Chest Pain: Cardiac Or Not
advertisement

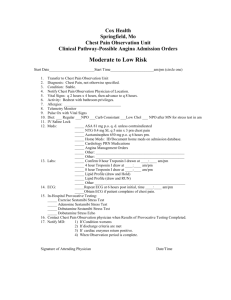
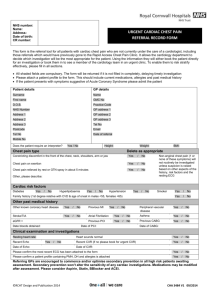
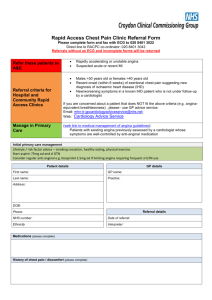
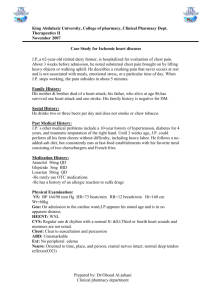
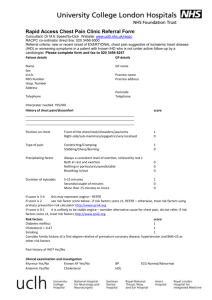
SECTION Cardiovascular Disease CHAPTER 52 Chest Pain: Cardiac or Not Gary B. Green Peter M. Hill The management of the patient with chest pain is a diagnostic and therapeutic challenge of critical importance. Three key chapters in this textbook discuss the identification of acute presentations of ischemic cardiac disease and its differentiation from other life-threatening disorders: the current chapter, Chapter 53, Acute Coronary Syndrome: Acute Myocardial Infarction and Unstable Angina and Chapter 55, Low Probability Acute Coronary Syndrome. The current chapter covers the assessment of acute chest pain with emphasis on identification of patients with potentially serious disorders and differentiating cardiac disease from noncardiac disease. The Acute Coronary Syndromes chapter discusses ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), and unstable angina. The Low Probability Acute Coronary Syndrome chapter discusses the identification and management of the remainder of patients who do not meet criteria for acute coronary syndrome (ACS), yet require further evaluation beyond the immediate ED period. OVERVIEW ■ DEFINITIONS ACS is a constellation of signs and symptoms resulting from an imbalance between myocardial oxygen supply and demand. There are three general classifications: unstable angina, NSTEMI, and STEMI. Unstable angina is a type of ACS with no elevation of biomarkers and no pathologic ST-segment elevation. NSTEMI is characterized by biomarker elevation and no pathologic ST segment elevation. Acute myocardial infarction (AMI) is characterized by ST elevation and biomarker elevation (STEMI). The phrase acute chest pain, commonly used in emergency medicine, deserves discussion. The term acute means of sudden or recent onset. Although there is no precise time period defined, most studies of acute chest pain patients in the ED limit entry to those with symptoms of <24-hours duration. In common practice, acute means that the patient stops his or her usual activity to seek medical attention, typically within minutes to hours. The term chest in this context refers to a location described by the patient on the anterior thorax, between xiphoid and suprasternal notch and between the right and left midaxillary lines. As the major serious thoracic disorders typically manifest symptoms within these regions, thoracic pain localized to the back, between the base of the neck and the lumbar region, is approached differently (see Chapter 276, Neck and Back Pain). Occasional patients with serious and life-threatening intrathoracic disorders will describe the location of their pain outside the anterior thoracic boundaries noted above. Some patients will have migratory pain that is no longer perceived to be in the chest by the time the patient reaches medical attention. Therefore, include significant intrathoracic disorders in the differential diagnosis whenever patients describe symptoms in adjacent regions (e.g., epigastric, neck, jaw, shoulder, and arm). The term pain describes a noxious, uncomfortable sensation. However, pain perception and description vary widely, and patients may use terms such as pressure, heaviness, ache, or discomfort. Be attuned to variation in the patient’s description of the perceived sensation. In summary, acute chest pain is pain 7 (1) of recent onset, typically <24 hours, which causes the patient to seek prompt medical attention; (2) with location on the anterior thorax; and (3) with a sensation distressing to the patient. ■ PATHOPHYSIOLOGY OF CHEST PAIN Stimulation of visceral or somatic afferent pain fibers results in two distinct pain syndromes. The dermis and parietal pleura are innervated by somatic pain fibers, which enter the spinal cord at specific levels and are arranged in dermatomal patterns. Visceral pain fibers are found in internal organs, such as the heart and blood vessels, the esophagus, and the visceral pleura. These visceral pain fibers enter the spinal cord at multiple levels and map to areas on the parietal cortex corresponding to the cord levels shared with the somatic fibers. Pain from somatic fibers is usually easily described, precisely located, and experienced as a sharp sensation, whereas pain from visceral fibers is more difficult to describe and is imprecisely localized. Accordingly, those experiencing visceral pain are more likely to use terms such as discomfort, heaviness, or aching. Patients frequently misinterpret the origin of visceral pain, as it is often referred to a different area of the body corresponding to an adjacent somatic nerve. For example, diaphragmatic irritation can present as shoulder pain, and arm pain may actually represent myocardial ischemia. In addition, gender, age, comorbidities, medications, drugs, and alcohol may all interact with psychological and cultural influences to affect the patient’s perception and communication of pain. INITIAL APPROACH The recommended initial approach to acute chest pain takes into account that some causes are serious and life-threatening, and prompt medical attention may prevent death and limit morbidity. Therefore, all patients should be triaged promptly. Patients with visceral-type chest pain (described above in Definitions), abnormal vital signs, significant vascular disease risks, and those with dyspnea should be placed into a treatment bed, a cardiac monitor initiated, an IV line established, oxygen administered, and an ECG performed. Other, less well-defined patients may simply appear ill; this insight should be respected. The initial evaluation should focus on immediate life threats: ensuring adequate airway, breathing, and circulation. The vital signs should be assessed and repeated at regular intervals as determined by the patient’s condition. The initial history should focus on specific questions concerning the character of the chest pain, the presence of associated symptoms, and a history of cardiopulmonary conditions. The patient is asked to grade pain