria Molina, District 1
Fabian Nunez (D), Assembly District 46
Gil Cedillo (D), Senate District 22
Lucille Roybal-Allard (D), Congressional District 33
Hospital Services:
Emergency and Trauma Services
Obstetrics, Neonatal Intensive Care, Pediatrics,
Medical/Surgical Services, Critical Care,
Orthopedics, Skilled Nursing, Cancer Care
Community Benefit Programs:
Health Ministry Program; Para Su Salud Program; Healthy
Eating Lifestyle Program; Type 2 Diabetes Prevention,
Screening and Intervention Program; Community Dental
Partnership; Hope Street Family Center Early Head Start
Program; Hope Street Youth Center; School Readiness
Program; Child Development Center; Early Childhood Center;
Early Care & Education Center; Family Childcare Network;
Central High School; Pico Union Family Preservation Network;
Nurse Family Partnership; Responsible Fatherhood Program;
Healthy Marriage Program; Los Angeles Best Babies Network’s
Center for Healthy Births.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
3
Since 1887 California Hospital has been at the heart of downtown and
active in caring for our downtown and inner city communities. The 316-bed
private, non-profit hospital is a leader in acute care services and in the
development of innovative programs that make a difference in both the
local community and the medical profession.
The J. Thomas McCarthy Center for Emergency Services is the only full-service, 24-hour
emergency department in central Los Angeles, serving more than 45,000 patients per year.
In December 2004, CHMC opened its Level II Trauma Center—the first new trauma center
to open in more than a decade and one of only 13 in Los Angeles County. CHMC’s trauma
team is ready 24 hours a day, 7 days a week, and cares for an average of more than 185
patients per month. These patients span a diversity of ages and walks of life, and require
life-saving care following severe car crashes and industrial or other accidents. The
availability of trauma care at California Hospital is critical for those who live in, work in, or
visit the greater Los Angeles area.
High quality, cost-effective, state-of-the-art cancer care is provided by the Donald P. Loker
Cancer Center.
The Keith P. Russell Women's Health Center provides complete gynecological and
obstetrical services, including a birthing center featuring nurse midwives and birthing tubs
for water births.
A comprehensive prenatal program, Babies First/Primeros Pasitos offers expectant
mothers friendly and efficient service in a relaxed setting, leading up to labor and delivery.
Para Su Salud (For Your Health) aims to increase the enrollment and retention of eligible
residents in health insurance programs, especially Medi-Cal and Healthy Families.
The Hope Street Family Center works to (a) enhance the overall development of children,
(b) strengthen the economic and social self-sufficiency and stability of families, and (c)
enhance the local service delivery network of agencies serving young children and families.
The Hope Street Family Center (HSFC) impressive list of awards:
2002 American Hospital Association’s NOVA Award Winner. This award recognizes
collaborative projects aimed at improving the health status of communities.
2002 Selected as a Model School Readiness site by the Pathways Mapping Initiative
of Harvard Medical School and the Annie E. Casey Foundation. “HSFC
illustrates how an array of health, education, early childhood and social services
can be blended into a coherent strategy for improving child and family
outcomes.”
2004 Received the Communities of Excellence Award on behalf of Central Los
Angeles from the Federal Interagency Coordinating Council. The Communities
Can! Award honors HSFC’s commitment to making sure that all children and
families, especially those with or at risk for disabilities, have the services and
supports they need to develop, flourish, and be valued members of the
community and that those services are family-centered and culturally-competent.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
4
2006
HSFC’s Early Head Start program was selected by the U.S. Substance Abuse
and Mental Health Services Administration as a model for innovative services for
young children and families. HSFC successfully integrates behavioral health into
primary care for pregnant women and families with young children.
HIGHLIGHTS OF MAJOR COMMUNITY BENEFITS PROGRAMS IN FY08
In July 2007 the Hope Street Family Center received a grant from California Department of
Education, Child Development Division to establish a classroom for 20 four-year-olds at the
new Early Care and Education Center, located at the Mercy Housing Development across
the street from CHMC’s campus. The Prekindergarten and Family Literacy Program will
enable children to receive high-quality services to prepare them for success as learners in
kindergarten and beyond and their parents to learn how to be active partners in the
education of their children, with an emphasis on promoting their young children’s prereading and school readiness skills. Through a partnership with the Los Angeles Unified
School District, parents will also have the opportunity to improve their own literacy skills
through English-as-a Second-Language and adult basic education instruction.
In August 2007 the Hope Street Family Center’s School Readiness Program was
selected by First 5 LA to participate in their Sustainability Project which supports providers
in developing and implementing plans to sustain high-quality outcomes for children ages 0-5
years in Los Angeles County. It includes monthly workshops and follow-up support by first 5
LA staff and Sustainability Project consultants. The goal is to build providers’ capacity to
plan for sustainability, and to successfully pursue funding and other resources. The Project
trains teams from community-based organizations serving children and their families within
Los Angeles County. The sustainability team from HSFC consisted of Vickie Kropenske,
Richard Hume, Laura Diaz, Sherrie Segovia, and Maria Avila. Monthly workshops walked
the team through each step of the sustainability planning process with the ultimate goal of
creating a comprehensive sustainability plan. HSFC’s Sustainability Plan was presented in
June 2008 at a Resource Forum to a group of leaders from local foundations, County
offices, and other nonprofit organizations.
In September 2007 M. Lynn Yonekura, M.D. participated with Kate Lorig, PhD on an Audio
Conference and Community Benefits 101 Workshop for the Catholic Health Association of
the United States entitled Chronic Disease Management: An Evidence-Based Approach
That Works. Dr. Lorig described the Chronic Disease Self Management Program and the
evidence that it works. Dr. Yonekura discussed the implementation of the CDSMP at CHMC
and the telephone survey of CHMC participants documenting at 50% reduction in
hospitalizations and a 80% decrease in ER visits in the year after program participation
compared to the year prior to program participation.
In October 2007 Los Angeles Best Babies Network was selected by First 5 LA to
participate in the same Sustainability Project described above. Their sustainability team
consisted of Carolina Reyes, M. Lynn Yonekura, Janice French, Deborah Munoz, and
Joseph Hobbs. They also presented their Sustainability Plan in June 2008 at the Resource
Forum.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
5
In October 2007 the Hope Street Family Center was awarded a five year grant from the
U.S. Department of Health and Human Services, Administration for Children and Families,
Office of Head Start to initiate and sustain a Healthy Marriage Program, targeting parents
who participate in or are eligible for Head Start or Early Head Start services. The program
will help parents and couples achieve and maintain nurturing and healthy marital
relationships, which, in turn, will strengthen the family unit and support the creation of a
home environment where children can thrive. Parents will have the opportunity to
participate in classes to build their communication, conflict management, parenting, and
relationship skills; develop positive social support networks with other parents; enjoy
structured weekend retreats; and access services to address healthcare, mental health, and
social service issues that are jeopardizing their marriages and family stability.
In October 2007 Dr. Carolina Reyes, Executive Director of Los Angeles Best Babies
Network, spoke at the Second National Summit on Preconception Health and Health Care.
Her presentation was entitled “Building Sustainable Networks to Provide Interconception
care and Reduce Disparities”.
First 5 LA approved $125 million for the Prenatal-Three focus area which included plans for
a universal home visitation program for all new parents in Los Angeles County. This is
based on three basic premises: 1) the health of parents is important to the growth and
development of young children; 2) the time during fetal development through age three is
the most critical developmental period of life; and that 3) the primary relationships between
parents and infants are the foundation of social and emotional health and development.
These factors provide the foundation for school readiness for children. In November 2007
the Los Angeles Best Babies Network was commissioned to provide an implementation
plan for a pilot of a universal home visitation program, entitled Welcome, Baby! based on
a framework provided by First 5 LA staff and provide an assessment of feasibility and
scalability of this program if adopted countywide. First 5 LA wanted to build on their current
investment in developing a vibrant Network of providers who share in the mission of
improving health and well-being of mothers, families, and children.
In December 2007 President Mark Meyers awarded seven recipients $15,000 each through
the CHW Community Grants Program at a luncheon at the California Club. The
Community Grants Program is sponsored by CHMC and its parent company, Catholic
Healthcare West. Through this program, CHMC partners with other nonprofit organizations
working to improve the health status and quality of life of local communities. The grants
provide services to underserved populations and address specific community needs
delineated in our Community Needs Assessment. The following causes and their sponsoring
organizations received the grants:
Mental Health Services for the Uninsured: The 1736 Family Crisis Center is providing
an innovative school-based intern training program for master’s-level counselors working
toward licensure. The proposed program will increase the capacity to serve the mental
health needs of the community, particularly for persons who need but cannot afford
services or have no insurance.
Mental Health Services for Homeless Families: Beyond Shelter’s grant will support group
and individual counseling to an estimated 90 homeless parents and 15-20 at-risk
children from South Los Angeles. these families also have access to a broad range of
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
6
additional social and human services through Beyond Shelter’s Neighborhood Resource
Centers.
Community Yoga Classes: Immanuel Presbyterian Church was awarded funding for its
Community Yoga Classes. This proposal builds upon a highly successful and unique
pilot program that demonstrated effectiveness in reducing adult stress, promoting weight
loss and improving emotional well-being.
First Steps Program: Los Angeles Child Guidance Clinic’s grant will help fund its First
Steps Program. First Steps provides early intervention mental health services for at-risk
families raising infants and toddlers on limited resources in Central and South Los
Angeles, where intense stressors negatively impact the healthy development of children.
The Hope Street Youth Circus: Opportunities Team’s grant will support the Hope Street
Youth Circus, a supervised after-school program that involves 40 youth, ages 7-18, who
attend CHMC’s Hope Street Youth Center. Twice weekly circus training sessions
provide physical activity, fitness training, and skill development. The Youth Circus
performs at a variety of public venues around Los Angeles.
Red Shield After School Program: The Salvation Army was awarded funding for its Red
Shield After School Program, which provides supervised, safe and structured academic
and recreational activities for children ages 6-12 and teens ages 13-17 during the critical
after-school hours.
Psychosocial Support for Cancer Patients at CHMC’s Donald P. Loker Cancer Center:
The Wellness Community-West Los Angeles was awarded funding for its Psychosocial
Support Program for Cancer Patients at CHMC’s Donald P Loker Cancer Center. The
Wellness Community provides two psychosocial support groups each week for cancer
patients and their families, with one group in English and one in Spanish. A licensed
psychotherapist facilitates the groups which help cancer patients learn to better manage
feelings of anxiety and uncertainty about their disease. Participants develop new coping
skills and support one another in managing the day-to-day challenges that accompany a
life-threatening illness.
In December 2007, CHMC received a three-year grant from the UniHealth Foundation for
the Community Dental Partnership. Responding to recent studies linking periodontal
disease and chronic diseases such as diabetes and cardiovascular diseases, as well as
preterm births, the CDP will offer free periodontal care at Eisner Pediatric and Family
Medical Center’s dental clinic for uninsured adults with diabetes. The program will also
provide access to discounted basic dental care, dental health education, care coordination
for patients between their dental provider and their primary care physician and establish a
loan program with favorable terms to help patients purchase critical but expensive dental
care not covered by the grant.
In January 2008, the Chronic Disease Management Consortium consisting of CHMC, Good
Samaritan Hospital, Huntington Memorial Hospital, and the National Health Foundation
received a planning grant from the Good Hope Medical Foundation for its Heart HELP
Program, a cardiovascular health promotion/ cardiovascular disease prevention program.
This program will provide outreach education and screening for risk factors, smoking
cessation classes, and five weekly 2-hr workshops.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
7
California Hospital Medical Center was named the Official Hospital for the 23rd Annual
Los Angeles Marathon held on March 2, 2008. Under the leadership of CHMC more than
300 doctors, nurses, paramedics and firefighters worked to ensure the safety of 25,000
runners and one million spectators at the 23rd Annual Los Angeles Marathon. The event is
the largest marathon held in California, the fourth largest in the country and the seventh
largest in the world. Eight medical aid stations along the race route and two mobile
emergency hospitals at the finish line served those who gave their all along the course that
covered most of the city. “We did our best to anticipate as many scenarios as possible, from
blisters and bruises to dehydration, broken bones and heart attacks,” said CHMC
Emergency Nursing Director Sarah Stevens. The medical teams saw about 500 cases
reporting minor injuries, with very few needing treatment and stabilization for stress
fractures, asthma, and heat exhaustion or transfer to local emergency rooms. In addition to
CHMC’s volunteer nursing and physician staff, this meant recruiting and coordinating a team
of 140 highly trained family medicine doctors, emergency and trauma specialists, and
orthopedists, as well as skilled physician assistants, nurse practitioners, intensive care and
emergency room nurses from other medical facilities including cross town rivals USC and
UCLA. It also meant months of preparation, including weekly medical strategy meetings
with the leadership of the Los Angeles Fire Department, marathon organizers, and hospital
and academic administrators, working with suppliers for medical and pharmaceutical
equipment, transportation, and communications, as well as consulting with other medical
race directors across the country. In the end, marathon organizers complimented the
medical staff as having provided the most comprehensive coverage in the race’s history.
“As medical providers, it’s our job to make race day a safe and healthy celebration for the
city of Los Angeles,” said LA Marathon Medical Commissioner and CHMC Medical Staff
Member Maureen Strohm, M.D. “We all worked diligently to provide the best outcomes
possible for those seeking medical attention. It’s one more way California Hospital says,
‘We’re here for you, Los Angeles.’”
In April 2008 the Hope Street Family Center was awarded a grant from the Atlas Family
Foundation to implement Phase I of the Integrated Behavioral Health Training Program
at HSFC. This program will create a model for providing paraprofessionals and
professionals (including physicians, nurses, social workers, and child development
educators) with training in the mental health assessment of infants, toddlers, and their
families. This program is a collaborative effort of HSFC, UCLA, and Cedars Sinai Medical
Center. In addition, the program is part of a long-term strategy to grow revenue-generating
mental health services at HSFC.
In June 2008, the Los Angeles Best Babies Network launched phase II of the Healthy
Births Care Quality Collaborative. The HBCQC goal is to improve the quality and content
of prenatal care to improve birth outcomes, as well as early infant health and development.
The HBCQC is working in tandem with LABBN and their consultants to roll out phase II of
the Healthy Births Care Quality Improvement efforts over an 18-month period using an
evidence-based care quality framework modeled after the Chronic Care model. Eleven
clinical sites are participating in the Collaborative.
In June 2008, the Los Angeles Best Babies Network also launched phase II of the Best
Babies Collaboratives Planning Workshops. The existing BBCs in the Antelope Valley,
Harbor Freeway Corridor South , South Los Angeles, and Long Beach/Wilmington
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
8
welcomed three new BBCs: the Heart of the City, the Hope of the (San Fernando)Valley,
and San Gabriel Valley. The goal of the BBCs is to improve birth outcomes in communities
in which women often lack prenatal care and infant mortality rates are especially high by
uniting community groups and providing interconception care, case management, outreach,
social support and health education. LABBN hosted 10 planning workshops for new and
existing BBCs. Now, approximately 40 organizations with ~ 40 home visitors will be
providing direct services and support to at-risk women to reduce their risks for subsequent
poor birth outcomes.
In June 2008 CHMC was selected by the State as one of four hospitals in Los Angeles
County to participate in the Birth & Beyond California: Breastfeeding Training and
Quality Improvement Project. The BBC project seeks to improve breastfeeding rates in
the hospital setting by training a variety of healthcare workers to support a mother’s choice
to breastfeed and through continuous quality improvement efforts.
A total of 3,652 people were enrolled in various public insurance programs by staff of the
Para Su Salud Program, exceeding our enrollment goal by 10%.
In July 2008 the Hope Street Family Center received a three-year grant from First 5 LA
Community Opportunities Fund to establish a Fundraising and Development Program
exclusively focused on generating resources for HSFC and the construction of the Center’s
new home. The grant will fund a development professional who will organize and implement
a fundraising program that includes grants, individual donor solicitation, and online giving.
In July 2008 LABBN received a five-year grant from the First 5 LA Community Opportunities
Fund for policy and advocacy entitled the L.A. County Perinatal Mental Health Task
Force. The goal of this project is to improve access to perinatal mental health services by
supporting universal screening and referrals for women experiencing perinatal depression.
They will do this by: 1) increasing awareness of perinatal depression among policy makers;
and 2) identifying the appropriate policy changes needed to increase education and training
of providers and improve access to perinatal mental health care for women in the County.
The L.A. County Perinatal Mental Health Task Force is the only multi-institutional effort
leveraging leadership and expertise to improve perinatal mental health in the County. It was
established in February 2007 in response to the Governor’s veto of postpartum depression
legislation in 2006 and his call for coordinated local efforts in this area. Key partners
include: PSI, LA MCAH, LA DMH, and mental health care providers. The mission of the
Task Force is to support women and families by raising awareness of perinatal depression,
increasing screening, and providing trainings for providers who serve pregnant and
postpartum women.
The Chronic Disease Management Consortium consisting of CHMC, Childrens Hospital Los
Angeles, Huntington Memorial Hospital, Harbor-UCLA Medical Center, and the National
Health Foundation, with funding from the UniHealth Foundation, successfully launched the
Healthy Eating Lifestyle Program (HELP) in 2005. As the name implies, the primary goal
of HELP is to help overweight and obese children aged 5-12 years and their families adopt
healthier eating habits and increase physical activity. In September 2008 the final results of
this highly successful program were presented at the 18th Annual CityMatCH Urban
Maternal and Child Health Leadership Conference in Albuquerque, NM by Heather Kun,
PhD from the National Health Foundation and M. Lynn Yonekura, M.D.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
9
The Chronic Disease Management Consortium consisting of CHMC, Huntington Memorial
Hospital, Good Samaritan Hospital and the National Health Foundation, with funding from
the Good Hope Medical Foundation, successfully launched a multi-year comprehensive
educational program focusing on a Type 2 Diabetes Prevention, Screening, and
Intervention in 2006. In September 2008 M. Lynn Yonekura, M.D. presented the results of
this extremely successful program at the 18th Annual CityMatCH Urban Maternal and Child
Health Leadership Conference in Albuquerque, NM.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
10
California Hospital Medical Center
Classified Summary of Quantifiable Benefits
July 1, 2007 - June 30, 2008
Classified as to the Poor and the Broader Community
Persons
Total
Offsetting
Net
Community
% of
Total
% of Total
Served
Expense
Revenue
Benefit
Expense
Revenue
Traditonal charity Care
2,328
13,968,151
9,023,581
4,944,570
2.6
2.7
Unpaid Costs of Medicaid/Medi-Cal
8,556
105,297,450
91,314,294
13,983,156
7.3
7.7
7,959,759
2,241,602
5,718,157
3.0
3.2
Benefits for Poor
Other Public Programs
402
Community Services
Community Health Services
0.1
0.1
Health Professions Education
-
-
-
-
0.0
0.0
Subsidized Health Services
-
-
-
-
0.0
0.0
Financial and In-kind Contributions
24,147
10,461,507
10,298,688
162,819
4,100
582,643
-
582,643
0.2
0.3
Community Building Activities
-
11,393
657
10,736
0.0
0.0
Community Benefit Operations
-
567,114
273,715
293,399
0.2
0.2
Total Community Services
28,247
11,622,657
10,573,060
1,049,597
0.5
0.6
Total for the Poor Community
39,533
138,848,017
113,152,537
25,695,480
13.4
14.2
9,356
212,202
-
212,202
0.1
0.1
-
2,290,801
-
2,290,801
1.2
1.3
61,890
3,122,835
-
3,122,835
1.6
1.7
2.9
3.1
16.3
17.3
Benefits for Broader Community
Community Services
Community Health Services
Health Professional Education
Subsidized Health Services
Research
-
-
-
-
Financial and In-Kind Contributions
-
-
-
-
Community Building Activities
-
-
-
-
Community Benefit Operations
-
-
-
-
Total Community Services
71,246
5,625,838
-
5,625,838
-
Total Benefits for the Broader
Community
71,246
5,625,838
-
5,625,838
-
Total Community Benefits
110,779
144,473,855
113,152,537
31,321,318
-
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
11
Unpaid Costs of Medicare
Total Community Benefits
Including Unpaid
Costs of Medicare
2,312
38,319,721
36,954,440
1,365,281
0.7
0.8
113,091
182,793,576
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
150,106,977
32,686,599
17.0
18.1
12
MISSION STATEMENT
Mission Statement
Catholic Healthcare West
Catholic Healthcare West and our Sponsoring Congregations are committed to furthering the
healing ministry of Jesus. We dedicate our resources to:
delivering compassionate, high-quality, affordable health services;
serving and advocating for our sisters and brothers who are poor and
disenfranchised; and
partnering with others in the community to improve the quality of life.
California Hospital Medical Center
California Hospital Medical Center (CHMC) is a non-profit public benefit health care center that
has been a member of the downtown Los Angeles community since 1887. CHMC is committed
to making quality, cost-effective healthcare available to, and improving the overall health of, the
multi-ethnic communities it serves by providing specialized services, health screenings, and
education which reflect the unique needs of these communities.
Several phrases written into the hospital’s mission statement are key to the Community Benefit
Plan:
CHMC is committed to increasing access to care.
CHMC will develop services based on the needs of the community.
CHMC will work with available community resources in creating a network of
care.
CHMC’s vision statement: CHMC is committed to improving the health and well being of the
community by helping people help themselves.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
13
ORGANIZATIONAL COMMITMENT
In order to complete a 2007 Community Needs Assessment, California Hospital Medical Center
pooled its resources with five other hospitals and one group of community clinics to collect
information about the health and well-being of residents in their service community. This report
is included at the end of this document. The highlights of the report are featured on pages 2633.
In July 2006 the Hope Street Family Center (HSFC) completed its own Community Needs
Assessment for its service area, which is a subset of CHMC’s primary service area. This Needs
Assessment primarily focused on children, especially those aged 0-5 years, and their families.
The HSFC has its own Community Advisory Board comprised of: three members of the CHMC
Community Board, six members of the CHMC Foundation Board, three members from CHW
Corporate Office, two professors from UCLA, two members involved in community
development, one former HSFC participant, CHMC’s President and Foundation President, and
the Director of Community Benefits who is also the Executive Director of HSFC.
From June 9-11, 2005 the CHMC Community Board and the CHMC Foundation Board
embarked on a joint Strategic Planning Process during their Annual Retreat. Other key
participants included the Hospital President and Executive Management Team, the Director of
Community Benefits, and the Director of Grants and Contracts. Additional Work Group
meetings took place on September 7 and October 27, 2005.
As themes began to emerge from the Strategic Planning Process, a Community Benefit
Planning Work Group began to develop the Community Benefit Plan for FY06-08. The
Community Benefit Plan for FY09 is a continuation of this plan. The Work Group consists of:
Hospital President, Foundation President, Senior Vice President of Business Development,
Director of Community Benefits, Director of Grants and Contracts, and three members of the
Community Board. Details of the planning process and prioritization of programs are presented
in the section entitled Community Benefit Planning Process.
The Community Board has the following expectations regarding the Community Benefits
Planning Process:
The Plan should be responsive to Community Need and, when possible, to CHMC’s
Strategic Plan.
To the extent possible, the Plan should be budget neutral, i.e., the majority of the
Programs should be grant funded.
Programs should be culturally sensitive and evidence-based.
Programs should have measurable objectives and should be continuously monitored.
The Community Board delegates the following decisions to the Foundation President and his
staff: budget decisions, program content, program design, program continuation or termination,
and program monitoring. Any major deviations from the approved Community Benefit Plan
must be brought back to the Community Board for its consideration and approval.
Once the Community Benefit Planning Work Group completes the prioritization process, the
Director of Community Benefits and Foundation staff completes the Plan. The completed
Report and Plan are then reviewed by the Work Group and, after approval, distributed to the
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
14
Community Board. The Director of Community Benefits presents an Executive Summary of the
Community Benefit Report and Plan at a meeting of the Community Board for their approval.
However, in 2006 some major revisions were made. Faced with challenges to their tax exempt
status, the Catholic Health Association (CHA) Board of Trustees formed a task force to develop
a ministry-wide approach to community benefit/tax exemption challenges. This task force
reached a consensus on key components for report community benefit in an effort to enable the
ministry to better communicate the many ways they meet and exceed the legal requirements of
tax exemption. Its recommendations were subsequently adopted by CHA’s Board of Trustees.
Specifically, the task force recommended that Catholic health organizations:
Use the categories and accounting guidelines developed last year by CHA and VHA and
published as The Guide for Planning and Reporting Community Benefit. The Guide was
distributed to all members in May 2006.
Report all community benefit at cost (not charges)
Not report bad debt as community benefit
Not report the Medicare shortfall as community benefit (although programs and services
that continue at a loss and are needed by the community can be reported as subsidized
services and the Medicare shortfall can be reported in other financial reports)
In May 2006, CHW sent all system and facility CEOs a packet of information from CHA that
included “
A Community Benefit Reporting video with an overview of the issues
A Community Benefit Reporting brochure and accompanying prayer card
A board resolution and an organizational pledge letter
A CD-ROM viewer reporting form
CHW’s Executive Management Team reviewed the CHA recommendations and the CHW Board
adopted the proposed resolution at its September meeting on behalf of all CHW hospitals.
However, CHW has advised member hospitals to report the Medicare shortfall “below the line”
for transparency with and without this expense as shown on the attached sample, as California
law does require the inclusion of this expense. In August 2006, the CHA Community Benefit
Reporting video was shown to CHMC’s Community Board and the proposed board resolution
was formally adopted. Moreover, the Community Board was informed about two revised CHW
policies and procedures.
CHW Governance Policy 3.45, Community Benefits, establishes the community benefit
structure and processes to ensure the standardization and institutionalization of CHW’s
Community Benefit practices. Notably, it calls for the establishment of a board level
community benefit committee to provide oversight and policy guidance for all charitable
services and activities supported by the hospital. This committee must include at least
two Board members with a majority representation from a range of community
stakeholders who have knowledge of the community. The two board members will
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
15
ensure that the Board is regularly briefed on community benefit activities and
developments. In addition, the entire Hospital Board is responsible for review and
approval of the annual Hospital Community Benefit Plan and Report.
CHW Administrative Policy 40.4.001 delineates the administrative requirements for the
implementation of Governance Policy 3.45, defining staff requirements and
responsibilities and sets forth the core principles and accountabilities of Community
Benefit programming. This policy calls for the integration of the five core principles
developed by the Advancing the State of the Art of Community Benefit (ASACB)
demonstration project into community benefit programming. The core principles include:
1. Emphasis on Disproportionate unmet health-related Needs – Seek to respond to
the needs of communities/neighborhoods with disproportionate unmet healthrelated needs
2. Emphasis on Primary Prevention – Address the underlying causes of persistent
health problems
3. Building a Seamless Continuum of Care – Emphasize evidence-based
approaches by establishing operational linkages (that is, coordination and
redesign of care modalities) between clinical services and community health
improvement activities
4. Building Community Capacity – Target resources to mobilize and build the
capacity of existing community assets
5. Emphasis on Collaborative Governance – Engage diverse community
stakeholders in the selection, design, implementation, and evaluation of program
activities.
To assist in implementation, specifically the review of existing programs and the
integration of the five principles into community benefit programming, CHW held all day
joint education/training meetings in both northern and southern California in May 2006
with the partners in this demonstration (St. Joseph Health System, Hoag Memorial
Hospital, Whittier Intercommunity Hospital, Lucile Packard Children’s Hospital at
Stanford, Texas Health Resources, and The Public Health Institute). In addition, CHW
convened a series of conference call workgroup sessions to share enhancement ideas
for community benefit programs that focus on: chronic disease management, health
promotion, increasing access to care, and community grants.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
16
COMMUNITY
Community Profile
California Hospital Medical Center is located in Service Planning Area (SPA) 4 of Metro Los
Angeles. Its service area, however, also includes parts of SPA 6 (South) and SPA 8 (South
Bay).
The CHMC service area encompasses a large area that includes all or portions of the following
SPAs, Health Districts and cities:
Service Planning Areas
SPA 4 - Metro
SPA 6 - South
SPA 8 - South Bay
Health Districts
HD 9 - Central
HD 34 - Hollywood/Wilshire
HD 37 - Inglewood
HD 69 - South
HD 72 - Southeast
HD 75 - Southwest
HD 84 - West
Cities/Areas
Crenshaw
Los Angeles
Pico-Union
South Central
Westlake
Wilshire
The Community that California Hospital Medical Center serves is defined by CHMCs primary
and secondary service areas and is located in Central/Downtown and South Central Los
Angeles.
Primary Service Area Zip Codes:
90003, 90006, 90007, 90011, 90015, 90016, 90017, 90018, 90019,90037,
90044,90062, 90071
Secondary Service Area Zip Codes:
90001, 90002, 90004, 90005, 90008, 90010, 90017, 90020, 90026, 90043,
90047, 90057, 90255
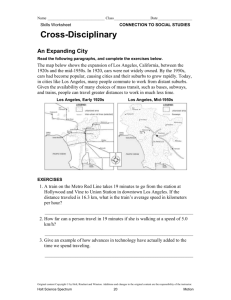
Over one-half million people (617,262) live in CHMC’s primary service area and a total of almost
1.2 million live in its primary and secondary service area. A majority of residents are Latino
(62.1%; Figure 1) and are of Mexican origin (59.7%). The remaining population is mostly
African-American (28.1%). Compared to the County there is a higher concentration of Latinos
and African Americans in the CHMC service area. This area is populated with immigrants,
many of which are not U.S. citizens (Figure 2).
Over a quarter of community residents are less than 20 years of age while only 7.1% are
seniors (see table below). Over half of the residents have not received a high school diploma,
and household incomes are generally low with a median household income of only $23,328,
nearly $20,000 less than the County median. Over a third of households (34.9%) live below the
poverty level. A majority of residents living below the poverty level are under 65 years of age.
I
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
17
Figure 1. Race/Ethnicity of CHMC's Service Area & LA County
70%
62%
60%
50%
CHMC
45%
LA County
40%
31%
28%
30%
20%
10%
12%
10%
5%
4%
0.2%
0.3%
1% 2%
0.3% 0.2%
0%
Latino
Race/Ethnicity
Gender
Age
Place of Birth
Asian/Pac Is.
White
African Amer
Latino
African-American
White
Asian/Pacific Islander
Multiracial/Multiethnic
Other
American Indian
Total
Male
Female
Total
Under 5
Between 5 and 19
Between 20 and 34
Between 35 – 64
65 and over
Total
U.S. Native
Foreign-born
Citizen
Non-citizen
Total
Amer Indian
Other
Multiracial/ethnic
CHMC Service Area
Number
%
383,471
62.1%
173,485
28.1%
28,071
4.5%
22,092
3.6%
1,126
0.2%
7,356
1.2%
1,661
0.3%
617,262
100.0%
303,132
49.1%
314,130
50.9%
617,262
100.0%
59,759
9.7%
170,188
27.6%
163,941
26.6%
179,627
29.1%
43,747
7.1%
617,262
100.0%
344,925
55.9%
272,352
44.1%
58,806
21.6%
213,546
78.4%
617,277
100.0%
LA County
%
44.6%
9.5%
12.1%
31.1%
0.3%
2.3%
0.2%
100.0%
49.4%
50.6%
100.0%
7.7%
23.2%
24.0%
35.3%
9.4%
100.0%
63.8%
36.2%
38.0%
62.0%
100.0%
Figure 2. Place of Birth of CHMC Service
Area Population
FB, Citizen
21.6%
US Native Foreign-born
44.1%
55.9%
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
FB, Noncitizen 78.4%
18
Educational attainment
No formal schooling
Some schooling
High school degree
Some college
College degree
Graduate degree
Total
Household income
<$10000
$10000 – $19999
$19999 – $39999
$40000 – $59999
$60000 – $99999
$100000+
Total
Median Household Income
Poverty
Below poverty
<65 years
65 – 74 years
75+ years
Above poverty
<65 years
65 – 74 years
75+ years
Total
CHMC Service Area
Number
%
31,882
9.7%
148,057
45.1%
58,750
17.9%
59,990
18.3%
19,954
6.1%
9,664
2.9%
328,297
100.0%
39,757
22.5%
36,842
20.8%
51,144
28.9%
24,235
13.7%
17,136
9.7%
7,634
4.3%
176,748
100.0%
$23,328
211,361
34.9%
201,868
95.5%
5,212
2.5%
4,281
2.0%
393,892
360,878
18,202
14,812
605,253
65.1%
91.6%
4.6%
3.8%
LA County
%
4.7%
25.4%
18.8%
26.2%
16.1%
8.8%
100.0%
10.5%
12.8%
24.0%
17.7%
19.9%
15.1%
100.0%
$42,189
17.9%
94.4%
2.9%
2.7%
82.1%
89.5%
5.8%
4.7%
Natality
In all of the CHMC health districts, but the West district, the majority of births in 2005 were to
Latino mothers. Births to White mothers were most common in the West district (55.3%)
followed by Latino mothers (21.7%). The South (22.8%) and Southwest (31.2%) districts had
the highest percentage of births to African American mothers. Births to mothers younger than
20 years old were highest in the South (15.8%), Southeast (15.3%), and Southwest (12.6%)
districts. These rates were higher than the county rate (9.5%). The rate of births to mothers
younger than 20 years old was lowest in the West district (1.9%). More than 90% of the babies
across all health districts were of normal birth weight (more than 2500 grams). However, the
percentages of low (1500-2500 grams) and very low (less than 1500 grams) birth weight infants
for all health districts do not meet the Healthy People 2010 goals of 5% and 0.9%, respectively.
Regarding prenatal care, the Healthy People 2010 objective is that at least 90% of mothers
receive prenatal care in the first trimester. The following health districts did not meet the
Healthy People 2010 objective: Inglewood (89.9%), South (86.3%), Southeast (87.8%), and
Southwest (87.3%).
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
19
Mortality
CHMC health districts with the highest number of infant mortality are Inglewood (46), Southwest
(44), and Hollywood (32). The first three age-adjusted mortality rates are the same for all
service area health districts and the County – heart disease, cancer, and stroke. Fourth and
fifth leading causes vary by district but are restricted to four causes: pneumonia and flu,
diabetes, chronic lower respiratory disease, and unintentional injury. Central is the only CHMC
health district with a high rate of death by unintentional injury (25.7 per 100,000)
Premature Death
Understanding how persons die prematurely provides additional information needed to
understand community health and well-being. A ranking of causes of premature death can be
calculated using a statistical measure that accounts for loss of years of life compared to the
expected lifespan. Similar to L.A. County, in the health districts served by CHMC, the most
common first ranked cause of premature death is heart disease (Central, Hollywood, and West)
and homicide (South, Southeast, and Southwest). Inglewood is the only CHMC health district
where the leading cause of premature death was cancer. Cancer was the second leading
cause of premature death in all CHMC health districts with the exception of Inglewood where
heart disease was the second leading cause.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
20
Community Needs and Assets Assessment Process
Background and Purpose
In order to complete a 2007 Community Needs Assessment, five hospitals and one group of
community clinics decided to pool resources to collect information about the health and wellbeing of residents in their service community. This group, called the Metro Collaborative,
includes:
California Hospital Medical Center
Childrens Hospital Los Angeles
Good Samaritan Hospital
Kaiser Foundation Hospital – Los Angeles
Franciscan Clinics
St. Vincent Medical Center
In 1994, the California State Legislature enacted Senate Bill 697 (SB 697) requiring non-profit
hospitals to conduct a needs assessment every three years. Based on the needs and priorities
identified in the tri-annual assessment, the hospital will develop a community benefit plan. The
plan will include proposed activities designed around disease prevention efforts and
improvement of health status. A needs assessment has been conducted every three years
since 1995 that includes most of the current Metro Collaborative members.
Metro Collaborative Members
California Hospital Medical Center
California Hospital Medical Center (CHMC) has been a proud community member for more
than a century. Founded in 1887 by three physicians, CHMC is a non-profit, acute care
hospital with 316 private beds and an array of social service programs, including the nationally
recognized Hope Street Family Center, that benefit both the downtown and the central city
areas.
Childrens Hospital Los Angeles
Established in 1901, Childrens Hospital provides health care to seriously ill and injured children
and adolescents in Los Angeles County and is a major referral center for specialized care. It is
a local, regional, and national resource for pediatric clinical care, teaching and research.
Good Samaritan Hospital
Good Samaritan Hospital is both a community hospital and a regional tertiary medical center
with “a tradition for caring” since it opened in 1885. The hospital represents Los Angeles'
multicultural community and has an international reputation as a world-class medical center.
Collectively, medical staff and employees speak almost 60 languages/dialects and offer
outstanding diagnostic, surgical and therapeutic care in a state-of-the-art setting. Annually, the
hospital admits approximately 17,000 patients and provides more than 90,000 outpatient visits.
Kaiser Foundation Hospital – Los Angeles
Kaiser Foundation Hospital – Los Angeles (KHF-LA) is a 507 licensed-bed acute care hospital
offering both primary and tertiary care services. It is situated on approximately 17.9 acres in
the East Hollywood/Los Feliz area. It is the tertiary care center for Kaiser Permanente
members throughout Southern California, with outstanding programs in cardiac surgery,
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
21
radiation oncology, cochlear implants, and epileptic surgery. In addition, the medical center is
home to the Center for Medical Education, which includes an extensive graduate medical
education program with 169 interns, residents, and fellows in 19 different specialties and
subspecialties. The medical center also has a research program that includes about 150 active
projects, with more than 100 publications in the last three years. The medical center has a staff
of more than 4,500 employees and physicians, and outlying facilities in East Los Angeles,
Glendale, Pasadena, and a mental health center in Chinatown.
Franciscan Clinics
Founded in 1897, Franciscan Clinics d.b.a. QueensCare Family Clinics’ mission is to bring
quality primary health care that is accessible, compassionate, comprehensive, and affordable to
the low-income communities of Los Angeles County.
St. Vincent Medical Center
Los Angeles’ first hospital, St. Vincent Medical Center, was founded by the Daughters of
Charity of St. Vincent de Paul in 1856. Since that time, the hospital has grown into a 347-bed
regional acute care, tertiary referral center, specializing in heart care, cancer care, spine care,
multi-organ transplantation, and the treatment of ear and hearing disorders. Committed to
serving its community, St. Vincent Medical Center provides comprehensive, excellent
healthcare that is compassionate and attentive to the whole person--body, mind and spirit.
Planning the Community Needs Assessment
Developing a plan for the needs assessment required that collaborative members share their
perspective about what was important to include as well as document major changes or trends
in the community since the last assessment. The assessment team met with a representative
from each organization to gather information about their agency’s mission and goals, primary
target populations and geographic areas, and impressions about the unique needs of their
community.
Responses were reviewed, and a community needs assessment plan was presented at
individual meetings with the hospitals, as well as a meeting with the entire Collaborative for
their approval. It was agreed that the organization of previous reports would be a guide for the
reporting of this assessment. Proposed methods were approved, and the assessment team
began collecting data in June 2007.
In the previous assessment, seven major content areas were used to report community needs:
Access, Health Behaviors, Risk Behaviors, Chronic Disease, Communicable Diseases, Mental
Health, and Community and Social Issues. This report includes these areas as well as
additional topics within these areas covering major health care needs of the community
identified in focus groups and interviews.
Organization of Report
This report (Attachment D) presents the methods and findings from a community needs
assessment of portions of the Los Angeles metropolitan area. First, methods and sources of
data are presented. Findings are organized into major content areas:
Community Health Profile
Access
Health Behaviors
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
22
Risk Behaviors
Chronic Diseases
HIV/AIDS
Communicable Diseases
Mental Health
Community and Social Issues
Methods
This needs assessment used multiple methods to collect information about the health needs of
residents in the communities served by the Los Angeles Metropolitan Hospital Collaborative.
Numerous sources of secondary data were used to describe the service area and the health
needs of its residents. It was equally important to collect primary data (using qualitative
methods) from residents and services provider key informants to better understand what the
community’s needs and assets are. Each Collaborative member was asked to identify potential
interviewees and contacts for focus groups.
Document Reviews
Previous available needs assessment and community benefit plans were reviewed to identify
data that should be updated. These documents provided background about the most
prominent needs at the time of the last assessment so that patterns, trends or changes could
be noted in this review.
Analysis of Secondary Data
Local, county, state and national data were gathered to describe community needs. Sources
included data from the United States Bureau of the Census as well as information from federal
health organizations such as the Centers for Disease Control and Prevention (CDC) and
Substance Abuse and Mental Health Services Administration (SAMHSA). State data includes
the California Department of Health Services and California Health Insurance Survey (CHIS).
Local studies provided through the Los Angeles County Department of Health Services
(LAC/DHS) such as the Los Angeles County Health Survey (LACHS; LAC/DHS, 2003 and
2005) and the Patient Assessment Survey III (PAS III; Diamant, 2005) provided better
estimates of needs than state or national data sources. An important consideration is the
nature of how survey data were collected. Both were telephone surveys that limited
respondents to those who had a telephone and agreed to participate. The PAS III included
patients utilizing publicly funded services provided by the Los Angeles County Department of
Health Services so that their responses could be best generalized to those who received
services through the County. This data provide estimates of the health behavior and attitudes
of residents in Los Angeles County.
