doi:10.1093/brain/aws065
Brain 2012: 135; 1370–1386
| 1370
BRAIN
A JOURNAL OF NEUROLOGY
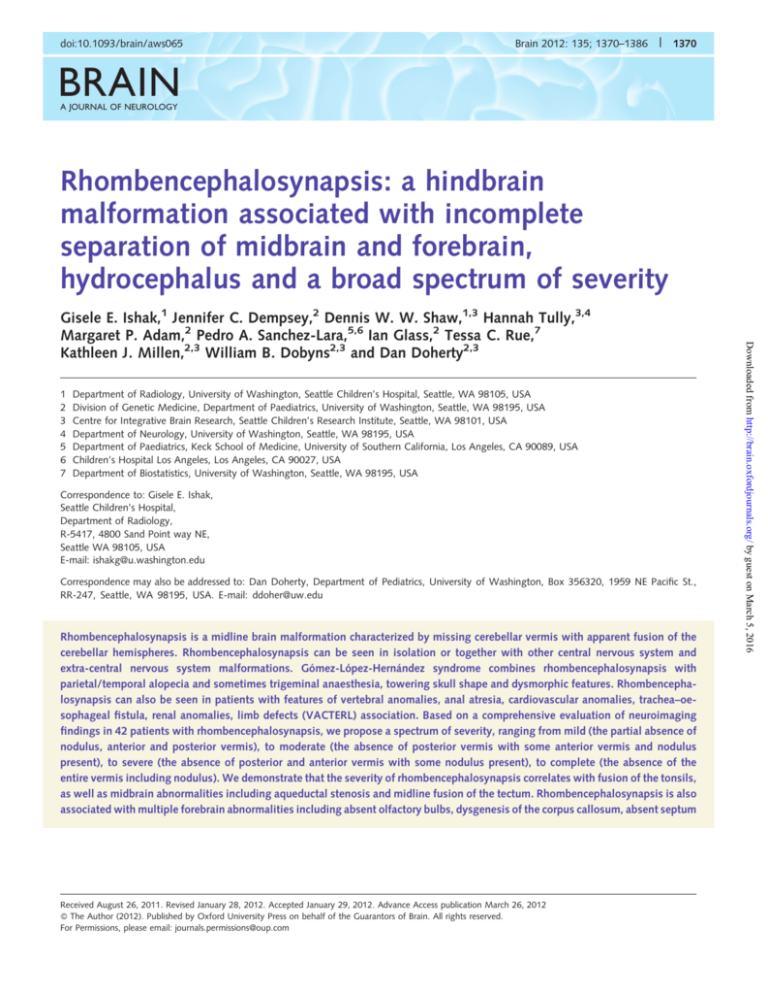
Rhombencephalosynapsis: a hindbrain
malformation associated with incomplete
separation of midbrain and forebrain,
hydrocephalus and a broad spectrum of severity
1
2
3
4
5
6
7
Department of Radiology, University of Washington, Seattle Children’s Hospital, Seattle, WA 98105, USA
Division of Genetic Medicine, Department of Paediatrics, University of Washington, Seattle, WA 98195, USA
Centre for Integrative Brain Research, Seattle Children’s Research Institute, Seattle, WA 98101, USA
Department of Neurology, University of Washington, Seattle, WA 98195, USA
Department of Paediatrics, Keck School of Medicine, University of Southern California, Los Angeles, CA 90089, USA
Children’s Hospital Los Angeles, Los Angeles, CA 90027, USA
Department of Biostatistics, University of Washington, Seattle, WA 98195, USA
Correspondence to: Gisele E. Ishak,
Seattle Children’s Hospital,
Department of Radiology,
R-5417, 4800 Sand Point way NE,
Seattle WA 98105, USA
E-mail: ishakg@u.washington.edu
Correspondence may also be addressed to: Dan Doherty, Department of Pediatrics, University of Washington, Box 356320, 1959 NE Pacific St.,
RR-247, Seattle, WA 98195, USA. E-mail: ddoher@uw.edu
Rhombencephalosynapsis is a midline brain malformation characterized by missing cerebellar vermis with apparent fusion of the
cerebellar hemispheres. Rhombencephalosynapsis can be seen in isolation or together with other central nervous system and
extra-central nervous system malformations. Gómez-López-Hernández syndrome combines rhombencephalosynapsis with
parietal/temporal alopecia and sometimes trigeminal anaesthesia, towering skull shape and dysmorphic features. Rhombencephalosynapsis can also be seen in patients with features of vertebral anomalies, anal atresia, cardiovascular anomalies, trachea–oesophageal fistula, renal anomalies, limb defects (VACTERL) association. Based on a comprehensive evaluation of neuroimaging
findings in 42 patients with rhombencephalosynapsis, we propose a spectrum of severity, ranging from mild (the partial absence of
nodulus, anterior and posterior vermis), to moderate (the absence of posterior vermis with some anterior vermis and nodulus
present), to severe (the absence of posterior and anterior vermis with some nodulus present), to complete (the absence of the
entire vermis including nodulus). We demonstrate that the severity of rhombencephalosynapsis correlates with fusion of the tonsils,
as well as midbrain abnormalities including aqueductal stenosis and midline fusion of the tectum. Rhombencephalosynapsis is also
associated with multiple forebrain abnormalities including absent olfactory bulbs, dysgenesis of the corpus callosum, absent septum
Received August 26, 2011. Revised January 28, 2012. Accepted January 29, 2012. Advance Access publication March 26, 2012
ß The Author (2012). Published by Oxford University Press on behalf of the Guarantors of Brain. All rights reserved.
For Permissions, please email: journals.permissions@oup.com
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Gisele E. Ishak,1 Jennifer C. Dempsey,2 Dennis W. W. Shaw,1,3 Hannah Tully,3,4
Margaret P. Adam,2 Pedro A. Sanchez-Lara,5,6 Ian Glass,2 Tessa C. Rue,7
Kathleen J. Millen,2,3 William B. Dobyns2,3 and Dan Doherty2,3
Rhombencephalosynapsis neuroimaging
Brain 2012: 135; 1370–1386
| 1371
pellucidum and, in rare patients, atypical forms of holoprosencephaly. The frequent association between rhombencephalosynapsis
and aqueductal stenosis prompted us to evaluate brain magnetic resonance images in other patients with aqueductal stenosis at our
institution, and remarkably, we identified rhombencephalosynapsis in 9%. Strikingly, subjects with more severe rhombencephalosynapsis have more severely abnormal neurodevelopmental outcome, as do subjects with holoprosencephaly and patients with
VACTERL features. In summary, our data provide improved diagnostic and prognostic information, and support disruption of dorsal–
ventral patterning as a mechanism underlying rhombencephalosynapsis.
Keywords: rhombencephalosynapsis; Gómez-López-Hernández syndrome; aqueductal stenosis; holoprosencephaly; hydrocephalus;
VACTERL
Abbreviations: DTI = diffusion tensor imaging; GLH = Gómez-López-Hernández syndrome; HPE = holoprosencephaly; NOS = not
otherwise specified; RES = rhombencephalosynapsis; VACTERL = vertebral anomalies, anal atresia, cardiovascular anomalies, trachea–
oesophageal fistula, renal anomalies, limb defects
Introduction
Materials and methods
We identified 10 patients with RES by searching the Seattle Children’s
Hospital imaging database, which contains all clinical MRI reports for
the 15 562 patients who had brain MRI studies between 2002 and
mid-2011. After noting a frequent association between RES and congenital aqueductal stenosis, we reviewed the MRIs for 56 patients with
aqueductal stenosis identified in the database and found five additional
patients with RES. We ascertained another 27 patients with RES by
referral from outside clinicians for a total of 42 patients. At Seattle
Children’s Hospital, MRIs were performed on Siemens Symphony 1.5
T, Siemens Avanto 1.5 T or Siemens Trio 3 T scanners. Imaging
sequences included sagittal and axial T1 spin echo, T2/FLAIR, diffusion
weighted and coronal T2 sequences. T1 MPRAGE (Magnetization
Prepared RApid Gradient Echo) was performed instead of spin echo
on the 3 T magnet. All outside imaging studies included sequences in
three planes, with the exception of Subject 27 for whom only limited
images were available. The Institutional Review Boards at Seattle
Children’s Hospital, the University of Washington and the University
of Chicago all approved this study.
The imaging studies were evaluated by two paediatric neuroradiologists and two paediatric neurogeneticists who arrived at consensus
for any structural abnormalities. The infratentorial evaluation included
qualitative assessment of the cerebellum for size (normal or hypoplastic), shape (superior and inferior ectopia), morphology (normal or folial
disorganization), patterns of vermian deficiency (nodulus, anterior or
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Rhombencephalosynapsis (RES) is a rare brain malformation
defined by midline fusion of the cerebellar hemispheres with partial or complete loss of the intervening vermis. RES occurs in
isolation or in combination with other CNS and extra-CNS malformations. The most common congenital anomaly syndrome
associated with RES is Gómez-López-Hernández (GLH) syndrome,
which is characterized by RES and scalp alopecia, as well as
abnormal head shape (usually turricephaly or tower skull), lowset and posteriorly angulated ears and trigeminal anaesthesia in
subsets of patients (Sukhudyan et al., 2010). While the prevalence
of RES is unknown, more than 90 individuals with RES have been
reported in the literature, including at least 25 with GLH (Gomy
et al., 2008; Fernandez-Jaen et al., 2009; Pasquier et al., 2009;
Poretti et al., 2009; Sukhudyan et al., 2010).
