Thymosin ??1 activates dendritic cells for antifungal
advertisement

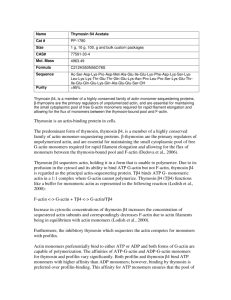
Blood First Edition Paper, prepublished online February 24, 2004; DOI 10.1182/blood-2003-11-4036 Thymosin D 1 activates dendritic cells for antifungal Th1 resistance through Toll-like receptor signaling Luigina Romani1, Francesco Bistoni1, Roberta Gaziano, Silvia Bozza1, Claudia Montagnoli1, Katia Perruccio2, Lucia Pitzurra1, Silvia Bellocchio1, Andrea Velardi2, Guido Rasi3, Paolo di Francesco4 and Enrico Garaci4 From the 1Microbiology Section, Department of Experimental Medicine and Biochemical Sciences, University of Perugia, Perugia, Italy; 2 Division of Hematology, Clinical Immunology, Department of Clinical and Experimental Medicine, University of Perugia, Perugia, Italy; 3Institute of Neurobiology and Molecular Medicine, CNR, Rome, Italy; 4 Microbiology Section, Department of Experimental Medicine and Biochemical Sciences, University Tor Vergata, Rome, Italy. This study was supported by the National Research Project on AIDS, contract n. 50D.27 and the Project n. 1AF/F, both from the ISS, by the Basic Research Funds n.01p4B5-006 and the Project n. 120.5/RF00.121, both from MIUR, Italy. Corresponding author: Luigina Romani, M.D., Ph.D. Department of Experimental Medicine and Biochemical Sciences - Microbiology Section, University of Perugia, Via del Giochetto, 06122 Perugia, Italy Telephone and Fax: 039-075-585-7411 E-mail: lromani@unipg.it Running title: Thymosin and Dendritic Cells in Aspergillosis Word count: 5048 Copyright (c) 2004 American Society of Hematology Abstract Dendritic cells (DCs) show a remarkable functional plasticity in the recognition of Aspergillus fumigatus and orchestrate the antifungal immune resistance in the lungs. Here we show that thymosin α 1, a naturally occurring thymic peptide, induces functional maturation and interleukin-12 production by fungus-pulsed DCs through the p38 mitogen-activated protein kinase/NF-KB-dependent pathway. This occurs by signaling through the myeloid differentiation factor 88-dependent pathway involving distinct Toll-like receptors. In vivo, the synthetic peptide activates T-helper (Th) cell 1-dependent antifungal immunity, accelerates myeloid cell recovery and protects highly susceptible hematopoietic transplanted mice from aspergillosis. By revealing the unexpected activity of an old molecule, our finding provide the rationale for its therapeutic prescriptions and qualify the synthetic peptide as a candidate adjuvant promoting the coordinated activation of the innate and adaptive Th immunity to the fungus. Introduction Invasive aspergillosis (IA), characterized by hyphal invasion, destruction of pulmonary tissue and dissemination to other organs, is the leading cause of both nosocomial pneumonia and death in allogeneic bone marrow transplantation (BMT) with an estimated infection rate of 5 to 10% and an associated mortality rate of 90 to 100%.1-3 The most important risk factor for IA has historically been neutropenia, such that reconstitution with myeloid progenitors offered protection against IA in a murine model of allogeneic BMT.4 However, recent studies on the epidemiology of IA in BMT recipients indicated a reduced neutropenia-related 2 infection and an increase "late-onset" infection, in concomitance with the occurrence of graftversus-host disease.3 These findings, together with the occurrence in non-neutropenic patients,1 attest to the importance of specific defects in both the innate and adaptive immune effector mechanisms in the pathogenesis of the disease.3,5 Clinical and experimental evidence point to the crucial role of a Th1 reactivity in the control of IA.5,6-8 DCs instruct Th1 priming to the fungus in vivo and in vitro.9-11 Evidence indicate that the ability of pulmonary DCs to instruct the appropriate T cell responses to fungal antigens may be affected by local immuno-regulatory events, including signaling through Toll-like receptors (TLRs).10-13 This is consistent with a certain degree of flexibility of the immune recognition pathways to Aspergillus antigens and allergens, such that an allergen could be converted to a potential protective antigen, provided CpG as adjuvant.11 The model has brought DCs to center stage as promising targets for intervention for immunotherapy and vaccine development14 and has shifted the emphasis from the "antigen" towards the "adjuvant".15,16 Thus, the promise of a fungal vaccine will demand for an adjuvant capable of both stimulating the appropriate type of response best tailored to combacting the infection and being effective in conditions of immunosuppression. Thymosin α 1 is a naturally occurring thymic peptide first described and characterized by A. Goldstein.17 In the form of a synthetic 28-amino acid peptide, thymosin α 1 is in clinical trials worldwide for the treatment of some viral infections, either as monotherapy or in combination with interferon α.18,19 Additional indications are some immunodeficiencies20, malignancies21 and HIV/AIDS.18 The mechanism of action of the synthetic polypeptide is not completely understood but is thought to be related to its immuno-modulating activities, centered primarily on the augmentation of T-cell function. Because of its immunomodulatory function on cells on the innate immune system,22 including the ability to activate mitogenactivated protein kinases (MAPKs)23 and gene expression24 on macrophages, we hypothesized 3 that thymosin α 1 could act as an adjuvant capable of activating DCs for Th1 priming to Aspergillus. In this article, we present evidence that thymosin α 1 activates DCs for antifungal Th1 priming in vitro and in vivo by signaling through distinct TLRs and the MyD88 adaptor protein. Materials and methods Animals Female, 8- to 10-weeks old, BALB/c and C57BL6 mice were from Charles River (Calco, Italy). NOD/SCID were from The Jackson. Breeding pairs of homozygous TLR2-, TLR9- and MyD88-deficient mice, raised on C57BL6 background, and of homozygous IFN- - and IL-4deficient mice, raised on BALB/c background, were bred under specific-pathogen free conditions at the breeding facilities of the University of Perugia, Perugia, Italy. Microorganism, culture conditions, infection and treatments The strain of A. fumigatus and the culture conditions were as described elsewhere.7,10 For