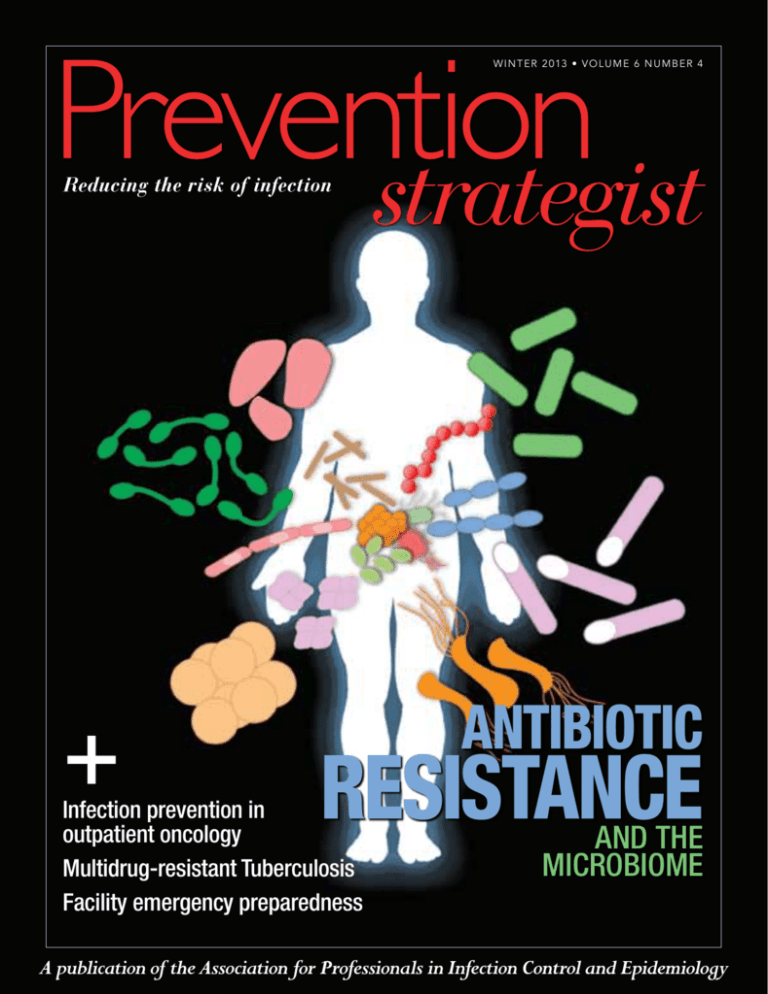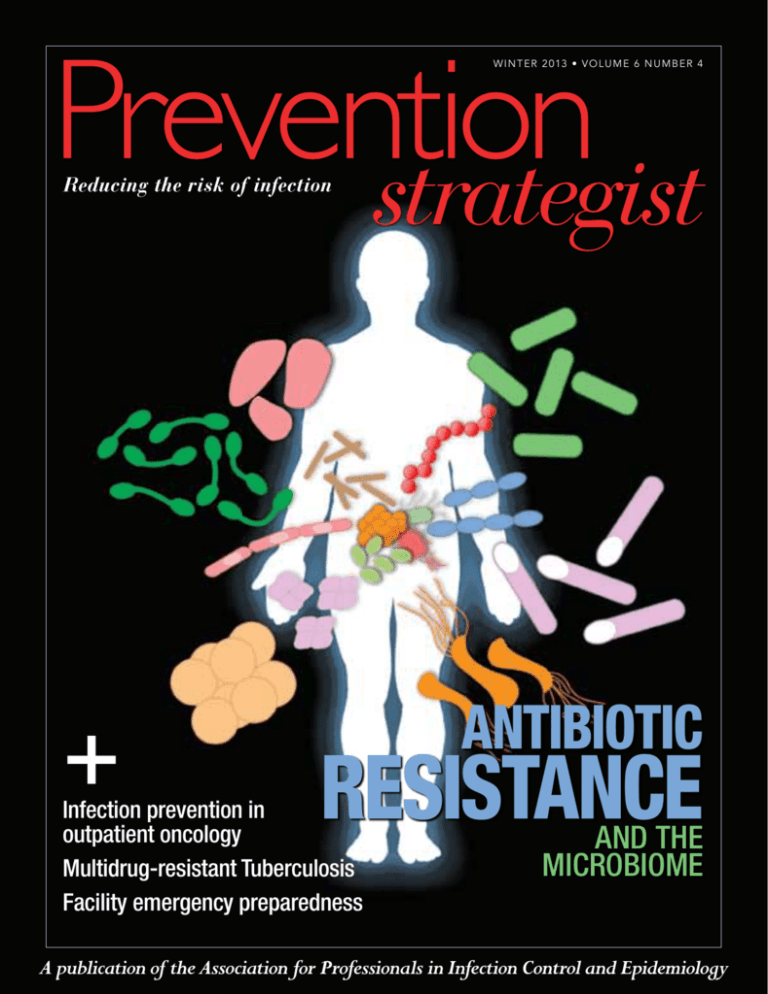
w i n t er 2 013 • VO LU M E 6 N U M B ER 4
+
ANTIBIOTIC
RESISTANCE
Infection prevention in
outpatient oncology
Multidrug-resistant Tuberculosis
Facility emergency preparedness
AND THE
MICROBIOME
This homecoming
moment made possible by
YOU PDI
Getting patients home to their
families is the goal we all share.
That’s why PDI is there for you with educational tools, clinical
support and a complete portfolio of innovative and effective
Infection Prevention solutions–all designed to meet your
environmental hygiene, skin antisepsis and hand hygiene needs.
Because we know that everyone in the chain of Infection Prevention
can Be The Difference™.
For more information, visit PDIBeTheDifference.com
© 2013 PDI. All rights reserved.
Not all UVC devices are created equal
Only the R-D™
Rapid Disinfector™
System solves the 3 most
important UVC issues
SHADOWED AREAS
Patent pending, wireless, remote CHALLENGE DEVICES
(sensors) ensure proper UVC dosing to every point of
interest – including shadowed areas – every time.
TREATMENT TIME
Remote UVC sensors determine when to use the
proprietary “pause and reposition” feature to
significantly reduce disinfection time – disinfect
a standard patient room in as little as 8 minutes1.
UTILIZATION
Real-time, online data reporting automatically
delivers detailed system usage data
and comprehensive information you
need to manage more effectively.
99.96% cleaning efficacy2
Proven to deliver, measure, record and report UVC
dosages needed to kill C.diff at 3.4 log10 or better –
elevating cleaning efficacy to 99.96%. 2
Learn more and schedule a free, live demonstration.
Call 855.UVC.2013 (855.882.2013)
or e-mail sales@steriliz.us.
www.steriliz.us
No Guessing! Measure, Record and Report
1. Data on file. 2. Clostridium Spore Inactivity Study Using Ultraviolet-C Energy. Moog Life Science Laboratories, Moog Medical Devices Group,
7500 West Henrietta Road, Rush, NY 14543, May, 2012. © 2013 Steriliz, Inc. Steriliz is a trademark of Steriliz, LLC.
5x lower observed
nick rate than CareFusion®.*
160 minutes use time.
One blade for all procedures.
Big hairy deal.
The New 3MTM Surgical Clipper Professional 9681
Upgrade to the next generation of surgical clippers.
go.3M.com/clippers
* Study EM-05-012508
© 3M 2013. All rights reserved.
Contents
Features
WINTER 2013
60
A closer look—Antibiotic
resistance and the
microbiome
By Marilyn Hanchett
Infection prevention in
outpatient oncology settings
Spread Knowledge
By Dr. Alice Guh, Dr. Lisa Richardson,
and Angela Dunbar
65
Share Prevention Strategist articles with others.
Check out the icons next to each article to help you navigate Prevention Strategist easily and identify articles to
share with others in your healthcare organization or beyond. Audiences include:
Infection Prevention
Colleagues
6 | WINTER 2013 | Prevention
Patient Care
Services
Environmental
Services
Quality and Risk
Management
Disaster
Preparedness
C-Suite
Let the sharing begin!
VOICE
8
Celebrating APIC’s first 40 years and looking forward The infection preventionist of tomorrow
10
CBIC: Using the building blocks placed by someone before
12
By Patricia Grant, 2013 APIC President
By Katrina Crist, APIC CEO
By Craig Gilliam, 2013 CBIC President
PREVENTION IN ACTION
My Bugaboo: Multidrug-resistant Tuberculosis
29
Ready, set, implement! An innovative nurse-driven Foley
catheter protocol to prevent CAUTI
34
Facility emergency preparedness starts at home
41
Collaboration in infection prevention: Infusion nurses and
infection preventionists
44
Centralized sterile processing in ambulatory facilities 47
Today’s infection prevention challenges in long-term care:
Are we ready to manage them?
53
By Dr. Irena Kenneley
By Brooke Buras
By Steve Hilley
By Mary McGoldrick
By Jody Church and Martha Young
By Vicky Uhland
DEPARTMENTS
CIC Profile: Stephanie Tismer—Years of infection prevention
experience and knowledge, now validated
15
22
29
Briefs to keep you in-the-know
• Infection Prevention and You: APIC’s consumer campaign
makes waves
• Competency Advancement Assistance (CAA) program
recipients announced
Capitol Comments: The National Action Plan to Prevent HAIs
five years later—Measuring progress and mapping out the future
22
Global Insight: Egypt’s Professional Diploma in Infection
Control (PDIC): A success story
24
Heroes of Infection Prevention
71
By Lisa Tomlinson and Nancy Hailpern
By Dr. Ossama Rasslan
16
By Michele Parisi
34
w w w.apic.org | 7
PRESIDENT’S MESSAGE
Celebrating
APIC’s first
40 years
and looking
forward
By Patricia S. Grant,
RN, BSN, MS, CIC
APIC 2013 PRESIDENT
“As infection
preventionists, we
challenge ourselves
to know when to
lead astutely, bravely
follow, and how to
seek and listen to
our multitude of
internal and external
customers.”
Having the honor to serve as APIC’s 2013 president cannot be easily
placed into words. The APIC membership has sanctioned leadership
through exercising the power to vote resulting in an incisive Board of
Directors, supported by the exceptional content expertise of our volunteer committee/chapter systems, and our dedicated/astute professional
headquarters staff. Being true to the definition, purpose, mission, and
expectations of APIC president has been surreal, yet bluntly palpable
at times in a very positive way.
Because APIC can never be about any one individual, to close out
this year’s final Prevention Strategist message, I can think of no better
way than to thank the pioneers of infection prevention who have made
APIC’s existence and survival possible. To enjoy the entire opening 2013
ceremonies for APIC’s 40th Annual Conference in Fort Lauderdale, visit
http://apic.org/About-APIC/History/APIC-Conference-Videos. There you’ll see
the Difference Makers and the Infection Prevention Leaders representing
each decade from the 1970s through 2000s—be sure to follow them
in the order they occurred on June 8, 2013, so you, too, can enjoy the
flow and excitement of what you help make possible through your
infection prevention quest. If you were unable to attend, the wisdom,
retrospective, and earth-shattering revelations shared in each section of
APIC’s opening ceremonies is worth your undivided attention because
it states where we’ve been and where we are clearly going to continue to
improve patient safety. Our APIC history serves us well as a roadmap
for the future while we heed words of wisdom shared by those during
the opening ceremonies.
To celebrate our 40 years together, the first 39 APIC presidents are
listed below to remind each of us that we must continue to lead and
move infection prevention forward within our own daily realities and
within our APIC volunteerism. Each of us can manage our time to realize both. As infection preventionists, we challenge ourselves to know
when to lead astutely, bravely follow, and how to seek and listen to our
multitude of internal and external customers.
As I stated in my opening remarks of the APIC 2013 Annual
Conference, “We are here today because of those who came before us,
their willingness to learn, and their ability to adjust to those experiences. Mostly, we are here because of their perseverance in paying it
forward.” Will You?
Patricia S. Grant, RN, BSN, MS, CIC
APIC 2013 President
1972-73: Patricia Lynch, RN, MBA
1974: Shirley Chewick, RN
1975-76: Carole DeMille, RN
1977: Shirley Bradley
1978: Kathleen DeLuca, RN
1979: Cheryl Cox
1980: Kathy Holl, RN, BSN
1981: Mary Jane Freeburn, RN, CIC
1982: Jean Parret, RN
1983: George Counts, MD
1984: Ronnie Leibowitz, RN, MA, CIC
1985: Robert Sharbaugh, PhD, CIC
1986: Nancy Click, RN, MA, CIC
1987: Lorraine Harkavy, RN, MS, CIC
1988: Elizabeth Bolyard, RN, MPH, CIC
8 | WINTER 2013 | Prevention
1989: Darnell Dingle, MPH, CIC
1990: Elizabeth Horan-Murphy, MT (ASCP), RN, MSN, CIC
1991: Betsy Palmer, RN, MSN, CIC
1992: Vicky Zelenka, RN, CIC
1993: Linda McDonald, RN, MSPH, CIC
1994: Barbara Russell, RN, MPH,
CIC, ACRN
1995: Terrie Lee, RN, MS, MPH, CIC
1996: Ava Lancaster, RN, BSN, CIC
1997: Candace Friedman, BS, MT (ASCP),
MPH, CIC
1998: Frances Slater Feltovich, RN, BSN,
MBA, CIC
1999: Janet Franck, RN, MBA, CIC
2000: Susan Slavish, BSN, MPH, CIC
2001: Judith English, RN, MSN, CIC
2002: Georgia Dash, RN, MS, CIC
2003: Barbara Soule, RN, MPA, CIC
2004: Jeanne Pfeiffer, RN, MPH, CIC
2005: Sue Sebazco, RN, BS, CIC
2006: Kathy Arias, MS, MT, SM, CIC
2007: Denise Murphy, MPH, BSN,
RN, CIC
2008: Janet Frain, RN, CIC, CPHQ, CPHRM
2009: Christine Nutty, RN, MSN, CIC
2010: Cathryn Murphy, RN, PhD, CIC
2011: Russell Olmsted, MPH, CIC
2012: Michelle Farber, RN, CIC
Prevention
W I N T E R 2 013 • VO L U M E 6 , I S S U E 4
Board of Directors
President
Patricia S. Grant, RN, BSN, MS, CIC
President-Elect
Jennie L. Mayfield, BSN, MPH, CIC
Treasurer
Vickie M. Brown, RN, MPH, CIC
Secretary
Linda R. Greene, RN, MPS, CIC
Immediate Past President
Michelle R. Farber, RN, CIC
Directors
Barbara DeBaun, RN, MSN, CIC
Susan A. Dolan, RN, MS, CIC
Donna Giannuzzi, RN, MBA, NEA-BC
Linda K. Goss, MSN, APRN, ANP-BC,
CIC, COHN-S
Carole S. Guinane, RN, MBA
Mary Lou Manning, PhD, CRNP, CIC
Connie Steed, RN, MSN, CIC
Jacie C. Volkman, MPH, CIC, CHEP
Sharon R. Williamson,
MT(ASCP)SM, CIC
Marc-Oliver Wright, MT(ASCP), MS, CIC
EX OFFICIO
Katrina Crist, MBA
Disclaimer
Prevention Strategist is published by
the Association for Professionals in
Infection Control and Epidemiology,
Inc. (“APIC”). All rights reserved.
Reproduction, transmission,
distribution, or copying in whole
or in part of the contents without
express written permission of
APIC is prohibited. For reprint
and other requests, please email
editor@apic.org. APIC makes no
representations about the accuracy,
reliability, completeness, or timeliness
of the material or about the results to
be obtained from using this publication.
You use the material at your own risk.
APIC assumes no responsibility for
any injury and/or damage to persons
or property as a matter of products
liability, negligence or otherwise,
or from any use or operation of any
methods, products, instructions,
or ideas contained in the material
herein. Because of rapid advances in
the medical sciences, in particular,
independent verification of diagnoses
and drug dosages should be made.
Although all advertising material
is expected to conform to ethical
(medical) standards, inclusion in
this publication does not constitute
a guarantee or endorsement of the
quality or value of such product
or of the claims made of it by its
manufacturer.
Daily Patient Bathing
Don’t just cleanse…
HIBICLENS®
HIBICLENS, a 4% chlorhexidine gluconate solution, delivers high levels of protection from
pathogens.1,2 Patient bathing helps stimulate circulation, promotes range of motion, and improves
patient comfort levels.3 SHEA and IDSA recommend routine bathing of patients with antiseptics such
as HIBICLENS to reduce the risk of infections.4
In recovery, patients have bigger battles to win than fighting hospital-acquired infections. By using
HIBICLENS as part of the daily bathing routine, you can deliver the power of 4% CHG with a product
that is gentle enough for everyday use.5
References: 1. Climo MW, et. al. Crit Care Med. 2009 Jun; 37(6):1858-65. 2. Rupp ME. Infect Control Hosp Epidemiol 2012;33(11). 3. Caroline Bunker Rosdahl.
Textbook of Basic Nursing 2007. 4. Calfee, David MD, et. al. Strategies to Prevent Transmission of MRSA in Acute Care Hospitals. Infection Control and Hospital
Epidemiology. October 2008, Vol. 29, Supplement 1, Page S - 73. 5. Data on file. Mölnlycke Health Care. Study R05-0225.
Hibiclens, the Hibiclens logo and Mölnlycke are registered trademarks of Mölnlycke Heath Care AB.
Distributed by Mölnlycke Health Care US, LLC, Norcross, Georgia 30092.
© 2013 Mölnlycke Health Care AB. All rights reserved. 1.800.843.8497.
CEO’S MESSAGE
The infection
preventionist
of tomorrow
By Katrina Crist, MBA
APIC CEO
“To increase your
value as an IP,
the value of the
overall profession,
and to ensure
relevancy in a
newly emerging
healthcare
landscape,
adaptive change
starts with each
and every one
of us at the
individual level.”
“Where you come from is not nearly as important as
where you are going.” — Unknown.
I recently attended the “Hospital of Tomorrow” conference, a leader-
ship forum by U.S. News and World Report where several hundred hospital CEOs came together to discuss the complex business of healthcare
transformation in the United States.
This begs the question, “What does the IP of Tomorrow look like?”
At APIC board meetings, leadership is engaged in strategic thinking on
how to increase the value of infection preventionists (IPs). Throughout
2014, we will be asking the membership to provide information through
surveys and focus groups and participate in ongoing dialogue to develop
and shape strategy for increasing your value within the ever-changing
healthcare landscape.
The forerunner to increasing value is development of leadership skills
and competencies. The IP of Tomorrow will be adept at analyzing data
and making compelling arguments to senior administrators on how to
drive not only technical change, but more importantly adaptive change
that leads to safer care (patient safety), quality care (performance improvement), and more affordable care (sustainable lower cost) all while providing higher levels of customer service (patient satisfaction) and high
reliability.
Adaptive change requires changing long-standing habits and deeply
rooted assumptions. It involves overcoming feelings of loss and sometimes
feelings of betrayal of established values and beliefs. Solutions require
learning new ways of thinking and developing new relationships and
models of collaboration.
To increase your value as an IP, the value of the overall profession, and
to ensure relevancy in a newly emerging healthcare landscape, adaptive
change starts with each and every one of us at the individual level.
APIC looks forward to helping guide you through this journey.
Sincerely yours,
Katrina Crist, MBA
APIC CEO
“The future we predict today is not inevitable. We can
influence it, if we know what we want it to be. We can
and should be in charge of our own destinies in a time
of change.” — Charles Handy, The Age of Unreason.
To learn more, please see the following articles in the American Journal of Infection Control:
• Tensions inherent in the evolving role of the infection preventionists. Laurie J. Conway,
Victoria H. Raveis, Monika Pogorzelska-Maziarz, May Uchida, Patricia W. Stone, Elaine L.
Larson [November 2013 (Vol. 41, Issue 11, Pages 959-964, DOI: 10.1016/j.ajic.2013.04.008)]
• Competency in infection prevention: A conceptual approach to guide current and future
practice. Denise M. Murphy, Marilyn Hanchett, Russell N. Olmsted, Michelle R. Farber,
Terri B. Lee, Janet P. Haas, Stephen A. Streed [May 2012 (Vol. 40, Issue 4, Pages 296-303,
DOI: 10.1016/j.ajic.2012.03.002)]
10 | WINTER 2013 | Prevention
Prevention
winter 2 013 • volume 6 , issue 4
PUBLISHER
Katrina Crist, MBA
kcrist@apic.org
MANAGING EDITOR
Janiene Bohannon
jbohannon@apic.org
ADVERTISING
Brian Agnes
bagnes@naylor.com
GRAPHIC DESIGN
Emma Law
elaw@naylor.com
PRODUCTION
Heather Williams
hwilliams@naylor.com
EDITORIAL COMMITTEE
George Allen, PhD, CIC, CNOR
Megan Crosser, BS, MPH, CIC
Charles Edmiston Jr., PhD, CIC
Mary L. Fornek, RN, BSN, MBA, CIC
Brenda Helms, RN, BSN,
MBA/HCM, CIC
Linda Jamison, MSN, RN, CIC, CCRC
Irena Kenneley, PhD, APRN-BC, CIC
Kari L. Love, RN, BS, MSHS, CIC
Caroline McDaniel, RN, BSN, MSN
May M. Riley, RN, MSN, MPH,
ACNP, CCRN, CIC
Steven J. Schweon, RN, MPH,
MSN, CIC
CONTRIBUTING WRITERS
Janiene Bohannon
Brooke Buras, Rn, Bsn
Jody Church, Rn, Cpnp
Katrina Crist, Mba
Angela Dunbar, Bs
Elizabeth Garman
Craig Gilliam, Bsmt, Cic
Patricia Grant, Rn, Bsn, Ms, Cic
Alice Y. Guh, Md, Mph
Nancy Hailpern
Marilyn Hanchett, Rn, Ma, Cphq, Cic
Steve Hilley, Rn
Irena Kenneley, PhD, Aprn-Bc, Cic
Mary McGoldrick, Ms, Rn, Crni®
Michele Parisi
Ossama Rasslan, Md, PhD
Lisa C. Richardson, Md, Mph
Lisa Tomlinson
Vicky Uhland
Martha Young, Bs, Ms, Cspdt
Mission
APIC’s mission is to create a safer
world through prevention of infection.
The association’s more than 14,000
members direct infection prevention
programs that save lives and improve
the bottom line for hospitals and other
healthcare facilities. APIC advances
its mission through patient safety,
implementation science, competencies
and certification, advocacy, and data
standardization. Visit APIC online at
www.apic.org.
PUBLISHED DECEMBER 2013 •
API-Q0413 • 9090
FATAL ATTRACTION
XSTREAM Infection Control kills C-Diff and other deadly bacteria
that bleach can’t reach.
No matter how much you disinfect, sanitize and sterilize, there are
still going to be those certain infectious microbes that no amount of
conventional cleaning, UVX light, aqueous H202 or coating supplies
can remove. Unfortunately, those bacteria are often the ones that do
the most damage to your people, your patients and your profits.
XSTREAM 2000 is the most powerful, deployable, and cost-effective
technology available to confront the crisis of healthcare-associated
infections. The result is significantly reduced spread of infectious
microbes and cost of patient care.
Most importantly, XSTREAM improves your standard of care.
150 Units available for trial evaluation at no cost to you!
Visit XSTREAMInfectionControl.com
today to learn more
Celebrating Excellence
Using the
building
blocks placed
by someone
before
®
The title of my final column as CBIC president speaks volumes as CBIC’s 30th anniversary
By Craig Gilliam,
BSMT, CIC
2013 CBIC President
“Coming
together is a
beginning,
keeping together
is progress,
and working
together is
success.”
— Henry Ford
12 | WINTER 2013 | Prevention
comes to an end. Pat Lynch, the first CBIC president, said it best in 1985 when she explained
that “the challenge is there; the certification process is critical in attaining success.” I believe
this means the certification process is used to validate practice—not demonstrate knowledge
from an examination. As the 2013 president of CBIC, I have been fortunate that recent CBIC
presidents Terrie Lee, RN, MS, MPH, CIC, and Barbara Russell, RN, MPH, CIC—who
mentored me and prepared our board for future challenges—were visionaries of what we can
accomplish.
