The Coding Institute — SPECIALTY ALERTS
CodingInstitute.com; SuperCoder.com — Inspired by Coders, Powered by Coding Experts
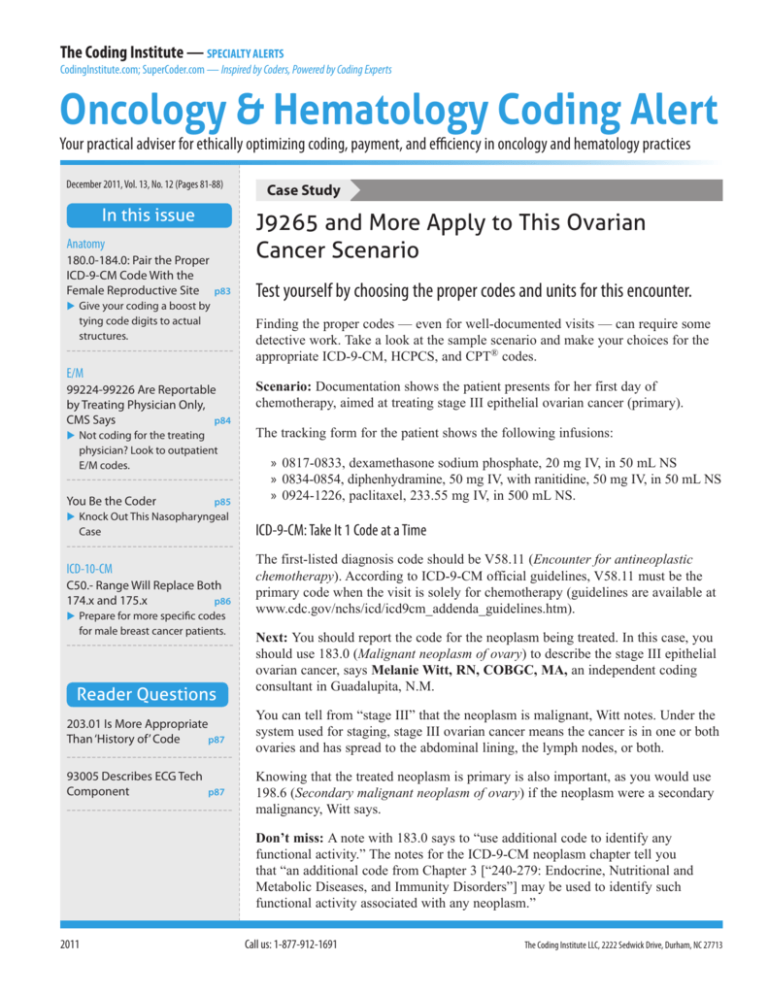
Oncology & Hematology Coding Alert
Your practical adviser for ethically optimizing coding, payment, and efficiency in oncology and hematology practices
December 2011, Vol. 13, No. 12 (Pages 81-88)
In this issue
p83
Give your coding a boost by
tying code digits to actual
structures.
Test yourself by choosing the proper codes and units for this encounter.
Finding the proper codes — even for well-documented visits — can require some
detective work. Take a look at the sample scenario and make your choices for the
appropriate ICD-9-CM, HCPCS, and CPT® codes.
E/M
99224-99226 Are Reportable
by Treating Physician Only,
CMS Says
p84
Not coding for the treating
physician? Look to outpatient
E/M codes.
You Be the Coder
p85
Knock Out This Nasopharyngeal
Case
ICD-10-CM
C50.- Range Will Replace Both
174.x and 175.x
p86
Prepare for more specific codes
for male breast cancer patients.
Reader Questions
203.01 Is More Appropriate
Than ‘History of’ Code
p87
93005 Describes ECG Tech
Component
}
J9265 and More Apply to This Ovarian
Cancer Scenario
Anatomy
180.0-184.0: Pair the Proper
ICD-9-CM Code With the
Female Reproductive Site
Case Study p87
Scenario: Documentation shows the patient presents for her first day of
chemotherapy, aimed at treating stage III epithelial ovarian cancer (primary).