Primary Data Collection
Key informants were selected for this needs assessment based on their expertise, prior
involvement with this assessment, and relationships with Collaborative members. As with other
qualitative approaches, interview and focus group data may be subject to personal biases and
agenda. However, their responses are considered fair and important indications of the status
of health in the communities this organization serves. When possible, their responses are
supported with secondary data.
Focus groups – A total of 12 focus groups were conducted with a total of approximately 120
participants over a two-month period. Organizations that assisted in organizing the focus
groups are listed in Attachment 1. Topics in the focus group included major areas from previous
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
23
needs assessments and other issues anticipated to be important in health care. These areas
were: health care utilization, preventive and primary care, health insurance, access and
barriers to care, emergency room use, chronic disease management and other relevant
community issues. Groups that collaborative members commonly identified as important
stakeholders in the needs assessment were prioritized. Groups included residents from major
ethnic groups, geographic areas and health promoters from the Collaborative’s service areas.
Residents from ethnic communities were Armenian, Korean, Latino, and Thai representing
areas of downtown Los Angeles, East Los Angeles and other metro areas. Translation was
provided in the Armenian, Latino and Thai focus groups. Focus groups with seniors and
community health promoters were conducted separately.
Interviews – A total of 25 interviews with service provider key informants such as agency
administrators, county health personnel and social service agencies took place over a twomonth period. Interviews were conducted over the phone and lasted approximately 45
minutes. The content of the interviews was similar to that of the focus groups with additional
questions about mental health needs and services. A list of key informants’ organizations is
included in Attachment 1.
Attachment 1
Interview and Focus Group Participant Agencies
Angelus Plaza
Armenian Relief Society
Asian Pacific Counseling and Treatment Centers
Central City Neighborhood Partners
Children’s Bureau of Southern California
City of West Hollywood Social Services
Coalition for Community Health
Community Health Councils, Inc.
Community Health Ministries Center
Eisner Pediatric and Family Medical Center
Esperanza Housing Corporation
Los Angeles County Department of Health Services, Office of Ambulatory Care
Emergency Medical Services Agency
The Los Angeles Free Clinic
Los Angeles County Emergency Medical Services
Maternal and Child HealthAccess
Mental Health-University of Southern California
People Assisting The Homeless (PATH)
St. John's Well Child and Family Center
Service Planning Areas 3 and 4 Area Health Officer
Service Planning Areas 7 and 8 Area Health Officer
Shelter Partnership
St. Barnabas Senior Services
Thai Health and Information Services, Inc.
Community Health Alliance of Pasadena
Watts Senior Center
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
24
Inventory of Community Assets
In 1992, staff of the Hope Street Family Center created a bilingual (English/Spanish) Resource
Directory of the Pico Union/Westlake service area. The motivation for the creation of this
resource directory at that time was that this was the only service area in Los Angeles County
lacking such a directory and community residents, community based organizations and HSFC
staff would all benefit from its creation. HSFC staff updates the directory annually.
Disproportionate Unmet Health Needs
To complement the traditional methodology used to conduct community needs assessments,
in May 2004 CHW announced the development of a standardized measure of community need
that provides an objective measure of access to health care. The Community Need Index (CNI)
is a tool that uses socio-demographic and hospital utilization data to provide an “at a glance”
view of disproportionate unmet health care needs in a geographic area. The CNI measures
community need in a specific zip code by analyzing the degree to which a community has the
following barriers to health care access:
1.
2.
3.
4.
5.
Income barriers
Educational/literacy barriers
Cultural barriers
Insurance barriers
Housing barriers
Using statistical modeling, the combination of the above barriers results in a score between 1
(less needy) and 5 (most needy). Analysis has indicated significant correlation (97%) between
the CNI and preventable hospital admissions. Individuals living in communities with scores of
“5” are more than twice as likely to need inpatient care for preventable conditions (otitis media,
pneumonia, etc.) as those residing in communities with a score of “1”.
The CNI map of CHMC’s service area is shown in Attachment B. California Hospital Medical
Center is located in zip code 90015. As the CNI map illustrates, all of CHMC’s primary service
area zip codes have CNI scores of 4.8-5.0 and therefore fall into the “most needy” category.
Similarly, CHMC’s secondary service area zip codes also have CNI scores of 4.4-5.0.
Zip Code
90011
90044
90255
90026
90019
90006
Score
5.0
5.0
4.8
5.0
4.8
5.0
Population
109,354
95,589
83,382
75,854
72,190
62,935
Zip Code Score
90003
5.0
90037
5.0
90001
5.0
90018
5.0
90047
4.8
90061
5.0
Population
66,536
58,810
61,541
53,514
50,510
26,058
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
Zip Code Score Population
90002
5.0
50,879
90043
4.6
46,850
90016
4.8
48,518
90007
5.0
45,700
90057
5.0
48,205
90059
5.0
42,899
Zip Code Score Population
90005
5.0
41193
90008
4.4
31,739
90062
5.0
30,309
90017
5.0
26,228
90015
5.0
20,845
90302
4.8
31,185
25
CHMC 2007 COMMUNITY NEEDS ASSESSMENT:
SUMMARY OF FINDINGS
The following information contains key findings of health and welfare conditions and needs
among community members residing in the California Hospital Medical Center (CHMC)
service area. In some cases, the Office of Disease Prevention and Health Promotion, U.S.
Department of Health and Human Services Healthy People 2010 (Healthy People 2010)
objectives are highlighted as benchmark indicators to provide context to health and welfare
conditions in Los Angeles County. In many instances, only 2005 Los Angeles County
Department of Health Services data were available.
Natality - The Healthy People 2010 objective is to decrease the rate of low birth weight
and very low birth weight to 5% and 0.9%, respectively. In 2005, the percentages of low
birth weight (between 1500-2500 grams) and very low birth weight (less than 1500
grams) for all CHMC health districts were higher, and thus did not meet the 2010
objectives. The Healthy People 2010 objective is to increase the percentage of mothers
who receive prenatal care to 90%. Of the CHMC health districts, the Central,
Hollywood, and West health districts met the 2010 objective for prenatal care in the first
trimester.
Mortality- the Healthy People 2010 objectives for cancer death ranged from 2 to 28.8
per 100,000, depending on the type of cancer. For the CHMC health districts in 2005,
cancer death rates were much higher and ranged from 115.99 to 198.51 per 100,000. The
Healthy People 2010 objective for heart disease is 166 per 100,000. With the exception
of the Central (157.6 per 100,000) and West (160.74 per 100,000) health districts, heart
disease death rates in all districts were higher than the 2010 objective. Lastly, the
Healthy People 2010 objectives for stroke death rate is 48 per 100,000. All CHMC
health districts but the Central (34.04 per 100,000), Hollywood (42.39 per 100,000), and
West (40.96 per 100,000) districts exceeded of the 2010 objective for stroke death.
Premature Death –The first-ranked cause of premature death in Los Angeles County in
2005 was heart disease. Of the CHMC health districts, the most common (first-ranked)
cause of premature death was homicide along with heart disease. Homicide was ranked
first in the South, Southeast, and Southwest districts and heart disease was ranked first in
the Central, Hollywood and West districts. Cancer was ranked second in all of the CHMC
health districts except Inglewood where it was ranked first followed by heart disease.
Insurance - The Healthy People 2010 objective is to achieve a 100% insurance rate.
Despite progress, neither the County nor the CHMC service area achieved this objective
in 2005. In Los Angeles County in 2005, the rate of uninsured children age 0-17 was
8.3%, slightly lower than in 2003 (10.3%). From 2003 to 2005, rates of uninsurance for
all non-elderly adults dropped in all CHMC health districts with available data, except the
Central district. The highest percentage of uninsured residents in the CHMC service area
remained in the Central district (40.7%), while the lowest rate was reported in the West
district (11.8%). The South (18.2%) health district reported the highest rate of
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
26
uninsurance among children in 2005, while the West district (4.0%) reported the lowest
rate.
Regular Source of Care - The Healthy People 2010 objective is to increase the
percentage of persons with a usual primary care provider to 85%. Rates of a usual
source of care remained similar county-wide (80.7% in 2003 to 80.2% in 2005). In 2005,
all of the CHMC health districts, except the Inglewood (80.9%) and West (84.2%)
districts reported lower rates of adults with a regular source of care compared to the
county as a whole, and all CHMC health districts failed to meet the 2010 objective. With
the exception of the Central, Inglewood, and West districts, all CHMC health districts
also reported decreases in rates of regular source of care from 2003 to 2005.
Emergency Room Visits – Approximately 22% of adults in Los Angeles County
indicated visiting the emergency room (ER) in 2005. The highest rates of ER visits in the
CHMC health districts in 2005 were in the Southeast district (33.8%), followed by the
Southwest (25.1%) and Inglewood (25.1%) districts. The lowest rate was reported in the
Hollywood district (19.2%).
Childhood Immunization - Vaccination coverage in California is high and has nearly
reached the 2010 objective (90% for individual antigens and 80% for vaccine series) for
children 19 to 35 months. Furthermore, data indicate that cases of vaccine preventable
diseases are at or near the lowest ever. In 2005, the estimated vaccination rates in Los
Angeles County for children age 2 to 4 years and 11 months (94.3%) and children
enrolled in kindergarten (91.3%) were comparable to the state, as was the estimated
vaccination rate for children age 11 to 13 years (77.7%).
Influenza Vaccination - The Healthy People 2010 objective is to increase the
percentage of adults (65+) who are vaccinated annually against influenza to 90%. In
2005, neither the county nor the CHMC health districts achieved the 2010 objective, but
there were improvements among CHMC health districts. Over half (61.6%) of Los
Angeles County adults 65+ received influenza vaccinations in 2005, an 8% decrease from
2003. Of the CHMC health districts, the Hollywood district reported the greatest increase
(7.8%) from 2003 to 2005. In 2005, the highest rate of vaccination was reported by the
Central (75.9%) district.
Pneumonia Vaccination- The Healthy People 2010 objective is to increase the
percentage of adults (65+) who are vaccinated annually against pneumococcal disease
to 90%. In 2005, this objective was not met at the county level or within any of the
CHMC health districts. In Los Angeles County, 57.7% of adults reported ever having
received a pneumonia vaccination. Among the CHMC health districts in 2005, the lowest
rate of pneumonia vaccination was reported in the Central district (35.6%), while the
highest was reported in the Hollywood district (58.4%).
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
27
Cervical Cancer Screening - The Healthy People 2010 objective is to increase the
percentage of women aged 18+ who received a Pap test within the preceding three
years to 90%. In 2005, this objective was not met at the county level or within any of the
CHMC health districts. In Los Angeles County in 2005, 83.8% of women age 18+
reported receiving a Pap smear during the previous three years. Of the CHMC health
districts in 2005, the South (74.3%) and Southwest (78.9%) districts reported the lowest
rates of Pap smear screening, while the Southeast district (88.8%) reported the highest. In
2005, the Central district experienced the greatest increase (8.5%) in Pap smear rates of
the CHMC health districts, but in general, rates were consistent from 2003 to 2005 across
all districts.
Breast Cancer Screening - The Healthy People 2010 objective is to increase the
percentage of women aged 40+ who have received a mammogram within the preceding
two years to 70%. In 2005, the county met the 2010 objective, with 70.6% of women age
50+ having received a mammogram within the previous two years. Among the CHMC
health districts, only the Hollywood (70%), Inglewood (70.7%) and Southeast (73.3%)
districts achieved the 2010 objective.
Colorectal Screening -The Healthy People 2010 objective is to increase the percentage
of adults aged 50+ who have received colorectal cancer screening via blood stool test or
sigmoidoscopy to 50%. In 2005, this objective was met in Los Angeles County with
63.8% of adults reporting that they had received colorectal cancer screening. Among the
CHMC health districts in 2005, all met the Healthy People 2010 objective for colorectal
cancer screening, with the Inglewood district (70.0%) reporting the highest rate of
screening and the Hollywood district (53.9%) the lowest.
Prostate Cancer - The Healthy People 2010 objective is to reduce the prostate cancer
death rate to 28.8 per 100,000. In 2004, the Los Angeles County prostate cancer death
rate met this objective (23.0 per 100,000).
Cholesterol - The Healthy People 2010 objective is to increase the percentage of adults
who have had their blood cholesterol checked within the preceding five years to 80%.
In 2005, Los Angeles County reported 88.9% of adults with cholesterol screenings,
meeting the 2010 objective. Of the CHMC health districts in 2005, the majority reported
cholesterol screening rates that were comparable to that of Los Angeles County; all but
the Central district met the 2010 objective. The Inglewood district (91.6%) reported the
highest rate and the Central district (79.4%) the lowest.
Dental Care – The Healthy People 2010 objective is to increase the proportion of
children and adults who use the oral health care system each year to 56%. In 2005,
74.4% of adults and 82.9% of children obtained dental care meeting the 2010 objective
(25.6% of adults and 17.1% of children in the county did not obtain dental care in the
past year because they could not afford it). Compared to the county, in the CHMC service
area in 2005, SPA 4 (31.8%) and SPA 6 (35.1%) reported notably higher rates of adults
who did not obtain care because they could not afford it, while SPA 4 reported higher
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
28
rates of children (21.2%) who did not obtain oral care because their parents could not
afford it.
Obesity - The Healthy People 2010 objective is to reduce the percentage of adults who
are obese to 15%. In Los Angeles County in 2005, 20.9% reported being obese, a slight
increase from 2003 (19.3%). The obesity rate for the county was higher than the Healthy
People 2010 objective of 15%. Of the CHMC health districts in 2005, the Southeast
(27.5%) and Southwest (27.5%) districts reported the highest rates of adult obesity. No
CHMC health district met the 2010 objective. The Hollywood district (16.5%) reported
the lowest rate and the Southeast and Southwest districts (27.5%, respectively) reported
the highest.
Physical Activities - The Health People 2010 objective is to reduce the percentage of
adults who engage in no leisure-time physical activity to 20%. In Los Angeles County
from 2003 to 2005, there were decreases in the rates of people who reported a sedentary
lifestyle from 42.6% to 37.5%; however, this was still higher than the 2010 objective. All
CHMC health districts except the Southeast district also reported decreases from 2003 to
2005, but the 2010 objective was still not met. In 2005, especially high rates were
reported in the Southeast (45.5%) and Southwest (42%) districts.
Smoking - The Healthy People 2010 objective is to reduce the percentage of adults who
smoke cigarettes to 12%. In Los Angeles County, the rate of smoking decreased from
2003 to 2005 (15.6% to 14.6%), but failed to meet the 2010 objective. Rates of adult
smoking increased in all of the CHMC health districts except the West and Hollywood
districts, which reported the greatest decreases (1% and 6.7%, respectively). Of the
CHMC health districts in 2005, the South district (25.2%) reported the highest rate of
adult smokers followed by the Inglewood and Southeast health districts (18.4% and
18.1%, respectively); the lowest rate was reported in the West district (13.3%); all fell
short of the 2010 objective.
Binge Drinking - The Healthy People 2010 objective is to reduce the percentage of
adults engaging in binge drinking during the past month to 6%. In Los Angeles
County, the percentage of adults who reported binge drinking did not meet the 2010
objective in either 2003 (17.1%) or 2005 (17.3%). Among the CHMC health districts in
2005, the Southeast district (20.3%) reported the greatest percentage of adult binge
drinking, while the Southwest district (10.7%) reported the lowest; thus no CHMC
district met the Healthy People 2010 objective of 6%.
Drug Use – the Healthy People 2010 objective is to reduce the percentage of adults
using any illicit drugs during the past 30 days to 2%. In 2005, reported use of marijuana
in Los Angeles County was 8.2%, higher than the 2010 objective. Of the CHMC health
districts in 2005, the Hollywood district reported the greatest use of marijuana (13.9%)
while the West district (8.6%) reported the lowest; no CHMC district met the 2010
objective.
Diabetes - The prevalence of diabetes among adults in Los Angeles County increased
from 7.2% in 2003 to 8.1% in 2005. Of the CHMC health districts, the Central district
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
29
reported the greatest increase (7.5%) in adults with diabetes from 2003 to 2005. In 2005,
the highest rate was reported in the Southwest district (12.1%) and the lowest in the
West district (4.5%).
Asthma – In 2005, 6.5% of adults in Los Angeles County were diagnosed with asthma,
an increase of 0.4% from 2003. In the CHMC service area in 2005, SPA 5 reported the
greatest percentage of adults with asthma (7.6%), as well as the greatest increase in adults
with asthma from 2003 (5.7%) to 2005 (7.6%). Of the CHMC health districts in 2005, the
Southwest district reported the greatest percentage of adults diagnosed with asthma
(8.1%), while the Central district (5.2%) reported the lowest. The Central district (9.1%)
reported the greatest percentage of children diagnosed with asthma.
Heart Disease - The prevalence of heart disease increased in Los Angeles County from
2003 (6.3%) to 2005 (6.8%). Among the CHMC health districts in 2005, the Inglewood
and West health districts reported the greatest increase (2.8%, respectively) in adults
diagnosed with heart disease. The Central district (4.9%) reported the largest decrease in
heart disease diagnosis (2.7%) from 2003 to 2005. In 2005, the Inglewood (8.1%) health
district had the highest rate of heart disease diagnosis, while the Southeast (3.8%) district
had the lowest.
HIV/AIDS - The Healthy People 2010 objective is to reduce the rate of AIDS among
adolescents and adults to 1 per 100,000. General trends from 1992 to 2006 county-wide
show that annual rates and the total number of AIDS cases have been declining. In Los
Angeles County in 2005, the rate of AIDS diagnosis was 12 per 100,000. Within the
CHMC service area from 2002-2006, AIDS infection rates were consistently highest in
the Central (20 per 100,000 in 2006—preliminary data) and Hollywood (14 per 100,000
in 2006—preliminary data) health districts; the rates for both of these districts increased
from 2005 to 2006. The Healthy People 2010 objective is to reduce the rate of deaths
from HIV infection to 0.7 per 100,000. Within the CHMC service area, the cumulative
number of AIDS related deaths was highest in SPA 4 with 11,849 deaths between 1982
and 2006. This is slightly more than one-third of all AIDS related deaths in Los Angeles
County during this time period. Neither the county nor the CHMC service area met the
2010 objectives for HIV infections or deaths from HIV infection
Tuberculosis - The Healthy People 2010 objective is to reduce the rate of tuberculosis
cases to 1 per 100,000. In Los Angeles County, there has been a slight downward trend
in tuberculosis cases but the county accounted for the largest percentage (31.2%) of
tuberculosis cases reported in California in 2005. In Los Angeles County in 2005, there
were 9.5 reported cases of tuberculosis per 100,000, higher that the 2010 objective. In the
CHMC health districts from 2003 to 2004, the number of tuberculosis cases increased in
the Hollywood (70 to 86 cases), and South (38 to 40 cases) districts and in 2004, the
Central (107 cases) and Hollywood (86 cases) districts had the highest number of
reported tuberculosis cases.
Hepatitis B - The Healthy People 2010 objective is to reduce the number of chronic
hepatitis B infections in infants and young children to 400 infections. In Los Angeles
County alone in 2005, 768 infants were born to 756 hepatitis B surface antigen (HBsAg)
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
30
positive women, an increase of 4% from 2004 (LAC/DHS, 2005); this was higher than
the Healthy People 2010 objective.
Hepatitis C - The Healthy People 2010 objective is to reduce the rate of chronic
hepatitis C infections to 1 per 100,000. From 2001 to 2003, the crude case rates of newly
reported cases in Los Angeles County (0.07 per 100,000) met the 2010 objective. More
recently in 2005, there were 3 cases of confirmed acute hepatitis C in Los Angeles
County, a decrease from 5 cases confirmed in 2004.
Chlamydia - In 2005, the rate of chlamydia in Los Angeles County was 405.5 per
100,000 compared to the California rate of 352.1 per 100,000 and the national rate of
332.5 per 100,000. In the CHMC service area, SPA 6 reported the highest rate of
chlamydia (859.5 per 100,000). Of the CHMC health districts, the South (1,172.6 per
100,000), Southeast (737 per 100,000), and Southwest (816.9 per 100,000) districts
reported the highest infection rates.
Gonorrhea - The Healthy People 2010 objective is to reduce the rate of gonorrhea to 19
per 100,000. In 2005, the infection rate for gonorrhea in Los Angeles County (109.5 per
100,000) did not meet the 2010 objective. In the CHMC service area in 2005, the
gonorrhea rate was highest in SPA 6 (290.1 per 100,000). Among the CHMC health
districts, the Southwest (318.5 per 100,000) and South (419.4 cases per 100,000) districts
had the highest rates. No CHMC health district achieved the 2010 objective.
Syphilis - The Healthy People 2010 objective is to reduce sustained domestic
transmission of primary and secondary syphilis to 0.2 per 100,000. In 2005, the
infection rate in Los Angeles County was 6.7 per 100,000. In the CHMC service area in
2005, SPA 4 (16.8 per 100,000) had the highest infection rate. Among the CHMC health
districts, the Hollywood (38.9 per 100,000) and Central (16.4 per 100,000) districts
reported the highest rates. Neither the county nor the CHMC health districts achieved the
2010 objective.
Mental Health - In Los Angeles County in 2005, 18.9% of respondents reported needing
help for emotional or mental health problems. In the CHMC service area in 2005, SPA 5
(23.7%) and SPA 6 (21.8%) reported the greatest percentages of individuals needing help
for emotional or mental health problems. SPA 6 reported the greatest percentage of
respondents at risk for mental illness (9.2%).
Housing/Homelessness - In 2005, it was estimated that there were 82,291 homeless
individuals living in Los Angeles County. Of those individuals, the majority were
unsheltered, living on the streets, in a vehicle, or an abandoned building. In the CHMC
service area, SPA 4 and SPA 6 had the largest homeless populations. SPA 4 did,
however, report the highest ratio (approximately 1:4 ratio) of beds to homeless persons.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
31
Food Insecurity - In 2005, 25.5% of households living below 300% Federal Poverty
Level (FPL) were experiencing food insecurity in the county, an increase from 21.8% in
2003. In the CHMC service area in 2005, SPA 6 (33.1%) and SPA 4 (28.8%) reported the
largest percentages of households with food insecurity. Among the CHMC health
districts, the South (45.8%) and Southeast (40.7%) districts reported the highest
percentages of households with food insecurity, as well as, the largest increases from
2003 to 2005. The Hollywood district reported the largest decrease in the rate of food
insecurity, from 30.7% in 2003 to 25.6% in 2005.
Safety/Crime – The violent crime rate in Los Angeles County has decreased in recent
years to a rate of 649 per 100,000 in 2005. In the City of Los Angeles in 2005, 6,668
gang-related crimes occurred, the lowest number in the past five years. However, in
2006, gang-related crimes increased 15% from the previous year. Although most of the
increase in gang crimes occurred in the central and south region of the city, recent
increases were also found in the San Fernando Valley and West areas of the city. The
juvenile felony arrest rates increased from 1,325.9 per 100,000 in 2004 to 1,384.7 per
100,000 in 2005 and the homicide death rate increased from 10.8 per 100,000 in 2004 to
11.3 per 100,000 in 2005.
Domestic Violence - In Los Angeles County, the number of domestic violence related
calls has been decreasing steadily from 2000 to 2005. Domestic violence arrests in the
county have also been steadily declining from 2001 to 2005. However, in 2004, the City
of Los Angeles accounted for 57% of all domestic violence-related calls for assistance in
the county, much larger than the next city, Long Beach (4.5%).
Child Abuse - The Healthy People 2010 objective is to decrease the rate of child abuse
to 10.3 per 100,000. The child abuse rate in Los Angeles County in 2005 was 61.2 per
100,000, much higher than the 2010 objective. The percentage of children in the Los
Angeles County DCSF caseload (3.9%) as well as the percentage of emergency referrals
(1.2%) increased from 2004 to 2005. In the CHMC service area in 2005, SPA 6 reported
the highest number child abuse and neglect referrals (24,244 referrals) but this is a
decrease from 2004 (26,385 referrals). While SPA 6 decreased in the number of referrals
from 2004 to 2005, SPA 8 increased from 16,148 to 21,822 and SPA 4 increased from
15,729 to 16,532.
Teen Pregnancy - In Los Angeles County, the teen birth rate has been consistently
dropping in recent years, and in 2004, the rate was 8.1 per 1000. In the CHMC service
area from 2002 to 2004, SPA 6 consistently reported the highest teen birth rate in Los
Angeles County followed by SPA 4. In 2004, SPA 6 reported the highest number of live
births to teen mothers (1,256 births).
Immigration - In 2004, Los Angeles County was home to approximately 3.8 million
foreign born individuals. Of the immigrant population in the county, documented
immigrants (74%) were much more prevalent than undocumented immigrants (26%). The
Majority of children in the county (62%) had immigrant parents and of these children,
43% had documented immigrant parents and 19% had undocumented immigrant parents.
Compared to the native-born population in the county, large numbers of immigrant adults
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
32
and children are not covered by health insurance. The uninsured rate is much higher for
undocumented
immigrant
adults
and
their
children.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
33
COMMUNITY BENEFIT PLANNING PROCESS
Developing CHMC’s Community Benefit Report and Plan
The Community Benefits Planning Work Group for FY 08-09 consisted of: Hospital
President, Foundation President, Senior Vice President of Business Development,
Director of Community Benefits, Director of Grants and Contracts, and three members of
the Community Board. The Work Group considered the following documents as it began
its deliberations:
Hope Street Family Center’s 2006 Community Needs Assessment
2007 California Hospital Medical Center Community Needs Assessment
California Hospital Medical Center’s Draft Strategic Plan
Problems linked to high utilization rates at CHMC
The table below lists key focus areas of CHMC’s Strategic Plan and key findings of the
2007 Community Needs Assessment:
Hospital Strategic Plan
Downtown development/population growth
Population growth projected of 6.6% by 2009
Highest growth segments in age groups 45-64
(3.2%) and 65+ (2.7%); predominantly
Hispanic with decline in African Americans
and Asians
Upscale housing construction downtown to
North and East of CHMC. New demographic
(N=30,000):Caucasian (53%), Asian (25%),
Hispanic (10%), and African American (5%);
predominantly young, single, male
professionals between 23 and 34.
Capacity constraints
High volume: Obstetrics
NICU
Pediatrics
ED
Community Needs Assessment
Gentrification may lead to shortage of low
cost/affordable housing and increased
homelessness.
Early prenatal care, teen pregnancies
High LBW, VLBW, and infant mortality rate
Asthma
Crime, gang violence, DV, safety issues
Access problems: primary & specialty care
Drug overdosing
Asthma
Critical care beds
Impact of providing Trauma services
Injury prevention program necessary
Increased focus on Medicare population
Cardiovascular
Crime, gang violence, DV, safety issues
Homicide is a leading cause of premature death .
CV disease = leading cause of death;
cerebrovascular disease = 3rd
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
34
Pulmonary
Oncology
Asthma, tuberculosis, COPD; high rates of
smoking
Cancer = 2nd leading cause of death; low
screening rates
Orthopedics
HIV/AIDS and STDs high prevalence rates
Obesity
Diabetes = 4th leading cause of death; increasing
prevalence
Binge drinking
Illicit drug use
Problem: high rate of uninsured patients
Access Problems
Health insurance
Primary care
Specialty care
Preventive health services
Mental health services
Dental care
Community characteristics
Primarily young Latino families
Large % of foreign born residents (61%)
Extremely poor
Low literacy level, low educational attainment
High rates of food insecurity
Working in low wage jobs
Overcrowded housing; very old housing stock
Insufficient licensed childcare capacity
High rates of disabilities among school children
(5%), especially speech & language
impairments
Large #s of unimmunized/underimmunized
children
70% of elementary schools with API < 3
1.
To address capacity constraints of the hospital, it is important to provide
comprehensive community-based patient education on common chronic
conditions. Patients seen in the ED or being discharged from the hospital will be
referred to relevant Community Benefits educational programs.
Health Ministry Program will continue to provide health screens, health
education, and referrals for primary healthcare at our Health Ministry sites in
the community. Examples of common chronic conditions that will be
discussed include: asthma, diabetes, cardiovascular disease, cancer, arthritis
and nutrition and your body.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
35
Healthy Eating Lifestyle Program addresses the current epidemic of
pediatric obesity. The long-term goal of this program is to prevent the
development of complications such as type 2 diabetes, cardiovascular
disease, osteoarthritis, and various cancers.
Type 2 Diabetes Prevention, Screening, and Intervention Program
provides comprehensive educational offerings for patients at high risk for the
development of type 2 diabetes and for those already diagnosed with the
disease. This program fulfills the recommendations of the CDC’s Task Force
on Community Preventive Services in that it integrates disease management,
case management, and self-management education. A recent telephone
survey of past participants of Living with Diabetes Program at CHMC
revealed an amazing 87.2% reduction in hospitalizations and an 87.5%
decrease in ED visits for glucose control during the six months following
program participation.
Chronic Disease Self-Management Program helps patients with one or
more chronic conditions learn to manage their health and maintain active and
fulfilling lives. A recent telephone survey of past CDSMP participants at
CHMC revealed a remarkable 50% reduction in hospitalization and an 80%
reduction in ED visits during the year following program participation.
Poor dental hygiene and periodontal disease contribute to the development
of, and complications from, various diseases such as diabetes,
cardiovascular disease, and premature and low birthweight babies. The
Community Dental Partnership provides oral health education, access to
free basic dental services and periodontal services for uninsured adults with
diabetes mellitus living in Central Los Angeles.
2.
In order to increase access to primary healthcare, Para Su Salud Program
assists children and their families to enroll in health coverage programs and
utilize and retain these benefits.
3.
As a result of being designated as a Trauma Center, CHMC must provide the
following array of injury prevention services. These prevention services are
based on identification of specific injuries and risk factors in the community.
Gang Prevention
.
Developed in collaboration with the Bresee Foundation, the Hope Street
Youth Center is an afterschool program for school-aged youth, often the
older sibling of participants in our early intervention programs or graduates of
our programs. Eighty-nine percent of the students read below grade level,
with the average difference being 3.2 years, with a range of 1-8 years below
grade level. Through the Center, children are able to participate in an
innovative literacy program – Help One Student to Succeed (HOSTS)-that
matches volunteer mentors with students needing assistance in reading and
language arts. An educational plan is developed for each HOSTS student,
who then works with an adult mentor to achieve identified goals one hour a
week. The Center also provides homework assistance, a computer lab,
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
36
supervised recreational and social activities, including soccer, arts and crafts,
circus arts, field trips, and other outings.
CHMC is one of only three medical facilities nationwide with an on-site
continuation high school program. Established in partnership with LAUSD,
Central High School provides a safe and supportive classroom environment
for 25 students, who have experienced difficulties in other school settings and
many of whom are former dropouts, an opportunity to graduate and earn a
high school diploma. Some of these students are parents or older siblings of
EHS children. Approximately 90% of these at risk students successfully
graduate. UCLA donated several new computers for the classroom’s
computer learning lab. Students of the HSYC use these computers in the
afternoons with the help of a UCLA work-study student. These computers
were also used for a college course on Media studies taught by faculty from
Trade Tech on Saturday morning for the continuation high school students
and other students from HSYC. This experience motivated many students to
aspire to attend college rather than ending their education with a high school
diploma.
Nurse Family Partnership is one of the six original replication sites for the
Prenatal and Early Childhood Nurse Home Visitation Program developed by
Dr. David Olds. This highly acclaimed, well-tested and cost-effective model
improves the health and social functioning of low-income, first-time young
mothers and their babies. Program participants have fewer reports of child
abuse and neglect and fewer subsequent children; they are less likely to use
welfare, have substance abuse problems, engage in crime or be
unemployed. Moreover, an economic evaluation by the RAND Corporation
found that government funds invested in this program were recovered by the
time participating children were four years old and that the cost savings over
the life of the child far exceeded the investment. At CHMC, 100 young,
unmarried, first-time pregnant women receive regular home visits by public
health nurses funded by the L.A. Department of Health. These nurses provide
carefully prescribed case management, parenting education, and
psychosocial support that begins during pregnancy and continues until the
child is two years old.
“Adolescents born to women who received nurse visits during pregnancy and
postnatally and who were unmarried and from households of low
socioeconomic status (risk factors for antisocial behavior), in contrast with
those in the comparison groups, reported fewer instances of running away,
fewer arrests, fewer convictions and violations of probation, fewer lifetime sex
partners, fewer cigarettes smoked per day, and fewer days having consumed
alcohol in the last 6 months.” JAMA 1998;280:1238-1244.
The Responsible Fatherhood Program offers the following mental health
services:
Preparing for Successful Fathering, a 12 week parenting curriculum
developed by Dr. Ron Klinger, a practicing psychologist. Curriculum
topics include: Fathers as Role Models, Creating a Vision for Fathers,
Bonding through Play (incorporating children), Care-Giving Differences
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
37
between Mothers and Fathers, Discipline and Limit Setting, Game Plan
for Success, and Preparing for Solo Time with Kids.
Conflict Management classes, a series of 26 sessions that will address
conflict and anger issues in relationships.
Fathers’ Group, a support group co-facilitated by the Father Service
Specialist and a Father mentor
Brief, solution-focused individual, conjoint, and group counseling led by a
masters level clinician (Fathers Service Specialist) trained in conflict
resolution and family systems theory.
Youth ALIVE!’s Caught in the Crossfire program hires young adults who
have overcome violence in their own lives to work with youth who are
hospitalized due to violence-related injuries. The purpose is to reduce
retaliation, re-injury, and arrest and promote positive alternatives to violence.
A study of 112 violently injured youth (12-20 yr of age; 80% male;
predominantly African American [60%] and Latino [26%]) hospitalized in
Oakland, CA participated in a retrospective case-control study. Clients were
matched by age and injury severity. Treatment and control youth were
followed for six months after their original dates of injury. Intervention youth
were 70% less likely to be arrested for any offense (odds ratio = 0.257) and
60% less likely to have any criminal involvement (OR=0.356) when compared
to controls. No statistically significant differences were found for rates of reinjury or death, which were 1.8% and 0, respectively. CHMC’s ED plans to
implement this program this year.
As soon as a young person is admitted to the hospital with a violencerelated injury, staff call in the Intervention Specialist, who arrives within
one hour to help the injured patient and his/her families and friends cope
with the injury and talk about alternatives to retaliation. Alternative
strategies for dealing with conflict are promoted, the youth’s short-term
needs are identified, and a plan for staying safe is developed.
After the young person leaves the hospital, the Intervention Specialist
continues to foster the relationship, easing the youth’s transition back into
the community through personal and telephone follow-up contact. The
Specialist provides support and mentoring to the youth as well as to
his/her family through intensive case management. This continues for as
long as the youth desires, typically six months to one year, with contact
occurring at least once a week.
The Intervention Specialist coordinates assistance from social services
providers; probation officers; school teachers, administrators, and
guidance counselors; medical staff; and other youth service
professionals.
The Intervention Specialist links the youth and his/her family with local
resources that meet the participants’ basic needs and promote healthy,
nonviolent lifestyles, such as: medical coverage and follow-up care;
educational programs; job training programs; employment opportunities;
counseling; life skills training; legal assistance; and recreational
programs.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
38
Pedestrian Safety
CHMC will distribute bilingual information re pedestrian safety at local Health
Fairs.
Community health promoters of CHMC’s Health Ministry Program give
educational classes on pedestrian safety. It is emphasized that since the
opening of our Trauma Center, almost one third of the patients were
pedestrians struck by automobiles.
Child Seat Safety
Car seat safety is stressed during Hospital Tours for pregnant women and
their partners and again when the baby is discharged from the Hospital.
Every new parent receives a free “Kit for New Parents” developed by First 5
California. The kit contains 6 videos with helpful parenting information, a
parenting resource guide, tips on important topics including: health and
nutrition, child safety, early literacy, discipline, and finding quality child care.
Child Abuse and Neglect
Founded in 1996, the Pico-Union Family Preservation Network offers an
integrated, comprehensive approach to strengthen and preserve families at
risk of, or already experiencing, problems in family functioning. Its goal is to
assure the physical, emotional, social, educational, cultural, and spiritual
development of children in a safe and nurturing environment. Referred by the
Los Angeles Department of Children and Family Services, up to 60 families
each year receive a variety of services that are delineated in individual case
plans. Such services can include: in-home counseling, childcare, physical
and developmental services, housing, income support, mental health
services, parenting education, substance abuse treatment, domestic violence
counseling, and therapeutic day treatment for juvenile offenders. After
receiving 6-12 months of services in the program, families with young
children sometimes transition to HSFC’s EHS program where they can be
followed for a longer period of time.
Early Head Start, the centerpiece of the HSFC, provides 152 low-income
pregnant women and their families with children, 0-3 years of age, with
family-centered services to facilitate child development, support parental
roles, and promote self-sufficiency. Core services include early childhood
education; healthcare and mental health services; parenting education;
childcare; adult education; and housing, legal and financial assistance.
The Nurse Family Partnership is one of the six original replication sites for
the Prenatal and Early Childhood Nurse Home Visitation Program developed
by Dr. David Olds. This highly acclaimed, well-tested and cost-effective
model improves the health and social functioning of low-income, first-time
young mothers and their babies. Program participants have fewer reports of
child abuse and neglect and fewer subsequent children; they are less likely to
use welfare, have substance abuse problems, engage in crime or be
unemployed
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
39
The Responsible Fatherhood Program offers a variety of mental health
services and educational groups that improve interpersonal and parenting
skills of fathers.
The Healthy Marriage Program provides one-day skill-based workshops for
couples and/or single parents aimed to support parents in developing and
sustaining healthy relationships in ways that help them be better parents and
experience more satisfying, long-lasting relationships, which will in turn have
beneficial long-term effects on their children’s development and future life
choices.
In order for parents to work and/or attend school, they must have safe places
to leave their children. Therefore we established three Child Development
Centers and an Extended Day Family Childcare Network.
In 1997, CHMC opened the Child Development Center, a licensed
childcare facility on the first floor of Leavey Hall that fills a community
need for local, quality childcare with a strong developmental focus. The
facility can accommodate 46 children daily, ranging in age from 6 weeks
to 5 years, and meets federal EHS/HS performance standards. Center
hours are 7 a.m. to 6 p.m., Monday through Friday. This facility primarily
serves EHS families working toward self-sufficiency, i.e., employed in the
nearby garment and light manufacturing district or enrolled in LAUSD
Adult Education Centers. Children enrolled in the CDC continue to
receive home-based EHS services three times per month. In addition, the
home visitor makes one visit per month, with the parent present, at the
CDC to talk together with the teacher and learn more about the child’s
skills within the classroom environment.
Family Childcare Network includes 12 childcare providers who are
licensed to provide childcare in their homes. HSFC helped these
providers start their own childcare businesses and continues to provide
technical assistance, support, training and guidance for them. They now
provide high quality, culturally responsive, developmentally focused
childcare for children, 0-5 years of age, that meets the rigorous EHS/HS
performance standards. Moreover, they offer childcare during
nontraditional hours such as evenings and weekends. This meets the
needs of many working and studying EHS parents.
Early Childhood Center is another licensed, center-based childcare
facility, co-located at a church in the middle of CHMC’s service area, and
administratively supported by CHMC. It accommodates 8 infants, 24
toddlers, and 24 preschool aged children, Monday through Friday, from
6:30 a.m. to 6:00 p.m., and it meets EHS/HS performance standards. Like
HSFC’s other childcare programs, it uses the Creative Curriculum as the
basis for the arrangement of the physical environment, weekly lesson
planning, weekly observational notes, and ongoing child assessments
and observations
In 2007, HSFC opened their third licensed child development center
across the street from CHMC in Mercy Housing, the Early Care and
Education Center. It accommodates 16 young children, ages 6 wks to
24 months and 36 children ages 2-5 years. It is open Monday through
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
40
Friday, from 6:30 a.m. to 6:00 p.m. and meets EHS/HS performance
standards. Like HSFC’s other childcare programs, it uses the Creative
Curriculum as the basis for the arrangement of the physical environment,
weekly lesson planning, weekly observational notes, and ongoing child
assessments and observations
Family Violence Prevention
A community health promoter conducts single session classes at our Health
Ministry sites that cover topics such as the dynamics of domestic violence,
power and control, impact of domestic violence on children, and safety
planning. In addition, she conducts four-week discussion groups entitled
“Building Healthy Relationships” that covers self- esteem, healthy
communication, and conflict resolution. We also do a lot of community
outreach to raise local awareness about domestic violence and available
resources at local community health fairs and disseminate of resource
information at natural community gatherings sites such as laundromats, nail
and hair salons, primary care clinics, schools, and churches.
4.
The Responsible Fatherhood Program offers a series of 26 sessions that
address conflict and anger issues in relationships.
