looking at symptoms with a middle-range theory lens
advertisement

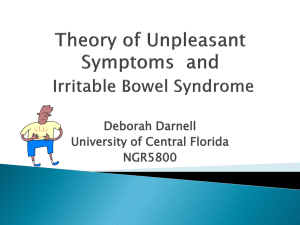
PROCEEDINGS LOOKING AT SYMPTOMS WITH A MIDDLE-RANGE THEORY LENS* — Patricia Liehr, PhD, RN† ABSTRACT One of the most challenging expectations for nurses—in research or clinical settings—is the translation of nursing theory for use in practice and research. The Ladder of Abstraction is a construct depicting 3 different levels of ideas regarding a health issue, such as pain. The Ladder of Abstraction has 3 rungs: the philosophical, theoretical, and empirical rungs—3 different ways to think about and approach a health issue. The higher the level on the ladder, the more abstract the ideas. Middle-range theory exists on the middle rung and it is described as theory occurring at the intersection of practice and research. For this discussion, we consider chronic pain through a middle-range lens using middle-range theories from differing levels of abstraction. None of these theories are more “correct” than the other, but each theory provides a different lens for seeing everyday nursing practice. It is up to the practicing nurse to choose a theory that fits her own personal values and to let the theory guide action, enabling evaluation from the view with the middle-range theory lens. (Adv Stud Nurs. 2005;3(5):152-157) *Based on a presentation given by Dr Liehr at the Fourth Annual Sigma Theta Tau International Chesapeake Consortium Research Conference. †Associate Dean for Nursing Research and Scholarship, Christine E. Lynn College of Nursing, Florida Atlantic University, Boca Raton, Florida. Address correspondence to: Patricia Liehr, PhD, RN, Associate Dean for Nursing Research and Scholarship, Christine E. Lynn College of Nursing, Florida Atlantic University, 777 Glades Road, Boca Raton, FL 33431. E-mail: pliehr@fau.edu. 152 O ne of the most challenging expectations for nurses today—in research or practice settings—is the translation of nursing theory and science for use in practice and research. There are many ways to think about practice issues, such as symptom experience, and nurse researchers and practitioners are looking at frameworks to guide study and intervention with people experiencing symptoms. Symptoms are a subjective experience, appraised by the patient. Examples of symptoms are pain, nausea, or fatigue. By contrast, signs are observable indicators of a change in health status. A nurse identifies a sign through careful observation and evaluation. Pain, nausea, and fatigue may be evaluated as signs when measured as the amount of pain medication used, the frequency of vomiting, and the number of hours spent recumbent, respectively. Chronic pain has recently been a common topic in the lay press, in part because of the withdrawal of cyclooxygenase-2 inhibitors.1 Chronic pain affects approximately 1 in 6 Americans and costs the United States approximately $100 billion annually.2,3 Most people seek pain relief solely from medication (ie, “pharmaceutical salvation”), but pain is affected by many factors (physiologic and nonphysiologic), which may demand pain management approaches other than medication. Generally, pain is undertreated because patients and physicians underestimate its effects on functioning. Nonpharmacologic treatments for pain have expanded to include interventions, such as lifestyle changes, mindfulness therapy, or alternative therapies (eg, vitamins and herbs).1 All of these interventions are within the realm of nursing practice and could be considered in addition to traditional pharmacologic interventions. The effect of pain on psychosocial factors and the effect of psychosocial factors on Vol. 3, No. 5 ■ August 2005 PROCEEDINGS pain can be difficult to quantify and assess, but this reciprocal relationship falls squarely within the realm of nursing practice. Nurses think about and approach pain differently than other members of the healthcare team, and nurses can have a significant impact on pain experience when viewing pain through their disciplinary lens. knowledge base for this paradigm is founded in social sciences. The unitary-transformative world view suggests that change is unpredictable and constantly evolving, and through a transformative process, people find meaning. It suggests that people are capable of awareness beyond just the physical (ie, more spiritual). This paradigm is grounded in the human sciences.7 Most nurses practice in the interactive-integrative world view, most of the time. However, from that position, nursing practice routinely calls us to move to the particulate-deterministic or the unitary-transformative world view. Middle-range theory sits on the middle rung of the ladder between microrange and grand theory (Figure 1).4 Microrange theory is situation-specific and limited to particular populations or fields of practice, such as menopausal transition of African-American women or learned response to chronic illness in patients with multiple sclerosis.8 Grand theories are broad in scope, such as theories of human becoming, adaptation, and THE LADDER OF ABSTRACTION Advanced Studies in Nursing ■ Figure 1.The Ladder of Abstraction more abstract Philosphical level Particulatedeterministic Interactiveintegrative Unitarytransformative Middlerange theory Microrange theory Grand theory more abstract Theoretical level more concrete Each discipline offers its own constructs for considering theories and theory applications. The Ladder of Abstraction is a construct depicting 3 different levels of ideas regarding a health issue, such as pain. As shown in Figure 1, the Ladder of Abstraction has 3 rungs: