MALE REPRODUCTIVE
SYSTEM
Reproductive System
To Accompany: Anatomy and Physiology Text and
Laboratory Workbook, Stephen G. Davenport, Copyright
2006, All Rights Reserved, no part of this publication can be
used for any commercial purpose. Permission requests
should be addressed to Stephen G. Davenport, Link
Publishing, P.O. Box 15562, San Antonio, TX, 78212
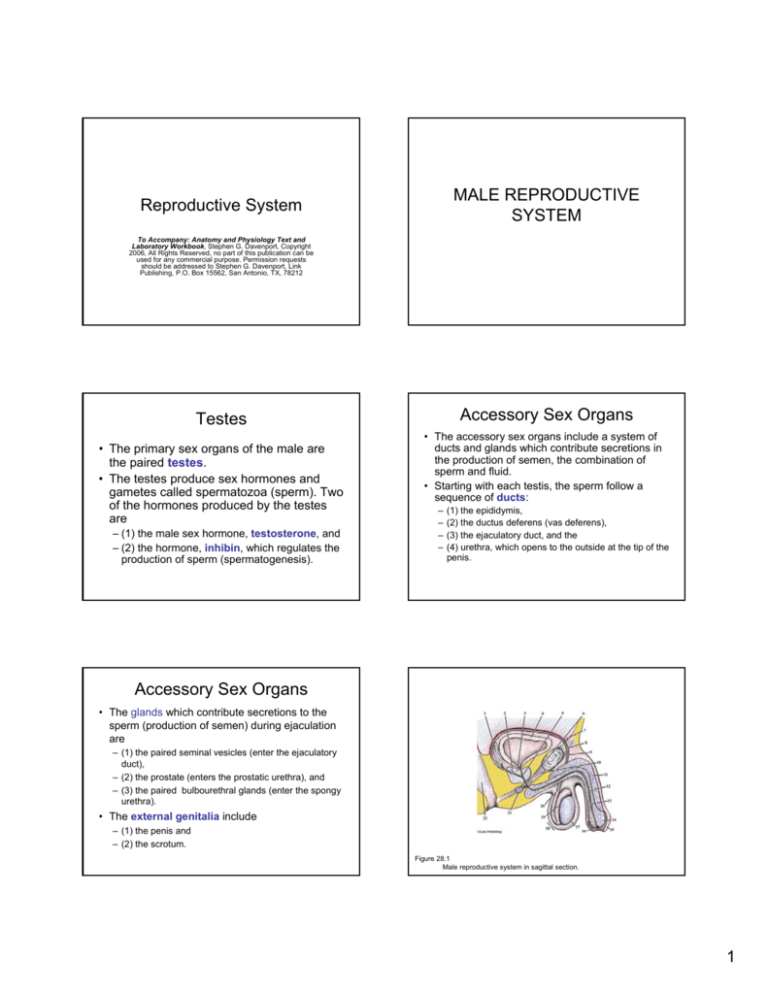
Accessory Sex Organs
Testes
• The primary sex organs of the male are
the paired testes.
• The testes produce sex hormones and
gametes called spermatozoa (sperm). Two
of the hormones produced by the testes
are
– (1) the male sex hormone, testosterone, and
– (2) the hormone, inhibin, which regulates the
production of sperm (spermatogenesis).
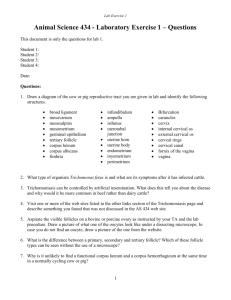
• The accessory sex organs include a system of
ducts and glands which contribute secretions in
the production of semen, the combination of
sperm and fluid.
• Starting with each testis, the sperm follow a
sequence of ducts:
–
–
–
–
(1) the epididymis,
(2) the ductus deferens (vas deferens),
(3) the ejaculatory duct, and the
(4) urethra, which opens to the outside at the tip of the
penis.
Accessory Sex Organs
• The glands which contribute secretions to the
sperm (production of semen) during ejaculation
are
– (1) the paired seminal vesicles (enter the ejaculatory
duct),
– (2) the prostate (enters the prostatic urethra), and
– (3) the paired bulbourethral glands (enter the spongy
urethra).
• The external genitalia include
– (1) the penis and
– (2) the scrotum.
Figure 28.1
Male reproductive system in sagittal section.
1
Male Reproductive System
• Scrotum
– The scrotum is the pouch that contains the testes.
The scrotum is divided into halves by a midline
septum for the housing of the right and left testes.
• Testes
– The paired testes produce sperm and hormones.
– Seminiferous tubules are located within the testes
and are the sites of the production of sperm and the
hormone, inhibin, which is involved in the regulation
of sperm production.
– Located in the connective tissue surrounding the
seminiferous tubules are the interstitial (Leydig) cells
which produce the sex hormone, testosterone.
Male Reproductive System
• Seminal vesicles
– The paired seminal vesicles are located posterior to the bladder.
The alkaline fluid produced by each seminal vesicle is
transported to an ejaculatory duct by each seminal vesicle’s
duct. During ejaculation, seminal fluid and sperm mix in the
ejaculatory duct and are propelled into the urethra (prostatic).
• Urethra
– The urethra is the tube that serves both the urinary and
reproductive systems and is divided into three regions,
– (1) the prostatic urethra (passes through the prostate gland)
– (2) the membranous urethra (passes through the urogenital
diaphragm)
– (3) the spongy urethra (passes through the penis and opens to
the exterior)
Male Reproductive System
• Epididymis (pl. epididymides)
– An epididymis is located posterior to each testis. The epididymis
receives sperm from the testis and is the site where the sperm
are stored and develop motility. During ejaculation, smooth
muscle contractions within the walls of its tubules force sperm
into the ductus (vas) deferens.
• Ductus (vas) deferens (pl. vasa deferentia)
– The ductus deferens is the tube that transports sperm from the
epididymis to the ejaculatory duct. The paired ejaculatory ducts,
are located within the prostate. Each is formed by the union of a
ductus deferens and a duct from a seminal vesicle. An
ejaculatory duct propels sperm (from the vas deferens) and the
secretions from a seminal vesicle into the urethra (prostatic).
Male Reproductive System
• Prostate gland
– The prostate gland is located inferior to the bladder
and surrounds the urethra (prostatic).
– It produces an alkaline fluid that during ejaculation
enters the urethra (prostatic) through several small
openings.
• Bulbourethral glands
– The paired bulbourethral glands are located inferior to
the prostate. They secrete an alkaline fluid that
enters the spongy (penile) urethra.
Male Reproductive System
• Penis
– The penis is attached by its proximal portion called
the root. The root leads to the body (shaft) that
terminates in the glans penis.
– The glans penis is surrounded by the prepuce
(foreskin) unless the prepuce was removed by a
procedure called circumcision.
– The body of the penis consists of three regions of
erectile tissue, two dorsal corpora cavernosa (only
one corpus cavernosum is seen in a sagittal section)
and a medial corpus spongiosum. The corpus
spongiosum surrounds the spongy (penile) urethra.
– The glans penis surrounds the terminus of the
urethra, the external urethral orifice.
TESTES
The testes are located in the scrotum.
They are slightly oval shaped and
average about two inches in length and
one inch in width.
