1 Chapter 13: The Perineum The perineum is the part of the pelvic
advertisement
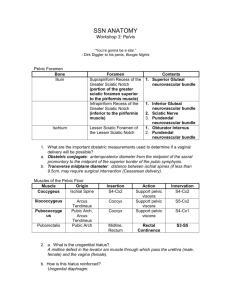
Chapter 13: The Perineum The perineum is the part of the pelvic cavity below the pelvic diaphragm. It is a diamond-shaped space between the pubic symphysis and the coccyx. It is bounded anterolaterally by the ischiopubic rami, laterally by the ischial tuberosities and posterolaterally by the lower borders of the sacrotuberous ligaments. It is divided by a line joining the ischial tuberosities into an anal triangle posteriorly and a urogenital triangle anteriorly. The anal triangle contains the canal in the midline and the ischiorectal fossae laterally. The ischiorectal fossa is a wedge-shaped space, lying with its base inferiorly between the ischium and the anal canal. It is bounded superomedially by levator ani attached to the obturator fascia above, and blending with the external anal sphincter below. Laterally it is bounded by fascia on obturator internus, and inferiorly by perineal skin. Posteriorly it extends between the sacrotuberous and sacrospinous ligaments deep to gluteus maximus; anteriorly it extends between levator ani and the superior fascia of the urogenital diaphragm. The two fossae communicate with each other round the anal canal and are separated by the anococcygeal body, the anal canal and the perineal body. Each fossa contains: (i) a mass of loose fatty tissue; (ii) the internal pudendal vessels and the pudendal nerve which lie in the lateral wall within a sheath, the pudendal canal, formed by a split in the fascia covering obturator internus. The canal lies about 3 cm above the ischial tuberosity. (iii) the inferior rectal nerve and vessels which pass medially across its roof; (iv) scrotal nerves and vessels; (v) perineal branch of the 4th sacral nerve which crosses the fossa and supplies the peri-anal skin and the external sphincter muscle. Infection of the glands of the anal canal may spread through the anal wall into the ischiorectal space to produce large abscesses. Should they discharge externally through the skin, a chronic fistula between the anal canal and the skin may occur (fistula-in-ano) which will demand surgical treatment. The urogenital triangle is divided by the inferior layer (perineal membrane) of the urogenital diaphragm into superficial and deep compartments (pouches). The urogenital diaphragm is a triangular double layer of fascia (stronger in the male than the female) stretching across the pubic arch between its attachments to the ischiopubic rami. It has a free posterior border, the centre of which is attached to a fibrous mass, the perineal body. It is pierced by the urethra, vessels and nerves passing to structures in the superficial perineal pouch and, in the female, by the vagina also. Its inferior layer (perineal membrane) gives attachment to the bulb and crura of the penis or clitoris. The superior (deep) 1 layer is continuous with the pelvic fascia where the viscera pass through between the levatores ani. It fuses posteriorly with the posterior border of the perineal membrane. The superficial and deep perineal pouches differ markedly in the two sexes and are considered separately. The Male Urogenital Triangle The superficial perineal pouch This lies between the membranous layer of the superficial fascia and the inferior layer of the urogenital diaphragm. The superficial fascia is attached posteriorly to the free border of the diaphragm, laterally to the ischiopubic rami and anteriorly it is continuous between the pubic tubercles with the membranous layer of superficial fascia of the anterior abdominal wall. It provides inferiorly a fascial sheath around the penis and scrotum. The pouch contains the root and body of the penis, the superficial perineal muscles, the scrotal vessels and nerves. The testis and spermatic cord lying within the scrotum are in a space continuous with the superficial pouch. Leakage of urine into the superficial perineal pouch spreads firstly into the subfascial tissues of the scrotum and penis and then ascends the anterior abdominal wall deep to the superficial fascia. This may occur in cases of rupture of the spongy urethra after direct trauma or after pelvic fractures. The penis The penis comprises three longitudinal cylinders of erectile tissue, the central corpus spongiosum and the two lateral corpora cavernosa, all covered by fascia and skin. It has a root attaching it to the perineal membrane, and a pendulous cylindrical body. The corpus spongiosum lies inferiorly (ventral) and is expanded to form the bulb of the penis posteriorly and the glans penis anteriorly. The bulb is attached to the perineal membrane and is covered by the bulbospongiosus muscle. The corpus spongiosum is traversed by the urethra which opens at the external urethral orifice on the apex of the glans. The two corpora cavernosa are united dorsally and their anterior extremities are embedded in the glans. Posteriorly, beneath the symphysis pubic they diverge and form the crura of the penis. The crura are covered by the ischiocavernosus muscles. The membranous layer of superficial fascia surrounds the body of the penis and fuses with the corpora just behind the glans. It gives attachment to the short suspensory ligament