The tracking form for the patient shows the following infusions:
» 0817-0833, dexamethasone sodium phosphate, 20 mg IV, in 50 mL NS
» 0834-0854, diphenhydramine, 50 mg IV, with ranitidine, 50 mg IV, in 50 mL NS
» 0924-1226, paclitaxel, 233.55 mg IV, in 500 mL NS.
ICD-9-CM: Take It 1 Code at a Time
The first-listed diagnosis code should be V58.11 (Encounter for antineoplastic
chemotherapy). According to ICD-9-CM official guidelines, V58.11 must be the
primary code when the visit is solely for chemotherapy (guidelines are available at
www.cdc.gov/nchs/icd/icd9cm_addenda_guidelines.htm).
Next: You should report the code for the neoplasm being treated. In this case, you
should use 183.0 (Malignant neoplasm of ovary) to describe the stage III epithelial
ovarian cancer, says Melanie Witt, RN, COBGC, MA, an independent coding
consultant in Guadalupita, N.M.
You can tell from “stage III” that the neoplasm is malignant, Witt notes. Under the
system used for staging, stage III ovarian cancer means the cancer is in one or both
ovaries and has spread to the abdominal lining, the lymph nodes, or both.
Knowing that the treated neoplasm is primary is also important, as you would use
198.6 (Secondary malignant neoplasm of ovary) if the neoplasm were a secondary
malignancy, Witt says.
Don’t miss: A note with 183.0 says to “use additional code to identify any
functional activity.” The notes for the ICD-9-CM neoplasm chapter tell you
that “an additional code from Chapter 3 [“240-279: Endocrine, Nutritional and
Metabolic Diseases, and Immunity Disorders”] may be used to identify such
functional activity associated with any neoplasm.”
2011
Call us: 1-877-912-1691
The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
The Coding Institute — SPECIALTY ALERTS
Editorial Advisory Board
Michael L. Berman, MD, FACOG, FACS
Ian S. Easton, PhD, FACMPE
The appropriate code for chemotherapy drug paclitaxel is J9265 (Injection,
paclitaxel, 30 mg). To determine the number of units, you should divide the
amount administered (233.55 mg) by the amount in the code definition (30
mg). Do the math, and the answer is 7.785. Because Medicare allows you to
round up to find your final number for units, the correct number of units is 8.
Alice G. Ettinger, RN, MSN, CPNP
argaret M. Hickey, MS, MSN, RN, OCN,
M
CORLN
Former President, Society of Otorhinolaryngology and
Head-Neck Nurses
Dianna B. Hofbeck, RN, CCM
President (retired), North Shore
Medical Inc.
Before you can choose the appropriate infusion codes, you’ll need to identify
the specific agents administered. The nature of the agent will affect your
CPT® infusion code choice.
Note that if the record shows the drug is instead paclitaxel protein-bound, you
should report J9264 (Injection, paclitaxel protein-bound particles, 1 mg). You
would report this code per milligram (for instance, 234 units for 234 mg).
For the dexamethasone (a steroid), you should report J1100 (Injection,
dexamethasone sodium phosphate, 1 mg). You report the code per milligram,
so you should report 20 units to represent the 20 mg administered.
The appropriate code for the antihistamine diphenhydramine is J1200 (Injection,
diphenhydramine HCl, up to 50 mg). One unit will report the 50 mg administered.
Use J2780 (Injection, ranitidine hydrochloride, 25 mg) for the ranitidine,
a histamine H2-receptor antagonist. You’ll need 2 units for the 50 mg the
patient received.
Past President, American Academy of Professional
Coders
Tip: The documentation notes the amount of normal saline (NS) used in the
infusions. But CPT® guidelines state, “Fluid used to administer the drug(s)
is incidental hydration and is not separately payable,” noted Lynn M.
Anderanin, CPC, CPC-I, COSC, in her presentation, “Don’t Get Stuck with
Rejected Claims for Infusion Therapy Services” (www.audioeducator.com).
Gary P. Riedmann, FACHE
CPT®: Start With the ‘Initial’ Code
Janet McDiarmid, CMM, CPC, MPC
Past Chairman, American Academy of Medical
Administrators
President & CEO, St. Anthony Regional Hospital, Iowa
Another possibility for ovarian cancer “might be an elevated CA-125 prior to
surgery, so you can add this code as a secondary diagnosis,” Witt says. The
appropriate code would be 795.82 (Elevated cancer antigen 125 [CA 125]).