2
Testes
Lab Activity 1 - Testes
• Each testis is surrounded by two layers of
connective tissues, the
– (1) tunica vaginalis- forms a capsule (lined with
serous membranes) which surrounds the testis
– (2) tunica albuginea- lines the surface of the testis. A
portion of the tunica albuginea folds into the testis and
divides it into many compartments called lobules.
Each lobule consists of one to three coiled
seminiferous tubules, which contain the germinal
(spermatogenic) epithelium.
Lab Activity 1 - Testes
Figure 28.3
Scanning power photograph of a cross section of a testis (rat). The testis
houses numerous highly convoluted seminiferous tubules and interstitial cells.
Lab Activity 1 - Testes
• Tunica albuginea
– The tunica albuginea is the connective tissue
layer covering the surface of the testis.
• Interstitial (Leydig) cells
– The interstitial (Leydig) cells are located in the
connective tissue around the seminiferous
tubules. The interstitial (Leydig) cells are
endocrine in function and produce the
hormone testosterone.
Figure 28.2
Scanning power photograph of a section of a testis and its associated
epididymis. The testis houses numerous highly convoluted seminiferous tubules.
Lab Activity 1 - Testes
Figure 28.4
Scanning power photograph of a portion of a longitudinal section of a
testis (human) showing its organization into lobules. Each lobule contains one to
three highly convoluted seminiferous tubules
Lab Activity 1 - Testes
• Seminiferous tubules
– The seminiferous tubules are the convoluted tubules
within the testis where sperm production occurs by
the process called spermatogenesis.
– Additionally, the seminiferous tubules are the sites of
the production of the regulatory hormone called
inhibin. The tubules are associated with connective
tissues, lymphatic vessels, blood vessels (capillaries
are especially abundant), and interstitial (Leydig)
cells.
3
Lab Activity 1 - Testes
• Spermatogenesis
– Spermatogenesis is the process of the production of
the male gametes, the spermatozoa, or sperm.
– Spermatogenesis involves
• the meiotic division of primary spermatocytes to secondary
spermatocytes (meiosis I),
• the meiotic division of the secondary spermatocytes to
spermatids (meiosis II), and the
• transformation of the spermatids into spermatozoa
(spermiogenesis).
• Spermiogenesis
– Spermiogenesis is the process of transformation of
spermatids into spermatozoa.
MEIOSIS
and Gamete Production
Meiosis is nuclear division in gamete
producing cells that results in a reduction in
the number of chromosomes from diploid (2n)
to haploid (n).
Meiosis
Meiosis
• In meiosis, one of each pair of
homologous chromosomes is distributed
to a daughter cell.
• Haploid daughter cells function as
gametes, sperm and eggs.
• The number of chromosomes that are
found in the somatic (body) cells of the
organism is referred to as the diploid
number (2n). The diploid number of
chromosomes in humans is 46.
• Each chromosome has a homologous
chromosome, a chromosome that carries the
same genes (mostly). Thus, in humans there are
23 pairs of homologous chromosomes.
• The set of one each of the homologous
chromosomes, or the set of different
chromosomes, is described as the haploid (n)
number.
• The haploid chromosome number for the human
is 23 chromosomes, and it is this number found
in the sperm and egg.
• Before meiosis begins, the chromosomes are
replicated
• Meiosis is divided into meiosis I and meiosis II
Meiosis I
Meiosis I
• Meiosis I
– In meiosis I, the replicated homologous chromosomes
are paired, an event called synapsis.
– During synapsis crossing-over of portions of the
chromosomes (chromatids) occurs.
– After crossing-over occurs, the pairs are separated,
and one replicated chromosome (a homologous
chromosome) is distributed to each daughter cell.
• Thus, the daughter cells (n) of Meiosis I have
only one of each type of replicated chromosome.
Figure 28.5
4
Meiosis II
Meiosis II
• Entering into meiosis II are the daughter cells from
meiosis I.
• These cells have one of each type of chromosome (one
homolog) in the replicated form (a replicated
chromosomes consists of two sister chromatids).
• In meiosis II, the sister chromatids are separated and
one of each sister chromosome is distributed to the
daughter cells. Thus, the daughter cells, which function
as gametes, have only one of each homologous
chromosome.
• The gametes are haploid (n). Fusion of the gametes, a
sperm and an egg, during fertilization produces the
diploid (2n) number of chromosomes and produces a
single cell called a zygote.
Figure 28.5
Meiosis - Spermatogenesis
• Spermatogenesis is the process of male gamete
(sperm) production. Spermatogenesis occurs in the
seminiferous tubules of the testis.
• Precursor (stem) cells called spermatogonia, located at
the periphery of the seminiferous tubules, undergo
mitotic divisions. Some of the daughter cells remain at
the periphery of the tubules as precursor cells. Others
differentiate into primary spermatocytes (2n.)
• Primary spermatocytes enter meiosis I and produce two
haploid daughter cells called secondary spermatocytes
(n.)
• The two secondary spermatocytes enter meiosis II and
each produces two haploid spermatids (n.)
• Spermatids undergo a process of transformation called
spermiogenesis and develop into spermatozoa
(sperm.)
Meiosis - Spermatogenesis
Figure 28.6
Spermatogenesis is the process of male gamete production. Meiosis reduces
the diploid human chromosome number of 46 to the haploid number of 23. Meiosis
assures that each of the gametes contains only half of the homologous chromosomes.
Lab Activity 2 – Testis
Lab Activity 2 – Testis
Spermatogenesis - Microscopic Study
Spermatogenesis - Microscopic Study
Figure 28.7
Section of testis showing seminiferous tubules, c.s.
Figure 28.8
High power photograph of a seminiferous tubule (rat) showing cell
division. Dividing cells are not always observed in testis preparations.
5
Lab Activity 2 – Testis
Lab Activity 2 – Testis
Spermatogenesis - Microscopic Study
Spermatogenesis - Microscopic Study
Figure 28.9
Low power photograph of a seminiferous tubule. The specific identification of the
cell types is difficult and is based mostly by their sequence of development.
Figure 28.10
High power photograph of a seminiferous tubule (rat) showing sustentacular cells
and spermatogenic cells. The cells are mostly identified by the location and shape
of their nuclei. Interstitial cells are located around the seminiferous tubule.
Sustentacular cells
Sustentacular cells
• The sustentacular cells are permanent residents
of the germinal epithelium and undergo very little
if any cell division.
• The sustentacular cells occupy the space
between the outer margin of the seminiferous
tubule and its lumen. The sustentacular cells
partially invest the spermatogenic cells, which
causes the spermatogenic cells to be located
between the plasma membranes of adjacent
sustentacular cells.
• Sustentacular cells function to support the
cells of spermatogenesis, and thus, are often
called “nurse” cells.
• In addition to metabolically supporting the
spermatogenic cells, sustentacular cells function
to support spermatogenesis by the production of
the blood-testis barrier.
• The blood-testis barrier is necessary to prevent
an auto-immune response toward the haploid
spermatogenic cells located toward the lumen of
the seminiferous tubule.
• The fusion of the membranes of the adjacent
sustentacular cells divides the seminiferous
tubes into an outer basal compartment and an
inner luminal compartment.
Sustentacular cells
Sustentacular cells
Figure 28.11
Sustentacular cells fuse by tight junctions to form a blood-testis barrier.