The aetiology of RES is unknown. One hypothesis is that RES is
caused by dorsal–ventral patterning defects that result in loss of
midline and fusion of lateral structures (Sarnat, 2000; Yachnis,
2002). Alternatively, RES could represent loss of anterior cerebellar
anlage cells destined to become the vermis, or from transformation of these anterior cells to a more posterior and/or ventral
hemispheric fate. The cerebellar fusion is in some ways comparable with holoprosencephaly (HPE) in the forebrain, and indeed,
these two malformations have been reported in multiple patients,
suggesting a shared, but unknown, developmental mechanism
(Siebert et al., 2005; Pasquier et al., 2009). Understanding the
developmental mechanism(s) for RES is hampered by the paucity
of known genetic causes and the lack of an animal model.
Although Ramocki et al. (2011) recently reported ZIC2 mutations
in sisters with RES and HPE (Ramocki et al., 2011), the RES diagnosis has come into question (Guleria, 2011); therefore, no single
gene cause of RES has been conclusively reported. Several observations are consistent with a genetic basis for RES: (i) recurrence in
brothers (Pasquier et al., 2009; Ramocki et al., 2011); (ii) affected
children with non-recurrent chromosomal abnormalities including
interstitial deletion of 2q (Truwit et al., 1991), unbalanced
translocation of 2p and 10q (Lespinasse et al., 2004), tetrasomy
9p (di Vera et al., 2008), deletion of 7q and duplication of 1p
(Pasquier et al., 2009); (iii) parental consanguinity in at least four
families; and (iv) highly reproducible clinical features. However, a
large majority of patients with RES, and especially GLH, are sporadic, suggesting de novo autosomal dominant mutations as the
most common cause (Romanengo et al., 1997; Toelle et al.,
2002; Sandalcioglu et al., 2006; Chemli et al., 2007). RES has
been associated with other brain abnormalities (Kepes et al.,
1969; Michaud et al., 1982; Schachenmayr and Friede, 1982;
Isaac and Best, 1987; Savolaine et al., 1991; Truwit et al.,
1991; Simmons et al., 1993; Boltenstern et al., 1995; Demaerel
et al., 1995; Shaw, 1995; Sergi et al., 1997; Utsunomiya et al.,
1998; Sener, 2000; Jellinger, 2002, 2009; Toelle et al., 2002;
Yachnis, 2002; Boltshauser, 2004; Pavone et al., 2005; Siebert
et al., 2005; Chemli et al., 2007; Pasquier et al., 2009), but no
large post-natal series exists to determine the spectrum and
prevalence of associated imaging features and neurodevelopmental outcomes.
1372
| Brain 2012: 135; 1370–1386
(i) GLH: subjects with RES and scalp alopecia (usually temporal or
parietal), with or without trigeminal anaesthesia, abnormal head
shape, midface hypoplasia, low-set and/or posteriorly rotated
ears, telecanthus and/or hypertelorism.
(ii) RES + VACTERL features: subjects with RES plus at least one of:
vertebral, cardiac, limb or renal structural abnormalities, without
scalp alopecia.
(iii) RES + HPE: subjects with RES plus focal or diffuse interhemispheric cerebral fusion without alopecia or vertebral, cardiac,
limb or renal structural abnormalities.
(iv) RES NOS (not otherwise specified): subjects who did not fit into
the categories above, many of whom had RES with abnormal
head shape, midface hypoplasia, low-set and/or posteriorly
rotated ears, telecanthus and/or hypertelorism.
Statistical analysis was performed using SAS, version 9.3 (SAS
Institute). An exact test of Kendall’s tau-b statistic was used to compare two ordinal variables (RES severity and neurodevelopmental
outcome severity), while Fisher’s exact test was used to compare
non-ordered categorical variables (clinical category) (Kendall, 1938).
Results
As described above, we reviewed imaging studies from 42 subjects
(17 females, 25 males) ranging in age from 2 days to 44 years (at
the time of the MRI) with a partial or complete absence of the
cerebellar vermis and fusion of the hemispheres. Thirty-seven of
the subjects were diagnosed with RES by their treating clinicians,
while an additional five subjects (Subjects 25, 26, 28, 29 and 40)
with a range of RES severity were identified after review of 56
local patients with aqueductal stenosis.
Hindbrain
Cerebellar fusion
In the literature, RES has been characterized as partial or complete,
but the pattern of cerebellar fusion has not been described. In our
subjects, we found a spectrum of cerebellar fusion in which the
posterior vermis was most severely involved, followed by the anterior vermis and then the nodulus. Based on this observation, we
were able to group all but four of our subjects into the following
categories, ordered by severity (Fig. 2 and Table 1):
(1) complete (n = 9): absence of all parts of the vermis
(Fig. 2A–E);
(2) partial–severe (n = 9): absence of the posterior and anterior
vermis, with a distinct nodulus still seen although it may be
variably underdeveloped (Fig. 2F–J);
(3) partial–moderate (n = 8): absence of the posterior vermis
and variable deficiency of the anterior vermis and nodulus
(Fig. 2K–O);
(4) partial–mild (n = 12): fusion of the central part of the vermis—mostly involving the posterior vermis—with some anterior vermis seen above the fusion and posterior vermis and
nodulus seen below the fusion (Fig. 2P–T);
(5) atypical (n = 4): absence of the posterior vermis and nodulus
with some residual anterior vermis.
Box 1 Definition of key imaging features
Fusion of the cerebellum: continuity of the folia and white matter across the midline without a recognizable transition to vermis and
hypoplasia or absence of the posterior cerebellar incisura and vallecula (Fig. 1A and B).
Posterior vermis: midline cerebellar tissue posterior (caudal) to the primary fissure. In complete RES, it is absent. In partial RES, it is
present (although frequently hypoplastic) at the position of the uvula, just caudal and dorsal to the nodulus (Fig. 1C and F).
Anterior vermis: midline cerebellar tissue anterior (rostral) to the primary fissure. In complete RES, it is absent. In partial RES, it is
variably deficient, being present at the most cranial and ventral aspect of the vermis, just posterior to the superior cerebellar
peduncle at the level of junction of the cerebral aqueduct and fourth ventricle (Fig. 1D).
Nodulus: midline cerebellar tissue just caudal to the fastigium. On the coronal image, it is a thumb-like projection from the floor of
the fourth ventricle. On axial images, it is typically seen in the same plane as the flocculi, except when this region is distorted by
superior ectopia (Fig. 1E and F)
Pons hypoplasia: subjectively small dorsal–ventral dimension of the pons.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
posterior vermis deficiency), the posterior fossa for size (normal or
small) and the fourth ventricle for shape (normal or abnormal shape
such as keyhole appearance). On sagittal and axial images, we evaluated the superior cerebellar peduncles for orientation of their confluence and for the presence of ectopic tissue, the superior medullary
velum for thickness and the presence of ectopic tissue, the posterior
commissure for thickness, the cerebral aqueduct for patency and the
pons for size (normal, flat, mild or moderately hypoplastic). On axial,
coronal and sagittal images, we evaluated the inferior and superior
colliculi (normal, fused across the midline, fused craniocaudally, the
presence of ectopic tissue).
Within the supratentorium, we evaluated for interhemispheric cerebral fusion, migrational disorder (the presence of polymicrogyria and
heterotopia), septum pellucidum (present or absent), corpus callosum
(normal, thinning, agenesis, dysgenesis), fornices (normal or fused),
mamillary bodies (normal or hypoplastic/absent), pituitary gland (present or absent), olfactory bulbs (present or absent) and ventricles
(normal or dilated). Definitions of key imaging features are listed in
Box 1.
Clinical information was collected using a structured intake form
and review of medical records. Blinded to the imaging results, two
authors (J.D. and D.D) classified the abnormal neurodevelopmental
outcome for each subject as mild, moderate or severe, according to
the criteria listed in Supplementary Table 1. Based on the literature, we
divided the subjects into four clinical categories using the following
criteria:
G. E. Ishak et al.
Rhombencephalosynapsis neuroimaging
Brain 2012: 135; 1370–1386
| 1373
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Figure 1 Typical neuroradiological findings in RES. (A and B) Fusion of the cerebellar hemispheres with continuity of the cerebellar folia
and white matter across the midline in Subject 9 (A) and Subject 18 (B). Note the abnormal shape of the fourth ventricle in A. The
cerebellum is pear shaped in B, consistent with mild superior herniation. (C) Residual posterior vermis (white arrowhead points to uvula) in
Subject 28. (D) Residual anterior vermis in Subject 28 (black arrowhead). (E) Substantial residual nodulus (black arrow) in Subject 18. (F)
Hypoplastic residual nodulus (black arrow) in Subject 32. Note the residual posterior vermis (white arrow) that is continuous superiorly
with the nodulus (black arrow), as well as ectopic tissue within the cerebral aqueduct at the level of the inferior colliculus. T = Tonsil. (A, C
and D) axial T2; (B) coronal T2; (E and F) sagittal T1.
1374
| Brain 2012: 135; 1370–1386
G. E. Ishak et al.
aqueductal stenosis and intraventricular cysts (D). (F–J) Severe partial RES in Subject 2. The nodulus (arrow) is present and projects into the
4th ventricle on the coronal image (I) and the tonsils are fused (F). Note the absent septum pellucidum, narrow transverse diameter of the
cerebellum and the small posterior fossa. (K–O) Moderate partial RES in Subject 18. The nodulus (arrow) and anterior vermis (black
arrowhead) are present. Note the absent septum pellucidum in (N). (P–T) Mild partial RES in Subject 6. The nodulus (arrows) is present but
deficient. Anterior (black arrowhead) and posterior (white arrowhead) vermis is also present. The primary fissure is indistinct on the sagittal
images (E, J, O and T). (A–C, K–M and P–R) axial T2 ranging from caudal to rostral; (F–H) axial T1 ranging from caudal to rostral; (D, N
and S) coronal T2; (I) coronal T1; (E, J, O and T) sagittal T1. Lower case alphabets in E, J, O and T refer to the level of sections of the
corresponding axial images labeled with upper case alphabets.