In the beginning of 2013, I envisioned three main objectives to help advance our profession. First I wanted infection preventionists (IPs) to recognize and celebrate the anniversary
of certification, promote professionalism within our chapters, and advocate for certification
to IPs and epidemiologists beyond our borders. I suggest you look around in your chapter and
at national educational meetings to observe the number of the early advocates of certification from the 1980s and 1990s who are still involved and mentoring newer IPs. In October, I
attended the 13th meeting of International Federation of Infection Control (IFIC) in Buenos
Aires, Argentina. At the meeting, Patti Grant, RN, BSN, MS, CIC, 2013 APIC president,
Bruce Gamage, RN, BSN, CIC, 2013 CHICA-Canada president, and I all spoke at sessions
on professionalism and certification. Not only did attendees discuss similar solutions and challenges as North American IPs, they also expressed their desire to demonstrate and communicate
that healthcare facilities with trained certified professionals will have better patient outcomes.
Second, I think it imperative for CBIC and APIC to continue to work together to demonstrate value to its members. APIC is showing IPs a path to improve their competency—and
certification is integral to this advancement. CBIC appreciates the strong verbal support at
national education forums from recent APIC leaders and presidents on the importance and
necessity of IPs becoming certified. The number of new certificants continues to increase and
Self Achievement Certification Exam (SARE) numbers are 10 percent higher than the predicted
numbers for 2013. The SARE recertification pass rate is 95 percent; I think this reflects the
preparation IPs put forth. The CBIC website also tracks the number of current certificants;
we are approaching the 6,000 mark at year’s end.
Third, adding the personal touch makes a difference. People notice and appreciate when IPs
who attain or maintain certification are recognized. Every month when the new certificant
list is released, I write a personal note to a random selection of successful individuals. I truly
believe this is recognition of the importance of professionalism we strive to achieve. Your
efforts are an example for others to follow in making patients safer in all healthcare settings.
If I and others are successful in demonstrating the value of professional certification, we
will remember the process started with those who have a vision!
As Henry Ford once said: “Coming together is a beginning, keeping together is progress,
and working together is success.”
Worldwide Pandemics, Emerging Pathogens, Rising HAI Rates, Increased Pathogen Resistance?
Looks like a job for Accel!
Accel is the first line of defense against emerging pathogens. Accel products are effective against NOROVIRUS, MRSA, VRE,
Pseudomonas, Staphylococcus, Salmonella and other difficult to kill pathogens.
Accel is powered by the revolutionary and globally patented Accelerated Hydrogen Peroxide (AHP) Technology. AHP has been the
CLEANER, FASTER, SUSTAINAIBLE and RESPONSIBLE disinfectant technology for over 15 years. Isn’t it time you made the switch?
For more information about Accel, visit ViroxAccel.com
Engineering Revolutionary Disinfectants
for the War Against Microbes
Patented
There’s prep.
And then there’s
ChloraPrep .
®
ChloraPrep SEPP ®
0.67mL Applicator
Fast-acting. Broad spectrum. Persistent.1,2,3
ChloraPrep® puts confidence at your fingertips. The ChloraPrep formulation
has been studied in more than 20 peer-reviewed publications. And according
to a recent survey, it’s also the leader in overall customer satisfaction.4
Trust the evidence. Trust your peers. Trust ChloraPrep.
References: 1. Hibbard JS. Analyses comparing the antimicrobial activity and safety of current antiseptic agents: a review. J Infus
Nurs. 2005;28(3):194–207. 2. Larson E. Guideline for use of topical antimicrobial agents. Am J Infect Control. 1988;16(6):253–266.
3. Denton GW. Chlorhexidine. In: Block SS. Disinfection, Sterilization, and Preservation. 5th ed. Philadelphia, Pa: Lippincott Williams &
Wilkins; 2001:321–336. 4. CareFusion Awareness & Usage Study. MRSI, April 2012.
carefusion.com/chloraprep | 800.523.0502
© 2012 CareFusion Corporation or one of its subsidiaries. All rights reserved.
CHLORAPREP, SEPP and FREPP are registered trademarks of CareFusion Corporation or one of its subsidiaries. ADV-SEPP0812
ChloraPrep FREPP®
1.5mL Applicator
CIC PROFILE
®
Meet
a
CIC
Stephanie Tismer, RN, CIC
Regions Hospital
St. Paul, Minnesota
Q:
Why did you choose
infection prevention
as a career?
It was actually by default. I suffered a back
injury while working in the surgical intensive
care unit. I was given the opportunity to work
in quality then infection control. I realized
after a couple of weeks on the job that this was
what I needed to be doing all along.
Q:
How long have you
been working in
infection prevention?
It has been eight very interesting years.
Q:
How many years had
you been practicing
infection prevention
when you started pursuing
board certification?
I was encouraged to seek board certification
after a few years but didn’t really think I
could pass the exam. There is always more
to learn and understand about the profession. I marveled at the women in my
department that studied and passed. My
colleagues would continuously encourage
me to just do it. I wanted to but always felt
short of the energy to make it a reality. How
was I going to squeeze one more activity
into my life?
Q:
What inspired you
to pursue board
certification in
infection prevention and
control (CIC)?
It was at the San Antonio conference [APIC
2012 Annual Conference] when I decided I
was going to get certified. I wanted the special dessert that was given to the certified
folks. As crazy as it sounds, I wanted to be
able to attend the special dessert table. I came
home and announced I would be taking the
exam. I needed to study like the women in
my department. I bought the study guide and
read through to the last chapter. In order to
pass, I made a commitment to use the study
guide and review what I didn’t know. I took a
two-week vacation and studied for three to four
hours in the morning and rewarded myself in
the afternoon. I reserved a room at the library.
I was not even available to kids by cell phone!
Q:
In what ways has your
CIC benefitted you?
While studying for the CIC exam I reviewed
the entire APIC Text. In doing that I found
areas in which our facility could improve. I was
able to measure our performance. I had the
confidence and ability to find the answers in
a pinch. I was better able to further my education around the topics in which I felt weak. It
gave me a foundation to understand the APIC
model and the desire to further my career.
Q:
In what ways has
your CIC benefitted
your healthcare
organization?
It can depend on me for a body of knowledge. I am a member of the team and am
expected to make recommendations for preventing infections in all areas. They can rely
on me to participate with others to improve
patient outcomes. During a CMS or Joint
Commission Survey they will be very happy
I am there!
Q:
Do you have any
tips for infection
preventionists
(IPs) who are pursuing their
certification?
You are a unique individual. Ask yourself honestly, “What do I need to do to take the exam
and pass?” For everyone, the answer will be
different. Take the practice test, and don’t look
at the answers until you complete the entire
section. If you get a question wrong, study
that entire chapter—not just the paragraph
to answer the question. Set limits with friends
and family about when and where you are
studying. I found out after my exam was over
that my significant other was in the hospital.
He didn’t want to have my thoughts go elsewhere. Wow—I guess I effectively communicated about how important CIC certification
was to me.
w w w.apic.org | 15
Briefs to keep you in-the-know
Infection Prevention and You
APIC’s consumer campaign makes waves.
By Elizabeth Garman and Janiene Bohannon
You are an
rt
important pa
of infection
prevention!
Wash your hands
water
with soap and
r
or use hand sanitize
often.
Ask healthcare
workers and your
visitors to do the
same.
Speak up for
your care!
Sneeze and cough
not
into your elbow,
your hand.
ns
Take medicatio
as directed.
Healthcare
workers will
clean their hands
before and after
they care for you.
ness effort titled “Infection Prevention and
You” helps patients, families, and healthcare professionals understand their role
in preventing infections. Launched in
conjunction with International Infection
Prevention Week (IIPW), October 20–26,
the centerpiece of the campaign this year
was a new website (www.apic.org/infectionpreventionandyou) with content and resources
for both patients and healthcare professionals, designed to simply and clearly convey
important infection prevention and patient
safety information.
APIC’s Communications Committee
conceived of the idea for the “Infection
Prevention and You” campaign after a 2010
discussion about the need for consumers and
other healthcare personnel to understand the
importance of infection prevention and the
profession. Since then, the campaign was
created and expanded to include:
• The new content-rich website (www.apic.
org/infectionpreventionandyou) for both
consumers and healthcare professionals
who are not infection preventionists (IPs).
• A one-of-a-kind infographic poster for
patients that was mailed to all members
with the fall issue of Prevention Strategist.
APIC encourages members to display it
in a patient care area of their respective
healthcare facilities. The full-size poster
includes tips on how consumers can play
an active role in infection prevention.
• Engagement via Facebook (www.facebook.
com/APICInfectionPreventionandYou) and
Twitter (http://twitter.com/@APIC). “Like”
or “follow” us for a continuous stream
of timely (and fun) information you can
share with others.
Word about the campaign has been
quickly spreading. It was featured in a
September 30 Wall Street Journal article titled, “Why hospitals want patients to
16 | WINTER 2013 | Prevention
workers
Your healthcare
gowns,
will wear gloves,
the right
and masks at
if you still
Every day, ask
need your catheter.
What are
healthcareassociated
infections?
ction
Who are infe
ts?
preventionis the bad germs and
devices
Catheters or other your
in
will be placed
skin
body after your
cleaning.
receives proper
ask doctors, ‘Have you washed your hands?’”
The story, which appeared in the Journal’s
Informed Patient column, includes a quote
from Carol McLay, DrPH, RN, CIC, chair
of APIC’s Communications Committee, who
helped design the campaign.
“We’ve been focusing on intensive interventions to improve hand hygiene among
healthcare workers for decades, yet we’ve really
shown very little progress,” says McLay in the
article. “We are trying to empower patients
and families to speak up and understand their
role.” Furthermore, the campaign was featured
If your room looks
it
dirty, ask to have
cleaned.
.
injection practices
Ask about safe
Needle, One
Remember: One
Time.
Syringe, only One
to find
detective skills
you safe.
nists use their
things to keep
Infection preventio
is doing the right
make sure everyone
APIC’s new multiyear education and aware-
Surgical site infections
along
When germs travel in your bladder or kidney.
cause an infection
Pneumonia
lungs.
Infection of the
in
for Professionals
Association
and Epidemiology
Infection Control
ectionPrevention
happens after
An infection that the body where
part of
surgery in the
place.
the surgery took
Bloodstream infections
the blood by way
When germs enter that is placed in
tube
of a catheter or
your vein.
Your room and
www.apic.org/Inf
ed infections are
Healthcare-associat
body
entering your
a result of germs
care.
during medical
urinary tract infections
and
Catheter-associated
a urinary catheter
any equipment
that is used on
you will be clean.
times.
If you are in isolation,
visitors
you and your
this too.
may need to do
Learn more
and
Clean your hands
make sure everyone
too.
around you does
surgery,
If you are having
shower
ask if you should soap
ng
with a germ-killi
ahead of time.
AndYou
www.facebook.com
entionandYou
/APICInfectionPrev
twitter.com/apic
on the CDC’s Safe Healthcare blog via a post
authored by Vicki Allen, MSN, RN, CIC,
APIC Communications Committee member.
APIC members and more than 30 association partners helped spread the message about “Infection Prevention and You”
throughout IIPW with live events, social
media messages, photo-sharing, and more.
APIC headquarters staff, Henry the Hand®
Champion Handwasher,
and APIC Washington,
“We received Prevention Strategist today.
DC Metro Chapter
Membership Chair Kissa
We LOVE the poster! Thanks to any and
M. Robinson, RN, BSN,
all who thought of it! LOVE IT!”
joined together to pass
—Susan Kraska, RN, CIC, Memorial Hospital
out hand sanitizer and
of South Bend, South Bend, Indiana
“Infection Prevention
and You” posters in front
of the Foggy Bottom
metro stop next to the
APIC staff members express their enthusiasm for infection prevention with Henry the Hand. Left to right,
back row: Monti Bush, Jacqueline Manson, Katrina Crist, Yolanda Tillery, Kathryn Hitchcock. Front row: Bach
Truong, Christina James, Elizabeth Garman, Janiene Bohannon, and Lynn Schneider.
“I REALLY like the new resources on the website! The
infographic is concise but thorough. I had already printed one
from the website, but I was thrilled to get the big one in my
[issue of] Prevention Strategist. I have it proudly displayed on
my door! ...Thanks for all of the hard work that you all and
your teams put into this resource!”
—Tiffany Horsley, RN, BSN, CIC, Coffeyville Regional Medical Center,
Coffeyville, Kansas
We thank the 2013 APIC
Communications Committee
for its ongoing support and
volunteerism in enhancing and
furthering infection prevention
communication initiatives.
Chair: Carol McLay, DrPH, RN, CIC
Lexington, Kentucky
George Washington University Hospital
in Washington, DC.
APIC will continue to expand its
“Infection Prevention and You” campaign to
educate both patients/consumers and healthcare professionals. We encourage members
to spread the word about the new site
(www.apic.org/infectionpreventionandyou) to
help engage everyone in infection prevention. If you still haven’t visited the new site,
here’s a run-down of what you will find:
The consumer tab provides tips, tools, and
links to reputable sources of information to
promote infection prevention in every setting:
healthcare facilities, at work, at school, on
vacation, at home, and even in locker rooms.
The healthcare professionals tab is designed
for healthcare workers who are not trained
IPs, which provides basic information on how
to keep patients safe regardless of their roles
within healthcare organizations. With the continued help of the
Communications Committee, APIC
also continues to improve and expand
its Consumer section of the main site—
www.apic.org/patientsafety. This section of
the site was specifically created to house
resources for IPs to use in their educational
efforts. Here, members can find:
• A new flier that explains isolation precautions (Materials for Healthcare Facilities
section)
• I nfection prevention brochures,
PowerPoint presentations, posters, and
fliers to display in acute care, home care,
long-term care, and ambulatory/outpatient settings (Materials for Healthcare
Facilities section)
• Links to reputable consumer-focused
resources on a variety of infection prevention topics (Additional Patient Safety
Resources page)
• A rchived monthly email alerts for consumers on everything from antibiotics to
vaccines
continued on page 18
Vice-Chair: Elizabeth Monsees, RN,
MSN, MBA, CIC
Children’s Mercy Hospitals and Clinics
Kansas City, Missouri
Vicki Allen, MSN, RN, CIC
CaroMont Health
Huntersville, North Carolina
Laura Buford, RN, BSN, CIC
St. David’s HealthCare
Austin, Texas
Deb Patterson Burdsall MSN,
RN-BC, CIC
Lutheran Life Communities
Arlington Heights, Illinois
Nicole Gualandi, RN, MS/MPH, CIC
Centers for Disease Control
and Prevention
Atlanta, Georgia
Crystal Heishman, BSN, RN, CIC, ONC
University of Louisville Healthcare
Louisville, Kentucky
Sharon Jacobs, RN, MS, CIC
Bridgeville, Pennsylvania
Irena L. Kenneley, PhD, APRN-BC, CIC
Frances Payne Bolton School of Nursing
Cleveland, Ohio
Nancy Szilagyi, LPN, CIC
Capital Health
Trenton, New Jersey
Kim Whisman, RN, BSN
Hospice of the Bluegrass
Lexington, Kentucky
APIC members Robert L. Geist, MPH, CIC, epidemiologist, Kansas Department of Health and Environment (KDHE)
Healthcare-Associated Infections Program; Tiffany Horsley, RN, BSN, CIC, infection prevention nurse, Coffeyville
Regional Medical Center; and Joseph M. Scaletta, MPH, RN, CIC, director, KDHE Healthcare-Associated Infections
Program, pose in front of the “Infection Prevention and You” poster during International Infection Prevention Week.
Maria Whitaker, MT, CIC
Cortland Regional Medical Center
Cortland, New York
w w w.apic.org | 17
Briefs to keep you in-the-know
“We [California Department of Public Health] are currently
in the process of redesigning our entire HAI Program website
and are creating an ‘HAI Education and Prevention Library’ on
a new ‘Me and My Family’ webpage. We would be thrilled to
feature APIC’s infographic, which we believe provides the right
information to the public in an accessible and visually appealing
format. Thank you for letting us use it for this purpose!”
—Lanette Corona, California Department of Public Health, Richmond, California
Competency
Advancement
Assistance
(CAA) program
recipients
announced
To help infection preventionists (IPs) bet-
ter manage costs associated with obtaining
the CIC® credential, APIC has continued
the Competency Advancement Assistance
program (CAA) for 2013-2014, which is
designed to support this critical component
of competency advancement. Last year,
APIC provided financial assistance to more
than 80 individuals for costs related to either
initial certification or recertification.
Staff members at Charlotte Endoscopy Surgery Center
demonstrated their support for “Infection Prevention
and You” by wearing black polka-dot ribbons on the
right side of their chests to encourage everyone to
commit to hand hygiene. The black dots indicate the
“the invasion of bacteria” and the white background
represents “the purity of sterility.”
continued from page 17
“It’s unfortunate but true that one in 20
patients will develop an infection as a result of
their healthcare. As patient safety advocates,
APIC wants to empower patients, families,
and healthcare professionals to speak up and
take action to prevent infections,” said McLay.
So, what’s in store for the campaign? APIC
and the Communications Committee hope
to offer more infographic posters for other
healthcare settings and obtain feedback from
members on ways we can help make their
jobs easier. Thanks to the hard work of APIC
members, the word is spreading to others, but
we still have more work to do.
Elizabeth Garman is APIC senior director
of Communications. Janiene Bohannon is
APIC associate director of Communications
and managing editor of Prevention Strategist.
18 | WINTER 2013 | Prevention
2013 Partners
We thank our 2013 Association Partners for their support in spreading the
message about the importance of infection prevention.
Accreditation Association for Ambulatory Health Care
(AAAHC)
American Academy of Urgent Care Medicine (AAUCM)
American Cancer Society Cancer Action Network
American Society for Healthcare Engineering (ASHE)
American Society of Ophthalmic Registered Nurses
(ASORN)
Associação Paulista de Epidemologia e Controle
de Infecção Relacionada à Assistência à Saúde
(APECIH)
Association of periOperative Registered Nurses (AORN)
California Department of Public Health (CDPH)
Healthcare-Associated Infections Program Centers for Disease Control and Prevention (CDC)
Center for Disease Dynamics, Economics & Policy
(CDDEP)
Certification Board of Infection Control and
Epidemiology (CBIC)
Children’s HeartLink
Coffee Regional Medical Center (CRMC)
Colorado Department of Public Health and Environment Community and Hospital Infection Control Association
(CHICA)
Connecticut Center for Patient Safety (CTCPS)
Det Norske Veritas Germanischer Lloyd (DNV GL
Healthcare)
Georgia Hospital Association (GHA)/Georgia Hospital
Engagement Network (HEN)
Healthcare Laundry Accreditation Council
Henry the Hand—Champion Handwasher
Infusion Nurses Society (INS)
Institute for Healthcare Improvement (IHI)
Le Bonheur Children’s Hospital
MedStar Health
Methodist Le Bonheur Healthcare
National Foundation for Infectious Diseases (NFID)
National Patient Safety Foundation (NPSF)
National Resource for Infection Control (NRIC) Organization for Safety, Asepsis and Prevention
(OSAP)
Safe Injection Practices Coalition (SIPC)
Society for Healthcare Epidemiology of America
(SHEA)
Society of Gastroenterology Nurses & Associates,
Inc. (SGNA)
St. Jude Children’s Research Hospital
The Joint Commission
Think About It Colorado
Webber Training, Inc.
We are pleased to announce the 2013 CAA
program recipients:
Debra Summers (Franklin, TN)
Donna C. McDaniel (Ronan, MT)
Heidi LePard (Great Falls, MT)
Debra Spavone (Newnan, GA)
Amanda Guspiel (Minneapolis, MN)
Victoria Mieth (Phoenix, AZ)
Scarlett Rivera (Valdosta, GA)
Laura Kehler (Garden City, MI)
Katelyn Harms (Madison, WI)
Susan O’Connor-Wright (Sandy, UT)
Maura K Kivlin RN, BSN (Scranton, PA)
Kathleen Pitts (Rochester, NY)
Ann P. North (Florence, SC)
Heidi Leeper (Rensselaer, IN)
Sue Ann B. Avin (Florence, SC)
Valerie Lambiase (Salt Lake City, UT)
Pamela Webb (Great Falls, MT)
Karen C. Ray (Bel Air, MD)
Erin Minnerath (Fort Harrison, MT)
Kisha Wilkinson (Philadelphia, PA)
Kathryn Larsen (Miles City, MT)
Debra Graem (Fort Worth, TX)
Rhonda K. Reed (South Bend, IN)
Kelley Tobey (Knoxville, TN)
Lauri Holmes (White House, TN)
Deborah Paul-Cheadle (Wyoming, MI)
Sheri Bishop (Fayetteville, AR)
Mary Kowatch (Sebastopol, CA)
Karen K. Pitman (Olympia, WA)
Tersa Bonifant (Portales, NM)
Sarah E. Partain (Tigard, OR)
Elaine Flowers (Mount Vernon, OH)
Paula Simplot (Ottumwa, IA)
Karel A. Curtis (Williamsburg, VA)
Teresa Barnett (Temple, TX)
Mary Post (Lake Oswego, OR)
Maribeth Blethen Coluni (Blacksburg, VA)
Cheri Bell (West Bend, WI)
Sonia Rodriguez (Milwaukee, WI)
Ranay Storms (Knoxville, AR)
Sheila S. Newman (Troy, AL)
Cindy Barloga (Highlands, NC)
Teal Jeffers (Metter, GA)
Perri Brooks-Correll (Dalton, GA)
Angela Howell (Watsonville, CA)
Brittain Avery Wood (Morrisville, NC)
Sherry Brace (Saint Petersburg, FL)
Joyce E. Weaver (Bucyrus, OH)
Kayera Kashmiri (Tampa, FL)
Michael Grow (Williamsport, IN)
Sandra Neola (South Russell, OH)
Lee Ann Angelini (Clearwater, FL)
Catriona MacBean-Mann (Saint Paul, MN)
Stacia Brown (Tacoma, WA)
Amy Michelle Gray (Corinth, MS)
Jennifer VanderZee (Cedar Rapids, IA)
Paola Beatriz Acuna (Lima, Peru)
Rebecca Bartles (Colorado Springs, CO)
Elizabeth Coe (Corbin, KY)
Michelle Raab (Branson, MO)
Donna Sears (Attleboro, MA)
Thank you to APIC’s Strategic
Partners—the sole sponsors of the CAA
program.
With
Sani-Cloth Bleach,
PDI has you totally
covered.
®
One company to cover all
your germicidal wipe needs.
NEW XL canister!
)RUXVHLQKLJKULVNDUHDV
HQGHPLFZLWKClostridium
difficile VSRUHVDQG1RURYLUXV
(IIHFWLYHDJDLQVW
PLFURRUJDQLVPV
PLQXWHFRQWDFWWLPH
© 2013 PDI. All rights reserved.
662816_PDI.indd 1
)RUPRUHLQIRUPDWLRQYLVLWPDIBeTheDifference.com
w22/10/13
w w.apic.org
7:43 PM | 19
TWO is always better than ONE.
SANUVOX introduces
ASEPTIX
The Sanuvox Aseptix Dual UV Sterilization System uses a Primary and
Secondary unit specially designed to eliminate “shadow areas”
sterilizing a room in less than 15 minutes. The Aseptix is the fastest,
most effective room sterilizer available at a fraction of the cost of the
competition.
FEATURES AT A GLANCE
· Dual unit operation guarantees most effective
sterilization / terminal cleaning possible
· Minimizes “shadow area”
A
· Tested to show >99.9999% reduction of C. difficile & MRSA
· Wireless communication with any smart device
· Eight (8) Wide-Range Infra-Red Motion Safety Sensors
· Data Log records sterilization process
· Medical grade stainless steel & aluminum
Secondary Unit
No need for repositioning. Dual
unit system
dramatically reduces
shadow area.
Primary Unit
Controlled & monitored
through any Wi-Fi
enabled smart device.
DESIGNED & MANUFACTURED BY
LEADER IN ULTRAVIOLET STERILIZATION SINCE 1995
CAPITOL COMMENTS
The National Action Plan to
Prevent HAIs five years later—
Measuring progress and
mapping out the future
BY NANCY HAILPERN AND
LISA TOMLINSON
September 25–26, 2013, just days before
“If you can’t explain it simply, you
don’t understand it well enough.”
