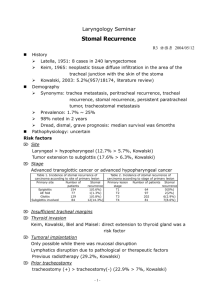
Stomal Complications
advertisement

RING OF FIRE: WALKING THE LINE BETWEEN SUCCESS AND FAILURE IN OSTOMY MATURATION http://www.youtube.com/watch?v=FhE6Izmkpx4 Joyce Pittman PhD, FNP-BC, ANP-BC, CWOCN Indiana University Health Indianapolis, IN Paul Szotek, MD Indiana University Health Indianapolis, IN • Physiologic vs Psychosocial • Physiologic involve changes of the stoma and peristoma skin • Psychosocial involve quality of life or adjustment to having an ostomy • Early vs late • Early= within 30 days following surgery • Late = greater than 30 days following surgery • Stomal vs Peri-stomal • Involving stoma • Involving area around the stoma Prevalence/Incidence: • Several studies report complication rates range from 10- 80% of individuals with an ostomy. • Study design differences, inconsistent definitions and terminology, and timing of measurements make it difficult to accurately measure ostomy complication incidence (Salvadalena, 2008). June 22, 2014 1 Most common physiological complications include: ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ peristomal irritant dermatitis stoma pain stoma mucocutaneous separation stoma necrosis stoma retraction stoma stenosis stoma prolapse herniation around or beside the stoma (J. Colwell, Goldberg, M., Carmel, J., 2001; Park, 1999; C. Ratliff, Scarano, K., Donovan, A., 2005) Stomal Complications Peristomal Complications Mucocutaneous separation (Early) Irritant dermatitis (Early or Late) Stomal necrosis (Early) Candidiasis (Early or Late) Stomal retraction (Early) Folliculitis (Early or Late) Stomal stenosis (Late) Mucosal transplantation (Late) Stomal prolapse (Late) Pseudo verracous lesions (Late) Stomal trauma (Early or Late) Pyoderma gangrenosum (Late) Parastomal hernia (Late) Suture granulomas (Early) Varices (Late) Stomal Necrosis • Death of the stomal tissue resulting from impaired blood flow. (Colwell & Beitz) • Most common early complication • Caused by: – tension on or inadequacy of the mesenteric vasculature to the intestinal end – trauma during creation • Associated with obesity and higher BMI (Colwell & Fichera) • Severity varies- whole stoma, extending below the fascia, or only a portion of the stoma and above skin level. June 22, 2014 2 Stomal necrosis Stomal Necrosis Management • Watch and wait • Superficial - top layer may slough leaving red viable stoma • If above fascia but below skin level- stomal tissue sloughs, malodorous, flaccid. Debridement needed • MC Separation usually occurs • With healing- stomal retraction and stenosis • If stenosis below fascia- and output decreases or stops- surgery likely indicated Mucocutaneous Separation • Detachment of stomal tissue from the surrounding peristomal skin (J. Colwell, Beitz, J., 2007). • Result of poor healing, tension, or infection. • Incidence reported 4% to 24% (Park, Cottom). • Varies in severity: – – – – Partial- only a portion of the stomal circumference Complete- entire circumference is involved. Superficial- only the skin level, Full thickness- extends to the fascia level (Franchini, 1983). June 22, 2014 3 Mucocutaneous separation & retraction MC Separation Management • Depends on severity of separation • The more severe the separation, the more likely retraction will occur. With healing, the likelihood of stenosis is high. • Partial and superficial Separation- may be able to be managed conservatively. Fill defect with skin barrier powder, hydrofiber, or calcium alginate • If separation is severe and involves the fascial layer, stoma may drop into abdominal cavity and return to surgery may be indicated Stomal Retraction • Disappearance of stoma tissue protrusion in line with or below skin level (J. Colwell, Beitz, J., 