The nodulus was present in 29/33 subjects with partial RES; however, it was severely hypoplastic in Subjects 6, 11, 28, 32 and 37.
Portions of the anterior vermis were seen in 24/33 subjects with
partial RES and portions of the posterior vermis were seen in 12/33
subjects. While fusion of the dentate nuclei has been described in
pathology specimens and occasionally by imaging, the dentate nuclei
were not visualized well enough to include in our analysis. Fusion of
the tonsils strongly correlated with severity of cerebellar hemisphere
fusion. The severity of RES did not correlate with the clinical categories as defined in the ‘Materials and methods’ section (GLH,
RES + VACTERL features, RES + HPE and RES NOS). Note that
RES + VACTERL features do not indicate that a patient meets criteria
for VACTERL, just that they have at least one feature associated with
this condition. Although the severe and complete groups had more
females, this was not statistically significant, nor was sex associated
with clinical category.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Figure 2 Spectrum of severity in RES. (A–E) Complete RES without residual vermis in Subject 17. Note the absent septum pellucidum,
Rhombencephalosynapsis neuroimaging
| 1375
Brain 2012: 135; 1370–1386
Table 1 Extent of cerebellar fusion and cerebellar ectopia in subjects with RES
Subject
MRI age
Sex
Clinical
categorya
RES
severity
NDV
outcome
NDV
outcome
age
Absent
post
vermis
Absent
ant
vermis
Absent
nodulus
Tonsil
fusion
Ectopiab
1
8
15
17
27
35
36
38
41
2 days
6 days
0 days
5 days
19 m
2 days
10 m
25 days
18 days
Unknown
Mod
Severe
Mild
Mod
Severe
Mod
Mild
Mild
Totals
Mod
Mild
Mod
Mod
Unknown
Severe
Severe
Mod
Mild
Totals
Unknown
Mod
Mild
Severe
Mild
Mild
Mild
Mild
Totals
Unknown
Mild
Mild
Mild
Mild
Mild
Mild
Mod
Mod
Unknown
Mild
Mild
Totals
Mild
Severe
Mild
Mod
10 m
3 yrs 6m
3 yrs
4 yrs 5m
2 yrs
Deceased
1 yr 7 m
13 m
16 m
+
+
+
+
+
+
+
+
+
9/9
+
+
+
+
NA
+
+
+
+
8/9
+
+
+
+
+
+
+
+
8/8
+
+
+
+
+
+
+
+
+
9/9
+
+
+
+
+
+
+
+
+
9/9
+
+
+
+
+
+
+
+
+
9/9
+
+
S
9 m
5 m
2 yrs 3 m
26 yrs
16 m
17 m
14 m
1 days
6 days
RES NOS
GLH
HPEc
GLH
RES NOS
HPE
VACTERL featuresd
RES NOS
GLH
Female
GLH
GLH
GLH
RES NOS
RES NOS
RES NOS
VACTERL featurese
RES NOS
GLH
Female
GLH
HPE MIF
RES NOS
VACTERL features
GLH
GLHf
GLH
RES NOS
Female
GLH
GLH
GLH
GLH
RES NOS
RES NOS
RES NOS
GLH
VACTERL features
Unknown
GLH
RES NOS
Female
RES NOSg
VACTERL features
GLH
RES NOS
Complete
Complete
Complete
Complete
Complete
Complete
Complete
Complete
Complete
2
3
5
10
13
20
21
26
31
F
F
F
M
M
M
F
F
M
56%
F
F
F
M
M
M
M
F
F
56%
M
M
F
M
M
M
M
M
12%
M
M
F
M
F
F
M
M
M
M
M
F
33%
M
F
M
F
2 yrs 11 m
1 yrs 3 m
7 weeks
4 yrs
9 m
3 days
3 yrs 10 m
17 m
4
6
7
9
11
16
23
28
29
30
32
37
5 weeks
19 m
2 yrs
6 yrs 9 m
15 m
44 yrs
10 m
3 yrs 3 m
16 yrs
6 yrs 2 m
3 yrs 2 m
3 yrs 9 m
22
33
34
40
11 yrs 11 m
6 yrs 6 m
22 m
6 days
Moderate
Moderate
Moderate
Moderate
Moderate
Moderate
Moderate
Moderate
Mild
Mild
Mild
Mild
Mild
Mild
Mild
Mild
Mild
Mild
Mild
Mild
Atypical
Atypical
Atypical
Atypical
3 yrs
22 m
5 yrs 6 m
29 yrs 2 m
2 yrs
6 yrs 6 m
3 yrs 10 m
5 yrs 9 m
6 yrs 1 m
4 yrs 6
8 yrs 1
8 yrs 3
8 yrs 5
6 yrs 5
27 m
4 yrs 6
2 yrs
m
m
m
m
m
m
+
+
0/9
+
+
0/8
0/8
5 m
6 yrs 2 m
6 yrs 5 m
14 yrs 5 m
6 yrs 11 m
44 yrs
2 yrs
4 yrs 4 m
17 yrs
Unknown
5 yrs 2 m
4 yrs
7 yrs 3 m
12 yrs
5 yrs 6 m
9 yrs
+
6/9
2/8
S
NA
S
I
4/8
B
S
S
B
B
S
B
S
8/9
B
B
S
B
S
S
I
7/8
I
p
0/12
+
+
+
+
0/12
0/12
+
+
+
+
+ = abnormality present;
= abnormality not present; yrs = years; m = month; p = partial; NA = Not Available; NDV = Neurodevelopmental.
a See definitions in ‘Materials and methods’ section.
b B = both inferior and superior; I = inferior only (Chiari I); S = superior only.
c Subject had rib and vertebral anomalies.
d Subject had bitemporal hair thinning but not alopecia.
e Subject had crossed renal ectopia but not vertebral, rib, heart, or limb malformations.
f Subject had mutation-confirmed neurofibromatosis I.
g Subject had microtia, corneal scarring and ectopic salivary gland tissue (Adam et al., 2007).
1/12
p
p
+
+
S
B
S
S
S
S
7/12
S
S
S
B
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
12
14
18
19
24
25
39
42
Severe
Severe
Severe
Severe
Severe
Severe
Severe
Severe
Severe
NA
+
+
+
+
6/8
+
+
+
1376
| Brain 2012: 135; 1370–1386
Posterior fossa
The posterior fossa was small in all patients with complete RES, reflected by a subjectively small transverse diameter and to a lesser
extent small anterior–posterior diameter. This correlated with the
severity of the cerebellar hemisphere hypoplasia. In partial RES, the
transverse diameter was variably small in 8/9 patients with severe
fusion, 6/8 with moderate fusion, 3/12 with mild fusion and 4/4 with
atypical fusion. It is unclear whether the small posterior fossa size
reflects abnormal development of the bony posterior fossa associated with turricephaly, or is secondary to hydrocephalus (and expansion of the supratentorial calvarium), shunting and subsequent
distortion, or a combination of the above.
Cerebellar size and ectopia
Pons
The pons was abnormal in only 10 subjects: flat in Subjects 8, 38, 40
and 41 (who also had severe cerebellar hypoplasia), moderately
hypoplastic in Subjects 31 and 36 and mildly hypoplastic in
Subjects 4, 16, 17 and 20. The pons appeared compressed rather
than hypoplastic in Subjects 12 and 14, possibly due to the small
posterior fossa in these subjects. In contrast, Subject 20 also had a
very small posterior fossa but the pons appeared mildly hypoplastic
rather than compressed. The basilar sulcus of the pons was present in
all but one subject (Subject 1), indicating that the ventral midline was
generally intact. We were unable to consistently evaluate the cranial
nerves due to limitations in the imaging.
Superior cerebellar peduncles and
midbrain
We identified superior cerebellar peduncle abnormalities in 19 of
42 subjects and midbrain abnormalities (aqueductal stenosis and
fusion of the colliculi) in 22 of 42 subjects. The severity of the
midbrain abnormalities roughly correlated with the severity of RES
(Table 2). In addition, the three subjects with holoprosencephaly
and 3/5 subjects with VACTERL features had aqueductal stenosis
and fused colliculi.