—Albert Einstein
“Because federal law links
the targets and metrics of the
HAI Action Plan to Medicare
payment, updates to the
HAI Action Plan are a good
indicator of the direction
federal agencies may move
when developing regulations.”
22 | WINTER 2013 | Prevention
the federal government shutdown, the U.S.
Department of Health and Human Services
(HHS) convened its “Road Map to Eliminate
HAI: 2013 Action Plan Conference” to
assess progress made in reaching the initial
five-year targets and metrics of the plan and
to discuss setting new targets.
As you likely recall, the Federal HAI
Action Plan originated out of a 2008 report
by the U.S. Government Accountability
Office (GAO) that recommended better
consistency and compatibility of data across
HHS agencies and prioritization of recommendations, followed by a Congressional
hearing that highlighted the report’s recommendations. Although HAI data collection and the best way to approach it can
be complex, the goal was somewhat simple:
to take all the data the federal government
collects related to HAIs and provide a simple
dashboard of our nation’s progress, and to
coordinate around HAI elimination.
The first step in developing a National
HAI Action Plan was for HHS to convene a steering committee consisting of a
variety of agencies within HHS, as well as
the U.S. Departments of Labor, Defense,
and Veterans Affairs, to coordinate and
maximize the efficiency of HAI prevention
efforts across the federal government. The
first phase of the HAI Action Plan focused
on acute care hospitals and determined fiveyear prevention targets for process and outcome metrics in acute care. In order to better
understand how the various federal agencies
were doing as a whole on reduction of HAIs,
it was necessary to come up with federal
targets and metrics that drew on the existing data collection methods of the various
federal agencies, specifically the Centers for
Disease Control and Prevention (CDC), the
Centers for Medicare & Medicaid Services
(CMS), and the Agency for Healthcare
Research and Quality (AHRQ).
The outcome metrics include data drawn
from a variety of sources, although APIC
has advocated moving away from using
administrative data when presenting HAI
data. In fact, a presenter from the CDC
pointed out that AHRQ Healthcare Cost
and Utilization Project (HCUP) data
includes both hospital and community
onset Clostridium difficile infection (CDI)
and reflects an overall trend in burden,
while the CDC’s National Healthcare
Safety Network (NHSN) is specific to
hospital-onset CDI based on laboratory
identification and is intended to reflect
trends in hospital performance.
Measuring Progress Toward
HAI Action Plan Outcome Goals
The plan included process measures as
well, including Surgical Care Improvement
Project (SCIP) measures related to infection,
but many of those measures (SCIP-Inf-1,
SCIP-Inf-2, SCIP-Inf-3, SCIP-Inf-4) have
seen compliance of more than 90 percent
in the most recent HAI Action Plan. In
addition, SCIP-Inf-6, Appropriate Hair
Removal, was suspended in 2012 due to
topped-out status.
As we review progress on the National
HAI Action Plan as reported at the
September 2013 HHS stakeholder meeting, we see that targets are likely to be met in
some areas but others will need more focused
attention. Review of this information also
allows for identification of opportunities
“Although HAI data collection and the best way to
approach it can be complex, the goal was somewhat simple:
to take all the data the federal government collects related
to HAIs and provide a simple dashboard of our nation’s
progress, and to coordinate around HAI elimination.”
for improvement in reducing HAIs. One of
the CDC presenters outlined the following
opportunities for improvement based on
where we are to date:
CLABSI
• Explore best practices for CLABSI prevention outside the ICU.
• Conduct research to assess the current
proportion of CLABSIs that are not
preventable.
CAUTI
• Reduce catheter use.
• Widely implement best practices for catheter insertion.
• Increase focus on catheter maintenance.
• Provide education on appropriateness of
diagnostic testing (urine cultures).
Metric
SSI
• Implement updated recommendations for
SSI prevention from upcoming HICPAC
guideline.
• Collaborate with external partners to produce procedure-specific recommendations
for surveillance and prevention.
MRSA
• E xpand MRSA prevention efforts to
healthcare-associated community onset
cases.
Clostridium difficile
• Improve antimicrobial use in inpatient
settings.
• Improve environmental decontamination.
In addition to updating the acute care
metrics, future iterations of the plan will
Baseline
Source
Central Line-Associated Bloodstream
Infections (CLABSI)
2006-2008
NHSN/SIR
Invasive MRSA infections (population)
2007-2008
EIP/ABC
Surgical Site Infections (SSI)
2006-2008
Hospital-Onset Clostridium difficile infections
Hospital-Onset MRSA bacteremia
further refine targets and metrics for areas
added to the plan as parts of Phase 2, focused
on HAI prevention in ambulatory surgical
centers and end-stage renal disease facilities, and influenza vaccination of healthcare
personnel; and Phase 3, focused on HAI
prevention in long-term care facilities.
With all of the attention focused on targets
and metrics, how does this impact the day-today work of infection preventionists? Because
federal law links the targets and metrics of
the HAI Action Plan to Medicare payment,
updates to the HAI Action Plan are a good
indicator of the direction federal agencies
may move when developing regulations.
Nancy Hailpern is APIC director of Regulatory
Affairs, and Lisa Tomlinson is APIC senior
director of Government Affairs.
Description of Target
Update at sept. 13 HHS Meeting
50% reduction
in ICU and ward-located patients
44% reduction
(SIR = .56)
50% reduction
in incidence of healthcare-associated
invasive MRSA infections
31% reduction*
NHSN/SIR
25% reduction
in SSIs following SCIP-like procedures on
admission or readmission
20% reduction*
(SIR =.80)
2010-2011
NHSN/SIR
30% reduction
in facility-wide inpatient healthcare
facility-onset Clostridium difficile LabID
Events
2% reduction
(SIR = .98)
2010-2011
NHSN/SIR
25% reduction
in facility-wide inpatient healthcare
facility-onset MRSA blood LabID Events
3% reduction
(SIR = .97)
Catheter-Associated Urinary Tract Infections
(CAUTI)
2009
NHSN/SIR
25% reduction
in ICU and ward-located patients
2% increase
(SIR =1.02)
Clostridium difficile (hospitalizations)
2008
HCUP
30% reduction
in hospitalizations with C. diff
22% increase**
Note: Information based on federal agency presentations at National Action Plan to
Prevent HAIs meeting on September 25–26, 2013.
*Estimate based on preliminary 2012 data when noted in the presentation.
**Projection for 2013.
Abbreviations: EIP/ABC is the CDC’s Emerging Infections Program Antibacterial
Core Surveillance program.
NHSN is the CDC’s National Healthcare Safety Network.
SIR is Standardized Infection Ratio, which is observed number of HAIs/predicted
number of HAIs.
HCUP is AHRQ’s Healthcare Cost and Utilization Project, an all-payer inpatient care
database that uses an ICD-9 code for Clostridium difficile.
w w w.apic.org | 23
GLOBAL INSIGHT
Egypt’s Professional
Diploma in Infection
Control (PDIC):
A success story
Until 2003, there was no structured infec-
BY OSSAMA RASSLAN,
MD, PhD
“More than 70 percent of the
graduates are now working
as infection control doctors/
infection control team leaders,
and infection control nurses in
different healthcare facilities
in Egypt and other
Arab countries.”
24 | WINTER 2013 | Prevention
tion control program in Egypt, neither
at the national level nor at the peripheral facility level. There were only some
individual efforts and isolated trials in
some healthcare facilities. Early in 2003,
the Ministry of Health (MOH), World
Health Organization (WHO), Eastern
Mediterranean Regional Office (EMRO),
and other relevant governmental and nongovernmental healthcare authorities and
organizations established an infection control program.
Education in infection prevention and
control was targeted as one of the main
objectives of the infection control program.
The MOH in conjunction with the APIC
Egypt chapter (formerly the Egyptian
Society for Infection Control [ESIC]) developed short-term infection control Training
of Trainers (ToT) courses. These courses
were conducted in one of two forms: a oneweek per month course over a six-month
period with the three-week gap during
each month used for practical on-the-job
training in the field, and a one-day per
week course for a six-m onth period, with
field assignments and projects throughout
the course, followed by the awarding of a
training certificate after sitting for written,
oral, and practical exams.
After four years of the certified training, APIC Egypt and the Arab Institute
for Continuing Professional Development
(AICPD) decided that if qualified professionals are to take over infection prevention and control activities in Egypt, as well
as the EMRO region, it was important to
have a more comprehensive training program. Thus, the idea for the Professional
Diploma in Infection Prevention and
Control (PDIC) was born.
PDIC curriculum
The PDIC aims to provide candidates
with sufficient knowledge, skills, and
attitudes that are essential for leading and
managing infection prevention and control programs in various healthcare organizations. The program is organized into
two main phases. The first phase covers
the basic principles and general measures
for prevention and control of healthcareassociated infections (HAIs). The second
phase focuses on the applied practices and
advanced issues for prevention and control
of HAIs. The two phases are conducted as
nine learning modules:
1.Basic Principles and Practices for
Prevention and Control of HAIs
2. Support Services and Environmental
Infection Prevention and Control Measures
3. Infection Prevention and Control Aspects
of Occupational Health Programs
4.Basics of Healthcare-Associated Infection
Epidemiology and Surveillance
5. B asics of Infection Prevention and Control
Program Management
6. Infection Prevention and Control Strategies
in Core Healthcare Units
7. Infectious Disease Process and
Antimicrobial Stewardship
8. Specific Infection Prevention and Control
Measures
9. Patient Safety Issues and Quality
Improvement
The main teaching and training sources are listed in the references
section at the end of the article.
The program was delivered as part-time
training over a 16-month period. The
workload equals 22 credit hours, fulfilling the following activities: face-to-face
instruction and interactive discussion, field
visits and hands-on training, and independent self-study comprising of assignments
and project work. Candidates are graduates
of medical and nursing schools who have
successfully completed the pre-registration
house officer year. Enrollment in the program is open three times a year: in January,
May, and September. Expert instructors
deliver different methods of learning in the
form of formal didactic lectures, practical
sessions, interactive workshops, and structured, supervised field training.
Program administrators evaluate participants using different methods including
final summative written exams, objective
structured practical exams (OSPEs), periodical written assignments, and final project presentations. All program participants
must maintain and update a logbook in
which they document their participation
in formal teaching sessions and field work
activities. A number of factors are taken
into consideration when evaluating the program including participant and instructor
feedback, peer-review, annual reporting,
and external assessment.
Participants
To date, 777 participants have joined 16
classes; comprising two classes in 2007/2008,
two in 2008/2009, three in 2009/2010, three
in 2010/2011, three in 2011/2012, and three
in 2012/2013. Participants in 12 classes have
graduated. The other four are ongoing.
Nationalities: PDIC participants were
from nine different Arab countries. About
90 percent were Egyptian. Other participants
were from Sudan, Yemen, Iraq, Syria, Libya,
Palestine, Saudi Arabia, and Kuwait. Some
candidates (mainly from Iraq) were funded
by EMRO/WHO, and Palestinian candidates were sponsored by the Arab Medical
Union (AMU).
Affiliations: Candidates were affiliated
with a variety of healthcare organizations
and authorities in different Arab countries
including MOH, teaching hospitals, health
insurance hospitals, charity hospitals, private
hospitals, academic institutions, and university hospitals, in addition to some independent participants.
Field work
Expert instructors deliver
different methods of
learning in the form of
formal didactic lectures,
practical sessions, interactive
workshops, and structured,
supervised field training.
Practical field training included a wide
variety of essential topics such as hand
hygiene, personal protective equipment
(PPE), disinfection and sterilization, support services (e.g., laundry, kitchen, air
conditioning, ventilation systems, water
services, and maintenance), and unit specific measures (e.g., dialysis unit, ICU,
NICU, burn unit, endoscopy unit). Many
general or specialized tertiary hospitals
belonging to the MOH, a university, or
teaching hospitals have been included in
the practical training sessions. Participation
depends on the relevance of students’ specialty to the training topic, how well they
are equipped, and the presence of expert
trainers within the facilities.
Each of the two PDIC phases (basic
and advanced) include seven to eight daytime supervised practical training sessions.
Participants were divided into groups of
10–12 people, each under supervision of an
experienced trainer. Each training session
was conducted by a specialty expert with
relevant experience in the specialty, under
the supervision of a faculty staff member
(a professor or senior infection prevention
and control consultant).
w w w.apic.org | 25
GLOBAL INSIGHT
Field Projects
Participants of each PDIC class are divided
(at the beginning of the course) into groups
of five. While under supervision, students
agreed to conduct a field project throughout the course and to present their findings,
conclusion, and recommendations at the end
of the project as a prerequisite for taking the
final exam. Students targeted a variety of topics for conducting field projects, including:
• Situation analysis and benchmarking
among different facilities
• Surveillance studies in different settings
• Intervention studies in some critical
care units
• Outbreak investigation (e.g., MRSA,
VRSA, food poisoning)
• Developing and implementing an infection prevention and control program, and
measuring its impact
• Developing an education program
Output and influence
“Infection prevention
and control is an essential
element in providing
high-quality healthcare
in achieving accreditation
in healthcare facilities.
Knowledge, education,
and training are the
cornerstones in proper
implementation of an
infection prevention and
control program.”
26 | WINTER 2013 | Prevention
More than 70 percent of the graduates are
now working as infection control doctors/
infection control team leaders, and infection control nurses in different healthcare
facilities in Egypt and other Arab countries.
Consequently, about 15 percent of the secondary and tertiary care hospitals in different
healthcare authorities in Egypt are currently
employing PDIC graduates—and the number is increasing. A number of graduates are
now working as consultants and advisory
board members in large governmental and
non-governmental hospitals. A group of
graduates is also working as strategic planners and infection prevention and control
directors at the central level of the MOH,
specialized medical centers, teaching hospitals, and Institutes Authority in Egypt. Some
of the graduates are university staff members
in schools of medicine in Cairo, Ain Shams,
Alexandria, and Misr International universities and are currently responsible for running
infection prevention and control courses and
master degree programs.
Research
Many infection preventionists (IPs) are
now research-minded. A multidisciplinary
research movement is currently underway
in important aspects and core functions of
HAIs and infection prevention and control
such as bloodborne pathogens, antimicrobial resistance, antimicrobial stewardship,
hand hygiene, isolation precautions, surveillance issues, and others. Many PDIC
graduates have published original research
articles in different infectious diseases and
infection prevention disciplines in local,
regional, and international peer-reviewed
journals in the last few years.
Recognition
PDIC has been recognized locally by the
Egyptian Medical Syndicate (EMS), and
graduates are listed as infection control
specialists in the EMS registry. PDIC
has also been recognized by the Egyptian
Board for Medical Specialties. PDIC degree
holders who join the Egyptian Board for
Medical Specialties receive a one-year
period deducted from the mandatory three
years for the Egyptian Board for Infection
Control. The PDIC was also recognized by
EMRO/WHO and AMU. Both organizations have specific scholarships and grants
to cover the PDIC course fees for candidates
from some of their member states (e.g.,
Palestine and Iraq). EMRO/WHO signed
a memorandum of understanding to support PDIC by providing infection prevention and control experts, meeting rooms,
and some small grants. PDIC was also
endorsed by the International Federation
for Infection Control (IFIC).
Progress
Basic PDIC courses were conducted in
Libya (two courses in 2008-2009) and in
Syria (one course in 2009-2010) in cooperation with EMRO/WHO. In the fall
of 2013, a PDIC course was launched in
Khartoum-Sudan at the Sudan Branch
of the Arab Institute for Continuing
Professional Development (AICPD), in
cooperation with the Sudan Medical
Union. PDIC is currently undergoing an
accreditation process by the International
Board for Certified Trainers through the
Egyptian Supreme Council for Universities
TOP LEFT. Participants received
practical on-the-job training in
many fields including dentistry.
ABOVE. Practical field training
included a wide variety of essential
topics such as hand hygiene, PPE,
disinfection and sterilization, support
services, and unit specific measures.
To date, 777 graduates have received their Professional
Diploma in Infection Prevention and Control (PDIC).
in Egypt and is expecting recognition for
accreditation soon. Webber Training will
soon post an Arabic version for the PDIC
course presentations to its website.
PDIC has future plans to:
• Extend to other medical and paramedical specialties, namely dentists and
pharmacists
• Develop specialized courses for laboratory
technicians and veterinarians
• E stablish a consultation center (from
PDIC staff and graduates) to prepare
healthcare facilities for accreditation in
infection control areas
• Extend to other countries in the region
and to develop an e-learning module of
PDIC for distant learning in remote countries in the region
Ossama Rasslan, Md, Phd, delivers a speech
during a pdic graduation ceremony.
Conclusion
Infection prevention and control is an essential element in providing high-quality healthcare in achieving accreditation in healthcare
facilities. Knowledge, education, and training
are the cornerstones in proper implementation of an infection prevention and control
program. Certification in infection prevention and control is a key professional standard
for any IP. A well-organized and structured
infection prevention educational program
in an appropriately equipped training center
under supervision of well-trained educators is
one of the main pillars of success in practicing infection prevention.
Hands-on sessions, log books, practical
assignments, and field projects should be
the core elements in conducting an infection
prevention educational program to facilitate
translating knowledge into practice. Baseline
assessment should be the starting point in
tailoring a successful infection prevention
educational program, and key concepts
should involve teaching basic knowledge
and helping others understand how to do
the most with limited resources using their
existing systems.
Ossama Rasslan, MD, PhD, is president of the
APIC Egypt chapter and chair of the PDIC
Scientific Council in Cairo, Egypt.
w w w.apic.org | 27
The truth is,
C. difficile may have been
admitted to all these rooms.
When the problem is facilitywide,
the solution has to be.
• 33% of non-CDI rooms have tested positive for C. difficile.1
• 55% of high-touch areas in patient rooms have tested positive for C. difficile.1
Clorox Healthcare™ Bleach
Germicidal Disinfectants
kill C. difficile spores quickly:
wipes – 3 minutes, sprays – 5 minutes.
Wipes, sprays, pull-tops, refills —
solutions for everywhere.*
Learn more at www.cloroxhealthcare.com.
© 2013 Clorox Professional Products Company.
NI-20892
1. B. Koll, American Journal of Infection Control, June 2009
*Use as directed on hard, nonporous surfaces
prevention in action
My Bugaboo:
Multidrug-resistant
Tuberculosis
A microbiological overview of MDR-TB.
BY IRENA KENNELEY, PHD, APRN-BC, CIC
Greetings fellow infection preventionists!
The science of infectious diseases involves hundreds of bacteria, viruses, fungi, and protozoa. The amount of informa-
tion available on microbial organisms poses a special problem to infection preventionists (IPs). Obviously, the impact of
microbial disease cannot be overstated. Traditionally the teaching of microbiology has been based mostly on memorization
of facts (the “bug parade”). Too much information makes it difficult to tease out what is important and directly applicable
to practice. This quarter’s My Bugaboo column features information about multidrug-resistant Tuberculosis (MDR-TB). The
intention is to convey succinct information to busy IPs for common etiologic agents of healthcare-associated infections.
Please feel free to contact me with questions, suggestions, and comments at irena@case.edu.
Under a high magnification of 15549x, this colorized SEM depicted some of the ultrastructural details seen in the cell wall configuration of a
number of Gram-positive Mycobacterium tuberculosis bacteria. Photo courtesy CDC/Dr. Ray Butler; Janice Haney Carr.
w w w.apic.org | 29
PREVENTION IN ACTION
T
uberculosis (TB) is one of the world’s deadliest infectious diseases. The
World Health Organization (WHO) estimates that at least one third of
the world’s population is infected with TB. In 2011, TB caused approximately 1.4 million deaths worldwide. TB is the leading cause of death for people
infected with the human immunodeficiency virus (HIV).1
Genus Mycobacterium
Bacteria within the genus
Mycobacterium are rod-shaped
organisms that are resistant to
decolorization in the staining
process. Because of this property, they are known as “acidfast bacteria” (also known as
acid-fast bacilli). The cell wall
of the TB bacterium is composed mainly of lipids, which
in turn is responsible for many
of the commonly known characteristics of this organism.
These characteristics include
not only acid-fastness, but
resistance to disinfectants and
detergents (hence the need for
tuberculocidals), slow growth
in the laboratory, and resistance to common antibacterial
products.2
Most Mycobacteria grow
slowly, and the isolation of M.
tuberculosis, M. avium-intracellulare, and M. kansasii can
require three to eight weeks
of incubation. Other human
pathogens of this genus include:
M. leprae (leprosy), M. fortuitum, M. chelonae, and M. abscessus among others.2
Mycobacterium tuberculosis
M. tuberculosis is an intracellular pathogen that can cause
lifelong infection. The organism is acquired through the airborne route via inhaled droplets.
Infection of the lungs is the most
common course of TB disease,
estimated to be 70 to 80 percent
of all cases. Overall, only 5 to
10 percent of people exposed to
TB progress from infection to
30 | WINTER 2013 | Prevention
disease. The risk of progression
is much higher in the immunosuppressed.1, 2
Definitions
• M ultidrug-resist ant
TB
(MDR-TB): strains resistant
to the most effective antiTB drugs (isoniazid and
rifampin).1 See Table 1 for
more information about the
medications used to treat TB.
• E xtensively Drug-resistant TB
(XDR-TB): strains that have
developed resistance not only
to isoniazid and rifampin but
are also resistant to any of the
second-line anti-TB drugs.
These resistant strains of TB
do not respond to the standard six-month treatment
with first-line anti-TB drugs
and can take two or more
years to treat with drugs that
are less potent, more toxic,
and much more expensive
(see Table 1).1
In 2013, the WHO published
key findings in TB surveillance.
Essentially, resistant TB strains
are widespread and occur in virtually all countries. By March
2013, 84 countries had reported
at least one case of XDR-TB.
WHO estimates that there were
500,000 new cases of MDR-TB
in 2011. Of these, 60 percent of
cases occurred in Brazil, China,
India, the Russian Federation,
and South Africa (the so-called
“BRICS” countries).1
A total of 9,945 TB cases were
reported in the United States in
2012, or 3.2 cases per 100,000
persons. According to the CDC,
the percentage of MDR-TB
cases decreased slightly from 1.6
percent (127 cases) in 2011 to
1.1 percent (83 cases) in 2012.1
Treatment and drug update
Figure 1 illustrates medications
currently used to treat TB and
the drug’s mode of action. TB
disease is treated with a multiple drug regimen administered
by directly observed therapy
(DOT) for six to nine months
(usually isoniazid, rifampin,
ethambutol, and pyrazinamide
for two months, followed by
isoniazid and rifampin for an
addition four months) if the
TB strain is not MDR-TB. If
it is MDR-TB, the treatment is
more difficult, requiring four to
six drugs for 18 to 24 months;
the case should be managed
by an expert in MDR-TB. The
American Thoracic Society
(ATS), Centers for Disease
Control and Prevention (CDC),
and Infectious Disease Society
of America (IDSA) have
published guidelines on TB
treatment.5
The drug, known generically as bedaquiline (brand
name Sirturo), is the first new
type of TB drug to be approved
by the U.S. Food and Drug
Administration in more than 40
years. The initial recommendations were issued in December
2012 for treatment of MDR-TB
as part of combination therapy
in adults over the age of 18
with TB infections of the lung.
Table 1: First and second line of treatment of TB and new TB drugs in development
First-Line TB
Treatment
Drugs
Drug
Abbreviation
Second-Line TB
Treatment
Drugs
Drug
Examples
New TB Drugs
in Development
Nitroimidazoles*
Ethambutol
EMB or E
Aminoglycosides
amikacin (AMK) kanamycin
(KM)
SQ-109**
Isoniazid
INH or H
Polypeptides
capreomycin viomycin
enviomycin
PA-824**
Pyrazinamide
PZA or Z
Fluoroquinolones
ciprofloxacin (CIP)
levofloxacin moxifloxacin
(MXF)
Rifampin
RMP or R
Thioamides
ethionamide, prothionamide
Cycloserine
closerin
OPC 67683
Terizidone
*Nitroimidazoles: novel, complex mechanisms of action: inhibit cell wall synthesis AND inhibit cell respiration.
**NIAID has supported the development of two compounds denoted by asterisks (*) above.3
However, in October 2013 the
CDC (TB Elimination branch)
issued recommendations for
treatment beyond the original
narrow group of adults to children, pregnant women, and
those with diabetes and HIV
infection. However, further
study is required before routine
use of bedaquiline can be recommended in these populations.