of the penis which descends from the front of the symphysis pubis. This layer of superficial fascia is devoid of fat, consists of loose areolar tissue and contains superficial vessels and nerves. The skin over the body of the penis is thin and hairless and is prolonged forwards as a fold, the prepuce, over the glans. The glans is covered with thin skin. Ventrally there is a narrow skin fold, the frenulum, between the glans and the prepuce. This contains a small artery which has to be ligated in excision of the prepuce (circumcision). Blood supply By branches of the internal pudendal artery. The artery to the bulb supplies the bulb, corpus spongiosum and the glans; the deep artery of the penis, the corpora cavernosa; and the 2 dorsal artery of the penis, the skin. The veins correspond to the arteries; the corpora drain to the internal pudendal vein and also through the deep dorsal vein of the penis to the prostatic plexus. Lymph drainage To the upper superficial inguinal nodes. Nerve supply The skin is supplied by the dorsal nerve of the penis and the ilio-inguinal nerve. The skin over the glans is very sensitive. Parasympathetic vasodilatator nerves from the pelvic splanchnic supply the erectile tissue. Histology Each of the three corpora is surrounded by a thick fibrous coat (the tunica albuginea) and the two corpora cavernosa are separated by an incomplete fibrous septum. From the tunica and the septum numerous fibro-elastic trabeculae arise, subdividing the cavities of the corpora into blood-filled cavernous spaces lined by flattened endothelium. The tortuous terminal branches of the penile arteries open directly into these spaces. Erection of the penis is caused by an increased blood flow in the penile arteries distending the cavernous tissue coincident with a reduced venous drainage. Embryology The penis forms from a swelling, the genital tubercle, lying cranial to the urogenital opening. The penile urethra develops from a ventral groove on the penis. The scrotum This is a pouch of thin, rugose skin enclosing the two testes and spermatic cords, and separating them is a midline septum. Its walls contain a layer of smooth muscle (the dartos). It develops from the fusion of two lateral scrotal swellings. Superficial muscles of the perineum The superficial muscles lies in the superficial perineal pouch. They are supplied by the perineal branch of the pudendal nerve. (i) Bulbospongiosus - covers the bulb of the penis. The two halves of the muscle arise from the perineal body and from a common midline raphe on the under surface of the bulb. The fibres wind around the penis to be attached to the dorsal surface. (ii) Ischiocavernosus - these two muscles cover the crura of the penis. Posteriorly each is attached to the ischiopubic ramus, anterior to the corpus cavernosum. Bulbospongiosus and ischiocavernosus constrict the corpora, playing a subsidiary role in erection and micturition but a major role in ejaculation. 3 (iii) Superficial transverse perineal muscle is a scarcely definable transverse bundle running along the posterior edge of the perineal membrane. The deep perineal pouch This lies between the superior and the inferior layers of the urogenital diaphragm and below levator ani. It is a closed space, filled mainly by the sphincter urethrae muscle surrounding the membranous urethra. The bulbo-urethral glands and ducts, the internal pudendal vessels and pudendal nerves and their branches, lie in the pouch and leave it by piercing the perineal membrane. The sphincter urethrae muscle This is a broad sheet of striated muscle surrounding the membranous urethra, attached on each side to the ischiopubic ramus. Urinary continence is largely dependent on the action of this muscle which is supplied by the perineal branch of the pudendal nerve. The Female Urogenital Triangle As in the male, the perineal membrane divides the triangle into superficial and deep pouches but these are almost completely divided again by the passage of the vaginal canal. The superficial pouch contains the crura of the clitoris, the bulb of the vestibule, the greater vestibular glands, superficial perineal muscles and the terminal parts of the urethra and vagina. The sphincter urethrae which lies in the deep pouch also gains attachment to the vaginal wall. All these tissues may be temporarily distorted during the passage of the child in parturition. Female external genitalia comprise the mons pubis, a fatty elevation over the symphysis, and two pairs of skin folds, an outer labia majora and an inner labia minora surrounding a median cleft, the vestibule, into which opens the urethra and posteriorly the vagina. Anterior to the urethral opening is the clitoris, a small sensitive mass of erectile tissue attached to the ischiopubic rami. It is homologous with the penis and has a very similar structure, possessing two corpora cavernosa capped by a diminutive glans. A fibrous mass, the perineal body, separates the vagina and anal canal, it is commonly damaged during childbirth. In the superficial pouch and alongside the vagina are the vestibular bulb and the greater vestibular glands. (i) The vestibular bulb comprises two elongated masses of erectile tissue lying on the perineal membrane, one on each side of the vaginal opening. They are united anteriorly by a median commissure and are covered by the bulbospongiosus muscle. (ii) The two greater vestibular glands lie behind the bulb, one on each side of the vaginal opening. 