Table 2 Superior cerebellar peduncle and midbrain
abnormalities correlate with severity of RES
Subject
Abnormal
SCP
Fused
colliculi
Aqueductal
stenosis
Level of
obstruction
1
8
15
17
27
35
36
38
41
Totals
3
2
5
10
13
20
21
26
31
Totals
12
14
18
19
24
25
39
42
Totals
4
6
7
9
11
16
23
28
29
30
32
37
Totals
22
33
34
40
+
+
+
+
PC, SC, IC, V, SCP
IC
PC, SC, IC, V, SCP
SCP
NA
PC, SC, IC, V, SCP
+
+
NA
+
NA
+
(+)
+
+
+
+
+
+
+
8/9
IC, V
SC, IC
4/8
+
+
6/8
+
V, SCP
+
+
IC
+
+
+
+
5/9
PC, SC, IC, V, SCP
SC, IC, V
SC, IC
IC, V
+
+
+
+
+
6/9
+
+
+
+
SC, IC, V
+
SCP
+
3/8
+
5/8
IC, V
+
+
+
SC
SC, IC
2/12
1/12
2/12
+
+
+
+
+
+
+
+
+
+
+
7/9
+
+
+
+
4/8
a
SC, IC
+
+
SC, IC
+ = abnormality present;
= abnormality not present; (+) = Aqueduct did not
appear patent but the ventriculomegaly was mild; IC = inferior colliculus;
PC = posterior commissure; SC = superior colliculus; SCP = superior cerebellar
peduncle; V = superior medullary velum.
a Deformed tectum with midbrain hypoplasia.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Cerebellar hypoplasia was noted predominantly in subjects with
complete RES; however, in subjects with partial RES, the transverse diameter of the cerebellum was small, with preserved or
even increased craniocaudal dimension. We observed ectopia of
the cerebellum superiorly through the tentorial notch in 25 subjects, resulting in a striking pear shape (Shaw, 1995; Pasquier
et al., 2009) on coronal images (Fig. 1B). Superior ectopia was
not associated with the severity of RES. It is also unlikely to represent simple upward herniation due to shunted hydrocephalus,
since several subjects with no/mild ventriculomegaly (Subjects 3,
5, 9, 22, 24, 30 and 32) and several with unshunted moderate
ventriculomegaly (Subjects 1, 13, 23 and 33) had superior ectopia.
In addition, Subjects 25 and 31 had superior ectopia before shunting. Subjects 4 (with non-shunted mild/moderate ventriculomegaly) and 8 (with shunted hydrocephalus) did not have superior
ectopia, potentially due to a quadrigeminal plate cistern cyst and a
superior posterior fossa cyst, respectively, while Subject 10 had
shunted hydrocephalus without superior ectopia without an obvious reason. In contrast, superior ectopia was worse after shunting
in Subjects 17, 20, 21, 25, 26 and 28. Inferior cerebellar ectopia
was present in 10 subjects. Although cerebellar dysplasia was rare,
Subjects 5 and 21 had abnormal foliation of the cerebellar hemispheres at the cranial midline and right para-midline, respectively.
G. E. Ishak et al.
Rhombencephalosynapsis neuroimaging
Aqueduct and superior cerebellar peduncles
Aqueductal stenosis was present in 22/42 subjects and was
strongly associated with the degree of cerebellar fusion
(Table 2). Patency of the aqueduct was compromised at the
level of the superior (Fig. 3A and B) or inferior colliculus
(Fig. 3C and D), or more caudally at the level of the superior
cerebellar peduncles (Fig. 4). All subjects with aqueductal stenosis
had fusion of the overlying structures at the level of obstruction
Brain 2012: 135; 1370–1386
| 1377
except Subject 28, in whom the superior colliculus did not appear
to be fused, and in Subject 12 who had aqueductal stenosis at the
most superior aspect of the aqueduct with a deformed tectum. In
eight subjects (Subjects 1, 2, 15, 20, 21, 31, 19 and 42), the
superior medullary velum also appeared thickened, with
non-visualization or severe narrowing of the aqueduct at that
level (Fig. 3E and F). In four subjects (Subjects 1, 15, 20 and
35), the aqueductal stenosis was more diffuse, extending from
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Figure 3 Aqueductal stenosis in RES. (A and B) Obstruction at the level of the superior colliculi (white arrow in A and black arrow in B),
which are fused across the midline in Subject 29. Note the shunted hydrocephalus and severely dysgenetic corpus callosum with intact
rostrum. (C and D) Obstruction at the level of the inferior colliculi (arrowheads), which are fused across the midline in Subject 8. Note the
severe hydrocephalus with funnelling of the aqueduct, the retrocerebellar fluid collection and hypoplasia of the cerebellum and pons.
(E and F) Obstruction at the junction of the aqueduct and fourth ventricle in Subject 2. The superior medullary velum is thickened (white
arrow) and the superior cerebellar peduncles are angled medially. Note the mild inferior cerebellar ectopia in (E). Note the tiny focus of low
signal within the superior aspect of the fourth ventricle (adjacent to the white arrow in F) and within the lateral ventricles in E is related to
air from recent shunt manipulation. (G–I) Obstruction from the level of the thickened posterior commissure (bracket) to the level of the
superior cerebellar peduncles with midline fusion of the superior colliculi (black arrow) in Subject 1. Note partial agenesis of the corpus
callosum in (G) and the absence of hydrocephalus, despite complete obliteration of the cerebral aqueduct on imaging. Note also the
severely hypoplastic mammillary bodies in Subjects 8, 2 and 1 (long white arrows in C, E and G). (A, C, E and G) sagittal T1; (B, F and I)
axial T1; (D, H) axial T2.
1378
| Brain 2012: 135; 1370–1386
G. E. Ishak et al.
anterior vermis (arrows) that extends just posterior to the confluence of the superior cerebellar peduncles. The superior medullary velum is
seen superior to the arrow in (B), and inferior to the inferior colliculus. (C and D) Subject 39, partial RES. There is anterior vermis that
extends beyond the confluence of the superior cerebellar peduncles into the most caudal aspect of the cerebral aqueduct, reflecting a
more severe pattern of ectopic tissue. No associated aqueductal stenosis. The superior medullary velum is not seen in this case, which may
relate to the extent of the ectopic cerebellar tissue, in addition to thick slices. (E and F) Subject 17, complete RES. The anterior vermis is not
visualized in this case, however, small ectopic tissue is seen at—and obscuring—the confluence of the superior cerebellar peduncles, which
appear fused at the midline. This is causing obstruction at the most caudal aspect of the cerebral aqueduct. The superior medullary velum is
present superior to the arrow in (F). After shunting, the subject developed an intraventricular cyst (asterisk).
the level of the superior cerebellar peduncle up to the posterior
commissure (Fig. 3G–I). In particular, Subject 15, and to a lesser
extent Subject 35, had a mass-like fusion of all of the midbrain
including the superior cerebellar peduncle, superior medullary
velum, inferior colliculus, superior colliculus—as noted by other
authors (Garfinkle, 1996; Pasquier et al., 2009)—and extending
cranially with fusion of the thalami and hypothalami (Fig. 5A and
B). We did not observe deficiency of the superior medullary velum
as described previously (Gross, 1959; Barth, 2008).
In 19 subjects, the superior cerebellar peduncles were closer to
the midline than normal and angled more medially (Fig. 4). This
abnormal superior cerebellar peduncle configuration was accompanied by several different patterns of abnormalities of the
aqueduct.
(1) Non-visualization of the entire aqueduct, associated with
thickening of the posterior commissure and superior medullary velum, and midline fusion of the superior and inferior
colliculi, in Subjects 1, 15, 20 and 35 (discussed below).
(2) Narrowing of the aqueduct at the level of the tectum in
Subjects 10, 19, 21, 31, 40 and 42 (Table 2).
(3) Aqueductal stenosis at the level of the superior cerebellar
peduncles caused by a small focus of ectopic tissue seen at
the convergence of the superior cerebellar peduncles in
Subjects 2, 17 and 25 (Fig. 4E and F). In Subjects 2 and
25 (and in Subjects 34 and 39 described below), this tissue
appeared to be foliated and continuous with the anterior
vermis, so it could represent ectopic cerebellum.
(4) Absence of aqueductal stenosis in Subjects 5, 6, 9, 13, 34
and 39, despite ectopic tissue at the convergence of the
superior cerebellar peduncles in Subject 34 (Fig. 4A and B)
and within the aqueduct in Subject 39 (Fig. 4C and D).
Tectum
Fusion of the tectum across the midline, defined as the absence of
the two prominences of the superior and/or inferior colliculi on
axial images (Fig. 3B, D and I), was present in 16 subjects
(Subjects 1, 8, 10, 14, 15, 19–21, 26, 29, 31, 35, 38, 40, 41
and 42). Craniocaudal fusion of the colliculi was demonstrated
on sagittal sections in at least four subjects (Subjects 1, 20, 21
and 40). This may under-represent the true frequency, as craniocaudal fusion may be difficult to identify when the sagittal sections
are not thin enough. In contrast, Subject 32 had ectopic tissue
within the cerebral aqueduct seen on thin cuts at the level of
the inferior colliculus, without collicular fusion, as noted by other
authors (Takano et al., 2010). The absence of ventriculomegaly
and funnelling of the aqueduct excluded aqueductal stenosis in
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Figure 4 Ectopic cerebellar tissue and superior cerebellar peduncle configuration in RES. (A and B) Subject 34, partial RES. There is
Rhombencephalosynapsis neuroimaging
Brain 2012: 135; 1370–1386
| 1379
hypothalamus (A) with occipital holoprosencephaly (black arrow) and aplasia of the ventricles (B) in Subject 15. (C) Middle interhemispheric fusion (arrowhead) in Subject 14. (D) Absent olfactory bulbs in Subject 17 (white arrows). (A) coronal T2; (B) axial T1; (C) sagittal
T1; (D) axial T2.
this subject. Subject 12 had deformed tectum with the absence of
fusion of the colliculi and hypoplasia of the midbrain.
Forebrain
Ventriculomegaly and hydrocephalus
Almost half of the subjects (19/42) had obstructive hydrocephalus
due to aqueductal stenosis requiring shunting (Table 3). Of the
other subjects, two had moderate, four had mild and 17 had no
ventriculomegaly. Of note, the aqueduct did not appear patent in
three subjects; Subject 1 had mild ventriculomegaly and Subjects
15 and 35 did not have visible lateral ventricles, as noted by other
authors (Garfinkle, 1996) (Fig. 5B). The severity of ventriculomegaly/hydrocephalus was not strongly correlated with severity of
RES or the clinical diagnosis.
