Dissection 3, Exposure of Cranial Cavity and Brain
advertisement

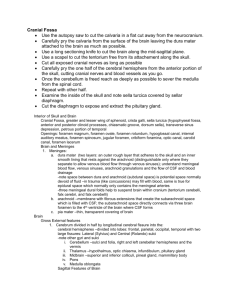
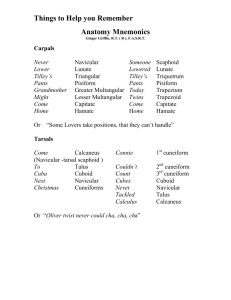
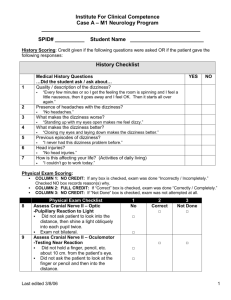
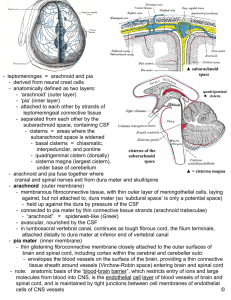
DISSECTION 3 Exposure of the Cranial Cavity and Brain References: M1 822-844, 865-878, 1054-1060, N 4-7, 94-98, 103, 137; N 4-7, 99-104, 109, 144; R 24-27, 34-36, 85-91 AT THE END OF THIS LABORATORY PERIOD YOU WILL BE RESPONSIBLE FOR THE IDENTIFICATION AND DEMONSTRATION OF THE STRUCTURES LISTED BELOW: l. Bones and bony features: frontal, parietal, occipital, temporal, sphenoid, ethmoid; glabella, supraorbital notch, frontal crest, grooves for the middle meningeal artery, groove for the superior sagittal sinus, pits for arachnoid granulations (granular fovea), parietal foramen, foramen magnum, external occipital protuberance, internal occipital protuberance, groove of the transverse sinus, internal occipital crest, occipital condyles, hypoglossal canal, jugular foramen, groove for the inferior petrosal sinus, clivus, internal acoustic meatus, groove for the sigmoid sinus, carotid canal, dorsum sellae, posterior clinoid processes, hypophyseal fossa, tuberculum sellae, anterior clinoid processes, foramen ovale, foramen spinosum, foramen rotundum, superior orbital fissure, optic canal, greater and lesser wings of the sphenoid, cribriform plate of the ethmoid, crista galli, foramen cecum, pericranium, outer table, diploë, inner table. (NOTE: some texts use the terms sulcus instead of groove, fovea instead of pits, lamina instead of table.) coronal suture, sagittal suture, lambdoid suture. 2. Layers of the scalp: Skin, tela subcutanea (Connective tissue), galea Aponeurotica, Loose connective tissue, and the Pericranium. 3. Nerves: trochlear, trigeminal, facial, vestibulocochlear, glossopharyngeal, vagus, spinal accessory, and hypoglossal. (NOTE: you should be able to identify each of these nerves at their origin from the brain and where they penetrate the dura or otherwise leave the cranial cavity.) 4. Meninges: dura mater, falx cerebri, tentorium cerebelli, arachnoid, arachnoid granulations, arachnoid trabeculae, subdural space, subarachnoid space, cisterna magna (cisterna cerebellomedullaris), and pia mater. 5. Vessels: middle meningeal and vertebral arteries, the superior sagittal, straight, and transverse sinuses, the confluence of the sinuses, one or more emissary veins, and one or more cerebral veins. YOU SHOULD ALSO BE ABLE TO DO THE FOLLOWING THINGS: 1. Give a definition of emissary veins. 2. State the differences between the cranial dura and the spinal dura and give the innervation of both types of the dura. 3. State the location of nerves and vessels of the scalp, and explain why scalp wounds bleed so freely. 4. State the locations where the anterior and posterior fontanels would be present in an infant. State the normal time of closure of these fontanels. 5. State the vascular route by which blood flows from the heart to the brain and back to the heart and state which vessels produce hemorrhage in the various intracranial spaces. 6. Draw and label a diagram of an arachnoid granulation and trace the route taken by cerebrospinal fluid from its point of formation to the arachnoid granulation. Dissection 3, Exposure of Cranial Cavity and Brain The Scalp Before beginning the dissection, identify on a skull the bones and bony features listed on page one. Then make a mid-sagittal incision across the top of the skull from the GLABELLA (G7.1, 7.2; N2, N2) to the EXTERNAL OCCIPITAL PROTUBERANCE, cutting all the way to the bone. Reflect a small portion of the SKIN OF THE SCALP away from the TELA SUBCUTANEA, and then, using sharp dissection, separate the tela from the underlying GALEA APONEUROTICA (the aponeurosis of the epicranius muscle). Look for nerves and vessels in the tela subcutanea, and note the ease with which the galea aponeurotica can be separated from the skull. Identify the layer of LOOSE CONNECTIVE TISSUE between the galea and the PERICRANIUM (the periosteum of the outer surface of the skull). Removal of the Calvaria Next strip the scalp away from the skull down to the level of the line shown in the illustration. This is the line at which the skull has its maximum circumference, the so-called line of maximum cranial length. Page 2 skull cap has been completely separated from the rest of the skull, a scalpel handle or forceps may be used to loosen the dura attached to its inner surface. If unusual