2007). • Caused by: – – – – – – – Tension on stoma Short mesentery High BMI Inadequate initial stoma length Improper skin excision Stomal necrosis Mc separation June 22, 2014 4 Stomal Retraction Stomal Retraction • Prevalence ranges 4-40% (Ratliff, Pittman, Cottom) • Incidence more than doubled between 1996 and 2004 (22% versus 51%) (Cottom). Management • • • • Goal is to augment the level of stoma above the skin Convex pouching system Belt Surgical revision- local revision or new stoma Stomal Stenosis • Impairment of effluent drainage due to narrowing or contracting of the stoma tissue at the skin or fascial level (J. Colwell, Beitz, J., 2007). • Causes: – – – – – – MC separation Stoma necrosis Stoma retraction Chronic disease Excessive scar formation (dilatation) Chronic inflammation (peristomal irritant dermatitis or hyperplasia June 22, 2014 5 Stomal stenosis Stomal Stenosis The incidence of stomal stenosis has been reported between 2- 23%. Typically, ribbon-like stool or projectile evacuation, frequent UTIs, or flank pain. Management: – Low residue diet, stool softeners, liquids – Dilation? – Surgery Stomal Prolapse Stomal prolapse is the telescoping of the intestine through the stoma (J. Colwell, Beitz, J., 2007). Causes: – Increased abdominal pressure – Obesity – Stomal opening is created too large – Stoma outside of rectus muscle – Double-barrelled loop ostomies June 22, 2014 6 Stomal Prolapse Stomal prolapse – Study of 322 stomas, 156 were end colostomies and 6.8% (Cheung, 1995), developed prolapse. • Management• Conservative management recommended • Pouch needs to accommodate the length of the stoma • Flexible pouching system (avoid rigid systems) to minimize trauma • To reduce prolapse- lie flat, apply gentle pressure, cool compress/ice pack, sugar directly to stoma • Hernia support belt with prolapse strap. Stomal (parastomal) hernia Parastomal (peristomal) hernia is defined as a defect in abdominal fascia that allows the intestine to bulge into the parastomal area (Colwell & Beitz, 2007). Incidence- 30- 50% (Israelsson, 2008) Causes of abdominal hernias: • Natural anatomical openings in abdominal wall- inguinal ring, umbilicus, esophageal hiatus. • Previous surgical entry sites- incisional, stomal site • Increased abdominal pressure- obesity, heavy lifting, coughing with COPD, straining with BM or urination, ascites. • Poor site selection or technical issues- fascial opening too large, stoma in an incision, lateral to rectus(?) June 22, 2014 7 Parastomal Hernia NuHope, 2014 Parastomal Hernia Management: Nonsurgical: – Hernia support belts – Flexible pouching system• 1 pc or • 2 pc with floating flange – Irrigation – hold if difficulties encountered – Regular diet/fluid to ensure soft stool/prevent constipation – Routine follow-up with provider/WOC nurse Parastomal Hernia Management Surgical repair Indications: (depends on degree) – – – – – – – – – Obstruction Incarceration with/without strangulation Prolapse Stenosis Intractable dermatitis Difficulty with appliance management Large size Cosmesis Pain June 22, 2014 8 Walking the Line of Success using Fluorescence Angiography Paul P. Szotek, MD Acute Care & Trauma Surgery Indiana University Health Indianapolis, IN Most common physiological complications include: ◦ Stoma necrosis Anatomical ◦ Stoma MC separation ◦ Stoma retraction ◦ Stoma stenosis ◦ Stoma prolapse ◦ Parastomal Hernia June 22, 2014 Vascular / Blood Flow 9 Clinical Judgment by Visual Inspection & Doppler Calling Dr. Antelope ... we need your primitive “Gold Standards” No problem … I hear it coming but where’s it going? (Doppler) Does not look like a lion hiding in the brush (Looks ok…just a little beat up) My years of judgment will save me…. I’ll get away with it.. or not… Often Fail / insufficient/ unreliable….. Run like #$%! 