The New NICE Quality Standard for Intravenous Fluid Therapy in
advertisement

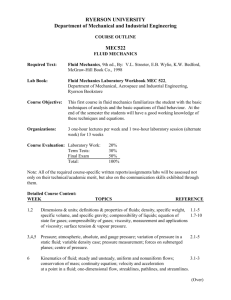
The New NICE Quality Standard for Intravenous Fluid Therapy in adults in hospitals Marlies Ostermann Consultant in Critical Care & Nephrology Content • The New Quality Standard • Implementation of the quality statements in practice • Monitoring and demonstrating competence • IV fluid management plan • Implications for community IV services Background Reasons for iv fluid therapy To resuscitate circulation and ensure organ perfusion To correct hypovolaemia To maintain euvolaemia when patients are “nil by mouth” To replace ongoing losses and oral intake is inadequate To replace essential electrolytes To provide nutrition For drug administration Background: Amount of fluid Critical Care Medicine 2012;40(6) Background: Risks of fluid overload Cerebral oedema Myocardial oedema Pulmonary oedema Fluid overload Hepatic congestion Gut oedema Renal oedema risk of multi-system dysfunction Tissue oedema Prowle J et al. Nat Rev Nephrol 2010;6 Background: Types of fluids Na+ Cl- K+ Ca2+ mmol/L mmol/L mmol/L mmol/L Plasma 140 100 4 0.9% NaCl 154 154 Hartmann’s Solution (CSL) 131 Plasma Lyte HCO3mmol/L pH mosmol/L 2.4 24 7.4 280 - - - 5 308 111 5 2 29 5.0-7.0 278 140 98 5 - 4 – 6.5 294 NaHCO3 1.2% 150 - - - 150 8.17 300 Dextrose 5% (50g/L) - - - - - 3.5–5.5 278 8.4% NaHCO3 1000 0 0 0 1000 14 2000 Gelofusine 154 120 - - - 7.1–7.7 290 as lactate 27 as acetate Osmol Background: Types of fluids 9g NaCl = 36 bags of crisps or 1 bag of saline Background: Fluid charts • often inaccurate • uncertain which patients need a catheter • what does OTT plus wet++ equal? Background Problems with solutions: drowning in the brine of an inadequate knowledge base Telephone questionnaire to determine fluid prescribing practices and knowledge among 200 surgical preregistration house officers (PRHOs) and senior house officers working in 25 UK hospitals. RESULTS • PRHOs were responsible for prescribing in 89% of instances. • 56% stated that fluid charts were checked on morning ward rounds. • <50% knew the Na content of 0.9% NaCl or the daily Na requirement. CONCLUSIONS Inadequate knowledge and suboptimal prescribing of fluid is common. Lobo DN et al. Clin Nutr. 2001;20(2):125-30 NICE guideline 28 recommendations Aims: Guidance on iv fluid therapy for general hospital practice to reduce morbidity and mortality associated with fluid therapy and to improve patient outcomes Exclusion of patient groups with more specialised fluid prescribing needs. NICEStandards: AKI guideline NICE Quality Fluid therapy 1. Hospitals have an IV fluids lead who has overall responsibility for training, clinical governance, audit and review of IV fluid prescribing, and patient outcomes. 2. Adults receiving IV fluid therapy in hospital are cared for by healthcare Guidance from the National Institute for professionals Acute kidneycompetent injury in assessing patients' fluid and electrolyte needs, Health and Care prescribing and administering IV fluids, andExcellence monitoring patient response. NICE pathway and information for the public August 2013 3. Adults receiving IV fluid therapy in hospital have an IV fluid management plan, determined by and reviewed by an expert, which includes the fluid and Anne-Louise Clayton electrolyte prescription over the next 24 hours and arrangements for assessing patients and monitoring their plan. 4. For adults who receive IV fluid therapy in hospital, clear incidents of fluid mismanagement are reported as critical incidents. NICE AKI guideline NICE Quality Standards 1. Hospitals have an IV fluids lead who has overall responsibility for training, clinical governance, audit and review of IV fluid prescribing, and patient outcomes. Rationale • To promote best practice • To ensure that healthcare professionals are trained in prescribing and administering IV fluid • To review learning from 'near miss' and critical incident reporting • To ensure continuity of care in relation to fluid management NICE AKI guideline NICE Quality Standards 1. Hospitals have an IV fluids lead who has overall responsibility for training, clinical governance, audit