intensity to follow response to therapy. If immediate life threats are not detected or have already been addressed, a more extensive evaluation can be performed. This “secondary survey” consists of a more comprehensive history and physical examination and appropriate laboratory and diagnostic testing. This evaluation should focus on those variables that will aid in establishing a tentative diagnosis and ruling out immediate life threats. The physical examination during this phase should complete those body systems not evaluated initially as well as rechecking abnormalities noted earlier. Many organizations have developed structured history and physician examination forms for acute chest pain to direct the information-gathering process and organize the diagnostic approach. Although such structured records may be helpful to less experienced physicians, they should never preempt sound clinical judgment. After consideration of a broad differential diagnosis, further diagnostic testing is then directed by history and 7-1 7-2 SECTION 7: Cardiovascular Disease physical findings toward the goal of systematic exclusion and/or confirmation of serious pathology. TABLE 52-2 Historical and Exam Factors That Decrease the Likelihood of Acute Myocardial Infarction Pain Descriptor Study No. of Patients Studied Described as pleuritic Described as positional Described as sharp Reproducible with palpation Inframammary location Not associated with exertion Chun et al.7 Chun et al.7 Chun et al.7 Chun et al.7 Everts et al.8 Goodacre et al.6 8822 8330 1088 8822 903 893 ■ HISTORY A thorough history will provide data useful for both diagnosis and risk stratification. Routine questions should determine the quality, location, area of distribution, radiation, intensity, frequency, duration, first occurrence, associated symptoms, and precipitating factors of chest pain. Although open-ended queries should be used initially, patients who have difficulty explaining symptoms in a narrative fashion should be asked directed questions. Pain intensity is commonly graded on a scale of 1 to 10, with 10 representing the worst pain the patient can imagine and zero being no discomfort whatsoever. The frequency, severity, and duration of pain episodes should be assessed over a continuum of the past weeks to better determine whether the condition might represent a stable or unstable symptom pattern. Precipitating factors, such as symptom changes with inspiration, movement, palpation, or exertion and during sleep or rest should also be identified. The classic description of angina pectoris is a retrosternal left anterior chest or epigastric discomfort described as crushing, tightening, squeezing, or a pressurelike sensation. Conversely, patients whose pain is described as stabbing, positional, or pleuritic do have a reduced likelihood of ACS as a cause of chest pain. The presence of certain associated symptoms during chest pain—dyspnea, diaphoresis, nausea, and/or vomiting—is common and does indicate a twofold higher risk of ischemia. Discomfort radiating from the chest to either shoulder, arm, hand, or jaw also indicates a significantly increased probability of ACS.3–5 However, lack of such radiation does not exclude ischemia. Anginal pain (or other anginal symptoms) is typically described as lasting from 2 to 20 minutes and pain from an uncomplicated AMI lasting up to 2 hours. In contrast, chest pain that is described as lasting a “split second” or only a few seconds is more likely to be due to another cause. This is also true for constant, unremitting pain lasting 12 to 24 hours or more. Anginal pain is often brought on by exertion and relieved by rest, although pain worsened by body movement or body position is suggestive (but certainly not diagnostic) of another etiology. Angina may also occur at rest, either due to destabilization of a preexisting coronary lesion or to coronary artery spasm with or without underlying atherosclerotic lesions. Most important, although the emergency physician can begin to estimate the risk of AMI based on symptoms alone, it must be recognized that in ACS, atypical characteristics are the rule rather than the exception. For example, up to 22% of patients with AMI describe symptoms as being sharp or stabbing in character, and up to 6% describe pain that is pleuritic.3 Tables 52-1 and 52-2 list factors that can be used to risk stratify patients based on clinical TABLE 52-1 Historical Factors That Increase the Likelihood of Acute Myocardial Infarction Pain Descriptor Study No. of Patients Studied Positive Likelihood Ratio (95% CI) Radiation to right arm or shoulder Radiation to both arms or shoulders Associated with exertion Radiation to left arm Associated with diaphoresis Associated with nausea or vomiting Worse than previous angina or similar to previous myocardial infarction Described as pressure Chun et al.7 770 4.7 (1.9–12.0) Goodacre et al.6 893 4.1 (2.5–6.5) Goodacre et al.6 Panju et al.3 Panju et al.3 Panju et al.3 893 278 8426 970 2.4 (1.5–3.8) 2.3 (1.7–3.1) 2.0 (1.9–2.2) 1.9 (1.7–2.3) Chun et al.7 7734 1.8 (1.6–2.0) Chun et al.6 11,504 1.3 (1.2–1.5) Positive Likelihood Ratio (95% CI) 0.2 (0.1–0.3) 0.3 (0.2–0.5) 0.3 (0.2–0.5) 0.3 (0.2–0.4) 0.8 (0.7–0.9) 0.8 (0.6–0.9) criteria, combining the data from four studies that assessed the clinical predictors of myocardial infarction (MI).3,4,6–8 Despite the existence of this information from studies, there is no identifiable symptom complex that allows for the safe discharge of the undifferentiated chest pain patient without objective testing. Atypical presentations of ACS occur more frequently in women, nonwhite minorities, diabetics, the elderly, and patients with psychiatric disease or altered mental status, compared with white males.9–11 In addition, disorders such as vasospastic and microvascular angina (also known as Syndrome X) and mitral valve prolapse are more common in women. Ischemia also produces different patterns of pain in women with known coronary artery disease compared with men. For example, chest pain at rest but not during exercise does not decrease the likelihood of disease in women as it does in men, and women with stable angina are more likely than men to have pain