HCPCS: Bring Out the Units Calculator
Past President, Association of Pediatric
Oncology Nurses
Program Coordinator, Division of Pediatric
Hematology-Oncology
Saint Peter’s University Hospital, N.J.
The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
Past President, Society of Gynecologic Oncologists
Professor, Department of Obstetrics and Gynecology, Division of Gynecologic Oncology, University of
California, Irvine
Past President, American College of Medical Practice
Executives
Department Head — Applied Technology,
Coastal Georgia College, Ga.
Call us: 1-877-912-1691
Samuel M. Silver, MD, PhD
Professor, Department of Internal Medicine, Assistant
Dean for Research, Director of Cancer Center Network,
University of Michigan
To choose your infusion codes, you’ll need to understand and apply CPT®
guidelines related to these codes.
One key rule is that when you’re reporting multiple infusions, you should
report only one “initial” service. (There is an exception if the protocol
requires two separate IV sites.) Physician coders should identify the primary
reason for the encounter and use the initial code for that service.
For the sample case, the patient presents for chemotherapy. That makes the
paclitaxel infusion your primary service. The infusion lasted three hours and
two minutes. For the first hour, you should report 96413 (Chemotherapy
(Continued on page 84)
Oncology & Hematology Coding Alert (USPS 019-321) (ISSN 1941-3262 for print; ISSN 1947-6884 for
online) is published monthly 12 times per year by The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC
27713. ©2011 The Coding Institute. All rights reserved. Subscription price is $249. Periodicals postage is paid at
Durham, NC 27705 and additional entry offices.
POSTMASTER: Send address changes to Oncology & Hematology Coding Alert 2222 Sedwick Drive,
Durham, NC 27713
p82
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!
Call us: 1-877-912-1691
Anatomy The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
The Coding Institute — SPECIALTY ALERTS
}
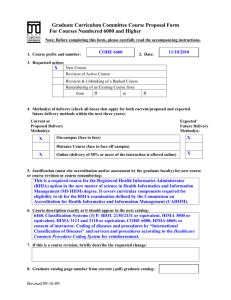
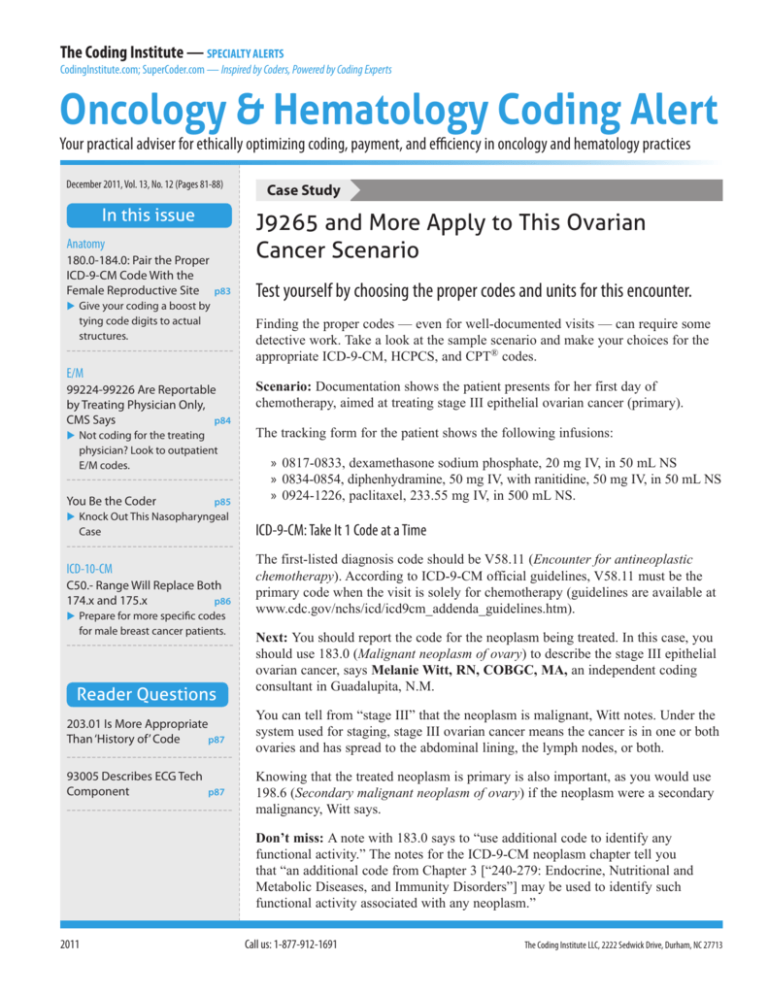
180.0-184.0: Pair the Proper ICD-9-CM Code With the Female
Reproductive Site
Give your coding a boost by tying code digits to actual structures.
