presentation
advertisement

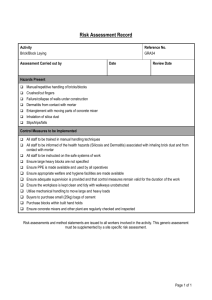
Western Occupational and Environmental Medical Association CME Webinar - June 27, 2012 Occupational Dermatology Heather P. Lampel, MD, MPH, FAAD Duke University Assistant Professor of Dermatology June 27, 2012 PLEASE STAND BY - WEBINAR WILL BEGIN AT 12:00pm (Pacific Time) FOR AUDIO: Call: 866-740-1260 / Access Code: 764 4915# Disclosures ! SmartHealth " TRUE Test ! I will be discussing off-label use of patch testing and off-label treatment of contact dermatitis Objectives ! ! ! ! ! ! Emphasize the importance of occupational contact dermatitis Discuss the epidemiology of contact dermatitis in the occupational setting Differentiate irritant from allergic contact dermatitis Understand the role of patch testing in diagnosis Explore common occupational allergens Outline treatment options and long-term management of occupational contact dermatitis Why should we care? ! Occupational skin disease is a topic “hot” AI-Hoqail R. Use of diesel oil for removal of tar from bitumen burns. Annals of Burns and Fire Disasters. 10:3; September 1997. Healthy People 2020 “Reduce occupational skin diseases or disorders among full-time workers” http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx ACOEM Core CompetenciesClinical Dermatology ! ! OEM physicians can provide early recognition, diagnosis, and management of these disorders and make necessary recommendations to minimize their occurrence both in the workplace and at home Diagnose primary irritant-induced dermatoses ! ! Differentiate occupational skin disorders by history, examination, and diagnostic evaluation Diagnose and determine the cause of allergic contact dermatitis (including urticaria), particularly those caused by common antigens such as latex, epoxy monomer, and nickel http://www.acoem.org/uploadedFiles/Publications/OEM_Competencies/ACOEM%20OEM%20COMPETENCIES.pdf ACOEM Core CompetenciesClinical Dermatology (con’t) ! Manage occupational and environmental skin injuries and dermatoses ! Treat and prevent recurrence of contact dermatitis http://www.acoem.org/uploadedFiles/Publications/OEM_Competencies/ACOEM%20OEM%20COMPETENCIES.pdf Epidemiology of Occupational Contact Dermatitis http://www.pennmedicine.org/encyclopedia/em_PrintArticle.aspx?ptid=1&gcid=000869 Contact Dermatitis ! ! Contact dermatitis (CD) is reported to account for up to 30% of all occupational disease in industrialized nations CD is the most common occupational skin disorder " About 90-95% of all cases of occupational skin diseases Occupational Contact Dermatitis Epidemiology ! ! ! ! Incidence rate of 0.5-1.9 cases per 1000 fulltime workers per year 1 year prevalence estimate of 10% Lifetime prevalence rate of 20% Likely underestimated due to underreporting " Mild cases specifically Occupational Contact Dermatitis Epidemiology ! Hands are usually involved " " ! 80-90% of cases Great impact on quality of life True epidemiologic data are lacking " " No standardization of data, methods of collection Underreporting Occupational Contact Dermatitis Epidemiology ! ! US Bureau of Labor Statistics 2000 estimated 41,800 cases of Occupational CD This is felt to be underreported " ! Estimates are closer to 400,000 to 2 million cases per year 1985 Mathias estimated annual costs of Occupational CD to be between $222 million and $1 billion Occupational Contact Dermatitis Epidemiology ! Survey of established cases of Occupational CD, reported that over one year: " " 19.9% reported prolonged sick leave 23% experienced job loss What percent of all contact dermatitis is allergic versus irritant? Contact Dermatitis Overview ! Irritant contact dermatitis accounts for 60-80% of all CD ! Allergic contact dermatitis accounts for remaining 20-40% Contact Dermatitis Overview ! ACD is a SPECIFIC immunologic reaction, requiring prior sensitization Image from: www.dermnet.com Immunology of Allergic Contact Dermatitis Elliott G and Das PK. Using p-Phenylenediamine: A Gateway to Chemical Immunology. Journal of Investigative Dermatology (2010) 130, 641–643. Contact Dermatitis Overview ! 