Tamoxifen a endometrium
advertisement
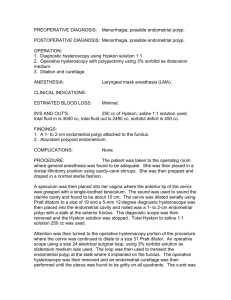
Precancer, benign and malignant tumors of the uterus and ovary Eduard Kučera UTERINE FIBROIDS RISK FACTORS ● They are many risk factors1 associated with the development of uterine fibroids 1.Flake GP et al, Environmental Health Perspectives 2003; 111(8):1037-54 WHAT ARE THE SYMPTOMS? ● ● ● Not all fibroids are symptomatic When symptomatic, fibroids can be linked to at least three major problems3 However, for the 50% of women with symptomatic fibroids, the condition is debilitating.1 Bleeding complaints Pregnancy complications Symptoms can include: ● ● ● Abnormal or heavy menstrual bleeding1, 2 Pain,1,2 pressure symptoms1,2 and urinary symptoms2 Impairment of Quality of Life Mass effects related to the size and location of fibroids These symptoms and consequences have been shown to diminish quality of life3 2 1. Tropeano G, Amoroso S, Scambia G. Hum. Reprod. Update (2008) 14 (3): 259-274. 2. Downes E, Sikirica V, Gilabert-Estelles J. et al. Eur J Obstet Gynecol Reprod Biol. 2010; 152(1): 96-102. 3. Viswanathan M, Hartmann K, McKoy N. et al. Evid Rep Technol Assess (Full Rep). 2007 Jul;(154):1-122. Review. MECHANISMS FOR FERTILITY IMPACT • Mechanistic: space; abnormal contractions • Local inflammation for sperm and embryo • Inadequate blood supply DIAGNOSIS - WHEN AND HOW? ● ● Physical examination may be the first signal that a woman might have uterine 1 fibroids. Imaging methods to evaluate 1 these benign tumours: ● Ultrasonography ● Hysteroscopy ● Magnetic resonance imaging (MRI) 1. Evans P, Brunsell S. Am Fam Physician. 2007 May 15;75(10):1503-1508.ian Uterine Fibroids TREATMENT THERAPEUTIC APPROACH Currently, therapies are intended to reduce or eliminate uterine fibroid symptoms through one of the following options 1 ● ● ● Reduction of the size of tumours Reduction of the amount of bleeding Removal of the uterine fibroids or uterus 1. Miller CE, Journal of Minimally Invasive Gynecology 2009; 16:11–21 THERAPEUTIC APPROACH The choice of therapy is influenced by the patient’s ● ● ● ● ● Symptom severity Tumour characteristics (e.g. volume, localisation) Age Uterine preservation wishes Fertility preservation wishes Endometrial cancer Endometrial cancer – most common gynecological malignancy 4th most frequent malignancy in women In Czech Rep. incidence 32/100 000 year 1500 new cases diagnosed per year (e.g. in UK 6,430) Maximum around 60 - 70 years Obesity of women – typical phenotype Etiology so called „endometrial carcinoma syndrome“: obesity, (DM, hypertension) - peripheral transformation of androgens - insufficiency of ShBG recently often used so celled.: postmenopausal syndrome age: 6. - 7. decade nulliparity (RR=2,8) Infertility (RR=8) late menopause (RR= 2,4) estrogen producing ovarian cancers high intake of animal proteins and fats exogenous estrogens - unopposed gestagens (RR=2,3) tamoxifen (RR=2,4) Carcinogenesis in periand postmenopausal women younger women older women complex hyperplasia de novo hyperplasia with atypia endometrial carcinoma ( Type I usually well diff. ) endometroid carcinoma ( Type II usually poorly diff. ) papillary serous clear cell carcinoma Histological types Carcinoma (98%) endometroid adenocarcinoma adenocarcinoma with squamous cells clear cell carcinoma papillary serous spinocellular Sarcoma (2%) leiomyosarcoma endometrial stromal sarcoma mixed mesodermal cancers Hyperplasia of endometrium Complex atypical hyperplasia = precancerosis of endometrial carcinoma ( especially endometroid type) - cell polymorphism, mitosis, index, hyperchromatosis nucleoplasmic - creation is independent on estrogen stimulation in atrophic endometrium Motlík,K, Živný,J.:Patologie v ženském lékařství,Grada,2001. FIGO staging 2010 The 2010 FIGO staging system is as follows: Carcinoma of the Endometrium IA Tumor confined to the uterus, no or < ½ myometrial invasion IB Tumor confined to the uterus, > ½ myometrial invasion II Cervical stromal invasion, but not beyond uterus IIIA Tumor invades serosa or adnexa IIIB Vaginal and/or parametrial involvement IIIC1 Pelvic lymph node involvement IIIC2 Para-aortic lymph node involvement, with or without pelvic node involvement IVA Tumor invasion bladder mucosa and/or bowel mucosa IVB Distant metastases including abdominal metastases and/or inguinal lymph nodes 5 – year survival year Stage 5 year survival rate I-A 90% I-B 88% I-C 75% II 69% III-A 58% III-B 50% III-C 47% IV-A 17% IV-B 15% Hysteroscopy and dg. curettage Curettage – frequent false negative results (10-50%) Curettage – in polyps up to 61% Hysteroscopy and targeted biopsy < 2% false negative results (Gimbelson, Loffer 1988, 1989, AJOG) Studies in 1383 histological findings obtained with D&C - 60% inadequate results (Smith, 1985) In 60% patients curetted < 1/2 cavity of the uterus (Stock, Obst.Gyn.,1975) Diagnostic hysteroscopy - options Panoramatic view – magnified 1x conventional hysteroscopy allows viewing the whole uterine cavity and locate pathologies panoramatic macro-hysteroscopy – 20x magnification in distance < 1 cm Micro-contact hysteroscopy – 80x magnification allows evaluation of endometrial vascularisation, gland characteristic and their openness Tamoxifen a endometrium Nonsteroidal synthetic anti-estrogen Adjuvant therapy in breast carcinoma Accumulation of effective substance in basal endometrium Endometrial proliferative abnormality (up to 40% postmenopausal women) - polyps, hyperplasia as much as endometrial carcinoma (2-3/1000/year) Higher risk of endometrial carcinoma after using more then 5 (?) years (2-7.5x) Most safe and effective screening is hysteroscopy in yearly intervals Tamoxifen – endometrium pathology Length of therapy not more then 5 years Metrorrhagia always indication to endometrial examination In asymptomatic women (cca 70%) HSK vs. UZ part of periodic yearly check ups High percentage of false positive results with ultrasound examination– stromal edema (vacuolar degeneration) Tamoxifen - 37 - 71% incidence of polyps – proliferative activity in epithelial and stromal part Incidence of endometrial carcinoma cca in 3% Tamoxifen and endometrium International agreement – 1997 Bioptical examination of the endometrium before beginning the therapy After 3 years of using observation in yearly intervals Lancet,1698-1711,2000. Tamoxifen and endometrium Hysteroscopy with biopsy – first choice in patients with Tamoxifen therapy Symptomatic patients and therapy longer then 3 years Positive family history Taponeco,F et al. Indication of hysteroscopy in tamoxifen treated breast cancer patients. J.Exp.Clin.Cancer,21,2002 Endometrial cancer - therapy Surgery - radical Radiotherapy Hormonal therapy