The Healthy Marriage Program provides one-day workshops entitled
“Talking Points” for couples and/or single parents; meals and childcare are
provided during the workshop. The 8-hour skills-based class, offered in
either English or Spanish, on a week-end day aims to support parents in
developing and sustaining healthy relationships in ways that help them be
better parents and experience more satisfying, long-lasting relationships,
which will in turn have beneficial long-term effects on their children’s
development and future life choices. The objectives are to:
Strengthen parents’ communication
Improve relationship skills
Increase conflict management skills
Improve problem solving skills
Reinforce positive parenting skills
Create parent peer support networks
Reduce family stress through linkages to additional services
Increase relationship satisfaction and appreciation of one another as coparents
Peer-led support groups reinforce material learned in workshops. Couples
have access to couples counseling provided by social work interns. They can
also participate in Weekend Relationship Growth Retreats, bi-annual
overnight growth retreats for twelve couples at the Holy Spirit Retreat Center
in Encino, CA.
More than 5,000 babies are delivered at CHMC annually and CHMC is the
acknowledged provider of choice for women’s health services in Central Los
Angeles. But, CHMC was not satisfied with just optimizing birth outcomes; it
wanted these children to reach adulthood having experienced a safe, healthy
(physical, cognitive, social, and emotional), and nurturing childhood that prepares
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
41
them to become responsible and contributing members of the community. Only
then could CHMC achieve its vision of “improving the health and well-being of the
community by helping people help themselves.” In September, 1992 the Hope
Street Family Center was founded to address several critical factors: prevalence
of poverty, prevalence of immigrants, low literacy rate, issues regarding the
delivery of healthcare, including prenatal care, lack of affordable, quality child
care, and the need for family mental health services.
Moreover, since it is well known that literacy skills predict an individual’s health
status more strongly than age, income, employment status, education level, and
racial or ethnic group, most of HSFC’s program have a strong focus on improving
literacy skills. For low-income households in particular, pregnancy is often the
only time that a woman and her family come in contact with the health care
system. Prenatal care may serve as a critical point of entry for services related
to early child development. For example, risk assessments done in conjunction
with healthcare help identify families who would most benefit from early
intervention services. In addition, early identification of fetuses with congenital
anomalies and of newborns who are medically fragile or at high risk for
developmental delay allows triage to appropriate case management and early
intervention services upon discharge from the hospital. It is therefore fitting to
nest the HSFC in the midst of CHMC – what better way to optimize a child’s
life course trajectory?
Up until the 1960’s, a “healthy child” was usually equated to a disease-free child.
However, today’s evolving child health paradigm defines a healthy child to be not
merely disease-free, but one who functions at the highest potential in all aspects
of life, including physical, mental, and social functioning. It considers the child “in
context” within his/her family, community, and society at large. Stakeholders are
no longer limited to traditional medical providers and the healthcare system;
today’s child health community involves multidisciplinary, multi-sector
stakeholders. Moreover, the focus of healthcare is shifting toward
preventing adult disease that begins prenatally and in childhood and
toward addressing the family determinants of children’s long-term health
status. Therefore, the complete integration of health services and family support
services at a busy birthing hospital makes a lot of sense.
In 1995 David Barker wrote: “The fetal origins hypothesis states that fetal
undernutrition in middle to late gestation, which leads to disproportionate fetal
growth, programmes later coronary heart disease.” The association between
birth size and cardiovascular morbidity is largely modified by growth later in life.
The highest risk of coronary heart disease is seen among individuals who are
born small and rapidly increase their body weight during childhood.
Fetal growth restriction resulting in low birthweight and low weight gain in
infancy are risk factors for childhood obesity, and adult cardiovascular
disease (abnormal lipid values, hypertension, and ischemic heart
disease), type 2 diabetes, and the metabolic syndrome.
The risk for cardiovascular disease is also increased in people who have
an early adiposity rebound in childhood and who are obese during
childhood, adolescence and adult life. The adverse effects of
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
42
childhood and adult obesity on cardiovascular disease and its risk factors
are exaggerated in people of low birthweight and relatively small in those
of high birthweight.
Fetal macrosomia is a risk factor for childhood and adult obesity and type
2 diabetes.
Maternal obesity during pregnancy is associated with a host of problems
including:
Antepartum: higher prevalence of chronic medial conditions such as
type 2 diabetes, coronary heart disease, hypertension, and
osteoarthritis; gestational diabetes, preeclampsia, preterm birth,
multifetal gestation, and urinary tract infections.
Intrapartum: labor induction, dysfunctional labor, higher cesarean birth
rates, anesthetic complications, postpartum hemorrhage
Postpartum: infections, prolonged hospitalization, thrombotic
complications, pregnancy weight retention, lactation dysfunction,
increased risk for maternal death.
Perinatal: birth defects, prematurity, macrosomia, birth injury, perinatal
mortality
Childhood obesity
Adult obesity and obesity-related diseases
Thus, the promise of the fetal origins paradigm is that attending to the health of
women of reproductive age will have profound impact on the wellbeing of their
offspring. The importance of this issue closely parallels WHO’s World Health
Report 2005 – “Make every mother and child count.” Lu and Halfon (Maternal
and Child Health Journal 2003; 7: 13-30) posit that a woman’s reproductive
potential is a function of her developmental trajectory set forth by early life
experiences (early programming mechanism) and altered by cumulative
allostatic load (chronic accommodation to stress) over the life course.
(See Figure below) The trajectory is drawn as curves rather than as straight
lines to underscore the notion of sensitive periods during which development
is particularly vulnerable to the influences of “risk factors” (downward
arrows) and amenable to those of “protective factors” (upward arrows). These
sensitive periods are depicted as steep accelerations in the slopes of the
developmental trajectory that occur in utero and early life and possibly during
puberty.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
43
Life Course Perspective
Disparities in Birth Outcomes
Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective.
Matern Child Health J. 2003;7:13-30.
From the life-course perspective, eliminating racial-ethnic disparities in birth
outcomes will require 1) closing the gap in one generation to give the next
generation an equal start, 2) targeting interventions during sensitive
developmental periods (e.g., in utero development, early childhood, puberty,
pregnancy), and 3) risk reduction and health promotion strategies across the
life span. Such strategies “pull up” the trajectory by mitigating risk factors,
and “push up” the trajectory by promoting protective factors. The following
table lists some of the risk factors and protective factors that are addressed
by CHMC’s Community Benefits Programs.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
44
Risk Factors
Protective Factors
Poverty
ESL
Low literacy skills
Adult educational and
vocational training
programs
Low wage jobs
Community Benefit
Program
Family Literacy Program
Uninsured
Health insurance
Para Su Salud Program
Food insecurity
WIC, food banks, job
training
Home visiting programs;
family literacy program
Overcrowded housing
Section 8 housing; low
income housing
Home visiting programs
Domestic violence
Healthy communication
Home visiting programs;
Anger management
Responsible Fatherhood
Program;
Healthy Marriage Program
“Building Healthy
Relationships” classes
through Health Ministry
Program
Behavioral Health Clinic
Child abuse and/or neglect
Prevention of child
abuse/neglect
Pico Union Family
Preservation Network
Early intervention services
for child/children
Home visiting programs
Responsible Fatherhood
Program
Healthy Marriage Program
Behavioral Health Clinic
Insufficient licensed
childcare
High quality licensed
childcare
Child Development Center
Early Childhood Center
Early Care and Education
Center at Mercy Housing
Family Childcare Network
Poor quality of schools
Early childhood education
Early Head Start
Universal pre-school
Family Literacy Program
After-school mentoring
program
School Readiness Program
Hope Street Youth Center
Central High Continuation
School
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
45
Risk Factors
Protective Factors
Community Benefit
Program
High rates of disabilities in
young children
Early intervention programs
Teen pregnancy
Access to prenatal care
Nurse Family Partnership
Home visiting program
LABBC’s Centering
Pregnancy Collaborative
Achieve healthy weight
prior to pregnancy
“Health Habits Before
Pregnancy” class through
Health Ministry Program
Obesity
Early Head Start
Licensed childcare centers
Exclusive breastfeeding for
first 6 months
Healthy lifestyle during
childhood, adolescence,
and adulthood
“Raising a Healthy Eater”
through Health Ministry
Program
Healthy Eating Lifestyle
Program
Food, Fitness, & Type 2
Diabetes Prevention
Program
Type 2 diabetes
Weight loss
Healthy lifestyle
Medical care
Periodontal care
Living with Diabetes
Program
Referral to local FQHC
Community Dental
Partnership
CDSMP
Smoking, alcohol, and/or
drug abuse
Smoking cessation
Alcohol/drug treatment
Freedom from Smoking
through Health Ministry
Program
Responsible Fatherhood
Program
Home visiting programs
Behavioral Health Clinic
Gang involvement
After-school program
Hope Street Youth Center
Healthy role models
Central Continuation High
School
Responsible Fatherhood
Program
Nurse Family Partnership
for first time young mothers
Youth ALIVE!’s Caught in
the Crossfire Program
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
46
Risk Factors
Poor birth outcome
Protective Factors
Preconceptual counseling
Interconception care
Depression
Community Benefit
Program
LABBC’s Best Babies
Collaborative – case
management
High quality prenatal care
LABBC’s Care Quality
Collaborative
Mental health services
Behavioral Health Clinic
It is now clear that the leading causes of morbidity and mortality in the United
States are related to health behaviors and lifestyle factors; these factors have
been called the “actual” causes of death. Insofar as abuse and other potentially
damaging childhood experiences contribute to the development of these risk
factors, then these childhood exposures should be recognized as the basic
causes of morbidity and mortality in adult life. The Adverse Childhood
Experiences (ACE) Study, based at Kaiser Permanente’s San Diego Health
Appraisal Clinic, was undertaken to describe the long-term impact of abuse and
household dysfunction during childhood on the following outcomes in adults:
disease risk factors and incidence, quality of life, health care utilization, and
mortality. The study population of over 17,000 HMO members was
predominantly white (77%), college educated (72%), and 50 or older (62%).
Adverse Childhood Experiences (during first 18 years of life) were defined as:
Abuse
o Psychological
o Physical
o Sexual
Household dysfunction
o Substance abuse
o Mental illness
o Parental separation or divorce
o Mother (or stepmother) treated violently
o Criminal behavior in household (household member went to
prison)
Adverse Childhood Experiences were common. More than half the members
experienced one ACE. 1 in 4 were exposed to 2 categories of ACEs; 1 in 16
were exposed to 4 categories. 22% were sexually abused as children. 66% of
the women experienced abuse, violence or family strife in childhood. Only a third
of members experienced no ACEs.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
47
Women
Men
Total
(N = 9,367)
(N = 7,970)
(N = 17,337)
Emotional Abuse
13.1
7.6
10.6
Physical Abuse
27.0
29.9
28.3
Sexual Abuse
24.7
16.0
20.7
Emotional Neglect1
16.7
12.4
14.8
9.2
10.7
9.9
Mother Treated Violently
13.7
11.5
12.7
Household Substance
Abuse
29.5
23.8
26.9
Household Mental Illness
23.3
14.8
19.4
Parental Separation or
Divorce
24.5
21.8
23.3
Incarcerated Household
Member
5.2
4.1
4.7
ACE Category*
Abuse
Neglect
Physical
Neglect1
Household
Dysfunction
The ACE Study (Am J Prev Med 1998;14:245-258) demonstrated a clear relationship
between childhood abuse and/or household dysfunction during childhood and multiple
risk factors for several leading causes of death in adults (smoking, severe obesity,
physical inactivity, depressed mood, suicide attempts, alcoholism, any drug abuse, a
high lifetime number of sexual partners). The higher the ACE score, the greater the
likelihood of: health risk behaviors (starting in adolescence), adult diseases, disabilities,
severe social problems, and severe mental health problems. For example:
A child with > 6 ACEs is 250% more likely to become an adult smoker.
A person with 4 ACEs is 260% more likely to have chronic obstructive
pulmonary disease (COPD)
A 500% increase in adult alcoholism is directly related to ACEs.
Two thirds of all alcoholism can be attributed to ACEs.
A male child with an ACE score of 6 has a 4,600% increase in the likelihood
that he will become an IV drug user later in life.
78% of drug injection by women can be attributed to ACEs.
Women with an ACE score of 4+ are 500% more likely to become victims of
domestic violence.
They are almost 900% more likely to become victims of rape.
There is a significant and graded relationship between a history of multiple
childhood traumas (ACEs) and hallucinations.
Compared to persons with 0 ACEs, those with 7 or more ACEs had a fivefold increase in the risk of reporting hallucinations.
Abuse and trauma suffered in the early years of development resulted in a
far greater likelihood of pre-psychotic and psychotic symptoms.
In an inpatient sample, 77% of those reporting contact sexual abuse (CSA)
or chronic physical abuse had one or more of the characteristic symptoms of
schizophrenia listed in the DSM-IV: hallucinations (50%); delusions (45%), or
thought disorder (27%).
Adults with an ACE score of 4 or more were 460% more likely to be suffering
from depression.
The likelihood of adult suicide attempts increased 30-fold, or 3,000% with an
ACE score of 7 or more.
Childhood and adolescent suicide attempts increased 51-fold or 5,100% with
an ACE score of 7 or more.
The ACE Study views health risk behaviors as attempts to cope with impacts of adverse
childhood experiences and ease the pain of prior trauma. It does not view them as
symptoms, bad habits, self-destructive behaviors, or public health problems. Similarly,
suicidality is not usually caused by “mental illness”, drugs, rejection by peer groups,
school pressure, failures, etc. Rather it is a coping device – a way to manage or escape
from the unbearable impacts of adverse childhood experiences and/or adult trauma.
Persons who experienced > 4 categories of childhood exposure, compared to those
who had experienced none, had 4- to 12-fold increased health risks for alcoholism, drug
abuse, depression, and suicide attempt; a 2- to 4-fold increase in smoking, poor selfrated health, > 50 sexual partners, and sexually transmitted disease; and a 1.4- to 1.6fold increase in physical inactivity and severe obesity. The number of categories of
ACEs showed a graded relationship to the presence of adult diseases including ischemic
heart disease, cancer, chronic lung disease, skeletal fractures, and liver disease. (see
figure below)
The ACE Study thus has profound public health implications. It is imperative to prevent
the occurrence of adverse childhood experiences. Research has demonstrated the longterm benefit of early home visitation on reducing the prevalence of ACEs. In fact the
U.S. Advisory Board on Child Abuse and Neglect recommends that a universal home
visitation program for new parents be developed. This is precisely what First 5 LA is in
the process of piloting through its Welcome, Baby! Program. Secondary prevention of
the effects of ACEs will first require increased recognition of their occurrence and
second, an effective understanding of the behavioral coping devices that commonly are
adopted to reduce the emotional impact of these experiences. This will require
significant improvements in the content and provision of adolescent health care which is
grievously inadequate in terms of psychosocial assessment and anticipatory guidance.
In the meantime, tertiary care of adults whose health problems are related to
experiences such as childhood trauma will continue to be a difficult challenge. The
relationship between childhood experiences and adult health status is likely to be
overlooked in medical practice because the time between exposure during childhood
and recognition of health problems in adult medical practice is lengthy. Moreover, these
childhood exposures include emotionally sensitive topics such as family alcoholism and
sexual abuse. Many physicians fear that discussions of sexual violence and other
sensitive issues are too personal even for the doctor-patient relationship. Furthermore,
many physicians lack to confidence and skills to inquire and respond to patients who
acknowledge these types of childhood exposures. Increased awareness of the
frequency and long-term consequences of adverse childhood experiences may also lead
to improvement in health promotion and disease prevention programs.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
49
Adverse Childhood
Experiences
Abuse of Child
Recurrent severe
emotional abuse
Recurrent physical abuse
Contact sexual abuse
Trauma in Child’s
Household Environment
Substance abuse
Parental separation or
divorce
Chronically depressed,
emotionally disturbed or
suicidal household
member
Mother treated violently
Imprisoned household
member
Loss of parent - best by
death unless suicideworst by abandonment
Neglect of Child
Abandonment
Child’s basic physical
and/or emotional needs
unmet
Impact of Trauma and
Health Risk Behaviors to
Ease the Pain
Neurobiologic Effects of
Trauma
Disrupted
neurodevelopment
Difficulty controlling
anger-rage
Hallucinations
Depression
Long-Term Consequences
of Unaddressed Trauma
(ACEs)
Disease and Disability
Ischemic heart disease
Cancer
Chronic lung disease
Chronic emphysema
Panic reactions
Anxiety
Asthma
Liver disease
Multiple (+6) somatic
problems
Skeletal fractures
Sleep problems
Impaired memory
Flashbacks
Poor self-rated health
Sexually transmitted
diseases
HIV/AIDS
Dissociation
Health Risk Behaviors
Smoking
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
Social Problems
Homelessness
Prostitution
50
Severe obesity
Physical inactivity
Suicide attempt
Alcoholism
Drug abuse
50+ sex partners
Repetition of original
trauma
Self injury
Eating disorders
Perpetrate interpersonal
violence
Delinquency, violence,
criminal behavior
Inability to sustain
employment
Re-victimization, rape, DV
Compromised ability to
parent
Intergenerational
transmission of abuse
Long-term use of health,
behavioral health,
correctional, and social
services
The Hope Street Family Center offers a seamless, flexible, comprehensive, culturallysensitive, and responsive array of services free of charge to meet a family’s individual
and changing needs for at least the first five years of a child’s life. One of the aims of
HSFC is to prevent children from experiencing adverse childhood experiences and to
enhance their resilience. HSFC’s Programs include the following:
Early Head Start Program
Child Development Center
Early Childhood Center
Early Care & Education Center
Family Childcare Network
Family Literacy Program
School Readiness Program
Responsible Fatherhood Program
Responsible Marriage Program
Hope Street Youth Center
Central High Continuation School
Nurse Family Partnership
Pico Union Family Preservation Network
California Behavioral Health Clinic
What is resilience? Resilience is the ability to thrive, mature, and increase competence
in the face of adverse circumstances; in other words, it’s the ability to face, overcome, be
strengthened by and even be transformed by adversity. Emmy Werner was one of the
first scientists to use the term resilience; her landmark longitudinal study followed a
cohort of children from Kauai, Hawaii (Development and Psychopathology 1993; 5: 50-3515) In this study, the risk group (~1/3 of the children) was defined by having four or
more early risk factors that included poverty, perinatal stress, family conflict, and low
parental education. Many of these children grew up with alcoholic or mentally ill parents.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
51
Two-thirds of these children exhibited destructive behaviors during adolescence, such as
substance abuse, teen pregnancy, and delinquency. However, one-third of these high
risk children developed well in terms of getting along with parents and peers, doing fine
in school, avoiding serious trouble, and having good mental health. Werner called the
latter group resilient. What made them different from the others? They had more
resources and fewer adversities from an early age. They had good parenting, more time
before the next child in the family came along, more appealing temperaments as babies,
better intellectual skills, more connections with prosocial adults, fewer separations from
caregivers, better physical health, etc. They also were more responsible, self-confident
and motivated to achieve. They took advantage of opportunities such as military service
or community education to shape their lives in positive ways.
Studies of resilient children and youth point to a small set of crucial protective factors for
healthy human development. The most important protective resource for development is
no surprise; it’s a strong relationship with a competent, caring, prosocial adult. The most
important individual quality is probably normal cognitive development, i.e., average or
better IQ scores, good attention skills, and “street smarts.” Research shows that
catastrophic stressors can threaten the integrity of a child’s ability to think and solve
problems, but if good parenting and good cognitive development are sustained, human
development is robust even in the face of adversity. The “short list” of human protective
factors include: connections to positive role models, feelings of self-worth and selfefficacy, feelings of hope and meaningfulness of life, attractiveness to others (in
personality and appearance), talents valued by self and others, faith and religious
affiliations, socioeconomic advantages, good schools, and other opportunities to learn or
quality for advancement in society. Resilient individuals are also able to seek out people
(mentors) and environments that are good for their development, a kind of “niche
seeking.”
The International Resilience Project identified 36 qualitative factors that contribute to
resilience. These can be divided into three major categories, each consisting of five
parts. The I HAVE factors are the external supports and resources that promote
resilience. Before the child is aware of who she is or what she can do, she needs
external supports and resources to develop the feelings of safety and security that lay
the foundation for developing resilience. The I AM factors are the child’s internal,
personal strengths. These are feelings, attitudes, and beliefs within the child. The I
CAN factors are the child’s social and interpersonal skills. Children learn these skills by
interacting with others and from those who teach them.
I HAVE…
Trusting relationships
Structure and rules at home
Role models
Encouragement to be
autonomous
Access to health, education,
welfare, and security services
I AM…
Lovable and my temperament
is appealing
Loving, empathetic, and
altruistic
Proud of myself
Autonomous and responsible
Filled with hope, faith, and
trust
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
I CAN…
Communicate
Problem solve
Manage my feelings and
impulses
Gauge the temperament of
myself and others
Seek trusting relationships
52
5.
CHMC has been a leader in perinatal services for over half a century. Therefore, it
seemed only natural to become the host agency for the Los Angeles Best
Babies Network (LABBN) Center for Healthy Births. The mission of the Center is to
provide the infrastructure, programs, advocacy and support to enhance capacity of the
network of community stakeholders working to achieve healthy births throughout Los
Angeles County. It envisions positive, productive networks supporting families and
communities to achieve healthy births.
The LABBC Center for Healthy Births:
Provides training and technical assistance for the seven Best Babies
Collaboratives (BBCs) that are partnerships funded to link, expand and enhance
services in communities with the worst birth outcomes. The BBCs aim to decrease
recurrent poor birth outcomes by providing interconception care for high-risk women.
Leads Care Quality Improvement activities to help providers implement evidencebased practice guidelines and to link health care providers to community-based
services and resources.
Supports and participates in the Healthy Birth Learning Collaboratives (HBLCs) in
each of the eight Service Planning Areas in the County. The HBLCs are networks of
perinatal stakeholders who voluntarily work together to improve pregnancy and birth
outcomes in their SPA. The Center provides administrative support, technical
assistance, training and other support for the HBLCs in order to increase community
and organizational capacity.
Coordinates and institutionalizes a broad perinatal health policy agenda, working
with community stakeholders and others required to build sustainable improvement
in pregnancy and birth outcomes
Builds the infrastructure necessary for the growth, integration and sustainability of
the Healthy Births Initiative. First 5 LA designated $15 million for its Healthy Births
Initiative to improve birth outcomes in Los Angeles County. The goals of the initiative
are to reduce low birthweight and very low birthweight babies and to reduce disease
and disability among newborns. This innovative approach, begun prior to birth, was
designed to optimize each child’s capacity for health, growth, development, and
learning throughout his/her lifespan
6.
Access to mental health care is a major problem in our service area, as delineated in
our Community Needs Assessment. The President’s New Freedom Commission on
Mental Health (2003) reported that ~ 50% of people in the U.S. who need mental health
treatment do not receive it. Furthermore, the mental health treatment rate among ethnic
minorities is lower than that for the general population. (U.S. Dept. of Health and Human
Services, 2001). In Los Angeles County, the needs of a large number of children and
adults with serious mental illness and emotional disturbances remain unmet (California
Mental Health Planning Council, 2003). Participants of focus groups conducted for our
Community Needs Assessment reported mental health disorders to be among the
primary health concerns facing their communities. The 2005 California Health Interview
Survey and the 2005 Los Angeles County Health Survey also show a substantial need in
mental health treatment and care among Los Angeles residents:
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
53
In Los Angeles County in 2005, 19% of respondents reported needing help for
emotional or mental health problems.
In Los Angeles County in 2005, rates of those who needed help for emotional or
mental health problems were especially high in SPA 5 (23.7%), SPA 6 (23.7%),
and SPA 4(20.6%).
In Los Angeles County in 2005, SPA 6 had the highest percentage of
respondents at risk for mental illness (9.2%).
Diagnosed with
Depression
SPA 4
SPA 6
SPA 8
LA
County
11.9%
12.2%
13.7%
12.9%
Mental Health Issues by SPA, 2005
At Risk for
Received MH Needed Help
Serious
Counseling
for Emotional/
Mental Illness
MH Problems
5.6%
7.8%
20.6%
9.2%
7.5%
21.8%
7.0%
5.3%
19.2%
5.2%
6.1%
18.9%
Treatment
Not Covered
by Insurance
21.8%
32.0%
21.1%
22.1%
Mental health experts identified a number of mental health conditions beyond depression
and anxiety as serious needs in the community. These conditions include past trauma
(post traumatic stress disorder), acculturation, marital difficulties, parenting problems,
domestic violence, stress, and poverty. They commented that often these conditions are
sub-clinical, meaning that they are not severe enough to qualify as a serious mental
illness. The L.A. County Department of Mental Health focuses on treating those with
serious mental illness and those patients are prioritized over sub-clinical patients. As a
result, adults with mental health problems go untreated because insurance plans
typically do not cover payment for the treatment of these conditions.
In FY05 CHMC underwrote the start-up of the California Behavioral Health
Clinic across the street from the hospital. This clinic provides the following
psychological services in English and Spanish to children, adolescents and their
families:
Individual, family, and group therapy
Assistance in accessing medical, educational, social, and financial resources
Community referrals to after-school programs
Coordination of treatment services
Medication evaluations by a child psychiatrist
Psychological assessments.
In order to qualify, the child must be Medi-Cal eligible. Services are funded
through EPSDT. In addition to providing culturally competent mental health
services, this clinic also serves as a training site for post-doctoral psychology
fellows who learn: how to integrate primary health care and mental health
services (at the USC Family Medicine Clinic), how to do developmental
assessments (through a collaboration with HSFC), and how to manage chronic
conditions.
In FY05 HSFC’s Early Head Start Program was selected by SAMHSA as a model
for innovative services for young children and families. HSFC successfully integrates
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
54
behavioral health into primary care for pregnant women and families with young
children.
7.
The Pico Union Family Preservation Network offers parenting classes as well as
anger management classes.
The Responsible Fatherhood Program offers the following mental health services:
Preparing for Successful Fathering, a 12 week parenting curriculum developed
by Dr. Ron Klinger, a practicing psychologist. Curriculum topics include: Fathers
as Role Models, Creating a Vision for Fathers, Bonding through Play
(incorporating children), Care-Giving Differences between Mothers and Fathers,
Discipline and Limit Setting, Game Plan for Success, and Preparing for Solo
Time with Kids.
Conflict Management classes, a series of 26 sessions that will address conflict
and anger issues in relationships.
Fathers’ Group, a support group co-facilitated by the Father Service Specialist
and a Father mentor
Brief, solution-focused individual, conjoint, and group counseling led by a
masters level clinician (Fathers Service Specialist) trained in conflict resolution
and family systems theory.
The Healthy Marriage Program provides one-day, skill-based workshops for
couples and/or single parents to support parents in developing and sustaining
healthy relationships in ways that help them be better parents and experience more
satisfying, long-lasting relationships, which will in turn have beneficial long-term
effects on their children’s development and future life choices. Peer-led support
groups reinforce material learned in workshops. Couples also have access to
couples counseling provided by social work interns.
The CHW Community Grants Program is another way that we increase access to
mental health services in our community. In fact, the American Hospital Association
commended our work in this area and recommended it as a Best Practice that other
hospitals with similar community needs could emulate. As you can see from the list
of last year’s grant awardees, 5 of the 7 grantees provided mental health services.
“Literacy skills predict an individual’s health status more strongly than age,
income, employment status, education level, and racial or ethnic group, according
to an analysis of the research by the nonprofit organization Partnership for Clear Health
Communication” (Wilson, 2003, pg. 875). Literacy skills can directly affects a patient’s
ability to follow physician instructions, take medication as prescribed, understand how to
prevent disease and, self-manage and understand their rights (Wilson, 2003; California
Healthline, 2004; Institute of Medicine, 2004)). Illiteracy affects patients’ ability to access
care, in particular because of difficulties completing application forms for insurance
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
55
coverage or reading an appointment card. Most significant of all, it increases the
chances of dying of chronic or communicable diseases.
A higher percentage of adults in Los Angeles County (27%) are estimated to be at the
lowest literacy proficiency level than for the state (19%) or the U.S. (20%). Moreover,
CHMC’s service area has the highest rate of low literacy (66%) in the County. The
greatest need for literacy services is for younger adults, particularly Latino and
Asian/Pacific Islander populations. Disability is also correlated with lower literacy
scores; CHMC’s service area has disability rates well above the County average of 9%with Downtown LA at 11% and South Los Angeles at 14%. Almost without exception,
the highest levels of Limited English Proficiency (LEP) are the lowest literacy areas in
the County. Every low-literacy area also had an above average proportion of recent
immigrants. Moreover, residents of the lowest literacy areas show low levels of
educational attainment. While the County average for education less than 9th grade is
14%, in the low literacy areas 24-40% of residents have less than a 9th grade education.
For decades, educators, researchers, and policy makers have puzzled over so-called
achievement gaps – the disparities in academic performance by race and ethnicity that
consistently show up on standardized tests, grade point averages, and a host of other
measures. A growing body of evidence suggests that any serious effort to eliminate
these disparities at the primary and secondary school levels must also address the
School Readiness Gap – the variations in academic performance and certain social
skills among children entering kindergarten and first grade. Recent studies document
specific dimensions of this gap:
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
56
On average, African American, Hispanic, and American Indian students demonstrate
significantly lower reading, math, and vocabulary skills at school entry than white and
Asian American children.
According to a 1995 study by Betty Hart and Todd Risley, 3-year-olds whose parents
are professionals have vocabularies that are 50% larger than those of children from
working-class families, and twice as large as children whose families receive welfare.
Using data from the U.S. Department of Education’s Early Childhood Longitudinal
Study, University of California researchers have shown that fewer than 20% of
California kindergartners from non-English speaking backgrounds score above the
50th percentile on reading and mathematics tests.
Many researchers today cite an analysis in the 1998 Brookings Institute book The BlackWhite Test Score Gap, in which it is estimated that about half of the black-white test
score gap at twelfth grade is attributable to gaps that exist at first grade. Researchers
have since made similar claims about gaps existing among other ethnic groups.
Moreover, most researchers agree that socioeconomic status – closely associated with
race and ethnicity- is one of the strongest predictor of low skills at school entry. In a
2002 study, Lee and Burkam found that at kindergarten entry, cognitive scores of
children in the highest socioeconomic group were 60% higher than those of the lowest
group. Thus improving all children’s access to high-quality prekindergarten programs
could do a great deal to narrow early learning disparities. Indeed, a 2004 study by
Magnuson, Waldfogel and Ruhm found preK participation to be associated with
significantly higher reading and math skills at school entry, narrowing gaps if not fully
closing them. They also found that these advantages were long-lasting for children from
low-income homes, many of whom were African American, Latino, or from immigrant
families. A 2006 study, which included children randomly assigned to either full day or
half-day preK programs, found that the children who had attended full-day preK
outperformed the others on literacy and math assessments and that these gains held
through at least the end of the first grade. Moreover, the full-day preK programs were
found to narrow skill gaps between children from upper- and lower-income homes.
It has also been recommended that preK education should be incorporated with the
early elementary grades as part of a preK-3 continuum model, which aligns both
academic and social development goals under a common structure for children in
preschool through grade 3. Such alignment is associated with less “fade out” of
children’s skills from year to year and fewer behavior problems as children move
between systems with different goals and structures. And finally, kindergarten teachers
may someday be required by statute to be certified in early childhood education, as they
currently are in Massachusetts, Mississippi, and Oklahoma. It has long been
recognized that kindergartners learn very differently from sixth graders.
Recognizing the challenges that many of our families face, CHMC offers a variety of
literacy programs.
HSFC’s Even Start Family Literacy Program, described in the Program Digest,
integrates early childhood, parenting, and adult education.
HSFC’s School Readiness Program, described in the Program Digest, serves 80
children, ages 0-5 years, and their families.
HSFC’s Family Childcare Network includes 13 child care providers who have
become licensed to provide quality childcare in their homes. HSFC helped these
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
57
providers start their own childcare businesses and continues to provide technical
assistance, support, training, and guidance for them, particularly on the topics of
language enhancement and the support of emerging literacy skills.
HSFC’s Youth Center offers educational support, academic enrichment, and
recreational opportunities to help school-aged youth reach their full potential.
Through the Youth Center, children are able to participate in an innovative literacy
program – Help One Student to Succeed (HOSTS) –that matches volunteer mentors
with students needing assistance in reading and language arts.
Central High School is a continuation high school classroom co-located at HSFC.
Established in partnership with LAUSD, Central High School provides a safe and
supportive environment for 25 students who have experienced difficulties in other
school settings. These students, many of whom are former dropouts or gang
members, boast an amazing 90% graduation rate!
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
58
Community Benefit Planning Process
Primary Prevention - Altering susceptibility or reducing exposure for susceptible
individuals
Health Promotion/Disease Prevention
Health Ministry Program
Healthy Eating Lifestyle Program
Type 2 Diabetes Prevention, Screening, and Intervention Program
Hope Street Family Center's Early Head Start Program
Community Dental Partnership
California Behavioral Health Clinic
Injury Prevention
Gang Prevention
Responsible Fatherhood Program
Hope Street Youth Center
Central High School
Nurse Family Partnership
California Behavioral Health Clinic
Youth ALIVE!’s Caught in the Crossfire
Pedestrian Safety
Health Ministry Program
Child Abuse and Neglect
HSFC Early Head Start
Nurse Family Partnership
Child Development Center
Early Childhood Center
Early Care and Education Center
Family Childcare Network
Pico Union Family Preservation Network
California Behavioral Health Clinic
Responsible Fatherhood Program
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
59
Healthy Marriage Program
Family Violence
Health Ministry Program
Responsible Fatherhood Program
Healthy Marriage Program
Secondary Prevention – Early detection and treatment of disease
Disease Management
Health Ministry Program
Healthy Eating Lifestyle Program
Type 2 Diabetes Prevention, Screening, and Intervention Program
Chronic Disease Self-Management Program
Healthcare Access
Health Insurance
Para Su Salud
Healthy Communities
Community Wide Measures
LABBC's Center for Healthy Births
HSFC's Family Literacy Program
HSFC's School Readiness Program
HSFC's Early Head Start Program
HSFC’s Responsible Fatherhood Program
HSFC’s Healthy Marriage Program
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
60
CHW Horizon 2010 System-Wide 5-Year Goal in Community Benefit
In April 2006 CHW announced the launch a new initiative entitled Horizon 2010. Residents of
communities with multiple socioeconomic barriers are more than twice as likely to be
hospitalized for ambulatory sensitive conditions (ASC), conditions that, if treated properly in an
outpatient setting, do not generally require acute care admissions. Appropriate prior
ambulatory care might prevent the onset of an illness, control an acute condition, or help to
manage a chronic disease. In response to this compelling information, which correlated with
CHW’s hospital utilization data, they developed this strategic initiative. The objectives of this
initiative are:
To expand and/or enhance services for persons with disproportionate unmet health
needs resulting in care delivery in settings most appropriate to meet their needs.
To ensure appropriate access to care for the poor and disenfranchised, which is
evidenced by a 5% reduction in hospital admissions for ambulatory sensitive conditions
over the next five years.
It is believed that by applying the science of community benefit, with a focus on disease
management programs in communities with greatest need, we have a unique opportunity to
reduce health disparities. The goal is to improve health status and quality of life in a sustainable
manner and reduce the demand for high cost medical care to treat preventable conditions.
CHW developed a report for each of its hospitals to help enhance or develop community health
initiatives that would help the hospital achieve the community benefit objectives outlined in
Horizon 2010. It is intended that programs will focus on the areas where fulfillment of the
mission imperative to serve and advocate for our brothers and sisters who are poor and
disenfranchised can be best realized. CHMC was charged with developing an intervention
strategy which will be implemented in FY07 and the objectives achieved by 2010.
UTILIZATION FOR INPATIENT AMBULATORY SENSITIVE CONDITIONS AT CALIFORNIA HOSPITAL MEDICAL CENTER
This utilization data reflects all inpatient admissions that included an ASC DRG diagnosis.
DRG
ASC Description
Cases Net Margin (Loss)*
127
Heart Failure and Shock
366
(244,144)
79/80
Respiratory Infection
82
(234,493)
143
Chest Pain
231
(102,186)
88
Chronic Obstructive Pulmonary disease
133
(74,079)
294/295
Diabetes
165
(54,504)
140
Angina Pectoris
35
(29,320)
179
Inflammatory Bowel Disease
11
(12,266)
All other ASC
233
42,963
Total
1256
(708,029)
Payer Group
Net Margin (Loss)*
Medicaid/MediCal
(1,189,048)
Commercial
3,870
Self-Pay/Charity Care/Bad Debt
20,318
Other
139,640
Medicare
317,191
Total
(708,029)
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
61
Heart disease, chest pain, diabetes and chronic obstructive pulmonary disease are the
top ASCs at CHMC. Prevention programs that manage the incidence of these conditions may
improve the health status and quality of life for individuals and lower hospital admissions and
expenses. Measures to prevent or manage diabetes, a known contributor to the other diseases,
are of great importance, particularly in this service area where community demographics
indicate a high risk for, and incidence of, this disease among Hispanic/Latino residents.
Because of the decreased responsiveness of the immune system during older adulthood, a
common cold may become complicated by bronchitis and pneumonia before it runs its course.
For this reason, and the greater susceptibility of older adults to lower respiratory tract infections
in particular, it is advisable for all individuals who are 65 or older to be immunized with
pneumococcal vaccine once and with influenza vaccine every year.
On October 3, 2007 CHW hospitals received another memorandum re Horizon 2010: The Next
Generation of Excellent Care. As noted in this memo, “as we move toward fulfillment of the
initiatives identified in Horizon 2010, a long-term improvement program (LTIP) goal has been
established to bring even greater focus to our direction.
CHW LTIP Goal FY 08-FY10
Our Objective: Reduce health disparities by addressing key ambulatory care sensitive
conditions among populations with disproportionate unmet health-related need.
Our Goal: Demonstrate a 5% decrease in readmissions of participants in the hospital’s
preventive health intervention for one of the following ACSC:
Asthma: Decrease emergency department readmissions among children or adult
participants in the preventive health intervention.
Diabetes: Decrease uncontrolled diabetes readmission rates of participants in the
preventive health intervention.
Congestive Heart Failure: Decrease readmissions of CHF participants in preventive
health intervention.
Or for a
Facility-specific identified health need: not addressed in the previous four (e.g., public
inebriates, mental health conditions, obesity, oral health, etc.) , with the outcome goal
established in collaboration with system office staff and approved by CHW executive
management.
Threshold =
Target =
Maximum =
75% of CHW hospitals achieve the quantifiable targets for a preventive health
intervention.
80% of CHW hospitals achieve the quantifiable targets for a preventive health
intervention.
90% of CHW hospitals achieve the quantifiable targets for a preventive health
intervention.
Intervention Strategy:
1. Identify a health issue in a neighborhood with disproportionate unmet health-related
need, as indicated by the CNI, community needs assessment, and hospital specific data
related to ambulatory care sensitive conditions.
2. Plan and develop, or enhance an existing, preventive health program, using evidencebased intervention strategies to address the identified disproportionate unmet health-
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
62
related need, focusing on the uninsured, and populations covered by MediCal,
Medicare/MediCal or other government-funded insurance programs for the indigent.
3. Continuously define a focus population from hospital utilization, physician referral or
community-referral for the preventive health intervention.
4. Using enrolled participants’ prior year’s hospitalization history and/or current health
status as a baseline, demonstrate a decrease in utilization by program participants as a
result of the preventive health intervention.
Participants may or may not utilize your facility’s services. This population-based
approach to an intervention is required in order to qualify the program as a
community benefit.
Ask the participants for their past utilization history at the time of enrollment and
then again 6-months post-intervention.
5. Submission of your plans and quarterly reporting expectations
On or before January 11, 2008 report what health issue you have identified and
the evidence-based program you are or will be using. Also report the current
status of the health intervention program, e.g., in place, in need of enhancement
to be evidence based, or start up.
Report the ongoing progress of your interventions quarterly on the CIBSA online
reporting program beginning on January 11, 2008 for existing program.
If the health intervention program is in need of enhancement or is a start up
program, it is expected that the process of enhancement or implementation will
be completed on or before April 11, 2008 and outcomes will be tracked on a
quarterly basis throughout FY2009.
In FY2010 we will continue to track outcomes on a quarterly basis with the new
participant population.
The final report will be cumulative, demonstrating the outcomes for all groups
participating in the health intervention program by year.
CHMC’s Horizon 2010 Intervention Strategy (’07-’10)
CHMC will address the root causes of the top ASCs in our service area. The primary root
cause of type 2 diabetes is obesity. Type 2 diabetes and hypertension are major contributors to
heart disease. Smoking is the primary cause of chronic obstructive pulmonary disease.
Obesity
The latest results from the 2005 Los Angeles County Health Survey (LACHS) show that the
prevalence of adult obesity in the county continues to increase, with 1 out of 5 adults in the
county now obese.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
63
Prevalence of Obesity Among Adults in
Los Angeles County
25
20
15
%
10
5
0
1997
1999
2002
2005
The prevalence of obesity rose among all racial/ethnic groups except Asians/Pacific Islanders,
and in 2005 was highest among Latinos and African Americans. The prevalence of obesity
increased the fastest among men, Latinos, and young adults (18-29 years old). Adults living in
lower income households were more likely to be obese.
Trends in the Prevalence of Obesity Among Adults in Los Angeles County, 1997-2005
1997 (%)
1999 (%)
2002 (%)
2005 (%)
Los Angeles Co.