90% of the population can be sensitized to certain antigens such as dinitrochlorobenzene Contact Dermatitis Overview ! What percent of North American Caucasian adults are allergic to Rhus antigen? " 25% " 40% " 60% " 75% www.ohio-nature.com www.gmcsc.org www.duke.edu Contact Dermatitis Overview ! What percent of North American Caucasian adults are allergic to Rhus antigen? " 25% " 40% " 60% " 75% www.ohio-nature.com www.gmcsc.org www.duke.edu Contact Dermatitis Overview ! Irritant contact dermatitis is NONSPECIFIC ! Requires no prior sensitization ! Clinically can be difficult to distinguish ICD from ACD http://www.skincareguide.ca/glossary/i/irritant_contact_dermatitis.html Common Occupational Irritants ! Alkalis " " " ! Soaps Detergents Cleansers Acids ! Hydrocarbons " " ! Petroleum Oils Solvents Common Occupational Irritants ! Frictional Dermatitis ! ! Repetitive handling of objects or materials Likely underappreciated ! Examples ! ! ! ! Fabric Paper Metal objects Driving Common Occupational Irritants ! Gloves ! Prolonged contact with skin affects the epidermal barrier ! May be irritant itself ! May make epidermal barrier more susceptible to allergens or other irritants Ramsing DW, Agner T: Effect of glove occlusion on human skin (II). Long-term experimental exposure. Contact dermatitis 1996; 34:258-62. ACD vs ICD Feature ACD ICD Pain, burning ++ ++++(Early) Erythema ++++ ++++ Vesicles ++++ + Pustules + +++ Hyperkeratosis ++ ++++ Itch ++++(Early) +++(Late) ACD vs ICD Feature Fissuring ACD ++ ICD ++++ Sharp demarcation Yes Yes Necrotic keratinocytes + +++ Dermal Edema ++++ ++++ Lymphocytic infiltrate ++++ ++++ Neutrophilic infiltrate + +++ Photo Quiz Allergic or Irritant Contact Dermatitis? Allergic or Irritant? Dermaamin.com Irritant Dermaamin.com Allergic or Irritant? http://hardinmd.lib.uiowa.edu/pictures22/dermnet/contact_dermatitis_04rhus080105.jpg Allergic http://hardinmd.lib.uiowa.edu/pictures22/dermnet/contact_dermatitis_04rhus080105.jpg Allergic or Irritant? Skincareguide.com Irritant Skincareguide.com Allergic or Irritant? Allergic Allergic or Irritant? http://www.cdc.gov/niosh/topics/skin/occderm-slides/ocderm10.html Allergic and Irritant http://www.cdc.gov/niosh/topics/skin/occderm-slides/ocderm10.html Debunking the myths… webseoanalytics.com CD Misconceptions ! Allergy only develops to new exposures/products CD Misconceptions ! Allergy only develops to new exposures/products " FALSE " Allergy can develop after years of using the same product CD Misconceptions ! If a change in chemical/product exposure does not clear the rash, that product is not etiologic CD Misconceptions ! If a change in chemical/product exposure does not clear the rash, that product is not etiologic " FALSE " There are many cross-reactants in other products, it is best to have NO exposures to topicals/cross-reactors when clearing a rash CD Misconceptions ! If product exposure is bilateral, the eruption should be bilateral CD Misconceptions ! If product exposure is bilateral, the eruption should be bilateral " NOT NECESSARILY " Common misconception held by MDs " There are many aspects affecting endproduct eruption CD Misconceptions ! ACD is NOT patchy- it is usually the same intensity at all areas of exposure CD Misconceptions ! ACD is NOT patchy- it is usually the same intensity at all areas of exposure " FALSE " Again, many factors affect the presenting eruption pattern CD Misconceptions ! Adult onset “eczema” CD Misconceptions ! Adult onset “eczema” " If no history of eczema as a child, likely ACD " Especially if on hands, face, neck “The greatest abuse of patch testing is failure to use the test.” ! Coleman, 1982 Patch testing ! Intended to detect allergens relevant to eruption ! Is at least a week-long process ! Detects Type IV allergic reaction (delayed-type hypersensitivity) ! Requires at least 2-3 visits to clinic for complete testing T.R.U.E. Test ! Thin-layer Rapid Use Epicutaneous Test ! Allerderm product ! Only FDA-approved patch testing product ! 