Slide Template 1
advertisement

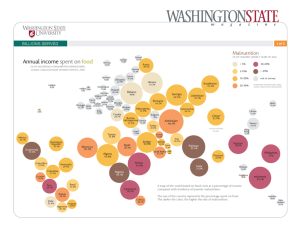
9/14/2011 The Skeleton’s Out: A Standardized Approach to the Recognition and Documentation of Malnutrition Jane White, PhD, RD, FADA Annalynn Skipper, PhD, RD, FADA September 25, 2011 Objectives • Review the development of evidence-based/consensus ADA / A.SP.E.N. Committees • ADA Malnutrition Workgroup • ASPEN Malnutrition Task determined characteristics of malnutrition • Promote the characteristics standardized use • Encourage data collection to validate this approach to malnutrition diagnosis and characterization Force – Maree Ferguson MBA, PhD, RD – Annalynn Skipper, MS, PhD, RD, FADA – Louise Merriman, MS, RD, CDN – Terese Scollard MBA, RD, LD – Sherri Jones MS, MBA, RD, LDN – Ainsley Malone, MS, RD, LD, CNSD – Nilesh Mehta, MD, DCH – Jane White PhD, RD. FADA, LDN, Chair – Steve Plogsted, PharmD, RPh, BCNSP – Staff: Pam Michael, MBA, RD, – Annalynn Skipper, PhD, RD, FADA – Staff: Marsha Schofield, PhD, RD – Jennifer Wooley, MS, RD, CNSD – Gordon L. Jensen, MD, PhD, Co-Chair – Ainsley Malone, MS, RD, CNSC, Co-Chair – Rose Ann Dimaria, PhD, RN, CNSN – Christine M. Framson, RD, PHD, CSND – Jay Mirtallo, RPh, BCNSP Board Liasion – Staff: Peggi Guenter, PhD, CNSN In-Patient Prospective Payment System – MS-DRGs • 1983 –Diagnosis Related Groups (DRGs) – Malnutrition recognized as a secondary diagnosis or “cc” (complication / co-morbid condition) – DRG relative weights on estimated hospital costs, rather than charges. (Medicare & Medicaid) • 2007 – Medical Severity DRG (MS DRGs) – Recognize malnutrition as impacting acuity and severity of patients, so reimbursement may be increased due to increased cost of care Rationale for Developing ADA/A.S.P.E.N Characteristics to Identify Malnutrition: • No standardization • Multiple Definitions • Multiple Diagnostic (ICD-9)Codes • Multiple characteristics used to Diagnosis • Limited evidence base • Emerging role of inflammation • Influence on Assessment Parameters • Influence on Response to Nutrition Intervention • Anti-inflammatory Interventions / Nutrition interventions outcomes divergence 1 9/14/2011 A Vision for the Identification of Malnutrition in all Settings Wouldn’t it be amazing to have standardized definitions/characteristics and to know the prevalence of Adult Malnutrition in… Our Country Our Health System Our Our World World Rationale for Developing Characteristics to Identify Malnutrition Hospital chain, under scrutiny, reports rare illness • February 20, 2011 • By LANCE WILLIAMS, CHRISTINA JEWETT and STEPHEN K. DOIG California Watch • Redding, near Mount Shasta, and Victorville, in the Mojave Desert, have little in common but an unusual statistic: In each city, a hospital has reported alarming rates of a Third World nutritional disorder among its Medicare patients. • Kwashiorkor -- a Ghanaian word for "weaning sickness" -- almost exclusively afflicts impoverished children in developing countries, especially during famines, experts say. ADA/A.S.PE.N Member Inquiries Poll Question 1 • ADA/A.S.P.E.N have received numerous requests from •Do you use Albumin in RDs, physicians, nurses and other professionals: • How to diagnose malnutrition • How to document malnutrition diagnosing/documenting malnutrition? Yes No • Correlation of current IDNT definitions with existing diagnostic coding terminology • Which characteristics to use Why not serum proteins (albumin / prealbumin, etc.)