Reported side effects include
hepatotoxicity, renal impairment,
and cardiac toxicity.9
Figure 1: Multidrug-Resistant Tuberculosis (MDR-TB) and possible effective treatments
Infection Prevention
All healthcare settings need
an infection control program
designed to ensure the following:
1.Prompt detection of infectious patients
2.Airborne precautions
3.Treatment of people who
have suspected or confirmed
TB disease
In order to be effective, the
primary emphasis of the TB
infection-control program
should be on achieving these
three goals.
Policies and procedures for
TB control should be developed, reviewed periodically,
and evaluated for effectiveness
to determine the actions necessary to minimize the risk for
transmission of M. tuberculosis
in all healthcare settings.
Overview of TB infection
prevention and control
measures
The TB infection-control program should be based on a
three-level hierarchy of control
measures and include6:
1.Administrative controls
2.Environmental controls
3.Use of respiratory protective
equipment
Infection prevention and
control ad minist rat ive
Figure 1: MDR-TB occurs when a Mycobacterium tuberculosis strain is resistant to isoniazid and rifampin, two of the most powerful first-line drugs. To cure MDR-TB, healthcare providers must turn to a combination of second-line drugs, several of which
are shown here. Second-line drugs may have more side effects, the treatment may last much longer, and the cost may be up
to 100 times more than first-line therapy. MDR-TB strains can also grow resistant to second-line drugs, further complicating
treatment.4 ILLUSTRATION CREDIT: NATIONAL INSTITUTE OF ALLERGY AND INFECTIOUS DISEASES (NIAID). ILLUSTRATOR: KRISTA TOWNSEND.
controls include the following activities:
• A ssigning responsibility for
TB infection-control in the
setting
• Conducting a TB risk assessment of the setting
• Developing and instituting a
written TB infection-control
plan to ensure prompt detection, airborne precautions,
and treatment of persons who
have suspected or confirmed
TB disease
• Ensuring the timely availability of recommended laboratory processing, testing, and
reporting of results to the
ordering physician
• Implementing effective work
practices for the management
of patients with suspected or
confirmed TB disease
• Ensuring proper cleaning and
sterilization or disinfection
of potentially contaminated
equipment (e.g., bronchoscopes, endoscopes)
• Training and educating
healthcare personnel (HCP)
regarding TB, with specific
focus on prevention, transmission, and symptoms
• S creening and evaluating
HCP who are at risk for
TB disease or who might be
exposed to M. tuberculosis
• A pplying epidemiologicbased prevention principles,
including the use of settingrelated infection control
data
• Using appropriate signage
advising respiratory hygiene
and cough etiquette
• Coordinating efforts with the
local or state health department
The environmental controls
listed below are used to prevent
transmission and reduce the
concentration of infectious
droplet nuclei in ambient air:
• P rimary environmental
controls restrict the source
of infection by using local
exhaust ventilation (e.g.,
hoods, tents, or booths) and
dilute and remove contaminated air by using general
ventilation.
• S econdary environmental
controls control the airflow to
prevent contamination of air
w w w.apic.org | 31
PREVENTION IN ACTION
2013 TB diagnosis update
Rapid diagnosis and treatment of TB is a major breakthrough
to prevent further infections.
In July 2013, the U.S. Food and Drug Administration (FDA)
allowed marketing of the Xpert MTB/RIF Assay, the first FDAreviewed test that can simultaneously detect bacteria that cause
tuberculosis (TB) and determine if the bacteria contain genetic
markers that makes them resistant to rifampin, a first-line
drug in the treatment of TB.
The new test is less complex to perform than other previous
FDA-cleared tests for the detection of TB bacteria. Test results,
including the detection of TB bacteria and whether the bacteria
are drug resistant, are available in approximately two hours.
Traditional methods to detect multidrug-resistant TB usually
require one to three months.8
in areas adjacent to the source
(airborne infection isolation
[all] rooms).
32 | WINTER
2013 | Prevention
638106_Nanosonics.indd
1
• C lean the air by using
high efficiency particulate air (HEPA) filtration,
or ultraviolet germicidal
irradiation.
Use of respiratory protection equipment can further
reduce risk for exposure of HCP
to infectious droplet nuclei that
have been expelled into the air
from a patient with infectious TB
disease. The following measures
can be taken to reduce the risk
for exposure:
• Implementing a respiratory
protection program; N95 respirator training and use
• Training HCP on respiratory
protection
• Training patients on respiratory hygiene and cough etiquette procedures
Transmissibility of TB
appears to decline rapidly after
adequate treatment is started;
how quickly this occurs
varies from patient to patient.
Patients can be considered noninfectious when they meet all
of the following criteria:
1.They have been receiving adequate treatment for two weeks
or longer.
2.Their symptoms have improved
(e.g., they are coughing less and
no longer have a fever).
3.They have THREE consecutive negative sputum smears
from sputum collected in eightto 24-hour intervals (at least
one being an early morning
specimen).6
Infection prevention and
diagnostic testing
The Mantoux tuberculin skin test
(TST) is the standard method of
determining whether a person
is infected with Mycobacterium
18/04/13 6:09 AM
tuberculosis. Reliable administration and reading of the TST
requires standardization of procedures, training, supervision,
and practice. Results can be
obtained 48 to 72 hours after
inoculation, previous vaccination
with the BCG vaccine can cause
false positive results.7
Interferon-Gamma Release
Assays (IGRAs) are whole-blood
tests that can aid in diagnosing Mycobacterium tuberculosis
infection. They do not help
differentiate latent tuberculosis
infection (LTBI) from tuberculosis disease. Two IGRAs that
have been approved by the U.S.
Food and Drug Administration
(FDA) are commercially available
in the U.S. Advantages include:
1) results within 24 hours; and
2) prior BCG (Bacille CalmetteGuérin) vaccination does not
cause a false-positive IGRA
test result.
1.QuantiFERON®-TB Gold
In-Tube test (QFT-GIT);
2.T-SPOT®.TB test (T-Spot)
The CDC recommends using
one test or the other, but not both
on the same patient.7
Summary
MDR-TB most commonly
develops in the course of TB
treatment regimens. Resistance
occurs when a physician prescribes inappropriate treatment
or patients miss doses or fail to
complete their treatment. MDR
tuberculosis is an airborne pathogen, so persons with active, pulmonary tuberculosis caused by
a multidrug-resistant strain can
transmit the disease by coughing.
Advancements and FDA approval
of diagnostic testing has aided
the identification and treatment
of MDR-TB within hours rather
than months, a major infection
prevention development.
Irena Kenneley, PhD, APRN-BC,
CIC, is assistant professor at Case
Western Reserve University, Frances
Payne Bolton School of Nursing in
Cleveland, Ohio.
References
1.WHO March 2013. Multidrug-resistant tuberculosis (MDR-TB). Site accessed October 6,
2013: www.who.int/tb/challenges/mdr/en/.
2. Strelkauskas A. (2009). Microbiology: A Clinical
Approach. ISBN-10: 0815365144 | ISBN-13:
978- 0815365143.
3. CDC (2012). Treatment of Tuberculosis (2003).
Site accessed October 6, 2013: www.cdc.gov/
tb/publications/slidesets/Treatment_Guidelines/2003/default.htm.
4.National Institutes of Allergy and Infectious
Disease (2007). Scientific Illustrations of
Drug-Resistant TB: Multidrug-Resistant TB
(MDR-TB) and Possible Effective Treatments.
Site Accessed October 6 2013: www.niaid.
nih.gov/topics/tuberculosis/Understanding/
WhatIsTB/ScientificIllustrations/pages/multidrugresistantillustration.aspx.
5. CDC, American Thoracic Society and Infectious Disease Society of America (2011).
Recommendations for use of an isoniazidrifapentine regimen with direct observation to
treat latent Mycobacterium tuberculosis infection. MMWR Morb Mortal Wkly Rep. 2011 Dec
9;60(48):1650–3.
6. CDC. Guidelines for preventing the transmission
of Mycobacterium tuberculosis in health-care
settings, 2005. MMWR 2005; 54(No. RR-17).
Site Accessed October 6, 2013: www.cdc.gov/
tb/publications/factsheets/prevention/ichcs.
htm.
7. CDC (2010). Updated Guidelines for Using Interferon Gamma Release Assays to Detect Mycobacterium tuberculosis Infection-United States,
2010. MMWR; June 25, 2010 / 59(RR05);125. Site Accessed October 6, 2013: www.
cdc.gov/mmwr/preview/mmwrhtml/rr5905a1.
htm?s_cid=rr5905a1_e.
8. Food and Drug Administration (2013). FDA
permits marketing of first U.S. test labeled for
simultaneous detection of tuberculosis bacteria
and resistance to the antibiotic rifampin. U.S.
Food and Drug Administration, released July
25, 2013. Site Accessed October 6, 2013:
www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm362602.htm.
9. CDC (2013). Provisional CDC Guidelines for
the Use and Safety Monitoring of Bedaquiline Fumarate (Sirturo) for the Treatment of
Multidrug-Resistant Tuberculosis. MMWR
Division of Tuberculosis Elimination, National
Center for HIV/AIDS, Viral Hepatitis, STD, and
TB Prevention, CDC. Recommendations and
Reports October 25, 2013 / 62(rr09);1-12.
Site accessed October 26, 2013: www.cdc.
gov/mmwr/preview/mmwrhtml/rr6209a1.
htm?s_cid=rr6209a1_e.
662823_JanPak.indd 1
w w w.apic.org
10/10/13| 33
10:06 AM
PREVENTION IN ACTION
Ready, set,
implement!
Guided by the principles of implementation science, a team of nurses develops
an innovative nurse-driven Foley catheter protocol to prevent CAUTI.
By Brooke Buras, RN, BSN
A
fter reading the fall 2012 edition of Prevention
Strategist, some ambitious and eager nurses
were inspired to develop an innovative, nursedriven Foley catheter protocol at North Oaks Medical
Center, a 330-bed, acute care facility in Hammond,
Louisiana.
The focus of an article on
a patient-centered approach
to preventing catheter-associated urinary tract infections
(CAUTIs) captured the nurses’
interest. Ultimately, a CAUTI
Reduction Team was established at North Oaks as part
of the facility’s participation in
the Centers for Medicare and
Medicaid Services Partnership
for Patients Campaign.
With infection prevention
leading the team and a nursing
representative from each major
patient care area as members,
the team decided that developing a nurse-driven Foley catheter removal protocol would
be the best strategy to decrease
device days and prevent infections. Prompt removal of the
Foley catheter remains a core
preventative measure, as recommended by the Centers for
Disease Control and Prevention
(CDC).1
Getting started
Members of the CAUTI team provide individualized education to ensure all questions
and/or concerns are addressed. LEFT TO RIGHT: CAUTI team member Jessica Purvis
and staff nurse Nicole Milazzo.
34 | WINTER 2013 | Prevention
After three months of research,
multidisciplinary collaboration,
partnering with the medical
staff, and several revisions, an
evidenced-based, nurse-driven
Foley catheter removal and postFoley catheter removal protocol
was approved by the Medical
Executive Committee for use
at North Oaks Medical Center
(Fig. 1 and 2).
A nurse now has the autonomy, as granted by the medical
staff, to remove a Foley catheter,
barring specific criteria outlined
in the protocol. Additionally, the
nurse can perform one straight
catheterization if the patient has
not voided within the determined timeframe. This places
North Oaks in the small percentage of U.S. hospitals that
use evidenced-based practice to
monitor Foley catheter duration
and/or discontinuation to help
prevent CAUTIs.2, 3
As the team leader of the
CAUTI team, I label the two
protocols “mutts” because they
were devised using multiple
resources, including the publications Prevention Strategist,
American Journal of Infection
Control, and Journal of Nursing
Care Quality; guidance from
eQ Health Solutions and
the Institute for Healthcare
Improvement; and input from
North Oaks’ own nurses and
physicians.
I alluded to Neil Armstrong’s
famous quote, “This is one small
step for man, one giant leap for
mankind,” when informing
team members, nursing leadership, and staff of the Medical
Executive Committee’s decision to approve the protocol.
The protocol is a triumph for
North Oaks because it facilitates
nurse empowerment by granting
After a team meeting, some members of the CAUTI team show their team spirit. LEFT TO RIGHT: Brooke Buras, Tammy Murphy, Edna Scott, Melissa Fisher, Jessica Purvis,
and Amanda Hecker.
autonomy and represents true
multidisciplinary collaboration
to incorporate evidence and
research into practice. In addition, it helps the hospital prevent
healthcare-associated infections
(HAIs) and reach the ultimate
goal of providing patients with
the best care possible.
Implementation
Using the quality improvement
methodology of rapid-cycle
change (introduced to the team
by the Partnership for Patients
Campaign) and implementation science, the team was
able to expedite change that
yielded reliable results. Rapidcycle methodology uses the
traditional Plan-Do-Study-Act
(PDSA) cycle to facilitate rapid
improvement. PDSA guided
the team to test interventions
on small scales. If the intervention provided favorable results,
then the change was applied to
a larger population.4 Directly
applying the PDSA cycle, the
two nurse-driven protocols were
first introduced to the hospital’s
three surgery units. Within a
month, those units’ device days
decreased significantly. The next
month it was rolled out to the
remaining seven nursing units.
Implementation of the two
nurse-driven protocols proved
to be a challenge for the CAUTI
team. Developing the protocols and obtaining approval for
utilization was the easy part.
Educating the nursing staff on
the appropriate use of the protocols and helping them feel comfortable having the autonomy to
employ them continues to be the
most challenging aspect for the
CAUTI reduction team.
Implementation science
guided the team, as it accomplished the monumental task of
properly putting the protocols
into action. Implementation
science is an action-oriented
model, as well as a clinical and
a social specialty, and provides
an operational framework for
the systematic uptake of this
evidence-based intervention into
healthcare practice.5 It includes
the four “Es”: engage, educate,
execute, and evaluate.
Engage
During the whirlwind of tasks
and responsibilities in a shiftlong tornado, it is challenging
to adjust nursing priorities.
Infection preventionists and
administrative personnel alike
often wonder: “What else can
be done to engage employees so
they will give an issue the attention it requires?”
The answer to that question
is very simple. Engagement
should come from an internal
source in a patient care area. It’s
vital to have a competent, determined team to lead by example.
Those informal leaders on the
units will facilitate a sustained,
meaningful change.
Engagement was accomplished by obtaining a crew
of high performers who were
well-respected by their peers.
Real-life stories about how a
CAUTI affected a patient’s life
were shared with the crew, followed by practical suggestions to
decrease infections. Teamwork
flourished thereafter, dramatically increasing the frequency
of desired results. Consequently,
the critical part of this step is
to successfully engage the team
members. Once members of the
team realize the vital nature of
the subject matter, they will
act as role models in delivering
excellent care, and peers will follow suit.
w w w.apic.org | 35
PREVENTION IN ACTION
Updated 4/13
FOLEY CATHETER REMOVAL PROTOCOL:
Removal Protocol
To be addressed daily on all patients with Foley catheters
No
Does the patient have an
indwelling Foley that has
been in longer than 24
hours?
•
•
•
Continue to assess
daily. Document
reason for
continuing Foley
catheter.
•
Yes
•
•
Yes
Does the patient meet
criteria to justify
continuing the Foley?
See chart A.
Continue to assess
daily. Document
reason for
continuing Foley
catheter.
•
•
•
•
No
Does the patient meet
criteria for removal,
when applicable?
See chart B.
No
Continue to assess
daily. Document
reason for
continuing Foley
catheter.
•
Chart A
Criteria for Continuing Foley Catheter
Known or suspected urinary tract obstruction
Neurogenic bladder dysfunction
Recent urologic surgery, bladder injury, pelvic surgery, or recent
surgery involving structures contiguous with the bladder or
urinary tract, after pelvic surgery (e.g., GYN, colorectal)
Other post surgical procedure—with an order stating do not
remove Foley
Urinary incontinence in the patient with Stage III or Stage IV
pressure ulcers on the trunk, perineal wounds, necrotizing
infections
Need for accurate measurement of urinary output in a critically
ill patient, patient undergoing aggressive diuresis, or presence
of renal impairment (unless patient is able to cooperate with
strict output monitoring—can use a bed pan or commode)
Gross hematuria in patients with potential clots (for irrigation)
Epidural catheter still in place
Palliative care for terminally ill
Foley placed within 24 hours
Execute
Chart B
Criteria for Removal by RN (when applicable)
Patient is awake, alert, and oriented or is at baseline mental
capacity. Verbally expresses no trouble voiding before the
catheter was placed or return to baseline urinary status (i.e.,
incontinent before Foley was placed)
•
If surgical procedure, patient able to comfortably use a bed
pan/commode which will not interfere with intent of
procedure
•
Order for strict output monitoring is discontinued, or the
patient is able to cooperate with strict output monitoring
•
Epidural catheter is removed
Note: A physician order is required for discontinuing Foley in patients who have
had a recent urologic surgery, bladder injury, pelvic surgery, and/or recent
surgery involving structures contiguous with the bladder or urinary tract.
Yes
RN may remove Foley—before 7 a.m. is most optimal time
.
Removal Reason: Per protocol. Follow post-catheter removal
protocol.
FIGURE 1
Educate
Some nurses know the appropriate indications for and
timeframe to maintain a Foley
catheter, but is this common
knowledge among all nurses?
Healthcare reform has placed
increasing strain on America’s
bedside caregivers, increasing
patient-to-nurse ratios and
pressure related to performance-based reimbursement.
All nurses should realize that
their actions (and omissions)
could impact patient mortality. With those issues in mind,
the CAUTI team decided to
carry out a massive educational
agenda to ensure that everyone
was aware of CAUTI prevention. Initially, team members
attended each nursing unit staff
meeting to promote CAUTI
awareness. Additionally, they
attended conferences to explain
the newly approved nursedriven protocols. They also
provided individualized education for each day and night shift
to ensure all questions were
36 | WINTER 2013 | Prevention
addressed and to discuss realtime scenarios. Every unit knew
its CAUTI team representative
and what actions to take if there
was confusion when exercising
protocols.
POST-CATHETER REMOVAL PROTOCOL:
Post-Removal Protocol
Has the patient voided
within 6 hours after
removing the Foley?
For all patients when a Foley catheter is removed
Yes
Does the patient appear
comfortable and doesn’t
express a desire to void?
No
No
See chart A.
Has the patient voided
within 4 hours after
straight catheterization?
Yes
Continue to monitor
patient comfort and
for retention.
FIGURE 2
Execution occurs when evidenced-based interventions are
converted into practice. The
CDC recommends using a
combination of core prevention
strategies.1 One of these methods includes leaving a catheter
in place for short periods of
time (with regard to medical
necessity, as opposed to nursing convenience) to minimize
infection risks.1 The nurse-driven
Foley catheter removal protocol allows nurses to determine
the need for the Foley catheter
on a daily basis and remove it
promptly when it is no longer
necessary. Furthermore, the
No
Notify
physician.
Continue to monitor
patient comfort and
for retention.
Chart A
Do a bladder scan.
If bladder scan volume is <400 ml and the patient is
comfortable and does not express a desire to void,
encourage oral fluid intake (unless contraindicated) and
repeat bladder scan in 2 hours.
If bladder scan volume is 400-600 ml the RN will first
ensure position of the patient allows comfortable voiding if
applicable (standing, sitting up). Reassess in 2 hours. If the
patient is not able to void, perform a straight
catheterization. See 2 bullets below.
If bladder scan volume is >600 ml, perform a straight
catheterization.
• Document bladder scan volume in the Intake/Output
Flowsheet under group: Urine Assessment.
• If straight cath performed, document volume in the Intake/
Output Flowsheet under group: Urine Assessment.
Document patient tolerance as a Progress Note, Service:
Nursing.
*A bladder scan should be done for any of the following:
patient is uncomfortable at anytime, whether voiding or not,
patient has an urge to void but is unable to do so,
patient is incontinent at any time (that is not baseline).
Call to action
Regular updates on progress facilitated and sustained team engagement. LEFT TO
RIGHT: CAUTI team members Brooke Buras, Tammy Murphy, Edna Scott, Melissa
Fisher, Jessica Purvis, and Amanda Hecker.
Engaging bedside caregivers, increasing CAUTI awareness,
executing evidenced-based interventions, and continuously
evaluating progress—along with using rapid-cycle methodology—resulted in a massive culture change at North Oaks
Medical Center.
In summary, here are five tips that will be useful in implementing a nurse-driven Foley protocol:
Seek team members who are highly engaged to act as role
models for delivering excellent care.
Determine a framework/model to guide implementation.
Rapid-cycle methodology and implementation science can
be applied to many HAI prevention strategies.5
Ensure that communication with team members and healthcare workers is clear and concise. When expectations are
well defined, courses of action are easy to follow.
Provide multiple opportunities for education. Visit staff meetings and individual shifts, and employ passive education
strategies (e.g., poster boards and computer-based learning) to
allow individuals to learn at their own pace.
Have a mechanism for staff to provide feedback and follow up on a routine basis. Education should be ongoing
and resources should be available if staff has questions and/or
concerns along the way.
1
2
3
4
5
Real patient scenarios are discussed to enhance applicable knowledge of the nursedriven Foley removal protocols. LEFT TO RIGHT: CAUTI team members Amanda
Hecker, Jessica Purvis, Melissa Fisher, and Edna Scott. Brooke Buras is seated.
criteria for continuing use of a
Foley catheter outlined in the
protocol serves as a guide for
appropriate placement. The
basics of preventing CAUTIs
were reinforced—inserting
catheters using aseptic technique
and proper maintenance of the
urinary catheter.1 Also, the team
used a Foley catheter securement
device, which the CDC also considers a core prevention strategy.1
Catheter securement is important to prevent catheters from
exerting excessive force on the
bladder neck or urethra, causing
inflammation.6, 7
Evaluate
The team chose infection
rates as an outcome measure
because the CDC provides
standardized, scientifically
rigorous definitions.
The nurse-driven Foley
catheter removal protocols
were first implemented in
February 2013, and within
months North Oak’s CAUTI
infection rates plummeted.
The hospital’s 2013 CAUTI
rate is projected to fall close to
the National Healthcare Safety
Network’s (NHSN) 10th percentile, with the ultimate goal
of zero infections. Surgical
Care Improvement Project
statistics and Partnership for
Patients comparative data are
also evaluated to determine
progress and are shared with
the team and other administrators on a monthly basis. After
the nurse-driven protocols were
implemented, the CAUTI team
served as a resource to the staff
and accepted positive and negative feedback. Future team
goals relate to continuously
evaluating current processes,
as well as validating that staff
are inserting catheters aseptically and monitoring duration and/or discontinuation
of Foley catheters.
Brooke Buras, RN, BSN, is an infection prevention surveillance nurse
at North Oaks Health System in
Hammond, Louisiana.
References
1. Gould CV, Umscheid CA, Agarwal RK, Kuntz
G, Pegues DA, and HICPAC. Guideline for Prevention of Catheter-associated Urinary Tract
Infections 2009. Available at: www.cdc.gov/
hicpac/cauti/001_cauti.html. Accessed July
1, 2013.
2.Krein SL, Kowalski CP, Hofer, TP, Saint, S. Preventing Hospital-Acquired Infections: A National
Survey of Practices Reported by U.S. Hospitals
in 2005 and 2009. Journal of General Internal
Medicine 2012; 27: 773-779.
3. Saint S, Kowalski CP, Kaufman SR, Hofer TP,
Kauffman CA, Olmsted RN, Forman J, Banaszak-Holl J, Krein SL. Preventing hospitalacquired urinary tract infection in the United
States: a national study. Clinical Infectious
Diseases 2008; 46: 243-250.
4. Brown P, Hare D. Rapid cycle improvement:
Controlling change. The Journal. 2002; 98:
2-3. Available at: www.ashp.org/DocLibrary/
Policy/QII/Rapid-Cycle.aspx. Accessed July 1,
2013.
5. Saint S, Howell JD, Krein SL. Implementation
Science: How to Jumpstart Infection Prevention. Infection Control and Hospital Epidemiology
2010; 31(Suppl 1): S14-S17.
