Serial Casting for the Management of Spasticity in the Head
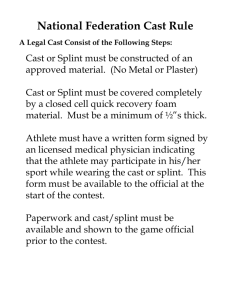
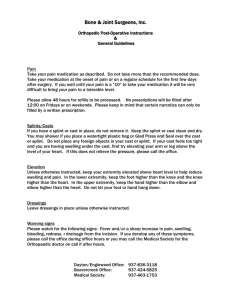
advertisement

Serial Casting for the Management of Spasticity in the Head-Injured Adult B. J. BOOTH, MARI DOYLE, and JACQUELINE MONTGOMERY Soft tissue contractures resulting from spasticity are a frequent sequella of traumatic head injuries. This article identifies rationale for the use of serial casting to manage these deformities, provides guidelines for cast fabrication and application, and reports the results of lower extremity casting on 42 headinjured adults at Rancho Los Amigos Hospital. Key Words: Contracture, Head injuries, Physical therapy, Plaster casts. After traumatic head injury, many patients develop soft tissue contractures as a result of spasticity. Passive range-of-motion (ROM) exercises, positioning, stretching, and splinting techniques1 are often inadequate for maintaining joint motion in the head-injured patient. Serial plaster casting is a technique that has been used effectively for over a decade to manage spasticity-induced contracture in these patients.2, 3 This technique can also be used in the presence of potentially deforming spasticity to prevent the development of contractures. The purposes of this article are to identify the rationale for using serial casting, to present guidelines for the fabrication and application of casts, and to report the results of lower extremity casting on 42 head-injured adults at Rancho Los Amigos Hospital in Downey, California. INDICATIONS AND CONSIDERATIONS FOR SERIAL CASTING Indications for serial casting are ROM limitations or presence of potentially deforming spasticity. The causes of ROM limitations must be assessed carefully. Serial casting is most effective in managing soft tissue contractures resulting from spasticity. Range of motion limitations in head-injured patients can also be the result of heterotopic ossification, fractures, or ligament injuries. Serial casting may be used in these conditions but may not be as effective. Serial casting has been the most effective in our experience when used within the first six months after Ms. Booth is a physical therapist and Co-director of The Head Injury Center at Lewis Bay, 89 Lewis Bay Rd, Hyannis, MA 02601 (USA). Ms. Doyle is an occupational therapist and Co-director of The Head Injury Center at Lewis Bay. Ms. Montgomery is Physical Therapy Supervisor II, Physical Therapy Department, Rancho Los Amigos Hospital, 7601 E Imperial Hwy, Downey, CA 90242. 1960 injury and with patients demonstrating ongoing neurological recovery. Patients with long standing and fixed joint contractures may demonstrate some improvement in ROM after a serial casting program. If no underlying motor control is unmasked and spasticity is not reduced after the casting procedure, the probability of maintaining improvement in ROM without bracing or splinting is poor. When assessing a patient for serial casting, the clinician must take several factors into consideration. In the early acute phase, the initial consideration is the patient's medical stability. Some physicians believe that casting increases intracranial pressure, but others do not believe that casting has a direct effect on intracranial pressure changes. The therapist must consult the attending physician before initiating a casting program. Other medical considerations include unhealed fractures, poor skin condition because of lacerations or abrasions, and need for easy accessibility of the limbs to monitor vital signs and to administer medications. These factors may necessitate postponement or modification of the casting program. Another factor to consider with the head-injured patient is that cognitive impairment often interferes with the patient's ability to cooperate and relax, and to interpret and respond to pain. The therapist must develop skill in assessing the actual easily obtained ROM and the point at which the limb should be casted and must not be confused by the patient's initial response to pain. GUIDELINES FOR THE APPLICATION OF CASTS For patients in a treatment program scheduled for five days a week, all casts should be applied early in PHYSICAL THERAPY the week so that the patients can be closely monitored for possible complications, such as pressure areas and swelling. During the cast application, we check for vasoconstriction or discoloration of the fingers or toes. Temporary skin discoloration during the actual cast application is not uncommon, but if the discoloration persists for more than 20 to 30 minutes, the cast should be removed and a new cast applied. Special care should be taken to ensure that all areas that are vulnerable to pressure, such as bony prominences, are