29 allergens with an additional 7 recently FDA-approved ! Comes pre-filled T.R.U.E. Test ! ! ! ! ! ! ! ! ! ! ! ! Nickel Sulfate Wool Alcohols Neomycin Sulfate Potassium Dichromate Caine Mix Fragrance Mix Colophony Paraben Mix Negative Control Balsam of Peru Ethylenediamine Dihydrochloride Cobalt Dichloride ! ! ! ! ! ! ! ! ! ! ! ! p-tert-Butylphenol Formaldehyde Resin Epoxy Resin Carba Mix Black Rubber Mix Me- Cl- Isothiazolinone (MCI/MI) Quaternium-15 Mercaptobenzothiazole p-Phenylenediamine Formaldehyde Mercapto Mix Thimerosal Thiuram Mix T.R.U.E. Test ! ! ! ! ! Diazolidinyl urea Imidazolidinyl urea Budesonide Tixocortol-21pivalate Quinoline mix Dermnetnz.org TRUE versus Chamber ! TRUE testing is helpful, but many patients have at least one relevant allergen not detected by TRUE testing ! Consider referral for more extensive patch testing if no improvement Patch testing ! Step 1: Take extensive exposure history " Include home exposures, work tasks and exposures, implants, intermittent exposures, MSDS if appropriate ! Step 2: Determine allergen panel " Would be pre-determined if only TRUE Test is available Patch testing ! Step 3: Prepare allergen tray as appropriate " TRUE test is pre-prepared Patch testing ! Step 4: Apply patches to back " Back must be clear of " Patches are marked " Securing rash paper tape is used Patch testing ! Step 5: Patches removed in 48 hours " Variability in how " Areas remarked " Reactions this is done noted- Irritant Patch testing ! Step 6: Patches read at 3-7 days after application " Our clinic reads at 4 days " Consider delayed read for late reactors Patch testing ! Step 7: Determine clinical relevance " Consider the Mathias Criteria for Occupational cases ! " Excellent tool for ascertaining occupational causation Keep in mind that irritant CD remains a diagnosis of exclusion, and dermatitis may be both ICD and ACD, multifactorial, etc. Mathias CG. Contact dermatitis and workers’ compensation: criteria for establishing occupational Causation and aggravation. J Am Acad Dermatol 1989; 20(5):842-8. Patch testing ! Step 8: Instruct in avoidance of allergen(s) and crossreactors " If in topical medicaments, cosmetics, etc. it is best to print out the CAMP “safe list” ! ! " " " On American Contact Dermatitis Society member webpage Mayo Clinic also has a database Also consider all objects that may contain allergen Information (written) and verbal counseling of patient is KEY May include modified work, increased or alternative PPE, modified environment- both home and work Mathias CG. Contact dermatitis and workers’ compensation: criteria for establishing occupational Causation and aggravation. J Am Acad Dermatol 1989; 20(5):842-8. Mathias Criteria 1. Is the clinical appearance consistent with contact dermatitis? 2. Are there workplace exposures to potential cutaneous irritants or allergens? 3. Is the anatomic distribution of the dermatitis consistent with cutaneous exposure in relation to work tasks? 4. Is there a temporal association between onset of dermatitis and exposure consistent with contact dermatitis? Mathias CG. Contact dermatitis and workers’ compensation: criteria for establishing occupational Causation and aggravation. J Am Acad Dermatol 1989; 20(5):842-8. Mathias Criteria 5. Are non-occupational exposures excluded as probable causes? 