14.3
16.7
19.3
20.9
Gender
Male
13.5
15.0
19.8
21.8
Female
15.2
18.5
18.7
20.0
Race/Ethnicity
Latino
17.1
19.7
24.3
28.7
White
12.3
15.3
16.3
16.6
African-American
22.2
24.2
30.5
27.7
Asian/PI
4.0
7.2
6.2
6.0
Age Group
18-29
9.4
9.6
13.9
18.1
20-49
14.8
18.6
21.1
21.4
50-64
21.5
21.9
24.8
25.9
65+
13.1
16.0
16.0
16.6
Federal Poverty
Level
0-99% FPL
20.3
19.3
26.5
28.2
100-199% FPL
17.6
20.8
21.8
23.9
200% or above FPL
11.5
14.5
15.8
17.4
Moreover, the prevalence of obesity increased in almost all SPAs. The next graph highlights
trends in the prevalence of obesity in CHMC’s three SPAs.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
64
Trends in Prevalence of Obesity
Among Adults in Los Angeles County
35
30
% Obese
25
Metro
20
South
15
South Bay
10
5
0
1997
1999
2002
2005
Obesity increases a person’s risk of developing many other chronic conditions and of dying
prematurely. In fact, obesity is the second leading cause of preventable death in the United
States today. Obese individuals have a 50-100% increased risk of premature death from all
causes compared to individuals with a healthy weight. Adults who are obese are significantly
more likely to have type 2 diabetes, coronary artery disease, hypertension, stroke, dyslipidemia,
gallbladder disease, osteoarthritis, sleep apnea and respiratory problems such as asthma, and
endometrial, breast, prostate, and colon cancers. Obese individuals also suffer from social
stigmatization and discrimination and depression
Women who are obese have higher rates of amenorrhea and infertility and when pregnant, have
an increased risk of pregnancy and delivery complications. Maternal obesity affects pregnancy
outcome primarily through increased rates of chronic hypertension and preeclampsia, diabetes
(pregestational and gestational), cesarean section and infections. Maternal obesity is associated
with a higher rate of cesarean deliveries and a higher incidence of anesthetic and postoperative
complications in these deliveries. Moreover, maternal obesity threatens the child’s health from
the fetal period through adulthood. Complications associated with maternal obesity are fetal
macrosomia, shoulder dystocia, small for gestational age, late fetal death, and congenital
anomalies such as neural tube defects, abdominal wall defects, and heart defects. Large for
gestational age or macrosomic neonates are at increased risk of subsequent childhood obesity
and its associated morbidity. Therefore, experts now strongly recommend that women achieve
an optimal weight and adopt a healthy diet before becoming pregnant.
Lifespan Approach to Obesity Prevention
Preconception Child
Adolescent
Mother
Achieve
Breastfeed for 6healthy weight 12 mo.
Child/adult
Healthy diet; minimize intake of
sweetened beverages and fast
food; < 2 hr screen-time/day;
>1 hr physical activity/day
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
20s
30+
Maintain healthy weight by eating healthy
diet and at least 30 minutes of moderate
physical activity 5 days/wk
65
Physical
environment
Food security
School food policies & physical education
Neighborhood safety to allow physical activity
Workplace food policies, offerings
Workplace promotion of physical activity
Social
environment
Learn stress
management
Weight reduction support networks
Address domestic violence
AMCHP/CityMatCH Women’s Health Partnership Action Learning Collaborative on
Healthy Weight
In 2005 the Association of Maternal and Child Health Programs (AMCHP) and CityMatCH
formed a Women’s Health Partnership to build state and local capacity to promote safe
motherhood and enhance women’s health before, during, and after pregnancy. The
maintenance of healthy weight among women of childbearing age was chosen as their first
focus area. In September 2006 Los Angeles was selected as one of seven counties to
participate in the Partnership’s Healthy Weight Action Learning Collaborative (ALC). The
purpose of the ALC is to bring together multi-disciplinary teams to strengthen partnerships,
implement evidence-based strategies, build community participation and overcome challenges
to help women of reproductive age achieve healthy weight before, during, and after pregnancy.
The primary strategies of the ALC are:
Up to four fact-to-face National Meetings over a two year time period
Regular conference calls and web-based seminars focused on key issues, training
needs, sharing related experiences and resolving common issues (no more than 8/year)
Materials provided that assist participating teams in promoting healthy weight in women
of reproductive age
Mechanisms for participating teams to get assistance from other teams and national
experts.
The Los Angeles Team consists of the following individuals:
Cynthia Harding, MPH (Leader)
Director, MCAH, Los Angeles County Public Health
Suzanne Haydu, MCH, RD
Public Health Nutrition Consultant, MCAH, Office of
Family Planning, California Dept. of Health Services
Margaret L. Yonekura, M.D.
Director of Community Benefits, CHMC
Michael Fassett, M.D.
Director, Maternal-Fetal Medicine, Kaiser West LA
Ellen Eidem, MS
Director, Office of Women’s Health, LA County Public
Health
Eloisa Gonzales, MD, MPH
Director, Physical Activity Program, LA County Public
Health
Sylvia Drew Ivie
Consultant, The California Endowment
Sharon Anthony, RD, MFCC
Senior Nutritionist, PHFE-WIC
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
66
Nicole D. Vick, MPH, CHES
Diana Ramos, MD, MPH
Lauren Frank, MPH
Jean Tremaine, MA, MPH
Antronette Yancey, MD, MPH
Carolina Reyes, MD
Julia Heinzerling
Health Educator, SPA 5/6, LA County Public Health
Director, MCAH Programs, LA County Public Health
Research Analyst, MCAH, LA County Public Health
Director, Nutrition Program, LA County Public Health
Assoc. Professor, UCLA School of Public Health
Executive Director, LA Best Babies Network
Chief, Community Health Services, South LA Best
Babies Collaborative
Kiko Malin, MPH, MSW
State Director of Program Services, March of Dimes
CHMC is represented by the two individuals whose names are bolded.
The first National meeting of all the ALC teams took place in Atlanta, GA on December 4 and 5,
2006. A subsequent meeting took place in June 2007 in Salt Lake City and the final meeting
took place in Alexandria, VA in February 2008.
Extent and duration of breastfeeding have been found to be inversely associated with risk of
obesity later in childhood. Von Kries (BMJ 1999; 319:147-150) found a 57% reduction in the
adjusted odds of being overweight at 5 or 6 years of age when contrasting those who were
breastfed for at least 12 months with those who were never breastfed. Liese et al (Int J Obes
2001; 25:1644-1650) found even strong effects contrasting > 1 year of breastfeeding with those
who were not breastfed, a 71% reduction in odds. However, according to the literature, the
protective effects of breastfeeding are gained only when exclusive breastfeeding continues for
at least 3 months.
CHMC is involved in the promotion of breastfeeding in a variety of ways:
Los Angeles Best Babies Network’s Prenatal Care Quality Collaborative selected
Early Breastfeeding Education as one of its process measures. A comprehensive
breastfeeding assessment must be documented on the prenatal record within the first
four weeks of prenatal care. Then documentation of breastfeeding education, guidance,
and encouragement must be documented at least every trimester for which the patient
received care.
CHMC is a member of the Breastfeeding Task Force of Greater Los Angeles and is
listed in their Breastfeeding Resource Directory. CHMC staff provides lactation consults
in the hospital and telephone support after discharge.
In March 2007, CHMC formed a Task Force, chaired by Dr. Yonekura, to move toward
becoming certified as a Baby Friendly Hospital. We plan to provide 16 hrs of
breastfeeding education to our nursing staff, ban the use of “formula marketing bags”,
change our policies and procedures on Labor & Delivery, Couplet Care, and NICU to
support the initiation and maintenance of breastfeeding, and work closely with our local
WIC providers and newborn and postpartum mother health care providers.
In June, 2008, CHMC was selected as one of four hospitals in Los Angeles County to
receive a grant from the State for Birth and Beyond California: Breastfeeding
Training and Quality Improvement Program. The BBC project seeks to improve
breastfeeding rates in the hospital setting by training a variety of healthcare workers
(including physicians, nurses, lactation educators and consultants, among others) to
support a mother’s choice to breastfeed and through continuous quality improvement
efforts. The 16-hour Learner Workshop is a component of the training arm of the BBC
project. The goal of this workshop is to provide healthcare workers the tools to:
1. Enhance parent-infant attachment
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
67
2. Engender newborn breastfeeding competence; and
3. Increase patient satisfaction with no increase in staff workload.
The project aims to accomplish this goal through the following Learner Workshop
objectives:
1. Contribute to creating an environment for maternal-infant care based on best
practice guidelines as defined in the Providing Breastfeeding Support: Model
Hospital Policy Recommendations;
2. Demonstrate the skills necessary to organize care to maximize mother and infant
skin-to-skin contact and bonding;
3. Identify biologic, nutritional and immunologic properties of breastfeeding and the
risks of artificial milk; and
4. Recognize and discuss solutions to alleviate common barriers in supporting a
mother’s choice to exclusively breastfeed.
In October 2008 20 CHMC perinatal nurses and lactation educators together with the
future CHMC trainers received the 16-hour Learner Workshop. In January 2009, the
trainers will receive train-the-trainers workshops. It is then anticipated that CHMC
trainers will train the rest of the perinatal staff beginning in the Spring of 2009.
Participants of the Hope Street Family Center’s Early Head Start Program or NurseFamily Partnership Program are strongly encouraged to breastfeed.
“The remarkable and unexpected rise in obesity among our children and youth in a relatively
short time span is one of the 21st century’s most critical public health challenges. We really
need to reduce the overall weight of our country.”
-Jeffrey Koplan, M.D., MPH
Vice President for Academic Health Affairs at Emory University
Former Director of U.S. Centers for Disease Control and Prevention
The prevalence of obesity (defined as an age- and sex-specific body mass index at or above
the 95th percentile) among very young children is also on the rise. Although there are fewer
nationally representative data presently available on children in this age group, a
comparison of the NHANES I, II, and III survey results reveals that younger children are
becoming more obese, with the most dramatic increases occurring among older (4- to 5year old) preschoolers.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
68
Trends in Age-Adjusted Percentage of
Obesity Among U.S. Boys
% Overweight
8
7
6
5
4
3
2
1
0
6-11 12-23
mo
mo
NHANES I
NHANES II
NHANES III
2-3 yr 4-5 yr
Trends in Age-Adjusted
Percentage of Obesity Among
U.S. Girls
% Overweight
12
10
8
6
4
2
0
6-11 12-23 2-3 yr 4-5 yr
mo
mo
NHANES I
'71-74
NHANES II
76-80
NHANES III
88-94
In addition, data from the most recent NHANES (1999-2000) survey reveal that among
infants from birth through 23 months, 11.4% were obese (weight for length > 95th percentile).
While there were no significant differences in prevalence between younger boys and girls,
there were significant differences between racial/ethnic groups. About 10% of non-Hispanic
whites were at or above the 95th percentile, compared with 18.5% of non-Hispanic blacks
and 13.7% of Mexican Americans.
For young children, if one parent is obese the odds ratio is ~3 for obesity in adulthood, but if
both parents are obese, the odds ratio increases to more than 10. Before 3 years of age,
parental obesity is a stronger predictor of obesity in adulthood than the child’s weight status.
Such observations have important implications for recognition of risk and routine anticipatory
guidance that is directed toward healthy eating and activity patterns in families of young
children.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
69
The Health Ministry Program offers a class focused on optimal nutrition and physical
activity for children ages birth-five years entitled Raising a Healthy Eater. Classes are
offered at a variety of venues including Healthy Start sites, other elementary schools, Head
Start sites, child care sites, and other community gathering places.
“This generation that is growing up now may have a shorter life expectancy than the
generation before it. The consequences of overweight and obesity are felt in many areas.”
-Philip Nader, M.D.
Professor Emeritus of Pediatrics, University of California, San Diego
During the past three decades, the prevalence of obesity (defined as an age- and sexspecific body mass index at or above the 95th percentile) among children in the United
States more than tripled among youngsters aged 6-11 years, and more than doubled among
adolescents aged 12-19 years. A recent study from the National Institute of Child Health
and Human Development found that children who are obese in early childhood tend to be
obese as teens. Researchers followed 1000 children born in 1991 from ages 2 to 12,
periodically measuring the children’s height and weight. The study showed children who
were obese during their elementary school years were 25 times more likely to be obese at
age 12 than were children who were not obese during their time in elementary school.
Trends in Obesity for U.S. Children
20
18
16
14
12
%
10
Overweight
8
6
4
2
0
6-23 mo
2-5 yr
6-11 yr
12-19 yr
1971- 1976- 1988- 1999- 2001- 200374
80
94
2000
2
4
These figures are particularly alarming because of the health problems associated with
obesity. Children and adolescents who are obese are more likely to have risk factors for
cardiovascular disease (such as increased blood pressure and cholesterol), type 2 diabetes,
asthma, sleep apnea, and orthopedic problems. Moreover, obese girls are more likely to
have early puberty. In addition, obese youth are likely to suffer significant psychosocial
morbidity including low self-esteem, poor body image, social discrimination, and depression.
Tragically, children and adolescents who are obese are more likely to remain so as adults.
Among obese adolescents, an estimated 75% will be obese as young adults. This
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
70
increases to over 80% if one or more parent is overweight or obese. Thus, there is an
urgent need to intervene prior to puberty if we are to turn back this epidemic!
Healthy Eating Lifestyle Program is a free, community-based, family focused pediatric
obesity prevention program for children at risk for overweight (defined as a BMI for age and
gender from the 85th to the 95th percentile) aged 5-12 years and their families. This program
is funded by the UniHealth Foundation for 3 years (1/1/04-12/31/06)-we received a 6 month
no-cost extension of this grant and will seek additional grant funding to continue this highly
successful program. The program goals are: 1) to adapt approaches that have been shown
to work in clinical settings for implementation in communities: 2) to help families with
overweight children ages 5-12 years adopt healthier lifestyles; and 3) to document the effect
of the intervention on clinical and self-reported outcomes. Each of the six two-hour
workshops is highly interactive so that program participants are able to both learn and apply
the facts, principles, and concepts being taught. An Olympic Food Guide was developed as
a tool to help participants make healthier food choices. Workshops are offered at a variety
of sites in the community. CHMC partnered with Red Shield Youth and Community Center, a
full service after-school recreation center in the heart of Pico Union. Classes are offered two
to three days a week. Participating children and their adult partners attend five consecutive
weekly workshops; the sixth workshop is given three to six months after the fifth workshop.
Classes are taught in English and Spanish by two bilingual community health promoters.
Adolescence is another critical period for the development of obesity. The normal tendency
during early puberty for insulin resistance may be a natural cofactor for excessive weight
gain as well as various co morbidities of obesity. Early menarche is clearly associated with
degree of overweight, with a twofold increase in rate of early menarche associated with BMI
greater than the 85th percentile. The risk of obesity persisting into adulthood is higher
among obese adolescents than among younger children. The roles of leptin, adiponectin,
ghrelin, fat mass, and puberty on development of adolescent obesity are being actively
investigated. Data suggest that adolescents who engage in high risk behaviors, such as
smoking, ethanol use, and early sexual experimentation also may be at greater risk of poor
dietary and exercise habits.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
71
CHMC and other members of the Chronic Disease Consortium will seek grant funding to
modify HELP for adolescents at risk for overweight or already overweight. Overweight
adolescents with serious medical problems will continue to be referred to Childrens Hospital
Los Angeles’ Kids ‘N Fitness Program.
“A new generation is entering adulthood with unprecedented levels of obesity. This, in
addition to the existing burden of adult obesity, reinforces the concern that weight-related
chronic diseases will be the most significant public health concern throughout the 21st
century.”
-International Diabetes Federation
The National Institutes of Health and the World Health Organization adopted similar body
weight (adjusted for height) guidelines for overweight and obesity. The body mass index
(BMI = weight in kg/height in m2) continues to be the most commonly used index of weight
status.
Classification of Overweight and Obesity by BMI
Obesity Class
Underweight
Normal
Overweight
Obesity
Extreme obesity
I
II
III
BMI
<18.5
18.5-24.9
25.0-29.9
30.0-34.9
35.0-39.9
> 40
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
72
Although BMI is not a measure of body composition, it is commonly considered an index of
fatness because of the high correlation between BMI and percentage of body fat in children
and adults.
Age-Adjusted Prevalence of Overweight and
Obesity Among U.S. Adults, Ages 20-74 yr
70
60
50
%
40
30
Overweight
20
Obese
10
0
197680
198894
1999- 2001-2 2003-4
2000
Overweight and obese individuals are at increased risk for many diseases and health
conditions, including the following:
Hypertension (high blood pressure)
Osteoarthritis (a degeneration of cartilage and its underlying bone within a joint)
Dyslipidemia (for example, high total cholesterol or high levels of triglycerides)
Type 2 diabetes
Coronary heart disease
Stroke
Gastrointestinal problems including gastroesophageal reflux disease (GERD), nonalcoholic fatty liver, gall stones, diverticulitis, and hernias
Sleep apnea and asthma
Genitourinary problems including urinary stress incontinence, obesity-related
glomerulopathy, hypogonadism (men), polycystic ovarian syndrome (PCOS), irregular
menstrual cycles and infertility
Some cancers (endometrial, postmenopausal breast, colon, prostate, kidney and gall
bladder)
Excess abdominal or visceral adipose tissue (VAT) is recognized as an important risk factor
in the development of coronary heart disease and type 2 diabetes. The most accurate
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
73
measurement of VAT requires imaging techniques (MRI and CT), that are impractical in a
clinical setting. However, VAT can be estimated by measuring waist circumference at the
level of the iliac crest in a plane parallel to the floor at the end of a normal expiration.
Classification of Overweight and Obesity and Associated Disease Risk*
BMI
Obesity Class
Disease Risk*
Waist circ < 35
inches for
women and 40
inches for men
Underweight
<18.5
----Normal
18.5-24.9
----Overweight
25.0-29.9
Increased
Obesity
30.0-34.9
I
High
35.0-39.9
II
Very high
Extreme obesity
> 40
III
Extremely high
*Risk for type 2 diabetes, hypertension, and cardiovascular disease
Waist circ > 35
inches for
women or 40
inches for men
--------High
Very high
Very high
Extremely high
Type 2 Diabetes Mellitus
CHMC has selected diabetes as the ambulatory care sensitive condition that we will
focus on for our CHW LTIP FY08-FY10. Therefore, our CHW LTIP Goal is to decrease
by 5% readmission rates for uncontrolled diabetes among participants in our Living
with Diabetes Program.
Obesity is one of the principal risk factors for type 2 diabetes. Type 2 diabetes, formerly
called adult-onset or noninsulin-dependent diabetes, is the most common form of diabetes.
People can develop type 2 diabetes an any age, even during childhood. This form of
diabetes usually begins with insulin resistance, a condition in which fat, muscle and liver
cells do not use insulin properly. At first, the pancreas keeps up with the added demand
producing more insulin. In time, however, it loses the ability to secrete enough insulin in
response to meals. As a result, the amount of glucose in the blood increases while the cells
are starved for energy. Over the years, high blood glucose damages nerves and blood
vessels, leading to complications such as heart disease, stroke, blindness, kidney damage,
nerve problems, gum infections, and amputation. Being overweight and inactive increases
the chances of developing type 2 diabetes.
A recent report on L.A. Health Trends (August 2007) documented a steady rise in the rate of
diabetes among adults 18 years and older, from 6.6% in 1997 to 7.5% in 1999, 7.6% in
2002-3, and 8.6% in 2005. This increasing prevalence “likely reflects the impact of
sedentary lifestyles and the obesity epidemic.” The Los Angeles County Health Survey
(LACHS) identified large disparities in diabetes by race/ethnicity, income, and educational
level.
Diabetes rates among Latinos and African Americans were nearly double the
rates among Whites and Asian/Pacific Islanders.
Nearly one in five adults 65 years and older have been diagnosed with diabetes
according to the 2005 LACHS.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
74
From 1997 to 2005, the rate of diabetes increased most rapidly among those
living in poverty and was more than two times higher in this group than among
those with incomes at or above 200% of Federal Poverty Level (FPL).
In 2005, the prevalence of diabetes among adults who did not graduate from
high school (14%) was more than two times higher than the prevalence among
adults who graduated from college (6%).
Trends in Prevalence of Diabetes Among Adults, 1997-2005
1997 (%)
1999 (%)
2002-3 (%)
L.A. County
6.6
7.5
7.6
Gender
Male
6.7
7.7
7.7
Female
6.6
7.4
7.6
Race/Ethnicity
Latino
9.5
11.3
11.4
White
4.6
5.5
5.4
African Amer.
10.1
9.5
9.4
Asian/PI
5.9
5.6
5.1
Age Group
18-29
0.8
1.7
0.9
30-39
2.8
2.9
2.1
40-49
5.1
6.1
6.0
50-64
11.6
11.8
13.4
65 or over
14.3
16.8
17.8
FPL
0-99% FPL
9.0
11.1
12.7
100-199% FPL
9.0
9.2
9.1
200% or above
5.3
6.1
5.8
SPA
1
6.7
6.6
7.1
2
5.7
6.3
6.5
3
7.0
7.2
6.8
4 Metro
6.9
7.8
7.8
5
5.3
6.1
4.3
6 South
11.5
9.5
11.2
7
5.7
9.3
10.1
8 South Bay
6.0
7.1
8.2
2005 (%)
8.6
8.8
8.4
12.3
5.6
12.0
7.1
1.3
3.3
7.0
15.2
18.3
14.0
10.2
6.5
9.0
6.3
7.3
11.4
4.7
14.5
10.5
8.3
Among adults, clear evidence exists that surprisingly modest weight reductions can
markedly reduce the development of type 2 diabetes, if not prevent it completely, in
susceptible individuals and that weight loss can reverse the type 2 diabetic state. The
remarkable effect of weight loss through diet and increased activity has been demonstrated
in the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Diabetes
Prevention Program to benefit particularly the over-60s, in whom nearly three-quarters of
new cases of diabetes were prevented. This and other studies provide hope to those with
impaired glucose tolerance and a susceptibility to diabetes. Dietary and activity changes to
produce a 5-7% weight loss can successfully reduce the incidence of type 2 diabetes;
reductions in fat and calorie intake accompanied by half an hour’s extra walking or other
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
75
exercise a day 5 days a week have been demonstrated to lower the incidence by 58%.
Great success has been achieved among people over 60 years, reducing the development
of diabetes in that high-risk age group by 71%.
The Chronic Disease Consortium, consisting of CHMC, Good Samaritan Hospital, and
Huntington Memorial Hospital, received a three year grant from the Good Hope Medical
Foundation (6/1/05-5/31/08) for the Type 2 Diabetes Prevention, Screening, and
Intervention Program. This program consists of three main activities, all of which are
offered in English and Spanish:
Outreach education and Screening using the ADA Risk Test at variety of
sites in the community
Prevention Program for those at high risk for type 2 diabetes: 4 weekly
workshops promoting weight loss if overweight or obese through healthy
eating and increased physical activity to prevent or delay the onset of
diabetes
Classes are held at a variety of schools, churches, and other community
venues.
Intervention Program for those with type 2 diabetes
-Living with Diabetes: 5 weekly workshops designed to help patients
understand what diabetes is, strategies and benefits of good control,
importance of blood glucose monitoring, nutrition, lifestyle behaviors,
mental health, identifying and avoiding complications, and preventive
care.
-Chronic Disease Self-Management Program: 6 weekly workshops about
living a healthy life with chronic conditions such as diabetes.
Classes began in 2006. (Please see Program Digest)
Cardiovascular diseases (CVD) remain the leading cause of death and disability in diabetic
patients. Nearly 80% of all deaths and most hospitalizations in diabetic patients are
attributable to cardiovascular causes. Among elderly, diabetic patients, about 40% of all
preventable hospitalizations are due to congestive heart failure. Similarly, coronary heart
disease (CHD) accounts for as many as 44% and 33% of the deaths in diabetic white and
black men, respectively. Although remarkable advances have been made in the
management of acute myocardial infarction, the case fatality in diabetics exceeds twice the
rate in nondiabetics. Diabetic patients who have not had previous myocardial infarction have
as high a risk of subsequent myocardial infarction as nondiabetic patients who have had a
previous myocardial infarction; this led to the designation of diabetes as a “coronary
equivalent”. More recently, pooled data from nine prospective epidemiologic studies in the
United States suggest that diabetes also may be a cardiovascular risk equivalent for fatal
stroke in women.
An important contributor to the increased risk of cardiovascular complications is the
clustering of atherogenic risk factors, including dyslipidemia, hyperinsulinemia, and
hyperglycemia, that is seen commonly in diabetic and prediabetic persons and their adverse
impact on the endothelium, vascular smooth muscle cell, and platelet function. In addition,
overweight and obesity, which are powerful predictors of type 2 diabetes and key
components of the metabolic syndrome, also predispose to CHD and other CVDs. Together,
overweight, obesity, other components of the metabolic syndrome, and diabetes play major
roles in the development of cardiovascular morbidity and mortality.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
76
Coexistence of three or more of the following criteria makes a diagnosis of the metabolic
syndrome according to the Adult Treatment Panel (ATP) III criteria:
Abdominal obesity: waist circumference at least 102 cm in men and at least
88 cm in women
Hypertriglyceridemia: at least 150 mg/dL
Low high-density lipoprotein cholesterol: up to 40 mg/dL in men and up to 50
mg/dL in women
High blood pressure: at least 130/85 mm Hg
High fasting glucose: at least 110 mg/dL
The key to the prevention and control of the metabolic syndrome is multi-factorial application
of behavioral change, therapeutic lifestyle interventions, and pharmacologic treatment in
eligible subjects. Increased physical activity, weight loss, a prudent diet that is rich in fruits
and vegetables but low in saturated fat and increased intake of food with a low glycemic
index are recommended. The use of statins, fibrates, angiotensin-converting enzyme
inhibitors, and other antihypertensive drugs for the control of dyslipidemia and hypertension
are supported by the established impact on coronary risk reduction. In eligible patients, the
use of these drugs is guided ideally by the level of their global risk assessment. The
thiazolidinediones have important, demonstrable beneficial effects on several components of
the metabolic syndrome and have also been shown to be useful in preventive strategies for
the syndrome.
Heart Disease
Most cardiovascular disease is preventable. The AHA Guidelines for Primary Prevention of
Cardiovascular Disease and Stroke: 2002 Update: Consensus Panel Guide to
Comprehensive Risk Reduction for Adult Patients Without Coronary or Other Atherosclerotic
Vascular Diseases (Circulation 2002;106:388-391) emphasize that the cornerstone of
primary prevention is the adoption of healthy life habits: avoidance of tobacco including
secondhand smoke, healthy dietary patterns, weight control and regular, appropriate
exercise.
Guide to Primary Prevention of CVD and Stroke: Risk Assessment
Risk Assessment
Recommendations
Risk factor screening
Risk factor assessment should begin at age 20
Goal: Adults should know the levels and
yr. Family history of CHD should be regularly
significance of risk factors as routinely
updated. Smoking status, diet, alcohol intake,
assessed by their primary care provider
and physical activity should be assessed at
every routine evaluation. Blood pressure,
BMI, waist circumference, and pulse (to
screen for atrial fibrillation) should be recorded
at each visit (at least every 2 yr). Fasting
serum lipoprotein profile (or total and HDL
cholesterol if fasting not available) and fasting
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
77
Global risk estimation
All adults > 40 yr of age should know their
absolute risk of developing CHD. Goal: as low
risk as possible.
blood glucose should be measured according
to patient’s risk for hyperlipidemia and
diabetes, respectively (at least every 5 yr; if
risk factors are present, every 2 yr).
Every 5 yr (or more frequently if risk factors
change) adults, especially those > 40 yr of age
or those with > 2 risk factors, should have their
10 yr risk of CHD assessed with a multiple risk
score. Risk factors used in global risk
assessment include age, sex, smoking status,
systole (and sometimes diastolic) blood
pressure, total ( and sometimes LDL)
cholesterol, HDL cholesterol and in some risk
scores, diabetes. Persons with diabetes or 10
yr risk > 20% can be considered at a level of
risk similar to a patient with established
cardiovascular disease (CHD risk equivalent).
Equations for calculation of 10 year stroke risk
are also available.
The Guidelines for Primary Prevention of Cardiovascular Disease and Stroke provide
detailed Risk Intervention Recommendations. The Risk Intervention and Goals are briefly
summarized below.
Risk Intervention
Goals
Smoking
Complete cessation. No exposure to
environmental tobacco smoke
BP control
< 140/90 mm Hg; < 130/85 mm Hg if renal
insufficiency or heart failure is present; or <
130/80 mm Hg if diabetes is present.
Dietary intake
An overall healthy eating pattern. Match
energy intake with energy needs and make
appropriate changes to achieve weight loss
when indicated.
Aspirin
Low-dose aspirin in persons at higher CHD
risk (especially those with 10-y risk of CHD >
10%)
Blood lipid management
Primary goal: LDL-C < 160 mg/dL if < 1 risk
factor present; LDL-C < 130 mg/dL if > 2 risk
factors present and 10 y CHD risk is < 20%; or
LDL-C < 100 mg/dL if > 2 risk factors present
and 10-y CHD risk is > 20% or if patient is
diabetic.
Secondary goals (if LDL-C is at goal range): if
triglycerides are > 200 mg/dL, then use nonHDL-C as a secondary goal: non-HDL-C < 190
mg/dL if < 1 risk factor; non-HDL-C < 160
mg/dL for > 2 risk factors and 10-y CHD risk <
20%; non-HDL-C < 130 mg/dL for diabetics or
for > 2 risk factors and 10-y CHD risk > 20%.
Other targets for therapy: triglycerides >150
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
78
Physical activity
Weight management
Diabetes management
Chronic atrial fibrillation
mg/dL; HDL-C < 40 mg/dL in men and < 50
mg/dL in women.
At least 30 min of moderate-intensity physical
activity on most (preferably all) days of the
week.
Achieve and maintain desirable weight (BMI
18.5-24.9). When BMI is > 25, waist
circumference at iliac crest level < 40 inches in
men and < 35 inches in women.
Normal fasting plasma glucose (<110 mg/dL)
and near normal HbA1c (<7%)
Normal sinus rhythm or, if chronic atrial
fibrillation present, anticoagulation with INR
2.0-3.0 (target 2.5).
The challenge for healthcare professionals is to engage greater numbers of patients, at an
earlier stage of their disease, in comprehensive risk reduction with the use of interventions
that are designed to circumvent or alleviate barriers to participation and adherence, so that
many more individuals may realize the benefits that primary prevention can provide.
The Cardiovascular Health Promotion/Cardiovascular Disease Prevention Program
which will be entitled the Heart HELP Program was planned thanks to a planning grant from
the Good Hope Medical Foundation.. We are now actively seeking grant funding to
implement this program. It is anticipated that program activities will include:
Outreach Education and Screening for risk factors: family history of
premature CHD (definite MI or sudden death before 55 y in father or male
first-degree relative or before 65 y in mother or female first-degree relative),
current cigarette smoking, hypertension, abnormal lipid panel, diabetes,
obesity, sedentary lifestyle, age > 45 if male and > 55 if female
o Screening is already on-going at our Health Ministry sites
o Health education class on “HTN and High Cholesterol” is already
being offered.
o Tobacco cessation workshops are also being offered.
The Heart HELP Program will consist of five 2-hour consecutive weekly
workshops on the following topics:
o Meet Your Heart, Good Nutrition, and Weight Management
o Heart Healthy Meals
o Reading Food Labels for a Healthy Heart
o Eating Out, Managing Stress, & Long Term Change
o HELP to Understand and Manage Heart Failure
Secondary prevention of cardiovascular disease involving aggressive risk factor
management clearly improves patient survival, reduces recurrent events and the need
for interventional procedures and improves quality of life for these patients. AHA/ACC
Guidelines for Preventing Heart Attack and Death in Patients with Atherosclerotic
Cardiovascular Disease: 2001 Update (Circulation 2001;104:1577-1579) detail secondary
prevention management. A brief summary of Goals are listed below.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
79
AHA/ACC Secondary Prevention for Patients With Coronary and Other Vascular Disease
Goals
Smoking
Complete cessation
BP control
<140/90 mm Hg or < 130/85 mm Hg if heart failure or renal
insufficiency; < 130/80 mm Hg if diabetes
Lipid management
LDL< 100 mg/dL
Lipid management
Secondary goal: if TG>200 mg/dL, then non-HDL should be <
130 mg/dL
Physical activity
Minimum goal: 30 minutes 3-4 days/wk; optimal goal: daily
Weight management
BMI 18.5-24.9
Diabetes management
HbA1c < 7%
Antiplatelet
Start and continue indefinitely aspirin 75-325 mg/d if not
agents/anticoagulants
contraindicated. Consider clopidogrel 75 mg/d or warfarin if
aspirin contraindicated.
ACE inhibitors
Treat all patients indefinitely post MI.
Β-blockers
Start in all post-MI and acute ischemic syndrome patients.
Continue indefinitely.
Ideally we would like CHMC to implement AHA’s Get with the Guidelines, a hospital-based
quality improvement program designed to close the treatment gap in cardiovascular disease.
The program provides physicians and healthcare providers with materials, education, and tools
based on AHA/ACC Secondary Prevention guidelines on cardiovascular disease. Utilizing
discharge protocols in the hospital setting will help ensure that cardiovascular disease patients
are placed on appropriate medications, informed of recommended behavioral modifications, and
improve the rate of intervention with CVD patients both in-hospital and post-discharge to reduce
the incidence of CVD events. A key component of this continuous quality improvement program
is to monitor progress through the web-based Patient Management Tool (PMT).
Implementation of this program would ensure that patients would have continuity of care from
their acute care hospitalization, discharge planning, and return to the community where they
would receive continued reinforcement of their discharge plan instructions.
As with our Type 2 Diabetes Prevention, Screening, and Intervention Program, we would also
encourage patients with cardiovascular disease to attend the Chronic Disease Self
Management Program workshops.
The clinical syndrome of heart failure is the final pathway for myriad disease that affect the
heart. The symptoms of heart failure – fatigue, shortness of breath, and congestion/edema –
are related to the inadequate perfusion of tissue during exertion and often to the retention of
fluid. The primary cause is an impairment of the heart’s ability to fill or empty the left ventricle
properly. Nearly 5 million Americans have heart failure today, with an incidence approaching
10/1000 population among persons older than 65 years of age. Heart failure is the reason for at
least 20% of all hospital admissions among persons older than 65. Over the past decade, the
rate of hospitalizations for heart failure has increased by 159%. Moreover, 8% of elderly patients
require readmission for heart failure within 6 months of the initial hospitalization. Studies have
demonstrated that more than half of these readmissions are preventable. Poor compliance is
an important contributing factor in many patients requiring readmission. In one series, lack of
adherence to the prescribed medical program (drugs and/or diet) was the most common reason
for readmission, occurring in 41% of the cases.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
80
Although heart failure is a major public health problem, there are no national screening efforts to
detect the disease in its earlier stages. Heart failure is largely preventable, primarily through the
control of blood pressure and other vascular risk factors. Yet, until recently, the factors that
render a patient at high risk for heart failure had not been clearly defined or publicized. The
guidelines for the evaluation and management of chronic heart failure that were published
recently by the American College of Cardiology and the American Heart Association have
corrected this deficit. (J. Am. Coll. Cardiol 2005;46:1-82) The new approach to the
classification of heart failure emphasizes its evolution and progression and defines four stages
of heart failure.
Stage A
High risk for heart failure, without structural heart disease or symptoms
Stage B
Structural abnormality of the heart but asymptomatic
Stage C
Structural abnormality of the heart and current/previous symptoms of HF
Stage D
End-stage symptoms of HF that are refractory to standard treatment
This staged classification underscores the fact that established risk factors and structural
abnormalities are necessary for the development of heart failure, recognizes its progressive
nature, and superimposes treatment strategies on the fundamentals of preventive efforts. The
classification is a departure from the traditional New York Heart Association (NYHA)
classification, which has primarily been used a shorthand to describe functional limitations.
Heart failure may progress from stage A to stage D in a given patient but cannot follow the path
in reverse.
The treatment of heart failure involves counteracting two related but largely independent
processes. Left ventricular dysfunction, regardless of cause (coronary artery disease,
cardiomyopathy, hypertension, or valvular disease), develops through ventricular remodeling
that results in a dilated chamber with a low ejection fraction, leading to episodes of arrhythmia,
progressive pump failure, and premature death. Noncardiac factors (neurohormonal
stimulation, endothelial dysfunction, vasoconstriction, and renal sodium retention) may or may
not be stimulated by left ventricular dysfunction, but ultimately contribute to the same
progressive process of cardiac remodeling; the noncardiac factors independently cause the
dyspnea, fatigue, and edema that are characteristic of the clinical syndrome of congestive heart
failure. (N Engl J Med 1999; 341:577-85)
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
81
Left ventricular remodeling is the process by which mechanical, neurohormonal, and possibly
genetic factors alter ventricular size, shape and function. Remodeling occurs in several clinical
conditions, including myocardial infarction, cardiomyopathy, hypertension, and valvular heart
disease; its hallmarks include hypertrophy, loss of myocytes, and increased interstitial fibrosis.
For example, after a myocardial infarction, left ventricular remodeling usually begins within the
first few hours and progresses over time. The entire heart may be involved in disproportionate
thinning and dilation in the infarct region (i.e., infarct expansion) is accompanied by a distortion
in shape of the entire heart with volume-overload hypertrophy of noninfarcted myocardium.
Patients with no or limited dilation at four weeks tend to remain stable, while those with
progressive dilation over this period tend to deteriorate over time with loss of function in initially
normally contracted myocardium.
The magnitude of the remodeling changes is roughly related to infarct size. Progressive
remodeling is always deleterious and associated with a poor prognosis. As the heart undergoes
remodeling, it becomes less elliptical and more spherical, which deleteriously affects its function
as a pump. There are also changes in ventricular mass, composition, and volume, all of which
may adversely affect cardiac function. In patients with progressive postinfarction dilation, the
end-systolic volume index increases progressively and the LV ejection fraction (LVEF) declines
due in part to loss of function in initially normally contracting myocardium. These changes are
important predictors of mortality.
Another potential deleterious outcome of remodeling is the development of mitral
regurgitation. The presence of mitral regurgitation results in an increasing volume overload on
the already overburdened left ventricle that further contributes to remodeling, the progression of
disease, and symptoms.
Supraventricular arrhythmias, particularly atrial fibrillation, are often the precipitating events that
herald the onset of either systolic or diastolic heart failure. Recognition of atrial fibrillation is
critical in order to prevent stroke by initiation of oral anticoagulant therapy. Abnormal
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
82
myocardial conduction can also lead to delays in ventricular conduction and bundle branch
block. Left bundle branch block is a significant predictor of sudden death and a common finding
in patients with heart failure. The rate of sudden cardiac death among persons with heart failure
is 6-9 times that seen in the general population. Increasing use of implantable cardiovertdefibrillators has unequivocally reduced mortality in a subgroup of patients with heart failure.
Control of risk factors in Stage A (e.g., hypertension, coronary artery disease, and diabetes
mellitus) has a favorable effect on the incidence of later cardiovascular events. Results from
trials have shown that the effective treatment of hypertension decreases the occurrence of left
ventricular hypertrophy and cardiovascular mortality, as well as reducing the incidence of heart
failure by 30-50%. ACE- inhibitor treatment of asymptomatic high-risk patients with diabetes or
vascular disease and no history of heart failure has also yielded reductions in the rates of death,
myocardial infarction, and stroke. In short, the goal of treatment in stage A is to prevent
remodeling.
The goals of therapy for patients with heart failure and a low ejection fraction are to improve
survival, slow the progression of disease, alleviate symptoms, and minimize risk factors.
Modification of lifestyle can be helpful in controlling the symptoms of heart failure. For example,
basic habits of moderate sodium restriction, weight monitoring, and adherence to medication
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
83
schedules may aid in avoiding fluid retention or alerting the patient to its presence. Moderation
of alcohol intake is advised; avoidance of NSAIDS is also important. NSAIDS have been
associated with an increase in the incidence of new heart failure, decompensated chronic heart
failure, and hospitalizations for heart failure. For selected patients, regularly schedule exercise
program may have beneficial effects on symptoms. ACE inhibitors are recommended for many
patients with stage A heart failure and all patients with stage B, C, or D heart failure.
Beta-blockers have long been used for the treatment of hypertension, angina, and arrhythmias
and for prophylaxis in patients who have had a myocardial infarction. This class of medication
has had a remarkable effect on chronic heart failure. The primary action of beta-blockers is to
counteract the harmful effects of the sympathetic nervous system that are activated during heart
failure. They improve survival, morbidity, ejection fraction, remodeling, quality of life, the rate of
hospitalization, and the incidence of sudden death. Beta-blockers should be used in all patients
in stable condition without substantial fluid retention and without recent exacerbations of heart
failure requiring inotropic therapy.
CHMC’s Heart Failure Education and Counseling Program is currently in the planning stage.