Other forebrain abnormalities
Although hydrocephalus can account for a number of the forebrain imaging abnormalities, our data support a role for primary
forebrain developmental defects as well, since a number the
abnormalities were seen in subjects without hydrocephalus and
some of the abnormalities are not typically caused by hydrocephalus. The septum pellucidum was absent in 26 subjects, including
all with obstructive hydrocephalus (Table 3). It was also absent in
four subjects with ventriculomegaly (three with mild, one with
mild/moderate) and three without ventriculomegaly. To
determine whether the septum forms and later disappears, we
evaluated prenatal imaging in two subjects with mild ventriculomegaly (Subjects 18 and 23). Subject 18 had a normal septum
pellucidum at 22 weeks gestation that was then partially deficient
at 32 weeks. The ventricles were at worst moderately dilated
(16 mm atrial measurement) in utero and only mildly dilated on
post-natal imaging. Subject 23 had a partially absent septum
posteriorly on foetal MRI at 18 weeks gestation with moderate
ventriculomegaly (16 mm atrial measurement). A cranial ultrasound at birth revealed a partially absent septum with mild prominence of the ventricles, but the septum was completely absent on
MRI by 1 month of age.
The corpus callosum was abnormal in 30/41 subjects with
adequate imaging (Table 4). Most commonly, the corpus callosum
was severely thinned and dysplastic in association with obstructive
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Figure 5 Supratentorial abnormalities associated with RES. (A and B) Mass-like fusion of the mesencephalon, diencephalon and
1380
| Brain 2012: 135; 1370–1386
G. E. Ishak et al.
Table 3 Forebrain features in subjects with RES
Aqueductal
stenosis
VM
Absent
septum
1
8
15
17
27
35
36
38
41
Totals
3
2
5
10
13
20
21
26
31
Totals
12
14
18
19
24
25
39
42
Totals
4
6
7
9
11
16
23
28
29
30
32
37
Totals
22
33
34
40
+b
+
+
+
+
+
+
+++
*
+++
+++
*
+
+
NA
+
+
NA
NA
NA
+
+
8/9
+++
+++
6/9
+
+
6/8
+
+++
+
+
++
++
++
++
++
++
7/9
++
++
+
++
+
+++
+
5/8
+++
6/8
++
+
+
+
+
6/9
+
+
Abnormal
temporal
cortex
Abnormal
mammillary
bodiesa
Fused
fornices
+
+
NA
+
NA
NA
+
+
NA
+
NA
NA
+
NA
NA
+
+
2/6
+
+
NA
+
NA
NA
+
+
+
6/6
+
+
5/6
+
+
5/6
+
3/7
+
+
+
+
+
+
+
+
+
+
+
+
+
+
+
+
6/9
+
+
+
+
+
+
+
+
+
+
+
+
+
7/9
+
+
+
+
+
+
7/8
+
Abnormal
anterior
commissure
NA
5/9
+
+
+
3/9
+
+
+
+
4/8
+
+
+
+
5/8
+
+
+
NA
NA
+
+
+
3/8
Single
+
+
NA
+
+
+
+
4/8
4/7
+
+
Absent
olfactory
bulbs
NA
1/7
+
+
NA
2/7
+
+
+
+
+
NA
NA
NA
+
+
+
+++
+++
+
+
+
+
+
+
+
+
2/12
4/12
5/12
4/11
5/12
+
+
+++
+
+
Single
0/12
4/12
+
+
+
+
+
+
3/10
+
+
+
+
+
NA = not available; single = single unilateral fornix (rather than midline fusion); + = abnormality present;
= abnormality not present; VM = ventriculomegaly.
In the column ‘VM’: + = mild ventriculomegaly; + + = moderate ventriculomegaly; + + + = severe or shunted ventriculomegaly; * = absent lateral ventricles.
a Hypoplastic aqueduct did not appear patent but the ventriculomegaly was mild.
b Aqueduct did not appear patent but the ventriculomegaly was mild.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Subject
Rhombencephalosynapsis neuroimaging
Brain 2012: 135; 1370–1386
| 1381
Table 4 Relationship between ventriculomegaly/hydrocephalus and callosal abnormalities in subjects with RES
Aqueductal
stenosis
VM
Corpus callosum phenotype
Proposed
mechanism
1
8
15
17
27
35
36
38
41
Totals
3
2
5
10
13
20
21
26
31
Totals
12
14
18
19
24
25
39
42
Totals
4
6
7
9
11
16
23
28
29
30
32
37
Totals
22
33
34
40
( + )a
+
+
+
+
+
+
+++
*
+++
+++
*
+
+
8/9
+++
+++
6/9
Diffuse thinning and partial posterior agenesis
Diffuse thinning
Absent
Diffuse thinning
NA
Total agenesis
Normal
Diffuse thinning
Diffuse thinning
DM
HRD
DM
HRD
NA
DM
–
HRD
HRD
+
+++
+
+
+
+
+
+
6/9
+
+
DM
HRD
–
DM
DM
DM
DM
DM
HRD
+
++
++
++
++
++
++
7/9
++
++
+
++
Diffuse thinning
Diffuse thinning
Normal
Absent rostrum with
Absent rostrum with
Absent rostrum with
Absent rostrum with
Absent rostrum with
Diffuse thinning
+
+++
+
5/7
+++
6/7
++
+
+
+
+
+
+
+
+
+
+
+
+
+++
+++
2/12
4/12
+
+
+++
dysgenesis
dysgenesis
dysgenesis
dysgenesis
dysgenesis
of
of
of
of
of
post
post
post
post
post
corpus
corpus
corpus
corpus
corpus
callosum
callosum
callosum
callosum
callosum
Diffuse thinning
Rostrum present with dysgenesis of post corpus callosum
Mild thinning
Absent rostrum with dysgenesis of post corpus callosum
Diffuse thinning and partial posterior agenesis
Diffuse thinning
Diffuse thinning (mild)
Diffuse thinning
HRD
HRD
DM
DM
DM
HRD
DM
HRD
Diffuse thinning
Normal
Normal
Normal
Normal
Normal
Diffuse thinning
Absent rostrum with dysgenesis of post corpus callosum
Rostrum present with dysgenesis of post corpus callosum
Normal
Normal
Normal
DMb
–
–
–
–
–
DMb
DM
HRD
–
–
–
Normal
Thickened
Diffuse thinning (mild)
Rostrum present with severe dysgenesis of post corpus callosum
–
DM
DM
HRD
DM = developmental malformation; HRD = hydrocephalus-related deformation; NA = not available; + = abnormality present;
= abnormality not present;
VM = ventriculomegaly.
In the column "VM": + = mild ventriculomegaly; + + = moderate ventriculomegaly; + + + = severe or shunted ventriculomegaly; * = absent lateral ventricles.
a Aqueduct did not appear patient but the VM = ventriculomegaly was mild.
b Hydrocephalus was not severe enough to explain corpus callosum thinning.
hydrocephalus; however, obstructive hydrocephalus does not explain the absence of the rostrum in six of these subjects, and we
hypothesize that they also have a primary defect in callosal development. Similarly, the corpus callosum was variably thin or partially/completely absent in a total of nine subjects without
obstructive hydrocephalus, also supporting the role of a primary
developmental defect.
The mammillary bodies were not observed and considered to be
hypoplastic or absent in 13/39 subjects with adequate imaging
(Fig. 3C, E and G), as noted by other authors (Schachenmayr
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Subject
1382
| Brain 2012: 135; 1370–1386
Holoprosencephaly
Subjects 14, 15 and 35 also had abnormal midline continuity of
posterior cerebral hemispheres associated with dysplastic or even
absent lateral ventricles. Subjects 15 and 35 had diencephalontelencephalosynapsis with an unusual but similar pattern of
fusion involving the occipital lobes, thalami, basal ganglia and
hypothalamus with absent or nearly absent ventricles (Fig. 5A
and B), as described by other authors (Garfinkle, 1996). In
Subject 35, fusion of the occipital lobes extended more superiorly
and anteriorly to involve posterior inferior frontal and parietal
lobes. Both Subjects 15 and 35 had severely dysplastic infolded
cortex in the same regions. The falx was present but deficient in
the frontal lobes, with separation of the frontal, temporal and
anterior parietal lobes. This is distinct from the known HPE spectrum, in which the frontal lobes are more severely affected than
the occipital lobes. In contrast, Subject 14 had a much smaller area
of continuity between the posterior frontal lobes across the midline (Fig. 5C) resembling the ‘middle interhemispheric’ variant of
HPE in location; however, the frontal polymicrogyria and dysplastic ventricles differ from other reports of this malformation. Not
surprisingly, these subjects all had aqueductal stenosis and substantial midline fusion of the midbrain.
The olfactory lobes were present in Subjects 14 and 35, but
absent in Subject 15. The olfactory bulbs were also absent in
eight additional subjects (Fig. 5D), possibly representing a form
fruste of telencephalosynapsis. Due to limitations in the clinical
imaging studies, it was not possible to determine whether the
olfactory bulbs were hypoplastic in six subjects. The olfactory
lobes were present and appeared normal in all subjects.
Neurodevelopmental outcome
We were able to obtain sufficient clinical information to classify the
severity of the abnormal neurodevelopmental outcome as mild,
moderate or severe in 37 subjects (88%), losing five to follow-up.