during rest, sleep, or stress. Other features that have been particularly associated with atypical presentations of ischemia in women include pain relieved by antacids, pain unrelated to exercise, pain not relieved with rest or nitroglycerin, palpitations without chest pain, and fatigue as a chief compliant.12 This may partly explain the observation that women, along with the elderly, take a longer time to seek care once their symptoms begin and have further delays in evaluation once they reach the ED. One study showed that although men presenting with AMI were more likely to have chest pain, this was explained by their younger age and delayed development of diabetes mellitus when compared with women. The associated symptoms more commonly found in women were nausea, emesis, jaw pain, neck pain, and back pain, although diaphoresis was more commonly found in men.12 All patients should also be questioned regarding the presence of cardiac risk factors, although these “risks” are valid only for predicting the presence of coronary artery disease within a given population and are not predictive of the presence or absence of acute ischemia in an individual patient.13 Major risk factors identified by large epidemiologic studies include age >40 years old, male or postmenopausal female, hypertension, cigarette smoking, hypercholesterolemia, diabetes, truncal obesity, family history, and sedentary lifestyle.7,8 Cocaine use is associated with AMI even in young people with minimal or no coronary artery disease. Chronic cocaine use has also been associated with accelerated atherosclerosis and severe coronary artery disease. The patient’s medical record should be reviewed, and any previous ECGs should always be compared with current tracings. Results of prior stress testing, echocardiograms, catheterizations, or radionuclide scans should be reviewed, if available, and the present symptoms interpreted in light of those results. For a more detailed discussion of the evaluation of patients with prior studies, see Chapter 55, Low Probability Acute Coronary Syndrome. ■ ISCHEMIC EQUIVALENTS Because of the visceral afferent innervation of the myocardium as well as the many confounding factors affecting the perception of ischemia, many patients with ACS will not experience chest discomfort. In fact, among 434,877 MI patients entered into the National Registry of Myocardial Infarction 2, 33% did not have chest pain upon presentation to CHAPTER 52: Chest Pain: Cardiac or Not the hospital.9 “Painless” presentations are more common in women, 37.5% versus 27.4% of men.12 Atypical presentations may be even more common in inner city EDs. One large public hospital recently reported that 47% of 721 consecutive patients with MI presenting to their ED did not report chest pain.10 Furthermore, MI patients with atypical presentations are less likely to receive appropriate anti-ischemic therapies and have an inhospital mortality rate more than twice that of those who present with chest pain.9 Although truly “silent” ischemia does also occur, ED physicians must always remain vigilant to recognize angina-equivalent symptoms. These may include one or any combination of the following: dyspnea at rest or exertion; shoulder, arm, or jaw discomfort; nausea; light-headedness; generalized weakness; acute changes in mental status; or diaphoresis. For example, one study found that those patients with dyspnea alone, without chest pain, had a fourfold increased risk of sudden death from cardiac causes compared with asymptomatic patients and a twofold increased risk compared with patients with typical angina.5 Epigastric or upper abdominal discomfort, even when relieved with antacids, should also raise the suspicion of myocardial ischemia, especially for patients >50 years old and those with known coronary artery disease. Among these highrisk groups, evaluation of abdominal pain should routinely include an ECG. Patients predisposed to sensory impairment due to diabetes, advanced age, psychiatric disease, or altered mental status are also more likely to present with atypical symptom.9 Palpitations, although a common and nonspecific symptom, should also raise concern about myocardial ischemia. Palpitations may indicate dysrhythmia induced by ischemia or, conversely, the inducement of ischemia by a primary tachyarrhythmia. Palpitations are often intermittent, and symptoms may have resolved by the time ED evaluation occurs. Patients often describe palpitations in association with nonspecific chest discomfort or dyspnea, making evaluation more difficult. The history should include questions about prescribed or over-the-counter medications or herbals, use of caffeine-containing beverages, symptoms of metabolic disorders such as hyperthyroidism, and any prior individual or familial heart disease. If the presentation suggests hypokalemia or hypomagnesemia, electrolytes should be checked. ■ SPECIAL POPULATIONS There are a number of interrelated and unquantifiable factors that influence how a patient perceives, interprets, and communicates symptoms. These factors span the physiologic, psychological, and cultural differences between peoples and individuals.14 Physiologically, there are true differences in pain signal propagation and mediation related to gender, age, and race as well as permanent or transient metabolic influences.15 It is well understood that the elderly patient is more likely to present with atypical symptoms of myocardial ischemia, and the diabetic patient may not be able to accurately sense or describe pain, making the diagnosis more difficult. The presence of multiple prescription medications, drugs, and alcohol will also alter the patient’s ability to perceive discomfort. There are gender and cultural differences in the perception and interpretation of pain, and the patient’s communication of symptoms and the clinician’s interpretation is affected by several “filters” that represent a wide spectrum of social, cultural, and personal biases of both parties.14,16 For example, the term “sharp” in some cultures is interpreted to mean “severe,” rather than knife-like.4 Therefore, to rapidly and effectively identify the minority of patients with life-threatening illness