Your ability to identify the body part described in your oncologist’s documentation can help sharpen your coding.
Use the anatomic illustration below to locate the site described, and then match that site to the sampling of applicable
ICD-9-CM codes in the table.
1
3
2
4
5
Location on illustration
Anatomic site
Sample ICD-9-CM code
1
Fallopian tubes
183.2, Malignant neoplasm of the fallopian tube
2
Ovaries
183.0, Malignant neoplasm of ovary
3
Uterus
182.0, Malignant neoplasm of corpus uteri except isthmus
4
Cervix
180.0, Malignant neoplasm of endocervix
5
Vagina
184.0, Malignant neoplasm of vagina
Important: The above table indicates only sample codes for the anatomic structure. When coding a report, you
should use the most specific code available for the patient’s diagnosis. For example, the cervix has multiple other site
categories to choose from: exocervix (180.1), other (180.8), and unspecified (180.9). q
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!
p83
The Coding Institute — SPECIALTY ALERTS
Call us: 1-877-912-1691
(Continued from page 82)
administration, intravenous infusion technique; up to 1
hour, single or initial substance/drug).
You should report +96415 (… each additional hour [List
separately in addition to code for primary procedure])
with a quantity of 2 to represent the next two hours.
You should not report the final two minutes of the
infusion separately. To report an “Additional hour” code,
documentation must show an interval more than 30
minutes beyond an hour, and the final two minutes in this
case don’t meet that requirement.
Next: You also need to report the dexamethasone,
diphenhydramine, and ranitidine infusions.
“The administration of anti-anemia drugs and anti-emetic
drugs by injection or infusion for cancer patients is not
considered chemotherapy administration,” Anderanin said.
So for these infusions, you’ll use the “Therapeutic,
prophylactic, or diagnostic injection” sequential codes.
Although these codes are in a different section than the
chemotherapy infusion codes, you should not report a
non-chemotherapy initial code if a chemotherapy admin
is your initial service.
To report the 16-minute dexamethasone infusion, you
should use +96367 (Therapeutic, prophylactic, or
diagnostic injection [specify substance or drug]; additional
sequential infusion, up to 1 hour [List separately in
addition to code for primary procedure]). Note that this
16-minute service is an infusion and not a push. Per CPT®,
E/M The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
the definition of a push is “(a) an injection in which the
health care professional who administers the substance/
drug is continuously present to administer the injection
and observe the patient, or (b) an infusion of 15 minutes
or less.” Because this service was recorded as 16 minutes,
you should report it as an infusion.
The 20-minute administration of the diphenhydramine
and ranitidine mixture also does not qualify as a push,
and you should report the admin with another unit of
+96367. (Note: Some coders report that their payers
request +96367, +96367-59, Distinct procedural service,
instead of 2 units of +96367. If this is your payer’s
preference, be sure to get the instructions in writing so
you can support your coding if necessary.)
You should report only one additional unit for the mixture
admin because the drugs are mixed in a single bag. The
mixture in a single bag also means you should not use
concurrent code +96368 (Intravenous infusion, for therapy,
prophylaxis, or diagnosis [specify substance or drug];
concurrent infusion [List separately in addition to code for
primary procedure]). To report that code, providers must
administer drugs in distinct bags at the same time.
