attachment p note writing - Program in Physical Therapy
advertisement

fType text]
ATTACHMENT
P
NOTE WRITING
I.
General Descriptions of Types of Notes PT's Write
A.
Initial Notes
The initial note should contain all data obtained from evaluating the patient on his first visit.
This includes the data and reason for referral, who referred the patient and medical diagnosis.
A statement of chief complaints and other relevant information gleaned from the
patient/patient's family are included. It must contain all of your objective findings from your
evaluation. Also included is your assessment is a summary list of problems, recommended
interventions, response to treatment provided, goals and plan. Documentation stating
interventions initiated, what it consisted of, and level of patient participation/concurrence with
PT plan should be included.
B.
Progress Notes
Progress notes are written at a frequency determined by the patient's condition and by
departmental policy. Progress notes should address new problems and information about any
ongoing problems which are being treated. They should include exact measurements of
changes from the initial evaluation, exact statements of treatment procedure (length of
treatment, temperature or settings of equipment, positioning or equipment used in treatment)
and of patient response to treatment (vital signs, skin changes, patient complaints etc.)
Indicate whether consultation with other professionals (doctor, OT, prosthetist, etc.) has
occurred and what the patient has been taught about his condition. Conclude by indicating the
plans for fuither treatment or discontinuation of treatment. Depending on the facility,
attendance notes stating what treatment was done and how patient handled the treatment may
be required for every P.T. session.
C.
Discharge Notes
Discharge notes should summarizethe course of treatment, response and final status of the
patient. There should be a comparison of the final status and initial condition. The reason for
discharge or discontinuation, the disposition of the patient and follow-up plan for PT should
also be included.
75
fType text]
II.
Format for Initial. Interim. and Discharge Notes
The S.O.A.P. form is used in many hospitals to facilitate organization of relevant patient information,
even if the Problem Oriented Medical Record system is not strictly enforced.
S - subjective
O - objective
A - assessment
P - plan
m.
General Format of an Initial Note
Initial note should include the following information prior to the S.O.A.P. component of the note:
Date:
Time in:
Patient is
Time out:
a
year old man/woman with the diagnosis of
(date) for physical therapy
Dr.
includine
,
referred by
Date of lnitiation:
Date of Onset:
The patient has consent to be examined and evaluated.
The following outline contains suggestions for inclusion under the headings in the S.O.A.P. format
(initial, progress and discharge notes):
S:
Subjective Information (what you hear)
a.
Patient's description of his complaints, loss of function, pain and date of onset.
patient cannot speak, note non-verbal communication.
If
b.
Relevant data obtained from interview with the patient and"/or family which cannot be
verified from the medical record or previous treatment.
c.
Staternents taken from interviews with the family about the patient's problems or
condition.
d.
The patient's goals for him/herself
e.
Patient's prior level of function
f.
Patient's home environment
g.
If in out-patient, PMH
(past medical history obtained in the interview. Also include
76
[T1pe text]
screening checklist information, medications, tests etc.
O:
A:
Objective Information (what you observe and do)
a.
Portions of patient's chart history relevant to the current problem and treatment in PT.
This might include a summary of recent surgery, reason for admission and referral,
laboratory reports or x-rays, but should be bne[. Many times "chart reviewed and
PMH noted" is sufficient. also include any precautions or restrictions. Examples of
precautions are weight-bearing status, medications, aspiration, fall risk etc.
b.
Results of your examination: listing all impairments and functional limitations tested,
e.g. strength, sensation, anthropometrics, goniometry, edema, functional performance,
observations that are specific regarding posture and quality of movements.
c.
Interventions performed: where, when, what, how long? This does not usually include
the specific exercise used in treatment but rather the tlpe of exercise.
Assessment (what you think)
a.
Professional evaluation of overall impairments based on integration of the subjective
and objective findings.
b.
Identify and interpret problems, relate to overall function.
1.
2.
Clarit'the problerns which physical therapy
can address. These may include
impairments and/or functional limitations. List and number them, in order of
priority for treatment or severity.
Specifu the (contributing factors) (impairments) which explain the problems on
the problem list.
c.
List the diagnosis for physical therapy (or classification.)
d.
Patient's specific response to intervention: physical response to treatment (improved,
unchanged, worsened), emotional reaction to treatment. Never document that the
patient "tolerated treatment well."
lnclude a statement of rehabilitation prognosis (excellent, good, fair, poor, guarded)
for functional recovery and the deductions and expectations that support the prognosis
(may not be required). These deductions are based upon moderating factors that are
either positive or negative. ** Must document why patient needs continued physical
therapy.
e.