Clinical category was correlated with developmental outcome: the
subjects with RES + HPE had poorer outcomes (two severe, one
moderate), as did the subjects with RES + VACTERL features
(three severe, two moderate), while the subjects with GLH (none
severe, four moderate, 12 mild) and RES NOS (one severe, four
moderate, eight mild) had less severe outcomes (P-value = 0.0012,
Fisher’s exact).
The severity of RES was also correlated with the severity of the
outcome: the subjects with complete RES had poorer outcomes
(two severe, three moderate, three mild), while the subjects with
mild RES had less severe outcomes (none severe, two moderate,
eight mild), with the moderate and severe RES subjects falling in
between (one-sided P = 0.0028, Kendall tau-b). Of note, each of
the components of RES severity (absent posterior vermis, absent anterior vermis and absent nodulus) did not correlate with the severity
of neurodevelopmental outcome. The only other imaging features
that correlated with neurodevelopmental outcome were severity of
ventriculomegaly (P 5 0.0001, Kendall tau-b), aqueductal stenosis
(P = 0.0054, Fisher’s exact), fused colliculi (P = 0.0087, Fisher’s
exact) and abnormal temporal cortex (P = 0.016, Fisher’s exact).
Discussion
RES is an uncommon malformation of the cerebellum characterized by loss of cerebellar midline structures such that the right and
left cerebellar hemispheres and peduncles are fused. Although partial RES and midbrain involvement have been previously reported
(Obersteiner, 1916; Gross, 1959; Shaw, 1995; Demaerel et al.,
2004; Pavone et al., 2005; Alkan et al., 2009; Pasquier et al.,
2009), we provide the first evidence for an ordered spectrum of
RES severity that correlates with the severity of midbrain involvement. Our analysis of brain-imaging studies in 42 previously unreported patients provides systematic evidence for the previously
reported associations between RES and hydrocephalus, mesencephyalosynapsis and holoprosencephaly. In addition, we identified
RES in almost 10% of patients with aqueductal stenosis, indicating
that RES is more common than previously appreciated and should
be specifically evaluated in patients with aqueductal stenosis.
Strikingly, the clinical categories defined in the literature as well
as the severity of RES defined in this work correlate strongly with
neurodevelopmental outcome.
Spectrum of imaging severity
In our series, most patients fit into an ordered spectrum of severity, from loss of posterior vermis, to loss of posterior and anterior
vermis, to loss of posterior and anterior vermis plus nodulus. Prior
studies have not noted the presence of anterior vermis, and this
may be under-reported due to young age, lack of spatial resolution and other technical issues. The anterior vermis, if present, is
usually seen most ventrally and cranially. Careful evaluation of the
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
and Friede, 1982). Subjects 15 and 35 had fusion of the hypothalamus including the mammillary bodies (Garfinkle, 1996). The
fornices were fused in 18/37 subjects, all of whom also had absent
septum (Fig. 2N). The fornices could not be visualized in five subjects (Subjects 15, 19, 20, 27 and 35), while a single thinned out
fornix was seen in two subjects (Subjects 12 and 29); these findings could be related to severe distortion due to hydrocephalus destroying and/or limiting visualization of the fornices.
Subjects 15 and 35 had the absence of the ventricles, septum
and fornices.
We noted that the anterior commissure was absent or hypoplastic in 16/38 subjects: 14 with obstructive hydrocephalus and
two without ventriculomegaly, indicating that most anterior commissure abnormalities are secondary to hydrocephalus, rather
being due to abnormal brain development. Assessment of the anterior commissure was challenging in a number of subjects due to
immature myelination and/or inadequate imaging quality.
Similarly, the medial temporal lobes were thin and excessively
folded in 25/39 subjects, including 19 with obstructive hydrocephalus and six without hydrocephalus. The pituitary gland was unremarkable in all subjects.
We did not identify cortical abnormalities except in Subjects 14,
15 and 35 with variants of HPE (see below), Subjects 2 and 20
with bilateral frontal polymicrogyria and heterotopia and Subjects
7 and 22 with right frontal periventricular heterotopia.
G. E. Ishak et al.
Rhombencephalosynapsis neuroimaging
dorsal and posterior vermis is required to diagnose the mildest
forms of partial RES. This may indicate a gradient of severity
more severe dorsally and less severe ventrally.
Cerebellar and posterior fossa size
Rhombencephalosynapsis, mesencephalosynapsis and holoprosencephaly
A variety of midbrain abnormalities have been reported in patients
with RES, including aqueductal stenosis, midline fusion of the colliculi (Obersteiner, 1916; Schachenmayr and Friede, 1982;
Jellinger, 2002; Yachnis, 2002) and abnormal configuration of
the superior cerebellar peduncles (Schachenmayr and Friede,
1982; Shaw, 1995). In line with these prior reports, we observed
midbrain abnormalities that ranged from isolated fusion of inferior
or superior colliculi, to a mass like fusion of the entire mesencephalon, extending from the superior cerebellar peduncles up to the
level of the posterior commissure, reflecting a variable degree of
mesencephalosynapsis in 52% of our subjects with RES. Fusion of
the colliculi occurs both across the midline (involving both superior
and inferior colliculi) or craniocaudally (fusing superior and inferior
colliculi). We also observed ectopic (likely cerebellar) tissue associated with the inferior colliculus, superior medullary velum and
superior cerebellar peduncles, as previously described by Shaw
(1995) and Takano et al. (2010).
The pattern of forebrain fusion (HPE) in our most severely affected
subjects was strikingly atypical, predominantly involving the occipital
lobes. The absence of the olfactory bulbs in almost 30% of our subjects also points to forebrain defects in the HPE spectrum. Based on
these data, RES should be viewed as part of a malformation that
typically includes the midbrain and sometimes extends to the diencephalon and occasionally telencephalon. In our series, the severity of RES correlated well with these midbrain and forebrain defects,
likely indicating a shared biological mechanism.
Rhombencephalosynapsis and
hydrocephalus
Barth (2008) reported that the minimum rate of hydrocephalus from
his review of the literature was 25%, while we observed obstructive
| 1383
hydrocephalus in 45% of our subjects. In our series, hydrocephalus
is primarily related to aqueductal stenosis (seen in 52% of patients in
this series) with obstruction at different points along the aqueduct in
different subjects. Obstruction may occur more cranial to the aqueduct in patients with thalamic fusion (Kepes et al., 1969; Simmons
et al., 1993) or possibly distal to the aqueduct in patients with crowding of the posterior fossa (with or without ectopia).
Surprisingly, the aqueduct did not appear patent in two subjects
with HPE and aventriculy, as well as one subject with mild ventriculomegaly. We hypothesize that the absence of hydrocephalus
in these subjects may represent inadequate formation of cerebrospinal fluid, patency of the aqueduct below the resolution of imaging and/or ectopic routes for cerebrospinal fluid drainage.
Rhombencephalosynapsis and other
forebrain abnormalities
In general, the severity of RES did not correlate well with the frequency and severity of forebrain imaging abnormalities, most of
which seem to correlate better with the degree of hydrocephalus,
with notable exceptions. The septum pellucidum was absent in all
subjects with obstructive hydrocephalus implicating a destructive
process in these patients. In contrast, the septum was missing in
17% of the subjects without obstructive hydrocephalus, and we
were able to document loss of the septum between mid-gestation
and the neonatal period in two subjects without overt hydrocephalus. Thus, absent septum is not likely to be due to a destructive
process in these subjects and may be due to defects in proliferation,
survival and/or fate determination of septal cells.
Although the posterior corpus callosum is strikingly thinned and
dorsally deviated in many patients with RES and hydrocephalus,
we do not think that this finding is specific for RES, since we have
observed it in patients with hydrocephalus but not RES.
Conversely, the corpus callosum was abnormal in multiple subjects
without hydrocephalus, indicating that primary developmental defects of the corpus callosum occur as well. Furthermore, several
other forebrain structures (anterior commissure, temporal cortex
and mammillary bodies) were often abnormal in patients with
severe hydrocephalus. Therefore, these imaging abnormalities are
most often due to deformation and/or destruction from hydrocephalus and not primarily due to intrinsic defects in the development of these forebrain structures.
Limitations
This study has several limitations. Despite being the largest RES
cohort to date, the number of subjects is still quite small, especially
for the VACTERL and HPE groups. In addition, the cohort is likely
skewed towards more severely affected subjects with associated
abnormalities due to ascertainment bias. This is particularly relevant
for estimating the prevalence of findings like aqueductal stenosis in
patients with RES. Due to recruitment of subjects from all over the
world, the imaging was performed at different institutions using different protocols resulting in variable imaging quality. Similarly, we
were unable to perform standardized developmental and neurological assessments, limiting the quality of the outcome data.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
We report the first association between RES and inferior cerebellar
ectopia (Chiari I malformation) in 24% of the subjects and confirm an
association between RES and superior cerebellar ectopia in 60% of
the subjects. We attribute this to disproportionately small posterior
fossa size relative to cerebellum size. In partial RES, the transverse
diameter of the cerebellum was variably small with relatively
increased craniocaudal dimension, reflecting the severity of superior
herniation. In several subjects, superior ectopia was exacerbated by
ventriculoperitoneal shunting; however, ectopia was not more
common or pronounced in subjects with complete RES, likely because the cerebellum was markedly hypoplastic in these subjects.
The cause of cerebellar ectopia in the setting of RES is not clear,
but could reflect abnormal development of the cerebellum, abnormal
development of the surrounding meninges and bone, hydrocephalus
and shunting, or a combination of these factors.