0hrs Op #1: Surgeon 1 – 25yrs experience + Doppler – Left Colon Resection – “Rest Prob OK” 14hrs Op #2: Surgeon 2 – 23yrs experience + Doppler – Remainder of Colon Resected – “SB Prob OK” 36hrs Op #3: Surgeon 3 – 5 yrs experience Szotek parts ways with IU Health Szotek, Paul P Stoplight Report Service Dates From Aug 1, 2012 to Jul 31, 2013 https://catalyst.nrcpicker.com/iuhcg2012b/iuhealthp/iuhpadult/iuhpsca/providerb/PPSzotek/default.aspx Picker Dimensions Pay for Performance Benchmarks September 25, 2013 Fiscal Year-to-Date Szotek, Paul P Overall NRC 75th Percentile* Current YTD Previous Year Qtr 3 FY2013‡ Qtr 2 FY2013 Using any number from 0 to 10, where 0 is the worst provider possible and 10 is the best provider possible, what number would you use to rate this provider? 88.1% (n=576,428) 100.0%µ PR=100 (n=11) -- 100.0%µ (n=7) 100.0%µ (n=4) -- -- Key Drivers NRC 75th Percentile* Current YTD Previous Year Qtr 3 FY2013‡ Qtr 2 FY2013 Qtr 1 FY2013 Qtr 1 FY2013 Qtr 4 FY2012 Qtr 4 FY2012 In the last 12 months, when you made an appointment for a check-up or routine care with this provider, how often did you get an appointment as soon as you needed? 75.0%µ PR=52 (n=4) 50.0%µ (n=2) -- -- Access to Care 81.4% (n=403,581) -- 100.0%µ (n=2) During your most recent visit, were clerks and receptionists at this provider's office as helpful as you thought they should be? Emotional Support 94.1% (n=574,978) 90.9%µ PR=54 (n=11) -- 100.0%µ (n=7) 75.0%µ (n=4) -- Does this provider involve you in decisions about your care as much as you want? Respect for Patient Preferences 92.7% (n=447,483) 81.8%µ PR=23 (n=11) -- 85.7%µ (n=7) 75.0%µ (n=4) -- -- NRC 75th Percentile* Current YTD Previous Year Qtr 3 FY2013‡ Qtr 2 FY2013 Qtr 1 FY2013 Qtr 4 FY2012 -- 63.6%µ (n=11) -- 71.4%µ (n=7) 50.0%µ (n=4) -- -- -- 50.0%µ (n=10) -- 57.1%µ (n=7) 33.3%µ (n=3) -- -- 72.7%µ (n=11) -- 85.7%µ (n=7) 50.0%µ (n=4) -- -- NRC 75th Percentile* Current YTD Previous Year Qtr 3 FY2013‡ Qtr 2 FY2013 Qtr 1 FY2013 Qtr 4 FY2012 Respect for Patient Preferences 95.7% (n=579,515) 100.0%µ PR=100 (n=11) -- 100.0%µ (n=7) 100.0%µ (n=4) -- -- Would you recommend this provider's office to your family and friends? Would Recommend Provider's Office 94.4% (n=575,064) 100.0%µ PR=100 (n=11) -- 100.0%µ (n=7) 100.0%µ (n=4) -- -- During your most recent visit, did this provider seem to know the important information about your medical history? Coordination of Care 91.4% (n=576,686) 90.9%µ PR=73 (n=11) -- 100.0%µ (n=7) 75.0%µ (n=4) -- -- Focus During your most recent visit, did this provider's staff introduce themselves to you and explain their role in your visit? During your most recent visit, did this provider's staff keep you updated on your wait time while in the waiting area and the exam room? When you last called our office, did this provider's staff demonstrate a courteous and caring attitude over the telephone? Highest Scores During your most recent visit, did this provider spend enough time with you? -- -- Green - score is equal to or greater than the NRC 75th Percentile Yellow - score is less than the NRC 75th Percentile, but may not be significantly µ - Warning: n-size is low! ‡ - Data is not final and subject to change. ©2013 National Research Corporation June 22, 2014 Red - score is significantly less than the NRC 75th Percentile * - Benchmark that is used to determine the color on each line. PR=Percentile Rank Page 1 of 1 10 of intra-operative perfusion assessment as we know it ? • Be Cost-effective • Be easy and efficient to use intra-operatively • Allow for real-time tissue perfusion analysis • Allow for multiple opportunities to assess tissue during procedure • Allow for more informed