P:
Plan (what you
will do)
a.
What PT treatment is planned - continue or change treatment.
b.
Progression of the plan.
c.
Education planned for patient/family.
d.
Differentiate and outline the short and long term goals in measurable terms and with
time frames indicated. Long Term Goals must be functionally oriented (not focused on
impairments.) Short Term Goals may focus on impairment or function, although
Medicare requires all goals to be in functional terms. Also state that the patient
participated in establishing the goals if they did.
e.
Estimate the exact expected length of time needed to realistically complete the
treatment program.
f.
Frequency/duration of treatment.
g.
Follow-up
l.
Consultation with or referral to other professionals or agencies
planned (if appropriate).
2. Anticipated needs after discharge: equipment, setting,
3. Informed consent: document that the patient has been informed of the findings
and consents to further intervention as planned. (See specific format later in
this handout.)
[Type text]
IV.
"Service" Treatment Note - Inpatients
A brief note is written in the chart every time the patient is treated in order to meet requirements
from third party payers and risk management and to improve continuity of care. Also as
communication to other health care providers about patient's rehabilitation status. SOAP format may
be used, but is not necessary.
The date and the time the treatment was completed should be written in the margin. If the chart is
unavailable and you have to write the note later, indicate the time you write the note in the left
margin. The time the treatment occurred should be in the body of the note.
The treatment administered should be listed. If the treatment follows a well-known protocol or has
been stated in the initial note, just state the title of the treatment (ex: LE ROM, ADL Training,
Speech/Language, Swallowing Therapy per plan). If the treatment deviates from protocol or the
original plan, the difference should be stated along with the reason for a change.
The patient's response to treatment is important. Patient complaints should be noted and/or your
statement of how patient responded. Your staternent may include objective measures, i.e., BP, pulse,
SOB. Any deviation from the expected response should be documented, as well as your follow-up.
The active therapy plan should be designated clearly. Do not write "as above" or "continue per
plan". State what the plan is.
79
[T1pe text]
V.
Service Progress Note
Date:
S:
This includes pertinent data from the patient and/or family. May include comments the
patient/family have made RE: progress, compliance to treatment plan, specific complaints,
etc. If no comments were made, state that "patient voiced no concerns."
DO NOT LEAVE THIS SECTION BLANK!
O:
Current Problem List: List existing problems only. Use abbreviated format. There is no
need to list resolved problems. They should be listed in daily notes as they are resolved.
Address the problerns that is/are of concern, i.e. dressing, gut, swallowing. Provide objective
measures of progress. Note: Each problem should be addressed at least one time per month.
Treatment provided: Describe the interventions provided to the patient.
A:
Professional opinion of how patient is doing and why they would benefit from continued
therapy. Review status of goals. List goals currently being addressed. State any goals that
have been achieved. Be brief. You do not have to re-state entire goal in behavioral terms. Restate in abbreviated form, i.e. gait, ROM, dressing.
Any new problems that may be identified during therapy should be listed here. New problems
are numbered and added seque'ntially to the existing problem list.
P:
Any new goals should be listed here. If goals are added or a change in the treatment plan is
*ud", a statsment of patient participation is needed. Time frames for achievement of
additional goals should also be included.
Signature:
Phone/Beeper:
80
fType text]
VI.
"Seryice"Initial-DischareeNote
Date:
Patient with (Djasnosis) referred by Dr.
@)
on (Date) for (84-p!4).
DATE OF SERVICE: (If different than above)
S:
(PMH perpt)
O:
PMH: per chart
Evaluation results
Treatment provided
A:
Brief summary of findings of the evaluation and the patient's limitations.
Rehab Proenosis:
Problem List
P:
Patienflpt's family participated/unable to participate in establishing the following goals
and plans.
treatment sessions)
Goals: (to be achieved itt
Treatment Plan:
-
Patient discharged/discontinued secondary to :
Discharge Plan/follow-uP
:
Signature:
Phone/Beeper
8l
[Type text]
VII.
PT ConsultNote
Date of visit
Patient is a _
year old man/woman with the diagnosis of
on
_(date) for physical therapy
referred by
including
S:
Pertinent data from patient and./or family.
O:
Screening results.
A:
Summary of status per screening.
P:
Any follow-up.