Brain 2012: 135; 1370–1386
1384
| Brain 2012: 135; 1370–1386
Clinical applications
Genetics and pathogenesis
Several clinical categories have been proposed for patients with
RES, including GLH, a VACTERL H-like presentation and RES associated with holoprosencephaly (Gomez, 1979; Lopez-Hernandez,
1982; Pasquier et al., 2009). Intriguingly, the severity of RES and
the other brain imaging abnormalities did not correlate with these
clinical subcategories in our cohort. Several subjects with VACTERL
features, as well as the subjects with HPE, had more severe midbrain involvement; however, with the exception of HPE, the clinical categories cannot be distinguished based on the brain imaging
features, in agreement with prior publications (Toelle et al., 2002;
Poretti et al., 2009).
RES is a fascinating malformation that differs from all other
vermis hypoplasias, in which the cerebellar hemispheres are separated rather than fused. Consanguinity and recurrences point to an
autosomal recessive cause in a minority of families, while the predominance of sporadic patients is consistent with de novo dominant mutations although a possible association with maternal
diabetes has been noted (Garfinkle, 1996; Sergi et al., 1997).
While the developmental basis of RES remains unknown, a
number of developmental mechanisms have been proposed to explain RES. Numerous studies have shown that defects in dorsal midline signalling lead to malformations of the brainstem and
cerebellum. The mouse cerebellar hypoplasia and human Dandy–
Walker syndrome phenotypes associated with mutations in Zic1
and Zic4, Foxc1, as well as the mouse cerebellar phenotype associated with mutations in Lmx1a, serve as good examples (Millonig
et al., 2000; Grinberg et al., 2004; Aldinger et al., 2009; Chizhikov
et al., 2010). Other studies have shown that defects in dorsal midline
signalling can result in HPE, as recently demonstrated with mutations
of genes in the fibroblast growth factor and bone morphogenetic
protein pathways (Shimogori et al., 2004; Fernandes et al., 2007;
Geng and Oliver, 2009; Ramocki et al., 2011). Alternatively, several
authors (Tan et al., 2005; Gomy et al., 2008; Poretti et al., 2008;
Fernandez-Jaen et al., 2009) have proposed that a mouse with a
missense mutation in the lysosomal acid phosphatase (Acp2) gene
(Mannan et al., 2004) might represent a model for GLH due to cerebellar and skin involvement; however, these mice display defective
hair and cerebellar development without true alopecia or RES. Our
analysis of human RES confirms a link between human HPE and RES
and shows that both dorsal midbrain- and hindbrain-derived structures are more severely affected than ventral-derived structures.
These observations collectively suggest that defects of dorsally expressed genes cause the combination of HPE and RES, and by extension that defects in related dorsal signalling pathways may cause
other forms of RES.
Acknowledgements
The authors thank all of the patients, their families and many
referring physicians for participating in this study.
Funding
NIH (grants KL2-RR025015 to D.D. and T.C.R.); (R01-NS050375
to W.B.D. and K.J.M.); CHLA-USC Child Health Research Career
Development Program (K12-HD05954 to P.A.S.), by The Arc of
Washington Trust Fund (to D.D.); Harold Amos Faculty
Development Program through the Robert Wood Johnson
Foundation (to P.A.S.); NIH/NINDS T32 (Grant 5T32NS051171
to H.T.).
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Our work also indicates that, although rare, RES may be substantially more common than previously thought. Prior to this work,
10 patients with RES had been identified at our institution. With
heightened awareness and additional scrutiny of patients
with aqueductal stenosis, we identified five additional patients
with RES of various degrees of severity. We were unable to evaluate for RES in patients who only had CT scans, so we may have
missed additional patients with RES who were not imaged by MRI.
Based on our findings and the literature, RES should be specifically
evaluated by MRI in patients with aqueductal stenosis, absent
septum pellucidum, small cerebellum, superior cerebellar herniation and/or the absence of the normal folial pattern of the cerebellar vermis on the sagittal image. Additional signs of RES on the
sagittal view include the following: absence of the primary fissure,
abnormal rounded contour of the fourth ventricle (rather than
triangular contour of fastigium) and deficient indentation of the
fourth ventricle by the nodulus. On axial and coronal images, RES
can be identified by continuity of the cerebellar folia and fissures
across the midline, particularly dorsally. In addition, the posterior
cerebellar incisura and vallecula may be absent, and the dentate
nuclei and superior cerebellar peduncles may be apposed. DTI has
been shown to demonstrate the absence of the transversely oriented white matter tracts of the vermis and vertical orientation of
the tracts in the medial aspect of the fused cerebellum. In addition, DTI can demonstrate that the deep cerebellar nuclei and the
superior cerebellar peduncles are oriented more medially; however, it cannot distinguish close apposition from actual fusion
(Widjaja et al., 2006; Merlini et al., 2011).
RES may be misdiagnosed in patients with Chiari II malformation (Guntur Ramkumar et al., 2010). Prenatally, cerebellar hypoplasia and ventriculomegaly, with or without the absence of the
septum pellucidum, should prompt careful evaluation for hindbrain
fusion (Litherland et al., 1993; Napolitano et al., 2004).
Perhaps most important are the correlations between RES severity
and clinical diagnosis with neurodevelopmental outcome. The identification of RES on brain imaging should prompt additional evaluations for other malformations, particularly vertebral, rib, renal and
limb abnormalities, as well congenital heart disease. Our data greatly
improve the quality of information available for counselling families
about prognosis. Patients with HPE, VACTERL features and/or
severe to complete RES are at substantially increased risk for moderately to severely abnormal neurodevelopmental outcome. This information allows families to set appropriate expectations, anticipate
needs and develop plans for treatment. In the future, this clinical
data may help direct specific genetic testing and/or help with the
interpretation of genome-wide genetic testing data.
G. E. Ishak et al.
Rhombencephalosynapsis neuroimaging
Supplementary material
Supplementary material is available at Brain online.
References
| 1385
Guleria S. ZIC2 mutations are seen in holoprosencephaly and not partial
rhombencephalosynapsis. Am J Med Genet Part A 2011; 155A: 2901;
author reply 2902.
Guntur Ramkumar P, Kanodia AK, Ananthakrishnan G, Roberts R. Chiari
II malformation mimicking partial rhombencephalosynapsis? A case
report. Cerebellum 2010; 9: 111–4.
Isaac M, Best P. Two cases of agenesis of the vermis of cerebellum, with
fusion of the dentate nuclei and cerebellar hemispheres. Acta
Neuropathol 1987; 74: 278–80.
Jellinger KA. Rhombencephalosynapsis. Acta Neuropathol 2002; 103:
305–6.
Jellinger KA. Rhombencephalosynapsis with and without associated malformations. Acta Neuropathol 2009; 117: 219.
Kendall M. A new measure of rank correlation. Biometrika 1938; 30:
81–89.
Kepes JJ, Clough C, Villanueva A. Congenital fusion of the thalami (atresia of the third ventricle) and associated anomalies in a 6-months-old
infant. Acta Neuropathol 1969; 13: 97–104.
Lespinasse J, Testard H, Nugues F, Till M, Cordier MP, Althuser M, et al.
A submicroscopic unbalanced subtelomeric translocation t(2p;10q)
identified by fluorescence in situ hybridization: fetus with increased
nuchal translucency and normal standard karyotype with later
growth and developmental delay, rhombencephalosynapsis (RES).
Annales de Genetique 2004; 47: 405–17.
Litherland J, Ludlam A, Thomas N. Antenatal ultrasound diagnosis of
cerebellar vermian agenesis in a case of rhombencephalosynapsis. J
Clin Ultrasound 1993; 21: 636–8.
Lopez-Hernandez A. Craniosynostosis, ataxia, trigeminal anaesthesia and
parietal alopecia with pons-vermis fusion anomaly (atresia of the
fourth ventricle). Report of two cases. Neuropediatrics 1982; 13:
99–102.
Mannan AU, Roussa E, Kraus C, Rickmann M, Maenner J, Nayernia K,
et al. Mutation in the gene encoding lysosomal acid phosphatase
(Acp2) causes cerebellum and skin malformation in mouse.
Neurogenetics 2004; 5: 229–38.
Merlini L, Fluss J, Korff C, Hanquinet S. Partial Rhombencephalosynapsis
and Chiari Type II Malformation in a Child: a True Association
Supported by DTI Tractography. Cerebellum. Advance Access published on July 21, 2011, doi:10.1007/s12311-011-0300-3.
Michaud J, Mizrahi EM, Urich H. Agenesis of the vermis with
fusion of the cerebellar hemispheres, septo-optic dysplasia and
associated anomalies. Report of a case. Acta Neuropathol 1982; 56:
161–6.
Millonig JH, Millen KJ, Hatten ME. The mouse Dreher gene Lmx1a controls formation of the roof plate in the vertebrate CNS. Nature 2000;
403: 764–9.
Napolitano M, Righini A, Zirpoli S, Rustico M, Nicolini U, Triulzi F.
Prenatal magnetic resonance imaging of rhombencephalosynapsis
and associated brain anomalies: report of 3 cases. J Comput Assist
Tomogr 2004; 28: 762–5.
Obersteiner H. Ein Kleinhirn ohne Wurm. Arbeit Neurol Inst Univ Wien
1916; 21: 124–36.
Pasquier L, Marcorelles P, Loget P, Pelluard F, Carles D, Perez MJ, et al.