6. Does dermatitis improve away from work exposure to the suspected allergen or irritant? 7. Do patch or provocation tests identify a probable causal agent? Mathias CG. Contact dermatitis and workers’ compensation: criteria for establishing occupational Causation and aggravation. J Am Acad Dermatol 1989; 20(5):842-8. Mathias Criteria ! Answer of “yes” to 4 or more of the 7 criteria yields a greater than 50% probability of occupational cause ! Provides a “reasonable degree of medical certainty” Mathias CG. Contact dermatitis and workers’ compensation: criteria for establishing occupational Causation and aggravation. J Am Acad Dermatol 1989; 20(5):842-8. Pearls Regarding Patch Testing ! Do NOT test when dermatitis anywhere is acute or severe " Leads to angry back syndrome " Worsening of existing dermatitis http://dermnetnz.org/procedures/patch-tests.html Pearls Regarding Patch Testing ! Do NOT test when dermatitis is present on the back http://www.rash-pictures.com/279-dermatitis-back-man.html Pearls Regarding Patch Testing ! What about " Wait medications? at least 1 week after d/c of oral steroids " If unable to stop oral steroids, taper to 10mg/day or less, may cause falsenegative rxn " Do not test within 2 weeks of using topical steroids on back " Systemic antihistamines do not interfere with results Pearls Regarding Patch Testing ! What about sunburn? " Do not test back within 1-2 weeks of sunburn (false-negatives are possible) Wikipedia.org Pearls Regarding Patch Testing ! What about hairy backs? " The patient will need to shave 24-48 hours PRIOR to patch application ! DO NOT shave in the office prior to placing patches- leads to irritant and false-positives Sbrforum.com Pearls Regarding Patch Testing ! What about " No showering? showering or wetting the back for the entire testing period, up until the final read (at least 5 days) " Modified work note for outside workers or heavy laborers Pearls Regarding Patch Testing ! Patient comes in convinced that a liquid he works with is the “cause” of his rash ! He wants you to patch test this, what should you do? 2ols.com Pearls Regarding Patch Testing ! Patient comes in convinced that a liquid he works with is the “cause” of his rash ! He wants you to patch test this, what should you do? " DO NOT " MSDS TEST UNKNOWNS! " DeGroot (4300 chemicals for test concentrations) 2ols.com Allergens Top 10 Allergens in North America ! Nickel sulfate ! Bacitracin ! Balsam of Peru ! Formaldehyde ! Fragrance mix I ! Cobalt chloride ! Quaternium-15 ! Methyldibromoglutaronitrile Neomycin ! p-Phenylenediamine ! Zug KA, Warshaw EM, Fowler JF Jr, et al: Patch-test results of the North American Contact Dermatitis Group 2005-2006. Dermatitis 2009;20:149-160 Top Allergens in the Workplace ! Carba Mix ! Thiuram Mix ! Epoxy Resin ! Formaldehyde ! Nickel Rietschel RL, Mathias CG, Fowler JF Jr, et al. North American Contact Dermatitis Group. Relationship of occupation to contact dermatitis (OCD): evaluation in patients tested from 1998 to 2000. Am J Contact Dermatitis 2002;13(4):170-6. Top Allergens in the Workplace ! Carba Mix ! Thiuram Mix Onlygloves.com ! Epoxy Resin ! Formaldehyde ! Nickel cdc.gov Instructables.com Rietschel RL, Mathias CG, Fowler JF Jr, et al. North American Contact Dermatitis Group. Relationship of occupation to contact dermatitis (OCD): evaluation in patients tested from 1998 to 2000. Am J Contact Dermatitis 2002;13(4):170-6. Top Allergens in the Workplace ! Carba Mix ! Thiuram Mix ! Epoxy Resin ! Formaldehyde ! Nickel http://epoxy.fiberglassmoldss.com/epoxy/ Ehow.uk.eu Wikipedia.com Rietschel RL, Mathias CG, Fowler JF Jr, et al. North American Contact Dermatitis Group. Relationship of