6.Wound, Ostomy and Continence Nurses Society. Indwelling Urinary Catheter securement:
Best practice for clinicians.2012. Available at:
www.faet.org/docs/IndwellingUrinaryCatheterSecurement.pdf. Accessed July 1, 2013.
7. Oman KS, Flynn MB, Fink, R, Schraeder N,
Hulett T, Keech T, Wald H. Nurse-directed
interventions to reduce catheter-associated
urinary tract infections. American Journal of
Infection Control 2012; 40: 548-553.
w w w.apic.org | 37
Association for Professionals in
Infection Control and Epidemiology
PREVENTION IN ACTION
Facility emergency
preparedness
starts at home
BY STEVE HILLEY, RN
W
hen it comes to infection prevention, don’t
overlook the basics. Emergency preparedness doesn’t start at the healthcare facility;
it starts at home. While every healthcare facility needs
an emergency preparedness plan, the plan is not complete if healthcare administrators overlook the personal
safety and security of each employee and their families.
It sounds obvious, but facility staff must be prepared
at home because emergency preparedness plans require
employees to come into the facility during disasters. It’s
vital to assist colleagues in preparing for disasters—more
specifically, preparing staff for an event where they feel
comfortable leaving their family safe and secure at home.
Without that sense of comfort, staff may not come into
the healthcare facility to assist in community response
during an emergency or disaster.
Staff show off their 10-gallon bins/totes used to build their own home emergency
preparedness kits.
You’ve heard it before—emergencies can strike anytime, anywhere. Without warning, your
community can be left without
power, water, sanitation, and
communications. Being prepared for disasters takes time
and resources. The most basic
element of preparedness starts
with a home emergency preparedness kit.
miles from Denver and 150 miles
from Grand Junction, resources
can be scarce—especially during a disaster. When internal or
external disasters occur, healthcare facilities in rural communities must be self-sustaining for
at least 96 hours. After YVMC
conducted an informal study on
home emergency preparedness
among employees, it concluded
Although many Yampa Valley
Medical Center (YVMC) staff
members have attended workshops that stress the importance
of having an emergency preparedness kit at home, it previously didn’t have any data about
how many employees actually
created a home kit. Because
YVMC is situated in Northwest
Colorado, approximately 150
that only about 5 percent of the
staff had an adequate personal
emergency preparedness kit at
home or in their car. Thus, part
of YVMC’s emergency preparedness plan included assisting its
employees with their personal
emergency preparedness.
To prepare its staff, YVMC
started with a basic one-day
employee safety fair in 2000.
w w w.apic.org | 41
PREVENTION IN ACTION
LEFT: Glenn Sommerfeld and Steve Hilley assemble a personal home emergency preparedness kit. RIGHT: Staff during the YVMC Safety Fair, where employees are rewarded
with first aid kits, small emergency preparedness kits, and other gifts of appreciation.
Resources to
help build a
home emergency
preparedness kit
• www.ready.gov/be-informed
• www.ready.gov/make-a-plan
• www.ready.gov/build-a-kit
• www.ready.gov/get-involved
• For monthly preparedness text
messages, text PREPARE to
43362 (4FEMA) to receive preparedness tips (message/data
rates apply).
•To order publications, call
800-BE-READY, 888-SE-LISTO,
and TTY 800-462-7585.
The goal of the fair is to help
educate and equip staff to be
trained members of the community—not victims. YVMC
recruits vendors from the community to assist with training
and education needs. For example, YVMC has organized the
sheriff’s office to advise on firearms safety, the fire department
to train on fire extinguisher use,
local bike shops to teach bike
safety, public health partners
to educate about emergency
preparedness, the dangers of
texting/drinking and driving,
and more. During its safety fairs,
YVMC rewards employees with
first aid kits, small emergency
preparedness kits, and other
gifts of appreciation.
The Federal Emergency
Management Agency (FEMA)
declared September 2013
as Emergency Preparedness
Month. In honor of Emergency
Preparedness Month, the
focused goal of this year’s safety
fair was to assist staff in building
their own home emergency preparedness kits. YVMC invited
vendors from all over the county
to educate staff on emergency
preparedness, influenza, fire
extinguisher use, interpretation
services, clear text/review of
internal emergency codes, N95
respirator fit-testing, biohazard
waste disposal, MRI safety,
as well as topics covered from
previous years (e.g., effects of
drinking and driving, and firearm safety).
This year, when an employee
signed in to the fair, he/she
received a 10-gallon tote with
lid. Y VMC chose this size
because of its portability for
One case of Legionnaires’ disease is one too many.
PROTECT YOUR PATIENTS.
PARTNER WITH
THE LEGIONELLA EXPERTS®.
Clinical and environmental
expertise in Legionella,
detection, control and
remediation.
877-775-7284 | WWW.SPECIALPATHOGENSLAB.COM
42 624296_Special.indd
| WINTER 2013 1| Prevention
17/01/13 7:52 PM
both the car and at home.
After receiving their tote, they
proceeded into the conference rooms where the vendors
were set up. Each vendor give
a brief five- to 10-minute presentation. After each presentation, they give out one small
component for the home preparedness kit. The items of this
year’s kit included a fire starter,
bottles of water, matches in a
waterproof container, a whistle,
nylon rope, an emergency blanket, paper towels, toilet paper,
and a small mirror. It’s important to note that this event
was not intended to produce a
complete emergency preparedness kit; it was intended to
assist staff in starting to build
their kits. Y VMC encouraged all the staff to complete
their kits and included a list
of other items needed for the
kit. To continue engagement
after the event, YVMC held a
contest for the best completed
home emergency preparedness
kit. Employees could send in
a photo of their finished kits
and whoever had the best kit
was awarded a prize.
This year’s safety fair was a
huge success. The staff truly
enjoyed the hands-on interaction with the vendors and
building their own kits. YVMC
strives to prepare its staff for
disasters and emergencies.
Because of YVMC’s physical
location, it can be limited in
its access to resources; thus, the
concept of “self-help” is considered paramount.
Steve Hilley, RN, is emergency
preparedness coordinator/infection
preventionist for Yampa Valley
Medical Center in Steamboat Spring,
Colorado. He is also chair of the APIC
Emergency Preparedness Committee.
PATIENT SAFE SYRINGE
®
SYRINGES
DESIGNED TO
PROTECT PATIENTS
Patient Safe ® syringes are
uniquely designed to reduce the
risk of bloodstream infections resulting
from catheter hub contamination
Patient Safe ® Syringes do not transfer
contaminants to luer-activated
valves or patients
Unique luer guard reduces the risk of
luer tip contact contamination.
Standard syringes transfer
contaminants to luer-activated
valves and intravenous fluid
Compatible with most available hypodermic
needles, including those with manually
activated safety features, vial access devices,
and luer-activated catheter hubs.
Reduces the risk of medication contamination.
Patient Safe® Syringe
NEW! See our website for additional sizes.
®
511 Lobo Lane U Little Elm, Texas U 75068-0009
Tel: (972) 294 -1770 UÊÊFax: (972) 294-4400
Toll Free: 1-888-703-1010
USA/Canada: rtisales@vanishpoint.com
International: rti.intl@vanishpoint.com
PREVENTION IN ACTION
Collaboration in
infection prevention
Infusion nurses and infection preventionists.
BY MARY MCGOLDRICK, MS, RN, CRNI ®
I
nfusion nurses and infection preventionists (IPs) both share a mutual goal of
preventing patient infections in all care settings and in all patient populations;
however, the role of the IP is much broader in its scope and requires a more
extensive body of knowledge to prevent a broader spectrum of patient infections
(e.g., catheter-associated urinary tract infections [CAUTI], surgical site infections
[SSIs], central line-associated bloodstream infections, ventilator-associated pneumonia). The infusion nurse’s role is typically much narrower in focus and limited
to preventing infections associated with the insertion, use, and management of a
myriad of intravascular devices. This article will focus on the role of the infusion
nurse and the IP, and how they can work together in a collegial, collaborative
manner to achieve their mutual goal of preventing patient infections.
CRNIs® and CICs®: Partners in
preventing infections
Infusion Nurses
Certification Corporation
Chair Mary McGoldrick,
MS, RN, CRNI®
44 | WINTER 2013 | Prevention
Just like not all IPs are CICs,
not all infusion nurses are
CRNIs (Certified Registered
Nurse Infusion)… unfortunately. Certification, like the
CRNI and CIC designation,
is an earned credential that
demonstrates an individual’s
specialized knowledge, skills,
and experience and is awarded
by a third-party, nongovernmental entity, such as the
Infusion Nurses Certification
Corporation (INCC) for the
CRNI and the Certification
Board of Infection Control
and Epidemiology (CBIC),
for the CIC. The CRNI is
the only nationally recognized
and accredited certification in
infusion nursing. Like the CIC,
certification candidates receive
their CRNI credential only after
meeting strict eligibility criteria
and successfully completing a
150-question standardized exam
that is based on the following
eight core areas: 1) Technology
and Clinical Applications; 2)
Fluid and Electrolyte Therapy;
3) Pharmacology; 4) Infection
Prevention; 5) Antineoplastic/
Biological Therapy; 6)
Parenteral Nutrition; 7) Special
Populations; and 8) Transfusion
Therapy. Note that one of the
core areas on the CRNI exam
is infection prevention, which
overlaps with the body of knowledge and focus of that of an IP.
Incorporating standards
into practice
IPs and infusion nurses know
that patient care practices are
to be based on evidence-based
guidelines to reduce the risk
of vascular access device-associated infections. Evidencebased guidelines include the
Centers for Disease Control
and Prevention’s (CDC) 2011
Guidelines for the Prevention of
Intravascular Catheter-Related
Infections 1 (both INS and APIC
collaborated with the CDC on
its development), as well as the
Infusion Nurses Society’s (INS)
Infusion Nursing Standards of
Practice (Fig. 1).2 APIC also has a
position paper on safe injection,
infusion, and medication vial
practices in healthcare, which
provides practice guidance.3
INS’ Infusion Nursing
Standards of Practice provides
the framework that guides clinical practice in infusion nursing
and is applicable in all care settings and addresses all patient
populations. In the latest edition of the Infusion Nursing
Standards of Practice, the practice criteria are supported by
the latest available research and
ranked by the strength of the
body of evidence. The ranking
“The knowledge and research in the
field of preventing infections in patients
with intravascular infections is growing
and will continue to evolve.”
FIGURE 1: Infusion Nursing Standards of Practice.
system identifies the level of
evidence and research that supports each of the practice criteria. The rankings range from
Level I, which includes metaanalyses, systematic literature
reviews, and guidelines based
on randomized controlled trials,
to Level V, which includes clinical articles, consensus reports,
and generally accepted practices.
As both IPs and infusion nurses
strive to prevent infections and
meet the infusion needs of their
patients, the Infusion Nursing
Standards of Practice can be
an invaluable guide for decision making and developing a
patient-centered plan of care.
Infusion nursing and IPs
Infusion nursing has become
a highly specialized practice,
with procedures ranging from
inserting a peripherally inserted
central catheter in a healthcare
facility to teaching a patient and
his or her caregiver how to set up
and self-administer parenteral
nutrition in the home setting.
The infusion nurse can assist the
IP in preventing vascular access
device-associated infections by:
1.Providing consultation and
serving as a resource person
(in collaboration with the IP)
on patient care practices;
2.Providing educational programs that include both
didactic and interactive
components for those staff
who insert and maintain
peripheral and central venous
catheters;
3.Participating in competenceassessment activities;
4.Allowing the IP to focus limited infection prevention and
control resources on other
priority-directed surveillance
activities;
5.Writing, reviewing, and/or
approving infusion-related
policies and procedures; and
6.Offering input in analysis of
patient surveillance data collected, and as needed, actionplanning activities.
Infusion nurses and IPs have
successfully collaborated in
specific clinical scenarios (e.g.,
validating effective vascular
access device insertion practices,
selecting skin antisepsis products). This collaborative effort
is supported by the CDC’s 2011
Guidelines for the Prevention of
Intravascular Catheter-Related
Infections, as it states: “to
improve patient outcomes and
to reduce healthcare costs, there
is considerable interest…in
reducing the incidence of these
infections. This effort should
be multidisciplinary, involving
healthcare professionals who
order the insertion and removal
of CVCs, those personnel who
insert and maintain intravascular catheters, infection control
personnel… and those who allocate resources… Specialized ‘IV
teams’ have shown unequivocal effectiveness in reducing the
incidence of CRBSI [catheterrelated bloodstream infections],
associated complications, and
costs.”1
The knowledge and research
in the field of preventing infections in patients with intravascular infections is growing and
will continue to evolve as we
collect and publish research and
outcome data, which ultimately
affects patient care practices and
outcomes. It is together, in collaboration with infusion nurses
and IPs, that we can truly meet
our mutual goal of zero patient
infections!
Mary McGoldrick, MS, RN,
CRNI®, is chair, Infusion Nurses
Certification Corporation, in Norwood,
Massachusetts.
References
1. Centers for Disease Control and Prevention.
2011 Guidelines for the Prevention of Intravascular Catheter-Related Infections. www.cdc.gov/
hicpac/bsi/bsi-guidelines-2011.html. Accessed
September 24, 2013.
2. Infusion Nurses Society. (January/February
2011). Infusion Nursing Standards of Practice.
Journal of Infusion Nursing, 34(suppl. 1S). www.
ins1.org/i4a/pages/index.cfm?pageid=3310.
3. Dolan, S., Felizardo, G., Barnes, S., Cox, T., Patrick, M., Ward, K., et al., (2010). APIC position
paper: Safe injection, infusion, and medication
vial practices in health care. American Journal
of Infection Control. 38:167-72. http://apic.
org/Professional-Practice/Practice-Resources/
Position-Statements. Accessed September 24,
2013.
w w w.apic.org | 45
Peace of Mind in Just 1-Minute
and
You stand between infection and the people you care about.
You can trust CaviCide1™ and CaviWipes1™ to stand with you.
Only one brand provides a 1-minute kill time on all product labeled
organisms, including TB, and excellent materials compatibility.
Go to Metrex.com/Prevent
and get started on the road
to become a black belt ninja.
SURFACE DISINFECTANTS TRUSTED BY
220,000 HEALTHCARE FACILITIES
©2013 Metrex Research. All rights reserved. CaviWipes1 and CaviCide1 are trademarks of Metrex Research, LLC.
PLCO 2013-06-0014
PREVENTION IN ACTION
Centralized sterile
processing in
ambulatory facilities
Recommendations and resources to implement a safe, economic,
and efficient centralized sterile processing program.
BY JODY CHURCH, RN, CPNP, AND MARTHA YOUNG, BS, MS, CSPDT
T
he Association for the Advancement of Medical Instrumentation (AAMI)
recommends that “Whenever possible, centralized processing (i.e., decontamination, preparation, packaging, and sterilization processing in one
department) is encouraged and preferred over replicating this function in multiple areas for both safety and cost-effectiveness” (Section 3.1).1 It’s important to
understand the best way to design a centralized sterile processing area suitable for
ambulatory care settings and to offer ideas for workflow practices, equipment,
personal protective equipment (PPE), and transport of contaminated and sterilized instruments. The key is using resources with evidence-based, recommended
practices from AAMI and others to ensure safe and effective processing of reusable
medical devices in both ambulatory care and ambulatory surgery centers (ASCs).
Sterile processing
area design
When setting up a sterile processing area, consider the following questions:
• Is your site an office setting
or ASC?
• W hat types of procedures
will be done?
• W hat type of instruments
will be processed?
• W hat will the instrument
volume/workload be like?
The answers to these questions will guide you on how to
customize sterile processing for
your particular site.
A success story from
the field
Northeast Valley Health
Corporation (NEVHC) is a
Joint Commission accredited
ambulatory health center with
13 licensed sites in multiple
locations. In the past, reusable
instruments used for invasive
procedures were processed at
six separate sites. All procedures
such as ingrown toenail removal,
IUD insertion/removal, LEEP,
colposcopy, and dental extractions are done in exam rooms,
not operating rooms. In 2011,
The Joint Commission (TJC)
released findings related to
sterile processing, which illuminated pitfalls in the NEVHC
system. A number of weaknesses
helped drive the change to a centralized program: staff didn’t
have up-to-date sterile processing training; there was a lack
of supervision at each site; and
the busy clinical setting was not
optimal for correct processing to
be performed.
Organizations may resist
change and put up barriers to
implementing a new system. To
facilitate the transition to the
new program, NEVHC created
an action plan and timeline and
engaged key stakeholders in the
sterile processing program to
help nurture buy-in from resistant staff.
Finally, NEVHC emphasized
the safety and economic benefits
of centralization to justify the
change. They communicated
that the centralization would:
• A llow for consistent processing personnel
• Facilitate updated and ongoing training for staff
• Improve quality assurance
practices
w w w.apic.org | 47
PREVENTION IN ACTION
FIGURE 2: Wrapping/packaging and sterilizer stations at
an ambulatory care center.
FIGURE 1: Receiving, cleaning, milking, and drying stations
at an ambulatory care center.
• E
nhance ability for monitoring and supervision of staff
• Free up staff at local health
centers
The new process did accomplish all of the aforementioned
goals. It is possible to implement
a safe, economic, and efficient
centralized sterile processing
program. Just keep in mind
some important points.
Resources
To avoid taking risks in processing reusable medical devices,
ambulatory facilities must follow recommended practices and
standards. TJC National Patient
Safety Goal (NPSG) 07.05.01
advises developing policies and
procedures based on evidencebased guidelines to prevent surgical site infections.2
Healthcare organizations
should follow evidence-based
guidelines and recommended
practices published by AAMI,
the Association of periOperative
Registered Nurses (AORN), and
48 | WINTER 2013 | Prevention
the Centers for Disease Control
and Prevention (CDC).1, 3, 4 The
CDC’s 2011 Infection Prevention
Guide & Checklist for Outpatient
Settings is also very helpful.5, 6
In addition, the manufacturer’s
instructions for use (IFU) need to
be available and followed.
To obtain updated manufacturer’s IFU for instruments,
cleaning equipment, disinfectants, cleaning solutions,
packaging, and sterilization
equipment, check corporate
websites.
The ECRI Institute listed
inadequate reprocessing
of flexible endoscopes and
instruments for patient use
as hazard No. 8 on its “Top
Ten Technology Hazards for
2013.” 7 To improve processing of reusable endoscopes and
instruments, ECRI advises that
a facility should have adequate
space and equipment, and
trained staff, instructional
materials (e.g., IFU), resources
(e.g., A AMI ST79), and
sufficient instruments to meet
demand and allow adequate
time for processing.7 Now is the
time to collect data and ask for
additional resources to ensure
improvement of the processing
of reusable medical devices in
your facility.
AAMI ST79 states that all
staff who perform sterilization
processing activities should
be certified within two years
(Section 4).1 The Certification Board for Sterile Processing and Distribution, Inc.
(www.sterileprocessing.org),
and the International Association of Healthcare Central
Service Materiel Management
(www.iahcsmm.org) can provide additional information on
certification.
Workflow practices
Instrument flow in the processing area should be unidirectional
with clear transitions between
each process. Ambulatory facilities need stations for:
• Soiled receiving to one side of
sink(s)
• Washing (at least one sink)
• R insing (an additional/second
sink)
• Milking/lubrication
• Drying
• Wrapping/packaging
• Sterilization
Figure 1 shows an example
of receiving, cleaning, milking,
and drying stations at an ambulatory care center, and Figure 2
shows an example of wrapping/
packaging and sterilizer stations
at an ambulatory care center.
Summary of
recommended practices
Options for workflow practices
AAMI ST79 discusses the setup
of the processing area. Section
3.3.7.1 states, “Ideally, the area
in which instruments and other
devices are decontaminated
should be physically separated
from all other processing areas
and from areas in which clean
or sterile patient care procedures
“AAMI ST79 states that all staff who
perform sterilization processing activities
should be certified within two years
(Section 4).1 The Certification Board
for Sterile Processing and Distribution,
Inc., and the International Association
of Healthcare Central Service Materiel
Management can provide additional
information on certification.”
FIGURE 3: Bagged instruments that have
been placed into a puncture-resistant,
leak-proof, closable container, labeled as
biohazard.
are carried out.”1 For ASCs, the
only option is physical separation of decontamination and
clean areas. Because of limited
space, this may be a challenge
for an ambulatory care center.
TJC is concerned about droplet
contamination and ventilation.8
Ambulatory facilities could have
the option of placing a Plexiglas
divider next to the sink to ensure
that splashes, splatters, or droplets
from the decontamination area
do not enter the cleaning area.
AAMI ST79 Section 3.3.7.1
also states that in ambulatory clinics and dental or medical offices,
a procedural barrier separation
could be adequate “provided that
work practices prevent splashing,
the production of aerosols, and
the contamination of clean items
and work surfaces, and provided
that work practices promote the
changing of PPE [personal protective equipment] when personnel leave the decontamination
area and enter clean areas.”1 First,
clean the medical devices; next,
change PPE to package and sterilize the devices.
AAMI ST79 Section 3.3.7.1
states that decontamination
should preferably have a threesection sink; but if not, there
should be an adequate number
of sinks to accommodate concurrent soaking, washing, and
rinsing.1 Ideally, sinks should be
36 inches from the floor, eight
to 10 inches deep, and wide and
long enough to allow a tray or
container basket of instruments
to be placed flat for pretreatment
or manual cleaning.1 Sink inserts
are available to create two sinks
in one area or to place next to
one sink to create another sink.9
AAMI ST79 Section 7.5.4
states to use treated water (e.g.,
deionized, distilled, or reverse
osmosis) as the final rinse to prevent staining of instruments and
recontamination from tap water.1
Equipment
Readily available hand hygiene
dispensers (A AMI Section
3.3.6.8), installed emergency
eyewash/shower devices (Section
3.3.7.1, 3.3.8), and a variety
of brushes and other cleaning implements (Section 3.4,
7.5.3.2) are also needed in the
area.1 Make sure the sterilizers
are appropriately sized to accommodate your facility’s packaging types and instruments. Plan
ahead so there will be enough
sterilizer volume to meet instrument turnaround demands.
Personnel protective
equipment (PPE)
Section 4.5.2 of AAMI ST79
stipulates that the following PPE
should be worn while cleaning
instruments:
• Fluid-resistant masks to protect from splash and splatter
• Goggles or full-length face
shields to protect eyes against
liquid splashes, microorganisms, and chemicals (in addition to the masks)
• Liquid-resistant covering with
sleeves to protect from splash
Key points for
ambulatory
facilities
1. Follow the latest recommended practices when writing policies and procedures
in order to establish stateof-the-art sterile processing.
2. Follow the most up-todate IFU to ensure instruments are being effectively
processed.
3. Collect data to support
your requests for additional
resources (e.g., space,
equipment, instrumentation,
trained staff, and educational
material).
Resources are the key to
improving patient outcomes.
Patients are depending
on you.
w w w.apic.org | 49
PREVENTION IN ACTION
Access peer-reviewed articles on
sterile processing in the American
Journal of Infection Control
A multi-site field study evaluating the effectiveness of manual
cleaning of flexible endoscopes with an ATP detection system,
Marco Bommarito, Grace A. Thornhill, Dan J. Morse [June 2013 (Vol. 41, Issue
6, Supplement, Page S24, DOI: 10.1016/j.ajic.2013.03.049)]
Validation of adenosine triphosphate to audit manual cleaning
of flexible endoscope channels, Michelle J. Alfa, Iram Fatima, Nancy
Olson [March 2013 (volume 41 issue 3 Pages 245-248 DOI: 10.1016/j.
ajic.2012.03.018)]
The role of biofilms in reprocessing medical devices, Charles G.