Final coding: For this case, your final coding should
include:
» ICD-9-CM: V58.11, 183.0 (you may use additional
codes to identify functional activity)
» HCPCS: J9265 (8 units), J1100 (20 units), J1200 (1
unit), J2780 (2 units)
» CPT®: 96413, +96415 (2 units), +96367 (2 units). q
}
99224-99226 Are Reportable by Treating Physician Only, CMS Says
Not coding for the treating physician? Look to outpatient E/M codes.
In effect for nearly a year now, CPT®’s subsequent
observation care codes have been something of a mystery
since they were released, but CMS finally ended that by
issuing clarifications about how to report these codes.
Pinpoint Services Included in 99224-99226
The codes in focus are:
» 99224, Subsequent observation care, per day, for
the evaluation and management of a patient, which
requires at least 2 of these 3 key components:
p84
Problem focused interval history; Problem focused
examination; Medical decision making that is
straightforward or of low complexity. Counseling
and/or coordination of care with other providers
or agencies are provided consistent with the nature
of the problem(s) and the patient’s and/or family’s
needs. Usually, the patient is stable, recovering, or
improving. Physicians typically spend 15 minutes at
the bedside and on the patient’s hospital floor or unit.
» 99225, Subsequent observation care, per day, for
the evaluation and management of a patient, which
requires at least 2 of these 3 key components: An
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!
Call us: 1-877-912-1691
expanded problem focused interval history; An
expanded problem focused examination; Medical
decision making of moderate complexity. Counseling
and/or coordination of care with other providers
or agencies are provided consistent with the nature
of the problem(s) and the patient’s and/or family’s
needs. Usually, the patient is responding inadequately
to therapy or has developed a minor complication.
Physicians typically spend 25 minutes at the bedside
and on the patient’s hospital floor or unit.
» 99226, Subsequent observation care, per day, for
the evaluation and management of a patient, which
requires at least 2 of these 3 key components: A
detailed interval history; A detailed examination;
Medical decision making of high complexity.
Counseling and/or coordination of care with other
providers or agencies are provided consistent with
the nature of the problem(s) and the patient’s and/or
family’s needs. Usually, the patient is unstable or has
developed a significant complication or a significant
new problem. Physicians typically spend 35 minutes at
the bedside and on the patient’s hospital floor or unit.
CMS notes that subsequent observation care pay
includes “all the care rendered by the treating physician
Are You Prepared for Upcoming Coding Changes?
Join Audio Conferences by Industry Experts on 2012 Coding Updates!
There will be 278 new, 139 revised, 98 deleted and 22 resequenced CPT® codes in
2012. Make plans to attend our audio conferences provided by our panel of coding
veterans and experts this December, in order to keep up with these changes.
Here’s what you’ll learn:
• Which updates and guidelines affect your coding and reimbursement in 2012
• Examples of how to apply CPT® changes affecting your specialty
• What documentation payers expect you to provide for full reimbursement
To find the audio conference for your specialty(s), log on to www.audioeducator.
com/2012-coding-updates today!
Book any conference within 07 days to get $25 discount. Enter Discount
Code PUB25 at check-out!
Audio Educator, 2222 Sedwick Drive,
Durham, NC 27713
Email: customerservice@audioeducator.com
The Coding Institute — SPECIALTY ALERTS
The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
5 to !
6
9
8-2 pdates
5
4
u
6-86 ultiple
1
l
Cal on m
e
sav
on the day(s) other than the initial or discharge date,”
according to MLN Matters article MM7405, with an
implementation date of Nov. 28, 2011.
In addition to specifically referring to the “treating
physician” in the above passage, the agency goes on to
qualify that any other physicians evaluating or consulting
on the observation care patient “must bill the appropriate
outpatient service codes,” and not the subsequent
observation care codes. This eliminates prior confusion
that existed about exactly who could report subsequent
observation care.
MAC advice: WPS Medicare, a Part B payer in
four states, put its advice in writing back in January,
noting that “only the physician admitting the patient to
observation care status may bill these codes,” including
the admission (99218-99220), subsequent observation
(99224-99226), and discharge from observation
(99217) codes. Anyone else seeing the patient while
in observation care would bill using an office or other
outpatient procedure code (99201-99215), as appropriate.