??? Poll Question 2 •Do you use prealbumin in documenting/diagnosing malnutrition? Yes No Why not serum albumin/visceral proteins? Gordon Jensen, MD, PhD • Acute Phase Response – Inflammatory disease, illness, injury elicit cytokinemediated response – Interleukin-1(IL-1), interleukin-6 (IL-6), tumor necrosis factor (TNF) – Alter hormone secretion and target organ function – Favor a catabolic state 2 9/14/2011 Why not serum albumin/visceral proteins? Gordon Jensen, MD, PhD •Acute Phase Metabolic Response – Elevation of resting energy expenditure Poll Question 3 •Do you use C Reactive Protein to interpret albumin or prealbumin? – Export of amino acids from muscle to liver Yes – Increase in gluconeogenesis No – Expansion of extracellular fluid – Shift toward production of positive acute phase reactants, i.e. CRP Why not serum albumin/visceral proteins? Why not serum albumin/visceral proteins? Gordon Jensen, MD, PhD Body down regulates albumin synthesis so that urgently needed proteins for immune, clotting, and wound healing functions can be made. • Positive - antibodies, complement, C-reactive protein, and fibrinogen • Negative - albumin, transferrin, prealbumin, retinol binding protein – Over the short run the acute phase metabolic response with resulting catabolism is likely an appropriate adaptive response. – If the underlying stressor is severe, protracted or repeated, then adverse outcomes will result. Roles of cytokines in muscle regulation in inflammation Gordon Jensen, MD, PhD Gordon Jensen, MD, PhD • Malnourished individuals (pure semi-starvation) may exhibit normal visceral proteins (anorexia nervosa). • Obese persons in diet programs with low protein and energy intakes and resulting weight loss may exhibit normal proteins. – Changes in body cell mass correlate poorly with visceral proteins. – Changes in dietary intake correlate poorly with visceral proteins. – Sick people eat less. • Other disease states impact visceral protein synthesis or losses. – Volume status can limit interpretation. – Protracted half-life of albumin renders it insensitive to measure changes in status. – Prealbumin suffers most of the same limitations but has a shorter half-life. Inflammation promotes--Gordon Jensen, MD, PhD – Metabolic dysregulation • Promote muscle catabolism • Inhibition of protein synthesis and muscle repair • Trigger apoptosis – programmed cell death • Influence contractility and function – Hyperglycemia – Decreased visceral proteins – Muscle catabolism – Edema – Anorexia – Malaise / deconditioning • Nutrition alone is ineffective in preventing muscle protein loss in inflammation Inflammation can blunt favorable responses to nutrition intervention 3 9/14/2011 “Practical” Indicators of Inflammation? Gordon Jensen, MD, PhD • Lab ADA Evidence Analysis: Albumin/Prealbumin • ADA Evidence Analysis Library Resources on Albumin and – Albumin, prealbumin Prealbumin: – C-reactive protein (CRP) http://www.adaevidencelibrary.com/conclusion.cfm?conclusi on_statement_id=251 263&highlight=albumin&home=1 – Cytokines - IL-6 – Procalcitonin • Clinical signs – Fever, leukocytosis, hyperglycemia http://www.adaevidencelibrary.com/conclusion.cfm?conclusi on_statement_id=251 313&highlight=prealbumin&home=1 Clinical Diagnostic Expertise Needed ADA Evidence Analysis: Albumin/Prealbumin • Does serum albumin correlate with weight loss in four models of prolonged protein-energy restriction: anorexia nervosa, non-malabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation? – In the four models of prolonged protein-energy restriction, there was no correlation between serum albumin and weight loss. – Grade II • Does serum prealbumin correlate with weight loss in four models of prolonged protein-energy restriction: Anorexia nervosa, non-malabsorptive gastric partitioning bariatric surgery, calorie-restricted diets or starvation? Proposal by ADA/A.S.P.E.N. to NCHS JPEN 2009; 33:710-716; JPEN 2010: 34:156-9 • Define the characteristics of adult malnutrition syndromes in developed countries using an etiology-based approach that incorporates an appreciation of the continuum of inflammatory response. • Recognize the contributors to the development of malnutrition: – Semi starvation – Inability to assimilate nutrients consumed – Systemic inflammatory response – In the four models of prolonged protein-energy restriction, there was no correlation between serum prealbumin and weight loss. – Grade III ADA/A.S.P.E.N. Joint Recommendation to NCHS - Results-to-Date •The National Center for Health Statistics (NCHS) has received multiple Etiology Based Malnutrition Definitions requests to clarify the malnutrition