infection, mice were intranasally injected for 3 consecutive days with a suspension of 2 x 107 conidia/20 µl saline. For the quantification of fungal growth in the lungs, the chitin assay was used as described.7,10 The chitin content was expressed as micrograms of glucosamine per organ. The glucosamine content of lungs from uninfected mice was used as a negative control (range, 0.80 and 2.25 µg glucosamine/organ). For histological analysis, lungs were excised and immediately fixed in formalin. Sections (3 to 4 µm) of paraffin-embedded tissues were stained with the periodic acid-Schiff procedure as described.7 Thymosin α 1 and the scrambled polypeptide (both from SciClone Pharmaceuticals, Inc. San Mateo, California) were supplied as purified (the endotoxin levels were less than 0.03 pg/ml, by a standard limulus lysate assay) sterile lyophilized acetylated polypeptides. The sequences were as 4 follows: Ac-Ser-Asp-Ala-Ala-Val-Asp-Thr-Ser-Ser-Glu-IIe-Thr-Thr-lys-Asp-Leu-Lys-Glu- Lys-Lys-Glu-Val-Glu-Glu-Ala-Glu-Asn-O (Thymosin α 1) and Ac-Ala-Lys-Ser-Asp-ValLys-Ala-Glu-Thr-Ser-Ser-Glu-Ile-Asp-Thr-Thr-Glu-Leu-Asp-Glu-Lys-Val-Glu-Val-Lys-AlaAsn-Glu-OH (sThymosin α 1). The lyophilized powders were reconstituted in sterile water. Treatments were as follows: in BMT-mice, thymosin α 1, at different doses/intraperitoneally, sthymosin α 1, 400 µg/kg/intraperitoneally and human recombinant G-CSF (Granocyte 34; Aventis Pharma S.p.A. Antony Cedex, France), 250 µg/kg/intravenously, were given daily beginning the day of the BM infusion, in concomitance with the infection and continuing for additional 3 days; amphotericin B (A-2942, Sigma) was given daily for 3 days in concomitance with the infection, at the dose of 4000 µg/kg/intraperitoneally. In preliminary experiments, this dose was found to cure IA in cyclophosphamide-treated mice (data not shown). Cyclophosphamide (Sigma), 150 mg/kg/intraperitoneally, was given a day before the infection. In cyclophosphamide-treated mice, 400 µg/kg thymosin α 1 was given intraperitoneally for 5 consecutive days beginning the day of the infection; neutrophil depletion was obtained by treatment with 1 mg of Gr-1-neutralizing RB6-8C5 antibody intravenously, a day before and after the infection. In preliminary experiments, lower amounts of antibodies did not completely ablate the highly represented population of Gr1+F480neutrophils in the lungs of NOD/SCID mice (twice as much that present in wild type mice, i.e., from 7 to 15%) or in the peripheral blood (a mean of 24.8 x 105 cells /ml, that is >70% of white blood cells, the remaining being represented by monocytes (about 27%) and <2% by lymphocytes). The treatment dramatically reduced the number of lung neutrophils (see footnote of Table 1) but not that of DCs (between 5 to 6 x 105 CD11c+, MHC Class II+, F480cells before and after treatment). Control mice received an equivalent amount of purified rat IgG2b (Cat. 02-9288, Zymed Laboratories Inc. South San Francisco, CA). FACS analysis of lung cells a day after treatment with cyclophosphamide revealed a profound and long-lasting 5 (for up to 5 days) leukopenia (from 35% of CD4+ T cells in controls to <5 % in treated mice; from 20 to 4 % of CD8+ T cells; from 19 to 7% of B220+ cells and from 7 to <2% of Gr1+ F480- cells. The percentages of F480+ cells (about 20%) and that of CD11c+, MHC Class II+, F480- DCs (<3%) were unaffected by treatment. TLR ligands Zymosan from Saccharomyces cerevisiae, lipoteichoic acid (LTA) from Staphylococcus aureus, lipopolysaccharide (LPS) from Salmonella minnesota Re 595 and Poly(I:C) were purchased from Sigma. CpG oligonucleotides 1826 and 2006 of proven immunostimulatory sequences were obtained as described.11 Generation of BMT mice C57BL6 mice were exposed to a lethal dose of 9 Gy and infused with T cell-depleted donor cells from BALB/c mice as described.25 More than 95% of the mice survived showing stable, donor type hematopoietic chimerism, as revealed by donor type MHC class I antigen expression on cells from spleens.25 DC isolation and culture Blood CD1c+ myeloid DCs (MDCs) were generated from CD14+ mononuclear cells by magnetic cell sorting (MiniMACs, Miltenyi Biotec S.R.L, Bologna, Italy) and cultured for 5 days in Iscove’s modified medium, containing 10% fetal bovine serum, 50 M 2- mercaptoethanol, sodium pyruvate (1 mM), 2 mM L-glutamine, HEPES (10 mM), and 50 g/ml gentamycin in the presence of 50 ng/ml rHuman GM-CSF (Schering-Plough, Milano, Italy) and 200 U/ml rHuman IL-4 (Peprotech, Inalco, Milano, Italy)26. Immature MDCs were cultured for 24 hours with 1000 ng/ml trimeric human CD40 ligand-leucine-zipper fusion 6 protein (Immunex, Seattle, Washington State) to obtain mature DCs. CD123+ plasmacytoid DCs (PDCs) were isolated using the BDCA-4 isolation kit (Miltenyi Biotec). Purity of CD123+ cells was > 96%. For mature PDCs, immature DCs were cultured with the trimeric human CD40 ligand as above and 10 ng/ml IL-3 (R&D System, Space Import-Export s.r.l. Milano Italy). FACS analysis revealed that PDCs were CD123bright, CD4+, CD45RA+ and CD11c- as opposed to MDCs characterized as being CD1a+, CD11c+, CD11b+, CD4+, CD14low and CD8-. The expression of HLA Class II, CD80 and CD86 was high in both immature and mature DCs. Murine lung CD11c+ DCs (between 5 to 7% positive for CD8α and between 30 to 35% positive for Gr-1) were isolated by magnetic cell sorting.10 For phagocytosis, DCs were pre-exposed to 100 ng/ml thymosin α 1 for 60 minutes and subsequently incubated at 37°C with Aspergillus conidia for additional 60 minutes.10 Percentage of internalization was calculated as described.10 Photographs were taken using a high Resolution Microscopy Colour Camera AxioCam, using the AxioVision Software Rel. 3.1 (Carl Zeiss S.p.A., Milano, Italy). For functional maturation and cytokine determination, purified DCs were resuspended in Iscove's medium (with no serum but with polymixin B, to avoid non-specific activation by serum components and endotoxin) and pulsed with 100 ng/ml thymosin α 1 for 24 hours either alone or together with TLR ligands or unopsonized Aspergillus conidia. Phenotypic analysis Cell surface phenotype was assessed by reacting samples with FITC- or PE-conjugated rat anti-mouse antibodies from PharMingen (San Diego, CA). Unrelated hisotype matched antibodies were used as control. Analysis was performed on a FACScan (Becton Dickinson, Mountain View, CA). 