Tip: CMS expects use of the subsequent observation care
codes to be infrequent, noting, “In the rare circumstance
when a patient receives observation services for more
than two calendar days, the physician will bill observation
services furnished on day(s) other than the initial or
discharge date using subsequent observation care codes.”
To read the complete MLN Matters article, visit www.
cms.gov/MLNMattersArticles/Downloads/MM7405.
pdf. q
You Be the Coder
Knock Out This Nasopharyngeal Case
Question:
How should I report the following case? A patient
presented for chemotherapy to treat a primary
malignant neoplasm of the nasopharyngeal floor.
The patient complained of new onset of extreme
fatigue, and the oncologist performed a level-3 office
visit to evaluate her. The patient then received a 30minute gemcitabine infusion followed by a 60-minute
cisplatin infusion. We did not supply the drugs.
Montana Subscriber
Answer: See page 87. q
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!
p85
The Coding Institute — SPECIALTY ALERTS
ICD-10-CM Call us: 1-877-912-1691
The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
}
C50.- Range Will Replace Both 174.x and 175.x
Prepare for more specific codes for male breast cancer patients.
ICD-9-CM codes for breast neoplasms are fairly specific,
but your ICD-10-CM options kick the detail requirements
up another notch. Here’s the lowdown on how ICD-10CM incorporates additional anatomic information and
increases the data needed when you code for male patients.
ICD-9-CM coding rules: Using ICD-9-CM 2011, your
coding options for primary breast neoplasms differ
based on sex.
For female patients you use 174.x (Malignant neoplasm
of female breast), and your fourth digit options relate to
anatomic location:
»
»
»
»
»
»
»
»
»
174.0, … nipple and areola
174.1, … central portion
174.2, … upper-inner quadrant
174.3, … lower-inner quadrant
174.4, … upper-outer quadrant
174.5, … lower-outer quadrant
174.6, … axillary tail
174.8, … other specified sites of female breast
174.9, … breast (female), unspecified.
For male patients, you use 175.x (Male neoplasm of
male breast). The fourth digit again relates to anatomic
site, but the list is much shorter:
» 175.0, …nipple and areola
» 175.9, … other and unspecified sites of male breast.
ICD-9-CM instructions for both 174.x and 175.x tell
you to report an additional code to identify the patient’s
estrogen receptor status (V86.0, Estrogen receptor
positive status [ER+]; V86.1, Estrogen receptor
negative status [ER-]).
ICD-10-CM changes: You’ll find a lot of similarities
between your ICD-9-CM and ICD-10-CM coding
options for breast neoplasms, such as the terminology
used to identify anatomic locations. There are some
differences you need to be aware of, though. Here’s
how ICD-10-CM structures the primary malignant
breast neoplasm range.
1. C50.- is the range for “Malignant neoplasm of
breast.” As with ICD-9-CM, you will use an
additional code to identify estrogen receptor status
(Z17.0, Estrogen receptor positive status [ER+];
Z17.1, Estrogen receptor negative status [ER-]).
2. The fourth character of the C50.- range identifies
the anatomic area: nipple and areola, central
p86
portion, upper-inner quadrant, etc. One difference
between ICD-9-CM and ICD-10-CM is that ICD9-CM has an “other sites” code for the female
breast. ICD-10-CM does not offer an “other sites”
code. It does offer a code range for “overlapping
sites”: C50.8-. The range applies to male and
female patients, as explained in point 3.
3. The fifth character of the C50.- range allows you
to identify whether the patient is male or female.
As a result, you’ll need to know the precise
anatomic location of the neoplasm for both male
and female patients. This differs from ICD-9-CM,
which has only two code options for male breast
cancer patients.
4. The sixth character of the C50.- range identifies
the affected breast (right, left, or unspecified).