from the majority with less serious pathology, consistently use a thorough and systematic approach. ■ PHYSICAL EXAMINATION The physical examination of patients with the pain of ACS is often normal. Abnormalities in vital signs may include hyper- or hypotension, sinus tachycardia, or bradycardia. Tachycardia often results from increased sympathetic tone and decreased left ventricular stroke volume, although bradycardia may represent inferior wall ischemia. Patients with acute ischemia have a higher incidence of abnormal heart sounds, such as a di- 7-3 minished S1, a paradoxically split S2, and/or an S3 or S4, due to changes in ventricular function or compliance. Auscultation of the lungs may reveal the presence of ischemia-induced congestive heart failure. However, none of these findings are uniformly present, nor are they diagnostic. Chest wall tenderness reproducing the patient’s pain is somewhat suggestive of a musculoskeletal etiology. However, reproducible chest wall tenderness has also been reported in up to 15% of patients with confirmed MI. Therefore, this finding alone should not be used to exclude the diagnosis of myocardial ischemia.17 Despite a lack of specific diagnostic findings, a thorough physical examination remains essential, as it may provide clues to a nonischemic origin of symptoms and is often helpful in identifying or excluding other life-threatening causes of chest pain. ■ CLINICAL FEATURES During the initial assessment of patients with chest pain, the diagnosis of ACS should be considered in concert with other life-threatening conditions. These conditions include aortic dissection, pulmonary embolism, pneumothorax, pericarditis, pericardial tamponade, pneumonia, and esophageal rupture (Table 52-3). Other significant causes of chest pain include mitral valve prolapse, aortic stenosis, and GI conditions, such as perforated ulcer and cholecystitis. Table 52-4 contrasts the classic symptoms of life-threatening causes of acute chest pain. Although atypical presentations are common with all listed disorders, the classic symptoms are included here to stimulate the process of differential decision making. Pulmonary embolism is common and life-threatening, and is a diagnosis that can be missed in the ED due to the frequently atypical nature of its presentation. Pulmonary embolism can manifest with any combination of chest pain, dyspnea, syncope, shock, and/or hypoxia. In theory, the pain associated with a pulmonary embolism occurs when inflammation of the parietal pleura overlying the infarction causes chest pain that is generally sharp and related to respiration; however, most patients with pulmonary embolism and pleuritic chest pain have no radiographic evidence of pulmonary infarction. The discomfort of massive pulmonary embolism (such as saddle embolism) is described using more visceral terms such as a heaviness and tightness. Dyspnea, fever, cough, and/or hemoptysis also may be present, and the chest wall may be tender to palpation. Patients with massive pulmonary embolism often present with unstable vital signs and chest pain and dyspnea associated with tachypnea, tachycardia, and hypoxemia. Criteria can be used to determine the need for diagnostic testing in the evaluation for pulmonary embolism18 and to guide the intensity of the investigation19 (see Chapter 60, Thromboembolism). Risk factors for aortic dissection include atherosclerosis, uncontrolled hypertension, coarctation of the aorta, bicuspid aortic valves, aortic stenosis, Marfan syndrome, Ehlers-Danlos syndrome, and pregnancy (see Chapter 62, Aortic Dissection and Related Aortic Syndromes). The pain of aortic dissection (i.e., midline substernal chest pain) is classically described as tearing, ripping, or searing and radiating to the interscapular area of the TABLE 52-3 Important Causes of Acute Chest Pain Chest Wall Pain Pleuritic Pain Visceral Pain Costosternal syndrome Costochondritis (Tietze syndrome) Precordial catch syndrome Slipping rib syndrome Xiphodynia Radicular syndromes Intercostal nerve syndromes Pulmonary embolism Pneumonia Spontaneous pneumothorax Pericarditis Pleurisy Typical exertional angina Atypical (nonexertional) angina Unstable angina Acute myocardial infarction Fibromyalgia Aortic dissection Pericarditis Esophageal reflux or spasm Esophageal rupture Mitral valve prolapse 7-4 SECTION 7: Cardiovascular Disease TABLE 52-4 Life-Threatening Causes of Chest Pain: Classic Symptoms Compared* Disorder Pain (Location) Pain (Character) Angina pectoris Retrosternal or epigastric Massive pulmonary embolism Whole chest Crushing, tightness, squeezing, R or L shoulder, R or L arm/ pressure hand, jaw Heaviness, tightness None Segmental pulmonary embolism Focal chest Aortic dissection Midline, substernal Pneumothorax One side of chest Esophageal rupture Substernal Pericarditis Pneumonia Perforated peptic ulcer Substernal Focal chest Epigastric Pain (Radiation) Pleuritic Ripping, tearing Sudden, sharp, lancinating, pleuritic Sudden, sharp, after forceful vomiting Sharp, constant or pleuritic Sharp, pleuritic Severe, sharp None Intrascapular area of back Shoulder, back Back Back, neck, shoulder None Back, up into chest Associated Symptoms Dyspnea, diaphoresis, nausea Dyspnea, unstable vital signs, feeling of impending doom Tachycardia, tachypnea Secondary arterial branch occlusion Dyspnea Dyspnea, diaphoresis, may see signs of sepsis Fever, pericardial friction rub Fever, may see signs of sepsis Acute distress, diaphoresis Abbreviations: L = left, R = right. *Note: Atypical presentations are common with all listed life-threatening disorders. back. Typically, the pain is at its worst at symptom onset and is often felt above and below the diaphragm. Secondary symptoms resulting from arterial branch occlusions include stroke, AMI, or limb ischemia, and may overshadow the clinical presentation. No combination of clinical factors or chest radiography findings are adequate to exclude the diagnosis of aortic dissection, and specific imaging studies are usually required.20 Spontaneous pneumothorax may occur due to sudden changes in barometric pressure, in smokers or patients with chronic obstructive pulmonary disease or idiopathic pleural