Roberts [May 2013 (volume 41 issue 5 Pages S77-S80 DOI: 10.1016/j.
ajic.2012.12.008)]
Disinfection and sterilization: An overview, William A. Rutala, David
J. Weber [May 2013 (volume 41 issue 5 Pages S2-S5 DOI: 10.1016/j.
ajic.2012.11.005)]
High-level disinfection, sterilization, and antisepsis: Current issues
in reprocessing medical and surgical instruments, Rose Seavey [May
2013 (volume 41 issue 5 Pages S111-S117 DOI: 10.1016/j.ajic.2012.09.030)]
New developments in reprocessing semicritical items, William A. Rutala,
David J. Weber [May 2013 (volume 41 issue 5 Pages S60-S66 DOI: 10.1016/j.
ajic.2012.09.028)]
The adenosine triphosphate test is a rapid and reliable audit tool to
assess manual cleaning adequacy of flexible endoscope channels,
Michelle J. Alfa, Iram Fatima, Nancy Olson [March 2013 (volume 41 issue 3
Pages 249-253 DOI: 10.1016/j.ajic.2012.03.015)]
Comparison of adenosine triphosphate, microbiological load, and
residual protein as indicators for assessing the cleanliness of flexible
gastrointestinal endoscopes, Ryo Fushimi, Masaki Takashina, Hideki
Yoshikawa, Hiroyoshi Kobayashi, Takashi Okubo, Seizoh Nakata, Mitsuo
Kaku [February 2013 (volume 41 issue 2 Pages 161-164 DOI: 10.1016/j.
ajic.2012.02.030)]
Development and validation of rapid use scope test strips to determine
the efficacy of manual cleaning for flexible endoscope channels, Michelle
J. Alfa, Nancy Olson, Pat DeGagné, Patricia J. Simner [November 2012 (volume
40 issue 9 Pages 860-865 DOI: 10.1016/j.ajic.2011.10.006)]
In vitro evaluation of cleaning efficacy of detergents recommended for
use on dental instruments, Gordon W.G. Smith, June McNeil, Gordon Ramage, Andrew J. Smith [November 2012 (volume 40 issue 9 Pages e255-e259
DOI: 10.1016/j.ajic.2012.05.009)]
50 | WINTER 2013 | Prevention
“To facilitate the transition to the new
program, NEVHC created an action plan
and timeline and engaged key stakeholders
in the sterile processing program to help
nurture buy-in from resistant staff.”
and splatter (change if the
covering gets wet or soiled)
• Liquid-resistant shoe coverings to protect shoes if there
is a potential for shoes becoming contaminated and/or
soaked with blood or other
bodily fluids
• General purpose heavy duty,
waterproof, long and cuffed
gloves to prevent punctures,
contact with microorganisms,
and decrease cross-contamination.1, 4
Instrument transport
Establish a plan for preparing
contaminated instruments at the
outlying clinical sites to transport
to the centralized sterile processing area. One choice is to train
staff at the point of use to don
PPE and remove gross soil using
a disposable sponge moistened
with water. Instruments can
then be air dried and double red
bagged. See the following recommended practices for further
details.
Figure 3 shows bagged instruments that have been placed into
a puncture-resistant, leak-proof,
closable container, labeled as biohazard. These “transport bins”
have a reversible label that is used
to identify the destination of the
instruments. An inventory sheet
quantifying the number of sets
and/or individual instruments
should be placed on the outside
of the bin under the label.
If your facility has an existing courier service, this can be
used to transport contaminated
instruments from clinics to the
centralized sterile processing
area. Depending on travel distance and courier routes, this
method may require increased
instrument inventory to
ensure acceptable turnaround
time. Sterilized instruments
should be transported back to
the outlying sites by the same
courier method.
Recommended practices
Instruments should be precleaned at the point of use as
described in recommendation IV and V of the AORN
Recommended Practices for
Cleaning and Care of Surgical
Instruments and Powered
Equipment.10 A AMI ST79
states that if decontamination
of the instruments will not
occur immediately, the instruments must be kept moist to
prevent the formation of biofilm (Section 6.3).1 Options
for keeping instruments moist
include placing a towel soaked
with water (not saline) over
the instruments or using an
instrument spray designed for
pretreatment.1
Contaminated instruments
need to be contained and readily identifiable by everyone who
handles them, per AAMI ST79,
Section 6.2.1 It is not necessary
to double red bag instruments
before placing them into the
containment devices if you have
a hazardous material label.
Instrument storage
Per AAMI ST79:
• Store sterilized instruments
in a clean, dry area in a controlled environment (Section
8.9.2).
• Shelf life is event-related
(Section 8.9.3).
• Rotate storage of stock by “first
in, first out” (Section 8.9.3).
• Inspect all packages for damage before transporting, storing, or using (Section 8.10.1).
• Label packages with a control
date for stock rotation and a
statement such as “Contents
sterile unless package is
opened or damaged. Please
check before using” (Section
10.3.3).
1
Available at: www.cdc.gov/hicpac/pubs.
html.
5. Centers for Disease Control and Prevention
(CDC). Guideline to Infection Prevention for
Outpatient Settings: Minimum Expectations
for Safe Care, July 2011. Available at: www.
cdc.gov/HAI/pdfs/guidelines/standatds-ofambulatory-care-7-2011.pdf.
6. Centers for Disease Control and Prevention
(CDC). Infection Prevention Checklists for
Outpatient Settings: Minimum Expectations
for Safe Care. Available at: www.cdc.gov/
HAI/pdfs/guidelines/ambulatory-carechecklist-07-2011.pdf.
7.ECRI. Health Devices: Top 10 Health Technology Hazards for 2012. Available at: www.ecri.
org/Documents/Secure/Health_Devices_
Top_10_Hazards_2012.pdf.
8. Eiland, John E, Surveyor, The Joint Commission. Joint Commission presentation at
IAHCSMM annual meeting in May 2013.
Presentation available on flash drive pro-
vided to attendees. Martha Young attended
the presentation.
9. Pure Processing. Accessed July 9, 2013 at:
www.pure-processingcom.
10.R ecommended Practices for Cleaning and
Care of Surgical Instruments and Powered
Equipment. Perioperative Standards and Recommended Practices. Denver, CO: AORN,
2013. www.aorn.org.
Conclusion
A centralized sterile processing
program can ensure a safe, economic, and efficient system to
sterilize reusable medical devices.
Ambulatory settings can customize a program that meets their
individual facility’s needs.
Jody Church, RN, CPNP, is infection control coordinator of Northeast
Valley Health Corporation in San
Fernando, California. Martha
Young, BS, MS, CSPDT, is president of Martha L. Young, LLC, in
Woodbury, Minnesota.
References
1.Association for the Advancement of Medical
Instrumentation. Comprehensive guide to
steam sterilization and sterility assurance in
health care facilities, ANSI/AAMI ST79:2010
& A1:2010 & A2:2011 & A3:2012 (Consolidated Text). Arlington, VA.www.aami.org.
2.The Joint Commission. National Patient
Safety Goals, NPSG.07.05.01. Hospital Accreditation Standards (HAS), 2013.
Available at: www.jointcommisssion.org/
standards_information/npsgs.aspx.
3.AORN. Recommended practices for sterilization. Perioperative Standards and Recommended Practices. Denver, CO: AORN, 2013.
www.aorn.org.
4. Centers for Disease Control and Prevention (CDC). Guideline for Disinfection and
Sterilization in Healthcare Facilities. 2008.
660442_Ivera.indd 1
w26/09/13
w w.apic.org
1:59 AM | 51
3M Infection Prevention Solutions for the OR
en
Pre-Op
•
•
•
•
•
•
Pa
ti
•
•
Pe
rs
on
al
Pro
tec
tio
tW
n
a
r
mi
Pa
ng
tie
nt
Mo
nit
Su
ori
rgi
ng
ca
lH
an
Pa
dA
tie
nti
nt
se
Sk
ps
i
nP
Dr
is
ap
rep
ing
Ste
rile
Su
rfa
Sk
ce
in
Clo
su
res
The OR expertise you can trust
Post-Op
Intra-Op
Clearly at the
cutting edge.
In clean wounds (219 patients total)
there was a significant difference in
wound contamination. Contamination
occurred in 9.1% of the patients draped
with Ioban drapes compared with 16.2%
of the patients without drapes (P<0.05).*
Wound Contamination*
50
40
30
20
10
3M™ Ioban™ 2 Antimicrobial
Incise Drapes
*Dewan PA, Van Rij AM, Robinson RG, et al. The use of an iodophor-impregnated plastic incise drape in abdominal surgery--a controlled clinical trial. Aust N Z J Surg.
1987;57(11):859- 863. Poster presented at: 19th Annual Scientific Meeting of the Society for Healthcare Epidemiology of America (SHEA), March 19-22, 2009, San Diego, Calif.
www.3m.com/Ioban
© 3M 2013. All rights reserved.
0
Wound Classification
No drape used (disinfected skin)
3M™ Ioban™ 2 Antimicrobial Incise Drape (sterile surface)
PREVENTION IN ACTION
Today’s infection
prevention challenges
in long-term care
Are we ready to manage them?
BY VICKY UHL AND
I
t’s no secret that the number of people entering long-term care facilities (LTCFs) is growing
every day, and with that burgeoning population comes increased instances of LTCF-associated
infections. And yet, notes Irena Kenneley, PhD,
APRN-BC, CIC, there is a lack of adequately trained
personnel and resources to prevent those infections.
Learn more about
the new Infection
Preventionist’s Guide
to Long-Term Care at
www.apic.org/store.
Kenneley, who is an assistant professor at Case Western
Reserve University, is one of
eight authors of APIC’s new
book, Infection Preventionist’s
Guide to Long-Term Care.
This comprehensive resource
examines infection prevention
practice in the larger scope of
long-term care (LTC) trends,
initiatives, and regulations. The
new book, which is available at
www.apic.org/store, discusses
how to develop infection prevention programs in response
to integration of LTCFs within
the larger healthcare community, addressing issues such as
frequent resident movement in
and out of facilities and the use
of laboratory, pharmaceutical,
and other types of consultants.
There is also a strong focus on
interdisciplinary collaboration,
a lengthy chapter on emergency
and disaster preparedness, and
an accompanying CD-ROM
with tools and resources.
In preparation for the launch
of the book, Kenneley; coauthor Deb Burdsall, MSN,
RN-BC, CIC, corporate infection preventionist, Lutheran Life
Communities; and lead author
Steven J. Schweon, RN, MPH,
MSN, CIC, HEM, an infection
prevention consultant, discussed
a series of questions on LTC
infection prevention.
Q:
What do you
think the biggest
infection
prevention and control
challenge is in long-term
care?
Burdsall: The
increased complexcare needs of the
people living and
staying in the LTC continuum.
Older adults used to come
into LTC when they still were
ambulatory and could care for
themselves, but now they are
staying in their own homes for
a longer period of time. The
days of “rest homes” are gone.
Now, people enter LTC with
significant physical, psychological, social, and spiritual needs.
w w w.apic.org | 53
PREVENTION IN ACTION
Increased physical needs mean
more dependence on caregivers,
more exposure to antibiotics,
and a history of invasive procedures—all of which have been
shown to increase the chance
that LTC residents are colonized
with multidrug-resistant organisms (MDROs).
Kenneley: The vast
majority of LTCF
infection preventionists (IPs) have
multiple responsibilities and
work part-time on infection
prevention regardless of the bed
size or acuity of the residents in
their facility. Additionally, less
than 10 percent of the current IPs in LTCFs have any
specific infection prevention
and control training—such
as a Certification in Infection
Control (CIC)—compared to
more than 95 percent of acutecare IPs in some states. Other
issues include limited staff
resources, high staff turnover,
funding difficulties, and limited
information technology access
and infrastructure to support
infection prevention and control activities.
Q:
What needs to be
done to improve/
expand infection
surveillance and reporting
in nursing homes?
Schweon: First,
the facility can
make a voluntary
decision to upgrade
its infection prevention program and promote resident
safety by expanding its surveillance program. The other alternative is to have a regulatory or
legislative mandate requiring
selected, targeted surveillance
54 | WINTER 2013 | Prevention
such as central line-associated
bloodstream infections or total
house surveillance. Secondly,
public reporting of surveillance needs to be regulatory
driven. For example, a legislative mandate is required for
LTCFs to report surveillance
findings. In my home state
of Pennsylvania, LTCFs must
perform total house surveillance, and infections meeting
the Pennsylvania LTC surveillance definitions must be electronically reported.
Kenneley: There
are two major
areas that must be
addressed:
1. Standardized surveillance definitions. In October 2012, a Society
for Healthcare Epidemiology of
America (SHEA)/Centers for
Disease Control and Prevention
(CDC) position paper was published that updated the 1991 surveillance definitions specifically
for LTCFs. It is imperative that
all LTCFs use the same infection
definitions so reported data is
meaningful, baseline statistics
can be compiled, and comparisons can be made.
2. Implementation of infection
prevention best practices. The
CDC developed a standardized
assessment tool that, among
other things, measures the
extent of best-practice implementation in LTCFs within six
categories.
Q:
How does a
rapidly aging
population—
and one that increasingly
needs LTC services—impact
infection prevention
practice? Are IPs ready to
face these new challenges?
Schweon: Residents
of all ages with complex medical needs
were once kept in
the hospital for management;
today, they may be discharged
to LTC, possibly with MDROs
such as ESBLs (extended spectrum beta-lactamase) or CRE
(carbapenem-resistant Enterobacteriaceae), where the goal is
to maintain or improve their
ability to function as independently as possible, for as long
as possible. Some residents may
also have advance directives or
expressed wishes to limit a diagnostic workup and treatment in
the event of an infection such as
pneumonia.
IPs can be prepared to meet
these challenges by:
• Having a basic and hopefully
an advanced understanding
of infection prevention and
implementing best practices
• Having awareness of the residents’ health status
• Having policies and procedures that are evidencebased and that are being
implemented
• Being visible in the facility
and developing collegial relationships with all disciplines
• A ssisting with staff education
and training
• Being a role model; IPs are
continually watched to see
whether they perform hand
hygiene, take the influenza
vaccine, etc.
• Realizing that what may work
in a hospital may not work in
LTC; for instance, you can’t
keep a resident with a MDRO
in his or her room for the next
10 years
• Accepting that there may be
human capital, bed space, and
equipment limitations compared to acute care
Kenneley: The
geriatric population has many
unique aspects
that contribute to the severity and frequency of infections, including limited
physiologic reserves, defects
in host defenses, higher rates
of chronic diseases, poorer
responses to antimicrobial
therapy, increased frequencies
of therapeutic toxicity (secondary to increased rates of liver
and renal failure), and complications from invasive diagnostic procedures. Symptoms
of infection may be vague or
atypical compared to younger
populations. There is also the
additional risk of infection from
exposure to MDROs, delays
in diagnosis and therapy, and
complications from treatments.
The U.S. Department of
Health and Human Services’
Long-Term Care chapter of the
National Action Plan to Prevent
Healthcare-Associated Infections:
Roadmap to Elimination, published in 2012, compiles current
statistical data and information
and provides a chapter specifically on infection prevention
and control in LTCFs, offering
a roadmap to decrease HAIs
that IPs can follow.
Q:
What do you think
the top infection
surveillance
priority is/should be in
long-term care?
Bu rdsa ll:
We
need to make it
clear that diagnostic definitions
of infection focus on the individual, which is important, but
surveillance definitions focus
on identifying patterns within
a group so interventions can
be put into place. The MDS
3.0 definitions are based upon
a mixture of diagnosis and criteria that need to be brought
into line with the currently
revised CDC/SHEA/Stone, et
al. definitions. Everyone also
needs to get on the same page
for surveillance so we can all
compare apples to apples.
Q:
What do you
think are the
most urgent
education and training
needs for LTC staff? Is
this information readily
available? Does our
process of educating LTC
staff need to change and
if so, how?
Kenneley: There
are three crucial
areas in which IPs
need to educate
LTCF staff: hand hygiene, urinary tract infections (UTIs),
and environmental controls.
Evaluation of educational programs must be done to assess
whether a training event was successful, and evaluation of staff
practices such as observation of
hand hygiene compliance also
needs to be documented and a
part of the educational process.
For IPs who are not trained
or are part-time, this information may not be readily available. National standardization
of regulatory guidelines for
IPs working in LTCFs needs
to take place so that IPs are able
to properly educate LTC staff.
Some states have stricter regulatory guidelines for IP training
and education than others. This
will change when surveillance
data are reported and the results
made public.
Q:
How can nurses
and IPs better
collaborate
to improve infection
prevention in U.S. nursing
homes? What makes up an
effective team approach in
long-term care?
Burdsall: An interdisciplinary team
includes the person
who needs care and
his or her family and significant
others, the nursing department,
therapy department, culinary
and dining services, life enrichment/activities, environmental services, plant operations,
materials management, and
maintenance. As an example,
take a person who needs to
be placed on isolation precautions for an infection with an
MDRO. Everyone on the team
needs to know how they should
approach the person and the
environment to prevent the
spread of microorganisms to
others and to the surrounding
environment.
Q:
What can IPs do
to help meet the
increasingly
complex medical needs of
residents in skilled LTCFs?
Schweon: It’s mission critical to have
IPs who like (or
love) their job. The
program will fail if infection
prevention is viewed as a mundane chore or task. IPs must also
have an awareness and understanding of:
• The changes that occur in the
immune, respiratory, urinary,
gastrointestinal, and circulatory system during aging
• Polypharmacy that may lead
to drug interactions
“...less than 10 percent of the current IPs in
LTCFs have any specific infection prevention
and control training—such as a Certification
in Infection Control (CIC)—compared to
more than 95 percent of acute-care IPs in
some states.”
—Irena Kenneley, PhD, APRN-BC, CIC
• Medications that impact the
immune system
• M alnutrition/failure to
thrive’s impact upon the body
• Functional impairments that
may impair assessment and
performance of activities of
daily living
• A ltered ability to metabolize
medications
• Limited physiological reserves
• Slower response to treatment
• Blunted immune response to
infection
Q:
Do you think
current clinical
management
strategies for MDROs
in nursing homes are
adequate? Is there anything
else we should be doing?
Kenneley: A major
opportunity for
improvement lies in
the full implementation of antimicrobial stewardship programs. Antibiotic
stewardship is recognized as a
national challenge in LTCFs.
In effective LTCF antimicrobial stewardship programs, the
medical director shares personalized reports with prescribers
detailing antibiotic usage and
infection rates for the LTCF’s
residents compared with peer
facilities. Several LTCFs have
also indicated that there is a
challenge in educating the
nursing staff regarding definitions for infections that require
treatment, as many prescribers
report ordering antibiotics at the
request of nursing staff based
on positive microbiology culture
results alone.
Q:
There have
been disease
outbreaks
in LTCFs due to unsafe
injection practices,
especially related to blood
glucose testing and insulin
administration. Are we
doing enough to protect
residents? Why is this issue
so problematic?
Schweon: Unsafe
practices have
become problematic in acute/LTC/
ambulatory care due to inadequate disinfection of multiple-patient-use glucose testing
equipment such as glucometers; and failure to follow basic
safe-injection practices during
medication preparation and
administration, which leads to
contamination and infection.
In my view, the IP must target zero infections and adverse
events. Realistically, we will
never achieve this when working
w w w.apic.org | 55
PREVENTION IN ACTION
“We need to advocate a nimble approach to infection prevention that focuses on the
individual first. The LTC IP needs to understand LTC, the resident and patient populations,
what types of interventions are helpful, and what types of interventions have been shown to
be harmful.” —Deb Burdsall, MSN, RN-BC, CIC
with residents who are biologically/chemically/physiologically
complex; however, we need a target for our implementations. To
say “only one resident” had pneumonia this month diminishes the
significance of that infection on
the resident.
Q:
Only a few
states currently
require public
reporting of infections by
nursing homes. What needs
to happen to include more
facilities in this process?
Schweon: Currently, there is no
national mandate or
legislative requirement for public reporting of
all LTCFs. However, in 2012,
the CDC’s National Healthcare Safety Network (NHSN)
released a voluntary LTC component. This secure, Internet-based
surveillance system uses a standardized and precise approach
for tracking healthcare-associated
infections. The LTC component
(www.cdc.gov/nhsn/LTC) includes
the recently released “Revisiting
McGeer” LTC surveillance UTI
and C. difficile standardized epidemiological definitions. Additionally, MDRO activity and
preventative process measures
can be monitored. LTCFs now
have the capability of benchmarking their data against other
organizations.
The National Action Plan
to Prevent Healthcare-Associated Infections in Long-Term
Care Facilities has a goal of 5
percent of certified nursing
homes enrolling in NHSN over
the next five years. In my view,
for facilities that have a strong
commitment to resident safety
and preventing infection, joining and actively participating in
the LTC component may lead to
improved resident outcomes and
decreased expenditures related
to infectious diseases.
Q:
What needs to be
done to better
prepare IPs to
work in LTC settings?
Burdsall: Basic
training in infection prevention
strategies, such
as APIC’s infection prevention training programs. This
training shows a person how
to look at infection prevention in the context of a more
global view of how LTC fits
into the healthcare continuum.
We need to advocate a nimble
approach to infection prevention that focuses on the individual first. The IP needs to
understand LTC, the resident
and patient populations, what
types of interventions are helpful, and what types of interventions have been shown to be
harmful. This takes consistent
review of the current evidence.
Our understanding of what we
thought were effective strategies 10 years ago has changed
significantly.
Vicky Uhland is a medical writer for
Prevention Strategist.
Use SOMAY “STERI-SHIELD”®
Everywhere that the Highest Standards
of Hygiene & Cleanliness are Important
www.somay.com/steri-shield/steri-shield.html
EFFECTIVE
SOMAY “STERI-SHIELD”® Fungistatic
Paint contains an exceptionally
effective combination of antimicrobial
additives including algaecides,
bactericides, biocides, fungicides
and mildewcides. Helps avoid “Sick
Building Syndrome”, possible allergic
reactions and unpleasant odors. Avoid
Building Code violations.
56 | WINTER 2013 | Prevention
653063_Somay.indd 1
SAFE
The effective active
ingredients are nonsoluble, non-leachable,
non-toxic, non-poisonous,
non-polluting and nonhazardous, so SOMAY
“STERI-SHIELD”® is as
safe to use as any acrylic
latex paint.
PROVEN
The active
ingredients in
SOMAY “STERISHIELD”® have
been proven in use
around the world
for over 40 years.
TESTED
Independent Laboratory
Tests using standard testing
procedures according to
ASTM D-5590 concluded
SOMAY “STERI-SHIELD”®
provides the “greatest
resistance to (microbial)
growth (of all paints tested)”.
Call and Order Today
(888-247-6629)
(888)2~4~SOMAY
8/12/13 8:38 PM
CURTAINS PROVIDE PRIVACY.
AND PATHOGENS.
92% of privacy curtains have been found contaminated one week after laundering.1
Fortunately, now you can kill bacteria on soft surfaces* in 30 seconds.
Disinfecting hard surfaces is only half the battle.
In healthcare environments, soft surfaces — like privacy curtains, chairs and
couches — can be carriers of HAI-causing pathogens. Dangerous bacteria can
survive up to 90 days2 on fabric, putting patients, families and staff at risk.
Now, a solution for soft surfaces.
Clorox Healthcare® Hydrogen Peroxide Cleaner Disinfectants are EPA-registered
to disinfect hard surfaces and kill bacteria on soft surfaces. Finally, a single
solution for all surfaces — to help you kill infection-causing pathogens wherever
they may be.
For your free sample, visit cloroxhealthcare.com/softsurface.
1. Ohl, M., et al. (2011). Hospital privacy curtains are frequently and rapidly contaminated with potentially pathogenic bacteria.
Am J Infect Control. 2012 Dec; 40(10):904-6.
2. Neely AN, Maley MP, “Survival of enterococci and staphylococci on hospital fabrics and plastic.” J Clin Microbiol 2000; 38:724-726.
* 100% polyester and 100% cotton. Soft surface claim has been registered by the Federal EPA and may not be available in all 50
states. Please check with your sales representative for updates in your state.
© 2013 Clorox Professional Products Company.
NI-22353
A closer look—
60 | WINTER 2013 | Prevention
—Antibiotic
resistance
and the
microbiome
BY MARILYN HANCHETT, RN, MA, CPHQ, CIC
T
he current analysis of the human microbiome is providing a more comprehensive understanding
of the diverse types of bacteria that not only exist in various anatomical locations (e.g., skin, oral
cavity, nasopharynx, groin, axilla), but whose presence is essential to health. Caroline McDaniel,
RN, BSN, MSN, provided an overview of the microbiome in the fall 2013 Prevention Strategist
article titled, “The Human Microbiome Project: What’s in it for IPs?” Foremost among these
is the intestinal tract, where the normal flora, often called the microbiota, are the most dense
and diverse than any other location. Recent studies have estimated that over 40,000 bacterial
species, primarily anaerobes, are part of the natural biodiversity of the gut ecosystem.1 In fact,
the variety and complexity of the gut microbiota is now described as a “virtual organ” or emerging body
system.2 In addition, bacterial diversity changes along the gastrointestinal tract; high levels are reported in
the oral cavity and intestines but are low in the stomach.3
Research conducted during
the past 10 years consistently
reports that homeostasis within
the intestinal microbiota is
essential for health. Disruptions
may occur from diet, surgery,
alcohol abuse, and medications—especially antibiotics.
