The Endometrium
advertisement

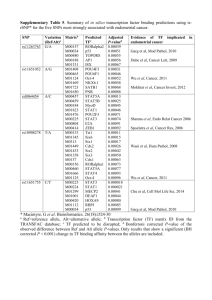
Nem’s Notes… Phase 2 Year 3 HUMAN LIFE CYCLE 6 (page 1 of 2) The Endometrium Uterus The two main parts of the uterus are: (a) Body (b) Cervix It is approximately 7-8 cm in length, 5-7cm wide and 2-3 cm thick. The three layers are: (a) Perimetrium (b) Myometrium (c) Endometrium Endometrium The endometrium is 4-5mm thick at its peak of development and varies according to the endometrial cycle. The three layers of the endometrium are: (a) Compact Layer connective tissue (nearest lumen) (b) Spongy Layer thick oedematous connective tissue (c) Basal Layer ends of uterine glands (not shed in period) Endometrial Cycle Fertilization The endometrial cycle controls menstruation and mirrors the ovarian cycle responding to fluctuations in hormone concentration. It has a length of 28 days with day 1 being menstrual flow. (a) Menstrual Phase Menstruation, flow shedding blood and endometrium 4-5 days (b) Proliferative Phase Growth of follicles controlled by oestrogen, 2-3 times increase in endometrium. Increased glands and lengthening of spiral arteries 9 days (c) Secretory Phase Formation of corpus luteum controlled by progesterone. Ovulation. Increased endometrial thickening 13 days After fertilization the zygote forms and cleaves to become the morula and blastocyst. Implantation occurs on day 20-28 of the cycle (6th day of secretory phase). The sycytiotrophoblast produces hCG and the corpus luteum continues secretion of oestrogen and progesterone. The secretory phase then continues and menstruation does not occur. The endometrium enters pregnancy phase. If fertilization does not occur the corpus luteum degenerates and oestrogen and progesterone levels fall. This causes an ischaemic phase of the endometrium and menstruation occurs. Glandular secretion stops, interstitial fluid decreases and the spiral arteries constrict. Venous stasis ensue with patchy necrosis. Blood breaks through the endometrial surface into the uterus and vagina. Menstrual Flow Menstrual flow is approximately 20-80 mls of blood over 3-5 days. The compact and spongy layers are shed whilst the basal layer remains. more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 1 of 2 Nem’s Notes… Phase 2 Year 3 HUMAN LIFE CYCLE 6 (page 2 of 2) The Endometrium Fertility The embryo will not implant in the endometrium unless the conditions are favourable. This is called the ‘window of implantation’. Implantation failure is common and is the major reason for IVF fertility treartment. Contraceptive techniques can interfere with endometrial receptivity to the embryo. These include: (a) Intrauterine contraceptive device (IUD coil) (b) Combined oral contraceptive (and progestogen-only) (c) Post-coital contraception Endometrial Cancer Normal growth of the vascular, stromal and epithelial cells is tightly controlled. Excess growth may lead to hyperplasia and then onto endometrial cancer. It mostly occurs in post-menopausal women (55-65 years) and are mainly adenocarcinomas which spread locally and to the pelvic nodes. Most present with postmenopausal bleeding. Risk factors for endometrial cancer include: (a) Polycystic Ovaries (b) Obesity (c) Diabetes (d) Nulliparity Diagnosis is by means of hysteroscopy and biopsy, and treatment is by total abdominal hysterectomy and bilateral salpingo-ooterectomy. Menorrhagia Menorrhagia is most commonly caused by fibroids and is one of the most common causes for women to consult their GP and gynaecologist. Most have heavy regular bleeds but some have irregular bleeding. Most have dysfunctional uterine bleeding not associated with any pathology. Menorrhagia appears linked to endometrial changes including: (a) Increased vasodilatation (prostaglandins) (b) Decreased vasoconstriction (endothelins) But it is still poorly understood. Endometriosis Deposits of endometrium outside the uterine lining are called endometriosis and are most commonly found in the pelvis. They are thought to migrate down the fallopian tubes and implant. It is associated with the following: (a) Pain (b) Infertility (c) Menstrual irregularity (d) Menorrhagia (e) Adenomyosis Amenorrhoea Secondary amenorrhoea may result if the basal layer is destroyed. This may be accidental or deliberate. Hormonal levels will be normal and ovulation will still occur. Imaging & Sampling Different imaging and sampling techniques are available: (a) Ultrasound (assess thickness and structures) (b) Hysteroscopy (direct imaging + biopsy or operative) (c) Biopsy (investigate bleeding/thickening/hyperplasia) more online at http://homepage.virgin.net/nemonique.sam/noteindx.htm page 2 of 2



![04 Lecture 4[1]](http://s3.studylib.net/store/data/009259632_1-99448882b99895746cd105d04644046b-300x300.png)