The sustentacular cells fuse to divide the seminiferous tubule into a basal
compartment and a luminal compartment. The inner luminal compartment, which
contains haploid cells, has no direct blood exchange.
Figure 28.11
Sustentacular cells fuse by tight junctions to form a blood-testis barrier.
The sustentacular cells fuse to divide the seminiferous tubule into a basal
compartment and a luminal compartment. The inner luminal compartment, which
contains haploid cells, has no direct blood exchange.
6
Follicle Stimulating Hormone (FSH)
MALE HORMONAL
REGULATION
Follicle-stimulating hormone
(FSH)
Follicle Stimulating Hormone (FSH)
• Sustentacular Cells
• The sustentacular cells also function in the
regulation of spermatogenesis by responding to
blood levels of follicle stimulating hormone
(FSH).
• FSH promotes the release of androgen binding
protein (ABP) from the sustentacular cells.
– Androgen binding protein targets the spermatogenic
cells and results in their increased uptake of
testosterone. Increased stimulation of the
spermatogenic cells by testosterone results in an
increased rate of spermatogenesis
Follicle Stimulating Hormone (FSH)
• Sustentacular Cells
• Sustentacular cells also release the hormone
inhibin, which functions in the regulation of the
release of follicle stimulating hormone (FSH)
from the anterior pituitary gland.
– Increased stimulation of the sustentacular cells by
FSH, increases inhibin release, which by negative
feedback targets the hypothalamus, reduces the
release of GnRH, which reduces the release of FSH.
– Decreased levels of inhibin result in hypothalamic
increase of gonadotropin-releasing hormone (GnRH),
which results in an increase of follicle-stimulating
hormone (FSH).
Luteinizing hormone (LH)
• Luteinizing hormone (LH) is produced and
released from the anterior pituitary gland (pars
distalis).
• Luteinizing hormone (LH) targets the interstitial
cells of the testes and increases the release of
testosterone.
• Negative feedback controls the secretion of
luteinizing hormone (LH). Increased levels of
testosterone result in hypothalamic reduction of
gonadotropin-releasing hormone (GnRH).
Figure 28.12
Follicle-stimulating hormone (FSH) is
produced and released from the
anterior pituitary (pars distalis).
Follicle-stimulating hormone (FSH)
targets the sustentacular cells.
Sustentacular cells release androgen
binding protein (ABP) and inhibin.
Androgen binding protein targets the
spermatogenic cells and inhibin
targets the hypothalamus.
Luteinizing Hormone (LH)
Figure 28.13
The release of luteinizing hormone
from the anterior pituitary is regulated
by gonadotropin-releasing hormone
(GnRH). Luteinizing hormone (LH) is
produced and released from the
anterior pituitary (pars distalis).
Luteinizing hormone (LH) targets the
interstitial cells to increase
testosterone production.
7
Spermatozoa (Sperm)
SPERMATOZOA (SPERM)
Spermatozoa are the gametes of
the male.
Spermatozoa (Sperm)
• Head of Sperm
– The head of the spermatozoon contains the
nucleus of the cell.
– A structure called the acrosomal cap (or
acrosome) is located at the tip of the head.
The acrosomal cap releases enzymes which
function in the penetration of the egg.
• The nucleus of each sperm contains one
of each homologous chromosome for a
total of 23 chromosomes.
• A spermatozoon is divided into three
regions, a
– head,
– midpiece, and the
– tail.
Spermatozoa (Sperm)
• Midpiece of Sperm
– The midpiece of the spermatozoon is connected to the head by a
short neck.
– The neck is the origin of the microtubules which pass through
the center of the midpiece into the tail, or flagellum. Numerous
mitochondria are located at the periphery of the microtubules
and provide the energy (ATP) to drive the movement the
microtubules.
– The movement of the microtubules results in the movement of
the tail (flagellum). Simple sugars such as fructose are absorbed
from the fluid surrounding the spermatozoa and serve as the
primary fuel molecule in the production of ATP.
• Tail of Sperm
– The tail, or flagellum, contains microtubules and functions to
move the spermatozoon.
Lab Activity 3 - Sperm
EPIDIDYMIS
The ductus epididymis functions
as the site where sperm are
stored and mature.
Figure 28.14
Oil immersion photograph of human spermatozoa. A spermatozoon is
divided into a head, midpiece, and a tail (flagellum).
8
Epididymis
Epididymis
• \The seminiferous tubules of the testis merge into a
region of the testis called the rete testis. The rete testis
consists of a group of small ducts lined with simple
cuboidal epithelium that deliver spermatozoa into the
efferent ducts located in the head of the epididymis. The
efferent ducts (ductuli efferentes) are lined with ciliated
columnar epithelium and merge to form the highly coiled
long duct of the body and tail of the epididymis, the
ductus epididymis.
• The ductus epididymis functions as the site where
sperm are stored and mature. The ductus epididymis
forms the ductus deferens, which connects the
epididymis to the ejaculatory duct.
• The short ejaculatory duct passes through the prostate
gland and enters the urethra.
• The ductus epididymis consists of
pseudostratified columnar epithelium with long
stereocilia (microvilli).
• The stereocilia do not function in movement, but
function to increase surface area for the
secretion of glycoproteins and the absorption of
fluid released by the testis.
• The glycoproteins function in the process of
spermatozoa maturation; the spermatozoa
become physiologically capable of fertilization of
the egg.
Lab Activity 4 - Epididymis
Lab Activity 4 - Epididymis
Figure 28.15
Scanning power photograph of a section of the epididymis and its
associated testis. The body and tail of the epididymis contains the ductus
epididymis, a long highly convoluted tube.
Figure 28.16
Low power photograph of a section of the epididymis. The body and tail of
the epididymis consists of a long highly coiled tube, the ductus epididymis.
Lab Activity 4 - Epididymis
DUCTUS DEFERENS
The ductus deferens, or vas deferens,
originates from the ductus epididymis
at the tail of the epididymis.
Figure 28.17
High power photograph of a section of the ductus epididymis. Stereocilia
(microvilli) extend from the columnar epithelial cells and function to increase the
surface area for secretion of glycoproteins and absorption of fluid.
9
Ductus (vas) Deferens
• The ductus deferens, or vas deferens, originates from
the ductus epididymis at the tail of the epididymis. It
turns upward to leave the scrotum as a component of the
spermatic cord and enters the abdominal cavity at the
opening of the inguinal canal (ring).
• From here the ductus deferens enters the pelvic cavity
ultimately to pass medially to the seminal vesicle and
downward to the base of the prostate gland.
• At the base of the prostate gland the ductus deferens
merges with the duct from the seminal vesicle to form
the ejaculatory duct, which passes through the prostate
gland and enters the prostatic urethra.
• The ductus deferens functions to transport sperm
from the epididymis to the ejaculatory duct.
Movement of sperm during ejaculation is by
peristaltic waves of the muscularis.
Lab Activity 5 – Ductus (vas)
Deferens
Figure 28.18
Low power photograph of a section of the ductus deferens. The ductus
deferens is a muscular tube with a small lumen. Its muscular layer consists of
smooth muscle which functions in the movement of sperm by peristalsis.
Seminal Vesicles
SEMINAL VESICLES
The two seminal vesicles are
located posterior to the urinary
bladder and anterior to the rectum
Lab Activity 6 – Seminal Vesicles
Figure 28.19
Low power photograph of a section of the seminal vesicle (primate). The
seminal vesicle consists of a highly coiled duct.