7 Antifungal effector activity For phagocytosis, bronchoalveolar macrophages and peripheral neutrophils were pre-exposed to 100 ng/ml thymosin α 1 for 60 minutes and incubated at 37°C with unopsonized Aspergillus conidia for 60 minutes.10 For the conidiocidal activity, the number of colony forming units and the percentage of colony forming units inhibition (mean ± SE), referred to as conidiocidal activity, were determined as described.10 Assay with HEK293 transfected cells. The human embryonic kidney cell line HEK293, wild type or stably transfected with human TLR2, TLR9 and TLR4/CD1427 were cultured in low glucose Dulbecco’s modified Eagle’s medium supplemented with 10% FCS, HEPES (10nM), L-glutamine (2 µg/ml), gentamycin (50 µg/ml) (Invitrogen S.r.l. Life Technologies, Milano, Italy). Transfectants were additionally supplemented with puromycin (100 µg/ml, Sigma). For stimulation experiments, cells were cultured at a density of 3 to 5 x 105 cells/wells in 12-well tissue culture plates overnight. Cells were washed and stimulated with 100 ng/ml thymosin α 1 either alone or together with TLR ligands for 5 h before the assessment of IL-8 production in the supernatants. Cytokine and spot enzyme-linked immunosorbent (ELISPOT) assay The levels of TNF-α, IL-10, IL-12 p70, IFN-α and IL-8 in culture supernatants were determined by Kit ELISAs (Endogen Human Elisa Kits, S.r.l., R&D Systems and Euroclone, Ltd, Milan, Italy). The detection limits (pg/ml) of the assays were <3 (human) and <32 (murine) for TNF-α, <12 (murine) and <5 (human) for IL-10, <16 (murine) and < 3 (human) for IL-12 p70 and <25 (human) IL-8. For human IFN-α, <3 ng/ml. For enumeration of 8 cytokine-producing cells, an ELISPOT assay was used on purified CD4+ T cells and DCs from lungs, as described.10 Proliferation assay by flow cytometric analysis Proliferation of lung CD4+ T lymphocytes stimulated with 10 µg/ml Con A or heatinactivated conidia in the presence of lung DCs, was assessed by labeling with CFSE 5(6)carboxyfluorescein diacetate succinimidyl ester (Molecular Probes, Eugene, OR), as described.11 Reverse transcriptase (RT)-PCR Total RNA was extracted (TRIZOL Invitrogen) from immature DCs pre-treated with 100 ng/ml thymosin α 1 for 60 minutes followed by the exposure to unosponized Aspergillus conidia for 60 minutes, as suggested by initial experiments. Synthesis and PCR of cDNA were done as described.10 The forward and reverse PCR primers and the cycles used for murine and human TLRs and HPRT were as described.28 The synthesized PCR products were separated by electrophoresis on 2% agarose gel and visualized by ethidium bromide staining. Analysis of p38 and NF-KB activation The activation of p38 and NF-KB on lung DCs exposed for 20 minutes (as suggested by initial experiments) at 37°C to Aspergillus conidia and/or 100 ng/ml thymosin α 1 was done as described.29 Blots of cell lysates were incubated with rabbit polyclonal Abs recognizing either the unphosphorylated form of p38 MAPK, or the double-phosphorylated (Thr-180/Tyr-182) p38 MAPK (Cell Signaling Technology, Celbio S.r.l., Milano, Italy), or Abs specific for the Rel A, 65 kDa DNA binding subunit of human NF-KB (Zymed Laboratories Inc.), followed by horseradisch peroxidase-conjugated goat anti-rabbit IgG (Cell Signaling Technology), as 9 per manufacturer’ instructions. Blots were developed with the Enhanced Chemiluminescence detection kit (Amersham Pharmacia Biothech, Cologno Monzese, Milano, Italy). Bands were visualized after exposure the blots to a Kodak RX film. To ensure similar protein loading in each lane, the phospho blots were stripped and the membranes were reprobed with Abs against p38 and NF-KB. Statistical analysis Survival data were analyzed using the Mann-Whitney U test. Student’s t test was used to determine the significance of values in experimental group (significance was defined as P < 0.05). In vivo groups consisted of 6 animals. Results Thymosin D 1 activates DCs Previous studies have shown that murine DCs phagocytose Aspergillus in vitro and at the site of infection.10 We show here that thymosin α 1, but not the scrambled peptide (sThymosin α 1) activates lung DCs for phagocytosis of unopsonized conidia (more than hyphae), costimulatory antigen expression and cytokine production (Figure 1A). In line with previous findings,10 Aspergillus conidia alone did not represent a sufficient stimulus to induce the activation of DCs, but the combined exposure to thymosin α 1 remarkably increased the expression of MHC Class II antigens, CD86 and CD40 molecules (Figure 1B) and the frequency of IL-12 p70-producing DCs. Interestingly, IL-12 p70-producing DCs were also increased by thymosin alone (Figure 1C). 10 11 The assessment of the actual cytokine production in supernatants of DCs confirmed the higher production of IL-12 p70 along with TNF-α in response to conidia and thymosin α 1 as compared to conidia or thymosin α 1 alone [from 0,75 ± 0,15 (conidia alone) or 1.4 ± 0,37 (thymosin alone) to 2.6 ± 0,51 (in combination) ng/ml of IL-12 p70 and from 147 ± 32 (conidia alone) or 289 ± 60 (thymosin alone) to 681 ± 97 (in combination) pg/ml of TNF-α]. The scrambled peptide failed to up-regulate Class II antigens and costimulatory molecule expression and to induce cytokine production by DCs in response to conidia (data not shown). Thymosin α 1 also activated human MDC and PDC subsets. Both immature and mature DC subsets phagocytose conidia. Thymosin α 1 increased the phagocytic activity of immature DCs, affected the DC morphology, as more cytoplasmic projections were detected in immature MDCs (Figure 2A) and up-regulated the HLA Class II antigens and costimulatory molecule expression in response to conidia (data not shown). In terms of cytokine production, thymosin α 1 significantly increased the release of IL-12 p70 in response to conidia (Fig. 2B) and to zymosan (data not shown) by immature MDCs and that of IL-10 in response to conidia by immature PDCs (Fig. 2B). The production IFN-α , known to be produced by immature PDCs,30 was also assessed and found not to be released by either DC subset in response to conidia and/or thymosin α 1. However, it was produced by PDCs in response to the TLR9 ligand CpG and significantly potentiated by thymosin α 1 (Figure 