difficulty is experienced, be sure to ask for help from one of the instructors. Place the body in the prone position and reflect the remnants of the suboccipital muscles from the OCCIPITAL BONE and use the pencil to mark lines from the lateral margins of the FORAMEN MAGNUM to the cut margin of the skull. These lines should intersect the line of maximum cranial length about one inch lateral to each lambdoid suture. Cut through the outer table along these lines with the saw, and then use the mallet and chisel to break through the inner table. Take care not to damage the dura as this is done. The wedge of bone may then be removed by prying it loose from the dura. Examine the surface of the dura near the midline and look for ARACHNOID GRANULATIONS. On the inner surface of the calvaria, identify the GRANULAR FOVEA, small pits produced by the arachnoid granulations (G7.14; N95; N100). Identify examples of EMISSARY VEINS which pass through the parietal foramina identified in the calvaria. As usual, gloves should be worn during dissection; this is imperative whenever the brain is handled. The Meninges and Meningeal Spaces The Dural Venous Sinuses Identify the CORONAL, SAGITTAL, and LAMBDOID SUTURES and look for the PARIETAL FORAMINA (A756, G7.3; N4-7; N4-7). Place a rubber band around the skull along the line of maximum cranial length. Use it as a guide for marking the skull with a pencil. Then saw through the outer table ONLY of the skull along this line. Use a chisel and mallet to gently break through the inner table. Use great care not to damage the underlying dura or brain. When the Incise the SUPERIOR SAGITTAL SINUS and the TRANSVERSE SINUSES and then remove the dura covering them. The junction of the superior sagittal sinus and the transverse sinuses is called the CONFLUENCE OF THE SINUSES. Identify the STRAIGHT SINUS. (A768; G7.27; N97, 98; N103, 104) Into which transverse sinus does it empty? Does the superior sagittal sinus drain predominantly to one side? Taking care not to remove the the transverse sinuses. vertebral canal, the dura ARACHNOID, injure the underlying dura that is inferior to Note that, as in the and arachnoid are not Dissection 3, Exposure of Cranial Cavity and Brain fused but the intervening SUBDURAL SPACE is very narrow, filled in life with only a molecular layer of fluid. Note the thickness of the arachnoid in this region and compare it with the arachnoid in the vertebral canal. Open the arachnoid and note the ARACHNOID TRABECULAE which pass through the SUBARACHNOID SPACE between the arachnoid and the PIA MATER. The large space that you have opened inferior to the cerebellum is called the CISTERNA CEREBELLO–MEDULLARIS or CISTERNA MAGNA, and it is the largest of the intracranial cerebrospinal fluid cisterns. The arachnoid covering the cisterna magna may now be removed. (See G7.66; N103; N109) Identify the MIDDLE MENINGEAL ARTERY (G7.16; N95; N100) in the dura and look in the calvaria to observe the GROOVES in the skull associated with it. Then open the DURA ONLY by incisions parallel to the superior sagittal sinus and the transverse sinuses. Identify the CEREBRAL VEINS deep to the surface of the arachnoid. Observe other cerebral vessels in the subarachnoid space. Through what meningeal spaces do the cerebral veins pass? Where are they most likely to be torn and into what space are they most likely to bleed? Cut through all the veins entering the superior sagittal and transverse sinuses. Then pull the cerebral hemispheres away from the midline and identify the FALX CEREBRI and the TENTORIUM CEREBELLI. (See A767, 777; G7.15A; N97, 98; N103, 104). Page 3 Identification of the Cranial Nerves Cut through the cerebellum in the midsagittal plane and then make a parasagittal cut about 5 mm to the right. Remove the narrow slice of cerebellum and push the two cerebellar hemispheres gently apart to see the brainstem and the floor of the fourth ventricle. Make a second parasagittal cut about one inch from the lateral margin of the cerebellum and remove this lateral segment of the right hemisphere. Then carefully slice away small portions of the remaining tissue until the TROCHLEAR NERVE can be identified (G7.20; N108, 109; N114, 115). CAREFULLY retract the cerebellar hemispheres away from the floor of the posterior cranial fossa and identify the TRIGEMINAL, VESTIBULOCOCHLEAR, GLOSSOPHARYNGEAL, VAGUS, SPINAL ACCESSORY, and HYPOGLOSSAL NERVES. The FACIAL NERVE is usually hidden from view by the vestibulocochlear. DO NOT break these nerves by forcible retraction of the brain. DO NOT cut these nerves, but spend some time studying their attachments to the brainstem, their relationships to the vessels in the area, and the location where they disappear into the dura. Also note the VERTEBRAL ARTERIES as they enter the cranial cavity by passing through the foramen magnum. When you are finished, replace the skullcap and scalp over the cranial cavity to keep the tissues moist. STUDY QUESTIONS ARE ON THE NEXT PAGE Dissection 3, Exposure of Cranial Cavity and Brain Page 4 Study Questions 1. What are the layers of the scalp? 