occupation to contact dermatitis (OCD): evaluation in patients tested from 1998 to 2000. Am J Contact Dermatitis 2002;13(4):170-6. Top Allergens in the Workplace ! Carba Mix ! Thiuram Mix ! Epoxy Resin ! Formaldehyde ! Nickel Travelandleisure.com Rfid-weblog.com Rietschel RL, Mathias CG, Fowler JF Jr, et al. North American Contact Dermatitis Group. Relationship of occupation to contact dermatitis (OCD): evaluation in patients tested from 1998 to 2000. Am J Contact Dermatitis 2002;13(4):170-6. Formaldehyde-Releasers ! Carba Mix ! Thiuram Mix ! ! Epoxy Resin ! ! Formaldehyde ! Nickel ! ! ! ! Quaternium-15 Imidazolidinyl urea (Germall 115) Diazolidinyl urea (Germall II) DMDM hydantoin (Glydant) 2-Bromo-2nitropropane-1,3-diol (Bronopol) Sodium hydroxymethyl glycinate Top Allergens in the Workplace ! Carba Mix ! Thiuram Mix ! Epoxy Resin ! Formaldehyde ! Nickel Wikipedia.org The prevalence of ACD to nickel is: ! Greater in women than in men ! Greater in younger than older patients ! Higher than ACD to palladium ! All of the above ! None of the above Cellphone contact dermatitis with nickel allergy; CMAJ • January 1, 2008; 178 (1) The prevalence of ACD to nickel is: ! Greater in women than in men ! Greater in younger than older patients ! Higher than ACD to palladium ! All of the above ! None of the above Cellphone contact dermatitis with nickel allergy; CMAJ • January 1, 2008; 178 (1) Dealing with Nickel Allergy ! Lobbying Congress to pass nickel standard ! Manufacturers would have to limit content of any item with prolonged skin contact to restrict release of nickel to 0.5 mcg/cm per week ! Similar 2001 legislation in Europe decreased childhood nickel dermatitis from 19% to 6% Dealing with Nickel Allergy ! Dimethylglyoxime spot test " ! Can purchase at www.delasco.com Barrier coating " " " ! meteorites.wustl.edu Nickel Guard (Athena Allergy) is best Can also use Beauty Secrets Nail Hardener Super glue not so super (within 7 days consumers had rashes) AVOID nickel " Take magnet shopping ! Does not attract aluminum, does attract nickel North American Contact Dermatitis Group ! Publish update on “most commons” ! Pool results from major centers ! Review trends (increasing and decreasing reactivity in the population) ! Make changes to recommended trays from this population-based data Allergen of the Year 2009 ! Mixed dialkyl thioureas ! Mixed quaternium bases ! Mixed thiuram alkylates ! Mixed tetra-alkyl thiurams Allergen of the Year 2009 ! Mixed dialkyl thioureas ! Mixed quaternium bases ! Mixed thiuram alkylates ! Mixed tetra-alkyl thiurams Allergen of the Year 2009 ! Mixed dialkyl thioureas (MDTU) " Used as an accelerant in rubber and antioxidant in neoprene production " Combination of diethylthiourea and dibutylthiourea (most prevalent in mix) " NOT in TRUE test, but present in standard rubber series Allergen of the Year 2009 ! Mixed dialkyl thioureas " Occupational: ! Gloves most commonly on hands leaching MDTU " Non-occupational: feet ! Foot most commonly on the supports, athletic shoes leaching MDTU " Sleep apnea masks, wetsuits, neoprene braces, goggles lowerextremityreview.com homehealthmedical.com Gemplers.com Allergen of the Year 2010 ! Bacitracin ! Nickel sulfate ! Neomycin ! Polymyxin B sulfate Allergen of the Year 2010 ! Bacitracin ! Nickel sulfate ! Neomycin ! Polymyxin B sulfate Allergen of the Year 2010 ! Neomycin " " " In medicaments ACD in healthcare workers, veterinarians Cross-reacts: Paromycin, butirosin ! Framycetin ! Tobramycin, kanamycin ! Gentamycin ! Streptomycin ! Wikipedia.org Allergen of the Year 2011 ! Dimethyl Fumarate ! No occupational relevance at this time Allergen of the Year 2012 ! Gold ! Propolis ! Quaternium-15 ! Acrylates Allergen of the Year 2012 ! Gold ! Propolis ! Quaternium-15 ! Acrylates