diagnosis codes and use of the codes Nutritional Risk Identified • ADA and A.S.P.E.N. submitted recommendations (September 2010 and Compromised intake or loss of body mass. March 2011public hearings) • Current decision regarding the proposed revisions to the existing malnutrition code definition(s). Jensen GL. JPEN 2009;33:710 Inflammation present? No / Yes – No change at this time to 262 (severe Malnutrition) and 263 (Other and unspecified protein-calorie malnutrition) • ICD-9/ICD-10 transition in 2014 – new codes possible at this time • Continue to try to identify language that allows development of pre-coordinated codes – Language to qualify the use of kwashiorkor and marasmus • Pediatric populations • Poorly resourced countries, typically Yes No Starvation Related Malnutrition (pure chronic starvation, anorexia nervosa) Mild to Moderate Degree Chronic Disease – Related Malnutrition (organ failure, pancreatic cancer, rheumatoid arthritis, sarcopenic obesity) Yes Marked Inflammatory Response Acute Disease or InjuryRelated Malnutrition (major infection, burns, trauma, closed head injury) 4 9/14/2011 Consensus Regarding Malnutrition Definition Characteristics to Identify Malnutrition • Constraints: • ADA Workgroup agrees with the A.S.P.E.N./International Work Group’s etiologically–based system of malnutrition classification that recognizes the influence of inflammation on nutritional status • A.S.P.E.N.’s Malnutrition Workgroup has accepted the ADA Workgroup’s proposed characteristics. • Basic parameters (hallmarks, few in total #) • Support diagnosis of malnutrition • Characterize severity • as nutritional status changes • Evidence-based (when possible) / expert opinion • Will change over time as evidence of validity accrues • Any 2 or more characteristics may be used to identify Malnutrition Characteristics to Identify Severe Malnutrition Characteristics to Identify Non-Severe (moderate) Malnutrition • Evidence of Reduced Intake • Evidence of reduced Intake – Compromised intake of varying degree and duration • > 5 days with intake of < 50% of total estimated energy requirement (acute illness/injury category) • > 1 month with intake of <75% total estimated energy intake (chronic disease category) – Compromised intake of varying degree and duration – Evidence of suboptimal intake • > 7 days with a nutrient intake of <75% of total estimated energy requirements (acute injury/illness category) • > 1month days with a nutrient intake of <75% of total estimated energy requirements (chronic illness/condition category) • > 1 month with intake of < 50% total estimated energy intake (environmental/social circumstances category) • > 3 months with a nutrient intake of < 75% of total estimated energy requirements (environmental/social circumstances categories) • avoid contributing to iatrogenic malnutrition in these patients* • avoid contributing to iatrogenic malnutrition in these patients * A number of people with acute or chronic illness/trauma may present as “apparently healthy” without prior history of malnutrition or chronic disease. As such, unintended weight change and inability to eat may be the main parameters of significance, although the presence of low or excessive BMI, when present, could signify increased risk. People with illness/trauma may present as “apparently healthy” without prior history of malnutrition or chronic disease. As such, inability to eat and unintended weight change may be the parameters of significance for people in this category also, although the presence of low or excessive BMI, when present, could signify increased risk. Characteristics to Identify Severe Malnutrition Characteristics to Identify Non-Severe (moderate) Malnutrition •Unintended Weight Loss • Unintended Weight Loss • Interpretation of Percent Weight Loss** Severe (%) Time >2 1 week >5 1 month > 7.5 3 months >10 6 months > 20 1 year • Interpretation of Percent Weight Loss** Significant (%) **Height, weight and usual weight need to be obtained in order to determine the percentage and interpret