well padded to prevent skin breakdown. Lower extremity casts should be allowed a minimum of 24 hours to dry before the patient resumes weightbearing activities to ensure the integrity of the cast and to prevent unwanted indentations that may be a source of pressure and skin breakdown. All casts used for weight bearing should be provided with a plantigrade surface. At every cast change, the therapist should provide passive ROM to maintain full mobility of all immobilized joints. Patients who are agitated may require extra plaster to prevent breakdown of the cast from abuse. Fiberglass casting material is not recommended in these cases because it often splinters, leaving sharp edges. GENERAL PROGRESSION OF SERIAL CASTING The initial cast in a serial casting program is referred to as the resting cast. It is applied with the limb positioned at the end of its easily obtainable ROM and is left on for 7 to 10 days. After the resting cast, a series of positional or drop-out casts are applied at weekly intervals. Between cast changes, the therapist guides the limb through a complete ROM and applies each new cast in a slightly improved position of correction. Most often, three to four positioning casts are used to achieve the desired ROM corrections. Once the desired or maximally obtainable ROM has been achieved, the final or holding cast is applied. The holding cast remains in place for 7 to 10 days to ensure the maintenance of the newly acquired ROM. The holding cast is then bivalved and converted into an anterior-posterior splint. The patient is gradually weaned from the anterior-posterior splint as he becomes more active. A patient who continues to have weakness and increased spasticity wears his anteriorposterior splint at night. Materials for Cast Application In preparation for initiating a casting program, the therapist should obtain adequate materials and supplies. Supplies required include the following: bandage scissors; cast saw, trimming knife, spreader, and bender; plaster bucket; and tepid water. Materials Volume 63 / Number 12, December 1983 required include the following: 3-in,* 4-in, and 6-in rolls of cotton cast padding; 2.5-in tubular stockinette for upper extremity casts and 4-in stockinette for lower extremity casts; foam padding; felt padding; 4in and 6-in fast-setting or extra fast-setting plaster rolls; 3-in by 5-in plaster splints for upper extremity casts and 4-in plaster splints for lower extremity casts. The procedure is explained to the patient in simple terms, and if he is nervous or frightened, an attempt is made to allay the anxiety. The patient is positioned correctly before beginning. Lower extremity casts are applied with the patient in the supine position. For upper-extremity cast application, the patient can be either supine or sitting. Sheets or plaster drapes are used to protect against plaster spillage. Procedures for Cast Application Tubular stockinette is precut to approximately the length of the limb receiving the cast and is rolled into a "doughnut." The stockinette is rolled onto the limb and smoothed out to eliminate wrinkling. Cotton padding is applied in a spiral fashion by working in smoothly overlapping 1.5-in layers. At least two to three layers are required. Special caution is taken to prevent wrinkles. Foam padding is applied to all bony prominences, and an additional roll of cotton padding is applied over the foam. Plaster rolls are dipped with the ends up in tepid water for several seconds. The ends of the role are crimped to avoid a wringing motion when removing excess water. The plaster is applied to the limb in the same spiral fashion as the padding and is smoothed and molded as progress is made. When the plaster is rolled, the roll is kept as close to the limb as possible to avoid pulling the plaster, which causes tension on it. The limb is maintained in the desired position as the plaster sets; care is taken to avoid indenting the plaster with the fingers and producing unwanted pressure points. Two rolls of plaster are usually adequate for upper extremity casts and three to four rolls for most lower extremity casts. Larger or stronger patients may require additional plaster. When the plaster sets, the stockinette is folded over the cast edges and secured with plaster splints. Casts can be fabricated without the use of stockinette. However, stockinette is recommended for those casts that will be bivalved and converted to anteriorposterior splints. The stockinette protects the cotton padding from fraying and becoming wadded during frequent splint removal. If the stockinette becomes stained, it can also be easily replaced. The procedure for fabricating plaster casts is essentially the same for all casts. Drop-out casts are