EX: "No interyention indicated."
or "Will obtain referral for (seirrice)
"evaluation and treatnent.
u
Therapist:
Date:
Phone:
82
[Type text]
Additional Guidelines for Specific Sections of the Note
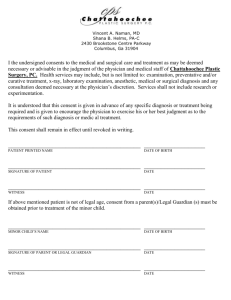
Infarmed Consent
-
fundamental right in case law, by statute or as a matter of customary practice
required by APTA and accreditation standards
Checklist Disclosure Elements for Patient Informed Consent to Treatment
- Diagnosis or evaluative findings
- Description of the recommended treatment
- Material (decisional) risks/foreseeable complications/precautions associated with the
proposed treatment
- Prognosis if the treatment is carried out
- Reasonable altematives to the proposed treatment, and attendant risks and prognosis
if an alternative treatment is used
- Solicit and answer the patient's questions about treatment
Documenting Informed Consent
1. consent forms
2. documentation if treatment records
3. use of informed consent checklists
4. reference to standard operating procedures or clinic policy staternents
Example from Legal Aspects of Documentation by Ronald Scott, page 144:
Pt. verbqlizes/demonstrates understanding of pt.'s diagnosis, proposed treqtment
program, major risl<s (if any), expected benefits, reasonable alternatives (if any)- I
askidfor pt.'s questions and answered them to pt.'s satisfaction. Pt. understands all
and agrees to undergo proposed treatmentLegal Aspects of Documentation, Ronald Scott, Aspen Publication, 1994,pp. ll5-147.
Guidelines for Documentation, APTA, 1996, p' 1'
83
[Type text]
Problem Lists
Problem lists should be complete and numbered for each patient. They must be limited to
problems which can be addressed directly by a physical therapist through direct
treatment. Problems are not medical diaenoses or problems outside the realm of PT
practice. The following examples demonstrate ac"ceptable ways of stating the patient's
functional problems.
Examples of functional limitations
inability to perform trunk flexion without pain
dependent transfers
inability to reach overhead
need for assistance with home exercise program
unsafe ambulation in the community
inability to perform age-appropriate gtoss motor tasks
improper lifting technique
Examples of lack of equipment for the patient
inadequate protection of surgical repair
unprotected fracture
lack of equipment for bath transfers
Examples of education needed by the patient
decreased knowledge of j oint protection methods
inability to demonstrate surgical precautions
inability to modifu activity level safely and independently
decreased knowledge of use and care of wheelchair
need for education in Precautions
need for education in fall prevention
need for family instruction
NOTE: Education is a problern that is addressed with just about any
patient. It most likely should not be listed as an isolated problem,
Lo*"rr"t. Don't document treatrnent ofjust education alone.
84
fType text]
Other acceptable examples of problems:
-
Impaired safety with
home mobility
community mobility
Decreased independence
with
mobility
transfers
stairs
gait
-
-
lnstability
with sitting
with standing
in the home
in the community
Risk for musculoskeletal pain
Unable to tolerate continuous activity
Need for home exercise program
Pain with mobility
Need for symptom control
Need for wound healing (Failure of wound healing)
Need for wound care
Need for positioning progrirm (Lacks positioning program)
Need for secretion clearance (inadequate secretion clearance)
Avoid listing as problerns, those which cannot be directly measured, or treated, or for
which you cannot formulate goals. For example - impaired sensation, tone, abnormal
reflexes. (Note these tend to be impairments.)
B)
Assessment of the Problern
The assessment section of a note must also include the following:
1.
Contributing Factors (not necessarily listed or numbered)
The contributing factors help explain the problem list. The student must include
this information to convey their professional opinion of what is causing the
impairment or functional limitation.
85
[Type text]
Examples of impairments/contributing factors:
Decreased ROM
Decreased motor function
Inaccurate perception of stability
Delayed balance reactions
Abnormal physiological response
Adventitious breath sounds
Altered alignment
Change in weight bearing status
Decreased activity tolerance
Decreased chest expansion
Decreased coordination
Decreased level of consciousness
Impaired mental status/cognition
Decreased muscle endurance
Decreased strength
D ecreased voluntary movement
Decreased wound healing
Effects of increased muscle tone
Impaired oxygenation
Impaired postural adjustments
Impaired secretion clearance
Impaired sensation
Ineffective cough
Pain with movement
ROM limitations
Skin breakdown
2.
Diagnosis for Physical TheraPY
The physical therapist should be able to make a diagnosis at the end of the
assessment describing the primary dysfunction. This diagnosis differs from a
medical diagnosis in that it is limited to dysfunction which can be identified by
the tests a PT is educated and licensed to perform or request'
You will learn various classifications or diagnoses throughout the curriculum.