• The two seminal vesicles are located posterior to the
urinary bladder and anterior to the rectum. Each is
associated with its respective ductus deferens by way of
an ejaculatory duct formed from the union of the ductus
deferens and the duct from its associated seminal
vesicle.
• A seminal vesicle is formed from a long coiled and highly
branched tube. The posterior end of the tube is a blindend, and anteriorly the tube forms a narrow straight
vesicular duct that joins with its associated ductus
deferens.
• The seminal vesicles function to secrete vesicular
fluid, the major component (about 60%) of semen.
Vesicular fluid is a fructose rich slightly alkaline
fluid.
Lab Activity 6 – Seminal Vesicles
Figure 28.20
Low power photograph of a section of the seminal vesicle (human). This
photograph shows a section of the highly coiled duct. The duct has a secretory
mucosa that is highly branched (diverticula).
10
Lab Activity 6 – Seminal Vesicles
Prostate Gland
Figure 28.21
High power photograph of a section of the seminal vesicle (human). This
photograph shows a section of the mucosa of the highly coiled duct. The secretory
mucosa is highly branched (forms diverticula), which functions to increase its
secretory surface area.
Prostate Gland
• The prostate gland is located inferior to the urinary
bladder at the origin of the urethra (prostatic urethra),
which it completely surrounds.
• Transversing the prostate is the ejaculatory duct, formed
from the union of the ductus deferens and the duct from
its respective seminal vesicle. The prostate is formed
from highly branched glands (tubuloalveolar units), which
merge into ducts that enter the prostatic urethra.
• The highly branched prostatic glands are lined with
columnar epithelium which functions in the secretion of
prostatic fluid. Prostatic fluid comprises about 30% of
semen and is a slightly acid fluid that mostly functions in
the activation of sperm.
• The interstitial tissue (tissue between the glands), or
stroma, consists mostly of smooth muscle and
connective tissue. Contraction of the smooth muscle
during ejaculation moves prostatic fluid into the prostatic
urethra.
Lab Activity 7 – Prostate Gland
Figure 28.23
Low power photograph of a section of the prostate (primate). The glands
(tubuloalveolar units) are lined with columnar epithelium which functions in the
secretion of prostatic fluid.
Lab Activity 7 – Prostate Gland
Figure 28.22
Scanning power photograph of a section of the prostate (primate). The prostate is
composed of glands (tubuloalveolar units) with function in the secretion of prostatic
fluid.
Lab Activity 7 – Prostate Gland
Figure 28.24
High power photograph of a section of the prostate (primate). The glands
(tubuloalveolar units) are lined with columnar epithelium which functions in the
secretion of prostatic fluid. The glands empty into the prostatic urethra.
11
Penis
PENIS
The penis is the copulatory organ of the male
and is formed from three bodies of erectile, or
cavernous, tissue, which are supported by
connective tissue and covered with skin.
Penis
• The three bodies of erectile tissue are the two dorsal
corpora cavernosa and the corpus spongiosum.
• A portion of the penis is internal and forms the root of
the penis. The external portion of the penis is called the
shaft. The single ventral corpus spongiosum houses the
spongy, or penile, urethra. The corpus spongiosum
expands at the tip of the penis to form the glans penis,
the head of the penis.
• The penis is covered with skin, which folds over the
glans penis as the prepuce, or foreskin. The procedure
called circumcision removes the prepuce. The three
bodies of cavernous tissue are each surrounded by
connective tissue called the tunica albuginea.
Penis
• The tunica albuginea surrounding the two dorsal
corpora cavernosa meets in the midline to form
the median septum. The tunica albuginea that
surrounds the corpus spongiosum is thinner
than that surrounding the corpora cavernosa.
• The cavernous tissue is formed from large
vascular areas (sinuses), or cavernous spaces.
Partitions called trabeculae divide the
cavernous spaces which fill with blood
during erection of the penis.
Figure 28.27
The penis is formed from three bodies of erectile, or cavernous tissue that
are supported by connective tissue and covered with skin.
Lab Activity 8 - Penis
Figure 28.28
Scanning power photograph of a section of the human penis. The preparation
shows a portion of the corpus cavernosum, corpus spongiosum, and the urethra.
Lab Activity 8 - Penis
Figure 28.29
Low power photograph of a section of the human penis. The preparation
shows a portion of the corpus spongiosum and the urethra.
12
Lab Activity 8 - Penis
Lab Activity 8 - Penis
Figure 28.30
Low power photograph of a section of the human penis. The preparation
shows a portion of the corpus cavernosum. Increase blood flow into the cavernous
spaces during sexual arousal increases blood pressure within the spaces resulting
in erection. Decreased blood flow allows the elastic and smooth muscle fibers of
the trabeculae to recoil, allowing the penis to become flaccid.
Figure 28.31
Low power photograph of a section of the human penis. The preparation
shows a portion of the corpus cavernosum which has been cleared of blood
during processing of the tissue.
Female Reproductive System
FEMALE REPRODUCTIVE
SYSTEM
The primary sex organs of the
female are the paired ovaries.
Female Reproductive System
•
•
•
•
•
•
•
•
• The ovaries produce hormones and
gametes called eggs (ova).
• Sex hormones produced by the ovaries
include (1) estrogen and (2) progesterone.
• The accessory sex organs, starting with the
ovaries, are the
– (1) uterine tubes (Fallopian tubes, or oviducts),
– (2) uterus, and
– (3) vagina.
Female Reproductive System
The external genitalia (vulva) include the
(1) mons pubis,
(2) labia majora,
(3) labia minora,
(4) vestibule,
(5) clitoris
(6) vestibular glands, and the
(7) paraurethral glands.
Figure 28.32
Illustration of a midsagittal section of the female pelvis.
13
External Genitalia
• Labia majora
– The labia majora are two skin-covered folds of mostly
adipose tissue located inferior to the mons pubis and
form the lateral boundary of the vulva.
EXTERNAL GENITALIA
The external genitalia (or vulva)
are the external genital organs of
the female reproductive system.
• Labia minora
– The labia minora are two skin-covered folds, each
located medially to its respective labium majus. The
labia minora form the lateral boundary of the vestibule
(opening) of the vagina.
• Vestibule
– The vestibule is the chamber, or space, that is formed
within the boundary of the labia minora. Both the
urethra and the vagina open into the vestibule.
External Genitalia
• Clitoris
– The clitoris is a small rounded erectile organ
located at the anterior of the vulva at the
junction of the labia minora. The prepuce of
the clitoris is formed from an extension of the
labia minora.
• Mons pubis
– The mons pubis is an elevated area that
covers the pubic bones. After puberty it is
covered with hair and is usually soft due to
the presence of fat.
External Genitalia
• Greater vestibular glands (Bartholin’s
glands)
– There are two greater vestibular glands. One of each
vestibular gland is located lateral to the vagina and
opens into the vagina’s vestibule.
– The glands produce a mucus lubricating fluid during
intercourse. The greater vestibular glands are
homologous (similar in structure) to the male’s
bulbourethral glands. Several smaller glands called
lesser vestibular glands also open into the vestibule.
• Paraurethral glands
– The paraurethral glands open into the external
orifice (opening) of the urethra and are homologous to
the male’s prostate gland.