bleb disease, or in those with another pulmonary pathology (see Chapter 71, Spontaneous and Iatrogenic Pneumothorax). Patients usually complain of a sudden, sharp, lancinating, pleuritic chest pain and dyspnea. Auscultation of the lungs may reveal absence of breath sounds on the ipsilateral side and hyper-resonance to percussion, but clinical impression alone is unreliable. Diagnosis of a simple pneumothorax is made by chest radiography. Esophageal rupture (Boerhaave syndrome) is a rare but potentially lifethreatening cause of chest pain. Patients classically present with a history of substernal, sharp chest pain of sudden onset that occurs immediately after an episode of forceful vomiting (see Chapter 80, Esophageal Emergencies, Gastoesophageal Reflux Disease, and Swallowed Foreign Bodies). The patient is usually ill-appearing, dyspneic, and diaphoretic. The physical examination is often normal but may reveal evidence of pneumothorax or subcutaneous air. Chest radiography may be normal or may demonstrate pleural effusion (left more common than right), pneumothorax, pneumomediastinum, pneumoperitoneum, and/or subcutaneous air. The diagnosis can be confirmed by a study with water-soluble contrast. The pain of acute pericarditis is typically acute, sharp, severe, and constant (see Chapter 59, The Cardiomyopathies, Myocarditis, and Pericardial Disease). It is usually described as substernal, with radiation to the back, neck, or shoulders, and is exacerbated by lying down and by inspiration. It is classically described as being relieved by leaning forward. A pericardial friction rub is the most important diagnostic finding. The ECG may show diffuse ST-segment elevation and T-wave inversion. In addition, depression of the PR segment is a highly specific ECG finding for pericarditis. Pneumonia can produce chest pain or discomfort that is usually sharp and pleuritic (see Chapter 68, Community-Acquired Pneumonia, Aspiration Pneumonia, and Noninfectious Pulmonary Infiltrates). It is usually associated with fever, cough, and, possibly, hypoxia. Physical examination may reveal rales over the affected lobes, decreased breath sounds, and signs of consolidation (i.e., bronchial breath sounds). A chest radiograph confirms the diagnosis. Mitral valve prolapse is the most frequently diagnosed cardiac valvular abnormality and is more commonly diagnosed in women than in men. The discomfort of mitral valve prolapse often occurs at rest, is atypical for myocardial ischemia, and can be associated with dizziness, hyperventilation, anxiety, depression, palpitations, and fatigue (see Chapter 58, Valvular Emergencies). Discomfort may be related to papillary muscle tension, and many patients benefit from the administration of β-adrenergic blocking agents. Two-dimensional echocardiography is the diagnostic tool of choice and, with physical examination findings, helps to stratify patients into high- and low-risk categories for developing serious complications. Palpitations and every type of supraventricular or ventricular dysrhythmia have been associated with mitral valve prolapse. Musculoskeletal or chest wall pain syndromes are characterized by highly localized, sharp, positional chest pain. Pain that is completely reproducible by light to moderate palpation of a discrete area of the chest wall often represents pain of musculoskeletal origin, although chest wall tenderness occurs in some patients with pulmonary embolism and myocardial ischemia. Costochondritis is an inflammation of the costal cartilages and/or their sternal articulations and causes chest pain that is variably sharp, dull, and/or increased with respirations. Tietze syndrome is a particular cause of costochondral pain related to fusiform swelling in one or more upper costal cartilages and has a pain pattern similar to that of other costochondral syndromes. Xiphodynia is another inflammatory process that causes sharp, pleuritic chest pain reproduced by light palpation over the xiphoid process. Texidor twinge or precordial catch syndrome is described as a short, lancinating chest discomfort that occurs in episodic bunches lasting 1 to 2 minutes near the cardiac apex associated with inspiration and poor posture and inactivity. GI disorders cannot be reliably discriminated from myocardial ischemia by history and examination alone. Dyspepsia syndromes, including gastroesophageal reflux, often produce pain described as burning or gnawing, usually in the lower half of the chest, and often accompanied by a brackish or acidic taste in the back of the mouth (see Chapter 81, Peptic Ulcer Disease and Gastritis). The recumbent position usually exacerbates the symptoms, and although the pain is typically relieved with antacids, this therapeutic response also can be observed in myocardial ischemia. Esophageal spasm is often associated with reflux disease and is characterized by a sudden onset of dull, tight, or gripping substernal chest pain, frequently precipitated by the consumption of hot or cold liquids or a large food bolus and often lasting for hours (see Chapter 80, Esophageal Emergencies, Gastoesophageal Reflux Disease, and Swallowed Foreign Bodies). The pain may disappear with the administration of sublingual nitroglycerin, typically with a slight delay. Peptic ulcer disease is classically characterized as a postprandial, dull, boring pain in the midepigastric region (see Chapter 81, Peptic Ulcer Disease and Gastritis). Patients often describe being awakened from sleep by discomfort. Duodenal ulcer pain is usually relieved after eating food, in contrast to gastric ulcer symptoms, which are often exacerbated by eating. CHAPTER 52: Chest Pain: Cardiac or Not Symptomatic relief is usually provided by antacid medications. Acute pancreatitis and biliary tract disease present with right upper quadrant or epigastric pain and tenderness but also can cause chest pain. Panic disorder is a syndrome characterized by recurrent unexpected panic attacks (discrete periods of intense fear or discomfort) with at least four of the following symptoms: palpitations, diaphoresis, tremor, dyspnea, choking, chest pain or discomfort, nausea, dizziness, derealization or depersonalization, fear of losing control or