Common diagnoses for physical therapy that are used for acute care patients
include
Tissue Impairment Classification Stage I
Movernent Pattern Coordination Defi cit
Force Production Deficit TlPe IA
Perceptual Deficit
86
fType text]
If signs and symptoms are recognized as pertaining to a medical diagnosis, then
the PT needs to refer to the appropriate professional.
3.
The assessment section must include the patient's response to treatment.
4.
Deductions and expectations that support the rehabilitation prognosis
The physical therapist must form an opinion about what the results of the clinical
evaluation reveals and what the expectations are for recovery/remedy of the
patient's problem. This opinion can be written in narrative form. In addition a
rating of the prognosis must be included. Prognosis should be stated at the end of
your assessment on initial and discharge notes. This is a prognosis for functional
recovery, not a medical diagnosis.
This is a staternent of the therapist's professional opinion of the patient's potential
for further improvement. It is a determination of the level of optimal improvement
that might be obtained through intervention and the amount of time required to
reach that level. This statement should be based on objectivs measurements of
status, progfess, time post-onset, motivation, support, age, compliance, and other
complication conditions. Below are definitions for assigning prognosis:
Poor:
Limited potential for improvement.
Guarded:
There exists a question of the potential for improvement secondary
to any of the above questions. This may be the patient you place on
trial therapy. This includes the patient with an undetermined
prognosis.
Fair:
Presents potential to improve in some areas while other
deficit areas may remain imPaired.
Good:
Presents potential to improve to the status of functional
independence. However, the patient may continue to demonstrate
certain minimal limitation.
Excellent: Presents potential to fully recover with no residual deficits.
Because these definitions represent a continuum' you may list prognosis as such;
excellent.
e.g. good
)
87
[T1pe text]
Ilelpful Hints for Writine Patient Goals
Well-written goals should be functional, measurable (using parameters that a P.T. would
evaluate and monitor objectively), and contain an end-point for therapeutic intervention.
There are common methods to writing goals or behavioral objectives. These methods can be
applied when setting personal goals, (which you will do prior to clinical experiences), for any
teaching experience, and when writing goals of patient care.
Essentially, every goal should contain the following generic structure:
Condition
Degree
competency
under what conditions,
measurable end point/
time frame & criteria
for acceptable
performance, e.g. level
Behavior
Subject
patient or other person
measurable
action verb
what person is to do
given what
intervention, given
what information, cues,
etc.
ofindependence
proportion, percent,
grade
Examples:
The patient
ambulate
will
on with a cane
independently for 300
feet by 1211104.
climb
independentlY for I
stairs
with one rail
flight by 9130104.
home
program
perform his
with the home aide with supervision, once
of written instructions daily by 9lIl04'
Examples of measurable behaviors
to demonstrate
to increase
to improve
to achieve
to perform
to identifu
to list
to compare and contrast
to predict
to promote
to interPret
to recall
to apply
to use
to state
to classiff
to dif[erentiate
to construct
to order
to describe
88
[T1pe text]
*** NEVER
use the terms
"maintain" or "preventrr
Short and long term goals are set with/for the patient. They should not be staternents about what
the P.T. plans to do (e.g. complete the evaluation, call the M.D., continue to work on...)
Goals should be directed specifically toward the problem and be functional in nature. Goals do
not have to match the problem one for one. That is, one goal may address more than one
problem, and more than one goal may be needed for one specific problem.
Definitions and Guidelines:
Short-term
goals:
no longer than2 weeks in length; may address impairments or functional
limitations
Long-term
goals:
end point should be discharge from PT altogether; must address functional
limitations
Note:
STG may be reviewed and/or revised throughout course to progress the patient toward
LTG.
Examples:
1)
Problem:
1)
2\
3)
4)
STG: 1)
2)
3)
LTG: l)
2)
2)
mobility (R) shoulder
Pain with active shoulder flexion and abduction
Decreased ROM
Decreased functional
Muscle imbalance
Patient to dernonstrate active shoulder flexion to l20o and abduction to 90o
inby I2lll04
Patient to report decrease in pain from 7/10 to 5/10 by l2lll05
Patient to isolate lower trap mm muscle contraction x3 l2lll05
Patient to report independent functional household activities using (R)
upper extremity, with2ll} pain, upon discharge'
pJient to demonstrate independence with home exercise program x 2
upon discharge.