the philosophical, theoretical, and empirical rungs—3 different ways to think about and approach a health issue.4 The higher the level on the ladder, the more abstract are the ideas. Hence, philosophical levels of thought are more abstract than theoretical levels, which in turn are more abstract than empirical levels. A brief overview is given later in this section, followed by an example of how it applies to the symptom of pain.4 The philosophical level of thought is a global view, which guides perspectives about health issues. A philosophy is based on and represents well-accepted ways of viewing the world. The theoretical level is expressed as symbols, ideas, and concepts. Middle-range theory resides at this level. The empirical level represents what can be observed (eg, self-reports, behavior, biologic indicators, and personal stories). Empirical thinking is concrete.5,6 At the philosophical level of the ladder, world views are described. For instance, Newman et al describes 3 world views: particulate-deterministic, interactiveintegrative, and unitary-transformative.7 Of these 3 world views, unitary-transformative is most abstract (Figure 1)4 and particulate-deterministic is most concrete. Each world view incorporates values regarding health and healthcare, which guide nurse-patient interaction. The particulate-deterministic world view revolves around cause and effect and is often considered to be the medical model of patient care. The patient is considered as an isolated entity and change in health status emerges from specific causes (eg, taking a drug); the knowledge base is founded in biophysical science. In the interactive-integrative world view, patients are viewed as interacting with (influencing and being influenced by) their surroundings; the Empirical level Questionnaire Physiological indicators Interview Observation Narrative more concrete Reprinted with permission from Smith and Liehr.4 153 PROCEEDINGS the science of unitary human beings.9-11 Middle-range theories are broader than microrange, but they are more focused than grand theories. Middle-range theories emerge at the intersection of research and practice, when theory guides practice, practice generates research questions, and research informs understanding of theory and practice. Importantly, the names of constructs on the Ladder of Abstraction are not intended to indicate that one construct is more important or more correct than another (eg, grand theory is no better than middle- or microrange theory). There are no inherent value judgments attached to constructs, and each serves a purpose in understanding the health experience. For example, a patient who is coding in the emergency room would not benefit from application of self-efficacy theory, but rather demands astute observation of indicators, such as heart rate, blood pressure, and electrocardiogram readings, guided by the particulatedeterministic world view. MIDDLE-RANGE THEORIES To merge the Ladder of Abstraction constructs with symptom content, consider pain through 3 middle-range theories (ascending order of abstraction): symptom management theory, unpleasant symptom 12-15 Symptom management theory, and story theory. theory uses a systematic approach to determine intervention strategies through questions, such as who delivers the intervention, and how and when the intervention is delivered. This approach is taken to affect symptom experience and patient outcomes (eg, selfcare, costs, and functional status). In this model, person, environment, and health state are interrelated (Figure 2).12 Within the symptom experience, evaluation, perception, and response are interrelated. For example, the patients’ perception of pain will affect evaluation (eg, the patient says, “It’s not so bad.”) and response to the symptom (eg, the patient says, “I don’t need pain medication yet.”). These ideas of the symptom management theory (ie, the interrelatedness of patient, environment, and health status) are not intended to be novel, but rather to simply provide a structure for guiding nursing practice decisions when approaching patients experiencing pain. Figure 3 places the symptom management theory on the Ladder of Abstraction.4 The assumptions about symptom management (ie, the philosophical level of 154 Figure 2. Symptom Management Model Person Demographic, psychological, sociological physiological, and developmental Symptom Management Strategies Symptom Experience Perception Evaluation Who? What? Response How? To whom? When? Where? How much? Why? Environment Sympom outcomes Functional status Emotional QOL status Symptom Costs Status Self-care Physical, social, and cultural Health service use Mortality Adherence Health and Illness Morbidity & comorbidity Risk factors, health status, disease, and injury QOL = quality of life Adapted with permission from Dodd et al. J Adv Nurs. 2001;33:668-676.12 Figure 3. Ladder of Abstraction: Symptom Management Assumptions Gold standard is perception of patient Nonverbal patients may experience symptoms Management may be targeted at individual, group, family, work Symptom management is dynamic Concepts Symptom experience Components of symptom management strategies Outcomes Practice Research -Assessment of symptom experience -Functional status -Symptom management via answering questions, such as who, where, what -Emotional status -Quality of life -Morbidity and mortality -Health service use Reprinted with permission from Smith and Liehr.4 Vol. 3, No. 5 ■ August 2005 PROCEEDINGS thought) are the patient’s perception is the gold standard; nonverbal patients may experience symptoms; management