1. Skin, tela subcutanea, galea aponeurotica (epicranius), a layer of loose connective tissue, and the pericranium. 2. Which of these layers make up the movable portion of the scalp? 2. 3. In which layer are the nerves and vessels of the scalp found? 3. The nerves and vessels are in the tela subcutanea. 4. Into which layer then should a local anesthetic be injected? 4. Into the tela subcutanea, where the nerves are. 5. Why are scalp wounds usually very bloody? 5. The arteries of the scalp are numerous and they anastomose freely with each other on the same side and across the midline. In addition, they are tightly embedded in the dense connective tissue of the tela subcutanea, so that they are unable to retract, but remain open when they are cut. 6. What is the "danger space" of the scalp? 6. The layer of loose connective tissue between the epicranius and the pericranium allows easy movement of the outer layers of the scalp. However, it also readily permits the spread of infections or fluids. Since it is traversed by emissary veins which connect the dural venous sinuses with veins in the scalp, abscesses in this layer may result in intracranial infection. Therefore, this layer is called the danger space or danger zone of the scalp. 7. What is the calvaria? 7. The calvaria is the skull cap or roof of the skull. It is formed by the frontal bone, the parietal bones, and part of the occipital bone. Name the bones which form the calvaria. 8. Name the layers which are in direct contact with the bone of the calvaria. The outer three layers -- the skin, the tela subcutanea, and the galea aponeurotica -- are tightly bound together and move as a unit. Some authors (e.g. Hollingshead and Grant) limit their definition of the term scalp to these three layers. 8. The calvaria is covered with periosteum on its inner and outer surfaces. The outer periosteum is called the pericranium, while the inner periosteum forms the outer layer of the dura. Dissection 3, Exposure of Cranial Cavity and Brain 9. The bones of the calvaria have what layers? 9. Page 5 The bones of the calvaria have three layers: The outer table (external lamina), the cancellous diploë, and the inner table (internal lamina). 10. Of these layers, which is the thinnest and most liable to fracture? 10. The inner table is thinner than the outer, and it may be fractured by blows that do not break the outer table. 11. What are the fontanels? 11. The fontanels are membranous spaces between the incompletely developed cranial bones of the fetus and the newborn. These spaces are bridged by the pericranium externally and the dura mater internally. Since most of the bones of the skull are formed either partially or entirely as membrane bones and since ossification is not complete at the time of birth, the bones forming the sides and roof of the skull are still united by membrane. 12. What are the names of the two most easily felt fontanels? 12. The anterior fontanel and the posterior fontanel. 13. Where is the anterior fontanel and when does it close? 13. The anterior fontanel lies at the intersection of the sagittal and coronal sutures, that is, at the common corner of the frontal and parietal bones. It closes during the second year. 14. Where is the posterior fontanel? 14. The posterior fontanel is located at the intersection of the sagittal and lambdoid sutures. When does it close? It closes approximately 2 months after birth. 15. What are the major subdivisions of the floor of the cranial cavity? 15. The floor of the cranial cavity is divided into three large, depressed areas, the anterior, middle, and posterior cranial fossae. 16. What is the boundary between the anterior and middle cranial fossae? 16. The anterior and middle cranial fossae are separated by the sphenoid ridges made up for the most part by the posterior margin of the lesser wing of the sphenoid bone. In the midline, the anterior border of chiasmatic sulcus separates the anterior fossa from the middle fossa. 