dying, paresthesias, chills, or hot flushes. The diagnosis can be made only in the absence of direct physiologic effects of a substance disorder, a general medical condition, or symptoms better accounted for by another mental disorder. In a small trial, investigators found that ED physicians can successfully diagnose panic disorder by using a brief screening procedure, and they suggested that patients with panic could benefit from the initiation of specific pharmacologic therapy (serotonin reuptake inhibitors) in the ED21 (see Chapter 287, Panic Disorder). Many patients with panic disorder and other anxiety disorders have elevated baseline sympathetic tone that may be an independent risk factor for coronary artery disease. In fact, when all ED chest pain patients were screened for panic disorder, 25% of those screening positive had a discharge diagnosis of ACS (9.3%) or stable angina pectoris (15.7%).22 Thus, panic disorder must be considered a diagnosis of exclusion. ANCILLARY TESTING Ancillary testing in acute chest pain applies electrocardiography, laboratory testing, and imaging studies within the context of a focused, evidencebased approach to initially screen for, and subsequently distinguish, those with dangerous intrathoracic pathology from those with more benign conditions. Although the specific studies are chosen according to individual clinical circumstances, ACS is by far the most common serious cause of acute chest pain. Treatment is time dependent, and its presence cannot be excluded by history and exam alone. Accordingly, consensus guidelines and common practice direct the early, routine application of ECG and myocardial marker measurements for the early detection of ACS. The remainder of this chapter focuses on the indications, interpretations, and synthesis of ancillary testing during the initial assessment of undifferentiated chest pain in the ED. The subsequent application of either serial or continuous ECG monitoring, serial myocardial marker measurements, advanced imaging techniques and/or stress testing to definitively diagnose or exclude ACS or for risk stratification is the focus of Chapter 55, Low Probability Acute Coronary Syndrome. The chest radiograph is of limited value in the evaluation of ACS, but aids in detection and exclusion of a variety of other serious diagnoses. The appropriate utilization and interpretation of radiography and other diagnostic modalities in the evaluation of specific pathologic conditions (i.e., pulmonary embolism, aortic dissection, etc.) are discussed in detail in their respective chapters. ■ ECG Patients with chest pain or other symptoms suggestive of ACS should receive a 12-lead ECG upon ED presentation. The 2007 American College of Cardiology/American Heart Association Guidelines for Management of Patients with Unstable Angina/Non ST-Elevation MI recommend that an ECG “be performed and shown to an experienced emergency physician as soon as possible after ED arrival, with a goal of within 10 minutes of ED arrival for all patients with chest discomfort or other symptoms suggestive of ACS.”23 Although complete compliance with this guideline may be challenging in the resource-constrained environments of many high-volume EDs, delay in identification of high-risk ECG findings has been associated with increased inhospital mortality.24 ED systems that reduce delays to ST-elevation AMI identification improve guideline compliance and patient outcomes.25 About half (range, 13% to 69%) of patients with AMI have “diagnostic” changes on the initial ECG (new ST-segment elevation >1 mm in two contiguous leads),26 whereas another 20% to 30% have new ST-seg- 7-5 ment depression or T-wave inversion suggestive of myocardial ischemia. An additional 10% to 20% have ST-segment depressions and/or T-wave inversions similar to those seen on previous tracings. About 10% of patients with AMI present with nonspecific ST-segment (deviation <0.5 mm) and/or T-wave abnormalities (≤2 mm) while a minority (1% to 7%) will have a truly normal initial ECG.23,27 The sensitivity of the initial ECG in unstable angina is not well defined, because unstable angina is a clinical diagnosis. In addition, the initial ECG may normal if a patient with intermittent ischemia presents during a symptom-free period. The positive predictive value of different ECG patterns is well known. For new ST-segment elevation (≥1 mm in at least two contiguous leads), the positive predictive value for AMI is >90%, and patients with such ECG findings should be targeted for immediate reperfusion modalities. For new ST-segment depression and T-wave inversions, the positive predictive value is about 20% for AMI and between 14% and 43% for unstable angina. With acute chest pain and an initial ECG showing preexisting ST-segment depressions or T-wave inversions, the positive predictive value is about 4% for AMI and 21% to 48% for unstable angina. The initial 12-lead ECG has much greater diagnostic value when compared with a previous tracing and when evaluated in conjunction with clinical history. Risk stratification based on the initial ECG may also improve ED decision making. Although the initial ECG cannot exclude AMI , stable ED patients whose initial ECG is without ischemic changes or is unchanged from a previous ECG are at low risk of subsequent life-threatening complications and usually can be managed in a non–intensive care setting. Conversely, patients whose initial ECG demonstrates new ischemic changes (ST-segment depression or T-wave inversion), even in the absence of confirmed AMI, are at significantly greater risk of short- and long-term morbidity and mortality and should be managed accordingly. Variations on the standard 12-lead ECG technique have been proposed to improve the sensitivity for detection of ACS in the ED. ECGs with added leads—for a total of 15, 18, and 22 leads—have been studied in the ED setting, as has 80-lead ECG body surface mapping.28 Adding more leads increases the sensitivity for AMI detection. However, specificity is generally reduced, and, to date, there is inadequate evidence of positive therapeutic impact to justify routine use for most of these techniques. The exception is the use of supplemental ECG