of the symptom may be targeted to any or all of the following: the individual, a group, the family, or work environment; and symptom management is dynamic (ie, it is not a static entity that is “fixed”). The concepts of this theory are the symptom experience, the components of symptom management strategies, and the outcomes of symptom management. In practice, symptom management is determined though a series of questions which enable assessment and define the intervention. In research, symptom management can be evaluated by functional status, quality of life, emotional status, morbidity and mortality, and health service use.12 The theory of unpleasant symptoms is slightly more abstract than symptom management theory. Unpleasant symptoms are subjectively experienced indicators affecting performance, which are described specifically by timing, quality, intensity, and distress and are influenced by physiological, psychological, and situational factors (Figure 4).4,13,14 The performance outcomes can, in turn, influence the symptom experience and the factors affecting that experience. Although Dodd et al introduced the idea of symptom clusters into the nursing literature, the theory of unpleasant symptoms actually models symptom clusters.15 The assumptions for this theory (Figure 5) are that persons in varied situations can experience common symptoms, and that symptoms are individual phenomena occurring in family and community contexts.4 The concepts include symptoms, the influencing factors, and performance as an outcome. In practice, unpleasant symptoms are operationalized by symptom assessment, symptom management, and symptom relief intervention. In research, symptoms can be described using a symptom scale, which measures duration, quality, and intensity of the symptom, and the symptom experience. Story theory, the most abstract of these 3 theories, defines “story” as the active process of recognizing self in relation to others through intentional nurse-patient dialogue.16 The story emerges through purposeful conversation between the nurse and the patient about a health challenge (Figure 6).4 For example, a nurse may say, “Tell me about the nausea you’ve been experiencing,” and then really be there to hear about the complex story of the nausea, including what makes it better or worse and who provides the most help in get- Advanced Studies in Nursing ■ Figure 4.Theory of Unpleasant Symptoms Physiologic factors Psychologic factors Situational factors Performance timing intensity distress quality Symptom 1 Key: Symptom 2 Influences intensity distress quality Interacts with Symptom 3 Feedback (reciprocal influence on factor or symptoms) Reprinted with permission from Smith and Liehr4; Lenz et al. Adv Nurs Sci. 1997;19:14-27.14 Figure 5. Ladder of Abstraction: Unpleasant Symptoms Assumptions There are commonalities across different symptoms experienced by persons in varied situations. Symptoms are individual subjective phenomena occurring in family and community contexts. Concepts Symptom(s) Influencing factors Performance Practice Research Assessment of symptom Symptom scale Symptom management Duration, intensity, and quality Symptom relief intervention Symptom experience Reprinted with permission from Smith and Liehr.4 155 PROCEEDINGS ting through it. The purpose of story gathering is to create ease—the feeling of relief when pieces of a story come together to create a bigger picture (sometimes experienced as an “Aha!” moment). The assumptions grounding this theory (Figure 7) are that each person lives in the moment influenced by the present, the past, and the future, and that each person changes as he or she interacts with the world.4,16 Each person also creates and experiences meaning. The concepts that form this theory are intentional dialogue (or purposeful conversation), connecting with self in relation (ie, we are not alone), and creating ease by “putting the story pieces together.” In practice, story theory guides story gathering through approaches, such as a story path or a family tree. In research, story theory relies on narrative as data, enabling analysis through qualitative methods or linguistic analysis.16 As mentioned earlier in this article, no theory is more correct than another. Each theory offers a point of view (or pair of glasses) through which a health situation can be assessed and addressed. Different theories may highlight different pieces of the often complex health situation. Figure 6. Story Theory with Method Connecting with Self-in-Relation Developing story plot Intentional Dialogue Nurse Person Complicating health challenge Creating Ease Movement toward resolving Reprinted with permission Smith and Liehr.4 A CASE HISTORY USING MIDDLE-RANGE THEORIES Figure 7. Laddder of Abstraction: Story Theory The following case history was originally described in reference to using a story path approach to gather a health challenge story.17 It will be used here as a realworld example that enables application of differing theoretical views. Mr. T is a 55-year-old AngloAmerican who woke to “grasping” chest pain. He presented to his cardiologist who performed angioplasty, followed by a coronary artery bypass graft 6 months later. He currently attends cardiac rehabilitation and continues to complain of chest pain, which limits his exercise sessions. He was married for the first time at age 54 years—2 years after the death of his mother. He is currently employed as a construction field manager. When evaluating this patient using symptom management theory, the nurse would ask specific questions to assess the symptom experience and