Internal Organs
• Broad ligament
INTERNAL ORGANS
– The broad ligament is a double fold of the peritoneum that folds
over and anchors the ovaries, uterine tubes, and uterus. The
broad ligament anchors the uterus to the lateral walls of the
pelvis, and between its two layers of peritoneum the broad
ligament provides a route for the passage of the uterine tubes.
The ovary is attached to the dorsal surface of the broad ligament
near the broad ligament’s lateral merging with the peritoneum of
the pelvis.
• Rectouterine pouch
–
The rectouterine pouch is the area formed between the uterus
and the rectum by the broad ligament.
• Vesicouterine pouch
– The vesicouterine pouch is the area formed between the uterus
and the posterior wall of the bladder by the broad ligament.
14
Internal Organs
• Ovary
Internal Organs
• Ovary
– The paired ovaries are located laterally to the uterus
and are attached to the dorsal surface of the broad
ligament.
– Each ovary is supported and anchored by the
mesovarium, the ovarian ligament, and the
suspensory ligament.
– The ovary is lined with modified visceral peritoneum.
At the margin of the ovary, the visceral peritoneum
changes from simple squamous to simple columnar
epithelium, which covers the ovary as the layer of the
ovary called the germinal epithelium. The germinal
epithelium only functions to structurally line the ovary.
– Internally, the ovary is divided into an outer region
called the cortex and a deep central region called the
medulla.
– Cortex
The cortex of the ovary is the outer region of the
ovary and contains numerous follicles embedded in
a surrounding tissue called the stroma. The follicles
are the sites of oocyte production and maintenance,
and along with the corpus luteum, produce the
primary sex hormones of the female, estrogen and
progesterone. The follicles also release the regulatory
hormone called inhibin.
– Medulla
The medulla of the ovary is the inner central region of
the ovary. The tissue of the medulla, the stroma,
provides a pathway for blood vessels, nerves, etc.
Internal Organs
• Mesovarium
– The mesovarium is a sheet of peritoneum that
attaches the ovary to the lateral wall of the pelvis.
• Ovarian ligament
– The ovarian ligament attaches the medial surface of
the ovary to the lateral wall of the uterus, at a point
just inferior to the entrance of the uterine tube.
• Suspensory ligament
– The suspensory ligament is a fold of peritoneum that
attaches the lateral wall of the ovary to the wall of the
pelvis, and serves as a site for the passage of the
ovarian blood vessels.
Internal Organs
• Uterine tubes (Fallopian tubes or Oviducts)
– Each of the uterine tubes extends from an ovary to the
superior, lateral region of the uterus.
– Extending from the uterus toward the ovary is the
region called the isthmus.
– Near the ovary, they have an expanded region called
the ampulla. The open end of the ampulla is called the
infundibulum.
– Small projections called fimbriae extend from the
infundibulum and drape over the ovary.
Internal Organs
• Uterus
– The uterus is located posterior and superior to the
bladder. It receives the two uterine tubes and serves
as the site for the implantation and development
of the fertilized egg.
• Three major regions are the
– (1) fundus, the rounded portion superior to the
entrances of the uterine tubes.
– (2) body, the central portion of the uterus
– (3) cervix, the narrow portion that projects outward
into the vagina. The cervical canal provides a
pathway from the vagina to the interior cavity of the
uterus.
Internal Organs
Uterine wall
• The three layers of the wall of the uterus are,
from the outside inward, the
– (1) perimetrium, the serous membrane that covers the
outside of the uterus
– (2) myometrium, the thick middle smooth muscle
layer
– (3) endometrium, the inner layer that undergoes cyclic
changes in response to ovarian hormones. The
endometrium is divided into the stratum functionalis
and the stratum basalis.
Vagina
– The vagina is the tubular organ that extends from the
cervix to the exterior region called the vestibule. It
serves as a passageway for the delivery of a baby
and receives the penis during sexual intercourse.
15
Internal Organs
OVARY
The paired ovaries are located laterally
to the uterus and are attached to the
dorsal surface of the broad ligament.
Figure 28.33
Anterior view of the uterus and associated organs.
Ovary
Lab Activity 9 - Ovary
• The paired ovaries are located laterally to the
uterus and are attached to the dorsal surface of
the broad ligament. The ovary is lined with
modified visceral peritoneum called the germinal
epithelium.
• The germinal epithelium functions as a lining of
the ovary. Internally, the ovary is divided into an
outer region called the cortex and a deep
central region called the medulla.
– The cortex of the ovary is the outer region of the
ovary and contains numerous follicles embedded in a
surrounding tissue called the stroma.
– The medulla of the ovary is the inner central region of
the ovary. The tissue of the medulla, the stroma,
provides a pathway for blood vessels, nerves, etc.
Lab Activity 9 - Ovary
Figure 28.34
Scanning power photograph of an ovary (monkey). Numerous follicles are
observed in the cortex.
Lab Activity 9 - Ovary
Primordial follicles
Primordial follicles are
located toward the
periphery of the cortex.
Each primordial follicle
consists of a primary
oocyte that is surrounded
by a single layer of
squamous cells called
follicular cells.
Figure 28.35
Low power photograph of the cortex of an ovary (monkey). Three types of
follicles can be observed, primordial, primary, and secondary follicles.
Figure 28.36
High power photograph of primordial follicles (monkey ovary).
16
Lab Activity 9 - Ovary
Primary follicles
Primary follicles
develop from
primordial follicles.
Each primary follicle
consists of a primary
oocyte that is
surrounded by several
layers of cuboidal cells
called granulosa cells.
Figure 28.37
High power photograph of primary follicles (monkey ovary).
Secondary follicles (tertiary,
vesicular, or Graafian)
Secondary follicles (tertiary,
vesicular, or Graafian)
• Secondary follicles develop from primary
follicles.
• The secondary follicle consists of an oocyte
surrounded by several layers of granulosa cells
that produce a fluid-filled central cavity called the
antrum.
• A layer of granulosa cells, the corona radiata,
surrounds the oocyte and the region of
glycoproteins, the zona pellucida. The zona
pellucida is a glycoprotein matrix with microvilli,
microvilli of the granulosa cells and microvilli of
the oocyte. The microvilli allow for the exchange
of materials between the primary oocyte and the
granulosa cells.
Lab Activity 9 - Ovary
• Upon ovulation, the secondary oocyte and its
associated zona pellucida and corona radiata
are discharged from the mature secondary
follicle.
• A mature secondary follicle that is ready to
rupture in ovulation is referred to as a vesicular
(Graafian) follicle. After ovulation, the vesicular
follicle is transformed into an endocrine organ,
the corpus luteum.
Figure 28.38
High power photograph of an early secondary follicle (monkey ovary).
Lab Activity 9 - Ovary
CORPUS LUTEUM
The corpus luteum develops from
the ruptured vesicular (or
Graafian) follicle after ovulation
Figure 28.39
High power photograph of a late secondary follicle (monkey ovary). Secondary
follicles are also called vesicular, tertiary, or Graafian follicles.
17
Corpus Luteum
• The corpus luteum develops from the ruptured vesicular
(or Graafian) follicle after ovulation.
• The corpus luteum functions as an endocrine gland and
produces progesterone (mostly) and estrogen.