modifications of cylinder casts. For example, the elbow * One in equals 2.54 cm. 1961 Fig. 1. Elbow drop-out cast Fig. 2. Knee drop-out cast with the anterior portion of cast removed below the knee. Fig. 6. Short-arm cast. Fig. 5. Elbow drop-out cast with the hand included. drop-out cast is fabricated from a long-arm cylinder cast (Fig. 1). The posterior upper arm is cut out along the medial and lateral aspects with a cast saw. The two cuts are connected with a curved cut just distal to the olecranon process. After the shell is removed, the cotton padding and foam are cut to the cast edges. The exposed stockinette is split down the posterior aspect of the arm, folded over the cast edges, and affixed to the cast with 3-in by 15-in plaster splints. The edge of the cast distal to the olecranon process is bent out slightly with a cast bender to provide a smooth rounded edge. The knee drop-out cast is an adaptation of the long-leg cylinder cast including the foot (Fig. 2).4 The anterior lower shell of the cast is removed from anterior to the medial and lateral epicondyles and femoral condyles to just superior to the patella. The cotton padding and foam are removed, and the stockinette affixed to the cast in the same manner as described with the elbow drop-out cast. When the patient is in the prone position, his knee is permitted to extend, but not to flex. When he is in the supine or sitting position, his foot is supported in the posterior shell of the cast and held in good alignment. If a patient has a severe equinovarus deformity, the lower portion of the knee drop-out cast can remain intact and the anterior thigh portion of the cast can be 1962 removed from anterior to the femoral condyles to just inferior to the patella (Fig. 3). Two of the more commonly used casts are applied as follows: 1. Long-arm cast. The patient's hand is placed through a precut 2.5-in tubular stockinette "doughnut," and the stockinette is rolled from the wrist up to the axilla. The 3-in cotton padding is applied by working from the wrist, just proximal to the ulnar styloid process to about 2 in below the axilla. Foam padding is applied to all bony prominences at the wrist and elbow. At the elbow, a foam pad is placed over the olecranon process and both humeral condyles. An additional roll of cotton padding is used to cover the foam. A 4-in roll of plaster is moistened, applied to the arm starting at the wrist, and smoothed and molded. The elbow is maintained in the desired position as the cast sets. The stockinette is folded over the cast edges and incorporated with 3-in by 15-in plaster splints. 2. Short-leg cast. A 4-in piece of tubular stockinette is measured and cut to extend from the knee to about 1 in distal to the great toe. The stockinette is placed on the foot and unrolled up to the knee. The excess stockinette is gathered at the anterior aspect of the ankle and folded smoothly. The fold may need to be cut and overlapped to prevent PHYSICAL THERAPY Fig. 3. Knee drop-out cast with the anterior portion removed above the knee. Fig. 4. Elbow drop-out cast with the wrist included. Fig. 7. Short-arm cast with thumb spica. Fig. 8. Short-arm cast with the hand included. Note flexion of MCP joints. wrinkling. A roll of 3-in or 4-in cotton padding is applied as described before. Use of a figure-eight wrapping technique around the ankle and heel helps to prevent gapping. Again, two to three layers of padding are desired. Foam pad is applied around the posterior heel and over the medial malleolus and lateral malleolus. If the tibia is prominent, a foam pad is placed from the ankle to the knee. The foam is covered with an additional roll of cotton padding. A 4-in or 6-in plaster is moistened and applied, working from the toes to the knee and avoiding wrinkles at the uneven surfaces of the foot and ankle. The foot is held in the desired position by using the palm of the hand to avoid pressure from the fingers. If additional cast strength is needed, five 5-in by 30-in plaster splints are applied along the plantar surface of the foot and the posterior aspect of the leg and incorporated into the cast with an additional roll of plaster. The top of the cast is trimmed back to expose the toes and the stockinette is incorporated as before. CLINICAL APPLICATION OF SERIAL CASTING The most common problems of the upper extremity that are managed with serial casting occur at the Volume 63 / Number 12, December 1983 elbow, wrist, and hand. The most prevalent problem at the elbow, amenable to serial casting, is limited elbow extension. A long-arm resting cast is applied at the end of the easily obtainable passive extension ROM. Seven to 10 days after application, the cast is removed and followed by a progression of elbow