This program will likely include the following components:
Use of Cardiovascular Hospital Atherosclerosis Management Program (CHAMP) as a
model for initiation of secondary preventative measures before hospital discharge. (Am J
Cardiol 2000; 85:10A-17A). This program included the initiation of aspirin, beta-blockers,
statins, exercise, smoking cessation, and dietary counseling. The scope of the program
was enhanced by the dissemination of treatment guidelines and algorithms to hospital
staff, educational lectures, preprinted admission orders, patient education materials, and
periodic reports on treatment use.
Alternatively, we could use the Organized Program to Initiate Life-Saving Treatment in
Hospitalized Patients with Heart Failure (OPTIMIZE-HF), a program designed to improve
the medical care and education of patients who are hospitalized for HF and to accelerate
the initiation of evidence-based, guideline-recommended HF therapies by starting these
lifesaving therapies before hospital discharge. (Am Heart J 2004; 148:43-51)
OPTIMIZE-HF is a hospital-based process of care improvement program and a Webbased registry that provides physicians an opportunity to benchmark their use of
treatment against regional and national use. The program uses established treatment
algorithms, care maps, standing orders, and educational initiatives to encourage its
adoption by providers. The registry tracks data on HF conditions, medications at
admission and discharge, rehospitalizations and deaths, discharge status and
instructions, and stresses compliance with instructions to advance the understanding of
the best approaches to initiate optimal HF management.
Before discharge, all HF patients will be educated about heart failure, including advice
on daily weights, dietary restrictions including sodium and fluid, and signs and symptoms
of a heart failure decompensation. Patients will be advised to report these changes in
weight and symptoms to their physician. Patients who do not have a primary care
physician will be assisted in obtaining an appointment within a week of discharge.
Patients with HF will also be recruited from local FQHCs and community clinics with no
formalized HF education program.
Upon Program enrollment, baseline information including relevant demographics,
medical history, and current medications will be collected, and questionnaires measuring
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
84
knowledge and self-care behavior will be administered. A blood sample for -natriuretic
peptide (BNP) will be drawn to measure HF severity; BNP levels will be measured using
the Triage test device (Biosite Diagnositcs Inc.), a CLIA waived test that takes < 15
minutes.
Each patient will receive a copy of Learning to Live with Heart Failure: A Self-Care
Handbook (Channing Bete Co.) in either English or Spanish.
The patient will receive one-on-one education and counseling by a nurse using a
portable, standardized, high-impact, colored flip chart either at the clinic or patient’s
home. The information imparted will include the causes and mechanisms of heart
failure, signs and symptoms of HF, the importance of daily weights (emphasizing the
differences in fluid vs fat weight), and the importance of seeking help promptly if
symptoms worsen. Patients will be advised to call their health care provider if a weight
gain of 3 lb in 1 day or 5 lb in 1 week occurs. In addition, potential barriers to seeking
care will be addressed and discussed with the patient. ( Am Heart J 2005; 150:983.e7983.e12) The educator will record the patient’s current medications in the Handbook and
make sure that the patient understands when and how often to take each medication.
The educator will also show the patient where to chart his/her daily weight in the
Handbook. The Handbook also has a food diary and an activity log.
Patients will be strongly encouraged to participate in CDSMP workshops.
Patients will be recontacted by a community health promoter at 2wk, 4 wk, and monthly
thereafter for at least 1 year. The purpose of these contacts will be to reinforce the
content of the education program, as well as to determine if symptoms had worsened
and whether they had sought medical attention. A follow-up questionnaire and
assessment of self-care behaviors (using an abbreviated form of the European Heart
Failure Self-Care Behavior Scale [Eur J Heart Fail 2003; 5:363-70]) will be administered
at 3 month intervals along with an assessment of HF severity using BNP.
Depending on the number of participants, we may hold support group sessions for HF
patients, co-facilitated by a social worker and the nurse.
As with all of our programs, we will seek grant funding for this Program. Dr. Faye Lee,
cardiologist on staff at CHMC, has volunteered to be a consultant for this project.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
85
Chronic Obstructive Pulmonary Disease
Trends in Current Smoking by High School Seniors and Adults, United States, 1965–
2004
In 2005 an estimated 45.1 million adults in the United States were current cigarette smokers,
the same percentage as in 2004, even though this single behavior will result in death or
disability for half of all continuing smokers. Tobacco use is the leading preventable cause of
death in the United States, resulting in approximately 440,000 deaths each year. More than 8.6
million people in the United States have at least one serious illness caused by smoking.
Smoking rates remain high among men (23.9% vs. women, 18.1%) and American
Indians/Alaska Natives (32%), followed by non-Hispanic whites (21.9%) and non-Hispanic
blacks (21.5%). Smoking prevalence was also highest among those who had earned a GED
diploma (43.2%) and those with 9-11 years of school (32.6%) and those living below vs above
(29.9% vs 20.6%) the poverty level.
If current patterns of smoking persist, an estimated 5 million people currently younger than age
18 will die prematurely of a tobacco-related disease. Coupled with this enormous health toll is
the significant economic burden of tobacco use: more than $75 billion per year in medical
expenditures and another $92 billion per year resulting from lost productivity.
Since 1964, 28 Surgeon General’s reports on smoking and health have concluded that tobacco
use is the single most avoidable cause of disease, disability, and death in the United States.
Over the past 4 decades, cigarette smoking has caused an estimated 12 million deaths,
including 4.1 million deaths from cancer, 5.5 million deaths from cardiovascular diseases, 2.1
million deaths from respiratory diseases, and 94,000 infant deaths related to mothers smoking
during pregnancy. Smokeless tobacco, cigars, and pipes also have deadly consequences,
including lung, larynx, esophageal, and oral cancers. Low-tar cigarettes and other tobacco
products are not safe alternatives.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
86
The harmful effects of smoking do not end with the smoker. Babies of women who smoke
during pregnancy are more likely to have lower birth weights, an increased risk of death from
sudden infant death syndrome, and respiratory distress. In addition, secondhand smoke also
has harmful effects on nonsmokers. Each year, primarily because of exposure to secondhand
smoke, an estimated 3,000 nonsmoking Americans die of lung cancer, and more than 35,000
die of heart disease. Each year, an estimated 150,000–300,000 children younger than 18
months of age have lower respiratory tract infections because of exposure to secondhand
smoke.
Although smoking rates fell among youth from 2000 to 2003, recent surveys indicate that the
rate of decline may have stalled among both middle school and high school students. This lack
of progress suggests the need for greater use of proven anti-smoking strategies and for new
strategies to promote further declines in youth smoking.
About 438,000 U.S. Deaths Attributable Each Year to Cigarette Smoking
The Health Ministry Program began offering a health education class on the health effects of
smoking and exposure to secondhand smoke. People will be encouraged not to start smoking
or to stop smoking. Freedom from Smoking ® is the American Lung Association’s revamped
and upgraded smoking cessation program; it is available free online, as a group clinic, through
Lung HelpLine (1-800-LUNG-USA) or via a Self Help book (www.lungusa.org and click the FFS
logo). We recently started offering this program through our Health Ministry Program. At least
one “Freedom from Smoking Series of Workshops” will be offered each quarter.
Chronic Obstructive Pulmonary Disease (COPD) is a preventable and treatable disease state
characterized by airflow limitation that is not fully reversible and is usually progressive.
Although airflow limitation is associated with an abnormal inflammatory response of the lungs to
noxious particles, the impact of COPD is not restricted to the lungs; significant systemic
consequences are also produced. Lung function impairment, characterized by expiratory flow
limitation leading to air trapping, or hyperinflation, is worsened by periodic exacerbations.
Together, lung function impairment and disease exacerbations promotes a cycle of decline that
includes dyspnea, reduced exercise endurance, physical inactivity, and deconditioning, leading
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
87
to disease progression, and consequently to disability, poor health-related quality of life and
premature death.
COPD is the fourth leading cause of death in the United States, and it is the only common
cause of death that is increasing in incidence. The leading cause of COPD is smoking.
Between 15% and 20% of long-term smokers will develop COPD. This strongly suggests that
genetic factors may determine in which smokers airflow limitation will develop. Further evidence
that genetic factors are important comes from the familial clustering of patients with early-onset
COPD and from the differences in the prevalence of COPD among different racial groups. More
recently the literature also indicates that 15-20% of all cases of COPD are work-related, i.e.,
caused by occupational exposures. Specific settings and agents have been implicated or
confirmed. Coal miners, hard-rock miners, tunnel workers, concrete-manufacturing workers,
and nonmining industrial workers have been shown to be at highest risk for developing COPD.
Agents associated with work-related COPD include:
Minerals: coal, human-made vitreous fibers, oil mist, Portland cement, silica, silicates
Metals: osmium, vanadium, welding fumes
Organic dusts: cotton, grain, wood
Moreover, smoking and occupational exposure to dusts, gases, and/or fumes have greater than
additive effects. Hnizdo and coworkers from the National Institute for Occupational Safety and
Health used data collected in the US population-based Third National Health and Nutrition
Examination Survey on more than 9800 subjects to estimate the population-attributable risk
(PAR) for COPD attributable to work. (Am J Epidemiol 2002; 156:738-746) The analysis was
adjusted for multiple factors, including smoking history. The industries with increased risk
included rubber, plastics, and leather manufacturing; utilities; building services; textile
manufacturing; the armed forces; and food products manufacturing; chemical, petroleum, and
coal manufacturing; and construction. The PAR for COPD attributable to work was estimated at
19% overall and 31% among never smokers. Other studies have confirmed that occupational
exposure to dust, fumes, and gases increases mortality due to COPD especially among
nonsmokers. In another US study, the PAR for COPD attributable to work was 20%. In this
study the PAR for combined current and former smoking was 56%. Smoking and occupational
exposures to dusts, gases, and/or fumes had greater than additive effects.
Most patients with COPD have three pathologic conditions: chronic obstructive bronchitis,
emphysema (enlargement of air spaces and destruction of lung parenchyma, loss of lung
elasticity) and mucus plugging of small airways, but the relative extent of emphysema and
obstructive bronchitis within individual patients can vary. The following figure demonstrates the
mechanism of airflow limitation in COPD. In the peripheral airways of patients with COPD, as
compared with normal peripheral airways, there is airflow limitation due to a variable mixture of
loss of alveolar attachments, inflammatory obstruction of the airway, and luminal obstruction
with mucus.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
88
The primary physiological abnormality in COPD is an accelerated decline in the forced
expiratory volume in one second (FEV1) from the normal rate in adults over 30 years of age of
approximately 30 ml per year to nearly 60 ml per year. As shown in the following figure, the
disease course begins with an asymptomatic phase in which lung function deteriorates without
associated symptoms. The onset of the subsequent symptomatic phase is variable but often
does not occur until the FEV1 has fallen to ~50% of the predicted normal value.
Hyperinflation (over-expanded lungs), which occurs at rest and worsens with exercise, is an
additional physiologic abnormality commonly seen in patients with moderate-to-severe COPD. It
is manifested by an increase in the functional residual capacity, which places the muscles of
respiration at a mechanical disadvantage, thereby increasing the work of breathing and
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
89
reducing exercise tolerance. This is manifested by nasal flaring during air intake and the lips
may be pursed (the shape lips make when you whistle) while exhaling. Additional abnormalities
include hypoxemia (low levels of oxygen in arterial blood) and high levels of carbon dioxide.
Better methods are needed for early detection of COPD to identify patients who may benefit
from early intervention. Because the majority of cases occur in patients who have smoked, all
current or former smokers should be considered at increased risk for COPD. (N Engl J Med
2004;350:2689-97) Another approach used by the Department of Veterans Affairs hospitals is to
perform screening spirometry in patients > 50 years of age who are smokers. This approach
resulted in the detection of a greater number of patients with asymptomatic COPD. In some
cases, patients are identified as asymptomatic because they have already given up activities to
avoid or limit exertion. It is therefore important to question patients with newly diagnosed
COPD about their activity levels so that signs of avoidance or reduction of activity can be
identified and acted on before the cycle of deconditioning advances too far. Maintenance
therapy should be instituted at an early stage, before symptoms restrict activity levels.
Guidelines from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) state that the
airflow limitation in COPD is characterized by an FEV1 <80% of the predicted normal value and
and FEV1:FVC ratio <70%. Staging guidelines differ somewhat with regard to setting thresholds
for mild, moderate, and severe disease.
The stage of the disease suggests the prognosis and follow-up data from longitudinal studies
indicate that moderate and severe stages of the disease are associated with higher mortality.
However, in the largely asymptomatic group of patients that GOLD categorizes as “stage 0, at
risk”, only 18.5% of the patients progressed to more severe airflow limitation at 15 years.
COPD management must focus on 5 major areas (see algorithm below):
Earlier diagnosis of the disease
Risk reduction through smoking cessation, decreased exposure to inhaled irritants, and
immunization against respiratory pathogens (Pneumococcal vaccine once and influenza
vaccine yearly)
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
90
Treatment with pharmacotherapy and pulmonary rehabilitation to improve patients’ daily
and long-term functioning
Decrease in complications by reducing the number of exacerbations and improving
pulmonary function with drug therapy
Improvement of health-related quality of life (HRQOL).
GOLD Guidelines --- COPD Severity
0: At Risk
I: Mild
II: Moderate
III: Severe
IV: Very severe
Exposure to risk
factors
FEV1/FVC <
70%
FEV1/FVC <
70%
FEV1/FVC <
70%
FEV1/FVC < 70%
Normal
spirometry
FEV1 ≥ 80%
50% ≤ FEV1 <
80%
30% ≤ FEV1 <
50%
FEV1 < 30% or presence of chronic
respiratory failure or right heart
failure
Avoidance of risk factor(s): influenza vaccination
Add short-acting bronchodilator when needed
Add regular treatment with one or more long-acting bronchodilators
Add inhaled glucocorticosteroids if repeated
exacerbations
Add long-term oxygen if chronic
respiratory failure, consider
surgical treatments
FEV1=forced expiratory volume in 1 second; FVC=forced vital capacity
As shown in the landmark study by Fletcher and Peto of London transit workers, lung function
evaluated by FEV1 declines naturally with aging; however, in susceptible smokers the rate of
decline is greatly accelerated. (BMJ 1977;1:16454-1648) It is well recognized that baseline
FEV1 is predictive of mortality in patients with COPD. The prognostic significance of FEV1 was
particularly evident at baseline values <30% of predicted. Smoking cessation changes the
clinical course of COPD by preserving lung function. The earlier the age of smoking cessation,
the greater the lung function that is preserved. For example, compared with a patient who quits
smoking at the age of 65 years, a patient who quit at the age of 45 prevents additional loss of
lung function that would occur over the next 20 years, thereby reducing the risk that FEV1 will
decline below the thresholds for disability. (Am J Med2006;119:S46-S53)
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
91
In the Lung Health Study, smoking cessation resulted in a significant impact on FEV1 even in
patients with mild COPD, with lung function very close to normal. (Am J Respir Crit Care Med
2002;166:675-679) Over an 11 year follow-up, the rate of FEV1 decline among continuing
smokers was more than twice the rate of decline among those who were sustained quitters.
This benefit of smoking cessation was evident in both men and women. In addition, FEV1 fell to
<60% of predicted after 11 years in more continuing smokers than sustained quitters (38% vs.
10%, respectively).
In a recent analysis from this study conducted at 14.5 years, patient randomly assigned to the
smoking cessation intervention had a significant 18% reduction in all-cause mortality compared
with usual care (no smoking cessation intervention). (Ann Intern Med 2005;142:233-239) When
the cause of death was considered in the Lung Health Study, patients allocated to the smoking
cessation intervention had lower rates of death due to coronary heart disease, cardiovascular
disease, lung cancer, and respiratory disease other than lung cancer compared with those
assigned to usual care. Sustained smokers had significantly lower death rates for CHD,
cardiovascular disease and lung cancer compared with the other group (continuing smokers
and intermittent quitters).
Appropriate strategies to reduce occupational exposures to respiratory tract irritants, in order of
decreasing efficacy, include elimination (e.g., substitute alternate materials), engineering
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
92
controls (e.g.,exhaust ventilation or process enclosure), administrative controls (e.g., transfer to
another job or change in work practices), and personal protective equipment (e.g., masks or
respirators). (J Occup Environ Med 2005;47:154-160) The effective use of personal protective
equipment, however, requires that the appropriate equipment be selected, properly fit-tested,
maintained, and worn when there is potential for exposure.
Prevention must be the primary tool for decreasing the incidence of morbidity and disability from
work-related COPD. Prevention must involve cooperation between employers, workers, and
their representatives, regulators, and medical personnel. The goal of primary prevention is to
prevent occupational exposure. Primary prevention strategies involve the same hierarchy of
exposure controls. Secondary prevention detects COPD early so that its duration and severity
can be minimized. Tertiary prevention applies to individuals who have already been diagnosed
with work-related COPD. It includes the institution of appropriate health care and an effort to
prevent permanent disease by early removal from, or reduction of, exposure.
Another important component in the prevention of irritant-induced COPD is surveillance for
these diseases in the workplace. Surveillance programs are a type of secondary prevention in
that their principal goal is the early detection of disease. Any diagnosis of irritant-induced
COPD must be considered a sentinel event; other exposed workers are at risk and need to be
identified promptly. For medical surveillance of COPD, short symptom questionnaires can be
administered annually that include items such as improvement in respiratory symptoms on
weekends and holidays. In addition, spirometry can be performed on an annual basis and
compared to baseline spirometric testing at the time of hire. Review of peak expiratory flow rate
records over several weeks can also detect workers at risk for developing irritant-induced
COPD. Industrial hygienists can perform environmental monitoring to ensure that appropriate
engineering controls are in place to protect worker safety. Reviewing and updating lists of
agents used at a given workplace should be performed on a periodic basis, to identify possible
respiratory tract irritants.
CHMC’s COPD Prevention, Detection, and Intervention Program is currently in the planning
stage. This program will likely include the following components:
Outreach to schools and churches to prevent initiation of smoking, especially by middle
school-age children
Outreach to schools, churches, and various worksites to educate people about risks of
smoking and occupational exposures.
Screen current or former smokers and workers in high risk occupations using the
Chronic Respiratory Disease Questionnaire and peak expiratory flow rate or FEV1 in
order to increase early detection of COPD
Intervention components:
o Risk reduction: smoking cessation and/or reduction of occupational exposure to
irritants.
o Referral to primary care provider and/or pulmonologist, as needed
o “Learning to Live with COPD” workshops
o Chronic Disease Self-Management workshops
o Better Breathers Club or other community-based support group
o Pulmonary rehabilitation, as needed
o Nurse or respiratory therapist to provide case management for patients with
frequent exacerbations and subsequent hospitalizations.
As with all of our programs, we will seek grant funding for the COPD Program.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
93
Planning for the Uninsured/Underinsured Patient Population
California Hospital Medical Center’s Charity Care/Financial Assistance Policy is attached
(please see Attachment A).
Eligibility for charity care/financial assistance is considered for those individuals who are
uninsured, underinsured, ineligible for any government program, and who are unable to pay for
their care.
Currently Financial Counselors interview all private pay patients who are being admitted to the
hospital as an inpatient. If the patient requires charity care/financial assistance, a financial
assistance application is completed prior to admission. For emergency cases, charity
care/financial assistance will be considered after the rendering of service if there is a
documented need. Future consideration is also given if, after billing, patients are unable to pay.
Close family members, friends or associates of the patients may also request consideration for
charity care/financial assistance consideration. Any member of the medical or hospital staff who
may be aware of the potential need for charity care/financial assistance consideration
may also initiate a referral.
Outpatients are given the payment assistance brochure and signs are posted in all registration
areas about our payment assistance program in order to inform the public.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
94
PLAN REPORT AND UPDATE INCLUDING MEASURABLE
OBJECTIVES AND TIMEFRAMES
A summary of key community benefits programs that have been a major focus of our hospital
over the last year is included in the Program Digests.
Type 2 Diabetes Prevention, Screening, and Intervention Program
Hope Street Family Center Early Head Start Program
Hope Street Family Center Family Literacy Program
Health Ministry Program
Healthy Eating Lifestyle Program
Para Su Salud
Hope Street Family Center School Readiness Program
A summary of the key programs that will be a major focus for our hospital over the next one to
three years, based on the findings from our needs assessment process and information related
in the Community Need Index is also included in the Program Digests.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
95
PROGRAM DIGESTS
Catholic Healthcare West has adopted five core principles recommended by the Advancing the
State of the Art in Community Benefit project that will guide the selection and prioritization of
Community Benefit program activities. These core principles are:
Disproportionate Unmet Health-Related Needs
Seek to accommodate the needs to communities with disproportionate unmet health-related
needs.
Primary Prevention
Address the underlying causes of persistent health problem.
Seamless Continuum of Care
Emphasis evidence-based approaches by establishing operational linkages (i.e.,
coordination and re-design of care modalities) between clinical services and community
health improvement activities.
Build Community Capacity
Target charitable resources to mobilize and build the capacity of existing community assets.
Collaborative Governance
Engage diverse community stakeholders in the selection, design, implementation, and
evaluation of program activities.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
96
Type 2 Diabetes Prevention, Screening, and Intervention Program
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2 Health Promotion/Disease Prevention
Priority Area 3 Disease Management
Priority Area 4
Priority Area 5
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
The prevalence of diabetes among the adult population in Los Angeles County is 7% (Los Angeles
County/Department of Health Services, 2004e). This is nearly three times higher than the Healthy
People 2010 objective of 2.5%. The prevalence is higher among American Indians (12%), Latinos
(12%) and African Americans (10%) compared to Whites (6%) and Asian/ Pacific Islanders (5%) and
higher among low-income groups (LAC/DHS, 2004e). The highest prevalence of diabetes was
among adults aged 65 years and older, where one in five reported having been diagnosed with
diabetes. Among adults who were obese, the prevalence of diabetes was nearly five times higher
than those not overweight or obese. Nationally, 90-95% of diagnosed diabetics have type 2 diabetes
with an adult onset. Estimates suggest that one out of every three adults with diabetes has not yet
been diagnosed.
Diabetes, the sixth leading cause of death in the U.S. (Centers for Disease Control and Prevention,
2004c), is associated with cardiovascular conditions such as heart disease and strokes. Persons
with diabetes are also three times more likely to die from pneumonia or influenza. Heart disease is
the leading cause of death among persons with diabetes. Heart disease and stroke account for
approximately 65% of deaths among people with diabetes. Diabetes is the fourth leading cause
(age-adjusted) of mortality in the CHMC service area. Between 1990 and 2000 there was an
increase of 53% in diagnosed diabetes, suggesting a growing health care condition in L.A. County.
Nationally, it is expected that diabetes among Latinos will increase by 100% between 2002 and
2020.
The August 2007 edition of L.A. Health Trends documents a steady rise in the rate of diabetes
among adults 18 years and older, from 6.6% in 1997 to 7.5% in 1999, 7.6% in 2002-3, and 8.6% in
2005. This increasing prevalence likely reflects the impact of sedentary lifestyles and the obesity
epidemic. Obesity is the single most important risk factor for type 2 diabetes, the major form of
diabetes in adults. Other risk factors include increasing age, family history, and physical inactivity. In
Los Angeles County, direct costs of medical care for diabetes and indirect costs associated with
disability and lost productivity were estimated to be $5.6 billion in 2005. The LA County Health
Survey (LACHS) identified large disparities in diabetes by race/ethnicity, income, and educational
level.
Diabetes rates among Latinos (12.3%) and African Americans (12%) were nearly double
the rates among Whites (5.6%) and Asian/Pacific Islanders (7.1%).
Nearly one in five adults 65 years and older have been diagnosed with diabetes according
to the 2005 LACHS.
From 1997 to 2005, the rate of diabetes increased most rapidly among those living in
poverty and was more than two times higher in this group than among those with incomes
at or above 200% of FPL.
In 2005, the prevalence of diabetes among adults who did not graduate from high school
(14%) was more than two times higher than the prevalence among adults who graduated
from college (6%).
The prevalence rate of diabetes among adults was the highest in SPA 6 (14.5%) followed
by SPA 4 (11.4%).
The U.S. Healthy People 2010 preventive health targets for people with diabetes include selfmonitoring blood glucose at least once a day, having a diabetic eye exam and foot exam once a
year, and being up-to-date on immunizations. The 2005 LACHS revealed that adults with diabetes in
LA County were far from complying with these targets.
63% had received a foot exam in the past year. Diabetes can cause blood vessel and
nerve damage that, without preventive measures, frequently lead to leg or foot amputation.
57% had received an eye exam in the past year. Diabetes is the leading preventable
cause of blindness in the U.S.
47% had received a flu shot in the past year. Diabetics are at increased risk for severe
complications of influenza.
63% of adults (65 years and older) reported ever having a pneumonia shot. Diabetics are
at increased risk for contracting pneumonia and developing complications from it.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
97
On 6/24/08 the CDC released a news bulletin announcing that 24 million (8%) of Americans now
have diagnosed diabetes, an increase of 3 million in the past 2 years. The number of new cases of
diagnosed diabetes varied by aged:
o
281,000 were ages 20-39 yr
o
819,000 were ages 40-59 yr
o
636,000 were ages 60+
There are also striking racial/ethnic disparities among those with diagnosed diabetes:
16.5% of Native Americans/native Alaskans
11.8% of African Americans
10.4% of Hispanics
7.4% of Asian Americans
6.6% of Whites
Another 57 million Americans have Prediabetes.
Moreover, the prevalence of diagnosed and undiagnosed diabetes increases with increasing age:
o
2.6% of those aged 20-39 yr
o
10.8% of those aged 40-59 yr
o
23.8% of those aged 60+
Having health insurance and access to a regular source of care are essential for effective
management of diabetes.
In 2005, only 26% of adults with diabetes who did not have a regular source of care had an
eye exam in the past year, compared to 60% of adults with diabetes who did have a
regular source of care.
Similar to findings from 2002-3 LACHS, in 2005 a larger percentage of insured adults with
diabetes (59%) reported having an eye exam compared to uninsured adults (43%).
In 2002-3, only 32% of uninsured adults with diabetes self-monitored their blood glucose at
least once daily compared to 60% of insured adults with diabetes.
Diabetics are at increased risk for heart disease and stroke, so addressing hypertension, high
cholesterol, obesity, smoking and physical inactivity is important. Among adults with diabetes:
58% had hypertension
56% had high cholesterol.
48% reported minimal to no regular physical activity
41% were obese based on self-reported height and weight.
14% reported being a current smoker.
Program Description
In 2004, the Chronic Disease Management Consortium (CHMC, Good Samaritan Hospital,
Huntington Memorial Hospital, and the National Health Foundation) designed, submitted, and
received a multi-year grant from the Good Hope Medical Foundation for a comprehensive program
for the prevention, screening, and treatment of type 2 diabetes. This program has three distinct
goals: 1) To increase early identification of those at high-risk for developing diabetes and to provide
education and promote behavioral changes that prevent its development (Primary Diabetes
Prevention Services); 2) To increase early diagnosis of those with diabetes and to provide education
and support to help them manage their disease (Secondary Prevention Services); and 3) To educate
providers to promote quality diabetes care in the community (Provider Education).
CHMC’s community health promoters provide outreach education about type 2 diabetes at local
schools, churches, and community-based organizations and encourage all class participants to
complete the American Diabetes Association’s Diabetes Risk Test. Participants scoring 10 or more
points are at a greater risk for having diabetes and will be referred to a health care provider to
determine if they have diabetes. Participants not found to have diabetes will be invited to participate
in Primary Diabetes Prevention Services that includes 4 weekly workshops promoting healthy eating
and increased physical activity.
Diagnosed type 2 diabetics will be invited to participate in Secondary Prevention Services that
include:
Living with Diabetes: 5 weekly workshops designed to help patients understand their condition.
Topics include:
Understanding what diabetes is
Strategies and benefits of good diabetes control
Importance of blood sugar monitoring
Nutrition
Lifestyle behaviors (physical activity, weight management, smoking
cessation)
Mental health
Partnership with healthcare team
Identifying and avoiding diabetes complications
Social support
Preventive care
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
98
Community resources
Chronic Disease Self-Management Program (CDSMP): This six week intervention is based on
self-efficacy theory and emphasizes problem solving, decision making and confidence building.
The Program was designed by K.R. Lorig et al of the Stanford Patient Education Research
Center. Two bilingual, indigenous community health promoters lead the 6-week, small group
intervention using a highly structured manual. Subjects covered include: techniques to deal
with problems such as frustration, fatigue, pain, and isolation; appropriate exercise for
maintaining and improving strength, flexibility, and endurance; appropriate use of medications;
communicating effectively with family, friends, and health professionals; nutrition; and making
informed treatment decisions. The sessions are highly participatory. Mutual support and
success build patients’ confidence in their ability to manage their health and maintain active and
fulfilling lives. .
Additional educational interventions:
Dental hygiene class given by Community Dental Partnership community health promoter.
Referrals for dental care through the UniHealth Community Dental Partnership Program.
Referrals for smoking cessation classes, as needed.
Provider education will be open to all providers (physicians, nurse practitioners, physicians’
assistants, etc.) and will emphasize quality improvement, identifying new resources, and providing
information. Providers will be updated about the California Diabetes Program and its useful website,
www.caldiabetes.org/about.cfm. This website includes: Basic Guidelines for Diabetes Care, an
evidence-based, user-friendly packet of materials to aid health professionals deliver quality care to
their patients; Diabetes Health Record card; Take Charge! PowerPoint presentation; Diabetes Care
Coordinator Program, a train-the-trainer program aimed at medical office assistants to elevate their
role to become an important member of the diabetes health care team; and much more.
All data are entered into the web-based data system housed at the National Health Foundation, the
program evaluator.
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
1)
To increase early identification of those at high-risk for developing diabetes and to provide
education and promote behavioral changes that prevent its development (Primary Diabetes
Prevention Services);
2) To increase early diagnosis of those with diabetes and to provide education and support to help
them manage their disease (Secondary Prevention Services);
3) To educate providers to promote quality diabetes care in the community (Provider Education).
The Executive Committee met monthly during the start-up period and at least six times each year
thereafter.
Project dieticians developed the Food, Fitness, and Diabetes Prevention curriculum based on current
recommendations and the Healthy Eating Lifestyle Program curriculum that they’d previously
developed.
Project dieticians developed the Living with Diabetes Curriculum based on the following curricula:
United Against Diabetes from the National Alliance for Hispanic Health, Diabetes Empowerment
Education Program from the University of Illinois, and Take Charge with the Diabetes Health Record
from the Diabetes Coalition of California and the California Diabetes Prevention and Control
Program.
Staff were hired and trained to teach using the two curricula. Teaching tools/props will be
developed/purchased.
Outreach to local physicians and clinics to recruit diabetes who could benefit from this
comprehensive diabetes education program began.
The web-based data system was designed by staff at NHF.
Patient enrollment began in October 2005.
Primary Diabetes Prevention Services
At least 2000 will participate in community-based education on type 2 diabetes during the 3 year
grant.
600 will complete the ADA Diabetes Risk Test.
All of those with scores of > 10 will be referred to health care provider for definitive diagnostic testing
for diabetes.
50% of those referred to health care providers will follow-up on these referrals and determine their
diabetes status.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
99
40% of those referred to health care provider but determined not to have diabetes yet will participate
in the Primary Diabetes Prevention Services.
Of those participating in the Diabetes Prevention Workshops:
80% will self-identify as being at high-risk for diabetes.
80% will report increasing their knowledge about healthy eating.
80% will report increasing their knowledge about the importance of physical activity.
60% will report increasing their amount of exercise (frequency and length of time): goal 30
minutes a day, 5 days a week.
60% will report eating more healthily.
50% will reduce their weight by 5-7%.
70% will report asking their health care provider if they should be tested for pre-diabetes.
Secondary Prevention Services
60% of patients diagnosed with diabetes will participate in Secondary Prevention Services.
Of patients participating in these services:
70% will show reduced Hemoglobin A1c (goal < 7).
50% will show reduced Body Mass Index ratios.
50% will reduce their weight 5-7%.
50% will show reductions in waist circumference.
70% will report eating more well-balanced healthy meals.
70% will report eating less fat.
70% will report eating less calories.
60% will report cooking more healthily (i.e., less fat).
80% will know that their blood sugar records should be reviewed at every visit.
80% will know that their blood pressure should be checked at every visit.
80% will know that their weight should be checked at every visit.
80% will know that their feet should be examined at every visit.
80% will know that their HgbA1c should be measured every 3 months.
80% will know that the target for the HgbA1c is less than 7.
80% will know that their urine should be tested once a year for protein.
80% will know that they should have a dilated eye exam once a year.
80% will know that they should have a blood test to measure “fats” (i.e., a lipid profile) once a
year.
80% will know that they should have a flu shot once a year.
80% will know that they should have a pneumonia vaccine at least once.
80% of those who smoke will know that they should stop.
50% will check blood sugars at least daily.
50% will check their feet daily for sores.
Of patients participating in the CDSMP:
70% will complete the workshop series.
80% will report increasing confidence in managing their care.
70% will report increasing their physical activity.
70% will report eating more well-balanced, healthy meals.
70% will report taking their medication as directed by their health care provider.
60% will report visiting their doctor for problems related to their diabetes.
60% will report feeling more comfortable asking their doctor about their diabetes.
70% will report feeling less sad, lonely, or down in the dumps due to their diabetes.
Provider Education
Information is presented at educational forums (Grand rounds, lectures, etc.) for providers
at least twice a year by each participating hospital.
Baseline
A minimum of 60 providers/hospital will participate each year.
Residents in our service area have a high prevalence of the following risk factors for type 2 diabetes:
ethnicity, family history, obesity, lack of physical activity, food insecurity; and lack of access to
prevention programs.
Residents in our service area have the following risk factors for delayed diagnosis and treatment of
type 2 diabetes: uninsured, poverty, lack of access to primary care for screening and initiation of
treatment.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
100
Intervention Strategy for
Achieving Goal
Result FY 2008
Residents in our service area are at increased risk for morbidity/mortality secondary to type 2
diabetes because they lack access to regular source of care, lack access to specialty care, cannot
afford medications or supplies (glucometer, test strips, lancets), and lack access to comprehensive
diabetes education.
Once grant funding was secured for this program, curriculum development began while the Executive
Committee obtained IRB waivers, developed plans to patient recruitment and later began to recruit
and train professional staff. Once staff was hired, all staff participated in Diabetes Empowerment
Education Program training by staff from the University of Illinois. Project dieticians later trained the
community health promoters (CHPs) on the two curriculums. Kaiser Pasadena staff trained the CHPs
to be lay leaders for the CDSMP workshops in English and Spanish. CHPs then began outreach to
local physicians and clinics. CHPs also began Outreach Events. Participant recruitment, screening,
and assessment began. We then began to offer Prevention, Intervention , and CDSMP workshops.
The Executive Committee meets every other month.
Patient enrollment began in October 2005.
The following results represent all participants between October 2005 and August 2008.
286 Outreach Events were held and 5418 participants completed the ADA Risk Test. 13% were low
risk, 36% were intermediate risk and 52% were high risk for diabetes according to their ADA Risk
Test results. 2095 high risk individuals accepted a referral to a local physician/clinic for further
medical evaluation for diabetes.
128 4-wk series of Prevention workshops were presented, 53% in English and 47% in Spanish.
80% of 852 enrolled participants completed the 4-wk series of Prevention workshops. The
demographic profile of the participants was: 67% Hispanic, 7% African American, and 17%
Caucasian, and 7% Asian. 12% were male and 88% were female. 32% were overweight and 41%
were obese. 66% had a waist circumference > desired cutoff (35” for women and 40” for men). .
Paired data of Prevention participants demonstrated the following:
27% lost weight from the beginning until 3-6 mo. follow/up. 9% lost > 5% of their weight
during this period.
46% improved their knowledge about healthy eating. 36% eating > 5 servings of fruits and
vegetables/d; 76% drinking > 4 cups of water/d; 72% eating breakfast daily; 76% eating
fast food 0-1 days in last week.
At beginning of program 63% knew how much physical activity is recommended. 21%
improved their knowledge about physical activity. 62% increased duration of PA to > 30
minutes each time; 49% increased the distance walked/d; 35% increased frequency of
being physically active to > 4 times/wk.
106 5-wk series of Intervention workshops were presented, 40% in Spanish and 59% in English.
75% of 496 enrolled participants completed the 5-wk series of Intervention workshops. The
demographic profile of the participants was: 58% Hispanic, 20% African American, 5% Asian and
14% Caucasian. 32% were male and 68% were female. 29% were overweight and 56% were obese.
77% had a waist circumference > desired cutoff.91% of participants were already diagnosed with
diabetes; 7% were newly diagnosed. 62%% had a Hemoglobin A1c above the normal range at
intake. In terms of pre-existing diabetic complications:10% had a heart attack, 9% had a stroke, 7%
had kidney disease, 16% had diabetic retinopathy, 2% had an amputation, 32% had diabetic
neuropathy, and 15% had gastroparesis.
Paired data of Intervention participants demonstrated that by the end of the Program:
35% lost weight during the 5-wk interval.
14% lost > 5% of their body weight by the 3-6 mo. follow-up visit.
12% decreased their HgbA1c below 7; total of 53% had Hgb A1c < 7 at end.
51% improved their confidence in being able to improve their eating habits.
o
37% eating > 5 servings of fruits & vegetables/d
o
79% drinking > 4 cups of water/d
o
82% eating breakfast daily
o
75% eating fast food 0-1 days in last week.
51% improved their confidence in being able to improve their exercise habits.
o
12% started being physically active
o
37% physically active > 4 times/wk; 62% total.
o
37% increased frequency
o
56% physically active > 30 minutes each time; 79% total.
o
39% increased duration of PA
o
51% increased distance walked each time.
42% increased their emotional wellbeing
65% improved their confidence in being able to manage their diabetes.
o
20% began asking questions about their diabetes and treatment
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
101
o
14% increase in discussing their personal problems related to diabetes with their
doctor
o
46% learned what the HgbA1c target was
o
79% checked feet daily for sores
o
71% had dilated eye exam in past year
o
5% quit smoking
o
23% requested pneumonia vaccine.
o
40% requested flu shot.
54 CDSMP workshops were held, 48% in English and 52% in Spanish. A total of 252 participants
and 282 guests attended. The retention rate was 72%
LTIP Results
Hospital’s Contribution / Program
Expense
See table below Program Digest.
The impact of Living with Diabetes on healthcare utilization for glucose control was that there was an
87.2% decrease in hospitalizations and an 87.5% decrease in ER visits for glucose control
during the six months following program participation compared to the 6 months prior to program
participation.
CHMC provides office space and office equipment for program staff. CHMC Foundation provides
grants management and fiscal oversight.
CHMC receives $228,013 per year for this 3-year project, which is funded by a grant from the Good
Hope Medical Foundation.
Due to delayed start-up, a no-cost extension was requested. Therefore the program’s grant funding
will now end in December 2008. The project will continue as part of Community Benefit programming
because it is our LTIP.
FY 2009
Goal 2009
1)
2)
3)
2009 Objective
Measure/Indicator of Success
Baseline
Intervention Strategy for
Achieving Goal
To increase early identification of those at high-risk for developing diabetes and to provide
education and promote behavioral changes that prevent its development (Primary Diabetes
Prevention Services);
To increase early diagnosis of those with diabetes and to provide education and support to help
them manage their disease (Secondary Prevention Services);
To educate providers to promote quality diabetes care in the community (Provider Education).
Maintain same modified measurable objectives as FY08.
Outreach to federally qualified health centers (FQHCs) who care for many diabetics but may not
have the resources to provide comprehensive diabetes education.
Begin to develop sustainability plan for this much needed program.
There is a growing need for this program in CHMC’s service area. See data above from 2005
LACHS.
Continue to monitor and report measurable objectives.
Link the hospital discharge planning process to the Secondary Prevention Services
Develop collaborative agreements with local FQHCs that would like us to provide diabetes education
for their diabetics.
Increase outreach to predominantly African American churches.
Work toward securing ADA accreditation of the Living with Diabetes curriculum in order to assist with
continuation funding of the intervention program.
Identify grant funding for the continuation of this program.
Present results of project to LA Care to see if they would pay for this educational program for their
members.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
102
Impact of Living with Diabetes on
Healthcare Utilization for Glucose Control
LWD Contacted 6 mo Prior to LWD 6 mo After LWD
Hospital
Stay
7/1-12/31/07
1/1-3/31/08
4/1-6/30/08
7/1-9/30/08
Total
45
45
27
20
15
11
27
21
114 97 (85%)
9
3
3
2
17
ER Visit
0
0
6
2
8
Hospital
Stay
1
0
0
1
2
ER Visit
0
0
0
1
1
87.2% decrease in hospitalizations; 87.5% decrease in ER visits
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
103
Hope Street Family Center Early Head Start Program
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2
Priority Area 3
Priority Area 4
Priority Area 5 Healthy Communities
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
According to the 2000 U.S. Census, the Hope Street Family Center’s (HSFC’s) service area has a
population of 351,734 with 10% of the population under 5 years of age (compared with 7% of the
population under age 5 for L.A. County). A vast majority (74%) of the population in this area
identifies themselves as Latino, compared with 45% in the county. In addition, residents who identify
themselves as “Other” make up the plurality of residents, followed by Whites and Asians. This is in
contrast with L.A. County where Whites comprise a near majority of the population. Residents in
HSFC’s service area are younger in comparison to the county as a whole. Sixty-four percent (64%)
of the population are under 35 years of age compared with 55% of the population of L.A. County. A
younger population indicates that there are more women of child-bearing age and likely more
families. A younger population also means that there is a higher percentage of working individuals.