Occupations at High-Risk for Hand Dermatitis ! ! ! ! ! ! Hairdressers Musicians Food Industry workers Agricultural workers Factory workers Electronics workers ! ! ! ! ! Cleaners/Washers Housekeepers Printers Builders Medical and Dental workers Treating Hand DermatitisStep 1 ! Recommended shortterm high-potency topical steroids for hands: " For body: " Clobetasol propionate ! " ! Ointment Halcinonide ointment ! ! No propylene glycol, no sensitizers “Halog” " Short-term hydrocortisone 2.5% bid for face, neck, axillae, groin, intertriginous areas Short-term triamcinolone 0.1% bid for body Treating Hand DermatitisStep 1 ! ! Avoid more than a few weeks of potent steroid use topically Can thin the skin making hands more susceptible to allergen/irritant! ! ! Consider IM steroids x1 Doxycycline for antiinflammatory effects Treating Hand DermatitisStep 1 ! Barrier creams " Tetrix creams " Creams with ceramide, urea and dimethicone " Studies are variable in demonstrating any benefit from barrier creams when compared to regular emollients Treating Hand DermatitisStep 1 ! Appropriate gloves " Match task with glove " “Quick Selection Guide to Chemical Protective Clothing” by Forsberg and Mansdorf " ACDS website lists glove manufacturers Treating Hand DermatitisStep 2 (Maintenance) ! Calcineurin inhibitors Tacrolimus 0.1% " Pimecrolimus 0.1% " ! Therapeutic moisturizers " ! Lower potency steroids for hands: " " MimyX ! Palmitate monoethanolamine Shea butter " Aquaphor " Petrolatum " " Triamcinolone 0.1% Fluticasone cream or lotion (great for atopics) Hydrocortisone butyrate lipid cream ! " (Locoid lipocream) Clocortolone cream ! (Cloderm) Treating Hand DermatitisStep 3 (Recalcitrant) ! Hand psoralen- ultraviolet A therapy (PUVA) ! Narrow-band UV B therapy (NBUVB) ! Often used for recalcitrant body dermatitis ! Excimer laser ! 308 nm Treating Hand DermatitisStep 3 (Recalcitrant) ! ! Methotrexate Mycophenolate mofetil " ! 2-3g/day recommended for control Acitretin " " Best for psoriasiform hand dermatitis 2-4 month course ! Cyclosporine " 2.5-5 mg/kg daily ! Azathioprine " 1-3 mg/kg daily ! Biologics are not helpful overall Summary ! ! ! Allergic and irritant contact dermatitis can be difficult to distinguish We are constantly being exposed to new allergens, often earlier in life Occupational contact dermatitis is underreported ! ! ! Patch testing for ACD is the gold standard Can try TRUE test, consider referral for comprehensive panels History, history, history Summary ! ! Think outside the box Try a stepwise approach " " " Elimination Treatment Escalate treatment ! ! Will be chronic if exposure continues You can make a huge difference in patient’s quality of life References ! ! ! ! ! ! ! ! ! ! ! ! ! Marks et al., 2002. Marks J.G., Elsner P., DeLeo V.A.: Contact and Occupational Dermatology, 3rd ed. St Louis, Mosby, 2002. Nelson and Yiannias, 2009. Nelson S.A., Yiannias J.A.: Relevance and avoidance of skin-care product allergens: Pearls and pitfalls. Dermatol Clin 2009; 27(3):329-336. Thin-layer rapid-use epicutaneous test. Thin-layer rapid-use epicutaneous test (TRUE-test) : Available at:[accessed 03.07.11] http://www.truetest.com/PatientPDF/File18.pdf Zug et al., 2009. Zug K.A., Warshaw E.M., Fowler J.F., et al: Patch-test results of the North American Contact Dermatitis Group 2005-2006. Dermatitis 2009; 20:149-160. Emmett EA. Occupational contact dermatitis I. Incidence and return to work pressures. Am J Contact Dermatitis 2002;13:30– 2002;13:30–4. Bureau of Labor Statistics. Occupational injuries and illnesses in the United States. [Bulletin 2512]. Washington (DC): US Department of Labor, Bureau of Labor Statistics; 1999. Lushniak BD. The epidemiology of occupational contact dermatitis. Dermatol Clin 1995; 13:671– 13:671–9. Skoet R, Olsen J, Mathiesen B, et al. A survey of occupational hand eczema in Denmark. Contact Dermatitis 2004;51(4):159– 2004;51(4):159–66. Staton I, Ma R, Evans N, et al. Dermal nickel exposure associated with coin handling and in various occupational settings: assessment using a newly developed finger immersion method. Br J Dermatol 2006;154(4):658– 2006;154(4):658–64. Veien NK, Menne T. Treatment of hand eczema. Skin Therapy Lett 2003;8(5):4– 2003;8(5):4–7. 