and review of IV fluid prescribing, and patient outcomes. Role of IV fluids Lead • overall responsibility for the quality of care relating to IV fluid therapy • should be somebody in a senior position • may delegate specific functions through normal governance structure • not expected to be the person who delivers the training, clinical governance, audit and review of IV fluid prescribing NICE AKI guideline NICE Quality Standards 2. Adults receiving IV fluid therapy in hospital are cared for by healthcare professionals competent in assessing patients' fluid and electrolyte needs, prescribing and administering IV fluids, and monitoring patient response. Background: 1. At the end of medical training, new doctors feel unprepared for fluid prescribing. (Coombes et al. 2008) 2. Interns feel unprepared in iv fluid management on commencement of clinical roles. (Kelly et al, 2011) 3. Retrospective review of 250 fluid charts showed large discrepancy in quality. (Chung et al, 2002) NICE AKI guideline NICE Quality Standards Competency Need to establish systems to ensure that all healthcare professionals involved in prescribing and delivering IV fluid therapy are trained and formally assessed and re-assessed at regular intervals to demonstrate competence in: • understanding the physiology of fluid and electrolyte balance in patients with normal physiology and during illness • assessing patients' fluid and electrolyte needs • assessing the risks, benefits and harms of IV fluids • prescribing and administering IV fluids • monitoring the patient response • evaluating and documenting changes and • taking appropriate action as required NICE AKI guideline NICE Quality Standards Competency Need for training and formal assessment at undergraduate level during early medical training during nursing training during specialist training (as directed by specialty) Examples from other areas: Benefits of protocol led care (ie. sepsis bundles) Simulation training to improve knowledge and allow competency assessment NICE e-learning tools NICE AKI guideline NICE Quality Standards Competency needs to be tailored to the professional role Responsible authorities for delivery and competency review: Deans of Medical Schools Training Programme Committees GMC Nursing Council NICE AKI guideline NICE Quality Standards 3. Adults receiving IV fluid therapy in hospital have an IV fluid management plan, determined by and reviewed by an expert, which includes the fluid and electrolyte prescription over the next 24hrs and arrangements for assessing patients and monitoring their plan. IV fluid management plan fluid and electrolyte prescription over the next 24-hour period including type, rate and volume of fluid Assessment evaluation of response to IV fluid therapy specific checks for adverse effects of IV fluid therapy Monitoring of the plan monitoring and review within appropriate timescales initially, daily review by an expert in stable patients on longer-term IV fluid therapy, less frequent reviews NICE AKI guideline NICE Quality Standards 4. For adults who receive IV fluid therapy in hospital, clear incidents of fluid mismanagement are reported as critical incidents. • not all adverse consequences of IV fluid therapy are due to fluid mismanagement • clinically significant problems caused by IV fluid mismanagement should be reported as critical incidents, even when well-managed Adverse events: hypovolaemia pulmonary oedema hyponatraemia (Na <130mmol/L) hypernatraemia (Na ≥155mmol/L) peripheral oedema NICE Quality care standards • central to supporting the Government's vision for a health and social care system focused on delivering the best possible outcomes for people who use services • consider the complete care pathway • set out aspirational but achievable care and are not targets • should be integrated when planning services, as part of a general duty to secure continuous improvement in quality NICE Quality care standards Implementation: • will be challenging • at present limited to hospital based care • will require change of “traditional dogmas” • will only be effective through multidisciplinary approach • likely to cost money (at least in beginning)