The need for jobs leads to increased pressure on the job market and higher need for child care. The
households in the HSFC service area have much lower incomes than that of L.A. County. More than
a quarter of these households earn less than $10,000 per year. Furthermore, the percentage of
households earning less than $25,000 a year is 59%, compared with 26% for L.A. County. Thirtyeight percent (38%) of the individuals who live in the service area meet the federal definition of
poverty ($8,501/year for one individual)—more than twice the percentage of L.A. County. In HSFC’s
service area 90% of the children under 5 years of age and living in poverty are Latino. Compared
with L.A. County the residents in the HSFC service area are less educated. Forty percent (40%) of
people over 25 years of age have less than a 9th grade education. This rate is almost 2.5 times
higher than that of LA County (16%). The lower educational attainment indicates that, in general,
residents will become part of the unskilled workforce, working low-wage jobs with little prospect for
upward mobility. Spanish is the primary language spoken at home by 69% of those living in HSFC
service area, while English is the primary language in only 18% of the service area. The high degree
of Spanish-only homes leads to more cultural and linguistic isolation, and more difficulty in accessing
services. At the time of the Census, HSFC’s service area had a significantly higher percentage of
foreign born residents than native born (61% vs. 39%, respectively). Of the foreign born inhabitants,
~ 20% are naturalized citizens while 80% are not currently U.S. citizens. In addition, many of the
foreign born inhabitants entered the US in the past decade (48%). In contrast, LA County has a
higher proportion of native born inhabitants (64%) with 38% of the foreign born population being
naturalized citizens. HSFC service area is densely populated and the household size tends to be
larger than that of LA County. The service area has a larger proportion of the population living with
four or more persons per household than LA County (38% vs 31%, respectively). In addition, the
larger household size for HSFC service area could be an underestimation, since there are many
undocumented immigrants in this area and thus they are not calculated into the figure. Overcrowding
is often associated with increased social and economic pressure, higher poverty, and lower health
status. There is a serious shortage of licensed childcare capacity in HSFC service area. There is only
space for 9% of children 0-5 in the HSFC service area compared with 17% for LA County.
Significantly more children 4 years old and older have disabilities in the HSFC service area than in
LA County (5% vs 1.3%, respectively) (see table below). Speech or language impairment is the most
frequently occurring disability followed closely by a specific learning disability. Rates for speech or
language impairments are 3 times higher in HSFC’s service area than in the county as a whole. The
percentage of children with learning disabilities in the service area is twice as high as L.A. County.
In 2001 there were 9,275 live births in the HSFC service area. Low birthweight infants comprised 6%
of those births and very low birth weight infants made up 1%. Eighty-two percent (82%) of the
mothers received prenatal care in the first trimester, 10% in the second trimester, and 2% in the third
trimester. Only 0.4% received no prenatal care. The percentage of teenage mothers in our service
area (12.5%) is almost three times higher than the countywide percentage (4.6%).
The California Department of Education’s Academic Performance Indicator (API) is a numeric
measurement of school growth and performance. Schools’ API scores are ranked against each
other in order to identify schools that are underperforming. Schools are given a rank between 1 and
10, where a rank of 1 indicates the lowest statewide performance level and represents the lowest
10% in the state. In our service area 70% of the elementary schools had a rank in the lowest third,
compared to only 42% of elementary schools countywide.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
104
Program Description
The impetus for the Hope Street Family Center came from the hospital’s community needs
assessment and input from community leaders and other service providers. Our goal was to help
optimize the developmental outcome of children born at our hospital and/or living in our community.
More than 5,000 babies are delivered at California Hospital Medical Center (CHMC) annually and
CHMC is the acknowledged provider of choice for women’s health services in Central Los Angeles.
But CHMC was not satisfied with just optimizing birth outcomes; it wanted these children to reach
adulthood having experienced a safe, healthy (physical, cognitive, social and emotional), and
nurturing childhood that prepares them to become responsible and contributing members of the
community. Only then could CHMC achieve its vision of “improving the health and well-being of the
community by helping people help themselves.”
In September 1992, the Hope Street Family Center (HSFC) was founded with a research and
demonstration grant from the federal Head Start Bureau, part of a national effort to develop more
effective ways to break the cycle of intergenerational poverty and school failure. The HSFC is a
collaborative venture between CHMC and the University of California, Los Angeles (UCLA). From its
inception, the advice of community leaders, other service providers, and families with young children
was sought to help inventory existing services, identify service needs and gaps, and to guide the
creation of HSFC. Several critical factors needed to be addressed: a) prevalence of poverty; b)
prevalence of immigrants; c) low literacy rate; d) issues regarding the delivery of health care,
including prenatal care; e) lack of affordable, quality child care; and f) the need for family mental
health services.
The HSFC is dedicated to: a) enhancing the overall development of children; b) strengthening the
economic and social self-sufficiency and stability of families; and c) enhancing the local service
delivery network of agencies serving young children and their families. Families with young children
can access a vast menu of services to meet their individual and changing needs through this family
resource center. The primary target population is pregnant women, infants, and children 0-5 who live
within the HSFC service area and whose family income is at or below 100% of the poverty line.
Referrals are received from CHMC departments and programs and an array of over 80 community
organizations (health centers, elementary and secondary schools, adult education programs, Head
Start programs, child and family service agencies, substance abuse treatment programs, and
churches). Currently, more than half of HSFC referrals are from CHMC (Women’s Health Center,
Family Health Center, community clinics, NICU, and emergency department). Increasingly, current
and former HSFC clients, pleased with their long-term experience with the program, refer relatives,
neighbors, and acquaintances.
HSFC offers a variety of programs that fall into three major categories: 1) early childhood education;
2) family literacy; and 3) family support/home visiting. Many programs include more than one of
these elements. Early childhood education programs include: Early Head Start, School Readiness
Program, Child Development Center, Early Childhood Center, Early Care & Education Center, and
Extended Day Family Childcare Network. Family literacy programs include: Even Start Family
Literacy Program, First 5 LA Family Literacy Program, English-as-a-Second-Language classes, Hope
Street Youth Center, and a Los Angeles Unified School District (LAUSD) Continuation High School
site. Family support/home visiting programs include: Early Head Start, School Readiness Program,
Nurse-Family Partnership Program, and Pico-Union Family Preservation Program.
The CHMC Hope Street Family Center has been providing comprehensive Early Head Start (EHS)
services since 1998. The EHS service area covers a four-mile radius in the heart of downtown Los
Angeles and includes a number of distinct central city neighborhoods, including PicoUnion/Westlake, Adams/Normandie, University, and Hoover. Early Head Start, the centerpiece of
the HSFC, provides 152 low-income pregnant women and their families with children, 0-3 years of
age, with family-centered services to facilitate child development, support parental roles, and
promote self-sufficiency. Priority for EHS enrollment is given to children with special needs; women
with high-risk pregnancies; parents interested in ESL or high school diploma/GED studies; and teen
parents. Enrollment priorities reflect community assessment data which document a high incidence
of teen pregnancy and developmental disabilities within our service area; large numbers of recent
immigrants and monolingual Spanish-speaking young families; and low adult literacy and educational
levels. The EHS program is funded to provide services for 152 children and pregnant women
through home-based (96), center-based (32), and combination (24) options.
Core services include early childhood education (ECE); healthcare and mental health services;
parenting education; childcare; adult education; and housing, legal and financial assistance. We
have put into place a continuum of home and center-based early childhood education services that
responsively meet the individual and changing needs of young families. Options currently available
to families include: 1) home-based services, with weekly in-home ECE, along with twice-per-month
socialization opportunities; 2) full-year, full-day center-based ECE, with monthly home visits; 3)
combination option services, with daily center-based family literacy services, combined with biweekly
in-home ECE; and 4) biweekly in-home ECE, concurrent with enrollment in high-quality childcare,
and bimonthly visits at the childcare site.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
105
The HSFC Child Development Center (CDC), a licensed childcare center, provides full-day, full-year
ECE to 32 EHS infants and toddlers, 0-3 years of age. Within the CDC, EHS performance standards
are maintained through the following practices: 1 ) A staff to child ratio of 1:3, with a group size of 8
maintained in the infant classroom. A staff to child ratio of 1:4, with a group size of 8 maintained
within the toddler classroom; 2) The Creative Curriculum is utilized, with monthly themes coordinated
across program options. Weekly lesson plans are developed based upon Creative Curriculum
principles and individualized according to children’s assessed needs and strengths. Individual
observation notes are written for all children on a weekly basis; 3) Teachers are required to hold or
be working toward an AA degree in child development, with a BA preferred. Among current teachers,
5 hold BA degrees, 5 hold AA degrees, and 3 teachers are completing coursework toward an AA.
Teachers participate in individual supervision on a twice per month basis with group supervision
provided by classroom on a weekly basis; 4) Classroom environments foster the child’s primary
language and reflect children’s cultures; and 5) The Infant-Toddler Environmental Rating Scale is
used to regularly monitor classroom environments and caregiving practices. Center-based infants
and toddlers also benefit from monthly home visits with a focus on maintaining continuity between
center and home environments. Quarterly parent-teacher conferences also support continuity,
facilitate parent involvement, and help to optimize children’s developmental progress. To ensure
collaboration and coordination between home and center-based services, the CDC Director meets on
a regular basis with the EHS Director and Child Development Coordinator regarding issues of
curriculum, children’s development, and EHS performance standards. The CDC Director also
participates in EHS management meetings that are held twice per month and include the EHS home
visitor supervisors. The CDC gives preference to EHS graduates for enrollment in the school
readiness pre-school classroom.
Combination center- and home-based services are provided through our Family Literacy Program,
funded by the California State Department of Education and First 5 LA. The program has the
capacity to provide comprehensive family literacy services for 24 EHS parents and their infants and
toddlers, 0-3 years of age. In collaboration with LAUSD, the program offers ESL and parenting
instruction, 3 hours per day, Monday to Friday; 3 hours per day of center-based ECE for children 0-3
years; and 1 hour per day of parent-child activities within the child’s classroom setting. In addition, 2
home visits are made per month, with both parent and child present. Center-based ECE activities
within the family literacy program mirror those described previously for the CDC. To ensure
collaboration and connection between home- and center-based services the Family Literacy
Coordinator meets on a weekly basis with the EHS Director, ECE Coordinator, and Child
Development Coordinator. The Family Literacy Coordinator also meets weekly with the home visitor
supervisors to ensure coordination of family literacy services with home-based EHS services. Family
literacy ECE staff attends EHS case conferences when a family who is receiving family literacy
services is discussed.
Weekly home visits are provided to home-based pregnant women and children, with attempts made
to schedule visits when fathers are available whenever possible. Using materials from the EHS
home visiting library, in-home ECE activities are based upon developmental assessment findings, as
well as staff’s periodic assessments of children’s developmental progress. Weekly visits last ~one
and one-half hours and include discussions of health, safety, nutrition, and child development issues,
as well as engagement of parents and children in pre-planned ECE activities. Supporting children’s
emerging communication and language skills has continued to be an important emphasis during
home visits, based upon the high incidence of early language delay within our community.
Funds from the California State Department of Education supports a network of 13 licensed family
day care providers, serving children 0-6 years of age. All providers are located within the EHS
service area, with the majority of providers offering care during non-traditional hours in order to
accommodate parents who work or study in the evening and on weekends. To ensure quality care
Network providers are required to attend monthly group training and are visited at least once per
month by the EHS Program Specialist, who provides technical assistance regarding individual
children and offers assistance related to general quality improvement issues. The Program
Specialist monitors each family childcare home using the Environmental Rating Scales for Family
Childcare (Harms) and the Health and Safety Checklist. EHS infants and toddlers who are care for in
the Network homes receive home-based services. The EHS home visitor makes a minimum of two
visits per month to the family home with both the parent and child present. The home visitor also
makes one visit per month to the family childcare home, with the parent and childcare provider
present. This gives an opportunity for the parent, home visitor, and provider to talk together about
the child’s development and individual caregiving issues. To ensure continuity between childcare
and in-home services, the Childcare Network Coordinator meets on a regular basis with the EHS
Director, Child Development Coordinator, and home visitor supervisors.
All children receive a developmental screening within 45 days of enrollment (Gesell), with
subsequent ongoing assessments (Desired Results Developmental Profile) by the Early Childhood
Coordinator-Disabilities Coordinator. This enables us to assess each child’s developmental
strengths and areas of vulnerability, identify previously unidentified children who have special
developmental needs and serves as the basis for providing developmentally appropriate center- and
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
106
home-based ECE activities.
The Health Coordinator provides leadership for health care services, in consultation with the EHS
Health Committee which is comprised of physicians from local clinics and hospitals, Los Angeles
County Department of Health Services administrators and local public health nurses, Women,
Infants, and Children program personnel, community psychologists, and parents. Health-related
activities focus on: 1) ensuring that children and families have access to primary prevention and
acute health care services, including well-child care, immunizations, WIC services, prenatal care,
adult health care, and dental services; 2) providing parents with information and anticipatory
guidance related to common health issues and concerns; 3) supporting staff in their educational and
case management roles; and 4) supporting the educational and health access needs of parents and
children with chronic health conditions. The Health Coordinator (a registered nurse) provides a home
visit to all women during pregnancy and within 2 weeks after delivery, establishes access to dental
screening and treatment for all pregnant women, and introduces weekly yoga classes for mothers.
The Mental Health Coordinator (Psy.D) and the Social Services Coordinator (MSW) share
responsibility for oversight of family support services. Daily on-site mental health services ensure
families’ access to direct clinical assessment, as well as supportive services. Assessment,
screening, crisis intervention, and brief counseling are provided for individuals, couples, and family
units, both at the Center and in the family home, as needed. Improved housing continues to be a
primary goal for many families with the majority of families requiring some form of housing
assistance. Acquiring additional vocational, English language, and/or educational skills is critical to
increasing self-sufficiency for many families. Through collaborative agreements, EHS has
established community linkages with local legal advocacy and legal service agencies. EHS
assistance with transportation needs has been critical to enabling families to participate in centerbased program activities, as well as actively work toward self-sufficiency goals through employment
or attendance in educational programs. The EHS van is utilized on a daily basis to help families
attend medical and other special appointments and participate in socialization and ECE related
activities, including community-based functions. Emergency funds are used to increase family
stability and assist families with achieving self-sufficiency goals. Childcare continues to be a
pressing need for families as they identify and pursue educational and training goals. The EHS
Outreach Coordinator has the primary responsibility for overseeing our collaborative agreements with
Crystal Stairs and Pathways, our local childcare funding agencies.
Governance: The EHS Policy Council meets monthly with additional meetings held on an as needed
basis to address personnel, finance, and Council orientation and training issues. The CHMC
Community Board and HSFC Community Board provide leadership with respect to budget,
personnel, service delivery, and long term planning issues. The Policy Council, Community Advisory
Committee, and the Parent Committee also work to expand the service delivery network through
ongoing activities that build relationships with a variety of community organizations. Additionally, the
Project Director holds weekly management meetings with the area coordinators (Mental Health,
Social Services, Child Development, Family Literacy, Outreach, and Health) and program specialists
to review and problem-solve issues related to recruitment, services, program administration, and
personnel. Smaller unit meetings of teachers and home visitors with their supervisors are held
weekly. All clinical staff participates in weekly case conference discussions.
Annual Self Assessment: We utilize the 2008 Office of Head Start Monitoring Protocol along with
standardized and locally developed tools that assisted with gathering information about program
management and services. Tools utilized during the self-evaluation process included the
Infant/Toddler Environmental Rating Scale (ITERS) and Family Day Care Rating Scale (FDCRS)
which were used to assess the quality of caregiving environments in classrooms and family childcare
homes; the Parent Survey, which provided information regarding parent and family satisfaction; the
Classroom Chart Review Instrument, Family File Chart Review Instrument, the Fiscal Review
Instrument, and the Eligibility Verification Instrument which were used to gather additional
programmatic and fiscal information. To monitor child and family needs, the extent to which the
program is implementing required activities, and the extent to which parents and children are
participating in program services, the following MIS reports are prepared and reviewed by EHS
management and clinical staff on a monthly basis: Developmental Screening/Assessment Dates and
Results Report; Family Assessment Tracking Report; Summary of Contacts by Service Report; Child
Medical History Report; Health Services Received Report; Immunization History Report; Pregnancy
Outcome and Prenatal Care Report; Assessed Family and Individual Needs Report; and Mental
Health Services Report.
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
Optimize the overall development of infants and toddlers participating in HSFC’s EHS program.
Strengthen the economic and social self-sufficiency and stability of their families.
Enhance the local service delivery network of agencies serving young children and their families.
1)
Maintain full enrollment
2)
Promote the overall (physical, cognitive, social, and emotional) development of infants and
toddlers through a continuum of early childhood development and health services that include
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
107
3)
4)
5)
Baseline
Intervention Strategy for
Achieving Goal
Result FY 2008
in-home and center-based early childhood education (ECE) activities and opportunities,
comprehensive health and nutritional services and anticipatory guidance on these matters,
social service and mental health support services, and early intervention services.
Enhance the capacity of parents to nurture and care for their very young children by providing a
variety of parent education and family support services that bolster their roles as parents and
the self-sufficiency of their families. Parent education opportunities are made available through
a) individualized in-home parent education; b) an on-site parenting education program; and c)
monthly meetings of the HSFC Parent Committee. Family support and links to community
resources are provided through weekly or biweekly in-home case management activities.
Build on an existing service delivery network and foster community partnerships that will keep
the network accessible, responsive, and sensitive to the developmental, cultural, and familial
characteristics of the service population.
Continuously refine and expand the existing base of knowledge, skills, and abilities of program
staff to improve their capacity to serve very young children and their families, especially
families at high risk due to developmental disabilities, substance abuse, domestic violence, or
child abuse.
HSFC’s service area has the highest population density and the oldest housing stock in the county. It
is the home of the working poor. The median annual household income is $19,930. Moreover, 42%
of households earn less than $15,000 per year. More than 21,000 children under the age of five live
below poverty, yet more than half of these children live in households in which one or both parents
work. A third of the labor force is employed in the garment industry and other light manufacturing
industries and a fifth in service occupations. In terms of ethnicity, 72% are Latino, 9% African
American, 7% Asian, and 6% Caucasian. However, more than 90% of the elementary school-aged
children are Latino. Children under age 14 represent 28% of the population and only 7% of residents
are > 65. Spanish is the primary language for more than 55% of families in the area. In a study of
Latinos in South Central Los Angeles, 96% of the children were born in the U.S. compared to only
20% of their parents. Downtown Los Angeles is ranked as the lowest literacy area in the city. The
region has high levels of limited English proficiency; more than 70% of school-aged children are
limited English proficient. In the core service area, 23% of persons 16 years and older have a high
school education or less; 36% have less than a ninth grade education; and 61% have only
rudimentary education. Parents in this community often find themselves isolated, feeling depressed
and overwhelmed by their daily struggle for economic survival. Hence, they are less likely to
verbalize a great deal with their young children or to utilize communication styles that nurture early
language skills. Likewise, the babysitters with whom they leave their children while they work are
unaware of the importance of language development in children and how to foster such development
in children in their care. This lack of knowledge can seriously impact children’s futures since studies
show that impairment of early language development becomes a disability for children, limiting their
subsequent social and educational growth
Continue to provide EHS services for qualifying families in our service area in accordance with EHS
performance standards and guidance as specified in our contract and implementation plan.
The EHS program served 158 families, with an average family income of $8,408. With respect to
ethnicity, 96% of families were Latino and 4% African-American. Spanish was the primary language
for 93% of parents. Eighty-one percent (83%) of families were two-parent households. Parental
educational levels were low, with 35% of parents having had less than an 9th grade education. 63%
of parents had not completed high school. On a more promising note, 8% of parents had had some
college coursework and 5% had completed a bachelors or graduate degree. However, in the
majority of these cases parents were significantly under-employed, frequently due to a lack of
English language skills.
We received 104 referrals; sources of referrals included word-of-mouth (31%), current parents and
HSFC staff (21%), CHMC and other surrounding clinics and hospital such as Children’s Hospital Los
Angeles and Orthopedic Hospital (15%), social service agencies (9%), LAUSD (6%), and others
(7%). The Outreach Coordinator maintains an active waitlist, with the selection of children and
pregnant women based on established enrollment priorities. Priority for EHS enrollment is given to
children with special needs; homeless families; foster children; parents interested in ESL or high
school diploma/GED studies; and families participating in other HSFC programs. At the present time
there are 34 families on the waitlist. Families with priority status generally have a 2-3 week wait
before they are contacted for enrollment. Families without priority status typically remain on the
waitlist for a minimum of 3-5 months.
We enrolled 51 new EHS clients, including 9 pregnant women. Full program enrollment has been
maintained throughout the program year . During the same period 56 children have exited the
program. Reasons for leaving included family relocation outside the HSFC-EHS service area (7);
parent withdrew from the program (15); parent secured employment or full-time studies that
prevented participation (7); and child’s graduation from EHS at 3 years of age (27).
Among currently enrolled clients, 32 children are enrolled in the center-based option; 97 children and
5 pregnant women are enrolled in the home-based option; and 24 children are enrolled in the
combination option. Of the 97 children who are home-based, 11 currently receive childcare services
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
108
through our family childcare network. Our Family Day Care Network providers have served 13 EHS
children.
Our EHS program served 51 children with special needs. Identified disabilities included prematurity,
including extreme prematurity (under 26 wk), Down syndrome, autism, Treacher Collins Syndrome,
cerebral palsy, seizures, microcephaly, hydrocephaly, vision and hearing impairments, and spina
bifida. Several children also have the additional challenge of being technologically dependent
(hearing aids, G-tube, catheter, braces, etc.) Our present special needs enrollment is 31 infants and
toddlers, representing 20% of total enrollment. Within our special needs population, the most
prevalent problem is speech and language delay, with the greatest area of difficulty in the area of
expressive language. Currently 19 children (61% of children with special needs) are receiving early
intervention services due to speech delays. In addition, several other children have been found to be
at high risk but the extent of delay is not yet significant enough to warrant a referral. In response to
this issue we have placed a strong preventive focus on language development. These efforts have
been directed toward helping parents to more effectively promote speech and language in the home
and identifying staff training opportunities to enhance staff’s skills in working with parents and
children to promote early language skills.
Among the 223 children and 17 pregnant women served, 100% of children had a comprehensive
physical examination; 100% of pregnant women were/are enrolled in prenatal care services; 94% of
children had current immunizations and 92% of children were current with respect to well-child care
follow-up. Additional health related accomplishments have included the provision of nurse home
visits to all women during pregnancy and within two weeks of delivery. Additionally, through our
collaboration with the USC School of Dentistry EHS children participated in a dental screening
program, with education and follow-up services. Finally, a partnership with a local church and funding
from Catholic Healthcare West enabled us to continue a highly successful program of weekly on-site
yoga class for mothers. The Health Coordinator also worked closely with home visitors and area
coordinators in helping to address the needs of children with more complex health challenges.
Mental Health and Social Service Coordinators continued to provide direct assessment and
intervention services, as well support for home visitors in their ongoing work with families
impacted by maternal depression, substance abuse, marital discord, and domestic violence During
this funding period significant accomplishments in the area of family support and mental health
services included: 1) securing federal funding for Health Marriage services and began initial program
implementation; 2) increased involvement of fathers through Fatherhood and Healthy Marriage
Programs; 3) strengthened access to mental health services for children through staff development
activities and strengthened collaboration with CHMC Behavioral Health clinic; 4) increased access to
legal services through new partnership with Public Council. 56 families received direct clinical and
supportive services through EHS mental health component. Presenting issues included domestic
violence, paternal depression, psychiatric disorders, health, and extreme financial difficulties due to
unemployment or underemployment, threat of homelessness, and teen pregnancy. Ten families
were referred for child welfare services due to children’s exposure to domestic violence. One such
case involved a mother with schizoid affective disorder who has a child with developmental delays
and possible psychological issues. Another case also involved a mother with mental health issues
and a child with special needs. In this case the child was a micro-preemie with numerous health
complications. Additional examples of dire and complex cases include a young mother diagnosed
with HIV who is currently pregnant and has no social supports; and a family with 3 daughters, one of
whom suffers from seizures and twins who are exhibiting symptoms of autism.
With the addition of the Fatherhood Program, we have had an opportunity to serve families impacted
by substance abuse, depression, marital discord, and domestic violence in a much more
comprehensive manner. Several parents experiencing codependency issues were seen and referred
to al-anon groups The Healthy Marriage Program provides marriage education classes for lowincome families with young children. Classes are designed to help couples strengthen relationships,
improve communication, and gain skills to more effectively manage conflict.
As a result of our increased collaboration with the CHMC Behavioral Health Clinic, several successful
referrals were made for siblings of EHS children, with collateral support provided for parents.
Referral issues included exposure to domestic violence, anxiety, abuse, attention deficit,
hyperactivity, loss of an immediate family member, exposure to substance abuse, childhood
depression, and post-traumatic stress.
As noted above, the average annual income for families enrolled this past year was $8,408, with
unemployment, underemployment, and sporadic employment continuing to be challenges. Due to
gentrification, many families also experienced increased rents accompanied by deplorable living
circumstances. Thus, issues of poverty, childcare, and housing were pressing concerns and
habitually dominated the focus of case management services. In this regard, staff experienced some
success in referring families for Crystal Stairs subsidies and to Public Council for legal supports with
housing concerns. Through these interventions several families were able to secure funding for
childcare, as well as low-income or improved housing.
The immigration issues that surfaced at the national level were also a local focus. In this regard
parents were supported in accessing tax identification numbers (ITIN) so that they could demonstrate
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
109
their willingness to pay taxes; referred to legal immigration forums; and supported in their efforts to
learn English.
Acquiring additional vocational, English language, and/or educational skills was an additional
concern for many families. During this reporting period 49 parents participated in adult education and
training programs.
Finally, our EHS Mentoring Project, initially funded through a special ACF grant, has continued to
show positive benefits. Implemented in collaboration with the Hope Street Youth Center, this year the
project included 24 adolescent youth, many of whom are older siblings of EHS children, and fifty-two
EHS and HS-aged children. On a weekly basis youth provide three hours of classroom assistance,
including reading with children, and support with special projects. Youth are required to maintain a
minimum grade-point; complete homework on a daily basis; and participate in college and career
activities. Through this program we are able to: 1) support the academic achievement of adolescent
youth; 2) encourage the development of civic and community service values, through work-study
mentoring with Head Start and Early Head Start age children; 3) promote early language
development and pre-literacy skills among Head Start and Early Head Start age children; and 4)
create a career and college-bound culture, including giving youth an opportunities to explore a career
in child development.
The current EHS Policy Council was elected on March 15, 2008 and has met on a monthly basis,
with additional special meetings held on an as needed basis to address personnel, orientation, and
training issues. The Policy Council President is Zulys Gallegos..
The California Hospital Medical Center Community Board and Hope Street Family Center
Community Board continue to provide administrative and fiscal oversight for the EHS program, as
well as leadership for long term planning issues. Gene Grigsby, PhD services as president of the
CHMC Community Board.
Day-to-day program oversight is provided by the Project Director who meets twice monthly with the
CHMC Foundation President and on a monthly basis with Finance and Contracts & Grant staff. The
Director also holds weekly management meetings with the area coordinators (Mental Health, Social
Services, Child Development, Family Literacy and Outreach), childcare center director, and program
specialists to review and problem-solve issues related to recruitment, services, program
administration, and personnel. Smaller unit meetings of teachers and home visitors, with their
respective supervisors, are held weekly.
During this project year the EHS program experienced the following personnel changes as current
staff moved on to new opportunities and additional staff were hired.
On 5/27/08 Karen Estrada, BA, infant teacher, replace Tanya Suarez, BA who left the program
to work for LAUSD.
On 7/21/08 Mai Huynh, BA, infant teacher, replaced Rebecca Ramirez, BA who returned to
school.
All home visiting staff holds a minimum of a bachelor’s degree in early childhood education or a
related field. All classroom teachers hold an early childhood education teacher’s permit issued by the
State of California, Child Development Division. Additionally, among the sixteen teachers, five (31%)
have an associate degree in early childhood education or child development and seven (44%) have
completed a bachelor’s degree in early childhood education or child development. The 3 teachers
who have not achieved an associate’s degree are enrolled in coursework leading to a degree in early
childhood education.
All area coordinators hold a minimum of a master’s degree, within their area of clinical expertise.
Formal Memorandum of Understanding (MOU) were newly established, revised, or remained in
effect with the following twenty-six community partners:
Asian Pacific American Legal Center
Bay Area Addiction Treatment (BAART)
California Family Care Medical Group
California Behavioral Health Clinic
Children’s Hospital of Los Angeles
Community Counseling Services-Amanecer
Crystal Stairs
Eisner Pediatric and Family Medical Center
Esperanza Community Housing Corporation
Frank D. Lanterman Regional Center
Los Angeles Unified School District
Abram Freidman Occupational Center
Central Adult High School
Division of Special Education- Infant/Preschool Programs
Pacific Asian Consortium (PACE)
Pathways
Pico Union Housing Corporation
Public Health Foundation-WIC
St. Francis Center
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
110
Scott Newman Center
Soledad Enrichment Action, Inc.
South Central Los Angeles Regional Center
USC Head Start
USC School of Dentistry
USC Family Practice Center, USC School of Medicine
1736 Family Crisis Center
Hospital’s Contribution / Program
Expense
CHMC provides 1½ floors of Leavey Hall for the Hope Street Family Center (SB 697 in-kind
contribution value of $474,900).
The annual EHS budget is $2,047,216. The US Department of Health and Human Services funds
this program.
Goal 2009
Optimize the overall development of infants and toddlers participating in HSFC’s EHS program.
Strengthen the economic and social self-sufficiency and stability of their families.
Enhance the local service delivery network of agencies serving young children and their families.
Maintain full enrollment.
Promote the overall (physical, cognitive, social, and emotional) development of infants and
toddlers through a continuum of early childhood development and health services that include
in-home and center-based early childhood education (ECE) activities and opportunities,
comprehensive health and nutritional services and anticipatory guidance on these matters,
social service and mental health support services, and early intervention services.
Enhance the capacity of parents to nurture and care for their very young children by providing a
variety of parent education and family support services that bolster their roles as parents and
the self-sufficiency of their families. Parent education opportunities are made available through:
a) individualized in-home parent education; b) an on-site parenting education program; and c)
monthly meetings of the HSFC Parent Committee. Family support and links to community
resources are provided through weekly or biweekly in-home case management activities.
Build on an existing service delivery network and foster community partnerships that will keep
the network accessible, responsive, and sensitive to the developmental, cultural, and familial
characteristics of the service population.
Continuously refine and expand the existing base of knowledge, skills, and abilities of program
staff to improve their capacity to serve very young children and their families, especially families
at high risk due to developmental disabilities, substance abuse, domestic violence, or child
abuse.
FY 2009
2009 Objective
Measure/Indicator of Success
Baseline
Intervention Strategy for
Achieving Goal
Over the course of the past three years there has been no significant change in the demographic
make-up of the EHS service area, the estimated number of eligible EHS children and families, or the
ethnic and racial composition of eligible families. There are ~ 34,000 children under age 4 living in
the service area, with approximately 47% meeting the federal definition of poverty. Among children
in poverty living within the service area, 90% are Latino. The estimated number of children with
disabilities, four years old or younger and living in the area is ~ 5% with speech or language delay
being the most common disability.
The changes that have occurred within the service area are a result of the significant construction
and business expansion that has occurred within downtown Los Angeles, which comprises the
northern portion of our service area. The expansion of the Staples Center and the related new
condominium construction has the potential of offering increased employment opportunities and
better wages. In addition, three new low-income housing developments, also undertaken in
conjunction with Convention Center expansion, have positively impacted our community. As
documented above, the target EHS population experiences a significant lack of resources (income,
education, training, and housing) that place them at high risk for a variety of health and social
problems. Better housing and increased economic development are important and emerging
community strengths.
Continue to provide EHS services for qualifying families in our service area in accordance with EHS
performance standards and guidance as specified in our contract and implementation plan.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
111
Hope Street Family Center Family Literacy Program
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Program Description
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2
Priority Area 3
Priority Area 4
Priority Area 5 Healthy Communities
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
“Literacy skills predict an individual’s health status more strongly than age, income, employment
status, education level, and racial or ethnic group, according to an analysis of the research by the
nonprofit organization Partnership for Clear Health Communication” (Wilson, 2003, pg. 875).
Literacy skills can directly affects a patient’s ability to follow physician instructions, take medication
as prescribed, understand how to prevent disease, and self-manage and understand their rights
(Wilson, 2003; California Healthline, 2004; Institute of Medicine, 2004). Illiteracy affects patients’
ability to access care, in particular because of difficulties completing application forms for insurance
coverage or reading an appointment card. Most significant of all, it increases the chances of dying of
chronic or communicable diseases. A higher percentage of adults in Los Angeles County (27%) are
estimated to be at the lowest literacy proficiency level than for the state (19%) or the U.S. (20%).
Moreover, CHMC’s service area has the highest rate of low literacy (66%) in the county. The
greatest need for literacy services is for younger adults, particularly Latino and Asian/Pacific Islander
populations. Disability is also correlated with lower literacy scores; CHMC’s service area has
disability rates well above the county average of 9%: Downtown L.A. 11%, and South Central 14%.
Almost without exception, the highest levels of Limited English Proficiency (LEP) are the lowest
literacy areas in the county. Every low-literacy area also had an above average proportion of recent
immigrants. Moreover, residents of the lowest literacy areas show low levels of educational
attainment. While the county average for education less than 9th grade is 14%, in the low literacy
areas 24-40% of residents have less than a 9th grade education.
California Hospital Medical Center’s (CHMC) Hope Street Family Center (HSFC) has completed its
seventh year of providing comprehensive year-round Even Start Family Literacy program services to
families. The program is a cooperative effort between the Hope Street Family Center and the Los
Angeles Unified School District’s (LAUSD) Central Adult School. The HSFC’s Even Start Family
Literacy Program integrates early childhood, parenting, and adult education and serves ~ 40 Early
Head Start (EHS) families. This program targets low-income, recent immigrant Latino families, with
an emphasis on serving families with special needs children, 0-5 years of age. Approximately 2533% of the families served include children with special needs. Based on families’ needs and
schedule preferences, the program operates a 12-month intensive afternoon family literacy program
five days a week, Monday through Friday, from 12:00 p.m. to 4:00 p.m. While parents attend adult
education and parenting classes, their children, ages 0-5, receive early childhood education in infant,
younger toddler, older toddler, and preschool classrooms. Parent/child interactive literacy activities
(PCILA) take place regularly in the children’s classrooms. Even Start children ages 5-7 who are in
LAUSD elementary schools receive weekly language arts mentoring in the Hope Street Youth
Center. The project incorporates the National Center for Family Literacy/Kenan Family Trust centerbased model within a clinical setting, with home visits provided by caseworkers employed by CHMC .
In addition, CHMC offers Even Start staff access to its extensive community referral network and
Even Start families receive additional health, mental health, housing, and other social services.
Program enhancements for the past year focused on parent involvement and the development of
parent leadership skills. Toward this end, during September 2005 we provided an opportunity for
parents to participate in an intensive 4-day workshop that focused on developing group presentation
skills, small-group facilitation skills, and collaborative teamwork. Parents also continue to develop
their reading and storytelling skills. To support our parent education curriculum, morning yoga
exercise classes were implemented, along with a curriculum that includes nutrition presentations.
In addition to regularly scheduled on-site training, staff also participated in numerous other
professional development activities, including monthly LAUSD workshops focused on special needs
topics such as language development, autism, and challenging behaviors. Faith Polk, Ph.D., Family
Literacy Support Network, provided a special two-day Desired Results Developmental Profile
(DRDP) training.
Please see table below documenting collaborator/community partners.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
112
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
To promote parent literacy.
To help parents become full partners in the education of their children.
To prepare children for success in regular school programs.
Develop parent leadership skills.
Enhance staff development to enable them to better meet the needs of special needs children and
their families.
Identify alternative source of funding for this Program
Performance Indicator 1.2: English-as-a-Second Language Acquisition
At least 50 percent of adult learners enrolled in ESL classes who: (1) pass the CASAS oral
screen; and (2) achieve a pretest scale score of 210 or below on the Comprehensive Adult
Student Assessment System (CASAS) Reading Test will demonstrate a five-point posttest
gain after a minimum of 100 hours of instruction.
At least 50 percent of adult learners enrolled in ESL classes who achieve a pretest scale
score of 211 to 240 on the CASAS Reading Test will demonstrate a three-point posttest gain
after a minimum of 100 hours of instruction.
Performance Indicator 1.4: Goal Attainment Postsecondary Education, Job Training Program,
Employment, Military Service
Each year, at least 50 percent of adults will meet their goals of postsecondary education,
employment, and entry into military or career advancement.
Performance Indicator 2.1: Reading/School Readiness Indicator for Ages Three to
Five Years Old (Does not include Children Entering Kindergarten in 2005)
For each reading readiness behavior measured with the DRDP (13 items) or DRDP+ (12
items), at least 80 percent of children in this age range will show growth in the reading/school
readiness skills after a minimum of 100 hours of early childhood education during the project
year.
Performance Indicator 2.2: Reading/School Readiness Indicator For Students Entering Kindergarten
Definition of Pre-Kindergarten (Pre-K): The term Pre-kindergarten (as used in this report) refers to
children ages four or five years who will be entering kindergarten in 2005.
For each reading readiness behavior measured with the DRDP, 80 percent of the Even Start
children entering kindergarten will demonstrate that they have mastered the behaviors/skills
necessary for transition to kindergarten after a minimum of 100 hours of early childhood
education during the project year.
Performance Indicator 2.3: School Attendance for Grades K-2
Eighty-five percent of the children enrolled in the Even Start program will attend at least 95
percent of possible school days from the date of enrollment in Even Start
Performance Indicator 2.4: Grade Level Promotion for Grades K-2
At least 75 percent of the Even Start children enrolled in kindergarten through grade two who
received academic support beyond the regular instructional program for a minimum of 100
hours will advance to the next grade level as reported by the child’s school records.
Performance Indicator 2.5: Reading and Math Content Standards Progress for Kindergarten
Through Grade Two
Each year, at least 75 percent of the Even Start children enrolled in kindergarten through
grade one who received academic support beyond the regular instructional program for a
minimum of 100 hours will meet grade level content standards in reading and mathematics as
measured by the school’s standards-aligned report cards.
Each year, at least 75 percent of the Even Start children enrolled in grade two who received
academic support beyond the regular instructional program for a minimum of 100 hours will
perform at the proficient level or above in reading and mathematics as measured by the
California Content Standards Test and at the 50th percentile or above as measured by the
CAT-6.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
113
Performance Indicator 3.1: Parents’ Support for Children’s Learning in the Home Environment
By the conclusion of each project year, 70 percent of parents who participated in a
minimum of 50 hours of family literacy instruction will report that they support their child’s
learning through adult reading and writing and having books in the home as measured by
the California-Even Start Performance Information Reporting System (CA-ESPIRS) Items
#1, #2, and #10.
Performance Indicator 3.2: Parents’ Role in Interactive Literacy Activities:
By the conclusion of each project year, 70 percent of parents who participated in a
minimum of 50 hours of family literacy instruction will report that they engage in interactive
literacy activities as demonstrated by parents 1) reading to child at least three times per
week, and 2) using interactive reading strategies as measured by the of the CA-ESPIRS item #3 and # 4.
Performance Indicator 3.3: Parents’ Role in Supporting Child’s Learning in Formal Educational
Settings
By the conclusion of each project year, 70 percent of the K-2 parents who participated in a
minimum of 50 hours of family literacy instruction will report on school activities as
measured by the CA-ESPIRS Survey- item #13: School.
Staff demonstrate increased ability to meet the needs of special needs children and their families.
Baseline
Intervention Strategy for
Achieving Goal
Identify potential alternative funding sources for the continuation of this program. Prepare and
submit grant proposals.
CHMC’s service area has the highest rate of low literacy (66%) in the county. Parents feel unable to
become full partners in the education of their children because they themselves are so poorly
educated. The common philosophy in the community has been to “wait until the child reaches
kindergarten” when the teacher will introduce the child to reading.
HSFC has had a grant-funded family literacy program since 1998. We continue to implement the
family literacy program based on the National Center for Family Literacy/Kenan model. The following
program enhancements were successfully integrated into the program this year: the development of
parent leadership skills, reading and storytelling skills, yoga, nutrition classes, and other activities
provided in collaboration with our community partners.