2B). Together, these data point to a novel, previously undefined, immuno-regulatory role for thymosin α 1 in the activation and functioning of DCs. 12 Thymosin D 1 activates the MyD88-dependent pathway through TLR signaling TLRs signaling occurs in response to Aspergillus and mediates functional responses to the fungus.11-13 Thymosin α 1 strongly activated the expression of TLR2, TLR5, and TLR9 on 13 murine DCs, as opposed to conidia that poorly or none activated TLR expression, with the exception of TLR4. TLR2 and TLR9 were still activated upon the combined exposure to conidia and thymosin α 1, whereas this was not the case for TLR5 whose expression was instead inhibited. Importantly, the scrambled peptide failed to activate TLR2 and TLR9 expression in response to conidia (Figure 3A) or alone (data not shown). The pattern of TLR expression was not different with and without polymixin B (data not shown). Similar to murine DCs, conidia induced the expression of TLR4 on human MDCs and thymosin α 1, alone or together with conidia, induced TLR2 expression on both DC subsets and TLR9 on PDCs (Figure 3B). No TLRs expression was induced upon incubation of cells with the diluent alone (Figures 3A and B). To get further insights into the ability of thymosin α 1 to activate TLR-dependent signaling, HEK293 cells transfected with TLR2, TLR9 and TLR4/CD14 were assessed for IL-8 14 production in response to thymosin α 1 alone or together with the relevant TLR ligands. The results show that thymosin α 1 significantly increased the production of IL-8 by TLR9transfected cells either alone or in response to CpG; it did not stimulate the production of IL-8 by TLR2-transfected cells alone but slightly increased the production in response to zymosan and it did not induce IL-8 by TLR4/CD14-transfected cells either alone or in response to LPS (Fig. 3C). Therefore, thymosin α 1 appears to be able to signal directly through TLR9 and to potentiate TLR2 signaling by the relevant ligand. As NF-KB and p38 MAPK activation are early events in triggering TLR-induced gene expression,31,32 and thymosin α 1 activates MAPK-transduction pathways,23 the nuclear translocation of NF-KB as well as p38 phosphorylation in murine DCs was also assessed. Conidia alone failed to induce NF-KB activation and p38 phosphorylation that were instead induced upon treatment with thymosin α 1, but not with the scrambled peptide, either alone or combined with conidia (Figure 3D). 15 The SN50 (an inhibitor of NF-KB nuclear translocation)33 or SB202190 (an inhibitor of p38 MAPK)34 inhibitors ablated the effect of thymosin α 1 on DCs in terms of IL-12 p70 production [from 1.6 ± 0.62 ng/ml of the control to undetectable levels (<16 pg/ml) in the presence of both inhibitors]. Further studies showed that thymosin α 1 affected the ability of murine DCs to produce IL-12 p70 and IL-10 in response to known microbial TLR ligands.31,32,35 Thymosin α 1 did not affect the cytokine production in response to Poly(I:C) and LPS. However, it significantly increased (at about four folds) the production of IL-12 p70 and decreased that of IL-10 to stimulation with the TLR2 ligands, such as zymosan and LTA. The production of IL12 p70 was also increased to stimulation with the TLR9 ligand CpG, although to a lesser extent (Figure 4A). Among others,31,32 the myeloid differentiation factor 88 (MyD88) is an adaptor protein essential for the activation of NF-KB and MAPK and the production of IL-12 16 p70 upon signaling by TLRs. We found here that the IL-12 p70 production was dramatically ablated in MyD88-deficient mice in response to conidia and/or thymosin α 1. Interestingly, IL-10 production was observed in response to conidia in MyD88-deficient mice but was not modified by thymosin α 1 (Figure 4B). Therefore, it appears that the MyD88-dependent pathway plays an essential role in the ability of thymosin α 1 to modulate IL-12 p70 production by DCs. To assess whether the MyD88-dependent pathway could play an essential role also in vivo, we resorted to an experimental model of IA, in which wild type, TLR2-, TRL9- and MyD88-deficient mice were intranasally infected with Aspergillus conidia, treated with thymosin 1 and assessed for the local fungal growth. The fungal growth in TLR2- and TLR9-deficient mice was comparable to that of wild type mice; it was similarly impaired upon thymosin treatment in wild type, TLR9- and, to a lesser extent, TLR2-deficient mice; however, it was not impaired in MyD88-deficient mice and could not be restored by thymosin α 1 (Figure 4C). Together, these data provide evidence that, despite a degree of redundancy in the TLR usage, the MyD88-dependent signaling pathway is essential in the activity of thymosin 1 in vitro and in vivo. 17 18 Thymosin D 1 protects BMT-mice from IA Based on the above findings, we assess whether treatment with thymosin α 1 would increase antifungal resistance in BMT mice with IA.25 Treatment with thymosin α 1, but not with the scrambled peptide, cured the mice from the infection, as revealed by the increased survival after the infection that paralleled the reduced fungal growth in the lungs. The effect on protection was dose-dependent, full protection (>60 d survival) was achieved in mice treated with 200 and 400 µg/kg thymosin α 1 and was superior to that of amphotericin B. Interestingly, thymosin α 1 appeared to increase the therapeutic efficacy of amphotericin B, as indicated by the increased survival and decreased fungal burden of mice treated with both agents (Figure 5A). Thymosin α 1 also decreased lung pathology. Lung sections from infected mice showed the presence of numerous Aspergillus hyphae infiltrating the lung parenchyma, with severe signs of bronchial wall damage and necrosis and scarce inflammatory cell recruitment (Figure 5B). These features were not observed in thymosintreated mice, whose lungs were characterized by healing infiltrates of inflammatory cells with no evidence of fungal growth and bronchial wall destruction (Figure 5C). These data point to the therapeutic efficacy of thymosin α 1 in IA and suggest the benefit of the association with antifungals known to have a reduced activity in BMT settings.3 19 Thymosin D 1 accelerates myeloid and Th1 cell recovery in mice with IA To evaluate whether thymosin α 1 would activate protective FN-γ-producing Th1 cells in