identify approaches for symptom management. To assess the experience, the nurse may ask, “What is the chest pain experience like for you? What is the sensation? How do you judge it? What do you usually do when it happens? What effect does it have on you?” Information regarding these questions could also be gleaned from the patient’s wife. To develop the symptom manage- 156 Assumptions Persons live in an expanded present Persons change as they interrelate with their world Persons experience meaning Concepts Intentional dialogue Connecting with self-in-relation Creating ease Practice Health Story • Story path • Family tree • Present focus Research Health Story • Phenomenological analysis • Linguistic analysis • Case study analysis Reprinted with permission from Smith and Liehr.4 Vol. 3, No. 5 ■ August 2005 PROCEEDINGS ment plan, the nurse may ask, “What will the intervention be? Who will do the intervention? When will the intervention be applied? How will it be performed?” Unpleasant symptoms theory suggests performance will be affected as symptom quality, intensity, timing, and distress are altered, and attention to physiological, psychological, and situational factors will influence the symptom’s quality, intensity, timing, and distress. Evaluating this patient through unpleasant symptoms theory, the nurse would ask questions, such as “What is the chest pain experience like for you?” (listening for quality, intensity, timing, and distress); “Are there other symptoms that happen when you are having chest pain?”; “What contributes to making the pain better or worse?” (physiological, psychological, and situational factors); or “What effect does the pain have on your everyday living?” (performance). Story theory suggests that there is the potential for creating ease as the story unfolds and there is movement toward resolving the health challenge the patient is facing. The nurse evaluating this patient with story theory as a guide would speak with the patient or ask questions, such as “What is hard about living with this pain?” (the complicating health challenge); “Tell me the story of the pain, when did it start?”; “How is the pain now?” (developing a story plot); or “What are you expecting as you look ahead?” (movement toward resolving). When story theory was used in working with this patient, he revealed that he had “just gotten out from under the control” of his mother when she died and now feels controlled by having to take medication for heart problems. He admitted to struggling with the unfairness of his situation (continuing chest pain in spite of intervention), trying to reconcile the life he had envisioned with the one he had now. This information was offered during 4 sessions with the nurse. Although no treatment plan was developed, the pain subsided over time as the patient shared his story with someone who really took time to listen. CONCLUSIONS In brief, none of these theories is more correct than the other, but different theories guide different actions. It is up to the practicing nurse to choose a theory that fits with her own personal values and to let the theory guide action, enabling evaluation from the view with the middle-range theory lens. To make the most of what middle- Advanced Studies in Nursing ■ range theory has to offer, it is essential that advanced practice nurses be skilled in moving up, down, and across the Ladder of Abstraction when studying, practicing, or researching the science of nursing. It is this flexibility and exploration that fosters the development and implementation of new and better ideas about caring for patients to promote health and healing. REFERENCES 1. The Right (and Wrong) Way to Treat Pain. TIME magazine. February 28, 2005. 2. American Pain Foundation Web site. Available at: www.painfoundation.org/page.asp?file=Media/fastfacts.htm. Accessed May 16, 2005. 3. The NIH guide: new directions in pain research I. Washington, DC: GPO; 1998. 4. Smith MJ, Liehr P. Introduction to middle-range theory and the ladder of abstraction. In: Smith MJ, Liehr P, eds. MiddleRange Theory for Nursing. New York, NY: Springer; 2003:1-23. 5. Ford-Gilboe M, Campbell J, Berman H. Stories and numbers: coexistence without compromise. Adv Nurs Sci. 1995;18:14-26. 6. Reed P. A treatise on nursing knowledge development for the 21st century: beyond postmodernism. Adv Nurs Sci.1995;17:70-84. 7. Newman M, Sime AM, Corcoran-Perry SA. The focus of the discipline of nursing. Adv Nurs Sci. 1991;14:1-6. 8. Im E, Meleis AI. Situation-specific theories: philosophical roots, properties, and approach. Adv Nurs Sci. 1999;22:11-24. 9. Parse RR. Human becoming: Parse’s theory of nursing. Nurs Sci Q. 1992;5:35-42. 10. Roy C, Andrews HA. The Roy Adaptation Model: The Definitive Statement. Norwalk, Conn: Appleton & Lange; 1991. 11. Rogers ME. The science of unitary human beings: current perspectives. Nurs Sci Q. 1994;7:33-35. 12. Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33:668-676. 13. Lenz ER, Suppe F, Gift AG, et al. Collaborative development of middle-range nursing theories: toward a theory of unpleasant symptoms. Adv Nurs Sci. 1995;17:1-13. 14. Lenz ER, Pugh LC, Milligan RA, et al. The middle-range theory of unpleasant symptoms: an update. Adv Nurs Sci. 1997;19:14-27. 15. Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. 2001;28:465-470. 16. Smith MJ, Liehr P. Introduction to middle-range theory and the ladder of abstraction. In: Smith MJ, Liehr P, eds. MiddleRange Theory for Nursing. New York, NY: Springer; 2003:167-188. 17. Liehr P, Smith MJ. Using story theory to guide nursing practice. Int J Hum Caring. 2000;4:13-18. 157