Below is an example of the ICD-10-CM code options
for an upper-outer quadrant neoplasm:
» C50.411, Malignant neoplasm of upper-outer
quadrant of right female breast
» C50.412, Malignant neoplasm of upper-outer
quadrant of left female breast
» C50.419, Malignant neoplasm of upper-outer
quadrant of unspecified female breast
» C50.421, Malignant neoplasm of upper-outer
quadrant of right male breast
» C50.422, Malignant neoplasm of upper-outer
quadrant of left male breast
» C50.429, Malignant neoplasm of upper-outer
quadrant of unspecified male breast.
Coder tips: All of the information you’ll need to choose
the most specific ICD-10-CM code already may be in
the patient’s chart. The physician may not be pulling the
specific site information into his own documentation
in the progress note, however. When you’re billing the
professional fee, the provider’s documentation should
support your code choice. So as part of your ICD-10CM transition plan, educate your providers to routinely
document the laterality (right or left) and anatomic
location to support appropriate code choice.
Remember: When ICD-10-CM goes into effect on
Oct. 1, 2013, you should apply the code set and official
guidelines in effect for the date of service reported.
Learn more at www.cms.gov/ICD10/ and www.cdc.gov/
nchs/icd/icd10cm.htm#10update. q
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!
Call us: 1-877-912-1691
Reader Questions The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
}
203.01 Is More Appropriate Than ‘History of’ Code
Question:
Which “history of” code applies to myelomatosis in
remission?
Texas Subscriber
You Be the Coder
Knock Out This Nasopharyngeal Case
(Question on page 85)
Answer:
For the diagnoses indicated, you should report V58.11
(Encounter for antineoplastic chemotherapy), 147.3
(Malignant neoplasm of nasopharynx; anterior wall),
and 780.79 (Other malaise and fatigue).
The procedure codes and modifiers you should use
include:
» 96413 (Chemotherapy administration, intravenous
infusion technique; up to 1 hour, single or initial
substance/drug) for the gemcitabine infusion
» +96417 (Chemotherapy administration,
intravenous infusion technique; each additional
sequential infusion [different substance/drug], up
to 1 hour [List separately in addition to code for
primary procedure]) for the cisplatin infusion
» 99213 (Office or other outpatient visit for the
evaluation and management of an established
patient ...) for the E/M service
» Modifier 25 (Significant, separately identifiable
evaluation and management service by the same
physician on the same day of the procedure
or other service) appended to 99213 to show
that the E/M service was distinct from the
chemotherapy administration.
Tip: Although your practice did not supply the drugs
and therefore should not report them on your claim,
you still need to understand the drugs used so you
can choose the appropriate administration codes.
In other words, you need to know whether to use
a chemotherapy administration code or a different
therapeutic administration code. Individual payers
define which drugs qualify for the higher paying
chemotherapy administration codes, but gemcitabine
and cisplatin would both qualify.
ICD-9-CM link: On your claim, you should link
V58.11 and 147.3 to both 96413 and +96417. You
should link 780.79 to 99213-25. q
The Coding Institute — SPECIALTY ALERTS
Answer:
Rather than looking for a “history of” code, you should
use 203.01 (Multiple myeloma; in remission).
The fifth digit allows you to describe the disease as being
in remission, which basically means that the disease is
no longer observable in the patient. The disease is not
considered “cured,” however.
Your other fifth digit options for 203.0x include:
» 0, … without mention of having achieved remission
(also appropriate for failed remission)
» 2, … in relapse. q
93005 Describes ECG Tech Component
Question:
Techs employed by our center perform ECGs on certain
patients to check for toxicity. A different group provides
the interpretation and reports it. How should we report
our service?
Virginia Subscriber
Answer:
For the services your center performs, you should report
93005 (Electrocardiogram, routine ECG with at least 12
leads; tracing only, without interpretation and report).
Rationale: Although for many codes you would
indicate performance of only a portion of the service by
appending either modifier TC (Technical component) or
26 (Professional component), that method does not apply
for ECGs.
Instead, this family of codes provides separate options
depending on whether you perform the entire service
(93000, … with interpretation and report), the technical
component only (93005), or the professional component
only (93010, ... interpretation and report only).
Caution: Be sure payer agreements include the
component codes (93005, 93010) in the payer fee
schedule and not just the global code (93000). q
— Clinical and coding expertise for You Be the Coder
and Reader Questions provided by Kelly C. Loya,
CHC, CPC-I, CPhT, managing consultant with Sinaiko
Healthcare Consulting Inc.