Problem:
1)
2)
3)
STG:
Patient to demonstrate in 9ll8l05:
1) Transfers WC €t mat with minimal assist'
Dependent mobility transfers/gait
Decreased motor function (L) U/LE
DelaYed Protective reactions
89
[T1pe text]
LTG:
2)
3)
Ambulate with SBQC, (L) AFO and minimal assist 150'x 2.
(L) LE hip flexion 2+15, extension2l5, abduction 2l5,knee extension 3/5.
Patient to dernonstrate by discharge:
1) Independenttransfers.
2) Ambulate 500'with straight cane independently.
3) Ascend/descend 5 steps with railing SBA.
4) Independent with home exercise program.
Critical Features of Phvsical Therapv Notes
The format of physical therapy notes may vary with individual styles and facility requirements,
but notes should alwavs show:
1.
2.
3.
4.
5.
6.
7.
8.
9.
Correct grammar and sPelling
Correct use of medical terminology
Legibility
Clear differentiation of objective and subjective information
Judicious use ofabbreviations and PTjargon
Clear organization of all information; conciseness
Tactfulness
Failure to date and time notes
Documentation of a patient's informed consent to treatment
*** Your
documentation is a reflection of the quality of work you do. Well-written, accurate and
neat records will reflect well on you as a physical therapist, conveying competence, organization
and concern to others. Avoid:
l.
2.
3.
A.
Untimely documentation
Blaming or criticizing another provider in the treatment record
Expressing personal feelings about the patient in the treatment record
The following are common enors found in PT notes: AVOID THEM ALWAYS.
1.
"ROM is WNL for the patient's aqe" Either it is within normal limits according to standards or it is not. This applies
also to strength, function, etc. There are no joint ROM standards available for
different ages at this point in time.
2.
"functional ROM" Again, there are no standards for "functional" ROM. This is an assessment. If
y* ao not measure ROM because it is not indicated then in O: report it as not
measured and in A: indicate why. Or, simply do not address it in O: and in A:
90
[T1pe text]
make a statement that there are no losses of ROM which interfere with function
and why specific measures were not taken.
3.
"The pt. responded to tx. well" -
or
"The pt. tolerated the treatment well" This is vague, non-specific. Better to state: "pt. had no complaints during or
after treatment", or "the pt. improved with treatment" and state how. Use of the
word "tolerate" implies a negative experience. Be more informative. Be exact
in documenting how the treatment affected the patient.
4.
In writing goals - never use the word "maintain" and
avoid use of the word "prevent" -
It is not the purpose of PT to "maintain" the status of the patient. While we do
have a big role in prevention, it is inappropriate to include in the written goals.
Use of either term will jeopardize approval and payment for all services.
(Comment: There are other items or phrases which are commonly seen in P.T. notes which
jeopardize reimbursement, especially by third party payers such as Medicare/Medicaid' These
lerms/phrases change over time somewhat and will be expounded upon in other parts of the
curriculum).
B.
When an e11or is made in your note for any reason, use a single line to cross it out and
initial the error. For examPle:
,ss
The patient has the diagnosis of Mr*kipfe{eieresis Parkinson Disease.
,s5
a walker.
en*+ehes
with
patient
walked
The
Do not obliterate what you have written.
C.
In most places you will be required to use black ink (it Xeroxes best).
D.
Avoid spaaes (lines) in between sections or parts of your note. This can be interpreted
legally is you're leaving space to go back later and change or add information. If filling
out a formatted note, cross through sections not completing.
E.
please sign your notes at the
bottom. It is often customary to add the date the note was
9l
[Type text]
completed and your phone number. As students you do not use the initials RPT or PT. In
some facilities the following are acceptable (follow their guidelines).
or
Smith SPT (student
Smith PT lntern
Smith PT Student
Smith
l0-29-0s 362-3670
Jane
Jane
Jane
Jane
PT)
*must sign legal name
*Remember to have all of your notes co-signed by a licensed PT until you too are
licensed.
F.
Your notes should be organized so that you and other professionals can read or skim
them quickly, and so you can find pertinent sections readily. Make it easy to read-
-
keep it brief, but thorough and informative
make S.O.A.P. sections distinct
avoid cramming information together or spreading it over unnecessary pages.
use outline format for the objective section or use underlined headings to
organize yourself and the reader.
be careful not to use too many abbreviations especially those specific to
physical therapy that physicians may not be as familiar with, i.e. EOB.
document why patient did not receive treatment, i.e. refusals, tests, missed
appoinbnent.
G.
Under Assessment section, do not write just "no change." Be specific.