4 The Urethra The male urethra This is an S-shaped tube about 20 cm long extending from the internal (vesical) urethral orifice through the prostate, deep perineal pouch and corpus spongiosum to the external urethral orifice. It is divided into prostatic, membranous and spongy parts. (i) The prostatic urethra is the widest and most dilatable part. It is about 3 cm long and descends through the gland in a slightly forward direction. The upper part of its posterior wall is marked by a fusiform elevation, the urethral crest which makes the urethral cavity C-shaped on transverse section. On the summit of the crest is a small pit, the prostatic utricle, on each side of which open the ejaculatory ducts. Into the groove on the sides of the crest open the 20-30 prostatic ducts. (ii) The membranous urethra is narrow and more rigid. About 1 cm in length, it descends through the deep perineal pouch, about 3 cm behind the symphysis pubis, surrounded by the sphincter urethrae muscle. Two bulbourethral glands lie posteriorly to it embedded in the sphincter muscle. They secrete a lubricant fluid along ducts which pierce the perineal membrane and enter the spongy urethra. (iii) The spongy urethra is about 16 cm long. It traverses the whole length of the corpus spongiosum. Its slit-like lumen is narrowest at the external urethral orifice. It is dilated posteriorly in the bulb forming the intrabulbar fossa and anteriorly in the glans forming the navicular fossa. Blood and nerve supply This comes from the inferior vesical and branches of the internal pudendal artery. Its veins drain to the prostatic venous plexus and the internal pudendal vein. The mucous membrane is supplied mainly by the pudendal nerve. Lymph drainage This is from the prostatic and membranous parts to the internal iliac nodes and from the spongy part to the superficial inguinal nodes. Histology It possesses muscular, submucous and mucous coats. The mucous membrane is very vascular. In the prostatic part it is lined with transitional squamous epithelium. It possesses numerous mucous glands. Embryology The prostatic and membranous parts of the urethra are developed from the urogenital sinus; the spongy part by the fusion of the lips of the urethral groove on the ventral surface of the penis. 5 The female urethra This is about 3 cm long. It descends from the neck of the bladder through the deep perineal pouch where it is surrounded by the sphincter muscle, the superficial pouch and opens into the vestibule. The external urethral orifice lies between clitoris and the vaginal opening. It is similar to the proximal parts of the male urethra in structure and develops from the urogenital sinus. Vessels and Nerves of the Perineum The pudendal nerve The pudendal nerve is a branch of the sacral plexus. It leaves the pelvis through the lower part of the greater sciatic foramen, crosses the ischial spine and enters the perineum through the lesser sciatic foramen. In the perineum it passes forwards within the pudendal canal where it ends by dividing into the perineal nerve and the dorsal nerve of the penis (clitoris). Branches (i) Inferior rectal nerve - arises in the posterior part of the pudendal canal. It passes medially across the roof of the ischiorectal fossa to reach and supply levator ani, the external anal sphincter and the peri-anal skin. (ii) Dorsal nerve of the penis - runs forwards on the medial side of the ischiopubic ramus into the deep perineal pouch and pierces the perineal membrane to gain the dorsum of the penis. It supplies the glans and skin of the penis and carries parasympathetic fibres to the corpora. (iii) Perineal nerve - runs forwards into the superficial pouch. It supplies the perineal muscles and, via its scrotal (labial) branch, the perineal and scrotal (labial) skin. The internal pudendal artery This is a branch of the internal iliac artery. It leaves the pelvis and enters the perineum alongside the pudendal nerve, and its branches to a large extent correspond to those of the nerve. It ends in the deep perineal pouch by dividing into deep and dorsal arteries of the penis (clitoris) and the artery to the bulb. Branches (i) Inferior rectal artery - accompanies the inferior rectal nerve and supplies the lower part of the anal canal. (ii) Scrotal (labial) branches. (iii) Artery to the bulb - arises in the deep perineal pouch. It pierces the perineal membrane supplying the corpus spongiosum. 6 (iv) Deep artery of the penis - supplies the corpus cavernosum. (v) Dorsal artery of the penis - pierces the perineal membrane and passes along the dorsum of the penis supplying the prepuce and glans. Lymph drainage From the perineal skin to the superficial and deep inguinal nodes. Cutaneous nerves Perineal skin is supplied by the perineal branch of the posterior femoral cutaneous nerve and the scrotal (labial) branches of the perineal nerve. Injection of local anaesthetic into the pudendal nerves in the pudendal canals will anaesthetise the skin and deeper tissues of the perineum, and is performed as an aid to obstetric procedures. 7