BMT-mice with IA,7,8,10 we assessed cell recovery by FACS analysis together with the antigen-specific lymphoproliferation, pattern of local cytokine production and antifungal activity of effector phagocytes. Although the absolute number of circulating lymphocytes and neutrophils significantly increased after thymosin treatment (data not shown), a cytofluorimetric analysis was performed on lung cells, as blood neutrophil levels do not predict susceptibility to aspergillosis.4 The numbers of CD4+, CD8+ cells and neutrophils were 20 significantly increased in BMT mice upon treatment with thymosin α 1 (Figure 6A). Recovered lung CD4+ T lymphocytes were functionally active as indicated by the antigenspecific proliferation (Figure 6B) and the IFN-γ production. The frequency of IFN-γproducing cells was higher and that producing IL-4 lower in mice treated with thymosin α 1 as compared to untreated mice (Figure 6C). On assessing the level of antifungal activity of effector phagocytes it was found that the conidiocidal activity of both macrophages and neutrophils was higher in thymosin-treated than untreated mice (data not shown). The finding that the phagocytosis and killing of conidia by alveolar macrophages and circulating neutrophils from uninfected mice were also significantly potentiated in vitro in the presence of thymosin α 1 (Figure 6D) suggests that thymosin α 1 not only promotes DC maturation but will also activate local effector cells for prompt phagocytosis and killing of the fungus. 21 However, recovery from neutropenia alone, as by treatment with a dose of G-CSF known to accelerate neutrophil recovery in mice,4 was not sufficient to mediate a degree of antifungal resistance comparable to that obtained with thymosin α 1, as BMT mice were unable to survive the infection (Table 1). Similarly, despite a significant neutrophil recovery and the ablation of resistance upon neutrophil depletion, thymosin α 1 had a limited therapeutic efficacy in mice devoid of T cells or IFN- -producing Th1 cells. In contrast, the optimal therapeutic efficacy of thymosin α 1 was achieved in the presence of an hightened antifungal Th1 reactivity, such as that occurring in IL-4-deficient mice (Table 1). Therefore, although neutrophils play an essential role in mediating antifungal resistance in the absence of an adaptive Th1-dependent immunity, the achievement of a state of full protection to the fungus, 1, appears to rely on the coordinated action as that obtained by treatment with thymosin between innate effector phagocytes and protective Th1 cells. Discussion The results of our study identify a novel immuno-regulatory activity of thymosin α 1 that may have important theoretical and therapeutic implications. Thymosin α 1 promoted the production of IL-12 p70 in DCs through the MyD88-dependent pathway, which is known to lead to production of Th1-promoting cytokines. The production of IL-12 p70 occurred to a different degree between the different DC subsets, a finding in line with the observation that, unlike murine PDCs that produce IL-12 p70 in response to TLR9 stimulation,36 human PDCs are known to produce little IL-12 p70.26 However, human PDCs produced IL-10 more than IL-12 p70 in response to conidia alone or together with thymosin α 1 and produced IFN-α in response to CpG and, more, in response to CpG and thymosin α 1. In TLR-transfected cells, thymosin α 1 directly activated TLR9 but not TLR2 signaling, the last being potentiated in response to the relevant ligand. Preliminary experiments seem to indicate a role for MD2, known to potentiate TLR2 signaling,37 in the TLR2 activating ability of thymosin α 1 (data 22 not shown). It appears, therefore, that thymosin α 1 activates TLR signaling either directly or indirectly. However, whether TLR9 activation occurs in the endoplasmic reticulum of PDCs, as recently reported28 and whether intermediate molecules are licensed by thymosin α 1 in vivo to increase functional expression of TLRs are as yet unsolved issues. In this regard, it is worth mentioning that the 28-residue peptide thymosin α 1 may undergo conformational changes depending upon the environment.38 Whatever the case will be, it is conceivable that thymosin α 1 may exploit the TLR2-dependent pathway on MDCs for IL-12 p70 production and the TLR9-dependent on PDCs for IFN-α production. However, the production of IL-10 by PDCs in response to thymosin α 1 is also of interest. Much evidence indicates that the TLR signaling pathways differ from one other and elicit different biological responses.30,31 Our data would suggest that the production of IL-10 in response to distinct TLR ligands and to conidia mainly occurs in a MyD88-independent manner. Thymosin α 1 did not modify the production of IL-10 in MyD88-deficient mice, a finding confirming the essential role of the MyD88-dependent pathway in the regulation of IL-10 production by thymosin α 1. However, an activity of thymosin α 1 on additional signaling pathways cannot be excluded. Regardless, as IL-10 production by DCs is an essential component of memory protective antifungal immunity, 39 balancing the IL-12/IL-10 production on DCs and/or different DC subsets may represent the very essence of adjuvanticity of thymosin α 1 in aspergillosis. The effects of thymosin α 1 on DCs are consistent with its anti-apoptotic activity40 as well as with its ability to induce prostaglandins41 and to share structural homology with human IFN-α,42 both agents known to induce DCs maturation.15 Given that DCs are central in the balancing act between immunopathology, immunity and autoimmunity,43 and that PDCs signaling through TLR9 are present in the thymus,44 the ability to modulate DC functioning qualifies thymosin α 1 as a novel endogenous regulator of the innate and adaptive immune systems acting through TLR exploitation. From a conceptual point of view, this may provide 23 an explanation for the, as yet elusive, function of naturally occurring thymosin α 1 that is produced in vivo by lysosomal asparaginyl endopeptidase cleavage of prothymosin α in diverse mammalian tissues45 and also the rationale for the therapeutic prescription of thymosin α 1 in some viral infections, where PDCs producing IFN-α, for which TLR9 is essentially required,46 are considered to play a central role.47,48 It is interesting that PDCs also participate