At the beginning of each year, program staff meets with the evaluator to go over the evaluation
design and the management plan. The management plan outlines the evaluation activities and data
to be collected during the year, persons responsible, and due dates. These activities include items
related to meeting the Even Start Performance Indicators, the annual self-study, as well as other
activities related to program needs and the local evaluation, including parent interviews, parent
satisfaction surveys, and Gesell developmental assessments for children. Intake forms are
completed for families upon enrollment, which include information on family demographics and goals.
Adults are pre-tested within the first 30 days of enrollment and children are assessed within the first
60 days. Adults are administered the CASAS reading as well as the LAUSD promotion tests which
measure reading, writing, listening, and oral language. Even Start staff conducts parent interviews
using the CA-ESPIRS instrument. Children ages 0-5 are observed and rated using the DRDP
instrument appropriate for their age and according to the DRDP schedule by their early childhood
classroom teachers. Post-testing for adults is ongoing every 100 instructional hours in reading and
at the end of the year in the other areas. Whenever possible, post-tests are administered to
participants at the time of exit. Participant attendance is reviewed weekly and entered monthly into a
database. Report cards, standardized test results, and attendance for school-age children are
obtained at the end of the year from their schools.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
114
Result FY 2008
The project served a total of 41 families (46 children ages 0-3, 9 children ages 4-5, 39 parents with
children 0-5). 100% of families were Hispanic/Latino. Spanish was the primary language of 95%,
with 5% of parents reporting an indigenous dialect as their primary language, and 63% of adult
participants were between the ages of 25 and 35 years of age. With regard to income, four of the 41
family’s income exceeded $19,000 gross per year
32% children aged 0-5 had special needs, including speech and language impairment, hearing
impairment including deafness, health impairment, gross motor delay, non categorical/developmental
delay, Down syndrome, and autism.
Program changes this year include: 1) increased the intensity of adult education (ESL) and Early
Childhood Education (ECE) instruction- increasing the hours of monthly ESL instruction to 60
hr/month and the hours of monthly ECE instruction to 72 hr/month. This increase is consistent with
California Department of Education-Even Start requirements as well as research data demonstrating
the benefits of high intensity ESL and ECE instruction. 2) added distance learning opportunities (ESL
and Parenting) to supplement ongoing center-based instruction. 3) implemented the Parent
Education Profile (PEP) to assist with assessing parenting education needs and in planning PCILA
activities. The PEP consists of four scales: Parent’s Support for Children in the Home Environment,
Parent’s Role in Interactive Literacy Activities, Parent’s Role in Supporting Child’s Learning in Formal
Education Settings, and Taking on the Parent Role
Our Parent Advisory Board is comprised of four elected parent representatives from each of the Early
Childhood Classrooms: one infant parent representative, one young toddler parent representative,
one older toddler parent representative and one preschool parent representative. This format has
served as an excellent process for preparing parents for leadership roles. It also has helped them
feel connected, valued, and respected within the program, as they see that their input is reflected in
the program’s group norms, field trips, special events, PCILA plans and incentives.
Our Family Literacy Program has been successful in achieving and supporting component integration
that includes each of the four areas of the program: Parent Education, Adult Education, PCILA and
Early Childhood Education. Home visits are conducted bi-weekly and serve to reinforce learning in
the home and as a “bridge” between the home and the center. We also continue to use a common
monthly theme to help integrate instruction and curriculum components, i.e., integrated planning for
daily ECE classroom activities, PCILA, home visit activities, and field trips. Program integration is
also supported through a weekly interdisciplinary meeting that includes the social services
coordinator, mental health coordinator, ESL/parent education instructor, ECE teachers, and the
program coordinator. Weekly meetings provide a forum for discussing parent and child
accomplishments, strengths, needs, barriers to participation, and needed resources. This results in a
more coordinated, focused approach to working with families. This year we also began using the
PEP to help better ensure that parenting education and PCILA activities are relevant to parent needs.
The ESL/Parent Education instructor, ECE teachers, and Program Coordinator were involved in
planning specific topics and lessons geared towards helping parents grow in the areas pertinent to
the four PEP scales
The other community partnership that was strengthened this year was the partnership with Central
Library Los Angeles. Our Family Literacy Program has traditionally taken families on library trips at
least once a month. This year the library and our program partnered in a new activity that involved
volunteer senior citizens reading aloud to children. This intergenerational activity was something that
both the seniors and the families enjoyed. Recently the Children’s Department Manager contacted
us hoping to include our families as part of a grant they received from Read to Me LA. We agreed to
have our monthly library visits coincide with their monthly preschool read aloud sessions from
September through December 2007. We were pleased to be involved in this series of literacy
activities in our community.
Major accomplishments included 1) maintaining full enrollment throughout the year; 2) achieving a
retention rate of 83%; 3) meeting the proposed goal for number of children served and exceeding the
goals for parents and families; and 4) achieving attendance rates that exceed First 5 requirements in
all four program components, i.e., ESL (76%), Parenting (77%), PCILA (75%), and ECE (76%).
Additionally 82% of parents achieved the CASAS indicator gain. Children have continued to
demonstrate strong developmental progress, with the greatest growth in the areas of literacy and
language. We were also able to successfully offset the decrease in PCILA hours – caused by the
increase in hours of ESL instruction – by adding a monthly library trip to the curriculum and twice
monthly home visits. The addition of Distance Learning was an additional enhancement to the
center-based Adult Education/ESL services that we have traditionally provided. One of the
unanticipated benefits that this enhancement brought to the family literacy program was the idea of
“learning as a family”. Of the 10 moms who participated in Distance Learning this year, 7 reported
watching the DVD and reviewing the written material with their partners. Many families reported that
they began setting time aside in the evenings and weekends to learn English together, in the
convenience of their home. The benefits have been many – parents learning English as a Second
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
115
Language; strengthening families as they share the love for learning; and parents modeling for their
young children a priority on learning together.
The successful implementation of the PEP is an additional program accomplishment. The family
literacy program used the PEP as an assessment and instructional tool for working with parents.
Use of the tool helped us to further integrate instruction, leading us to develop and implement lesson
plans that were meaningful and relevant in helping parents grow and achieve gains in these four
distinct areas.
Finally, we hosted a highly successful California Department of Education, Even Start on-site
monitoring review in February 2008. Final report stated, “Program to be commended for its
collaboration with partners. Program to be recommended as a model program of the State for other
Even Start Programs to visit and generate new ideas.”
The major challenge our family literacy program faced this year was the unexpected loss of state
Even Start funding, used to support family literacy services. Nonetheless, we remain committed to
providing comprehensive, high-quality family literacy services to families in our community. We are
actively seeking funding to sustain and grow family literacy services.
One of the major changes this program year was having a single instructor for both Adult Education
and Parent Education. HSFC is characterized by its emphasis on building strong relationships, trust,
and rapport in order to effectively impact on the lives of families. Having a single instructor for ESL
and Parent Education components of our program goes hand-in-hand with this overall agency
philosophy. Positive results have come from this single instructor approach. Trust and rapport
between teacher and participants has been strengthened and is reflected in parents’ willingness to
engage in more group activities and oral presentations and in their initiative to share their ideas.
39 adults participated in Adult Education; 480.31 mean hours attended; 76% attendance rate. 39
adults participated in parenting education; 65.37 mean hours attended; 77% attendance rate. 55
children participated in ECE; 389.25 mean hours attended; 76% attendance rate. 39 parents
participated in PCILA; 45 mean hours attended; 74.7% attendance rate.
Performance Indicators
Adult Education: All of the adult education performance indicators applicable to the participants were
achieved and exceeded. Adults from both our ESL beginning level group (78.6%) and
intermediate/advanced group (88.9%) have exceeded the CASAS reading performance indicator
standard for their level. Overall,82.6% of our ESL adult students attained the minimum gain on the
CASAS reading test for their level.
Child Education:
Children ages 0-3: Classroom teachers use the DRDP-R as one of the classroom instruments to
monitor children’s progress and for tailoring instruction and individualization. Children ages 0-3 were
administered the DRDP-R for infants/ Toddlers. All children with matched assessments made
progress in their developmental ratings.
Children ages 3-5: Classroom teachers use the DRDP-R as one of the classroom instruments to
monitor children’s progress and for tailoring instruction and individualization. Our program children
ages 3-5 showed progress on the DRDP-R items.
Children ages 0-5: Classroom teachers use the DRDP-R as one of the classroom instruments to
monitor children’s progress and for tailoring instruction and individualization. In addition to the
DRDP-R, program also administers the Revised Geselle Developmental Schedules annually. The
results are used to screen for appropriate developmental progress and possible developmental
delays. The results of this developmental screening are also used as a tool for individualization of
instruction for children. Home visitors and co-teachers use the recommendations given by the Child
Development/ Disabilities Coordinator as stated in the Geselle to support child in his/her
development. Children whose results indicate significant delays are referred to the Regional Center
or local school district, depending on child’s age.
Children ages 3-5 (entering K): We administer the PPVT-III and the PALS Upper-case Letter
Recognition tests to children who will be entering kindergarten. These are the assessments used by
Even Start to assess receptive language and letter recognition.. All of the children are English
Language Learners, assessed in English.
Retention: We have maintained a high retention rate for the year of 82%. In addition, among families
who have exited the program, the majority have transitioned from our program into full-time early
childhood education programs for children and employment or other training programs for adults.
Our data reflect families’ commitment to Family Literacy. Even under difficult economic times, most
families remained in the program for 6 months or longer. Of the 41 enrolled families, 78% remained
in the program for longer than 6 months and 51% of these families remained in the program for 12
months or longer. In fact, nearly one-third of parents have participated in the program for more than
2 years. This demonstrates the high value they place on their children’s education as well as on their
own English language acquisition and education. Attendance rates within each of the program
components provide further evidence of parental commitment and eagerness to achieve the goals
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
116
that they have set for themselves and their children.
Attendance: 39 adults participated in Adult Education; 292.9 mean hours attended; 76% attendance
rate. 39 adults participated in parenting education; 65.4 mean hours attended; 77% attendance rate.
55 children participated in ECE; 389.25 mean hours attended; 76% attendance rate. 39 parents
participated in PCILA; 44.7 mean hours attended; 74.65% attendance rate.
We have begun recognizing attendance achievements for families who achieve perfect or best
attendance each month and cumulative best attendance for the year. Every month we take a photo
of the family who achieved perfect or best attendance and the photo is posted in “The Wall of Fame”
for everyone to admire. This year, at our culmination celebration, the top three participants and their
families also were publicly recognized with a certificate of achievement as well as prizes that support
their good effort as students, such as back packs, dictionaries, and other essential school supplies.
Our Family Literacy Program has established written MOUs with 28 community agencies. The
following is a listing of those agencies that have provided significant support and ongoing assistance
with Family Literacy activities.
Museum of Contemporary Art: series of weekly art instructional activities and experiences
for parents and children including outings to MOCA. Program funded entirely by MOCA.
Children’s Nature Institute: provides interactive nature experiences, including field trips to a
nature site. Program funded by the Institute.
Book Ends: provides recycled books.
Motheread/Fatheread: a family reading program that promotes literacy. Program provides
children’s books, training, and technical assistance. Program funded by United Way.
The Outdoor Classroom Project: series of trainings and technical assistance to help staff
design, create, and enhance outdoor play space.
Emanuel Presbyterian Church: weekly yoga classes for all program parents to improve
emotional and physical health.
LAUSD/Abram Friedman Occupational Center: provides personnel to teach adult and
parent education classes.
WestEd: provides training and technical assistance.
Sonnenschein Nath and Rosenthal LLP: small donations for program and participants
Hospital’s Contribution / Program
Expense
Three grant proposals were submitted; two were funded ($50,000 from the Dwight Stuart Foundation
on 3/15/2007 and $188.367 from the Department of Education for Pre-Kinder and Family Literacy on
3/15/2007). Funding from the Department of Education for Even Start was denied.
Additional sources of funding are being identified and proposals submitted.
CHMC provides all the space for the HSFC, 1½ floors of Leavey Hall. SB 697 in-kind contribution
$123,700.
The Family Literacy Program is supported by $188,367 from First 5 LA and $50,000 from the Dwight
Stuart Foundation.
FY 2009
Goal 2009
2009 Objective
Measure/Indicator of Success
To promote parent literacy.
To help parents become full partners in the education of their children.
To prepare children for success in regular school programs.
Continue to develop parent leadership skills.
Enhance staff development to enable them to better meet the needs of special needs children and
their families.
Secure alternative source of funding for this Program.
Performance Indicator 1.2: English-as-a-Second Language Acquisition
At least 50 percent of adult learners enrolled in ESL classes who: (1) pass the CASAS oral
screen; and (2) achieve a pretest scale score of 210 or below on the Comprehensive Adult
Student Assessment System (CASAS) Reading Test will demonstrate a five-point posttest
gain after a minimum of 100 hours of instruction.
At least 50 percent of adult learners enrolled in ESL classes who achieve a pretest scale
score of 211 to 240 on the CASAS Reading Test will demonstrate a three-point posttest gain
after a minimum of 100 hours of instruction.
Performance Indicator 1.4: Goal Attainment Postsecondary Education, Job Training Program,
Employment, Military Service
Each year, at least 50 percent of adults will meet their goals of postsecondary education,
employment, and entry into military or career advancement.
Performance Indicator 2.1: Reading/School Readiness Indicator for Ages Three to
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
117
Five Years Old (Does not include Children Entering Kindergarten in 2005)
For each reading readiness behavior measured with the DRDP (13 items) or DRDP+ (12
items), at least 80 percent of children in this age range will show growth in the reading/school
readiness skills after a minimum of 100 hours of early childhood education during the project
year.
Performance Indicator 2.2: Reading/School Readiness Indicator For Students Entering Kindergarten
Definition of Pre-Kindergarten (Pre-K): The term Pre-kindergarten (as used in this report) refers to
children ages four or five years who will be entering kindergarten in 2005.
For each reading readiness behavior measured with the DRDP, 80 percent of the Even Start
children entering kindergarten will demonstrate that they have mastered the behaviors/skills
necessary for transition to kindergarten after a minimum of 100 hours of early childhood
education during the project year.
Performance Indicator 2.3: School Attendance for Grades K-2
Eighty-five percent of the children enrolled in the Even Start program will attend at least 95
percent of possible school days from the date of enrollment in Even Start
Performance Indicator 2.4: Grade Level Promotion for Grades K-2
At least 75 percent of the Even Start children enrolled in kindergarten through grade two who
received academic support beyond the regular instructional program for a minimum of 100
hours will advance to the next grade level as reported by the child’s school records.
Performance Indicator 2.5: Reading and Math Content Standards Progress for Kindergarten
Through Grade Two
Each year, at least 75 percent of the Even Start children enrolled in kindergarten through
grade one who received academic support beyond the regular instructional program for a
minimum of 100 hours will meet grade level content standards in reading and mathematics as
measured by the school’s standards-aligned report cards.
Each year, at least 75 percent of the Even Start children enrolled in grade two who received
academic support beyond the regular instructional program for a minimum of 100 hours will
perform at the proficient level or above in reading and mathematics as measured by the
California Content Standards Test and at the 50th percentile or above as measured by the
CAT-6.
Performance Indicator 3.1: Parents’ Support for Children’s Learning in the Home Environment
By the conclusion of each project year, 70 percent of parents who participated in a
minimum of 50 hours of family literacy instruction will report that they support their child’s
learning through adult reading and writing and having books in the home as measured by
the California-Even Start Performance Information Reporting System (CA-ESPIRS) Items
#1, #2, and #10.
Performance Indicator 3.2: Parents’ Role in Interactive Literacy Activities:
By the conclusion of each project year, 70 percent of parents who participated in a
minimum of 50 hours of family literacy instruction will report that they engage in interactive
literacy activities as demonstrated by parents 1) reading to child at least three times per
week, and 2) using interactive reading strategies as measured by the of the CA-ESPIRS item #3 and # 4.
Performance Indicator 3.3: Parents’ Role in Supporting Child’s Learning in Formal Educational
Settings
Baseline
By the conclusion of each project year, 70 percent of the K-2 parents who participated in a
minimum of 50 hours of family literacy instruction will report on school activities as
measured by the CA-ESPIRS Survey- item #13: School.
Staff demonstrate increased ability to meet the needs of special needs children and their families
CHMC’s service area continues to have the highest rates of low literacy in the county and high rates
of special needs children.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
118
Intervention Strategy for
Achieving Goal
Continue to implement the family literacy program based on the National Center for Family
Literacy/Kenan model.
Continue the development of parent leadership skills.
Ongoing training in early childhood education is key to supporting our work with infants and toddlers,
especially those with special needs. Training in this area will continue.
Prepare and submit multiple grant proposals in order to secure funding for the continuation of this
critical program.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
119
Health Ministry Program
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2 Health Promotion/Disease Prevention
Priority Area 3 Disease Management
Priority Area 4
Priority Area 5
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
Lack of access to health care, especially preventive care and health screenings.
Lower rates of hospitalization and greater use of preventive health services are associated with a
regular source of care or a medical home. Focus groups and providers report that for many of the
community’s residents, the local community clinic is commonly a regular source of care. Data from
the previous Los Angeles County Health Survey (LAC/DHS, 2002) found that a quarter of county
residents do not have a regular health care provider. People are less likely to have a regular source
of care if uninsured (49%) compared to those with MediCal (20%), private insurance (16%) and
Medicare (5%). Latinos and Asian/Pacific Islanders had the highest proportion of persons reporting
no regular source of care (30%) while African Americans and Whites had the same rate (17%).
Current LACHS data demonstrate some improvements though ethnic disparities still exist. In L.A.
County, 19% reported not having a regular source of care (LAC/DHS, 2004b), 15% above the
Healthy People 2010 objective. Latinos (27%) and Asian/Pacific Islanders (22%) still have higher
rates than Whites (12%) or African Americans. Service Planning Area (SPA) comparisons found that
SPA 4 had significantly more residents without a regular source of care (28%) with SPA 6 close
behind (21%; LAC/DHS, 2004b).
“Many people, both with and without insurance, don’t obtain preventive
care, but only seek care when they are sick. Although awareness of the
importance of preventive care and access are important factors, even
some people with awareness and access don’t seek preventive care. Lowincome people with no coverage generally are not aware of the services
and do not obtain preventive care.” – Service Provider
Community residents have some understanding about how to care for themselves, though they may
not be pursuing preventive health care measures as a usual strategy. Some focus group participants
reported good sleep, nutrition, and exercise are ways to care for themselves and their family. A few
reported that regular check-ups with their physician to monitor a chronic illness, like hypertension,
are important. Despite these reports, providers and community health promoters stated that often
community residents do not seek preventive care from their doctor and only appear for services
when they or a member of their family is sick.
Screening for a variety of cancers and early detection can dramatically increase survival rates.
Knowledge about the importance of screenings and access to them are important in keeping the
community healthy. As with other health conditions, having insurance increases the likelihood of
using related health services. Data from the California Health Interview Survey found that those
using MediCal are more likely to receive a cancer screening than uninsured Californians (Babey, et.
al, 2003). Many residents are not aware of free or low-cost screening programs for cervical, breast,
and prostate cancer.
Chronic diseases continue to be leading causes of premature death and disability in Los Angeles
County and if unmanaged will affect quality of life. To manage a chronic disease it is imperative that
the afflicted person knows how to manage their illness. Focus group participants reported common
chronic illnesses in their community include asthma, allergies, heart disease, high cholesterol,
hypertension and diabetes. Community residents and providers alike reported needing more handson education on how to manage chronic diseases. Educational materials were viewed as an
important component of health education, but because of various language needs and literacy levels,
oral presentations and workshops were identified as possible educational methods as well.
Domestic violence is the single leading cause of injury to women between 15 and 44 years old (Los
Angeles Police Department, n.d.(a)). Nationally, health-related costs of domestic violence are $8.5
billion (Centers for Disease Control and Prevention, 2003). Almost a third of African American
women and a quarter of White women experience domestic violence in their lifetime. In the City of
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
120
Program Description
Los Angeles, 70% of all police calls for service are related to domestic violence, and domestic
violence is the number one public safety issue for females in the city (Los Angeles Police
Commission, 2004). There are numerous health effects resulting from domestic violence. Physical
injuries including bruising, abdominal injuries, fractures, and ocular damage may result in chronic
pain, reduced physical functioning, disability, and death (CDC, 2004b). Women who are battered
suffer more miscarriages and are likely to give birth to babies with low birthweight (LAPD, n.d.(a)).
There are also serious psychological consequences including depression, anxiety, poor self-esteem
and suicidal thoughts (CDC, 2004b). Providers identified domestic violence as a serious concern
and potential barrier to accessing health care.
CHMC sponsors parish nurses and community health promoters (CHPs) at 18 local schools and
churches to provide health screenings, immunizations, health education, and information and referral
services. Each site selects their health education classes from a menu of choices offered annually.
Health Ministry staff also participate in local health fairs.
CHPs together with a volunteer lay leader conduct Chronic Disease Self-Management Program
(CDSMP) Workshops at Health Ministry sites. This 6-week intervention is based on self-efficacy
theory and emphasizes problem solving, decision-making, and confidence building. Two bilingual,
indigenous leaders, at least one of who has a chronic disease, lead the 6-week, small group
intervention using a highly structured manual. Subjects covered include: techniques to deal with
problems such as frustration, fatigue, pain, and isolation; appropriate exercise techniques for
maintaining and improving strength, flexibility, and endurance; appropriate use of medications;
communicating effectively with family, friends, and health professionals; nutrition; and making
informed treatment decisions. The sessions are highly participatory. Mutual support and success
build patients’ confidence in their ability to manage their health and maintain active and fulfilling lives.
The goal of the Domestic Violence Prevention Program offered through our Health Ministry Program
is to provide community members with information, support, and resources to help them achieve and
maintain healthy relationships. Single-session prevention education classes (I½ hr long) cover topics
such as the dynamics of domestic violence, power and control, impact on children, and safety
planning. The in-depth four-week discussion group titled “Building Healthy Relationships” covers
self-esteem, healthy communication, and resolving family conflict.
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
Baseline
Intervention Strategy for
Achieving Goal
Result FY 2008
Eliminate health disparities in CHMC’s service area.
Promote healthy communities by decreasing domestic violence.
Increase in awareness, knowledge, attitudes, and skill development/acquisition regarding high
prevalence health conditions, especially chronic conditions.
Increase in health screens for chronic conditions.
Increase the ability of people with chronic conditions to manage their health and maintain active and
fulfilling lives.
Provide participants of the Domestic Violence Prevention Program with knowledge and tools to help
them maintain healthy, violence-free relationships and to recognize what constitutes domestic
violence.
The following factors contribute to lack of access to health education, health screenings, and
referrals to regular source of health care: high rates of uninsured adults, highest rates of low literacy
in Los Angeles County, 44% of residents are foreign born, median household income ~ $20,000 less
than county median.
Although clinics and physicians attempt to provide disease-specific education on various chronic
conditions, low-income, often uninsured, community residents do not have access to evidence-based
self-management education. They struggle with their chronic conditions, often becoming very
depressed and increasingly isolated from family and friends. Their quality of life spirals downward as
does their health.
The prevalence of domestic violence remains very high in our service area. Provision of prevention
and intervention services here is complicated by the fact that a large proportion of residents are lowincome, have low levels of literacy, speak little or no English, are recent immigrants, and may be
undocumented.
Provide free health education classes in English and Spanish at Health Ministry sites on a variety of
topics. Conduct pre- and post-tests to assess knowledge acquisition.
Provide health screenings for diabetes, hypercholesterolemia, hypertension, tuberculosis, anemia,
obesity, and depression.
Provide referrals to local primary care clinics when screening tests are positive.
Provide flu shots.
Participate in health fairs.
Provide Chronic Disease Self-Management Program workshops.
Provide single-session prevention classes on domestic violence and 4-week discussion groups on
“Building Healthy Relationships.”
Please see the table documenting classes/participants following this Program Digest.
We added a number of screening sites this year; we are currently doing health screens at over 29
sites.
95% of class participants completed both pre-and post-tests. Of those, 90% demonstrated increased
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
121
Hospital’s Contribution / Program
Expense
knowledge.
91% of CDSMP participants completed the series of 6 weekly workshops.
Please see the table documenting health screens below.
Please see table documenting number of referrals made.
400 flu shots were given.
Participated in 5 health fairs.
A satisfaction survey of the “Building Healthy Relationships” groups demonstrated that 94% of
participants rated the overall content to be excellent and 100% participated in all 4 weekly sessions.
The hospital contributed the majority of the operating budget for this program and provided office
space and office equipment for staff.
The annual budget is $248,000 for the Health Ministry Program.
.
FY 2009
Goal 2009
2009 Objective
Measure/Indicator of Success
Baseline
Intervention Strategy for
Achieving Goal
Eliminate health disparities in CHMC’s service area.
Promote healthy communities by decreasing domestic violence.
Increase in awareness, knowledge, attitudes, and skill development/acquisition re high prevalence
health conditions, especially chronic conditions.
Increase in health screens for chronic conditions.
Increase the ability of people with chronic conditions to manage their health and maintain active and
fulfilling lives.
Provide participants of the Domestic Violence Prevention Program with knowledge and tools to help
them maintain healthy, violence-free relationships and to recognize what constitutes domestic
violence
The lack of access to health education, health screenings, and regular source of care is increasing
due to closure of county clinics and some community clinics. The prevalence of uninsured people
continues to increase in our service area. The prevalence of people living with chronic conditions
continues to increase in our service area. The prevalence of domestic violence in our service area
remains high.
Increase outreach to churches serving African Americans in our service area.
Continue intervention strategy used in FY08 detailed above.
Health Ministry Classes/Workshops FY 08
Topic
Arthritis
Asthma
Basic First Aid
Building Healthy Relationships
Blood Pressure
Cancer
CDSMP
Child Abuse
Cholesterol
Communication Skills
Depression
Diabetes "Are You at Risk"
Domestic Violence
Emergency Preparedness
Immunizations
Healthy Habits Before Pregnancy
HIV/AIDS
Home Safety
Menopause
Nutrition
Oral Hygiene
Pedestrian Safety
Personal Hygiene
# of Classes
# of Participants
5
15
18
10 four-week sessions (40 classes)
18
10
12 six-week sessions (36 classes)
11
3
16
6
17
0
15
1
8
8
6
2
32
30
9
2
105
217
212
128
365
122
157
163
78
170
94
206
0
168
6
112
109
60
14
364
305
74
23
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
122
Topic
# of Classes
# of Participants
9
10
4
8
10
1
350
122
114
36
74
98
4
3700
5
180
Raising a Healthy Eater
Self Esteem
Sexuality
STD's
Stress Management
Tuberculosis
Total Classes/Participants
Health Fairs
Referrals from HM Classes/Workshops FY 08
Referred to:
Diabetes Program
Comm. Dental Part/Low Cost Dental
Chronic Disease Self-Man. Program
Domestic Violence Prevention Program
Depression
Health Screens FY08
Blood Pressure
Glucose
Cholesterol
Tuberculosis
Height/Weight/Body Mass Index
Hemoglobin
Influenza Vaccines
# Referred
10
20
20
15
5
# Screened
# Referred
2246
1847
1178
193
390
341
400
195
136
160
22
138
15
0
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
123
Healthy Eating Lifestyle Program (HELP)
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2 Health Promotion/Disease Prevention
Priority Area 3
Priority Area 4
Priority Area 5
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
Los Angeles County has roughly the same age-adjusted rate (19.8 per 100) of obesity among adults
as the State (19.1; California Department of Health Services, 2004). Approximately 20% of all adults
in the county are obese (Body Mass Index > or = 30). This is above the Healthy People 2010
objective of 15%. The National Institutes of Health report that obesity can place persons at risk for
chronic illness and death. Obesity and being overweight increases the risk of hypertension, type 2
diabetes, coronary heart disease, stroke, osteoarthritis, and breast, prostate, and colon cancers.
National statistics suggest some ethnic disparities in the rates of obesity in children and adults.
About 23% of Latino children and teenagers between 6 and 19 years are overweight compared to
15% of other non-Latino children (Vida Activa, 2004). For Latino adults, approximately 74% are
overweight or obese while national rates for all adults is about 65%.
Program Description
Over the last 20 years in California, the prevalence of overweight children has doubled and in
adolescents, the rate has tripled (California Department of Health Services, 2004). In Los Angeles
County, it is estimated that 21% of 5th, 7th and 9th grade students are overweight and that another
19% are at risk of becoming overweight. Also, in the state a third of Latino children are overweight,
and Latino children have the highest prevalence of obesity in Los Angeles County (Childhood
Obesity Brain Trust, 2004).
In 2002, the Chronic Disease Management Consortium (CHMC, Huntington Memorial Hospital,
Childrens Hospital Los Angeles, and the National Health Foundation) received a planning grant from
the Good Hope Medical Foundation to address the challenging problem of pediatric obesity. The
Consortium decided to attempt to intervene before children reach adolescence in order to prevent the
most long-term morbidity. In 2003 the Consortium, together with a new member, Harbor-UCLA
Medical Center, received a multi-year grant from UniHealth Foundation for HELP. As the name
implies, the primary goal of HELP is to help overweight children aged 5-12 years and their families
adopt healthier eating habits and increase physical activity. The emphasis is on long-term lifestyle
changes (making better food choices, integrating activity into their every day lives, decreasing
screen-time to < 2 hrs/d), rather than short-term diets.
The HELP curriculum was developed by dieticians from the 4 collaborating hospitals, led by CHMC’s
dietician, Coralyn Andres Taylor, MPH, RD, CHES. Each module is highly interactive so that
program participants are able to both learn and apply the facts, principles, and concepts being
taught. The Olympic Food Guide is a tool that was developed to help participants make healthier
food choices. Most people recall seeing winners of the Olympics standing on a platform to receive
their medals. Our food guide is divided into gold, silver, and bronze categories and the bottom or
lowest category is the brick that represents the ground the platform was on. Foods belonging in the
Gold category are packed with nutrients (vitamins, minerals, fiber, water, carbohydrates, and
proteins) and are relatively low in fat and calories. Foods in the Silver group also contain many
nutrients but they have slightly more calories. Foods in the Bronze group have more of their calories
coming from fats and sugars than foods in the Silver and Gold groups. Foods in the Brick group are
mainly fat and sugar. They have many calories per bite and fewer vitamins or minerals. To review
and reinforce this concept, at the second workshop families are given a variety of food models. Each
family determines which category each food belongs to and the child races up to put it into the right
bucket!
CHMC’s community health promoters provide outreach education about pediatric obesity at local
schools, churches, community based organizations, clinics, and doctors’ offices and seek referrals of
overweight children aged 5-12 years. In addition, Dr. M. Lynn Yonekura makes quarterly
presentations to new medical staff members at CHMC informing them of the availability of HELP and
seeking referrals. Potential participants and their parents complete an intake process that includes a
health screen as well as activity and nutrition assessments. Each child and his/her primary caretaker
participates in a series of five weekly workshops (see grid below) conducted at a convenient site in
the community. The majority of our workshops take place at The Salvation Army Red Shield Youth
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
124
and Community Center in Pico-Union. The Center offers a full range of exercise choices including
aerobics, free weights, soccer, basketball, karate, swimming, ballet, and drill team Families receive
free yearlong membership at the Center for completing the five workshop series. Families may also
participate in weekly support group meetings facilitated by a social worker to share success stories
and problem solve barriers to their new lifestyle changes. Six months after completing the workshop
series, participants reconvene for the sixth workshop and a reassessment of their health status and
activity and nutrition assessments.
All data are entered into a web-based system housed at National Health Foundation, the program
evaluator.
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
Baseline
Intervention Strategy for
Achieving Goal
Help overweight children aged 5-12 years, living in CHMC’s service area, and their families adopt
healthier eating habits and increase physical activity.
Each of the four hospitals will complete the recruitment of 2,100 target children and parents.
Each of the four hospitals will complete the screening of 720 target children and parents.
Each of the four hospitals will complete the assessment of 720 target children and parents.
Each of the four hospitals will complete the enrollment of 384 target children and parents.
240 target children and parents from each of the four hospitals will participate in the series of five
workshops.
120 target children and parents from each of the four hospitals will participate in the 6-month followup workshop and assessment.
Clinical measurable objectives:
Reduced weight or weight velocities; BMI < 85% for age in children
Normal cholesterol levels
Normal lipid levels (if initial screening cholesterol > 200)
Reduced % of body fat
Improved exercise tolerance
Self-reported:
Improved food selection
Increased exercise frequency: goal 20 minutes, 3 times/wk
Reduced TV viewing time: goal < 2 hr/d
Decrease in fast food purchases: goal < 2 times/wk
Improved exercise and nutrition self-efficacy
The Executive Committee will prepare and submit a letter of inquiry to UniHealth Foundation for the
preparation of HELP curriculum and toolkit for publication and for the development of four seasonal
modules.
The Executive Committee will prepare and submit a letter of inquiry to UniHealth Foundation and
other foundations for the continuation and expansion of HELP at the four original hospital sites.
During the past 3 decades, the childhood obesity rate has more than doubled in preschool children
aged 2-5 years and adolescents aged 12-19 years, and more than tripled among children 6-11 years.
These figures are particularly alarming because of the health problems associated with children
being overweight. Already, it is adversely affecting children’s health as overweight youngsters
develop disorders once found only in adults, such as type 2 diabetes. Moreover, 80% of overweight
adolescents will grow up to be overweight or obese adults, at risk for heart disease, stroke, diabetes,
osteoarthritis, and several types of cancer. In fact, as Professor David Katz, a preventive medicine
specialist at Yale University School of Medicine, states “our children are projected to have a shorter
life expectancy than their parents . . . they are being more harmed by poor diet than by exposure to
alcohol, drugs, and tobacco combined.”
There are a limited number of programs addressing pediatric obesity in our service area and most
require that the child have health insurance to pay for the program and have long wait-lists. HELP,
on the other hand, is free to participants and we make every effort to promptly enroll new families.
Local physicians continued to eagerly refer children to HELP. Participant recruitment, screening,
and assessment continued. We continued to offer HELP workshops primarily at the Red Shield
Youth and Community Center in the heart of Pico-Union. Red Shield rewards graduating families with
a free yearlong family membership so that they can continue to exercise.
Result FY 2008
The final data report for HELP was run on 8/22/07. A total of 1135 target children and 991 parents
registered for HELP between 10/1/05 and 8/22/07. The original goal was for 60 families to completed
HELP from each of the four sites. We greatly exceeded this goal at ¾ sites. A total of 1130 modules
were conducted, 35.5% in English and 64.5% bilingual, Spanish/English. The retention rate was
58% for modules 1-5 and 51% for modules 1-6. The national benchmark for retention in similar
programs is ~40%. The retention rate was higher for bilingual workshops vs. English (72.5% vs. 34%
for #1-5; 65% vs. 29% for #1-6).
458 children and 402 adults completed the program.
12% of the children were aged 5-6 years, 38% were aged 7-9 years, 43% were aged 10-12 years
and 7% were aged 13-16 years. 50% were boys and 50% were girls. 81% were Hispanic, 7%
Caucasian, 4.8% African American, 1.5% Asian, and 2.2% mixed. 8.8% of the children were
overweight and 81% were obese at the beginning of the program. 87.5% of the adults were mothers,
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
125
8.3% were fathers, 2% guardians, 1% grandparents and 0.3% aunts or uncles of target children. 91%
of adult participants were female. 80% of adults were Hispanic, 7.9% Caucasian, 6% African
American, and 2% Asian. 27% of the adults were overweight and 50% were obese.
69% of the target children improved their nutrition scores, 73.5% improved their fitness scores, and
92% decreased the amount of time they spent watching television. By program completion, 77% of
children were watching TV < 2 hrs/day.
53% of the adults lost weight and 1.1% lost > 10% of their body weight. 61% of adults significantly
improved their nutrition scores and 79% improved their fitness scores. Moreover, 54% of adults
reduced their BMI.
After controlling for demographic differences, HELP’s paraprofessional-led groups yielded greater
pediatric BMI z-score reductions than professional-led groups. Paraprofessional-led group z-score
reduction = -0.20 (S.E. 0.023); professional-led group z-score reduction = -0.09 (S.E. 0.018);
paraprofessional – professional difference = -0.11 ( S.E. 0.036) Improved nutrition behaviors
predicted BMI z-score reduction in paraprofessional groups after controlling for individual-level
heterogeneity.
Only 115 participants attended support groups run by social worker.
HELP was presented at two professional meetings this year.
The Consortium obtained funding from the UniHealth Foundation to prepare the HELP curriculum
and toolkit for publication. All curricular materials were reviewed and edited by the Executive
Committee prior to being sent to the graphic artist. The replication toolkit is now ready for
dissemination. Hospital Association of Southern California is very interested in having its member
hospitals replicate this program.
Last year the Consortium obtained funding from the UniHealth Foundation to develop and pilot
quarterly seasonal update classes for program graduates. These classes focused on season fresh
fruits and vegetables and healthy holiday menus and family activities. 69 children and 59 adults
attended at least one of these Enhanced HELP workshops. Interestingly, 56% of adults who attended
Enhanced HELP had lost 1-10% of their initial body weight and 2.78% had lost > 10% of their body
weight, suggesting that these were some of the more motivated clients seeking additional information
to assist them in maintaining a healthy lifestyle.
HELP continued to be offered using a no-cost extension granted by the UniHealth Foundation.
CHMC will thus be able to continue offering HELP until May 2008. LA Care would like to contract
with us so we can continue to offer HELP to children covered by Medi-Cal, Healthy Families, and
Healthy Kids.
Hospital’s Contribution / Program
Expense
CHMC provides office space and office equipment for program staff.
CHMC’s two-year budget for HELP is $991,103. This includes the facilitation/evaluation costs of the
National Health Foundation - $370,030. This project was funded by a grant from UniHealth
Foundation. Our no-cost extension will allow us to continue this program until May 2008.
Goal 2009
Help overweight children aged 5-12 years and their families adopt healthier eating habits and
increase physical activity.
Present program results at a major pediatric meeting and publish results in a peer-reviewed journal.
Each hospital will seek funding to continue this successful program beyond May 2008.
CHMC will obtain continuation funding from a variety of sources.
CHMC will sign a contract with LA Care.
Clinical measurable objectives:
Reduced weight or weight velocities; BMI < 85% for age in children
Normal cholesterol levels
Normal lipid levels (if initial screening cholesterol > 200)
Reduced % of body fat
Improved exercise tolerance
Self-reported:
Improved food selection
Increased exercise frequency: goal 20 minutes, 3 times/wk
Reduced TV viewing time: goal < 2 hr/d
Decrease in fast food purchases: goal < 2 times/wk
Improved exercise and nutrition self-efficacy
FY 2009
2009 Objective
Measure/Indicator of Success
Baseline
Intervention Strategy for
Achieving Goal
Recruitment is picking up momentum as more physicians/clinics learn about the availability of HELP.
There is increased awareness in the community about the impact of pediatric obesity on long-term
health and the need to address this problem.
Monitor and report measurable objectives.
Publication committee will draft article for publication in a peer-reviewed journal.
Each hospital will seek funding for continuation of this successful program.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
126
Para Su Salud
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Program Description
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2
Priority Area 3
Priority Area 4 Health Insurance
Priority Area 5
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
A number of variables influence a person’s ability to access health care, that is, to obtain care when
they want it and need it. In previous needs assessments, significant barriers to accessing health
care were identified. Many of these barriers persist. Because the current health care system
depends largely on insurance for compensation, whether or not one has insurance plays a large part
in facilitating and limiting access to care.
Reasons that some participants did not have health insurance included lack of eligibility (e.g., too
young for Medicare), inability to afford private insurance, unemployment, or lack of legal resident
status. Among those respondents in the Patient Assessment Survey II (Diamant, 2003) that were
uninsured and foreign-born, 29% of them were afraid that applying for MediCal would affect whether
they could become a citizen. Similar to prior assessments, focus group participants and key
informants report easier access to health insurance and health services for children than adults.
According to the 2002-2003 Los Angeles County Health Survey (LAC/DHS, 2003a) 26% of adults
between 18 and 64 years of age had no health insurance. Previous estimates report nearly 30% of
L.A. County residents as uninsured (Wulsin, 2000). Latinos have the highest rate of uninsured nonelderly adults (39.8%) compared to other ethnic groups. Service Planning Areas (SPAs) 4 and 6
have the highest proportion of uninsured adults (37.6% and 36.4%, respectively). Families USA
(2001) reported that the uninsured with chronic health conditions are more likely to go without
medications that are important for maintaining health when compared to insured persons with similar
conditions. In the previous LACHS (LAC/DHS, 2002a), it was estimated that 20% of children were
uninsured, with 33% enrolled in MediCal/Healthy Families and 47% privately insured. Also, Latino
children were disproportionately represented among the uninsured (29%) when compared to
Asian/Pacific Islanders (12%), Whites (8%) and African Americans (7%). Estimates from the most
recent survey (LAC/DHS, 2003a) demonstrate some improvement in the proportion insured. Nine out
of ten children have some form of insurance in Los Angeles County. Comparisons of SPAs found
that SPA 4 has the second highest rate of uninsured children across the SPAs.