H.
Exercise special caution when countersigning another provider's evaluation or treabnent
entry.
L
Carefully document a patient's noncompliance with treatnent orders.
J.
Carefully document a patient's or family member/significant other's possible negligence
or abuse.
92
[T1pe text]
The N{echanics of a Business Lefter
Source: Shurter, Robert L: Written Communication in Business, McGraw-Hill Book Company,
Inc., NY, 1957
1.
Arrange and center the letter on the page for symme@ and balanced appearance.
2.
In the salutation and complimentary closing, capitalize only the first letter of the first
word except for proper nttmes and titles.
e.g.
3.
"My dear Mr. Davidson" or "Yours very truly,"
The salutation and the complimentary close should agree in tone.
e.g.
formal
Smith:rr
"Yours very truly,'r
"Very sincerely yours,"
"My dear Mr.
less formal
I'Dear Mr. Smith:"
I'Sincerely yours,"
"Sincerely,"
ttYours truly,"
"Cordially yours" implies acquaintances or long business relationship. "Respectfully
yours" is generally used in letters to those of higher rank or age than the letter writer.
4.
Punctuate the salutation with a colon (:) and complimentary, close with a comma (,).
5.
Signature should be legible.
6.
Be sure to include the date.
7.
To direct the letter to the attention of an individual within the company, add an
"Attention" line two spaces below the inside address; the salutation follows below this.
8.
The signer of the letter has final responsibility for it.
93
[Tlpe text]
Washington University, PT Program, P.T. Initial Note Checklist
Name:
Pass:
Resubmit on:
YES
1.
INCOMPLETE
Introductory information (dx, date, type of refenal and patient's consent to be
examined is present.
2.
3.
Statements of Subiective component are obtained from
patienUfamily.
Statement "The patient has consented to be examined and
evaluated."
Objective section includes
4.
Objective information from chart
5.
Objective information from P.T. Examination
6.
Intervention (treatment) performed
Assessment includes:
7.
interpretation of objective results
8.
a list of the patient's P.T. problems are listed
12.
9.
problems that are specific to physical therapy
10.
11.
a diagnosis for physical therapy
patient response to intervention (treatment)
prognosis for functional recovery
Plan includes:
13.
14.
frequency of tx and length of intervention (treatment)
intervention plan (includes statement about patient's consent to the plan of care)
15.
16.
recommendations and follow-up
all goals are written in measurable terms and include a time
frame
17
short and long term goals are both included and are differentiated
18.
long term goals are functional
19.
The patient has consented to the treatment plan
General characteristics of the note:
20. correct grammar and spelling (more than 3 enors will result in "NO" being
checked).
21.
22.
Correct use of medical terminology'
Legible.
94
NO
[Type text]
YES
23.
Judicious use of abbreviations, P.T. jargon.
24.
Organized, concise.
in Physical Therapy P.T
Washington
Name
NO
INCOMPLETE
Statement of "S" component
Objective section includes
2.
Existing P.T. problems are listed
3.
Objective information from PT's examination is present
4.
Treatment performed is included
Assessment includes:
5.
6.
Patient's response to treatment
7.
Explanation of why patient requires skilled physical therapy
8.
Status of goals: current goals and achieved goals noted
9.
New problems are listed (if needed)
Objective results are interpreted
Plan includes:
10.
Treatment plan
11.
Frequency of treatment and length of treatment
12.
New goals are written in measurable terms
13.
Recommendations,follow-uP
General characteristics of the note:
14.
conect grammar & spelling (more than 3 errors will result in "No" being
checked)
15.
Conect use of medical terminology
16.
Legible
17.
Judicious use of abbreviations
18.
Organized, concise
NO
Progress Note Checklist
YES
1.
INCOMPLETE
95
Washington University Program in PhysicalTherapy P.T.
Name
Discharge Note checklist
Pass:
Resubmit On:
YES
1.
Statements of "S" component
Objective section includes
2.
Problems not previously resolved are listed
3.
Objective information from PT's examination
4.
Treatment performed is included
Assessment includes:
5.
Patient's response to treatment
6.
Objective results are interpreted in regards to patient's progress or lack of
progress
7.
Status of goals
Plan includes:
8.
Why patient has been discharged
L
Discharge recommendations and plan
General characteristics of the note:
10.
Conect grammar and spelling (more than 3 enors will result in "No" being
checked)
11.
Conect use of medical terminology
12.
Legible
13.
Judicious use of abbreviations
'14.
Organized, concise
INCOMPLETE
NO