17. What is the boundary between the middle and posterior cranial fossae? 17. The posterior cranial fossa is separated from the middle cranial fossa by the petrous ridges of the temporal bones and by the dorsum sellae in the midline. Dissection 3, Exposure of Cranial Cavity and Brain 18. Name the cranial fossa in which each of the following openings is found and list the structures passing through each opening. Page 6 18. a. foramen cecum a. anterior cranial fossa – frontal emissary vein b. openings in the cribriform plates of the ethmoid bone b. anterior cranial fossa – filaments of the olfactory nerve c. optic canal c. middle cranial fossa – optic nerve and ophthalmic artery d. superior orbital fissure d. middle cranial fossa –ophthalmic vein, ophthalmic division of the trigeminal nerve, the oculomotor nerve, the trochlear nerve, the abducens nerve e. foramen rotundum e. middle cranial fossa – the maxillary division of the trigeminal nerve f. foramen ovale f. middle cranial fossa – the mandibular division of the trigeminal nerve g. foramen spinosum g. middle cranial fossa – the middle meningeal artery h. foramen lacerum h. middle cranial fossa – nothing of consequence. (It is filled with cartilage in life which forms the floor of the anterior end of the carotid canal.) The greater petrosal nerve passes through the upper part of the foramen lacerum but enters the pterygoid canal before completely traversing the foramen lacerum. i. internal acoustic meatus i. posterior cranial fossa – facial nerve, vestibulocochlear nerve, labyrinthine artery j. jugular foramen j. posterior cranial fossa –glossopharyngeal nerve, vagus nerve, accessory nerve, inferior petrosal sinus, and sigmoid sinus k. hypoglossal canal k. posterior cranial fossa – hypoglossal nerve l. foramen magnum l. posterior cranial fossa – brainstem, vertebral arteries, spinal roots of the accessory nerves, anastomotic connections between the basilar plexus and the internal vertebral venous plexus Dissection 3, Exposure of Cranial Cavity and Brain Page 7 19. What are the meninges and what is their function? 19. The meninges are the three membranes, the dura mater, the arachnoid, and the pia mater, which envelop the central nervous system and separate it from the walls of the bony cavities in which it lies. They function to protect, support, and nourish the central nervous system. 20. How does the cranial dura mater differ from the spinal dura? 20. The cranial dura, instead of being separated from the bone and the periosteum by an extradural (epidural) space, is fused to the periosteum of the inner surface of the skull, so that this periosteum becomes an outer layer of the dura. In addition, the cranial dura contains endothelial lined venous sinuses which are responsible for the return of almost all the blood that enters the cranial cavity. Also, the inner layer of the cranial dura has several duplications or folds which partition the cranial cavity. 21. What are the names of these dural folds? 21. The dural folds are: 1) the falx cerebri, 2) the tentorium cerebelli, 3) the falx cerebelli, and 4) the diaphragma sellae. 22. To what bones is the tentorium cerebelli attached? 22. The outer border of the tentorium is attached on each side to the posterior clinoid process of the sphenoid bone, to the petrous ridge of the temporal bone, and to the transverse ridges of the occipital bone. The inner border of the tentorium attaches to the anterior clinoid process of the sphenoid bone. 23. Name and locate the dural venous sinuses that are closely associated with the tentorium cerebelli. 23. The superior petrosal sinus lies in the outer border of the tentorium where it is attached to the petrous ridge of the temporal bone. The transverse sinus is in the outer border of the tentorium where it attaches to the groove for the transverse sinus on the occipital bone. The straight sinus is along the line of intersection of the tentorium and the falx cerebri. 24. What is the tentorial notch? 24. The tentorial notch or tentorial incisure is the opening bounded by the anterior free border of the tentorium cerebelli and the posterior surface of the dorsum sellae. What part of the brain is partially encircled by the tentorial notch? The upper portion of the midbrain is found within the tentorial notch. Dissection 3, Exposure of Cranial Cavity and Brain Page 8 25. In addition to the midbrain, what other structures pass through the tentorial notch? 