leads V7 through V9 (“posterior leads”) in patients with a clinical history suggestive of AMI whose initial ECG is nondiagnostic. This technique can detect isolated posterior ST-segment elevation in approximately 4% of AMI, and the presence of this finding does qualify these patients for acute reperfusion therapy as an acute STEMI.29,30 The diagnostic and prognostic value of the initial ECG is inherently limited by its single time point representation of a highly dynamic pathophysiologic process. Serial ECGs over the initial 2 to 3 hours of the patient’s presentation will significantly increase the sensitivity of ECG for AMI diagnosis and is therefore indicated whenever clinical suspicion of AMI is significant and the initial ECG is nondiagnostic. Continuous 12-lead ECG monitoring with computer-assisted ST-segment analysis can also identify patients with otherwise undetected ischemia. However, frequent false positive alarms can be problematic in a busy ED, and, to date, no large randomized trials have been conducted to determine if routine use of continuous ST-segment monitoring impacts overall patient outcome or is cost-effective.31 ■ SERUM MARKERS OF MYOCARDIAL INJURY Cardiac Troponins The troponin complex is the main protein of the thin filament of the myofibrils that regulate the Ca2+-dependent adenosine triphosphate (ATP) hydrolysis of actomyosin. The complex consists of three subunits: an inhibitory subunit, troponin I; a tropomyosin-binding subunit, troponin T; and a calcium-binding subunit, troponin C. Immunoassays have been developed for the cardiac-specific isoforms of both troponin I and troponin T, and an extensive body of literature now documents their diagnostic and prognostic value in a wide variety of clinical circumstances. Although troponin testing offers many advantages and is rapidly replacing the previously standard myocardial markers, such as SECTION 7: Cardiovascular Disease Conditions Associated with Elevated Troponin Levels in the Absence of Ischemic Heart Disease Cardiac contusion Cardioinvasive procedures (surgery, ablation, pacing, stenting) Acute or chronic congestive heart failure Aortic dissection Aortic valve disease Hypertrophic cardiomyopathy Arrhythmias (tachy- or brady-) Apical ballooning syndrome Rhabdomyolysis with cardiac injury Severe pulmonary hypertension, including pulmonary embolism Acute neurologic disease (e.g., stroke, subarachnoid hemorrhage) Myocardial infiltrative diseases (amyloid, sarcoid, hemochromatosis, scleroderma) Inflammatory cardiac diseases (myocarditis, endocarditis, pericarditis) Drug toxicity Respiratory failure Sepsis Burns Extreme exertion (e.g., endurance athletes) TABLE 52-5 peak between 12 and 24 hours, and return to normal between 3 and 4 days (Figure 52-1). The CK-MB isoenzyme curve parallels the total CK curve but peaks slightly earlier and is cleared more rapidly, usually within 48 hours (vs. 72 to 96 hours). Historically, CK-MB had been universally adopted as the gold standard for diagnosis of AMI. However, 37 conditions other than AMI have been associated with elevated CK-MB levels (Table 52-6), and it has now been largely replaced for routine use by the more sensitive and specific cardiac troponins. Despite this, an elevated CK-MB does have independent prognostic value, even among the small group of ED patients with a discordant (negative) troponin result. CK-MB testing may also be useful in the evaluation of patients with new or recurrent symptoms within 2 weeks of a previous cardiac event or cardiac procedure to diagnose infarct extension or reinfarction in the presence of a positive troponin. Myoglobin is a small (17,500 d), heme-containing protein found in skeletal and cardiac muscle. After AMI, serum myoglobin levels rise within 3 hours of symptoms and are elevated in 80% to 100% of patients at 6 to 8 100 cTnT 50 cTnI 15 MLC Myoglobin creatine kinase, subunits muscle and brain (CK-MB) and myoglobin, clinicians must maintain an accurate understanding of appropriate applications, proper results interpretation, and assay limitations. When highly sensitive assays are used, both troponin I and troponin T may be detectable in serum as early as 2 hours after AMI but are not reliably elevated in all patients until 6 to 12 hours. Levels reach their peak at 12 hours and remain elevated for 7 to 10 days, making troponin a uniquely useful test for patients with delayed presentations. However, the diagnosis of reinfarction or infarct extension must then be based upon an alternative marker (i.e., CK-MB) or recognition of a newly increasing pattern of troponin elevation. As troponin has greater cardiac specificity than CK-MB, either troponin I or troponin T is also a preferred marker in the setting of possible skeletal muscle injury, recent surgery, trauma, skeletal muscle disease, or cocaine use. Elevation of either troponin is associated with a higher risk of subsequent cardiovascular complications and mortality compared with those with a negative troponin test, independent of CK-MB and the ECG.32 Accordingly, the European College of Cardiology/American College of Cardiology Consensus Document on redefinition of MI declared that (when utilizing recent generations of troponin assays) “there is no discernible threshold below which an elevated value of cardiac troponin would be deemed harmless.”33 However, although it should never be ignored, an elevated troponin must always be considered within the clinical context of the patient’s presentation. Considered alone, an elevated troponin level does not diagnose the presence of coronary artery disease or identify any particular etiology of cell death. Indeed, elevated troponin levels have been documented in many clinical conditions in the absence of coronary artery disease, including, but not limited to, tachyarrhythmias, left ventricular hypertrophy, myocarditis, pericarditis, heart failure, pulmonary embolism, and sepsis (Table 52-5).34,35 Recognizing this, 2007 consensus guidelines recommends the term myocardial necrosis be applied to any patient with an elevation of troponin above the 99th percentile of normal while reserving the diagnosis of MI for those with troponin elevation and at least one of the