No matter what the trigger,
impaired bacterial function,
referred to as dysbiosis, has been
associated with inflammatory
bowel conditions, insulin resistance, diabetes, and obesity. In
many cases it remains unclear if
w w w.apic.org | 61
the changes in intestinal microbiome are a symptom of the disease or a contributing factor.4
Due to the wide variation in
microbiota among individuals,
no single bacterial species can
serve as a marker of disease.3
Other factors are thought to
contribute to bacterial homeostasis in the gut. Environmental,
immunological, hormonal, and
genetic variables have been
investigated. While much
remains unknown, it is clear that
maintenance of the microbiota is
a far more complex process that
previously believed.5
The emerging science of
metagenomics or environmental gene sequencing holds great
promise for a deeper understating of gut ecology. The intestinal microbiota has been almost
impossible to analyze using traditional laboratory approaches
such as culture and strain typing, as less than 1 percent of
intestinal bacteria have been
successfully cultured.6 PCRbased approaches eliminate the
need for culture, but they can
only detect previously identified
genes when compared to the
metagenome that now lists more
than 5 million non-redundant
genes. The field of metagenomics uses this vast pool of information to produce a more complete
description of all types of human
microbiota, as well as reduce the
previous risk of underreporting
the size and nature of microbial
communities.7
The environmental
resistome
The first step in understanding
antibiotic resistance is recognition of the environment as
a natural reservoir. A growing
number of studies suggest that
human health may not only be
62 | WINTER 2013 | Prevention
determined by individual genetics, but also by the genes of the
trillions of microorganisms that
exist on and within the human
body.8
Antibiotic resistance is now
viewed as an ancient process.
New technologies have revealed
the presence of antibiotic resistance in the environment, suggesting a co-evolution between
antibiotic and antibiotic resistance that occurs as a natural event. The environmental
microbiota, even in antibioticfree conditions, possesses a large
and diverse number of antibiotic resistant genes—some of
which resemble the genes of
pathogenic microbes.9 This
global environmental combination of susceptible and resistant
bacteria comprises a worldwide
resistome. The contemporary
resistome is under increasing
selective pressure from human
activities—especially agriculture—that may accelerate resistance and gene transfer. Changes
in the environment then impact
the clinical resistome. For example, evidence now suggests links
between aminoglycoside and
vancomycin resistance enzymes
and the environment.10
Today’s commercial production and widespread use of both
natural and synthetic antibiotics intensifies the pressure on
both environmental and clinical
resistomes. For this reason, scientists have used the beta lactamases for modeling as they
represent the most widespread
mechanism of resistance among
pathogenic bacteria worldwide.11
Early testing has been promising. For example, in one of
the first metagenomic studies
on antibiotic resistance in the
human intestinal microbiome,
researchers identified 10 novel
beta lactamase families that
reflected only 35–61 percent of
known genes.12
Antibiotic resistance
and new research
Antibiotic resistance is a serious and growing threat to the
prevention and containment of
communicable diseases worldwide. According to the most
recent data, antibiotic resistance
in the United States causes an
estimated $20 billion a year in
excess healthcare costs, $35 million in other societal costs, and
more than 8 million additional
acute care inpatient days.13 In the
United States, a growing list of
resistant pathogens includes not
only the long-recognized MRSA
and vancomycin-resistant
Enterococci, but also cases of
H1N1 influenza, carbapenemresistant Enterobacteriaceae,
Klebsiella pneumoniae, TB, and
gonorrhea.13
Antibiotic resistance develops in one of two basic ways. A
bacterium can undergo spontaneous genetic mutation. It can
also receive genetically coded
resistance via plasmids or transposons from other bacteria that
already contain this genetic
information. However, bacteria
can also receive resistance genes
from viruses, as well as via direct
exposure to DNA in the environment. These processes can
occur at varying times, increasing the number and types of
antibiotics that they can resist.
Once resistance is acquired, it
may be transferred vertically,
through bacterial replication,
or horizontally, via contact
between bacteria without any
type of reproduction.
The density of intestinal bacteria, especially during disease
progression, increases the risk of
horizontal transfers of antibiotic
resistant genes within the microbiota. Due to the probability of
genetic exchange during disease,
the intestinal microbiota may
represent the largest reservoir for
resistance.12 Previous antibiotic
susceptibility studies, attempting to analyze this lateral transfer mechanism, have relied on
Escherichia coli. However the
use of metagenomic sequencing has, as in the study of beta
lactamases, now identified resistant genes previously unknown
and not recognized using E. coli
cultures.14
New research is also examining the role of bacteriophages
(also known as phages). Phages
are viruses that attack bacteria. The community of phages
is referred to as a phageome.
The rapid increase in antibiotic
resistance since the 1990s has
focused renewed attention on
phage-based research. Recent
research in animal models has
attempted to analyze the role of
phages in the spread of antibiotic
resistance. In one study, phages
were studied as a potential reservoir for bacterial adaptation. In
this study, antibiotic treatment
led to enrichment of phageencoded genes. This research
demonstrated that phages from
treated laboratory mice lead to
increased resistance in aerobically cultured naïve microbiota.15 More research is needed
to fully understand the role
of the phageome in antibiotic
resistance.
Another area of investigation
focuses on biochemical alteration of the intestinal epithelium.
Disruption of normal epithelial permeability and mucous
integrity can impact the microbiota. For example, one project
has examined carbohydrate
metabolism. Laboratory analysis
has shown that antibiotic impact
on intestinal microbiota changed
mucosal carbohydrate availability in ways that supported the
growth of S. typhimurium and
Clostridium difficile.16 Other
studies have looked for relationships between medication
use, especially antibiotics and
proton pump inhibitors, and
Clostridium difficile. Research
in these areas is ongoing.
Microbiota and obesity
Obesity is rarely a consequence
of only nutritional imbalance.
It is a complex problem linked
to both metabolic and immunologic functions.17 The intestinal microbiota are increasingly
recognized as part of the connection between genes, environmental factors, and the immune
system. Specifically, emerging
research shows a link not only
between gut microbiota and
obesity, but also with insulin
resistance and type 2 diabetes.
Although a causal relationship
is not yet absolutely described in
the literature, experts are increasingly looking at the association
of gut microbes, a high fat/high
sugar diet, and excessive weight
gain. While studies are ongoing,
the number of potentially confounding variables—including
factors such as antibiotic use,
previous dietary habits, meal
frequency, and physical activity—makes conclusive investigation challenging.17
Manipulating the microbiota
As more is learned about the
intestinal microbiome and its
impact on overall health, various strategies have been proposed to restore or maintain gut
homeostasis. Foremost among
these future strategies is the
judicious use of antibiotics. In
addition, the future may yield
new pharmacological treatments, immunomodulatory vaccines, and nutritionally based
therapies. Targeted modification of microbial communities
may be accomplished through
deployment of antibiotics (to
remove or suppress undesirable segments of the microbiota), and/or administration
of pre- and probiotics. A better
understanding of the development of gut microbiota early
in life may yield new opportunities to prevent or manage
adult disease. More information about nutritional components is needed to understand
and manage endotoxinemic
and inflammatory responses
in the gut, especially related
to lipid and fructose intake.
However, all proposed methods
of manipulation are based on
varying approaches to human
host-microbiota co-regulation
of intestinal homeostasis.18
Marilyn Hanchett, RN, MA, CPHQ,
CIC, is APIC senior director of
Professional Practice.
References
1. Frank DN, Pace NR. Gastrointestinal microbiology in the metagenomics era. Curr Opin
Gastroenterol, 2008. Jan; 24 (1): 4-10.
2. Evans JM, Morris LS, Marchesi JR. The gut
microbiome: the role of a virtual organ in the
endocrinology of the host. J Endocrinol 2913
Aug; 218 (3): R37-47.
3. Luke KU, Clemente JC, Rideout JR, Gevers D,
Caporaso JG, Knight R. The interpersonal and
interpersonal diversity of human-associated
microbiota in key body sites. J Allergy Clin
Immuno. 02012 May; 129 (5):1204 -1208.
4. Blumbert R, Powrie F. Microbiota, disease and
back to health: a metastable journey. Sci Transl
Med. 2012; 4:137rv7.
5. Dave M, Higgins PD, Middha S, Rioux KP. The
human gut microbiome: current knowledge,
challenges and future directions. Transl Res.
2012 Oct; 160 (4): 246-57.
6.Konkel, L. The environment within: exploring the
role of the gut microbiome in health and disease.
Environ Health Perspect. 2013 September; 121
(9): A276-A281.
7. Pehrsson EC, Forsberg KJ, Gibson MK, Ahmadi
S, Dantas G. Novel resistance functions uncovered using functional metagenomic investigations of resistance reservoirs. Front Microbiol
2013; 4:145.
8.Konkel, L. The environment within: exploring the
role of the gut microbiome in health and disease.
Environ Health Perspect. 2013 September; 121
(9): A276-A281.
9.Aminov RI. The role of antibiotic and antibiotic
resistance in nature. Environ Microbiol 2009
Dec; 11 (12): 2970-88.
10.Perry JA, Wright GD. The antibiotic resistance
mobilome: searching for the link between environment and clinic. Front Microbiol 2013 May
30; 4:138.
11.Galan JC, Gonzalez-Candelas F, Rolain JM, Canton
R. Antibiotics as selectors and accelerators of
diversity in the mechanisms of resistance: from the
resistome to genetic plasticity in the B-lactamases
world. Front Microbiol 2013 Feb 8; 4:9.
12.Sommer MO, Church GM, Dantas G. The human
microbiome harbors a diverse reservoir of antibiotic resistance genes. Virulence. 2010 July-Aug;
1 (4): 299-303.
13.CDC. Antimicrobial resistance posing growing
health threat. Press release: April 7, 2011. www.
cdc.gov.
14.Penders J, Stobberingh EE, Savelkoul PH, Wolffs
PF. The human microbiome as a reservoir of
antimicrobial resistance. Front Microbiol 2013
April 17; 4:87.
15.Modi SR, Lee HH, Spina CS, Collins JJ. Antibiotic
treatment expands the resistance reservoir and
ecological network of the phage metagenome.
Nature 2013 July 11; 499 (7457): 21922.
16.Ng KM, Ferreyra JA, Higginbottom SK, Lynch
JB, Kashyap PC, Gopinath S et al. Microbiotaliertaed sugars facilitate post-antibiotic expansion
of enteric pathogens. Nature 2013 Sept 1: 10.
17.Giovanni M, Gambino R, Cassader M. Obesity,
diabetes and gut microbiota. Diabetes Care
2010 Oct; 33 (10): 2277-2284.
18.Burcelin R, Serino M, Chabo C, Garidou L, Pomie
C, Courtney M et al. Metagenome and metabolism: the tissue microbiota hypothesis. Diabetes
Ober Matab 2013 Sept 15; Suppl 3: 61-70.
w w w.apic.org | 63
OUR PULSED XENON UV
S Y S T EM D I SINF EC T S
SINK, TOILET SEAT, TISSUE BOX, PILLOW CASE, SHOWER, DOOR
KNOB, BATHROOM DOOR, TOILET BASE, BATHROOM DOOR HANDLE,
LATEX GLOVE BOX, PAPER TOWELS, SINK FAUCET, BED SHEETS,
BED LINING, HEADBOARD, LAMP, MATTRESS, TELEVISION REMOTE,
ASSISTANCE BUTTON, SIDE TABLE, FLOWERS, GLASS OF WATER,
DRAWERS, CLEANING SUPPLIES, DRIP STANDS, PULSE METERS, TILED
FLOOR, MACHINE CORDS, TELEVISION, TELEVISION STAND, TRASH
CAN, LAMP SWITCH, BED SIDE HANDLES, FILED MANILA FOLDERS,
WHEEL CHAIR, TABLE TOP, FACE PLATES OF MEDICAL EQUIPMENT,
STOOL, CEILING, TILE MOLDING, TELEPHONE, TOILET PAPER HOLDER,
BAR OF SOAP, TISSUES, DOOR STOPPER, CLEANING BUCKET, LIGHT
SWITCH, SURGICAL MASKS, OPERATING TOOLS, WINDOWS, LAMP SHADE,
HOSPITAL GOWN, SURGE PROTECTOR, OVERHEAD LIGHTS, PERSONAL
PROTECTIVE EQUIPMENT, SHELVES, WINDOW BLINDS, FIRE SPRINKLERS,
WALL MOUNTED LIGHTS, OUTLETS, VISITOR COUCH, PENS, BED WHEELS,
COMPUTER MOUSE, MIRRORS, MAGAZINES, WOOD PANELS, WIRED
EQUIPMENT HOLDERS, PICTURE FRAME, CHAIRS, PLASTIC SEPARATION
DRAPES, FOOD TRAY, ARM RESTS, PAPER TOWEL HOLDER, EXPOSED
SINK PIPES, DRAIN, AIR VENTS, COMPUTER, KEYBOARD, BED LEVER,
COMPUTER MONITOR, LATEX GLOVE DISPOSAL BIN, INTERCOM, SMOKE
DETECTORS, PILLOW, IV STAND, EQUPIMENT-HOLDING TRACK,
DRAWER HANDLES, CLOCK, SOAP DISPENSER, AM/FM RADIO
IN JUS T 5 MINU TE S.
Call 1-888-340-7832
to learn how Xenex is 20X more effective than chemical
cleaning and is proven effective against C. diff, MRSA & VRE.
Quezada R, Huber T, Copleand L, Zeber J, Jinadatha C [Poster Session]. “Evaluation of a Pulsed-Xenon Ultraviolet Rom Disinfection Device for
Impact on Contamination Levels of MRSA.” VA National Research Week Symposium. Temple, TX. April, 2012.
Infection
prevention
in outpatient oncology settings
CDC offers tools to fight back against infections among cancer patients.
BY ALICE Y. GUH, MD, MPH, LISA C. RICHARDSON, MD, MPH, AND ANGEL A DUNBAR, BS
D
espite advances in oncology care, infections remain a major
cause of morbidity and mortality among cancer patients.1-3
Several factors predispose cancer patients to developing infections, including immunosuppression from their underlying
cancer and chemotherapy treatment. Frequent contact with
healthcare settings may expose them to other patients with
transmissible infections. Patients with cancer often require the placement
of long-term intravascular devices, such as implanted ports, to provide
ease with chemotherapy infusion. However, these devices can provide
direct portal-of-entry for microorganisms to enter the bloodstream if
they are not appropriately disinfected prior to access. Thus, careful
attention to proper infection prevention practices is essential to the care
of cancer patients to minimize their risks for infectious complications.
In recent decades, the vast majority of
oncology services have shifted from inpatient to outpatient settings. Each year nearly
650,000 patients with cancer receive outpatient chemotherapy.4 However, not all
outpatient facilities maintain regular access
to infection prevention expertise or have
dedicated infection prevention policies for
patient protection.
Furthermore, unlike acute care hospitals,
there is limited federal and state regulatory oversight of many outpatient settings,
including outpatient oncology facilities. As
a result, many outpatient facilities are not
routinely inspected for infection prevention
practices.
Breaches in basic infection prevention practices have resulted in a number of outbreaks
www.preventcancerinfections.org
1. What? PREPARE: Watch Out for Fever!
When?
blood cell count is likely to be the lowest since
this is when you’re most at risk for infection
(also called nadir).
• Keep a working thermometer in a convenient
location and know how to use it.
• Keep your doctor’s phone numbers with you at
all times. Make sure you know what number to
call when their office is open and closed.
• If you have to go to the emergency room, it's
important that you tell the person checking you
You should take your temperature any time you
feel warm, flushed, chilled or not well. If you get a
temperature of 100.4°F (38°C) or higher for more
than one hour, or a one-time temperature of 101°
F or higher, call your doctor immediately, even if
it is the middle of the night. DO NOT wait until the
office re-opens before you call.
You should also:
• Find out from your doctor when your white
Why?
in that you are a cancer patient undergoing
chemotherapy. If you have a fever, you might
have an infection. This is a life threatening
condition, and you should be seen in a short
amount of time.
• If you develop a fever during your chemotherapy treatment it is a medical emergency.
• Fever may be the only sign that you have an infection, and an infection during chemotherapy can be life threatening.
2. What? PREVENT: Clean Your Hands!
When?
Why?
Keeping your hands clean is important in
preventing infections. This should include you, all
members of your household, your doctors,
nurses and anyone that comes around you. Don't
be afraid to ask people to clean their hands. If
soap and water are not available, it's o.k. to use
an alcohol-based hand sanitizer.
Clean your hands:
• Before, during, and after cooking food
• Before you eat
• After going to the bathroom
• After changing diapers or helping a child to use
the bathroom
• After blowing your nose, coughing, or sneezing
• After touching your pet or cleaning up after
your pet
• After touching trash
• Before and after treating a cut or wound or
caring for your catheter, port or other access
device
• Many diseases and conditions are spread by not cleaning your hands.
• Cleaning your hands is EXTREMELY important during chemotherapy treatment because your body can’t fight off infections like it used to.
3. What? PROTECT: Know the Signs and Symptoms of an Infection!
When?
During your chemotherapy treatment, your body
will not be able to fight off infections like it used
to. Call your doctor immediately if you notice any
of the following signs and symptoms of an
infection:
• Fever (this is sometimes the only sign of
an infection)
• Chills and sweats
• Change in cough or new cough
• Sore throat or new mouth sore
• Shortness of breath
Why?
•
•
•
•
•
•
•
•
•
•
•
Nasal congestion
Stiff neck
Burning or pain with urination
Unusual vaginal discharge or irritation
Increased urination
Redness, soreness, or swelling in any area,
including surgical wounds and ports
Diarrhea
Vomiting
Pain in the abdomen or rectum
New onset of pain
Changes in skin, urination, or mental status
Find out from your doctor when your white blood
cell count is likely to be the lowest since this is
when you’re most at risk for infection. This usually
occurs between 7 and 12 days after you finish
each chemotherapy dose—and will possibly last
up to one week.
• When your counts are low, take even the slightest sign or symptom of an infection as serious and call your doctor immediately.
• Infection during chemotherapy can be very serious, and can lead to hospitalization or death.
Write the number(s) to call in
an emergency here:
Doctor’s daytime number:
________________________________
Doctor’s after-hours number:
________________________________
Emergency Number Card
1. Treat a fever as an emergency.
2. Call your doctor immediately if you develop a fever.
3. If you have to go to the emergency room, tell them right
away that you are undergoing chemotherapy treatment.
Doctor’s daytime number:___________________________
Doctor’s after-hours number:_________________________
FEVER: TEMPERATURE OF 100.4°F (38°C) OR HIGHER FOR MORE THAN ONE
HOUR OR A ONE-TIME TEMPERATURE OF 101° F OR HIGHER.
www.preventcancerinfections.org
Cut out the emergency number card. Fill in your doctor’s information. Carry this card with you at all times.
The Three Steps Brochure was created for cancer
patients and caregivers to help increase awareness
about the importance of infection prevention.
Image COURTESY cdc/www.preventcancerinfections.org.
w w w.apic.org | 65
involving outpatient oncology settings. For
example, in a Nebraska oncology clinic,
syringe reuse to access saline bags shared
among multiple patients led to the transmission of hepatitis C virus to at least 99
cancer patients, resulting in one of the
largest healthcare-associated outbreaks of
viral hepatitis.5 Similar lapses in injection
safety (e.g., reusing single-dose vials on
multiple patients, storing prefilled saline
flush syringes for later use) have also been
implicated in outbreaks of bacterial bloodstream infections among cancer patients.6-8
Other identified lapses have included poor
hand hygiene, suboptimal disinfection of
injection caps (e.g., needleless connectors)
prior to accessing central lines, and inadequate environmental conditions for chemotherapy preparation.
To help combat this public health challenge, CDC launched its Preventing Infections
in Cancer Patients campaign in October
2011. This public health program offers
healthcare providers, patients, and families a
set of user-friendly resources designed to help
reduce the risk of life-threatening infections
during a cancer patient’s treatment. Each of
these tools is described in more detail in the
following sections.
Basic Infection Control and Prevention
for Outpatient Oncology Settings (BICAPP)
The BICAPP (www.cdc.gov/hai/pdfs/guide-
lines/basic-infection-control-preventionplan-2011.pdf) can be used by any outpatient
oncology facility to standardize and improve
infection prevention practices. The document is based on the CDC’s evidence-based
guidelines as well as relevant guidelines from
professional societies and is tailored for quick
implementation in outpatient oncology facilities. It includes key policies and procedures that will ensure a facility meets or
exceeds minimal expectations of patient
safety. The main components of the plan
include the following:
Education and training. All facility staff
should receive appropriate education and
training in infection prevention during
orientation as well as annually and any time
policies change. Competency evaluations of
facility staff should be regularly conducted to
66 | WINTER 2013 | Prevention
storage and handling; and 5) safe handling
and cleaning/disinfection of potentially
contaminated equipment or surfaces in
the patient environment. Procedures for
each component of Standard Precautions
are detailed in the BICAPP. For example,
as part of respiratory hygiene, triaging of
patients upon entry to the facility should
be performed, especially during periods
of increased community respiratory virus
activity, to prevent spread of respiratory
infections among clinic patients. Safe
injection practices that are relevant to
oncology facilities include appropriate
preparation and handling of saline and
heparin syringes for flushing central lines.
Transmission-based
BICAPP can be used by any outpatient oncology facility to standardize and improve infection prevention
practices. Image COURTESY the cdc.
assess adherence to recommended infection
prevention practices.
At Your Fingertips: A list of names of designated personnel and their specific roles
and tasks and contact information that can
be tailored to your facility is provided as an
appendix.
Surveillance and reporting. Routine
surveillance of infections (e.g., bloodstream
infections) and process measures related to
infection prevention practices (e.g., hand
hygiene) should be conducted for outbreak
detection and improvement of healthcare
practices. Facility staff should also be aware
of and adhere to local, state, and federal
requirements for reportable diseases and
outbreak reporting.
At Your Fingertips: The BICAPP contains
an appendix where a facility can insert a list of
reportable disease/conditions specific to their
state and the appropriate contact information
for their local and state health authorities.
Standard Precautions. All facility staff
should adhere to Standard Precautions,
which include: 1) hand hygiene; 2) use
of personal protective equipment (e.g.,
gloves, gowns, facemasks) depending on
the anticipated exposures; 3) respiratory
hygiene and cough etiquette; 4) safe injection
practices, including appropriate medication
precautions.
Implementation of additional precautions,
such as Contact Precautions, Droplet
Precautions, and Airborne Precautions, may
be warranted in certain situations and should
be applied based on a patient’s history and
symptoms.
Central venous catheters. When accessing
a patient’s central line for infusions and
blood draws, all facility staff should use
OUT OF SIGHT, OUT OF MIND...
NOT THIS TIME!
One of the most dangerous
side effects of chemotherapy
cannot be seen?
That’s right, a low white blood cell count,
or neutropenia, puts cancer patients at a
higher risk for getting an infection.
An infection in people with cancer is an
emergency. Be prepared, and remember the
following three things during chemotherapy:
1. Treat a fever as an emergency, and call your doctor right away
if you develop a fever.
2. Find out from your doctor when your white blood cell count
will be the lowest because this is when you are most at risk
for infection.
3. If you have to go to the emergency room, it’s important that
you tell the person checking you in that you have cancer and
are receiving chemotherapy. If you have an infection you
should not sit in the waiting room for a long time. Infections
can get very serious in a short amount of time.
Learn more at: www.cdc.gov/
cancer/preventinfections
National Center for Chronic Disease Prevention and Health Promotion
Division of Cancer Prevention and Control
Made possible by a CDC Foundation partnership with Amgen
The Out of Sight, Out of Mind poster alerts both providers and consumers that patients undergoing chemotherapy are at a higher risk of developing infections.