• Hormone producing cells are the theca and granulosa
lutein cells. The theca is the outer covering of the
Graafian follicle. Some of its cell, the theca lutein cells
produce estrogen. The granulosa cells develop into
granulosa lutein cells and produce progesterone.
• If an embryo implants, a hormone is produced by the
developing placenta that maintains the corpus luteum. If
an embryo does not develop, the corpus luteum begins
to degenerate, and its hormonal functions are terminated
by the time of menstruation. The corpus luteum
degenerates into the corpus albicans.
Lab Activity 10 – Corpus Luteum
Figure 28.41
Scanning power photograph of the corpus luteum (monkey ovary). This
corpus luteum is relatively late in development as the lutein cells, which develop
from the granulosa cells, have completely filled the prior location of the antrum.
Lab Activity 10 – Corpus Luteum
Figure 28.40
Scanning power photograph of the corpus luteum. This corpus luteum is relatively
early in development as the lutein cells, which develop from the granulosa cells,
have not completely filled the prior location of the antrum.
Lab Activity 10 – Corpus Luteum
Figure 28.42
High power photograph of the corpus luteum (monkey ovary). The
progesterone-secreting cells of the corpus luteum are the lutein cells which
develop from the granulosa cells of the follicles.
Lab Activity 11 – Corpus Albicans
CORPUS ALBICANS
The corpus albicans is the fibrous
connective tissue that develops as a
result of the degeneration and
reabsorption of the corpus luteum.
Figure 28.43
Scanning power photograph of the corpus albicans (monkey ovary). The corpus
albicans is usually pale-stained as it consists mostly of fibrous connective tissue.
18
Lab Activity 11 – Corpus Albicans
MEIOSIS - OOGENESIS
Oogenesis is the process of
production and maturation of the
egg (ovum).
Figure 28.44
High power photograph of the corpus albicans (monkey ovary). The
pale-stained corpus albicans consists mostly of fibrous connective tissue.
Meiosis and Oogenesis
• Oogenesis is the process of production and
maturation of the egg (ovum).
• Oogenesis begins in early fetal development
with the mitotic production of oogonia (2n), the
precursor (stem) cells to the ova.
• The oogonia develop into primary oocytes as
they become surrounded by a single layer of
follicular cells, forming a primordial follicle.
Meiosis and Oogenesis
• A primary oocyte (2n) completes meiosis I to produce
two cells of very unequal size. The smaller of the two
cells is called the first polar body. The larger secondary
oocyte (n), which received most of the cytoplasm,
continues with meiosis II until metaphase II and then
stops.
• The secondary oocyte in metaphase II is ovulated. If
fertilization occurs, the secondary oocyte finishes
meiosis II. It produces a second polar body and an ovum
(n), or mature egg.
• Nuclear union between the ovum and sperm
produces a diploid (2n) zygote. The second polar
body, as with the other two second polar bodies
produced by meiosis II of the first polar body,
degenerates.
Meiosis and Oogenesis
• The primary oocytes enter meiosis I, which quickly
stops in prophase I. At birth and until puberty, the ovary
contains several million primary oocytes, each in a
primordial follicle.
• At puberty and mostly under the influence of
gonadotropic hormones (mostly follicle stimulating
hormone, FSH) cyclically released from the anterior
pituitary, some hormone sensitive primordial follicles
begin to develop. The primary oocyte continues with
meiosis I, and the single layer of follicular cells develops
into layers of cells, the granulosa cells, forming a
primary follicle.
Meiosis and Oogenesis
Figure 28.45
Oogenesis is the process of female gamete production. Meiosis reduces
the diploid human chromosome number of 46 to the haploid number of 23. Meiosis
assures that the ovum contains only half of the homologous chromosomes.
19
Lab Activity 12 – Oogenesis
Figure 28.46
Ovary (human) of a infant. Primary oocytes are produced early in fetal
development and their meiotic activity stops in prophase I. The primary oocytes are
surrounded by a single layer of follicular cells. A primary oocyte and its follicular
cells are called a primordial follicle. Primordial follicles remain inactive until the
onset of puberty.
Lab Activity 12 – Oogenesis
Figure 28.47
Ovary (monkey) showing various stages of oocyte and follicular development.
Lab Activity 12 – Oogenesis
OVARIAN CYCLE
Figure 28.48
Primordial follicles. Each primordial follicle consists of a single layer of follicular cells
and a primary oocyte. It is estimated that at birth each ovary contains up to
2,000,000 primordial follicles.
The ovarian cycle is the approximate 28 days
(monthly) sequence of changes that occur in
the ovary in relation to its follicular
development, ovulation, and development of
the corpus luteum
Ovarian Cycle
Follicle-stimulating hormone (FSH)
The ovarian cycle is the approximate 28
days (monthly) sequence of changes that occur
in the ovary in relation to its follicular
development, ovulation, and development of the
corpus luteum.
• The cycle of the ovary is regulated by the two
gonadotropic hormones (released from the
anterior pituitary (pars distalis) called follicle
stimulating hormone (FSH) and luteinizing
hormone (LH), and by negative feedback from
three hormones, estrogen, progesterone, and
inhibin.
• Follicle-stimulating hormone (FSH) is
produced and released from the anterior
pituitary gland (pars distalis).
• Follicle-stimulating hormone (FSH) targets
the follicles of the ovaries to stimulate
follicular development. Developing
follicles under the influence of FSH
release the regulatory hormone inhibin
and mostly the sex hormone estrogen.
•
20
Follicle-stimulating hormone (FSH)
• A negative feedback mechanism controls the
secretion of follicle-stimulating hormone (FSH).
– Increased levels of inhibin result in hypothalamic
reduction of gonadotropin-releasing hormone
(GnRH), which results in a reduction of folliclestimulating hormone (FSH);
– decreased levels of inhibin result in hypothalamic
increase of gonadotropin-releasing hormone (GnRH),
which results in an increase of follicle-stimulating
hormone (FSH).
Luteinizing Hormone (LH)
• Luteinizing hormone (LH) is produced and
released from the anterior pituitary (pars
distalis).
• Luteinizing hormone (LH) targets
– (1) the mature follicle of the ovary to trigger
ovulation,
– (2) and promotes the development of the
corpus luteum, which secretes estrogen and
progesterone.
Follicle-Stimulating Hormone (FSH)
Figure 28.49
Follicle-stimulating hormone
(FSH) is produced and
released from the anterior
pituitary gland (pars distalis).
Follicle-stimulating hormone
(FSH) targets the follicles and
promotes their development.
Developing follicles release
inhibin which results in the
reduction of GnRH, thus
reducing FSH.
Luteinizing Hormone (LH)
• A negative feedback mechanism controls the
secretion of luteinizing hormone (LH).
• Increased levels of estrogen and progesterone
result in hypothalamic reduction of
gonadotropin-releasing hormone (GnRH), which
result in a decrease of luteinizing hormone (LH);
• Decreased levels of estrogen and progesterone
result in hypothalamic increase of gonadotropinreleasing hormone (GnRH), which results in an
increase of luteinizing hormone (LH).
Luteinizing Hormone (LH)
Figure 28.50
Luteinizing hormone (LH) is produced
and released from the pars distalis.
For females, luteinizing hormone (LH)
targets the mature follicle, and
supports corpus luteum and
secretion of estrogen and
progesterone.