drop-out casts. These casts permit passive and active motion into extension while maintaining the already acquired extension ROM. The advantage of cutting out this cast at the proximal end is that the weight of the cast will act with gravity to provide a passive stretch when the patient is sitting or upright. Variations of this cast can be made to include the wrist or hand (Figs. 4, 5). When the cast is applied, the forearm is placed in a position of neutral supination and pronation. These casts should be changed weekly. Once the maximal extension ROM has been obtained with drop-outs, the patient is placed in a holding cast to ensure maintenance of the final ROM. This cast is bivalved and removed in 7 to 10 days and made into an anterior-posterior splint to be used mainly as a night splint. The straps are attached to the splint with plaster to prevent them from being lost. The confused patient may also need the straps taped down to prevent him from removing the splint. 1963 The most common problems in the wrist and hand, amenable to serial casting, also relate to limited extension ROM. A series of short arm casts are used to bring the wrist to a functional position and maintain it in about 30 degrees to 45 degrees of extension (Fig. 6). Casts are changed every 7 to 10 days. During application, special attention is given to the web space and thumb to ensure free mobility of the thumb and to the volar surface to ensure that the cast is cut back proximal to the distal palmar crease, which allows the metacarpophalangeal (MCP) joints to flex and prevent shortening of the collateral ligaments. Variations of the cast can be used to address more specific problems. For example, the thumb may be included through incorporating a thumb spica (Fig. 7). The spica helps maintain the web space and prevent the thumb from posturing in the palm. Positioning the thumb in abduction and extension has also been known to decrease flexion tone in the wrist and hand.5 Another variation is the full-hand cast in which the fingers as well as the thumb are included (Fig. 8). This cast is most often used with patients who demonstrate a severe increase in finger flexion and intrinsic muscle tone. Special precautions must be taken with this type of cast to prevent ROM limitations at the MCP joints. Therefore, this cast should be applied with the MCP joints in flexion, changed every five to seven days, and never used in progression for more than two weeks. Any of the above short-arm casts can be bivalved and made into anterior-posterior splints. The most common problems of the lower extremity that respond well to casting occur at the knee and ankle. At the knee, casting can be used for improvement of knee flexion contractures. Initially, the leg is positioned in an easily obtained passive knee extension ROM and placed in a long-leg resting cast. Patients who are unable to assume a prone position or who have knee flexion contractures of 60 degrees or more will continue on a progressive serial casting program until the knee flexion contracture decreases to less than 60 degrees. At that point, if the patient can tolerate a prone position, a progression of knee drop-out casts can be used. The knee drop-out cast permits free extension but does not allow flexion. Once optimal knee extension ROM is achieved, a long-leg holding cast is used to maintain the knee in its corrected position for two weeks. The holding cast is converted to an anterior-posterior splint, which the patient wears full time initially. He is gradually weaned from the splint as he becomes more active and eventually uses it as a night splint only. TABLE 1 Equinovarus deformity is the most common spastic Changes in ROM and Muscle Tone with Use of Shortdeformity after head injury because it occurs with Leg Casts in Patients with Cortical Lesions both decorticate and decerebrate posturing. A progressive short-leg serial casting approach is recomDorsiflexiona ROM (°) Plantar Flexor b Tone mended. After the initial resting cast, a series of shortleg casts are used to correct the equinus and varus Range Range positions gradually. After the foot has been corrected - 5 0 to0 1.9 1 to 3 Precast -16 to neutral position, it is maintained in plaster for two 1.4 0to3 Postcast 0.7 - 1 5 to 20 weeks. Once the holding cast has been converted to 0.5 0to2 17 Change - 5 to 50 an anterior-posterior splint, the splint can be used as a Ankle motion measured from right-angle neutral po- a night splint, and foot positioning can be maintained sition. during the day in a well-fitting ankle-foot orthosis b 0 = Normal, 1 = Slightly Increased, 2 = Moderately Increased, and 3 = Severely Increased, based on resist- with the ankle locked in neutral position. Adaptations can