In order to increase access to health care for low-income, uninsured families living in CHMC’s
service area, CHMC obtained funding from the Los Angeles County Department of Health Services
to establish the Para Su Salud Program in 2002. Six full-time Community Health Access Specialists
(CHASs) who are bilingual in English and Spanish, bicultural and trained as Certified Assistors,
provide information and counseling services to families regarding low-cost insurance options at a
variety of sites including the hospital, various clinics, health fairs, and throughout the community.
They conduct enrollment activities (intake and enrollment, enrollment verification, enrollment followup and troubleshooting) utilizing DHS approved forms. All data are entered into DHS data system
utilizing appropriate codes. The CHASs also conduct redetermination assistance and retention
contacts/verification.
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
Increase access to health care by assisting children and their families in Los Angeles County to
enroll in health coverage programs and utilize and retain these benefits.
Successfully engage a minimum of 7,500 of the target population in an outreach contact: SPA 4
3,750 and SPA 6 3,750.
Complete applications for a minimum of 3,500 clients for Healthy Kids, Medi-Cal, Healthy Families,
Kaiser Cares for Kids 1 or 2, Access for Infants and Mothers, or California Kids: SPA 4 1,750 and
SPA 6 1,750. CHMC will provide clients with referrals to appropriate health programs or health
agencies.
Investigate enrollment status within three months of application completion date on 100% of clients
for whom agency assisted with or facilitated applications.
Confirm enrollment of 75% of client applications assisted with or facilitated by CHMC.
Provide ongoing assistance to 2,500 clients experiencing problems with enrollment, utilizing benefits,
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
127
or retention: SPA 4 1,250 and SPA 6 1,250.
Offer redetermination assistance at 11-12 months to 75% of clients whose applications were assisted
or facilitated by CHMC.
Provide redetermination assistance to clients who submitted their original application elsewhere, but
have requested redetermination assistance from CHMC.
Have a minimum 75% retention rate at 14 months for a sample of clients who submitted applications
and were confirmed enrolled.
Enter data on program participants into DHS’s web-based data system to monitor, facilitate, and
evaluate health insurance enrollment and retention.
Ensure that 100% of enrollment staff, including staff at subcontracting agencies, are fully trained to
provide outreach, enrollment, utilization and retention services and all new staff are fully trained
within 30 days of their start date.
Participate in a minimum of 10 of the monthly contractor meetings.
Participate in 100% of the outreach, enrollment utilization and retention required evaluation activities.
Conduct 100% of Quality Improvement Plan (QIP) activities.
Baseline
Intervention Strategy for
Achieving Goal
Result FY 2008
Ensure that 100% of funded staff participate in the Medi-Cal Administrative Activities (MAA)
reimbursement program.
There remains a high rate of uninsured people in our service area. Due to a recent initiative funded
by First 5 LA, LA Care Foundation and many other foundations, all children aged 0-18 living at or
below 300% FPL in Los Angeles County are now eligible for some form of health insurance
regardless of documentation status. Many people are not aware of this new initiative.
Implement the Quality Improvement Plan in order to achieve targets specified in contract.
Laptop computers will be purchased so staff can complete applications in the field.
From their outreach contracts, staff successfully completed applications for 4629 clients, 132% of
goal of 3500. 27 were submitted to AIM, 1426 for Emergency Medi-Cal, 320 for HF-Healthy Kids, 77
for HK-Healthy Kids,39 for KPCHP-Kaiser Permanente Children’s Health Plan, 2695 for MC-MediCal and 45 for MSOC-Medi-Cal Share of Cost.
653 individuals were referred to various other health programs/agencies.
In terms of the demographic profiles of the individuals for whom applications were submitted: 25
White, 4382 Hispanic, 200 African American, 9 Filipino, 1 Amerasian, 2 Cambodian, 2 Asian Indian,
and 8 Other. 1726 were male and 2901 were female. 1618 were less than 1 yr old, 488 were ages 15 yr, 707 were ages 6-17 yr, 387 were ages 18-21 yr, 1429 were 22 or older.
1051 lived in SPA 4 and 2960 lived in SPA 6; therefore 4011 lived in SPA 4/6, 115% of our minimum
goal of 3500 from SPA 4/6.
80.4% of AC1 client applications had confirmed enrollment. 93.6% of AC2 client applications had
confirmed enrollment. 85.43% of AC1/AC2 client applications had confirmed enrollment.
CHMC investigated enrollment status within three months of application completion date on 100% of
clients for whom we assisted with or facilitated applications.
CHMC provided ongoing assistance to 2102 clients experiencing problems with enrollment, utilization
benefits, or retention. This program does such a thorough job initially that problems aren’t
experienced very often.
CHMC attempted to offer redetermination assistance at 11-12 months to 95.89% of clients whose
applications were assisted or facilitated by us and were confirmed enrolled. 82.92% were
successfully contacted. 80.96% of clients were still enrolled at 11-12 months.
CHMC provided redetermination assistance to 36 clients who submitted their original application
elsewhere, but requested our assistance with redetermination.
Hospital’s Contribution / Program
Expense
CHMC provides office space and office equipment for program staff.
The total program budget is $347,858. The Los Angeles County Department of Health Services
through its Children’s Health Outreach Initiative (CHOI) funds this program.
Goal 2009
Increase access to health care by assisting children and families in Los Angeles County to enroll in
health coverage programs and utilize and retain these benefits.
Same as for FY08
FY 2009
2009 Objective
Measure/Indicator of Success
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
128
Baseline
Intervention Strategy for
Achieving Goal
Since 44.1% of residents in our service area are foreign born and since this is a fairly transient
population, there will always be a need to inform new residents of the available low-cost insurance
options.
In order to confirm enrollment for at least 75% of client applications, the program director and staff
will regularly check the status of this objective by monitoring the CHOI Data System and its “monthly
detailed report” section to ensure that all calls and enrollment confirmations are being attempted and
competed. Staff will continue to identify resources that increase their confirmations, i.e., health plan
representatives, state program representative, our Medi-Syn program, AEVS/MEDS, and other
informational programs.
Staff will document all calls attempted when trying to verify enrollments. This will be continuously
monitored and evaluated.
Staff will diligently try to provide redetermination assistance to 75% of clients whose applications
were assisted or facilitated and were confirmed enrolled. This will remain a challenge due to the fact
that families often change addresses/phone numbers.
.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
129
Hope Street Family Center School Readiness Program
Hospital CB Priority Areas
Program Emphasis
Link to Community Needs
Assessment
Program Description
Please add the Hospital Priority Areas identified in the Community Needs Assessment for your
hospital here
Priority Area 1
Priority Area 2
Priority Area 3
Priority Area 4
Priority Area 5 Healthy Communities
Please select the emphasis of this program from the options below:
Disproportionate Unmet Health-Related Needs
Primary Prevention
Seamless Continuum of Care
Build Community Capacity
Collaborative Governance
“Literacy skills predict an individual’s health status more strongly than age, income, employment
status, education level, and racial or ethnic group, according to an analysis of the research by the
nonprofit organization Partnership for Clear Health Communication” (Wilson, 2003, pg. 875).
Literacy skills can directly affects a patient’s ability to follow physician instructions, take medication
as prescribed, understand how to prevent disease and, self-manage and understand their rights
(Wilson, 2003; California Healthline, 2004; Institute of Medicine, 2004). Illiteracy affects patients’
ability to access care, in particular because of difficulties completing application forms for insurance
coverage or reading an appointment card. Most significant of all, it increases the chances of dying of
chronic or communicable diseases. A higher percentage of adults in Los Angeles County (27%) are
estimated to be at the lowest literacy proficiency level than for the state (19%) or the U.S. (20%).
Moreover, CHMC’s service area has the highest rate of low literacy (66%) in the county. The
greatest need for literacy services is for younger adults, particularly Latino and Asian/Pacific Islander
populations. Disability is also correlated with lower literacy scores; CHMC’s service area has
disability rates well above the county average of 9%: Downtown L.A. 11%, South Central 14%.
Almost without exception, the highest levels of Limited English Proficiency (LEP) are the lowest
literacy areas in the county. Every low-literacy area also had an above average proportion of recent
immigrants. Moreover, residents of the lowest literacy areas show low levels of educational
attainment. While the county average for education less than 9th grade is 14%, in the low literacy
areas 24-40% of residents have less than a 9th grade education.
The Hope Street Family Center (HSFC) at California Hospital Medical Center has been providing
school readiness services to families and schools in the Pico-Union/Westlake and central city
neighborhoods of downtown Los Angeles since 1992. Together the HSFC Early Childhood Center
(ECC) and Child Development Center (CDC) comprise the School Readiness Program that serves
80 children, ages 0-5 years, and their families.
The HSFC School Readiness service area covers a 16-square-mile radius in the heart of Los
Angeles. Service boundaries are Third Street to the north, Central Avenue to the east, Vernon
avenue to the south, and Western avenue to the west. A number of distinct neighborhoods are found
in the area, including downtown, Pico Union/Westlake, Koreatown, Adams/Normandie, University,
and Hoover. According to the 2000 Census, the target area has 664,188 residents, of which 62,563
residents are children four years of age or younger.
The primary target population for School Readiness services is low-income, two-parent Latino
families who are relatively recent immigrants. The target population experiences a significant lack of
resources (income, education, training, community supports) that place them at high risk for a variety
of health and social problems (developmental disabilities, acute and chronic illness, substance
abuse, domestic violence, substandard housing, and homelessness.).
The Early Childhood and Child Development Centers are located approximately one mile apart.
Housed on the campus of California Hospital Medical Center, the Child Development Center is colocated with a number of health, mental health, family literacy, child welfare, and after-school
programs. In contrast, the Early Childhood Center is located in a residential area in a large multi-use
building owned by the Angelica Evangelical Lutheran Church. The church serves as a hub for the
surrounding community, providing such services as congregate meals for seniors and emergency
food and clothing as well as office space for community organizations. Immediately across the street
from the ECC is a small, well-kept public park which is frequented by local residents. The ECC has a
distinctly community feel, compared to the CDD which is situated in an institutional setting in a
downtown Los Angeles business district.
During the 2005-2006 grant year the HSFC School Readiness program provided comprehensive
center and home-based services to a core group of 91 children ages 0-5 and their families. Core
program services included daily center-based early care and education activities conducted Monday
through Friday, from 6:30 a.m. to 6:00 p.m. within six classrooms, five that are located at the Early
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
130
Childhood Center, and one that is housed at the Child Development Center..
Classrooms offer full-day, year-round early childhood education services for 80 children, including 8
infants (0-24months); 32 toddlers (24 to 40 months), and 40 pre-school aged children (40-60
months). SR services also include developmental assessments, referral and early intervention
activities; monthly parent education classes; intensive case management, including monthly home
visits; individual and family counseling; and comprehensive family health care services.
The following Promising Practices were added in FY07 and were continued.
1. Preschool-kindergarten transition plan
Beginning of the preschool year (August to October): As children
begin their preschool year teachers assess them using the DRDP and
the Are You Ready for Kindergarten Checklist. Weekly observations
further assist teachers in becoming familiar with children’s individual
needs. Children’s receptive vocabulary and pre-literacy skills are
assessed by the SR Coordinator using the PPVT and the PALS.
Parent-Teacher conferences attended by the family’s case manager
and the center director serve to enhance communication and share
information about a child’s individual needs. Information from
assessments plus classroom and home observations and parent
feedback are incorporated into curriculum planning and classroom
activities. A classroom meeting serves to inform parents of preschool
expectations and emphasize importance of parent participation in
children’s preparation for kindergarten, including support with
“homework”. Teachers start sending homework home to reinforce
concepts learned in class and practice developing skills.
Middle of the preschool year (November to February): Teachers
continue to assess children’s progress through weekly observations
and a DRDP administered six months from the initial one. Any
concerns are addressed with the child’s parents in coordination with
the family’s case manager. Preschool Prep Parent Meetings begin,
focusing on parent’s choices for children’s kindergarten, including
private, charter, and magnet schools for which applications are due
early.
End of Preschool Year (March to June): Preschool Prep Parent
Meetings continue. Meetings provide information on the application
process (neighborhood schools, dates when applications are
available, are due), as well as prepare parents to be involved and
knowledgeable partners in their child’s education during the rest of the
year and beyond. A Transition List identifying children’s neighborhood
school, parent’s choice, if different from the neighborhood school, and
possible transition dates is used to plan enrollment and prioritize exit
paperwork for children and families. Children participate in field trips
to local schools together with their teachers. Frequently asked
(children’s) questions are answered in a letter to parents sent home
prior to the field trip. In the classroom, teachers incorporate
discussions and materials about the transition to kindergarten and
continue to emphasize the importance of completing and returning
homework. Parents begin receiving notices of enrollment from
schools and start dates. A Moving On Celebration provides closure
and celebrates children, families, and staff’s team work.
Transition (July to September): Parents complete exit paperwork
with program staff. Staff complete exit assessments of children.
Children begin leaving for kindergarten. Staff supports children and
families with the logistical and emotional steps of transition.
Written MOUs were completed with 10 local elementary schools and
3 charter schools. We continue to work on ways to facilitate smooth
transitions for children and families to the more than 30 schools they
will attend each year.
2. Partnership with the USC School of Dentistry
Students from the USC School of Dentistry-Pediatric Clinic provide onsite dental screenings to all children in our School Readiness program,
free of charge. In addition to screenings, children received fluoride
treatments on site. Parents receive a summary of findings and
appointments for f/u care at USC School of Dentistry if they are not
already receiving dental care elsewhere. Children in our community
often suffer from early and untreated dental problems due to improper
dental hygiene and lack of adequate nutrition. Dental care, especially
pediatric care is not easily available. Even when available, children
are often fearful and uncooperative when visiting dentists. Our
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
131
3.
4.
program tries to make the experience as pleasant and fun as possible
for children (and dental students). Prior to the screenings, teachers
prepare children through various means that include conversations
about taking care of their teeth, developmentally appropriate books
(including stories of animals and children going to the dentist), and
pretending to brush the teeth of a giant plastic denture and with a giant
toothbrush. On screening day, children are well-prepared for the
experience and also encouraged by having their classmates
participate. More cooperative children make better patients for the
dentistry students to practice giving exams.
Responsible Fatherhood Program
This federally funded program seeks to support fathers in their role through
classes and group activities.
A group of between four and eight men meets every Thursday night and
covers topics such as controlling your anger and being involved with your
children. The program held a camp for dads and kids this summer and is
looking for ways to involve men in their children’s lives. The fathers work
on projects together at the EDD and Mercy Housing, such as assembling
chairs, painting a bike lane and playground equipment, and planting plants
in the playground.
According to one father, “we talk with one another more now and have
activities with our children”. One mother offered the following comment,
“My husband says that the fatherhood meetings have helped him to
understand his son. Maybe that is why they get along so well. He says that
he wishes he had had this support when our daughters were young.”
A preschool teacher at the ECC commented that the summer has allowed
parents to spend more time with their children doing fun activities such as
taking family trips.
Calendar of Parenting Education Activities and Family Involvement
Activities
In FY07 we developed and began implementing a calendar of parenting
education activities and posting the calendar (English/Spanish) throughout
the ECC. The activity calendar included information about center-wide
events, parent classes, classroom parent involvement activities, field trips,
holidays, and monthly staff development days (when we close early).
Developing and posting this calendar has been very helpful in enhancing
communication with parents, boosting parent participation in different
events, and helping parents to plan their time.
FY 2008
Goal FY 2008
2008 Objective
Measure/Indicator of Success
All children living in HSFC’s service area will start school ready to learn.
Readiness in children is confirmed by evaluating the following 5 dimensions:
Physical well-being and motor development-health status, growth, disabilities, gross and fine
motor skills, as well as conditions before, at, and after birth such as exposure to toxic
substances.
Social and emotional development: Social development refers to children’s ability to interact
socially (e.g., ability to take turns and to cooperate). Emotional development includes a child’s
perception of him/herself, the ability to understand the emotions of other people, and the ability
to interpret and express one’s own feelings.
Approaches to learning refer to the inclination to use skills, knowledge, and capacities. Key
components include enthusiasm, curiosity, and persistence on tasks, as well as temperament
and cultural patterns and values.
Language development includes verbal language and emerging literacy. Verbal language
includes listening, speaking, and vocabulary. Emerging literacy includes print awareness (e.g.,
assigning sounds to letter combinations), story sense (understanding that stories have a
beginning, middle, and end) and writing process (e.g., representing ideas through drawing,
letter-like shapes, or letters).
Cognition and general knowledge includes knowledge about properties of particular objects and
knowledge derived from looking across object, events, or people for similarities, differences,
and associations. It also includes knowledge about societal conventions, such as the
assignment of particular letters to sounds, knowledge about shapes and spatial relationships,
and number concepts (e.g., one-to-one correspondence of numbers and objects, and the
association of counting with the total number of objects).
Family and community supports for children’s readiness are demonstrated by the following:
All children have access to high-quality and developmentally appropriate preschool programs
that help prepare them for school.
Every parent is the child’s first teacher and devotes time each day to helping his/her preschool
child learn. To this end, parents should have access to the training and support they need.
Children receive the nutrition, physical activity, and health care they need to arrive at school
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
132
Baseline
Intervention Strategy for
Achieving Goal
with healthy minds and bodies and to maintain mental alertness.
HSFC’s service area has the highest population density and the oldest housing stock in the county. It
is the home of the working poor. The median annual household income is $19,930. Moreover, 42%
of households earn less than $15,000 per year. More than 21,000 children under the age of five live
below poverty. Yet more than half of these children live in households in which one or both parents
work. A third of the labor force is employed in the garment industry and other light manufacturing
industries and a fifth in service occupations. In terms of ethnicity, 72% are Latino, 9% African
American, 7% Asian, and 6% Caucasian. However, more than 90% of the elementary school-aged
children are Latino. Children under age 14 represent 28% of the population and only 7% of residents
are > 65. Spanish is the primary language for more than 55% of families in the area. In a study of
Latinos in South Central Los Angeles, 96% of the children were born in the U.S. compared to only
20% of their parents. Downtown Los Angeles is ranked as the lowest literacy area in the city. The
region has high levels of limited English proficiency; more than 70% of school-aged children are
limited English proficient. In the core service area, 23% of persons 16 years and older have a high
school education or less; 36% have less than a ninth grade education; and 61% have only
rudimentary education. Parents in this community often find themselves isolated, feeling depressed
and overwhelmed by their daily struggle for economic survival. Hence, they are less likely to
verbalize a great deal with their young children or to utilize communication styles that nurture early
language skills. Likewise, the babysitters with whom they leave their children while they work are
unaware of the importance of language development in children and how to foster such development
in children in their care. This lack of knowledge can seriously impact children’s futures since studies
show that impairment of early language development becomes a disability for children, limiting their
subsequent social and educational growth
Provide high quality, full-day, year-round, center-based early childhood care and education activities
with a strong developmental focus and meet federal EHS/HS performance standards.
Use the Creative Curriculum as the basis for the arrangement of the physical environment, weekly
lesson planning, weekly observational notes, and ongoing child assessments.
Result FY 2008
Provide the following SR services: developmental assessments, referral and early intervention
activities, monthly parent education classes, intensive case management including monthly home
visits, individual and family counseling, and comprehensive family health care services.
A total of 138 children ages 0-5 and 188 parents were served in our SR program during the 20072008-grant year. This number reflects the natural flow of children in and out of the program, as new
children are enrolled to replace those who leave to enter kindergarten or for other reasons (e.g.
family re-location or family no longer requires childcare).
All children receiving SR services received comprehensive developmental assessments using the
Desired Results Developmental Profiles instead of the Gesell Developmental Profiles. Through this
assessment process we identified or confirmed 28 children with significant developmental concerns.
Thus, 20% of children receiving core services were exhibiting developmental problems significant
enough to warrant services through a Regional Center (0-3yrs) or the LAUSD school district (3-5yrs).
Ensuring that eligible children receive all the services identified on their IFSP/IEPs is often a
challenge because the need in our area is high and resources are scarce. This is especially true for
children with identified speech and language difficulties. During this period we assisted families in
coordinating services for their special needs children in a variety of ways. Support included helping
to find therapists, arranging for transportation to off-site services, attending meetings to amend an
IEP, working with PKIT teachers on how to support children in the classroom and helping parents to
advocate for their children. Children with IEPs and IFSPs continued to receive support for their
IEPs/IFSP objectives through an overall enriched ECE curriculum as well as specific activities
designed by their classroom teachers and coordinated with their individualized service/education
plans.
A total of 45 children has already transitioned or is in the process of transitioning to kindergarten.
Children leaving our program will attend kindergarten at over 30 different schools, starting at several
time points over the Summer. Transitions to kindergarten continued to prove somewhat challenging
due to a combination of children attending several possible schools (over 30) with several start dates
(public traditional, public year-round with three or four tracks, independent {charter, magnet, private})
and frequently very short notices on start dates (both for children wait listed at non-public schools
and for children who have been enrolled in a public year round school for some time but only receive
confirmation of their start date a day or two ahead.) In addition to the stress and anxiety that
children and parents experience at not being able to plan ahead (families often have to make quite
significant arrangements to accommodate a new schedule), our staff is significantly impacted too,
since there is a great deal of planning and paperwork that needs to be done. In addition to enrolling
new children to fill the vacant spots (which involve recruitment, orientation, application, income
verification, home visit, orientation to the classroom), staff also has to complete paperwork for the
exiting children. Teachers complete the modified DRDP and the Are You Ready for Kindergarten
checklist as well as put together a farewell portfolio for children. The program coordinator needs to
administer post-tests to children (PPVT, PALS). Case managers complete exit forms with all
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
133
departing children and families. Graduation ceremonies were held at the ECC to provide closure and
celebrate children, families, and staff’s team work. The theme was “Aloha-Look How Far We’ve
Come”. We were honored to host Councilman Ed Reyes (District 1), Dr. Celia Ayala (Los Angeles
Universal Preschool), and Pastor Paiva (Angelica Lutheran Church), who all delivered inspirational
speeches to parents about their role as their children’s teachers and guides. Graduating children
received gifts of fully stocked backpacks from LAUP and books from Preschool California. CDC
graduation ceremonies will be held in July.
Eighty-six percent (86%) of children transitioning to kindergarten have Almost Mastered or Fully
Mastered skills necessary to be personally and socially competent.
When these preliminary results are examined against a backdrop of high familial need (poverty,
language barriers, low formal education) and high proportion of developmental concerns (one third of
all SR children, one third of children transitioning to kindergarten), the achievement of preschoolers
in our SR program becomes especially meaningful.
Promising Practices:
Cross-discipline support of teaching staff: Weekly meetings comprised of classroom staff, the
center’s director, and the family service coordinators promoted better understanding of children’s
and families’ needs, identified opportunities for supporting children and families as a team, and
promoted overall communication and understanding across different service providers.
Center Self-Assessment: Provided program staff with tools to assess program’s strengths and
opportunities for growth; contributed to staff development plan; provided data used in our
Evaluation report to First 5.
Agency Sustainability Planning: Promoted understanding of program vision, goals, challenges;
engendered in-depth discussions among participants and with agency director; resulted in a
Sustainability Plan that will help in our efforts to secure capital for a new building; facilitated
process of hiring a director of planning and development.
Management Team Development: Enhanced awareness of different programs within Hope
Street, deepened relationships, renewed our commitment to work together toward a common
purpose.
Parent Involvement: Offered more opportunities for parent involvement that incorporated
parents’ input. Topics included some new themes we had not before considered, such as Stress
Management (2/15/08), and Self-Defense (3/21/08), which were fun, useful, and very well
received by parents.
A brief summary of the many benefits of participating in Hope Street Family Center’s School
Readiness Program is provided below :
Benefit to Children: 1. Appropriate overall development, 2. enhanced socio-emotional
skills, 3. Improved English skills, 4. school readiness. Parents report progress in their
children, teachers of Kindergarten graduates praise children’s work, early identification of
issues, early referral for services avoids problems getting bigger. Results from PPVT testing
indicate that children going to Kindergarten enhance their Receptive Language Skills (in
English) by 11.9 standard score points. PALS results show that children leaving for
Kindergarten can name (on average) 20 Upper Cap letters and learn an average of 14.6 letters
in about 7 months of participating in our preschool classes. This number includes children with
IEPs and children.
Benefit to Parents: 1. Having children in high quality early care and education center
allows parents to work and study while children learn. (increased income and reported well
being; parents report great satisfaction with program; 90% of new enrollment from word of
mouth). 2. Parents increase parenting skills. From parent report and staff observations alike,
we know that as a result of participating in our program, most parents experience increased
enjoyment of their parent role, better parent-child interactions, and fewer future referrals to child
and family services and other law-enforcement agencies.3. Opportunities for involvement
and personal leadership. Many parents also report that they have grown as individuals and
achieved success in areas they would never have imagined they could, such as mentoring
other parents or taking positions of leadership such as those available through our Parent
Councils.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
134
Benefit to Providers: Teachers in our program receive support for continuing their
education and enhancing their skills (support through stipends; flexible work schedules when
possible; in-services; staff development opportunities). One area in which our program staffs
have grown over the past year is in our ability to truly work together as a team, giving and
receiving support and assistance when needed. The need for more cohesiveness and better
communication across disciplines was previously identified as part of our yearly self
assessment and staff interviews done for the purposes of reporting to First 5LA. These positive
effects can be attributed generally to some changes in staff, more staff development, and a
more concerted effort to provide ongoing feedback and information to teaching staff and to
involve all staff in planning and decision making as appropriate to their work and qualifications.
Feedback from staff indicate more satisfaction with job, feeling more respected, opinion
valued, requests and concerns addressed by administrative staff in a timely manner;
more mutual accountability.
Success Story: Since a majority of children transitioning to kindergarten are new to the program
at the beginning of the school year, transition efforts often include addressing socio-emotional,
behavioral, health, or familial issues that interfere with their readiness to learn. During this
reporting period, we had one very salient example of how a team of dedicated, observant staff,
can help remove obstacles to a child’s ability to be ready for school:
A child in a preschool class at the Early Childhood Center had been struggling in class since the
beginning of the school year: she had great difficulty paying attention during circle time, often fell
asleep during stories, seemed not to hear when teachers spoke to her, and had difficulty
enunciating sounds in an intelligible way. Her pre-test scores on the PPVT and the PALS were
low. Her teachers raised their concern with the child’s case worker and the center director, who
worked with her mother to identify a reason for the child’s poor performance. After other options
were ruled out (domestic violence, late bed times, etc), the child was referred to various specialists
to determine if there was a medical reason for her malaise and poor performance. A doctor was
finally able to determine that the child had a serious case of dairy intolerance, the primary
symptom of which was congestion so severe she could not breathe well, sleep well, or even hear
well. Once dairy was removed from her diet (completely at school, and mostly at home) this child’s
attention, participation, and language skills improved dramatically. Her progress was noted by her
teachers and mother, and was further reflected in her PPVT post-test performance, just 7 months
later.
Qualitative data were obtained through in-depth interviews of staff and select parents whose children
are receiving SR services. The parent interviews focused on the impacts of the program on their
children and on themselves as parents; the types of assistance that families have received; any
concerns about needs that have not been addressed; level of satisfaction with the program; and
recommendations for improving the program.
As part of our Annual Self-Assessment, we administered Parent Surveys to parents at both SR sites.
For the purposes of this report only the findings from the ECC are reported. 44 parents completed
this anonymous survey and returned it in a sealed envelope. Program parents identified many
changes that their children have enjoyed due to the services received from ECC staff. Children have
improved their English speaking ability, learned how to count, and know their alphabet. Some
parents noted an improvement in social skills, respect, and behavior in their children. Many parents
also noticed that their children are much more socially active, participate in social relationships with
other children, and are overall more comfortable in a social environment.
For this program year nine families were selected to participate in the interviews. All interviews were
conducted in Spanish. This sample was compiled to help better understand: (1) how well the SR
program prepares children for kindergarten and (2) how well children who have left the SR program
and entered kindergarten are faring. This information can be used to help improve (1) the steps that
are taken by staff to ensure a smooth transition to the school environment and (2) the methods that
are effective in helping children excel in their new school.
Parents interviewed reported noticing changes in their children and commented on their
newfound independence, maturity, and ability to follow the rules
Many of the children have learned to get along with others and to follow the rules. “My
child used to be a loner and would not participate. She now says her opinion; she’s very
opinionated and is very much a part of the crowd. My other child knows her numbers, her
address and cell number, her ABCs and I’ve also learned ways to teach her new sounds.
I am surprised to hear my four-month-old sing and clap his hands, even though he is only
four months!”
Perhaps the greatest change is that children enjoy learning and look forward to it
Parents of children with special needs discussed ways that their children have benefited
from the program. Parents mentioned that their children improved their social skills, they
share with others, can communicate better, and are no longer as overly active as they
used to be. Some parents said that their children are more independent, such as being
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
135
able to dress themselves. One parent explained “ I noticed my child now likes to share
and he likes to play in the group. My child could not express his feelings before. He would
cry a lot. Now he can express his feelings. My child is now more developed. It used to be
very difficult for him to write his name. He couldn’t dress himself before.” Another mother
discussed the struggles she used to have with her child and his lack of social skills. “My
child used to be very anti-social, he had problems speaking. He now speaks well, he can
express himself with words, and he socializes/plays with other kids. My youngest child
can now walk and communicate with me. My child has received language therapy; he can
now talk, before he never talked at all.”
Parents also credited the program for allowing them to become more self-sufficient.
“Because of the Center I have been able to get employment. I trust my children’s safety
here at the Center. I have been given economic opportunities because of the Center,
through the referrals and all the information I have been provided…If it wasn’t for
programs like these, a lot of moms could not work. I can advance economically because
of this center.”
Another ECC parent discussed that the social worker provided them assistance with
immigration issues. The social worker was able to obtain legal services for this family,
hence allowing them the opportunity to seek employment. This family also felt that
because of the services they received from the ECC, their lives have improved
economically.
Program involvement has helped parents make progress towards positive parenting
practices. HSFC SR parents are sometimes facing outside stressors that compromise
their ability to provide positive parenting. An ECC staff member noted :”One parent I
worked with would often scream at her children and hit them. I have worked with that
family and that mother and she has recently told me she has become a different and
better person.”
One mother said that she attended anger management classes and classes on how best
to introduce new significant others into her child’s life. Another mother mentioned that she
is more aware of how to deal with her personal relationships in front of her child. “I noticed
that I have become more positive. I take advice and I get what I need. I used to have a
lot of problems with my partner. He didn’t get along with my 16-year old son. My partner
came to talk to the social workers and he received advice. We no longer fight in fron of
the little child.”
Among the respondents to the Parent Survey, 93% indicated that enrollment in the
program had made it easier to keep their job, 82% accepted a better job, and 74%
attended educational or training programs.
Overall findings for children in our program indicate that children of all ages are making progress in
all areas of development, although there is some variability in areas of strength. Preschoolers exiting
our program for kindergarten have made tremendous progress in the areas of English vocabulary
acquisition and letter recognition. Program parents also report making very positive and significant
changes of their life and their parenting abilities.
The ECC participated in a California Department of Education, Child Development Division program
audit in May 2008. The audit included an extensive 2-day review of our records, including children’s
files, attendance records, and binders with program activities. We were commended on our
organization and sound record-keeping and passed the audit with no findings. The experience
allowed us to re-think some practices and put in place some different ways to keep records for ease
of access.
During this reporting period, our agency had the opportunity to participate in a Sustainability Project
sponsored by First 5 LA. Our designated Sustainability team was composed of Sherrie Segovia,
PsyD, Maria Avila, PsyD, Rich Hume, JD, Vickie Kropenske, MS, and Laura Diaz, MA. Our
participation in the sustainability project workshops enhanced our teams’ understanding of the way
our agency works, our mission, our values, and our future. In April, our team completed a written
Sustainability Plan (attached). Our presentation in June at the California Endowment was very well
received.
Goal 2009
2009 Objective
Measure/Indicator of Success
CHMC provides space for HSFC’s CDC in Leavey Hall, for an SB 697 in-kind contribution of
$79,307. The Early Childhood Center is at Angelica Lutheran Church in Pico Union. The annual
budget is $654,333. This program is funded by First 5 LA.
FY 2009
All children in CHMC’s service area will start school ready to learn.
Readiness in children is confirmed by evaluating the following 5 dimensions:
Physical well-being and motor development-health status, growth, disabilities, gross and fine
motor skills, as well as conditions before, at, and after birth such as exposure to toxic
substances.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
136
Baseline
Intervention Strategy for
Achieving Goal
Social and emotional development- Social development refers to children’s ability to interact
socially (e.g., ability to take turns and to cooperate). Emotional development includes a child’s
perception of him/herself, the ability to understand the emotions of other people, and the ability
to interpret and express one’s own feelings.
Approaches to learning- This refers to the inclination to use skills, knowledge, and capacities.
Key components include enthusiasm, curiosity, and persistence on tasks, as well as
temperament and cultural patterns and values.
Language development-includes verbal language and emerging literacy. Verbal language
includes listening, speaking, and vocabulary. Emerging literacy includes print awareness (e.g.,
assigning sounds to letter combinations), story sense (understanding that stories have a
beginning, middle, and end) and writing process (e.g., representing ideas through drawing,
letter-like shapes, or letters).
Cognition and general knowledge- includes knowledge about properties of particular objects
and knowledge derived from looking across object, events, or people for similarities,
differences, and associations. It also includes knowledge about societal conventions, such as
the assignment of particular letters to sounds, knowledge about shapes and spatial
relationships, and number concepts (e.g., one-to-one correspondence of numbers and objects,
and the association of counting with the total number of objects).
Family and community supports for children’s readiness are demonstrated by the following:
All children have access to high-quality and developmentally appropriate preschool programs
that help prepare them for school.
Every parent is the child’s first teacher and devotes time each day to helping his/her preschool
child learn. To this end, parents should have access to the training and support they need.
Children receive the nutrition, physical activity, and health care they need to arrive at school
with healthy minds and bodies and to maintain mental alertness
Unchanged from last year.
Provide high quality, full-day, year-round, center-based early childhood care and education activities
with a strong developmental focus and meet federal EHS/HS performance standards.
Use the Creative Curriculum as the basis for the arrangement of the physical environment, weekly
lesson planning, weekly observational notes, and ongoing child assessments.
Provide the following SR services: developmental assessments, referral and early intervention
activities, monthly parent education classes, intensive case management including monthly home
visits, individual and family counseling, and comprehensive family health care services.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
137
COMMUNITY BENEFIT AND ECONOMIC VALUE
A copy of the Classified Summary of Unsponsored Community Benefit Expense is
included in the Executive Summary section of this report.
Cost ratio calculations for Traditional Medicare, Medi-Cal care services, Charity Care
and Other Government programs is based on cost report provided by Cost
Reimbursement Department of the hospital.
Communication Plan
Internal communication plan
Updates on various community benefit programs are provided in the monthly enewletter distributed to all CHMC network users.
New employees are briefly informed about community benefits programs during the
New Employee Orientation Day. Each employee is given the latest copy of our
annual Service to Our Community Report.
The Contract Manager for Community Partnerships participates in the Patient
Education Committee.
The Contract Manager for Community Partnerships meets with individual Service
Managers at least annually to provide an update on relevant Community Benefit
Programs.
The Director of Community Benefits provides an annual update on Community
Benefit Programs and classes to all Department Managers at the request of the
President.
External communication plan
At least one community benefit program is highlighted in each edition of the
Foundation Update that is published twice each year and mailed to our medical
staff, donors, supporters, and Board members.
Each quarter, the Director of Community Benefits informs new medical staff and their
office staff about our community benefit programs and how they can refer patients to
them.
Each year CHMC publishes its annual Service to Our Community Report that
summarizes our community benefits programs and services.
Attachments
A. Charity Care Policy
B. Community Need Index, Map of the Community
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
138
APPENDIX A
CATHOLIC HEALTHCARE WEST
SUMMARY OF PATIENT FINANCIAL ASSISTANCE POLICY
(June 2008)
Policy Overview:
Catholic Healthcare West (CHW) is committed to providing financial assistance to persons who have
health care needs and are uninsured or under-insured, ineligible for a government program, and
otherwise unable to pay for medically necessary care based on their individual financial situations.
Consistent with its mission to deliver compassionate, high quality, affordable health care services, and to
advocate for those who are poor and disenfranchised, CHW strives to ensure that the financial capacity
of people who need health care services does not prevent them from seeking or receiving care. Financial
assistance is not considered to be a substitute for personal responsibility, and patients are expected to
cooperate with CHW’s procedures for obtaining financial assistance, and to contribute to the cost of
their care based on individual ability to pay. Individuals with financial capacity to purchase health
insurance shall be encouraged to do so as a means of assuring access to health care services.
Eligibility for Patient Financial Assistance:
Eligibility for financial assistance will be considered for those individuals who are uninsured, ineligible for
any government health care benefit program, and unable to pay for their care, based upon a determination
of financial need in accordance with the policy.
The granting of financial assistance shall be based on an individualized determination of financial need,
and shall not take into account age, gender, race, or immigration status, sexual orientation or religious
affiliation.
Determination of Financial Need:
Financial need will be determined through an individual assessment that may include:
a. an application process in which the patient or the patient’s guarantor is required to
cooperate and supply all documentation necessary to make the determination of financial
need;
b. the use of external publicly available data sources that provide information on a patient’s
or a patient’s guarantor’s ability to pay;
c. a reasonable effort by the CHW facility to explore and assist patients in applying for
appropriate alternative sources of payment and coverage from public and private
payment programs; and will take into account the patient’s assets and other financial
resources.
It is preferred but not required that a request for financial assistance and a determination of financial need
occur prior to rendering of services. The need for financial assistance may be re-evaluated at each
subsequent rendering of services, or at any time additional information relevant to the eligibility of the
patient for financial assistance becomes known.
CHW’s values of human dignity and stewardship shall be reflected in the application process, financial
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
139
need determination and granting of financial assistance. Requests for financial assistance shall be
processed promptly, and the CHW facility shall notify the patient or applicant in writing within 30 days of
receipt of a completed application.
Patient Financial Assistance Guidelines:
Services eligible under the policy will be made available to the patient on a sliding fee scale, in
accordance with financial need as determined by the Federal Poverty Level (FPL) in effect at the time
of the determination as follows:
Patients whose income is at or below 200% of the FPL are eligible to receive free care;
Patients whose income is above 200% but not more than 350% of the FPL are eligible to receive services
at the average rates of payment the CHW facility would receive from Medicare, Medicaid (Medi-Cal),
Healthy Families, or any other government-sponsored health program in which the hospital participates,
whichever is greater in amount for the same services;
Patients whose income is above 350% but not more than 500% of the FPL are eligible to receive services
at 135% of the average rates the CHW facility would receive from Medicare, Medicaid (Medi-Cal),
Healthy Families, or any other government-sponsored health program in which the hospital participates,
whichever is greater for the same services;
Patients whose income exceeds 500% of the FPL may be eligible to receive discounted rates on a case-bycase basis based on their specific circumstances, such as catastrophic illness or medical indigence, at the
discretion of the CHW facility.
CHW’s administrative policy for Eligibility and Application for Payment Assistance shall define what
qualifies as income for these purposes.
Communication of the Financial Assistance Program to Patients and the Public:
Information about patient financial assistance available from CHW, including a contact number, shall be
disseminated by the CHW facility by various means, including the publication of notices in patient bills
and by posting notices in the Emergency and Admitting Departments, and at other public places as the
CHW facility may elect. Such information shall be provided in the primary languages spoken by the
populations served by the CHW facility.
Any member of the CHW facility staff or medical staff may make referral of patients for financial
assistance. The patient or a family member, a close friend or associate of the patient may also make a
request for financial assistance.
Budgeting and Reporting:
Specific dollar amounts and annual plans for patient financial assistance will be included within the Social
Accountability Budget of the CHW facility. CHW facilities will report patient financial assistance
calculated at cost in the annual Social Accountability Report and may voluntarily report such information
as deemed appropriate.
Patient financial assistance statistics shall be disclosed in annual financial statements but shall not include
amounts that are properly considered to be bad debt or contractual discounts.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
140
Relationship to Collection Policies:
CHW system management shall develop policies and procedures for internal and external collection
practices by CHW facilities that take into account the extent to which the patient qualifies for financial
assistance, a patient’s good faith effort to apply for a governmental program or for financial assistance
from CHW, and a patient’s good faith effort to comply with his or her payment agreements with the CHW
facility.
For patients who qualify for financial assistance and who are cooperating in good faith to resolve their
hospital bills, CHW facilities may offer interest-free extended payment plans to eligible patients, will not
impose wage garnishments or liens on primary residences and will not send unpaid bills to outside
collection agencies.
Regulatory Requirements:
IN IMPLEMENTING THIS POLICY, CHW MANAGEMENT AND CHW FACILITIES SHALL COMPLY WITH ALL
FEDERAL, STATE AND LOCAL LAWS, RULES AND REGULATIONS THAT MAY APPLY TO ACTIVITIES CONDUCTED
PURSUANT TO THIS POLICY.
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
141
APPENDIX B
California Hospital Medical Center
Community Need Index
California Hospital Medical Center
CNI Score by ZIP Code
1.0 Less Needy
3.0
5.0 Most Needy
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
142
California Hospital Medical Center
Community Benefit Report FY 2008 – Community Benefit Plan FY 2009
143