Image COURTESY cdc/www.preventcancerinfections.org.
EMERGENCY ROOM PERSONNEL
in
ever tients
f
A r pa re
mo
ce
can ay be eets
m nm .
tha he eye
t
This is
especially
true for a
cancer patient
undergoing
chemotherapy
who develops a fever.
Get the full picture about people with
cancer who are receiving chemotherapy.
If they have a fever, remember—
1. A fever may be the only sign of infection and should be
treated as an emergency.
2. Developing an infection is a life-threatening complication.
3. A minor infection can turn serious fast. Quick action can
save a life.
Learn more at: www.cdc.gov/
cancer/preventinfections
National Center for Chronic Disease Prevention and Health Promotion
Division of Cancer Prevention and Control
Made possible by a CDC Foundation partnership with Amgen
Intended for healthcare personnel, the Emergency
Room Personnel poster increases awareness of the
dangers of fevers in cancer patients.
Image COURTESY cdc/www.preventcancerinfections.org.
aseptic technique, including scrubbing the
access port with an appropriate antiseptic
agent. Additional maintenance and access
procedures, such as changing catheter site
dressing and injection caps, are outlined in
the BICAPP for various types of central lines.
At Your Fingertips: The appendix provides a list of relevant resources, including
the United States Pharmacopeia (USP)
Chapter <797> Guidebook to Pharmaceutical
Compounding—Sterile Preparations. All
oncology facilities that provide on-site chemotherapy preparation should follow USP
guidance in consultation with the state pharmacy board.
At Your Fingertips: The BICAPP also
includes the CDC Infection Prevention
Checklist for Outpatient Settings that can
be tailored by an outpatient oncology facility
to systematically assess personnel adherence to
recommended infection prevention practices.
Interactive website for cancer
patients and caregivers to
prevent infections
While the BICAPP is a resource for healthcare providers, the Preventing Infections in
Cancer Patients campaign also created an
educational tool for patients and their caregivers that addresses one of the most common and potentially deadly side effects in
patients receiving chemotherapy treatments:
neutropenia (low white blood cell count).
Patients with neutropenia are more susceptible to bacterial infections. Their risk
for acquiring a life-threatening infection
increases progressively with both the duration and magnitude of neutropenia. The
CDC used knowledge gained through
formative research to tailor messages and
launch a website aimed at helping cancer
patients understand their risk for developing
a low white blood cell count and steps they
can take to lower their risk of infection when
they are most vulnerable.
Three Steps Toward Preventing
Infections During Cancer Treatment
(www.preventcancerinfections.org), is an
evidence-based tool that assesses a cancer
patient’s risk for developing neutropenia during chemotherapy. After the assessment is
completed, patients can receive downloadable
information about how to help lower their
risk for infection and keep themselves healthy
while receiving chemotherapy. Educational
information is available for everyone even
if the assessment is not completed. The
CDC hopes this information will lead cancer patients and caregivers to take actions
to seek care if they develop this potentially
life-threatening condition.
For more information, action steps, and
tools to help reduce a cancer patient’s risk of
developing potentially life-threatening infections during chemotherapy treatment, please
visit www.cdc.gov/cancer/preventinfections or
www.preventcancerinfections.org.
References
1.Kamboj M, Sepkowitz KA. Nosocomial infections in patients with
cancer. Lancet Oncol 2009;10:589−597.
2. Maschmeyer G, Haas A. The epidemiology and treatment of infections in cancer patients. Int J Antimicrob Agents 2008;31:193−197.
3. Guinan JL, McGuckin M, Nowell PC. Management of healthcare-associated infections in the oncology patient. Oncology
2003;17:415−420.
4.Halpern MT, Yabroff KR. Prevalence of outpatient cancer treatment in the United States: estimates from the Medical Panel
Expenditures Survey (MEPS). Cancer Invest 2008;26:647−651.
5. Macedo de Oliveria A, White KL, Leschinsky DP, Beecham BD,
Vogt TM, Moolenaar RL et al. An outbreak of hepatitis C virus
infections among outpatients at a hematology/oncology clinic.
Ann Intern Med 2005;142:898−902.
At your fingertips: Basic
Infection Control and
Prevention for Outpatient
Oncology Settings
(BICAPP)
The BICAPP can be used by any outpatient
oncology facility to standardize and improve
infection prevention practices.
•The BICAPP also includes the CDC Infection
Prevention Checklist for Outpatient Settings
that can be tailored by an outpatient oncology
facility to systematically assess personnel
adherence to recommended infection prevention practices.
•The appendix provides a list of relevant
resources, including the United States
Pharmacopeia (USP) Chapter <797>
Guidebook to Pharmaceutical Compounding—
Sterile Preparations. All oncology facilities that
provide on-site chemotherapy preparation
should follow USP guidance in consultation
with the state pharmacy board.
•The BICAPP contains an appendix where a
facility can insert a list of reportable disease/conditions specific to their state and
the appropriate contact information for their
local and state health authorities.
•A list of names of designated personnel and
their specific roles and tasks and contact
information that can be tailored to your facility
is provided as an appendix.
6.Watson JT, Jones RC, Siston AM, Fernandez JR, Martin K, Beck
E, et al. Outbreak of catheter-associated Klebsiella oxytoca and
Enterobacter cloacae bloodstream infections in an oncology chemotherapy center. Arch Intern Med 2005;165:2639−643.
7.Abe K, Tobin D’Angelo M, Sunenshine R, Noble-Wang J, Cope J,
Jensen B, et al. Outbreak of Burkholderia cepacia bloodstream
infection at an outpatient hematology and oncology practice. Infect
Control Hosp Epidemiol 2007; 28:1311-1313.
8.Kim MJ, Bancroft E, Lehnkering E, Donlan RM, and Mascola L.
Alcaligenes xylosoxidans bloodstream infections in outpatient
office. Emerg Infect Dis 2008;14:1046-1052.
Alice Y. Guh, MD, MPH, is with the Centers
for Disease Control and Prevention’s Division of
Healthcare Quality Promotion in Atlanta, Georgia.
Lisa C. Richardson, MD, MPH, is with the Centers
for Disease Control and Prevention’s Division
of Cancer Prevention and Control in Atlanta,
Georgia. Angela Dunbar, BS, is with the CDC
Foundation in Atlanta, Georgia.
w w w.apic.org | 67
68 | WINTER 2013 | Prevention
RISK:
Blood on glucose test strip vials1
Two independent laboratory analyses found blood on exterior and
interior surfaces of vials in active use in a hospital environment.
Of 51 vials tested: 2 tested positive for blood on the exterior
1 tested positive for blood on the interior
Visible blood smear on actual
glucose test strip vial collected
from clinical setting
Luminol test
positive for blood
Positive Teichmann test showing
brown crystals, indicating
presence of blood
Could this pose a risk to your patients and your clinical staff?
Q Are you routinely and consistently inspecting test strip vials for blood?
Q In addition to glucose meters, should vials be cleaned?
Q
SOLUTION:
Minim the risk with
Minimize
the only individually
th
foil-wrapped test strips2
Blood Glucose and ß-Ketone Monitoring System
PERFORMANCE THAT PROTECTS YOUR PATIENTS.
Is your institution at risk?
To learn how Abbott Diabetes Care can help minimize potential risks to your patients and staff,
contact us at 1.877.643.2098 or email adc_mychoice@abbott.com.
For In Vitro Diagnostic Use
1. Analysis funded by Abbott Diabetes Care. Fifty-one opened vials of Roche Accu-Chek Comfort Curve test strips being used in two hospitals were obtained and tested for the presence of blood. Of the 51 vials, three
vials (5.9%) tested positive for blood by two methods (luminol test and either the phenolphthalein test or Teichmann test). Two of the three vials tested positive for blood on the exterior surface of the vial; one tested
positive for blood on the interior surface. Blood detection analysis was performed in April-June 2013 by Microbe Inotech Laboratories, Inc., St. Louis, MO. Data on file at Microbe Inotech Laboratories. Reports MILB0024A and MILB-0127A. Results show blood contamination from two facilities and are provided for informational purposes only. Contamination at other facilities may vary. 2. As of June 2013 among leading hospital
brands of blood glucose test strips (Roche, Nova Biomedical and LifeScan). Source: Manufacturer’s websites.
Precision and related brand marks are trademarks of the Abbott Group of Companies in various jurisdictions.
© 2013 Abbott ART25579 Rev A 07/13
NE
W
DON’T JUST KILL MICROBES.
REMOVE THEM.
Eliminate the food sources for live pathogens.
INNOVATIVE MICROBE
REMOVING TECHNOLOGY
WITH BUILT-IN SCRUBBERS
REMOVES
99.9%
of microorganisms,
including
C. DIFF*
Introducing the Rubbermaid HYGEN™
Disposable Microfiber System.
Stop the chain of infection with the new Rubbermaid
HYGEN™ Disposable Microfiber System. It’s the only
disposable microfiber system proven to remove 99.9%
of microbes, including C. diff.*
Free samples at rubbermaidcommercial.com/99
* Based on third party testing with water only.
The product can be used with a wide array of cleaning solutions.
Heroes of Infection Prevention
Meet the
2013 Heroes of Infection Prevention
PROFILES BY MICHELE PARISI
E
ach year, APIC presents Heroes of Infection Prevention awards to members who have developed and applied innovative
infection prevention programs. Heroes and their programs represent some of the best practices in infection prevention.
Since the inception of the award in 2006, 96 individuals and groups have been recognized for their exceptional work
in reducing healthcare-associated infections.
Four Heroes are featured in this issue of Prevention Strategist. For more information on the award, visit www.apic.org/heroes.
Improving infection prevention
practices worldwide
Chandrakant Ruparelia, MD, MPH
Jhpiego (an affiliate of Johns Hopkins University)
Baltimore, Maryland
Over the past 10 years, Chandrakant
Ruparelia, MD, MPH, has helped improve
infection prevention practices in more than
20 resource-challenged countries.
Dr. Ruparelia is a senior technical advisor
at Jhpiego, an international non-profit health
organization affiliated with Johns Hopkins
University. He supports the organization’s
mission of enhancing the health and saving
the lives of women and families in limitedresource settings by providing governments
with technical assistance in infection prevention and control, family planning, HIV/
AIDS, maternal and child health, and other
health issues.
“The most important thing is to understand each country’s culture and people,”
said Dr. Ruparelia. “We never impose ourselves, but instead work hand-in-hand with
in-country colleagues. The more the local
stakeholders own a program, the more likely
it will be sustainable.”
Infection prevention program development in every country starts with advocacy
for evidence-based guidelines and grassroots
level competency-building. In Ethiopia, for
example, Dr. Ruparelia coordinated a threeday infection prevention workshop with
local thought leaders—including Ethiopian
Ministry of Health (MOH) representatives—to gain buy-in for improved practices.
Since then, he has worked with the MOH
and local medical professionals to develop
national infection prevention guidelines and
performance standards, recruit and train
more than 20 master trainers, and implement quality improvement approaches. He
and in-country colleagues also conducted
onsite infection prevention and control training for more than 600 healthcare providers
in less than six months.
In Tanzania, Dr. Ruparelia developed the
technical approach with the Jhpiego Tanzania
team for a project to improve quality of infection prevention practice in hospitals and medical schools. So far, he and local colleagues
have created national infection prevention
and control guidelines, standards, training
materials, and site strengthening approaches.
Dr. Ruparelia also hopes to establish a
Tanzanian APIC chapter and adapt the
APIC competency model to low-resource
settings.
As he tackles infection prevention challenges in widely varying cultures with
limited resources, Dr. Ruparelia remains
motivated by one thought: “At the end of
the day, if I am able to change the practices
of even one healthcare provider in a remote
area, I’m happy.”
w w w.apic.org | 71
Heroes of Infection Prevention
Acting as a powerful voice for infection
prevention in India
Sanjeev K. Singh, DCH, MD, MPhil
Amrita Institute of Medical Sciences
Kochi, Kerala, India
Faced with a staggering lack of infec-
tion prevention resources and policies in
his native India, Sanjeev Singh, DCH,
MD, MPhil, can only be described as
“undaunted.” Through relentless focus on
collaboration and best practices, Dr. Singh
has generated infection prevention practice
and policy improvements benefiting patients
and practitioners in his 1,200-bed hospital
and across India.
As the medical superintendent at the
Amrita Institute of Medical Sciences teaching hospital in Southern India, Dr. Singh is a
powerful voice for infection prevention. “Our
country has 1.2 billion people, but no national
infection control policy,” he says. “My mission
is to make people see it is important.”
Dr. Singh grew his own infection prevention department by demonstrating that good
infection-prevention practices improved his
hospital’s bottom line. He chairs the hospital’s infection control committee, which
meets weekly to review surveillance practices
and key issues.
Dr. Singh is a role model for infection
preventionists who want to affect change
beyond their own institutions, spearheading
infection prevention and control program
and policy creation at district, state, and
national levels. He initiated a district-wide
infection control certification program and
is working closely with two Indian states to
implement standardized infection prevention and control policies. “We can’t tackle all
28 states at once, so we start small,” he said.
In October 2012, Dr. Singh coordinated a
meeting between representatives from every
Indian clinical society, doctors, nurses, and
experts from the Centers for Disease Control
and Prevention (CDC), and World Health
Organization (WHO). The group developed
a declaration calling for a national Indian
infection prevention and control policy,
which they submitted to India’s National
Health Ministry.
Dr. Singh is also working toward founding APIC’s India chapter and hopes to build
India’s infection prevention and control
capacity through online and multi-state
APIC training. He is enthusiastic about
other future projects as well: a national
infection prevention and control database
and antimicrobial stewardship programs,
and an infection prevention journal, to start.
“Look outside your institution; let others
be enriched by your expertise, and you can
create broad, impactful change,” he said.
Dramatically reducing C. difficile
with best practices and leadership
Azalea Wedig, BS, CIC
The Jewish Hospital – Mercy Health
Cincinnati, Ohio
When daily surveillance revealed an
increasing rate of Clostridium difficile
(C. difficile) at her 200-bed hospital in
2009, Azalea Wedig, BS, CIC, immediately jumped into action. A microbiologist who transitioned to infection
prevention after personal experience with
72 | WINTER 2013 | Prevention
a healthcare-associated infection (HAI),
Wedig is particularly adept at connecting
the science of infection prevention to the
people most deeply affected and involved.
Wedig’s first step was to form a cross-disciplinary C. difficile performance improvement team. After a thorough review of
Establishing best practices for municipal
infectious disease prevention
Carolyn Williams, RN
City of Portland
Portland, Oregon
Carolyn Williams, RN, has spearheaded
“A group of us agreed we
needed an ‘on the street’ guide
in addition to the well-written
APIC chapter on this topic
[emergency medical services].”
comprehensive infectious-disease (ID) prevention and education programs that are
protecting the health of 7,000 municipal
workers in the city of Portland.
Williams’ responsibilities encompass the
full spectrum of municipal ID prevention,
from managing and implementing city-wide
immunization and needlestick prevention
programs to conducting department risk
assessments and evaluating waste-water
management systems. Her constituents
range from lifeguards and daycare staff to
police officers, the latter of whom absorb
about 80 percent of her time. “Police officers
are a very complex population from an ID
standpoint,” she said. “They’re exposed to
a lot of people on a daily basis. Bloodborne
pathogens are a big risk.”
Williams’ primary strategy for protecting
her diverse population is education. In 2012,
she taught 45 infection prevention classes to
almost 1,900 city employees. “I’ve learned
that the information has to be understandable and fact based,” she said. “The police
officers, in particular, always want evidence.
They say, ‘Show me.’”
Motivated by this need as well as her years
of experience in nursing and infection prevention, Williams spearheaded the development of the Guide to Infection Prevention
in Emergency Medical Services, a free APIC
implementation guide now available to emergency medical services (EMS) and public
safety personnel nationwide.
“A group of us agreed we needed an ‘on the
street’ guide in addition to the well-written
APIC chapter on this topic,” said Williams,
who serves as national chairperson of the
EMS/Public Safety Section of APIC. “There
wasn’t a lot of evidence-based literature on
this topic, but many, many people contributed, and I’m very proud of the result.”
Williams is a believer in the power of
collaboration among infection prevention
professionals. “I’m a one-person office working with limited resources; most municipal
nurses are,” she said. “We need to create
networks so our populations can benefit
from other perspectives.”
literature, data, and existing guidelines,
the team agreed to focus on three areas:
environmental services, antibiotic stewardship, and standardization of clinical care.
They committed to reduce their hospital’s
C. difficile incidence rate by 10 percent for
the first quarter of 2010.
“We didn’t do anything new,” said
Wedig. “We didn’t reinvent wheels. We
used science, best practices, and teamwork.”
Wedig and her team members systematically identified specific environmental,
pharmacy, and clinical practice behaviors
that were contributing to the hospital’s
C. difficile rates and then worked to change
them. Ongoing education and engagement
of staff, patients, visitors, and volunteers
played a significant role.
Within six months, the Jewish Hospital
C. difficile rate had dropped from 33.3 per
10,000 patient days to 15.8. By June 2011,
the rate had fallen to 3.08—half the statewide incidence rate.
“Our hospital succeeded because we
worked as a team,” said Wedig. “Infection
prevention became everyone’s business. Empowerment and encouragement
were key.”
Over the past three years, the team has
sustained the lower C. difficile rate through
staff education and recognition programs,
including an annual hospital-wide infection
prevention award.
“You have to make everyone in the facility feel like part of the infection prevention
team,” said Wedig.
The Heroes program is supported by a grant from BD.
w w w.apic.org | 73
INDEX TO ADVERTISERS
CLEANING, DISINFECTION & STERILIZATION
Rubbermaid Commercial Products . . . . . . . . . . . . . . 70
www.rubermaidcommercial.com/99
CLEANING, DISINFECTION & STERILIZATION
Clorox Healthcare . . . . . . . . . . . . . . . . . . . . . . . . 28, 59
www.cloroxhealthcare.com
Ivera Medical Corporation . . . . . . . . . . . . . . . . . . . . 51
www.curos.com
JanPak . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
www.janpak.com
Molnlycke Health Care Inc. . . . . . . . . . . . . . . . . . . . . . 9
www.molnlyckehc.com
Steriliz, LLC . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
www.steriliz.us
Vernacare . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40
www.vernacare.com
Virox Technologies Inc. . . . . . . . . . . . . . . . . . . . . . . . 13
www.viroxaccel.com
ENVIRONMENTAL SERVICES & SOLUTIONS
JanPak . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
www.janpak.com
HAND HYGIENE
CareFusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
www.carefusion.com/chloraprep
JanPak . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
www.janpak.com
INFECTION PREVENTION PRODUCTS
& SERVICES
Abbott Diabetes Care . . . . . . . . . . . . . . . . . . . . . . . . 69
www.abbott.com
74 | WINTER
2013 | Prevention
666514_Editorial.indd
1
Association for Professionals in Infection
Control and Epidemiology . . . . . . Outside Back Cover
www.apic.org/partners
BD Diagnostics . . . . . . . . . . . . . . . . Outside Back Cover
www.bd.com/ds/labefficiency
Eloquest Healthcare
www.mastisol.com . . . . . . . . . . . . . . . . . . . . . . . . . 68
www.ReliaFitDevice.com . . . . . . . . . Inside Back Cover
Metrex . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46
www.Metrex.com/Prevent
Nanosonics Limited . . . . . . . . . . . . . . . . . . . . . . . . . 32
www.nanosonics.us
PDI, Professional Disposables
International . . . . . . . . . . . . . . Inside Front Cover, 19
www.PDIBeTheDifference.com
Sanuvox Technologies Inc. . . . . . . . . . . . . . . . . . . . . 20
sBioMed LLC . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58
www.steriplex.com
XSTREAM Infection Control . . . . . . . . . . . . . . . . . . . 11
www.xstreaminfectioncontrol.com
INFECTION PREVENTION SOLUTION - CONSULTING
3M . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52
www.3m.com/Ioban
JanPak . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
www.janpak.com
Xenex Healthcare Services . . . . . . . . . . . . . . . . . . . . 64
www.xenex.com
INFECTION RESISTANT COATING
Somay Products, Inc. . . . . . . . . . . . . . . . . . . . . . . . . 56
www.somay.com/steri-shield/steri-shield.html
LABORATORY SERVICES
Special Pathogens Laboratory . . . . . . . . . . . . . . . . . 42
www.specialpathogenslab.com
MANAGING INFECTION RISK
DNV Business Assurance . . . . . . . . . . . . . . . . . . . . . . 5
www.dnvcert.com
MEDICAL DEVICES & INSTRUMENTS
3M . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
wwwgo.3m.com/clippers
Association for Professionals in Infection
Control and Epidemiology . . . . . . Outside Back Cover
www.apic.org/partners
Eloquest Healthcare
www.mastisol.com . . . . . . . . . . . . . . . . . . . . . . . . . 68
www.ReliaFitDevice.com . . . . . . . . . Inside Back Cover
Ivera Medical Corporation . . . . . . . . . . . . . . . . . . . . 50
www.curos.com
Retractable Technologies, Inc. . . . . . . . . . . . . . . . . . 43
www.vanishpoint.com
SKIN & WOUND CARE PRODUCTS
Eloquest Healthcare
www.mastisol.com . . . . . . . . . . . . . . . . . . . . . . . . . 68
www.ReliaFitDevice.com . . . . . . . . . Inside Back Cover
07/11/13 4:11 PM
>> > > >> ReliaFit reduces the risk of CAUTIs
associated with indwelling catheters1
s.ONINVASIVEDESIGN1
ReliaFit offers a superior alternative
to condom catheters
s5NIQUEDESIGNFORSUPERIOR
LEAKPREVENTION2
s0ROTECTSSENSITIVESKIN1
s/NESIZElTSALL1
Contact your sales consultant,
call 866.329.4149, or visit
ReliaFitDevice.com to learn
more about ReliaFit
3FGFSFODFT6SJOBSZ0VUQVU.POJUPSJOHBOE.BOBHFNFOUJO"DDVUF
$BSF$MJOJDBM1BUIXBZGPS$.4$PNQMJBODFBOE1PTJUJWF&DPOPNJD*NQBDUPG
$PNQMJBODFXIJUFQBQFS
IUUQNFOTMJCFSUZDPNIFBMUIQSPGFTTJPOBMTSFEVDFVUJXJUI
NFOTMJCFSUZ"DDFTTFE.BZ-VDBT-.*TFMFS+(BMF-&WBMVBUJPOPGBOFX
OPWFMNBMFFYUFSOBMVSJOBSZNBOBHFNFOUEFWJDF1PTUFSQSFTFOUFEBU$MFWFMBOE$MJOJDT4QSJOH
80$/VSTJOH4ZNQPTJVN"QSJM$MFWFMBOE0)
ReliaFitTM is a trademark of Ferndale IP, Inc.
©2013 Eloquest Healthcare®, Inc
BD MAX™ System
For Molecular Detection of Healthcare Associated Infections
2013 APIC Strategic Partner
BD is proud to support
Infection Preventionists
worldwide as a 2013 APIC
Strategic Partner.
Visit www.apic.org/partners
f
X™ Cdif
BD MA
A
NOW FD !
D
CLEARE
The BD MAX System gives your hospital
the ability to quickly respond to
Healthcare Associated Infections
BD MAX™ MRSA
1
Enables active surveillance for methicillin-resistant Staphylococcus aureus
2
This product is not available for sale or use in the U.S.
This product is for Research Use Only and is
not for use in diagnostic procedures.
BD MAX™ Cdiff
Detection of toxin B gene (tcdB) found in toxigenic Clostridium difficile
BD MAX™ StaphSR1
Designed to detect Staphylococcus aureus and methicillin-resistant
Staphylococcus aureus from nasal swabs
BD MAX™ CRE RUO2
Research Use Only assay designed to detect three antimicrobial
resistant genes (KPC, OXA-48 and NDM) found in carbapenemresistant Enterobacteriaceae (CRE)
BD Diagnostics
7 Loveton Circle
Sparks, MD 21152-0999
800.638.8663
www.bd.com/ds/labefficiency
BD, BD Logo and BD MAX are trademarks of
Becton, Dickinson and Company. © 2013 BD