be made to existing lower extremance to passive motion. ity casts to address ROM limitations of abduction TABLE 2 and internal rotation at the hip. Adductor contracChanges in ROM and Tone with Use of Short-Leg Casts tures can be stretched out with the use of a "spreader in Patients with Brain-Stem Lesions bar." A predetermined length of wooden slat or doweling is attached to bilateral long-leg casts, between Plantar Flexor a Dorsiflexion ROM (°) the thighs, and just superior to the knees. The patient's Tone5 legs are abducted to their available range and rigidly Range Range maintained by the cut section of doweling, which is -24 Precast - 6 0 t o - 5 1.8 1 to 3 affixed to the casts with plaster strips. This method is 2 - 2 5 to 20 1.5 0 to 3 Postcast successful for patients with severe spasticity of both 26 -2cto2 Change 60 to 10 0.4 lower extremities, but its use is not always practical a Ankle motion measured from right-angle neutral po- because the spreader bar creates some difficulty with sition. side-lying and wheelchair positioning and makes b 0 = Normal, 1 = Slightly Increased, 2 = Moderately lower extremity dressing an impossibility. A removIncreased, 3 = Severely Increased, based on resistance able spreader bar can be made by putting stockinette to passive motion. c over the thigh or heel portion of existing casts and Indicates increase of tone. 1964 PHYSICAL THERAPY making a thin plaster mold over the stockinette. The spreader bar is attached to the plaster mold. Once the new plaster is dry, it is cut with a cast saw to form a plaster cup, which can be worn or removed as necessary. Another common deformity occurring at the hip that can be alleviated with adaptations to existing lower extremity casts is external rotation tightness. The technique used is similar to the one described for the spreader bar. In this case, a 6- to 8-in piece of wooden doweling is attached to the lateral aspect of an existing short-leg or long-leg cast. We refer to this adaptation as an outrigger or derotation bar. The doweling is attached with plaster strips to the posterior-lateral aspect of the existing cast, superior to the lateral malleolus. When the patient is supine in bed, the outrigger is supported against the mattress and holds the lower extremity in neutral rotation. When the patient is sitting in a wheelchair, the outrigger is supported against the legrest bracket of the wheelchair and once again, holds the limb in neutral rotation. Nonremovable outriggers cause the same problems as nonremovable spreader bars. Removable outriggers can be constructed by attaching the doweling to removable plaster heel cups. RANCHO LOS AMIGOS HOSPITAL CHART REVIEW Patients by Lesion PostPrecasting casting Dorsiflexion Dorsi- Change (°) ROM (°) flexion ROM (°) Cortical (n = 5, 8 limbs) Range -15 4 - 2 0 to - 5 0 t o 2 0 19 - 5 to 30 9 -15 - 4 5 to - 5 0 t o 2 0 24 10 to 45 Brain Stem (n - 4, 5 limbs) Range a Ankle motion measured from right-angle neutral position. TABLE 4 Long-Leg Casts Applied to Increase Knee Extension ROM and to Decrease Knee Flexor Tone in Patients with Cortical Insults Patients (n = 5) Precasting Postcasting Change Knee Extension ROM (°) Range -32 -5 - 1 0 to - 9 0 - 2 0 to 0 + 27 - 1 0 to 90 Tonea Charts of 201 patients admitted to the Adult Head Trauma Service at Rancho Los Amigos Hospital from January 1980 through September 19, 1981 were reviewed to determine the frequency of cast use and to assess the results of lower extremity serial casting. Forty-two of the 201 patients (21%) had lower extremity serial casting for problems of decreased ROM, increased muscle tone, or both. Patients who received casts for these problems but had concomitant limb pathology, such as fracture, heterotopic ossification, and peripheral nerve injuries, were excluded from the review. For purposes of data analysis, patients were grouped by area of brain injury and indications for and type of cast applied. The largest number of patients who had serial casting were those with cortical lesions. This group had short-leg casts applied because of decreased dorsiflexion ROM and increased plantar flexor muscle tone. Twenty-four of the 42 patients (57%) were in this classification. Ten of these patients had bilateral short-leg casts. Nineteen of the patients were men, 5 were women, and the average age was 23 years old. The mean time from injury to the beginning of casting was 78 days. Mean casting duration was 28 days with a range of 7 to 88 days. Results are shown in Table 1. The second highest number of patients who received short-leg casts were those with brain-stem or Volume 63 / Number 12, December TABLE 3 Short-Leg Casts Applied to Increase Dorsiflexion ROMa 1983 Range 2.5 2 to 3 2.75 2 to 3 -0.25 -1b to 0 a 0 = Normal, 1 = Slightly Increased, 2 = Moderately Increased, and 3 = Severely Increased, based on resistance to passive motion. b Minus indicates increase of tone. both cortical and brain-stem lesions. These casts were applied because of decreased dorsiflexion ROM and increased plantar flexor muscle tone. Fifteen patients (36%) received casts; five casts were bilateral. Nine of these patients were men, six were women, and the average age was 20 years old. The mean onset of casting interval was about three months. Mean casting duration was 39 days with a range of 7 to 92 days. Results are shown in Table 2. Table 3 shows the results of patients with cortical or brain-stem lesions who received short-leg casts to correct decreased dorsiflexion ROM only. Long-leg casts, incorporating the ankle and foot, were applied to increase knee extension ROM and to decrease hamstring muscle tone. During the 20month period reviewed, five patients with cortical lesions had unilateral long-leg casting. Their average age was 25 years. Mean casting duration was 22 days with a range of 8 to 66 days. Their mean onset to casting interval was 114 days; this period indicates their acute care was longer than those patients who had short-leg casts. Results are shown in Table 4. 1965 TABLE 5 Long-Leg Casts Applied to Increase Knee Extension ROM and to Decrease Knee Flexion Tone in Patients with Brain-Stem Lesions Patients (n=4) Precasting Postcasting Change -25 - 9 0 to - 5 -10 - 3 0 to 0 15 - 1 5 to 90 1.8 1 to 3 1.6 1 to 3 0.2 0 to 1 Knee Extension ROM (°) Range Serial short-leg casting is an effective technique to increase dorsiflexion ROM and to decrease plantar flexor muscle tone in the young adult after head injury. Serial long-leg casting in itself is not the answer to reducing knee flexor tone, although casts prevent further loss of knee extension ROM and, in fact, increase range. CONCLUSION Tone a Range „, a 0 = Normal, 1 = Slightly Increased, 2 = Moderately Increased, 3 = Severely Increased, based on resistance to passive motion. Four men, averaging 24 years old, with brain-stem lesions received long-leg casts for both decreased ROM and increased tone. Casting started an average of 111 days from onset and was continued for an average of 31 days with a range of 7 to 58 days. Results are shown in Table 5. All patients who received casts for decreased dorsiflexion range improved in ROM, All patients, except two, who had casts for decreased ankle ROM and increased plantar flexor muscle tone improved in range. The two who did not improve had severely increased muscle tone both precasting and postcasting. Thirty-seven percent of the patients who received casts for decreased ankle ROM and increased plantar flexor muscle tone had decreased tone postcasting. Knee flexion tone decreased in only one patient who had serial long-leg casting. One-half of the limbs in casts failed to gain full knee extension. As compared with patients with cortical lesions, patients with brain-stem lesions who had both decreased ankle ROM and increased plantar flexor muscle tone started with worse contractures, received casts later from onset, and took longer to make ROM gains. 1966 Progressive serial casting is a technique that can be used for the management of deformity resulting from spasticity in the head-injured adult. Casting is recommended during the early and acute management so that immobilization occurs while the patient is at his lowest level of consciousness. General guidelines for a casting program have been described as well as specific clinical applications. Cast application procedures require technical skill to prevent complications. The results of a chart review of lower extremity casting of 42 head-injured adults have been described. Serial casting is an adjunct to treatment and should be incorporated into an ongoing therapeutic program. REFERENCES 1. Cherry DB: Review of physical therapy alternatives for reducing muscle contracture. Phys Ther 60:877-881, 1980 2. Booth BJ, Doyle MM, Woodword J: Application of casts for control of spasticity. In Rehabilitation of the Head Injured Adult: Comprehensive Management. Downey, CA, Professional Staff Association of Rancho Los Amigos Hospital, Inc, 1980, pp 25-30 3. Garland D, Doyle MM, Booth BJ: Early management of spastic deformities. In Rehabilitation of the Head Injured Adult: Comprehensive Physical Management. Downey, CA, Professional Staff Association of Rancho Los Amigos Hospital, Inc, 1979, pp 45-51 4. Cherry DB, Weigand GM: Plaster drop-out casts as a dynamic means to reduce muscle contracture. Phys Ther 61:1601-1603, 1981 5. Bobath B: Adult Hemiplegia: Evaluation and Treatment. London, England, Heinemann Medical Books, 1978, p 130 PHYSICAL THERAPY