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!
p87
The Coding Institute — SPECIALTY ALERTS
Call us: 1-877-912-1691
CodingInstitute.com; SuperCoder.com — Inspired by Coders, Powered by Coding Experts
Oncology & Hematology
C O D I N G
A L E R T
The Coding Institute LLC, 2222 Sedwick Drive, Durham, NC 27713
We would love to hear from you. Please send your comments, questions, tips, cases, and suggestions for articles
related to Oncology & Hematology coding and reimbursement to the Editor indicated below.
Deborah Dorton, JD, MA, CPC, CHONC
Kelly C. Loya, CHC, CPC-I, CPhT
deborahd@codinginstitute.com
Editor
Consulting Editor
Mary Compton, PhD, CPC
Jennifer Godreau, CPC, CPMA, CPEDC
maryc@codinginstitute.com
Editorial Director and Publisher
jenniferg@codinginstitute.com
Content Director
The Coding Institute - 2222 Sedwick Drive, Durham, NC 27713 Tel: 1-877-912-1691 Fax: (800) 508-2592 service@codinginstitute.com
Oncology & Hematology Coding Alert is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold with
the understanding that the publisher is not engaged in rendering legal, accounting, or other professional services. If legal advice or other expert assistance is
required, the services of a competent professional should be sought.
CPT® codes, descriptions, and material only are copyright 2011 American Medical Association. All rights reserved. No fee schedules, basic units, relative
value units, or related listings are included in CPT®. The AMA assumes no liability for the data contained herein. Applicable FARS/DFARS restrictions apply
to governement use.
Rates: USA: 1 yr. $249. Bulk pricing available upon request. Contact Medallion Specialist Team at
medallion@codinginstitute.com. Credit Cards Accepted: Visa, MasterCard, American Express, Discover
This publication has the prior approval of the American Academy of Professional Coders for 0.5 Continuing Education Units. Granting of
this approval in no way consitutes endorsement by the Academy of the content. Log onto Supercoder.com/membersarea to access CEU quiz.
To request log in information, e-mail service@codinginstitute.com
The Coding Institute also publishes the following specialty content both online and in print. Call 1-877-912-1691 for a free sample of any or all of the specialties below:
Part B (Multispecialty)
Anesthesia
Billing & Collections
Cardiology
Dermatology
Emergency Medicine
Family Medicine
Gastroenterology
General Surgery
Internal Medicine
Neurology& Pain
Management
Neurosurgery
Ob-Gyn
Ophthalmology
Optometry
Orthopedics
Otolaryngology
Pathology/Lab
Pediatrics
Physical Medicine &
Rehabilitation
Podiatry
Pulmonology
Radiology
Urology
Announcing Supercoder, the online coding wiz. Call us (800-508-2582) with your customer number for a special price, free trial, or just to find out more.
Order or Renew Your Subscription!
Yes! Enter my: one-year subscription (12 issues) to Oncology & Hematology Coding Alert
for just $249.
Extend! I already subscribe. Extend my subscription for one year for just $249.
Subscription Version Options: (check one) ❑ Print ❑ Online* ❑ Both*(Add online to print
subscription FREE) E-mail
Payment Options
Charge my:
❑ MasterCard
❑ AMEX
❑ VISA
❑ Discover
Card #
Exp. Date: ________/________/________
Signature:
* Must provide e-mail address if you choose “online” or “both” option to receive issue notifications
❑ Check enclosed
(Make payable to The Coding Institute)
Name
❑Bill me (please add $15 processing fee for
all billed orders)
Title
Company
Address
City, State, ZIP
Phone
Fax
Oncology & Hematology Coding Alert
The Coding Institute
PO Box 933729
Atlanta, GA 31193-3792
Call 1-877-912-1691
Fax (801) 705-3942
E-mail: service@codinginstitute.com
E-mail
To help us serve you better, please provide all requested information
p88
SuperCoder is a property of CodingInstitute.com
Specialty specific codesets, tools and content on one page in SuperCoder.com. Call 1-866-228-9252 now for a super deal!