in immune responses after hematopoietic cell transplantation,49 a finding that may explain, among others,50 the beneficial effect of thymosin α 1 in the immuno-reconstitution in BMT mice. TLRs activate the innate immune system not only to assist the adaptive immune system but also for direct antimicrobial effector activity.31,32 The fact that thymosin α 1 not only activated murine and human DCs for Th1 priming to A. fumigatus, but also effector neutrophils to an antifungal state, further points to the beneficial effect of thymosin α 1 in fungal infections.22 However, in line with the notion that the recovery from neutropenia is not sufficient to confer protection against IA in BMT mice4 an action on neutrophils alone is not sufficient to mediate the curative effect of thymosin α 1. In conclusion, the unique nature of Aspergillus, a saprophytic fungus colonizing immunocompromised hosts, demands for a better understanding of immunological mechanisms required to both oppose fungal infectivity and optimize the efficacy of antifungal therapy. This study shows that the deliberate targeting of cells and pathways of cell-mediated immunity may increase resistance to Aspergillus and qualifies thymosin α 1 as a promising candidate adjuvant programming the appropriate Th reactivity to the fungus through TLR exploitation. 24 Table 1. Neutrophils and Th1 cells are required for the therapeutic efficacy of thymosin α 1 Group Micea Treatmentb Neutrophils/lung Chitin contentc 3 c (days)c (x 10 ) a MST 1 BMT None 71±8 44±6 4.5 2 BMT G-CSF 544±28* 25±4* 10* 3 BALB/c None 54±4 38±4 5.5 4 BALB/c Thymosin α 1 714±12* 18±2 >60* 5 NOD/SCID None 194±19 68±12 6 6 NOD/SCID Thymosin α 1 491±22* 31±7* 15* 7 NOD/SCID Thymosin α 1 + neutrophil-depletion 69±14 * 59±10 5.5 8 IFN-γ-deficient None 84±10 49±5 7.5 9 IFN-γ-deficient Thymosin α 1 681±44* 25±4* 18* 10 IL-4-deficient None 88±8 32±5 22 11 IL-4-deficient Thymosin α 1 704±51* 0.9±0.3* >60* BMT (groups 1 and 2) or cyclophosphamide-treated (groups 3-11) mice were infected with 2 x 107 Aspergillus conidia intranasally for 3 consecutives days. b In BMT mice, G-CSF (250 µg/kg/i.v.) was given i.v. daily beginning the day of the BM infusion, in concomitance with the infection and continuing for additional 3 days. In cyclophosphamide-treated mice, thymosin α 1 (400 µg/kg/i.p.) was given for 5 consecutive days beginning the day of the infection; neutrophil depletion was obtained by treatment with 1 mg of RB6-8C5 antibody i.v., a day before and after the infection. c Lungs were assessed for the presence of fungal cells (chitin content, expressed as µg glucosamine/lung) and neutrophils (FACS analysis) a day (untreated mice, None) or 3 days (treated mice) after the last Aspergillus inoculation. Values are the mean ± SE. MST, median survival time (days). *P < 0.05, treated vs untreated mice. Each type of intact mice survived the infection and efficiently controlled the fungal growth. 25 Acknowledgments We thank Dr. Lara Bellocchio for superb editorial assistance, Dr. Paolo Mosci for the histology, Drs. Giorgio Trinchieri and Elisabeth Beth from Schering-Plough, Dardilly, France, for providing us with breeding pairs of TLR9-, TLR2- and MyD88-deficient mice, Dr. Manfred Kopf from Swiss Federal Institute of Technology, Zurich, Switzerland, for providing us with breeding pairs of IFN-γ- and IL-4-deficient mice and Dr. Terje Espevik from the Norwegian University of Science and Technology, Trondheim, Norway for the generous supply of transfected HEK cell lines through the courtesy of Prof. Giò Teti (University of Messina, Italy). 26 References 1. Denning DW. Aspergillus. In: Mandel GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. Philadelphia, PA: Saunders; 2000:2674-2682. 2. Marr KA, Carter RA, Boeckh M, Martin P, Corey L. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood. 2002;100:4358-4366. 3. Patterson TF, Kirkpatrick WR, White M, et al. Invasive aspergillosis. Disease spectrum, treatment practices, and outcomes. Medicine. 2000;79:250-260. 4. BitMansour A, Burns SM, Traver D, et al. Myeloid progenitors protect against aspergillosis and Pseudomonas aeruginosa infection following hematopoietic stem cell transplantation. Blood. 2002;100:4660-4667. 5. Hebart H, Bollinger C, Fisch P, et al. Analysis of T-cell responses to Aspergillus fumigatus antigens in healthy individuals and patients with hematological malignancies. Blood. 2002;100:4521-4527. 6. Grazziutti ML, Rex JH, Cowart RE, Anaissie EJ, Ford A, Savary CA. Aspergillus fumigatus conidia induce a Th1-type cytokine response. J. Infect. Dis. 1997;176:1579-1583. 7. Cenci E, Mencacci A, Bacci A, et al. T cell vaccination in mice with invasive pulmonary aspergillosis. J. Immunol. 2000;165:381-388. 8. Garlanda C, Hirsch E, Bozza S, et al. Non-redundant role of the long pentraxin PTX3 in anti-fungal innate immune response. Nature. 2002;420:182-186. 9. Grazziutti M, Przepiorka D, Rex JH, Braunschweig I, Vadhan-Raj S, Savary CA. Dendritic cell-mediated stimulation of the in vitro lymphocyte response to Aspergillus. Bone Marrow Transplant. 2001;27:647-652. 27 10. Bozza S, Gaziano R, Spreca A, et al. Dendritic cells transport conidia and hyphae of Aspergillus fumigatus from the airways to the draining lymph nodes and initiate disparate Th responses to the fungus. J. Immunol. 2002;168:1362-1371. 11. Bozza S, Gaziano R, Lipford GB, et al. Vaccination of mice against invasive aspergillosis with recombinant Aspergillus proteins and CpG oligodeoxynucleotides as adjuvants. Microbes Infect. 2002;4:1281-1290. 12. Wang JE, Warris A, Ellingsen EA, et al. Involvement of CD14 and toll-like receptors in activation of human monocytes by Aspergillus fumigatus hyphae. Infect. Immun. 2001;69:2402-2406. 13. Mambula SS., Sau K, Henneke P, Golenbock DT, Levitz SM. Toll-like receptor (TLR) signaling in response to Aspergillus fumigatus. J. Biol. Chem. 2002;277:39320-39326. 14. Steinman RM, Pope M. Exploiting dendritic cells to improve vaccine efficacy. J. Clin. Invest. 2002;109:1519-1526. 15. Gallucci S, Lolkema M, Matzinger P. Natural adjuvants: endogenous activators of dendritic cells. Nature Med. 1999;5:1249-1255. 16. Ibrahim MA, Gotch FM. Making smarter immunotherapies. Nat. Immunol. 2000;1:3. 17. Goldstein AL, Guha A, Zatz MM, Hardy MA, White A. Purification and biological activity of thymosin, a hormone of the thymus gland. Proc. Natl. Acad. Sci. USA. 1972;69:1800-1803. 