intraoperative decision making and planning • Be accurate • Be safe for patients The Spy Perfusion System utilizes a fluorescence imaging agent, indocyanine green (ICG), to enable visualization ICG has a 50 year record of safe clinical use First used as a fluorescence imaging agent for ophthalmic angiography Tightly binds with plasma protein in blood1 Stays within the vasculature – does not leak out1 Not nephrotoxic Excreted by the liver into bile1 Half-life of 2.5-3 minutes1 Contraindicated in patients allergic to iodide1 SPY 1. IC-Green™ (indocyanine green for injection, USP) [package insert]. Akorn Inc., Buffalo Grove, IL; November 2008. http://www.akorn.com/documents/catalog/package_inserts/17478-701-02.pdf. Accessed January 5, 2011. 32 Trauma Mesenteric Hematoma /Missed Bowel Injury Observation Vs Laparoscopy June 22, 2014 Acute Care Surgery Ischemic Bowel Consult Observation Vs Laparoscopy 11 Case #3: Embolic Small Bowel Ischemia Where would you resect ? A. White B. Blue C. Black www.autosuture.com Case #1: POD#2 – “Dusky but viable end colostomy” - Morbidy obese – 140kg , DM, CAD - Admitted for Nec Fasciitis of Perineum, Debrided, Floating Rectum - Elective Diverting End Colostomy 4:59 PM EGS Partner 1. Nec Fasciitis 2. Perforated Diverticulitis June 22, 2014 12 Spy uses in this case that Changed Management 1. Objective data to return patient to OR 2. Objective data to determine resection site of colon and possibly prevent identical complication 3. Improve mobilization of colon and identify colon site to make ostomy after pull through 4. Confirm ostomy perfusion after Brooke 5. Identify poorly perfused anterior abd wall blood flow and act on it intraoperatively Case #2: Perforated Diverticulitis s/p Proximal Diverting Loop & “Dusky but Viable Ostomy POD #2 , 140 KG, DM Revision Costs: ~ 20-60k Revision Costs: 40k Revision Rate: 5% Cost to Spy all 91pts = 91k 5/91 pts x 40k = 200k Savings = 108k E Estimated Charges > 1 Million Death Early stoma Vascular Compromise Rates Requiring Revision: 2.3-17% www.health.ny.gov/health.../potentially_preventable_complications.pdf Early Stomal Complications: Kann, Brian. Clin Colon Rectal Surg. 2008 February; 21(1): 23–30. June 22, 2014 13 Dr.inAntelope ICG FA (SPY) Acute Care Surgery No problem … I hear it coming but where’s it going? (Doppler) Does not look like a lion hiding in the brush (Looks ok…just a little beat up) My years of judgment will save me…. I’ll get away with it.. or not… Run like #$%! End organ microvascular perfusion Summary • Anatomical or Vascular or Both • Costly to the healthcare system • Never events….are they nuts? • Fluorescence Angiography may predict ischemia and help prevent early complications at the time of index surgery • “Dusky but viable” Special Thanks Questions ? Dr. Szotek’s Lab Naveed Nosrati, MD June 22, 2014 Lindsey Peters, MD 14 G L A S S IU Health first in Indiana to use Google Glass in surgery To Collaborate: Surgery goes sci-fi as Indiana hospital performs the nation’s first abdominal wall reconstruction using Google Glass google.com/+PaulSzotekMD @glasstestdummie @indyhernia INDIANAPOLIS—A sci-fi way of seeing things offers a new way of performing lifesaving surgery. Recently, physicians at Indiana University Health Methodist Hospital became the first in Indiana to perform a surgery using Google Glass, a wearable mini-computer and camera disguised as a pair of futuristic-style eyeglasses. IU Health Methodist Hospital is the first hospital in the United States to use this technology to both remove a tumor and reconstruct an abdominal wall. pszotek@iuhealth.org References Fitzgibbons, R., Cemaj, S., Quinn, T. 2011. Abdominal Wall Hernias. In Greenfield's Surgery Scientific Principles and Practice, 5th