Phases of Uterine Cycle
The ovarian cycle is divided
into the follicular phase and the
luteal phase.
21
Phases of Uterine Cycle
Phases of Uterine Cycle
• Follicular phase
– The follicular phase of the ovarian cycle is the
time of follicular development,
approximately days 1 - 14, with day 14 as the
day of ovulation.
• Luteal phase
– The luteal phase of the ovarian cycle is the
time following ovulation, approximately days
14 - 28, when the corpus luteum develops
and is maintained.
Phases of Uterine Cycle
Figure 28.52
Photographs of the structures of an ovarian cycle. During the ovarian cycle
follicles develop (follicular phase), ovulation occurs, and the corpus luteum
develops (luteal phase). A corpus albicans, a body of fibrous tissue forms from
the degeneration of the corpus luteum.
Phases of Uterine Cycle
Figure 28.54
Photographs of primary and secondary follicles of the ovary (monkey). Primary
follicles are developing follicles. Their granulosa and theca cells secrete
estrogen. As the number and size of the granulosa and theca cells increases so
does the level of estrogen. Primary follicles develop into secondary follicles.
Figure 28.51
Illustration showing the sequences of changes in the 28 day ovarian
cycle. The follicular phase (days 1 - 14) is the preovulatory phase and is the time
of follicular development. The luteal phase (days 14 - 28) is the postovulatory
phase and is the time of the development of the corpus luteum.
Phases of Uterine Cycle
Figure 28.53
Photographs of primordial and primary follicles of the ovary (monkey). Primordial
follicles receptive to follicle stimulating hormone (FSH) released by the
anterior pituitary gland develop into primary follicles.
Phases of Uterine Cycle
Figure 28.55
Photographs of an early secondary and a late secondary follicle of the ovary
(monkey). Secondary follicles secrete increasing amounts of estrogen as their
granulosa and theca cells increase in size and number. A late secondary
follicle develops into a vesicular (Graafian) follicle.
22
Phases of Uterine Cycle
Figure 28.56
Photograph of an early secondary follicle (monkey ovary) and an illustration of
ovulation. At ovulation the follicular phase ends, and the luteal phase begins
with the conversion of the vesicular follicle of ovulation into an endocrine
gland called the corpus luteum.
Phases of Uterine Cycle
Figure 28.57
Illustration of a vesicular follicle of ovulation and a photograph of the corpus luteum
(monkey ovary). The corpus luteum functions as an endocrine gland and
secretes progesterone and estrogen.
Phases of Uterine Cycle
Figure 28.58
Photographs of the corpus luteum and the corpus albicans (monkey ovary). The
corpus albicans consists of fibrous connective tissue that develops from the
degeneration of the corpus luteum.
Figure 28.59
Illustration of the ovarian cycle. The cycle of the ovary is regulated by the two
gonadotropic hormones released from the anterior pituitary (pars distalis), follicle
stimulating hormone (FSH) and luteinizing hormone (LH), and by negative
feedback from three hormones, estrogen, progesterone, and inhibin.
Uterine Tube
UTERINE TUBE
The uterine tube (also called oviduct,
or Fallopian tube) is the tube that
extends between the ovary and the
uterus
• The uterine tube (also called oviduct, or
Fallopian tube) is the tube that extends
between the ovary and the uterus.
• Each of the two uterine tubes is divided
into three regions,
– (1) isthmus,
– (2) ampulla, and
– (3) infundibulum.
23
Lab Activity 13 – Uterine Tube
Lab Activity 13 – Uterine Tube
Figure 28.62
Low power photograph of the ampulla’s wall. The highly folded mucosa extends
into the lumen of the uterine tube.
Figure 28.61
Scanning power photograph of the isthmus of the uterine tube.
Lab Activity 13 – Uterine Tube
UTERUS
Figure 28.63
High power photograph of the mucosa of the ampulla of the uterine tube. The
highly folded mucosa is lined with ciliated columnar cells. Numerous secretory
cells are found among the ciliated cells.
Uterus
The uterus is the organ that functions
as the site for the development of the
embryo and fetus prior to birth.
Uterus
• The uterus is located in the pelvic cavity
between the urinary bladder and the rectum.
• The uterine tubes open into its superior-lateral
body.
• The cervix of the uterus opens into the inferior
vagina.
• The uterus is the organ that functions as the
site for the development of the embryo and
fetus prior to birth.
Figure 28.64
The uterus is the organ that functions as the site for the development
of the embryo and fetus prior to birth.
24
Uterus
Uterus
• Isthmus
• Fundus
– The fundus of the uterus is the superior
portion of the uterus, the region above the
points of attachment of the uterine tubes.
• Body
– The body of the uterus is the region between
the superior fundus and the inferior isthmus
– The isthmus of the uterus is a narrow constricted
region inferior to and continuous with the body. The
uterine cavity of the uterus narrows to form the
internal orifice at the superior internal boundary of
the isthmus.
• Cervix
– The cervix of the uterus is the most inferior
portion of the uterus.
– The cervix is continuous with the isthmus and its
inferior surface curves outward into the vagina.
– The opening into the cervix is called the external
orifice (or cervical os). The external orifice opens into
the cervical canal, which leads to the internal orifice.
The internal orifice is continuous with the uterine
cavity.
Uterine Wall
• Perimetrium
– The perimetrium is the serous membrane, the peritoneum, which
covers the fundus and the anterior-posterior surfaces of the
uterus.
UTERINE WALL
• Myometrium
– The myometrium is the thick middle muscularis of the uterus.
• Endometrium
The wall of the uterus consists of three
layers, from the outside inward, the
layers are the (1) perimetrium, (2)
myometrium, and (3) endometrium.
Uterine Wall
– The endometrium is the inner mucosa of the uterus and consists
of two layers the (1) stratum functionalis and the (2) stratum
basalis. The endometrium undergoes cyclic changes, the
uterine cycle, in response to ovarian hormones.
– The endometrium consists of numerous uterine (endometrial)
glands and blood vessels located within a layer of connective
tissue, the stroma.
Uterine Wall
• Uterine glands
– Uterine glands are the tubular glands of the mucosa
(endometrium) of the uterus. Early in the uterine cycle the uterine
glands are small and relative straight. Under the influence of
increased estrogen and progesterone, the uterine glands but
become enlarged, contorted, and sacculated (having small
lateral branches). Uterine glands function in the secretion of
nutrient rich mucus fluid.
• Blood vessels - spiral arteries
– The blood vessels that deliver blood to the endometrium are the
spiral arteries. The development of the spiral arteries is
under hormonal control. Their growth is promoted by
increased estrogen and progesterone levels. Atrophy of the
spiral arteries occurs when levels of estrogen and progesterone
become low.
• Stroma
– The stroma is the connective tissue that forms the framework
of the endometrium, it contains the spiral arteries and the uterine
glands.
Figure 28.65
The endometrium is the inner mucosa of the uterus. It contains numerous uterine
(endometrial) glands and blood vessels located within connective tissue called the
stroma. The mucosa is located interior to the muscularis, the myometrium.
25
Endometrium
• Stratum basalis
– The stratum basalis is the layer of the
endometrium close to the muscularis. The
stratum basalis is the permanent layer of the
endometrium. Uterine glands and blood
vessels are maintained in the stratum basalis.