the significance of weight loss. Time 1- 2 1 week 5 1 month 7.5 3 months 10 6 months 20 1 year **Height, weight and usual weight need to be obtained in order to determine the percentage and interpret the significance of weight loss 5 9/14/2011 Characteristics to Identify Malnutrition Characteristics to Identify Malnutrition • Changes in Body Composition – Muscle Loss Changes in Body Composition » Loss of lean mass at temples (temporalis muscle); clavicles (pectoralis & deltoids); shoulders (deltoids); interosseous muscles; scapula (latissimus dorsi, trapezius, deltoids); thigh (quadriceps) and calf (gastrocnemius – Loss of Subcutaneous Fat » orbital, triceps, fat overlying the ribs » Mild in non-severe malnutrition » Moderate to severe in severe malnutrition » Mild in non-severe malnutrition » Moderate to severe in severe malnutrition Mild Characteristics to Identify Malnutrition Assessing Changes in Body Composition Changes in Body Composition • Assessing Edema, 2 methods: – 1+ Mild pitting, slight indentation, no perceptible swelling (2mm) • Fluid accumulation## – 2+ Moderate pitting, indentation subsides rapidly (4mm) – Localized (extremities or scrotal edema) – 3+ Deep pitting, indentation remains a short time, extremity looks swollen (6mm) – Generalized fluid accumulation - clinically evident edema on examination »Mild in non-severe malnutrition Severe – 4+ Very deep pitting, indentation lasts a long time, extremity is very swollen (8mm) • Or »Moderate to severe in severe malnutrition – 1+ if the pitting lasts 0 to 15 sec – 2+ if the pitting lasts 16 to 30sec ## May mask – 3+ if the pitting lasts 31 to 60sec weight loss, might be reflected as weight gain – 4+ if the pitting lasts >60sec Assessing Changes in Body Composition Characteristics to Identify Malnutrition • Assessing/Documenting Changes in Body Composition: • Measures of Physical Function/Performance – (for each trait specify: 0 = normal, 1+ = mild, 2+ = moderate, 3+ = severe) •# •# •# •# •# __________loss of subcutaneous fat (triceps, ribs, orbital) __________muscle wasting (quadriceps, deltoids, etc.) __________extremity edema (hand/arm, ankle/leg) __________vulvar/scrotal edema __________generalized edema • • • • • • (proxy for lean mass?) Hand Grip Strength * • • • • Dynamometer Standards (excellent, good, average, fair, poor) for dominant hand by gender and age Maximum reading (kg) from 3 attempts, allow 1 minute rest between attempts Measurably reduced 4-meter/other walk tests ^ Stair climbing/chair rising/balance ^ Peak Expiratory Flow/Lung Function Parameters being explored Fair results - Moderate Malnutrition Poor results – Severe malnutrition *Strongest correlation to date with muscle mass and nutritional status ^ Elderly populations 6 9/14/2011 ADA/ A.S.P.E.N. Caveats Questions • Characteristics to Identify Malnutrition • Work in progress • Parameters may change over time • Evidence to support their appropriateness • collected and evaluated on a broad scale – start data collection now • Impact of inflammation on • nutrient requirements/utilization • response to nutrition intervention • clinical markers of inflammation most relevant in malnutrition • All are yet to be determined ADA/A.S.P.E.N. Malnutrition Workgroup c/o Jane V. White, PhD, RD, Chair ADA MN-WG at: jwhite13@uthsc.edu Marsha Schofield, MS, RD, ADA staff liaison at: mschofield@eatright.org Ainsley Malone, MS, RD, CNSC, Co-Chair A.S.P.E.N. Malnutrition Task Force at: ainsleym@earthlink.net Bibliography 1. Jensen GL, Bistrian B, Roubenoff R, Heimburger DC. Malnutrition syndromes: a conundrum vs continuum. JPEN Nov-Dec 2009;33:710-716. 2. Jensen GL, Mirtallo J, Compher C, et al. Adult starvation and disease-related malnutrition: a proposal for etiologybased diagnosis in the clinical practice setting from the International Consensus Guideline Committee. JPEN Mar-Apr;34:156-159. 3. Norman K, Stobaus N, Gonzalez MC, Schulzke J-D, Pirlich M. Hand grip strength : Outcome predictor and marker of nutritional status. Clinical Nutrition. 2011;30:135-142. 7