Rhombencephalosynapsis and related anomalies: a neuropathological
study of 40 fetal cases. Acta Neuropathol 2009; 117: 185–200.
Pavone P, Incorpora G, Ruggieri M. A complex brain malformation syndrome with rhombencephalosynapsis, preaxial hexadactyly plus facial
and skull anomalies. Neuropediatrics 2005; 36: 279–83.
Poretti A, Bartholdi D, Gobara S, Alber FD, Boltshauser E. Gomez-LopezHernandez syndrome: an easily missed diagnosis. Eur J Med Genet
2008; 51: 197–208.
Poretti A, Alber FD, Burki S, Toelle SP, Boltshauser E. Cognitive outcome
in children with rhombencephalosynapsis. Eur J Paediatr Neurol 2009;
13: 28–33.
Ramocki MB, Scaglia F, Stankiewicz P, Belmont JW, Jones JY, Clark GD.
Recurrent partial rhombencephalosynapsis and holoprosencephaly in
siblings with a mutation of ZIC2. Am J Med Genet A 2011;
155A(7): 1574–80.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Adam MP, Abramowsky CR, Brady AN, Coleman K, Todd NW.
Rhabdomyomatous hamartomata of the pharyngeal region with bilateral microtia and aural atresia: a new association? Birth Defects Res
Part A, Clin Mol Teratol 2007; 79: 242–8.
Aldinger KA, Lehmann OJ, Hudgins L, Chizhikov VV, Bassuk AG,
Ades LC, et al. FOXC1 is required for normal cerebellar development
and is a major contributor to chromosome 6p25.3 Dandy-Walker malformation. Nat Genet 2009; 41: 1037–42.
Alkan O, Kizilkilic O, Yildirim T. Malformations of the midbrain and
hindbrain: a retrospective study and review of the literature.
Cerebellum 2009; 8: 355–65.
Barth PG. Rhombencephalosynapsis. In: Harvey BS, Paolo C, editors.
Handbook of clinical neurology, Vol 87 (3rd series) malformations of
the nervous system. Amsterdam: Elsevier BV; 2008. p. 53–65.
Boltenstern M, Konrad A, Jost W, Uder M, Kujat C.
[Rhombencephalosynapsis]. RoFo : Fortschritte auf dem Gebiete der
Rontgenstrahlen und der Nuklearmedizin 1995; 163: 91–3.
Boltshauser E. Cerebellum-small brain but large confusion: a review of
selected cerebellar malformations and disruptions. Am J Med Genet
Part A 2004; 126A: 376–85.
Chemli J, Abroug M, Tlili K, Harbi A. Rhombencephalosynapsis diagnosed in childhood: clinical and MRI findings. Eur J Paediatr Neurol
2007; 11: 35–8.
Chizhikov VV, Lindgren AG, Mishima Y, Roberts RW, Aldinger KA,
Miesegaes GR, et al. Lmx1a regulates fates and location of cells originating from the cerebellar rhombic lip and telencephalic cortical hem.
Proc Natl Acad Sci USA 2010; 107: 10725–30.
Demaerel P, Kendall BE, Wilms G, Halpin SF, Casaer P, Baert AL.
Uncommon posterior cranial fossa anomalies: MRI with clinical correlation. Neuroradiology 1995; 37: 72–6.
Demaerel P, Morel C, Lagae L, Wilms G. Partial rhombencephalosynapsis. Am J Neuroradiol 2004; 25: 29–31.
di Vera E, Liberati M, Celentano C, Calabrese G, Guanciali-Franchi PE,
Morizio E, et al. Rhombencephalosynapsis in a severely polymalformed
fetus with non-mosaic tetrasomy 9p, in intracytoplasmic-sperminjection pregnancy. J Assist Reprod Genet 2008; 25: 577–80.
Fernandes M, Gutin G, Alcorn H, McConnell SK, Hebert JM. Mutations
in the BMP pathway in mice support the existence of two molecular
classes of holoprosencephaly. Development 2007; 134: 3789–94.
Fernandez-Jaen A, Fernandez-Mayoralas DM, Calleja-Perez B, MunozJareno N, Moreno N. Gomez-Lopez-Hernandez syndrome: two new
cases and review of the literature. Pediat Neurol 2009; 40: 58–62.
Garfinkle WB. Aventriculy: a new entity? Am J Neuroradiol 1996; 17:
1649–50.
Geng X, Oliver G. Pathogenesis of holoprosencephaly. J Clin Invest
2009; 119: 1403–13.
Gomez MR. Cerebellotrigeminal and focal dermal dysplasia: a newly
recognized neurocutaneous syndrome. Brain Dev 1979; 1: 253–6.
Gomy I, Heck B, Santos AC, Figueiredo MS, Martinelli CE Jr,
Nogueira MP, et al. Two new Brazilian patients with Gomez-LopezHernandez syndrome: reviewing the expanded phenotype with molecular insights. Am J Med Genet Part A 2008; 146A: 649–57.
Grinberg I, Northrup H, Ardinger H, Prasad C, Dobyns WB, Millen KJ.
Heterozygous deletion of the linked genes ZIC1 and ZIC4 is involved
in Dandy-Walker malformation. Nat Genet 2004; 36: 1053–5.
Gross H. [Rhombencephalon synapsis, a systematized cerebellar abnormality]. Archiv fur Psychiatrie und Nervenkrankheiten, vereinigt mit
Zeitschrift fur die gesamte Neurologie und Psychiatrie 1959; 199:
537–52.
Brain 2012: 135; 1370–1386
1386
| Brain 2012: 135; 1370–1386
Simmons G, Damiano TR, Truwit CL. MRI and clinical findings
in rhombencephalosynapsis. J Comput Assist Tomogr 1993; 17:
211–4.
Sukhudyan B, Jaladyan V, Melikyan G, Schlump JU, Boltshauser E,
Poretti A. Gomez-Lopez-Hernandez syndrome: reappraisal of the diagnostic criteria. Eur J Pediatr 2010; 169: 1523–8.
Takano T, Kinoshita N, Narumiya S, Takeuchi Y. Aprosencephaly with
rhombencephalosynapsis and hamartomatous midbrain dysplasia.
Neuropathol Appl Neurobiol 2010; 36: 353–5.
Tan TY, McGillivray G, Goergen SK, White SM. Prenatal magnetic resonance imaging in Gomez-Lopez-Hernandez syndrome and review of
the literature. Am J Med Geneti Part A 2005; 138: 369–73.
Toelle SP, Yalcinkaya C, Kocer N, Deonna T, Overweg-Plandsoen WC,
Bast T, et al. Rhombencephalosynapsis: clinical findings and neuroimaging in 9 children. Neuropediatrics 2002; 33: 209–14.
Truwit CL, Barkovich AJ, Shanahan R, Maroldo TV. MR imaging of
rhombencephalosynapsis: report of three cases and review of the literature. Am J Neuroradiol 1991; 12: 957–65.
Utsunomiya H, Takano K, Ogasawara T, Hashimoto T, Fukushima T,
Okazaki M. Rhombencephalosynapsis: cerebellar embryogenesis. Am
J Neuroradiol 1998; 19: 547–9.
Widjaja E, Blaser S, Raybaud C. Diffusion tensor imaging of midline
posterior fossa malformations. Pediat Radiol 2006; 36: 510–7.
Yachnis AT. Rhombencephalosynapsis with massive hydrocephalus: case
report and pathogenetic considerations. Acta Neuropathol 2002; 103:
301–4.
Downloaded from http://brain.oxfordjournals.org/ by guest on March 5, 2016
Romanengo M, Tortori-Donati P, Di Rocco M. Rhombencephalosynapsis
with facial anomalies and probable autosomal recessive inheritance: a
case report. Clin Genet 1997; 52: 184–6.
Sandalcioglu IE, Gasser T, van de Nes JA, Menken U, Stolke D,
Wiedemayer H. Fusion of the cerebellar hemispheres ventral to the
brainstem: a rare hindbrain-related malformation. Childs Nerv Syst
2006; 22: 73–7.
Sarnat HB. Molecular genetic classification of central nervous system
malformations. J Child Neurol 2000; 15: 675–87.
Savolaine ER, Fadell RJ, Patel YP. Isolated rhombencephalosynapsis diagnosed by magnetic resonance imaging. Clin Imaging 1991; 15: 125–9.
Schachenmayr W, Friede RL. Rhombencephalosynapsis: a Viennese malformation? Dev Med Child Neurol 1982; 24: 178–82.
Sener RN. Unusual MRI findings in rhombencephalosynapsis. Comput
Med Imaging Graph 2000; 24: 277–82.
Sergi C, Hentze S, Sohn C, Voigtlander T, Jung C, Schmitt HP.
Telencephalosynapsis (synencephaly) and rhombencephalosynapsis
with posterior fossa ventriculocele (’Dandy-Walker cyst’): an unusual
aberrant syngenetic complex. Brain Dev 1997; 19: 426–32.
Shaw C. Hydrocephalus. In: Duckett S, editor. Pediatric neuropathology.
Baltimore: Williams and Wilkins; 1995. p. 149–211.
Shimogori T, Banuchi V, Ng HY, Strauss JB, Grove EA. Embryonic signaling centers expressing BMP, WNT and FGF proteins interact to
pattern the cerebral cortex. Development 2004; 131: 5639–47.
Siebert JR, Schoenecker KA, Resta RG, Kapur RP. Holoprosencephaly and
limb reduction defects: a consideration of Steinfeld syndrome and
related conditions. Am J Med Genet Part A 2005; 134: 381–92.
G. E. Ishak et al.