• Stratum functionalis
– The stratum functionalis is the layer of the
endometrium closest to the uterine cavity and
undergoes modifications in preparation of
implantation of the fertilized egg.
Uterine Cycle
• The uterine (menstrual) cycle is divided
into three phases, the (1) menstrual
phase, (2) proliferative phase, and (3)
secretory phase.
• During the cycle the stratum functionalis,
in response to changing levels of estrogen
and progesterone, undergoes
considerable structural changes.
Uterine Cycle
• Proliferative phase
– The proliferative phase begins the rebuilding
of the stratum functionalis. The proliferative
phase begins in response to increasing
levels of estrogen from the developing
follicles (granulosa cells) of the ovary.
Uterine Cycle
The uterine (menstrual) cycle is divided into three
phases, the
(1) menstrual phase,
(2) proliferative phase, and
(3) secretory phase.
Uterine Cycle
• Menstrual Cycle
– The menstrual cycle is the complete cycle of the
uterus (of approximately 28 days) from one menstrual
period to the next.
• Menstrual phase (period)
– The menstrual period is the time in the menstrual
cycle in which menses, the flow of menstrual fluid,
occurs.
– The menstrual period occurs when levels of estrogen
and progesterone are at their lowest, and is
characterized by the shedding of the existing
developed stratum functionalis.
– This phase corresponds to the ending of the luteal
phase of the ovarian cycle characterized by the
degeneration of the corpus luteum with the reduction
of progesterone (and estrogen) levels.
Uterine Cycle
• Secretory phase
– The secretory phase continues the rebuilding with
additional preparations such as the secretion of
glycoproteins for receiving the fertilized egg.
– The secretory phase is enhanced by increased
levels of progesterone and estrogen. Progesterone
and estrogen levels increase from the development of
the corpus luteum following ovulation.
– If implantation does not occur, the corpus luteum
degenerates resulting in reduced levels of
progesterone and estrogen. With reduced levels of
hormones, the next uterine cycle begins with the
menstrual phase. The menstrual phase results in the
removal of the developed stratum functionalis.
– If implantation occurs, the corpus luteum is
maintained for a short time and the uterus continues
to develop as the uterus of pregnancy and supports
the developing embryo and fetus.
26
Uterine Cycle
Figure 28.66
The uterine (menstrual) cycle is divided into three phases, the (1) menstrual phase,
(2) proliferative phase, and (3) secretory phase. During the cycle the stratum
functionalis, in response to changing levels of estrogen and progesterone, undergoes
considerable structural changes.
Lab Activity 14 –
Menstrual Phase
Figure 28.68
Scanning power photograph of the menstrual phase of the uterus. The
endometrium is thin, and the stroma and uterine glands are filled with blood from
ruptured blood vessels.
Uterine Cycle
Figure 28.67
Photographs of the phases of the uterus
(human). The uterine cycle is divided into
three phases, the (1) menstrual phase
(menses), (2) proliferative phase, and (3)
secretory phase. The phases may be
further divided into early and late.
A Menstrual Phase, Days 1 - 4
B Proliferative Phase, Days 4 - 14
C Early Secretory Phase, Days 14 - 18
D Secretory Phase, Days 18 - 23
E Secretory Phase, Days 23 - 25
F Late Secretory Phase, Days 25 - 28
G Pregnant uterus
Lab Activity 15 –
Proliferative Phase
Figure 28.70
Scanning power photograph of the proliferative phase of the uterus (human),
days 4-14. The uterine glands are observed as tubes with slight convolutions.
Lab Activity 16 –
Secretory Phase
VAGINA
The vagina is located between the
cervix of the uterus and the opens at
the external region between the labia
minora, the vestibule
Figure 28.71
Scanning power photograph of the late secretory phase of the uterus
(human), days 23-25. The uterine glands are large and highly coiled with
sacculations.
27
Vagina
The vagina is located between the cervix of
the uterus and the opens at the external region
between the labia minora, the vestibule.
• The vagina functions to receive the penis
during intercourse and serves as the lower
part of the birth canal.
• The inner layer of the wall of the vagina is the
mucosa and is lined with non-keratinized
stratified squamous epithelium. The middle
muscularis of the vagina is composed of circular
and longitudinal layers of smooth muscle.
Lab Activity 17 – Vagina
•
Figure 28.72
Scanning power photograph of the vagina (human). The inner layer of the
vagina, the mucosa, is lined by non-keratinized stratified squamous epithelium.
The muscularis consists of smooth muscle, an inner circular and an outer
longitudinal layer.
Lab Activity 17 – Vagina
MAMMARY GLANDS
Figure 28.73
Low power photograph of the stratified squamous epithelium of the mucosa.
Mammary Glands
• The paired mammary glands (commonly called
breasts) are modified sebaceous glands that
function in the production of milk, or lactation.
• They are located within the superficial fascia on
the anterior sides of the chest. Each mammary
gland is associated with a protuberance called a
nipple.
• A nipple contains ducts from the glandular
tissue that transport milk to the outside. Around
each nipple is a pigmented area called the
areola.
The paired mammary glands (commonly
called breasts) are modified sebaceous
glands that function in the production of milk,
or lactation.
Mammary Glands
• Mammary glands consist of glandular tissue surrounded
and organized by fibrous connective tissue and fat.
• The glandular tissue is organized into lobes, which are
subdivided into lobules. The secretory units of the
lobules are called alveoli, sacs of cells that are found at
the terminal ends of excretory ducts.
• The excretory ducts of the alveoli merge into small
lacteriferous ducts. The lacteriferous ducts continue to
merge and form a large lacteriferous duct for each lobe
(glandular unit). The lacteriferous ducts converge to the
base of the nipple and each expands to form a
lacteriferous sinus.
• The lacteriferous sinuses enter the nipple and open to
the outside.
28
Mammary Glands
Mammary Glands
• During pregnancy the primary hormones for the
development of the mammary glands include
estrogen, progesterone, and prolactin.
– Prolactin, secreted from the anterior pituitary is the
primary hormone for the production of milk.
– Milk is not produced prior to birth because estrogen
and progesterone have an inhibitory effect on
prolactin. However, following birth estrogen and
progesterone levels decrease and their inhibitory
effect on prolactin is removed.
Figure 28.74
Mammary glands consists of glandular tissue surrounded and organized by
fibrous connective tissue and fat. The glandular tissue is organized into lobes, which
are subdivided into lobules. Each lobe is associated with a lactiferous duct, which
expands near the nipple into a lacteriferous sinus.
Mammary Glands
Lab Activity 18 –
Active Mammary Glands
• Mammary glands that are hormonally
stimulated during pregnancy undergo
increased glandular development.
• The lobules, undergo dramatic increases
in the production and size of their
secretory units, the alveoli.
• Thus, mammary glands are described as
active and inactive by the degree of
glandular development and activity.
Figure 28.75
Low power photograph of the well developed lobules of an active mammary gland.
The secretory units of the lobules are called alveoli.
Lab Activity 18 –
Active Mammary Glands
Figure 28.76
High power photograph of a lobule of an active mammary gland showing the
secretory units called alveoli.
Lab Activity 19 –
Inactive Mammary Glands
Figure 28.77
Low power photograph of the lobules of an inactive mammary gland. The
connective tissue between the lobules, the interlobular septa, and associated fat
appear abundant because of the reduced size of the alveoli.
29