137. Warshaw E. Therapeutic options for chronic hand dermatitis. Dermatol Ther 2004;4:17240– 2004;4:17240–50. Schalock PC, Zug KA, Carter JC, et al. Efficacy and patient perception of Grenz ray therapy in the treatment of dermatoses refractory to other medical therapy. Dermatitis 2008;19(2):90– 2008;19(2):90–4. Abramovits W, Granowski P. Innovative management of severe hand dermatitis. Dermatol Clin 28 (2010) 453-65. References ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! Sprigle AM, Marks JG Jr, Anderson BE. Prevention of nickel release with barrier coatings. Dermatitis. 2008,19(1):28-31. Diepgen T.L., Coenraads P.J.: The epidemiology of occupational contact dermatitis. Int Arch Occup Environ Health 72. (8): 496506.1999. Keil J.E., Shmunes E.: The epidemiology of work-related skin disease in South Carolina. Arch Dermatol 119. (8): 650-654.1983. Mathias C.G.: Occupational dermatoses. J Am Acad Dermatol 19. (6): 1107-1114.1988. Goh C.L.: An epidemiological comparison between occupational and non-occupational hand eczema. Br J Dermatol 120. (1): 77-82.1989. Marks J.G., Elsner P., DeLeo V.A.: Contact & occupational dermatology. 3rd ed Mosby St. Louis, (MO)2002. Holness D.L.: Characteristic features of occupational dermatitis: epidemiologic studies of occupational skin disease reported by contact dermatitis clinics. Occup Med 9. (1): 45-52.1994. Belsito D.V.: Occupational contact dermatitis: etiology, prevalence, and resultant impairment/disability. J Am Acad Dermatol 53. (2): 303-313.2005. Kanerva L., Estlander T., Jolanki R.: Occupational skin disease in Finland. An analysis of 10 years of statistics from an occupational dermatology clinic. Int Arch Occup Environ Health 60. (2): 89-94.1988. Sertoli A., Gola M., Martinelli C., et al: Epidemiology of contact dermatitis. Semin Dermatol 8. (2): 120-126.1989. Rietschel R.L., Mathias C.G., Fowler , Jr. , Jr.J.F., et al: Relationship of occupation to contact dermatitis: evaluation in patients tested from 1998 to 2000. Am J Contact Dermatitis 13. (4): 170-176.2002. Nethercott J.R., Holness D.L.: Disease outcome in workers with occupational skin disease. J Am Acad Dermatol 30. (4): 569574.1994. Mathias C.G., Morrison J.H.: Occupational skin diseases, United States. Results from the Bureau of Labor Statistics Annual Survey of Occupational Injuries and Illnesses, 1973 through 1984. Arch Dermatol 124. (10): 1519-1524.1988. Koch P.: Occupational contact dermatitis. Recognition and management. Am J Clin Dermatol 2. (6): 353-365.2001. Bureau of Labor Statistics : Occupational Injuries and illnesses in the United States. Available at: http://www.bls.gov/iif Lushniak B.D.: Occupational contact dermatitis. Dermatol Ther 17. (3): 272-277.2004. Mathias C.G.: The cost of ccupational skin disease. Arch Dermatol 121. (3): 332-334.1985. Cvetkovski R.S., Rothman K.J., Olsen J., et al: Relation between diagnoses on severity, sick leave, and loss of job among patients with occupational hand eczema. Br J Dermatol 152. (1): 93-98.2005. Thank you! Thank you for participating in today’s webinar. At the conclusion of this call you will receive an email with a link to a post-webinar questionnaire. You will need to complete this questionnaire in order to receive CME for this webinar. This webinar presentation can be downloaded at www.woema.org