18. Billich A. Thymosin alpha1, SciClone Pharmaceuticals. Curr. Opin. Investig. Drugs. 2002;3:698-707. 19. Rasi G, DiVirgilio D, Mutchnick MG, et al. Combination thymosin alpha 1 and lymphoblastoid interferon treatment in chronic hepatitis C. Gut. 1996;39:679-683. 28 20. Wara DW, Goldstein AL, Doyle NE, Amman AJ. Thymosin activity in patients with cellular immunodeficiency. N. Engl. J. Med. 1975;292:70-74. 21. Garaci E, Pica F, Rasi G, Favalli C. Thymosin alpha 1 in the treatment of cancer: from basic research to clinical application. Int. J. Immunopharmacol. 2000;22:1067-1076. 22. Bistoni F, Marconi P, Frati L, Bonmassar E, Garaci E. Increase of mouse resistance to Candida albicans infection by thymosin α1. Infect. Immun. 1982;36:609-614. 23. Sodhi A, Paul S. Involvement of mitogen-activated protein kinases in the signal transduction pathway of bone marrow-derived macrophage activation in response to in vitro treatment with thymosin alpha 1. Int. Immunopharmacol. 2002;2:47-58. 24. Giuliani C, Napolitano G, Mastino A, et al. Thymosin-alpha1 regulates MHC class I expression in FRTL-5 cells at transcriptional level. Eur. J. Immunol. 2000;30:778-786. 25. Mencacci A, Perruccio K, Bacci A, et al. Defective antifungal T-helper 1 (TH1) immunity in a murine model of allogeneic T-cell-depleted bone marrow transplantation and its restoration by treatment with TH2 cytokine antagonists. Blood. 2001;97:1483-1490. 26. Kadowaki N, Ho S, Antonenko S, et al. Subsets of human dendritic cell precursors express different toll-like receptors and respond to different microbial antigens. J. Exp. Med. 2001;194:863-869. 27. Latz E, Schoenemeyer A, Visintin A, et al. TLR9 signals after translocating from ER to CpG DNA in the lysosome. Nat. Med. 2004;doi10.1038/ni1028. 28. Sweet MJ, Campbell CC, Sester DP, Xu D, McDonald RC, Stacey KJ, Hume DA, Liew FY. Colony-stimulating factor-1 suppresses responses to CpG DNA and 29 expression of toll-like receptor 9 but enhances responses to lipopolysaccharide in murine macrophages. J. Immunol. 2002;168:392-399. 29. Chen CH., Zhang DH, La Porte JM, Ray A. Cyclic AMP activates p38 mitogenactivated protein kinase in Th2 cells: phosphorylation of GATA-3 and stimulation of Th2 cytokine gene expression. J. Immunol. 2000;165:5597-5605. 30. Siegal FP, Kadowaki N, Shodell M, et al. The nature of the principal type I interferon-producing cells in human blood. Science 1999;284:1835-1837. 31. Akira S, Takeda K, Kaisho T. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat. Immunol. 2001;2:675-680. 32. Schnare M, Barton GM, Holt AC, Takeda K, Akira S, Medzhitov R. Toll-like receptors control activation of adaptive immune responses. Nat. Immunol. 2001;2:947-950. 33. Lin YZ, Yao SY, Veach RA, Torgerson TR, Hawiger J. Inhibition of nuclear translocation of transcription factor NF-kappa B by a synthetic peptide containing a cell membrane-permeable motif and nuclear localization sequence. J. Biol. Chem. 1995;270:14255-14258. 34. Singh RP, Dhawan P, Golden C, Kapoor GS, Metha KD. One-way cross-talk between p38 (MAPK) and p42/44 (MAPK). Inhibition of p38 (MAPK) induces low density lipoprotein receptor expression through activation of the p42/44 (MAPK) cascade. J. Biol. Chem. 1999;270:19593-19600. 35. Edwards AD, Manickasingham SP., Sporri R, et al. Microbial recognition via Tolllike receptor-dependent and -independent pathways determines the cytokine response of murine dendritic cell subsets to CD40 triggering. J. Immunol. 2002;169:3652-3660. 30 36. Gilliet M, Boonstra A, Paturel C, et al. The development of murine plasmacytoid dendritic cell precursors is differentially regulated by FLT3-ligand and granulocyte/macrophage colony-stimulating factor. J. Exp. Med. 2002;195:953958. 37. Dziarski R, Wang Q, Miyake K, Kirshning CJ, Gupta D. MD-2 enables Toll-like receptor 2 (TLR2)-mediated responses to lipopolysaccharide and enhances TLR2mediated responses to Gram-positive and Gram-negative bacteria and their cell wall components. J. Immunol. 2001;166:1938-1944. 38. Grottesi A, Sette M, Palamara AT, Rotilio G, Garaci E, Paci M. The conformation of peptide thymosin α 1 in solution and in membrane-like environment by circular dicroism and NMR spectroscopy. A possible model for its interaction with the lymphocyte membrane. Peptides. 1998;19:1731-1738. 39. Romani L, Bistoni F, Puccetti P. Fungi, dendritic cells and receptors: a host perspective of fungal virulence. Trends Microbiol. 2002;10:508-514. 40. Baumann CA, Badamchian M, Goldstein AL. Thymosin alpha 1 is a time and dose-dependent antagonist of dexamethasone-induced apoptosis of murine thymocytes in vitro. Int. J. Immunopharmacol. 2000;22:1057-1066. 41. Rinaldi Garaci C, Favalli C, Del Gobbo V, Garaci E, Jaffe BM. Is thymosin action mediated by prostaglandin release? Science. 1983;220:1163-1164. 42. Zav’Yalov VP, Zav’Yalova GA. Interferons alpha/beta and their receptors: place in the hierarchy of cytokines. APMIS. 1997;3:161-186. 43. Mellmann I, Steinman RM. Dendritic cells: specialized and regulated antigenprocessing machines. Cell. 2001;106:255-258. 44. Okada T, Lian ZX, Naiki M, Ansari AA, Ikehara S, Gershwin ME. Murine thymic plasmacytoid dendritic cells. Eur. J. Immunol. 2003;33:1012-1019. 31 45. Sarandeses CS, Covelo G, Diaz-Jullien C, Freire M. Prothymosin alpha is processed to thymosin alpha 1 and thymosin alpha 11 by a lysosomal asparaginyl endopeptidase. J. Biol. Chem. 2003;273:13286-13293. 46. Lund J, Sato A, Akira S, Medzhitov R, Iwasaki A. Toll-like receptor 9-mediated recognition of Herpes simplex virus-2 by plasmacytoid dendritic cells. J. Exp. Med. 2003;198:513-520. 47. Cella M, Facchetti F, Lanzavecchia A, Colonna M. Plasmacytoid dendritic cells activated by influenza virus and CD40L drive a potent TH1 polarization. Nat. Immunol. 2000;1:305-310. 48. Dalod M, Salazar-Mather TP, Malmgaard L, et al. Interferon α/β and interleukin 12 responses to viral infections: pathways regulating dendritic cell cytokine expression in vivo. J. Exp. Med. 2002;195:517-528. 49. Rossi M, Arpinati M, Rondelli D, Anasetti C. Plasmacytoid dendritic cells: do they have a role in immune responses after hematopoietic cell transplantation? Hum. Immunol. 2002;63:1194-1200. 