following additional criteria: ischemic symptoms, new ST and T-wave changes, new left bundle-branch block, new Q-waves, or imaging evidence of a new loss of viable myocardium or new regional wall motion abnormality.32,34 In the ED, the clinical utility of troponin I and troponin T assays can generally be considered equivalent, although there are a few notable differences. Although only one troponin T assay exists, various manufacturers produce assays based on antibodies to several different troponin I fragments, resulting in significant heterogeneity in troponin I assay performance. In addition, the two tests perform differently in the setting of renal failure. Among patients with end-stage renal disease, a greater proportion will have an elevated troponin T (15% to 50%) compared with troponin I (<10%), and, after dialysis, serum levels of troponin T generally increase while troponin I levels decrease.36 The reasons for this paradox is not completely clear but likely relates to protein fractionation and differential clearance as well as other factors. Despite this, renal failure patients with a positive test for either troponin I or troponin T have been repeatedly and consistently shown to be at significantly higher risk for death and other adverse events compared with those with a negative test regardless of symptoms and across the entire spectrum of renal dysfunction. Thus, similar to patients with normal renal function, a positive troponin test in the setting of renal failure may or may not indicate the presence of coronary obstruction and must be considered within the individual patient’s clinical context but should never be dismissed as a “false positive” test. Creatine Kinase, Subunits, and Myoglobin Creatine kinase (CK; ATP creatine N-phosphotransferase) is an intracellular enzyme involved in the transfer of high-energy phosphate groups from ATP to creatine. The enzyme is a dimer of two subunits, which may be of the M (muscle) or the B (brain) type, thus creating three distinct isoenzymes: CK-BB, predominant in brain; CK-MM, mostly in skeletal muscle, and CK-MB. The “cardiac isoenzyme,” CK-MB is found in greater proportion in cardiac muscle but accounts for only 14% to 42 % of total cardiac muscle activity. Thus, the predominant enzyme in the heart is also CK-MM. CK levels become elevated within 4 to 8 hours after coronary artery occlusion, Multiples of the upper reference limit 7-6 10 CK-MB LD1 5 Reference interval 0 1 2 3 4 5 6 7 10 Days after onset of AMI FIGURE 52-1. Typical pattern of serum marker elevation after acute myocardial infarction (AMI). CK-MB = creatine kinase-MB isoenzyme; cTnI = cardiac troponin I; cTnT = cardiac troponin T; LD1 = lactate dehydrogenase isoenzyme 1; MLC = myosin light chain. CHAPTER 52: Chest Pain: Cardiac or Not TABLE 52-6 Conditions Associated with Elevated CK-MB Levels Common Uncommon Unclear Unstable angina, acute coronary ischemia Congestive heart failure Inflammatory heart diseases (pericarditis, myocarditis, endocarditis) Coronary artery disease after stress test Angina pectoris Valvular defects Tachycardia Cardiac catheterization Electrical countershock Noncardiac surgery Brain and head trauma Peripartum period Miscellaneous drug overdoses CO poisoning Prostatic cancer Acromegaly Hypothermia Rocky Mountain spotted fever Typhoid fever Chronic bronchitis Lumbago Febrile disorder Isolated rare case in normal person Cardiomyopathies Circulatory failure and shock Cardiac surgery Cardiac trauma Skeletal muscle trauma (severe) Dermatomyositis, polymyositis Muscular dystrophy, especially Duchenne Extreme exercise Malignant hyperthermia Reye syndrome Rhabdomyolysis of any cause Delirium tremens Ethanol poisoning (chronic) Abbreviation: CK-MB = creatine kinase, subunits muscle and brain. hours, peak at 4 to 9 hours (Figure 52-1), and, with normal kidney function, return to baseline within 24 hours. False positive results are common because myoglobin found in myocardium is indistinguishable from that found in skeletal muscle, and false negatives may occur if the test is performed after myoglobin has already been cleared from serum. Although still useful for rapid diagnosis of AMI among patients presenting soon after symptom onset, the improved sensitivity of successive generations of troponin assays reduces the need for routine use of this “early marker.” Natriuretic Peptides and Other Laboratory Markers B-type natriuretic peptide (BNP) is a neurohormone that rapidly and reproducibly appears in blood in response to increased ventricular wall tension and pressure overload. It is initially released by ventricular myocytes as the precursor molecule, pro-BNP, which is then enzymatically cleaved in an equimolar ratio into the 76 amino acid N-terminal pro-BNP (NTproBNP) and the 32 amino acid BNP. Physiologically, BNP decreases blood volume through natriuresis and decreases peripheral resistance through vasodilation, having the net effect of decreasing afterload on the heart. The half-life of BNP is approximately 20 minutes, and its clearance mechanism is believed to be by natriuretic receptor internalization and enzymatic degradation by a neutral endopeptidase in the blood stream. NTproBNP, conversely, has a plasma half-life of approximately 90 minutes, and is excreted by the kidneys.37 Although initially adopted into routine ED use as highly sensitive diagnostic and prognostic markers of heart failure, BNP and NTproBNP have also each been shown to have high diagnostic and prognostic sensitivity among ED patients with possible ACS.37 However, in this clinical context, both tests have limited specificity, resulting in many “false positives” for each additional “true positive” patient detected. Therefore, although of great value in the evaluation of dyspnea, these assays are not be recommended for routine use among ED chest pain patients either as a replacement for or a supplement to troponin testing.38 TREATMENT, DISPOSITION, AND FOLLOW-UP Treatment and disposition of the diseases and disorders discussed in this chapter is contained in the specific cardiac chapters that follow this one. 7-7 REFERENCES The complete reference list is available on the included DVD or online at www.placeholderurl.com