EditionEditors: Mulholland, Michael W.; Lillemoe, Keith D.; Doherty, Gerard M.; Maier, Ronald V.; Simeone, Diane M.; Upchurch, Gilbert R..Lippincott Williams & Wilkins. Cheung, M. T. (1995). Complications of an abdominal stoma: an analysis of 322 stomas. Australian & New Zealand Journal of Surgery, 65(11), 808-811. Colwell, J. (2004). Principles of stoma management. In J. Colwell, Goldberg, M., Carmel, J. (Ed.), Fecal and Urinary Diversions (pp. 240-262). St. Louis: Mosby Colwell, J., Beitz, J. (2007). Survey of wound, ostomy and Continence (WOC) Nurse Clinicians on stomal and peristomal complications: A content validation study. Journal of Wound, Osotmy, Continence Nursing, 34(1), 57-69. Colwell, J., Goldberg, M., Carmel, J. (2001). The state of the standard diversion. Journal of Wound, Ostomy, Continence Nursing, 28, 6-17. Colwell, J. C., & Fichera, A. (2005). Care of the obese patient with an ostomy. Journal of Wound, Ostomy and Continence Nursing, 32(6), 378-385. Colwell, J. C., Goldberg, M., & Carmel, J. (2001). The state of the standard diversion.[see comment]. Journal of Wound, Ostomy, & Continence Nursing, 28(1), 6-17. Cottam, J. (2005). Audit of stoma complications within three weeks of surgery. Gastrointestinal Nursing, 3(1), 19-23. Cottam, J., Richards, K., Hasted, A., Blackman, A. (2007). Results of a nationwide prospective audit of stoma complications within 3 weeks of surgery. The Association of Coloproctology of Great Britian and Ireland. Colorectal Disease, 9, 834-838. Duchesne, J., Wang, Y., Weintraub, S., Boyle, M., Hunt, J. (2002). Stoma Complications: A Multivariate Analysis. American Surgeon, 66(11), 961. Franchini, A., Cola, B., Stevens, P.J. d'E. (1983). Atlas of stomal pathology. New York: Raven Press. Hampton, B. (1992). Peristomal and stomal complications. In B. Hampton, Bryant, R. (Ed.), Ostomies and continent diversions: Nursing management. St. Louis: Mosby Year Book Leong, A., Londono-Schimmer, E., Phillips, R. (1994). Life-table analysis of stomal complications following ileostomy. British Journal of Surgery, 81, 727-729. Park, J., Del Pino, A., Orsay, C., Nelson, R., Pearl, R., Cintron, J., Abcarian, H. (1999). Stoma Complications. Diseases of the Colon & Rectum, 42(12), 1575-1580. Pittman, J. (2011). OSTOMY COMPLICATIONS AND ASSOCIATED RISK FACTORS: DEVELOPMENT AND TESTING OF TWO INSTRUMENTS. [Dissertation PhD]. Indiana University Purdue University Indianapolis Library. Pittman, J., Bakas, T., Ellett, M., Sloan, R., Rawl, S. (2014). Pschometric evaluation of the Ostomy Complication Severity Index. Journal of Wound Ostomy Continence Nurses Society, 41(2), 1-11. Pittman, J., Rawl, S. M., Schmidt, C. M., Grant, M., Ko, C. Y., Wendel, C., & Krouse, R. S. (2008). Demographic and Clinical Factors Related to Ostomy Complications and Quality of Life in Veterans With an Ostomy. Journal of Wound, Ostomy and Continence Nursing, 35 (5), 493-503. Porter, J., Salvati, E., Rubin, R., Eisenstat, T. (1989). Complications of colostomies. Disease Volon & Rectum, 32(4), 299-303. Ratliff, C., Donovan, A. (2001). Frequency of peristomal complications. Ostomy/Wound Management, 47(8), 26-29. Ratliff, C., Scarano, K., Donovan, A. (2005). Descriptive study of peristomal complications. Journal of Wound, Ostomy, Continence Nursing, 32(1), 33-37. Salvadalena, G. (2008). Incidence of complications of the stoma and peristomal skin among individuals with colosty, ileostomy, and urostomy: A systematic review. Journal of Wound, Ostomy, & Continence Nursing, 35(6), 596-607. Steel, M., Wu, J. (2002). Late stomal complications. Clinics in Colon and Rectal Surgery, 15(3), 199- 207. Weideman, Y., Dunn, D., Culleiton, A. (2012). Ostomy Management. Brockton, MA: Western Schools Inc. June 22, 2014 15