25. The posterior cerebral arteries. 26. What is the diaphragma sellae? 26. The diaphragma sellae is a small circular fold of dura with a hole in its center that is attached to the margins of the hypophyseal fossa of the sella turcica. Its inferior surface covers the hypophysis. 27. Severe bleeding from the middle meningeal artery usually results in a collection of blood in what space? 27. In the extradural (epidural) space, a space that is produced by the blood as it strips the dura away from the inner surface of the skull. 28. What is the usual site of bleeding that produces a subdural hematoma? 28. Subdural hematomas are usually the result of bleeding from cerebral veins at their point of entry into the dural venous sinuses. 29. Trace blood from the motor cortex to the heart, naming in order all vessels traversed. 29. Superior cerebral vein draining the precentral gyrus superior sagittal sinus confluence of the sinuses transverse sinus sigmoid sinus internal jugular vein brachiocephalic vein superior vena cava right atrium 30. What is an emissary vein? Give several examples. 30. An emissary vein is a vein which connects a dural venous sinus with veins outside of the cranial cavity. Some of these are connected through the veins of the diploë with the outside, while others pass directly through the skull. The named emissary veins are the frontal emissary vein, parietal emissary veins, mastoid emissary veins, condylar emissary veins, and occipital emissary vein. There are other veins and venous plexuses which are not usually called emissary veins, but which fit the general definition as given above and can serve as important channels by which blood can leave the cranial cavity. The superior ophthalmic vein, which communicates with the cavernous sinus and the facial vein and the anastomoses between the basilar plexus and the internal vertebral venous plexuses fall into this category. 31. How does most of the blood normally get out of the cranial cavity? 31. Through the dural sinuses which drain into the internal jugular vein. Dissection 3, Exposure of Cranial Cavity and Brain Page 9 32. What is a lateral lacuna? 32. A lateral lacuna is an endothelial lined cleft between the two layers of the dura which communicates with or is a lateral extension of one of the dural sinuses, usually the superior sagittal sinus. The arachnoid granulations project into these lacunae. 33. What is an arachnoid granulation? 33. An arachnoid granulation is a structure composed of arachnoid cells which penetrates the dural wall of a venous sinus or lacuna and which is separated from the blood only by the endothelial lining of the sinus or lacuna. They are the principal sites of reabsorption of cerebrospinal fluid into the blood. 34. Draw and label a diagram of an arachnoid granulation. 34. 35. Trace the route of cerebrospinal fluid flow from the point of its formation to its site of reabsorption into the blood. 35. Choroid plexus of lateral ventricle interventricular foramen third ventricle cerebral aqueduct fourth ventricle lateral or median apertures of the fourth ventricle subarachnoid space arachnoid granulation blood. 36. What is a cerebrospinal fluid cistern? 36. A cistern is an enlargement of the subarachnoid space. 37. Name and locate one major cerebrospinal fluid cistern. 37. The cisterna magna (cerebellomedullaris) is located in the angle between the inferior surface of the cerebellum and the posterior surface of the medulla. Dissection 3, Exposure of Cranial Cavity and Brain Page 10 38. Where does the subarachnoid space extend beyond the confines of the cranial cavity? 39. What is the usual source of bleeding into the subarachnoid space? 40. In general terms, where may extravasated blood collect within the cranial cavity? 41. Be able to trace the route of blood flow from any general region of the brain to the heart. 42. How is the cranial dura innervated? Where are the cell bodies of afferent fibers to the tentorium cerebelli? 43. What is the cranium? Of how many bones does it consist? Name them. 44. The great cerebral vein drains into what structure? 45. What other cavities in the skull are in direct relation to the middle cranial fossa and separated from it by thin walls of bone? 46. What is a cephalhematoma? How could a cephalhematoma be distinguished from a hematoma of the scalp? 47. What is the metopic suture? 48. What is the clivus? What parts of the brain are resting on the clivus? LJ:bh revised 06/18/09