50. Knutsen AP, Freeman JJ, Mueller KR, Roodman ST, Bouhasin JD. Thymosinalpha1 stimulates maturation of CD34+ stem cells into CD3+4+ cells in an in vitro thymic epithelia organ coculture model. Int. J. Immunopharmacol. 1999;21:15-26. 32 Figure legends Figure 1. Thymosin D 1 activates murine DCs upon exposure to Aspergillus fumigatus. Murine lung CD11c+ DCs were pre-treated with thymosin α 1 or the scrambled peptide (sThymosin α1) before the exposure to conidia or hyphae for the assessment of (A) phagocytosis (the data are the means ± SE of three independent experiments and expressed as % internalization (numbers within figures). *P < 0.05, thymosin-exposed vs unexposed cells); (B) costimulatory molecule expression by FACS analysis (data from one representative experiment out of three. Black histograms represent cells stained with an irrelevant antibody. The numbers refer to the median fluorescence intensity) and (C) frequency of IL-12 p70producing cells (the values are the mean ± SE per 105 cells of samples from 3-5 experiments, calculated by ELISPOT assay *P < 0.05, exposed vs unexposed (None) or conidia-exposed cells. Figure 2. Thymosin D 1 activates human DCs upon exposure to Aspergillus fumigatus. Immature and mature myeloid (MDCs) and plasmacytoid (PDCs) DCs were obtained from blood mononuclear cells. For phagocytosis (A), see legend to Figure 1. The data are the means ± SE of three independent experiments and expressed as % internalization (numbers within figures). *P < 0.05, thymosin-exposed vs unexposed cells. (B) Cytokines were determined in 24 h-culture supernatants of DCs stimulated (+) or not (-) with thymosin α 1 in the presence of conidia or CpG 2006 (3 µg/ml). Bars indicate the standard errors. *P < 0.05, cytokine production in thymosin-exposed vs unexposed cells. **P < 0.05, thymosin+CpG versus CpG alone. 33 Figure 3. Thymosin D 1 activates TLR-dependent signaling. Murine lung DCs (A) and human DC subsets (B), pretreated with thymosin α 1 or the scrambled peptide (sThymosin α 1), were exposed to Aspergillus conidia and assessed for TLR expression by RT-PCR. cDNA levels were normalized against the HPRT gene. None, cells exposed to the diluent alone. (C) Production of IL-8 by wild type or TLR-transfected HEK293 cells stimulated with thymosin α 1 and/or zymosan (10 µg/ml), CpG 2006 (3 µg/ml ) and LPS (1 mg/ml). *P < 0.05, stimulated versus unstimulated (None) cells. **P < 0.05, CpG or zymosan+thymosin versus each single agent alone. (D) Activation of NF-KB and p38 on murine lung DCs exposed to Aspergillus conidia, thymosin α 1 or the scrambled peptide, either alone or in combination. The assay was done by probing the cell lysates with specific anti-phospho-38 and anti-NF-KB antibodies. Shown are the data from one representative experiment out of three. Figure 4. Thymosin D 1 activates the MyD88-dependent pathway of TLR signaling. (A) Production of IL-12 p70 and IL-10 by murine lung DCs upon exposure to TLR ligands and /or thymosin α 1. Zym (zymosan, 10 µg/ml), LTA (lipoteichoic acid, 1 µg/ml), Poly(I:C) (polyinosine-polycytidylic acid, 10 µg/ml), LPS (lipopolysaccharide, 1 mg/ml) and unmethylated CpG 1826 (CpG, 2 µM). *P < 0.05, cytokine production in the presence (+) or not (-) of thymosin α 1. (B) Production of IL-12 p70 and IL-10 from lung DCs from wild type or MyD88-deficient mice, upon exposure to conidia and/or thymosin α 1. Bars indicate the standard errors. *P < 0.01, cytokine production in MyD88-deficient versus wild type mice. (C) Mice were intranasally infected with Aspergillus conidia and treated with thymosin α 1 for 5 consecutive days, beginning the day of the infection. The fungal growth (chitin content of the lungs) was assessed a day after treatment. Bars indicate the standard errors. *P < 0.05, treated vs untreated mice. **P < 0.05, MyD88-deficient versus wild type mice. 34 Figure 5. Thymosin D 1 protects BMT mice from invasive aspergillosis. BMT mice were intranasally infected with Aspergillus conidia a week after the BM infusion. Thymosin α 1 or the scrambled peptide (group 7) was given intraperitoneally daily beginning the day of the BM infusion, in concomitance with the infection and continuing for additional 3 days. Amphotericin B was given intraperitoneally for 3 days, in concomitance with the infection. (A) MST, median survival times (days), calculated from the beginning of the infection. The numbers refer to died animals over total injected. The fungal growth was assessed at 1 (control) or 4 days after the last conidia inoculation. Bars indicate the standard errors. *P < 0.05, treated vs untreated mice. **P < 0.05, combined treatment versus each single treatment. (B and C) Periodic acid-Schiff-stained sections from lungs of infected BMT mice either untreated (B at 1 day post-infection) or treated with thymosin α 1 (C at 4 days post-infection). Numerous Aspergillus hyphae (arrows) infiltrating the lung parenchyma, with severe signs of bronchial wall damage and necrosis and scarce inflammatory cell recruitment are observed in the lungs of untreated mice, as opposed to what observed in thymosin-treated mice, whose lungs were characterized by healing infiltrates of inflammatory cells with no evidence of bronchial wall damage and fungal growth. Magnification x 400 in both panels. Figure 6. Thymosin D 1 accelerates functional Th1 cell recovery in BMT-mice with IA. BMT mice were infected and treated as in legend to figure 5. (A) The numbers refer to % positive cells in the lungs on FACS analysis. (B) Lung CD4+ T lymphocytes were CFSEstained (M1) and stimulated with Con A (M4) or heat-inactivated Aspergillus (M5) in the presence of lung DCs for 5 days before FACS analysis. M2 and M3, CD4+ T cells without and with DCs alone, respectively. Shown are the results from one representative experiment out of three. The numbers refer to the median fluorescence intensity, MFI. (C) Lung CD4+ T cells producing cytokines were enumerated by ELISPOT assays. *P < 0.05, thymosin-treated 35 vs untreated (none) mice. In A, B and C, the assays were done 4 days after the last conidia inoculation. (D) Bronchoalveolar macrophages and peripheral neutrophils from uninfected mice were pre-exposed to thymosin α 1 and then to conidia before the assessment of the phagocytic and conidiocidal activity. Values are the mean ± SE of samples taken from 3-5 experiments. *P < 0.05, thymosin-exposed vs unexposed (None) cells. 36